#allergy asthma & immunology
Explore tagged Tumblr posts
Text

Allergy Alarm
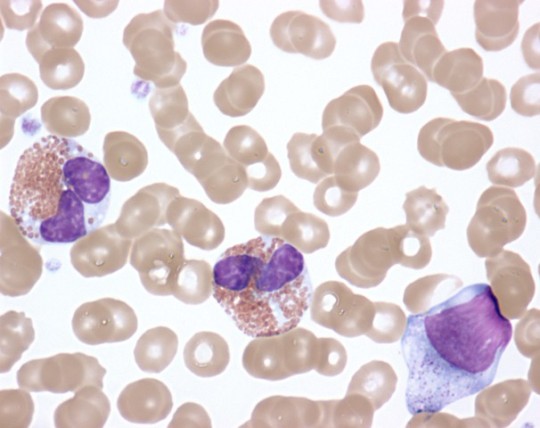
Allergic inflammation in the lungs and airways, such as underlies asthma, is initiated by cooperation of a protein called TL1A with another called IL-33 – together part of an 'alarm system' activated on first exposure to the allergen
Read the published research article here
Image from work by Pauline Schmitt and Anais Duval, and colleagues
Institut de Pharmacologie et de Biologie Structurale (IPBS), Université de Toulouse, CNRS, Université Toulouse III—Paul Sabatier (UPS), Toulouse, France
Image originally published with a Creative Commons Attribution 4.0 International (CC BY 4.0)
Published in Journal of Experimental Medicine, April 2024
You can also follow BPoD on Instagram, Twitter and Facebook
6 notes
·
View notes
Text

Dr. Sohaib Aleem is a board-certified allergy specialist at the AllergyX in Indiana. He holds certifications in Internal Medicine, Allergy and Immunology, and Preventive Medicine, and is a Fellow of the American College of Physicians. Dr. Aleem provides care for both adult and pediatric patients, addressing a wide range of allergy and immunology concerns. He is affiliated with medical facilities such as Community Hospital of Bremen and Elkhart General Hospital, and is proficient in multiple languages, including English, Urdu, Hindi, and Punjabi.
#allergies#allergist#allergy season#allergy specialist#allergy asthma specialists#allergy and asthma specialists#allergy and asthma doctor#allergy asthma & immunology#allergy experts#allergy asthma care#Allergy and Asthma Care
0 notes
Text
Welcome to the well-known center of asthma allergy and immunology Tampa that provides the most effective allergic treatment. To help you manage your symptoms and improve your quality of life, our expert allergists employ cutting-edge diagnostic procedures and treatments. We at “Advanced Allergy and Asthma Care, PLLC” provide personalized treatment strategies based on your specific needs, such as allergy injections and rapid desensitization. Make an appointment as soon as possible to see the difference for yourself! Please follow the link https://www.allergydoc.us/
0 notes
Text
Allergy
Allergy is a condition that arises when the body's immunity starts reacting to common substances such as food, drugs and even dust, pollen, animal dander leading to reactions in the body.
0 notes
Text
Climate Change Worsens Allergy and Asthma Symptoms
Experts Warn of Longer and Harsher Pollen Seasons For Allergy and Asthma Sufferers, Climate Change Means Worse Symptoms and Harsher Seasons If you suffer from allergies or asthma, you may have noticed that pollen season is getting worse and negatively impacting your symptoms. Experts from the American College of Allergy, Asthma & Immunology (ACAAI) warn that pollen season is starting earlier…

View On WordPress
#allergies and asthma management#allergy#American College of Allergy#asthma#Asthma & Immunology#climate change#healthcare#Immunotherapy#National Institute of Food and Agriculture#pollen season
0 notes
Text

Advanced Allergy, Asthma & Immunology Center is offering advanced allergy and asthma center
In Texas and the surrounding regions of US, Advanced Allergy, Asthma & Immunology Center is widely regarded as one of the most advanced allergy and asthma center. We are known to offer one of the most patient-centered, state-of-the-art allergy and asthma treatment for the whole family in a friendly, respectful environment.
#advanced allergy asthma & immunology center#allergy shots for cedar fever#botox treatments san antonio
0 notes
Note
Hi! Sorry to bother you with this - I checked your FAQ and MCAS tag and if the answers are there already I apologize for missing them! But I was wondering if you have a masterpost or similar with basic info on MCAS (what it is, how to figure out if you have it, what to do...) anyway thank you for posting so much about this, I'm learning a lot ^^
Hello! I don't have a list because if I started typing one out, I'd never stop. The Healthline article about it, however, is fairly comprehensive for the basics.
One thing the article doesn't list is that MCAS can also be a source of deep, deep tissue pain (sometimes I swear it's coming from my bones). Some recent research has linked unstable mast cells to fibromyalgia, which is why you'll often find a lot of anecdotal stories online about the two being co-morbid. MCAS can also be more likely in people with EDS or hypermobility spectrum disorder and can sometimes also be a source of dysautonomia. (Honestly, it's a bit chicken vs egg sometimes.)
They may have updated their criteria since the last time I checked, but the American Academy of Allergy and Asthma & Immunology used to list anaphylaxis as a requirement for diagnosis, but that is not true.
Many people experience MCAS without ever going into full anaphylactic shock.
They also used to stipulate that diagnosis was based on elevated tryptase tests, which is not accurate for MCAS. The tryptase tests are meant for diagnosing mastocytosis, which is like the big cousin disorder of MCAS. Most knowledgeable MCAS doctors now diagnose based on a history of symptoms and response to elevated doses of h1 and h2 antihistamines, as well as other mast cell stabilizers.
TMS for a cure has a lot more info, as well as a patient resource portal that includes a list of physicians, support groups, and ER protocols.
I'd highly rec having a read-through at some point.
Hope that helps!
252 notes
·
View notes
Text

Given the soaring temperatures, we all have to be extra mindful of dehydration 💦 Here are the 8 surprising signs of dehydration you need to know about!
1. Bad breath. Your saliva has natural antibacterial properties to keep your breath smelling fresh. When you’re dehydrated, production of this natural “mouthwash” falls — and in a dry mouth, stinky bad bacteria thrive.
2. Carb cravings. When you exercise while dehydrated, your body uses up stored glucose (glycogen) in your liver at a faster rate. Post-exercise, your body will attempt to quickly restock glycogen — leading to carb cravings for sugary foods.
3. Headaches. When you become dehydrated, brain tissue temporarily shrinks from fluid loss and pulls away from the skull. If this sounds painful — it is! Headaches + migraines are signals from the brain that it needs more water.
4. Fatigue and foggy thinking. Dehydration can trigger blood pressure to drop, and slow blood flow to the brain — leaving you feeling fatigued + unfocused. But before you reach for a cup of coffee, consider this: caffeine in coffee is actually a mild diuretic — meaning that you can lose more fluids, making dehydration even worse. Try a mug of energizing ginger tea instead.
5. Constipation: When you’re dehydrated, your body goes on the hunt for extra water sources, which often results in the body “stealing” water from your large intestine — causing serious constipation.
6. Digestive issues. A dehydrated body produces fewer digestive juices, leading to issues like acid reflux, gas, and bloating. Increase your intake of room temperature water — cold water “freezes” enzymes in your gut + constricts your blood circulation, making it more difficult to digest + absorb nutrients from your foods.
7. Worsening of allergy, asthma and arthritis symptoms. Dehydration triggers the body to produce higher histamine levels, which can worsen symptoms of allergies, asthma, rheumatoid arthritis + other immunological disorders.
8. Dark urine. When you’re dehydrated, your body tries to conserve water wherever it can. Check your first morning pee: dark yellow urine is a prime sign that you need more water!
Stay tuned for more healthy hydration hacks 🌿
14 notes
·
View notes
Text
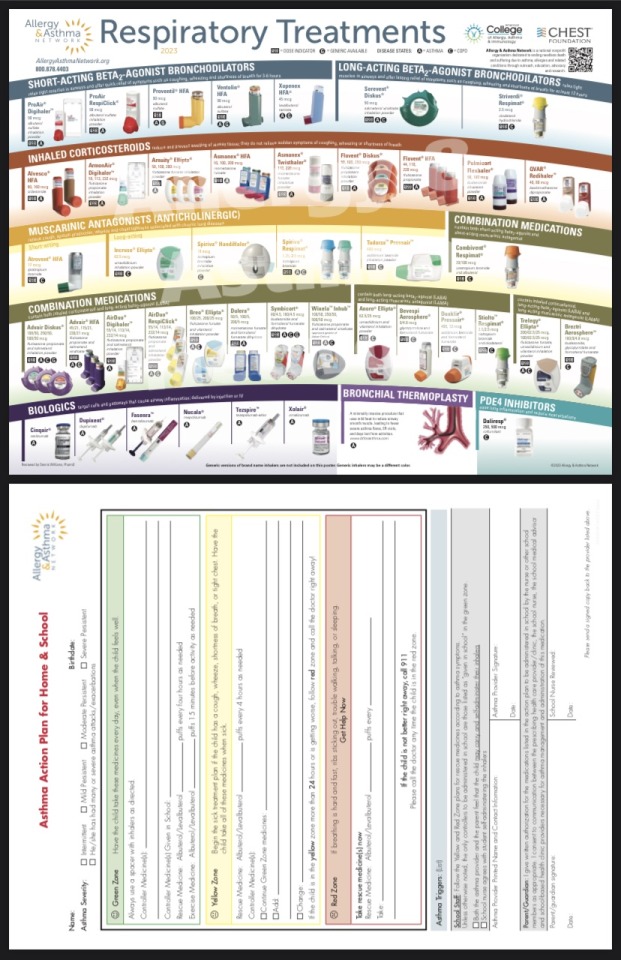
Found this chart super helpful! It's updated as of Feb 2023 from the American College of Allergy, Asthma, & Immunology.
4 notes
·
View notes
Text
Histamine Intolerance Test | FMD
Unlocking Health: Understanding Histamine Imbalance and the Significance of Histamine Testing with First Medical Diagnostics
Introduction

The body naturally produces histamine, which is essential to many physiological functions. Histamine is a versatile chemical that may control immunological response & digestion. On the other hand, an imbalance in histamine levels can result in a variety of symptoms and medical problems. This article examines the effects of histamine imbalance and explains why getting a histamine test is an essential first step in gaining control over one's health.
The Role of Histamine:
Histamine functions as a neurotransmitter and is essential to the immune system. It helps the breakdown of food in the digestive tract by signaling the production of gastric acid. In addition, histamine helps the body react to allergens and controls blood vessel dilatation and sleep-wake cycles.
Impacts of Imbalanced Histamine:
When histamine levels become imbalanced, it can lead to histamine intolerance or sensitivity. This condition is characterized by the body's inability to break down histamine efficiently, resulting in an accumulation of this compound in the bloodstream. The impacts of imbalanced histamine can manifest in various ways, including gastrointestinal issues, headaches, skin reactions, and respiratory symptoms. Conditions such as chronic urticaria, migraines, and irritable bowel syndrome (IBS) are often associated with histamine intolerance.
Gastrointestinal Symptoms:
Imbalanced histamine levels can contribute to digestive problems such as bloating, abdominal pain, diarrhea, and constipation. The digestive tract is highly sensitive to histamine, and its dysregulation can disrupt the normal functioning of the gut.
Skin Reactions:
Histamine is a potent vasodilator, meaning it can widen blood vessels. This can lead to skin reactions like hives, itching, and redness. Individuals with histamine intolerance may experience persistent skin issues that can significantly impact their quality of life.
Respiratory Symptoms:
Histamine's role in regulating blood vessel dilation extends to the respiratory system. Imbalanced histamine levels can contribute to symptoms like nasal congestion, sneezing, and difficulty breathing, particularly in individuals with asthma or allergies.
Migraines and Headaches:
Histamine has been implicated in the development of migraines and headaches. Imbalanced histamine levels can trigger these conditions in susceptible individuals, making it essential to address histamine regulation for effective management.
The Importance of Histamine Testing:
Given the diverse range of symptoms associated with imbalanced histamine, accurate diagnosis becomes crucial for effective management. A histamine test can provide valuable insights into an individual's histamine levels, helping healthcare professionals tailor interventions and treatment plans accordingly.
Personalized Treatment Approaches:
Histamine testing allows for a personalized approach to managing histamine intolerance. By understanding an individual's specific histamine levels, healthcare providers can recommend dietary adjustments, lifestyle modifications, and, in some cases, supplementation with diamine oxidase (DAO), an enzyme responsible for breaking down histamine.
Preventative Health Measures:
For individuals experiencing chronic symptoms that align with histamine intolerance, a histamine test can serve as a preventive health measure. Early detection of imbalances allows for proactive management, reducing the risk of complications and improving overall well-being.
Get Your Histamine Intolerance Test From First Medical Diagnostics
The Histamine Sensitivity Test from First Medical Diagnostics will help you find relief from histamine-related illnesses. Find the source of symptoms such as skin sensitivities, stomach troubles, and headaches. Our accurate test determines your histamine levels and offers customized management suggestions. First Medical Diagnostics is your partner in comprehending and treating histamine sensitivity.
For more information,
Call us at +91 8800929600
Visit us at www.fmdindia.in
#histamine#fmdindia#histamineintolerance#health#wellness#fever#allergy#winterdiseases#sneezing#runningnose
2 notes
·
View notes
Text
Q. What is nonallergic rhinitis with nasal eosinophilia syndrome (NARES)?
.
.
.
.
.
A. Nonallergic rhinitis with nasal eosinophilia syndrome is the most common inflammatory kind of nonallergic rhinitis. Sufferers have high eosinophils on nasal smear but negative skin or serum tests for IgE. It is associated with asthma and may reflect hyperactive nasal mucosal inflammation.
Credit: NIH Image Gallery
#TeachingRounds, #FOAMed, #pulmonology, #allergy, #immunology, #ENT
6 notes
·
View notes
Text
The misleading distinction between illnesses that are ‘physical’ (in other words, real) and illnesses that are ‘psychological’ (and therefore by implication not real) is starkly illuminated by the furore over chronic fatigue syndrome, otherwise known as myalgic encephalomyelitis (ME), post-viral fatigue syndrome or, if you read the tabloid press, yuppie ’flu.
[...]
Ironically, it turns out that the CFS sufferers who believe most strongly in a purely physical explanation have greater difficulty in recovering from their illness. This may be because they fail to confront and deal with the psychological problems that invariably accompany the illness. Evidence to support this conclusion has come from a study conducted by Michael Sharpe and colleagues in Oxford. They found that a form of cognitive behavioural therapy, in which CFS sufferers were helped to re-evaluate their attitudes towards their illness, was of major benefit. More than 70 per cent of CFS sufferers who received the behavioural therapy regained their ability to function normally, compared with a success rate of 27 per cent for sufferers who received only standard medical care.
[...]
Similar attitudes apply to other illnesses which, like CFS, have been tarred with the psychosomatic brush. Asthma and allergies are familiar examples. So too are inflammatory bowel disorders such as Crohn’s disease and ulcerative colitis. The pendulum of opinion has swung violently back and forth over the years. Half a century ago asthma was widely regarded as an essentially psychological illness. Nowadays it is normal to play down the role of psychological and emotional factors and instead focus almost exclusively on its immunological mechanisms and physical triggers, ranging from fitted carpets to car exhaust fumes. In truth, there are good grounds for believing that both immunological and psychological factors play important roles in these diseases. Nevertheless, the overwhelming tendency is to opt for one explanation to the exclusion of the other.
-- Paul Martin, The Sickening Mind: Brain, Behaviour, Immunity and Disease
3 notes
·
View notes
Text
Investigating the potential link between climate change and increasing prevalence of allergies
Introduction
Climate change is a global issue that has far-reaching consequences for the environment and human health. One of the impacts of climate change is the increasing prevalence of allergies. Recent studies have shown that there may be a potential link between climate change and the rising prevalence of allergies. In this article, we will investigate the potential link between climate change and increasing prevalence of allergies.
Understanding the causes of allergies
Allergies occur when the immune system overreacts to harmless substances, such as pollen, dust, or food. The overreaction of the immune system leads to the release of histamine and other inflammatory, which cause the symptoms as itching,, and wheezing. The causes of allergies andial, and include genetic predisposition, environmental factors, and lifestyle factors.
The impact of climate change on allergies
Climate change has far-reaching consequences for human health, including the increasing prevalence of allergies. There are several ways in which climate change can impact allergies:
1. Increasing levels of carbon dioxide: Climate change has led to an increase in the levels of carbon dioxide in the atmosphere. This increase in carbon dioxide has led to an increase in the production of pollen by plants. As a result, there is a greater exposure to pollen, which can trigger allergies.
2. Changes in temperature and humidity: Climate change has led to changes in temperature and humidity levels. These changes can affect the growth and distribution of plants, leading to an increase in the production of allergens such as pollen and mold.
3. Changes in air quality: Climate change can lead to changes in air quality, including an increase in the levels of air pollution. This increase in air pollution can exacerbate allergies, making symptoms worse.
The evidence for the link between climate change and allergies
Several studies have investigated the potential link between climate change and the increasing prevalence of allergies. A study published in the Journal of Allergy and Clinical Immunology found that the increasing levels of carbon dioxide in the atmosphere were associated with an increase in the production of pollen. Another study published in the Lancet Planetary Health found that climate change was responsible for an additional 2.7 million cases of asthma in the United States alone.
What can be done to prevent the impact of climate change on allergies?
Prevention is key when it comes to the impact of climate change on allergies. Some of the ways to prevent the impact of climate change on allergies include:
1. Reducing carbon emissions: Reducing carbon emissions is essential to prevent the impact of climate change on allergies. This can be achieved through the use of renewable energy sources, such as solar and wind power.
2. Improving air quality: Improving air quality is essential to prevent the exacerbation of allergies. This can be achieved through the reduction of air pollution and the implementation of measures to improve indoor air quality.
3. Developing allergy management strategies: Developing allergy management strategies is essential to cope with the increasing prevalence of allergies. This can include the development of new medications, the use of immunotherapy, and the implementation of measures to reduce exposure to allergens.
Conclusion
In conclusion, the increasing prevalence of allergies is a global health issue that is linked to climate change. Climate change has far-reaching consequences for human health, including the impact on allergies. The evidence suggests that the rising levels of carbon dioxide, changes in temperature and humidity, and changes in air quality are contributing to the increasing prevalence of allergies. Prevention is key when it comes to the impact of climate change on allergies, and this can be achieved through reducing carbon emissions, improving air quality, and developing allergy management strategies.
2 notes
·
View notes
Link
2 notes
·
View notes
Text
Postdoctoral Fellow - Moltke Lab University of Washington See the full job description on jobRxiv: https://jobrxiv.org/job/university-of-washington-27778-postdoctoral-fellow-moltke-lab/?feed_id=89944 #allergies #asthma #immunology #mucosal_immunology #parasitology #ScienceJobs #hiring #research
0 notes