#What PCV in blood test
Explore tagged Tumblr posts
Text
What is PCV in Blood Test | PDW Blood Test, Dengue, Home Collection
What is PCV in Blood Test?
Packed Cell Volume (PCV), also known as hematocrit, is a blood test that measures the proportion of red blood cells in your blood. Red blood cells are crucial for carrying oxygen from your lungs to the rest of your body. Consequently, understanding PCV is essential for diagnosing and monitoring various health conditions.
Understanding the Importance of PCV in Blood Tests
PCV is a critical parameter in a complete blood count (CBC) test. Additionally, it helps in diagnosing conditions like anemia, dehydration, and polycythemia. Moreover, an abnormal PCV level can indicate underlying health issues that may require further investigation.
How is the PCV Blood Test Conducted?
The PCV test is simple and usually performed alongside other tests in a CBC. First, a sample of your blood is taken and placed in a centrifuge, which separates the blood components. Consequently, the red blood cells settle at the bottom, and their volume is compared to the total blood volume.
Normal PCV Ranges
The normal PCV range varies by age and gender:
Men: 40.7% to 50.3%
Women: 36.1% to 44.3%
Children: 32% to 44%
Interpreting PCV Results
High PCV levels might indicate dehydration or disorders like polycythemia vera, while low levels could signify anemia or bleeding disorders. However, it is important to discuss the results with your healthcare provider to understand what they mean for your health.
What is PDW in Blood Test?
Platelet Distribution Width (PDW) measures the variability in the size of platelets. It is a part of the CBC test and provides insight into platelet production and function. Abnormal PDW levels can indicate conditions like thrombocytopenia or thrombocytosis.
Why is PDW Blood Test Important?
PDW is crucial for diagnosing platelet disorders, which can affect blood clotting and lead to conditions like excessive bleeding or clot formation. Understanding your PDW can help in managing these conditions effectively.
Conducting the PDW Blood Test
Similar to the PCV test, the PDW test involves drawing a blood sample and analyzing it in a laboratory. The variability in platelet size is measured, providing valuable information about your platelet health.
Interpreting PDW Results
A high PDW can indicate a higher variation in platelet size, often associated with platelet production issues or disorders. A low PDW suggests uniform platelet size, which is generally normal but must be interpreted in conjunction with other platelet indices.
Understanding Dengue Blood Test
Dengue is a viral infection transmitted by mosquitoes. The dengue blood test detects the presence of the virus or antibodies against it in your blood, helping diagnose dengue fever early and accurately.
Importance of Dengue Blood Test
Early detection of dengue through blood tests is crucial for timely treatment and preventing complications. Dengue can cause severe symptoms and potentially life-threatening conditions like dengue hemorrhagic fever and dengue shock syndrome.
Types of Dengue Blood Tests
NS1 Antigen Test: Detects the virus in the early stages of infection.
IgM and IgG Antibody Tests: Detect antibodies produced in response to dengue infection, useful in later stages or past infections.
Conducting the Dengue Blood Test
A blood sample is taken and analyzed in a laboratory. The type of test chosen depends on the stage of the infection and the symptoms presented.
Interpreting Dengue Test Results
Positive results indicate the presence of the dengue virus or antibodies. However, further tests may be required to confirm the diagnosis and, additionally, to assess the severity of the infection.
The Convenience of Blood Test Home Collection
Blood test home collection services offer a convenient and stress-free way to get your blood tests done. Moreover, this service is particularly beneficial for individuals with mobility issues, busy schedules, or those preferring the comfort of their home.
Benefits of Blood Test Home Collection
Convenience: Avoid long waits at diagnostic centers.
Comfort: Get tested in the comfort of your home.
Safety: Reduces exposure to potentially infectious environments.
How Blood Test Home Collection Works
You can book a home collection service through a diagnostic center's website or app. Then, a trained phlebotomist visits your home at the scheduled time, collects the sample, and subsequently delivers it to the lab for analysis.
Ensuring Accuracy and Reliability
Home collection services maintain strict protocols to ensure sample integrity and accurate test results. Furthermore, the collected samples are handled with care and transported to the laboratory under controlled conditions.
Choosing the Right Service
When selecting a home collection service, it is essential to consider factors such as the diagnostic center's reputation, the phlebotomist's training, and customer reviews. Additionally, these considerations help ensure you receive high-quality and reliable services.
Conclusion
Understanding what PCV in a blood test means and its importance is crucial for your overall health. Additionally, alongside PCV, knowing about PDW, dengue blood tests, and the convenience of blood test home collection can significantly enhance your healthcare experience. Therefore, for comprehensive diagnostic services, including home collection, H.R. Diagnostic is your trusted partner. In conclusion, stay informed, stay healthy!
Read More…..
Author Bio: Simi Gajala has been working in digital marketing since 2018, amassing 6 years of experience. Currently Working as a Digital Marketing Executive at H.R. Diagnostics. Simi specializes in SEO, SMO, Google Ads, Meta Ads, and blogs & content writing, Boosting Brands, Increasing Visibility, And Enhancing Online Performance.
1 note
·
View note
Text
Exploring the Packed Cell Volume (PCV) Test: Procedure, Results, and Clinical Implications
The Packed Cell Volume (PCV) test, also known as hematocrit, is a common diagnostic tool used in medicine to measure the proportion of blood volume occupied by red blood cells (RBCs). This test provides valuable information about a person's overall health and helps in diagnosing various medical conditions. Understanding the PCV test, its significance, and interpretation is essential for both healthcare professionals and patients alike.
What is PCV?
Packed Cell Volume (pcv), and it refers to the volume of red blood cells in a given volume of blood after centrifugation. It is expressed as a percentage of the total blood volume. For example, a PCV of 40% means that 40% of the blood volume consists of red blood cells, while the remaining 60% comprises plasma and other blood components.
Importance of PCV Test:
The PCV test is crucial in assessing the oxygen-carrying capacity of the blood. Red blood cells contain hemoglobin, a protein that binds to oxygen and transports it to various tissues and organs throughout the body. A decrease in PCV indicates anemia, a condition characterized by low levels of hemoglobin or fewer red blood cells. Conversely, an increase in PCV may suggest dehydration or certain medical conditions such as polycythemia vera, a rare blood disorder characterized by the overproduction of red blood cells.
Indications for PCV Test:
Healthcare providers may order a PCV test for various reasons, including:
1. Evaluation of anemia:
A low PCV may indicate different types of anemia, including iron deficiency anemia, vitamin deficiency anemia, or hemolytic anemia.
2. Monitoring of blood disorders:
Patients with blood disorders such as polycythemia vera or thalassemia require regular PCV tests to monitor their condition and response to treatment.
3. Assessment of hydration status:
Dehydration can cause an increase in PCV due to the hemoconcentration of blood.
4. Preoperative assessment:
PCV levels are often checked before surgery to ensure adequate oxygen-carrying capacity and overall health status.
Procedure for PCV Test:
The PCV test is typically performed as part of a complete blood count (CBC). A small sample of blood is drawn from a vein, usually in the arm, using a needle and syringe or through a finger prick. The blood sample is then placed in a special tube and centrifuged at high speed to separate the cellular components from the plasma. The PCV is calculated by measuring the height of the packed red blood cells relative to the total height of the blood column in the tube.
Interpretation of PCV Results:
The interpretation of PCV results depends on various factors, including age, sex, altitude, and underlying health conditions. In general, a PCV within the normal range (usually 40-50% in adults) is considered normal. However, deviations from the normal range may indicate underlying health issues:
1. Low PCV (Anemia):
A PCV below the normal range suggests anemia, which may be caused by factors such as iron deficiency, vitamin deficiencies, blood loss, or underlying medical conditions affecting red blood cell production or lifespan.
2. High PCV (Polycythemia):
An elevated PCV may indicate dehydration, lung disease, smoking, or conditions such as polycythemia vera, where there is an abnormal increase in red blood cell production.
Conclusion:
The PCV test is a valuable tool in the diagnosis and management of various medical conditions, particularly those affecting the blood and oxygen-carrying capacity. Understanding the significance of PCV results and their interpretation is essential for healthcare providers to make accurate diagnoses and formulate appropriate treatment plans. Additionally, patients can benefit from knowing about the PCV test and its implications for their health and well-being. Regular monitoring of PCV levels, along with other relevant tests, can help ensure timely intervention and optimal management of underlying health issues.
0 notes
Text
Complete Blood Count (CBC) Test Price in Jammu
Introduction
A CBC test, known as a complete blood count analysis, provides crucial insights into the different types of cells present in your blood. This test aids healthcare providers in evaluating general health and diagnosing specific symptoms or conditions like anemia and infections. Additionally, it helps determine the need for further investigations.
This comprehensive test examines various blood cell parameters such as red blood cells, white blood cells, and platelets. In addition to aiding in the diagnosis of different conditions, it helps assess the effectiveness of treatments and medications.
Test Criteria
To determine your eligibility for a CBC test in Jammu or any other location, consider the following:
Eligibility for CBC Test
Suitable for individuals of any age, gender, or demographic to evaluate general health.
Useful in diagnosing health conditions like infections, anemia, blood cancers, and more.
Recommended if you experience symptoms such as easy bruising, fatigue, signs of bleeding, infections, or inflammation.
Prescribed when a disease affecting blood cells or related parameters is suspected.
Utilized to assess the effectiveness of ongoing treatments like radiation or anemia management.
Why Take the CBC Test?
Consider taking the CBC test for the following reasons:
As part of your routine health checkup
To determine the cause of fatigue, weight loss, or fever
To check for anemia or abnormal bleeding
In the case of infections or during pregnancy
To monitor your response to certain drugs or treatments like radiation
Prior to undergoing surgery
To diagnose blood diseases such as leukemia or chronic inflammation
In many other health conditions
What are the Benefits of the CBC Test at O-Lab?
At O-Lab, we offer tailored test packages to cater to individual needs. Our lab ensures quick results with a high level of accuracy. With the best CBC test price in Jammu, we provide convenient options such as home collection and walk-in services. By opting for our accredited lab, you can benefit from early detection of various health conditions, facilitating timely and appropriate treatment. Our trained staff and phlebotomists prioritize your safety, comfort, and reliability throughout the testing process. Feel free to reach out to us for further information.
Preparation
No special preparation or fasting is required for the CBC test. However, if you are undergoing other tests that necessitate fasting, such as LFT or lipid profile, fasting may be necessary.
Test Parameters
The CBC test includes essential parameters that vary slightly based on the lab's methodology. Here are the important parameters typically included:
Haemoglobin (Hb)
RBC (Red Blood Cell) Count
WBC- TLC (Total Leucocytes Count)
Absolute Basophil Count, blood
Absolute Eosinophil Count, blood
Absolute Lymphocyte Count, blood
Absolute Monocyte Count, blood
Absolute Neutrophil Count, blood
Neutrophils
Eosinophils
Lymphocytes
Monocytes
Basophils
MCH (Mean Corpuscular Hemoglobin)
MCHC (Mean Corpuscular Hemoglobin Concentration)
MCV (Mean Corpuscular Volume)
MPV (Mean Platelet Volume)
PCV Hematocrit (Packed Cell Volume)
PDW (Platelet Distribution Width)
RDW (Red Cell Distribution Width)
Platelet Count/Thrombocyte Count
0 notes
Photo










SAYING GOODBYE TO CHARLEY
Charley became very sick two months ago, shortly after his birthday. One month ago, the doctors said that we had entered the hospice care phase of his illness. One week ago last Wednesday Charley had his kidney levels checked. They were terrible. He was no longer eating or drinking. A week ago last Tuesday, we learned he had a very serious eye injury requiring lengthy and unpleasant treatment. He had been doing ok, all things considered, until Tuesday a week ago. But the 24 hours after that were miserable for him. We (the vet and myself) put him to sleep around 7 pm Wednesday, August 4, 2021. I held him and he wasn’t scared as it happened. He went quickly and peacefully. I spent a very long time alone with him before and after. Some of his friends and family called and texted to wish him goodbye. It was about as good as something like that can be. He was very brave. I miss him so much. My beautiful boy.
Charley was diagnosed with kidney disease about three years ago and we managed his disease with a low-protein kidney diet. Typical life expectancy at the time of his diagnosis was about a year and we were lucky to have over three additional years together, instead of just one. Although he had been slowing down a bit in recent years and still having adventures, our walks were becoming a bit shorter and our adventures a bit less wide-ranging. He also had arthritis, which he took canine CBD for.
Not long after his most recent birthday, his kidney disease started catching up with him. He’d been gradually losing weight as part of the disease, which causes muscle loss. He then started losing a lot of weight more rapidly and having mobility issues — sometimes having trouble getting up or sometimes falling down.
Two months ago, he spent two nights at the hospital due to his kidney levels and rapid weight loss. Two days after getting out of the hospital he suffered a stroke, but recovered. The following day after his stroke, he had two seizures within an hour of one another (the second was pretty severe). After that, he began taking an anti-convulsant every 8 hours. He also took a blood thinner to reduce the likelihood of further strokes, and blood pressure medicine for his high blood pressure. He took an anti-nausea pill to counter the nausea from the kidney disease. And he took an appetite stimulant (Entyce), which is what really kept him eating.
One month ago, his vet said we were entering the hospice care phase of his illness. She estimated he probably had weeks remaining, not months, but more than days left.
I began doing everything I could to keep him eating, feeling comfortable and enjoying the remaining time we had. He’d been eating, drinking, peeing and pooping. He needed my help to walk and stand as his mobility had become increasingly limited. He eventually no longer had use of his back legs, but could hold himself up with his front legs. He got to the point where he needed my help to do everything, including eating, drinking, peeing and pooping. He could move his head and wiggle around a little as well as move his front legs back and forth a bit as he lay on his side, but was unable to get up or move from one place to another without help. I gave him 100ml subcutaneous fluids daily at home. And he made frequent trips to the vet for rechecks and to make sure he was doing ok and to address any issues that arose. He had bed sores that the vet wrapped with a bandage, which needed to be changed every few days. The sores were healing. He was anemic, but taking a weekly injection to get his red blood cells up into the normal range. He’d been seeing a group of doctors at the veterinarian practice that he’s been going to his entire life.
3 1/2 weeks ago, he was eating very little for a couple days but we switched foods and he began eating well again and he continued to eat well until the last day or so. His weight started to stabilize around that time and he did not lose too much more weight, aside from some further gradual weight loss. Regardless, he was emaciated (just under 8 pounds — half his healthy weight). Despite all this, he seemed mostly content given his severe limitations. He did still enjoy eating, being with me, he liked being touched, having his ears rubbed, getting a massage and being stroked and petted. Even though he could no longer walk, I would make sure to exercise his legs every day. He also enjoyed lying on my lap and and being sung to, where he would fall asleep.
When he needed something, he would “talk” or complain with a grumble or an occasional whispery bark if it was more urgent. That usually meant he needed to pee, or had peed or needed a drink of water or something similar. It was not always easy to tell what it was that he wanted and it could take a while to figure out what it was.
In the hospital, one of the technicians shaved the hair around Charley’s face, which I was not happy about, but it was slowly growing back. He had also been losing his hair, which was coming out in clumps when he visited the groomer. So he may look a bit different in some of his most recent pictures.
It was very difficult to see him deteriorate so quickly. But until the last 24 hours, he still enjoyed eating, resting, and interacting with people. He didn’t try to hide or avoid contact.
Charley treasured your friendship and appreciated all the likes, kind comments and the fact that he was able to meet so many of you in person — some from all over the world and some more than once.
He loved you very much.
#charley lhasa#lhasa apso#dog#illness#kidney disease#city vet care#city veterinary care#east flatbush#brooklyn#upper west side#manhattan#nyc#iphone se
25 notes
·
View notes
Text
Cat Facts: Why’s this Cat Vomiting?

Like most of my posts, this is coming more from a veterinary student/pre-vet education perspective, but hopefully some owners that follow me can get some useful info from this!
Unsurprising to most vet students, there’s about as many reasons for vomiting as there are diagnoses in general. We’re going to attempt to narrow that down a bit, break them into categories which makes it more useful for diagnostics and relevant differentials.
First off, you have to differentiate vomiting from regurgitation.
Vomiting: nausea (drooling, lip licking, swallowing, depression/restlessness), abdominal muscle contraction, contains bile/digested blood/digested food
Regurgitation: no nausea, no abdominal contractions or bile, presence of undigested food in a tubular shape.
Once you’re sure it’s actually vomiting, you’ll need to differentiate it into acute or chronic, as well as emergency/non-emergency. Acute will be in the last few days or day of presentation, often multiple times in the same day, and will often present as more “sick” than the chronic vomiter.
In chronic cases, the vomiting is usually more than 2 times a month and has been going on for months to years. Chronic vomiters can be “apparently healthy” and the vomiting only brought up at a wellness check or prompted by the vet/nurses and the owner didn’t think to bring it up because “cats just vomit, and they seem fine other than that.” History can help a lot! If there’s an acute case, and the cat has access to toxic substances, a habit or likelihood of eating foreign objects (hair ties, string, q-tips, etc), or has had a recent change in diet, that could lead you immediately to the most likely cause and the most appropriate next steps. Acute vomiting generally has fewer causes or at least more obvious causes, and next steps generally include abdominal radiographs or triage/supportive care if indicated. Physical exam can locate a linear foreign body that’s anchored to the underside of the tongue.
So, what if that doesn’t help? That’s when you start your baseline diagnostics! CBC/Chem/UA can rule in or rule out a lot of potential causes for vomiting:
Diabetes: hyperglycemia, glucosuria, ketonuria, low USG
Liver disease: hyperbilirubinemia, decreased BUN, increased liver enzymes, bilirubinuria
Renal disease: increased BUN/creatinine, low USG
Hyperthyroidism: increased T4, increased liver enzymes (ALP, ALT), mild increase in PCV, low USG
Electrolyte/acid-base derangements: Na, K, Cl, Ca, pH, bicarb, tCO2
Eosinophilia: parasites, IBD, hypereosinophilic syndrome, mast cell tumors
Neutrophilia: gastroenteritis, neoplasia
Neutropenia: salmonellosis, retroviruses
Hemoconcentration: dehydration
Anemia: chronic disease, GI blood loss
Fecal may also show parasites, and FeLV/FIV positive snap test might be supportive of vomiting from a FeLV/FIV related illness
Secondary diagnostics beyond bloodwork and urinalysis would be the next step after that. Radiographs may show abnormalities in organ size/architecture (small kidneys, enlarged liver), foreign bodies, GI obstruction, or masses.
Ultrasound is the diagnostic of choice for **chronic vomiting and normal bloodwork**. It can reveal thickening of the stomach/small intestines, wall layer changes, and/or enlarged lymph nodes. It can also show or allow better examination of abdominal masses, or the presence of free fluid.
fPLI may be indicated if pancreatitis is suspected, but may be normal in chronic pancreatitis cases. Heartworm testing if the cat lives in an endemic area, after other causes have been ruled out.
Intestinal biopsy and histopathology is recommended in cases of chronic vomiting with GI thickening seen on ultrasound. This will differentiate between IBD and lymphoma, which cannot be done without the histopath! Though presumptive and empirical treatment may be considered in cases of financial concern. IBD is often in younger cats and lymphoma in older, however that’s simply a generalization and not a hard and fast rule. IBD and lymphoma are the two most common causes of chronic vomiting in cats. Exploratory surgery and full thickness biopsies is preferred over endoscopic biopsy, as you can retrieve intestinal samples from more than just the duodenum, the samples will be higher quality for your pathologist, and you can determine the staging of the lymphoma (if that’s the cause).
What should I tell owners to keep a look out for? 2x a month or more vomiting, INCLUDING HAIRBALLS, is abnormal and justifies an ultrasound study. Cats should in theory be able to process hair since they evolved to groom their fur (a bit more leeway is given to long-haired cats since that’s a genetic mutation we’ve selected for), and vomiting hairballs regularly is suggestive of hypomotility of the GI tract.
The only exception to this is eating grass and vomiting, as grass is irritating to the stomach and can cause vomiting, but is more or less harmless on its own.
Due to this being a very wide topic I didn’t go much into specifics, but I can if you all are interested in any specific parts of this!
232 notes
·
View notes
Text
Loaf update (This one's a rollercoaster)
Since Loaf's recent emergency, a lot has happened! The vet who told us Loaf had a few days left to live has been let go from the practice. He was wildly wrong about her hemoglobin levels, and if he had given that advice to a different person, they might have jumped the gun and put their cat down. I had multiple outsiders telling me to do the same thing when I first posted asking for donations to cover her emergency care. So what happened? As soon as we reached the goal amount of donations, Preston and I took her to the 24 hour vet that was going to do her blood transfusion (different from her regular vet). That night they decided to do some chest x-rays to see if there was any other cause for her shallow rapid breathing. Something the other vet failed to even suggest to us. Chest x-rays revealed pretty healthy lungs other than signs of her lifelong asthma, but also an enlarged heart with a little fluid around it. A blood transfusion wasn't safe to do, they were shocked that was even suggested! At 18% PCV (hemoglobin) she was definitely anemic, but cats that go as low as 8% or 9% are candidates for transfusions. She just wasn't there. After getting a second opinion from their radiologist, we confirmed that a blood transfusion was definitely not the correct treatment for Loaf. We needed to treat with a bone marrow stimulant to up her PCV. I very nearly didn't get the medication in time because of her first vet's incompetence and some technical problems with our pharmacy, but she did get it and is getting weekly injections at home now! We will retest her PCV in a week to make sure it's working. Loaf's shallow rapid breathing was likely caused by a blood clot, since anemic cats can often get clots (yet another thing the original vet failed to inform us of). So she was put on a blood thinner, and within a few days here breathing evened out. We consulted with a cardiologist who agreed with the diagnosis and treatment. No clots showed up on imaging, but they often don't. Her breathing rate is now even and healthy, especially for an asthmatic cat! But Loaf wasn't out of the woods yet. Several days into her blood clot treatment, Loaf went blind... We rushed her to the 24 hour vet once more. They found she had high blood pressure (a side effect of her kidney disease), and as a result both her retinas had partially detached. Preston and I were heartbroken. We were sent home with a blood pressure medication prescription, and some advice on how to help her adapt. Apparently this is pretty common, and cats tend to adapt pretty fast so long as you don't move the furniture around. Loaf had been without sight for a little over 36 hours, and she was already navigating around the house with ease, eating a bunch, and seemingly doing just fine other than a little constipation. She's just incredible, I'm constantly amazed by her resilience. We gave her the first dose of her blood pressure medication the next day as soon as I could get it, and made some changes around the house to remove some possible hazards for her. The next day, Preston shook me awake yelling "She can see, Loaf can see!" He had walked into my office, found her on her windowsill shelf (which she had been avoiding while blind), and called her name. When she turned around she looked right at him with normal looking eyes, and gave him a big long slow cat blink! He did some quick vision tests much to her annoyance, and she indeed had her vision back! At least mostly, we think she still has some amount of vision impairment. Apparently there's a small chance that if you treat blood pressure related retinal detachment fast enough, their vision can come back partially, or all the way. And goddamnit, we hit that small chance!!! How is she now? Loaf now has three new permanent medications to her routine; a blood thinner, a blood pressure medication, and a bone marrow stimulant. Because of our quick action and your donations, she will not suffocate from within from anemia, her blood clot situation won't kill her, and she is not blind. We spent that donation money on several blood tests, 2 emergency vet visits, xrays, ultrasounds, specialist consultations, two cheap medications and one VERY expensive medication ($400 for a 1ml vial). Her kidney disease continues to progress, so while all this won't save her kidneys, it HAS given her more time, more comfort, and less pain. I know a lot of people were very unhappy with me asking for donations to help her, or very unhappy that I didn't choose to euthanize her. But my duty is not to those people, it is to HER and her alone. I will continue to give her every chance possible, and when she is ready I will help her pass so she doesn't suffer. That could be in a few weeks, or a few months. I'll just keep doing everything I can for her, and give her the best life possible. So for now, YOU GUYS SAVED HER. THANK YOU ALL SO MUCH, FROM THE BOTTOM OF MY HEART!!!
164 notes
·
View notes
Text
Veterinary Storytime: Dogs and Cruelty
There are not many veterinary clients I have genuinely hated, but there was one in my first job that definitely qualified.
While I have certainly learned to be more understanding and empathetic over the course of my career, even with the benefit of hindsight I cannot come to forgive this human’s intentions and selfishness even all these years later.
The last week of December is a busy time when a vet practice offers its own after hours. You don’t really close, you just take on less routine surgery that can be put off for a couple of weeks. This is because the general public want to save their money for Christmas, and other smaller practices in the area do close and fob off all their urgent cases to you, so you are extra busy with harder things.
We were on after hours services only on the 25th and 26th of December, and I was working them with one other vet to share the load. We were only seeing cases that couldn’t wait, and this was one of them.
The dog in question was a little fluffy thing that had been sick with quite a while. Her primary problem had been heart disease, but now she ‘hadn’t eaten for days’ which meant the owner now decided she was an emergency on Xmas day, as they do.
And this dog was indeed very sick. She was on frusemide to manage her chronic heart disease, among other things, and he frusemide had done what frusemide does, and was now causing chronic kidney failure as well.
She was dehydrated, vomiting, struggling to breathe as her lungs were slowly filling with fluid and generally looked miserable. But the owner didn’t want to euthanise, they wanted to treat.
This was against medical advice for a number of reasons.
Firstly, the dog was actively suffering with two chronic illnesses which would not be cured, only managed.
Secondly, the treatment for those two conditions were basically opposite to each other.
To treat the chronic kidney disease, we needed to rehydrate the dog with lots of intravenous fluids and absolutely no frusemide.
To treat the heart disease, we needed to dehydrate the lungs (and the dog) and use lots of frusemide to do that.
And we were not staffed 24 hours as a critical care hospital. The only blood tests I could run in the clinic were glucose, PCV and Total protein. I had no way of monitoring urea without sending blood to the local helpful human hospital, or potassium. Nor could I afford to sit cage-side by this patient all night, which was Christmas night, by the way, to monitor it while we tried to both rehydrate and dehydrate it at the same time (which is pretty darn close to a physical impossibility by the way), and in the meantime this dog is suffering.
But they wanted to treat. And at that stage I did not have the will or stubbornness that I have now to put my foot down. They wanted to treat. And they wanted a phone update every 2 hours through the night.
I did it. I came in, checked her every two hours, and called them with an update more or less on time unless I was seeing another patient (and they flipped out on the phone when I was 20 minutes late with an update because I was seeing another patient at the time) and every time I called, I recommended euthanasia.
The dog had two organs failing, and they wanted to take her home or continue struggling to treat something that would never get better instead of letting her pass.
By morning we were all exhausted - that’s what happens when you demand 2 hourly updates all night - and the dog was no better. She was probably worse, but the owner decided to fixate on the fact that she hadn’t urinated overnight as evidence that something was ‘wrong’. Never mind the heart and kidney failure.
So I performed an ultrasound on her bladder, only to find a liver tumor next door.
This was still not enough. Heart failure, kidney failure, a liver tumor and actively suffering with no response to treatment and they still refused to euthanize.
I gave up. I’d only been working for a year and I was ready to euthanize this dog without consent, but the owners were already there and making noise about taking her home. If she hadn’t been hooked up to a drip, they probably would have snatched her and left already.
I handed the case over to the other vet working that day. I had too, I was too tired to be nice any more. It took them another hour to finally get consent for euthanasia, and I don’t think she was particularly nice about it at this stage either. But she had to be.
The owners wanted to continue this cruelty, and they were dragging us into it as well, beyond what was a reasonable attempt at preserving life.
And I have to say, they hated us for not letting them have their way. And they argued about the bill for months later.
This story was chosen by my Patreon supporters, and viewed early! Thank you for your ongoing support!
437 notes
·
View notes
Text
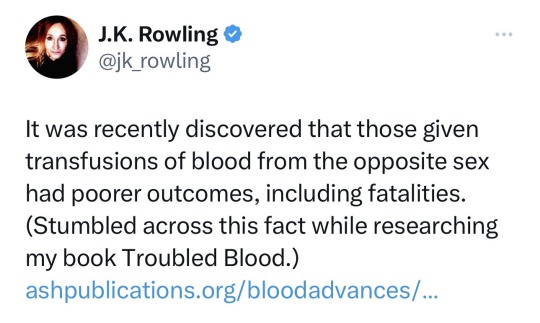
You know what, this is actually really annoying me, so I went and read the paper. Which is clearly more than JKR did
Bear in mind, this is not my area of expertise, and so there will be a lot of nuance to the subject that I won’t understand. But from when I read of it, these are the things that contradict what she is saying
1. The sample sizes are tiny. You can’t make a generalisation based on a study that has a sample size of between 80-130 in each sample group and then apply it to everyone in the world.
2. It only looked at a very specific sample population (critically ill ICU patients receiving a blood transfusing at a PCV of 7). You can’t take a small sample size, from a small group, and apply it to everyone in every situation.
3. Nowhere in the article does it state that “blood from the opposite sex has poorer outcomes, including fatalities”. There is a statistically significant increase in mortality rate in males receiving female blood. So higher fatality rate in men receiving non-male blood products. Those other poorer outcomes? They weren’t tested for, or they didn’t always back that up (for example, there was a higher incidence of AKI in females receiving female blood).
4. This is one study, and other studies are contradicting each other. This study found it was only female-to-male blood transfusions that showed higher mortality rates, another study found that it was just male-to-female transfusions that had worse outcomes. Other studies showed no difference at all. The paper itself acknowledges this mismatch and uses it as proof that further investigation is required to figure out if there is a difference, and if there is, what is driving that
5. The paper also acknowledges that even if there is a difference, that there are likely to also be other contributing factors
And to bring up something to directly relate it to JKR, there is no mention anywhere of factoring in trans people in this, and so it is so out there to even try to bring that into it (which she was absolutely trying to do).
IF there is a difference, we don’t know what causes that difference. Is it hormonal? If a trans woman is on estrogen or a trans man is on testosterone, would that counteract it? There is literally no way for us to know that right now, the study hasn’t been done.
(here is the paper for anyone interested. I think it’s the one she read, but I refuse to go on her twitter to look for it so who knows https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9198942/ )
The sequel ‘Skull Measuring for beginners’ is scheduled for 2025.
35K notes
·
View notes
Text
1. Heart in a woodchipper
9th May 2019
A quick word about Toby (before getting into his journey):
Toby is a fighter. He lived for 14 years, of which 1 year and 5 months was a battle with canine lymphoma. He went through various types of chemotherapy, a very strict diet with various boosters and supplements, hyperbaric oxygen therapy, and countless visits to the vet which he hates. Before lymphoma, Toby was the perfect picture of health. Everyone who met him thought he was at most 7 yrs old, when he was in fact 12. We had so many good laughs when children would call out to their mom or dad saying “Look at that puppy!” or “So cute… i want a puppy too”
He brought out the best in us through the 14 wonderful years he gave us. We love him so much and hope we’ll see him again someday in heaven.
Christmas 2017 – Toby is 12.5 yrs old and weighed ~8kg here and had the appetite and energy of a champion beardog!

“Raaaarrrr... I hate taking photos.. but i love you guys so i will put up with this.”
Nov 2017: Took Toby to the vet close by our place at Barkway Medical, due to eye discharge. The vet gave some eyedrops but noticed that Toby’s lymph nodes were swollen in both the submandibular (below the jaw, neck region) and popliteal (hind legs, behind the knees). Antibiotics prescribed. perhaps it was an infection. After a week, Toby’s lymph nodes continued to swell. Took him back for a blood test where lympocytes and neutrophils were off the charts. Doctor suggested that we check for canine lymphoma either by biopsy which means extracting an entire lymph node, or fine needle aspirate which is less invasive. We opted for FNA and hoped for the best. The test results confirmed that Toby was dealing with canine lymphoma.
At this point, it hit us really hard. Like our hearts were thrown into a woodchipper, shredded and spat out unceremoniously. Toby is a huge cornerstone of the life Junie and I built together and we love him like our own child. We reeled from the news and started googling the shit out of canine lymphoma. The prognosis for multicentric lymphoma (B-cell or T-cell) is very poor: 1~2 months if left untreated, ~6 months on average if prednisone (a type of inexpensive steroid with little side effects) is used, and on average 1 year ~14 months (for B-cell) using chemotherapy e.g. CHOP protocol (cyclophosphamide, doxorubicin, vincristine, prednisone). We were instantly thrown into a world of anguish, but wanted to believe that Toby, with help from his family, could fight this.
The doctor at Barkway tried to refer us elsewhere as they were not equipped to deal with dogs with cancer. He also mentioned that one of his staff was pregnant and for her safety would prefer if they did not have to handle cancer medication as some of it can be highly toxic. We started looking around for a vet who can help us. Natalie Prakash was mentioned by Barkway as the only certified canine oncologist in Singapore (Mt Pleasant) but the notoriety of that animal hospital made us look elsewhere. And so we began with Gentle Oak @Ghim Moh. Our friend had a good experience there for some other issue. We read the reviews and liked what we saw: holistic treatment of chemotherapy and alternative medicine. Dr.Lee in particular was more conservative on chemo dosage and advocated using other remedies. Having seen how cancer’s side effects had ravaged close friends and family and robbed them of quality of life, we decided to start with Dr. Lee.
Gentle Oak is extremely popular. Our first appointment there She started Toby on prednisone right away and scheduled Toby to come back a week later for his first dose of vincristine. We decided not to pursue finding out whether Toby’s lymphoma was B-cell or T-cell, and treated it as if it was B-cell. The reasoning behind this is, according to Dr.Lee, was that it wouldn’t make much difference in terms of the treatment. T-cell is the worst: the treatment barely works, and it’s very difficult to push it into remission; so just pray and hope that it’s B-cell which responds better to treatment and has longer remissions periods.
I will pause here .. this is the end of Chapter 1: how it first happened and how we reacted / steps we took. But… i’ve had a lot of time to reflect, and if i could turn back time I would do things differently. So, here goes.
WHAT WOULD WE HAVE DONE DIFFERENTLY?
Do not start with prednisone BEFORE Chemotherapy. Listen to this: http://www.radiopetlady.com/shows/podcast-pcv/lymphoma-importance-delaying-prednisone-chemo/ Basically the efficacy of the chemo in killing cancer cells is lowered due to prednisone. Prednisone (or prednisolone) should be given after chemotherapy begins.
Realize that for fast spreading cancers like lymphoma it’s best that chemo is started rightaway alongside a change in diet. Dogs tolerate chemotherapy much better than human beings so fret not. Especially if your doggo is already in good shape to start off. I felt that we ought to have been aggressive with it instead of relying on alternative / holistic / natural remedies. This is not a drill. Get your act quickly and do not fear chemotherapy. In fact it’s the only thing that really beat cancer back. You will see in later chapters that we threw everything at it.
Go see Dr. Tham at Jireh Vet, Balestier. He has heaps of experience treating cancer patients, and has a much wider repertoire of treatment and a much more dynamic approach. You see, the thing about cancer is that it is constantly evolving and your dog’s immunity can be compromised in many ways that typical studies do not cover off, while undergoing chemotherapy. This causes lots of complications. Dr. Tham’s approach works because he spends a lot more time understanding each case – as opposed to super popular vets like Gentle Oak where your pet is one of the 50 patients they see therefore the likelihood of the vet fine-tuning the treatment to factor in what worked better and what didn’t for your doggo, is a lot lower. Dr. Tham isn’t running his vet to maximize profit. He’s truly interested in the better outcome.
Put your dog on a 24 hour fast with water from time to time. There’s excellent research and data around how fasting helps improve cell health and promote autophagy. it basically helps to starve off cancer cells (sensitizing cancer cells to death). The re-feeding after fasting helps activate stem cells and the regrowth of healthy cells.
Additional information on intermittent fasting and caloric restriction https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5783752/
1 note
·
View note
Link
When decoding the results of your hematocrit test, your doctor will consider potential complicating factors. If the results are contradictory or unexpected, your doctor may also want to repeat the hematocrit test and perform additional blood tests.
0 notes
Text
Sharing from an animal rescuer.
<i>Oliver's Story
We found Oliver wearing a collar and a chewed-off leash, running into traffic on Lakeshore drive. He had no tag or chip but was super sweet and lost. After alerting CACC and our local police department, we began owner-searching, hoping someone would recognize their baby. We started calling him Oliver while we looked. He has been turned down by multiple rescues so far but he doesn't know that his breed and age are working against him for adoption and for him in fighting this terrible disease.
Then disaster struck. Ollie stopped eating and drinking, began vomiting and developed diarrhea. Within hours a pup that was so friendly and hopeful about finding his home turned into a sad little lethargic lump. After rushing him to the emergency vet, our worst fears were confirmed. Oliver caught a case of the devastating parvovirus ripping through the upper Midwest and is desperately ill.
If we had left him at the shelter, he wouldn't have made it out, would have no chance of finding his family, and could have passed the virus to other lost dogs.
So, for now, he is clinging to life on a wing and a prayer and the good graces of two Ph.D. students who put up the last of our summer stipends to cover what we could to give him a chance.
But Oliver needs more help. We need to raise $6047 to cover the life-saving care he desperately requires to live and find his family. Please help us save Oliver and stop parvo from taking another life. Even the smallest amount helps.
Below is the break-down of the costs:
Emergency Visit $175.00
Parvo SNAP Test $139.72
Parvo (Severe) $175.00
↳Liquid Diet CRI (Per 24 Hours) $158.34
↳Fluid Bag Additive $66.37
↳Miscellaneous $232.86
↳CBC - Complete Blood Count $99.65
↳Chemistry 17 Panel - Catalyst $241.53
↳IV Fluids (Per Hour) x 2 $24.68
↳Radiographs With Radiologist Review $525.61
↳IV Catheter (Peripheral) $118.76
↳IV Catheter (Sampling) $274.77
↳Hospitalization Level Isolation (per
hour) x 48 hours $1521.12
↳Hospitalization Setup $101.75
↳MetoclopramideCRI (Per 24 hours) $168.82
↳Blood Glucose (Serial - Per 12 Hours) x 2 $169.98
↳Electrolytes (Serial - Per 12 Hours) 2 x $288.74
↳Nasogastric Tube Placement $187.45
↳Hospital Injection 10 x $663.70
↳PCV/TS (Serial - Per 12 Hours) 2 x $163.00
↳Inpatient Exam 2 x $200.00
Subtotal
$5696.85
And we hope to raise another $350 to cover getting his adoption fees with a no-kill shelter if we cannot find his family.
Total ask: $6047</i>
1 note
·
View note
Text
Do you need to have your Lgv Driver Medical done to operate the vehicle?
Many people are asked to get their medical done to ensure that they can operate a commercial vehicle on public roads. If you, too, are asked for the same and are looking for some information, you are at the right place. For a PCV Driver Medical exam, you need to know everything beforehand to avoid future complications. Usually, there are a few circumstances when you are asked about the medical exam. These include: the candidate has reached a certain age, or you are suspected of having a medical condition. Whatever be the reason, contact Doctor Driver Assessment Limited to get your medical examination done.
What is a driver's medical examination?
Whenever a candidate applies to drive a medical vehicle, he must go through a PCV Driver Medical examination conducted by a special team of doctors. This process ensures that you don't have any disability that might affect your driving skills. Furthermore, you might be asked to go through a PCV Driver Medical examination that includes checking eyesight, Heart Conditions, or Neurological Problems. Get your medical done to ensure that you are fit and fine to drive a commercial vehicle.
What are the things that are examined during the test?
A team of most skilled doctors will diagnose a candidate's different health conditions, such as Sleep Disorders, Heart Conditions, Alcohol, Drugs, etc., that affect the driving ability. If you want to get your medical examination done, feel free to contact Doctor Driver Assessment Limited. Let's know the factors that are considered during the medical exam.
Eyesight and fluctuations in blood pressure are thoroughly checked. A person needs to go through an Lgv Driver Medical test to have a clear vision from the individual eye.
Alcohol or drug habits are diagnosed to ensure that candidates do not have any addictive habits.
Other factors that are checked thoroughly are Heart Conditions, Mental Health, and Neurological Problems.
CONCLUSION
If you have passed all the tests as mentioned above, the authority will provide your driving license. In some cases, they can perform a screen test for an in-depth examination. These tests include Mini-Mental Status Examination (MMSE), SIMARD-MD, and Montreal Cognitive Assessment (MoCA). Apply for your medical test at Doctor Driver Assessment Limited. Their doctors are well-versed who are registered under the General Medical Council (GMC). Be sure you book your initial appointment with the professionals of Doctor Driver Assessment Limited.
0 notes
Text
What’s HGE in dogs? Causes and symptoms of hemorrhagic gastroenteritis

HGE (Hemorrhagic gastroenteritis) in Dogs also known as acute hemorrhagic diarrhea syndrome (AHDS) is a serious (sudden) disorder of dogs with vomiting and bloody diarrhea. Most cases occur without warning in healthy dogs. The main and most disturbing clinical sign is large amounts of bloody diarrhea, most often bright red. Some dogs may have abdominal pain, loss of appetite, lethargy (fatigue), or fever. Also Read: 5 Best Orthopedic Dog Beds with Memory Foam Hemorrhagic gastroenteritis can affect any breed, age, size, or breed of dog, but it is most common in small and toy breed dogs. Young miniature poodles, miniature snoozers and Yorkshire Terriers are most affected. Other species commonly affected include Pekingese, Dutch, Maltese, Cavalier King Charles Spaniel, Shetland sheepdog, and Poodle.
What is HGE (hemorrhagic gastroenteritis) in dogs?
Hemorrhagic gastroenteritis in dogs occurs when large amounts of fluid enter the gut. It is not known what causes all cases of HGE in dogs, but it can lead to severe vomiting and bloody diarrhea in dogs. Sometimes diarrhea contains a lot of blood, which is similar to raspberry jam. HGE can be found in dogs of all ages and breeds, affecting small and toy dogs in general, especially small pinchers, miniature snorers, miniature poodles, Maltese, and Yorkshire Terriers. The average age of dogs with HGE is five, and most cases occur without warning.
What to do if your dog shows HGE (Hemorrhagic gastroenteritis) signs?
HGE is a deadly condition. If left untreated, it can quickly lead to hypoglycemia, low blood sugar, or hypovolemic shock, which occurs when dog blood or fluid levels drop dramatically. If your dog or puppy shows signs of disease you should consult your veterinarian immediately as it can be fatal.
What Causes Hemorrhagic gastroenteritis In Dogs?
The cause of HGE in dogs has been the subject of intense debate and research, but it is not known. Theories range from allergic reactions to food, parasites, and toxins to bacterial infections. It often affects overly sticky dogs, so stress, anxiety, and hyperactivity have been cited as possible causes.
How is HGE diagnosed in dogs?
Your veterinarian should be able to diagnose you based on your dog's symptoms and blood test results. Dogs with hemorrhagic gastroenteritis usually have a larger than normal packed cell volume (PCV), which is a measure of the ratio of red blood cells in their bloodstream. Your vet may also take steps to eliminate gastrointestinal problems and other causes of blood in the stool such as parvovirus, Addison's disease, intestinal parasites and rat poison anesthesia. This may include additional tests such as X-ray, ultrasound, biochemistry panel and taking urine and stool samples.
Why is my dog not eating after HGE?
Dogs with HGE often appear seriously ill and, in most cases, are unable to regain their appetite for at least a few days. It is unlikely that your veterinarian will feed your dog within the first 24 hours of treatment. After that, once their condition starts to improve and they are no longer sick, water and small, soft meals can be provided.
HGE treatment for dogs
Because HGE can lead to severe dehydration, aggressive intravenous fluid therapy is usually the mainstay of treatment. Anti-nausea and anti-diarrhea medications may also be given if antibiotics are prescribed if there is evidence of antibacterial infection if your dog becomes repeatedly ill. In the most severe cases, plasma treatment is required to correct low blood protein levels.
HGE survival rate
The prognosis for HGE in dogs is usually good at the beginning, as long as it is appropriate and aggressive. In most cases, dogs with HGE should be hospitalized for at least 24 hours. It is estimated that less than 10% of dogs treated for HGE die. However, there is a 10 to 15% chance that the condition will recur. The outcome can be worse for very young dogs or those with other ailments.
Prevention of HGE in dogs
Prevention advice is based primarily on common sense. For example, owners should try to make sure their dogs live in a low-stress environment, provide a high-quality balanced diet, and provide antimicrobial medications as prescribed by a veterinarian during the day. Read the full article
0 notes
Link
Complete Blood Count Test
Complete blood count (CBC) provides information about the type of cells and their numbers in the blood, such as red blood cells, white blood cells, and platelets. The CBC report to the doctor helps to check for symptoms such as weakness, fatigue, or injury. CBC test proves to be very useful in anemia, anemia, infection and many other disorders and also in their diagnosis. Diagnostic Centre in Shahdara
CBC tests include:
· White blood cells (WBC, leukocyte) count
· White Blood Sales (WBC Difference)
· Red Blood Sales (RBC Count)
· Hematocrit (HCT, packed cell volume, PCV)
· Hemoglobin (Hgb)
· Red blood sales index
· Platelet (thrombocyte) count
· Min Plate Plate Volume (MPV)
Your doctor may speak for a CBC test as well as a blood smear test. However, it is not part of the CBC test. During the test, a few drops of blood are spread on a slide made of glass and with the help of special dye marks are left on the slide.
In the further process, the slide is viewed with the help of a microscope and the number and size of RBCs and WBCs and platelets are recorded.
Cells of different sizes help a lot in the diagnosis of many diseases, such as leukemia, malaria or sickle cell disease. Diagnostic Centre in Shahdara
The CBC test is similar to the normal blood test but it is done for several reasons:
Your doctor may speak this test to review, monitor your total health. For routine screening of other diseases like anemia or leukemia, the doctor may recommend you to have a CBC test during a routine checkup.
This test is also done to diagnose medical conditions. In the condition of weakness, fatigue, fever, swelling, injury or bleeding, the doctor may ask you to have a CBC test.
CBC tests can help to understand the symptoms and causes of the disease and to cure it of the root. If the doctor feels that you are suffering from an infection, then through the CBC test, he can confirm this.
For monitoring medical conditions. If a blood disorder or blood-related illness is affecting your sales count, your doctor may seek the help of a complete blood count report for your medical condition.
For medical treatment monitoring. If you are taking any medicine which is affecting your blood cells, then the CBC test can monitor your health. Diagnostic Centre in Shahdara
What Should I Know Before Performing Complete Blood Count?
In many different positions of the body, the number of cells varies. Some of these conditions may require curing, while in other cases the body itself balances the sales count.
Recent blood infusions directly affect CBC
The normal CBC result of infants and children is different from that of adults. Pathology refers to several reference ranges of CBCs of different age groups. Doctors take this into consideration when looking at CBC data.
Red Blood Sales (RBC)
Dangerous conditions arising from RBC's high-level value: smoking, carbon monoxide, prolonged lung disease, kidney disease, cancer, heart disease, alcohol addiction, liver problems, boomers (polycythemia vera or hemoglobin-associated rarer disease that Holds oxygen.
Conditions that affect the body's water content may be responsible for the high RBC value. Such conditions may cause dehydration, diarrhea or vomiting, excessive sweating, and excessive urination. Lack of fluid in the body also increases the amount of RBC, it is called pulmonary polycythemia. Diagnostic Centre in Shahdara
White blood cells (WBC, leukocyte)
The high-level value of WBC can cause many serious conditions such as infection, inflammation, damage to body tissue (such as heart attack), severe physical or emotional stress (such as fever, injury or surgery), kidney failure, lupus, Tuberculosis (TB), included. Diseases such as arthritis, malnutrition, leukemia, and cancer. Diagnostic Centre in Shahdara Healserv also Provides 24X7 online appointment facilities of Hospitals for healthcare
☛🌏
Visit our website to get more details about HealServ-
https://www.healserv.com/diagnostic-centre/diagnostic-centre-in-dwarka-mor
#Iron #blood #DiagnosticLab #BodyCheckup #HealthCheckup #Checkups #UrineTests #CUE #UrineTestProfile #UrineInfection #DiabetesTest #KidneyDisease #seniorhealthpromo #ponsmedicaldiagnostics #pons medical #KidneyDiseases #UrineTests #HealthCheck #Liver_function_test #Liver #function #test
0 notes
Text
Day 4: Animal Lab and Bats
Today’s lecture was on animal reproduction. I am grateful for the animal science class at Rutgers because a lot of the information was familiar and I was able to follow along fairly well. We then got in the van to get samples for the animal lab we were doing later. We drove to a farm on one of the bumpiest roads I have ever been on; I felt like my teeth were rattling. We observed how to collect blood from the jugular vein of a horse. It looks a lot easier than I thought it would be! We also collected fecal matter before we left. For lunch the entire group enjoyed a meal at the Guava Limb Café, a really nice restaurant not far from where we are staying. When we got to the lab, we all put on lab coats and read a handout of the specific procedures we would be doing. We were told that this was the only major animal health lab in the entire country of Belize which I found interesting since there are a lot of labs in America. Even Rutgers University has labs and the ability to conduct PCR testing which is fairly new to Belize. I can tell that it takes a lot of practice to analyze fecal samples accurately since it was difficult to identify the parasite eggs and it was easy to mistake fibers for eggs. This was my second time trying to identify parasite eggs under a microscope and I definitely have a long way to go before I can confidently do it on my own. The blood lab was equally interesting. It is amazing how many things you can discover about an animal through its blood. We tested the horse’s hemoglobin levels to see if it was anemic, and we used a centrifuge to measure the PCV, or packed cell volume of the blood and everything seemed to be in order. We made a blood smear on the slide and died it properly, but were unable to analyze it while we were there because it needed time to dry. We also observed a dog’s blood parasite under the microscope, and it was fascinating. I enjoyed being able to take part in the sampling and analyzing because it allowed me to learn about how the tests are conducted through experience instead of learning about it from a book. Right after dinner we prepared to stay up late to try to capture bats. They have a method to capture vampire bats in order to control the population, thus reducing the spread of rabies among livestock which is also important for public health. The ride to the site was long and bumpy. We climbed into the back of a tractor and were brought deeper into the jungle. We waited all night to see if we could catch bats, listening to poetry, singing songs, and just talking. Just listening to the sounds of nature was such a nice change from what I am used to back at home. We were able to catch two of the vampire bats! This was such a great experience!
2 notes
·
View notes
Text
Global Pneumococcal Vaccines Market - Industry Analysis, Size, Share, Growth, Trends and Forecast 2020-2025
A new market study, “Global Pneumococcal Vaccines Market - Industry Analysis, Size, Share, Growth, Trends and Forecast 2020-2025 ” has been featured on WiseGuyReports.
PNEUMOCOCCAL VACCINES MARKET
Pneumococcal Vaccines help prevent pneumococcal disease, which is a type of infection caused by Streptococcus pneumoniae bacteria.
Pneumococcal disease is contagious and can cause severe infections in the lungs, the lining of the brain, invasive pneumococcal disease, concomitant administration.
Spinal cord, and blood. It is more common in children, but it’s most likely to cause severe complications in adults.
WHAT’S TRENDING IN THE PNEUMOCOCCAL VACCINES MARKET?
In 2017, demand for pneumococcal vaccines continued to increase.
Major factors that contributed to the demand include increasing prevalence of pneumonia globally,
post-marketing study
growing awareness, the rise in government focus on immunization programs for pneumonia, and the development of quality vaccines such as PPSV23.
However, high costs associated with the development of these vaccines and longer timelines required for their production hamper the growth of the market.
MARKET GROWTH ANALYSIS:
This report segments the market by product type, by dosage, by end-user, and by region.
Based on product type, the market is classified into two categories, namely pneumococcal conjugate vaccine and pneumococcal polysaccharide vaccine.
Pneumococcal conjugate vaccines are newer while the pneumococcal polysaccharide or concomitant administration. The unconjugated vaccine is older ones.
Based on end-user, the market is segmented into Infants/Young Children (2-10 Age), Young Adults/Adults (10-64 Age), and Geriatric (Over 65 Age).
Geographically, the market is segmented into five major regions, namely North America, South America, Europe, Asia Pacific, and RoW.
Globally North America is the largest market for pneumococcal vaccines with significant demand concentrated in the US owing to the high incidence of infections caused by pneumococcal disease every year in the US, with over 50,000 cases of pneumococcal bacteremia.
CDC recommends pneumococcal vaccination for all children under two years and all adults 65 years or older, hence driving the demand for PCV vaccines.
Also Read : https://www.einpresswire.com/article/501459624/pneumococcal-vaccines-market-2019-global-trends-share-growth-analysis-opportunities-and-forecast-to-2025
PRODUCT-BASED ANALYSIS:
The report profiles the following companies in Pneumococcal Vaccines market – Merck & Co., Inc., Pfizer Inc., GlaxoSmithKline Plc., Sanofi Pasteur, Astellas Pharma Inc, and Serum Institute of India Pvt. Ltd.
By Product Type
Pneumococcal conjugate vaccine
Pneumococcal polysaccharide vaccine
By End-User
Infants/Young Children (2-10 Age)
Adults/ Young Adults (10-64 Age)
Geriatric (Over 65 Age)
By Region
Asia Pacific (China, Japan, India, Australia, Rest of Asia Pacific)
Europe (Germany, France, The UK, Italy, Spain, Rest of Europe)
North America (The USA, Canada, Mexico)
South America (Brazil, Argentina, Rest of South America)
Rest of the World
REASONS FOR PURCHASING THIS REPORT?
Visualize the composition of Pneumococcal Vaccines market across each indication, regarding type and treatment options, highlighting the critical commercial assets and players.
Identify commercial opportunities in Pneumococcal Vaccines market by analyzing trends and co-development deals.
Excel data sheet with thousands of data points of the market – level 4/5 segmentation.
PDF report with the most relevant analysis cogently put together after exhaustive qualitative interviews and in-depth market study.
Product mapping in excel for crucial Pneumococcal Vaccines of all major market players
WHO ARE THE KEY VENDORS IN THE GLOBAL PNEUMOCOCCAL VACCINE MARKET?
Equipment Suppliers/ Buyers
Service Providers/ Buyers
Industry Investors/Investment Bankers
Education & Research Institutes
Research Professionals
Emerging Companies
Manufacturers
FOR MORE DETAILS: https://www.wiseguyreports.com/reports/3902873-global-nucleic-acid-testing-market-2019-2026
About Us:
Wise Guy Reports is part of the Wise Guy Research Consultants Pvt. Ltd. and offers premium progressive statistical surveying, market research reports, analysis & forecast data for industries and governments around the globe.
Contact Us:
NORAH TRENT
Ph: +162-825-80070 (US)
Ph: +44 2035002763 (UK)
0 notes