#Virtual GP appointment
Explore tagged Tumblr posts
Text
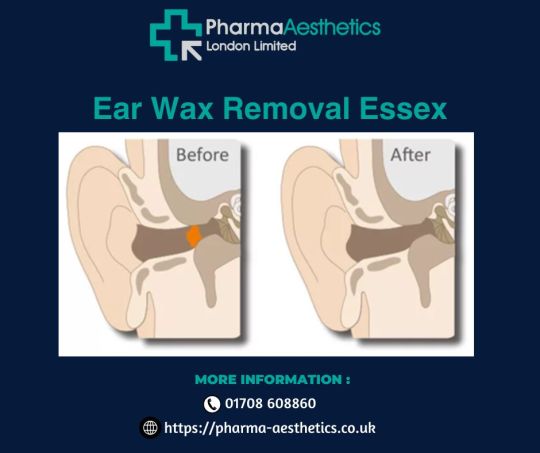
Pharma Aesthetics Provides Professional Ear Wax Removal in Essex
When it comes to ear wax removal, trust the expertise of Pharma Aesthetics in Essex. Our team of trained professionals understands the importance of clear and healthy ears for optimal hearing and well-being. Using safe and effective techniques, we offer professional ear wax removal services that address the buildup of ear wax and provide relief from discomfort and impaired hearing. For more details, please visit us at https://pharma-aesthetics.co.uk/ear-wax-removal-london/
#Hay-fever injection London#Yellow Fever Vaccine#Weight loss injection#Trichology Clinic#Online GP services UK#Virtual GP appointment#Fat Dissolving injection#Lipocavitation#Pharma Aesthetics
1 note
·
View note
Text
very really proud of myself for being so so very tired this week but not calling in sick. i had to allocate my spoons and give myself a bird bath today though
#also todays dinner is a leftover hamburger bc im too tired to cook#i have a virtual doctors appointment today which i dont like but i dont have a gp hngggg
8 notes
·
View notes
Text
The UTI did NOT in fact go away so it's to urgent care for me. Then to a virtual appt with my GP and then maybe to Raleigh's vet appointment, if I can get to the pharmacy for antibiotics.
I'm so done.
87 notes
·
View notes
Text
Britain was hit far harder by the Covid-19 pandemic than other developed countries because the NHS had been “seriously weakened” by disastrous government policies over the preceding decade, a wide-ranging report will conclude this week.
An assessment of the NHS by the world-renowned surgeon Prof Ara Darzi, commissioned in July by the health secretary, Wes Streeting, will find that the health service reduced its “routine healthcare activity by a far greater percentage than other health systems” in many key areas during the Covid crisis.
Hip and knee replacements, for instance, fell by 46% and 68% respectively. Hospital discharges as a whole dropped by 18% between 2019 and 2020 in the UK compared with the Organisation for Economic Co-operation and Development average of 10%, Lord Darzi will say.
In a key section of his report, the crossbench peer will also conclude that the NHS is still suffering the aftereffects of its inability to respond adequately to the Covid shock at the time.
“The state of the NHS today cannot be understood without recognising quite how much care was cancelled, discontinued, or postponed during the pandemic … The pandemic’s impact was magnified because the NHS had been seriously weakened in the decade preceding its onset.”
Darzi will be particularly critical of former Tory health secretary Andrew Lansley’s top-down reorganisation of the NHS under David Cameron’s prime ministership, which he will say “scorched the earth for health reform”.
“The Health and Social Care Act of 2012 was a calamity without international precedent – it proved disastrous,” Darzi will say, adding: “The result of the disruption was a permanent loss of capability from the NHS … This is an important part of the explanation for the deterioration in performance of the NHS as a whole.
“Rather than liberating the NHS, as it had promised, the Health and Social Care Act 2012 imprisoned more than a million NHS staff in a broken system for the best part of a decade.”
Lord Lansley defended his reforms, saying Darzi should be focusing on the “here and now” rather than reaching back over a decade for a “blame the Tories” narrative.
“The 2012 act created NHS England. It empowered the NHS. It reduced administration costs by £1.5bn. Waiting times fell to their lowest level. The longest waits were virtually eliminated,” said Lansley. He added that if his plans had been fully implemented, they would have made the NHS more internationally competitive.
The Tories are preparing to criticise the Darzi report as politically driven because its author was a minister under the previous Labour government and was a member of the Labour party until he resigned in 2019.
Labour will, however, point to his impressive CV and the fact that he held prominent positions while the Tories were in power, including sitting as the UK global ambassador for health and life sciences from 2009 until March 2013. Also, in 2015, Darzi was appointed as nonexecutive director of the NHS regulatory body Monitor, which oversaw the quality and performance management of healthcare in England.
The Darzi report – which will also find that more than 100,000 infants (0 to two-year-olds) were left waiting for more than six hours in A&E departments in England last year – is being seen as a watershed moment by senior NHS figures.
Streeting is expected to use the report as the foundation for his own blue-sky thinking on reform. The current NHS England long-term plan introduced in 2019 was drawn up before the pandemic, which has caused waiting lists to lengthen to a point where 6.39 million people are waiting for 7.62m treatments.
Streeting said last year that he believed the NHS required three big shifts, from sickness to prevention, from hospitals to GPs and community services, and from an “analogue service to one that embraces the technological revolution”.
Two other key reports to be published this week also paint a bleak picture of the health service’s prospects under current spending constraints.
A survey of trust chief executives and finance directors by NHS Providers, the membership organisation for hospital, mental health, community and ambulance service users, has found more than half (51%) to be “extremely concerned” about their ability to deliver on their priorities within the tight financial limits for 2024-5.
Nine out of 10 thought the financial situation more challenging than last year. Among the measures they were having to consider were “extending vacancy freezes”, “reducing substantive staffing numbers” and “scaling back services”.
Sir Julian Hartley, chief executive of NHS Providers, said that with funding so tight the message was that ways had to be found to secure multi-year investment in reforms that would increase productivity “instead of this stop-start approach to NHS funding which leaves them constantly worrying about budget cuts followed by quick fix, short- term funding announcements”.
In addition, a report from the NHS Confederation and healthcare consultancy CF (Carnall Farrar) has found that Labour’s pledge to create an extra 40,000 appointments a week in England would not stop waiting lists from rising.
It would only deliver 15% of what was needed to ensure 92% of patients start routine hospital treatment within 18 weeks – a key target that has not been hit for nearly a decade.
Matthew Taylor, chief executive of the NHS Confederation, said it was unlikely that there would be any significant reduction in waiting lists until spring or summer next year.
He added: “We need to be realistic about the fact that unless we do some pretty transformative stuff, demand is going to grow substantially. Almost everyone agrees we need to transform the NHS by investing in prevention. To do that, you have to double run [opening new services before old ones close].
“None of those things can be achieved for free. What we need from Rachel Reeves is a recognition that the long-term sustainability of the health service, the public sector and the economy as a whole, rests on shifting the health demand curve.”
Speaking to the BBC’s Laura Kuenssberg on Sunday morning, the prime minister, Keir Starmer, will echo Darzi’s assessment, saying the Tories “broke” the NHS in ways that were “unforgivable”.
He will add: “Our job now, through Lord Darzi, is properly to understand how that came about and bring about the reforms, starting with the first steps, the 40,000 extra appointments.”
12 notes
·
View notes
Text
BV Circa Medical Centre, Norwest: Comprehensive Healthcare Solutions

BV Circa Medical Centre, situated in Norwest, is dedicated to delivering high-quality healthcare services to the community. This article explores the diverse range of Medical Centre Norwest, the experienced healthcare team, and the center's commitment to patient well-being.
Comprehensive Medical Services
BV Circa Medical Centre offers a comprehensive range of medical services designed to address various health needs:
General Practice: Routine health check-ups, preventive care, and management of chronic conditions.
Specialist Care: Access to specialists in areas such as cardiology, dermatology, and orthopedics.
Women’s Health: Services include gynecological exams, family planning, and menopause management.
Men’s Health: Prostate health, sexual health, and general men’s wellness.
Children’s Health: Pediatric care, vaccinations, and developmental assessments.
Mental Health: Counseling services, mental health assessments, and referrals to psychiatrists.
Geriatric Care: Elderly health assessments, mobility aids, and management of age-related conditions.
Chronic Disease Management: Comprehensive care plans for diabetes, hypertension, and other chronic illnesses.
Experienced Healthcare Team
The centre boasts a team of dedicated healthcare professionals committed to providing compassionate and effective care:
General Practitioners (GPs): Primary healthcare providers offering ongoing management and treatment.
Specialists: Experts in various medical fields, ensuring specialized care for complex health issues.
Nurses and Allied Health Professionals: Supporting patient care through education, rehabilitation, and health promotion.
Patient-Centered Care
BV Circa Medical Centre adopts a patient-centered approach to healthcare delivery:
Personalized Treatment Plans: Tailored to meet individual health needs and preferences.
Holistic Care: Addressing physical, emotional, and social aspects of health.
Health Education: Empowering patients with knowledge to make informed health decisions.
Continuity of Care: Ensuring seamless coordination and follow-up for ongoing health management.
State-of-the-Art Facilities
The centre is equipped with advanced facilities to support comprehensive healthcare services:
Diagnostic Services: On-site pathology and imaging services for accurate diagnosis.
Treatment Rooms: Well-equipped for minor procedures and treatments.
Telehealth Services: Virtual consultations for convenient access to healthcare.
Community Engagement
BV Circa Medical Centre actively engages with the community through health promotion initiatives and educational programs:
Health Workshops: Providing information on wellness and disease prevention.
Community Health Events: Promoting health awareness and early detection of medical conditions.
Conclusion
BV Circa Medical Centre in Norwest is committed to providing exceptional healthcare services tailored to the needs of the community. With a focus on patient-centered care, an experienced healthcare team, and advanced facilities, the center ensures comprehensive health solutions for all patients.
To learn more about the services offered or to schedule an appointment, visit the BV Circa Medical Centre website or contact their friendly staff directly.
2 notes
·
View notes
Text
the state of the NHS after fourteen years of Tories is a terrifying and miserable capitalist hellscape
case in point, me, the last week or so:
have uti, picked up from a partner's infection. Very simple easy thing to treat. This one is a nasty little bugger, I feel like shit.
call gp. Ask for appointment.
No appointments.
At length told a pharmacy can prescribe 3 days of antibiotics without you seeing gp. Excellent!
Receive antibiotics. At this point we are ~3-4 days in. That's also how long it's been since I had a proper night's sleep because I HAVE TO GET UP TO PEE FOUR TIMES.
Antibiotics produce great improvement, but (surprise) perhaps not 100% by the time I finish the course. Nevrthless, am told by pharmacy I can't get any more from them. I must go to gp.
Call gp. Come down at 8am physically to surgery next day.
Arrive at 7.47. 12th in the queue. Total queue reaches >20 by 8am. For a cool parallel, they run out of appointments at person 8. The poor receptionist looks like if she has to tell one more person there's nothing she can do, she'll cry.
Receptionist tells me I can try again tmm (arrive at 7.30? I wonder thoughtfully) or try submitting a request through The App. Someone will call me today. I thank her and submit it in the car before I leave.
3.55 (GPs generally close at 4pm). No call. I squish down the fear that I am Karen-ing and call in. "I'm so sorry," I say, "do you know if I WILL be called today?"
She says I might get one up to 6pm, but that will only be a receptionist who will be booking an appointment in the next couple of weeks. "This can't wait two weeks," I say. "Your own guidance says so."
"There's nothing I can do," she says, and: "You shouldn't be using the online system for things that are urgent, anyway." "I tried to get an emergency appointment and there was nothing: I was TOLD to use this," I say, helplessly. "...Well anyway," she says, "the receptionist might call you by six."
AHA! I think. I am immensely lucky and have some small health insurance through work - including virtual gp. Maybe they can help! I book an appointment through that platform, relieved.
The appointment is over the phone within an hour - phenomenal. She tells me that she is not allowed to prescribe me anything: the uti not fully clearing up in 3 days of antibiotics means I need specialist urine testing as there is likely resistance. It needs to happen immediately, today, tonight, because I am at risk of a kidney infection. She can only refer me back to the NHS.
I say "but they don't have anything, and I can't argue - the poor receptionist can't do anything about not having appointments."
"You have to fight," she says. "You have to be seen. Go to urgent care if you have to."
It is now 6.05pm. The receptionist has not called.
Guess I'm spending the evening in a&e.
This is the struggle to get basic healthcare in the UK right now, and there is very often NO OPTION other than A&E. I HAVE some level of "private healthcare", and they could not do anything. Imagine what it's like for most people who don't even have the tiny level of access for a virtual GP to tell them that they ARE right, and they DO need to make a fuss.
I have been crying on and off all day. This is just not having healthcare. I wish I had any confidence at all that we'll change how we vote as a country.
#All bar 3 of those 20 in the queue were 60+#I wanted to ask them all who they intended to fucking vote for this year#nhs#nhs uk#fuck the tories#anti tories#tories out#tories#conservatives#conservative party
3 notes
·
View notes
Text
The Future of Geofencing Marketing – How It Works and Why Businesses Need It

What Is Geofencing Marketing?
Geofencing marketing is a location-based advertising technique that allows businesses to define a virtual boundary (geofence) around a specific geographic area. When potential customers enter or exit this boundary, they receive personalized ads, push notifications, SMS alerts, or promotions on their mobile devices.
This strategy helps businesses target high-intent customers in real time, increasing foot traffic, engagement, and conversions.
To understand how location-based marketing is shaping the future of advertising, check out this Forbes article.
How Does Geofencing Marketing Work?
Define a Virtual Geofence – Businesses create a customized radius around a store, competitor’s location, event venue, or any high-traffic area.
Detect Mobile Users – The system identifies potential customers who enter or exit the geofenced zone using GPS, Wi-Fi, Bluetooth, or cellular data.
Trigger Personalized Ads – When a customer enters the geofence, they receive a push notification, text message, or targeted ad on their device.
Encourage Immediate Engagement – The message includes an offer or incentive that encourages customers to visit the store or make a purchase.
Track User Behavior & Optimize Ads – Businesses analyze foot traffic, engagement, and conversion rates to improve future campaigns.
Why Businesses Need Geofencing Marketing
✔ Targets the Right Audience – Ads only reach customers in proximity, ensuring higher conversion rates. ✔ Enhances Brand Awareness – Even if users don’t act immediately, they become aware of your business. ✔ Increases Foot Traffic & Sales – Customers receive real-time offers, leading to instant engagement. ✔ Reduces Wasted Ad Spend – Instead of targeting a broad audience, businesses focus on high-intent customers.
Industries That Benefit from Geofencing Marketing
Retail Stores & Shopping Centers – Offer exclusive in-store discounts to nearby shoppers. Restaurants & Coffee Shops – Attract nearby customers with special dining promotions. Event Marketing – Engage attendees with VIP offers and location-based promotions. Healthcare & Wellness Centers – Send appointment reminders and exclusive wellness tips. Auto Dealerships – Target customers who visit competitor locations.
To explore how retailers are using geofencing for real-time sales, read this Think with Google report.
Case Study: Starbucks' Success with Geofencing Marketing
Starbucks leverages geofencing and AI to increase mobile orders and in-store traffic. When customers are near a Starbucks store, they receive customized push notifications offering discounts on their favorite drinks based on previous orders.
Results:
30% increase in mobile orders
Higher engagement from loyalty program users
Improved customer retention rates
FAQs About Geofencing Marketing
1. How is geofencing different from geotargeting? Geofencing targets customers in real time based on current location, while geotargeting focuses on past locations and behavioral data.
2. Can small businesses afford geofencing marketing? Yes! Many geofencing platforms offer budget-friendly pricing models based on ad clicks, impressions, or pay-per-engagement.
3. Does geofencing marketing require an app? Not always. Businesses can use SMS campaigns, mobile web ads, and social media ads without requiring an app.
Get Started with Geofencing Marketing
Check out Brandify’s targeting plan to create data-driven, location-based marketing campaigns.
The future of marketing is hyper-personalized and location-driven—and geofencing is leading the way.
Get a free targeting plan within the hour for your business here: https://brandify.io/targeting-plan/
Press Release: https://www.prlog.org/13053451
0 notes
Text
Comprehensive Guide to Dietetics in Liverpool

Dietetics plays a crucial role in promoting health and managing diseases through tailored nutritional guidance. In Liverpool, the demand for qualified dietitians has surged, reflecting a growing awareness of the importance of balanced nutrition for overall well-being. This blog delves into the world of dietetics in Liverpool, highlighting the services offered, the role of dietitians, and how they can support your health journey.
What is Dietetics?
Dietetics is the science of how food and nutrition affect human health. Dietitians are healthcare professionals trained to provide evidence-based dietary advice. They work in various settings, including hospitals, community health centres, private practices, and research institutions.
The Role of Dietitians in Liverpool
Dietitians in Liverpool offer a wide range of services to support individuals in achieving optimal health. Their roles include:
Clinical Nutrition: Managing medical conditions such as diabetes, heart disease, gastrointestinal disorders, and obesity through personalized nutrition plans.
Community Nutrition: Educating the public on healthy eating habits to prevent chronic diseases.
Sports Nutrition: Assisting athletes in enhancing performance through specialized dietary strategies.
Pediatric Nutrition: Supporting the growth and development of children with tailored nutritional advice.
Geriatric Nutrition: Addressing the unique dietary needs of the elderly to promote healthy aging.
Services Offered by Dietitians in Liverpool
Individual Consultations: Personalized dietary assessments and tailored nutrition plans.
Group Workshops: Educational sessions on various topics like weight management, healthy cooking, and disease prevention.
Corporate Wellness Programs: Nutritional guidance to enhance employee health and productivity.
Online Consultations: Virtual appointments for convenient access to dietary advice.
Why See a Dietitian?
Consulting a dietitian can be beneficial for:
Managing chronic health conditions
Weight management
Food intolerances and allergies
Digestive health issues
Improving athletic performance
Pregnancy and breastfeeding nutrition
Finding a Dietitian in Liverpool
Liverpool boasts a range of qualified dietitians available in hospitals, private clinics, and community health centres. To find the right professional:
Check Credentials: Ensure the dietitian is accredited by the Dietitians Association of Australia (DAA).
Specializations: Look for dietitians with expertise in your specific health needs.
Referrals: Your GP can recommend reputable dietitians.
0 notes
Text
GP virtual appointment today, so naturally have to take phone everywhere with me because my GP surgery doesn't keep accurate appointment times. Was just about to grumble a bit when I remembered, this is all free of charge, I am not going to go bankrupt just because I need a consultation and/or any follow up treatments. So bloody thankful I am not American.
So yeah, I'll just take my phone with me to the loo.
0 notes
Text
Comprehensive Healthcare at Your Convenience: Virtual-Doctor Private GP Services
Introduction Access to personalized, prompt, and professional medical care has never been more critical in today’s fast-paced world. Virtual-Doctor Private GP Service brings you a seamless healthcare experience with tailored solutions, offering the flexibility of a Private GP for your immediate health concerns, Weekend GP consultations for busy schedules, and specialized services like Physiotherapy and Dietitian support. Whether you need a trusted Private Doctor for general health or a specialist to guide your wellness journey, we ensure quality care delivered at your convenience.
The Role of a Private GP in Modern Healthcare
A Private GP serves as your primary healthcare provider, offering a personalized approach to diagnosing, treating, and managing your health. Unlike conventional appointments, which often come with long waiting times, a private GP ensures quick access to expert medical advice.
Advantages of Choosing a Private GP:
Immediate Access - Say goodbye to weeks-long waiting lists.
Extended Consultation Times - In-depth discussions tailored to your concerns.
Continuity of Care - Build a relationship with a doctor who understands your medical history.
Discretion and Privacy - Ideal for individuals seeking confidential consultations.
Weekend GP Services for Your Busy Lifestyle
Life doesn’t adhere to regular working hours, and neither do health concerns. Our Weekend GP service is designed for individuals who need expert medical advice outside of the traditional weekday schedule. Whether it’s a minor illness, a health check-up, or a prescription renewal, our doctors are here to assist you when it’s most convenient.
Why Weekend GP Services Matter:
Flexible Hours: Perfect for professionals and families juggling work and personal commitments.
Accessible Care: Receive immediate medical attention on weekends.
Convenience: Avoid taking time off work or disrupting weekday plans.
The Benefits of a Dedicated Private Doctor
Having a Private Doctor allows you to address medical concerns with continuity and confidence. With Virtual-Doctor, you can experience:
Customized Health Plans: Focused on your individual needs.
Advanced Diagnostics: State-of-the-art testing to ensure accurate results.
Holistic Healthcare: Integration of general practice with specialties like Physiotherapy and Dietitian services.
A private doctor is also invaluable for preventive care, helping you manage potential health risks before they become serious.
Physiotherapy: Restoring Movement and Alleviating Pain
Physiotherapy is an essential service for patients recovering from injuries, managing chronic conditions, or enhancing mobility. Our expert physiotherapists specialize in:
Post-Injury Rehabilitation: Regain strength and flexibility after an accident or surgery.
Chronic Pain Management: Reduce discomfort from conditions like arthritis or back pain.
Sports Therapy: Tailored plans to prevent injuries and improve athletic performance.
Lifestyle Guidance: Ergonomic advice and exercises to maintain long-term physical health.
Why Choose Virtual-Doctor for Physiotherapy? Our physiotherapists collaborate with our private doctors to develop comprehensive care plans. This interdisciplinary approach ensures that every aspect of your recovery and health is addressed.
Nutrition Matters: Dietitian Support for Optimal Health
Nutrition plays a pivotal role in maintaining and improving health. Our Dietitian services focus on empowering you with the knowledge and tools to make informed dietary choices. Whether your goal is weight management, improving digestion, or addressing food sensitivities, our dietitians offer evidence-based guidance tailored to your lifestyle.
Core Services Provided by Our Dietitians:
Weight Management Plans: Sustainable strategies for healthy weight loss or gain.
Nutritional Counseling: Learn how to balance your meals effectively.
Specialized Diets: Assistance with conditions like diabetes, hypertension, or food intolerances.
Wellness Coaching: Support for adopting healthier eating habits long-term.
Benefits of Integrating Dietitian Services with GP Care By combining dietitian expertise with GP advice, Virtual-Doctor creates a holistic healthcare model. This synergy ensures that every aspect of your health is supported for optimal well-being.
The Virtual-Doctor Difference
What sets Virtual-Doctor apart from other healthcare providers is our commitment to patient-centric care. Here’s why patients choose us:
Flexibility: Access services from the comfort of your home or visit our clinic.
Comprehensive Care: From general practice to specialized support, everything you need under one roof.
Experienced Professionals: A team of highly qualified GPs, physiotherapists, and dietitians.
Technology Integration: Teleconsultations and electronic health records for seamless communication and tracking.
Tailored Packages to Suit Every Need
We understand that healthcare needs vary greatly between individuals. That’s why we offer customized packages, including:
General GP Services: Regular check-ups, vaccinations, and chronic disease management.
Weekend Consultations: Available for urgent care or follow-ups.
Therapeutic Services: Physiotherapy sessions and rehabilitation plans.
Nutritional Wellness: Comprehensive dietary assessments and coaching.
How to Access Our Services
Getting started with Virtual-Doctor is simple:
Book an Appointment: Online or via phone, choose a time that suits you.
Consultation: Meet with your chosen GP, physiotherapist, or dietitian.
Follow-Up Care: Receive a detailed plan and continue care as needed.
Whether you require ongoing support or a one-time consultation, we are here to ensure you receive the best care possible.
0 notes
Text
Anytime Clinic

Address:
179 University Way Jamilah House, Flat 179
London, London E16 2RB
Phone: +44 (0) 1613910155
Email: [email protected]
Website: https://anytimeclinic.co.uk/
AnytimeClinic.co.uk is a modern healthcare solution designed to provide fast, convenient, and accessible medical services to patients across the UK. Whether you need a consultation, prescription, or expert medical advice, Anytime Clinic connects you with qualified healthcare professionals from the comfort of your home or office. The platform specializes in delivering flexible, patient-centered care through secure online consultations, eliminating the need for lengthy wait times or in-person visits. With a user-friendly interface and transparent pricing, Anytime Clinic ensures that everyone can access the care they need, when they need it. Available 24/7, AnytimeClinic.co.uk caters to a wide range of healthcare needs, from general medical consultations and mental health support to chronic condition management and preventative care. By leveraging technology, the service empowers patients to take control of their health while saving time and resources. Committed to quality and safety, Anytime Clinic employs a team of licensed and experienced professionals, ensuring that all advice and treatment meet the highest standards. Whether it's a minor ailment or ongoing health concern, AnytimeClinic.co.uk is your trusted partner for convenient and reliable healthcare. Your health, your time—on your terms. Visit AnytimeClinic.co.uk to experience healthcare made simple.
Keywords: Online Healthcare, Telemedicine, Virtual Doctor, Medical Consultation, Digital Health Services, E-Prescriptions, Remote Healthcare, Online GP Appointments, 24/7 Medical Access, Convenient Healthcare Solutions
Hour: 24 hours
Year of Est.: 2024
Number of Employee: 8
Payment Method: CC
1 note
·
View note
Text
Google Uses You
We’ve all been there. You’re in a rush, need an answer, and instinctively type your question into Google. A wealth of information is served to you in seconds, making your life easier and more efficient. We like to think that we’re using Google for our benefit, but what if I told you that Google is actually using you a lot more than you’re using it?
That might sound a bit conspiratorial, but it’s not far from the truth. The Google ecosystem is deeply integrated into almost every facet of our online experience. It isn’t just a search engine—it’s a data-gathering juggernaut that shapes, influences, and profits from our behaviors in ways most of us aren’t even aware of.
Data Is The New Currency
First, let’s break down a basic fact: in the digital world, data is king. Companies want to know everything about you—your habits, preferences, interests, and even your deepest fears (hello, targeted ads). Google is sitting at the top of this empire, collecting data from an almost unimaginable number of sources.
Every time you search for something, Google learns a little more about you. It tracks the keywords you use, the websites you click on, and even the amount of time you spend looking at certain content. And that’s just the tip of the iceberg.
How Google Tracks You
Google’s influence stretches far beyond its search engine. Whether you’re watching YouTube, checking Gmail, using Google Maps, or browsing with Chrome, Google is collecting data on you. This data includes:
1. Location Information: Google knows where you are at all times. Whether through Google Maps or your phone’s GPS, it tracks your every move. It uses this data to refine location-based advertising and suggest businesses or services nearby.
2. Search Habits: Google logs every search you make. From the mundane “best pizza in town” to the more personal “how to deal with stress,” each search reveals something about your personality, your needs, and your desires. This information is stored indefinitely and used to improve ad targeting.
3. Browsing History: If you’re using Chrome or are logged into a Google account while browsing, Google knows every site you visit. Even if you aren’t using a Google product directly, many websites use Google Analytics to track your visits. They can tie this data to your unique user profile, building a more complete picture of your online habits.
4. Email Content: It may sound unnerving, but Google’s AI scans the content of your emails. While this might be used to improve services or help you schedule calendar appointments, it also serves the primary purpose of making their advertising more precise.
5. Google Assistant: Google’s AI-powered virtual assistant listens to your voice and interprets your commands, but it’s also processing your voice data to better understand your patterns of speech, your needs, and, ultimately, how to serve you ads.
The Real Purpose: Advertising
So, what is Google doing with all this data? The answer is simple: advertising. In fact, over 80% of Google’s revenue comes from advertising. All those seemingly innocuous moments—searching for a restaurant, watching a YouTube video, or navigating through your emails—are meticulously analyzed to create a more detailed profile of you. With this profile, Google can target ads with a level of precision that’s almost unnerving.
Ever wonder how ads seem to follow you around the web? That’s Google’s algorithm at work. The more data it collects, the better it gets at predicting what you might buy, where you might go, and what services you might need. The more you interact with Google, the more it learns about you. But here’s the kicker: you don’t have to interact directly with Google at all. Many of the sites you visit use Google’s advertising or analytics services, so Google can track you even when you aren’t on a Google product.
The “Free” Services Trap
Google offers many services for free—search, email, maps, storage. And while we often marvel at how convenient and helpful these tools are, the old adage holds true: If you aren’t paying for the product, you are the product. In exchange for using these “free” services, you’re giving Google access to your personal data, which is far more valuable than a monthly subscription fee.
Every click, search, and keystroke you make within the Google ecosystem feeds the algorithm, refining your profile and making it easier for advertisers to reach you.
Can You Escape?
Realistically, completely opting out of Google’s reach is difficult in today’s interconnected world. You would need to use a different search engine (such as DuckDuckGo), avoid Gmail and Google Drive, stop using Chrome, and block Google Analytics on every site you visit. Even then, your smartphone may still be feeding Google location data and app usage statistics.
That said, there are ways to limit how much Google tracks you. Regularly clearing your search history, browsing in incognito mode, and disabling location services can reduce the amount of data you give away. Using privacy-focused apps and browsers is another step toward maintaining control over your data.
When we talk about how we “use” Google, we tend to think of the benefits we gain from its many services. And while those services are undoubtedly helpful, the reality is that Google is using us far more than we use it. It leverages the vast amounts of data we provide—whether knowingly or not—to fuel an enormous advertising engine, turning our digital lives into a currency it can trade.
So, the next time you fire up a Google search or open your Gmail, remember that the convenience you enjoy comes at a cost: your privacy. The power dynamic isn’t quite what it seems. Google isn’t just a tool we use—it’s a tool that’s using us.
This is something worth thinking about. What do you think about the trade-off between convenience and privacy?
#Google#Privacy#DataTracking#DigitalPrivacy#DataMining#BigTech#Advertising#GoogleTracking#UserData#InternetPrivacy#TargetedAds#GoogleServices#TechAwareness#OnlineTracking#DigitalFootprint#FreeServices#SurveillanceEconomy#TechTransparency#DataSecurity#OnlinePrivacyTips#new blog#today on tumblr
0 notes
Text

Apply SASSA Grants Administrators 2024 SASSA Grants Administrators 2024 Are you passionate about making a difference in people's lives while advancing your career in a dynamic, supportive environment? The South African Social Security Agency (SASSA) is hiring! A Grants Administrator position is available at the Midrand (Alexander) Local Office in Johannesburg. Join a forward-thinking team committed to providing essential services to South Africans. SASSA is a modern organization dedicated to enhancing the lives of millions of South Africans. With state-of-the-art facilities and an inspiring work environment, employees thrive and prosper in their roles. If you’re seeking a career where innovation meets service excellence, this opportunity is for you! - Salary: R216,417 – R254,928 per annum (exclusive of benefits) - Location: Midrand (Alexander) Local Office, Johannesburg District - Reference Number: GP/SAS 02/11/2024 - Closing Date: 10 December 2024 Minimum Requirements To be eligible for this role, candidates must meet the following criteria: - Educational Qualification: Senior Certificate (NQF Level 4) - Skills: Computer literacy is essential. Added Advantages - A valid driver's license. - Prior administrative or clerical experience. Key Responsibilities The successful candidate will play a vital role in the administration of social grants. Responsibilities include: - Providing customer care services to clients at the local office. - Screening grant applications for eligibility and completeness. - Processing social grant applications efficiently. - Conducting quality control checks on grant applications. - Assisting with medical, beneficiary maintenance, and payment processes. - Ensuring compliance with Section 57 of the Public Finance Management Act (PFMA). Benefits of Working with SASSA SASSA offers a supportive work environment that values diversity and inclusivity. Employees enjoy the following benefits: - Competitive salary packages. - Professional growth opportunities. - An innovative workspace designed to boost productivity and employee satisfaction. Important Notes - Applications must be submitted in PDF or scanned format as one attachment. - Ensure that all required documents are included. Incomplete applications may be disqualified. - Interviews may be conducted virtually, and shortlisted candidates will be contacted within three months of the closing date. Employment Equity and Inclusivity SASSA is committed to creating a diverse workforce and achieving its Employment Equity targets. Preference will be given to: - Candidates who will help the Agency achieve its Employment Equity Plan. - Persons with Disabilities are strongly encouraged to apply. Pre-Employment Screening All appointments are subject to pre-employment screening, which includes: - Qualification verification. - Reference checks. - Criminal and ITC checks. SEE ALSO: Capitec Bank ATM Assistants | Grade 12 How to Apply? Click Here to Apply Read the full article
0 notes
Text
Can't schedule a virtual appointment with my GP via the app. Call the office, and the sound is so faint and cutting out for two seconds at a time every 10 seconds so I am endlessly having to ask them to repeat themselves like 3 times and then finally just GUESSING what they are asking me. I can't even hear well enough to hear the list of available appointment times. I just have to hang up and have my boyfriend try from HIS phone. No idea if that will work any better.
Meanwhile, I can hear other calls just fine.
I'm so tired of this horseshit. I just want to make sure I don't have fucking cancer, okay? Is that so fucking difficult?
55 notes
·
View notes
Text
Transform Pet Care Services with Miracuves’ Rover Clone Solution
As pet owners increasingly seek convenient, reliable, and personalized care for their furry companions, businesses must rise to meet this growing demand. Miracuves’ Rover Clone Solution is the perfect platform to bridge the gap between pet owners and service providers. Designed to support a wide range of services, this customizable solution empowers businesses to deliver exceptional on-demand pet care experiences.

What is the Rover Clone Solution?
Miracuves’ Rover Clone is a feature-rich, ready-to-launch platform that mirrors the success of the Rover app while offering unparalleled flexibility. Whether your focus is dog walking, grooming, or veterinary care, this platform is fully customizable to cater to your business’s specific needs.
Key Benefits of the Rover Clone Solution
Comprehensive Customization: Adapt the platform to fit any pet care niche.
Rapid Time-to-Market: Save development time with a pre-built, scalable platform.
User-Centric Design: Prioritize seamless, intuitive experiences for both pet owners and service providers.
Core Features of Miracuves’ Rover Clone
Diverse Pet Care Services: Support multiple services, including grooming, training, pet sitting, and veterinary consultations.
Real-Time GPS Tracking: Give pet owners peace of mind by letting them track walks, transportation, or pet care activities in real-time.
Flexible Payment Integration: Offer secure payment options, including digital wallets, credit cards, and cash.
Intuitive User Interface: Ensure hassle-free navigation and interaction for pet owners and caregivers alike.
Feedback and Ratings: Build trust and accountability with a two-way rating and review system.
Admin Dashboard: Gain actionable insights into service trends, revenue, and user engagement for optimized operations.
Trends Shaping the Pet Care Industry
The pet care market is booming, with emerging trends setting new expectations for businesses. Miracuves’ Rover Clone Solution is designed to integrate these trends seamlessly:
1. Personalized Pet Services
Tailored care plans, such as dietary preferences or specific exercise routines, are a major draw for pet owners.
2. Eco-Friendly Practices
Sustainability is increasingly important, with services incorporating eco-friendly grooming products and waste disposal methods.
3. AI and IoT Integration
From smart pet collars to automated booking systems, technology is enhancing pet care experiences.
4. Safety and Hygiene Standards
Post-pandemic, contactless payments and verified, health-screened caregivers have become essential features.
5. Membership and Subscription Models
Offering subscription plans with perks like discounted rates or priority bookings drives customer retention and loyalty.
Applications of the Rover Clone Solution
Miracuves’ platform supports diverse use cases, making it ideal for businesses across the pet care industry:
Dog Walking Services: Enable pet owners to book reliable walkers for regular or one-time appointments.
Pet Sitting and Boarding: Offer trusted care for pets during vacations or overnight stays.
Grooming and Training: Provide professional grooming services or behavior training tailored to pets’ specific needs.
Veterinary Services: Facilitate easy access to routine checkups, virtual consultations, or emergency care.
Pet Transportation: Ensure safe and convenient transport for pets to clinics, groomers, or daycare facilities.
Why Choose Miracuves for Your Rover Clone Solution?
Miracuves brings unmatched expertise and innovation to the pet care industry, making it the go-to partner for businesses aiming to succeed in the on-demand economy.
1. Fully Customizable Platform
Personalize every aspect of the platform to reflect your brand identity and service offerings.
2. Scalable Infrastructure
Expand your business effortlessly, accommodating new locations or service categories as demand grows.
3. Advanced Technology
Our solution leverages cutting-edge frameworks to ensure smooth, secure, and efficient performance.
4. Dedicated Support
Miracuves’ 24/7 support ensures uninterrupted operations and prompt resolution of any technical challenges.
Success Stories with Miracuves’ Rover Clone
Businesses across the globe have transformed pet care delivery with Miracuves’ Rover Clone Solution. By offering innovative features and aligning with industry trends, these platforms have established trust, enhanced user satisfaction, and driven sustainable growth.
Launch Your Pet Care Platform Today
The on-demand pet care market is thriving, and businesses that invest in advanced, scalable platforms stand to gain the most. Miracuves’ Rover Clone Solution equips your business with the tools needed to succeed, from seamless booking and payment systems to real-time tracking and personalized features.
Partner with Miracuves today to redefine the pet care experience. Build trust, convenience, and reliability for pet owners while ensuring exceptional care for their beloved pets.
0 notes
Text
Taking Control: The Power of a Mental Health Care Plan Mental health is very crucial for a balanced and fulfilling life in today's fast pace of life. That is where having a Mental Health Care Plan comes into play, offering a tailor-made roadmap for overcoming emotional challenges and building your strength in it. The ease with which telehealth and services of Online Doctor Australia are now available makes access to mental health care easier than ever.

What is a Mental Health Care Plan?
A Mental Health Care Plan is a partnership with your doctor in mapping out your mental health journey. You set clear mental health goals, choose your treatment options, and decide what support you need. Here's what it can entail:
Therapy Sessions: Be it individual, group therapy, your doctor will design suggestions to best fit your preferences.
Medications: The doctor may talk to you about possible medications, including how to obtain a prescription through telehealth online in Australia.
Lifestyle Changes: Practicing stress management, proper sleep hygiene, and healthy nutrition can be effective weapons for a solid mental health care plan.
Support Services: The mental health professional may also advise you on some of the support services, such as community programs or peer support groups.
Advantages of a Mental Health Care Plan Coupled With Telehealth
Telehealth is the phenomenon of transformation in the delivery of mental health. The benefits include clarity and direction toward ways to improve your mental health and reaching your goal with appropriate, measurable progress tracked on the Mental Health Online Consultation Australia platforms.
Decisions Made Informed: You would be involved with your choice of the treatment option that best fits you with the comfort of an Australia consultation by Doctor on Phone. You're empowered to take control of your mental well-being hassle-free over in-person visits.
Financial Assistance: A Medicare card is required to access rebates for therapy sessions, and such therapy may become less costly. With cheap GP consultations and bulk billed telehealth services, mental health care becomes affordable.
Holistic Approach: A Mental Health Care Plan cares for you as a whole and to the root of the symptoms. Telehealth can be really useful in scheduling appointments, keeping you in contact with your doctor, and thus maintaining a balanced approach toward your mental health.
Improved Communication: Your treatment plan encourages open communication on your side and that of your healthcare providers, where both of you will be on the same page as you work towards finding the right course for your health. Virtual care and remote medical services have cut across into making this communication run efficiently.
Taking That First Step
It's strength, not weakness, to take the first step by seeking help for the care of your mental health. Contact your Online Doctor Australia or healthcare provider through telehealth and see if a Mental Health Care Plan is suitable for you. Your doctor will guide you through the whole process, ensuring that you receive every bit of support and tools needed for your mental health journey-all accessible online .
Beyond the Plan
Remember, the plan is an idea to start with, not a script you are going to do every time. As your needs change, so should your plan. Celebrate your successes, no matter how big or small they seem, and keep prioritizing your mental health. This can all be managed with telehealth options such as Mental Health Online Consultation Australia and Prescription Online Australia services.
Let's break the stigma of mental health care. Share your story, encourage others to seek help, and know that with the right support-including telehealth and bulk-billed consultations-a Mental Health Care Plan can be that key to unlock the doors to emotional resilience.
More Information on Teldoc
Teldoc offers bulk billing for mental health consultations and Mental Health Care Plans for eligible patients with a valid Medicare card. That may mean you won't need to pay out of pocket for your sessions.
#Online Doctor Australia#Doctor on Phone Australia Prescription#Cheap GP Consultations#online healthcare#virtual care
0 notes