#UnitedHealth
Explore tagged Tumblr posts
Text
A lot of people don't know this, but Luigi was actually a stunt double for Mel Gibson in the 1995 film Braveheart before he was born.


#Luigi Mangione#ceo#unitedhealthcare#united healthcare#unitedhealth#brian thompson#fuck ceos#corrupt#corrupt politicians#government corruption#anti-government#assassination#uhc ceo#unitedhealth group inc#ceo down#ceo shooting#uhc assassination#the adjuster#the claims adjuster#deny defend depose#briana boston#delay deny depose#braveheart
37 notes
·
View notes
Text


57K notes
·
View notes
Text
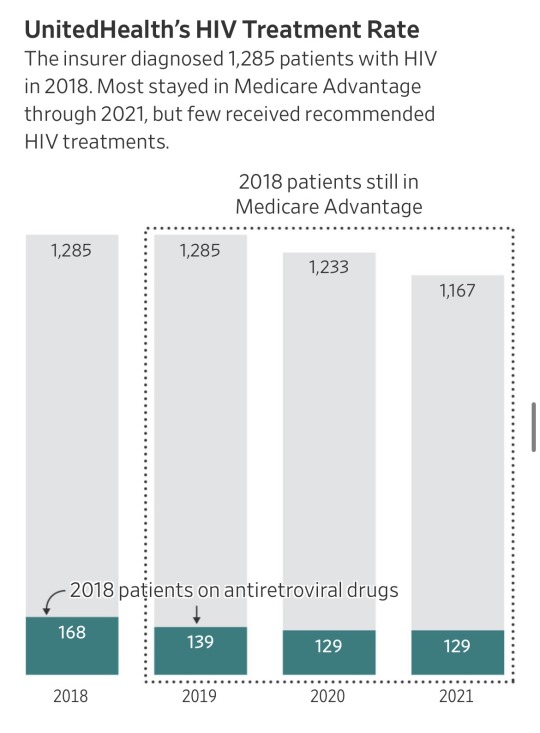
“It seems like almost all of those people don’t have HIV,” said Jennifer Kates, HIV policy director at KFF, a health-research nonprofit. “If they did, that would be substandard care at a pretty severe level,” she said.
Ya’ll. United Health just got accused of $17 billion in medicare fraud.
Basically they made up diagnosis which are improbable or impossible, “forgot” to remove ones which had been cured, and overall allegedly stole billions from taxpayers.
The government pays insurers a base rate for each Medicare Advantage member. The insurers are entitled to extra money when their patients are diagnosed with certain conditions that are costly to treat.
… About 18,000 Medicare Advantage recipients had insurer-driven diagnoses of HIV, the virus that causes AIDS, but weren’t receiving treatment for the virus from doctors, between 2018 and 2021, the data showed. Each HIV diagnosis generates about $3,000 a year in added payments to insurers.
… He said internal company data for 2022 showed a treatment rate for patients UnitedHealth diagnosed with HIV of more than triple what the Journal found. He said the pandemic disrupted care, lowering treatment rates during the period analyzed by the Journal, and that the analysis failed to account for patients who started treatments in future years.
The Medicare data, however, show UnitedHealth’s patients with insurer-driven HIV diagnoses were on the antiretrovirals at low rates even before the pandemic, and hardly any started the drugs in the years after UnitedHealth diagnosed them.
Source: https://www.wsj.com/health/healthcare/medicare-health-insurance-diagnosis-payments-b4d99a5d
I bet United Health really wishes it was a different week right now.
UPDATE/EDIT: Article is from July. I didn’t notice myself since it came up in my news feed. Don’t always trust the internet to be time accurate. 😎My guess is it is getting promoted due to current events. However, there are some updates concerning actions taken based on the report which you can look into by checking the authors’ other articles.
17K notes
·
View notes
Text
sits bolt upright in bed because i knew there would be an attempt to break the solidarity formed in the wake of the CEO shooting and i’m seeing it happen. people who were celebrating it are doing it themselves by digging through his social media and decrying him as just another alt right. but if this really is the guy who did it then like, what does that matter? are we really going to let this disrupt the momentum and the possibility for change? he did the thing. he (allegedly) killed the CEO and that same day another health insurance company backpedaled on one of its new dystopian ideas. now is not the time for “oh, he’s just another” – now is the time to drive that momentum forwards and to keep going. deny defend depose

#luigi mangione#brian thompson#unitedhealth#IM NOT EVEN AMERICAN BUT IM ROOTING FOR YOU GUYS. PLEASE DON'T BLOW THIS!!!
13K notes
·
View notes
Text

Interesting 🤔
#Interesting 🤔#health insurance#health#ausgov#politas#australia#usa#america#brian thompson#rest in piss#rest in pieces#rotinpiss#rot in hell#united healthcare#unitedhealth group inc#unitedhealthcare#unitedhealthgroup#unitedhealth#uhc generations#uhc ceo#uhc lb#uhc#fuck ceos#ceos#ceo#auspol#tasgov#taspol#fuck neoliberals#neoliberal capitalism
10K notes
·
View notes
Text
Health insurance is in the business of making people feel desperate and anxious.
The more desperate, the more money for CEOs.
No other leading country makes their citizens feel desperate and anxious via health care.
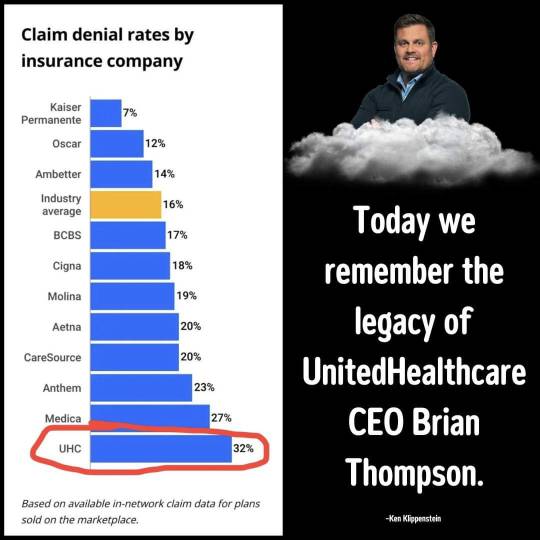
Seems UnitedHealthcare was exceptional at inflicting misery.

2K notes
·
View notes
Text
A sick tribute appeared outside the New York City hotel where UnitedHealthcare CEO Brian Thompson was gunned down by an assassin on Wednesday.
A balloon with a sign taped to it reading 'CEO DOWN' over the image of a smiling star and party poppers was found outside the Hilton Hotel in Midtown Manhattan after Thompson, 50, was gunned down there Wednesday morning.
The balloon was spotted as many Americans have joked about the CEO's death due to his company's track record of rejecting medical claims.

5 December 2024
Incredible.
2K notes
·
View notes
Text

Is the "outpouring of kindness and support" in the room with us right now? 👀
2K notes
·
View notes
Text
i still think the killer being hot is good for the morale of the country.
1K notes
·
View notes
Text
Dear Mr. Thompson,
The board at UnitedHealth has reviewed your claim of coverage for lead poisoning and after careful consideration the board has decided to reject your claim.
We thank you for choosing UnitedHealth for your healthcare needs and hope to continue providing coverage for you and your family. Have a blessed day and happy holidays.
Sincerely, UnitedHealth
#united healthcare#unitedhealthcare#medicare#brian thompson#unitedhealth#deny defend depose#luigi mangione
564 notes
·
View notes
Text
"He had a family" so did the huge numbers of people that he denied healthcare and let die 🥰. While he was sitting in his bathtub full of money and going on cruises with his family and probably going to the Bahamas he got was built from denied healthcare claims there were people in poverty and such who were out here dying. Stop using his family as an excuse to feel bad for him.
I feel bad for his kids but not him his kids don't know wtf going on and its been only 2 fucking days since the shooting but I ain't gonna feel bad for him cause he had it coming and his kids will probably NEVER know the truth about their father and UHC
But fuck him.
Over 15k people who are already struggling economically are slowly losing their lives then a rich ass CEO who benefits from our shitty country gets gunned down but we feel bad for the CEO.
crazy how..about musk next.
Sigh if that man who took his life came at my door so I could hide him he's going in my closet sorry officers never seen him a day in my life lol matter of fact I think he flew out the country.
Shooters get the CEOs not the children.
#feds this is a joke#brian thompson#fuck ceos#unitedhealth#unitedhealth group inc#unitedhealthcare#united healthcare#rip bozo#rest in piss
583 notes
·
View notes
Text

#Luigi Mangione#ceo#unitedhealthcare#united healthcare#unitedhealth#brian thompson#fuck ceos#corrupt#corrupt politicians#government corruption#anti-government#assassination#uhc ceo#unitedhealth group inc#ceo down#ceo shooting#uhc assassination#the adjuster#the claims adjuster#deny defend depose#briana boston#delay deny depose#luigi#douche in a suit
27 notes
·
View notes
Text

I'm so sorry guys
443 notes
·
View notes
Text

They picked a heck of a day to do this, not gonna lie.
413 notes
·
View notes
Text
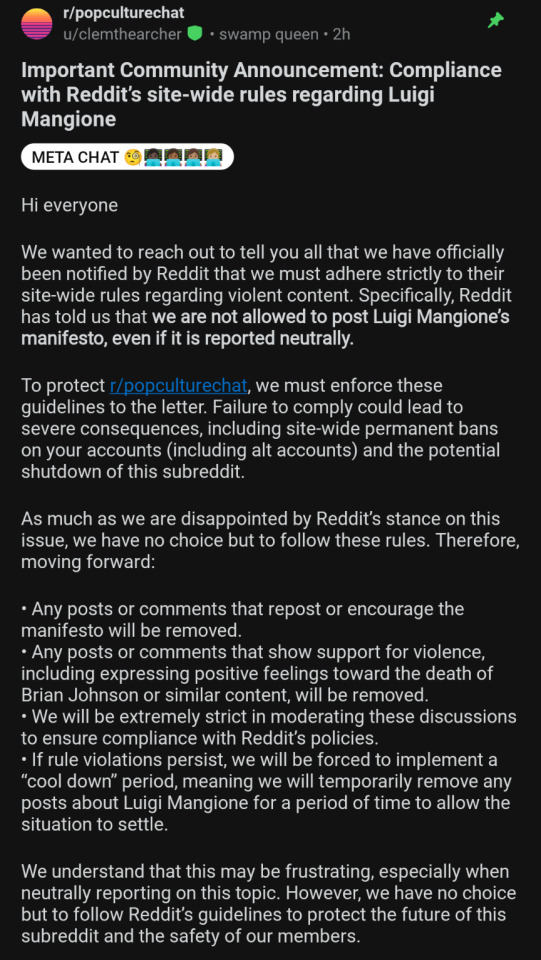
interesting that no other manifesto has ever been banned to my knowledge except one that criticises corporate america. very telling what reddit is choosing to ban here. was the unity a little too scary?
4K notes
·
View notes
Text

#united healthcare#unitedhealth group inc#unitedhealth#unitedhealthgroup#brian thompson#rest in piss#rotinpiss#rot in hell#fuck ceos#ceos#ceo#ausgov#politas#auspol#tasgov#taspol#australia#fuck neoliberals#neoliberal capitalism#anthony albanese#albanese government#insurance#health insurance#health#mental health#healthcare#health & fitness#health and wellness#healthylifestyle#class war
6K notes
·
View notes