#Tendinopathy Treatment
Explore tagged Tumblr posts
Text
Navigating Low Back Pain: 3 Treatments to Bring Relief
In the realm of running, knee pain is a common challenge, and understanding the specific diagnoses is key to addressing the nuances. Whether its patellar tendinopathy, patellofemoral pain, or a mysterious wildcard diagnosis, recognizing these conditions provides a foundation for informed and targeted management. Stay tuned for a better understanding of your knees on your running journey
#lower back pain#back pain treatment#back pain relief therapy#back pain therapies#knee pain common challenges#patellar tendinopathy#patellofemoral pain#back pain
0 notes
Text
Achilles tendinitis
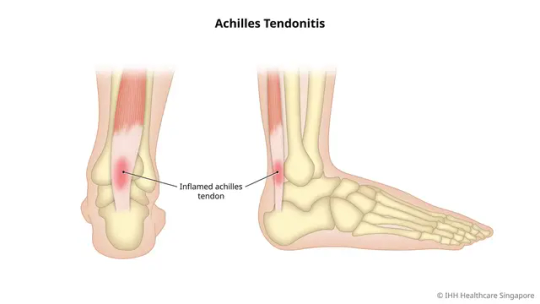
Overview
Achilles tendinitis is a condition that occurs when the Achilles tendon, which connects the calf muscles to the heel bone, becomes inflamed. This can cause pain and stiffness in the back of the ankle and can make it difficult to walk, run, or perform other activities that involve the lower legs. The Achilles tendon is one of the strongest and largest tendons in the body, and it plays a critical role in allowing us to move our feet and ankles. However, it is also prone to injury, particularly in athletes and people who engage in activities that involve repetitive jumping or running. Achilles tendinitis can be caused by a variety of factors, including overuse, improper footwear, tight calf muscles, and sudden increases in physical activity. People who are middle-aged or older, as well as those who are overweight or have certain medical conditions, such as diabetes, are also at an increased risk of developing Achilles tendinitis. Treatment for Achilles tendinitis typically involves rest, ice, compression, and elevation (RICE), as well as physical therapy exercises to help strengthen the calf muscles and improve flexibility. In some cases, non-steroidal anti-inflammatory drugs (NSAIDs) may be prescribed to help reduce pain and inflammation. Severe cases of Achilles tendinitis may require more aggressive treatments, such as immobilization in a cast or brace, corticosteroid injections, or even surgery. However, most people are able to recover from Achilles tendinitis with proper treatment and management.
Symptoms
The symptoms of Achilles tendinitis may vary from person to person, but common symptoms include: - Pain and stiffness in the back of the ankle, especially when walking or running - Swelling or tenderness in the area around the Achilles tendon - Difficulty flexing or pointing the foot - A crunchy or crackling sound when moving the ankle - Pain that worsens with activity and improves with rest - Mild to moderate pain after exercise or physical activity If left untreated, Achilles tendinitis can lead to more serious injuries, such as a ruptured tendon, which may require surgical intervention. If you experience any of the above symptoms, it is important to seek medical attention to determine the best course of treatment.
When to see a doctor
It is recommended to see a doctor if you experience any of the following symptoms: - Severe pain and swelling in the back of the ankle - Inability to bear weight on the affected leg - A popping or snapping sound at the time of injury - A feeling of a gap or indentation in the tendon - Redness, warmth, or fever in the affected area - Numbness or tingling in the foot or ankle - Recurring or persistent pain in the Achilles tendon that does not improve with rest or home remedies If you have any of these symptoms, you should seek immediate medical attention, as they may be indicative of a more serious injury or condition. In general, it is always a good idea to consult a doctor if you have any concerns about your health or if you are experiencing pain or discomfort that does not go away on its own.
Causes
Achilles tendinitis can be caused by several factors, including: - Overuse: Repeated strain on the Achilles tendon due to high-impact activities like running, jumping, or dancing can cause small tears in the tendon that eventually lead to tendinitis. - Tight calf muscles: Tightness in the calf muscles can put additional stress on the Achilles tendon, leading to tendinitis. - Improper footwear: Shoes that do not provide adequate support, cushioning, or shock absorption can increase the risk of developing Achilles tendinitis. - Sudden increase in physical activity: Starting a new exercise routine or increasing the intensity or duration of an existing one too quickly can put excessive strain on the Achilles tendon and cause tendinitis. - Age: As people age, their tendons become less flexible and more prone to injury. - Medical conditions: Certain medical conditions, such as diabetes, arthritis, and high blood pressure, can increase the risk of developing Achilles tendinitis. - Medications: Certain medications, such as fluoroquinolone antibiotics, can increase the risk of developing tendinitis. It is important to note that not all cases of Achilles tendinitis have a specific cause, and sometimes it may develop without an obvious trigger.
Risk factors
There are several risk factors that can increase the likelihood of developing Achilles tendinitis, including: - Age: As mentioned earlier, as people age, their tendons become less flexible and more prone to injury. - Sex: Men are more likely than women to develop Achilles tendinitis. - Physical activity: People who engage in high-impact activities, such as running and jumping, are at an increased risk of developing Achilles tendinitis. - Footwear: Wearing shoes that do not provide adequate support, cushioning, or shock absorption can increase the risk of developing Achilles tendinitis. - Tight calf muscles: Tightness in the calf muscles can put additional stress on the Achilles tendon, leading to tendinitis. - Obesity: Being overweight or obese puts additional stress on the Achilles tendon and can increase the risk of developing tendinitis. - Medical conditions: Certain medical conditions, such as diabetes, arthritis, and high blood pressure, can increase the risk of developing Achilles tendinitis. - Medications: Certain medications, such as fluoroquinolone antibiotics, can increase the risk of developing tendinitis. It is important to note that having one or more of these risk factors does not necessarily mean that a person will develop Achilles tendinitis, but it can increase their likelihood of developing the condition.
Complications
If left untreated, Achilles tendinitis can lead to more serious complications, including: - Tendon rupture: The Achilles tendon can rupture or tear completely if it is subjected to excessive stress or strain, especially in people who have untreated or chronic Achilles tendinitis. - Limited mobility: Achilles tendinitis can cause pain and stiffness, making it difficult to move the ankle joint and perform daily activities. - Chronic pain: In some cases, Achilles tendinitis can become chronic and lead to long-term pain and discomfort. - Infection: In rare cases, Achilles tendinitis can become infected, leading to further complications and requiring antibiotics or surgical intervention. - Tendinosis: Prolonged Achilles tendinitis can lead to degeneration of the tendon tissue, known as tendinosis, which can be more difficult to treat than tendinitis. It is important to seek medical attention if you suspect that you have Achilles tendinitis to prevent the condition from progressing to more serious complications. Early intervention and treatment can help to prevent the development of chronic pain or long-term mobility issues. Read the full article
#Achillestendinitis#achillestendonitis#activities#calfpain#Causes#determine#development#full#health#heelpain#home#long-term#men#overuseinjury#Physical#risk#symptoms#tendinopathy#Treatment#women
0 notes
Link
Achilles tendinopathy is a challenging condition that requires patience and dedication to overcome. By understanding the causes, seeking appropriate medical guidance, and adopting a comprehensive treatment plan, individuals can regain strength and mobility in their Achilles tendon.
0 notes
Text
The Benefits of Shockwave Therapy in Physiotherapy Treatment

Are you tired of living with chronic pain or dealing with nagging injuries that just won’t heal? Whether you’re struggling with tendonitis, plantar fasciitis, or lingering sports injuries, shockwave therapy could be the key to getting you back on track faster and more effectively than ever before.
What is Shockwave Therapy?
Shockwave therapy, or extracorporeal shock wave therapy (ESWT), involves sending high-energy acoustic waves to injured areas of the body. These waves stimulate the body’s natural healing mechanisms, increasing blood flow, reducing inflammation, and promoting tissue regeneration. Shockwave therapy is especially beneficial for conditions such as tendonitis, calcific tendinopathies, plantar fasciitis, and other musculoskeletal injuries that are resistant to conventional treatments.
How Does Shockwave Therapy Work?
The shockwave device generates pressure waves that travel through the skin and into the tissues. These waves trigger several beneficial effects, such as:
Improved Blood Circulation: Shockwaves stimulate the blood vessels, improving circulation to the injured area and helping to deliver oxygen and nutrients needed for tissue repair.
Collagen Stimulation: The therapy promotes collagen production, which is essential for tissue repair, particularly in tendons, ligaments, and muscles.
Breaking Down Calcifications: Shockwaves can help break down calcium deposits in tissues, which are common in conditions like calcific tendinopathy.
Reduced Inflammation: By stimulating the body’s healing processes, shockwave therapy helps reduce inflammation and alleviates pain.
The Benefits of Shockwave Therapy in Physiotherapy Treatment
1. Non-invasive and Drug-free Pain Relief
One of the most attractive benefits of shockwave therapy is that it is non-invasive. Unlike surgery, which requires recovery time and carries risks, shockwave therapy provides a non-surgical approach to healing. It also eliminates the need for medications, which can have side effects and lead to dependency. Shockwave therapy allows patients to manage chronic pain naturally, without relying on drugs or undergoing invasive procedures.
2. Effective for Chronic Conditions
Many people with chronic musculoskeletal conditions, such as tendonitis, plantar fasciitis, and calcific tendinopathy, often experience limited success with conventional treatments. Shockwave therapy has been shown to be highly effective in treating these stubborn conditions by addressing the root causes of pain and promoting healing at the cellular level. Studies have demonstrated that shockwave therapy significantly reduces pain and improves function in individuals with long-term musculoskeletal issues.
3. Accelerates Healing and Recovery Time
Shockwave therapy accelerates the body’s natural healing process. By improving circulation and stimulating tissue repair, it helps injuries heal faster. This is especially important for athletes or individuals who wish to return to their regular activities quickly. Shockwave therapy can significantly shorten recovery times, allowing patients to resume normal functions and sports with minimal downtime.
4. Promotes Tissue Regeneration
Shockwave therapy not only relieves pain but also actively promotes tissue regeneration. By stimulating the production of collagen, it encourages the healing of damaged tissues such as tendons, muscles, and ligaments. This regenerative effect helps to restore strength, flexibility, and mobility in the affected area. Whether you’re dealing with tendonitis or recovering from an injury, shockwave therapy helps to repair the underlying tissue and improve overall function.
5. A Safe Alternative to Surgery
Surgery can often be a last resort for patients suffering from musculoskeletal conditions, especially when conservative treatments have failed. Shockwave therapy offers a safe and effective alternative, helping to reduce the need for invasive procedures. For conditions like calcific tendinitis, where calcium deposits are causing pain, shockwave therapy can break down these deposits and alleviate discomfort without requiring surgery. In many cases, shockwave therapy can delay or even prevent the need for surgery.
6. Improves Mobility and Flexibility
In addition to relieving pain, shockwave therapy can improve the overall mobility and flexibility of the affected area. Conditions like frozen shoulder or Achilles tendinopathy can cause stiffness and limit movement, but shockwave therapy stimulates tissue healing and encourages a wider range of motion. As tissue health improves, so does mobility, helping patients return to activities like sports or everyday tasks without limitations.
7. Minimal Side Effects and Quick Recovery
One of the advantages of shockwave therapy is its minimal side effects. While mild discomfort or redness may occur after treatment, these are temporary and typically subside within hours. There is no significant downtime required, and patients can generally return to their normal activities immediately after treatment. The non-invasive nature of shockwave therapy makes it an attractive option for those looking to avoid long recovery periods associated with surgery.
8. Tailored to Individual Needs
Shockwave therapy can be customized to suit the specific needs of each patient. The intensity and duration of the shockwaves can be adjusted based on the severity of the condition and the patient’s response to treatment. This flexibility ensures that shockwave therapy can be optimized for maximum benefit, making it a highly effective treatment for a wide range of musculoskeletal conditions.
Conclusion
Shockwave therapy is a cutting-edge treatment that has proven to be effective for a wide range of musculoskeletal issues, offering benefits such as pain relief, faster healing, tissue regeneration, and improved mobility. Its non-invasive nature, combined with minimal side effects and the ability to accelerate recovery, makes it an ideal solution for those suffering from chronic conditions or injuries.
At Realign Chiro Physio, we are proud to offer shockwave therapy as part of our comprehensive physiotherapy treatment options. If you are dealing with chronic pain or a musculoskeletal injury and are looking for a safe, effective, and drug-free treatment, shockwave therapy may be the right choice for you. Contact us today to learn more about how shockwave therapy can help you recover and regain your quality of life.
2 notes
·
View notes
Note
Hi, just saw your post about having to see a male gyno and your chronic thrush. And as a person who went through years and years of similar issues, just wanted to say that last year I started seeing a new gyno who informed me about laser and prp treatments as long term solutions for chronic vulvar/vaginal issues. I had no idea those treatments existed and prp literally changed my life, my relationship with my body and with sex. I only tried prp since my issue was more related to skin sensitivity, but I know laser is super effective in cases of yeast and bacterial infections. Anyway, just sharing the info I wished someone had shared with me earlier. Sorry if the redaction is messy, English is not my first language. (You obviously don't need to publish this). Best wishes xx
That’s so interesting! I’m actually about to get PRP injections for something else - my chronic tendinopathies in my Achilles and hamstring. I so hope it changes my life
3 notes
·
View notes
Text
Vindicated (I'm not selfish, I'm not wrong)
I’m not sure how long I’ve been dealing with right shoulder pain and instability, but I remember it was already a known, old issue when I started working at the museum in September 2022. So let’s say it’s been 18 months. It’s probably been longer, but my memory is shit.
When I first mentioned it to a doctor in late summer 2022, she told me to take up weightlifting to strengthen my rotator cuff and help with weight loss (a problem for which I was not seeking advice). She did not offer specific advice to help me do that, and then shortly thereafter, she left for a different practice out west. I got switched to a different doctor, who failed to send a referral to PT for three months despite several reminders. When she transferred to another office in December 2022, I was blessedly assigned to my current doctor, who both listens to me and sends referrals and prescriptions out in a prompt manner. He had me in PT by the end of January.
I worked on my shoulder in PT until mid-April, when insurance refused to pay for more sessions, citing that my condition was stable. This was true, I did hit a plateau in my progress then--but my arm still hurt constantly, I could still feel what felt like bones shifting around when I moved, my range of motion was bad, and my shoulder would still “slip out” and lock up a few times a day, leaving me unable to lift my arm higher than my chest. Still, insurance said if I wanted more PT, I needed to see an orthopedic specialist and get a diagnosis that would qualify me for more sessions.
Seeing an ortho took a few weeks. I eventually got into a community orthopedics clinic at the end of May. The doctor I saw there was hyper focused on my weight and my self-harm scars, which he mentioned several times AND wrote about in my chart. He diagnosed me with “too fat and out of shape to lift her own arm,” essentially. He said all I needed was to keep doing the home exercises I’d been given in PT to strengthen my rotator cuff and soon I’d be all better. He said I didn’t need more imaging.
So I did those fucking exercises all summer. And yet, nothing improved. In fact, the pain and instability increased. It felt like my shoulder was becoming dislocated upwards of 20 times a day, leaving me unable to move my arm without severe pain. Whenever it happened, I’d have to physically push on my collar bone to get my arm working again. All summer and into the fall I muttered “my insurance company says I’m fine” every time I had to fix my shoulder, take OTC painkillers (that I’m not supposed to use because of my kidney function), or couldn’t sleep because of pain.
My insurance company’s treatment plan didn’t work out, surprisingly. I repeatedly found myself in tears due to the pain that simple motions cause me. My shoulder ached at a constant 4-5 on the pain scale, and the pain radiated into my collar bone, my top rib, and down to my wrist. If I moved my arm wrong, I’d drop what I was holding. I started walking around just constantly shaking my arm trying to get the joint to settle in a less painful way. There was no less painful way.
My primary doctor finally took pity on me in September and ordered the MRI that the ortho didn’t think I needed. It took 3 months to get an appointment. Three more months of grinding pain, tears caused by simple motions, and frustration at my useless body. Three more months of telling myself to toughen up and stop being a baby. Three more months of people rolling their eyes because I was being so dramatic about “a little joint pain.”
Well, I finally got in for my scan Wednesday. The results posted Thursday morning.
The MRI that ortho did not think I needed showed the following:
Superior tear of the right shoulder labrum.
Posterior tear of the right shoulder labrum.
Anterior tear of the right shoulder labrum.
AC joint degeneration.
Fluid in the AC joint.
Tendinopathy in 2 tendons of the rotator cuff.
The labrum is what keeps the shoulder joint stable. Mine is torn in 3 places. Which means, all these months I’ve been saying, “It feels like my shoulder is dislocating constantly and the bones are grinding together”, they WERE. That is EXACTLY what has been happening. The bones that make up my shoulder joint are so loosely connected that they are slipping all over the place, causing injury to nearby muscles, tendons, and ligaments.
For 18 months. At least.
I now have an urgent appointment scheduled with an orthopedic surgeon, because I might need surgery. Physical activity is a no-go until I’ve been evaluated and cleared for PT, and PT has to be done incredibly carefully if I can even do it.
I’ve been actively trying to get this taken care of for a year, during which I’ve been in constant, grinding pain, sleep deprived due to being woken up all night by pain, and damaging my kidneys by taking the forbidden NSAIDs. I’ve made changes to my wardrobe--I wear front close bras only, now. I’ve changed how I sleep--used to sleep on the right side, now it's the left side only.
And all of this could have been avoided if someone had taken me seriously last September.
Which is infuriating.
But also. The VINDICATION I feel.
I want to rub my MRI in the face of every person who rolled their eyes at me for “whining about a little joint pain.” I want to staple it to the forehead of the doctors who told me I just needed to lose weight. I want to put in on my refrigerator and point to it every time my sister implies I’m being dramatic or lying when I say I can’t do something, like put dishes on the top shelf or carry a heavy box.
Fuck all of them. Fuck every person who told me “just take some Aleve and get over it, it’s just joint pain, welcome to getting older.” Fuck every person who expected 100% from me on days my arm bones were grinding together and I had pain radiating to my wrist and my sternum.
Including me! Fuck me and my stupid need to persevere! I’ve pushed myself so hard the last year, because “I’m not going to let a little pain stop me!” even though “a little pain” sometimes had me crying and stopping would have prevented that. Yeah, I was failed by a lot of doctors, but I think it’s also partly my own fault that the damage is as bad as it is--I should have set more boundaries and had the backbone to listen to what my body was saying instead of people pleasing and trying not to make waves.
Fuck grinning and bearing it. Fuck putting up with pain because it’s easier for everyone else. Fuck doubting myself and taking the word of doctors over my own lived experiences. Doctors know medicine. I know how much this pain is affecting me. If we worked together, imagine what we could accomplish!
Yeah.
On a different note, I have more pictures of the inside of me.
Gross.
10 notes
·
View notes
Text
I had a pt in clinic today who had a UTI. I haven't actually treated a male outpt with UTI yet. All the ones I've treated have been in the hospital with IV ceftriaxone. Anyway, for men, their UTIs are always complicated. There is concern for prostatitis as a complication. So my pt had an IM ceftiaxone dose and then was prescribed PO ciprofloxacin 500 mg bid x7 days. His urine culture showed pansensitive E. coli. He also had a CBC at the previous visit where he had a leukocytosis to 14.2. His repeat UA in office today showed WBCs and he has a repeat urine culture and CBC pending. Because of concern for prostatitis, we continued antibiotics. Because of side effects of fluoroquinolones (tendinopathy), I decided to use TMP-SMX instead. You may need to treat UTI for 4 weeks. So I'm having my pt take TMP-SMX x4 weeks.
This is from UpToDate:
Dosing: Adult (Trimethoprim-sulfamethoxazole (co-trimoxazole))
Note: Weight-based dosing recommendations are based on the trimethoprim component. Each double-strength tablet contains trimethoprim 160 mg and sulfamethoxazole 800 mg. Each single-strength tablet contains trimethoprim 80 mg and sulfamethoxazole 400 mg. The undiluted IV solution contains trimethoprim 16 mg per mL and sulfamethoxazole 80 mg per mL. General dosing guidelines:
Oral: 1 to 2 double-strength tablets every 12 to 24 hours. Note: Serum creatinine and potassium concentrations should be monitored in outpatients receiving high-dose therapy (>5 mg/kg/day trimethoprim component]) (Ref).
IV: 8 to 20 mg/kg/day (trimethoprim component) divided every 6 to 12 hours.
Urinary tract infection:
Cystitis, acute uncomplicated or acute simple cystitis (infection limited to the bladder without signs/symptoms of upper tract, prostate, or systemic infection), treatment: Note: Avoid use if resistance prevalence is >20% or if patient has risk factors for multidrug-resistant gram-negative infection (Ref):
Oral: 1 double-strength tablet twice daily; treat females for 3 days and males for 7 days (Ref).
Cystitis, prophylaxis for recurrent infection: Note: May be considered in nonpregnant women with bothersome, frequently recurrent cystitis despite nonantimicrobial preventive measures. The optimal duration has not been established; duration ranges from 3 to 12 months, with periodic reassessment (Ref).
Continuous prophylaxis: Oral: One-half of a single-strength tablet once daily or 3 times weekly (Ref).
Postcoital prophylaxis (females with cystitis temporally related to sexual intercourse): Oral: One-half to 1 single-strength tablet as a single dose immediately before or after sexual intercourse (Ref).
Urinary tract infection, complicated (including pyelonephritis) (outpatient targeted therapy [if the isolate is known to be susceptible]):
Oral: 1 double-strength tablet twice daily for 14 days (Ref); for patients who have a rapid response to treatment, some experts treat for 7 to 10 days (Ref). Note: Oral therapy should generally follow appropriate parenteral therapy (Ref).
2 notes
·
View notes
Text
Effective Treatments for Pain Relief: ESWT and Stem Cell Infusion
Pain relief treatments have evolved significantly over the years, offering patients new hope for recovery. Among the most innovative treatments available today are ESWT treatment and stem cell IV infusion, both of which offer promising solutions for those suffering from chronic pain or injuries. These treatments focus on stimulating the body’s natural healing processes to address underlying issues and provide long-term relief.
What is ESWT Treatment? ESWT treatment, or Extracorporeal Shock Wave Therapy, is a non-invasive procedure designed to treat musculoskeletal conditions such as tendonitis, plantar fasciitis, and calcific shoulder tendinopathy. The treatment works by applying high-energy sound waves to the affected area, stimulating blood flow and accelerating tissue repair. This therapy is often recommended for patients who have not found relief through traditional methods like physical therapy or medication.
The key benefit of ESWT treatment is its ability to promote healing without the need for surgery or invasive procedures. Shockwaves penetrate deep into the tissue, encouraging cellular regeneration and improving the body’s natural ability to repair itself. As a result, many patients experience significant pain relief and improved mobility.
How Stem Cell IV Infusion Helps in Healing Another innovative treatment option gaining popularity is stem cell IV infusion. This method involves injecting stem cells into the bloodstream through an intravenous (IV) line. Stem cells are powerful cells with the ability to differentiate into various types of tissues, such as cartilage, muscle, and bone. By introducing stem cells into the body, the treatment aims to promote the repair of damaged tissues and reduce inflammation, ultimately improving overall function.
The primary advantage of stem cell IV infusion is its potential to treat a wide range of conditions, from joint pain to autoimmune disorders. Since stem cells can regenerate damaged tissues, they have the ability to provide relief from chronic pain and promote faster recovery. This treatment is becoming increasingly popular for conditions such as osteoarthritis, degenerative disc disease, and even sports-related injuries.
Benefits of ESWT and Stem Cell Infusion Both ESWT treatment and stem cell IV infusion offer numerous benefits for patients seeking alternative methods of pain relief. These treatments are not only effective in reducing pain but also help improve mobility and restore function in the affected areas. Additionally, both methods are minimally invasive, which means patients can avoid the risks and recovery time associated with surgery.
For individuals who have struggled with long-term pain or have not found success with conventional therapies, these advanced treatments offer a fresh approach. Whether it’s using shockwaves to stimulate healing or leveraging the regenerative power of stem cells, patients are experiencing enhanced outcomes and faster recovery times.
When to Consider These Treatments Patients dealing with chronic pain, injuries, or degenerative conditions may find ESWT treatment and stem cell IV infusion to be viable options when traditional therapies fail. A consultation with a medical professional will help determine if these treatments are suitable based on individual health needs and the specific condition being treated.
For those interested in non-invasive, natural approaches to pain relief, both ESWT treatment and stem cell therapies represent groundbreaking options that have the potential to significantly improve quality of life.
Conclusion In conclusion, ESWT treatment and stem cell IV infusion are two of the most promising therapies in modern medicine, offering hope to those suffering from chronic pain and injuries. With their ability to accelerate healing and promote tissue regeneration, these treatments can help patients find relief and return to their daily activities without the need for surgery.
0 notes
Text
How Long Does It Take to Recover from Achilles Tendinopathy?
Achilles tendinopathy recovery time varies significantly, ranging from weeks to several months, with factors such as age, activity level, and severity playing crucial roles. Treatment options like physical therapy, rest, and medication can aid recovery, while lifestyle changes, a proper diet, and carefully supervised exercise are essential for rehabilitation. Maintaining patience, positivity, and staying informed are crucial components for a successful recovery journey. For More:

How Long Does It Take to Recover from Achilles Tendinopathy?
0 notes
Text
What to Expect During Your Shockwave Therapy Session at Lakeside Sports Chiropractic

Noninvasive shockwave therapy is an effective treatment for various musculoskeletal conditions. It offers pain relief and promotes healing without the need for surgery. We prioritize patient comfort and care at Lakeside Sports Chiropractic and Physical Therapy. Here's what you can expect during your session.
Initial Consultation and Assessment
Your journey begins with a comprehensive consultation, during which our experienced practitioners assess your medical history and current condition. This evaluation helps determine whether noninvasive shockwave therapy treatment suits your specific needs. We then focus on understanding your symptoms and treatment goals to tailor a personalized therapy plan.
Understanding Non-Invasive Shockwave Therapy
Extracorporeal shock wave therapy (ESWT) is a non-invasive treatment that delivers shock waves to injured soft tissues, reducing pain and promoting healing. It's particularly effective for chronic tendinopathy and other conditions that have not responded to conservative treatments.
Preparing for Your Therapy Session
Before the session, you'll be comfortably positioned to allow easy access to the treatment area. No special preparation is required, and the procedure doesn't require anesthesia. Our team will ensure you're relaxed and informed about each process step.
The Shockwave Therapy Procedure
A handheld device delivers controlled shock waves to the targeted area during the session. Patients may experience a mild tapping sensation, but the procedure is generally well-tolerated. Each session lasts 15-20 minutes, depending on the treated condition.
Post-Treatment Care and Expectations
After the session, you can resume normal activities immediately, as no downtime is required. Some patients might experience slight redness or soreness in the treated area, which usually subsides quickly. Our practitioners provide guidance on post-treatment care to optimize healing. At Lakeside Sports Chiropractic and Physical Therapy, we provide noninvasive shockwave therapy, a safe and effective option for treating various musculoskeletal issues. Our focus on patient-centered care guarantees tailored treatment designed to alleviate pain and improve quality of life. If you're considering this therapy, our dedicated team will assist you at every stage of your healing process.
Lakeside Sports Chiropractic and Physical Therapy 11220 Treynorth Drive, Cornelius, NC, 28031, United States (704) 896-8446 www.lakesidesportschiro.com
0 notes
Text
Role of MSK Ultrasound Indore in Managing Chronic Pain

Chronic pain is a debilitating condition that affects millions of people worldwide, limiting their ability to lead active and fulfilling lives. For residents in Indore, MSK ultrasound offers an innovative and non-invasive approach to diagnosing and managing chronic pain. At Ultrascan Diagnostics, the best musculoskeletal ultrasound centre in Indore, patients receive high-quality imaging and personalized care to address their concerns effectively.
What Is MSK Ultrasound?
Musculoskeletal ultrasound (MSK ultrasound) is an advanced imaging technique used to evaluate muscles, tendons, ligaments, joints, and soft tissues. Unlike traditional imaging methods, MSK ultrasound provides real-time, detailed visuals, making it an ideal tool for identifying the root causes of chronic pain.
This diagnostic method is non-invasive, radiation-free, and allows for dynamic assessments, ensuring precise identification of injuries or abnormalities. At Ultrascan Diagnostics, we specialize in offering state-of-the-art diagnostic musculoskeletal ultrasound in Indore, helping patients achieve clarity about their conditions.
How MSK Ultrasound Helps in Managing Chronic Pain
Chronic pain often results from unresolved injuries, degenerative conditions, or inflammation. Accurate diagnosis is crucial for effective treatment. MSK ultrasound Indore plays a pivotal role in chronic pain management through:
1. Precise Diagnosis
Identifies soft tissue injuries such as tendon tears, ligament sprains, or muscle damage.
Detects joint inflammation and fluid buildup.
Evaluates nerve entrapments contributing to pain.
2. Real-Time Imaging for Interventions
Facilitates guided procedures like corticosteroid injections for targeted pain relief.
Enables physicians to monitor treatment efficacy over time.
3. Monitoring Disease Progression
Tracks degenerative conditions like arthritis.
Evaluates tissue healing in recovery phases.
By addressing the underlying causes of pain, musculoskeletal ultrasonography Indore provides a pathway to lasting relief.
Benefits of Choosing MSK Ultrasound for Chronic Pain Management
MSK ultrasound Indore offers several advantages over other imaging modalities:
Non-Invasive: No exposure to radiation, ensuring patient safety.
Dynamic Imaging: Captures movements and assesses functional abnormalities.
Cost-Effective: Affordable compared to MRI or CT scans.
Immediate Results: Provides real-time visuals for quicker diagnoses.
Patients at Ultrascan Diagnostics, the nearest ultrasound centre for many Indore residents, benefit from these advantages, ensuring a seamless diagnostic experience.
Why Ultrascan Diagnostics is the Best Choice
As the best musculoskeletal ultrasound centre in Indore, Ultrascan Diagnostics stands out for:
Cutting-Edge Technology: Equipped with advanced ultrasound machines for detailed imaging.
Experienced Radiologists: Skilled professionals with expertise in musculoskeletal ultrasonography Indore.
Patient-Centric Approach: Focused on comfort, accuracy, and clear communication.
Transparent Pricing: Affordable rates with no hidden charges.
By combining expertise with empathy, we ensure every patient receives the care they deserve.
Common Conditions Diagnosed with MSK Ultrasound
Musculoskeletal ultrasound in Indore is effective for diagnosing:
Tendonitis or tendinopathy
Bursitis
Ligament tears
Muscle strains or tears
Carpal tunnel syndrome
Arthritis and joint degeneration
Whether you’re dealing with an acute injury or persistent pain, our diagnostic centre in Indore is equipped to help.
The Procedure: What to Expect
Getting an MSK ultrasound at Ultrascan Diagnostics is a simple and comfortable process:
Preparation: No special preparation is needed for most cases.
Procedure: The radiologist applies gel to the affected area and uses a handheld transducer to capture images.
Duration: Most scans take 15-30 minutes.
Results: Reports are typically provided promptly, enabling timely consultations with your doctor.
FAQs About MSK Ultrasound Indore
1. What conditions can MSK ultrasound detect?
MSK ultrasound can identify soft tissue injuries, joint inflammation, arthritis, bursitis, and nerve entrapments. It is particularly effective for diagnosing chronic pain sources.
2. Is MSK ultrasound safe?
Yes, musculoskeletal ultrasound in Indore is completely safe as it uses sound waves, not radiation. It is suitable for patients of all ages, including pregnant individuals.
3. How does MSK ultrasound compare to MRI?
While MRI provides detailed static images, MSK ultrasound offers dynamic, real-time imaging and is more cost-effective. It is ideal for guiding procedures and assessing movement-related abnormalities.
Conclusion
Chronic pain doesn’t have to define your life. With MSK ultrasound Indore at Ultrascan Diagnostics, you gain access to precise diagnostics and effective management solutions. As the best musculoskeletal ultrasound centre in Indore, we’re committed to enhancing patient care through cutting-edge technology and compassionate service.
Book your appointment today at Ultrascan Diagnostics, the nearest ultrasound centre for high-quality care. Take the first step toward a pain-free life with reliable and affordable diagnostics.
Contact Ultrascan Diagnostics today to schedule your diagnostic musculoskeletal ultrasound Indore. Experience exceptional care and accurate diagnostics for managing chronic pain effectively!
Contact Details [email protected] Mon to Sat : 08:00 AM to 08:00 PM +91 78695 24599 Our Location 451-G Greater Brajeshwari,Near Kerala Bakery,Pipliyahana Road, Pipliyahana, indore, Madhya Pradesh 452016
0 notes
Text
What Is Shockwave Therapy and How Can It Help with Pain Relief?
What is shockwave therapy ?
Don’t worry. Don’t be scared. It is not a therapy where you are given a shock. Shockwave therapy uses a device which generates acoustic waves which are transmitted to the tissues with the help of an applicator. It triggers a biological effect which helps the healing process and formation of healthy tissues.
Shockwave therapy is commonly used to treat a variety of musculoskeletal conditions, particularly those involving soft tissue injuries, chronic pain, and inflammation.
This treatment is effective when conventional methods like rest, medication, or physical therapy have not provided sufficient relief.
Here are some of the conditions where shockwave therapy is commonly applied:
Tendinitis: For inflammation of tendons, such as tennis elbow, golfer's elbow, and Achilles tendonitis, shockwave therapy helps reduce pain and stimulate tissue repair.
Plantar Fasciitis: For persistent heel pain caused by inflammation of the plantar fascia, shockwave therapy can promote healing by increasing blood flow and collagen production.
Calcific Shoulder Tendinopathy: In cases of calcified tendons in the shoulder, shockwave therapy helps break down the calcifications, reduce pain, and promote the healing of the tissue.
Frozen Shoulder: This painful condition, marked by stiffness and limited mobility in the shoulder joint, can benefit from shockwave therapy to reduce pain and improve mobility.
Patellar Tendinopathy: Also known as jumper's knee, shockwave therapy can stimulate healing in the tendons around the knee joint, alleviating pain and improving function.
Muscle Strains and Ligament Injuries: Shockwave therapy can be used to treat various muscle strains, ligament injuries, and joint dysfunctions, promoting quicker recovery and reducing discomfort.
Chronic Pain: When pain persists for months or years and is resistant to other treatments, shockwave therapy can help reduce chronic pain by stimulating the body’s natural healing response.
Scar Tissue: It helps break down scar tissue and adhesions that can limit movement and cause pain after surgery or injury.
Shockwave therapy is often recommended for patients who are seeking a non-invasive, drug-free approach to pain relief and healing, especially for chronic conditions that have not responded well to other treatments. The therapy is also beneficial for accelerating recovery from sports injuries and for those looking to avoid surgery.
Benefits of Shockwave therapy:
Pain reduction
Stimulates collagen formation (collage is a protein that is the part of the structure of tissue, muscles, skin)
New blood vessel formation
Helps to dissolve the calcification
Trigger point release
#physiotherapy#backpaintherapy#excercisetherapy#jointpaintherapies#manualphysiotherapy#arthritis#activerehabilation#divinecarephysiotherapy#imslangley#divinephysiotherapy
0 notes
Text
Elbow Pain treatment in Hyderabad
Elbow pain can stem from various causes, such as overuse, injury, arthritis, or inflammation. Effective treatment options focus on relieving pain, promoting healing, and preventing further damage.
Elbow pain can affect your ability to perform daily tasks, from gripping objects to lifting your arm. Elbow pain can result from a variety of conditions such as overuse, injury, or inflammation. Treatment for elbow pain depends on the underlying cause, but here are some common methods to alleviate symptoms and promote healing:
Symptoms of Elbow Pain
Elbow pain can result from a range of conditions and often presents with varied symptoms, including:
Pain or tenderness: Often located on the inner or outer side of the elbow
Swelling and inflammation: Visible swelling or heat around the joint
Stiffness: Difficulty straightening or bending the elbow
Weakness: Reduced grip strength or difficulty lifting objects
Numbness or tingling: Sensations that may radiate down the forearm or into the hand
Common Causes of Elbow Pain:
Tennis elbow (lateral epicondylitis): Overuse of forearm muscles leading to pain on the outer side of the elbow.
Golfer’s elbow (medial epicondylitis): Pain on the inside of the elbow from overuse or repetitive motions.
Bursitis: Inflammation of the bursa (fluid-filled sac) in the elbow joint.
Arthritis: Can cause stiffness, swelling, and pain in the elbow joint.
Elbow fractures or dislocations: These require immediate medical attention.
Personalized Treatment Options
At Ashoka International Pain Management Centre, we develop customized treatment plans for each patient, focusing on non-invasive methods to restore function and alleviate pain. Our specialized elbow pain treatments include:
Physical Therapy: Strengthening and stretching exercises to restore flexibility, improve joint stability, and prevent reinjury.
Manual Therapy: Targeted, hands-on techniques to reduce tension, improve circulation, and alleviate joint stiffness.
Medication Management: Safe and effective use of anti-inflammatory medications to control pain and reduce swelling.
Interventional Pain Procedures: Minimally invasive options like platelet-rich plasma (PRP) therapy, offering targeted pain relief and tissue regeneration.
Ergonomic Guidance: Education on proper movement techniques and adjustments to daily activities to protect the elbow joint and prevent future injury.
In our clinic we use advance therapies for enhance healing and accelerate recovery. Options such as shockwave therapy and nerve block procedures provide effective pain relief while supporting the body’s natural healing processes.

Shockwave therapy
Shockwave therapy, also known as Extracorporeal Shock Wave Therapy (ESWT), involves the use of high-energy sound waves to stimulate healing in injured tissues. The sound waves are directed at the painful area of the elbow, and this treatment is typically used when other conservative treatments (like rest, physical therapy, or medications) have not provided relief.
Promote Blood Flow: The sound waves improve blood circulation in the affected area, promoting faster healing.
Stimulate Collagen Production: Shockwaves stimulate the production of collagen, which is essential for tendon and tissue repair.
Reduce Pain: The therapy helps desensitize the area and reduces pain by stimulating pain receptors and promoting the release of natural pain-relieving substances like endorphins.
Benefits of Shockwave Therapy for Elbow Pain
Non-invasive: Shockwave therapy does not require any cuts or needles, making it a relatively low-risk treatment.
No Downtime: Patients can return to normal activities immediately after the procedure, though it's often recommended to avoid strenuous activity for a short period.
Effective for Chronic Conditions: It is particularly useful for chronic tendinopathies, where other treatments have not worked. For conditions like tennis elbow or golfer's elbow, shockwave therapy can reduce pain and improve function.
Promotes Faster Healing: The therapy speeds up the healing process of damaged tissues by stimulating regenerative processes.
0 notes
Text
Shockwave Therapy Blue Mountains
For effective and non-invasive treatment, Birdwood Podiatry offers shockwave therapy in the Blue Mountains. This cutting-edge technology is ideal for treating conditions such as plantar fasciitis, Achilles tendinopathy, and heel spurs. Shockwave therapy stimulates healing by improving blood flow and reducing inflammation, providing relief from chronic pain without the need for surgery. If you’re seeking advanced care, visit Birdwood Podiatry for professional shockwave therapy in the Blue Mountains.
0 notes
Text
Biotronix Pneumatic Shockwave Therapy ESWT Radial Physiotherapy and Rehabilitation
Biotronix Solution Forever ® Shockwave Therapy Pneumatic Digital Machine ESWT for Sports Injuries Physiotherapy & ED
Mechanism:
ESWT involves the generation of high-energy shockwaves that are delivered to the affected area. These shockwaves create microtrauma in the tissue, promoting increased blood flow and the release of growth factors, which stimulate the body's natural healing processes. Applications for Sports Injuries:
Tendonitis and Tendinopathy: ESWT is commonly used to treat conditions like Achilles tendinopathy, patellar tendinitis, and rotator cuff tendonitis. Muscle Injuries: It can aid in the healing of various muscle injuries, including strains and tears. Calcific Deposits: ESWT is effective in breaking down calcific deposits in soft tissues. Applications for ED:
Pneumatic shockwave therapy, ESWT radial therapy, radial shockwave therapy device, shockwave therapy for rehabilitation, physiotherapy shockwave treatment, ESWT for pain management, shockwave therapy for muscle recovery, radial shockwave therapy for joint pain.
Contact us / What's app - 9711991264,9015251243,8076205625 ,8076549111 Website : www.solutionforever.com www.linktr.ee/biotronixcareinternational EMAIL : [email protected] ADDRESS : F-400, Sudershan Park ,Moti Nagar ,Near Gopal ji Dairy ,ND-110015 Location : Biotronix Care 097119 91264
#physiotherapy#Physiotherapist#physio#rehabilitation#rehab#health#PneumaticShockwaveTherapy#ESWTRadialTherapy#RadialShockwaveTherapy#ShockwaveTherapy#PhysiotherapyTreatment#PainManagementTherapy
0 notes
Text
How does shockwave therapy help patients?
Shockwave therapy is a highly effective treatment offered by our chiropractic clinic in Scarborough and North York to help patients recover from various musculoskeletal conditions. This non-invasive therapy uses acoustic waves to stimulate healing and promote tissue regeneration in areas of chronic pain or injury.
How does Shockwave Therapy help patients?
Pain Relief: Shockwave therapy helps reduce pain by increasing blood circulation and stimulating the release of natural pain-relieving substances in the body.
Accelerates Healing: By promoting the regeneration of damaged tissue and improving cellular repair, shockwave therapy can speed up recovery from injuries and chronic conditions such as tendonitis, plantar fasciitis, and calcific shoulder tendinopathy.
Breaks Down Scar Tissue: The acoustic waves help break down scar tissue and calcifications, which can improve mobility and reduce stiffness.
Improved Range of Motion: The treatment helps to restore flexibility and range of motion in affected areas, making it easier to return to daily activities and sports.
At our Scarborough and North York locations, shockwave therapy is part of a comprehensive treatment plan designed to address your specific needs. If you're dealing with persistent pain or looking for a non-surgical option to enhance recovery, visit our website to learn more and schedule a consultation. Our team is dedicated to helping you feel better and live pain-free!
0 notes