#SurgicalInterventional
Explore tagged Tumblr posts
Text
Anterior Neck Lipoma Enigma: Unmasking the Unusual- A Case Report
Abstract Lipomas are non-cancerous growths consisting of mature fat cells. Lipomas usually manifest as distinct, pliable lumps in the fatty tissues beneath the skin. Around thirteen percent of lipomas are observed in the head and neck area. An anterior neck lipoma is quite uncommon, and an anterior neck lipoma extending into the mediastinum is an exceedingly rare occurrence. Here, we present a case of 50 years old female who came with a huge swelling in anterior neck region (prevertebral space) which was slow growing. The purpose of this report is to keep in mind the differential diagnosis of lipoma when patient presents with anterior neck soft tissue swelling. Keywords: Lipoma; Anterior neck; Prevertebral space
#AnteriorNeckLipoma#LipomaCaseReport#MedicalEnigma#UnusualMedicalCases#NeckLipoma#CaseReport#MedicalMysteries#RareDiseases#ClinicalCaseStudy#MedicalResearch#HealthScience#MedicalJournal#SurgicalCases#MedicalDiagnosis#PatientCare#MedicalScience#HealthcareProfessionals#MedicalEducation#ClinicalPractice#TumorDiagnosis#SurgicalIntervention#MedicalInsights#DiagnosticChallenges#RareTumors#ClinicalFindings#HealthResearch#MedicalCaseReports#MedicalCommunity#MedicalStudies#HealthcareResearch
0 notes
Text

🔰BAJIS WEBINAR SERIES
OrthoTV is Glad to Collaborate with the Bone and Joint Infection Society (UK) and bring their content to OrthoTV platform for our Viewers
🔆Session 2: Fracture Related Infection
🔆Date : Tuesday 23rd April 🕕 Time : 6:00PM (IST)
🔆Click to Watch : https://tinyurl.com/OrthoTV-BAJIS-02
🔆Programme
👩⚕️Ms Deepa Bose Birmingham ▪️"FRI: Principles of Diagnosis"
👨⚕️Dr Neil Ritchie Glasgow ▪️"Pragmatic antibiotics prescribing in polymicrobial infection"
👨⚕️Professor Hamish Simpson Edinburgh ▪️"When and how to intervene surgically in the infected fracture"
🔆Moderators 🔺Mr Bilal Jamal - Glasgow
🔺Mr lan Kennedy - Glasgow
🤝 OrthoTV Team: Dr Ashok Shyam, Dr Neeraj Bijlani
📺 Streaming Live on OrthoTV www.orthotvonline.com
👨💻 Join OrthoTV - https://linktr.ee/OrthoTV
#BAJISWebinarSeries#OrthoTVCollaboration#BoneandJointInfectionSocietyUK#FractureRelatedInfection#MedicalWebinar#OrthoTV#MedicalEducation#DeepaBose#NeilRitchie#HamishSimpson#Orthopedics#BoneInfections#Antibiotics#SurgicalIntervention
0 notes
Text
Managing PCOS with Expert Care: Dr. Gayatri Kar Soni, the Best Gynaecologist for PCOD in South Delhi
Polycystic ovary syndrome (PCOS) poses unique challenges for women's health, requiring expert care and personalized treatment. In South Delhi, women facing PCOS turn to Dr. Gayatri Kar Soni, a renowned gynaecologist known for her expertise in managing PCOD effectively. In this informative blog, we delve into the diagnosis, treatment, and the pivotal role of Dr. Gayatri Kar Soni in empowering women to overcome PCOS.
Understanding PCOS with Dr. Gayatri Kar Soni: Best gynaecologist for PCOD in South Delhi
PCOS, also known as PCOD (Polycystic Ovary Disease), is a hormonal disorder characterized by irregular periods, hormonal imbalances, and ovarian cysts. Women with PCOS often experience symptoms such as irregular menstrual cycles, excessive hair growth, acne, and difficulty conceiving. While the exact cause of PCOS is unknown, genetic factors, insulin resistance, and hormonal imbalances are believed to contribute to its development.

Diagnosis and Assessment:
Diagnosing PCOS involves a thorough evaluation by a gynaecologist like Dr. Gayatri Kar Soni. Through a combination of medical history review, physical examination, and diagnostic tests, Dr. Gayatri accurately assesses the presence and severity of PCOS. Diagnostic tests may include blood tests to measure hormone levels, pelvic ultrasound to visualize ovarian cysts, and other assessments to evaluate insulin resistance and metabolic health.
Treatment Strategies:
Dr. Gayatri Kar Soni employs a multidisciplinary approach to treat PCOS, focusing on alleviating symptoms and addressing underlying hormonal imbalances. Her treatment strategies may include:
1. Lifestyle Modifications: Dr. Gayatri emphasizes the importance of adopting a healthy lifestyle, including regular exercise, balanced nutrition, and stress management techniques to improve symptoms and overall well-being.
2. Medications: Dr. Gayatri may prescribe medications such as birth control pills, anti-androgen medications, or insulin-sensitizing agents to regulate menstrual cycles, reduce hirsutism, and manage insulin resistance.
3. Fertility Management: For women struggling with infertility due to PCOS, Dr. Gayatri offers comprehensive fertility evaluations and treatments tailored to their unique needs. She may recommend ovulation induction, in vitro fertilization (IVF), or other assisted reproductive technologies to improve fertility outcomes.
4. Surgical Interventions: In certain cases, Dr. Gayatri may recommend surgical interventions such as ovarian drilling or laparoscopic cystectomy to manage ovarian cysts and restore fertility.
Empowering Women's Health:
As the best gynaecologist for PCOD in South Delhi, Dr. Gayatri Kar Soni goes above and beyond to empower women with PCOS. Through compassionate care, personalized treatment plans, and ongoing support, Dr. Gayatri helps her patients navigate the challenges of PCOS and achieve optimal health and fertility.
Conclusion:
PCOS is a complex condition that requires comprehensive care and expertise to manage effectively. With Dr. Gayatri Kar Soni as their trusted gynaecologist, women with PCOD in South Delhi can rest assured that they are receiving the highest quality care and support. By partnering with Dr. Gayatri, women can take control of their PCOS and embark on a journey towards improved health, fertility, and well-being.
#PCOS#PCOD#Gynaecologist#Women'sHealth#Fertility#HormonalDisorder#SouthDelhi#DrGayatriKarSoni#TreatmentStrategies#LifestyleModifications#Medications#FertilityManagement#SurgicalInterventions#Empowerment#Healthcare#Wellness#HealthAwareness#MedicalCare#HealthEducation#PatientCare
0 notes
Text
Buy healthcare franchise in India

The medical discipline of orthopedics is devoted to the identification, management, and avoidance of conditions and trauma involving the musculoskeletal system. Orthopedic doctors are qualified to treat a broad spectrum of illnesses, including congenital problems, degenerative diseases, and fractures and joint injuries. Orthopedic specialists use advanced imaging methods, like MRIs and X-rays, to diagnose and treat conditions with both surgical and non-surgical approaches to function and discomfort.
Buy healthcare franchise in India
0 notes
Text
Total Hip Replacement Surgery in Pune with Dr. Mayank Pathak
Dr. Mayank Pathak is a renowned orthopedic surgeon offering top-notch total hip replacement surgery in Pune. This procedure can be a life-changing solution for individuals suffering from hip pain, arthritis, or mobility issues. With expertise and dedication, Dr. Pathak provides comprehensive care to patients in various locations, including Mundhwa, Kharadi Rd, Viman Nagar, Thite Nagar, Keshav Nagar, Wagholi, and Vadgaon Sheri.
Total hip replacement is a surgical intervention that replaces the damaged hip joint with a prosthetic implant. Dr. Pathak's approach involves advanced techniques and personalized treatment plans to ensure optimal outcomes. He prioritizes patient comfort, post-operative mobility, and a pain-free future. With a commitment to excellence and a track record of successful surgeries, Dr. Mayank Pathak is the trusted choice for hip replacement surgery in Pune. If you're seeking relief from hip pain and wish to regain your mobility, consult with Dr. Pathak and take the first step towards a healthier, pain-free future.
#TotalHipReplacement#HipSurgery#OrthopedicSurgeon#PuneHealthcare#DrMayankPathak#Orthopedics#HipPainRelief#ArthritisTreatment#SurgicalIntervention#MobilityRestoration#ExpertCare
0 notes
Text

💉🩺 𝗘𝗻𝗵𝗮𝗻𝗰𝗶𝗻𝗴 𝗗𝗶𝗴𝗲𝘀𝘁𝗶𝘃𝗲 𝗛𝗲𝗮𝗹𝘁𝗵: 𝗦𝘂𝗿𝗴𝗶𝗰𝗮𝗹 𝗚𝗮𝘀𝘁𝗿𝗼 𝗦𝗲𝗿𝘃𝗶𝗰𝗲𝘀 ⚕️👨⚕️
Our Surgical Gastro Services are designed to optimize and restore digestive health through expert surgical interventions.
We strive to provide top-notch care, leveraging advanced surgical techniques and a patient-centric approach to ensure the best possible outcomes. 😇
Your well-being is our priority! 👯♀️
Explore our surgical gastro options and take a step towards a healthier digestive system.
Contact us today for more information and personalized consultations. 👨💻
☎️ Call us on +91 40-4200-7070
👉 Visit: https://www.healixhospitals.com/contact
#SurgicalGastroenterology#SurgicalGastro#DigestiveHealth#GastrointestinalSurgery#Healthcare#DigestiveWellness#SurgicalInterventions#HealthJourney#ExpertCare#PatientCentric#BookConsultation#HealthIsWealth#gastroenterologist#Gastroenterology#multispecialityhospital#Madhinaguda#HealixHospitals
0 notes
Text
#RetinaSpecialist#Aurangabad#EyeCare#RetinaDisorders#EyeExaminations#SurgicalInterventions#CompassionateCare#DrRohitBang#RetinaSpecialistAurangabad#EyeSpecialist#RetinaCare#Ophthalmology#EyeHealth#EyeClinic#AdvancedTreatment#EyeSurgery#EyeSpecialistAurangabad
1 note
·
View note
Link
🔍 Subscapularis tear is a common injury that affects the shoulder joint. It occurs when the subscapularis muscle, which is located in the front of the shoulder, is torn. This injury can cause a range of symptoms, including pain, weakness, and limited mobility. 🤕 The causes of subscapularis tear can vary, but it is often associated with repetitive overhead movements, such as throwing a ball or lifting weights. Other risk factors include age, gender, and previous shoulder injuries. Early diagnosis and treatment are essential to prevent further damage and promote healing. 💊 Treatment options for subscapularis tear depend on the severity of the injury. Conservative measures, such as rest, ice, and physical therapy, may be effective for mild cases. However, more severe tears may require surgery to repair the muscle. With proper treatment, most people can recover from a subscapularis tear and return to their normal activities.1. What is a Subscapularis Tear and How Does it Occur?The subscapularis muscle is located in the shoulder and helps rotate the arm. A tear can occur from overuse or injury. Symptoms include pain, weakness, and limited mobility. Diagnosis is done through physical examination and imaging. Treatment options include rest, physical therapy, and surgery. 🏥2. Identifying Subscapularis Tear Symptoms: Pain and Weakness in the Shoulder🔍 Subscapularis tear symptoms include pain and weakness in the shoulder. 🔍 Pain may be felt in the front of the shoulder or upper arm. 🔍 Weakness may make it difficult to lift the arm or perform daily activities. 🔍 Other symptoms may include a popping or clicking sensation in the shoulder. 🔍 If you experience these symptoms, see a doctor for a proper diagnosis. 🔍 Treatment options may include physical therapy, medication, or surgery. 🔍 Early diagnosis and treatment can lead to a quicker recovery. 🔍 Don't ignore these symptoms, as they can worsen over time. 🔍 Take care of your shoulder and seek medical attention if necessary.3. Diagnostic Tests for Subscapularis Tear: MRI and Physical ExaminationTwo diagnostic tests for subscapularis tear are MRI and physical examination. MRI is a non-invasive imaging test that uses magnetic fields and radio waves to create detailed images of the shoulder. Physical examination involves testing the strength and range of motion of the shoulder joint. MRI is the most accurate diagnostic test for subscapularis tear. It can detect tears in the subscapularis muscle and determine the severity of the tear. It is also useful in identifying other shoulder injuries that may be present. Physical examination is a quick and easy test to perform. It involves a series of movements and tests to assess the strength and mobility of the shoulder joint. It can help diagnose subscapularis tears, but it is not as accurate as MRI. Both MRI and physical examination are important in diagnosing subscapularis tears. MRI is the gold standard for accuracy, while physical examination is a useful tool for initial assessment. Consult with a healthcare professional to determine the best course of action for diagnosis and treatment. 🧐👨⚕️💪4. Conservative Treatment Options for Subscapularis Tear: Rest, Ice, and Physical TherapyConservative treatment options for subscapularis tear include rest, ice, and physical therapy. Rest: Avoid activities that aggravate the injury and allow the shoulder to rest. Ice: Apply ice packs to the affected area for 20 minutes at a time, several times a day to reduce pain and swelling. Physical therapy: Strengthening and stretching exercises can improve range of motion and reduce pain. Physical therapy may also include modalities such as ultrasound, electrical stimulation, and heat therapy. Conservative treatment may take several weeks to months to show improvement, but it can be effective in treating subscapularis tears. If conservative treatment fails, surgery may be necessary to repair the tear. 👍 Remember to consult with a healthcare professional before starting any treatment plan for subscapularis tear. 👍5. Surgical Treatment for Subscapularis Tear: Arthroscopic Repair and Open SurgeryArthroscopic repair is a minimally invasive surgery that uses a small camera to view the subscapularis tear. This method allows for smaller incisions and faster recovery time. Open surgery involves a larger incision and direct visualization of the tear. Both methods have high success rates and are determined by the severity of the tear. Consult with a qualified surgeon to determine the best treatment option. 💉💪 Arthroscopic repair is typically recommended for smaller tears, while open surgery is reserved for larger tears. Recovery time can vary, but physical therapy is crucial for regaining strength and mobility. Complications such as infection and nerve damage are possible but rare. Discuss potential risks and benefits with your surgeon. 💊👨⚕️ Post-operative care includes pain management, wound care, and physical therapy. It is important to follow your surgeon's instructions for a successful recovery. Return to full activity can take several months, but most patients experience significant improvement within the first few weeks. 🏋️♀️👍 In conclusion, surgical treatment for subscapularis tear can involve arthroscopic repair or open surgery. Both methods have high success rates and are determined by the severity of the tear. Post-operative care and physical therapy are crucial for a successful recovery. Consult with a qualified surgeon to determine the best treatment option for you. 💪👨⚕️6. Recovery and Rehabilitation for Subscapularis Tear: Timeline and ExercisesRecovering from a subscapularis tear can take several months. It's important to follow a rehabilitation program to regain strength and mobility. Week 1-4: Focus on gentle range of motion exercises and pain management. Week 4-8: Begin strengthening exercises with resistance bands or light weights. Week 8-12: Increase resistance and add more complex exercises. Exercises should target the subscapularis muscle, as well as the surrounding muscles that support the shoulder joint. Internal rotation with resistance band Scapular retraction with resistance band Shoulder external rotation with dumbbell Shoulder flexion with dumbbell It's important to listen to your body and not push yourself too hard, too fast. Gradual progress is key to avoiding re-injury. Other rehabilitation options may include physical therapy, massage, and acupuncture. Consult with a healthcare professional for personalized treatment. 👍 Stay consistent with your rehabilitation program and be patient with your progress. Recovery takes time, but with dedication and effort, you can regain strength and mobility in your shoulder. 💪7. Preventing Subscapularis Tear: Strengthening Exercises and Proper Technique for Shoulder MovementsStrengthening exercises are essential to prevent subscapularis tear. Proper technique for shoulder movements also reduces the risk of injury. Exercises like internal rotation, external rotation, and scapular retraction help strengthen the subscapularis muscle. Stretching exercises help improve flexibility and reduce the risk of injury. Proper technique for shoulder movements includes keeping the shoulders down and back, avoiding excessive force, and using proper form. It is important to warm up before exercising and to gradually increase the intensity of the workout. Start with light weights and gradually increase the weight as you get stronger. Listen to your body and stop if you feel pain or discomfort. Consult a doctor or physical therapist if you have any concerns about your shoulder health. Remember to rest and recover between workouts to prevent overuse injuries. Take breaks between sets and workouts to give your muscles time to recover. Get enough sleep and eat a balanced diet to support muscle recovery. Use ice or heat therapy to reduce inflammation and promote healing. By following these tips, you can prevent subscapularis tear and maintain healthy shoulders. 💪🏼👍🏼 In conclusion, subscapularis tear symptoms can be debilitating, affecting daily activities and causing pain. Early diagnosis and treatment are crucial for a successful recovery. 🏥💪 Treatment options include physical therapy, medication, and surgery. Consult with a healthcare professional for proper diagnosis and treatment. 🩺👨⚕️ Prevention is key, so avoid overuse, maintain good posture, and practice proper lifting techniques. Stay healthy and active! 🏋️♀️🌟 https://symptomfinder.com/subscapularis-tear-symptoms-causes-and-treatment/?_unique_id=6493ff901c43c
#Uncategorised#Physicaltherapy#Rotatorcuffinjury#Shoulderpain#Subscapularistear#SurgicalIntervention.#aiomatic_0
0 notes
Text
Say Goodbye to Edema with These 10 Powerful Diet Tips!
#edema#fluidretention#swelling#lymphaticsystem#treatmentoptions#diureticmedications#compressiontherapy#physicaltherapy#lifestylemodifications#surgicalinterventions#sodiumintake#potassiumrichfoods#proteinintake#hydration#fluidbalance#tissuerepair#overallhealth#healthcareprovider#personalizedcare#wellbeing#qualityoflife#inflammation#kidneydisease#heartfailure#liverdisease#lymphedema#electrolyteimbalances#nutrition#wholefoods#processedfoods
1 note
·
View note
Photo
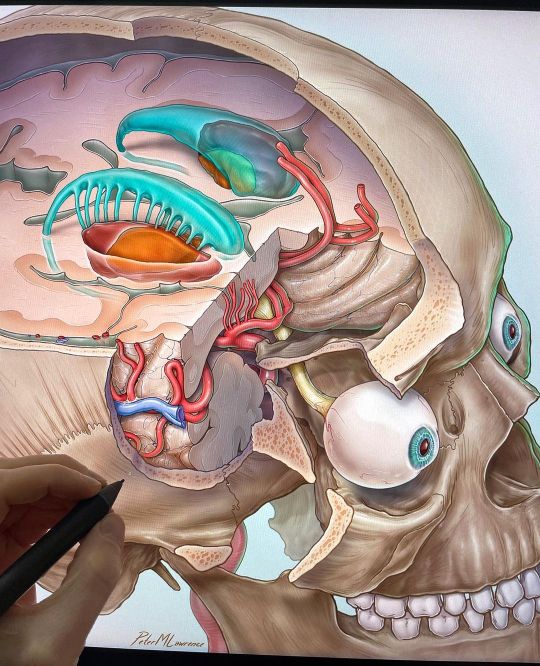
Work in progress #seven #cavernomas #neurosurgery #brainscience #neurosurgicalatlas #medicaljournal #neuroscience #residents #peerreview #medicalassistant #medstudentlife #medschool #generalsurgery #neurocirurgia #resident #learningmedicine #medicalassistantlife #spinesurgery #indirect #spinehealth #posturecorrection #decompression #backpain #spinesurgery #surgicalintervention #journalcover #neurologista (at Barrow Neurological Institute) https://www.instagram.com/p/CqIuMWKrEuv/?igshid=NGJjMDIxMWI=
#seven#cavernomas#neurosurgery#brainscience#neurosurgicalatlas#medicaljournal#neuroscience#residents#peerreview#medicalassistant#medstudentlife#medschool#generalsurgery#neurocirurgia#resident#learningmedicine#medicalassistantlife#spinesurgery#indirect#spinehealth#posturecorrection#decompression#backpain#surgicalintervention#journalcover#neurologista
18 notes
·
View notes
Text
Vocal Cord Surgery - explained By Dr. Rajesh Bhardwaj (Award Winning ENT Surgeon)
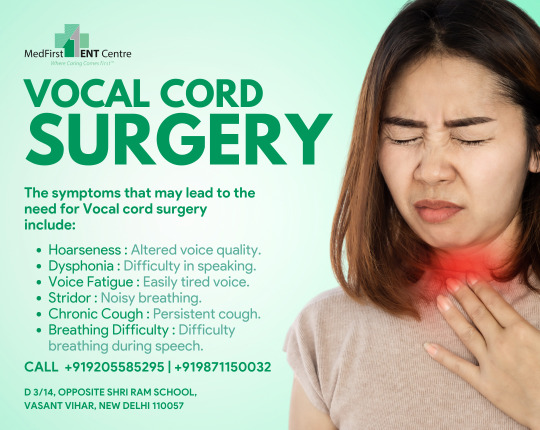
Vocal Cord Surgery
Vocal Cord surgery is performed when the vocal cords have growths, such as, polyps, tumors, or other masses that need to be removed for biopsy or to improve function.
The child will usually exhibit a hoarse or raspy voice.Vocal Cord surgery is also indicated to normalize vocal cord functioning when the vocal cords are scarred from various causes, paralyzed, or are otherwise abnormal.
These conditions may interfere with the complete opening and/or closing of the vocal cords, which is necessary for normal speech and breathing.Surgery on the vocal cords can be performed either directly in an open surgical approach (making an incision in the neck) or indirectly through an endoscopic approach (through a tube inserted into the mouth and throat).Either procedure is performed under general anesthesia (the patient is fully asleep).
Recovery after either an open or endoscopic approach includes minimizing damage to the larynx during surgery, as well as reducing inflammation after the surgery. Therefore, your surgeon will recommend the procedure he/she feels will minimize these complications.
Book Your Appointment
📲 +91 9205585295, +91 9871150032
🌐 https://entdelhi.com/
📍 MedFirst ENT Centre D 3/14, Vasant Vihar, New Delhi - 110057
https://maps.app.goo.gl/dksVuepUe7VxtBvz9
#VocalCordSurgery #ENTProcedure #VoiceHealth #SurgicalIntervention #VocalCordTreatment #VoiceRestoration #ENTCare #SurgicalVoiceCorrection #VocalCordRecovery #VoiceWellness #ENTSpecialist #SpeechTherapy #VocalHealth #SurgicalInnovation #VoiceCare #VoiceRehabilitation #HealthcareIntervention #VocalCordIssues #SurgeryForVoice #VoiceQualityImprovement
0 notes
Text

Discover hope and healing at Gunjan Hospital. Our expert team specializes in compassionate Fistula treatment, restoring lives one step at a time.
Contact us for appointments:-
Email Id:- [email protected]
Phone :- +91 9319358937
#gunjanhospital #hospital #treatment #FistulaTreatment #MedicalCare #Healthcare #SurgicalTreatment #HealingJourney #MedicalSpecialists #PatientCare #SurgeryRecovery #HealthAndWellness #FistulaSupport #SurgicalIntervention #RecoveryProcess #FistulaSurgery #MedicalProcedure #QualityHealthcare #MedicalRecovery #HealthcareExperts #FistulaCare #HospitalTreatment #ExpertMedicalCare
0 notes
Text
Hybrid Surgical/Interventional LV Reconstruction Improves Ejection Fraction and Patient Symptoms
Hybrid Surgical/Interventional LV Reconstruction Improves Ejection Fraction and Patient Symptoms
Although it’s early and the data are slim, using anchors to plicate and excide the fibrotic tissue appears to offer some promise for ischemic HF.
CHICAGO, IL—An unconventional approach to combat left ventricular remodeling following myocardial infarction appears to improve heart function and patient symptoms, although investigators caution it’s still early days for the new ventricular…
View On WordPress
0 notes
Photo

Amy Reveals Her Weight Loss! | 1000-lb Sisters http://ehelpdesk.tk/wp-content/uploads/2020/02/logo-header.png [ad_1] Tammy holds a party to show off ... #1000poundsisters #1000pounds #1000-lbsisters #1000lbsisters #acupressure #amyslaton #aromatherapy #arttherapy #cbt #dance #energyhealing #fat #fattvshow #fatvideo #fitness #health #healthcoaching #heavy #herbalism #hypnotherapy #massage #meditation #morbidlyobese #nutrition #overweight #overweightpeople #overweightsiblings #overweightsisters #pilates #qigong #realitytvseries #slatonsisters #surgicalintervention #taichi #tammyslaton #tlc #tlcfullepisodes #tlcshows #weightissues #weightloss #yoga
0 notes
Link
🌬️ Pneumobilia is a condition where air enters the biliary tree, causing symptoms such as abdominal pain, nausea, and vomiting. It is a rare condition that can be caused by various factors, including surgery, trauma, or infections. In this article, we will discuss the causes, symptoms, and treatment options for pneumobilia. 👨⚕️ The symptoms of pneumobilia can be vague and nonspecific, making it difficult to diagnose. Patients may experience abdominal discomfort, bloating, and indigestion. In severe cases, they may also develop jaundice, fever, and chills. It is important to seek medical attention if you experience any of these symptoms. 💊 Treatment for pneumobilia depends on the underlying cause. In some cases, the condition may resolve on its own without any intervention. However, if the symptoms persist, your doctor may recommend imaging tests such as ultrasound or CT scan to identify the cause. Treatment options may include antibiotics, surgery, or endoscopic procedures to remove the air from the biliary tree.1. Understanding Pneumobilia: Definition and CausesPneumobilia is the presence of air within the biliary tree. It is a rare condition that can be caused by a variety of factors, including gallbladder surgery, trauma, and infection. Symptoms of pneumobilia can include abdominal pain, nausea, vomiting, and jaundice. Diagnosis is typically made through imaging tests such as CT scans or MRIs. Treatment for pneumobilia depends on the underlying cause. In some cases, no treatment is necessary as the air will naturally be absorbed by the body. Complications of pneumobilia can include bile duct obstruction, cholangitis, and sepsis. It is important to seek medical attention if you experience any symptoms or have a history of gallbladder surgery. Prevention of pneumobilia includes proper management of gallbladder surgery and avoiding trauma to the abdomen. Early detection and treatment can lead to a better outcome. 🔎 Did you know? Pneumobilia can also be caused by a rare condition called pneumatosis cystoides intestinalis, which is the presence of gas-filled cysts in the intestinal wall.2. Common Symptoms of Pneumobilia: What to Look Out For Abdominal pain Jaundice Nausea and vomiting Fever Loss of appetite These are some of the common symptoms of pneumobilia. It occurs when air enters the bile ducts, causing discomfort and pain. If you experience any of these symptoms, seek medical attention immediately. Early detection is key to preventing complications. Other symptoms may include bloating, indigestion, and diarrhea. These symptoms can be confused with other conditions, so it's important to consult a doctor for proper diagnosis. Pneumobilia can be caused by gallstones, infections, or surgery. In severe cases, pneumobilia can lead to complications such as cholangitis or pancreatitis. These conditions can be life-threatening if left untreated. Treatment options may include antibiotics, surgery, or endoscopic retrograde cholangiopancreatography (ERCP). Don't ignore the symptoms of pneumobilia. Seek medical attention as soon as possible to prevent complications. Remember, early detection is key to a successful recovery. 🩺💊3. Diagnostic Tests for Pneumobilia: How to Confirm the DiagnosisSeveral diagnostic tests can confirm pneumobilia, including: Abdominal X-ray: shows air in the biliary tree Ultrasound: identifies air in the bile ducts CT scan: detects air in the biliary system and potential causes Magnetic resonance cholangiopancreatography (MRCP): visualizes the biliary system and identifies any obstructions Endoscopic retrograde cholangiopancreatography (ERCP) can also diagnose and treat pneumobilia by removing any obstructions causing the condition. Other tests may be necessary to determine the underlying cause of pneumobilia, such as blood tests, liver function tests, and a biopsy of the liver or bile ducts. It's crucial to confirm the diagnosis of pneumobilia to determine the appropriate treatment plan and prevent potential complications. Consult with a healthcare professional if you experience symptoms of pneumobilia, such as abdominal pain, jaundice, or fever. 🩺💉👨⚕️👩⚕️4. Treatment Options for Pneumobilia: Surgery, Medications, and MoreThere are various treatment options for pneumobilia, including surgery, medications, and more. Surgery: Surgery is the most common treatment for pneumobilia. The surgeon will remove the obstruction causing the bile to enter the liver. Medications: Medications can be used to treat the underlying condition causing pneumobilia, such as antibiotics for infections or bile acid sequestrants for bile acid malabsorption. ERCP: Endoscopic retrograde cholangiopancreatography (ERCP) can be used to remove gallstones or other obstructions in the bile ducts. Stenting: Stenting can be used to keep the bile duct open and allow the bile to flow freely. Observation: In some cases, observation may be the best course of action if the pneumobilia is not causing any symptoms or complications. Prognosis: The prognosis for pneumobilia depends on the underlying cause and the severity of the condition. Prevention: Preventing gallstones and other obstructions in the bile ducts can help prevent pneumobilia. 🩺 Remember to always consult with your doctor to determine the best treatment option for your individual case. 🩺5. Complications of Pneumobilia: Risks and Prevention MeasuresComplications of pneumobilia can be serious and even life-threatening. Risks include bile duct obstruction, sepsis, and perforation. Prevention measures include early diagnosis, proper treatment, and close monitoring. 🚨 Bile duct obstruction can lead to jaundice, abdominal pain, and fever. Sepsis can cause organ failure and death. Perforation can result in bile leakage and peritonitis. Timely intervention is crucial. 💉 Endoscopic retrograde cholangiopancreatography (ERCP) is the preferred diagnostic tool. Treatment options include sphincterotomy, stent placement, and surgery. Antibiotics may be necessary in case of infection. 🩺 Close monitoring is essential to detect any recurrence or complications. Follow-up imaging and blood tests are recommended. Lifestyle changes such as a low-fat diet and regular exercise can also help prevent recurrence. 🏃♀️ In conclusion, pneumobilia can have serious consequences, but early diagnosis, proper treatment, and close monitoring can prevent complications. If you experience any symptoms, seek medical attention immediately. 🚑6. Prognosis and Recovery for Pneumobilia Patients: What to ExpectAfter treatment, most patients with pneumobilia recover fully. 🎉 However, the prognosis depends on the underlying cause. Biliary obstruction: Patients with this condition may need further treatment to prevent recurrence. Gallstones: Surgery may be necessary to remove the gallbladder and prevent future complications. Infection: Antibiotics are usually effective in treating infections, and patients recover quickly. Recovery time varies depending on the severity of the condition and the patient's overall health. 💪 Patients may experience discomfort and fatigue during recovery. Diet: Patients may need to follow a low-fat diet to prevent future gallstones and biliary obstruction. Follow-up: Regular check-ups with a doctor are necessary to monitor recovery and prevent complications. Lifestyle changes: Quitting smoking and reducing alcohol consumption can improve overall health and prevent future complications. Overall, the prognosis for pneumobilia patients is good with proper treatment and follow-up care. 🙌 In conclusion, pneumobilia symptoms can be caused by a variety of factors such as gallstones, tumors, or infections. It is important to seek medical attention if you experience any of the symptoms mentioned in this article. Early detection and treatment can prevent complications. Treatment options for pneumobilia vary depending on the underlying cause. Surgery may be required to remove gallstones or tumors. Antibiotics may be prescribed for infections. Consult with your healthcare provider to determine the best course of action for your specific case. 🏥💊 Remember to prioritize your health and seek medical attention if you experience any unusual symptoms. Stay informed and take care of yourself. 🙌 https://symptomfinder.com/pneumobilia-symptoms-causes-and-treatment/?_unique_id=647c354e3628b
#Uncategorised#BileDuctObstruction#EndoscopicRetrogradeCholangiopancreatography#GallstoneIleus#PneumobiliaSymptoms#SurgicalIntervention.#aiomatic_0
0 notes
Photo

Work in progress on #7Cavernomas, subtypes of medullary lesions. @Barrowneuro #medicaljournal #neurosurgicalatlas #residents #medschool #brainscience #peerreview #medstudentlife #generalsurgery #neurocirurgia #resident #learningmedicine #medicalassistantlife #spinesurgery #indirect #spinehealth #posturecorrection #decompression #backpain #spinesurgery #surgicalintervention #journalcover #neurologist #medicalassistant (at Phoenix, Arizona) https://www.instagram.com/p/CZmZqcPFWkn/?utm_medium=tumblr
#7cavernomas#medicaljournal#neurosurgicalatlas#residents#medschool#brainscience#peerreview#medstudentlife#generalsurgery#neurocirurgia#resident#learningmedicine#medicalassistantlife#spinesurgery#indirect#spinehealth#posturecorrection#decompression#backpain#surgicalintervention#journalcover#neurologist#medicalassistant
2 notes
·
View notes