#SARS COV 2
Explore tagged Tumblr posts
Text
I’m so sorry I can’t describe images rn (shoutout long covid brain fog!), but the last two images purrsian-likethecat added seem to be of a graph, and a map of the United States. I can’t really tell what information is on there though as my wifi sucks rn and my magnifier doesn’t help with blurry text :/
I’ll try to edit this when I can describe things better tho so if u see this version rb’d, double check if I already have
Data source: https://pmc19.com/data/
#kinda described#mostly described#incomplete id#id in rb#id in alt text#mask up#public health#wear a mask#wear a respirator#covid isn't over#long covid#pandemic#sars cov 2#covid 19#still coviding#kipo tangents
5K notes
·
View notes
Text
If you have a cold and test negative for COVID you are not in the clear. Tests take a while to turn positive. Meanwhile you are spreading COVID to family and friends. Mask up if you have any symptoms. This virus is just evil.
20K notes
·
View notes
Text
Salmonella is "a part of life" too, but y'all don't go around forcing others to lick raw chicken. Why have you given up all caution around covid and other airborne diseases?
#covid is airborne#covid is still a thing#covid isn't over#covid 19#covid#sars cov 2#pandemic#covid pandemic#covid posting#covid awareness#covid conscious#covid cautious#public health
2K notes
·
View notes
Text
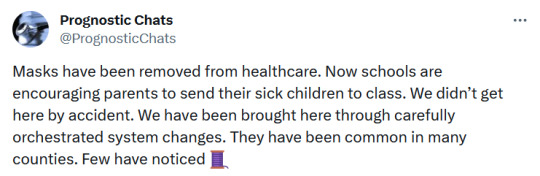
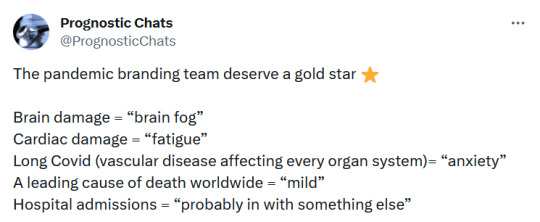
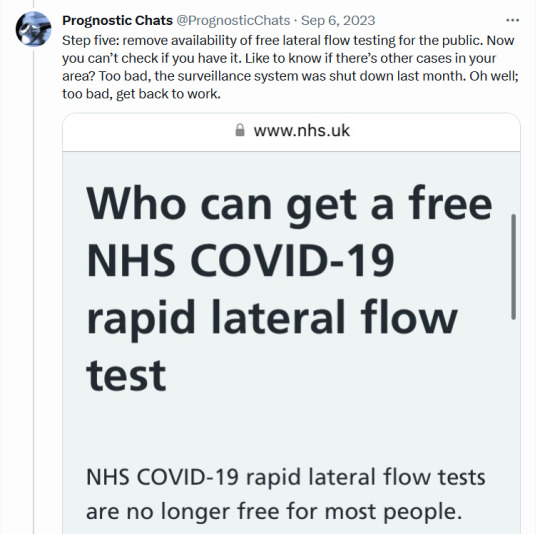
Politically, governments decided to sell a “we beat the pandemic” narrative to the public after vaccines failed to produce herd immunity as promised. For this reason, political health bodies like the CDC began putting out guidance from the very top encouraging people to accept the “new normal” of unending reinfections. Acceptance of constant reinfections relies heavily on the perception that COVID infections are a truly neutral event for your health- something that no research, and no study, has ever concluded.
COVID infection endangers pregnancies and newborns. Why aren't parents being warned?
5K notes
·
View notes
Text
tumblr just nuked @milf-adjacent's blog with zero warning, no explanation from staff or e-mail whatsoever. her blog has been a vital resource for documenting COVID-19, and she did nothing ban worthy. she seems to be another target of the transmisogyny being carried out by staff.
#covid 19#covid pandemic#mask up#sars cov 2#covid isn't over#tags for spreading the word#please get it out there!!#milf-adjacent
6K notes
·
View notes
Text
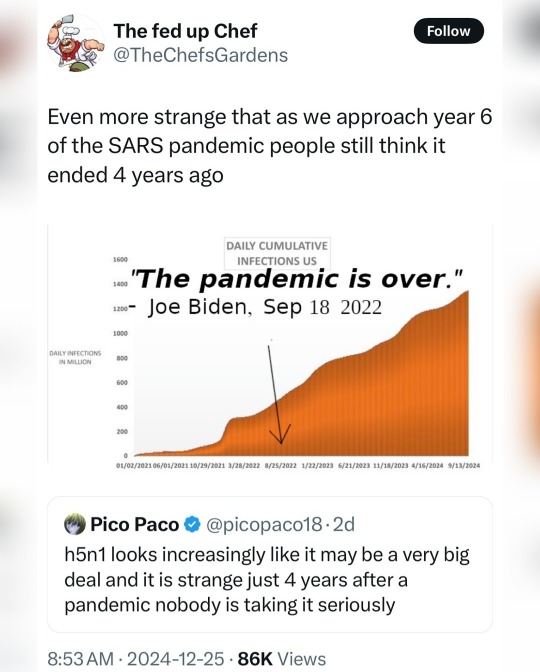
#covid isn't over#h5n1 bird flu#covid 19#covid#h5n1 virus#h5n1#bird flu pandemic#bird flu#yallmasking#yall masking#wear a mask#mask up#still masking#still isolating#still testing#still coviding#still living#sars cov 2
433 notes
·
View notes
Text
I’m seeing a lot of folks reblogging my post about free covid tests talking about being low income, so I wanted to throw out another resource for yall!
Find your local mask bloc! They’ll have free high quality masks, and many also have free tests!
Maskbloc.org has a great list of them including some outside the US!

#covid#covid is airborne#covid isn't over#mask blocs#free covid tests#free resources#mask up#sars cov 2#covid 19
456 notes
·
View notes
Text







#sars cov 2#covid isnt over#pandemic isnt over#wear a mask#wear a fucking mask#alt text covid#world issues#disability rights#disability justice#important#nonfiction
1K notes
·
View notes
Text

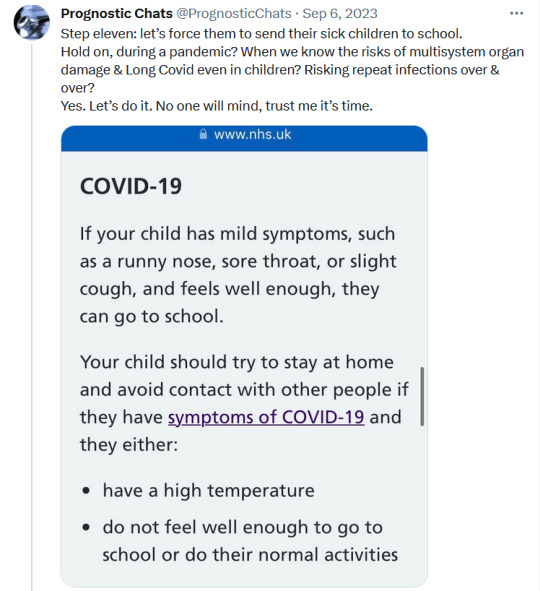
learn more at
#covid 19#covid conscious#still coviding#covid isn't over#covid#sars cov 2#wear a mask#school season
124 notes
·
View notes
Text
Source
#mask up#public health#wear a mask#wear a respirator#pandemic#still coviding#covid#covid 19#coronavirus#sars cov 2#long covid#covid conscious#covid19#covid is airborne
226 notes
·
View notes
Text

My husband who worked in healthcare gasped when he looked at the graphs. Our immune systems have been damaged by Covid. Click on the link View on Twitter to see the post
A few people have asked me where the graphs come from. This is the work of someone who has looked at the data and posted their observations. If you can't access Twitter to see the rest of the post then I cant help you. There are explanations there about the graphs.. I am sorry I can't give you more information. I tried to copy more of this thread but Tumblr won't recognize the link. As far as I know the information is valid, but as we all know you must question everything today.
I went back and copied 2 of the sources used for the graphs in the thread. There were some questions for others on the data used, and this was what the person who posted said he used. I do not have the background to ascertain how accurate the graphs are. This is the best I can do.
Other graphs were also posted which were discussed.


1K notes
·
View notes
Text
I hate that the average person is stupid and inattentive enough to be tricked by the media rebranding covid waves every 8 to 12 months. It was "waves" in 2020 and 2021 with each new variant getting a greek letter, then it was "surges" in 2022 with alphanumeric codes for each new variant, then it was "upticks" in 2023 and you were lucky if they posted what clade the current variants were in, and now in 2024 it's "bumps" with journalists misconstuing the name of a variant's spike protien mutation for the variant name and some covid minimizing doctors trying to claim "this is just descended from omicron" when the covid evoution chart looks like this

2K notes
·
View notes
Text

#covid 19#covid#covid isn't over#communism#anti capitalism#socialism#anarchy#leftism#sars cov 2#long covid#i think i hauve covid#mask up#pandemic#hood#mask girl#mask kink#mask k!nk#mask k1nk#covid masks#cdc#paxlovid#covid19#covid pandemic#covid is not over
314 notes
·
View notes
Text

SARS-COV-2 PCR percent positivity during the four-week reporting period from 24 June to 21 July 2024, increased from 7.4% in the beginning week of the reporting period to 13.0% in the last week across 85 countries.
Globally, JN.1 is the most reported variant of interest (VOI), accounting for 25.7%.
The number of new cases and deaths increase by 30% and 26% compared to the previous 28-day period. Over 186,000 new cases with more than 2,800 new fatalities reported.
As of 21 July 2024, over 775M confirmed cases and more than 7M deaths have been reported globally since the beginning of pandemic.
https://www.who.int/publications/m/item/covid-19-epidemiological-update-edition-170
102 notes
·
View notes
Text
"You might think that because you’ve had COVID-19 and lived through it that repeat infections will impact you similarly, but “reinfections aren't harmless. As cases continue to rise and more variants arrive on the scene, infectious-disease experts are warning that repeat infections could have cumulative, lasting effects.”
...If you want to maintain your current level of health and avoid potential damage to your body & organs (up to and including your brain & your heart) and/or want to live as long as possible, taking precautions to prevent COVID-19 infections is crucial."
#The Overstimulated#Substack#Personal Blog#Personal Experience#personal health#Disabled Writer#Disability#Disabled Experience#Disabled Blogger#chronically ill#chronic pain#chronically ill community#chronic illness#chronically ill blogger#covid isn't over#still masking#still isolating#still testing#covid#covid 19#covid19#sars cov 2#still coviding#still living#still relevant
411 notes
·
View notes
