#Post-op respiratory failure
Explore tagged Tumblr posts
Text
PATIENT MEDICAL RECORD SURGICAL REPORT #957
Patient Name: Misha Lupical Age: 14 Sex: Male Date of Surgery: ██ ██ ███ Surgeons: Doctor Paene Lupical, Petya Yordanovich (cardiologist) Anasthesiologist: Malcolm Grey Procedure: Organ Transplantation and Cardiovascular Augmentation
PRE-OP NOTES
Diagnosis: Multiple organ failure (lungs, gallbladder, liver, kidneys, spleen) due to malignancy and systemic toxicity; cardiovascular inefficiency requiring augmentation
Planned Procedure:
Organ Transplants: - Gallbladder, lungs, liver, kidneys, spleen excision and synthetic organ implantation - Major arterial and venous reinforcement with synthetic materials - Connection of transplanted organs to neurological implant
Cardiovascular Augmentation: - Secondary four-chamber heart implantation (continuous steady-state circulation with pre-coded heart rates for rest and different exertion modes)
Structural EnhancementsL - Endoskeletal reinforcement with flexible carbon-fiber mesh (beneath ribs)
Anesthesia plan: - General anesthesia with neuromuscular blockade - Continuous hemodynamic and neurological monitoring - Peripheral nerve stimulation for post-op functional assessment INTRA-OP NOTES:
Anesthesia Induction: - Patient intubated and placed under general anesthesia by anesthesiologist Malcolm Grey - Central venous access obtained (catheter inserted in subclavian vein) - Cardiopulmonary monitoring initiated
Intra-operation Actions: - Diseased lungs, liver, spleen, gallbladder, and kidneys removed - Synthetic organ replacements positioned and vascular connections established by Doctor Petya Yordanovich - Major arterial and venous structures reinforced with synthetic conduits - Endoskeletal mesh placed beneath ribcage; no interference with respiratory motion detected
Complications: - Initial rejection response to liver implant triggered hypercytokinemia, requiring instant immunosuppressive therapy - Temporary hypotension following spleen replacement; stabilized with IV fluids - Unexpected clot formation near secondary heart implantation site, requiring immediate removal and anticoagulant administration - Delayed vascular integration of synthetic kidneys, leading to brief renal hypoperfusion; resolved with perfusion adjustment
Closure & Recovery: - Hemostasis confirmed across all surgical sites - Incisions closed with bio-compatible sutures and synthetic dermal grafts - Patient transferred to ICU for post-op observation POST-OP NOTES:
Immediate Post-Op Status: - Patient successfully extubated, spontaneous respiration intact - Secondary heart maintaining consistent circulation with expected oxygen levels (confirmed by Dr. Petya Yordanovich) - Moderate pain and discomfort noted, managed with analgesics
Complications: - Acute hypertension episodes likely cause by vascular reinforcement adaptation; managed with a vasodilator medication - Persistent metabolic imbalance due to synthetic liver requiring enzyme therapy for stabilization - Mild pulmonary edema in left synthetic lung, resolving with respiratory support Ongoing Monitoring & Adjustments: - Secondary heart function optimization for long-term stability - Periodic enzyme regulation assessment for synthetic liver - Renal output monitoring for continued integration - Regular pulmonary function tests for synthetic lung efficiency
Discharge Plan: - Estimated hospital stay - 12-16 days - Physical rehabilitation for systemic adaptation (done by Doctor Lea Anderson and physical therapist John O'Nella) - Regular biomonitoring for cardiovascular and organ function stability - Regular neural implant monitoring to check for the integration of transplanted organs and their proper function
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
tags: @tobeyinabox
2 notes
·
View notes
Text
X-Plain New and Updated Topics
The Patient Education Institute has published, reviewed or updated 91 titles in Q1 and Q2 2023. We provide each topic in 5 instructional formats (tutorial, video, illustrated handout, XML, and overview).
Alcohol Use Disorder Amyotrophic Lateral Sclerosis (Arabic) Angina Arixtra Arrhythmias Asperger's Syndrome (Arabic) Asthma - Pediatric (Arabic) Atherosclerosis Atrial Flutter (Spanish) Attention Deficit Hyperactivity Disorder - ADHD (Arabic) Back Pain - Introduction to Pain Management Blepharoplasty - Eyelid Surgery Blood Pressure Medicines (Arabic) Bone Densitometry Breast Cancer - Hormonal and Targeted Therapies Breast Cancer - Hormonal and Targeted Therapies (Arabic) Bunionectomy Bursitis (Arabic) C. difficile Infections Cardiac Ablation for Atrial Fibrillation Cardiac Rehabilitation (Arabic) Cataract Surgery Cerebral Angiogram Chagas Disease (Arabic) Chemotherapy for Breast Cancer - General (Arabic) Chickenpox Cholera (Arabic) Colon Cancer (Spanish) Colon Cancer Surgery (Arabic) Colorectal Cancer (Arabic) Cystocele Dilation and Curettage (Spanish) Dust Mite Allergy Dystonia Erectile Dysfunction - Penile Implants Fetal Alcohol Syndrome Fibromyalgia Forehead Lift Galactosemia Gout (Spanish) Healthy Sleeping Hearing Problems in Children (Arabic) HIDA Scan HPV - Warts Hydrothermal Endometrial Ablation Incentive Spirometer Incentive Spirometer - Pediatrics Intrathecal Morphine Pump Placement Juvenile Idiopathic Arthritis (Arabic) Knee Replacement - Preventing Post Op Complications (Arabic) Living Healthy (Spanish) Living with Congestive Heart Failure Lung Cancer (Spanish) Lupus Lyme Disease (Arabic) Massage Therapy Meditation Melanoma Menstruation (Arabic) Miscarriage (Arabic) Monkeypox Multiple Sclerosis (Spanish) Nail Diseases and Problems (Arabic) Neuroblastoma (Arabic) Neurofibromatosis Non-Hodgkin's Lymphoma Nutrition During Cancer Treatment Pancreas Transplantation (Arabic) Personality Disorders (Arabic) Pregnancy - First Trimester - What to Expect Pregnancy - Second Trimester - What to Expect Pregnancy - Third Trimester - What to Expect Prenatal Testing (Spanish) Preventing Catheter Associated Bloodstream Infections (Arabic) PSA - Screening for Prostate Cancer Rhinoplasty Rubella Schizophrenia Severe Acute Respiratory Syndrome - SARS Sickle Cell Anemia (Arabic) Sigmoidoscopy Simpson-Golabi-Behmel Syndrome - SGBS Skin Cancer - Non-Melanoma (Spanish) Smoking Cessation Tendinitis (Arabic) Treatment of Myelodysplastic Syndromes - MDS Understanding the Different Types of Myelodysplastic Syndromes - MDS (Spanish) Urinary Tract Infections in Elderly Adults Uterine Diseases (Arabic) VP Shunts Warfarin - Review for Current Users - Pediatrics
2 notes
·
View notes
Note
Can you explain or cite where in the study it provides any data on the topic of autism's interaction with suicide risk?
I read through and I can't figure out where you got that from this study. Nobody who died in the study died of suicide.
(The 26 deaths were, respectively, (5), cardiac arrest (5), seizures (3), respiratory failure/pneumonia (3), choking on food (2), medication side effects (2), accidental poisoning (1), or unknown (5).)
Good point- looks like I got the information wrong, furthering the point of the OP’s post.
I’ve seen various studies and articles explaining correlations between various mental health difficulties and autism that could increase the risk of suicide, but yes good to remember correlation doesn’t equal causation.
But yes I’ve seen too many people online use the statistic from that article as their main point to encourage people to support autism support systems and self diagnosis. Although I want those two things to be encouraged still, the constant repetition and reminder of this study was really upsetting and at times debilitating during my post diagnosis/burnout/self discovery process.
0 notes
Text


symblepharon (pronounced sim-Blef-er-on, meaning “joined eyelid”) is a condition where the conjunctival tissue of the eye sticks together (or to the cornea) in a way which can physically obscure vision, and sometimes cause problems with tear drainage, etc. in kittens, this often happens as a sequela of herpesvirus infection at a very young age. surgery (I have learned from experience) has a high rate of post-op failure due to the adhesion reforming (which just happened to my buddy Mustard here). Herpes lies dormant in cats and flares up in times of stress, causing chronic, intermittent, mild upper respiratory symptoms in otherwise healthy cats. We can expect Mustard to live a long and active life, possibly with a few visits to the ophthalmologist and/or some eye drops along the way.
5 notes
·
View notes
Note
o great robin, tell us about organ failure. i wanna know what happens when someone's pancreas decides to nope out
ok so I’m on a stepdown ICU which means you’re not quite sick/unstable enough to warrant being in Intensive Care but you’re also not well enough that you can be on a regular floor bed. I’m on a general Medical floor (as opposed to Surgical, Peri-Op, etc) so we see patients with lots of chronic issues and comorbidities in addition to acute issues.
Top things I see: DKA (high sugar, need insulin drip and education), Sepsis (blood infection, antibiotics and wound care usually), CHF Exacerbation (heart failure, usually fluid overload so diuresing), cancer (chemo, radiation, surgery, preventing secondary issues from killing them) HTN emergency (high BP, get them on BPs meds, diuresing), various respiratory illnesses from Pneumonia to Covid (o2, antibiotics, steroids), AWS/COWS (alcohol or drug OD, gently getting them past seizure threshold with benzos) and Pre/Post- Transplant d/t organ failure.
Listen, modern medicine is amazing but transplants suck. They save lives but the a) exhaustive work up to transplant b) anxiously waiting for transplant c) going through the surgery d) the rigorous process of keeping the transplant e) the very likely possibility of rejection/failure within 5 years is just... not great. The failing organs/transplants we see on my floor most often are liver, kidney, lungs and occasionally the pancreas which can be paired with kidney transplant. Hearts have their own unit bc that shit is cray (they just... leave the chest open after surgery in case they need to go back in. They essentially cover the open chest with saran wrap. This image haunts me and I want nothing to do with that shit)
Kidney transplants usually are the easiest with the highest chances of success. I’ve had patients come in with transplants that have been going strong for a decade. Lung transplants are tricky and its so hard watching people do bad both before and after the transplant, watching the grief in their eyes when they realize the transplant isn’t a magical cure all. I think livers are the worst for me, liver failure (both alcoholic and NASH) causes swift physical and mental decline in which the patient can become a whole other person. Most of my liver patients have tried to physically fight me at some point, in between vomiting and having their abdomen swell to terrifying proportions from ascites. We pulled 8 liters off a man’s belly about a week ago. That’s 4 two liter soda bottles my friends.
When I first started my job, we had a lung transplant work-up on our floor. She was with us for an entire year, too stable for an ICU but on waaay too much oxygen to go home. We loved this lady, walked her around the unit every day shape which took almost an hour because she had to go so slow less we overwhelm her crappy lungs. She got transplanted and we celebrated only for it to not take well and her to spend another year in the cardiac ICU when her new transplant caused heart failure. We heard she died during Covid times after never leaving the hospital for 2 years. It still makes me sad to think about her.
Some people just live with chronic organ failure, too unstable to risk surgery or deemed by the powers that be not to be a suitable candidate for whatever reason. We have maybe a dozen patients that we see every 6 mo or so for exacerbations of these issues that we can’t really treat the underlying cause so we just patch a bandaid over the failing organ and send them away until next time. One lovable frequent flyer said “it’s good to be home” one of the times he was wheeled up to us from the ER.
TLDR: organ failure sux but so too does transplant, they’ll both cause you misery. Kidneys are fab, livers make you punchy, lungs make you sad.
#adventures in nursing#we get so many transplant work-up or post transplant patients#they make me so sad bc most of them don't do well#anyway hope someone finds this interesting#I could go on and on about the Shit I Have Seen#Anonymous
21 notes
·
View notes
Text
Watching House as a Physician. Season 2 Episode 3. Infectious diseases & Respiratory.
Welcome to another episode of medicine done badly. I’ve been watching House on Amazon prime. Got the subscription during the pandemic, as like everyone else, I’ve garnered an online shopping habit now.
Alright. In the opening scene a young roof worker falls off the roof presumably due to acute shortness of breath. i.e. trouble breathing. (why do we use the term shortness of breath? it’s the english version of the greek term dyspnoea - the actual preferred language of Western doctors. Fuck do I know why we like Greek and Latin so much. Moving on.) Then cut to Dr. Cuddy examining him in the back of the ambulance.

This would never happen in real life. Yes you can be on the scene and handover to the paramedics or EMT when they arrive as a doctor. But they would take over. I personally wouldn’t have the balls to look after a patient in a different environment, different resources and field I’m not familiar with. You can have field Emergency docs - but requires different training.
Also, ethically, you’re not meant to treat family or friends. Dr. Cuddy later in the episode gets a bit emotionally involved - this is why we don’t treat people close to us. We lose objectivity. We make mistakes. And you see later see Cuddy do some pretty bad ones.
I feel like much of this episode is not really IM. THere’s less differential diagnoses being made. More side tracks into trauma, emergency, intensive care or vascular surgery.
Anyhoo. Trauma and emergency would manage the fall and post fall traumatic injuries. And the trauma protocol was either not shown or completely off in this episode. Surgeons don’t seem to exist in House, at least not very much. Similarly, no other doctors exist except surgeons in Grey’s anatomy. Also you can’t clear a C Spine clinically, which is what Dr. Cuddy does in the back of the ambulance. You’d need a CT first and clearance both radiological (by a radiologist) and a clinician.
Aaaanddd, you can’t just listen to the chest and go no pneumothorax (air in lung or collapsed lung) - yes it’s reassuring, but again you’d need imaging to confirm this, given how serious a condition this is. It is realistic to consider in the setting of a fall, particularly if there are rib fractures that can puncture the lung.
Once the more critical injuries are managed, we would look after the IM side to things.
So. Finally.. differential diagnoses.
Takes what seems and feels like days before they finally sit down and go through differentials. Really not much on that white board. Dark fingers, broken ribs, fever and lung infiltrates. Time line’s not clear on when he developed the fever.
Presenting complaint isn’t really addressed. It could be: - Dyspnoea, leading to the fall, he’s requiring O2 via nasal prongs, which suggests that he’s hypoxic (this is definitely odd in a young guy who’s normally very physical fit if he works as labourer). so much to unpack here, but they never get into this well. Post fall, Cuddy notices his ring and pinky finger becoming dusky, which becomes very central in this episode. Very few things would cause this. pains me that they do no differentials on a white board for this alone.

Then a lot of throwing around medical terms.
PTT prolonged and Fibrinogen off. These are markers of your coagulation pathway and signs that you’re not forming the clots the way you should if you have an injury. DIC is also thrown around. What is DIC? Disseminated intravascular coagulopathy. Certainly severe sepsis and trauma can cause this and lead to severe bleeding. It will throw off your coagulation pathways (things that stop bleeding). It’s not common. I’ve treated it once, while I was rotating in ICU, it is not standard ward medicine practice. Standard therapy is fresh frozen plasma (FFP) and even large metropolitan hospitals only have a limited supply. It’s a huge concern for surgery and post-op (as you patient will just not stop bleeding after you cut them open, and if not treated, potentially bleed to death). Cuddy mentions ARDS. Acute respiratory distress syndrome, it could be a complication, but it’s not a cause. Again, falls more into the realm of critical care (a la ICU). However, patient had SOB prior to the fall. Finally HOuse makes the observation. of “what if he was sick before he had his run in with gravity...” Everyone jumps to Pneumonia. And this is where it gets confusing. If he was unwell, the minute he entered the emergency department with a fever and hypoxia, they would have worked him up for any garden variety pneumonia, bacterial or viral. Cultures would have been sent and imaging. Any young hypoxic patient would prompt a closer look at the chest. And no one waits that long to start antibiotics - “sepsis kills” is a slogan often used around hospitals. You have to initiate empirical therapy within 30 mins, to reduce mortality and morbiditiy.
Ordering an Echocardiogram (USS of the Heart) also makes no sense in the context of a lung infection. I would order one, but not to look at the lungs.
Then there’s the most unrealistic thing about this series. Doctors breaking into patient homes.
It is however, a good way to showcase social history. It’d be boring to watch a doctor ask the patient outright about their living situation etc, but it’s far more interesting to see exactly how they live. We try as much as possible to illustrate to each other and ourselves what the living environment and working environment of our patients are like.
In the context of infection, a good social history can point out exposure. As they exemplify by showing dead rodents and mould. This leads to 2 further differentials: Rat bite fever (caused by streptobacillus, something you’d see in the US, but probably not anywhere else), it’s an unrealistic differential in general. And the 2nd is aspergillosis. Okay.. So aspergillus is a mould commonly found in our environment. In fact it’s everywhere around us.
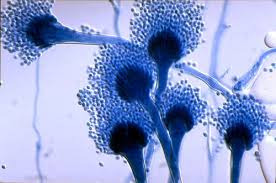
THere’s few times when it’s an issue. It is a concern in respiratory syndromes like asthma or bronchiectasis. And also as an opportunistic infection in immunocompromised individuals. in the context of asthma, it’s not so much the aspergillus itself that causes issue, it’s our body’s over reaction. It’s a hypersensitivity issue that causes inflammation in the lungs or a pneumonitis. We even gave it a name. Allergic bronchopulmonary aspergillosis. It’s still badness, but it doesn’t happen that quickly. We also have specific tests for this, which were obviously not considered in this episode of medicine done badly. In the immunocompromised host (steroid therapy in transplant patients or those on chemo, etc.), you can get the invasive mould as an opportunistic infection. I don’t really understand why they think it would be the case here. Also, killing the bug with heavy duty anti fungals will only give more issues rather than do anything. They start him on amphotericin. this is not standard practice. And now it flips to why amphotericin is not standard practice or first line treatment for invasive aspergillosis. The patient has now become anuric (not making any urine). (First line drug by the way is voraconazole, superior efficacy in trials with a lower mortality rate and ADRs) Also, note that they have just jumped straight to dire renal failure from the amphotericin. No work up. That said, heavy drugs like amphotericin are often a cause, but It’s often temporary with the appropriate supportive measures (stop insulting agents, give hydration, monitor fluid balance), reversible, even if you require temporary dialysis or haemofiltration. Anyways, would get into AKI another day, that’s a whole other post in and of itself. Then his hand is apparently “dying.” There’s pain on light touch, but it’s not a cold, pulseless limb. Or discoloured. doesn’t add up. This now enters vascular surgeon territory. Again. It’s interesting that there’s never any referrals to any other teams. If he has good circulation, I would imagine they would try to save the hand and consider other differentials.
The only time I can think of an emergency amputation in this situation is necrotising fascitiis. That’s the only thing that would occur that rapidly AND necessitate losing tissue or limb. With a young person who’s this ill, there’s often multiple subspecialties involved by this point. I’m also surprised he’s not in ICU.
Then there’s a buncha filler scenes of the cast of house getting emotional. Ho my god, they’ve taken the hand of a young 20 something physical labourer. Indeed, this is badness. Unlike House, we actually are trained to always consider how a patient’s illness impacts their activities of daily living and livelihood.
I find the general population assumes that we practice medicine in a vacuum, we merely treat the clinical illness and ignore everything else. They imagine that we all must be like house.
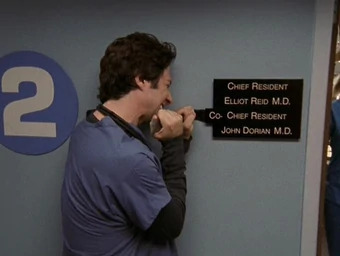
Actually we try to put things in perspective as much as possible and knowing our limitations in this area, we often enlist the help of friends - physiotherapists, occupational therapists and social workers. They never exist on TV or on the movies. Ever. Unless it’s to portray how terrible it is to be a social worker. From time to time in this episode, Cuddy laments that being chief of medicine is too administrative and she hasn’t been a doctor in years. That also doesn’t happen in real life. If you’re chief you’re still a doctor. You have admin shit to do deal with yes, but you still practice. It’s like being chief resident, in all the TV shows with one of these, you still seem them working as residents, be it scrubs or grey’s anatomy.
Back to the differential. They finally get to endocarditis. Culture negative to be precise. That indeed would explain the bilateral dusky fingers that led to unnecessary amputation. Septic emboli.
Going to stop here, more out of exhaustion now. I’ve created quite a lengthy post. Happy to reblog thoughts on culture negative endocarditis on request later. This is a worthy topic to study up on for students or residents. At least review Duke’s criteria and think about your clinical features like Roth Spots and Janeway lesions or Ouch Osler’s nodes.
The ending is also a far fetched connection to make, but is one that we would consider. In fact, we would ask in detail every time from day one - have you had any exposure to animals. It’s very rare to see someone so young be that sick out of the blue when you’re immunocompetent and have no underlying predisposing conditions. If there’s no focal source, then we would even ask about injectable recreational drugs, exotic travels, sexual health.
Most of the time, patients that sick are honest to their doctors.
But what about..

Frankly, much as we lie as humans, when our lives our on the line, we’re generally pretty honest (sometimes too honest) with the people we want to save us.
Any patient who is young and comes to hospital requiring inpatient admission, they’d be investigated by subspecialties with expertise in certain areas such as infectious disease. The dept of infectious disease would either be home team, or all over this patient as they special in the realm of both common and rare infectious diseases, culture negative endocarditis would have been considered before a hand amputation.
The term, “department of diagnostic medicine is laughable,” particularly when they consider it the only department in the world in the show.
In actuality, it’s a department that is universal and exists everywhere. it’s Internal medicine. Dr. Vivek Murthy, the next surgeon general (and also the last one under Obama) is an internal medicine physician. Ken Jeong of Community and the Hangover fame is also a physician of internal medicine.
Beginning to get the sense that most episodes are going to end with a diagnosis that is either infectious disease, rheumatology or haematology. But generally those tend to be most interesting and give the most plot twists or meaty differentials V.s. a stroke or acute myocardial infarction is fairly straightforward to diagnose.
This is a very twisty episode in all the wrong directions.
Dyspnoea is a very common presenting complaint. There’s a properly done approach to this in the podcast by the Curbsiders by the way.
22 notes
·
View notes
Text
Anion gap, alk/acidosis, lipase, A1C, UUN, labs, specialized labs, clinical presentation, BUN, Creatinine
Anion gap (will cover this in more depth with diabetes) is calculated from sodium level – (chloride + bicarbonate). You could do (sodium + potassium) – (chloride + bicarbonate). Potassium contributes so little that it’s often omitted, however. Anion gap means something else is contributing to the acid-base balance, not just the exchange of chloride for bicarbonate, for example.
Metabolic acidosis: Low pH, a low HCO3- concentration. Compensatory hyperventilation that contributes to a decreased pCO2. Most common causes: Inability of kidneys to excrete dietary hydrogen ion load, increase in hydrogen ion generation due to an addition of hydrogen ions or a loss of bicarbonate
Metabolic alkalosis: High pH, a high bicarbonate- concentration, and compensatory hypoventilation that contributes to an increased pCO2. Most common causes: loss of gastric acid from vomiting or nasogastric suction, loss of intravascular volume and chloride from diuretic use. Overtreatment of metabolic acidosis with bicarbonate. Excess of acetate in PN (parenteral nutrition), which becomes metabolized to bicarbonate
A1C distinguishes between diabetes and hyperglycemia associated with metabolic stress
Protein: Again:
First start by converting the protein intake of the patient (94g in this example) to grams of nitrogen. Second, calculate their nitrogen balance. We find that the patient is in negative nitrogen balance. Nitrogen balance should be the same amount of nitrogen coming into the body as is coming out in the urine. Third: Correct the deficit to get into nitrogen balance. Take that -2g of deficit that they are at (take the minus sign away), and multiply that by 6.25g of protein (1g of nitrogen = 6.25g of protein). Correcting the deficit of nitrogen finds that the patient will require 12.5 more grams of protein just to get into nitrogen balance. Fourth, we still need the patient to be in positive nitrogen balance, so, we increase protein and shoot for 2g more protein to promote anabolism (goal for anabolism is +2-4g of nitrogen a day more). So, that low end we are aiming for is 2g of nitrogen: 2N (6.25g of protein/1g of nitrogen) = 12.5g of protein needed to put the patient in positive nitrogen balance. Fifth, we want to try to promote anabolism, so we have to add the amount of protein that puts the patient at nitrogen balance to the amount of protein that puts the patient in positive nitrogen balance, and add the sum of those two to the amount of protein the patient is taking in (the 94g). Hence the new protein goal is 94g + 12.5g + 12.5g = 119g of protein/day or approximately 120g of protein per day.
Remember: even though you prescribed 100g of protein a day, the patient only actually got 94g. So, that’s why you use 94g in these calculations.
A valid 24-hour urine collection can be difficult to collect
Conversion factor of UUN to total nitrogen excretion may not be accurate in certain conditions: burns, major wounds, diarrhea, vomiting
Factor of 0.85 converts UUN to TUN
Assumes that 85% of urinary nitrogen is from urea
Other nitrogen sources in urine= ammonia, proteins
Conditions that alter or increase ammonia excretion will lead to underestimation
Ex if Adam had liver disease and ammonia excretion was higher/ UUN only 75%
◦ UUN = 13 (13/0.75) = 17 (vs 15)
Diminished renal function alters results
For the most part you are addressing whether the patient is renal insufficient or dehydrated. BUN:Cre ratio, if high BUN and Cre is normal, then it's usually dehydration. If the BUN and Cre are high, it's often renal failure.
LABS:
K+, Cr, and Phosphate are often looked at when assessing kidney function. K+, Mg2+, phosphate are often looked at together as well
Refeeding syndrome (hemodilution, hemodynamics) is indicated by labs. Lab error (e.g. blood that has been sitting out too long, things degrade), stress impacts labs, components of the blood (e.g. serum iron) need to be looked at with other portions of bloodwork. Disease states affect labs. High blood glucose can begin to displace sodium, causing sodium to appear low (false low result), like in diabetic ketoacidosis.
• Think about which labs are affected by which organ system
• Lungs: chloride, acetate
• Kidneys: BUN, creatinine, potassium, phosphorus, albumin, calcium
• Heart: Sodium, BUN (volume status)
• Pancreas: Blood glucose, serum lipase
• Liver: Liver function tests
• Liver disease: colloidal pressure AKA oncotic pressure. With liver disease, you’re not going to make as much visceral proteins (like albumin), which hang onto the water portion of the blood. If albumin is not hanging on, it will start to seep out and accumulate in different places (third spacing).
• Pleural effusions are seen commonly in malignancy. Ascites from cancer, for example. Just because patient doesn't have liver disease doesn't mean they won't have issues with fluid. Extra fluid creates a dilution efffect (causing sodium and albumin, calcium, etc. appear low. If you take those labs at face value, you can be thrown off.
Liver disease: colloidal pressure AKA oncotic pressure. With liver disease, you’re not going to make as much visceral proteins (like albumin), which hang onto the water portion of the blood. If albumin is not hanging on, it will start to seep out and accumulate in different places (third spacing).
Pleural effusions are seen commonly in malignancy. Ascites from cancer, for example. Just because patient doesn't have liver disease doesn't mean they won't have issues with fluid. Extra fluid creates a dilution effect (causing sodium and albumin, calcium, etc. appear low. If you take those labs at face value, you can be thrown off.
Serum sodium doesn't really relate to dietary sodium. Serum sodium is a marker of fluid status, because salt is like a sponge and pulls in a lot of fluid. So, if sodium is really low, often times there’s a fluid issue going on. High sodium indicates a fluid deficit.
• Potassium: 3.4– 5.1 mmol/L
• Magnesium: 1.7 – 2.6 mg/dL
• Low magnesium can make it difficult to successfully replete potassium and phosphorus (SO YOU WANT TO MAKE SURE MAGNESIUM IS NORMAL)
• Phosphorus: 2.4 – 4.3 mg/dL
Story: Patient with a phosphorus of 7 starting nutrition at a slow rate, but then his team gave him a bunch of dextrose-containing fluids to correct a sodium issue, and his phosphorus then dipped to a 2! This results from massive refeeding. The trends in your potassium, magnesium, phosphorus are important. What essentially happened was that the glucose (dextrose) activated insulin, and insulin activation caused a massive shift intracellularly of phosphorus, leading to lower levels of phosphorus in the blood. When not eating much, your cells aren’t taking in magnesium and phosphorus, etc. So, again, sugar stimulates intracellular shift because insulin will activate when sugar is reintroduced, leading to even lower blood levels of minerals. Your heart won’t have enough potassium to beat properly, your lungs won’t have enough phosphorus to breathe well. Certain diuretics can lead to potassium deficiency, E.g. thiamin follows potassium (Wernicke's Encephalopathy), certain diuretics that are potassium wasting come with a risk of thiamin deficiency. Can fix this by prophylactically give thiamin in anticipation of potassium drop.
CONSEQUENCES OF REPLETING TOO QUICKLY
• Low potassium: cardiac arrhythmia, cardiac arrest
• Low magnesium: seizure, coma
• Low phosphorus: respiratory distress, difficulty breathing/getting off mechanical ventilation
Patients who are at risk for refeeding syndrome can have a number of different conditions to begin with:
• Anorexia nervosa
• Chronic alcoholism
• Cancer
• Post-surgery (NPO for many days pre- and post-op)
• Elderly (poor dentition, reduced thirst/taste sensation)
• Uncontrolled diabetes mellitus (electrolyte abnormalities, polyuria)
• Critically ill and unfed for >7 days
• Inflammatory bowel disease, chronic pancreatitis, short bowel syndrome
• Cystic fibrosis
• Long-term antacid use (phosphorus levels are often low 2/2 magnesium and aluminum salts in the medications)
• Long term diuretic use (potassium-wasting) such as with CHF
• Patients who are vomiting frequently
Patients with poor blood levels at baseline (K/Mg/P) will be at risk of intracellular shifts and thus lower blood lab values. Patients with SBD have reduced absorptive capacity, for example, and are at risk for refeeding syndrome.
• When a patient is experiencing hyperkalemia (K+ > 5.1 mmol/L), there are a number of treatments a Team may utilize
• 50% Dextrose ampule + Insulin
• Calcium Gluconate
• Kayexalate or Lokelma
• Why would we use these medications? (insulin will stimulate intracellular K+ shift, Lokelma and Kayexalate bind potassium)
Giving dextrose and insulin mimics refeeding. So, you are pulling potassium out of the blood and giving it to the cells.
Giving dextrose and insulin mimics refeeding. So, you are pulling potassium out of the blood and giving it to the cells. With renal patients who are often in a hyperkalemic state, kayexalate and lokelma will stop potassium absorption in GI tract. When someone’s potassium hits the ceiling, arrhythmia can occur. Calcium is given to offset that. If a pt is hyperkalemic and EKG changes are seen, patient is given 2g of calcium. Calcium gluconate is the preferred IV administration for hypocalcemia (Severe symptomatic hypocalcemia should be corrected promptly with IV administration of calcium gluconate over 10 minutes to control symptoms. Calcium gluconate is the preferred salt for peripheral venous administration to avoid extravasation—leakage of liquid into surrounding tissue.)
Specialized labs: Liver function tests give you enzymes (alanine aminotransferase and aspartate aminotransferase, ALT and AST) and you are also given bilirubin as s measure of liver function, as bilirubin is a waste product of heme metabolism. When liver is not functioning well, bilirubin won't be cleared well. At that point, liver is also not good at clearing minerals such as copper and manganese.
Liver function tests give you enzymes (alanine aminotransferase and aspartate aminotransferase, ALT and AST) and you are also given bilirubin as s measure of liver function, as bilirubin is a waste product of heme metabolism. When liver is not functioning well, bilirubin won't be cleared well. At that point, liver is also not good at clearing minerals such as copper and manganese.
When T. bili is >5 mg/dL, give PO multivitamin without minerals, or remove copper and manganese from your TPN (total parenteral nutrition) solution
If patient is eating, give them a multivitamin without minerals. If patient is on TPN, remove copper and manganese, as toxicity of these can risk brain damage.
Blood and iron studies: Hemoglobin is the last thing to change. Look at ferritin as an earlier sign. Hematocrit can respond to anemia, but also to an overflow of other blood cells. Professor Trussler works with blood in the heme oncology setting. White blood cells in certain type of malignancies (e.g. leukemia) are elevated. Blood smear can count white blood cells and immature white blood cells (blasts). High blasts signals that something is wrong in bone marrow and they’re pumping a lot of immature white blood cells out. Also, immature blasts are a measure of whether someone’s chemotherapy has been effective. Treatment decisions can be made on this.
Absolute number of neutrophils can be used to determine treatment decisions. Low neutrophil count can be used as a guideline for a neutropenic (low bacteria) diet.
A1C: 3-month average blood glucose. When someone is acutely ill, you can see high glucose in the blood, but this is not diabetes, it’s “stress hyperglycemia” (due to injury). But if this is prolonged, an A1C can help you see if they have undiagnosed prediabetes. A1C is useful for newly diagnosed diabetic patients.
Lipase: You shouldn't be seeing a lot of lipase in the bloodstream, as this indicates pancreatic damage (e.g. pancreatitis)
Vitamin and mineral labs get expensive, so you don't want to be checking EVERYTHING for every situation. There are some vitamins and minerals where a serum lab isn't going to be helpful. E.g. pyridoxine (B6), Per the American Society of Parenteral and Enteral Nutrition (A.S.P.E.N.), you need serum B6, 24-urinary B6, erythrocyte AST, and erythrocyte ALT to assess sufficiency of B6.
Common vitamin labs:
· Someone who is having trouble absorbing fat will be at risk for vitamin A deficiency. Vitamin A is key to skin integrity and building (a pressure injury/injuries not healing well may indicate vitamin A deficiency), with substance use disorder deficiency comes up because you’re generating a lot of free radical damage from substance use disorders and the vitamin A is getting used up for that. Vitamin A is protein bound (RBP), so you can look at C-reactive protein in combination with this, because vitamin A may look low when it's not (falsely low result).
· B12 is worth looking at, esp. for vegans, vegetarians, elderly, heavy alcohol or substance users, and patients with IBD.
· Vitamin C builds collagen matrix for skin, thus wounds could cause a vitamin C deficiency in wound patients. Dialysis causes water loss, so you can lose vitamin C. COVID-19 may cause a vitamin C deficiency (the antioxidant vitamin is getting used up).
· Check vitamin D, after it's activated by the kidneys a second time, that active form doesn't last very long, so it may not give you a good result. Vitamin D labs are good to check for elderly patients who don’t synthesize enough vitamin D, and for kidney injury patients because their kidneys aren’t activating as much vitamin D. Checking vitamin D for oncology patients is also great, because they may have some complications in certain cancer treatments. COVID-19 appears to be affecting vitamin D levels.
· Vitamin E is good to check in a patient who is malabsorbing fat. If you think someone is malabsorbing, the team can do more work up.
Less common vitamin labs:
If the vitamin is water soluble, there’s less risk of toxicity, so you can give it prophylactically. For example, folate costs about $1, so it can be given for 3 days prophylactically.
B1 (thiamin) is given prophylactically if you think the patient is deficient. At Brigham and Women’s, if you anticipate that someone might refeed, you give them thiamin for the first few days that they’re getting nutrition support to anticipate that shift with potassium.
Professor T doesn’t usually check vitamin K often, because gut microbiota make vitamin K. Prothrombin (PT-INR, a marker of blood clotting) is a better indicator of vitamin K sufficiency because the clotting factors in your blood need vitamin K to work. If you were truly functionally deficient, you would have trouble clotting.
Common mineral labs
Both copper and ceruloplasmin must be low in order to diagnose a true copper deficiency. Bariatric patients tend to be low, esp. in Roux-en-Y gastric bypass patients, as the surgery is bypassing some of the areas where copper is absorbed. Wouldn't normally suspect a copper deficiency unless there's some sort of malabsorptive process occurring.
Zinc deficiency is caused by (and can also cause) diarrhea. If you have someone with diarrhea that isn’t resolving, it could be due to zinc deficiency, and also zinc could be causing the diarrhea. Zinc is lower in stressed state. If a patient is borderline deficient and their CRP is very high, you may want to hold off on repleting zinc, and then check zinc levels again.
Selenium, like zinc, decreases when someone has diarrhea, but can also cause diarrhea as a side effect of deficiency. Selenium will be low in substance use disorder patients, as it participates in antioxidant functioning (where antioxidants get used up).
Less common mineral labs:
Manganese: No good lab test to measure for this. If worried patient is getting too much, try to just remove it. E.g. taking manganese out of total parenteral nutrition, or giving a supplement that doesn’t have manganese. Manganese toxicity can cause brain damage
Chromium: No real lab measure for chromium, either, but people on long term TPN might develop this deficiency. Sometimes chromium is given prophylactically. People who are diabetic can be low in chromium, but it is difficult to figure out because you can’t check this mineral.
Specialty Lab
• Fecal Calprotectin
• Marker of inflammatory bowel disease
• Protein released by immune cells (neutrophils) at sites of inflammation in the GI tract, which is then excreted in the stool
• Low level (10-50 mcg/mg): likely IBS or viral infection
• Moderate level (>50 mcg/mg): potential IBD flare or worsening inflammatory condition such as parasitic infection
#anion gap#alkalosis#acidosis#lipase#A1C#UUN#labs#specialized labs#clinical#BUN#creatinine#dietetics#Medical Nutrition Therapy
2 notes
·
View notes
Text
if you live in America and are not on Twitter, you probably have a distorted view of what’s going on here right now
The situation is chaotic, so it’s hard to get an accurate picture. I’ve been sifting through... A LOT of different sources, checking who’s saying what, reviewing footage to see if it shows what I’m being told it shows.
Most protesters are peaceful. Most protesters are peaceful.
They turned out last week to protest racist violence and the fact that police engage in violence with impunity. The police are not out there for crowd control, public safety, or even protecting storefronts. They are counterprotesters demonstrating their perceived right to engage in violence with impunity.
Over the past days, I have watched so many videos from across the country showing over and over that the police are using unnecessary, indiscriminate violence to turn peaceful situations tense and tense situations violent. Their actions range from mild (shoving people with riot control shields) to concerning (spraying tear gas, an agent that causes coughing, in the midst of a pandemic that affects the respiratory system) to wanton (accelerating their SUVs into crowds) to gratuitously cruel (yanking down a teen’s face mask in order to pepper spray him right in the eyes even though he was simply standing there with his hands up).
Police have maced and tear gassed children at protests, like the nine year-old girl in Seattle. They’ve done the same to uninvolved bystanders who were just trying to walk home. In Salt Lake City, an old man at a bus stop couldn’t hobble away fast enough, so they knocked him down. In Minneapolis after curfew, troops fired rubber bullets / teargas at people who were on their own porches and balconies, because curfew. In another city, they stopped a civilian car, tased the people of color inside, and dragged them out for arrest on live news camera. Oh, also on live camera in Minneapolis they arrested a CNN correspondent and his crew, and many other journalists have been targeted with rubber bullets.
Rubber bullets sound kind of cute and cartoony, don’t they?
There’s no such thing as a non-lethal weapon, just less-lethal weapons. Rubber bullets are big hunks of metal jacketed in rubber. They’re supposed to be fired at the ground so that most of a bullet’s momentum can be harmlessly absorbed before it ricochets up and hits you in the legs. Used this way, they still bruise. They’re meant to hurt you enough to get you moving in the direction police want you to go. And you’d think that police are only supposed to use them when a crowd is already out of control or refusing to move, but that’s not what’s happening here.
Remember that CNN correspondent? His name is Omar Jimenez, and you can Google this: The police surrounded him and his crew. He very politely and deferentially asked them where they would like his crew to go. They didn’t respond despite Jimenez asking several times. Then they arrested them and led them away; all the while, Jimenez and the crew cooperated and calmly asked why they were being arrested, to which they initially received no answer. The police informed CNN that the arrest was made because Jimenez and his crew “refused to move.”
Surround. Give no directions, or make it impossible to follow directions. Arrest for failure to follow directions.
This is the same tactic that they’re using against crowds. They raise bridges or bring in barriers (”kettling”) to ensure protesters can’t leave. Then they arrest people for refusing to leave. Sometimes they fire teargas and/or rubber bullets at a crowd to drive them into a kettling situation. Sometimes they do it after the crowd is already kettled. The curfews? An excuse to arrest everybody on the street. Pay attention to when they’re announcing a curfew with little or no lead time. My city keeps claiming that essential workers are allowed to go to and from work even when a curfew is on, but would you bet cash money that no workers are getting swept up and arrested?
Journalists then report this as “protests turned violent” or “protesters clash with police.” Local authorities claim that the protesters are all or almost all outside agitators, from out of state, and journalists repeat this without (it seems) even asking themselves if that sounds plausible.
This is why Americans don’t know what’s going on.
(We should be skeptical of claims about outside agitators because it has a racist history. It is used to deny African-Americans of their agency in their own efforts to liberate themselves from white supremacy. On the other hand, to some unknown degree the protests are actually getting infiltrated by a) plainclothes LEOs possibly acting as agents provocateurs, b) white "allies” who mainly want to vandalize shit or start fights and don’t listen to the Black protesters who try to stop that crap, c) looters*, and d) white supremacists and other political opportunists**.)
All of the above is only a spoon-sized sample of what’s going on. You want more instances of police violence, you can find it. And all of these things have been happening for years, decades, generations. It’s not just Trump, though he certainly does bring out the worst in people, and his administration does like to loosen standards to enable the worst in people.
Yesterday morning (June 1, 2020), Trump called Putin. Then he called the governors of the states and basically told them to go to war against the American people. In the afternoon, he made a tough guy speech, calling himself the “law and order president,” promising he could fix it, promising to send the U.S. military into the states to establish order if the governors didn’t do it. While he was talking, you could hear people being teargassed and fired at with rubber bullets in the background. These were peaceful protesters in and near Lafayette Square. There was a water and medical station set up on the porch of St. John’s Episcopal church. The protesters and medics were driven away (again: with teargas, which causes coughing, in the middle of a pandemic) so that Trump could be seen posing in front of the church, holding up a Bible.
That church had no idea Trump was going to do that. Some of their clergy were at the medical station and got teargassed.
Please, please go read historian Heather Cox Richardson’s summary of yesterday, because there was more fuckery than I can summarize here: https://heathercoxrichardson.substack.com/p/june-1-2020
Law and order. “One law, one beautiful law.” I alone can fix it. We’ll use the military if the governors refuse to take action, “to protect the rights of law abiding Americans, including your second amendment rights.” Bible-waving. He fucking teargassed people for a photo-op.
In the middle of the night, the police herded hundreds of Washington, D.C. protesters into a residential neighborhood. The residents opened their doors for the protesters to take shelter. The police camped outside for hours, arresting anyone who came out. You may see accusations that protesters invaded people’s homes, but they didn’t -- they were invited. Some people are claiming police invaded people’s homes to get the protesters out, but I’m still looking for more information to substantiate that.
There are reliable reports that in addition to the National Guard and the regular military, ICE and CBP are being mobilized to “help.”
What they’ve done to D.C., they’re going to try to do in every city that has protests. What they’ve done to suspected undocumented immigrants, they’re going to try to do to all “rioters, looters, and antifa” -- which means anyone who opposes them.
-----------
WHAT CAN WE DO?
1. Support #BlackLivesMatter. The bail funds have actually received a lot of money lately, which is great; if you can give, and if you know of a bail fund close to you that needs money for protesters, go ahead and give, but the next thing we need is money for mutual aid organizations, because in the next 5-21 days, a lot of people are going to get sick.
2. Look to experienced organizers for guidance. Follow African-American anti-racist activists, and if you’re white make sure you stay humble, don’t talk over them, listen to their ideas and directions, and do what they fucking say. If you’re white and you go out to protest, your job is to stay calm and be a human shield. Your whiteness can actually reduce police violence [note: it’s a risk -- you might be beaten or otherwise hurt and you could be arrested too]. If you start violence or vandalism, African-Americans are more likely to suffer for it.
3. There’s a lot to do if you can’t go out. Again, there’s a lot of organizing going on. For example, the Indivisibles are still organizing people to contact their elected representatives, and this is good and important work even though it may feel less direct than hitting the streets.
4. Make common cause with organizations that have beliefs different from yours.
This takes a bit of discernment. Maybe you’re ready to swear you’ll never call the police again; maybe you want to end incarceration (we do have the largest imprisoned population in the world and the highest per-capita incarceration rate.) Or maybe you’re concerned about police brutality and racism in our justice system but you can’t imagine a world without policing and prisons. If you’re in the latter group, make sure that the policing reforms you support are in alignment with the general goal of reducing budgets for police departments and shrinking our prison system.
We need a big movement. That means you can’t refuse to work with other organizations just because they aren’t in complete lockstep with you.
3. Reblog posts like these with your own ideas / information / good sources of trustworthy information.
When you’re deciding which suggestions to follow and which posts to reblog, make sure the information is coming from someone who knows what they’re talking about. I’m not a veteran of many protests, so I can’t give you good advice about how to stay safe out there. I could probably (in an abundance of confidence) fake up something that sounds plausible based on what I’ve read. That kind of thing is dangerous. Don’t write shit that doesn’t either come from your experience or that you can’t back up with links to folks who really know.
-----------
* "Looters.” Yeah, remember when Congress promised to help with the economic crisis and then decided all we need is a one-time $1200 check and mmmmaybe some extra unemployment insurance? And remember when the House passed some more bills to help, but Republican Senate Majority Leader Mitch McConnell said they weren’t going to be doing any more of that and the important thing for the Senate to do right now was confirm more of Trump’s nominees for federal judicial appointments? You say “looters,” I say, “desperate angry people.”
** We all need to learn how to recognize Boogaloos, Neo-Nazis, and other far-right extremists on sight, because journalists are not always aware of who they’re talking to.
Boogaloos: https://www.independent.co.uk/news/world/americas/far-right-hawaiian-print-shirts-why-protesters-boogaloo-racist-a9539776.html
Anti-Defamation League’s Hate Symbols Database: https://www.adl.org/hate-symbols
6 notes
·
View notes
Text
Remifentanil-Induced Respiratory Failure in PACU after a Brainstem Tumor Debulking: Acute Diagnostic Dilemma-Juniper PublishersRemifentanil
Abstract
A 66 year old man developed sudden apnea and unresponsiveness after a large cerebellopontine angle tumor debulking. Based on the findings of a focused neurologic exam, the patient was emergently mask ventilated with subsequent return of spontaneous ventilation minutes later and recovery without further complications. Remifentanil bolus from residual infusion in an IV line was suspected due to rapid return to baseline and acute neurologic findings. We review remifentanil and highlight a challenging diagnostic dilemma in an acutely apneic patient after major neurosurgery.
Keywords: Remifentanil; Neuroanesthesia; Post-op respiratory failure; Neurologic Emergencies
Key Messages
a. A focused neurologic exam can affect emergent management.
b. A high index of suspicion and staff education are necessary for those involved in the care of patients receiving remifentanil.
Introduction
Remifentanil is a potent, ultra short-acting μ-opioid receptor agonist with a rapid onset of action in 30-60 seconds, peak analgesic and respiratory effects within 2.5 minutes (min), and rapid clearance (T1/2 = 3 min) [1]. It is commonly used as part of a balanced anesthetic in many anesthesia practices as well as in the intensive care unit. Its use is particularly prominent in neuroanesthesia, where precise hemodynamic control is as important as a crisp, quick emergence of anesthesia to facilitate neurologic evaluation. Respiratory depression is a common severe adverse effect of opioids that may be most prevalent with remifentanil [2].
Case History
A 66 year old man with a large acoustic neuroma presented for cerebellopontine (CP) angle tumor resection (Figure 1). Neuromonitoring of cranial nerves IX, X, XI, XII, somatosensory evoked potentials and motor evoked potentials was used during the case, while the patient received an intravenous anesthetic consisting of propofol 100mcg/kg/min and remifentanil at 0.3mcg/kg/min. Neuromuscular blockade was not used for the case. The surgery progressed without complication, and thepatient was stable throughout. The case lasted 7.5 hours, and propofol and remifentanil were discontinued 60min and 15min prior to conclusion of case, respectively. The patient was able to spontaneously ventilate, protrude tongue, and demonstrate intact cranial nerves IX and X with gag reflex prior to extubation.
In the PACU, the patient was awake and following commands. Shortly after administration of flush through a secondary peripheral IV, the patient acutely closed his eyes, becoming unresponsive and apneic. Rapid physical exam to check for increased intracranial pressure given the setting of recent intracranial surgery demonstrated the patient's pupils were actually pinpoint. The patient was then mask-ventilated until spontaneous ventilation returned several minutes later. Pinpoint pupils and rapid recovery makes a remifentanil bolus from residual infusion in the second IV line the most likely etiology. Patient recovered without further difficulty and was discharged home 3 days later.
Discussion
Remifentanil review
Remifentanil is a potent selective μ-opioid agonist. Its major distinction from other fentanyl analogues is its rapid onset and short duration of action with a terminal elimination half-life of 3-10 min, usually negating the need for Naloxone reversal [3]. The rapid onset of action is directly related to the rapid blood brain equilibration time of 1-2 minutes, while the short duration of action is a result of its unique structure of ester linkages making it susceptible to hydrolysis by blood and non-specific esterases (Figure 2). This rapid extra-hepatic metabolism makes its pharmacokinetics reproducible and dependable. Time to spontaneous movement, following commands, and extubation are all shorter than when compared with other opioids such as fentanyl and morphine. These pharmacokinetic and pharmacodynamic characteristics make remifentanil a nearly ideal analgesic in the operating room. However, due to its short duration of action, patients receiving remifentanil frequently require rescue analgesia in the postoperative period for pain management [4].
Remifentanil is rapidly metabolized regardless of the duration of infusion and is used commonly in clinical situations requiring a rapid offset with the benefit of minimal side effects such as respiratory depression [5]. While the risk for respiratory depression still exists, the ability to rapidly titrate the drug based on response allows for an overall lower rate when compared to most other opioids. In neuroanesthetic cases, it is commonly used in conjunction with propofolas part of a total intravenous anesthetic. It is easily titratable, facilitates stable hemodynamics, and minimally affects neuro-monitoring. Perhaps most importantly, this total intravenous anesthesia combination can allow for rapid emergence and the ability to perform post-operative examination for neurological status shortly after conclusion of the case [2].
Clinical experience
Rapid bolus of remifentanil can result in potentially life threatening respiratory depression, hemodynamic changes, or muscle rigidity. Respiratory depression has been documented in case reports after bolus in laboring patients with patient controlled analgesia [6] as well as in non-obstetric patients receiving remifentanil [7]. This appears to be even more pronounced and observed at lower doses in patients greater than 60 years old. Even infusions as low as 0.05mcg/kg/min have been reported to cause changes in ventilatory drive in healthy volunteers. Muscle rigidity, likewise, is a concerning complication of opioids that can lead to decreased ventilation and compliance resulting in hypoxia and hypercapnia. It is suggested that difficult ventilation may be primarily due to vocal cord closure. Remifentanil, however, primarily affects respiratory drive by activating opioid receptors on the respiratory neurons in the brainstem. By depressing the respiratory drive, the arterial carbon dioxide not only increases but increases in oxygen consumption and intracranial pressure are to be expected [8]. Muscle rigidity however can be prevented with pretreatment or concurrent administration of neuromuscular blockade [9].
Apnea
Our case brings up the challenge and importance of differentiating causes of sudden apnea and mental status change in the immediate post-operative period. The differential for postoperative respiratory failure is large and includes pharmacologic, hemodynamic and mechanical causes (Table 1). In addition to those listed, the patient's comorbidities may be one of the most fundamental things to consider. In the setting of recent intracranial surgery, both opioid overdose and intracranial pathology and dysfunction such as increasing intracranial pressure and seizures are important considerations. Cerebellopontine angle procedures are technically challenging and carry significant risk for postoperative bleeding, increasing intracranial pressure, venous insufficiency and cranial nerve palsy. Physical exam, including neurological exam, may be the most useful and potentially life-saving in this case.
Prevention
Prevention is a keystone of patient care, and the use of more dilute concentrations of remifentanil and initiating rapid resuscitation with possible muscle relaxation have been identified as ways to decrease the chance of similar events from occurring (Table 2). Remifentanil is a very useful opioid in a variety of settings for controlling autonomic responses during procedures and allowing for rapid recovery [2,5]. However, its dangers as a bolus should be known to healthcare providers and ancillary staff so appropriate identification and supportive care can be initiated as soon as a problem is identified.
Acknowledgement
Special thanks to Damian Pickering for assistance with manuscript preparation.
For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.com
For more articles in Journal of Anesthesia & Intensive Care Medicine please click on: https://juniperpublishers.com/jaicm/index.php
For more Open Access Journals please click on: https://juniperpublishers.com
0 notes
Text
youtube
Laryngeal Paralysis
• Other names: "Lar Par," geriatric onset laryngeal paralysis and polyneuropathy (GOLPP)
• Cause:
- The nerves of the muscles controlling the larynx become paretic or paralyzed, causing the cartilage to collapse inwards, blocking the airway.
- Most commonly this is due to an idiopathic neuromuscular disease, called "geriatric onset laryngeal paralysis and polyneuropathy (GOLPP)."
- The breeds most affected by the geriatric form are Labrador retrievers and Irish setters.
- Rarely may be secondary to trauma to the throat/neck or tumors in the neck or chest
- Endocrine diseases (ex. hypothyroidism and Cushing's disease) have also been associated with laryngeal paralysis in dogs.
- The congenital form is most common in Bouvier de Flandres, Siberian Huskies, Bull Terriers and Dalmatians.
• Species: Dogs, rarely cats
• Signs:
- usually middle aged and old, medium and large breed dogs -> owners often report patient as "slowing down" or "just getting older"
- congenital form shows clinical signs by 1 year of age
- shortage of breath
- exercise intolerance
- heat intolerance
- noisy breathing
- panting even when cool and calm
- dysphonia (hoarse or raspy)
- cough, especially with exercise, excitement, eating/drinking, or stress.
- dyspnea
- anxiety
- cyanosis, collapse, and death from asphyxiation in severe cases
• Diagnosis:
- Presumptive based on medical history, clinical signs, and diagnostic tests to rule out other causes of symptoms, such as heart disease
- Confirmation is via examination of the larynx with an endoscope or laryngoscope during voluntary respiration (requires sedation without anesthesia)
• Treatment:
- Medical management, such as anti-inflammatory drugs, antibiotics, and sedatives
- Lifestyle modifications:
avoid hot environments
avoid strenuous exercise
avoid swimming
do not use collars that will put pressure on the neck, but instead use harnesses
feed from elevated bowls
implement weight loss program
- sources were mixed as to whether mild cases can be successfully managed conservatively (with medications and lifestyle modifications alone), or if all cases eventually progress to requiring surgery or euthanasia.
- If in respiratory distress: oxygen therapy, external cooling, sedation, possibly intubation and assisted breathing
- Surgical correction is often successful at reducing or eliminating symptoms, but post-op complications such as aspiration pneumonia (up to 24% of dogs) or surgical failure (4-15%) can occur
- The most common surgical treatment is "unilateral arytenoid lateralization by tie-back" -> an incision is made through the side of the neck and the collapsed cartilage is permanently tied to the side of the larynx with suture to prevent it from creating an obstruction to breathing. [ETA: I shared a video of the surgery in a follow-up post]
- Only one side is tied back to decrease the risk of aspiration
- Recovery involves 6 weeks of post-op exercise restriction and minimizing barking
- Best performed by a boarded veterinary specialist surgeon!
•Sources:
- Video credit: Youtube user rejohnson58
- VCA Hospitals client education
https://vcahospitals.com/know-your-pet/laryngeal-paralysis-in-dogs
- American College of Veterinary Surgeons https://www.acvs.org/small-animal/laryngeal-paralysis
- University of Florida College of Veterinary Medicine Small Animal Hospital
https://smallanimal.vethospital.ufl.edu/clinical-services/surgery/soft-tissue-surgery/laryngeal-paralysis/
#veterinary#laryngeal paralysis#diseases#lar par#geriatric onset laryngeal paralysis and polyneuropathy#golpp#dogs#cats#videos#surgery
22 notes
·
View notes
Photo

A Brief Summary of My Week or How I Lost My Status as Second-Floor Gin Rummy Champion
I work four 10-hour shifts in the PACU at a 80-ish bed community hospital.
Tuesday: Pt comes out from the OR on a T-piece. Pt remains intubated for approx 45 minutes (this is a REALLY. LONG. TIME). CRNA chats with anesthesiologist while I assess, intervene, and chart so the (inexperienced) anesthesiologist doesn’t Narcan a post-op--(I remember the bay the patient was in. I remember the anesthesiologist’s and CRNA’s first and last names. I remember what time we extubated the patient (1814), his pH, pCO2, end-tidal CO2 at the end of the case, and when the MD drew the ABG. I cannot for the life of me remember whether the patient was male or female or what surgery s/he had)--so he doesn’t Narcan an immediately postop patient and reverse all his pain control.
(This was after surgery yelled at me for doing a urogyn’s voiding trial too early and made me cry. I haven’t cried because a doc yelled at me in ... over a decade? He refused to discharge her, ordered her foley replaced, and said repeat the voiding trial in two hours. She failed that time, too.)
Wednesday: Mr. I Don’t Want a Catheter for My Five-Hour Surgery’s first words upon waking from anesthesia? “I have to pee.” Scanned for 1007 within 10 minutes of PACU arrival, I&O’d for 1100.
Later on Wednesday: Young, healthy, DOC (read: freakishly strong) patient arrives in PACU accompanied by a corrections officer and an apologetic CRNA. Pt has received an enormous dose of ketamine and is batshit crazy experiencing emergence delirium. He’s verbally and physically aggressive, despite arriving restrained at wrist and ankle, which he protests vociferously and loudly with abundant use of both profanity and vulgarity. After 40 of Precedex and 2 of Ativan, 50 of fentanyl finally does the trick. Roughly forty-five minutes after his arrival, three nurses remain at his bedside to do everything necessary in as short a time as possible before he wakes up and starts swinging again. Dude wakes up less aggressive but still belligerent and irritable. I have the “here’s a urinal, it’s okay to pee--no, you’re not getting out of bed, you just had surgery” conversation every 90 seconds for the second time in six hours.
Thursday: CRNA and anesthesiologist (very bad sign) wheel my last patient around the corner and the CRNA’s first words are “we’re concerned about her breathing.” I take one look at the patient and know she’s approaching respiratory failure. MD says he wants a CXR. I open my mouth to ask about an ABG (I know her CO2 is high, it’s obvious she’s not blowing it off) but am distracted by the CRNA starting report, which gets worse the longer she talks. Patient is responsive, oriented, but lethargic and c/o 10/10 pain. Anesthesia asks if it’s ok to give pain meds. Having been burned before, I look up from my assessment and warily ask, “how much Dilaudid?” She hems and haws a bit, worrying out loud about giving narcs with her breathing, until I offer, “we usually give .2, but if you want to give .4, that’s okay.” She does. Pt seems to tolerate it ok, but just does not look good. She’s clearly struggling to breathe. I ask if the CRNA wants an ABG. “Yes!” I’m reaching to call the MD when she asks if I want her to order it. My yes is just as immediate, so off I go to hunt for an ABG syringe. But the ones with needles have mysteriously disappeared since I fetched them for Tuesday’s T-piece patient, so I call CCU and ask them to tube a couple over. (They send me six.)
I’m monitoring heart rate, breathing, blood pressure, oxygen status, respiratory effort, and mental status nearly constantly, drawing labs, doing wound checks and neurovascular assessments, giving IVF and non-narcotic pain meds, trying to get at least something charted, working around x-ray and keeping my patient informed and calm when my coworker passes me the charge phone.
Lab has just tried to call critical results to the teenage volunteer in the waiting room: pH 7.18 and pCO2 78.1. This patient just bought herself an ICU bed. I notify the anesthesiologist, he asks for BiPAP, I tell him to call respiratory, we page the hospitalist for admit and postop orders. I recognize the RT who arrives and chat pleasantly with her as we work on separate tasks for the same patient. Pt continues to c/o pain from her brand-new hip replacement; I’m discussing non-narcotic interventions with the MD and trying to explain to her that it’s more important to keep her safe than it is to keep her comfortable. Things settle enough for me to bring family back, ortho comes out with their last patient, and I snag the resident to chat about NSAIDs. Anesthesia repeats the ABG and I’m just starting to think about calling report when I look up and realize--it’s shift change. This patient is mine for at least another 33 minutes.
tldr; A series of crises forced me to prioritize patient care over playing cards ... or eating, or drinking, or urinating, or even charting.
In other words, I am a nurse.
#ktoo nurses#nurse life#pacu#nurses playing cards#I know most of you won't understand half of this#but that's kind of my point#feel free to message me to discuss
6 notes
·
View notes
Text
What Are The Risks Of Total Hip Replacement?By Best Orthopaedic Surgeon in RR Nagar Bangalore Dr Basavaraj CM

Total hip replacement is considered to be the most successful operation of the 20th century. It carries a success rate of 96-98 %. However there are some risks(although rare), which are infection(1%), deep vein thrombosis (normally blood does not clot with in our body, but following surgeries blood can clot within the blood vessels of the legs causing swelling of the legs. These clots could dislodge and the blood flow could carry them into the lungs(this is called pulmonary embolism). The other risks dislocation, leg length discrepancy, and anaesthetic complications.
Our Best Orthopaedic Surgeon in RR Nagar Bangalore Dr.Basavaraj CM says that ,The major complications of a hip replacement are:
Dislocation: This is rare as the hip is a very stable joint; the incidence is <2%
2. Infections: This can be further classified as acute<2 weeks; intermediate upto 15 months and delayed anytime later.
Acute infections occur in the immediate post op period and may be because of contamination; seeding of bugs from another source. This may be managed with IV medications and local care like a lavage without removing the prosthesis.
Intermediate infections again are usually from seeding from other sites like teeth,lungs, kidneys etc. The management may be similar to the acute stage but not always can you save the prosthesis. This may require a staged revision if eradication of infection is the goal says by our Best Orthopaedic Surgeon in RR Nagar Bangalore Dr.Basavaraj CM.
Late infections like the term means infection at a late stage. This is usually secondary to other factors like infections of the urinary tract; pneumonia, and other systemic infection, which cause a septicemia and seeding of the organisms into the joint. These are generally handled with staged revisions namely removal and clean out of the joint; placement of an antibiotic spacer to maintain soft tissue tension/ architecture followed by a secondary joint placement. The success rate of these in the best of hands is about 75-80%
3. Deep vein thrombosis/phlebitis: This is blood clots forming in the leg veins. These can propagate and when they break off and end up in the lungs they can cause severe respiratory distress and even death. This is the reason for the calf compression device and or blood thinners used.
4.
Respiratory problems like atelectasis/ pneumonia can happen. This is hopefully prevented with the chest compression exercises and deep breathing; you are encouraged to do coughing along with incentive spirometer
5.
Prosthetic failure; Lysis Periprosthetic fractures:
These though rare are seen with the longer duration the prosthesis is in place and can be due to wear; delamination of the polyethylene, cement failure with lysis.
These are now to a certain extent managed with the advent of better bearings like ceramic and highly crosslinked polyethylene. Revisions in these cases can be difficult and would require specialized equipment as well as surgeons trained for this.
6.
Loosening: There are 2 types of this problem, one caused by infection, when the organism creates /causes localized bone destruction and failure and the second due to aseptic causes which cannot be always identified. Mal alignment of the components especially of the stem can cause an abnormal dynamics which can increase wear and secondary failure.
7.
Stem fracture: A very rare complication caused by improper cementing leading to distal fixation and cantilever bending.
8. Cup disassociation: very rare but can happen and is due to failure of the cup locking mechanism
9. Leg length discrepancy
What would be the type of anaesthesia used?
Most of the times a Spinal anaesthesia would be given but sometimes a general anaesthetic would also be used. The anaesthesiologist would evaluate and administer the most appropriate anaesthetic. The blood loss from this operation is about 300ml and usually does not require a transfusion.
When would I walk? what would happen during postoperative days in the hospital?
I or a colleague will see you later on the day after the hip replacement and get you up standing and may get you to take a few steps.
Physical therapy starts the same day or next and he works with you to start walking with a walker, manipulating stairs and also will go through the programme for you to use post discharge. Ambulation will be with a walker and we suggest this for the first 3-4 weeks.We will make arrangements for a bed side commode for use in the hospital and suggest you modify your toilet at home so as to raise the seat. We do not want you to bend your hip more than 90 degrees. It is advisable to always have a pillow between your legs so that you don’t cross your legs. Try and keep the foot and knee looking straight up when lying in bed.
The dressings are changed prior to discharge and we do not want you to fool with it, till we see you in the clinic.You should avoid getting your wound wet till we see you in the clinic and so you will skip showers/bath and just sponge/towel baths.
Deep breathing, coughing will also be encouraged as well as the use of the spirometer. This is done to get your lungs to expand fully.
I generally let you go home the third or fourth day.
0 notes
Text
Price: [price_with_discount] (as of [price_update_date] - Details) [ad_1] Updated yearly. Last in July 2018. Over 390 illustrations and color photo's. We added detailed information on the treatment of the the most common admitting diagnosis. 1. Respiratory failure: ARDS. Pneumonia. Exacerbation of chronic lung disease (Asthma, COPD, Bronchiectasis). Pulmonary Embolism. 2. Shock: Hypovolemic (GI Bleed and Diarrhea). Cardiogenic (Acute MI / Infarct). Distributive (Sepsis and Anaphylaxis). Obstructive (massive Pulmonary Embolism. Tamponade. Adrenal Insufficiency / Crisis | 3. Cardiac disease: Acute MI / Unstable Angina. Heart Failure (CHF). Valvular Heart Disease. Hypertension Emergency. Arrhythmia’s with hemodynamic instability (see cardiology module). 4. TRAUMA: massive, involving multiple organs. Rhabdomyolysis | 5. Burns. 6. CNS injury: Stroke. Head injury. Hemorrhage (Subdural / Epidural). Status Epilepticus. Coma. Delirium. 7. Infections: Septic shock. Toxic Shock Syndrome. Meningitis. Neutropenic fever. Endocarditis. Diarrhea 8. Metabolic derangements: Acute Renal Failure / uremia. Diabetic ketoacidosis (DKA) and HHNKS. Severe Hyponatremia or Hypernatremia. Severe Hypokalemia or Hyperkalemia. Severe Hypophosphatemia. Intentional or accidental poisoning (See Trauma-Tox module for Toxidromes). 9. GI diseases: GI Hemorrhage. Acute Liver Failure / Encephalopathy. 10. Hematologic disease: Anemias. Thrombocytopenia. TTP-HUS. DIC. 11. Psychiatric diseases: Suicide attempt. Neuroleptic Malignant Syndrome. 12. Postoperative Crises: Post-Op Confusion | Hypotension | Fever & Infections | Oliguria & Short-of-Breath | Hyponatremia & Other Pearls | Filled with detailed work-ups, treatments, pearls, illustrations, differential diagnosis, references....Everything you ever needed to know about critical care and nutrition issues in an easy to read and navigate format created specifically for the handheld device. Edited by multiple specialists. The perfect text for internists, family physicians, urgent care clinicians, residents, medical students and mid-level providers. ASIN : B004I5BTW6 Publisher : Primary Care Software, PC; 18th edition (18 December 2013) Language : English File size : 9265 KB Text-to-Speech : Enabled Screen Reader : Supported Enhanced typesetting : Enabled X-Ray : Not Enabled Word Wise : Not Enabled Print length : 2167 pages [ad_2]
0 notes
Text
Postoperative Monitoring of Patients with Obstructive Sleep Apnea: How Long is Long Enough? by Raymond Kao MD MPH*

Abstract
Purpose: Practice guidelines recommend monitoring post-operative obstructive sleep apnea (OSA) patients longer than non-OSA patients. Literature suggests patients with OSA have a higher risk for postoperative pulmonary complications, cardiac events and ICU admission. The objective of this study is to determine the optimal duration of post-operative monitoring.
Methods: This is a retrospective review of two-hundred and three patient charts, age 18-83 years old (69.46% male) who underwent surgery from June 2011- March 2014. OSA patients were identified either by AHI diagnosis or by preoperative questionnaire. Patients were monitored in the Post Anesthetic Care Unit (PACU) for 4 hours seeking desaturation and/or apnea events equals ‘fail’ to guide overnight ward monitoring (5-24 hours) or no event equals ‘pass’ monitoring.
Results: Seventy-five patients (N=38 with AHI and N=37 at risk, 36.95%) had desaturation events in PACU. The mean time to desaturation was 55 ±43.33min. Females had more desaturation than males, 50.00% vs. 31.21%, p=0.01 with OR=1.91, 95%CI 0.90-4.05; Female age ≥ 50 with BMI >35 had more desaturation that male age ≥ 50 with BMI>35, 77.42% vs. 63.64%, but not statistically significant, p=0.51 with OR=3.95, 95% CI 2.00-7.80. No significant difference in mean AHI between passed or failed post-op monitoring (51.04±23.75 vs. 43.54±25.23, p=0.17), but AHI>40 and male (OR=3.18, 95%CI 0.38-26.62) has higher risk of desaturation compared to AHI=0-20. The logistic regression model has good discriminating ability between passed and failed monitored patients, C-statistic 0.7756.
Conclusion: All PACU desaturations occurred less than 3 hours after surgery, with no other adverse events recorded. Females, patients with OSA and BMI >35 had significantly higher rates of oxygen desaturation. It may be possible to limit postoperative monitoring for OSA positive and at risk patients up to 3 hours.
Keywords: Post-operative; Obstructive sleep apnea (OSA); Complications; Monitoring
Introduction
Patients with obstructive sleep apnea (OSA) experience periods of partial or complete upper airway obstruction lasting >10 seconds during sleep which can lead to frequent arousals, hypoxia, hypercarbia and/or cardiovascular dysfunction [1]. Approximately 24% of patients presenting for elective surgeries are found to be at high risk for OSA based on preoperative screening [2]. These patients are thought to be more sensitive to the respiratory depressant effects of opioids and sedatives. There is also evidence of increased apnea-hypopnea index (AHI) in postoperative OSA and non-OSA patients [3]. These post-operative patients are at higher risk of pulmonary complications including respiratory failure with desaturation and reintubation; cardiac events such as myocardial infarction and arrhythmia; and ICU admission [4,5]. However, other data suggests that neither diagnosis of OSA nor positive risk screen for OSA was associated with increased 30-day or 1-year postoperative mortality [6].
There is limited evidence in guiding postoperative monitoring and management of OSA patients or patients at risk for OSA. The 2006 American Society of Anesthesiologists practice guideline, recommended monitoring of postoperative patients with OSA for at least 3 hours longer than non-OSA patients [1,7]. At St. Josephs Health Care (SJHC) London, protocol for postoperative monitoring of OSA patients were developed, based on the 2006 ASA guideline. In some centers such monitoring can mean admission to the intensive care unit postoperatively. The ASA guidelines recognize that there is insufficient evidence to determine either a) the appropriate duration of PACU monitoring or b) whether it is safe to discharge the patient to a regular ward or home versus overnight oximetry monitoring. At SJHC in London, Ontario, 80% are outpatients’ day surgeries. The main surgical specialties are hand and upper limb, urology, ophthalmology, outpatient Otolaryngology – Head and Neck Surgery, general surgery and gynecology. Surgeries are low to intermediate intensity and patients are mainly ASA class I-III. Patients with known or suspected OSA are monitored for in the PACU for apneas or desaturations, as per the ASA guidelines. The 4 hours duration includes time to meet usual PACU discharge criteria plus 3 hours additional monitoring. Patients were deemed to ‘pass’ the monitoring if no events were detected, and to have ‘fail’ if desaturation or apnea occurred. Physicians and clinical nursing staff working in the PACU developed the clinical impression that patients would pass or fail the monitoring protocol significantly before completion of the 4 hours monitoring. It has been suggested that the monitoring could be shortened to 2 hours, potentially economizing hospital resources and allowing patients to be discharged to unmonitored ward or home sooner. Our primary study objective is to determine if postoperative monitoring of OSA patients and patients at risk for OSA can be shorter than 4 hours. Our hypothesis is that postoperative monitoring for OSA patients and patients at risk for OSA can be limited to 2 hours in the PACU. We also aimed to determine if this monitoring would allow us to predict and/or prevent postoperative complications in these patients.
Methods
A retrospective chart review between June 2011 and March 2014 of all patients undergoing extended postoperative monitoring at SJHC was completed. This study was approved by the Research Ethics Board at Western University, approval number 105093. We reviewed preoperative questionnaires, polysomnography (PSG) records, anesthesia records, and PACU records. From these sources we recorded documented apnea-hypopnea index (AHI), demographics, comorbidities, surgical procedure, and perioperative medications including inhalation agents, muscle relaxant and narcotics, length of procedure, as well as postoperative oxyhemoglobin saturation, PACU administration of narcotics, time from admission to PACU to desaturation or apnea. We also reviewed the inpatient chart if the patient was admitted prior to their surgery, and the extended electronic medical record for evidence of adverse outcomes. We searched for postoperative visits to the Emergency Room, clinics, and readmissions for up to ten days postoperatively. A total of 237 patients were reviewed and after exclusion of patients for reasons outlined in Figure 1, a total of 203 patients were entered into the study.
Our institutional policy identifies patients for extended monitoring if they have an existing PSG diagnosis of moderate (AHI 21-40) or severe (AHI >40) OSA, or are classified as probably having obstructive sleep apnea by the tool provided in the 2006 ASA Practice Guideline.1 Patients who met the criteria for definite OSA were extended monitored with oximetry, Table 1A. Eligible patients were monitored in the PACU for 4 hours, assessing for apnea of greater than 10 seconds in duration or desaturation with oxyhemoglobin saturation less than 90% while the patient was asleep or awake. Patients were given Continuous Positive Airway Pressure (CPAP) therapy if routinely used at home. Disposition after PACU was determined by results of monitoring. The options were either if there was no respiratory event during 4 hours monitoring the patient was discharged home or to the regular ward at the discretion of the surgeon or if there were apneas or desaturations during monitoring, the patient was admitted for overnight oximetry monitoring on the ward. The outcomes measured were failure of 4 hours monitoring as defined by desaturation or apnea event in PACU and incidence of postoperative complication occurring on the postoperative ward or following discharge.
Statistical Analysis
For continuous variables, data are expressed as mean ± SD and comparisons conducted using the student’s t-test. For categorical variables, data are reported as proportions and comparison made using Pearson’s Chi-square test. A 95% confidence interval computed for all continuous variables. All tests presented are two-sided, a p-value ≥ 0.05 and the range of the 95% confidence interval contains the value of no effect then considered statistically insignificant. For dichotomous outcomes, logistic regression was used to evaluate clinical factors predicting passed or failed at 4 hours post-operative monitoring. Independent variables included in the regression models were age, sex, body mass index (BMI), AHI, post-operative narcotic use and duration of anesthesia for the surgical procedure. All statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
From June 2011 to March 2014, 237 patients underwent extended postoperative monitoring for obstructive sleep apnea. After administrative cleaning, 203 patients were included in the study, Figure 1. Twelve patients had repeat surgeries, so the second admission was excluded. One patient could not be identified due to typographic error. Nine patients did not complete the full monitoring period due to insufficient PACU staffing and 12 patients had incomplete data in their medical records.
In Table 1A, no apnea events were recorded and 75 patients (36.95%) had a desaturation in the PACU. Females, N=31/62 (50.00%) were more likely to have desaturation than males, N=44/141 (31.24%), p=0.01. The mean time from PACU admission to desaturation was 87.55±43.33 minutes. No patients had desaturation between 0-30minutes, likely because all patients received oxygen by mask from PACU arrival until fully awake; 19/75(25.33%) patients had desaturation between 31-60minutes; 39/75(52.00%) had desaturation between 61-90minutes; 11/75(14.67%) had desaturation between 91-120minutes and 6/75(8.00%) had desaturation between 121-180minutes. There was no significant difference in desaturation based on mean age, p=0.17, but for age > 50, N=55 (73.33%) had a higher desaturation rate than age ≤ 50, N=20 (26.67%). Patients with high mean BMI more likely to have desaturation then lower mean BMI, (39.15±8.23 vs. 33.09±7.46, p<0.0001); BMI>35, N=52 (69.33%) were more likely to have desaturation compared to patients with BMI<35, N=23 (30.67%). Patients identified by screening questionnaire for OSA, N=37/121 (30.58%) were less likely to fail desaturation than patients with AHI diagnosis of OSA, N=38/82 (46.34%). In the desaturation group, patients with ASA 3, N=44 (58.67%) compared to ASA 1, 2 and 4 and those with chronic disease hypertension, N=50 (66.67%) and diabetes, N=26 (34.67%) compared to other chronic diseases had the highest failed monitoring at PACU. There was no statistically significant difference between the failed and passed monitoring groups at PACU for the adjusted post-operation narcotic use.
In Table 1B, desaturation by gender revealed male N=44 (58.67%) and female N=31(41.33%). Although the mean age between sexes with desaturation was not statistically significant, p=0.05, but for both gender age > 50 years old had higher proportion of desaturation [male N=32/44(72.73%) vs. female N=23/31(74.19%)] than age ≤ 50 years old [male N=12/44(27.27%) vs. female N=8/31(25.81%)]. The mean BMI between gender was not statistically significant, p=0.51, but for both gender BMI > 35 had higher proportion of desaturation [male, N=28/44(63.64%) vs. female, N=24/31(77.42%)] than BMI ≤ 35 [male, N=16/44(36.36%) vs. female, N=7/31(22.58%)]. For those patients with AHI, this was not statistically significant between genders. But male with severe AHI, N =13/23(56.52%) and female with moderate AHI, N=8/16 (50.00%) had the highest proportion of desaturation. The following chronic diseases have the highest proportion of desaturation in both genders, hypertension [male, N=30/44 (68.18%) vs. female, N=20/31 (64.52%)], diabetes [male, N=14/44 (31.82%) vs. female, N=20/31 (64.52%)] and asthma [male, N=8/44 (18.18%) vs. female, N=7/31 (22.58%)]. There is no statistical significance between genders with respect to number of pack-year smoking, the mean time to desaturation and adjusted post-operation opiates utilization.
Fourteen patients who passed PACU monitoring and 2 patients who failed PACU monitoring presented to the emergency room greater than 24 hours after discharge. The ER complaints found were pain (N=3), bleeding (N=4), urinary retention (N=2), adverse reaction to medication (N=1) and prescription refill/musculoskeletal injury/dressing change (N=6). There were no complications related to OSA, and no respiratory or cardiac events found in patients discharged home.
In Table 2, we performed multiple logistic regression analysis adjusting for age, sex, BMI, AHI, anesthesia duration and adjusted post-op narcotic dose. The model containing the explanatory variables compared to that with the intercept only, significantly impacted the predictive ability of the model with the likelihood ratio, χ2 =35.86, p<0.0001. The overall effect of each of the covariates on desaturation at PACU revealed only BMI (χ2 =35.86, p<0.0001) and anesthesia duration (χ2 =11.10, p=0.0009) had a significant independent effect on desaturation at PACU. Categorically, the odds of desaturation during PACU monitoring are higher for patient age ≥ 50 is 1.52 (95% CI 0.74, 3.13) and female is 1.91 (95% CI 0.91, 4.02); patients with BMI≥35 is 3.95 (95% CI 2.0, 7.80); patients with AHI 21-40 (moderate) is 1.07 (95% CI 0.12, 9.23) and AHI >40 (severe)is 3.10 (95% CI 0.38, 25.67) as compared to AHI 6-20 (mild); anesthesia duration between 2-4 hours 3.55 (95% CI 1.68, 7.47) compared to anesthesia duration 1-2 hours and adjusted post-op narcotic dose 5.1-25 mg 1.48 (95% CI 0.65, 3.36) compared to dose 0-5 mg. The discriminatory performance of the training model revealed the AUC was 0.776, Figure 2. This indicates that the model has good ability to distinguish between patients with diagnosis or at risk for OSA and those without OSA for post-operative desaturation. As a measure of calibration from the model in Table 3, the Hosmer and Lemeshow goodness-of-fit statistics revealed χ2=1.62 (p>0.99) indicating strong agreement between observed and expected post-operative desaturation in patient diagnosis or at risk for OSA.
Discussion
A large number of patients have ambulatory surgery [8]. The perioperative period is particularly high risk for patients with or at high risk for OSA due to the effect of anesthesia, narcotics and sedatives. Several studies found patients with OSA undergoing non-cardiac surgery have higher incidence of post-operative hypoxia, respiratory failure, cardiac events and ICU transfers compared to those without OSA [4,9]. An ability to predict patients at greater risk for postoperative complications would help hospitals target effective resource utilization while complying with various guidelines for managing OSA patients postoperatively. The 2006 American Society of Anesthesiologists (ASA) guideline for perioperative management of patients with OSA, which the SJHC protocol was based upon, recommends postoperative monitoring in the PACU for at least 4 hours, and for 7 hours after an episode of airway obstruction or hypoxemia.1 Subsequent publications have recommended different approaches to postoperative monitoring. Despite these recommendations, many institutions do not have a policy for perioperative management of patients with OSA [10], due to a lack of evidence clarifying duration of monitoring and or prevention of clinically significant adverse events. The implementation of the postoperative monitoring of OSA patients can have significant resource implications for hospitals. Our institution adopted a 4 hours PACU monitoring policy on the basis of the 2006 ASA guidelines. The protocol was chosen as it identifies only higher risk patients, which allowed us to restrict the number of patients monitored. This retrospective chart review found the mean time for patients who had desaturations in the PACU occurred at 1.46 hours of admission; 69/75 (92.00%) with desaturation between 0-2 hours and 6/75 (8.00%) with desaturation between 2-3 hours. Females with BMI≥35 with or at risk for OSA were more likely to have desaturation. These findings are similar to that of a study of perioperative risk assessment in patients with a propensity for OSA [11].
In general sleep physiology changes with age and gender [12-14]. Female have better objective sleep quality with shorter sleep onset latency and better sleep efficiency than male [12,15]. Factors that can impact female more than male sleep efficiency including anxiety and depression and hormonal changes specifically luteal phase of the menstrual cycle [16-18]. However, OSA is more common in men than women in the general population with a male to female ratio ranges 3:1 to 5:1 [19-21]. Obesity a well-known risk for OSA, and higher body mass index (BMI) is associated with greater severity of OSA for both sexes.22 But for the same AHI women tends to be more obese than men [23,24], this is likely due to differences in fat distribution between the sexes [25]. In our study, women with moderate AHI had similar proportion of desaturation as compared to male with sever AHI which can be explained by the fat distribution differences between genders which has physiological and mechanical effect in patients with OSA [26]. Female who are obese and with OSA have shown to have significantly increased hypercapnic and hypoxic response, which is not the case in male [27]. Furthermore, women with OSA are less likely to be evaluated and diagnosed for OSA [28]. In our study, the limitation for gender difference specifically female is the small numbers (N=62) with BMI >35 (N=24) and AHI moderate-severe (N=12/16)) are more likely to have post-operative desaturation.
Procedural related risk factors such as surgical site, surgical (anesthesia) duration, anesthetic techniques and emergency surgery have been shown to predict peri-operative complications [29]. In particular pulmonary complications for non-cardiac-thoracic surgeries requiring greater than 2-hours anesthesia and mechanical ventilation would need for prolonged oxygen therapy and atelectasis which required ICU admission may complicated by increasing post-operative-mortality and increasing ICU/hospital length of stay [30]. Russell KM et al. [31] reported patients after ophthalmologic surgery found that the expected duration of PACU recovery depends on the operations that requires general anesthesia. Patients having orbitotomy and strabismus procedures had a median anesthesia recovery time 2 to 3 times longer than for other procedures and more likely to have prolonged recovery with other procedures. In addition, their post-hoc analysis found a higher proportion of patients with respiratory depression during anesthesia recovery also had OSA [31. Our study indicated that in our ambulatory surgery cohort 56/75 (78.67%) of the patients with desaturation had longer anesthesia duration between 181-200 minutes than those with shorter anesthesia duration.
A major determinant for discharge after ambulatory surgery is the quality of post-operative pain control. Opioid consumption in the PACU can be used as an earlier surrogate for poor global quality of recovery after surgery. An inverse relationship noted between opioid consumption in the PACU and global quality of recovery at 24-hours after the surgical procedure [32]. It is also known obese patients with or without OSA experiences frequent oxygen desaturation episodes post-operatively after total anesthesia followed by patient-controlled intravenous analgesia with morphine [33]. However, in our study the adjusted opioid dose is much less as compared to other published studies [32,34], which had a much higher opioid dose for the higher pain patients than the lower pain patients. This may well be because our anesthesiologists focus on opiate sparing techniques for OSA patients. Multimodal analgesia and regional analgesia techniques are used routinely.
Certain co-morbidities predispose adult patients for high risk of post-operative OSA includes obesity, hypertension, diabetes, male sex, alcohol use and large neck size [35], coupled with chronic opioid use [36]. In our study there is a high proportion of patients with desaturation had hypertension and diabetes. Therefore a robust screening questionnaire would be very useful to select that patient at risk such as the STOP-BANG questionnaire [37]. Studies have shown that the STOP-BANG questionnaire can identify 93% of those patients as being at risk for OSA [35,38]. However, that sensitivity would lead to the inclusion of substantially larger numbers of patients, which would have taxed hospital resources significantly.
In an aging population the frequency of OSA increases and plateau after 65 years [39]. In our study group, patients > 50 years old had a higher number of desaturations as compared those patient ≤ 50 years old. There are multiple risk factors associated with the older population desaturation post ambulatory surgery such as preferential deposition of fat around the pharynx which reduces airway patency [40]; overnight fluid shift to the neck affect the surface tension of the upper airway [41,42] and restriction of chest wall movement due to decrease lung volume [43]. The greatest exacerbation of OSA and sleep-disordered breathing has been shown to occur on postoperative day three [3], at which point all of our patients had been discharged home. We did not identify evidence of OSA related complications following discharge from hospital. It is not clear whether increased AHI and increase in desaturations after general anesthesia are associated with clinically significant events.
There are several limitations with our study. Due to a small study population and exclusion of higher risk patients from this ambulatory surgical hospital we did not find any clinically significant adverse postoperative events in our study patients. Patients admitted to the inpatient ward for postoperative oximetry can be awakened by the oximeter alarm, and commence breathing prior to developing any further complication. Another limitation of this study was the lack of dedicated apnea monitoring, both in PACU and on the ward. Apneas presumable occurred but the events were only recognized when there was a resulting desaturation and oximeter alarm. Our protocol did not include assessment for sedation analgesia mismatch, but patients in the cohort did not exhibit this finding: there was a low rate of opiate requirement, and minimal sedation.
The absence of clinically significant adverse effects is notable. We cannot know whether the overnight oximetry monitoring, and application of oxygen to those with desaturations, prevented any complications. However, the data show that the majority of patients in our cohort of select lower acuity patients could safely be discharged home on the day of surgery. These findings echo that of a recent study of patients undergoing surgery to relieve obstructive sleep apnea symptoms [44].
In conclusion, this retrospective chart review found that all desaturation events in PACU occurred within the first 3 hours of arrival to PACU. Patients with a PSG diagnosis of OSA appear to be at higher risk than those identified by preoperative screening. Females and those with a BMI >35 were more likely to have desaturations. We did not capture any clinically significant adverse events in our study patients. A larger study may be required to determine the utility and optimal duration of postoperative monitoring.
Regarding our Journal: https://oajclinicalsurgery.com/ Know more about this article https://oajclinicalsurgery.com/oajcs.ms.id.10031/ https://oajclinicalsurgery.com/pdf/OAJCS.MS.ID.10031.pdf
#Post-operative#Obstructive sleep apnea#Complications#Monitoring#oajcs#clinical surgery#Raymond Kao MD MPH*
0 notes
Text
Does health insurance cover coronavirus in India? Are you safe?
While the coronavirus is on top of everyone’s mind, India is slowly marching towards a critical situation as the affected population grows each day. But even in this chaos, we cannot turn down the thoughts of the expenses that would come as a result of coronavirus treatment and the doubts regarding our insurance coverage for coronavirus. So, does health insurance cover coronavirus in India?
But first, let us take a step back and see why do we need a health insurance cover for coronavirus in India.
Why is insurance coverage for coronavirus important?
COVID-19 has affected lakhs and lakhs of people worldwide and its severity is only increasing. This disease will result in severe respiratory illness, kidney problems, lung infection and even multiple organ failure. And you will be admitted to the hospital for at least 3 weeks for the treatment of all these problems caused by the coronavirus. This will result in a hefty fee including the bed charges, medicines, food and the other charges incurred as a result of treatment and hospitalization.
Check out the treatment and test cost of Coronavirus
In times like these when the global economy is bad and financial problems are at our doorstep, dealing with a sudden medical charge can take a heavy toll on your life. This is why you need an insurance cover for coronavirus to act as a safety cushion. Health insurance for coronavirus can cut down your treatment and hospitalization cost and lessens your burden.
So, can you get health insurance for coronavirus in India?
Earlier this month, the Insurance Regulatory Development Authority of India (IRDAI), issued a circular stating that coronavirus treatment would be covered like any other illness “under products where hospitalization is covered”. For all policies covering the disease, the regulator also directed the companies to cover the cost of admissible expenses, including treatment during the quarantine period.
So, the answer is Yes. But you must already have an existing health insurance policy to get the benefits or you can enroll in a special coronavirus insurance cover. However, if you enroll in a health insurance policy after contracting the disease, you will not be eligible to claim any benefits for the treatment.
Furthermore, some general insurance companies like star health insurance, Digit healthcare and ICIC Lombard have introduced a limited period, non-renewable novel coronavirus policy for those who test positive for COVID-19.
Yet, still, the coverage for coronavirus will depend solely on the conditions of your life insurance policy, add-ons, and benefits that you adhered to when you signed up for the health insurance.
What does coronavirus health insurance plans cover?
According to the IRDAI, all the treatment and hospitalization charges for coronavirus will be covered under your health insurance plan. This includes medical costs including in-patient hospitalization, pre-hospitalization care, post-hospitalization care, ambulance, ICU, surgery and OPD charges.
Some important things to keep in mind about health insurance coverage for coronavirus in India:
If you have any confusion and questions regarding your insurance coverage for coronavirus, here are a few important things to keep in mind.
24-hour rule: You can only claim your insurance for coronavirus if are hospitalized for at least a period of 24-hours. If you are not hospitalized for this said period, it will be seen as an outpatient treatment (OP) and OP treatments are usually not covered in health insurance policies.
The ‘Pandemic’ criteria: The World health organization (WHO) has declared the coronavirus outbreak as a pandemic. This may be a concern because some of the insurers may not settle your health insurance claim if the disease comes under the pandemic criteria.
Waiting period: In an unfortunate situation where you contract the disease in your policy waiting period, you will not be eligible for the insurance claim. In general, the waiting period would be 30 days.
The ‘medical emergency’ reimbursement: Most insurance policies consider coronavirus infection as a medical emergency. So, even if you bear the burden of paying the treatment bills from your savings, you can later apply for reimbursement with the necessary documents.
Coronavirus outbreak in India is serious and we are definitely in a critical situation. And while most of the insurance providers are providing the health insurance cover for coronavirus in India, our utmost focus should be to stay safe at home following the precautionary measures against coronavirus.
0 notes
Text
A night in the life: Night shifts
[NB: all cases altered and de-identified, to point of being generic]
2100 hrs: Handover time. I’m on subspecialty cover for nights. As a rule where I work, no interns are allowed to cover a few of the subspecialties with potentially higher numbers of critically ill patients. Not all hospitals are like this in the area. At any rate, it means I do a mix bag of jobs, from your run of the mill answering of pages to admissions, to attending codes for affected patients. - I get handed over a patient at risk of deteriorating - 2 codes in one day for hypotension, in setting of a diabetic limb - they’re also post op day 5 of a mid foot amputation. ICU is full, but so far their BP has been holding after the last fluid bolus. They’re also on 3 different IV antibiotics. Asymptomatic. Teetering. But stable. - pager goes off. Need a sleeping tablet for one patient. Analgesia for another, no PRN ibuprofen charted. - one sick patient handed over and a couple of light pages, not a bad start to a night. on bad ones I might have 3 admissions lined up and 2 expected admissions from country.
2130 hrs: - prioritize the jobs and head over to see the sickest patient I have, and eavesdrop on the nursing handover for this particular one. Then call the night shift ICU registrar/senior resident, to discuss, but coincidentally, they’ve also arrived to assess. In the event of a code, we both now know the patient and scenario. - another patient reports 7/10 pain D3 post op amputation, just started on ketamine infusion that morning. Then they fall asleep mid sentence and start to snore. - quickly answer some pages, and give phone orders where I can.
0000 hrs - notified about a transfer from a country hospital. needs admission. - reminds me of the forrest gump quote, life is like a box chocolates, never know what you’re going to get. and that’s exactly how i feel about country transfers. you get some of the story over the phone, but you never what actually comes through the door until they arrive - it’s pyelonephritis of a renal transplant graft, with AKI in a 22 year old.
0100hrs - A concerned ED doc calls. New admission - patient with diabetes, but is not on treatment, who has necrosis or gangrene in the foot. Patient came in with a temperature and trouble breathing - they were in fluid overload too. They argued with their kids who called the Ambulance, who noted that the toes were so black, they looked like you could just snap them off. ED puts them on some of the strongest IV antibiotics under the sun. they’ve also notified the surgeons. - the patient in their 60s, had been treating their foot with tea tree oil, last saw a doctor about 20 years ago. They tell me they don’t believe in doctors and don’t want therapy - i later learn the patient was adamant about no further antibiotics, no diuresis, no surgery, nothing. they were palliated and died shortly after, of their own accord. - it reminded me of a couple of other patients I had. patients with advanced cancer whether lung or breast, or other major medical conditions. who refuse all treatment opting for homeopathy instead. Until at last, unable to cope at home they come to hospital. - in the end what we see is the natural progression of their disease. diabetes left untreated, heart failure left untreated, congenital heart disease, breast cancer with metastases to lungs, brain and bone. things you read in a text book and never expect to see in the age of modern medicine. but we now begin to see them all again, just like all the paediatric diseases we wouldn’t expect to see in the age of vaccination.
0200hrs: - paged to place an IDC into a delirious patient with urinary retention to 1L on a post void bladder scan. - I used to be slow and nervous about IDCs.. but after so many night shift requests for these.. I can do it under 10 mins now. Sometimes 5 mins if I’m really pressed for time and the nurses have already set up for me. It’s almost always awkward for the poor patients, but for me.. as one resident said, “it’s just another elbow in medicine”. - I reflect later that I’ve unintentionally seen possibly 100s of naked men on this job now. And handled their genitalia to put foley’s down too many times to count, I never thought that would happen 10 years ago. If you’re squeamish or prudish about sexual organs, this really isn’t the career for you. - a lot of older men go into urinary retention when they’re unstable or after surgery. - few more pages about hard cannulas on patients with no ‘veins left’ etc. at 0230hrs I hit the night shift coffee truck that pulls into ED. In queue are other residents, nurses, construction workers from a site next door, police officers. etc. there’s nearly always police officers in ED nowadays, often just babysitting outside a cubicle. a few months ago there were a couple of public service campaigns on hospital violence.
0300hrs: - page about a patient with tachypnoea after a bronchoscopy during day shift, despite 3 L of O2 via nasal prongs. - The saturations fluctuate between 88-93% (when they were previously 100% a week ago) recent diagnosis of PJP pneumonia in sputum PCRs. They’re a transplant patient on immune suppressants. - I take a blood gas, they’re in type I failure. but their saturations pick up with high flow. I briefly chat to an ICU registrar/senior resident, for extra support or advice. happy with high flow, wait till morning for a respiratory team review. we stress dose them with steroids.
0400hrs - another page, another admission -- 25 yo out on a saturday night, too many shots of tequila. in the setting of binging every weekend since their teens. they woke up with melaena and small vomits of frank red blood in the shower. ED starts them on PPI infusion, Hb is stable and their vitals are stable. They’re booked for an endoscope in a few short hours. - I hate counselling someone close to my age on drinking habits, I do it anyway. Remembering the night before I was having to have a family meeting with the family of one patient in liver failure at 2 am. they’d been drinking heavily for 20-30 years. They had portal hypertension, haemorrhoids. And they were coming in encephalopathic for the first time. It’d been a while since I’d seen such an emphatic hepatic flap. I forget sometimes, most of the general public have no idea what liver failure is or what it entails. It’s hard conversation to have. 0430hrs: - I review the sicker patients on shift briefly and get updates from the nurses. Reassure junior ones looking after the sicker patients about plans and vital signs.
0530hrs - things are settling. I eat an apple. It’s actually rare for things to settle, usually I’m catching up on smaller jobs. It hasn’t been a bad night. I contemplate catching up on studying for boards or research, but end up typing up some discharge summaries for day shift teams. Knowing how much it means to them having a couple of summaries ticked off.
After a time, it’s teaching and handover time. It’s nice to see ‘people’ again, the ward clerk, day shift residents & nurses all pouring. It’s like an invisible bell has gone off somewhere, as if to say ‘school’s started’ or something. Sometimes I forget how lonely nights are until I see them piling in. After a few moments to handover and a couple of ‘have a good sleep’s’, they turn to their computers, and hunch over. Looking intense, bracing themselves as shifts begin for them.
115 notes
·
View notes