#Paradigm process for depression treatment
Explore tagged Tumblr posts
Text
Anne's World: A New Century of Anne of Green Gables
Part 1: Introduction (Irene Gammel)
"Anyone who has ever encountered her in one of L.M. Montgomery's novels will never forget her, for she is what we're not - and all that we long for and shall never become." - Jack Zipes on Anne Shirley
Key questions the book wants to answer:
"How do we read this early twentieth-century novel in ways that are relevant for readers of the twenty-first century?
How do the novel’s ethical dimensions fit into our own era?
Can Anne of Green Gables be read as a therapeutic text, capable of counteracting depression?
What is the power and danger of digital encounters with Anne?"
The goal of this book:
To consolidate and expand upon previous scholarship and information by placing Anne in its contemporary context while also exploring the reception and cultural impact, providing new references for future study.
The essays:
'Seven Milestones: How Anne of Green Gables Became a Canadian Icon' (Carole Gerson) "argues that Anne’s longevity is partly the result of a series of ‘institutional, commercial, and grassroots interventions."
'Matthew Insists on Puffed Sleeves: Ambivalence towards Fashion in Anne of Green Gables' (Allison Matthews, David and Kimberly Wahl) "argues that the text allows Anne Shirley to have it both ways: others want her to be fashionable and ambitious, whereas she wants to fit in."
'I'll never be Agelically Good: Feminist Narrative Ethics in Anne of Green Gables' (Mary Jeanette Moran) "reveals that the novel conforms to a feminist ethical paradigm because it tends to value those ethical choices that preserve or maintain relationships to support the principle that those who nurture others must also care for themselves, and to challenge the assumptions that women naturally care for others or that they alone bear the responsibility to do so."
'Too Headless and Impulsive: Re-reading Anne of Green Gables through a Clinical Approach' (Helen Hoy) "argues for the possibility of reading Anne Shirley as a psychological case study."
'Reading to Heal: Anne of Green Gables as Biblio-therapy' (Irene Gammel) "argues for reading Montgomery’s fiction within the important context of bibliotherapy, or the use of books in the treatment of personal and mental disorders."
'Reading with Blitheness: Anne of Green Gables in Toronto Public Library's Children's Collections' (Leslie McGrath) "examines how Montgomery’s literary reputation endured wide swings of critical opinion"
'Learning with Anne: Early Childhood Education Looks at New Media for Young Girls' (Jason Nolan) "looks closely at Anne of Green Gables: The Animated Series, Anne’s Diary, and New Moon Girls as prominent examples of how Anne of Green Gables and the work of Montgomery in general have been taken up as locations for formal and informal learning, through the identifi cation of Anne as variously a marketing icon, as an ideal young girl, and through the way Montgomery constructed learning environments within her novels."
'On the Road from Bright River: Shifting Social Space in Anne of Green Gables' (Alexander MacLeod) "studies the ways in which the characters inside the novel, like the readers outside of the text and the real-world visitors to the Green Gables National Park site in Cavendish, Prince Edward Island, are all engaged in a complex process of reading and rewriting social space"
'Anne in a "Globalized" World: Nation, Nostalgia, and Postcolonial Perspectives of Home' (Margaret Steffler) "explores the impact of the novel and character both outside and within Canada, arguing that the attraction of Montgomery’s work continues into the twenty-first century because it resonates with conditions in contemporary lives and culture, specifically the emotions and activity involved in migratory patterns of losing and creating home"
'An Enchanting Girl: International Portraits of Anne's Cultural Transfer' (Andrew O'Malley, Huifeng Hu, Ranbir K. Banwait, Irene Gammel) "shines a light on the crossover points from one culture to another, identifying cultures that have ‘appropriated’ Anne for very different purposes"
'What's in a Name? Towards a Theory of the Anne Brand' (Benjamin Lefebvre) "draws on film and cultural theories to consider paratextual Annes in terms of authorial ownership, control, and narrative pleasure"
'Mediating Anne' (Richard Cavell) (afterword) "closes off the book by providing a jumping-off point, looking forward to future research exploring the global Anne."
hi hi hi! I just discovered this book from 2010, which is a collection of essays on Anne of Green Gables, and I thought I might go through each essay and share my thoughts on the pieces! If anyone else has this book or access to any of the essays (some of which I think you can find online) I would love to discuss them with you! xoxo lily
#anne of green gables#aogg#lm montgomery#lucy maud montgomery#anne shirley#anne's world#literary analysis#my love#lmm lockdown
25 notes
·
View notes
Text
I'm so sorry to get cognitive behavioral in this thread of creative commiseration. however. you do not need to be beholden to your brain's whims of expressive drive (yes, even with other complicating conditions like depression or chronic pain, assuming those have some treatment or control. if not, this might help, but other pressing issues make themselves known for a reason!)
"responsive desire" is when your friend invites you to a party/gathering, and you think "ugh I'm tired should I really go? I have fun once I'm there but UGH, actually going there is so hard." and once you've been there a while, you realize "hey, this is fun! it's not perfect and I am tired, but I like how it turned out and it was pretty rewarding!"
you gotta start before you want to. lots of people struggle with the inverse of responsive desire, which is spontaneous desire. the one where we are (supposed to just be) overcome with passion or outgoing urge to create, hang out, do something challenging, etc. if you have executive dysfunction or mood-related disorder, then spontaneous may not be the route for you! it's just not reliable enough. it's not fair that other people just want to do the thing and do it, but we're not up a creek yet! there are options still.
I can't force you to do anything, and I don't expect you to materialize willpower out of nothing. but knowledge about how creative drive is empowering and that might start to create the something out of nothing. the next time you think, "I really wanna do my creative thing but I just don't want to," maybe you won't beat yourself up for not being good enough or creative enough, etc etc, and so continue to teach yourself to feel bad about your creativity. maybe you'll remember this paradigm about drive. then this time or maybe another time, you set a 5-minute timer and just do the thing the entire 5 (or 3, or 1 even!) minutes and stop if you hate it but keep going if it's nice. either way you'll have at least 5 minutes of work in, which is all the more practice for habit-setting.
this isn't a linear process, it's not unidimensional. but it breaks my heart to see people hating on themselves so much! it's not your fault. you're just a person who can't perform perfectly in a system and world that demands too much. you're tired, and yet you're just supposed to become an artist or writer out of passion and spontaneous desire, as if you aren't stretched paper-thin? it's not right. you are a perfectly good person and deserve to be treated kindly, which includes you treating yourself. habits are hard to form, and no one gets taught these things in daily life!
learning to foster time to cultivate creative desire and reinforce regular joyful (not self-punishing) creative habit is such an important skill! there's nothing wrong with you for not being born knowing how to do something. I believe in you! start small, use reminders, and most of all be gentle and kind with yourself! you have plenty of time to grow.
160K notes
·
View notes
Text
A new era of weight loss: Mental health effects of GLP-1 drugs - American Psychological Association (APA)

Entering a new era of weight loss: Mental health effects of GLP-1 drugs is a topic increasingly gaining attention from the American Psychological Association (APA). As obesity remains a pertinent health issue worldwide, there's been a growing interest in exploring novel, effective, and safe solutions. GLP-1 drugs have emerged as a game-changer in the weight loss scene but have an unusual side effect – they appear to influence mental health. The connection between GLP-1 drugs and mental health opens up a brand new perspective on weight loss medication and sets the stage for new discoveries that can transform billions of lives. As experts unravel the mental health effects of GLP-1 drugs, they are finding the ties between obesity and mental health complexities. Precisely, GLP-1 drugs not only alleviate obesity but also show promise in treating mental health disorders. They're believed to impact the way brains process reward cues, thereby potentially reducing cravings for high-calorie food, curbing binge-eating tendencies, and simultaneously improving mental health. With data supporting these findings, the American Psychological Association (APA) identifies this as a new era of weight loss: Mental health effects of GLP-1 drugs. It signals a significant shift in the approach to obesity, showcasing potential two-fold benefits. On one hand, it may provide a solution to weight loss; on the other, it might pave the way to manage and treat mental health disorders simultaneously. Obesity often stirs up self-image issues and enhances vulnerability to depression, anxiety, and other mental health problems. Conversely, mental conditions can also make efforts toward weight loss more difficult. The emergence of these novel GLP-1 drugs provides a ray of hope, as they may act as a tether linking obesity and mental health, providing a potentially holistic solution. Clinical trials on GLP-1 drugs are ongoing, with promising results so far. However, as with any new treatment, several factors, including the potential for unknown side-effects, must be vigilantly observed. Further research is also needed to establish how these drugs can be best utilized to aid weight loss without adverse impacts on mental health. The new era of weight loss: Mental health effects of GLP-1 drugs, being championed by the American Psychological Association (APA), signifies an enticing shift in how obesity and mental health can be tackled together. It plants the seeds for a more empathetic and holistic approach to obesity, one that recognizes the importance of mental health in weight loss. This paradigm shift promises hope to millions battling obesity and mental health issues alike, illustrating that weight loss and mental wellness needn't be mutually exclusive but can harmoniously co-exist. Retail buyers → https://glp1weightloss.fit/ Wholesale buyers → Wholesale Registration {"@context": "http://schema.org", "@type": "Article", "headline": "A new era of weight loss: Mental health effects of GLP-1 drugs - American Psychological Association (APA)", "description": "Meta Description: Discover how GLP-1 drugs are sparking a new era of weight loss by potentially impacting mental health, as explored by the American Psychological Association (APA).", "image": "https://images.pexels.com/photos/8433470/pexels-photo-8433470.jpeg", "author": {"@type": "Person", "name": "Fitwiz25"}, "datePublished": "2025-07-03T04:01:10.296930"}
0 notes
Text
What Makes Patient Care Services So Essential Today?

As lifestyles become more demanding and families juggle between work, personal responsibilities, and health concerns, Patient Care Services in South Delhi have emerged as a critical solution for managing the care of elderly, chronically ill, or recovering patients. These services not only ensure medical support at home but also offer much-needed emotional and physical care, which can be difficult to provide consistently within families.
The Shift from Hospital to Home
Modern healthcare is witnessing a paradigm shift where home-based care is increasingly preferred over prolonged hospital stays. Hospitals are often associated with stress, unfamiliarity, and the risk of infection, especially for those with compromised immunity or mobility issues.
Home-based services allow patients to heal in a comfortable and familiar environment, surrounded by loved ones. This setting significantly boosts recovery, especially after surgeries, strokes, or long-term treatments like chemotherapy or dialysis.
Personalized Support for Every Need
One of the primary reasons home patient care services in South Delhi are in high demand is the level of personalized support they provide. Unlike hospital environments, where a nurse or doctor may be attending to several patients at once, home care is dedicated and one-on-one.
These services are customized to the specific health condition and lifestyle of the patient. Whether it involves monitoring blood pressure, assisting with mobility, or managing medication, the care is always centered around the patient’s comfort and well-being.
Vital Role of Trained Care Takers
Home patient care taker services in South Delhi bring trained professionals into your home who understand both the clinical and emotional aspects of patient care. Caretakers help with daily activities such as bathing, dressing, feeding, and maintaining hygiene. More importantly, they provide companionship, observe changes in behavior or health, and offer comfort that goes beyond medical needs.
Their presence offers relief to family members who may be unable to provide 24/7 care due to professional or personal commitments. With skilled caretakers, families gain peace of mind knowing that their loved ones are in safe, capable hands.
Managing Chronic Illness and Recovery
Chronic illnesses like diabetes, arthritis, dementia, and hypertension require consistent care and attention. Hospital visits for routine monitoring can be tiring and stressful. With professional patient care services, this burden is greatly reduced.
For patients recovering from surgeries or severe illnesses, in-home care accelerates the recovery process. Regular physiotherapy, medication reminders, nutritional guidance, and emotional support at home can lead to faster and more holistic healing.
Elder Care: A Growing Need
As the elderly population increases, so does the need for specialized elder care. Many seniors prefer to age in the comfort of their own homes rather than move to retirement facilities. Patient care services ensure that they receive medical attention, daily assistance, and social interaction, all while maintaining their independence and dignity.
For many families in urban areas, where nuclear family structures and busy schedules are common, this is an invaluable solution.
Emotional and Mental Well-Being
Beyond physical support, professional care services also play a huge role in improving mental health. Patients who are bedridden or dealing with long-term illness often face depression and isolation. Caregivers act as companions, offering encouragement, engaging in conversation, and helping patients stay mentally active and emotionally secure.
This emotional bond contributes to a more positive attitude and enhances the overall healing experience.
Conclusion
In today’s fast-paced world, the need for reliable and professional care at home has never been greater. From medical supervision to emotional companionship, Patient Care Services in South Delhi are proving to be an essential pillar in modern healthcare.
Whether it’s chronic illness, post-surgical care, or elder assistance, home patient care services in South Delhi and home patient care taker services in South Delhi offer a well-rounded, compassionate approach that blends professionalism with personal touch—right where it matters most: at home.
0 notes
Text
Navigating the Future: Can Innovative Approaches Solve the MDD Treatment Challenge?

Major Depressive Disorder (MDD) continues to present one of the most significant public health challenges globally, affecting over 280 million individuals worldwide. Despite considerable scientific advances over recent decades, the effectiveness of current MDD medications remains suboptimal for many patients. With remission rates for first-line treatments hovering around 30%, clinicians and researchers alike are looking toward emerging pipelines to address this persistent treatment gap.
The Limitations of Traditional Approaches
The conventional treatment pathway for MDD typically starts with prescribing SSRIs or SNRIs as first-line interventions. Despite their widespread use, these major depressive disorder medications present several limitations that hinder optimal outcomes. Response rates rarely exceed 60%, with substantially lower complete remission rates. Additionally, these medications typically require several weeks to demonstrate therapeutic efficacy, creating a critical vulnerability period during which patients may remain at elevated risk.
The heterogeneous presentation of depression further complicates treatment selection. With diverse symptom profiles and biological mechanisms potentially at play, the MDD treatment landscape has been characterized by incremental improvements rather than revolutionary breakthroughs. This reality has perpetuated a trial-and-error approach that extends suffering and increases the economic burden on healthcare systems.
Breaking New Ground: Novel Mechanism Therapies
The development of MDD therapies has experienced a paradigm shift in recent years, moving beyond the monoamine hypothesis that has dominated research for more than half a century. Innovative approaches targeting glutamatergic systems, neuroplasticity, and inflammatory pathways represent promising new frontiers in depression treatment.
Ketamine and its derivative esketamine have emerged as pioneering rapid-acting antidepressants, offering relief within hours rather than weeks for treatment-resistant patients. This breakthrough has sparked renewed interest in developing similar compounds with improved safety profiles and sustained efficacy.
The resurgence of interest in psychedelic-assisted therapies marks another innovative direction. Substances like psilocybin and MDMA, when administered within structured therapeutic frameworks, show promise in facilitating emotional processing and psychological insights that conventional treatments often fail to achieve.
The Promise of Personalized Treatment Approaches
A potentially transformative development in depression management is the emergence of precision psychiatry. This approach aims to match patients with optimal interventions based on their unique biological, psychological, and environmental characteristics, potentially minimizing the inefficiencies of conventional treatment selection methods.
Pharmacogenomic testing now enables clinicians to identify genetic variations that influence medication metabolism and response, potentially streamlining treatment selection. Emerging biomarkers based on neuroimaging, inflammatory profiles, and other biological measures may further refine treatment matching in the future.
This personalized approach extends beyond pharmacotherapy to encompass psychological interventions, lifestyle modifications, and neuromodulation techniques, creating comprehensive treatment strategies tailored to individual patient needs.
Technology as a Catalyst for Access and Engagement
Digital innovation represents another promising frontier in addressing the MDD treatment gap. Smartphone applications delivering evidence-based psychological interventions are increasingly prescribed alongside traditional MDD medicines, extending the reach of therapeutic support beyond clinical encounters.
These digital solutions help overcome significant barriers to care, including stigma, geographical limitations, and provider shortages. Telehealth platforms now offer remote psychiatric consultations, medication management, and therapy sessions through accessible interfaces, dramatically improving treatment accessibility.
Evaluating the Pipeline's Potential Impact
While the current development pipeline shows unprecedented diversity and innovation, significant hurdles remain before these advances can fully transform patient outcomes. Regulatory requirements, reimbursement challenges, and implementation barriers may delay or limit the real-world impact of these promising interventions.
Moreover, the complex, multifactorial nature of depression suggests that no single approach—however innovative—will likely resolve the treatment challenge completely. The future of effective depression management may instead lie in integrated approaches combining pharmacological, psychological, lifestyle, and technological interventions tailored to individual needs.
Conclusion
The robust pipeline of novel treatments for MDD offers substantial promise for addressing the limitations of current approaches. While it may not entirely solve the complex treatment challenges, it will likely transform clinical practice by providing more effective options, faster symptom relief, and more personalized care models.
As these innovations transition from development to clinical implementation, continued research, cross-disciplinary collaboration, and patient-centered care models will be essential to maximize their impact on this prevalent and debilitating condition.
Latest Blog Offered By DelveInsight:
Fierce Competition Lies Ahead for Pipeline Therapies in the Rheumatoid Arthritis Market
Which Key Player Holds the Potential to Corner the Rheumatoid Arthritis Therapeutics Market?
Huge Unmet Needs in the Glioblastoma Multiforme Treatment Market Driving the Market Size Growth
Glioblastoma Multiforme Market: Emerging Pipeline Therapies To Keep A Keen Eye On
13 of the most commonly asked questions about Glioblastoma multiforme, Answered
Glioblastoma Multiforme: Advancements in the Treatment Paradigm of the Malignant Condition
Latest Reports:-
Achondroplasia Market | Acral Lentiginous Melanoma Market | Ada-scid Competitive Landscape | Adrenal Cortex Neoplasms Market | Adult Spinal Deformity Market | Aicardi-goutières Syndrome Market | Anemia Market | Angelman Syndrome Market | Angioimmunoblastic T-cell Lymphoma Market | Ankylosing Spondylitis Bekhterevs Disease Market | Anovulation Market | Anterior Uveitis Market | Atherosclerotic Cardiovascular Disease Market | Bacteremia Market | Bcl-2 Inhibitors Market | Braf-mutant Metastatic Melanoma Market | Bronchiectasis Market | Bullous Pemphigoid Market | Burkitt Lymphoma Market | Cdkl5 Deficiency Disorder Market | Centronuclear Myopathy Market | Chlamydia Infections Market | Chondrosarcoma Market | Chronic Constipation Market | Chronic Hepatitis Delta Virus Market | Chronic Pulmonary Infections Market | Chronic Refractory Cough Market | Clostridium Difficile Infections Cdi Market | Clostridium Difficile Infections Market | Cluster Headaches Market | Community-acquired Pneumonia Market | Contact Dermatitis Market | Cushing Syndrome Market | Cutaneous Lupus Erythematosus Market | Dermatomycoses Market | Dermatomyositis Market
#major depressive disorder market#mdd in pharma#mdd medicine#auvelity#travivo#neumora therapeutics#pipe-307 depression#major depressive disorder medication#major depressive disorder therapies#mdd
0 notes
Text
The Impact of Gut Microbiome on Mental Health: Exploring the Gut-Brain Connection
Introduction
The relationship between gut health and mental well-being has emerged as one of the most fascinating areas of medical research. Scientists have discovered that the trillions of microorganisms residing in our digestive system play a crucial role in mental health, leading to a paradigm shift in our understanding of psychiatric conditions. This article explores the intricate connection between the gut microbiome and mental health, examining current research and potential therapeutic implications.
Understanding the Gut-Brain Axis
The Bidirectional Communication System
The gut-brain axis represents a complex communication network that includes:
The enteric nervous system
The vagus nerve
The immune system
The endocrine system
The microbiome-gut-brain axis
Key Mechanisms of Communication
The gut microbiota influences mental health through multiple pathways:
Neurotransmitter production
Inflammatory mediators
Hormone regulation
Vagus nerve signaling
Metabolite production
The Gut Microbiome's Role in Mental Health
Depression and Anxiety
Research has revealed significant correlations between gut microbiota composition and mood disorders:
Altered microbial diversity in depressed patients
Specific bacterial strains linked to anxiety levels
Inflammation's role in mood regulation
Neurotransmitter production by gut bacteria
Impact on stress response systems
Stress Response
The gut microbiome influences stress resilience through:
Regulation of cortisol levels
Modulation of the HPA axis
Impact on neuroplasticity
Influence on emotional processing
Stress-related immune responses
Cognitive Function
Emerging evidence suggests microbiome effects on:
Memory formation and recall
Learning capabilities
Attention and focus
Cognitive flexibility
Neural development
Research Findings and Clinical Evidence
Human Studies
Recent clinical research has demonstrated:
Associations between dysbiosis and mental health conditions
Effects of probiotics on mood and anxiety
Impact of dietary interventions on mental health
Microbiome changes in psychiatric disorders
Treatment response correlations
Animal Studies
Laboratory research has revealed:
Causal relationships between microbiota and behavior
Mechanisms of gut-brain communication
Effects of microbiome transplantation
Developmental impacts of gut bacteria
Strain-specific behavioral effects
Therapeutic Implications
Dietary Interventions
Evidence-based dietary approaches include:
Prebiotic-rich foods
Fermented foods
Anti-inflammatory diets
Fiber-rich nutrition
Specific dietary patterns
Probiotic Treatments
Promising probiotic interventions focus on:
Specific bacterial strains
Targeted supplementation
Combination approaches
Timing of administration
Individual response patterns
Clinical Applications
Diagnostic Potential
Microbiome analysis may aid in:
Early detection of mental health conditions
Treatment response prediction
Patient stratification
Disease progression monitoring
Intervention planning
Treatment Strategies
Emerging therapeutic approaches include:
Microbiome modulation therapy
Personalized dietary interventions
Combined psychological and gut-targeted treatments
Lifestyle modifications
Targeted supplementation
Future Directions
Research Priorities
Key areas for future investigation include:
Mechanism elucidation
Biomarker development
Treatment optimization
Individual variation understanding
Long-term effects assessment
Technological Advances
Emerging technologies enabling progress:
Advanced sequencing methods
Metabolomic analysis
Real-time monitoring systems
Artificial intelligence applications
Precision medicine approaches
Practical Implications
Lifestyle Recommendations
Evidence-based suggestions include:
Dietary diversity
Stress management
Regular exercise
Sleep hygiene
Environmental considerations
Prevention Strategies
Preventive approaches focus on:
Early life interventions
Microbiome protection
Stress reduction
Dietary education
Environmental factors
Conclusion
The growing understanding of the gut-brain axis represents a revolutionary advancement in mental health science. This knowledge opens new avenues for treatment and prevention of mental health conditions through microbiome-based interventions. As research continues, the integration of gut health strategies into mental health care may become a standard approach to treatment.
The future of mental health care likely lies in holistic approaches that consider both traditional psychiatric interventions and microbiome-based treatments. Continued research and clinical application of these findings will be crucial in developing more effective therapeutic strategies for mental health conditions.
0 notes
Text
Paradigm process for depression treatment
We learned to treat the personality with the best therapy model we could find which is the Paradigm process for depression treatment. We grew tired of hearing that people of the world now believe that they have to cope with depression, anxiety, burnout and personality or mood disorders. Medicine is not enough and has led to a further spike in the mental health crisis. We send people for…
#best therapy for depression#depression symptoms#depression treatment centre#inpatient treatment centre#Paradigm process for depression treatment#treatment resistant depression
1 note
·
View note
Text
MR3: The DSM has undergone significant changes since its first edition in 1952, particularly in diagnostic criteria and categories. How has its evolution shaped the understanding and treatment of mental health disorders?
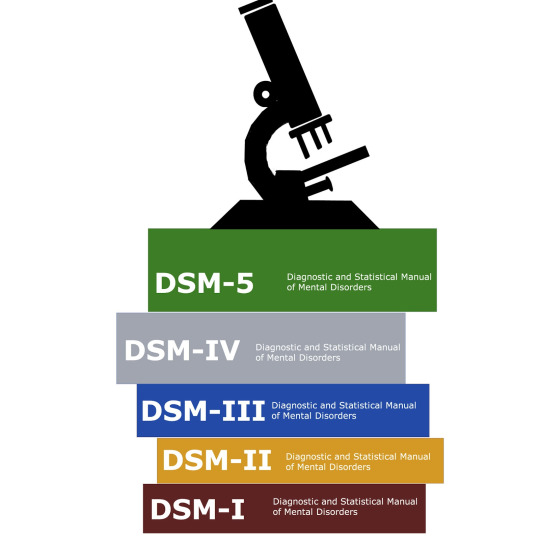
In the early 1800s, German physicians Kraepelin and Alzheimer developed methods to identify neurological diseases such as dementia. They discovered that mental illness has a biological basis, but their work was, unfortunately, ignored by American psychiatry during that time. In 1844, psychiatry was finally recognized as a specialty by the Association of Medical Superintendents of American Institutions for the Insane, which eventua;ly became the American Psychiatric Association (APA). In the 1970s, since there wasn’t a propper and unified diagnostic method, there was a large proportion of discrepancies regarding psychiatric illnesses in the U.S. and U.K. Many patients that were diagnosed with schizophrenia in the U.S. would be diagnosed with manic-depressive illness in the U.K. Finally, an agreement would come into existence in 1980, which was the DSM-III. During the mid 20th century, in St. Louis, Missouri, a group of researchers changed the way psychiatry would be diagnosed. They were unhappy because diagnostic classification was baked on clinical opinions rather than systematic research. They avoided assumptions and focused their work on strategies in order to care for patients who had psychiatric illness. 1952 saw the publication of the Diagnostic and Statistical Manual, Mental Disorders (DSM). The DSM was divided into two sections, one that had disorders which were established organic brain disease, and the other fir disorders with no evidence of brain diseases. Between 1952-2013 there have been 5 revised DSMs, all with the goal of improving from the previous revision. Kendler and First identified two strategies for future revisions: 1. An “iterative model” which is small changes to the current one, 2. A “paradigm shift model”, which discards the current one for a completely new diagnosis (Kendler & First, 2010).
References:
Kendler, K. S., & First, M. B. (2010). Alternative futures for the DSM revision process: iteration v. paradigm shift. The British Journal of Psychiatry, 197(4), 263-265.
Surís A, Holliday R, North CS. The Evolution of the Classification of Psychiatric Disorders. Behav Sci (Basel). 2016 Jan 18;6(1):5. doi: 10.3390/bs6010005. PMID: 26797641; PMCID: PMC4810039.
3 notes
·
View notes
Text
Enhance Cognitive Health Through Brain Mapping
Maintaining cognitive health is crucial for the best way of living and healthy life. Cognitive knowledge refers to the comprehension of the way the brain works to enhance its performance. Or how to get a clearer and sharper mind. One of the complicated methods of studying the electrical activity of the brain is so-called mapping. Here is a guide if you’re searching for “Brain Mapping Las Vegas”. So the article describes the principle of the procedure and the use of Brain Mapping for the health of the brain.

What Is Brain Mapping?
Brain mapping is also an investigative procedure that does not involve surgery to capture images. That illustrates the electrical activity of the human brain. It aids physicians and mental health practitioners in visualizing the way your brain gets information.
How Brain Mapping Works
PACE is done by the use of an electrode that is fixed on the scalp by a cap known as PACE.
The system measures the activity in the brain and can record the result in real-time.
Through the use of data, it is possible to notice the existence of some oddity or disparity in the functioning of the brain.
Benefits of Brain Mapping
There are various benefits associated with the utility of brain mapping in maintaining the cognitive health of a human being including the following;
Treatment paradigms: Can deliver individualized therapy methods depending on the signals produced by the brain.
Mental Purity: Signs that reflect on Lodz vascular efficiency to tell if one has concentration issues or not.
Stress Reduction: Assists in identifying the signals originating in the brain that are related to stress and anxiety.
Effectiveness of Sleep; used in diagnosing sleep disorders.
Memory Enhancer: Provides specific regions of the brain that is involved in memory storage.
So if you are looking for these benefits. Then you should go for brain mapping. Because it will help your loved one to not lose memory.
Who Can Benefit from Brain Mapping?
Neuroimaging maybe helpful in treating people provided they are suffering from:
Psychosis
Memory Loss
Learning Difficulties
Chronic Stress
ADHD
Autism
ADHD and Autism are disorders that help people comprehend neurological disorders. So, if you or your loved one is suffering from these diseases, Then you should not wait and go for treatment.
The Brain Mapping Process in Las Vegas
Looking for information on ‘Brain mapping Las Vegas’ Here's what you can expect:
Initial Consultation:
Consult with a specialist to make sure your symptoms are aligned with the treatment plan and keep your worries in mind.
Brainwave Recording:
Comfortable and painless data collection through a special cap.
Analysis:
As a result of the process, a comprehensive analysis report is produced with references. To the density of activity of various human brain areas.
Treatment Recommendations:
The offered remedies include individualized medical therapies, including neurofeedback therapy.
Cognitive Conditions Addressed Through Brain Mapping
So some of the cognitive conditions are as follows: Neuroimaging is useful in the diagnosis and treatment of many forms of cognitive disorder:
Mood Disorders: Anxiety, depression, and bipolar disorder
Cognitive Decline: Early detection of Alzheimer's disease
Behavioral Issues: Impulse control and emotional regulation
ADHD Focus Deficit: A paragraph discussing attention deficits that are associated with the ability to focus
Brain Mapping for Peak Performance
It is also important to note that brain mapping is not restricted to only the patients having cognitive disorders. It also assists those who are aspiring for:
Enhanced Productivity: Optimize brain function for work efficiency.
Sports Performance: Improve focus and mental resilience.
Creative Pursuits: Tap into creative brainwave patterns for artistic endeavors.
Why Choose Brain Mapping Las Vegas Services?
So, you want to find a place for professional brain mapping in Las Vegas? Here are some of the characteristics you should pay attention to when choosing.
A critical qualification of any clinic would be to make sure that there is enough qualified specialists, including brain mapping experts.
Electroencephalography (EEG): The organization should be equipped with the best equipment that is currently on the market.
Thorough Check-up: The clinic of your choice should offer extended treatments of therapies and additional consultations.
Patient Testimonials: Patient feedback from past patients to ensure the quality of the services delivered by the company.
Lifestyle Tips to Maintain Cognitive Health
The following are some tips that I would like to add to the techniques of Brain Mapping:
Regular Exercise: Boosts blood flow to the brain.
Healthy Diet: Include brain-friendly foods like nuts, berries, and fatty fish.
Mindfulness practices: Exercises include; simple tasks of meditation and breathing exercises to relieve stress.
Sufficient rest: 7-9 hours of sleep should be achieved every night.
Lifelong learning should be continued as this helps inежhe brain to be challenged by acquiring new skills and taking up new hobbies. Adopt these tips to maintain your cognitive health. So that you can focus on your daily routine life.
Final Thoughts
Mapping specifically of the brain is a relatively new method used in treatment, diagnosis, and understanding of the mind. Irrespective of whether one is suffering from a diseased brain or in search of a healthy optimum brain, this technology offers key information. If you are in search of “Brain Mapping Las Vegas”, find a proper clinic. And boost your brain function and continue developing your brain management plan. Then don’t waste time and go for the best treatment.
0 notes
Text
Reclaiming Life: Innovative PTSD Treatment Options in Irvine
Post-Traumatic Stress Disorder (PTSD) is a complex mental health condition that can arise after experiencing or witnessing a traumatic event. Those affected often find themselves grappling with persistent symptoms such as flashbacks, severe anxiety, and uncontrollable thoughts about the event. In Irvine, innovative treatment options are emerging, particularly through the use of Ketamine therapy, which is gaining recognition for its effectiveness in addressing the challenges of PTSD. At the Renew Ketamine Infusion Clinic & Wellness Center, individuals seeking relief can explore a holistic approach to their well-being.

Understanding PTSD and Its Impact
PTSD can significantly disrupt the lives of those affected, leading to difficulties in relationships, work, and daily functioning. Traditional treatments often include cognitive-behavioral therapy (CBT) and pharmaceutical interventions, which, while effective for some, may not provide the desired relief for everyone..
PTSD treatment in Irvine that harness the power of Ketamine therapy. Research indicates that Ketamine, a medication initially developed for anesthesia, has unique properties that can act quickly to alleviate symptoms of depression and anxiety, making it a promising candidate for PTSD treatment.
The Role of Ketamine Therapy in Treating PTSD
Ketamine therapy offers a paradigm shift in how PTSD is approached. Unlike traditional antidepressants that may take weeks or months to show effects, Ketamine can provide rapid relief. Patients often report significant improvements in their symptoms within hours of treatment. The mechanism behind this is believed to involve the enhancement of synaptic connections in the brain, potentially rewiring the way traumatic memories are processed and stored.
The integration of Ketamine therapy with psychotherapy is a cornerstone of their approach. This combination allows for a comprehensive treatment plan that not only addresses the immediate symptoms but also supports long-term healing. The clinic’s licensed clinical psychotherapists, trained in Ketamine-assisted therapy, facilitate post-infusion integration sessions. These sessions provide a safe space for patients to explore their experiences, gain insights, and develop healthier coping mechanisms.
Creating a Safe and Supportive Environment
One of the defining features of the Renew Ketamine Infusion Clinic is its commitment to creating a tranquil and supportive environment. The clinic is designed to resemble a spa-like setting, promoting relaxation and comfort. This atmosphere is essential for patients undergoing Ketamine therapy, as it helps to reduce anxiety and enhance the overall therapeutic experience.
Patients are guided through every step of the process, beginning with a thorough evaluation to determine the most effective treatment regimen tailored to their unique needs. The physician who are board-certified and experienced in the use of Ketamine, emphasize the importance of individualized care. They understand that PTSD manifests differently in each person, and therefore, treatment plans must reflect this diversity.
Patient Experiences and Transformations
Numerous testimonials from patients highlight the transformative impact of Ketamine therapy on their lives. Many individuals describe a newfound sense of hope and relief from the burdens of PTSD symptoms. For instance, one patient expressed gratitude for the empathetic care provided by Dr. Yanuck and Dr. Dall, noting how their comprehensive approach made a significant difference in their healing journey.
These personal stories are a testament to the effectiveness of the innovative PTSD treatment in Irvine. Patients often report that the combination of Ketamine and psychotherapy not only alleviates their symptoms but also empowers them to confront their trauma in a more constructive way. This empowerment is crucial in reclaiming their lives and fostering resilience in the face of adversity.
The Importance of Community and Support
The team recognizes that healing from PTSD extends beyond individual treatment. The clinic fosters a sense of community among its patients, encouraging connections and support. This communal aspect is vital, as individuals often find solace in sharing their experiences with others who understand their struggles. The clinic's commitment to holistic healing encompasses not only the physical and psychological aspects but also the social dimensions of recovery.
Exploring Treatment Options
For those in Irvine seeking effective PTSD treatment in Irvine, exploring Ketamine therapy can be a pivotal step towards reclaiming their lives. The clinic offers free consultations to assess individual needs and discuss potential treatment plans. This initial step is crucial in determining whether Ketamine-assisted psychotherapy is the right fit for each patient.
The innovative approach to PTSD treatment not only addresses the immediate symptoms but also lays the groundwork for sustainable healing. Through individualized care, a supportive environment, and the integration of Ketamine therapy with psychotherapy, patients can embark on a transformative journey toward reclaiming their lives.
0 notes
Text
What is the Microbiome? Unravelling the Mysteries of Microbial Communities.
The realm of microbiome research, delving into the intricate assemblage of microorganisms inhabiting our bodies, stands at the forefront of contemporary biological inquiry. This field uncovers the significant roles these microbial consortia play in human physiology, pathologies, and environmental interactions. This exploration has identified several pivotal research domains, each presenting distinct insights and scientific challenges.
Deciphering Human Health and Pathologies
A central thrust of microbiome research is its implications for human health and disease. Investigators are examining the influence of microbial equilibrium in our bodies on various health aspects, including digestive, immune, and mental health. Empirical evidence suggests correlations between microbiome disturbances and a spectrum of conditions such as obesity, diabetes, inflammatory bowel diseases, and psychological disorders like depression. Unraveling these interconnections paves the way for novel therapeutic approaches and preventive strategies.
Dietary Influences on Microbial Diversity
Nutritional intake significantly shapes the microbiome's composition. This research strand explores the impact of various diets and nutrition patterns on microbial diversity and functionality. This area holds particular relevance in framing dietary guidelines and interventions for conditions influenced by the microbiome, including metabolic disorders. The advent of personalized nutrition, tailored to individual microbiome profiles, marks a groundbreaking development in this field.
Antibiotic Utilization and Microbial Resistance
The pervasive use of antibiotics carries profound consequences for the microbiome. Such medications can disrupt microbial balance, leading to antibiotic resistance and susceptibility to infections. Research in this domain is vital for understanding these effects and devising strategies to counter the adverse impacts of antibiotic application, such as developing selective treatments that conserve beneficial microbes.
Environmental Microbiome Dynamics
The microbiome's role transcends human health, significantly influencing environmental ecosystems. Investigations in this area encompass the study of microbiomes in various ecological settings, including soil and marine environments. These studies are integral to understanding ecological processes like nutrient cycling, biodegradation of pollutants, and the effects of climatic shifts on microbial populations. Insights gleaned here are pivotal for biodiversity conservation and sustainable agricultural practices.
The Gut-Brain Communication
The gut-brain axis, representing the bidirectional communication between the gut microbiome and the brain, emerges as an especially captivating research area. This domain is revealing how gut microbes affect neurological functioning and behavior, offering novel perspectives on neurodegenerative and psychiatric disorders. The potential for microbiome-centric therapies in treating conditions like Parkinson's disease, autism spectrum disorders, and depression is a prominent research focus.
Personalized Medicine and Microbiome-based Therapeutics
The role of the microbiome in individual drug responses and treatment efficacy represents another critical area of interest. Personalized medicine, adapted to one's microbiome profile, promises to revolutionize treatment paradigms across various diseases. This line of inquiry is fostering the development of innovative therapeutics, such as fecal microbiota transplants and probiotics, aimed at modulating the microbiome for therapeutic purposes.
Conclusion
The investigation into the microbiome is revealing an unseen world of microorganisms with profound impacts on health, disease, and environmental dynamics. Each research area provides a unique lens into the intricate interplays between microbes and their hosts, with implications extending far beyond current scientific understanding. As this field advances, the potential for novel treatments, enhanced health outcomes, and a deeper comprehension of our ecological integration is increasingly apparent. The journey into understanding the microbiome is only beginning, and its capacity to transform scientific and medical paradigms is vast. Contact Olive fertility for reproductive health clinic.
0 notes
Text
Harnessing the Power of Evidence-Based Practice
Transitioning from working with patients with strokes and amputations to patients with spinal cord injuries has been a significant shift for me as an OT student. Welcomed by two patients—one paraplegic, the other quadriplegic—I felt a mixture of anticipation and uncertainty swirling within me. In this journey of exploration, I found myself captivated by the potential of evidence-based practice to illuminate the path ahead. Through the lens of research, I sought to unravel the complexities of spinal cord injuries, eager to discover how words and phrases could guide me through this intriguing terrain of occupational therapy.
With regards to my quadriplegic patient in particular, I was overwhelmed by a wave of sadness and doubt. Questions raced through my mind, questioning my abilities and pondering the challenges that lay ahead. Yet, as I delved into research and explored evidence-based practices, a shift occurred within me. I realized that beneath the surface of uncertainty lay a profound opportunity for growth and learning. I realized how important it is to remain strong in challenging situations and how empathy and compassion have the power to bring about positive change. This experience disrupted my previous thoughts and beliefs, opening my eyes to the resilience and determination of individuals facing spinal cord injuries. It was a journey of self-discovery, revealing the depth of my capacity to make a difference in the lives of others, guided by evidence-based principles that illuminated the path forward. I realized the importance of addressing not only physical limitations but also emotional and psychological well-being because individuals with SCI may also face emotional challenges such as frustration, depression, anxiety, and grief. Losing the ability to perform daily tasks and being dependent on others can be emotionally draining (OT & Me, 2023). I made sure that my activities promote independence, a sense of accomplishment and enjoyment for the patient despite his physical limitations. I learned about the significance of tailoring leisure and recreational activities to the patient’s abilities and interests (Gorgey & Dudley, 2009), as the patient could not do any other ADLs or IADLS and spent most of his time in bed doing nothing. Most of my intervention sessions included engagement in leisure activities like playing cards, mlabalaba etc, which was one of my client’s interests.
Engaging in critical reflection on my experiences with this patient, I began to see the evolution of my professional identity as an OT student. I realized that true growth stems not only from knowledge acquisition but also from a willingness to challenge existing paradigms and embrace new perspectives grounded in evidence-based practice. This shift in mindset was evident in my approach to practice, as I began to integrate evidence-based principles into my interventions with greater confidence and efficacy. Each decision was informed by a thorough analysis of the latest research findings, demonstrating my commitment to delivering the highest quality of care informed by the best available evidence.
Throughout my interaction with my patient, I engaged in critical thinking by interpreting evidence, identifying alternative viewpoints, and justifying assumptions. Research findings informed my decision-making process, particularly regarding the importance of stretching and passive movements of the patient’s limbs to prevent further contractures (Physiopedia, 2022) which I implemented during my treatment sessions everytime either was part of the session or the warm up. My experience with him allowed me to bridge the gap between theory and practice. By applying theoretical concepts to real-life situations, I gained a deeper understanding of occupational therapy principles and their practical implications. Research also played a pivotal role in guiding my interventions and decision-making process with the quadriplegic patient. From developing leisure strategies like him playing certain games using his mouth to creating a wrist extension splint for his wrist drop instead of choosing the functional resting splint as it helps prevent contractures better and allows for more functional improvement (Jennifer Swann, 2022), evidence-based practices enabled me to provide effective care and support.
In the tapestry of occupational therapy, each patient we encounter weaves a unique story of resilience and possibility. My journey with this patient illuminated the power of research and the unwavering spirit of human determination. As I reflect on our shared path, I am reminded of the profound impact we can make through evidence-based practice. So, let us embrace each challenge as an opportunity for growth, knowing that with knowledge and compassion, we can create a brighter future for those we serve.
REFERENCES:
Me, I. O. and. (2023, April 7). Occupational Therapy for Spinal Cord Injury Rehabilitation. OT and Me. https://www.otandme.ca/post/occupational-therapy-for-spinal-cord-injury-rehabilitation
Gorgey, A. S., & Dudley, G. A. (2009). Skeletal muscle atrophy and increased intramuscular fat after incomplete spinal cord injury. Spinal Cord, 47(8), 628-633.
Fun Things to do with a Quadriplegic: 23 Activities to Try. (2021, January 12). Flint Rehab. https://www.flintrehab.com/fun-things-to-do-with-a-quadriplegic/
OTR/L, J. M. (2023, December 4). The Importance of Evidence-Based Practice in Occupational Therapy. Myotspot.com. https://www.myotspot.com/evidence-based-practice/#:~:text=More%20Effective%20Treatment%20Techniques
Burns, A. (n.d.). LibGuides: Occupational Therapy Program - Evidence-Based Practice Guide: Evidence-Based Practice. Cabarruscollege.libguides.com. https://cabarruscollege.libguides.com/c.php?g=527815&p=3608849
Hand Splints for Spinal Cord Injury: Different Types and Benefits. (2022, November 14). Flint Rehab. https://www.flintrehab.com/hand-splints-for-spinal-cord-injury/
0 notes
Text
Exploring the Foundations of Functional Medicine: A Holistic Approach to Health and Wellness
Introduction:
Functional Medicine has gained considerable attention in recent years as an innovative and holistic approach to healthcare. Unlike conventional medicine, which often focuses on treating symptoms, Functional Medicine delves deeper into the root causes of health issues. This paradigm shift in healthcare emphasizes personalized, patient-centred care, aiming to restore balance and promote optimal well-being. Find one of the best Functional Medicine Doctors in Oakland CA.
Understanding Functional Medicine:
Full-fledged Perspective: Functional Medicine views the body as an interconnected system, recognizing the intricate relationships between various physiological functions. Rather than isolating symptoms, practitioners seek to understand the underlying imbalances that contribute to health issues.
Patient-Centred Care: Central to Functional Medicine is a personalized approach to patient care. Practitioners spend time understanding a patient's unique health history, genetics, lifestyle, and environment. This complete assessment allows for targeted interventions customized to individual needs.
Root Cause Analysis: Functional Medicine goes beyond merely managing symptoms; it aims to identify and address the root causes of diseases. By addressing these underlying factors, practitioners aim to support the body's natural healing processes and restore balance.
Biochemical Individuality: Each person is biochemically unique, and Functional Medicine recognizes and respects this diversity. Treatment plans are customized based on the individual's specific biochemistry, ensuring a more precise and effective approach to health management.
Principles of Functional Medicine:
Promotion of Health as a Positive Vitality: Rather than merely treating disease, Functional Medicine seeks to enhance overall well-being and vitality. This proactive approach involves optimizing nutrition, physical activity, and lifestyle to prevent illness and promote longevity. Functional Medicine Doctor Berkeley CA brings your vitality to your sight.
Integration of Multiple Therapeutic Modalities: Functional Medicine integrates a wide range of therapeutic approaches, including nutrition, exercise, stress management, supplements, and medications when necessary. This complete toolkit allows practitioners to address health issues from various angles.
Patient Empowerment: Empowering patients to take an active role in their health is a key principle of Functional Medicine. Education and collaboration between practitioners and patients are emphasized, creating a sense of responsibility and self-awareness in managing one's health. Functional Medicine Doctors in Oakland CA treats you fast.
Applications of Functional Medicine:
Disease Management: Functional Medicine is particularly effective in managing conditions such as autoimmune diseases, diabetes issues. By addressing underlying imbalances, it aims to improve long-term health outcomes.
Optimizing Mental Health: Mental health issues, including anxiety and depression, are approached completely in Functional Medicine. Lifestyle modifications, nutritional support, and stress management techniques are integral components of treatment plans.
Preventive Healthcare: Functional Medicine places a strong emphasis on preventive care, helping individuals identify and address risk factors before they conclude as symptoms or diseases.
Conclusion:
Functional Medicine represents a drastic shift in healthcare, emphasizing a personalized, holistic, and patient-centred approach. By focusing on root causes and promoting overall well-being, it offers a promising solution for individuals seeking to optimize their health and vitality. As the field continues to evolve, Functional Medicine holds the potential to reshape how we approach and experience healthcare in the future. Functional Medicine Berkeley CA treats you at the earliest.
#Functional Medicine Doctor Near Me#Functional Medicine Oakland CA#Functional Medicine Doctors in Oakland CA#Functional Medicine Berkeley CA#Functional Medicine Doctor Berkeley CA
0 notes
Text
In the realm of mental health, the journey to finding the right professional can be daunting yet crucial. Whether one seeks assistance for neuro-psychiatric concerns or struggles with depression, the selection of the right specialist significantly impacts the quality of care and the path to recovery. In a city like Indore, where the demand for mental health services is rising, navigating through the myriad of options requires careful consideration and strategic employment of keywords. Here, we delve into the process of identifying the best neuro-psychiatrist in Indore and a competent counselor for depression.
When embarking on the quest for mental health support, employing specific keywords is paramount in refining search results. The phrase "best neuro-psychiatrist in Indore" serves as a beacon, guiding individuals towards professionals renowned for their expertise, experience, and efficacy in treating neurological and psychiatric disorders. This search query not only emphasizes the importance of specialization but also highlights the geographical relevance, ensuring proximity and accessibility to services.
In Indore, a burgeoning metropolis witnessing a surge in mental health awareness, the significance of keywords transcends mere online searches. It permeates through word-of-mouth recommendations, healthcare directories, and professional networks, shaping perceptions and influencing decisions. Consequently, the reputation associated with being the "best neuro-psychiatrist" becomes a coveted accolade, symbolizing trust, credibility, and competence within the community.
In tandem with the quest for a neuro-psychiatrist, the need for a counselor adept in addressing depression arises. Here, the keyword "counsellor for depression" becomes instrumental in narrowing down the search parameters, directing individuals towards professionals specialized in providing therapeutic interventions tailored to alleviate symptoms of depression. Unlike neuro-psychiatrists who primarily focus on medical interventions, counselors offer a holistic approach encompassing psychotherapy, behavioral interventions, and emotional support.
In Indore, where the prevalence of depression mirrors global trends, the demand for proficient counselors is escalating. Thus, the efficacy of keywords extends beyond mere identification to facilitate timely access to appropriate interventions, thereby fostering resilience and recovery among individuals grappling with mental health challenges.
Moreover, the synergy between neuro-psychiatrists and counselors underscores the multidisciplinary nature of mental health care. While neuro-psychiatrists diagnose and prescribe pharmacological interventions for neurological and psychiatric conditions, counselors complement the treatment paradigm by addressing psychosocial factors, facilitating coping strategies, and fostering emotional well-being.
In the pursuit of mental health support, leveraging keywords is not merely a passive endeavor but a strategic imperative. It involves meticulous research, discernment, and advocacy, empowering individuals to make informed decisions and embark on a transformative journey towards healing and restoration. As the discourse surrounding mental health continues to evolve in Indore and beyond, the efficacy of keywords transcends mere semantics, embodying a catalyst for change, resilience, and hope.
In conclusion, the quest for the best neuro-psychiatrist in Indore and a counsellor for depression necessitates the strategic utilization of keywords to navigate through the labyrinth of options. By employing phrases that underscore specialization and relevance, individuals can identify professionals renowned for their expertise and efficacy in addressing specific mental health concerns. Furthermore, the synergy between neuro-psychiatrists and counselors underscores the multidisciplinary nature of mental health care, highlighting the importance of holistic interventions in fostering resilience and recovery. In a landscape where mental health awareness is burgeoning, the efficacy of keywords extends beyond mere identification to become a catalyst for change, resilience, and hope.
Reference url on Finding the Best Neuro-Psychiatrist in Indore and a Counselor for Depression
0 notes