#Oral Health and Diabetes Complications
Explore tagged Tumblr posts
Text
Does Oral Health Affect Overall Health?

Oral health is an integral component of overall health, and the connection between the two has been the subject of extensive research and discussion. Historically, dentistry and medicine were considered separate fields, each addressing distinct aspects of health. However, contemporary research has uncovered a significant interrelation between oral health and overall health, with evidence demonstrating that the condition of the mouth can have profound effects on the entire body. This article explores the answer to the question “Does oral health affect overall health” and the relationship between oral health and overall health.
Read the Complete Article: https://www.liferxpharmacy.com/blog/does-oral-health-affect-overall-health/
#Oral Health#Overall Health#Oral health important#Mouth-Body Connection#Diabetes and Oral Health#Diabetes and Gum Disease#Oral Health and Diabetes Complications#Cardiovascular Health#Respiratory Health#Mental Health and Well-being#Pregnancy and Oral Health#Aging and Oral Health#Lifestyle and Oral Health#better oral health
0 notes
Text

10 Complications of Diabetes Mellitus
Diabetes is a metabolic disorder, caused by the body’s inability to use the insulin produced by its own pancreas or insufficient insulin production. As glucose begins to accumulate in the bloodstream, it begins to damage the blood vessels in organs large and small across the body.
Read more how to Reduce Complication of Diabetes: https://www.freedomfromdiabetes.org/blog/post/10-complications-of-diabetes-mellitus/2713
#10 Complications of Diabetes Mellitus#Diabetes and Alzheimer's Disease#Diabetic Nephropathy#Diabetes and Cardiovascular Disease#Diabetic Retinopathy#Diabetic Neuropathy#Diabetes and Oral Health#Diabetes in Pregnancy#Diabetes and infertility#Diabetes and Hypertension#Obesity and Diabetes#complications of diabetes mellitus#chronic complications of diabetes mellitus#long term complications of diabetes
0 notes
Text
"Premium Probiotics For Premium Vibrant Teeth and Gums"
(Hint - No Toothpaste or Mouthwash Involved)
Elevate your dental game with our PRO DENTIM

1. Introduction to Dental Probiotics
Oral health is often confined to brushing, flossing, and routine dental visits. However, the advent of probiotics tailored for dental health heralds a new era in oral care. These innovative products promise to support and enhance the health of your teeth and gums through the power of beneficial bacteria.
2. The Importance of Oral Health
✮ Connection Between Oral Health and Overall Health
The mouth is a gateway to the body, and its health is intrinsically linked to overall well-being. Poor oral hygiene can lead to systemic issues such as heart disease, diabetes, and respiratory infections. Thus, maintaining a healthy oral environment is crucial.
✮ Common Dental Problems
Common dental issues include cavities, gum disease, and bad breath. These problems can cause discomfort, impact self-esteem, and lead to more serious health complications if left untreated.
3. What Are Probiotics?
✮ Definition and Benefits
Probiotics are live microorganisms that confer health benefits when consumed in adequate amounts. They are often associated with digestive health but have far-reaching effects on various bodily systems.
✮ How Probiotics Work
Probiotics work by balancing the microbiota in the body. They outcompete harmful bacteria, reduce inflammation, and enhance the body's natural defenses.

Elevate your dental game with our PRO DENTIM
4. Probiotics and Oral Health
✮ Mechanisms of Action in the Mouth
In the oral cavity, probiotics adhere to the surfaces of teeth and gums, creating a protective barrier. They produce substances that inhibit the growth of pathogenic bacteria and modulate the immune response.

✮ Research Supporting Oral Probiotics
Emerging research indicates that probiotics can reduce plaque, prevent gingivitis, and diminish bad breath. Studies have shown that specific strains of probiotics are effective in maintaining oral health.

5. Brand New Probiotics for Teeth and Gums
✮ Introduction to the Latest Products
The latest probiotics for dental health are designed to be integrated seamlessly into daily routines. These products come in various forms, including lozenges, mouthwashes, and toothpaste.
✮ Key Ingredients and Their Benefits
These cutting-edge probiotics contain strains like Lactobacillus reuteri, Streptococcus salivarius, and Bifidobacterium lactis. Each strain has unique properties that support the health of teeth and gums by reducing harmful bacteria and promoting a balanced oral microbiome.
6. How to Use Dental Probiotics
✮ Daily Routine for Optimal Results
For best results, dental probiotics should be used consistently. Incorporate them into your morning and evening routines, just as you would with brushing and flossing.
✮ Dosage and Administration
Follow the manufacturer’s guidelines for dosage. Typically, one lozenge or a specified amount of mouthwash per day is sufficient to reap the benefits of dental probiotics.
7. Benefits of Dental Probiotics
✮ Prevention of Dental Issues
Regular use of dental probiotics can prevent common dental problems such as cavities and gum disease by maintaining a healthy balance of bacteria in the mouth.
✮ Improvement in Gum Health
Dental probiotics help reduce inflammation and bleeding in the gums, leading to improved gum health and a lower risk of periodontal disease.
✮ Enhanced Oral Hygiene
Probiotics contribute to fresher breath and cleaner teeth, enhancing overall oral hygiene. They can be a valuable addition to traditional dental care practices.

8. Potential Side Effects and Considerations
✮ Possible Adverse Reactions
While probiotics are generally safe, some individuals may experience mild side effects such as digestive discomfort. These effects are usually temporary.
✮ Who Should Avoid Dental Probiotics?
Individuals with compromised immune systems or those undergoing certain medical treatments should consult a healthcare professional before using dental probiotics.

9. Integrating Probiotics with Traditional Dental Care
✮ Combining Probiotics with Regular Oral Hygiene Practices
Probiotics should complement, not replace, regular oral hygiene practices. Continue to brush, floss, and visit your dentist regularly while using probiotics to maximize oral health benefits.
✮ Consultation with Dental Professionals
Before starting any new oral health regimen, including probiotics, consult with your dentist. They can provide personalized advice and ensure that probiotics are appropriate for your specific needs.
10. Conclusion
The introduction of probiotics specially designed for dental health represents a significant advancement in oral care. These innovative products offer a promising solution for enhancing the health of your teeth and gums. By incorporating dental probiotics into your routine, you can achieve a healthier, more balanced oral environment and enjoy the benefits of improved oral hygiene and overall well-being.

Elevate your dental game with our PRO DENTIM
DISCLAIMER:
This is an amazing affiliate product do check it out for best possible dental care, Thankyou!!
#supplements#dental health#dental care#teeth whitening#gum health#mouth freshner#health and wellness#health & fitness
3 notes
·
View notes
Text

Credit: Dana Smith
Understanding The Sudden Rise of Type 2 Diabetes In Children
The Metabolic Disorder Was Long Known as a Disease of Adulthood. Now, It’s Spiking in Kids and Teens, With Worrisome Consequences.
— By Charlotte Huff | July 31, 2024
The appearance of type 2 diabetes in children and teens puzzled physicians from the start. Fida Bacha recalls working as a pediatric endocrinology fellow in Pittsburgh shortly after 2000 when young, overweight and obese patients began to arrive at the clinic, some describing increased thirst, more frequent trips to the bathroom and other symptoms of what was then called adult-onset diabetes.
“It was a new realization that we are dealing with a disease that used to be only an adult disease that is now becoming a disease of childhood,” says Bacha, who practices at Texas Children’s Hospital in Houston.
More than two decades later, physicians and researchers are still trying to unravel what’s driving the emergence and proliferation of youth-onset disease, particularly among marginalized communities including Hispanics/Latinos. The increasing prevalence of obesity among young people is clearly one contributor, but researchers are also scrutinizing the potential influence of other lifestyle and environmental factors — everything from exposure to chronic stress and air pollution to sugar-rich diets. Along with physiological factors, such as where they carry excess fat, youths from lower socioeconomic levels may be vulnerable due to aspects of daily life beyond their control, such as more limited access to healthy food and opportunities to safely exercise in less-polluted neighborhoods.
As researchers try to sort out the interplay among genetics, metabolic factors and environmental influences in Hispanic and other populations, their goal is to answer this key question: Why do some seemingly at-risk adolescents progress to diabetes while others do not?
Long-term, the challenges and health stakes are significant. When type 2 diabetes first emerged in youths, clinicians initially thought its progression would mirror that in adults and thus could be treated accordingly. That hasn’t panned out, says Barbara Linder, a pediatric endocrinologist and senior advisor for childhood diabetes research at the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). For instance, researchers have determined that metformin, a commonly prescribed oral antidiabetic medication in adults, doesn’t work as well in young people.
“We know that the disease is very aggressive in youth and very difficult to treat,” Linder says. “So it’s really imperative that we develop effective approaches to prevention. And to do this we obviously need to be able to effectively identify which youth are at the highest risk.”
Even with treatment, young people develop other medical problems related to diabetes faster than adults, according to a study that followed 500 youths, more than one-third of them Hispanic. Sixty percent developed at least one complication within about 15 years after diagnosis, when just in their 20s.
“It’s really alarming,” says Luisa Rodriguez, a pediatric endocrinologist who studies type 2 diabetes and obesity in children at the University of Texas Health Science Center at San Antonio. For every 10 adolescents with youth-onset diabetes, she points out, “six of them, within a decade span, are going to develop a significant comorbidity that will highly impact their lifespan and quality of life.”

Complications of diabetes appear more quickly in young people than in older adults. Researchers studied 500 overweight adolescents, aged 10 to 17, who had been diagnosed with type 2 diabetes. Within 15 years of their diagnosis, 60 percent of the participants had developed at least one medical complication of diabetes, and 28 percent had developed two or more.
Insulin Resistance
In type 2 diabetes, the body struggles to use insulin effectively. This vital hormone, made by beta cells in the pancreas, helps glucose in the bloodstream enter cells in muscle, fat and the liver, where it’s used for energy. But sometimes those cells gradually lose their ability to respond to insulin, forcing the beta cells to pump out more and more of it. If the beta cells can’t keep up, blood glucose levels will begin to rise, leading to a diagnosis of prediabetes and, eventually, diabetes.
In the past, type 2 diabetes typically didn’t arise until well into adulthood. But now, cases in US youths ages 10 to 19 are rising fast. Since 2002-2003, overall diagnoses have doubled from 9 per 100,000 youths to 17.9 per 100,000 in 2017-2018, particularly among Asians, Pacific Islanders, Blacks and Hispanics. If those rising rates persist, the number of type 2 diabetes cases in young people is projected to skyrocket from 28,000 in 2017 to 220,000 by 2060.
Various factors have been linked to insulin resistance in childhood or adolescence, including obesity, inactivity and genetics, according to a review of the causes of type 2 diabetes in youths published in the 2022 Annual Review of Medicine. The disease tends to run in families regardless of race or ethnicity, which suggests that genes matter. Among US Hispanics, adults of Mexican or Puerto Rican heritage are most likely to be diagnosed, followed by Central and South Americans and Cubans.
Obesity is also a contributing factor: Slightly more than one-fourth of Hispanic youths are obese, a higher percentage than for any other major racial or ethnic group. Children also are more likely to develop type 2 diabetes if their mother has the disease or developed gestational diabetes during pregnancy. One theory is that fetal exposure to maternal diabetes while in the womb can spur metabolic changes following birth.
Puberty is also highly influential — most cases are diagnosed after its onset. During puberty, youths temporarily experience insulin resistance, due in large part to an increase in hormones, Linder says. Most youths offset that transient resistance by secreting more insulin, she says. But for reasons that are still unclear, a subpopulation of adolescents does not. “When they’re faced with this stress test of puberty, they can’t increase their insulin secretion enough to compensate,” Linder says. “And that’s probably why they develop type 2 diabetes.”
One analysis, which looked at type 2 diabetes trends from 2002 to 2018, identified the peak age for diagnosis as 16 years in boys and girls. The sole exception involved Black youths, in whom diagnoses peaked at 13 years, and possibly earlier among Black girls, which may be linked to an earlier start of menstruation.
American Diabetes Association guidelines recommend that clinicians screen overweight or obese youths for the disease starting at age 10 or once puberty starts, whichever is earlier, if they have one or more risk factors. These include a family history of the disease, signs of insulin resistance or affiliation with certain racial/ethnic groups, including Hispanic/Latino.
During checkups, clinicians can look for a visible sign of insulin resistance, an associated skin condition called acanthosis nigricans, says Paulina Cruz Bravo, a physician and diabetes researcher at Washington University School of Medicine in St. Louis. The skin changes tend to appear in the neck area or along folds in the skin, including in the armpits and on the elbows and knees, she says. “The top layer of the skin gets thickened. It’s described as a velvety appearance of the skin — it’s darker compared to the skin in other places.”

The thickened, darker, velvety skin shown here, known as acanthosis nigricans, is a potential warning sign of developing type 2 diabetes. The condition is likely to appear on the neck, elbows, knees and other areas where the skin folds. People who notice acanthosis nigricans on themselves or their children should bring it to a doctor’s attention. Credit: S. Dulebohn/Statpearls 2024
Where an adolescent carries any excess pounds also matters, as insulin resistance has been associated with a type of fat called visceral fat, says Alaina Vidmar, a pediatric endocrinologist at Children’s Hospital Los Angeles. Unlike the more common type of fat, called subcutaneous and felt by pinching around the waistline, visceral fat surrounds the liver and other vital organs, increasing the risk for type 2 diabetes, fatty liver disease and other conditions.
“You really need the liver to process glucose to be able to utilize your insulin well,” Vidmar says. “And if it is full of fat, you are unable to do that.” Fatty liver disease, which has been associated both with obesity and type 2 diabetes, is most common in Hispanic adults, followed by white adults and Black adults, according to a meta-analysis looking at 34 studies.
Imaging scans would be the ideal way to identify the extent and location of visceral fat in adolescents, Vidmar says. But given that routine scanning would be costly, clinicians can instead measure an adolescent’s waist circumference, “a great surrogate marker,” she says.

Diabetes risk depends not just on how much fat you carry, but where you carry it. People with an “apple” body shape, with much of their fat in the abdomen, are at higher risk of diabetes than those with a “pear” body shape, who carry their fat under the skin, especially on the hips.
Still, obesity accounts for only a portion of the type 2 risk profile, reflecting the complexities involved in understanding the pathophysiology of youth-onset disease. Roughly one-fourth of youths with type 2 diabetes are not obese, according to a meta-analysis published in 2022 in JAMA Network Open. Asian youths are least likely to be obese; roughly one-third don’t meet the criteria for obesity.
Moreover, while obesity and insulin resistance boost the risk of developing diabetes, those factors alone don’t predict whether an adolescent is eventually diagnosed with the disease, according to the authors of the Annual Review of Medicine overview. Instead, they point to the role of impaired beta cell function.
In one study involving 699 youths with type 2 diabetes, the standard antidiabetic drug metformin controlled blood glucose levels in only about half the participants. (The medication was least effective among Black youths, for reasons that are unclear, according to the researchers.) Another analysis of the same study population identified a 20 percent to 35 percent decline in beta function each year in diabetic youths, compared with prior studies showing about a 7 percent to 11 percent annual decline in diabetic adults.
“What we see in the youth is that beta cell function fails very rapidly,” Linder says, adding that the beta cell decline tends to correlate with the lack of response to metformin.
It’s unknown whether specific racial or ethnic groups are more vulnerable to loss of beta cell function, says Linder, who hopes that a new large-scale NIDDK study launching this summer will identify any such physiological and other differences among populations. The study, called Discovery of Risk Factors for Type 2 Diabetes in Youth Consortium, aims to enroll 3,600 overweight or obese adolescent boys and girls, 36 percent of them Hispanic. Bacha and other investigators on the project plan to follow the youths through puberty, looking at genetic and physiological markers such as insulin resistance and beta cell function. Their goal is to track who develops type 2 diabetes and what factors precipitate the disease.
In addition, researchers will learn about the participants’ mental health, lifestyles and social determinants of health, Linder says. To that end, families will be asked to share details about nutrition, physical activity and sleep, as well as food insecurity, exposure to racism and other stressors.
“Stress induces certain hormones that antagonize insulin, so they create more insulin resistance,” Linder says. “Stress also is associated with chronic inflammation in the body, which affects the ability of the body to respond normally.”

Young people experience many of the risk factors that predispose people to type 2 diabetes, such as prenatal exposures, junk food, sedentary lifestyles and high levels of stress.
Zooming in on Risk Factors in Hispanic Kids
Already, researchers who have studied at-risk Hispanic youths and their families have begun to flesh out environmental and other influences rooted in daily life that can boost the likelihood of obesity or diabetes. Michael Goran, a child obesity researcher at Children’s Hospital Los Angeles, has led a research project called the Study of Latino Adolescents at Risk (SOLAR), which tracked 328 Hispanic/Latino youths considered at highest risk of youth-onset diabetes based on their body mass index and family history of the disease. The participants, recruited in two waves between 2000 and 2015, completed health questionnaires and underwent annual exams, including imaging scans and other measurements.
One analysis found that Hispanic youths who lived in neighborhoods with higher levels of air pollution were more likely to experience a breakdown in beta cell function. “Which we weren’t necessarily expecting — we don’t know the mechanism of that,” says Goran, who coauthored a close look at pediatric insulin resistance in the 2005 Annual Review of Nutrition.
In more recent years, he’s turned his attention to studying nutrition shortly after birth, with a focus on infant formulas that contain corn syrup. Those formulas are more likely to spike blood sugar than are lactose-based formulas, he says. “If you’re spiking blood glucose with corn syrup in babies,” he says, “you can see how that would be problematic for long-term control of blood sugars.”
In one study, Goran and colleagues looked at obesity trends in 15,246 children who received formula through the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). Babies who consumed any formula with corn syrup were 10 percent more likely to be obese by age 2 than babies who didn’t. Nearly 90 percent of the study’s participants were Hispanic.
In other research, epidemiologist Carmen Isasi of the Albert Einstein College of Medicine in New York helped lead the Study of Latinos (SOL) Youth study, which delved into the extent to which a child’s family circumstances contribute to obesity and metabolic changes that may boost risk of youth-onset diabetes. Isasi and colleagues found chronic stress to be pervasive. Three-quarters of parents and caregivers reported stress and 29 percent detailed three or more stressors related to health, work or relationships. The higher the number of parental stressors, the more likely the child was to be obese.
Isasi also has looked at the relationship between food insecurity and metabolic health. Hispanic youths raised in households with the highest levels of food insecurity had significantly worse metabolic results, including elevated blood glucose and triglycerides, a type of cholesterol. Families dealing with food insecurity, Isasi says, probably have a lower-quality diet and skimp on costlier protein and fresh produce.
Preventing diabetes has proved challenging. A review paper looking at diet-related and other lifestyle initiatives targeting Hispanic youths found few studies to date that have shown improvements in body mass index or blood glucose levels.
Adolescents of lower socioeconomic status may also shoulder responsibilities that can undercut efforts to stay healthy, says Erica Soltero, a behavioral scientist at Houston’s Baylor College of Medicine, who works with Hispanic youths. For instance, older teens may struggle to attend an exercise class if they have an after-school job or must pick up younger siblings or start dinner. Technology, Soltero says, may be a better way to reach busy Hispanic teens; she’s piloting a study that will provide text-based lifestyle guidance to Hispanic teens with obesity.
Approved medication options remain limited for children and teens. If metformin doesn’t work, the alternative is insulin, and parents may resist giving injections because of the difficulties involved, Rodriguez says. She’s involved with an ongoing study in youths with type 2 diabetes to study the effectiveness of oral semaglutide, one of the newer diabetes drugs that also has achieved notable weight loss. Rodriguez estimates the results will be available by 2026.
The new NIDDK study won’t assess medication treatments, as it’s an observational study. But researchers involved are bullish that study-related insights could lead to better prevention and treatment approaches. “If someone is predisposed to beta cell dysfunction, should we be much more aggressive in treating their overweight/obesity,” Bacha says, “so that this beta cell function is preserved for a longer period of time?” Doctors could, for example, decide to start treatment earlier, she says.
Neither are researchers like Soltero deterred by the long-standing difficulties involved with revamping lifestyle habits. Soltero, who has worked with overweight and obese Hispanic adolescents to improve exercise and make dietary changes, describes them as often highly motivated given the damage they’ve seen the disease inflict on their own families.
“A lot of times they’ll have a touch point with a relative who’s on dialysis and maybe had a digit amputated,” Soltero says. Or “they’ll say, ‘I don’t want to prick myself every day like my Uncle So-and-So.’ Or ‘I don’t want to be on medicine for the rest of my life like my grandma.’ ”
#Knowable Magazine#Diabetes#Type-2 Diabetes#Charlotte Huff#Children#Metabolic Disorder#Disease of Adulthood#Spikining Diabetes | Kids | Teens#Epedemiology#Food | Environment#Health & Disease#Nutrition#Public Health#Society
2 notes
·
View notes
Text
Important Facts About Gum Disease
Gum disease, also known as periodontal disease, is a common oral health condition that affects the gums and supporting structures of the teeth. Here are some important facts about gum disease:

Prevalence: Gum disease is widespread, with a significant portion of the population affected to varying degrees.
Causes: Poor oral hygiene, plaque buildup, smoking, hormonal changes, certain medications, and genetic factors can contribute to gum disease.
Stages: Gum disease progresses through stages, starting with gingivitis (inflammation of the gums) and advancing to periodontitis (infection and damage to the bone and tissues supporting the teeth).
Symptoms: Red, swollen, and bleeding gums, persistent bad breath, receding gumline, loose teeth, and changes in a bite are common signs of gum disease.
Complications: If left untreated, gum disease can lead to tooth loss, bone damage, and systemic health issues like heart disease and diabetes.
Prevention: Regular brushing, flossing, and professional dental cleanings are essential for preventing gum disease.
Treatment: Treatment options include deep cleaning procedures, medication, surgery, and lifestyle changes to manage the condition and restore gum health.
Early detection and prompt treatment are crucial for preventing the progression of gum disease and maintaining optimal oral health. Regular dental check-ups are important for monitoring and addressing any signs of gum disease.
Oral health is essential to overall health maintenance. Let Maple Dental, a trusted dentistry in Hesperia, help you achieve your best smile yet!
#dentist hesperia#childrens dentist in hesperia ca#emergency dentist#dentistry#professional dentist#hesperia dentist#desert dental hesperia
20 notes
·
View notes
Text
The Detrimental Health Effects of Smoking: A Comprehensive Overview
Smoking remains one of the most pressing public health issues globally. Despite widespread awareness campaigns, millions continue to smoke, often underestimating the severe health consequences. This article delves into the various smoking health issues, highlighting the extensive damage smoking inflicts on the body and emphasizing the importance of quitting.
The Respiratory System: A Primary Target
One of the most immediate and severe smoking health issues is its impact on the respiratory system. Smoking damages the airways and the alveoli, leading to chronic respiratory conditions such as:
Chronic Obstructive Pulmonary Disease (COPD): This progressive disease makes it increasingly difficult to breathe, significantly reducing the quality of life.
Chronic Bronchitis: Characterized by a persistent cough and mucus production, chronic bronchitis results from inflamed bronchial tubes.
Emphysema: This condition involves the destruction of the air sacs in the lungs, leading to severe shortness of breath.
Cardiovascular Complications
Smoking is a major contributor to cardiovascular diseases, which are among the leading causes of death worldwide. Key smoking health issues related to the cardiovascular system include:
Heart Disease: Smoking damages the lining of the arteries, leading to atherosclerosis—a condition where arteries harden and narrow. This can result in heart attacks and strokes.
High Blood Pressure: The chemicals in tobacco smoke can elevate blood pressure, increasing the risk of heart disease.
Peripheral Artery Disease (PAD): Smoking causes the narrowing of blood vessels outside the heart, particularly in the legs, leading to pain and mobility issues.
Cancer: A Grim Reality
The link between smoking and cancer is well-established. Smoking is a leading cause of various cancers, including:
Lung Cancer: The most well-known smoking health issue, lung cancer, is predominantly caused by smoking. It remains one of the deadliest cancers worldwide.
Mouth, Throat, and Esophagus Cancer: Smoking affects nearly every part of the respiratory and digestive tracts, significantly increasing the risk of cancers in these areas.
Bladder Cancer: Harmful chemicals from tobacco are filtered by the kidneys and stored in the bladder, where they can cause cancer.
Impact on Reproductive Health
Smoking health issues extend to reproductive health, affecting both men and women:
Fertility Problems: Smoking can reduce fertility in both genders. In women, it can damage the ovaries and reduce egg production. In men, smoking can affect sperm quality.
Pregnancy Complications: Pregnant women who smoke are at a higher risk of miscarriage, premature birth, and having babies with low birth weight. Smoking also increases the risk of sudden infant death syndrome (SIDS).
Other Health Issues
Smoking is linked to a host of other health problems, including:
Type 2 Diabetes: Smokers are more likely to develop type 2 diabetes, and the condition is harder to control in smokers.
Weakened Immune System: Smoking weakens the immune system, making it harder to fight off infections.
Poor Oral Health: Smoking causes bad breath, gum disease, and tooth loss. It can also affect the sense of taste and smell.
Conclusion: The Urgent Need to Quit
The myriad smoking health issues underscore the urgent need for smokers to quit. Quitting smoking can dramatically improve overall health and reduce the risk of developing many severe diseases. While quitting can be challenging, numerous resources are available to support those who want to stop. Nicotine replacement therapies, prescription medications, counseling, and support groups can all play a role in helping individuals quit smoking for good.
In conclusion, the detrimental health effects of smoking cannot be overstated. By understanding the extensive damage smoking causes and taking steps to quit, individuals can significantly improve their health and quality of life.
2 notes
·
View notes
Text
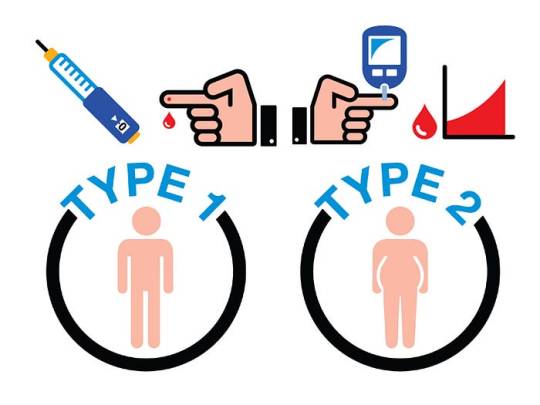
Understanding Different Types of Diabetes and Their Impact on the Body

Diabetes is a chronic condition that affects millions of people worldwide. It disrupts the body's ability to regulate blood sugar (glucose) levels, leading to serious health complications if not managed properly. There are several types of diabetes, each with unique characteristics and impacts on the body. This article will explore the different types of diabetes, how they affect the body, and the tests provided by RML Pathology to diagnose and manage this condition.
1. Type 1 Diabetes
Description:
Type 1 diabetes is an autoimmune disease where the immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. This results in little to no insulin production, which is essential for regulating blood sugar levels.
Impact on the Body:
Requires lifelong insulin therapy.
Increases the risk of complications such as diabetic ketoacidosis (DKA), a potentially life-threatening condition.
Long-term complications include cardiovascular disease, kidney damage (nephropathy), nerve damage (neuropathy), and vision problems (retinopathy).
Can cause frequent urination, excessive thirst, extreme hunger, weight loss, fatigue, and irritability.
2. Type 2 Diabetes
Description:
Type 2 diabetes is the most common form of diabetes. It occurs when the body becomes resistant to insulin or when the pancreas does not produce enough insulin. Lifestyle factors such as obesity, poor diet, and lack of exercise significantly contribute to its development.
Impact on the Body:
Often managed with lifestyle changes, oral medications, and sometimes insulin.
Can lead to complications like heart disease, stroke, kidney disease, eye problems, and nerve damage.
Symptoms include increased thirst, frequent urination, increased hunger, fatigue, blurred vision, slow-healing sores, and frequent infections.
3. Gestational Diabetes
Description:
Gestational diabetes occurs during pregnancy when the body cannot produce enough insulin to meet the increased needs. It usually resolves after childbirth but increases the risk of developing type 2 diabetes later in life.
Impact on the Body:
Can cause high blood pressure during pregnancy (preeclampsia).
Increases the risk of having a large baby, leading to complications during delivery.
May result in low blood sugar levels in the newborn and a higher risk of obesity and type 2 diabetes in the child later in life.
4. Prediabetes
Description:
Prediabetes is a condition where blood sugar levels are higher than normal but not high enough to be classified as type 2 diabetes. It is a critical stage for intervention to prevent the progression to type 2 diabetes.
Impact on the Body:
Often reversible with lifestyle changes such as diet and exercise.
Increases the risk of developing type 2 diabetes, heart disease, and stroke.
Symptoms are often absent or mild, making regular screening important.
Tests Provided by RML Pathology
RML Pathology offers a comprehensive range of tests to diagnose and manage diabetes effectively. These include:
Fasting Blood Glucose Test:
Measures blood sugar levels after fasting for at least 8 hours.
Helps diagnose diabetes and prediabetes.
HbA1c Test:
Provides an average blood sugar level over the past 2-3 months.
Used to diagnose diabetes and monitor long-term glucose control.
Oral Glucose Tolerance Test (OGTT):
Measures the body's response to a glucose solution.
Commonly used to diagnose gestational diabetes.
Random Blood Sugar Test:
Measures blood sugar levels at any time of the day.
Useful for diagnosing diabetes when symptoms are present.
Gestational Diabetes Test:
Specifically designed for pregnant women to detect gestational diabetes.
Conclusion
Understanding the different types of diabetes and their impact on the body is crucial for effective management and prevention. Regular testing and early detection play a vital role in managing diabetes and preventing complications. RML Pathology provides a wide range of diagnostic tests to help you monitor and manage your diabetes effectively. If you have any symptoms or risk factors for diabetes, consider visiting RML Pathology for a comprehensive evaluation.
Contact RML Pathology Today:
📞 7991602001, 7991602002 📞 0522-4034100 🌐 www.rmlpathology.com
Experience the best in diagnostics with RML Pathology – where your health is our priority.
#diabetes#type 1 diabetes#type 2 diabetes#gestational diabetes#prediabetes#diabetes management#blood sugar#glucose levels#RML Pathology#diabetes tests#HbA1c#fasting blood glucose#oral glucose tolerance test#random blood sugar test#health#healthcare#diabetes diagnosis
3 notes
·
View notes
Text
Diabetes

Introduction to Diabetes
Diabetes, a metabolic disorder characterized by chronic hyperglycemia, arises from abnormalities in insulin secretion, insulin action, or both. The condition’s prevalence has reached epidemic proportions globally, with significant health, economic, and social implications.
Types of Diabetes
Type 1 Diabetes: This autoimmune disease results from the destruction of pancreatic beta cells, leading to absolute insulin deficiency. Genetics and environmental triggers play pivotal roles in its pathogenesis. Despite being less common than Type 2 diabetes, its onset during childhood or adolescence significantly impacts individuals’ lives.
Type 2 Diabetes: Predominantly a disorder of insulin resistance, Type 2 diabetes accounts for the majority of diabetes cases worldwide. Lifestyle factors, genetic predisposition, and obesity contribute to its development. Its insidious onset often leads to delayed diagnosis and increased risk of complications.
Gestational Diabetes: Occurring during pregnancy, gestational diabetes poses risks to both maternal and fetal health. Hormonal changes and insulin resistance characterize its pathophysiology. Effective screening and management are crucial to prevent adverse outcomes.
Other Types of Diabetes: Variants like MODY, LADA, and secondary diabetes present unique challenges in diagnosis and management, requiring tailored approaches to care.
Epidemiology and Prevalence
Diabetes prevalence varies across demographics, with disparities observed in age, gender, ethnicity, and socioeconomic status. The escalating burden of diabetes underscores the urgent need for targeted prevention and management strategies.
Symptoms and Causes

Hyperglycemia-induced symptoms like polyuria, polydipsia, and unexplained weight loss serve as clinical indicators for diabetes diagnosis. Understanding the complex interplay of genetic, environmental, and lifestyle factors elucidates the condition’s etiology.
Complications
Diabetes complications encompass a spectrum of microvascular and macrovascular disorders, significantly impacting quality of life and life expectancy. From diabetic retinopathy to cardiovascular disease, nephropathy, neuropathy, and diabetic foot complications, the ripple effects of uncontrolled diabetes are profound.
Diagnosis and Tests

Accurate diagnosis relies on comprehensive evaluation, including fasting glucose, oral glucose tolerance tests, and hemoglobin A1c measurements. Screening recommendations aim to identify at-risk individuals early, facilitating timely intervention and risk reduction.
Management and Treatment
Diabetes management strategies encompass pharmacotherapy, lifestyle modifications, patient education, and multidisciplinary care. Individualized treatment plans address glycemic control, blood pressure management, lipid optimization, and prevention of complications.
Prevention
Prevention initiatives target modifiable risk factors through health promotion, public health interventions, and community engagement. Emphasizing the role of nutrition, physical activity, and behavioral changes empowers individuals to mitigate their diabetes risk.
Outlook and Prognosis
Prognostic factors such as glycemic control, adherence to therapy, comorbidity burden, and psychosocial support influence long-term outcomes. Enhanced collaboration among healthcare providers, policymakers, and stakeholders is essential to improve diabetes prognosis globally.
Living With Diabetes

Coping with diabetes requires resilience, self-management skills, and social support networks. Empowering individuals through education, self-monitoring tools, and peer support enhances their capacity to navigate the challenges of daily diabetes management.
Impact on Individuals and Society
Diabetes exerts a profound socioeconomic burden, encompassing healthcare costs, productivity losses, and reduced quality of life. Addressing the psychosocial dimensions of diabetes care is integral to fostering holistic well-being and societal resilience.
Future Directions and Research

Advancements in diabetes research, including precision medicine, digital health technologies, and novel therapeutics, offer promising avenues for disease management and prevention. Collaborative research endeavors aim to translate scientific discoveries into tangible clinical benefits.
Conclusion
In conclusion, diabetes represents public health challenge necessitating a comprehensive, patient-centered approach. By fostering awareness, promoting early detection, and advancing evidence-based interventions, we can mitigate the impact of diabetes on individuals, families, and communities worldwide.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at [email protected] for assistance.
#assignment help#healthcare#medical students#nursing student#nursing school#medical school#medical student#medicine#health tips#health and wellness#health#health & fitness#diabetes#diabetic#medical help#medical assistance#pharmacy student#pharmacy technician#homework help#academic assignments#expert assignment writers
2 notes
·
View notes
Text
Curing Diabetes Permanently
Curing Diabetes Permanently: Is It Possible?
Diabetes is a chronic disease that affects millions of people worldwide. It is characterized by high levels of sugar in the blood, which can lead to serious health complications if left untreated. While there are various treatments available to manage diabetes, many people wonder if it is possible to cure it permanently. In this article, we will explore this question and provide some insights into the potential for a permanent cure for diabetes.
Understanding Diabetes
Before we dive into the possibility of a permanent cure, it is important to understand what diabetes is and how it affects the body. There are two main types of diabetes: type 1 and type 2. Type 1 diabetes is an autoimmune disease where the body's immune system attacks and destroys the cells in the pancreas that produce insulin. Insulin is a hormone that helps regulate blood sugar levels. Type 2 diabetes, on the other hand, is a metabolic disorder where the body becomes resistant to insulin or does not produce enough of it. Both types of diabetes can lead to high blood sugar levels, which can cause damage to organs and tissues over time.
Current Treatments for Diabetes
Currently, there is no known cure for diabetes. However, there are various treatments available to manage the disease and keep blood sugar levels under control. These treatments include insulin injections, oral medications, and lifestyle changes such as diet and exercise. While these treatments can help manage diabetes, they do not provide a permanent cure.
Research on a Permanent Cure

Over the years, there have been numerous studies and research conducted on finding a permanent cure for diabetes. Some of these studies have shown promising results, while others have not been as successful. One of the most promising areas of research is the use of stem cells to regenerate the damaged cells in the pancreas that produce insulin. This approach has shown some success in animal studies, but more research is needed before it can be used in humans.
Another area of research is the development of a vaccine that can prevent type 1 diabetes. This vaccine would work by stopping the immune system from attacking the cells in the pancreas. While this approach is still in the early stages of research, it shows potential for preventing type 1 diabetes in the future.
Lifestyle Changes
While a permanent cure for diabetes may not be available yet, there are steps that individuals can take to manage the disease and potentially reverse its effects. Making lifestyle changes such as following a healthy diet, exercising regularly, and maintaining a healthy weight can help control blood sugar levels and reduce the risk of complications. These changes can also improve overall health and well-being.
Conclusion
In conclusion, while there is currently no known permanent cure for diabetes, there is ongoing research and promising developments in the field. In the meantime, individuals can manage the disease through various treatments and lifestyle changes. It is important to work closely with a healthcare professional to find the best treatment plan for each individual's unique needs. With continued research and advancements, a permanent cure for diabetes may become a reality in the future.
or you can going to : https://managethenow.com/diabetes/
2 notes
·
View notes
Text
Radiant Smiles Start Here: Embrace Dental Checkups Today

Welcome to a journey towards radiant smiles! At Burtonsville Dental Suite, we believe that dental checkups are the foundation of optimal oral health. Embracing regular dental checkups is key to achieving and maintaining a beautiful, healthy smile. Our experienced team of dental professionals is dedicated to providing comprehensive and personalized care during each visit. Through thorough examinations, professional cleanings, and preventive treatments, we help prevent dental issues and detect early signs of problems. By prioritizing dental checkups, you take proactive steps towards a confident smile and overall well-being. Don't wait any longer, schedule your dental checkup today and embark on the path to radiant oral health!
Benefits of Regular Dental Checkups
1. Early Detection of Dental Issues: Regular dental checkups allow dentists to identify potential dental problems at an early stage. This includes detecting tooth decay, gum disease, oral infections, and oral cancer. Early intervention can prevent the progression of these issues and minimize the need for more extensive and costly treatments later on.
2. Preventive Care and Treatment: During checkups, dentists perform professional cleanings, removing plaque and tartar buildup that regular brushing and flossing may miss. They also provide preventive treatments such as fluoride application and dental sealants, which help strengthen teeth and protect against cavities.
3. Oral Health Education: Dental checkups offer an opportunity for patients to learn proper oral hygiene techniques and receive personalized oral health advice. Dentists can address concerns, provide tips for maintaining good oral health, and recommend suitable dental products for individual needs.
4. Overall Health Assessment: Dental checkups not only focus on oral health but also provide insights into overall health conditions. Dentists Burtonsville can identify signs of systemic diseases like diabetes or vitamin deficiencies, as certain symptoms may manifest in the mouth. Regular checkups contribute to a comprehensive approach to overall well-being.
What to Expect During a Dental Checkup
youtube
Source - American Dental Association (ADA)
1. Comprehensive Dental Examination: During a dental checkup, your dentist will perform a thorough examination of your teeth, gums, and oral tissues. They will check for signs of tooth decay, gum disease, oral infections, and other dental issues.
2. Dental X-rays and Imaging: X-rays or other imaging techniques may be used to get a detailed view of your teeth and jawbone. These images help the dentist detect problems that are not visible during a regular visual examination, such as hidden cavities or impacted teeth.
3. Professional Cleaning: A dental hygienist will perform a professional cleaning to remove plaque and tartar buildup from your teeth. This cleaning helps prevent gum disease and keeps your teeth looking their best.
4. Oral Health Discussion: Your dentist will discuss your oral health with you, addressing any concerns or questions you may have. They may provide personalized recommendations for oral hygiene practices and offer tips to improve your dental care routine at home.
Overall, a dental checkup is a proactive measure to maintain good oral health and prevent potential dental issues from becoming more severe in the future.
Common Dental Issues Detected During Checkups
1. Tooth Decay and Cavities: Dental checkups often reveal the presence of tooth decay and cavities. Early detection allows for timely treatment, such as fillings, to prevent further damage and preserve the tooth's structure.
2. Gum Disease and Periodontal Issues: Dentists can identify signs of gum disease during checkups, such as redness, swelling, or bleeding gums. Early intervention helps prevent the progression of gum disease, which, if left untreated, can lead to tooth loss and other health complications.
3. Oral Infections and Abscesses: Dental checkups may uncover oral infections or abscesses, which are pockets of pus caused by bacterial infections. Prompt treatment is essential to prevent the infection from spreading and causing more significant health issues.
4. Bite and Alignment Problems: Dentists can assess your bite and jaw alignment during checkups. Detecting issues like malocclusions or misalignments early on can lead to appropriate orthodontic interventions, ensuring better oral health and preventing potential jaw pain or discomfort.
Regular dental checkups are crucial for addressing these common dental issues promptly, preserving oral health, and preventing more extensive and costly treatments in the future.
Preventive Measures and Recommendations
1. Maintain Good Oral Hygiene: Brush your teeth at least twice a day for two minutes each time and floss daily to remove plaque and food particles. This helps prevent tooth decay and gum disease.
2. Regular Dental Checkups and Cleanings: Schedule dental checkups every six months or as recommended by your dentist. Regular visits allow for early detection of dental issues and professional cleanings to remove stubborn plaque and tartar.
3. Fluoride Treatments: Fluoride helps strengthen tooth enamel and makes teeth more resistant to decay. Your dentist may recommend fluoride treatments to protect your teeth, especially if you are prone to cavities.
4. Dental Sealants: Dental sealants are thin protective coatings applied to the chewing surfaces of molars to prevent cavities in the grooves and crevices. This is especially beneficial for children and teenagers, as their newly erupted permanent teeth are more susceptible to decay.
By following these preventive measures and recommendations, you can maintain optimal oral health, reduce the risk of dental issues, and enjoy a confident and healthy smile for years to come.
Some FAQs about Dental Checkups
1. Why are dental checkups essential?
Dental checkups are crucial for maintaining good oral health. Regular visits allow dentists to detect and address dental issues early, preventing more extensive problems and preserving your teeth's health.
2. How often should I schedule a dental checkup?
For most people, dental checkups are recommended every six months. However, your dentist may suggest more frequent visits based on your oral health needs and risk factors.
3. What happens during a dental checkup?
During a dental checkup, your dentist will conduct a comprehensive examination of your teeth, gums, and mouth. X-rays may be taken to identify hidden issues, and a professional cleaning will be performed to remove plaque and tartar.
4. Does dental insurance cover checkups?
Many dental insurance plans cover preventive services like dental checkups. However, coverage may vary, so it's essential to check with your insurance provider to understand your benefits.
5. Are dental checkups painful?
Dental checkups are typically not painful. The examination and cleaning are performed gently, and any discomfort is minimal. If you experience anxiety or fear, inform your dentist, as they can provide options for making the experience more comfortable, such as sedation techniques.
In conclusion, dental checkups play a vital role in maintaining optimal oral health and a bright smile. By attending regular checkups, you can catch dental issues early, receive preventive care, and stay informed about your oral health. Embrace the habit of dental checkups, and enjoy the benefits of a healthy and confident smile!
2 notes
·
View notes
Text
Fungal Infection Treatment hyderabad
Fungal Infection Treatment hyderabad
Introduction
Fungal infections are common health issues affecting individuals of all age groups. These infections, caused by fungi thriving in warm and moist conditions, can be bothersome and sometimes painful. If left untreated, they may lead to severe complications. At Twaccha, we specialise in delivering the best Fungal Infection Treatment Hyderabad, ensuring comprehensive and effective solutions for all types of fungal infections. Our goal is to provide relief and restore your skin and nails to their healthiest state. For anyone searching for reliable Fungal Infection Treatment Hyderabad, Twaccha is the ultimate choice.
Understanding Fungal Infections
Fungal infections are caused by microorganisms that flourish in damp and warm environments. These infections can spread quickly and often appear on the skin, nails, scalp, or even inside the body. Twaccha’s specialised Fungal Infection Treatment Hyderabad focuses on identifying the type of infection and providing the most effective treatment for long-lasting results. With our expertise, we are proud to be a trusted name for Fungal Infection Treatment Hyderabad.
Causes of Fungal Infections
Fungal infections have several causes, including:
Environmental Factors: Prolonged exposure to damp or humid conditions.
Lifestyle Choices: Wearing tight, non-breathable clothing or footwear.
Health Conditions: Diabetes, obesity, or weakened immunity.
Prolonged Medication Use: Long-term use of antibiotics or steroids.
At Twaccha, our team identifies these causes and offers tailored solutions through the best Fungal Infection Treatment Hyderabad. Our treatments not only address the infection but also prevent future occurrences, making us a leading provider of Fungal Infection Treatment Hyderabad.
Who is at Risk of Developing Fungal Infections?
While fungal infections can affect anyone, certain individuals are more vulnerable:
Diabetic patients.
Individuals with compromised immune systems.
People frequently exposed to damp conditions, such as athletes.
Residents of humid climates like Hyderabad.
Our expert team at Twaccha not only provides excellent Fungal Infection Treatment Hyderabad but also offers preventive advice for those at higher risk. If you are in Hyderabad and need specialised care, our Fungal Infection Treatment Hyderabad is the right choice.
Common Types of Fungal Infections
The most common fungal infections treated at Twaccha include:
Athlete’s Foot (Tinea Pedis): Affects the feet, causing itching, peeling, and discomfort.
Ringworm (Tinea Corporis): Red, circular patches appearing on various body parts.
Candidiasis: Caused by Candida yeast, typically affecting the mouth, throat, or genital areas.
Fungal Nail Infections: Leading to thickened, discoloured, and brittle nails.
With our advanced Fungal Infection Treatment Hyderabad, we address these infections with precision and care. Trust Twaccha to provide you with the most effective Fungal Infection Treatment Hyderabad for all these conditions.

Symptoms of Various Fungal Infections
Symptoms of fungal infections vary but commonly include:
Itching and redness in the affected area.
Scaling, peeling, or cracking skin.
Discolouration and thickening of nails.
White patches in the mouth or throat (oral candidiasis).
If you notice any of these symptoms, seeking professional care is essential. At Twaccha, our Fungal Infection Treatment Hyderabad ensures accurate diagnosis and effective solutions. For anyone experiencing these symptoms, our Fungal Infection Treatment Hyderabad is a trusted remedy.
Different Types of Fungal Infections
Fungal infections can manifest in different ways:
Skin Infections: Affect areas like feet, hands, scalp, and groin.
Nail Infections: Lead to discolouration and brittle nails.
Systemic Infections: Rare but severe, these affect internal organs in immunocompromised individuals.
At Twaccha, our comprehensive approach ensures that every patient receives the right care through our trusted Fungal Infection Treatment Hyderabad. Whether it’s a mild skin infection or a more serious condition, our Fungal Infection Treatment Hyderabad is designed to meet all needs.
Methods for Treating Fungal Infections
Treating fungal infections involves various methods, such as:
Topical Treatments: Creams, gels, or powders applied to the infected area.
Oral Medications: Tablets for deeper or more severe infections.
Medicated Shampoos: Used for scalp infections.
Laser Therapy: Advanced treatment for stubborn nail infections.
Our experienced professionals at Twaccha use these methods to deliver the best Fungal Infection Treatment Hyderabad. Whatever the severity of the infection, our Fungal Infection Treatment Hyderabad ensures complete care and recovery.
Treatment Options
We offer a range of treatment options, including:
Antifungal Creams: Effective for mild to moderate infections.
Prescription Medications: Tailored for chronic or systemic fungal conditions.
Lifestyle Recommendations: Guidance to prevent recurring infections.
At Twaccha, we ensure that every individual receives a personalised Fungal Infection Treatment Hyderabad plan for optimal recovery. Choosing Twaccha for Fungal Infection Treatment Hyderabad guarantees professional care with excellent results.
Process of Treating Fungal Infections
The treatment process at Twaccha is thorough and effective. It begins with an expert diagnosis to determine the type and severity of the infection. Following this, a customised treatment plan is prepared, which may include topical medications, oral treatments, or advanced therapies. With our trusted Fungal Infection Treatment Hyderabad, patients can expect a seamless journey towards complete recovery. Every step of our Fungal Infection Treatment Hyderabad process is designed for patient comfort and satisfaction.
Duration of Treatment for Fungal Infections
The duration of treatment depends on several factors, such as the type of infection and its severity. While minor infections may resolve in 2–4 weeks, more persistent cases, like nail fungal infections, can take several months. At Twaccha, we provide clear timelines and regular follow-ups as part of our dedicated Fungal Infection Treatment Hyderabad. With consistent care, our Fungal Infection Treatment Hyderabad ensures lasting results.
Possible Side Effects of Fungal Infection Treatments (and How to Prevent Them)
Fungal infection treatments are generally safe but may occasionally cause mild side effects, such as:
Skin irritation or dryness from topical medications.
Stomach upset from oral antifungals.
At Twaccha, we minimise these risks by monitoring reactions and providing guidance on proper medication use. Our Fungal Infection Treatment Hyderabad prioritises patient safety and ensures a smooth recovery. Patients who choose our Fungal Infection Treatment Hyderabad can be confident in both the effectiveness and safety of the treatment.
Conclusion
Fungal infections can be challenging, but with the right care, they are entirely manageable. At Twaccha, we are committed to offering the best Fungal Infection Treatment Hyderabad using advanced methods and personalised care plans. Our focus is on delivering effective solutions that ensure long-term relief and a healthier you. Trust Twaccha for expert Fungal Infection Treatment Hyderabad and experience exceptional care. For all your needs related to Fungal Infection Treatment Hyderabad, Twaccha is here to help.
FAQs
1.What is the best clinic for fungal infection treatment in Hyderabad?
Twaccha is the top choice for expert care in Fungal Infection Treatment Hyderabad.
2.How long does fungal infection treatment take?Treatment duration depends on the infection type but typically ranges from a few weeks to months.
3.Are fungal infection treatments safe?Yes, treatments at Twaccha are safe and designed for effective recovery.
4.Can fungal infections recur after treatment?Yes, but preventive measures and expert care at Twaccha reduce the chances significantly.
5.Why choose Twaccha for fungal infection treatment in Hyderabad? Twaccha offers personalized care, advanced treatments, and proven results for Fungal Infection Treatment Hyderabad.
0 notes
Text
Periodontal disease, also known as gum disease, is a common yet often overlooked condition that affects the tissues surrounding your teeth. While many people focus on the impact periodontal disease has on their oral health, research has shown that this condition can also have significant implications for your overall well-being. In fact, gum disease has been linked to a variety of serious health issues, ranging from heart disease to diabetes and even Alzheimer’s disease. Understanding the connection between periodontal disease and overall health is crucial not only for your dental hygiene but for your general health as well.
What is Periodontal Disease?
Periodontal disease is an infection of the tissues that hold your teeth in place. It typically starts as gingivitis, a mild form of gum disease that causes redness, swelling, and bleeding of the gums. If left untreated, gingivitis can progress to periodontitis, a more severe form of gum disease where the infection spreads deeper into the tissues and can cause tooth loss.
The primary causes of periodontal disease include poor oral hygiene, smoking, genetics, certain medications, and conditions that affect the immune system. Factors like age, poor nutrition, and stress can also contribute to the development of periodontal disease. Regular dental checkups and good oral hygiene practices, such as brushing and flossing, are essential to preventing gum disease.
The Link Between Periodontal Disease and Heart Disease
One of the most significant connections between periodontal disease and overall health is the increased risk of heart disease. Studies have shown that people with gum disease are more likely to suffer from heart disease and other cardiovascular issues.
The bacteria from infected gums may enter the bloodstream, leading to an increased inflammatory response in the body. Chronic inflammation is a known risk factor for atherosclerosis (narrowing of the arteries), which can contribute to heart attacks, strokes, and other cardiovascular problems.
Diabetes and Periodontal Disease: A Two-Way Street
Diabetes and periodontal disease have a complex, bidirectional relationship. People with diabetes are more susceptible to gum disease because high blood sugar levels can weaken the immune system and make it harder for the body to fight infections, including gum infections.
The inflammation associated with gum disease can lead to higher blood sugar levels, increasing the risk of complications for people with diabetes. Research has shown that treating periodontal disease can improve blood sugar control in people with diabetes, further emphasizing the importance of maintaining good oral health in managing this chronic condition...Read More
0 notes
Text
Managing Diabetes: Tips for Better Blood Sugar Control
November marks Diabetes Awareness Month, a time to focus on the importance of managing diabetes effectively. At Endocrinology Associates, we are committed to providing practical strategies and expert care to help our patients maintain better blood sugar control and live healthier lives.
Understanding Diabetes
Diabetes is a chronic condition that affects how your body processes blood sugar (glucose).
Left unmanaged, it can lead to serious complications such as heart disease, kidney damage, nerve damage, and vision problems. However, with the right approach, diabetes can be managed effectively, empowering individuals to lead full and active lives.
Practical Tips for Managing Diabetes
1. Healthy Eating
The cornerstone of diabetes management is a well-balanced diet. Focus on these principles:
Monitor Carbohydrates: Keep track of your carb intake, as they have the most significant impact on blood sugar levels. Opt for complex carbs like whole grains, legumes, and vegetables.
Incorporate Protein and Healthy Fats: These can help stabilize blood sugar levels and provide lasting energy.
Portion Control: Be mindful of portion sizes to avoid overeating.
Stay Hydrated: Drinking water throughout the day helps maintain blood sugar balance.
2. Regular Exercise
Physical activity plays a vital role in managing diabetes. Exercise helps:
Lower blood sugar levels.
Increase insulin sensitivity.
Improve overall cardiovascular health.
Reduce stress levels.
Aim for at least 150 minutes of moderate aerobic activity, like brisk walking or swimming, each week. Strength training exercises are also beneficial for building muscle and improving insulin use.
3. Medication Management
Many individuals with diabetes require medications to maintain blood sugar levels. These may include:
Insulin Therapy: Essential for individuals with type 1 diabetes and some with type 2 diabetes.
Oral Medications: Help improve the body’s use of insulin or reduce sugar production in the liver.
Newer Options: Medications such as incretins may improve weight and glucose control in patients with type 2 diabetes.
Work closely with your healthcare provider to ensure your medication regimen is optimized for your needs.
4. Monitor Your Blood Sugar
Regular blood sugar monitoring is crucial for understanding how your body responds to food, medication, and activity. Continuous glucose monitors (CGMs) and traditional glucometers provide valuable insights to help make informed decisions.
5. Prioritize Mental Health
Managing diabetes can be overwhelming. Stress and anxiety can also impact blood sugar levels. Consider these strategies:
Practice mindfulness or meditation.
Seek support from family, friends, or diabetes support groups.
Talk to a counselor or therapist if you’re feeling stressed or burned out.
Diabetes Care at Endocrinology Associates
At Endocrinology Associates, we are dedicated to providing comprehensive diabetes care tailored to each patient’s unique needs. Our team, led by Dr. Elena A. Christofides, works to address all aspects of diabetes management, from lifestyle changes to advanced treatment options.
Our approach includes:
Personalized diet and exercise plans.
Expert guidance on medication use.
Cutting-edge technologies for blood sugar monitoring.
Ongoing support to help patients thrive.
Take Control of Your Diabetes Today
Whether you’re newly diagnosed or looking for better ways to manage your diabetes, Endocrinology Associates is here to help.
Our expertise in endocrinology and personalized care ensures you get the support you need to improve your health and quality of life.
Schedule a Consultation
Contact us to take the first step toward better blood sugar control.
Call us at (614) 453-9999 or visit our office at:
72 W 3rd Ave, 2nd Floor, Columbus, OH 43201
Together, we can help you achieve lasting health and well-being.
0 notes
Text
Improving Dental Implant Success Rate: What are the Top Determining Factors?
Dental implants prove to be an aesthetic, durable solution for missing teeth. With a high success rate of around 95%, these are regarded as a breakthrough in modern dentistry. However, proper care and consideration are the keys to their success. Know about top 3 factors that can significantly determine and improve the success rate of a dental implant Kolkata procedure.

Health of bones and gum line
Sufficient bone density and a healthy gum line are necessary for the implant to integrate with the jawbone successfully. Implantation can only be successful with a healthy mouth and body. If left untreated, conditions such as gum disease can compromise the stability of implants. The risks of failure can increase.
Presence of systemic health conditions
Systemic health conditions such as diabetes or autoimmune disorders can impede the healing process and affect implant success. It is crucial to manage these conditions through proper medical intervention.
Addictions
Quitting smoking also boosts the success rate significantly. Tobacco restricts blood flow to the gums, hindering healing and bone integration.
Diet
Avoid hard foods immediately after the procedure. You can prevent unnecessary strain on the implant.
Experience of your dental professional
The success of your implant procedure is also, largely decided by the expertise of your dental surgeon. A precise, delicate process, Implant placement needs in-depth knowledge of:
Dental anatomy,
Implant technology, and
Surgical techniques
With an experienced dentist, you can be assured of accurate placement. It can minimize your risks of complications such as nerve damage or improper osseointegration (bonding of the implant to the bone).
Further, dentists skilled in advanced imaging techniques, such as CBCT scans, can evaluate bone quality with greater precision and position implants accurately. This way, you can enjoy benefits from your dental implants for a long time to come.
Commitment to post-surgical care
It is equally important that you follow a proper oral hygiene routine is essential to prevent infections, such as peri-implantitis. Regular brushing, flossing, and the use of antimicrobial mouthwash can keep the area around the implant healthy.
Going for routine dental check-ups
These also play a vital role in the success of dental implants. Dentists can monitor the healing process, ensure the implant is integrating well, and address any potential issues early.
Focus on these key factors to make your implants work long-term, possibly for a lifetime.
#Dental Implants clinic in Kolkata#best dental implant clinic in Kolkata#Top-rated dental implant clinic in Kolkata#High-quality dental implants in Kolkata#dental clinic in Kolkata#top dental clinic Kolkata#top dental clinic in Kolkata
0 notes
Text
Bad Breath: What It Means, Why It Happens, and How to Fix It
Let’s talk about something we don’t always love to acknowledge: bad breath. Officially known as halitosis, it’s more than just an awkward moment in close conversations. It can seriously affect your confidence, your social life, and even your health. The good news? It’s manageable—and understanding the causes and solutions is the first step.
Why Does Bad Breath Happen?
The Usual Suspects: Oral Hygiene & Dental Health
Bacteria: Your mouth is full of bacteria that break down food particles and produce smelly sulfur compounds. Think of them as tiny, odor-causing party crashers.
Dental Problems: Cavities, gum disease, and poorly maintained dental appliances (like braces or dentures) can give bacteria extra places to hide and grow.
Blame Your Diet and Lifestyle
Food Choices: Garlic, onions, and spicy foods are famous for their lingering smells. They release compounds that enter your bloodstream and come out through your breath.
Tobacco & Alcohol: Smoking and drinking dry out your mouth, making it a paradise for bacteria.
High-Protein or Sugary Diets: Too much sugar feeds bacteria, and proteins can release sulfur gases as they’re metabolized. Yikes.
Underlying Health Issues
Diabetes: A fruity or acetone-like odor might mean your blood sugar isn’t under control—a serious complication called ketoacidosis.
Kidney Problems: A fishy smell could signal that your kidneys aren’t filtering toxins like they should.
Liver Disease & GERD: These can cause distinctive breath odors tied to serious internal health issues.
Other Triggers
Hormonal changes (like pregnancy or menstruation) and dry mouth (often caused by medications or dehydration) can also play a big role.
How Can You Tackle Bad Breath?
Step Up Your Oral Hygiene Game
Brush and Floss Regularly: Twice a day, with floss to reach what your toothbrush can’t.
Clean Your Tongue: Use a tongue scraper to get rid of bacteria that live there.
Rinse Smart: Alcohol-free mouthwash or salt water helps clean without drying out your mouth.
Take Care of Dental Appliances: Clean dentures, retainers, and braces properly.
Stay Hydrated and Mind Your Diet
Drink Water: A dry mouth makes bacteria thrive. Keep it moist!
Choose Wisely: Go easy on smelly foods and sugary snacks. Balance your meals with veggies and whole grains.
Try Natural Helpers
Peppermint, sage, and eucalyptus aren’t just for aesthetics—they’re antibacterial and refreshing.
Tea tree oil and clove? Absolute powerhouses against odor-causing bacteria.
When to See a Doctor
If bad breath sticks around despite your best efforts, it could be a sign of something more serious, like diabetes, GERD, or liver issues. Don’t ignore it—getting checked out could make all the difference.
It’s Not Just About Fresh Breath
Halitosis might seem small, but it’s tied to much bigger things—your health, your confidence, and your overall quality of life. With a little care, you can ditch the bad breath and feel good about flashing that smile.
Find dentist near me
So, whether you’re dealing with morning breath, a garlic hangover, or something that just won’t go away, know this: there’s always a solution—and you’ve got this. 💪✨
0 notes
Text
Why Choose the Best Dental Clinic in Palakkad for Your Oral Health
Dental health plays a crucial role in your overall well-being, and finding the right clinic ensures you receive the care you deserve. If you’re in Palakkad, look no further than the Best Dental Clinic in Palakkad, where expertise and innovation come together to offer top-notch dental care.
Comprehensive Services
Our clinic provides a wide range of dental treatments, including:
General Dentistry: Regular cleanings, fillings, and preventive care to maintain your oral health.
Cosmetic Dentistry: Smile makeovers with teeth whitening, veneers, and more.
Orthodontics: Straighten your teeth with braces or aligners.
Specialized Treatments: Root canals, gum care, and dental implants.
Why Choose the Best Dental Clinic in Palakkad?
Experienced Dentists: Our team comprises highly qualified professionals who bring years of experience to each treatment.
Modern Technology: We utilize advanced equipment and techniques to ensure precision and comfort.
Personalized Care: Every patient receives tailored solutions based on their specific needs.
Patient Comfort: From a welcoming ambiance to gentle treatments, your comfort is our priority.
Benefits of Regular Dental Visits
Early Detection: Regular check-ups help identify issues like cavities or gum diseases early.
Improved Aesthetics: Professional cleaning and cosmetic treatments enhance your smile.
Overall Health: Good oral hygiene prevents complications like heart disease or diabetes.
Convenient Location in Palakkad
Situated in the heart of Palakkad, our clinic is easily accessible, making it convenient for families and individuals alike. With a focus on creating long-term relationships, we aim to be your trusted partner in dental care.
Final Thoughts
Choosing the Best Dental Clinic in Palakkad means entrusting your oral health to professionals dedicated to excellence. With comprehensive services, a skilled team, and a commitment to patient satisfaction, we are here to keep your smile healthy and bright.
Book your appointment today and experience the difference!
0 notes