#Nonclassical @nonclassical
Explore tagged Tumblr posts
Text


Princess Zelda from The Legend of Zelda series is intersex and transmasculine, and their* variation is Non-classic Congenital Adrenal Hyperplasia (NCAH)!
Intersex flag-only and popular transmasc flag edits under the cut!




*pronouns not specified in ask + the requester said "Zelda/Sheik/Tetra" and was alright with me picking one, not from any specific source. So I went with Brawl's depiction of Zelda. Does my age show yet.
#requested by anon#intersex#intersex headcanon#congenital adrenal hyperplasia#nonclassic congenital adrenal hyperplasia#late onset congenital adrenal hyperplasia#CAH#NCAH#NCCAH#LOCAH#queer headcanons#gender headcanon#trans headcanon#trans#transgender#transmasc#transmasculine#the legend of zelda#tloz#loz zelda#tloz zelda#loz sheik#loz tetra
41 notes
·
View notes
Text
Some intersex flags! (Part 2)
Part 2 of making flags for intersex traits and variations that were flagless! (Part one is here.) There will be a part 3 & 4 and then all the main intersex traits/variations will officially have flags.
Please read (and reblog) our intersex guide. It is so important to understand intersex people, their bodies, and their health!
Accessory Ovary

The flag is based on the uterus didelphys and polyorchidism flags. The A is meant to represent the name of this variation. The three circles are meant to represent ovaries. The plus symbol is meant to stand for people who have more than one accessory ovary (aka 3+ ovaries.)
Supernummary Ovary

The flag is based on the uterus didelphys and polyorchidism flags. The S is meant to represent the name of this variation. The three circles are meant to represent ovaries. The plus symbol is meant to stand for people who have more than one accessory ovary (aka 3+ ovaries.)
Cervical Duplication

The flag is based on the uterus didelphys flag. In the center of the flag, the shape is meant to vaguely resemble a uterus with two cervixes.
Cervical Duplication + Uterus Didelphys

The flag is based on the uterus didelphys flag, with the shapes being changed to vaguely resemble two uteruses with cervixes.
Cervical Agenesis

The flag is based on the MKRH Syndrome flag. The symbol is meant to represent a uterus with an X over where the cervix would be.
Cervical Hypoplasia

The flag is based on MKRH Syndrome flag. The symbol is meant to represent a uterus with a minus symbol over where the cervix would be, representing its smaller size.
Uterine Hypoplasia

The flag is based on MKRH Syndrome flag, with a minus with a minus symbol, representing its smaller size.
Anorchia

The flag is based on the ovarian agenesis flag. The circle with the X represents a lack of gonads.
Monorchidism

The flag is based on the ovarian agenesis flag. The circle in the symbol represents the testicle itself. The 1 represents how there is only one gonad, and the M represents the name of this variation.
Unilateral Ovarian Agenesis

The flag is based on the ovarian agenesis flag. The circle in the symbol represents the ovary itself. The 1 represents how there is only one gonad, and the U represents the name of this variation.
Aromatase Excess Syndrome (AEXS/AES)

The flag uses the hyperestrogenism symbol, as it is a form of hyperstrogenism. The shades of pink represent the feminizing effects of the variation. The rainbow and monochrome coloring represents the gender spectrum, and how any gender can have this variation.
Classic CAH (Simple-Virilizing)

The flag is based on the CAH flag. The SV represents the name of this variation.
Classic CAH (Salt-Wasting)

The flag is based on the CAH flag. The SW represents the name of this variation.
Nonclassic CAH

The flag is based on the CAH flag. The NC represents the name of this variation.
Leydig Cell Hypoplasia (LCH)

The shades of blue represent the masculinizing effects of testosterone. The grey represents hypoandrogenism, and low levels of androgens. The grey circle represents the testes, and the underdeveloped/absent leydig cells within them.
17-KSR Deficiency

The purple and yellow represents that this variation is a form of intersex. The shades of grey surrounding the blue represents the "barrier" preventing androstenedione from converting into testosterone. The Ks and 17 represents the name of this variation.
Aromatase Deficiency

The purple and yellow represents that this variation is a form of intersex. The shades of blue represents the hyperandrogenism, and the pink surrounded by grey represents hypoestrogenism. The AD represents the name of this variation.
Mild Androgen Insensitivity Syndrome (MAIS)

The flag is based on the AIS flag. The M represents the name of this variation.
Partial Androgen Insensitivity Syndrome (PAIS)

The flag is based on the AIS flag. The Ps represents the name of this variation.
Complete Androgen Insensitivity Syndrome (CAIS)

The flag is based on the AIS flag. The Cs represents the name of this variation.
#lgbt#lgbtq#lgbtqia#lgbt pride#queer#educate yourself#body diversity#diversity#intersex#intersex spectrum#intersex community#accessory ovary#supernummary ovary#cervical duplication#uterus didelphys#classic CAH#congenital adrenal hyperplasia#nonclassic cah#17-KSR deficiency#17 KSR deficiency#aromatase deficiency#aromatase excess syndrome#aexs#aes#flag coining#pride flag#mild androgen insensitivity syndrome#mais#partial androgen insensitivity syndrome#pais
89 notes
·
View notes
Text
Okay I'm going to ask a question but I may delete this later: if any of my followers (or anyone who sees this) has nonclassic CAH how did you find out that you have it? What are some signs you'd say to look out for?
#speaks#to make it clear i am not self diagnosing with cah or anything else#i am probably over reacting to certian things but I'd like to get some opinions before going to a doctor about anything#nonclassic cah#ncah
4 notes
·
View notes
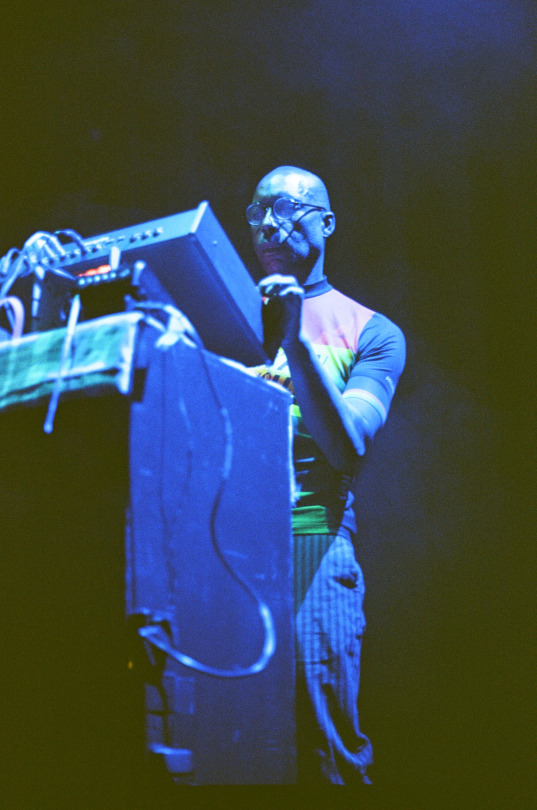
Audio
Nonclassical’s nonclassical at 20
#nonclassical at 20#nonclassical#music#electronic#ambient#electroacoustic#classical#field recording#sound collage#glitch#microsound#chamber music#orchestral#drone#dark ambient#minimal#experimental#bandcamp#nailah hunter#pavel milyakov#christina vantzou#kmru#matthew herbert
3 notes
·
View notes
Note
Hey, I have some questions rated to NCAH. I was AFAB and as far as I know don't have genital variations, but I had an early puberty and symptoms of hyperandrogenism such as acne and excess body and facial hair (noticeable but not severe). I had issues with my periods but I was diagnosed with endometriosis so I don't think they're connected. I did hormone testing and despite everything, my testosterone is average. However, I have high prolactin and 17-alpha-hidroxi-progesterone, which I know is associated with NCAH. Is it enough for a diagnosis though? I've done research on it but I'm not sure. Sadly I don't think my doctor will help in this regard because she already glossed over this part of the test results completely when I received them and wasn't open to the idea of me maybe having hyperandrogenism anyways
Hi anon! I'm sorry that your doctor hasn't been helpful in interpreting your test results. that's really frustrating that you aren't able to easily access medical support. Standard disclaimer that we can't diagnose people or provide medical advice on here, but I'm happy to share some resources for understanding your test results and explaining the CAH diagnosis criteria.
So, you're absolutely right that 17 alpha hidroxi progesterone (17 OHP) is associated with CAH. High levels of 17 OHP is one of biggest signs of CAH. I think it was really, really shitty and irresponsible of your doctor to refuse to test more because 17 OHP plus signs of hyperandrogenism are like textbook signs of CAH.
I'm going to share a chart explaining 17 OHP levels and CAH, sourced from myendoconsult. (Here's another medical journal with more information about diagnosis as well.)

ID: [A flowchart titled "Cosyntropin (ACTH) stimulation test. The first row of the flowchart shows the possible options for 17 OHP levels. Text of option 1 reads "Heterozygotes/Unaffected. 17 OHP less than 200 ng/dL or less than 6 nmol/L." Option 2 reads "Indeterminate. 17 OHP is 200 to 10,000 ng/dL or 6 to 300 nmol/L." The third option reads "Classic 21OH deficiency (CAH). 17 OHP is greater than 10,000 ng/dL or greater than 300 nmol/L." The next section of the flowchart has different options for what to do next if the results are indeterminate, and shares the three options for ACTH stim test results. The first ACTH stim test result option is less than 1000 ng/dL or less than 30 nmol/L, which would be heterozygotes/unaffected. The next category of ACTH stim test result is 1000 to 10,000 ng/dL or 31 to 300 nmol/L, which is Nonclassic CAH (NCAH). The third category of ACTH stim test result is greater than 10,000 ng/dL or greater than 300 nmol/L, which is Classic CAH. ]
This flowchart shows the role that 17 OHP plays in CAH diagnosis. First, doctors just test your 17 OHP levels and see if they can make a diagnosis just from that. If your 17 OHP levels were less than 200 ng/dL, they can see that you don't have CAH. If your 17 OHP levels were over 10,000, they can diagnose you with Classic CAH. However, if your 17 OHP levels are higher than normal but still below 10,000 CAH, that usually means they need to do more testing to figure it out.
The usual way they test this is through an ACTH stimulation test, where they inject you with ACTH and then measure your 17 OHP levels an hour afterwards. For people with NCAH or CAH, their 17 OHP levels will jump even higher, with a change of at least 1000 ng/dL or 30 nmol/L required for diagnosis.
So, long story short, one way you could try to figure out if your 17 OHP levels mean that you have CAH is by comparing your lab results to the flowchart above. If your 17 OHP levels are in the indeterminate range, this is something that you could bring back in to your doctor and say "Hey, best practices mean that since my 17 OHP levels are high enough to be in this range that you need to do an ACTH stimulation test for me so I can get actual results."
High prolactin can also be associated with CAH. Here's one study talking about high prolactin levels. In fact, here's another study specifically talking about high prolactin levels and normal androgen levels in a subset of people with CAH.
So, long story short, high levels of 17 OHP and high prolactin can be signs of CAH. To confirm a diagnosis, you'd probably need to look specifically at your records to figure out your 17 OHP levels, and potentially try to get an ACTH stim test depending on your results, although I know that can be difficult or impossible when doctors refuse to cooperate.
I hope this helps, and please feel free to send in another ask if you have any other questions!
17 notes
·
View notes
Text
i have hyperandrogenism but i think it's more likely cah than pcos.
pcos is more common i think. the symptoms are as follows: irregular/absent/heavy periods, excess body hair, acne, pelvic pain, infertility, patches of darker skin, ovarian cysts, hyperandrogenism, weight gain, metabolic syndrome, and alopecia.
i only experience the menstrual irregularity, body hair, acne, and hyperandrogenism. i'm not sure abt the infertility bc i don't want kids and never have, and i was supposed to get scanned for the cysts but it never happened. also 80% of ppl with pcos are obese and i have never been.
the symptoms of cah (more specifically, the nonclassic/late onset variant; the others would've been detected at birth): acne, hirstutism, rapid childhood growth, early or delayed puberty, menstrual irregularity, infertility, and a couple things that make me uncomfortable to mention here
i experience one of 3 unmentioned symptoms. like i said, idk abt infertility bc i don't want kids. but i experience literally everything else i listed.
it's 4/11 pcos symptoms, vs 7/9 cah symptoms
7 notes
·
View notes
Text


Fyodor Dostoevsky from Bungou Stray Dogs is intersex and transfeminine, and their* variation is Non-classic Congenital Adrenal Hyperplasia (NCAH)!
Intersex flag-only and popular transfem flag edits under the cut!




*pronouns not specified in ask
#requested by anon#skipping the queue#because my inbox starts to glitch over 20+ asks and. guess who let the asks build up. lol. lmao even#so tldr idk what place this request was in so just get yeeted to the top idc#intersex#intersex headcanon#congenital adrenal hyperplasia#nonclassic congenital adrenal hyperplasia#late onset congenital adrenal hyperplasia#CAH#NCAH#NCCAH#LOCAH#queer headcanons#gender headcanon#trans headcanon#trans#transgender#transfem#transfeminine#bungou stray dogs#bsd#fyodor dostoevsky#bsd fyodor#tw scopophobia#hamilton rule
16 notes
·
View notes
Text
We love you, intersex people!
We love you, intersex people.
We love you, AMAB, AFAB, CAMAB, CAFAB, UAB, and AXAB intersex people.
We love you, RFAB and RMAB intersex people.
We love you, intersex people whose SIG (socially imposed gender) differs from what you were assigned or reassigned.
We love you, intersex people who have suffered from medical abuse and medical neglect.
We love you, intersex people with any presentation, pronouns, or gender (be it feminine, masculine, androgynous, neutral, xenine, outherine, aporine, or a mixture!)
We love you, intersex people with any romantic, sexual, platonic, familial, sensual, queerplatonic, alterous, or waveric orientation.
We love you, intersex people with any relationship orientation.
We love you, intersex BIPOC.
We love you, disabled intersex people. That includes those of you who are neurodivergent (including those with commonly demonized forms of neurodivergence) and those of you with hidden disabilities.
We love you, intersex people of any weight or height.
We love you, intersex people with any religion. Whether it be Christianity, Catholicism, Judaism, Islam, Baha’i, Buddhism, Jainism, Hinduism, Sikhism, Confucianism, Taoism, Shintoism, Wiccanry, Druidism, Reconstructionist Paganism, Eclectic Paganism, or Zoroastrianism - we love you.
We love you, intersex people with penile traits. Whether it be congenital chordee, penoscrotal transposition, or diphallia - we love you.
We love you, intersex people with urethral traits. Whether it be hypospadias, epispadias, persistent urogenital sinus, persistent cloaca (partial or complete), or urethral duplication - we love you.
We love you, intersex people with ambiguous genitalia. Whether it be a bifid scrotum, fused labia, clitoromegaly, fused labia & clitoromegaly combo, pseudophallus, penis & vulva combo, or penis & vagina combo - we love you.
We love you, intersex people on the agenital spectrum. Whether it be urethral agenesis, urethral hypoplasia, vaginal agenesis, vaginal hypoplasia, imperforate hymen, microperforate hymen, cribriform hymen, septate hymen, sleeve hymen, vaginal septums (transverse, hemivagina, longitudinal,) labial hypoplasia, clitoral hypoplasia, clitoral agenesis, penile hypoplasia/micropenis, congenital buried penis, penile agenesis, aposthia, cryptorchidism, testicular agenesis, or microorchidism - we love you.
We love you, intersex people with reproductive traits. Whether it be ovotestes, ovarian hypoplasia, gonadal dysgenesis, uterus hypoplasia, unicornuate uterus, MRKH syndrome, WNT4 deficiency, prostate hypoplasia, prostate agenesis, seminal vesicle hypoplasia, seminal vesicle agenesis, fallopian tube agenesis, vas deferens aplasia, uterus didelphys, cervical duplication, accessory ovary, supernumerary ovary, polyorchidism, vas deferens duplication, or fallopian tube duplication - we love you.
We love you, intersex people with hormonal traits. Whether it be hypergonadism, hypogonadism, PCOS, congenital adrenal hyperplasia (classic or nonclassic), leydig cell hypoplasia, 17 KSR deficiency, 5α-Reductase 2 Deficiency, aromatase deficiency, estrogen insensitivity syndrome, or androgen insensitivity syndrome (mild, partial, or complete) - we love you.
We love you, intersex people with chromosomal variations. Whether it be Swyer syndrome, mixed gonadal dysgenesis, XYY syndrome, XYYY syndrome, XYYYY syndrome, XXYYY syndrome, XXXYY syndrome, XXYY syndrome, Klinefelter syndrome, XXXY syndrome, XXXXY syndrome, XXXXX Syndrome, XXXX syndrome, XXX syndrome, XX male syndrome, or Turner Syndrome - we love you.
If you are intersex, you are stunning/beautiful/handsome, and you deserve joy and peace!
#lgbtqia#lgbt#lgbtq#lgbt pride#queer#intersex#intersex spectrum#body diversity#intersex community#queer pride#queer community#lgbtq community#lgbtqi#lgbtq positivity#queer positivity#intersex positivity#lgbt positivity#body posititivity#body positive#varsex#body acceptance#agenital spectrum#penile variations#intersex variations#intersex traits#hormonal traits#hormone health#hormonally intersex#hormonal variations#hormones
302 notes
·
View notes
Note
pride headcanons for katya pafl?:]
KATYUSHA :((( I THINK OF HER...
shes an aroacespec lesbian! she isnt interested jn traditional dating but she loves to be in qprs. she's intersex [unrelated to her chimerism for the record], specifically she has nonclassic cah. it hasnt affected her too much yet at the time of canon and nobody knows abt it yet bcs of that. annnd shes fem-aligned but doesnt rlly care how she gets gendered. she asks her friends to switch it up a little for her every now and then. for fun <3
11 notes
·
View notes
Note
Can someone be considered intersex if they have non-salt-wasting nonclassical congenital adrenal hyperplasia (NCAH)?If they had non consensual surgery as an infant, but were raised as one gender and made to believe they are perisex?
I’m struggling with some recent life discoveries and trying to understand myself a bit better… any insight is very much appreciated!
I'm not super educated on the first words. But Google said it can cause intersex variations + if you had surgery against your will in order to better "fit" their idea of a sex, that's an intersex experience. Others who know more / have advice to help you figure things out feel free to reply
#03 ;; anon asks#intersex medical struggles#intersex questions#intersex#intersex experience#intersex experiences#intersexism
6 notes
·
View notes
Text

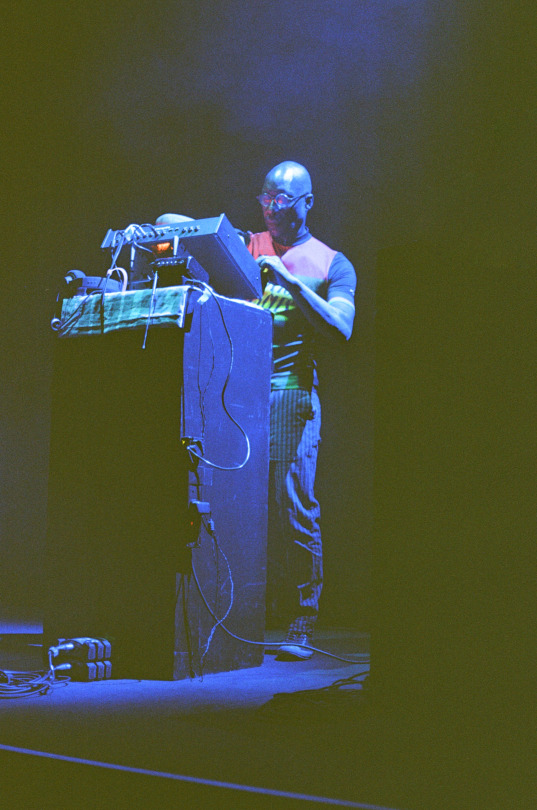










Disruptive Frequencies Live @ Kings Place - 15th July 23.
Beautiful moments captured by Stephen Akinyemi @Bare_Clips on Insta.
Disruptive Frequencies Vinyl/Digital Out Now - Purchase Here
#Nonclassical#NikNak#Dhangsha#NikkiSheth#Bantu#PoulomiDesai#noise#soundscapes#fieldrecordings#noisemusic#experrimentalsound#sonics#sonicart#soundartist#soundart#experimentalnoise#bassculture#harshnoise#harshbass#soundcollage#audiofragmentation#deepbass#dushume#experimentalmusic#glitch
0 notes
Note
do you know anything about late-onset congenital adrenal hyperplasia? i just found it on my file while looking for something else. i have an unrelated surgery coming up and i'm trying to figure out if this could have any effect on how my body handles that, especially wrt cortisol. but i can't find much on it at all, particularly how it affects ppl beyond infertility and sex characteristics. my impression is that at least the classic variant of it sounds like something intersex-related so i thought you might have heard of it. i remember asking my doctors for more information and they were basically like "don't worry about it unless you wanna get pregnant :)"
Hey anon.
So, late onset congenital adrenal hyperplasia, also called nonclassic congenital adrenal hyperplasia, is considered an intersex variation. (If you search NCAH on my blog or on @intersex-support, you might find some other posts about it). Because of the way it affects our testosterone levels and secondary sex characteristics outside of what is typically considered "female", late onset CAH is intersex, even if late onset CAH hasn't caused changes in genitalia.
Of course, there's no pressure to instantly start referring to yourself as intersex, or start participating in intersex community, but know that you are welcome here, and there are a lot of people who understand what it's like. I also have CAH, and I'm always happy to talk about it with anyone else. I know that it can be sort of shocking or overwhelming to get that information for the first time. Any feelings you have about it are completely valid. You can take as much time as you need to process. The community is here for you whenever you're ready.
In terms of surgery and CAH, there are some important considerations. For people with NCAH, there's going to be a range for how each individual makes and processes cortisol and aldosterone. Some people need daily glucocorticoid replacement therapy while others do not. However, even if you do not need daily steroid replacement, some people with NCAH need extra "stress dosing" of glucocorticoids when their body is under physical stress, such as during illness, injury, or surgery. It would be really important to talk to your surgeon, an anesthesiologist, and probably an endocrinologist before the surgery to make sure you know what your cortisol and aldosterone production is and make a plan if you need stress dosing during surgery or surgery recovery.
One book I would recommend for people with CAH is the Parent's Guide to CAH. In a lot of ways this book kind of sucks--it's directed towards parents, uses a lot of cissexist language, and uses a very medicalized model, but has some of the clearest nonacademic writing about what CAH is, how it works, treatment options, and talks about different considerations like surgery, illness, etc.
Please feel free to reach back out with any other questions, whether it's about CAH, intersex stuff, or if you want suggestions on any other resources. Thinking of you, anon, and hope your surgery goes well! 💜💛💜
33 notes
·
View notes
Text

NikNak (Nicole Raymond)
source: nonclassical © 📸: ???
4 notes
·
View notes
Note
Hi, this is sort of specific and probably requires more medical professional input but the doctors in my area are pretty interphobic and its like pulling teeth trying to get them to help me :/ I'm kind of lost between NCAH and Simple Virilizing CAH and I'm wondering if you can help point me in one direction?
Since 11, my periods have always been irregular, painful and very heavy. I've tried birth control (6 different ones) and none of them worked. I have slightly elevated T levels but still below what the average perisex man would have. During puberty, I didn't experience a lot of masculinising changes (maybe some slight upper lip hair) but I also didn't experience much of the feminising ones that I was supposed to either (barely any weight gain, no hip widening, no fat redistribution, I'm an A cup in bras).
(tmi warning here) I've had a 'bigger' clitoris since birth but during puberty it grew to the point where partners have asked if I'm on T. My vagina opening has always been very small and shallow, if that counts for anything as well.
Since learning about NCAH I thought that that was my variation (no diagnosis though, my doctors said I have pcos but refuse to test for NCAH) but about 2 years ago, I had a 'health spell' where I experienced a lot of symptoms of adrenal fatigue (fainting, weakness, craving salt, weight loss). That lasted for a few weeks and then suddenly disappeared, though I do experience fatigue every now and again. When I went to find answers, my doctors pinned it to anemia and basically said I don't need my cortisol levels checked :/
Since I've shown some signs of high T since birth, is this SV CAH? Or just NCAH with really severe symptoms? I know it's silly but I'm scared of having another 'health spell' and if its SV CAH, at least i can take precautions. (Totally understand if this is out of your ballpark, just needed to get this off my chest, thanks for reading)
Hi anon,
So as always, disclaimer that we are not doctors and cannot diagnose or provide medical advice.
It makes sense to me that you've been looking into NCAH and SV CAH. To my understanding, the only way to find out whether you have nonclassic or classic CAH would be through testing 17 OHP levels and seeing the extent that 17 OHP is elevated--there are different cutoff levels for diagnosis. If 17 OHP is borderline, then an ACTH stim test can be used to verify NCAH.
It's hard to say for certain whether the other traits you described would be caused by NCAH or SV CAH--there is case studies describing people with NCAH who are symptomatic with adrenal function suppressed/ cortisol response suboptimal. In fact, some people with NCAH also need stress dosing of glucocorticoids. So probably, at this point, the only way to know for sure would be to get blood testing done.
I know how frustrating it is to navigate doctors who aren't listening to us, and I'm sorry you're having to deal with it! I wish I could offer a better answer.
Sources: x, x
22 notes
·
View notes
Note
Hello! I was afab and I've been iding as tranmasc for a while. I've had friends and family assume that I'm on testosterone but I never thought much of it I do have solid sideburns, am def hairier than my sister, and my voice reads as p androgynous, but it makes me happy so I never thought much of it. However, I recently started the process to get on hrt and I found out that my testosterone levels are already notably higher than is typical for cis women, if still below the standard male range-- my doctor actually assumed that I'd been diying. He told me that there isn't any point of looking into specific conditions unless I have symptoms that are causing issues, so I don't have any sort of diagnosis. Could I be considered intersex? Is there any point to thinking abt it if I'm abt to start testosterone anyways? (also-- are there any conditions that just cause androgenisation? Bc I don't have any of the other symptoms of pcos)
Hi there! I’ve sorted this ask into sections for organization and easier reading. Since this regards whether being intersex or not, I will make it clear here and several times within the post that I am very inclusive in what intersex is.
Are you intersex?
Immediately, I’d say yes, you are, fullstop. Hyperandrogenism is an inherently intersex condition (which is an opinion of mine that I believe is true). There is definitely a vocal minority of intersex (and especially perisex people too) who think that you need more “qualifications” to be intersex. However, I don’t think that to be true. There is a large number of people in the intersex community who will welcome and accept you as you are and understand and truly see you as another intersex individual. To those who don’t agree, ignore them the best you can.
I also saw that you mentioned that it’s not something you can self-diagnose which can be true, but one does not necessarily have to go through medical processes to figure out you’re intersex. It’s okay if you decide you aren’t inherently intersex because of your hyperandrogenism or that you don’t want to label that way, but you are absolutely welcome to. If you feel like something additional might make you count as intersex,
Many individuals learn they’re intersex without having gone through any diagnoses or hidden altering of their body by medical professionals and find out on their own time throughout their own life. For example, if someone had ovotestes with a formed vagina and penis, but this was missed throughout their life and they grew up as and were raised as female, they might one day begin to question if they are perisex or intersex, and it would be completely fair of them to decide being intersex describes their life experience without going to a doctor who can test to see if they have ovotestes.
How are you intersex?
You are experiencing hyperandrogenism, which is an intersex condition of excess androgen hormones. This leads to increased “masculinization” of the body based on traditional views of masculinization vs feminiziation. This is a condition that does not need a diagnosis to know that one has. Hyperandrogenism is not to be confused with the mazculinizing effects of testosterone HRT as many trans+ individuals who go on testosterone HRT develop features that those born with hyperandrogenism already developed without it.
Potential diagnoses
I see that you mentioned LOCAH in your second ask, which is a great start. Before you sent that, I was going to say you could potentially have NCAH/LOCAH as my main recommendation. If you’ve done your own research, you might know this already, but I’m going to explain again just in case.
CAH stands for congenital adrenal hyperplasia and it is a group of genetic disorders affecting the adrenal glands. Adrenal glands control cortisol, mineralocorticoids, and androgens. CAH is split into two categories–classical and nonclassic(al).
The chances of you having classical CAH are extremely low as it can be life threatening and is almost always diagnosed at birth. Classical CAH (usually just referred to as CAH) is split into salt-wasting CAH and simple-virilizing CAH/non-salt wasting CAH, the latter often being less deadly. Both of these produce too little cortisol and produce extra androgen. Salt-wasting CAH has an extremely low aldosterone count, which is necessary for processing sodium, hence “salt-wasting”. Non salt-wasting CAH is like salt-wasting CAH but with a less severe aldosterone count.
The symptoms of classical CAH include but are not limited to:
Ambiguous genitalia for those who were assigned female at birth (often with genitalia looking like a penis but having internal female sex organs)/clitoromegaly
Larger penis at birth for those were assigned male at birth
Premature puberty
Androgenization/masculinzation of those who were assigned female at birth (like the things you described, deeper voice, facial hair)
Infertility
Benign tumors
Nonclassic/nonclassical CAH, or NCAH, is a far more likely candidate. NCAH is also less commonly known as LOCAH, the “LO” standing for late onset. The symptoms of NCAH include but are not limited to:
Ambiguous genitalia for those who were assigned female at birth(less frequent and severe than classical)/developed clitoromegaly
Early puberty
Androgenization/masculinzation of those who were assigned female at birth especially during and after puberty
Larger penis with smaller testicles in those who were assigned male at birth
Irregular periods
Infertility
Hormonal disorders/issues with individuals with NCAH are significantly lower but not insignificant. Those with NCAH often have issues with the synthesis of hormones like cortisol that are associated with the adrenal gland are often asymptomatic or unrecognized in tests.
It’s totally possible you could have another intersex condition, or not this at all. Regardless of why you experience hyperandrogenism, you do, and that alone makes you intersex.
You could also have PCOS. Ironically, you can have PCOS without having cysts. Symptoms of PCOS include:
Hyperandrogenism
Irregular periods
Large ovaries
Cysts on ovaries
Clitoromegaly
Skin tags
Hyperandrogenism can be a symptom of an adrenal gland disorder, those of which include but are not limited to:
Cushing’s syndrome
Addison’s disease
Adrenal gland tumors
CAH
Adrenal gland cancer
Pheochromocytoma
Diagnosis advice and testing/screening
Whether or not seeking a diagnosis is worth it is up to you. Because you have to outward health concerns because of your hyperandrogenism, it can be hard to qualify for testing. Being diagnosed with an intersex condition can lead to medical mistreatment, malpractice, and abuse, as well as difficulty in transitioning. I don’t want to say what you should do because I don’t want you to make your decision based off of anyone but yourself.
It can be difficult to test for NCAH once you have gone on HRT as tests for NCAH are usually done via checking the hormone levels in your body. I was actually in a nearly identical situation to yours when I was questioning if I was intersex, so I totally relate to you on pretty much everything! I was already on T by the time I was questioning if I was intersex, which meant testing would involve me going off of T (which triggers my dysphoria) and could be difficult because of the effects T had on my body.
Based on my knowledge, there IS a genetic test for NCAH, but I’m not sure how easy it is to get. If you want to be screened for NCAH, ask your doctor about it.
You could also be screened for PCOS, but the screening for PCOS can be very dysphoria inducing if things regarding your genitals or genitalia being inspected triggers that if you have dysphoria, as well as the fact that many gynecologists aren’t trans+ friendly or intersex friendly. Gynecologists can also be tough because many gynecologists aren’t required or refuse to give patients things that reduce pain during procedures or inspections. It can be tough to find one, but don’t be discouraged!
Going on HRT
Any trans+ patients starting testosterone should be starting with microdosing and have various things in their blood checked before they start HRT (things such as red blood cell count, bone density, testosterone count), etc. After you start, especially since you have hyperandrogenism, it’s really important to have your blood drawn at least once a month to check various levels. (Or modified based on doctor recommendation.) Starting HRT must be closely monitored in order to know and ensure your body is healthy and to figure out if you should increase or decrease a T dosage.
When I started T HRT, my testosterone wasn’t checked before hand or the records of it were inaccessible to my doctors, so I went from having an above average T count for a person who was assigned female at birth to a person with a T count ABOVE the average for cis men regardless of body size. And you must consider I am a tiny person (I was 4’11 and ~95 lbs at the time). My doctors ALSO thought I was dying, haha. They called all freaked out! Turns out I was fine.
Trans+ health doctors don’t usually think to check for potential intersex conditions that could affect HRT in my experience.
Make sure you advocate for yourself during your transition. It can be difficut but it is necessary!
Final notes
I saw you mentioned that you’ve been IDing as transmasc and the phrasing sorta makes it sound like you’ve been questioning that, so just in case–if you’re are questioning if you’re transmasc or not because you’re potentially intersex, you can still be transmasc! Generally speaking, transmasc is used to be synonymous with FTM and means someone who was assigned female at birth and then later identifies as/realizes they’re masculine-aligned or male*. I’d also like to say just, gender wise, label wise, you can do whatever you want, always. It doesn’t matter what people think. If not, ignore me and my little soapbox because I just wanted to make sure you know that!
And thank you for the kind words about this blog, I hope I can reach more and more intersex people on Tumblr and help as many people out as I can. And don't worry about "spamming", you didn't spam but even if you did I love spam so no worries. If you want to chat further you can DM me on here or on my Discord (which I can give via DM or via an ask off of anonymous and then I'll answer you privately)
If you have any other thoughts, questions, comments, concerns, etc., please let me know! Even if it’s just that this helped! I love getting to answer asks and help people out.
If I accidentally skimmed past any of your questions or concerns, let me know and I’ll edit this post to include any information.
And to anyone, if you see any false information, typos, grammar mistakes, formatting issues, etc., please let me know and I will change it.
*I’d like to make it clear that I fully support people who use this term otherwise. There is a significant number of intersex people who identify as transmasc because it describes part of their experience even if they were assigned female at birth. The terms transmasc/fem/neu(tral), FTM, MTF, FTNB, and MTNB are often used differently or used in a way that doesn’t fit the traditional expectations of many other queer people by groups such as: intersex people, bigender, multigender people, genderfluid people, genderflux people, genderqueer people, genderfucked people, and more. I absolutely support genderfuckery but also acknowledge that understanding of the term in how it’s usually used is necessary for understanding many individuals or conversations when the term is used.
14 notes
·
View notes
Text
Hot Schrödinger Cat States: High-Temp Quantum Superpositions
Hot Schrödinger cat states are quantum superposition states formed from thermally stimulated beginning states, not cooled systems. Schrödinger cat states are usually shown experimentally as 'cold' states, which start with a pure vacuum Fock state formed by cooling the system to its ground state.
A more detailed explanation:
Schrödinger's original thought experiment showed a cat, a macroscopic, out-of-equilibrium system at body temperature, in a superposition of two classical fluctuations-dominated mixed states. The “hot” Schrödinger cat states developed in this work are closer to the original notion since they are formed from mixed thermal states.
Motivation: Hot Schrödinger cat states arise from the difficulties of ground-state cooling for continuous-variable quantum systems like levitated particles and nanomechanical oscillators. These systems obtain long coherence periods but struggle to reach their quantum ground state. The capacity to develop and analyse quantum events like superposition in thermally excited states opens new doors for these systems.
Method of Prep: Using just unitary interactions with a transmon qubit, researchers developed microwave cavity hot cat states. Two famous “cold” cat state protocols from circuit quantum electrodynamics (cQED) were modified: echoing conditional displacement (ECD) and qcMAP. The process involves:
Equilibrate the cavity mode and commence thermally using a heat bath. Initial states with purity as low as 0.06 had a cavity mode temperature of up to 1.8 Kelvin, substantially hotter than the physical surroundings.
Applying modified ECD and qcMAP protocols to the transmon qubit to create a quantum superposition of displaced heat states.
Calculating “hot” Schrödinger cat states’ Wigner functions.
Key Findings and Features:
The hot Schrödinger cat states revealed Wigner-negative interference patterns for all starting thermal states, demonstrating their nonclassical character while being substantially mixed.
ECD and qcMAP performed differently in warm beginning states than in cold animals.
The ECD state's Wigner function showed an interference pattern with an envelope that expanded in radius and shrunk in amplitude as the thermal excitation number (nth) increased, like the displaced thermal states.
The qcMAP state's Wigner function interference pattern decreased in amplitude more slowly than the displaced thermal states, but its envelope shortened as nth rose.
Quantum superposition forms coherence through unitary processes, as seen by the extra peak in the prepared states' coherence functions.
In ideal conditions, the thermal occupancy number should not impact the contrast of the marginal distribution interference fringes, according to theoretical analysis.
Quantum technology implications: Generating and characterising hot Schrödinger cat states has several implications.
Quantum technologies and research on more physical systems require less cooling.
Noise-tolerant quantum protocols are possible due to quantum properties in heavily mixed systems.
Bosonic qubit encoding innovations, notably the qcMAP protocol, which has saturated parity values at finite mode temperatures.
Saturated parity allows quantum metrology at lower temperatures.
Better understanding of thermal noise's effect on quantum coherence.
Inspiration for high-temperature quantum control approaches.
This study proves quantum superposition is not restricted to low temperatures. Using unitary protocols, quantum features may be created and monitored in states with strong thermal excitation, expanding quantum technology.
In brief
In this Science Advances work, experimenters produce and assess “hot” Schrödinger cat states quantum superpositions from mixed heat states instead of pure ground states. The researchers created these very mixed quantum states in a microwave cavity with starting purities as low as 0.06 using unitary interactions with a transmon qubit.
Although impure, these hot cat states revealed quantum properties including Wigner-negative interference patterns, proving that quantum events may be observed without particularly pure initial states. The study also compared echoing conditional displacement (ECD) and qcMAP preparation methods for continuous-variable quantum systems where ground-state cooling is problematic and found different outcomes in thermal states.
What's quantum state?
Quantum physics defines a quantum state as a mathematical object that embodies quantum system knowledge. Quantum mechanics describes quantum state generation, development, and measurement. A state-represented system prediction is the result. Knowledge of a quantum system's quantum state and temporal evolution rules is all that can be learnt.
The system or issue may define quantum states differently.
#technology#technews#govindhtech#news#technologynews#hot Schrödinger cat states#Hot Schrödinger#quantum superposition#quantum state#Schrödinger#quantum
0 notes