#NaviHealth
Explore tagged Tumblr posts
Text
Laser Treatment for Varicose Veins Procedure - Anesthesia
Laser Treatment for Varicose Veins procedure: Navi Health Care, your well-being is our topmost priority. Our commitment to advanced medical solutions includes specialized treatments such as laser treatment for varicose veins. We believe that empowering you with comprehensive insights into this procedure is important. Understanding its procedure not only relieves worries but also empowers you to make informed decisions regarding your health journey. We aim to provide not just a treatment, but a pathway to informed choices and improved well-being.
Step 1: Preparation
Before your treatment at Navi Health Care, our team will give you clear instructions to prepare. They might suggest avoiding some medicines or certain foods before your appointment. These instructions are important to make sure everything goes smoothly during your procedure. Following these guidelines helps us ensure your safety and the success of your treatment. Our goal is to help you feel comfortable and ready for your procedure, so you can get the best possible care.
Step 2: Anesthesia
During the laser treatment for varicose veins procedure – Anesthesia plays a key role. We use local anesthesia to numb the treatment area, ensuring you feel no discomfort. Our experienced anesthetists specialize in this, focusing on your comfort throughout the procedure. They are dedicated to making sure you feel at ease during the laser treatment for varicose veins, using their expertise in anesthesia to keep you pain-free and relaxed.
Step 3: Insertion
During the laser treatment, a tiny cut is made to put a thin laser fiber into the vein that needs treatment. This step is careful and does not cause much disruption. It is done in a way that reduces any discomfort and lowers the chance of marks on your skin. Our expert healthcare team handles this part very gently and precisely. They are trained to do this in a way that is as gentle as possible, ensuring you feel as comfortable as can be during the laser treatment for varicose veins procedure – Insertion Laser Fiber.
Step 4: Laser Energy Application
After putting the thin fiber in place, a special kind of strong light called laser energy is sent through it. This light warms up the walls of the vein, making it close and seal on its own. This part is important, and we use modern technology to ensure it is done precisely and safely. Our advanced tools help us direct the energy exactly where it is needed, ensuring accuracy and safety during the laser treatment for varicose veins procedure – Laser Energy Application.
Step 5: Closure of Vein
After sealing the vein during the laser treatment for varicose veins procedure – Closure of Vein, blood starts flowing through healthier nearby veins. Gradually, the treated vein gets absorbed by your body, making varicose veins less visible. Our team keeps an eye on how you are doing after the treatment to make sure you are healing well. Monitoring your progress is crucial to ensure everything is going as it should post-procedure, aiding in optimal recovery from the laser treatment.
Why Choose Navi Health Care for Laser Treatment for Varicose Veins?
Navi Health Care stands out for its patient-centric approach and state-of-the-art facilities. Here is why our laser treatment for varicose veins stands apart:
• Expertise:
Our medical team knows a lot about doing small surgeries that do not need big cuts. Like the laser treatment for varicose veins, they are good at it because they have done it many times before.They are experts in making these treatments smooth and easy for you.
• Advanced Technology:
We use the newest and best laser machines. These machines are super modern and safe. They help us give you treatments that work well and are safe for you. So, you can trust that you are getting the most up-to-date and good treatments.
• Personalized Care:
We care a lot about how you feel while you are with us. Our team wants you to be happy and comfortable. That is why we pay attention to what you need and make sure you feel good every step of the way. We listen to your worries and take care of you like your family.
Conclusion
At Navi Health Care, our laser treatment for varicose veins procedure offers a safe and efficient solution for this common condition. With meticulous attention to detail and a patient-first approach, we aim to provide you with the best possible outcomes.
If you are considering laser treatment for varicose veins, Navi Health Care is here to guide you through the process. Contact us to schedule a consultation and take a step towards healthier veins and a healthier you.
#navihealthcare#NaviHealth#vericosveine#vericoseveintretment#vericoseveinsurgery#vericoseveintreatmentsnearme#thebesttreatmentforvericosevein#Gallbladderstone#GallbladderStones#gallbladderstonetreatment#Circumcision#Circumcisionsurgery
0 notes
Text
UnitedHealth: AI In the Way
UnitedHealth, the largest health insurance company in the US, is facing serious allegations over AI in their decision-making process. A lawsuit filed in the US District Court in Minnesota claims that use of a flawed AI algorithm that allegedly overrides doctors’ judgments has led to patients being prematurely removed from rehabilitation programs, forcing them to deplete their life savings for…

View On WordPress
0 notes
Text
Hitler had a family too.
The sympathization over killer-turning-victim, and what we learned from the recent CEO’s shooting in NYC.
Brian Thompson’s two teenage sons and widow are the latest addition to the grieving sea of people surrounding his name, but ironically the only ones who joined it after his death.
Thanks to his fruitful career path of being a healthcare bouncer, thousands of sick people’s coverage claims got denied, resulting in the deaths of at least 2 people.
His major in-office accomplishment is arguably the AI algorithm used to simplify the approval or denial process of insurance claims. More specifically, “the investigation, cited by the lawsuit, found UnitedHealth pressured medical employees to follow an algorithm, which predicts a patient’s length of stay, to issue payment denials to people with Medicare Advantage plans. Internal documents revealed that managers within the company set a goal for clinical employees to keep patients rehab stays within 1% of the days projected by the algorithm.”
The lawsuit, filed in the U.S. District Court of Minnesota, accuses UnitedHealth and its subsidiary, NaviHealth, of using the computer algorithm to “systematically deny claims” of Medicare beneficiaries struggling to recover from debilitating illnesses in nursing homes.
The reality of the matter is that although the shooter, Luigi Mangione, assumed the role of the judge and executioner, Brian Thompson was appointed to play the role of God. And only one of those situations is illegal.
It’s frankly really enticing to add that only one of these situations is morally reprehensible, but this is not true.
“Vigilante justice is fault proof” is not a hill most of us want to die on. Personal acts of violence can never equate to the judicial system, nor do they claim to most of the time. What they have in common, however, is the perpetrator’s objective goal for his initiative to incite a change for the better.
The proposed takeaway from this is the symbolic perception of Mangione’s act, as a telltale of greed, class war and injustice.
Immediately upon news were released, a hope for the class movement was born while a shiver run down the 1%’s spine.
The poor did not rejoice that a man is dead, though they most certainly cheered at the symbolized slaughter of Healthcare Inc.
The opportunity for this incident to awake class consciousness among the lower ranks must not be stifled by the mourning of human life.
Just because monsters die like humans doesn’t mean we have to mourn them.

#deny defend depose#luigi mangione#nyc ceo shooting#brian thompson#united healthcare#the great awakening#uhc ceo#ceo information#delay deny depose#healthcare
14 notes
·
View notes
Quote
You've doubtless seen the outpourings of sarcastic graveyard humor about Thompson's murder. People hate Unitedhealthcare, for good reason, because he personally decided – or approved – countless policies that killed people by cheating them until they died. Nurses and doctors hate Thompson and United. United kills people, for money. During the most acute phase of the pandemic, the company charged the US government $11,000 for each $8 covid test: https://pluralistic.net/2020/09/06/137300-pct-markup/#137300-pct-markup UHC leads the nation in claims denials, with a denial rate of 32% (!!). If you want to understand how the US can spend 20% of its GDP and get the worst health outcomes in the world, just connect the dots between those two facts: the largest health insurer in human history charges the government a 183,300% markup on covid tests and also denies a third of its claims. UHC is a vertically integrated, murdering health profiteer. They bought Optum, the largest pharmacy benefit manager ("A spreadsheet with political power" -Matt Stoller) in the country. Then they starved Optum of IT investment in order to give more money to their shareholders. Then Optum was hacked by ransomware gang and no one could get their prescriptions for weeks. This killed people: https://www.economicliberties.us/press-release/malicious-threat-actor-accesses-unitedhealth-groups-monopolistic-data-exchange-harming-patients-and-pharmacists/# The irony is, Optum is terrible even when it's not hacked. The purpose of Optum is to make you pay more for pharmaceuticals. If that's more than you can afford, you die. Optum – that is, UHC – kills people: https://pluralistic.net/2024/09/23/shield-of-boringness/#some-men-rob-you-with-a-fountain-pen Optum isn't the only murderous UHC division. Take Navihealth, an algorithm that United uses to kick people out of their hospital beds even if they're so frail, sick or injured they can't stand or walk. Doctors and nurses routinely watch their gravely ill patients get thrown out of their hospitals. Many die. UHC kills them, for money: https://prospect.org/health/2024-08-16-steward-bankruptcy-physicians-private-equity/ The patients murdered by Navihealth are on Medicare Advantage. Medicare is the public health care system the USA extends to old people. Medicare Advantage is a privatized system you can swap your Medicare coverage for, and UHC leads the country in Medicare Advantage, blitzing seniors with deceptive ads that trick them into signing up for UHC Medicare Advantage. Seniors who do this lose access to their doctors and specialists, have to pay hundreds or thousands of dollars for their medication, and get hit with $400 surprise bills to use the "free" ambulance service: https://prospect.org/health/2024-12-05-manhattan-medicare-murder-mystery/
Pluralistic: Predicting the present (09 Dec 2024) – Pluralistic: Daily links from Cory Doctorow
8 notes
·
View notes
Quote
看護師や医師たちもトンプソンとUnitedを憎んでいる。Unitedは金のために人を殺す。パンデミックの最も深刻な時期、同社は政府に8ドルのコロナ検査を1万1000ドルで請求した。 https://pluralistic.net/2020/09/06/137300-pct-markup/#137300-pct-markup UHCは保険金支払い拒否率32%(!!)で全米をリードしている。米国がGDPの20%を費やしながら、世界で最悪の医療しか得られない理由を理解したいなら、この二つの事実を結びつければいい。人類史上最大の医療保険会社が、政府にコロナ検査を183,300%の上乗せ価格で請求し、そして請求の3分の1を拒否しているのだ。 UHCは垂直統合型の、殺人的な医療利益追求企業である。彼らは米国最大の薬剤給付管理会社(「政治的な力を持ったスプレッドシート」――マット・ストラー)であるOptum(オプタム)を買収した。そしてOptumへのIT投資を絞り、浮かせた資金を株主に回した。その結果、Optumはランサムウェアギャングにハッキングされ、何週間も処方箋が受け取れない事態に陥った。これによって命を落とした人々がいる。 https://www.economicliberties.us/press-release/malicious-threat-actor-accesses-unitedhealth-groups-monopolistic-data-exchange-harming-patients-and-pharmacists/# 皮肉なことに、Optumはハッキングされていなくても十分にひどかった。Optumの目的は、より高額な医薬品を購入させることにあった。それが支払えないなら、死ぬ。Optum――つまりUHC――は人を殺してきた。 https://pluralistic.net/2024/09/23/shield-of-boringness/#some-men-rob-you-with-a-fountain-pen OptumはUHCの殺人部門の一つに過ぎない。Navihealth(ナビヘルス)もそうだ。これはUnitedが使用するアルゴリズムで、立つことも歩くこともできないほどの病人や怪我人を病院のベッドから追い出すためのものである。医師や看護師は、重篤な患者が病院から追い出されるのを日常的に目にしてきた。たくさんの人が死んだ。UHCは金のために彼らを殺したのだ。 https://prospect.org/health/2024-08-16-steward-bankruptcy-physicians-private-equity Navihealthによって殺された患者たちは、Medicare Advantageに加入していた。Medicareは米国が高齢者に提供する公的医療制度だが、Medicare AdvantageはMedicareに承認された民間企業のプランで、UHCはこの分���でも全米をリードしている。まぎらわしい広告を大量に流して高齢者をだまし、UHCのMedicare Advantageに加入させてきた。加入した高齢者たちは、かかりつけ医や専門医にかかれなくなり、薬代で数百、数千ドルを支払わなければならず、「無料」のはずの救急車サービスに400ドルを請求されることになった。 https://prospect.org/health/2024-12-05-manhattan-medicare-murder-mystery 通常のMedicareよりも、Medicare Advantageに公的資金が22%多く投入されているのも、なんら不思議ではない。 https://theconversation.com/taxpayers-spend-22-more-per-patient-to-support-medicare-advantage-the-private-alternative-to-medicare-that-promised-to-cost-less-241997 高齢者だけではない。依存症患者やメンタルヘルスの問題を抱える人々も同様だ。UHCは精神疾患や薬物依存の治療の保険適用を違法に拒否している。給料から数千ドルの保険料が天引きされているのに、健康保険会社が治療を拒否したせいで、家族が手に負えなくなり、過剰摂取で命を落とし、あるいは幻覚に苦しみながらホームレスになっていく様を見させられている。 https://www.startribune.com/unitedhealthcare-will-pay-15-7m-in-settlement-of-denial-of-care-charges/600087607 当然のことながら、UHC内部の企業文化は想像を絶するほどに冷酷だ。そうでなきゃ、こんな仕事できるはずがない。人を殺すことになる仕事を続けるのなら、犠牲者たちを非人間化するしかない。UHCの治療拒否を訴えた慢性疾患患者の訴訟で、UHC従業員たちの通話音声が明らかになった。拒否された請求を大声で笑い、患者の涙ながらの必死の嘆願を「かんしゃく」だと一蹴する通話音声だった。 https://www.propublica.org/article/unitedhealth-healthcare-insurance-denial-ulcerative-colitis もちろん、UHC従業員たちは自分の生活のために働いているだけだ。そしてその仕事を続けるために身につけた冷酷さは、先週の殺人事件で剥がれ落ちた。UHCの幹部たちもそれを理解しているようで、従業員たちが自身の恐ろしい体験を外部に話すことを阻止しようと躍起になっている。トンプソンの死に関する社内アナウンスを1万6000人の従業員が見たにもかかわらず、コメントを残したのはわずか28人だったという事実についてさえ言及を禁じている。 https://www.kenklippenstein.com/p/unitedhealthcare-tells-employees 医師や看護師たちは患者を思ってUHCを憎んでいるが、加えて個人的な理由もある。UHCは支払いを拒否し、何ヶ月も、時には何年も支払いを遅らせてクリニックを苦しめ、支払いが滞っている期間の生活を支えるためにペイデイ(給���担保)ローンを提案してきたのだ。 https://www.youtube.com/watch?v=frr4wuvAB6U 410億ドルの企業を率い、これらすべてを実行した年収1000万ドルのCEOの暗殺について、Redditの看護師フォーラムでは冷淡で、満足げな冗談が溢れている。驚くようなことだろうか。 https://www.thedailybeast.com/leading-medical-subreddit-deletes-thread-on-unitedhealthcare-ceos-murder-after-users-slam-his-record 路上で誰かが殺害されたとき、それがどのような人物であろうと、シャーデンフロイデ(訳注:他人の不幸や失敗を喜ぶ感情、メシウマ)を感じたり、ましてやそれを表現することはよしとはされない。政治的暴力には恐怖を表明すべきだとされる。たとえその暴力が、トンプソンの指揮下でUHCが生み出した死者数のほんの一部にすぎない、たった一人の命しか奪っていない場合でも。マルコム・ハリスが述べたように、「保険適用の拒否で知られる医療保険会社のCEOについて『すべての命は尊い』などと言う物言いは、実に馬鹿げている」。 https://twitter.com/BigMeanInternet/status/1864471932386623753 ウディ・ガスリーが書いたように、「ある者は拳銃で奪い/ある者は万年筆で奪う」。凶器が拳銃か保険会社であったなら、致命的である。保険会社は単に責任の空洞化(accountability sink)、つまり誰もが直接的な殺人者になることなく人を殺す間接的なレイヤとして機能しているにすぎない。 https://profilebooks.com/work/the-unaccountability-machine 保険会社の幹部が殺されてほしいとは思わないし、保険会社の幹部に人々を殺してほしくもない。だが、この事件が起きたことに驚きはない。むしろ、これほど時間がかかったことに驚いている。人を激怒させる組織を運営していれば、やがて人々はあなたに怒りを向けるようになる――それは当然のことだ。トマス・ピケティの『21世紀の資本』の主張そのものだ。富の集中は腐敗につながり、それは不安定化を招く。長い目で見れば、自宅の芝生にギロチンを設置させないように警備員を雇うよりも、公正な社会を運営する方が安上がりなのだ。
現在を「予言」すること――医療保険大手CEOの殺害はなぜ喜ばれたのか » p2ptk[.]org
4 notes
·
View notes
Text
holy fuck
if you/someone you know use UHC, makes sure whoever pays for your/their healthcare - you/them, a spouse, family, whatever - knows about this because to quote a content creator i follow called liv pearsall, "what in, and i do not say this lightly, fresh hell"
also, if you're like me (in my case it's autism but it could be something else for you) and struggle with understand big, fancy words (like the article) i ran the article through this informalizer to make a more simple version. it's under the cut! :)
Yo, so here's the deal. UnitedHealthcare, the biggest health insurance company in the US, is supposedly using this totally messed up AI algorithm to screw over old folks and deny them the coverage they really need. It's a total mess. These elderly patients are getting booted out of rehab and care facilities way too early, and they're being forced to drain their savings just to get the care that should be covered by their Medicare Advantage Plan.
And get this, someone actually filed a lawsuit about it. It's going down in the US District Court for the District of Minnesota. The lawsuit is all about how UnitedHealth denied health coverage to two people who eventually died. But it's not just about them — there could be thousands of other people in similar situations.
This lawsuit lines up with an investigation by Stat News that basically supports all the claims. Stat got their hands on internal documents and talked to former employees of NaviHealth, which is a subsidiary of UnitedHealth that created this messed up AI algorithm called nH Predict.
One former employee, Amber Lynch, spilled the tea to Stat. She used to work for NaviHealth and said that the whole company cared more about money than actually helping patients. She hated how they treated patients like data points instead of human beings.
Here's the deal with nH Predict. It started being used by UnitedHealth back in November 2019, and they're still using it. Basically, this algorithm tries to guess how much care a patient on Medicare Advantage will need after they have, like, a big injury or illness. Stuff like therapy and skilled care in hospitals and nursing homes.
No one really knows how nH Predict works exactly, but it apparently takes info from a database with cases from 6 million patients. The case managers at NaviHealth put in some details about a patient, like age and living situation, and the algorithm spits out estimates based on similar patients in the database. It tries to figure out stuff like how long the patient will need care and when they can be discharged.
But here's the problem — the algorithm doesn't take a bunch of important factors into account, like other medical issues the patient might have or if they catch something like pneumonia or COVID-19 during their stay. It's a mess.
According to the investigation and the lawsuit, the estimates the algorithm gives are usually way off. With nH Predict, patients are hardly ever getting the full 100 days of covered care they're supposed to get in a nursing home. Usually, they only get like 14 days before UnitedHealth denies payment.
And get this, when patients or their doctors ask to see the algorithm's reports, UnitedHealth just says no and claims it's top secret. And if the doctors try to disagree with UnitedHealth's decision, tough luck. UnitedHealth just overrides them.
This whole thing is messed up, but sadly it's not the first time the healthcare industry has screwed up with AI. They've been doing this racist algorithm stuff for a while now. But what makes this situation even worse is that it seems like UnitedHealth is deliberately denying coverage to save money.
Ever since UnitedHealth bought NaviHealth, former employees say the company cares more about hitting targets and making post-acute care as short and cheap as possible. They even have requirements for case managers to follow the algorithm's predictions. If they don't, they could get in trouble or even lose their jobs.
Apparently, case managers are trained to defend the algorithm's estimates to patients and their caregivers. They use all these tactics to shut down any objections. Like, if a nursing home doesn't want to let a patient leave, the case manager will say the patient doesn't need certain care because of some calorie rule. It's like they don't even care about the patients.
And even if patients manage to win an appeal and get the denial overturned, UnitedHealth just comes right back with another denial a few days later. It's a never-ending cycle.
The lawsuit is fighting back against UnitedHealth and NaviHealth for all this shady behavior. They're accusing them of breaking contracts, not acting in good faith, unfairly getting rich, and violating insurance laws in a bunch of states. They want damages, emotional distress compensation, and for UnitedHealth to stop using the AI-based claims denials.
We don't know exactly how much money UnitedHealth saves with nH Predict, but it's gotta be a crazy amount. Last year, the CEO made almost $21 million, and other execs made millions too.
In the end, it's just a messed up situation. These elderly people are getting screwed over by an AI algorithm that values money over their health. It's not cool, and something needs to change.
UnitedHealthcare, the largest health insurance company in the US, is allegedly using a deeply flawed AI algorithm to override doctors' judgments and wrongfully deny critical health coverage to elderly patients. This has resulted in patients being kicked out of rehabilitation programs and care facilities far too early, forcing them to drain their life savings to obtain needed care that should be covered under their government-funded Medicare Advantage Plan.
It's not just flawed, it's flawed in UnitedHealthcare's favor.
That's not a flaw... that's fraud.
53K notes
·
View notes
Quote
UnitedHealth, Humana and Cigna are facing class-action lawsuits alleging the insurers relied upon algorithms to deny lifesaving care. One of the lawsuits alleges that Cigna denied more than 300,000 claims in a two-month period, which amounts to about 1.2 seconds for each physician-reviewed claim. Such a practice is aided by algorithms, the lawsuit said. In 2020, UnitedHealth Group acquired naviHealth and its algorithm for predicting care, called nH Predict, which UnitedHealth uses and also contracts out to other insurers, including Humana. (A spokesperson for UnitedHealth Group denied that the algorithm is used to make coverage decisions; Humana did not respond to a request for comment.) The lawsuit against them alleged that nH Predict has a 90% error rate, meaning nine out of 10 denials are reversed upon appeal – but that vanishingly few patients (about 0.2%) appeal their denied claims, leading them to pay bills out of pocket or forgo necessary treatment.
New AI tool counters health insurance denials decided by automated algorithms | US healthcare | The Guardian
0 notes
Text

As one of the nation’s largest health insurers, covering more than 50 million people, UnitedHealthcare has battled a range of complaints and investigations from patients, doctors and lawmakers for its denial of medical claims.
Those practices may face new scrutiny after law enforcement officials said that the bullet casings found at the site of the killing of the UnitedHealthcare chief executive Brian Thompson on Wednesday appeared to have messages, including the words “deny” and “delay,” written on them. The shooter’s motive and identity still remained unknown on Thursday, and no evidence has emerged that the killer was a UnitedHealthcare customer.
While the words “deny” and “delay” have multiple meanings, they could be a reference to the tactics used by insurers of all kinds to avoid paying claims. The words are so linked to those practices that they were used in the title of a 2010 book probing them, “Delay, Deny, Defend: Why Insurance Companies Don’t Pay Claims and What You Can Do About It.”
“An insurance company’s greatest expense is what it pays out in claims,” wrote the book’s author, Jay Feinman, an emeritus professor at Rutgers. “If it pays out less in claims, it keeps more in profits.”
No one knows how often private insurers like UnitedHealthcare deny claims because they are generally not required to publish that data. People who bought coverage under Obamacare, a government-funded plan, had 17 percent of their care denied in 2021, according to KFF, a health policy group. Other surveys have found that denials are more prevalent among those with private insurance than those who carried government coverage.
UnitedHealthcare, part of the giant conglomerate UnitedHealth Group, reported more than $16 billion in operating profits last year and employed roughly 140,000 people. The company is a frequent lightning rod for criticism over how it handles claims.
Earlier this year, a Senate committee investigated Medicare Advantage plans denying nursing care to patients who were recovering from falls and strokes. It concluded that three major companies — UnitedHealthcare, Humana and CVS, which owns Aetna — were intentionally denying claims for this expensive care to increase profits. UnitedHealthcare, the report noted, denied requests for such nursing stays three times more often than it did for other services. (Humana had an even higher figure, denying at a rate 16 times higher.)
UnitedHealthcare did not respond to a request for comment about its history of claim denial.
Journalists have also scrutinized United’s denial practices. In January, the health news outlet Stat published a detailed investigation into how a UnitedHealthcare subsidiary, NaviHealth, used algorithms to deny care for seniors enrolled in the company’s Medicare advantage plan.
The Stat investigation noted specific instances that troubled United employees, like when an older woman who had a stroke was only covered for half the nursing days typically required for recovery.
UnitedHealthcare and its parent company now face a class-action lawsuit over its use of the algorithm. In response to the Stat article, the company issued a statement that “the assertions that NaviHealth uses or incentivizes employees to use a tool to deny care are false.”
A 2023 story from ProPublica dived deep into the experience of one United patient, a college student who racked up $2 million in medical claims a year to treat a severe case of ulcerative colitis. The story showed United disregarding an internal report finding the expensive treatment to be necessary. The patient eventually sued United and received an undisclosed amount in a settlement.
Insurance denials are rarely appealed, with some studies finding appeal rates of roughly 1 percent.
UnitedHealthcare, in response to the ProPublica story, said that the patient took his medication at dosages that “far exceed” Food and Drug Administration guidelines, which led the insurer to “review treatment plans based on current clinical guidelines to help ensure patient safety.”
Since the news of Mr. Thompson’s death on Wednesday, some individuals on social media have expressed frustration over the company’s history of denying claims. Others have gone even further, celebrating the death of a top insurance executive.
The insurance industry has pushed back against the outrage. “The people in our industry are mission-driven professionals working to make coverage and care as affordable as possible and to help people navigate the complex medical system,” said Michael Tuffin, the president of AHIP, a major trade group, on LinkedIn. “We condemn any suggestion that threats against our colleagues — or anyone else in our country — are ever acceptable.”
https://www.nytimes.com/live/2024/12/05/nyregion/brian-thompson-unitedhealthcare-news
0 notes
Text
The Massive UnitedHealth Hack Is Obamacare’s Fault and That’s No Lie
The following content is sponsored by Americans for Limited Government.
Remember that moment 15 years ago when then President Barack Obama promised that his plan for socialized medicine would not extend to illegal aliens, and Rep. Joe Wilson yelled out, “You lie!” Remember how Democrats and their media enablers all denounced Wilson both for his lack of decorum and for lying himself?
Wilson was wrong at the time. Not about calling out Obama for lying about Democrats’ plan to steal taxpayer money to give to their future voters; he was wrong to not say “You lie!” at every line that came out of Obama’s mouth. Even NPR gave Obama the “Lie of the Year” award in 2013 over Obamacare, and NPR only employs Democrats.
The ridiculously named Affordable Care Act (ACA) turns 15 years old next March. It is the crowning example of the Democrats saying that they just! want! to! help! people! but passing power grabs that only help themselves. Obama even found a way to twist the pejorative “Obamacare” into the catch-phrase, “Yes, Obama cares!”
Much like pre-Team America Iraq, the ACA was promised to make hospitals across America happy places with rainbow skies and rivers made of chocolate, where children dance and laugh and play with gumdrop smiles! However, what we’ve gotten instead is incompetence, massive profits for vertically integrated insurance companies, and even AI-backed healthcare rationing.
The incompetence that guided Obamacare was on display recently when cyber hackers outsmarted UnitedHealth Group in late February. The division of UnitedHealth Group that transmits claims, Change Healthcare, was the subject of a ransomware attack, delaying payments for prescriptions, doctors, and everything else. The company performs 15 billion transactions per year, so the consequences of UnitedHealth ignoring adequate cybersecurity is proving disastrous.
(...)
It appears you can get away with quite a bit when you’re a government-backed monopoly.
One of the reasons UnitedHealth pulls in its record profits is because it rations care. The company used AI to systemically deny benefits to people through an intermediary called NaviHealth. Insurance monopolies like UnitedHealth are increasingly trying to control every step of patient care, and technology is making that easy for them. So, if you’re one of the 52 percent of Americans worried about the future of AI, don’t worry: the bad stuff is already here.
It could get worse though.
From 2019 to 2022, AARP spent more than $60 million to push a “rent seeking” provision in the Inflation Reduction Act – legislation so dishonestly named that it makes the Affordable Care Act almost sound honest. This provision allows Medicare to engage in so-called “negotiations” with pharmaceutical manufacturers over prices. The problem is that making companies an offer they can’t refuse by imposing a 95 percent tax on them if they don’t agree isn’t a negotiation at all. And AARP’s victory lap article left it unsaid how these negotiation requirements would benefit private insurers who subsidize AARP. Moreover, the IRA expands subsidies under ACA to private insurance providers, which will help pad those billion-dollar profits even more.
Free market policy advocacy group American Commitment President Phil Kerpen wrote, “Under the IRA insurers like UnitedHealth are in line for a financial windfall with super-sized subsidies for Obamacare policies and government price controls dictating pricing of many medicines.”
(...)
Obamacare is 21st century snake oil. It seems like when Obama said: “If you like your plan, you can keep it,” “This won’t cover illegal aliens,” “This won’t add a dime to the deficit,” or even “Obama cares,” what he meant was: “We will make your healthcare a badly run vertically integrated monopoly that will withhold care, enrich executives, and expose you to hackers.”
1 note
·
View note
Text
Health Is Wealth | The Path To Creating A Venture - Recruiting - hbs.edu
Rachel Sanders (MBA 2017) started her professional career working in healthcare focused investment banking. After spending four years working at Raymond James focused on middle market transactions, M&A, and the intersection of technology and business, she had a strong understanding of the opportunities to leverage technology to help people experience their healthcare in a better way. Driven by her own personal health experiences in where she constantly used a guess and check methodology to improve her health, she sought to learn how to solve health outcomes for more than just herself. “That is really the crux of why I went to HBS, and why I chose to get an MBA. I knew that I wanted to build something that would make an impact on people’s lives. “ Rachel spent her two years at HBS immersed in learning and soaking up as much information and experience as she could. “Using those two years as a time to experiment, to learn to launch something, but also to gain the skills on the operational side, and to expand my network. I was great at finance, I understood the healthcare market, but there was a lot of opportunity for learning while at HBS that I was really excited about.” RC year gave Rachel the foundation to make decisions on the fly and with little information. “If you’re operating as the Protagonist, what would you do…the case method beyond everything else really prepares you for the cold calls that you experience as a Founder, and that preparation is hard to get elsewhere.” Leveraging the HBS alumni network, Rachel secured an internship between her RC and EC years at naviHealth, Inc... a digital health company. This internship allowed her to make an impact at the organization by working on projects that shaped new product development and strategy, allowing Rachel to gain experience across strategy, product, and operations within the healthcare space. She took that experience into her EC year, where she was able to continue to build her network and flex her skills. It was in her EC year that Rachel connected with Julia Austin, senior lecturer at HBS’ Rock Center for Entrepreneurship. Rachel credits her connection with Austin as the biggest influence in her journey to becoming a Founder. Austin became a mentor, which she remains today, introducing her to “Good for Her,” a cohort of female founders, and connecting Rachel into the startup ecosystem initially. Through her relationship with Austin, Rachel connected with Alex Iskold, Coach and VC in Resident at the Arthur Rock Center for Entrepreneurship at HBS and Managing Partner at 2048 Ventures . It was Iskold who would ultimately introduce Rachel to Dr. Daniel Wallerstofer, PhD, her Co-Founder at Rootine. Launching Rootine After launching her first venture during her EC year, Rachel started experiencing stress, fatigue, and signs of burnout. She started to look at not only her nutrition, but her overall lifestyle – what she was doing for exercise and her sleep patterns – to try to improve her performance. It was during this time that she connected with Wallerstofer, who had a PhD in biotechnology and had spent the previous decade building consumer facing nutrition products based on health data, starting with genetics, and then moving into blood levels. Collectively, Rachel and Wallerstofer saw an opportunity to build a precision nutrition brand that was more data driven, science backed, and truly personalized. “We came together on this mission to empower individuals to leverage their data to achieve optimal health.” Rootine unlocks total body health through at-home lab testing, a precision multivitamin membership, in-app progress tracking, and an engaged, health-focused community. By combining science with health and wellness data, Rootine delivers a precision nutrition system that addresses each individual’s unique nutritional needs and provides real health benefits, differentiating itself from the competition. Founded as a remote-first company, Rootine was positioned well when the pandemic forced companies to move to a remote work environment. With their technology already at scale, and the pandemic highlighting the need for consumer health at home, Rootine was able to harness this momentum and launch and deliver more, allowing people to live healthier lives in a more convenient way. Female Founded & Future Focused As a female founder, Rachel educated herself on the nuances of being the minority within the startup ecosystem. “I’ve learned a lot along the way related to fundraising, and specifically what it means to be a female founder fundraising. And those learnings, are very helpful as I think about raising future funding.” As a result of her experiences, Rachel is committed to paying it forward and increasing the diversity of the startup ecosystem. “The tech startup and venture ecosystem is simply not diverse…I do my best every day, both as a leader of Rootine and everything else that I’m doing to try to make a dent in that problem.” Close to 50% of the investors in Rootine’s seed round were diverse or non-traditional investors between women, people of color, and people from Latinx communities. Across most of their business, there is a fairly equal distribution between male and female employees. “We are paying attention to and making sure that we’re getting the most diverse perspectives around the table. Research shows us that you create better outcomes when you do that.” “Looking at my angel investing and venture partner side, I believe that change will come from focusing on both sides of the table. Investing in more underrepresented founders, but also getting more non-traditional investors on cap tables. When I think about where I’m putting my small angel check dollars, it’s investing in female founders and getting females like myself on cap tables so more women have a seat at the table to voice their opinions.” The absence of women on cap tables has contributed to the gender wealth gap in the industry. “Thinking about how I can impact that on a small or large scale eventually, is something I’m constantly working on.” Hiring for a Startup Rachel advises other startups to find talent that is predisposed to solve problems and challenges. “Regardless of the role, I hire for curiosity. People that like to learn do better at a startup than people who don’t, because it inherently means there is a ton of problems that need to be solved…so the more people you bring on that can lean into problems and are curious around how to solve them, the better.” Being a remote first company, culture is incredibly important. “Culture is different for every company, but making sure the person is an additive is a big one to focus on.” When hiring for Rootine, candidates are often asked to complete a take-home project to assess not only their communication skills and their professional abilities, but also their remote working capabilities. “When you’re remote, transparency is key. Communication is key, and the ability to set boundaries and understand when you do or don’t have to be on Slack without having to be told is key, especially at an early-stage startup.” What’s Next for Rootine As the first precision nutrition brand for the connected health consumer, Rootine is building an end-to-end platform to empower members to solve common health concerns like energy, stress, immune health and more through data, precision insights and nutrition products, and community. With an increase in awareness and interest in health and wellness highlighted by the pandemic, Rootine continues to see success and grow. Rachel is looking forward to seeing her company continue to provide cutting edge solutions to health on a larger scale. Partner with one of the 50 career-related clubs on campus to engage with targeted groups of students. → See all clubs Work with a member of our office, focusing on your industry or location, to create a personalized hiring strategy. → See all contacts source Read the full article
0 notes
Text

"Understanding Circumcision: Simple Facts, Clear Insights"
Contact Us: 70750 42888
Visit: https://www.navihealthcare.org/
#navihealthcare#NaviHealth#Circumcision#Circumcisionsurgery#vericosveine#vericoseveintretment#vericoseveinsurgery#vericoseveintreatmentsnearme#thebesttreatmentforvericosevein
0 notes
Link
Global competitors such as 3M, Aver Inc., Change Healthcare, Cognizant, Darena Solutions LLC. (My MIPS Score), Edifecs, ForeSee Medical Inc., HealthEdge Software, Inc., LexisNexis Risk Solutions Group, naviHealth, Inc., NEXTSTEP SOLUTIONS, INC., nThrive, Inc., Quadax, Inc., RevenueXL Inc., Signify Health, VIGILANCE HEALTH, INC., Lyfegen HealthTech AG are also highlighted in the study in order to get a stronger and effective outlook of the competition at domestic as well as global regions. The report further also offers comprehensive information based on primary and secondary research techniques to examine the data accurately.
0 notes
Text
Health Services Coordinator
Company Insight: • Being a pioneer in post-acute management and care transitions with 19 years of experience, naviHealth is uniquely positioned to manage patients, improve clinical and financial outcomes, and share risk with payors and providers. We provide clinical service support alongside proprietary technology and advisory solutions that empower health systems, health plans and post-acute providers to navigate care episodes across the continuum, with the goal of reducing waste and improving patient outcomes. Job Summary: The Health Services Coordinator (HSC) serves as the main point of contact for healthcare providers and members that are receiving post-acute services. In addition, the HSC role serves as administrative (non-clinical) support for the remote clinical services team. This role is responsible for providing direct support to the multi-disciplinary team to anticipate and plan for continuum of care and discharge needs. The HSC is responsible for processing incoming faxes, inbound and outbound telephone communication, maintaining accuracy of database documentation and the completeness of the medical record and naviHealth database. The HSC for the health plans will be accountable for productivity, service and quality standards including but not limited to average speed of answer, hold time, refusal rate, abandonment rate, and processing speeds. Required skills & experience (the 5 “must haves” to be considered): 1. High school diploma or GED required; Associate Degree or higher from an accredited college preferred 2. Able to use various office equipment, such as: copier, fax machine, telephone and scanner. 3. Familiarity with medical terminology and HIPAA laws strongly preferred 4. Must be organized and able to prioritize, plan, and handle multiple tasks/demands simultaneously 5. Required---Experience working in a call center environment. Experience in healthcare setting strongly preferred. What you need to know: • Please let candidate know that a drug screen and background check is required before we can send them to the client. • Please note that the client is looking for candidates that are not scheduled for time off during the holidays except for Thanksgiving Day and Christmas Day. • Looking for candidates with a Contact center/ call center background (preferably in a healthcare organization) • Process inbound and outbound faxes and emails according to productivity and quality standards. • Enter required data into the client's database accurately and in a timely manner. • Contract Start date: Nov 19th 2019 (6 month project) • This is role is in an office setting. All HSCs will be sitting in a big room together with 2-3 managers. Reference : Health Services Coordinator jobs from Latest listings added - JobsAggregation http://jobsaggregation.com/jobs/technology/health-services-coordinator_i7112
0 notes
Text
Health Services Coordinator
Company Insight: • Being a pioneer in post-acute management and care transitions with 19 years of experience, naviHealth is uniquely positioned to manage patients, improve clinical and financial outcomes, and share risk with payors and providers. We provide clinical service support alongside proprietary technology and advisory solutions that empower health systems, health plans and post-acute providers to navigate care episodes across the continuum, with the goal of reducing waste and improving patient outcomes. Job Summary: The Health Services Coordinator (HSC) serves as the main point of contact for healthcare providers and members that are receiving post-acute services. In addition, the HSC role serves as administrative (non-clinical) support for the remote clinical services team. This role is responsible for providing direct support to the multi-disciplinary team to anticipate and plan for continuum of care and discharge needs. The HSC is responsible for processing incoming faxes, inbound and outbound telephone communication, maintaining accuracy of database documentation and the completeness of the medical record and naviHealth database. The HSC for the health plans will be accountable for productivity, service and quality standards including but not limited to average speed of answer, hold time, refusal rate, abandonment rate, and processing speeds. Required skills & experience (the 5 “must haves” to be considered): 1. High school diploma or GED required; Associate Degree or higher from an accredited college preferred 2. Able to use various office equipment, such as: copier, fax machine, telephone and scanner. 3. Familiarity with medical terminology and HIPAA laws strongly preferred 4. Must be organized and able to prioritize, plan, and handle multiple tasks/demands simultaneously 5. Required---Experience working in a call center environment. Experience in healthcare setting strongly preferred. What you need to know: • Please let candidate know that a drug screen and background check is required before we can send them to the client. • Please note that the client is looking for candidates that are not scheduled for time off during the holidays except for Thanksgiving Day and Christmas Day. • Looking for candidates with a Contact center/ call center background (preferably in a healthcare organization) • Process inbound and outbound faxes and emails according to productivity and quality standards. • Enter required data into the client's database accurately and in a timely manner. • Contract Start date: Nov 19th 2019 (6 month project) • This is role is in an office setting. All HSCs will be sitting in a big room together with 2-3 managers. Reference : Health Services Coordinator jobs Source: http://jobrealtime.com/jobs/technology/health-services-coordinator_i7528
0 notes
Photo
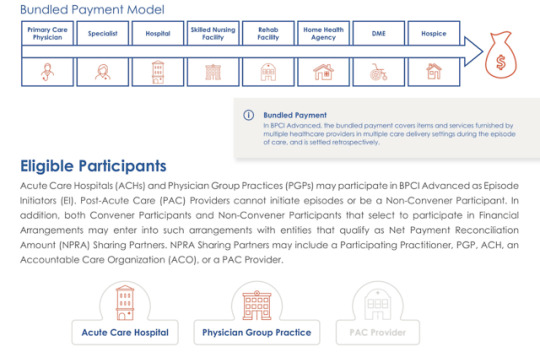
Cerner, naviHealth to Launch Medicare BPCI Advanced Offering https://hitconsultant.net/2019/04/12/cerner-navihealth-launch-medicare-bpci-advanced-offering/
0 notes
Link
New Job Opening in United States :
Daily review of census and identification of barriers to managing independent workload and ability to assist others. Work Conditions and Physical Requirements.
- August 26, 2020 at 12:42PM
0 notes