#NETosis
Text
Granulociti neutrofili e le loro "trappole": un'arma non convenzionale da calibrare prima di capire se sia utile o no
Una grande collaborazione di ricerca, guidata dal MRC Centre for Medical Mycology dell’Università di Exeter, si è concentrata su come le cellule immunitarie percepiscono il loro ambiente. Questa attività la flogosi che danneggia le cellule. La nuova ricerca, pubblicata sulla famosissima rivista Nature e finanziata dal Medical Research Council e Wellcome, ha esaminato il comportamento di un…
#artrite reumatoide#auto-anticorpi#autoimmunità#citochine#infiammazione#leucemia mieloide acuta#NETosis#neutrofili#recettore MICL#sistema immunitario#trappole neutrofiliche
0 notes
Text
immunology is the most interesting class ive had since microbio i think. learning so much cool shit ab cells
1 note
·
View note
Text
Immune cell regulator discovery could lead to treatments for arthritis and severe COVID - Published Aug 14, 2024
The discovery of a new regulator affecting immune cells could lead to new treatments to reduce inflammation in diseases including arthritis and severe COVID 19.
A large research collaboration, led by the University of Exeter's MRC Center for Medical Mycology, has focused on how immune cells sense their environment. This activity triggers responses which are finely balanced, to protect against disease and infection, and to reduce cell-damaging inflammation.
The research, titled "Recognition and control of Neutrophil Extracellular Trap formation by MICL" published in Nature, looked at the behavior of a receptor known as MICL, and its role in both preventing inflammation and protecting against infection.
Lead author Dr. Mariano Malamud, from the University of Exeter, said, "We've discovered that MICL is a key receptor that causes severe inflammatory disease when its functions are altered. This opens the door to the development of new therapies that target MICL, which could reduce the severity of inflammatory diseases and protect against infection."
Most receptors in the immune system sense their environment and send signals to cells, telling them to activate in response to changes such as infection or tissue damage. The team's work has revealed that MICL does the opposite, inhibiting the activation of the cell. This is an important function, as over-activation of cells can lead to cell damage and the development of auto-immune diseases if left unchecked.
The team went on to demonstrate the essential role that MICL plays in regulating inflammation in severe COVID 19, as well as arthritis and some other autoimmune diseases.
The new research, conducted in mice and verified in patients, focuses on the function of MICL present on the most abundant form of immune cell called a neutrophil.
As a result of an autoimmune disease or infection, neutrophils can undergo NETosis, a form of programmed cell death which is key for controlling infections but is very inflammatory. The team has found that MICL is able to detect this, and its inhibitory activity prevents more neutrophils from dying in this way.
NETosis cell death has been linked to several inflammatory diseases in humans, including Lupus, Rheumatoid arthritis and severe COVID. These inflammatory diseases lead to the production of antibodies that bind to MICL, preventing its inhibitory function and resulting in more severe disease.
Conversely, the study showed that increasing NETosis by blocking MICL function can protect against infection, such as those caused by fungi.
In mice with arthritis, the group showed that genetic loss of MICL led to more severe disease due to the excessive formation of NETs. More severe disease also occurred in normal mice when antibodies targeting MICL were applied.
Indeed, more severe disease was also seen in human arthritis patients who possessed antibodies targeting MICL, and the researchers could directly show that these patient antibodies drove exacerbated inflammatory response, using cell samples in labs.
Senior author Professor Gordon Brown, from the University of Exeter, said, "We've been working on how immune cells sense their environment for over 20 years, and this breakthrough is really exciting, revealing how the inhibition of inflammatory processes is finely balanced between controlling infection and the development of autoimmune disease"
More information: Gordon Brown, Recognition and control of neutrophil extracellular trap formation by MICL, Nature (2024). DOI: 10.1038/s41586-024-07820-3. www.nature.com/articles/s41586-024-07820-3
#covid#mask up#pandemic#covid 19#wear a mask#coronavirus#sars cov 2#still coviding#public health#wear a respirator#arthritis#auto-immune disease
21 notes
·
View notes
Text
WE HAVE SOLVED THE MYSTERY OF WHY CELLS HATE NEUTROPHILS SO MUCH IN CAW
So, last night, my boyfriend and I got into some random discussion about programmed cell death and some new breakthroughs in medicine, you know, the usual things you talk about with your boyfriend at 1 AM. It is well known that leftover bodies of dead cells are phagocytosed (literally consumed) by macrophages. And that’s why I always wondered why aren’t cells scared of macrophages as much as they are of neutrophils, since neutrophils don’t consume the dead cells. With my limited understanding of immunity (which we technically don’t learn a lot about in biology) I thought that neutrophils only consumed invader bacteria and fungi.
And OH BOY was I wrong about that.
Because (and yes I have spent whole night researching this, I’ll provide the links to papers in the end lol) neutrophils are little freaks and not only do they phagocytose leftovers of cells they actually cause them to die in the first place. This happens during infections, especially with viruses that cause the excess release of cytokines (like Coronaviridae). Cytokines activate neutrophils who basically just follow the signal towards the infection site and there all hell breaks loose. Neutrophils phagocytose bacteria and virions (those are viruses that haven’t infected a cell yet) which is fine, but they also degranulate and NETose. I’ll explain this in simple terms to my best ability.
Degranulation is when granulocytes (neutrophils, eosinophils, basophils and mastocytes are all different granulocytes) release their granules which are kind of like little sacks inside their cytoplasm which contain various chemicals. Releasing these chemicals happens when the cell receives appropriate stimulus, the little granules expel their contents out of the cell’s interior. In the case of neutrophils, granules contain very toxic compounds that cause the formation of free radicals which damage DNA and proteins of the surrounding cells, as well as granules filled with digestive enzymes which, well, digest the surrounding tissues.
NETosis is a special type of cell death specific to neutrophils in which they literally degranulate pieces of their own, or their mitochondrial DNA together with more toxic compounds. This creates a net of DNA strands called chromatin which entangles invading bacteria and severely damages them and also marks them for phagocytosis by macrophages. But this process is not well controlled and some of that chromatin and toxic compounds can land onto neighboring cells which is, as you can conclude, very bad for them.
With these two abilities at hand, neutrophils are very well equipped to kill cells and destroy tissue. Which is good in cases when the cells are infected and the tissue is damaged, but their quite aggressive methods can damage healthy cells in the area as well, some of them will die and neutrophils will phagocytose their dead particles.
Basically, to neutrophils every infection is a huge kill and eat all you can buffet. They literally phagocytose until they physically cannot anymore and then go to the spleen or bone marrow to die. They also allow macrophages to consume them and thus pass on the antigens for antigen presentation which influences further immune response. But they can also cause a lot of damage, especially if cytokine storm happens and they completely lose control. This is what causes SARS and it can kill you if it’s severe enough.
Biologically speaking, neutrophils are very important because they are the first ones to come to the sight of infection and their crazy methods usually finish the things before they get too severe. They themselves produce cytokines that mobilize macrophages and dendritic cells so that more immune cells can join and help them. They also have a role in repairing the tissues they damaged.
However, other immune cells, including macrophages and killer T cells, simply don’t cause as much damage. Neutrophils just go all out, which is why they live for such a short period of time compared to their colleagues (they live for only few days, compared to macrophages who can live up to a month and lymphocytes who can live for months, even years).
So, yeah, my boyfriend and I have concluded (at 4AM this morning) that neutrophils are so feared because they damage tissue, go crazy and violently kill healthy cells by accident, then consume them and that’s not by accident, it’s a mechanism to repair tissues.
I can’t believe I wasted whole night just for this. My boyfriend is also disappointed. But I hope that we finally have an explanation for this mystery. Tell me what you think lol.
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8589350/
https://www.nature.com/articles/nri.2017.105
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5820392/#:~:text=Neutrophils%20contribute%20to%20tissue%20injury,detail%20here%20(Kruger%20et%20al.
#cells at work#hataraku saibou#neutrophils#immunology#medicine#science#biology#i actually need help#it’s 4am
66 notes
·
View notes
Text
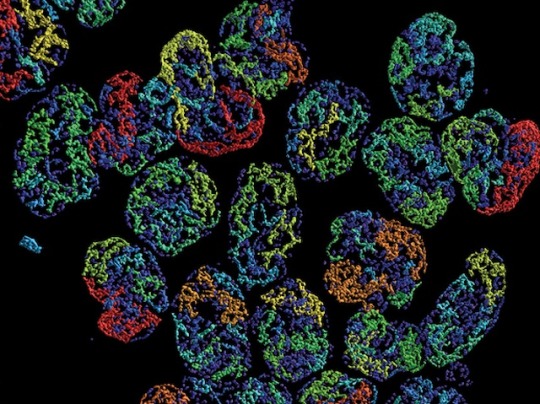
Die Another Way
If immune cells called neutrophils undergoing programmed cell death or apoptosis are not quickly cleared away by other immune cell processes, NETosis – the release of sticky extracellular traps (NETs) – is sparked by epigenetic signals which concludes their death
Read the published research article here
Image from work by Yanfang Peipei Zhu, Mary Speir and ZheHao Tan and colleagues
Department of Pediatrics, University of California San Diego, La Jolla, CA, USA
Image originally published with a Creative Commons Attribution 4.0 International (CC BY 4.0)
Published in Science Advances, December 2023
You can also follow BPoD on Instagram, Twitter and Facebook
16 notes
·
View notes
Note
for the science ask game: 🌏 📚 and 🔭!
🌏—fun fact from my area of study: there’s a type of white blood cell—a neutrophil—which (among other cool, but perhaps less iconic defense strategies) can release its own DNA, mixed with antibacterial proteins, outside of the cell to trap and destroy pathogens. The traps are named neutrophil extracellular traps, which are appropriately abbreviated NETs. (Here’s a review I found on NETosis, if you’re interested to learn more: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7590568/)
📚—something I want to understand better: I wish I could get into cell signalling and gene regulation. Whenever I take the time to study a signalling pathway, it’s always super interesting to see how all the different components work together, but then I just forget everything almost immediately.
🔭—what sparked my interest in science/my field: as far as I can remember I’ve always been interested in science, and I would credit my mom for that. When I was little she encouraged my curiosity and directed it towards science; she taught me about the scientific method, and I got very into the idea of discovering new things through observation and experimentation, which I think created sort of a positive feedback loop of my interest and her support—we read books about nature and about the process of science, we learned about famous scientists and their discoveries, we went to museums and zoos and aquariums and lectures about whatever I was interested in at the time. I think “being a scientist” has been part of my identity for as long as I’ve had one. I went through phases of interest in many different fields—astronomy, paleontology (yeah, I was a “dinosaurs and space!!” kid), ecology, astrobiology, and chemistry are some that I remember—and ended up settling on immunology. I got really interested in molecular biology from my 9th grade biology class—I had learned vaguely about cells and genetics before then, but for the first time I felt like I was really glimpsing the fundamental mechanisms of life, the individual interactions between proteins and other molecules that build upon one another and connect to give rise to the immense complexity of a living organism—a complexity which, until then, I had just sort of taken for granted. I was kind of amazed by all this, and I still am. My specific interest in immunology came from reading the manga Cells at Work. I knew little to nothing about how the immune system worked at that point, and I was confused about a lot of things in the story—so I would literally just start googling things like “how do memory b cells remember antigens” to try and figure out what the real-life processes were that were being portrayed. A lot of what I found went over my head, but I kept just looking up questions about how different parts of the immune system worked and slowly slipping into the vast and tangled rabbit warren that is immunology. A big part of why I’m still interested in the immune system is because it’s so complicated. I don’t feel like I could ever learn everything I want to know about how it works, and everything I do learn just brings up new questions to scroll through chains of half-understood PubMed articles trying to figure out. There’s so much I don’t know, and there’s so much we still have to figure out, and I would love to be part of that research.
3 notes
·
View notes
Text

See i feel like if it's in another type of cell it's not NETosis is the thing. its somethignelseETosis.
Vorobjeva, N.V., Chernyak, B.V. NETosis: Molecular Mechanisms, Role in Physiology and Pathology. Biochemistry Moscow 85, 1178–1190 (2020). https://doi.org/10.1134/S0006297920100065
2 notes
·
View notes
Text
New Study: Ginger Supplementation Shows Promise in Autoimmune Disease Treatment
Current research study highlights ginger supplements as possibly efficient in managing swelling in autoimmune illness by targeting neutrophils and hindering NETosis, providing a brand-new point of view on natural supplements in treatment prepare for conditions like lupus and rheumatoid arthritis.
New research study took a look at the impacts of ginger supplements on the performance of leukocyte…

View On WordPress
0 notes
Text
NEWTrophils an their NETworks: MICL "sparks" from the NETosis to a more C-lective role as an AML biomarker
A major research collaboration, led by the MRC Centre for Medical Mycology at the University of Exeter, has focused on how immune cells sense their environment. This triggers finely tuned responses to protect against disease and infection, and to reduce inflammation that damages cells. The new research, published in the world-renowned journal Nature and funded by the Medical Research Council and…
0 notes
Text
Long noncoding #RNA SNHG16 regulates TLR4-mediated autophagy and NETosis formation in alveolar hemorrhage associated with systemic lupus erythematosus
CONCLUSIONS: Our results demonstrate that l#ncRNA SNHG16 regulates TLR4-mediated autophagy and NETosis formation in the human and mouse AH lungs, and provide a therapeutic potential of intra-pulmonary delivery of sh#RNA targeting SNHG16 in this SLE-related lethal manifestation. https://pubmed.ncbi.nlm.nih.gov/37700342/?utm_source=dlvr.it&utm_medium=tumblr&utm_campaign=None&utm_content=1RYYbE7j9SUSBe_aHniaI_J1MQIFIBbfLuFxoWdLNMNDzVVIWF&fc=None&ff=20230916100529&v=2.17.9.post6%2086293ac
0 notes
Text

Today's Beauty-Marked Beauty is: Kasumi Haruno from Netosis
#beauty mark of the day#mod kaori#beauty mark#otd#girl#lemon#right eye#thigh#multiple#haruno kasumi#kasumi haruno#haruno#kasumi#posted
0 notes
Text
NETosis is still the funniest thing in immunology to me. The NET part stands for "Neutrophil Extracellular Trap." Neutrophils are an abundant type of white blood cell that are very good at killing things, and have a lot of different tools to do so, but their life span is pretty short. As one of my professors so eloquently put it, the purpose of a neutrophil is to "eat shit and die." So what is NETosis? It's when a neutrophil encounters a pathogen, and its response is to puke its DNA outside the cell. The DNA is beaded with antimicrobials so things get caught up in the DNA web and killed. You might recognize that DNA is supposed to be inside the cell. The neutrophil absolutely does not survive this.
36 notes
·
View notes
Photo

Higher levels of destructive white blood cells associated with more severe COVID-19
Patients with severe COVID-19 infections have higher blood levels of neutrophil extracellular traps (NETs), which produce NETosis, an inflammatory type of neutrophil cell death. Researchers believe the NETs may be relevant to numerous aspects of novel coronavirus as thrombosis and inflammation are hallmarks of the severe infection.
48 notes
·
View notes
Link
COVID-19: Blood Clots May Form via NETosis Patients with COVID-19 who endure dangerous life-threatening complications such as blood clots and inflammation also experience dysregulated NETosis – Cell death process that produces neutrophil extracellular traps (NETs), extracellular webs of DNA, and also toxic substances that capture and eliminates pathogens. Nonetheless, the neutrophil extracellular traps might interact […] The post Blood Clots In COVID-19 Patients Due To NETosis : New Study appeared first on BioTecNika .
1 note
·
View note
Text
stream of consciousness of a microbiologist/immunologist re-reading Cells at Work
“The zeal that WBC has for killing bacteria reminds me of the neutrophil bacteria killing assay I did last week!”
“Attaboy, WBC! Such hard working cells~ But how come he hasn’t undergone NETosis yet after fighting all these bacteria? That’s the neutrophil’s trump card!“
*Still thinking about NETosis*
“WBC only uses a knife? But neutrophils use lots of different mechanisms to kill bacteria. For example, antimicrobial proteins, ROS...”
“Does RBC/WBC count as self-cest? (Or is that cell-cest??) They’re cells in the same body, but one is male and the other female, but they should have the same genomic DNA. Yet, RBCs are enucleated, so she technically don’t even have genomic DNA, and therefore no X or Y chromosomes...???”
*Imagines THP-1 cells as a person in a hazmat suit and RAW264 cells as mice in maid costumes*
69 notes
·
View notes