#Maxillofacial injuries
Explore tagged Tumblr posts
Text
Facial Degloving: Causes, Important Symptoms, Treatment, and Recovery
Facial Degloving: Causes, Important Symptoms, Treatment, and RecoveryIntroductionWhat is Facial Degloving?Causes and Risk FactorsSigns and SymptomsDiagnosis and AssessmentTreatment ApproachesMultidisciplinary ApproachRecovery and RehabilitationPotential ComplicationsLong-Term OutcomesPrevention StrategiesPatient StoriesAdvancements in TreatmentSupport SystemsExpert InsightsConclusionFacial…

View On WordPress
#Aesthetic concerns#Bone realignment#degloved face picture#Disfiguring injuries#Emotional support#Facial bone fractures#Facial deformities#facial degloving#Facial injuries#Facial reconstruction#Facial rehabilitation#Facial trauma#High-impact accidents#Maxillofacial injuries#Medical innovations#Multidisciplinary treatment#Nerve damage#Plastic and reconstructive surgery#Prevention strategies#Protective gear#Recovery process#Skin detachment#Soft tissue damage#Soft tissue repair#Surgical reconstruction#Swelling and bruising
0 notes
Text
To whatever dentist that decided to shave my canines to match what were mostly baby teeth at the time. Thank you not only do i look slightly stupid but you fucking over did it a smidge , and now im in fucking pain you silly shit. If YOU every see this, i bring shame upon you, shame upon your family, shame upon your dam cow.
#to dentist out there dont shave down a childs teath on a huntch especaily after there faces have been bashed in You give em so mutch troble#down the fucking line aggg.#enamile past or whatever you used to repare it dosent turn well long turn you fucking goob. you fucking half baked maxillofacial surgeon#i may be miss identifing things but still#dentist#maxillofacial surgeon#maxillofacial surgery#child hood injury#dare i say medical malpractice#im only posting this in hopes that they or another dentist sees it and knows how fucking silly you fucking are#the fucker didnt even do it perficly evenly#did you hand me over to your fucking understudy#did you finish your fucking DMD or whatever the fuck your did clearly dishonestly#did they just look at your 3 years of residancy and go yea you know what you get a pass your clearly paying well and good atitnoeon to the#care with pacianct and are quilified to oporate on a child#was the child specialist simple not in on that faithful weanedness day#and you piped up like yeaaaa i can do oral surgary on an adult i can shur as hell oporate on a child i mean its mostly baby teath so it#coulnt be to long term right right#or did you walk in going whats it matter its not like it going to be my problem just save the skin off my back and hand it over to the next#guy#wear you fresh out of medical school.#its not noticible now but holy fuck is it anoying
2 notes
·
View notes
Text
You can’t shop your way out of a monopoly

I'm on tour with my new, nationally bestselling novel The Bezzle! Catch me in TUCSON (Mar 9-10), then SAN FRANCISCO (Mar 13), Anaheim, and more!

If you're running a business, you can either invest at being good at your business, or good at Google SEO. Choose the former and your customers will love you – but they won't be able to find you, thanks to the people who choose the latter. And if you're going to invest in top-notch SEO, why bother investing in quality at all?
For more than a decade, Google has promised that it would do something about "lead gens" – services that spoof Google into thinking that they are local businesses, pushing down legit firms on both regular search and Google Maps (these downranked businesses invested in quality, not SEO, remember). Search for a roofer, a plumber, an electrician, or a locksmith (especially a locksmith), and most or all of the results will be lead-gens. They'll take your call, pretend to be a local business, and then call up some half-qualified bozo to come out and charge you four times the going rate for substandard work:
https://www.nytimes.com/2016/01/31/business/fake-online-locksmiths-may-be-out-to-pick-your-pocket-too.html
Some of them just take your money and they "go back to the shop for a tool" and never return:
https://www.riverfronttimes.com/news/when-a-fake-business-used-a-real-st-louis-address-things-got-weird-32087998
Google has been promising to fix this since the late aughts, and to be fair, it's a little better. There was once a time when a map of Manhattan showed more locksmiths than taxis:
https://blumenthals.com/blog/2009/02/18/google-maps-proves-more-locksmiths-in-nyc-than-cabs/
But GMaps is trapped in the enshittification squeeze. On the one hand, the company wants to provide a good and reliable map. On the other hand, the company makes money selling "ads" that are actually payola, where a business can pay to get to the top of the listings or get displayed on the map itself. Zoom out of Google's map of central London and the highlighted landmarks are a hilarious mix of "organic" and paid listings: the British Museum, Buckingham Palace, the Barbican, the London Eye…and a random oral and maxillofacial clinic in the financial district:
https://twitter.com/dylanbeattie/status/1764711667663831455
Hell of a job "organizing the world's information and making it universally accessible and useful," Big G. Doubtless the average Londoner finds the presence of this clinic super helpful in orienting themselves relative to the map on their phone screens, and it's a real service to tourists hoping to hit all the major landmarks.
It's not just Maps users who'd noticed the rampant enshittification. Even the original design team is so horrified they're moved to speak out about the moral injury they experience seeing the product they worked so hard on turned into a giant pile of shit:
https://twitter.com/elizlaraki/status/1727351922254852182
Now, when it comes to locksmiths, I'm lucky. My neighborhood in Burbank includes the wonderful Golden State Lock and Safe, which has been in business since 1942:
https://www.goldenstatelock.com/
But you wouldn't know it from searching GMaps for a locksmith near me. That search turns up a long list of scams:
https://www.google.com/maps/search/locksmith/@34.1750451,-118.369948,14z/data=!3m1!4b1?entry=ttu
It also turns up plenty of Keyme machines – these are private-equity backed, self-serve key-cutting machines placed in grocery stores. Despite Keyme calling itself a "locksmith," it's just a badly secured, overcaptilized, enshittification-bound system for collecting and retaining shapefiles for the keys to millions of homes, cross-referenced with billing information that will make it easy for the eventual hackers to mass-produce keys for all those poor suckers' houses.
(Hilariously, Keyme claims to be an "AI" company):
https://www.businesswire.com/news/home/20200114005194/en/KeyMe-Raises-35-Million-to-Further-Its-Mission-of-Building-the-Premier-Locksmith-Services-Company-in-the-Nation
But despite the fact that you can literally see the Golden State storefront from Google Streetview, Google Maps claims to have no knowledge of it. Instead, Streetview labels Golden State "Keyme" – and displays a preview showing a locksmith using a tool to break into a jeep (I'd dearly love to know how the gadget next to the Slurpee machine at the 7-Eleven will drive itself to your jeep and unlock the door for you when you lose your keys):
https://www.google.com/maps/place/KeyMe+Locksmiths/@34.1752624,-118.3487531,3a,75y,350.19h,90.21t/data=!3m6!1e1!3m4!1ssHrtqjqvgFir3NBauMy13Q!2e0!7i16384!8i8192!4m15!1m8!3m7!1s0x80c2959cd65dbb1b:0x4b3744cf87492a71!2sBurbank+Blvd+%26+N+Hollywood+Way,+Burbank,+CA+91505!3b1!8m2!3d34.1750025!4d-118.3493484!16s%2Fg%2F11f37_3lq8!3m5!1s0x80c2951cedbf4d39:0xe8ff9fd5872e66e9!8m2!3d34.1755176!4d-118.349!16s%2Fg%2F11mw7nr4fx?entry=ttu
It's pretty clear to me what's going on here. Keyme has hired some SEO creeps and/or paid off Google, flooding the zone with listings for its machines. Meanwhile, Golden State, being merely good at locksmithing, has lost the SEO wars. Perhaps Golden State could shift some of its emphasis from being good at locksmithing in order to get better at SEO, but this is a race that will always be won by the firm that puts the most into SEO, which will always be the firm that puts the least into quality.
Whenever I write about this stuff, people inevitably ask me which search engine they should use, if not Google?
And there's the rub.
Google used predatory pricing and anticompetitive mergers to acquire a 90% search market-share. The company spends more than $26b/year buying default position in every place where you might possibly encounter a new search engine. This created the "kill zone" – the VC's term of art for businesses that no one will invest in, because Google makes sure that no one will ever find out it exists:
https://www.theverge.com/23802382/search-engine-google-neeva-android
That's why the only serious competitor to Google is Bing, another Big Tech company (Bing is also the primary source of results on Duckduckgo, which is why DDG sometimes makes exceptions for Microsoft's privacy-invading tracking):
https://en.wikipedia.org/wiki/DuckDuckGo#Controversies
Google tells us that the quid-pro-quo of search monopolization is search excellence. The hundreds of billions it makes every year through monopoly control gives it the resources it needs to fight spammers and maintain search result quality. Anyone who's paid attention recently knows that this is bullshit: Google search quality is in free-fall, across all its products:
https://downloads.webis.de/publications/papers/bevendorff_2024a.pdf
But Google doesn't seem to think it has a problem. Rather than devoting all its available resources to fighting botshit, spam and scams, the company set $80 billion dollars alight last year with a stock buyback that was swiftly followed with 12,000 layoffs, followed by multiple subsequent rounds of layoffs:
https://pluralistic.net/2024/02/21/im-feeling-unlucky/#not-up-to-the-task
The scams that slip through Google's cracks are sometimes nefarious, but just as often they're decidedly amateurish, the kind of thing that Google could fix by throwing money at the problem, say, to validate that new ads for confirmed Google merchants come from the merchant's registered email addresses and go to the merchant's registered website:
https://pluralistic.net/2023/02/24/passive-income/#swiss-cheese-security
Search is a capital intensive business, and there are real returns to scale, as the UK Competition and Market Authority's excellent 2020 study describes:
https://assets.publishing.service.gov.uk/media/5fe4957c8fa8f56aeff87c12/Appendix_I_-_search_quality_v.3_WEB_.pdf
But Google doesn't seem to think that its search needs that $80 billion to fight the spamwars. That's the thing about monopolists, they get complacent. As Lily Tomlin's "Ernestine the AT&T operator" used to say, "We don't care, we don't have to, we're the phone company."
That's why I'm so excited about the DOJ Antitrust Division monopolization case against Google. Trusting one company to "organize the world's information and make it universally accessible and useful," was a failure:
https://www.justice.gov/opa/pr/justice-department-sues-google-monopolizing-digital-advertising-technologies
I understand why people want to know which search engine they should use instead of Google, and I get why, "There aren't any good search engines" is such an unsatisfactory answer. I understand why each fresh round of printer-company fuckery prompts people to ask "which printer should I get?" and I understand why "There are only six major printer companies and they're all suffering from end-stage enshittification" isn't what anyone wants to hear.
We want to be able to vote with our wallets, because it's so much faster and more convenient than voting with our ballots. But the vote-with-your-wallet election is rigged for the people with the thickest wallets. Try as hard as you'd like, you just can't shop your way out of a monopoly – that's like trying to recycle your way out of the climate emergency. Systemic problems need systemic solutions – not individual ones.
That's why the new antitrust matters so much. The answer to monopolies is to break up companies, block and unwind mergers, ban deceptive and unfair conduct. "Caveat emptor" is the scammer's motto. You shouldn't have to be an expert on lead gen scams to hire a locksmith without getting ripped off.
There are good products and services out there. Earlier this year, we decided to install a (non-networked) programmable pushbutton lock. I asked Deviant Ollam – whom I know from Defcon's Lockpicking Village – for a recommendation and he suggested the Schlage FE595:
https://www.schlage.com/en/home/products/FE595PLYFFFFLA.html
I liked it so much I bought another one for my office door. Eric from Golden State Lock and Safe installed it while I wrote this blog-post. It's great. I recommend both of 'em – 10/10, would do business again.
Name your price for 18 of my DRM-free ebooks and support the Electronic Frontier Foundation with the Humble Cory Doctorow Bundle.

If you'd like an essay-formatted version of this post to read or share, here's a link to it on pluralistic.net, my surveillance-free, ad-free, tracker-free blog:
https://pluralistic.net/2024/03/05/the-map-is-not-the-territory/#vapor-locksmith

Image: alicia rae (modified) https://commons.wikimedia.org/wiki/File:Kehole_Red.jpg
CC BY 2.0 https://creativecommons.org/licenses/by-sa/2.0/deed.en
--
Budhiargomiko (modified) https://commons.wikimedia.org/wiki/File:Wasteland.jpg
CC BY-SA 4.0 https://creativecommons.org/licenses/by-sa/4.0/deed.en
245 notes
·
View notes
Text
Atlantis Expedition: Science Division Departments - Medical Department
Continuing from my starting post here, I'm now breaking things down by department, beginning with the Medical Department.
I did end up heavily revising this department after the commentary on the general departments post, and also after a lot of looking up of the actual divisions of medical specialties. So, first, the (new) numbers:
> Head: Carson Beckett (later, Jennifer Keller, later, whomever) > Contains: Surgery, psychiatry, physical therapy > Function: Maintaining health of expedition members > Examples of function: surgeries, medical prescriptions, recuperation from injuries, mental stability > Personnel quantity: 1 (Head) + 10 (surgical team) + 5 10 (nurses non-surgical team) + 1 (psych) + 1 (phys. therapy) + 1 (anesthesiologist) (grouped under non-surgical team) = 19 23 total > A/N: Nurses have training in medications and physical therapy, surgical team also doubles as general practitioners
Information carried over from the first post, with struck text indicating revisions. The new total is 23, and the author's note is now irrelevant in light of new information. Mostly.
After doubling the amount of nurses, realizing "nurse" is a very broad category of medical professional with multiple definitions and aspects of job duties in multiple countries, I did a bit of renaming of the teams within this department: surgical, non-surgical, and miscellaneous (sorry guys).
Something I had realized was that this was not going to be a typical medical department (duh, in hindsight). These people are all going through the SGC, and the SGC quite likely not already has their own training protocols in place for dealing with SGC-specific situations, but also adapted technology from Goa'uld tech. What is Goa'uld tech? Appropriated Ancient tech, but without the gene component - fascinating, but also a post for another time.
This did inform how I revised which personnel to include, their specialties, and their duties. You're not exactly going to be shoving a whole MRI machine through a gate, so a radiologist isn't going to be a necessary specialty. Because of this, there's going to be a lot more cross-training, and more of a focus that's similar to what Atlantis would actually operate as: a forward operating base.
So, on to the teams (commentary included).
Surgical Team
> Personnel quantity: 10 > Minimum education: Doctorate in Surgery (ChM) > All of these people are already trained in basic medical knowledge and practices, and also overall surgical practices in different areas of the body
Specialties
> Neurosurgery > Dentistry | Oral and maxillofacial surgery » In the US, trained to do general anesthesia and deep sedation > Orthopedics » Musculoskeletal > Trauma surgery » Can contain combat surgeons » 2x of these > OBGYN > Urology > Cardiothoracic » 2x of these, by speciality: ⇛ Cardiovascular surgeon ⟹ "involving the heart and the great vessels" ⇛ Thoracic surgeon ⟹ involving the lungs, esophagus, thymus, etc. > Surgical technologist » "In the military they perform the duties of both the circulator and the scrub." » Creates and maintains a sterile surgical environment » Anticipates the work a surgeon needs to do » Walking compendium of surgical techniques and stitches
I had wavered a bit on qualifications, and thus who to include - at the end of the day, it was probably going to be on an American standard, given the physical location of SGC. This meant I got to do a nifty thing of having my oral/maxillofacial surgeon be the dentist that's also an anesthesiologist, even if this is apparently considered odd in many other countries.
Mostly I wanted to go by section of the body, and see what kind of specialties there were, and what did and did not overlap. Surprisingly, it was more difficult to figure out who did abdominal surgeries than it was neurosurgery or dental surgery, hence two people in cardiothoracic surgery and two "general" surgeons in the form of trauma surgery because, again, forward operating base - they have no idea what Atlantis will be, so some assumptions will need to be made and better to err on the side of caution.
In a more delicate but still very necessary subject, one OBGYN (obstetrics and gynecology) and one urologist (aka urinary system and male reproductive system). For various obvious reasons, everyone's health in this area still needs to be taken care of, so it's better to have them on the team than politely handwave the idea.
Neurosurgery, for an obvious reason - it's highly specialized and without significant overlap, while also being a critical function on a surgical team with the demands the Atlantis Expedition will likely face.
Orthopedics are musculoskeletal, or deals with muscles and the skeletal system. A fair amount of what they do has overlap (see: trauma surgeons), but having someone specialized for the particularities of setting bones and handling surgeries on things like the joints is incredibly useful when presuming setting up camp in an active combat zone (which they really, really did).
Trauma surgeons are, more or less, the ones that you would see in an emergency situation - acute situations and their injuries are their specialty, and for this expedition likely the head of the surgical team by dint of their training to assess a patient quickly and develop a care plan very quickly. Because of this, I found the overlap of combat surgeons immensely helpful, which means that there's a significant probability that this surgical team has military personnel assigned to it. These surgeons are also the ones most likely to be SGC-imported, and trained to deal with things like injuries from Goa'uld and Goa'uld devices.
All these very highly-trained people, who are all probably very, very smart - who supports them? As it turns out, at least in the operating theater, not the nurses, but surgical technologists.
Surgical technologists main job, at least here, would be to set up the operating theater and anticipate whatever it is a surgeon needs in assistance. This includes things like training on a wide variety of surgical techniques (i.e. stitches), disinfection procedures, and medications such as anesthesia (ish). I included the quote about military duties because it saves money on how many people to include in the expedition, and penny-pinching is the backbone of any hiring process.
Now, the surgical team is all done! That's ten people right there, and on to the non-surgical team.
Non-Surgical Team
> Personnel quantity: 10 » 5 Technicians/Nurses, 5 Non-Surgical Medical Specialists
Nurses
> (Advanced Practice) Nurses » 5x of these » Registered Nurse ⇛ As the general minimum educational and experimental requirement » Perioperative nursing ⇛ Assists surgical team, helps with pre- and post-surgical patients » Emergency nursing ⇛ Can do triaging, suturing, casting/splinting, local/regional anesthesia, and other doctoral skills as needed ⇛ Likely the SGC training model incorporates all of the above, and also training on medical technology adapted from Goa'uld healing technology (which is really Ancient but without the ATA gene lock) ⟹ Radiology tech ⟹ MRI tech (which is radiology but a bit to the left) ⟹ Other adapted diagnostic equipment
Non-Surgical Medical Specialists
> Pathology » 2x of these » Coordinates with Life Science Department to develop diagnoses for novel diseases (in the Pegasus galaxy) > Internal medicine | Internists » 2x of these > Anesthesiology » For everything the OMS people don't do in terms of anesthesiology » See also: Anesthesia (topic)
Remember how I said the qualifications were a doozy, and that nurses were a broad category? ... Yeah, this is why. The medical field is probably current in flux right now, given the shifting priorities of medical personnel and so much research that is still in the process of being applied, but I waved my magic plot-fixing wand and assumed the SGC figured this out for me.
All of these nurses are likely to be SGC imports, and thus unbelievably well-trained in everything that the SGC needs them to do. These are the personnel who know how all of the Goa'uld tech works on a functional level, have gotten the goodies first from engineering, and are waving their handheld MRI and other diagnostic equipment over their patients like a fairy godmother in scrubs. As with a real world hospital, these are the people actually running the show, and likely making the surgical team look like hypercompetent show poodles.
As for non-nurses who are also non-surgeons, pathologists are the ones who work up what people will actually be diagnosed with, figuring out all the newest and shiniest diseases and cataloguing them for reference. Doctor Biro is a pathologist, for example.
The thought occurred to me that we still need something resembling a general practitioner, but in light of fancy things like handheld MRIs and other scanners, this role is much reduced in favor of people who pack a greater intellectual punch.
However, I found that internists not only fill this gap, but are also hyper-specialized in their own way, in the respect of their knowledge base being internal diseases and multi-system diseases. Ergo, two of them, because they're just that useful. They'd probably coordinate quite a bit with cardiothoracic surgeons, as those are overlapping areas of study based on region of the body.
One (1) anesthesiologist, because the OMS cannot - nor should they - be the only person to perform anesthesia. This person functions as a sanity checker, and also the thin margin of the anesthesia that the surgeon doesn't cover.
We still need to round out this department, though. So far I've managed to cover in-patient, out-patient, and the various surgical stages. What else?
Well, recuperation - patients can't actually linger in the infirmary for the entirety of their healing process, for such practical reasons as beds available and boredom of patient, so the transitional phase needs to be covered.
Hence, the highly uncreative placeholder section name of Miscellaneous:
> Psychiatrist » 1x of these, because canon says so? > Physical therapist » 1x of these, because canon says so?
Now while personnel such as nurses and internists are meant to convey educational material and instructions to patients about recuperation, it helps to actually have specialists on hand to make the patients commit to the bit.
Having only one psychiatrist on hand seems a bit of a Star Trek logical fallacy, but I'm once again waving my plot wand and assuming anyone that managed to get through the arduous employment process of 1) being told the Stargate exists (and coping with their world views being upended), 2) being employed by the SGC in general, and 3) passes their psychological assessment is probably mentally stable enough to only need one psychiatrist for the entire expedition.
(Yes, this does mean everyone on the expedition got their rubber stamp of sanity, and probably in grueling triplicate. Such as it can be defined a fanfiction-like world of scifi. I think they're coping pretty well with everything, no?)
With all the work that the surgical and non-surgical teams put into taking care of injured expedition members, a physical therapist is, as with everyone else here, very good at their job, but ultimately one of the last steps for patients that require longer term care. Think gaining back muscle after a broken leg, or more serious injuries that require months of guided exercise to be back to gate team-ready health (or general running for your life because Atlantis is just as dangerous).
Total Medical Department Personnel
Head of Department: 1
Surgical Team: 10
Non-Surgical Team: 10
Miscellaneous: 2
Total total: 23
I'll be going over headcanons on canonical personnel, such as Carson Beckett, Jennifer Keller, and Biro in their own posts, but for now this is a general accounting of the expedition's medical department.
Shout-out to @savestave and @stinalotte for the discussion and feedback on the original post!
21 notes
·
View notes
Text
Trauma Center Levels
As mentioned above, Trauma categories vary from state to state. Outlined below are common criteria for Trauma Centers verified by the ACS and also designated by states and municipalities. Facilities are designated/verified as Adult and/or Pediatric Trauma Centers. It is not uncommon for facilities to have different designations for each group (ie. a Trauma Center may be a Level I Adult facility and also a Level II Pediatric Facility).
Level I
Level I Trauma Center is a comprehensive regional resource that is a tertiary care facility central to the trauma system. A Level I Trauma Center is capable of providing total care for every aspect of injury – from prevention through rehabilitation.
Elements of Level I Trauma Centers Include:
24-hour in-house coverage by general surgeons, and prompt availability of care in specialties such as orthopedic surgery, neurosurgery, anesthesiology, emergency medicine, radiology, internal medicine, plastic surgery, oral and maxillofacial, pediatric and critical care.
Referral resource for communities in nearby regions.
Provides leadership in prevention, public education to surrounding communities.
Provides continuing education of the trauma team members.
Incorporates a comprehensive quality assessment program.
Operates an organized teaching and research effort to help direct new innovations in trauma care.
Program for substance abuse screening and patient intervention.
Meets minimum requirement for annual volume of severely injured patients.
Level II
A Level II Trauma Center is able to initiate definitive care for all injured patients.
Elements of Level II Trauma Centers Include:
24-hour immediate coverage by general surgeons, as well as coverage by the specialties of orthopedic surgery, neurosurgery, anesthesiology, emergency medicine, radiology and critical care.
Tertiary care needs such as cardiac surgery, hemodialysis and microvascular surgery may be referred to a Level I Trauma Center.
Provides trauma prevention and continuing education programs for staff.
Incorporates a comprehensive quality assessment program.
Level III
A Level III Trauma Center has demonstrated an ability to provide prompt assessment, resuscitation, surgery, intensive care and stabilization of injured patients and emergency operations.
Elements of Level III Trauma Centers Include:
24-hour immediate coverage by emergency medicine physicians and the prompt availability of general surgeons and anesthesiologists.
Incorporates a comprehensive quality assessment program.
Has developed transfer agreements for patients requiring more comprehensive care at a Level I or Level II Trauma Center.
Provides back-up care for rural and community hospitals.
Offers continued education of the nursing and allied health personnel or the trauma team.
Involved with prevention efforts and must have an active outreach program for its referring communities.
Level IV
A Level IV Trauma Center has demonstrated an ability to provide advanced trauma life support (ATLS) prior to transfer of patients to a higher level trauma center. It provides evaluation, stabilization, and diagnostic capabilities for injured patients.
Elements of Level IV Trauma Centers Include:
Basic emergency department facilities to implement ATLS protocols and 24-hour laboratory coverage. Available trauma nurse(s) and physicians available upon patient arrival.
May provide surgery and critical-care services if available.
Has developed transfer agreements for patients requiring more comprehensive care at a Level I or Level II Trauma Center.
Incorporates a comprehensive quality assessment program.
Involved with prevention efforts and must have an active outreach program for its referring communities.
Level V
A Level V Trauma Center provides initial evaluation, stabilization and diagnostic capabilities and prepares patients for transfer to higher levels of care.
Elements of Level V Trauma Centers Include:
Basic emergency department facilities to implement ATLS protocols.
Available trauma nurse(s) and physicians available upon patient arrival.
After-hours activation protocols if facility is not open 24-hours a day.
May provide surgery and critical-care services if available.
Has developed transfer agreements for patients requiring more comprehensive care at a Level I through III Trauma Centers.
4 notes
·
View notes
Text
I drew my character Vic if he was in the waiting room from beetlejuice. he's pissed cuz he cant smoke with not much mandible left.
This injury occured due to steering wheel column vs. face at high speeds. Death occured due to airway occulsion from significant maxillofacial trauma.
Ok now I have to study.

3 notes
·
View notes
Text
The Causes of Facial Pain are Numerous by Siniša Franjić in Journal of Clinical Case Reports Medical Images and Health Sciences
Abstract
One of the most difficult problems in modern medicine is facial pain. Sometimes an experienced doctor does not immediately recognize the symptoms and makes a misdiagnosis. The causes of facial pain are numerous. Therefore, the patient should be examined by physicians of several specializations.
Keywords
Facial Pain, Injuries, TN, TMD, CRS
Introduction
Facial pain occurring in the absence of trauma may be caused by a variety of disorders, many of which may be associated with referred pain, thereby making accurate localization of the source difficult [1]. For this reason, a careful examination of the face, orbits, eyes, oral and nasal cavities, auditory canals, and temporomandibular joints is an essential aspect of the evaluation of these patients.
Pain can result from many different disease processes [2]. The most common causes of facial pain are trauma, sinusitis, and dental disease. The history suggests the diagnosis, which is usually confirmed with the physical findings. With appropriate treatment and resolution of the disease, the pain also abates. Sometimes the cause of the pain is not apparent or the pain does not resolve with the other symptoms.
The trigeminal nerve (cranial nerve V) supplies sensation to the face. The first division (ophthalmic) supplies the forehead, eyebrows, and eyes. The second division (infraorbital) supplies the cheek, nose, and upper lip and gums. The third division (mandibular) supplies the ear, mouth, jaw, tongue, lower lip, and submandibular region. When pain is located in a very specific nerve distribution area, lesions involving that nerve must be considered. Tumors involving the nerve usually cause other symptoms, but pain may be the only complaint, and presence of a tumor at the base of the skull or in the face must be ruled out. When the work-up is negative, the diagnosis may be one of many types of neuralgia, which is a pain originating within the sensory nerve itself. Treatment is medical or, in some cases, surgical.
After immobilization, patients who are unconscious without respiratory effort require intubation to establish a functional airway, and this must be a first priority [3]. Laryngoscopically guided oral intubation is the technique of choice and must be undertaken without movement of the cervical spine; an assistant is essential in this regard and should remain at the patient’s head providing constant, in-line stabilization. Patients with inspiratory effort may be nasotracheally intubated provided that significant maxillofacial, perinasal, or basilar skull injuries are not present; when present or suspected, nasotracheal intubation is relatively contraindicated.
Facial pain remains a diagnostic and therapeutic challenge for both clinicians and patients [4]. In clinical practice, patients suffering from facial pain generally undergo multiple repeated consultations with different specialists and receive various treatments, including surgery. Many patients, as well as their primary care physicians, mistakenly attribute their pain as being due to rhinosinusitis when this is not the case. It is important to exclude non-sinus-related causes of facial pain before considering sinus surgery to avoid inappropriate treatment. Unfortunately, a significant proportion of patients have persistent facial pain after endoscopic sinus surgery (ESS) due to erroneous considerations on aetiology of facial pain by physicians. It should be taken into account that neurological and sinus diseases may share overlapping symptoms, but they frequently co-exist as comorbidities. The aim of this review was to clarify the diagnostic criteria of facial pain in order to improve discrimination between sinogenic and non-sinogenic facial pain and provide some clinical and diagnostic criteria that may help clinicians in addressing differential diagnosis.
History
Facial pain is pain localised to the face, and the diagnosis of facial pains has puzzled clinicians for centuries [5]. Some of the confusion is related to the delimitation of the facial structure and how pain is classified. The face is here defined as the part of the head that is limited by the hairline, by the front attachment of the ear and by the lower jaw, both the rear edge and the lower horizontal part of the jaw. The face also includes the oral and nasal cavity, the sinuses, the orbital cavity and the temporomandibular joint. Pain in the facial region can be classified in multiple ways, for example according to underlying pathology (malignant vs. non-malignant), the temporal course (acute vs. chronic), underlying pathophysiology (neuropathic, inflammatory or idiopathic), localisation (superficial vs. deep), the specific structure involved (the sinus joint, skin etc), and underlying etiology (infection, tumour etc). In some instances, the diagnosis of facial pain focuses on the involved structure, for example temporomandibular joint disorder, in other cases it is the underlying pathology (sinusitis), and in others it is the specific character of the pain that will dictate the diagnosis (e.g. trigeminal neuralgia).
A history of carious dentition in association with a gnawing, intolerable pain in the jaw or infraorbital region is seen in patients with gingival or dental abscesses [1]. Pressurelike pain or aching in the area of the frontal sinuses, supraorbital ridge, or infraorbital area in association with fever, nasal congestion, postnasal discharge, or a recent upper respiratory tract infection suggests acute or chronic sinusitis. Redness, swelling, and pain around the eye are suggestive of periorbital cellulitis. The rapid onset of parotid or submandibular area swelling and pain, often occurring in association with meals, is characteristic of obstruction of the salivary duct as a result of stone. Trigeminal neuralgia produces excruciating, lancinating facial pain that occurs in unexpected paroxysms, is initiated by the tactile stimulation of a “trigger point” or simply by chewing or smiling. Temporomandibular joint dysfunction produces pain related to chewing or jaw movement and is most commonly seen in women between the ages of 20 and 40 years; patients may have a history of recent injury to the jaw, recent dental work, or long-standing malocclusion. Facial paralysis associated with facial pain may be noted in patients with malignant parotid tumors. Dislocation of the temporomandibular joint causes sudden local pain and spasm and inability to close the mouth. Acute dystonic reactions to the phenothiazines and antipsychotic medications may closely simulate a number of otherwise perplexing facial and ocular presentations and must be considered. Acute suppurative parotitis usually occurs in the elderly or chronically debilitated patient and causes the rapid onset of fever, chills, and parotid swelling and pain, often involving the entire lateral face.
Injuries
Facial injuries are among the most common emergencies seen in an acute care setting [6]. They range from simple soft tissue lacerations to complex facial fractures with associated significant craniomaxillofacial injuries and soft tissue loss. The management of these injuries generally follows standard surgical management priorities but is rendered more complex by the nature of the numerous areas of overlap in management areas, such as airway, neurologic, ophthalmologic, and dental. Also, the significant psychological nature of injuries affecting the face and the resultant aftermath of scarring can have devastating and long-lasting consequences. Despite the fact that these injuries are exceedingly common, they are cared for by a large group of different specialists and as such have a remarkably heterogeneous presentation and diverse treatment schema. Nonetheless, guiding principles in the care of these injuries will provide the basis for the best possible outcomes. The following questions will guide general management and provide a framework for understanding the principles in the acute care of patients with facial injuries and trauma.
Despite the extremely common presentation of such injuries, there remains little standardization on repairing and then caring for the wounds or lacerations. There is great variation in the repair of lacerations as well as the different materials used to repair them. This is again because of the numerous different specialties involved in the care of the injuries and their desires to provide the best possible outcome with regard to scarring. Pediatricians, emergency department personnel, and surgeons may not all agree on the best modalities for repair. Placement as well as type of dressing are also controversial.
The timing of facial skin laceration closure is the same as that of any open wound. The presence of contaminating factors in the management of wound would generally not allow closure after six hours and would favor delayed closure. However, clinical practice is slightly more variable with facial lacerations because of the uniquely sensitive nature of facial scarring. Although we generally ascribe to experimental data regarding timing of closure, in practice the six-hour rule is often overlooked with an attempt to be vigorous in cleaning the wound. The presence of exceptionally rich blood supply in the face is also deemed of benefit in extending the six-hour rule.
TN
Facial pain, for all its rarity, can be a significant cause of morbidity when present [7]. The two types of non-odontological causes of facial pain that appear to be the most likely to be mistaken one for the other are trigeminal neuralgia (TN) and what used to be called atypical facial pain, but that is now called persistent idiopathic facial pain (PIFP). Confusion between causes of facial pain persists despite the fact that the diagnosis of classical TN should be rather straightforward and not present diagnostic difficulties to the trained clinician. (The term classical TN is generally restricted to TN caused by neurovascular compression.) The caveat is that secondary causes of TN need to be considered, and the cause of classical TN needs to be established for reasons that will be discussed later. A common mistake that should not be made is to treat TN medically without establishing the cause. PIFP, on the other hand, is a diagnostic problem that confronts us head on. Clearly stated guidelines are in fact ambiguous. Descriptive terms include dull, poorly defined, non-localized.
Individuals in whom attacks of pain last minutes to hours, or are persistent or chronic, waxing and waning over the course of the day, or in whom pain extends beyond one division of the trigeminal nerve, may still be mistakenly diagnosed as having trigeminal neuralgia. Such individuals may point to one side of the face as the site of their pain or may indicate that pain is bilateral. Their pain may be further atypical in lacking the usual triggers of pain such as brushing teeth or touching a trigger area. Such pain that is atypical for TN is a different kind of facial pain than classical TN. However, even in cases that are not characteristic trigeminal neuralgia, chewing, and even speaking, for example, may be triggers. Chewing and speaking activate orofacial and neck muscles, and are accompanied by small movements at the cervical–cranial junction. Nociceptive sites in these muscles may be activated by chewing or speaking. Patients with atypical facial pain are unlikely to have trigeminal neuralgia, and more likely to have what is now called persistent idiopathic facial pain (PIFP).
The diagnosis of classical TN is made on the basis of a characteristic history of lightning-like sharp, electrical pain that is felt in one division of the trigeminal nerve, leaving a dull after pain that lasts for a variable, usually short, period of time. There is often a trigger, but there does not need to be one. The attacks are typically infrequent at first, but become more frequent with the passage of time, and may increase in frequency to occur hundreds of times a day. Remissions occur, but relapses become more frequent with aging. There is no dullness or loss of feeling reported. Some patients tell atypical stories in which pain crosses divisions of the trigeminal nerve, or paroxysms of pain last longer than lightning attacks of pain. The neurological examination is normal in classical TN. Motor and sensory examination of the face in particular is normal in classical TN, but is useful in identifying secondary trigeminal nerve dysfunction that could lead to a diagnosis of secondary TN or trigeminal neuropathy. The same is true of the blink and other trigeminal reflex tests, as the presence or absence of an abnormal result does not affect the diagnosis of TN, but may indicate a need to examine for causes of secondary TN.
TMD
Painful temporomandibular disorder (TMD) is the most frequent form of chronic orofacial pain, affecting an estimated 11.5 million US adults with annual incidence of 3.5%. As with several other types of chronic, musculoskeletal pain, the symptoms are not sufficiently explained by clinical findings such as injury, inflammation, or other proximate cause [8]. Moreover, studies consistently report that TMD symptoms exhibit significant statistical overlap with other chronic pain conditions, suggesting the existence of common etiologic pathways. Most studies of overlap with orofacial pain have focused on selected pain conditions, classified according to clinical criteria (eg, headaches, cervical spine dysfunction, and fibromyalgia), location of self-reported pain (eg, back, chest, stomach, and head), or the number of comorbid pain conditions. Although there is a long tradition of depicting overlap between pain conditions qualitatively using Venn diagrams, we know of few studies that have quantified the degree of overlap between TMD and pain at multiple locations throughout the body.
Overlap of pain symptoms can occur when there are common etiologic factors contributing to each of the overlapping pain conditions. One example is diabetes that contributes, etiologically, to neuropathy in the feet and retinopathy in the eye, thereby creating overlap, statistically, of diseases at opposite ends of the body. The etiologic factor most widely cited to account for overlap of pain conditions is central sensitization, defined as “amplification of neural signaling within the central nervous system (CNS) that elicits pain hypersensitivity.” The amplification means that otherwise innocuous sensations are perceived as painful (ie, allodynia) and that formerly mildly painful stimuli now evoke severe pain (ie, hyperalgesia). However, somatosensory afferent inputs into the CNS are segmentally organized, making it plausible that sensitization is not uniform throughout the neuraxis.
Regardless of pain location, overlap creates serious problems for patients, adding to the suffering and disability caused by a single pain condition, and potentially complicating diagnosis and treatment for one or all of the overlapping conditions. This has broader implications for patients with multiple chronic illnesses who have poorer health outcomes and generate significantly greater health care costs than patients with a single illness. Thus, the aim of this epidemiological study was to quantify the degree of overlap between facial pain and pain reported elsewhere in the body.
CRS
Unfortunately, little is known of the underlying mechanisms that produce pain associated with CRS (chronic rhinosinusitis), but several mechanisms that may all contribute to some degree to the manifestation of facial pain in CRS have been postulated [9]. It has been hypothesized that occlusion of the osteomeatal complex may lead to gas resorption of the sinuses with painful negative pressures, yet most subjects with CRS have an open osteomeatal complex. Patients’ observations that pain and pressure is postural may reflect painful dilatation of vessels; however, postural pain is also observed in subjects with simply tension type headache. Local inflammatory mediators can excite nerves locally within the sinonasal mucosa directly illiciting pain. For example, maxillary rhinosinusitis can cause dental pain through the stimulation of the trigeminal nerve. In addition, local tissue destruction and inflammatory mediators may influence the central mechanism of pain via immune-to-brain communication through afferent autonomic neuronal transmission, transport across the blood brain barrier through the circumventricular organs and/or direct passage across the blood brain barrier.
The impact of inflammatory cytokines on the central nervous system have been associated with both pain as well as other health-related factors associated with chronic inflammation and sickness behavior such as disruption of sleep and mood. Interleukin-1[Beta] (IL-1[Beta]) and tumor necrosis factor-[alpha] (TNF-[alpha]) are two key pro-inflammatory cytokines with a pivotal role in the immune-to-brain pathway of communication. They are both upregulated in subjects with CRS and are two potential pro-inflammatory cytokines that have been implicated in fatigue, sleep dysfunction, depression, and pain. Characterizing the differential cytokine profiles of CRS subtypes and identifying associated symptom profiles may be an important step in understanding why some subjects experience greater health-related burden of disease, which is an important predictor of electing surgical intervention over continued medical therapy.
Examination
Carious dentition, gingivitis, and gingival abscesses may be diagnosed by inspection of the oral cavity and face [1]. Percussion tenderness over the involved tooth, swelling and erythema of the involved side of the face, and fever may be noted in patients with deep abscesses. Percussion tenderness to palpation or pain over the frontal or maxillary sinuses with decreased transillumination of these structures suggests sinusitis. Redness, tenderness, and swelling around the eye may suggest periorbital cellulitis. Pain with eye movement or exophthalmos may suggest an orbital cellulitis or abscess. Malocclusion may be noted in patients with temporomandibular joint dysfunction; tenderness on palpation of the temporomandibular joint, often best demonstrated anteriorly in the external auditory canal with the mouth open, is noted as well. Patients with temporomandibular joint dislocation present with anxiety, local pain, and inability to close the mouth. Unusual ocular, lingual, pharyngeal, or neck symptoms should suggest possible acute dystonic reactions. A swollen, tender parotid gland may be seen in patients with acute parotitis, in parotid duct obstruction secondary to stone or stricture, and in patients with malignant parotid tumors; evidence of facial paralysis should be sought in these latter patients. Palpation of the parotid duct along the inner midwall of the cheek will occasionally reveal a nodular structure consistent with a salivary duct stone. In patients with herpes zoster, typical lesions may be noted in a characteristic dermatomal pattern along the first, second, or third division of the trigeminal nerve or in the external auditory canal. It is important to remember that patients with herpes zoster may have severe pain before the development of any cutaneous signs. This diagnosis should always be considered when vague or otherwise undefinable facial pain syndromes are described. Simple erythema may be the first cutaneous manifestation of herpetic illness. Patients with trigeminal neuralgia have an essentially normal examination.
Ventilation
In patients with inspiratory effort but without adequate ventilation, mechanical obstruction of the upper airway should be suspected and must be quickly reversed [3]. The pharynx and upper airway must be immediately examined and any foreign material removed either manually or by suction. Such material may include blood, other secretions, dental fragments, and foreign body or gastric contents, and a rigid suction device or forceps is most effective for its removal. Obstruction of the airway related to massive swelling, hematoma, or gross distortion of the anatomy should be noted as well, because a surgical procedure may then be required to establish an airway. In addition, airway obstruction related to posterior movement of the tongue is extremely common in lethargic or obtunded patients and is again easily reversible. In this setting, insertion of an oral or a nasopharyngeal airway, simple manual chin elevation, or the so-called jaw thrust, singly or in combination, may result in complete opening of the airway and may obviate the need for more aggressive means of upper airway management. Chin elevation and jaw thrust simply involve the manual upward or anterior displacement of the mandible in such a way that airway patency is enhanced. Not uncommonly, insertion of the oral airway or laryngeal mask airway may cause vomiting or gagging in semialert patients; when noted, the oral airway should be removed and chin elevation, the jaw thrust, or the placement of a nasopharyngeal airway undertaken. If unsuccessful, patients with inadequate oxygenation require rapid sequence oral, or nasotracheal, intubation immediately.
If an airway has not been obtained by one of these techniques, Ambu-bag–assisted ventilation using 100% oxygen should proceed while cricothyrotomy, by needle or incision, is undertaken rapidly. In children younger than 12 years, surgical cricothyrotomy is relatively contraindicated and needle cricothyrotomy (using a 14-gauge needle placed through the cricothyroid membrane), followed by positive pressure insufflation, is indicated. During the procedure, or should the procedure be unsuccessful, Ambu-bag–assisted ventilation with 100% oxygen and an oral or a nasal airway may provide adequate oxygenation.
In addition, rapidly correctable medical disorders that may cause central nervous system and respiratory depression must be immediately considered in all patients and may, in fact, have precipitated the injury by interfering with consciousness. In all patients with abnormalities of mental status, but particularly in those with ventilatory insufficiency requiring emergent intervention, blood should immediately be obtained for glucose and toxic screening, and the physician should then prophylactically treat hypoglycemia with 50 mL of 50% D/W, opiate overdose with naloxone (0.4–2.0 mg), and Wernicke encephalopathy with thiamine (100 mg). All medications should be administered sequentially and rapidly by intravenous injection and any improvement in mental status or respiratory function carefully noted. Should sufficient improvement occur, other more aggressive means of airway management might be unnecessary.
Conclusion
Facial pain can be painful and frightening. Facial pain can be caused by a cold, sinusitis, muscle tension in the jaw or neck, dental problems, nerve irritation or trauma. One of the most common causes is sinusitis, but another common cause is jaw dysfunction which often occurs after trauma and can lead to jaw injury or meniscus irritation. In the case of major trauma, fractures of the jawbone or fractures of the face may also occur.
#Facial Pain#Injuries#TN#TMD#CRS#jcrmhs#Journal of Clinical Case Reports Medical Images and Health Sciences impact factor
3 notes
·
View notes
Text
Understanding the Role of a Maxillofacial Surgeon: Insights from Dr. Anurag Bhargava, a Leading Maxillofacial Surgeon in Indore
Maxillofacial surgery is a specialized field that addresses complex conditions of the face, mouth, and jaw. It requires a unique blend of dental, medical, and surgical expertise. Dr. Anurag Bhargava, a renowned maxillofacial surgeon in Indore, provides invaluable insights into this fascinating field, highlighting its importance and the transformative impact it can have on patients' lives.

What is Maxillofacial Surgery?
Maxillofacial surgery, also known as oral and maxillofacial surgery (OMS), involves surgical interventions to treat diseases, injuries, and defects of the face, mouth, teeth, and jaws. This specialty bridges the gap between medicine and dentistry, requiring a deep understanding of both fields. Procedures can range from corrective jaw surgery and facial trauma reconstruction to dental implants and cosmetic enhancements.
Common Conditions Treated by Maxillofacial Surgeons
1. Facial Trauma:
Fractures: Maxillofacial surgeons treat fractures of the jaw, cheekbones, and eye sockets, ensuring proper alignment and healing.
Soft Tissue Injuries: These include lacerations and injuries to the facial skin and muscles, often requiring precise suturing to minimize scarring.
2. Corrective Jaw Surgery (Orthognathic Surgery):
Malocclusion: This involves correcting misaligned jaws to improve chewing, speaking, and facial aesthetics.
Sleep Apnea: Surgical intervention can help reposition the jaw and airway structures to alleviate obstructive sleep apnea.
3. Congenital Disorders:
Cleft Lip and Palate: Maxillofacial surgeons perform surgeries to repair these congenital deformities, improving function and appearance.
Craniofacial Anomalies: These are complex conditions affecting the skull and face, often requiring multi-disciplinary surgical approaches.
4. Dental and Oral Health:
Impacted Teeth: Removal of impacted wisdom teeth and other problematic teeth.
Dental Implants: Placement of dental implants to replace missing teeth and restore oral function.
5. Temporomandibular Joint (TMJ) Disorders:
TMJ Dysfunction: Treatment includes surgical and non-surgical options to alleviate pain and improve jaw function.
The Importance of Maxillofacial Surgery
Maxillofacial surgery is vital for restoring both function and aesthetics. Conditions affecting the face and jaw can have profound impacts on a person's ability to eat, speak, and breathe, as well as their self-esteem and social interactions. A skilled maxillofacial surgeon can significantly enhance a patient's quality of life through meticulous surgical interventions.
Dr. Anurag Bhargava: Expertise and Approach
As a leading maxillofacial surgeon in Indore, Dr. Anurag Bhargava combines extensive training and experience with a patient-centered approach. His expertise spans a wide range of maxillofacial procedures, ensuring comprehensive care for his patients.
1. Personalized Treatment Plans:
Comprehensive Evaluation: Dr. Bhargava conducts thorough evaluations to understand each patient's unique needs and conditions.
Customized Care: He develops personalized treatment plans, considering both functional and aesthetic goals.
2. Advanced Surgical Techniques:
Minimally Invasive Procedures: Whenever possible, Dr. Bhargava employs minimally invasive techniques to reduce recovery time and enhance outcomes.
State-of-the-Art Technology: He utilizes the latest technology and surgical advancements to ensure precision and safety.
3. Holistic Patient Care:
Pre- and Post-Operative Support: Dr. Bhargava provides detailed guidance and support throughout the surgical process, from pre-operative preparation to post-operative recovery.
Interdisciplinary Collaboration: He works closely with other specialists, including orthodontists, plastic surgeons, and ENT specialists, to provide comprehensive care for complex cases.
Success Stories and Patient Testimonials
Dr. Anurag Bhargava’s expertise and compassionate approach have transformed the lives of many patients. Here are a few success stories:
1. Corrective Jaw Surgery: A young woman with severe malocclusion and facial asymmetry underwent orthognathic surgery. Post-surgery, she experienced improved chewing function, enhanced speech, and boosted self-confidence.
2. Facial Trauma Reconstruction: A patient with multiple facial fractures from a car accident received reconstructive surgery. Dr. Bhargava’s skillful intervention restored the patient’s facial structure and function, facilitating a remarkable recovery.
3. Cleft Lip and Palate Repair: A child born with a cleft lip and palate underwent surgical repair. The surgery not only improved the child’s appearance but also enhanced their ability to eat, speak, and breathe properly.
Why Choose Dr. Anurag Bhargava?
Choosing the right maxillofacial surgeon is crucial for achieving optimal outcomes. Here’s why Dr. Anurag Bhargava stands out:
Extensive Experience: With years of experience and numerous successful surgeries, Dr. Bhargava is a trusted expert in the field.
Comprehensive Care: From consultation to recovery, he provides thorough and compassionate care.
Patient-Centered Approach: Dr. Bhargava prioritizes patient comfort, safety, and satisfaction, ensuring a positive surgical experience.
Conclusion
Maxillofacial surgery is a transformative specialty that addresses complex facial and jaw conditions, enhancing both functionality and aesthetics. Dr. Anurag Bhargava, a leading maxillofacial surgeon in Indore, offers expert care and personalized treatment plans, ensuring the best possible outcomes for his patients. If you’re seeking skilled and compassionate care for maxillofacial issues, Dr. Bhargava is the go-to expert in Indore.
For more information or to schedule a consultation, visit Dr. Anurag Bhargava’s website.
2 notes
·
View notes
Text
maxillofacial avulsion is my favourite type of injury
dont search it up
10 notes
·
View notes
Text
Have an escooter? Please consider wearing a downhill helmet to protect your face
As someone whose relatives have escooters, and someone who has seen a lot of close calls with strangers, I wanna share a little-known bit of advice for anyone who's looking into escooters, or who already has one:
If you're on an escooter, you get the most protection by wearing a downhill or full-face helmet!
DO NOT GO HELMET-LESS!

By 'downhill' or 'full face', I mean the helmets that bmx riders use, or motorcycle riders wear, respectively. It sounds like overkill but here's the thing:
Escooters have a very high center of gravity because you're upright on them, and they have small wheels that don't absorb impact very well. It's super easy to go over your handle bars if you even hit a tiny pothole! According to this study where 212 patients presented to an emergency room, 11.8% of the patients had dental injuries
A lot of these patients presented with facial lacerations and facial fractures. Overall, 44% of patients needed surgery (5.9% needed major surgery and 38.2% needed minor surgery), and 50% needed maxillofacial follow-up
All 212 patients in this study received a head or face injury. 82% of patients didn't wear a helmet
Some more articles explaining dental injuries from escooter use:
Dental injuries on the rise thanks to e-scooter use
New study from U of A professor warns of dangers of scooter usage
In this Korean study, most patients without a helmet suffered some kind of facial trauma
This isn't just a matter of speed, either. If you're not convinced how often people go over the handlebars at lower speeds too, check out the first 25 seconds of this video by Electric Scooter Guide. That's a lot of faceplants at lower speeds! Or if you want a full playlist of people going over their handlebars, I've got you covered. Again see how many of them are faceplants!
And at higher speeds? It's not good. MAJOR TRIGGER WARNING for gore and death: here you will find a graphic picture of someone who was in an escooter accident, they weren't wearing a helmet and they sadly lost their life
I'll link some reddit posts of close calls where the posters were really glad to be wearing downhill/full face helmets, these are either text-only posts, or simple pics of scratched-up helmets: 1 2 3
Most of these accidents don't even involve other people or vehicles! According to this infographic, 80.2% of escooter accidents are 'falls':
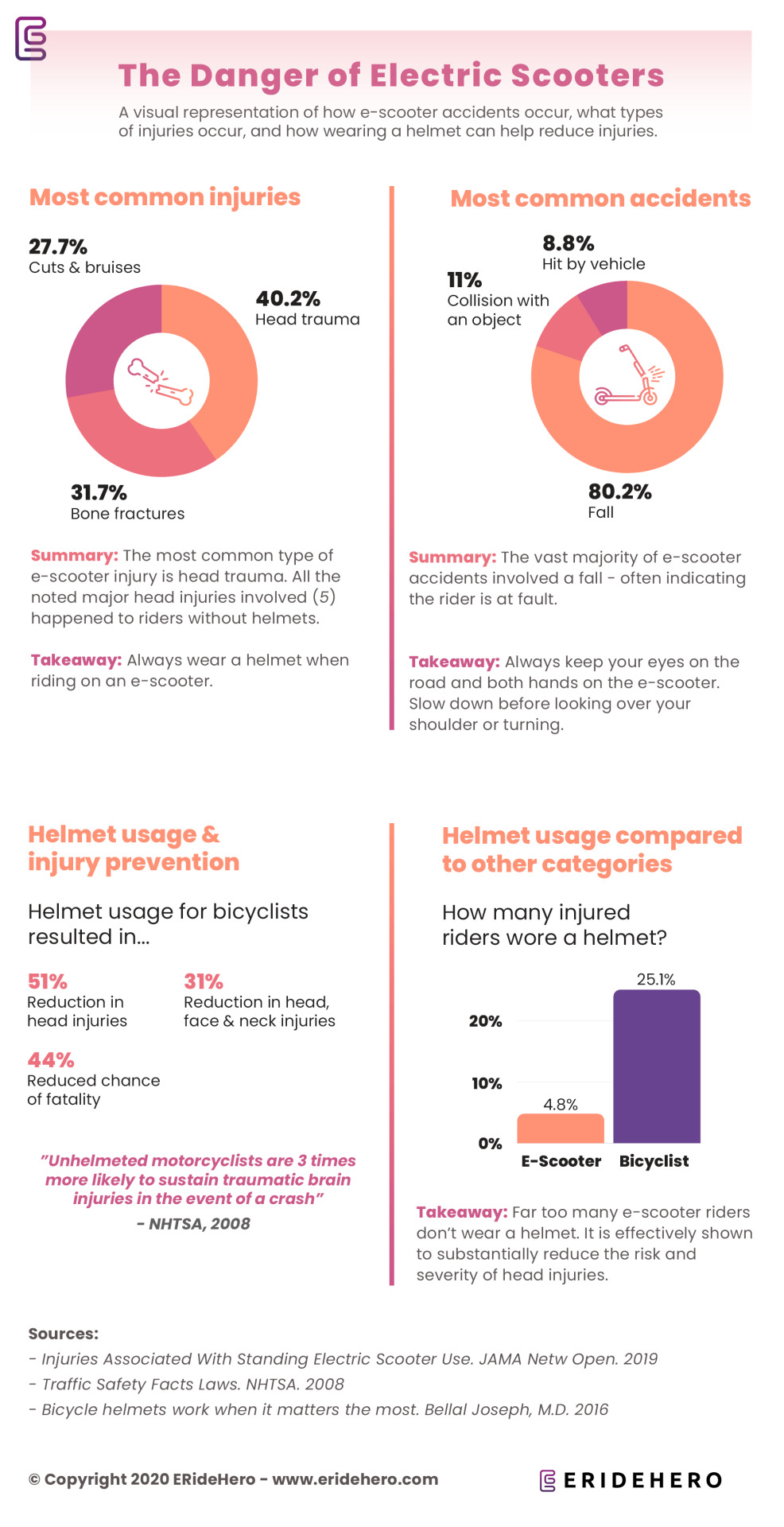
So, now what?
If you don't currently have a helmet and are considering getting one, yay! Your first impulse might be to go out and buy a regular bicycle helmet, but remember: a lot of these injuries happen around your jaw and the front of your face! A bicycle helmet doesn't protect that part! When you fall on an escooter, you're likely to fall in ways that are different from a fall on a bike. So consider a downhill helmet (or a full-face, if you wanna channel your inner motorhead)!
Yeah you'll look dorky, but you'll get home in one piece if you get unlucky on the way there 👍
#i was on my way home and saw a THING omg they were so close to hitting their face my heart skipped a beat#if even one person sees this post and remembers it i'll be happy#escooter#escooters#e-scooters#psa#safety#scooters#micromobility#commuting#ninebot#segway#electric scooter#electric scooters#injury ment cw#injury cw
10 notes
·
View notes
Text
Unmasking Degloved Faces
Facial trauma is a term that refers to any physical injury to the face, particularly the structures of the head and neck region. This type of trauma can result in severe facial disfigurement, including degloving injuries. Understanding the causes, management, and rehabilitation of degloved faces is crucial in providing appropriate care and support for affected individuals.
Facial trauma can occur due to various reasons, including:
Motor vehicle accidents
Workplace accidents
Sports injuries
Physical assaults
Accidental falls
These incidents can lead to the separation of the skin, soft tissues, and underlying structures from the facial bones. This degloving injury is often associated with significant damage to blood vessels, nerves, and facial function. The severity of the trauma can range from minor lacerations to extensive facial fractures.
Facial reconstruction surgeries
Facial reconstruction surgeries play a vital role in the management of degloved faces. The primary goals of these surgical procedures are to restore facial form and function, improve aesthetics, and enhance the patient's quality of life. The specific surgical techniques employed depend on the extent and nature of the facial trauma.
Some common facial reconstruction surgeries include:
Skin grafting: In cases where there is a loss of skin due to degloving, a skin graft may be performed. This involves taking healthy skin from another part of the body (donor site) and transplanting it onto the affected area.
Soft tissue reconstruction: Degloved faces often require reconstruction of soft tissues, including muscles, tendons, and blood vessels. Techniques such as tissue flaps, microvascular surgery, and facial reanimation procedures may be utilized.
Orthognathic surgery: Severe facial trauma can result in misalignment of the jaws. Orthognathic surgery aims to correct these skeletal deformities, improving function and facial aesthetics.
Maxillofacial implants: In cases where there is significant bone loss, maxillofacial implants may be used to restore facial symmetry and provide support for other facial structures.
Reconstructive rhinoplasty: Injury to the nose can cause functional and aesthetic problems. Reconstructive rhinoplasty can address these issues, improving breathing and restoring the natural appearance of the nose.
It is important to note that facial reconstruction surgeries are highly complex and require the expertise of a multidisciplinary team of healthcare professionals. Surgeons, plastic surgeons, oral and maxillofacial surgeons, and other specialists collaborate closely to develop comprehensive treatment plans tailored to each patient's unique needs.
Post-surgical rehabilitation
Rehabilitation plays a critical role in the overall management of degloved faces. It is aimed at maximizing functional recovery, promoting psychological well-being, and facilitating the reintegration of patients into their daily lives.
The rehabilitation process may involve:
Physical therapy: Physical therapists work with patients to restore muscle strength, flexibility, and range of motion. They utilize exercises, manual therapy techniques, and other modalities to optimize functional outcomes.
Speech and swallowing therapy: Facial trauma can affect speech and swallowing functions. Speech-language pathologists assess and treat communication and swallowing disorders, developing strategies to improve these functions.
Psychological support: Dealing with facial trauma and its consequences can have a significant psychological impact on patients. Mental health professionals provide counseling and support to help individuals cope with emotional challenges, promote self-esteem, and enhance body image.
Prosthetic rehabilitation: In cases where facial reconstruction is not feasible or desired, prosthetic rehabilitation may be considered. Specially designed facial prostheses can help restore appearance and function.
Throughout the rehabilitation process, close collaboration between healthcare professionals, patients, and their families is crucial. The treatment plan should be individualized, taking into account the specific needs and goals of each patient.
In conclusion, understanding the causes, management, and rehabilitation of degloved faces is essential in providing comprehensive care for individuals with facial trauma. Facilitating the recovery of form and function through facial reconstruction surgeries and post-surgical rehabilitation can significantly improve the quality of life for affected individuals. It is imperative for healthcare professionals to stay updated on the latest advancements in this field and adopt a multidisciplinary approach to deliver optimal care
2 notes
·
View notes
Text
Recent Advances in Oral and Maxillofacial Surgery | Transforming Patient Care
Oral and maxillofacial surgery has seen significant advancements in recent years, enhancing precision, safety, and recovery outcomes for patients. With cutting-edge technology and innovative techniques, the field continues to evolve, providing improved solutions for complex facial and jaw conditions.
One of the key advances in oral and maxillofacial surgery is the use of 3D imaging and computer-assisted planning, allowing surgeons to achieve greater accuracy in reconstructive procedures. Additionally, minimally invasive techniques have reduced recovery times, offering patients faster healing with minimal discomfort.
For those wondering, what is maxillofacial surgery? It is a specialized branch of surgery that focuses on treating diseases, injuries, and defects in the face, jaw, and mouth. This includes procedures such as corrective jaw surgery, facial trauma treatment, and dental implant placement.
With recent advances in oral and maxillofacial surgery, patients in the UAE and worldwide can now benefit from safer, more efficient treatments tailored to their needs. Learn more about these advancements and expert surgical care at Dr. Gagan Sabharwal’s website.
0 notes
Text
Craniomaxillofacial Devices Market Forecast: Growth, Opportunities, and Emerging Trends
The global craniomaxillofacial devices market size is expected to reach USD 3.5 billion by 2030, registering CAGR of 9.5% from 2023 to 2030, according to a new report by Grand View Research, Inc. Craniofacial surgery treats conditions that affect the head, skull, face, and neck. The rise in the number of facial and head injuries caused due to the road accidents and rise in the number of sports-related injuries expected to boost demand for the craniomaxillofacial devices. Apart from this, increase in the usage of minimally invasive surgeries is also one of the key factors expected to support the market growth.
Organizations such as the American Society of Craniofacial Surgery (ASCFS) and the International Society of Craniofacial Surgery (ISCFS) are conducting a research program in a probe to increase awareness of CMF surgeries, boosting consumer awareness about the craniomaxillofacial devices.
Neck injuries are one of the most common types of injuries in vehicle accidents. Over 800, 000 cases of vehicle crashes involving neck injuries reported per year in the U.S. Apart from this, sports injuries, car accidents, and falls were some of the leading causes of head injuries in the country. Hence, the U.S. expected to be a key market for the craniomaxillofacial device manufacturers.
Outbreak of the COVID-19 caused the cancellation and rescheduling of the elective surgical procedures, at a global level. For surgeons working in the craniomaxillofacial (CMF) field, surgical procedures were limited to urgent cases such as oncological procedures, emergent airway management, and surgical management of the facial fractures.
As the virus, transmission was high in CMF procedures, various professional societies in the fields of dentistry maxillofacial surgery recommended limited uptake of craniomaxillofacial procedures, which limited the demand for craniomaxillofacial devices in 2020. However, the market has shown significant recovery in 2021 as medical surgeries resumed under strict COVID-19 protocols.
Gather more insights about the market drivers, restrains and growth of the Craniomaxillofacial Devices Market
Craniomaxillofacial Devices Market Highlights
• In 2022, the CMF plate and screw fixation segment dominated the market due to the rise in the number of surgeries requiring bone stabilization
• Technological advancements in bio absorbable material make it the fastest-growing during the forecast period
• Temporomandibular Joint Replacement segment expected to witness the highest growth during the forecast period
• The neurosurgery and ENT surgery segment expected to show lucrative growth due to an increase in the volume of surgical procedures pertaining to trauma and the adoption of deep brain stimulation procedures
• Asia Pacific market is expected to be the fastest-growing during the forecast period due to the presence of untapped opportunities and constantly improving healthcare infrastructure
Craniomaxillofacial Devices Market Segmentation
Grand View Research has segmented the global craniomaxillofacial devices market based on the product, material, application, and region:
Craniomaxillofacial Devices Product Outlook (Revenue, USD Million; 2018 - 2030)
• Cranial Flap Fixation
• CMF Distraction
• Temporomandibular Joint Replacement
• Thoracic Fixation
• Bone Graft Substitute
• CMF Plate and Screw Fixation
Craniomaxillofacial Devices Material Outlook (Revenue, USD Million; 2018 - 2030)
• Metal
• Bio absorbable material
• Ceramics
Craniomaxillofacial Devices Application Outlook (Revenue, USD Million; 2018 - 2030)
• Neurosurgery & ENT
• Orthognathic and Dental Surgery
• Plastic surgery
Craniomaxillofacial Devices Regional Outlook (Revenue, USD Million; 2018 - 2030)
• North America
o U.S.
o Canada
• Europe
o Germany
o UK
o Spain
o France
o Italy
o Denmark
o Norway
o Sweden
• Asia Pacific
o China
o India
o Japan
o South Korea
o Australia
o Thailand
• Latin America
o Brazil
o Mexico
o Argentina
• MEA
o South Africa
o Saudi Arabia
o UAE
o Kuwait
Order a free sample PDF of the Craniomaxillofacial Devices Market Intelligence Study, published by Grand View Research.
#Craniomaxillofacial Devices Market#Craniomaxillofacial Devices Market Analysis#Craniomaxillofacial Devices Market Report#Craniomaxillofacial Devices Market Size#Craniomaxillofacial Devices Market Share
0 notes
Text
Atrauma: Advancing Surgical Techniques for Better Patient Outcomes

Atrauma refers to surgical techniques and instruments designed to minimize tissue damage during medical procedures. The goal is to enhance healing, reduce post-operative complications, and improve patient outcomes. By utilizing atraumatic instruments and approaches, surgeons can perform procedures with greater precision while preserving delicate tissues, reducing inflammation, and lowering the risk of infection. Atrauma concept has become increasingly important in modern medicine, particularly in microsurgery, cardiovascular surgery, and minimally invasive procedures.
The Importance of Atraumatic Surgical Techniques
Traditional surgical procedures often involve forceful manipulation of tissues, leading to increased trauma, prolonged recovery times, and higher risks of complications. Atraumatic techniques aim to counter these issues by using specially designed instruments that distribute pressure more evenly, preventing unnecessary damage. In addition to improving patient comfort, these methods also contribute to better long-term outcomes by preserving the integrity of soft tissues, blood vessels, and nerves.
In microsurgery, for instance, atraumatic handling of tissues is crucial for the success of delicate procedures such as nerve repairs and vascular anastomoses. Similarly, in laparoscopic and robotic surgeries, specialized atraumatic forceps and clamps ensure precise manipulation while minimizing tissue injury.
Atraumatic Surgical Instruments
Atraumatic surgical instruments are specifically designed to reduce pressure, friction, and mechanical stress on tissues. These include forceps, clamps, scissors, and retractors with smooth or finely serrated edges that prevent crushing and tearing. One of the most well-known examples is the Debakey forceps, widely used in vascular and cardiac surgeries for grasping delicate blood vessels without causing damage.
Hemostatic clamps, such as Bulldog and Satinsky clamps, are also designed with atraumatic principles in mind. Their smooth jaws apply even pressure, preventing unnecessary bruising or occlusion of blood flow. Similarly, specialized suturing techniques, combined with atraumatic needles, help reduce the risk of tissue necrosis and scarring, especially in cosmetic and reconstructive surgeries.
Applications in Various Surgical Specialties
Atraumatic techniques are widely employed in different fields of surgery to improve patient outcomes. In cardiovascular surgery, the use of atraumatic clamps and forceps helps preserve the function of delicate blood vessels. In neurosurgery, where precision is critical, instruments such as the Penfield dissector allow for gentle manipulation of brain and spinal cord tissues.
Orthopedic and plastic surgeons also rely on atraumatic instruments to reduce tissue stress and enhance post-operative healing. In dental and maxillofacial surgery, atraumatic extraction forceps help preserve the surrounding bone and soft tissue, making future restorative procedures more successful. The integration of these techniques into laparoscopic and robotic-assisted surgeries has further advanced the field by reducing post-surgical pain and scarring.
Benefits of Atraumatic Surgery
The use of atraumatic techniques in surgery offers numerous benefits. Reduced tissue damage leads to faster healing times, lower infection rates, and minimal scarring. Patients experience less post-operative pain and shorter hospital stays, making recovery more efficient and cost-effective. Additionally, preserving tissue integrity reduces the need for corrective procedures, further enhancing overall surgical success.
Surgeons also benefit from atraumatic approaches, as they provide better visibility, control, and precision during operations. This not only improves procedural efficiency but also minimizes complications and enhances long-term results.
Conclusion
Atrauma has transformed modern surgical practices, providing safer and more effective solutions for both patients and surgeons. The development and use of atraumatic instruments and techniques continue to evolve, shaping the future of minimally invasive and precision-based medical procedures. As technology advances, the focus on reducing tissue trauma will remain a cornerstone of surgical innovation, ultimately improving healthcare outcomes worldwide.
0 notes
Note
Hey! I love your Henry/Hal fics and would love to hear your commentary on Surfeited with Honey (and the thought of wound-fucking?) or the this thorn, this canker 'verse?
Oh hell yeah, I am ready to tell you about both of these!
Surfeited With Honey
This Thorn, This Canker series
[Behind the cut: discussion of (fictional) parent-child incest and serious consent issues, dysfunctional medieval royal families, wound fingering, violence/injury]
The first thing that occurs to me is that I wouldn’t use the “Other” archive pairing category if I were posting Surfeited today — the fic is more 'other' in the sense of an intermediacy between gen and shipfic than it is other in the sense of being located outside the binary of M's and F's but either way that’s confusing. (But I wrote this fic in 2019 so I would do other stuff differently too, I’m sure.) These two have a relationship that I love exploring at any point along the gen-to-not-gen spectrum as long as it's sufficiently fucked up.
Surfeited is a good example of how men’s shirts are horny-coded in my writing — I think the innermost layers of clothing always carry a little eroticism with them, that hint of being warmed by the body and worn closest to the skin, but that’s what a guy who horny-codes his characters in shirtsleeves would say. I think I just love writing descriptions of Hal looking gross and bedraggled, this thoroughly despoiled beauty. I like that as a chance to evoke his cavalcade of jokes about his martial aspect and unhandsome face in H5 — "Now beshrew my father’s ambition! He was thinking of civil wars when he got me", whew… — but I also just think it’s hot.
Rereading this now I love that Henry sees this disfigurement as somehow keeping Hal from being too pretty for his own good. He’s thinking of Richard naturally and his own inappropriate imaginings of Hal as an object of desire and temptation but usually people settle for growing a beard or getting some wrinkles rather than getting a nearly lethal maxillofacial wound.
It's also really, really obvious that I love using the word "queer".
I love writing wound fingering as specifically wound probing — Henry wondering what’s inside his son, how to take the depth of him, and also Henry wanting to re-wound him or access once more the initial vulnerability so he can savor it at leisure. He’s definitely conceiving of this wound as specifically vaginal, an orifice that can be virginal or habitually revisited, and that makes all the uhhhh actual wound care stuff involved (John Bradmore's treatment of H5's facial wound is a really interesting process) that's very reasonably concerned with making the orifice in question narrower very. Weird. Which I love! I love things to be weird! But whew, I low-key forgot about that.
All my favorite Halhenry things are in evidence here, sublimated desires, the eroticism of violence, Richard's ghost… and poor fucking John Bradmore as unwilling witness who really wishes he was not employed in this specific royal court. Absolutely no surprises that I’m really interested in both the ways power relationships change the relationship of witnesses to what they see and the ways characters in power either restrain themselves due to the scrutiny their position puts them under or let themselves run wild due to the impunity they feel.
My bruise-fingering/superficial injury inspection fic ("means and manners") has a similar weird mix of sublimation and violence -- Henry is talking his way around gay sex in a big way in this fic (not that Hal doesn't also fuck women, and that Henry isn't obsessively fixated on that too, but it would simply be a bridge too far to explicitly conceive of his son being fucked by men) but Hal also is in the awkward position of trying to keep his Eastcheap friends off his dad's radar.
Hal getting maimed horny-style is the common factor in these fics. Bradmore's Philomena and the account of the surgery in it is really cool and has a lot of interesting writing about it.
"The Disappearing Scar of Henry V: Triage, Trauma, and the Treatment of Henry’s Wounding at the Battle of Shrewsbury", Timothy D. Arner
The "Philomena" of John Bradmore And Its Middle English Derivative: A Perspective On Surgery In Late Medieval England, S.J. Lang (this is… fully just Lang's doctoral thesis… but it rules anyway, extreme apologies to any scholar who finds me linking their work in the context of sad erotica)
"Saving Prince Hal: Maxillo-Facial Surgery, 1403", Jo Cummins
…and this is how I came to recall that, fully ten years ago, I wrote a post on f_fa about the Shrewsbury wounding:
I don’t think it occurred to me as a conscious theme at the time I was writing, but across these fics Hal often tries to navigate his father’s moods and his power as both king and father using verbal strategies. It makes sense for practically any Histories character to try and leverage words to achieve an end but with Hal I really think what Henry perceives as so provoking and deliberately sexually antagonizing is in reality an attempt to get him back to a safe distance. Their relationship is really shaped by Henry’s absences from Hal’s early life — his exile and prior to that just being a distant, authoritarian father who didn’t do much to foster personal relationships with his kids — so it’s fairly easy for me to slip into writing their relationship as dysfunctional in this specific way. "means and manners" has Henry disclosing the existence of his own illegitimate children to Hal, and then misreading Hal's rather bewildered reaction to that; the idea of someone else also being his father's biological son but having such a paradigmatically different relationship to him than Hal's own (while not being defined by his relationship to Hal the way Hal's own brothers are in his mind) is upsetting and messy news on a couple levels.
All of these fics are tied together with a bunch of thoughts about the way parent-child incest and specifically royal family parent-child incest is framed in medieval European literature -- so much of Henry's preoccupations is dedicated to the fulfillment of these aggressively gendered male roles (obedient son, good Christian soldier, strong father, strong monarch) but the really confusing and violating stuff that Hal contends with is all informed specifically by literary treatments of father-daughter incest in the era, both because genderfucking with Hal's renunciation of his Eastcheap young-wanton-and-effeminate fuckboy lifestyle is a lot of fun for me and because there aren't any literary treatments (that I know of) of the multiply tabooed same-sex incest to draw on.
My Hanahaki disease series is so fucking silly but I had so much fun with it, the final installment is almost finished so I just need to get my shit together there. Looking through my notes I have a lot of different resources about medieval English (and French) floral symbolism, literary vs. legal treatments of incest in the era, humoral medicine, and the passage in Holinshed's Chronicles where Hal makes an emotionally manipulative public gesture about how if his dad doesn't trust him to be totally blameless and innocent, he should just STAB him right here, here's my knife to do it with, I'm waiting babe, I'd rather be dead than live one day enduring your displeasure :( while wearing a really weird outfit. I didn't even put that in any of these fics (that I can remember) but it's another historiographic element I had in mind writing their dynamic.
The Prince kneeling downe before his father ſayde: Moſt redoubted and ſoueraigne Lord and father, I am this time come to your preſence as your liege man and as your naturall ſonne, in all things to be at your commaundement. And where I vnderſtand you haue in ſuſpition my demeanour agaynſt your grace, you knowe very well, that if I knewe any man wythin thys realme of whome you ſhoulde ſtande in feare, my dutie were to puniſh that perſon, thereby to re|moue that griefe from your heart: Then howe much more ought I to ſuffer death, to eaſe your grace of that griefe which you haue of me, beeing your naturall ſonne and liegeman: and to that ende I haue this day made my ſelfe readie by cõ|feſſion and receyuing of the Sacramẽt: and ther|fore I beſeeche you moſte redoubted Lorde and deare father, for the honour of God, to eaſe your heart of all ſuch ſuſpition as you haue of me, and to diſpatche me here before your knees, with this ſame dagger: and withall hee deliuered vnto the king his dagger, in all humble reuerence, adding further, that his life was not ſo deare to him, that hee wiſhed to liue one daye with his diſpleaſure, and therefore (ſayth he) in thus ridding me out of life, and your ſelfe from all ſuſpition, here in pre|ſence of theſe Lordes, and before God at the day of the generall iudgement, I faythfully proteſt clearly to forgiue you.
(source) (under the heading His ſtrange Apparel)
Also the Pentangle version of "When I Was In My Prime", which is thematically fitting but not something I ended up drawing titles from.
For some reason I also have Hal and Richard's color seasons written down… at least back in the day I saw them as both springs, broadly resembling one another but not in the specifics, which is not NOT part of Henry's messy feelings there. There's also a long, long excerpt from a paper on Pietro d'Abano's understanding of sodomy and specifically anal pleasure/how someone might be able to orgasm from prostate stimulation -- he was writing a couple centuries too early but I'm still trying to figure out how I want to write Henry conceptualizing the prostate. This is a problem that dogs me in every fucking fandom, I swear, and it's never that important, but it's part of getting in the zone, I guess.
#ska writes a thing#why don't i have a histories tag that is specifically for these guys... a tragedy
1 note
·
View note
Text
Facial Trauma Treatment in Panchkula: Restoring Your Confidence with Expert Care

When life takes an unexpected turn, facial injuries can significantly affect your appearance, function, and confidence. At Dr. Sanjay Kalra’s Multispeciality Dental Clinic, we specialize in facial trauma treatment in Panchkula, offering compassionate care backed by advanced dental and maxillofacial expertise. Our goal is to restore not just your face but your confidence and quality of life.
Understanding Facial Trauma and Its Impact
Facial trauma refers to injuries to the face and jaw caused by accidents, falls, or sports-related incidents. These injuries can range from minor lacerations to complex fractures, potentially affecting speech, chewing, and appearance. Immediate and effective treatment is essential to prevent long-term complications.
At Dr. Sanjay Kalra’s clinic, our team of specialists employs cutting-edge techniques to address all types of facial trauma, ensuring optimal results for every patient.
Comprehensive Facial Trauma Treatment
Our approach begins with a thorough evaluation using advanced imaging technology to assess the extent of the injury. Depending on the severity, treatments may include:
Surgical repair of fractures.
Restoration of teeth and jaw alignment.
Aesthetic reconstruction to maintain facial harmony.
With a focus on precision and aesthetics, our team ensures a seamless recovery, leaving minimal scars and restoring functionality.
Why Choose Us for Facial Trauma Treatment in Panchkula?
Dr. Sanjay Kalra’s Multispeciality Dental Clinic stands out for its combination of expertise, state-of-the-art equipment, and patient-centered care. We prioritize your comfort and confidence throughout the healing process, offering a supportive environment for a smoother recovery.
Teeth Cleaning in Panchkula: Your Path to a Healthier Smile
While facial trauma treatment is critical for specific situations, regular preventive care is equally essential. Our clinic also provides professional teeth cleaning in Panchkula, ensuring optimal oral health and preventing issues like cavities and gum disease. This service complements our trauma care, promoting a healthy and radiant smile for all our patients.
Final Thoughts
Whether you need specialized facial trauma treatment in Panchkula or routine dental care like teeth cleaning in Panchkula, Dr. Sanjay Kalra’s Multispeciality Dental Clinic is your trusted partner in oral health and overall well-being. Contact us today to schedule a consultation and take the first step toward a confident, pain-free future.
Transforming lives, one smile at a time.
0 notes