#Kidney Function Evaluation
Explore tagged Tumblr posts
Text
Comprehensive Renal Function Tests for Kidney Health | H.R. Diagnostic

Renal Function Tests: Understanding the Importance for Kidney Health
Your kidneys play a crucial role in maintaining overall health. They filter waste, balance electrolytes, and regulate fluids in your body. However, many people don’t realize their kidneys may be failing until symptoms become severe. That’s why Renal Function Tests are essential. These tests help detect problems early and allow for timely treatment. At H.R. Diagnostic, we offer a range of Kidney Function Tests to assess your kidney health accurately and efficiently.
What Are Kidney Function Tests?
Kidney Function Tests measure how well your kidneys are working. They evaluate the ability of your kidneys to filter blood, remove waste, and maintain proper chemical balance. These tests also check if your kidneys are effectively removing excess fluids from your body. Early detection through these tests can help prevent further damage and complications.
Why Kidney Function Tests Are Important
Kidney diseases often progress without noticeable symptoms. Therefore, regular Kidney Function Tests are vital, especially if you are at risk. These tests give you a detailed insight into how well your kidneys are functioning. If there is an issue, you can address it early. Early intervention can improve the chances of treatment success and prevent severe kidney problems.
Who Should Get Nephrological Tests?
While everyone can benefit from Nephrological Tests, some individuals are at higher risk of kidney problems. Therefore, they should consider testing regularly.
Diabetes Patients: High blood sugar can damage kidney filters over time. Regular monitoring is crucial for those with diabetes.
People with High Blood Pressure: Hypertension can impair kidney function, so frequent testing is essential for early detection.
Individuals Over 60: As you age, kidney function naturally declines. Testing helps monitor this decline and manage any arising issues.
Family History of Kidney Disease: If kidney disease runs in your family, you may be at a higher risk.
People on Long-term Medications: Certain medications can affect your kidneys. Monitoring kidney health ensures that medications are not causing harm.
At H.R. Diagnostic, we offer comprehensive Nephrological Tests that suit your specific needs. We use advanced technology for accurate results, helping you stay proactive about your kidney health.
Common Renal Function Tests
Several tests fall under the category of renal function tests. Each provides unique insights into different aspects of kidney health.
1. Serum Creatinine Test
Creatinine is a waste product that your kidneys remove from your blood. The Serum Creatinine Test measures how much creatinine is in your bloodstream. High levels indicate that your kidneys are not filtering blood effectively.
Why It’s Important:
A high creatinine level is often the first sign of kidney dysfunction. This test is simple but offers critical insights into your kidney health. Therefore, it is one of the most commonly used renal function tests.
2. Glomerular Filtration Rate (GFR)
The Glomerular Filtration Rate (GFR) measures how well your kidneys are filtering blood. It estimates the rate at which your kidneys remove waste from the bloodstream. A lower GFR indicates reduced kidney function.
Key Insights:
GFR is a highly accurate measure of kidney function. Doctors often use it to stage chronic kidney disease (CKD) and determine the level of kidney impairment.
3. Blood Urea Nitrogen (BUN) Test
The Blood Urea Nitrogen (BUN) Test measures the amount of urea nitrogen in your blood. Urea is a waste product that kidneys normally remove. High BUN levels may suggest kidney dysfunction.
Why This Test Matters:
While a high BUN level could indicate kidney disease, it may also be a sign of dehydration or excessive protein intake. Therefore, doctors often interpret this test alongside others for a more comprehensive assessment.
4. Urinalysis
Urinalysis is a routine test that checks for protein, blood, or other abnormalities in your urine. It helps detect kidney damage early, even before noticeable symptoms occur.
Importance of Urinalysis:
If protein or blood is present in your urine, it could indicate kidney damage. Therefore, this test is critical for those with diabetes or hypertension who are at risk of kidney problems.
5. Urine Albumin-to-Creatinine Ratio (ACR)
This test measures the amount of albumin (a protein) in your urine. A high albumin level suggests that your kidneys may be leaking this protein, which they shouldn’t be.
Why It’s Important:
The Urine Albumin-to-Creatinine Ratio (ACR) helps detect early kidney damage. It is particularly useful for individuals with diabetes or high blood pressure. Therefore, early detection allows for timely treatment, preventing further deterioration.
Symptoms That May Indicate Kidney Problems
Kidney diseases often progress silently. However, certain symptoms suggest that it’s time for a Renal Function Test. If you experience any of the following, it’s essential to seek testing:
Swelling: When kidneys aren’t working efficiently, excess fluids build up in the body, causing swelling in the legs, feet, or ankles.
Fatigue and Weakness: Kidney dysfunction can lead to anemia, resulting in feelings of extreme tiredness and weakness.
Frequent Urination: If you are urinating more often, especially at night, this could indicate a kidney issue.
Foamy Urine: This may suggest that your urine contains too much protein, which is a sign of kidney damage.
Blood in the Urine: Blood in your urine is never a good sign. If you notice this, seek medical help immediately.
If you experience any of these symptoms, renal function tests can provide clarity. At H.R. Diagnostic, our specialists will guide you through the process and recommend the necessary tests.
Risk Factors for Kidney Disease
Certain factors increase the risk of kidney disease. If you have any of these, regular renal function tests become even more critical.
Diabetes: Diabetes is one of the leading causes of kidney disease. High blood sugar can damage the kidney’s filtering units.
High Blood Pressure: Chronic hypertension puts added stress on your kidneys, causing long-term damage.
Obesity: Carrying excess weight can lead to kidney problems. Maintaining a healthy weight is crucial for kidney health.
Smoking: Smoking reduces blood flow to your kidneys, accelerating the loss of kidney function.
Family History: A family history of kidney disease increases your risk of developing kidney problems.
If you fall into any of these categories, don’t delay. Get your renal function tested regularly.
How to Prepare for Renal Function Tests
Most renal function tests are straightforward, but preparation is key to ensuring accurate results. Here are a few simple steps to follow:
Stay Hydrated: Drink plenty of water unless instructed otherwise by your doctor.
Avoid Heavy Meals: Some tests may require fasting. Follow your healthcare provider’s instructions regarding food and drink.
Inform Your Doctor: If you’re on medications, let your doctor know. Some drugs can affect test results.
At H.R. Diagnostic, we provide you with all the information you need to prepare for your renal function tests. Our goal is to make the process smooth and stress-free.
Why Choose H.R. Diagnostic for Renal Function Tests?
At H.R. Diagnostic, we prioritize accuracy, convenience, and patient care. Here’s why you should choose us for your Renal Function Tests:
Accurate Results: We use state-of-the-art technology to ensure your test results are precise. Therefore, you can trust us to provide reliable data about your kidney health.
Experienced Staff: Our team of healthcare professionals is highly skilled in conducting renal function tests and interpreting the results. They are always available to address your concerns and answer any questions.
Affordable Testing Packages: We offer a variety of renal function test packages that are affordable and comprehensive. Therefore, you can take care of your health without financial strain.
Convenient Locations: We have multiple locations, so you can choose the most convenient one. Additionally, we offer home sample collection for your convenience.
When Should You Get a Renal Function Test?
The frequency of Renal Function Tests depends on your health status. However, here are some general guidelines:
Every 6 Months: If you have diabetes, hypertension, or a family history of kidney disease, consider testing twice a year.
Annually: For individuals over 60 or those taking medications that may affect the kidneys, annual testing is recommended.
Immediately: If you experience any symptoms of kidney disease, such as swelling, fatigue, or blood in your urine, seek testing as soon as possible.
Regular testing is crucial for maintaining kidney health. At H.R. Diagnostic, we make it easy to stay on top of your health with our advanced renal function tests.
How to Book a Renal Function Test at H.R. Diagnostic
Booking your Renal Function Test at H.R. Diagnostic is quick and easy. Follow these simple steps:
Visit Our Website: Go to our H.R. Diagnostic website and select the renal function test you need.
Choose Your Location: Select a convenient location or opt for home sample collection.
Pick a Time: Schedule your test at a time that suits you.
Get Tested: Arrive at the clinic or have your sample collected at home. Results will be available online within a few days.
Taking care of your kidney health has never been easier!
Read More…..
Author Bio: Simi Gajala has been working in digital marketing since 2018, amassing 6 years of experience. Currently Working as a Digital Marketing Executive at H.R. Diagnostics. Simi specializes in SEO, SMO, Google Ads, Meta Ads, and blogs & content writing, Boosting Brands, Increasing Visibility, And Enhancing Online Performance.
#HR Diagnostics#Kidney Assessment Tests#Kidney Diagnostic Tests#Kidney Function Evaluation#kidney function tests#Kidney Health Tests#Kidney Performance Tests#Kidney Screening Tests#Nephrological Tests#Renal Function Tests for#Renal Health Evaluation#Renal Performance Evaluation
0 notes
Text
"For the first time, genetically modified pig kidneys provided “life-sustaining kidney function” during the course of a planned seven-day clinical study—a first step in addressing the critical crisis worldwide of kidney donor organ shortage.
The University of Alabama’s pre-clinical human study at Birmingham also advances the science and promise of xenotransplantation as a therapy to potentially cure end-stage kidney disease—just as a human-to-human transplants can.
“It has been truly extraordinary to see the first-ever preclinical demonstration that appropriately modified pig kidneys can provide normal, life-sustaining kidney function in a human safely and be achieved using a standard immunosuppression regimen,” said UAB transplant surgeon scientist Jayme Locke, M.D., director of UAB’s Comprehensive Transplant Institute and lead author of the paper...
The peer-reviewed findings published last month in JAMA Surgery describes the pioneering pre-clinical human research performed on a recipient experiencing brain death...
The pre-clinical human brain death model developed at UAB can evaluate the safety and feasibility of pig-to-human kidney xenografts, or transplants, without risk to a living human. It is named for transplant pioneer Jim Parsons, an organ donor whose family generously donated his body to advance xenotransplant kidney research, like the latest patient did.
A Critical Need
Kidney disease kills more people each year than breast or prostate cancer, while more than 90,000 people are on the transplant waiting list. More than 800,000 Americans are living with kidney failure and 240 Americans on dialysis die every day. The wait for a deceased donor kidney can be as long as five to 10 years, and almost 5,000 people per year die waiting for a kidney transplant.
Groundbreaking Study Details
The 52-year-old study subject for this research lived with hypertension and stage 2 chronic kidney disease, which affects more than one in seven U.S. adults, or an estimated 37 million Americans. As part of this study, the subject had both of his native kidneys removed and dialysis stopped, followed by a crossmatch-compatible xenotransplant with two 10 gene-edited pig kidneys, or UKidney.
The transplanted pig kidneys made urine within four minutes of re-perfusion and produced more than 37 liters of urine in the first 24 hours. The pig kidneys continued to function as they would in a living human for the entirety of the seven-day study. Also, the kidneys were still viable at the time the study was concluded.
“In the first 24 hours these kidneys made over 37 liters of urine,” said Dr. Locke. “It was really a remarkable thing to see.” ...
Gene editing in pigs to reduce immune rejection has made organ transplants from pigs to humans possible. The natural lifespan of a pig is 30 years, they are easily bred, and they have organs of similar size to humans. Genetically modified pig kidneys have been extensively tested in non-human primates, and the addition of UAB’s preclinical human research model—the Parsons Model—now provides important information about the safety and efficacy of kidneys in human transplant recipients."
-via Good News Network, September 17, 2023
#organ donation#organ donor#organ transplant#medical news#medical research#pigs#kidney transplant#kidney diseases#dialysis#good news#hope#hope posting#human biology
574 notes
·
View notes
Text
⚕️Interpreting Gallifreyan Bloodwork
This guide is for use on Gallifreyans and Time Lords only. Always seek your human advice from human health providers.
🩸 How Gallifreyan Bloodwork Differs from Humans
Gallifreyan blood is vastly different from human blood due to triple-helix DNA, dual-heart circulation, and the presence of artron and lindos compounds. While some human blood tests can provide limited insights, many are ineffective, requiring Gallifreyan-specific diagnostics for accurate interpretation.
🧪 Blood Tests & Their Efficacy
Human Tests:
Venous Blood Gas (VBG) (Acid-base balance, oxygenation) ✅ Useful for pH, glucose, electrolytes, lactate.
Arterial Blood Gas (ABG) (Oxygenation accuracy) ❌ No advantage over VBG in Gallifreyan physiology.
Full Blood Count (FBC) (RBCs, WBCs, platelets) ❌ Useless—Gallifreyan cells do not match human equivalents.
Urea & Electrolytes (U&E) (Kidney function) ✅ Detects chloride (Cl⁻), creatinine, magnesium (Mg²⁺), potassium (K⁺), sodium (Na⁺).
Troponin (Heart damage/disease detection) ✅ Detects Gallifreyan troponin levels to assess myocardial strain.
Brain Natriuretic Peptide (BNP) (Heart failure monitoring) ✅ Detects NT-proBNP, useful for evaluating dual-heart strain.
Group & Save (G&S) (Blood typing for transfusions) ❌ Useless—Gallifreyan blood groups are House-specific and not compatible across Houses.
Liver Function Test (LFT) (Liver enzyme assessment) ✅ Detects ALP, GGT, ALT, AST to monitor liver health, particularly in relation to lindos metabolism and toxin exposure.
International Normalised Ratio (INR) (Clotting rate) ❌ Useless—Gallifreyan clotting mechanisms differ from human systems.
Specialised Gallifreyan Tests:
Z-Cell Count (Immune response monitoring) ✅ Essential for assessing general and specific immune function.
Artron Levels (Time-energy exposure, immune activation, healing response) ✅ Essential for assessing infection, injury healing, psionic function, and Time Vortex exposure.
Lindos Levels (Regenerative activity indicator) ✅ Detectable only before, during, or after regeneration. Presence at other times is abnormal and suggests systemic failure or forced regeneration attempts.
House Blood Testing (Genetic matching, transfusion compatibility) ✅ Detects House-specific protein markers, ensuring safe transfusions.
Platelet & Clotting Factors (Coagulation health, haemodynamic stability) ✅ Excess platelets indicate haemoinstability, increasing the risk of multiple embolisms and stroke, particularly in cases of aspirin poisoning or anticoagulant dysfunction.
🔬 Gallifreyan Blood Reference Ranges & Abnormalities
pH (VBG/ABG) (Acid-base balance, metabolic function)
🟢 Normal: 7.1 – 7.4 🛑⬆️ Higher pH suggests metabolic alkalosis, respiratory bypass activation, or regenerative instability. 🛑⬇️ Lower pH may indicate acidosis, systemic infection, or artron overload.
Glucose (Energy metabolism, regeneration status)
🟢 Normal: 3.0 – 6.5 mmol/L 🛑⬆️ High glucose suggests lindos activation, metabolic shifts from regeneration, or time-energy instability. 🛑⬇️ Low glucose suggests systemic metabolic failure, starvation, or hypoartronosis.
Lactate (Metabolic function, regeneration status)
🟢 Normal: 0.5 – 2.0 mmol/L 🛑⬆️ High lactate suggests metabolic distress, post-regeneration recovery, or artron dysregulation. 🛑⬇️ Low lactate suggests poor energy reserves or extreme starvation.
Troponin (Heart damage monitoring, dual-heart strain)
🟢 Normal: 0.01 – 0.15 ng/mL 🛑⬆️ High troponin suggests dual-heart strain, pre-regenerative cardiac failure, or bypass overuse.
NT-proBNP (Heart failure marker, circulation monitoring)
🟢 Normal: 0 – 500 pg/mL 🛑⬆️ Elevated levels indicate early-stage heart failure, one heart compensating for another, or cardiac stress.
Z-Cell Count (Immune response, infection monitoring)
🟢 Normal: 5,000 – 15,000 mcL 🛑⬆️ High Z-cell counts suggest active infection, systemic inflammation, or immune hyperactivation. 🛑⬇️ Low Z-cell counts indicate immunosuppression, chronic illness, or psionic burnout.
Artron Levels (Infection, healing, time-radiation exposure)
🟢 Normal: 500 – 4000 mcL (higher baseline in Time Lords) 🛑⬆️ 4000+ mcL suggests hyperartronosis (psionic overactivity, radiation exposure, tissue repair). 🛑⬇️ Below 500 mcL suggests hypoartronosis (immune suppression, tissue degeneration, metabolic failure).
Lindos Levels (Regeneration marker, biological restructuring)
🟢 Undetectable unless regenerating 🛑⬆️ Presence outside of regeneration suggests forced regeneration, internal instability, or pre-regenerative stress response.
Platelet & Clotting Factors (Haemostasis, stroke risk)
🟢 Normal: Variable based on individual regenerative state 🛑⬆️ Excess platelets suggest haemoinstability, aspirin poisoning, or embolism risk. 🛑⬇️ Low platelets indicate clotting failure, possible regenerative exhaustion, or internal bleeding risk.
📌 Key Takeaways for Bloodwork Interpretation
✔️ Z-Cells are elevated in Gallifreyan immune response.
✔️ Artron levels increase in infection, injury healing, and radiation exposure. Time Lords naturally have higher baseline artron levels than other Gallifreyans.
✔️ Lindos should only be present before, during, or after regeneration. Presence at other times is a major red flag.
✔️ Hyperartronosis and Hypoartronosis can cause severe neurological, metabolic, and cardiovascular consequences.
✔️ House-matching is essential for blood transfusions. Mismatched blood leads to systemic failure.
✔️ Clotting instability can cause multiple embolisms or stroke, requiring monitoring in cases of anticoagulant use or regenerative dysfunction.
---
📚 Clinical Case Studies
Now you know absolutely everything about Gallifreyan bloodwork, you can apply them to some simple clinical scenarios. There are three fully explained case studies, followed by two additional scenarios for you to think about.
🩺 Case 1: Post-Regenerative Complications
📝 Patient Background & Presentation: Patient is a Time Lord, 918/3rd generation, Newblood. They present 10 hours post-regeneration with severe fatigue, dizziness, difficulty walking, and pallor. They complain of "feeling wrong in my own body."
🧪 Tests Ordered: Venous Blood Gas (VBG), Lactate levels, U&E (Electrolytes & Kidney Function), Liver Function Test (LFT), Artron & Lindos Levels
📊 Lab Results: - pH: 7.08 (⬇️Acidosis) - Lactate: 5.6 mmol/L (⬆️Elevated) - Sodium (Na⁺): 128 mmol/L (⬇️Low) - Potassium (K⁺): 3.1 mmol/L (⬇️Low) - Magnesium (Mg²⁺): 0.9 mmol/L (⬇️Low) - Lindos: 14,500 mcL (⬆️Very High) - Artron: 650 mcL (⬇️Low)
🩸 Interpretation: - The low artron levels and high lindos levels indicate post-regenerative instability, where metabolic processes have not fully stabilised following regeneration. - The elevated lactate and acidosis suggest impaired metabolic clearance, possibly due to lingering regenerative strain. - The electrolyte imbalances (low sodium, potassium, and magnesium) are contributing to the patient's dizziness, weakness, and fatigue.
💡 Diagnosis: Post-Regenerative Metabolic Instability with Hypoartronosis
🩺 Case 2: Time Travel Incident
📝 Patient Background & Presentation: Patient is a Time Lord scientist, 402/1st generation, Oldblood. They were admitted following a collapse mid-experiment after direct exposure to a raw time vortex rift. Unconscious upon arrival, GASS score rapidly deteriorating.
🧪 Tests Ordered: Venous Blood Gas (VBG), Lactate levels, Z-Cell Count, Artron & Lindos Levels, Liver Function Test (LFT)
📊 Lab Results - pH: 7.25 (⚖️Normal, slightly acidic) - Lactate: 4.3 mmol/L (⬆️Elevated) - Z-Cell Count: 13,800 mcL (⚖️Normal) - Artron: 8,900 mcL (⬆️Very High) - Lindos: <50 mcL (⚖️Normal) - ALT/AST: Slightly elevated (⬆️)
🩸 Interpretation: - Critically elevated artron levels suggest hyperartronosis due to raw time-energy exposure. This has led to neurological overload, explaining the collapse and psionic disturbances. - Elevated lactate suggests tissue stress and impaired metabolic clearance, likely due to the overload of artron. - Liver enzyme elevation indicates mild systemic strain but not full organ failure.
💡 Diagnosis: Acute Hyperartronosis Due to Uncontrolled Time-Energy Exposure
🩺 Case 3: Severe Cardiac Distress
📝 Patient Background & Presentation: Time Lord ambassador, 2752/7th generation, Oldblood. The patient was admitted with chest pain, dizziness, palpitations, and difficulty maintaining balance. Heart rhythms are synchronous.
🧪 Tests Ordered: Troponin, NT-proBNP (Heart failure marker), Venous Blood Gas (VBG), Z-Cell Count, Electrolytes (U&E)
📊 Lab Results - pH: 7.38 (⚖️Normal) - Troponin: 0.22 ng/mL (⬆️Elevated) - NT-proBNP: 710 pg/mL (⬆️High) - Z-Cell Count: 6,900 mcL (⚖️Normal) - Potassium (K⁺): 5.8 mmol/L (⬆️Elevated)
🩸 Interpretation & Diagnosis: - Elevated troponin and NT-proBNP levels confirm cardiac distress, likely due to strain on both hearts attempting to compensate for each other. - Elevated potassium suggests possible metabolic involvement contributing to electrical disturbances in heart function. - Synchronous heart rhythm and symptoms indicate a high risk of impending heart/s failure.
💡 Diagnosis: Severe Dual-Heart Strain with Electrical Instability
🤔 Self-Interpretation Cases
🩺 Case 4: Post-Surgery Issues
📝Patient Background & Presentation: Patient is a Time Lord, 1890/5th generation, Oldblood. An hour ago, they underwent surgery to correct a post-regenerative issue in limb attachment, which required anaesthesia and a blood transfusion. Since surgery, they have had a rapid deterioration, with confusion, severe fever, and difficulty breathing.
🧪 Tests Ordered: Venous Blood Gas, Z-Cell Count, Liver Function Test, Electrolytes (U&E), Artron Levels
📊 Lab Results: - pH: 7.02 (⬇️Severe Acidosis) - Lactate: 6.1 mmol/L (⬆️ Critically Elevated) - Z-Cell Count: 18,200 mcL (⬆️Hyperactivation) - Liver Enzymes: Critically elevated (⬆️) - Sodium (Na⁺): 121 mmol/L (⬇️Dangerously low) - Artron: 9,200 mcL (⬆️ Very high)
💡 Questions to Consider
What could be a potential cause/diagnosis?
What does the elevated Z-cell count indicate about the immune response?
How does House-specific transfusion compatibility play a role in this case?
Why are sodium levels dangerously low?
What does the combination of high artron and high lactate suggest about metabolic function?
🩺 Case 5: Accidental Aspirin Ingestion in a Gallifreyan
📝Patient Background & Presentation: Patient is a Gallifreyan, 612/2nd generation. They were found unresponsive after a trip to an Earth hospital to see a friend. They present with swollen extremities and face, severe nosebleeds, petechiae (tiny bruises), slurred speech, and tachycardia.
🧪 Tests Ordered: Venous Blood Gas, Platelet & Clotting Factors, Liver Function Test, Electrolytes, Z-Cell Count, Artron Levels
📊 Lab Results: - pH: 7.45 (⚖️Normal, slightly alkaline) - Platelet Count: 350% above baseline (⬆️Dangerously high) - Liver Enzymes: Moderately elevated (⬆️) - Potassium (K⁺): 3.0 mmol/L (⬇️Low) - Z-Cell Count: 22,400 mcL (⬆️ Severe immune response) - Artron: 5,700 mcL (⬆️ Elevated, systemic activation detected)
💡 Questions to Consider:
What could be a potential cause/diagnosis?
Why is platelet count dangerously high?
How does aspirin toxicity affect Gallifreyan haemostasis differently from humans?
Why are Z-cell and artron levels elevated at the same time?
How does the presence of left-side weakness and slurred speech relate to this case?
Medical Guides These are all practical guides to assessing and treating a Gallifreyan in an emergency or medical setting.
⚕️💕Gallifreyan CPR
⚕️👽Gallifreyan Assessment Scoring System (GASS)
⚕️👽ABCDE Assessment
⚕️⚠️Sepsis Emergency Response (SER)
⚕️⚠️Severe Trauma Protocol
⚕️🌡️Gallifreyan Thermoregulation and Emergency Response
⚕️🔮Psionic Emergency Pathways
⚕️✨Post-Regeneration Management
⚕️🩸Interpreting Gallifreyan Bloodwork
⚕️👶Gallifreyan Paediatric Emergencies
Any orange text is educated guesswork or theoretical. More content ... →📫Got a question? | 📚Complete list of Q+A and factoids →📢Announcements |🩻Biology |🗨️Language |🕰️Throwbacks |🤓Facts → Features:⭐Guest Posts | 🍜Chomp Chomp with Myishu →🫀Gallifreyan Anatomy and Physiology Guide (pending) →⚕️Gallifreyan Emergency Medicine Guides →📝Source list (WIP) →📜Masterpost If you're finding your happy place in this part of the internet, feel free to buy a coffee to help keep our exhausted human conscious. She works full-time in medicine and is so very tired 😴
#doctor who#dr who#dw eu#gallifreyans#gallifrey institute for learning#Time Lord biology#GAP Quick Guides#whoniverse#GIL: Biology#gallifreyan biology#GIL: Species/Gallifreyans#GIL#GIL: Biology/Medical
34 notes
·
View notes
Text
Okay so there are two tapes in game where Harvey speaks.
youtube
The first tape Harvey appears in is (#10) where Harleen and Harvey appear. She complains to him about Crane's experiments, implying Harvey's partly responsible for his presence there? and that Harvey trusts him. Apparently Crane is there to help Harvey in court and evaluate inmates. He says it's a necessary evil and he tells her to kick rocks.
The second one, tape #13, is interesting. It's found in the ship where you find out Harvey is the rat king near the console. The tape starts with Harvey asking Crane for help. But then...

HARVEY: I just... I-I lost it. You shoulda seen the police photos. This bastard didn't just beat his kid, he starved him! Kept him locked in a closet for six months. Eight years old, fighting with this- with the rats over scraps of food. When the cops finally freed him, his kidneys had failed and his heart was scarred by infection.
Foreshadowing. And guess this confirms for me that Harvey becomes retraumatized by his job and knows it but won't quit.


CRANE: My goodness. Harrowing stuff.
HARVEY: And his dad has the nerve to take the stand and tell the court his kid deserved it? Piece of shit's lucky I only took a couple of swings at him. Besides, I might've just torched my whole career.
CRANE: Oh, I doubt that. You're a hero in the papers. "Two-Fisted DA Decks Deadbeat Dad." The public's behind you on this.
HARVEY: My own dad's to blame for my short fuse. But I can't lose my temper like that again.
CRANE: Your father? I'd like to hear more about him.
So Harvey had been having issues waaay before Batman was in the picture? (Also Harvey sounds so sinister saying "Piece of shit's lucky I only took a couple of swings at him." Love Troy Baker's performance and how Elijah Wood gives this impression that he's just letting Harvey talk to examine him like another one of his tests subjects-- i mean patients.)
And it's BTAA scarecrow and Harvey again, but Bruce isn't there to help


HARVEY: You really think this stuff will help?
CRANE: Early trials are quite promising. Now, hold this, hold it- There you go. And take three deep breaths. Good.
HARVEY: *Inhales loudly*
CRANE: I want you to consider that your recent outbursts may be stress -induced. Building a case agaisnt Carmine Falcone clearly had you burning the candle at both ends.
HARVEY: Well, tell that to the press. All i hear about is how "the batman brought down the Roman Empire." We worked together, y'know. Me, him, Gordon, too. [laughs] Ah, I'm starting to lose my cool again.
Harvey's voice is way way lower. Okay, Harvey is mad about someone else taking credit. Guess that explains his reaction to seeing batman again. More ppl taking advantage of him.


CRANE: No, no-no-no, that's good. Good. We've already touched on how much you've been repressing. Themore you try to contain your shadow, the more that aspect of your psyche starnates and festers. We need to bring it to the light.
HARVEY: [almost a whisper?] Drag if out of the darkness? That's what I've been trying to do with this whole city. Too many trials. Too many appeals. Better let fate judge. Fifty-fifty, like flippin' a coin. Better odds than my old man gave me.
HARVEY: No, it's um, getting worse. The headaches mostly.
CRANE: That's only a function of your conscious mind giving way to your shadow self. As it rises to the surface, your awareness becomes fuzzy in a neurological sense as you grapple with the--
HARVEY: [as a whisper? / hiss?] That's not it. It's never been this bad. Gilda is scared. And I am too.
OKAY so, Gilda must have left at some point because Crane is making him worse. He already believes in the coin. This Crane is so interesting thinking talk therapy is universally effective with dissociation and trauma. He seems to genuinely believe in what he's doing.


CRANE: you fear becoming your father. You fear you'll assume his worst traits as you get older.Please: sit. Have a sip of water. Good, good, good. Listen thins always feel more intense just before the real healing begins. You are making remarkable progress.
HARVEY: We.
CRANE: Hm?
HARVEY: 'We' are making remarkable progress
CRANE: Of course, Mr. Dent. This is good for both of us.
So, safe to say, Crane caused this lmao.
Also, In the tape between Arnold and Harley (#3), Arnold has the same symptoms as Harvey but he doesn't seem to have the puppet yet until she encourages her to do so? so unless i'm missing something, it kinda seems like Crane's treatment is the one causing DID like symptoms.
Okay, I heard the tape between Joe and Thompkins (tape #8) and it seems everyone gets headaches so it's not DID per se. (also Leslie used to have a free clinic in park row and a crisis center for kids. idk if at the same time or the same place, tho)

LESLIE: Any other complaints?
JOE: Just some reactions to Dr. Crane's treatment. Headaches. Can't remember some stuff.
Okay, next part.





HARVEY: Doctor, I wanna stop the treatments.
CRANE: But why?
HARVEY: Why? What the hell happened to your lab rat this morning?
CRANE: it's the unfortunate reality of medical testing that on occasion we have to put an animal through a measure of discomfort in order to-
HARVEY: The shit you got me breathing melted its fur off! Melted its skin.
CRANE: Mr Dent, the individual chemicals in this solution are heavily corrosive but, when properly diluted they are intert and stable.
HARVEY: Inert and stable? I-I-I don't know-
CRANE: Harvey, Harvey. I've been reviewing our recorded sessions and i'm confident you're on the cusp of a major breakthrough. Trust the process. If not for yourself, then do it for Gilda. Doesn't she deserve a healthier, happier husband?
HARVEY: [basically a growl] Crane, if my symptoms don't resolve soon, I'm out.
CRANE: I understood. You're making the right choice. I'll prepare the dose.
This is insane. There's... so much here. Crane manipulates Harvey into using the treatment bc Harvey loves Gilda so much. Harvey was aware of what that thing could do (adding humiliation to having his own face burnt off by some malone?) This must have implanted the idea in his head about being a lab rat and staying one forever bc of his self doubt and letting it get this far.
I wonder if Crane's treatment actually fucked him up the way something like, idk, joker gas would, rather than that darkness coming solely from Harvey? but then again, Harvey beat up a man in court in front of everyone so it wasn't that big of a step.
TLDR; Everything is kinda Crane's fault.
#long post#leslie thompkins#gilda dent#gilda gold#harvey dent#two face#bruce wayne#jonathan crane#scarecrow#batman#arkham shadow spoilers#arkhamverse#batman arkham shadow#Youtube#I hope I didn't miss anything
32 notes
·
View notes
Text

Happy Ash Valentine’s Wednesday!
Had my physical with my GP today. I have to monitor my blood pressure for two weeks and share the numbers so she can evaluate whether or not I can come off any of the meds after having lost 23% of my body weight. (I hate being on meds)
The dizziness … I’m dehydrated! So I have to ramp up the water intake. She said that’ll help with the joint pain too. But she’s gonna run some tests on my kidney function cuz sometimes chemo can mess with that. So off for a bunch of labs I went.
Now I have a killer headache. I think my body is rejecting the water.
36 notes
·
View notes
Text
Clinical Nutrition & Dietetics: Science for Better Health
Clinical Nutrition and Dietetics is a specialized field that uses nutrition to manage and prevent disease, improve health outcomes, and promote overall well-being. Here’s a deep dive into the essential aspects of this field:

What is Clinical Nutrition and Dietetics?
Clinical Nutrition and Dietetics involves assessing, diagnosing, and treating nutrition-related health issues. Dietitians and clinical nutritionists work closely with patients to develop dietary plans tailored to their medical conditions, lifestyle, and specific health goals.
Key Areas of Clinical Nutrition and Dietetics
Medical Nutrition Therapy (MNT): MNT is the cornerstone of clinical dietetics, involving specialized dietary interventions based on scientific evidence. It’s used to treat chronic illnesses like diabetes, cardiovascular disease, cancer, and kidney disease.
Nutritional Assessment: This includes evaluating a patient’s diet, medical history, physical health, and lab results to create personalized nutrition plans. Tools include BMI, body composition analysis, dietary history, and blood tests to assess nutrient levels.
Therapeutic Diets: Dietitians often develop therapeutic diets to manage health conditions, which can include:
Low-sodium diets for hypertension and heart health.
Low-glycemic diets for managing diabetes.
High-protein diets for malnutrition and muscle recovery.
Renal Diets for kidney disease patients to reduce the intake of specific nutrients.
Pediatric and Geriatric Nutrition: Clinical dietitians specialize in creating age-appropriate nutritional plans for children and elderly patients, addressing issues like growth, development, bone health, and cognitive function.
Mental Health and Nutrition: Dietitians are increasingly focusing on the connection between nutrition and mental health, as certain nutrients (e.g., omega-3s, and B vitamins) can impact mood and cognitive function.
Emerging Areas in Clinical Nutrition
Functional Foods and Nutraceuticals: Functional foods (like probiotics) and nutraceuticals (such as dietary supplements) are increasingly used in clinical nutrition to support specific health outcomes, such as immune function or gut health.
Personalized Nutrition and Genomics: Nutrigenomics studies how genes influence individual responses to nutrients, leading to personalized nutrition plans based on a patient’s genetic makeup. This method works especially well for treating chronic illnesses.
Integrative and Holistic Nutrition: Integrative nutrition considers lifestyle factors, stress, and mental health along with diet, promoting a more holistic approach to patient care.
Plant-Based Diets: The use of plant-based diets in clinical settings is becoming popular for their benefits in reducing inflammation, improving heart health, and supporting weight management.
Role of Clinical Dietitians in Healthcare Settings
Hospitals: Clinical dietitians are essential in hospitals, where they design dietary plans for patients recovering from surgeries, dealing with chronic illnesses, or undergoing treatment that affects their nutritional status.
Outpatient Clinics: Many dietitians work in clinics, providing ongoing support for patients with chronic conditions like diabetes or high cholesterol.
Rehabilitation Centers: Nutritionists here help patients with recovery, focusing on high-calorie or high-protein diets to promote healing.
Skills for Clinical Dietitians
Analytical Skills: Strong understanding of biochemistry and physiology to interpret lab data and develop dietary plans. Counseling and Communication: The ability to communicate effectively with patients to promote adherence to dietary plans.
Evidence-Based Practice: Staying updated with the latest research to provide science-backed advice. Career Opportunities
Clinical dietitian: employed by long-term care homes, clinics, or hospitals.
Nutrition Researcher: Contributing to research on disease prevention and dietary interventions.
Consultant Dietitian: Providing freelance or consultancy services for healthcare facilities, wellness centers, or private clients.
Corporate Wellness Programs: Supporting employees’ health and well-being through nutritional guidance in corporate settings.
Conclusion
In conclusion, Clinical Nutrition and Dietetics is a transformative field that bridges the gap between nutrition science and patient care, offering personalized approaches to health and wellness. By understanding the intricate relationship between diet, disease, and overall health, clinical dietitians play a crucial role in improving health outcomes and enhancing quality of life. As new research and innovations in nutrition continue to emerge, this field remains essential in advancing preventive care, supporting disease management, and promoting holistic well-being.
3 notes
·
View notes
Text
youtube
A Kidney Function Test Ensure Well Functioning of Your Organ
A kidney function test is a laboratory test that is being done to evaluate the functioning of the kidney. The increasing risk of kidney disease leading to increased demand for kidney function tests. According to click here National Kidney Foundation, 1 in 3 adults is at the risk of kidney disease in the United States.
So it is important to have an earlier diagnosis of these diseases. This in turn can help in proper treatment and complications and any permanent damage to the kidney can be avoided.
What is a kidney function test?
A kidney function test is a clinical or laboratory procedure. It is designed to evaluate the functioning of the kidney. It helps in the diagnosis of kidney disorders. So various aspects of kidney capacity can be evaluated by a kidney function test.
What functions does the kidney perform?
The kidney is a vital organ of your body. It is bean-shaped and two in number. The kidney is located in the posterior side of your abdomen just below the ribcage. It plays many important roles in the body.
The main function of the kidney is to filter waste materials from the blood that is removed from the body in the form of urine. It also helps in maintaining an osmotic balance of the body fluid. Not only this, but the kidney also helps in the production of vitamin D, red blood cells, releases hormones important for maintaining blood pressure. So now you can imagine how crucial it is for the kidney to work efficiently.
2 notes
·
View notes
Text
Blood Testing Services - Personalized Healthcare

Blood testing services have emerged as a cornerstone of modern healthcare, offering a window into the inner workings of our bodies. With a simple blood sample, these services can provide critical insights into our health, ranging from diagnosing diseases to monitoring treatment effectiveness. In this comprehensive guide, we will delve into the world of Blood draw at home services, exploring the wide range of tests available, their significance in healthcare, and how they empower individuals to take charge of their well-being.
The Significance of Blood Testing Services
Blood is a treasure trove of information, carrying vital clues about our health. Blood testing services have gained immense importance for several reasons:
Early Disease Detection: Blood tests can detect diseases and health conditions at an early stage, often before symptoms become apparent. Early detection allows for timely intervention and improved treatment outcomes.
Monitoring Chronic Conditions: For individuals managing chronic conditions such as diabetes, cardiovascular disease, and thyroid disorders, regular blood tests are essential for monitoring disease progression and treatment effectiveness.
Personalized Healthcare: Blood tests enable personalized healthcare by tailoring treatment plans and interventions based on an individual's unique health markers and needs.
Preventive Care: Blood tests play a crucial role in preventive care, identifying risk factors and enabling lifestyle adjustments to reduce the likelihood of developing certain diseases.
Treatment Guidance: Physicians use blood test results to guide treatment decisions, adjust medication dosages, and assess the impact of treatments.
The Range of Blood Tests

Blood testing services encompass a vast array of tests, each designed to assess specific aspects of health. Here are some common categories of blood tests:
Complete Blood Count (CBC): Measures various components of the blood, including red and white blood cells and platelets, providing insights into overall health.
Basic Metabolic Panel (BMP): Assesses essential metabolic functions such as glucose, calcium, and electrolyte levels.
Comprehensive Metabolic Panel (CMP): Extends the BMP by including liver and kidney function tests, as well as protein levels.
Lipid Profile: Evaluates cholesterol levels, including LDL (bad) cholesterol, HDL (good) cholesterol, and triglycerides, to assess cardiovascular risk.
Thyroid Function Tests: Measure thyroid hormone levels, helping diagnose thyroid disorders.
Blood Glucose Tests: Assess blood sugar levels, crucial for diagnosing and managing diabetes.
Coagulation Profile: Evaluates the blood's ability to clot, important for monitoring blood thinners and diagnosing clotting disorders.
Hormone Tests: Measure hormone levels, including sex hormones, thyroid hormones, and adrenal hormones.
Infectious Disease Testing: Detects antibodies or antigens for infections such as HIV, hepatitis, and Lyme disease.
Cancer Markers: Blood tests can identify specific markers associated with certain cancers, aiding in diagnosis and monitoring.
Vitamin and Mineral Levels: Assess levels of essential nutrients like vitamin D, vitamin B12, and iron.
The Process of Blood Testing
The process of blood testing typically involves the following steps:
Sample Collection: A trained healthcare professional collects a blood sample, usually from a vein in the arm, using a needle and syringe or a vacuum tube.
Sample Processing: The collected blood is processed in a laboratory to separate the various components for analysis.
Laboratory Testing: Specialized equipment and techniques are used to measure specific markers in the blood sample accurately.
Result Reporting: Test results are reported to the patient and their healthcare provider. Many blood testing services offer online access to results for convenience.
Blood testing services are a cornerstone of modern healthcare, offering a wealth of information about our health and well-being. They enable early disease detection, personalized treatment plans, and preventive care, ultimately empowering individuals to make informed decisions about their health. Regular blood testing, in collaboration with healthcare providers, is a powerful tool for maintaining and enhancing one's health throughout life. By understanding the significance of blood tests and their role in personalized healthcare, individuals can embark on a journey toward optimal well-being and longevity.
Certainly, here are some frequently asked questions (FAQs) about blood testing services:
What are blood testing services?
Blood testing services are healthcare facilities or providers that offer a range of tests and analyses using blood samples to assess various aspects of an individual's health, including disease detection, monitoring chronic conditions, and evaluating overall well-being.
Why are blood tests important?
Blood tests are crucial for early disease detection, monitoring chronic conditions, guiding treatment decisions, assessing risk factors, and promoting preventive care. They provide valuable insights into an individual's health.
How is a blood sample collected?
A trained healthcare professional typically collects a blood sample from a vein in the arm using a needle and syringe or a vacuum tube. The procedure is relatively quick and generally causes minimal discomfort.
What types of tests can be performed with a blood sample?
Blood testing services offer a wide range of tests, including complete blood counts, metabolic panels, lipid profiles, thyroid function tests, blood glucose tests, hormone tests, infectious disease testing, cancer marker tests, and vitamin/mineral level assessments, among others.
How long does it take to get blood test results?
The turnaround time for blood test results varies depending on the specific tests conducted and the laboratory's processing time. Some results may be available within a few hours, while others may take a few days.
Are blood test results confidential?
Yes, blood test results are confidential and protected by patient privacy laws, such as the Health Insurance Portability and Accountability Act (HIPAA). Only authorized healthcare professionals and the patient have access to these results.
Can I request specific blood tests?
Yes, many blood testing services allow patients to request specific tests based on their healthcare needs and preferences. You can discuss your testing requirements with the provider or your healthcare practitioner.
How often should I get blood tests done?
The frequency of blood tests depends on your age, overall health, family history, and any specific medical conditions you may have. Your healthcare provider can recommend an appropriate schedule for blood tests.
Do I need to fast before certain blood tests?
Some blood tests, like fasting blood glucose and lipid profiles, require fasting for a specific period (usually 8-12 hours) before the test to obtain accurate results. Your healthcare provider will provide instructions if fasting is necessary.
Are blood tests covered by insurance?
The coverage of blood tests by insurance may vary depending on your insurance provider, policy, and the specific tests being conducted. It's advisable to check with your insurance company to understand the extent of coverage.
Can I access my blood test results online?
Many blood testing services offer online portals or apps where patients can access their test results securely. This provides convenient access to your health information.
How can I find a reliable blood testing service near me?
You can search online for blood testing services in your area, ask your healthcare provider for recommendations, or use healthcare directories to locate nearby facilities. Reading reviews and checking accreditation can help you make an informed choice.
Blood testing services play a crucial role in healthcare by providing valuable information that guides diagnosis, treatment, and preventive care. If you have specific questions about blood testing or require particular tests, it's advisable to consult with a healthcare professional or a trusted blood testing service provider.
Read more at website: http://www.mobileblooddrawservices.com/
#blood testing services#blood testing#mobileblooddrawservices#Blood draw at home services#Blood draw at home
3 notes
·
View notes
Text
join me in pell (piss hell)
Let's talk kidneys!
Your kidneys are situated:
Inferior to the liver and the suprarenal glands
Superior to the ureters
Anterior to the posterior wall of abdomen and diaphragm
Posterior to the peritoneum (sack with yer guts in it)
Their job is to:
Regulate blood ions (like sodium) and control blood pH
Maintain blood volume (by extracting or conserving water)
Secrete hormones
Excrete toxic waste (urea, ammonia, creatinine…)
Guess what shape they are. Go on, guess.
YEAH THAT’s RIGHt – IT’S BEAN TIME, BITCHEs

[CW: beneath the cut you will find CT images of kidney trauma]
(and here is some very basic anatomy, sketched on… that same bean)
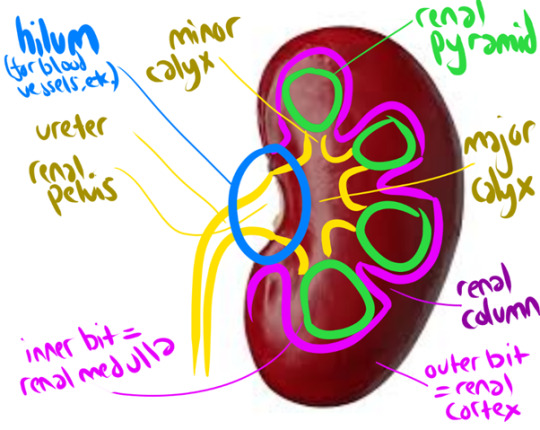
The renal cortex + renal pyramids together form the PARENCHYMA, aka the functional bit of the kidneys (aka where your peepee is made)
But HOW is that peepee made, I hear you cry?
Lemme introduce you to my good friend
The Nephron
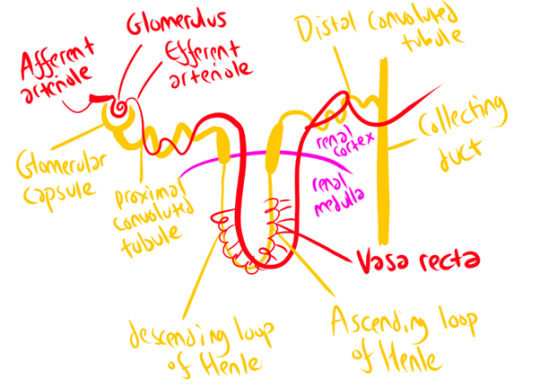
The afferent arteriole carries blood to the Glomerulus (which isn’t actually some weird DnD spell – just a knot of arteries surrounded by the Glomerular Capsule!) This arteriole then slims down considerably to form the efferent arteriole. This pressure increase forces loads of waste products and water out of the bloodstream into the glomerular capsule – but the holes in the arteriole wall are too small to release blood cells, plasma proteins, and other large molecules. This part of the nephron is called the ‘corpuscle’ (again, not a DnD spell). It’s where your blood plasma gets filtered!
The arteriole then follows the nephron around its windy path, wrapping around it at several points – notably the proximal/distal convoluted tubules, and the Vasa Recta that runs parallel to the Loop of Henle. To horrifically simplify a complex process, this provides lots of opportunities for secretion (Bad Stuff to be squeezed out of the blood – those dangerous ions and waste products we talked about earlier!) and selective reabsorption (Good Stuff (water) gets squeezed back in). It’s a careful balancing act, orchestrated in part by hormones! The end result (theoretically) is that all the stuff you DON’T want is shlorped into the nephron as urine, and all the water you need is shlorped back into the blood.
Once your kidneys have produced your peepee, it takes a fun rollercoaster ride through a series of ducts and tubes! Collecting duct -> papillary duct -> minor calyx -> major calyx -> renal pelvis -> ureter -> urinary bladder -> urethra -> you know the rest.
Your kidneys produce 180 litres of fluid a day (aka, a hell of a lot) but most of this is reabsorbed in these little nephrons, with water & useful solutes going back into the bloodstream! As a result, you only pee about 1-2 litres a day (though I swear I feel closer to the 180 litres some days)
Because kidneys are SOOOO important (your body does NOT like to be full of urea/ammonia/sodium, or acid!) they’re really, really vascular (lots of blood supply). They receive up to 25% of your resting cardiac output! So, when you’re just chilling, literally 25% of your blood is being gobbled by those hungry, hungry kidneys!
This means the kidney is VULNERABLE TO TRAUMA.
Although kidney trauma can be picked up on Ultrasound, we will take anyone who has suffered abdominal trauma through to CT, as you get better pictures there! We usually use a multiphase protocol – a longer scan, basically – to show us the extent of the injury, with a non-contrast phase (shows calculi clearly), an arterial phase (evaluates any injury to the renal arteries), a nephographic phase (shows renal lesions clearly), and a delayed phase (shows bleeding and injuries to the urinary collection system). Basically, contrast quickly moves to your kidneys from your blood stream, and filters through the collection system – so if we give a bolus of contrast and watch it flood through the renal arteries, then wait a little while, we can see how the kidneys are processing it or if it’s spilling into the surrounding space.
Kidney trauma is graded from 1 (no laceration but a haematoma (bruise) within the kidney capsule) to 5 (kidney torn away from renal vascular system and dying as a result, actively bleeding, structure of kidney shattered). Here’s a grade 5 (Left (looks like the right side of the image)) in comparison to the normal healthy kidney (Right (looks like the left side of the image)). Note the massive visible laceration + huge haematoma!


Loooooads of other stuff can go wrong with your kidneys too – but that’s a whole other post! Which I will make, one day soon, because it's super fascinating!
(Have you ever heard of a stag horn calculus? It will put you off holding onto your pee FOR LIFE. If you're sitting there kinda needing the loo but not going... GO NOW. PLEASE.)l
18 notes
·
View notes
Text
How to lose weight conveniently, safely, and quickly
Can't seem to lose weight no matter how much you exercise? Are you afraid of liposuction and not sure if it's safe? Today's product is a Beauty-line solution from the Bijunel series.

Beauty-line solution is a safe lipolysis solution whose main ingredient is L-carnitine.


What is L-carnitine?
Amino acid derivatives
Stored in skeletal and cardiac muscles
Affects heart, skeletal muscle, liver, nerves, and endocrine function
The vitamin B complex carnitine, which contains basic substances produced in the liver, brain, and kidneys, breaks down fatty acids in mitochondria and converts them into energy, helping to promote fat combustion and strengthen muscle exercise.
Who needs to take L-carnitine?
People who lack L-carnitine
People who want to increase weight loss
People who want to improve their athletic ability
People with certain diseases (People with heart disease, diabetes and chronic fatigue syndrome)
Treatment Cycle
It is generally recommended to inject the treatment every 1-2 weeks, depending on its purpose.
Should be noted
✦ 01. The suitability of L-carnitine injections for individuals is determined by medical professionals. It should be noted that decisions should be made based on specific requirements and medical history
✦ 02. Before you start a treatment, you should always consult with the doctor first.

Benefits
✦ 01. Decrease in body fat
The most representative efficacy of L-carnitine breaks down fat. It plays a role in promoting the energization of fatty acids, and the Ministry of Food and Drug Safety also acknowledged that L-carnitine helps reduce body fat.
✦ 02. Protection of the heart
It is effective in protecting the heart by reducing oxidative stress and inflammation of heart muscle cells. L-carnitine is also used as a treatment for ischemic cardiomyopathy that occurs after myocardial infarction.
✦ 03. Improvement of athletic ability
When taking L-carnitine, it plays a role in improving muscle activity by increasing blood flow.
✦ 04. Blood sugar control
L-carnitine is a protein hormone that plays an important role in metabolism. It is known to help control blood sugar by improving insulin levels.



Real Q&A
✦ 01. Is there an age limit for this procedure?
There is generally no specific age limit for receiving L-carnitine injections. However, it should be noted that the use of L-carnitine injections should be determined on a case-by-case basis and with the guidance of a medical professional. For children or individuals younger than 18 years of age, a pediatrician may evaluate the specific needs, medical history, and potential risks or benefits associated with L-carnitine injections. Alternatively, it is particularly important to consult with your doctor first.
✦ 02. As far as I know, lipolysis components have severe side effects, is it safe?
Yes, Hanchung Medical's beauty line solution is made with only safe ingredients and two ingredients. L-carnitine and deoxycholate, are safe and effective ingredients.
L-carnitine: It transfers fatty acids to mitochondria produces energy through oxidation and burns afterward. It accelerates body fat breakdown because it facilitates the process of transporting fat and uses more fat to generate energy.
Deoxycholate: Deoxycholate is effective in reducing fat and cellulite by activating metabolism and converting fat into a water-soluble form, which is then expelled from the body without steroids.
✦ 03. Does it have skin sagging side effect after lipolysis injections?
It can if lipolysis injections contain steroids. Continuous exposure to steroids can lead to various side effects such as menstrual irregularities, osteoporosis, skin spasms, and skin atrophy, which are dangerous. In addition, the ingredient of general fat-releasing products is PPC, which has a strong fat-releasing effect, while it has many side effects. Typical side effects include hypothermia, decreased skin elasticity, and a long recovery period.
✦ 04. So-called Britney's shot. Is it safe?
The PPC (Polyen Phodphatidy|choline) injection is called the "Britney injection" because it was injected by Hollywood's popular female singer Britney. When fat-dissolving substances extracted from soybeans are injected into fat-rich areas, a substance called deoxycholate activates metabolism. It helps to convert it into water solubility and releases it through sweat, urine, etc. Many plastic surgeons promote PPC injections as safe and simple obesity treatment injections, saying that you can easily select and lose the flesh of the desired area.

Fat Dissolving Injection VS Bijunel Beauty Line Solution VS Liposuction
Decide after you look up the differences between Fat Dissolving Injection, Bijunel Beauty Line Solution, Liposuction
Those who do not want to get a liposuction can try the Bijunel Beauty Line Solution Injection Procedure

Treatment areas
Cheekbone
Thighs
Double chin
Forearm
Abdomen
Thighs
Cheekbones
Just the parts you want! Lightly, slimly, smoothly

What if you felt that normal lipolysis injections had no effect?
Combine these procedures!
Bijunel Beauty line solution Iniection procedure (body) + High frequency
Bijunel Beauty line solution After the injection procedure the process of change
Bijunel Beauty line solution Injection (Face) + In-mode, Shrink
It can be managed with a V-line jawline and a firm and elastic face, and it is to see the combined effect of melting fat by injection and destroying fat cells by in-mod. Each has a different mechanism for reducing fat, so you can expect a better effect when you combine the two than when you combine them with one.
Do you have more questions about Beauty-line solution or want to buy it? Contact us Han's kin 🤩
We look forward to introducing you to more derma products in the future :)
2 notes
·
View notes
Text
Hypothyroidism in Dogs: Symptoms, Causes and Treatment

When a dog’s thyroid gland does not produce enough hormones, a condition called hypothyroidism occurs. Middle-aged and older dogs are most commonly affected. Thyroid hormones help regulate many internal functions, such as metabolism and heart rate. When these hormones are low, vital functions are impaired and symptoms develop. Fortunately, with early detection and treatment, most hypothyroid dogs have a normal life expectancy.
Causes of hypothyroidism in dogs
Lymphocytic thyroiditis, an immune-mediated condition, is the most common cause of hypothyroidism in dogs. It occurs when the immune system attacks and destroys the thyroid gland, resulting in significant inflammation and low hormone production. It is unknown why the immune system decides to attack the thyroid gland, but it is thought to be hereditary.
Hypothyroidism in dogs can also occur due to thyroid gland atrophy. During this process, the functional tissue of the thyroid gland is replaced by fat. Veterinarians also don’t know why this process occurs.
A pituitary gland tumor is another cause, but it is extremely rare. The pituitary gland is located at the base of a dog’s brain and is responsible for secreting thyroid stimulating hormone. In dogs with a pituitary tumor, this process is impaired, and the thyroid gland is not stimulated. Therefore, thyroid hormones are not produced.

Symptoms of hypothyroidism in dogs
Hypothyroidism causes numerous symptoms in dogs, which may include the following:
Weight gain despite a normal appetite
Fat accumulation around shoulders, neck, and hind end
Lethargy
Dull hair coat
Slow hair regrowth
Flaky and/or thickened skin
Patches of alopecia (hair loss)
Slow heart rate
Cold intolerance
Recurrent skin and ear infections
Fertility issues
Reduced tear production (dry eye)
Nerve abnormalities
Dogs with hypothyroidism may have high cholesterol, high fat content and mild anemia on bloodwork.
How to treat hypothyroidism in dogs
Dogs with hypothyroidism require oral supplementation of a synthetic thyroid hormone called levothyroxine. This medication is given daily and is relatively inexpensive. The dose, which is determined by the dog’s weight, may change over time based on his response to treatment. Periodic bloodwork helps the veterinarian assess hormone levels and adjust the dose when necessary. Supplementation is required for the remainder of the pet’s life.
Since hypothyroid dogs are already prone to high cholesterol, switching to a low-fat kibble is beneficial. Omega-3 fatty acids also promote a healthier skin and coat. Your veterinarian can recommend the best type of food to meet your dog’s specific needs.
Life expectancy
Hypothyroidism is not a curable condition. However, most healthy, hypothyroid dogs live long, happy lives with the proper monitoring and treatment. Dogs with additional health issues, such as heart disease or kidney disease, may have shorter lifespans due to the difficulty in managing hypothyroidism alongside concurrent illness.
If left untreated, hypothyroidism results in a poor quality of life, an increased risk of complications and a reduced lifespan. Early diagnosis ensures your pet receives the treatment he needs to be happy and healthy. If you notice any signs of hypothyroidism in your dog, bring him to the veterinarian for evaluation.
#hyperthyroidism#dog health#dog thyroid health#hyperthyroidism in dogs#Dog Hypothyroidism#dog thyroids
8 notes
·
View notes
Text
Pulmonary Edema

Introduction
Pulmonary edema is a condition that results from the abnormal accumulation of fluid in the lungs, leading to impaired gas exchange and respiratory distress. This comprehensive discourse aims to provide an in-depth analysis of pulmonary edema, covering its pathophysiology, etiology, clinical manifestations, diagnostic modalities, treatment strategies, prevention strategies, and associated complications.
Pathophysiology of Pulmonary Edema

Pulmonary edema develops when there is an imbalance between the hydrostatic and oncotic pressures within the pulmonary vasculature. This imbalance leads to an increase in capillary permeability and the extravasation of fluid into the interstitial space and alveoli of the lungs. Several mechanisms contribute to this process, including increased capillary hydrostatic pressure due to heart failure, increased vascular permeability due to inflammation or injury, and decreased oncotic pressure due to hypoalbuminemia or capillary leak syndrome.
Etiology of Pulmonary Edema
The etiology of pulmonary edema can be categorized into cardiogenic and noncardiogenic causes. Cardiogenic pulmonary edema occurs secondary to heart failure or other cardiac conditions that result in elevated left atrial pressure and pulmonary venous congestion. Noncardiogenic pulmonary edema, on the other hand, is caused by factors unrelated to heart dysfunction, such as acute respiratory distress syndrome (ARDS), aspiration, sepsis, or neurogenic pulmonary edema.
Clinical Manifestations of Pulmonary Edema

The clinical presentation of pulmonary edema varies depending on the underlying cause and severity of the condition. Common symptoms include dyspnea, orthopnea, paroxysmal nocturnal dyspnea, cough, frothy sputum, cyanosis, and crackles on auscultation. Severe cases may progress to respiratory failure, hypoxemia, and hemodynamic instability.
Diagnostic Modalities for Pulmonary Edema

Diagnosing pulmonary edema requires a thorough clinical evaluation, including a detailed medical history, physical examination, and various diagnostic tests. Imaging studies such as chest X-ray, computed tomography (CT) scan, and lung ultrasound can provide valuable information about lung parenchymal changes and the presence of pulmonary congestion. Laboratory tests, including arterial blood gas analysis, brain natriuretic peptide levels, and electrolyte measurements, may also aid in the diagnosis and assessment of disease severity.
Treatment Strategies for Pulmonary Edema
The management of pulmonary edema involves addressing the underlying cause, relieving symptoms, and preventing complications. Initial treatment often includes supplemental oxygen therapy to improve oxygenation and reduce respiratory distress. Diuretics, such as furosemide or bumetanide, are commonly used to reduce fluid overload and alleviate pulmonary congestion. In cases of cardiogenic pulmonary edema, vasodilators, inotropes, or mechanical ventilation may be necessary to improve cardiac function and gas exchange.
Prevention Strategies for Pulmonary Edema
Preventing pulmonary edema requires a broad approach aimed at managing underlying risk factors and promoting healthy lifestyle habits. Patients with known cardiac conditions should adhere to prescribed medications, maintain a low-sodium diet, and monitor fluid intake to prevent fluid retention and exacerbation of heart failure. Individuals at risk of noncardiogenic pulmonary edema should avoid exposure to toxins, practice proper respiratory hygiene, and seek prompt medical attention for respiratory infections or injuries.
Complications of Pulmonary Edema

Untreated or inadequately managed pulmonary edema can lead to several complications, including acute respiratory distress syndrome (ARDS), cardiogenic shock, acute kidney injury, pulmonary hypertension, and death. Prompt recognition and intervention are essential to prevent progression to these life-threatening complications and improve patient outcomes.
Conclusion
Pulmonary edema is a complex and potentially life-threatening condition that requires prompt recognition, accurate diagnosis, and appropriate management. By understanding the underlying pathophysiology, etiology, clinical manifestations, diagnostic modalities, treatment strategies, prevention strategies, and associated complications of pulmonary edema, healthcare providers can optimize patient care and outcomes. Continued research efforts aimed at elucidating the mechanisms underlying pulmonary edema and identifying novel therapeutic targets are essential to further improve patient outcomes and reduce the global burden of this condition.
Embarking on your journey in the field of medicine is both exciting and challenging. As you navigate through your rigorous study period, it’s essential to seek guidance and assistance whenever needed to ensure your success.
At Expert Academic Assignment Help, we understand the demands of medical education and are here to support you every step of the way. Whether you require assistance with assignments, research papers, or exam preparation, our team of experts is dedicated to providing you with the help you need to excel in your studies.
Don’t hesitate to reach out to us for guidance, academic support, or any questions you may have. You can contact us via email at [email protected]
#assignment help#medical students#healthcare#nursing student#nursing school#expert assignment writers#academic assignments#homework help#do your homework#pharmacy student#pharmacy technician#pharmacology#health and wellness#health tips#health#medicine#treatment#health & fitness#healthylifestyle#high school#essay writing#essay#academic writing
2 notes
·
View notes
Text
What Is A Dual Organ Transplant? When Do You Need A Dual Organ Transplant?

A combined or dual organ transplant is a viable option for those who have suffered multiple organ failures wherein the patient will receive two organs simultaneously during one surgical procedure. A dual organ transplant may usually include a combined liver and kidney transplant or a pancreas and kidney transplant. Whether a liver and kidney transplant or a pancreas and kidney transplant, both organs must be replaced when they fail to function properly. The most common type of dual organ transplant is a kidney-pancreas transplant, which is performed on patients with type 1 diabetes who also have end-stage renal/kidney failure.
When Do You Need Dual Organ Transplant?
When you suffer from end-stage diseases like kidney failure and liver failure associated with comorbidities such as diabetes, congenital defects, autoimmune disorders, chronic infections, or long-term damage from substance abuse, you may have to undergo dual organ transplantation. Some patients may have a genetic predisposition to develop multiple organ failure, while others may experience organ damage as a result of an accident or injury. Patients undergo liver and kidney transplants because their liver and kidney fail to function. Those who have to undergo pancreas and kidney transplantation have kidney failure and suffer from insulin resistance (diabetes) simultaneously. Liver and kidney transplantation is recommended in case of Chronic Kidney Disease and defects in the liver at the same time.
Visit a top multispecialty hospital if you or your loved one needs a dual organ transplant in Old Airport Road.
What to Expect from Dual Organ Transplant?
There are many advantages of dual organ transplants. Some of these are:
Two Organ Transplants Simultaneously
One of the significant benefits of a dual organ transplant is that you receive two organs simultaneously and do not need to undergo two surgeries separately.
Less Suffering
Undergoing surgery may drain a patient. When two organs are transplanted in one surgery, the patient is relieved from undergoing two surgeries. Thus, a dual organ transplant helps the patient avoid additional surgeries and recover faster.
Long-Term Outcomes
For patients with end-stage organ diseases, a dual organ transplant can greatly improve their quality of life and increase their life expectancy.
Steps Involved in Dual Organ Transplant
There are different steps involved in the transplantation of various organs.
Kidney and Liver Transplant
To perform kidney and liver transplants together, the patient has to undergo a series of tests and evaluations such as a comprehensive medical evaluation, blood tests, and imaging studies, to determine if they are healthy enough to undergo the transplantation surgery. The liver and kidneys are often received from a deceased donor. The size of the liver must exceed 2% of the recipient's body weight. After the liver implantation, the single kidney is implanted into the right or left of the liver transplantation.
The liver will be transplanted in the following procedure:
The doctor will make an incision in your abdomen.
Blood vessels will be separated from your diseased liver.
The diseased liver will be replaced with a healthy liver.
The blood vessels will be reconnected.
The incision will be closed and the patient will be moved to the recovery room.
To transplant a kidney, the doctor will follow the procedure mentioned below:
The surgeon will place your kidney in the area of the lower abdomen. The new kidney is placed under the existing kidney. The existing kidney is removed if the doctor finds it is cancerous or leads to increased blood pressure.
Kidney and Pancreas Transplant
A simultaneous kidney and pancreas transplant is required when a patient suffers from kidney failure and diabetes and needs a very high insulin dose to control diabetes. Once the doctor confirms that you require a kidney and pancreas transplant through a complete medical assessment, blood tests, imaging tests, etc., you will wait for a donor kidney and pancreas. The doctor will test the compatibility when the donor's kidney and pancreas are available.
During the procedure, the surgeon will place the new kidney below the left side of the abdomen and connects the blood vessels to the kidney. The vein and artery are then connected to the new kidney, and the ureter of the new kidney is also connected to your bladder. After that, the new pancreas is placed below the right side of the abdomen and connects the blood vessels. The kidney and pancreas combined surgery take almost 5 to 7 hours and you may have to stay in the hospital for up to 2 weeks.
The surgeon will monitor your condition for the next few days after the surgery, whether it is a combined liver and kidney transplant or a kidney and pancreas transplant. If everything is found normal, you will be discharged from the hospital with a post-transplant care module, which includes regular check-ups and monitoring of the function of the new organs. By following these guidelines and taking immunosuppressant medications as prescribed, patients can help ensure the long-term success of their dual organ transplant.
Risks Involved in Dual Transplants
Risks in dual organ transplants depend on the health of the patients. Since your surgeon will monitor your entire health, there is less chance of risk during the surgery. In rare cases, a patient undergoing dual transplant surgery may suffer bleeding, pain, and other infections.
Currently, dual organ transplant has emerged as an effective way for those who have suffered an acute disease. This transplant procedure is recommended when there is no other option left. The organs are received normally from a deceased patient, and you will be on a waiting list until the organs are available.
Consult a nephrologist in Old Airport Road if you require dual organ transplant services.
FAQs
Name some complications of organ transplant.
Rejection, infection, high blood pressure, and delayed graft function are common complications of organ transplants.
Which is the most complicated organ to transplant?
Lungs are the most complex organs for transplant as they are more susceptible to infections.
Can two organs be transplanted together?
Yes, two organs can indeed be transplanted together. This procedure is called a combined or dual organ transplant.
3 notes
·
View notes
Video
youtube
WATCH this 3 Min 3 Sec Shared Personal Testimony from Debra Shttps://youtu.be/GG1Rb-Yo_3oMAKE SURE TO SUBSCRIBE TO OUR YOUTUBE CHANNEL while watching so you never miss a testimonyI have experienced dramatic results using CTFO's 10xPure CBD 1500 & XanthoMyst. I have had severe inflammation complications due to using contrast dye in a CAT scan I had done at the hospital. While in the hospital, I suffered a heart attack on teh table, and my kidneys shut down, and I was out for 5 hours.Two years ago, I was diagnosed with stage five kidney disease. I began to see a kidney specialist. I asked him how long it would take for my kidneys to return to normal and for my inflammation to lessen. He said, “Debra, your kidney function will never return to normal.” …do you know what my response was? I told him to “just watch me.” lolToday my kidneys have bounced back to almost where they had been before this unfortunate “toxic overload” to my body due to the contrast dye.^ Disclaimer: These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.
1 note
·
View note
Text
There was actually a study that showed that riding Big Thunder Mountain Railroad in Walt Disney World can help pass kidney stones:
https://jom.osteopathic.org/abstract/validation-of-a-functional-pyelocalyceal-renal-model-for-the-evaluation-of-renal-calculi-passage-while-riding-a-roller-coaster/
https://www.livescience.com/56261-kidney-stones-roller-coaster.html
My urologist has said, multiple times, that she wishes she could get insurance to cover a trip to Disney World, because for LOT of her patients, this would be the simplest and most effective solution! Also that more studies were done to see about other roller coasters (thus far, other Disney coasters at least aren't as effective; something about BTMR Just Works)
So no, not a speedboat, but an example of something "absurd" that might be medically necessary anyway.

14K notes
·
View notes
Text
Top Nephrology Hospitals in Ambur: Your Guide to Kidney Health
When it comes to maintaining kidney health, finding a specialized nephrology hospital is essential for effective diagnosis and treatment. In Ambur, a town known for its vibrant community and rich history, residents have access to several nephrology hospitals that provide comprehensive care for various kidney-related conditions. This article will explore the importance of nephrology, the services offered by nephrology hospitals, and how to choose the best nephrology hospital in Ambur for your needs.
Understanding Nephrology
Nephrology is the branch of medicine that focuses on the diagnosis and treatment of kidney diseases. The kidneys play a vital role in filtering waste products from the blood, regulating blood pressure, and maintaining electrolyte balance. Kidney Treatment in Ambur When kidney function declines, it can lead to serious health issues, including chronic kidney disease (CKD) and kidney failure. Therefore, specialized care from a nephrologist is essential for managing these conditions effectively.

Services Offered by Nephrology Hospitals
Nephrology hospitals in Ambur provide a wide range of services to address various kidney-related issues. Here are some of the key services you can expect:
Comprehensive Diagnostic Services: Nephrology hospitals offer thorough diagnostic evaluations, including blood tests, urine tests, and imaging studies. These assessments help identify kidney problems early, allowing for timely intervention.
Medication Management: For patients with chronic kidney disease or other kidney disorders, nephrologists prescribe medications to manage symptoms and slow disease progression. This may include medications to control blood pressure, manage diabetes, and reduce cholesterol levels.
Dialysis Services: For patients with advanced kidney failure, dialysis is a critical treatment option. Nephrology hospitals in Ambur provide both hemodialysis and peritoneal dialysis, ensuring that patients receive the necessary care to filter waste from their blood.
Kidney Transplant Services: In cases where kidney function is severely compromised, a transplant may be necessary. Nephrology hospitals often have partnerships with transplant centers, facilitating the process for patients in need of a new kidney.
Nutritional Counseling: Diet plays a significant role in kidney health. Nephrology hospitals typically offer nutritional counseling to help patients develop meal plans that support kidney function and overall health.
Importance of Choosing the Right Nephrology Hospital
Selecting the right nephrology hospital is crucial for effective treatment and management of kidney-related issues. Here are some factors to consider when making your choice:
Expertise and Credentials: Look for hospitals with qualified nephrologists who have specialized training and experience in treating kidney diseases. Research their credentials and areas of expertise to ensure you receive the best care.
Facilities and Technology: A well-equipped nephrology hospital should have modern facilities and advanced technology for diagnosis and treatment. This includes state-of-the-art dialysis units and imaging equipment.
Patient Reviews and Testimonials: Reading patient reviews can provide valuable insights into the quality of care offered by a nephrology hospital. Look for testimonials that highlight successful treatment outcomes and patient satisfaction.
Accessibility and Location: Consider the hospital's location and accessibility. A conveniently located nephrology hospital can make it easier for you to attend regular appointments and treatments.
Support Services: A good nephrology hospital should offer comprehensive support services, including counseling, education, and resources for patients and their families.
Conclusion
When it comes to kidney health, finding a reputable nephrology hospital in Ambur is essential for effective diagnosis and treatment. With a range of services, including medication management, dialysis, and transplant options, these specialized facilities are equipped to handle various kidney-related issues. By considering factors such as expertise, facilities, and patient reviews, you can make an informed decision about where to seek care. Remember, your kidneys are vital to your overall health—don’t hesitate to reach out for help if you experience any symptoms or concerns. Prioritize your kidney health by choosing the right nephrology hospital in Ambur today!
0 notes