#Immunotherapy for lung cancer
Explore tagged Tumblr posts
Text
How Lung Cancer Affects Your Body?

Dr. Chinnababu Sunkavalli, a robotic surgical oncologist, explains how lung cancer affects your body. Symptoms include a persistent cough, trouble breathing, chest pain, and fatigue. The cancer can also spread, causing more severe health issues. To Know more about Dr. Chinnababu Sunkavalli, follow his YouTube channel.
youtube
#Lung cancer symptoms#Lung cancer treatment#Lung cancer diagnosis#Non-small cell lung cancer#Small cell lung cancer#Immunotherapy for lung cancer#Targeted therapy for lung cancer#Lung cancer awareness#Lung cancer research#Lung cancer survivor#Youtube
0 notes
Text

Immunotherapy for Lung Cancer
Experience groundbreaking Immunotherapy for Lung Cancer at our advanced medical center. Our tailored treatments harness the power of your immune system to target and fight cancer cells effectively. With a patient-centric approach, our expert team delivers personalized care, offering hope and improved outcomes for individuals battling lung cancer. Embrace innovative therapies designed to enhance your body's natural defenses and pave the way for a brighter future. Trust in our comprehensive Immunotherapy solutions to provide you with the strength and resilience needed to overcome the challenges of lung cancer with confidence.
0 notes
Text
Cancer Patient's Experience with Immunotherapy Treatment
youtube
Immunotherapy has brought about transformative changes in the landscape of cancer treatment, offering hope and improved outcomes for many patients. Here, we delve into a cancer patient's experience with immunotherapy treatment, highlighting the journey, challenges, and potential rewards.
#cancer immunotherapy#immunotherapy cost#immunotherapy for lung cancer#immunotherapy for liver cancer#Cancer Patients#Youtube
0 notes
Text
A blueprint for better cancer immunotherapies
New Post has been published on https://thedigitalinsider.com/a-blueprint-for-better-cancer-immunotherapies/
A blueprint for better cancer immunotherapies


Immune checkpoint blockade (ICB) therapies can be very effective against some cancers by helping the immune system recognize cancer cells that are masquerading as healthy cells.
T cells are built to recognize specific pathogens or cancer cells, which they identify from the short fragments of proteins presented on their surface. These fragments are often referred to as antigens. Healthy cells will will not have the same short fragments or antigens on their surface, and thus will be spared from attack.
Even with cancer-associated antigens studding their surfaces, tumor cells can still escape attack by presenting a checkpoint protein, which is built to turn off the T cell. Immune checkpoint blockade therapies bind to these “off-switch” proteins and allow the T cell to attack.
Researchers have established that how cancer-associated antigens are distributed throughout a tumor determines how it will respond to checkpoint therapies. Tumors with the same antigen signal across most of its cells respond well, but heterogeneous tumors with subpopulations of cells that each have different antigens, do not. The overwhelming majority of tumors fall into the latter category and are characterized by heterogenous antigen expression. Because the mechanisms behind antigen distribution and tumor response are poorly understood, efforts to improve ICB therapy response in heterogenous tumors have been hindered.
In a new study, MIT researchers analyzed antigen expression patterns and associated T cell responses to better understand why patients with heterogenous tumors respond poorly to ICB therapies. In addition to identifying specific antigen architectures that determine how immune systems respond to tumors, the team developed an RNA-based vaccine that, when combined with ICB therapies, was effective at controlling tumors in mouse models of lung cancer.
Stefani Spranger, associate professor of biology and member of MIT’s Koch Institute for Integrative Cancer Research, is the senior author of the study, appearing recently in the Journal for Immunotherapy of Cancer. Other contributors include Koch Institute colleague Forest White, the Ned C. (1949) and Janet Bemis Rice Professor and professor of biological engineering at MIT, and Darrell Irvine, professor of immunology and microbiology at Scripps Research Institute and a former member of the Koch Institute.
While RNA vaccines are being evaluated in clinical trials, current practice of antigen selection is based on the predicted stability of antigens on the surface of tumor cells.
“It’s not so black-and-white,” says Spranger. “Even antigens that don’t make the numerical cut-off could be really valuable targets. Instead of just focusing on the numbers, we need to look inside the complex interplays between antigen hierarchies to uncover new and important therapeutic strategies.”
Spranger and her team created mouse models of lung cancer with a number of different and well-defined expression patterns of cancer-associated antigens in order to analyze how each antigen impacts T cell response. They created both “clonal” tumors, with the same antigen expression pattern across cells, and “subclonal” tumors that represent a heterogenous mix of tumor cell subpopulations expressing different antigens. In each type of tumor, they tested different combinations of antigens with strong or weak binding affinity to MHC.
The researchers found that the keys to immune response were how widespread an antigen is expressed across a tumor, what other antigens are expressed at the same time, and the relative binding strength and other characteristics of antigens expressed by multiple cell populations in the tumor
As expected, mouse models with clonal tumors were able to mount an immune response sufficient to control tumor growth when treated with ICB therapy, no matter which combinations of weak or strong antigens were present. However, the team discovered that the relative strength of antigens present resulted in dynamics of competition and synergy between T cell populations, mediated by immune recognition specialists called cross-presenting dendritic cells in tumor-draining lymph nodes. In pairings of two weak or two strong antigens, one resulting T cell population would be reduced through competition. In pairings of weak and strong antigens, overall T cell response was enhanced.
In subclonal tumors, with different cell populations emitting different antigen signals, competition rather than synergy was the rule, regardless of antigen combination. Tumors with a subclonal cell population expressing a strong antigen would be well-controlled under ICB treatment at first, but eventually parts of the tumor lacking the strong antigen began to grow and developed the ability evade immune attack and resist ICB therapy.
Incorporating these insights, the researchers then designed an RNA-based vaccine to be delivered in combination with ICB treatment with the goal of strengthening immune responses suppressed by antigen-driven dynamics. Strikingly, they found that no matter the binding affinity or other characteristics of the antigen targeted, the vaccine-ICB therapy combination was able to control tumors in mouse models. The widespread availability of an antigen across tumor cells determined the vaccine’s success, even if that antigen was associated with weak immune response.
Analysis of clinical data across tumor types showed that the vaccine-ICB therapy combination may be an effective strategy for treating patients with tumors with high heterogeneity. Patterns of antigen architectures in patient tumors correlated with T cell synergy or competition in mice models and determined responsiveness to ICB in cancer patients. In future work with the Irvine laboratory at the Scripps Research Institute, the Spranger laboratory will further optimize the vaccine with the aim of testing the therapy strategy in the clinic.
#Analysis#antigen#author#Biological engineering#Biology#Cancer#cancer cells#cancers#cell#Cells#clinical#competition#data#dynamics#engineering#forest#Future#growth#Health sciences and technology#how#immune response#immune system#immunology#immunotherapies#immunotherapy#Impacts#insights#it#Koch Institute#lung cancer
0 notes
Text
Lung cancers stays one of the hardest cancers to deal with, however advancements in treatment alternatives are imparting desire. Among these, immunotherapy for lung cancers in India has emerged as a significant improvement. Visit us https://bit.ly/4erDtp5
0 notes
Text
youtube
1 note
·
View note
Text
Immunotherapy for Lungs Cancer
Cell therapy, specifically immunotherapy for cancer patients, is being researched as a potential treatment option for Lungs cancer patients. Personalized immunotherapy uses a person's own immune cells to fight cancer.
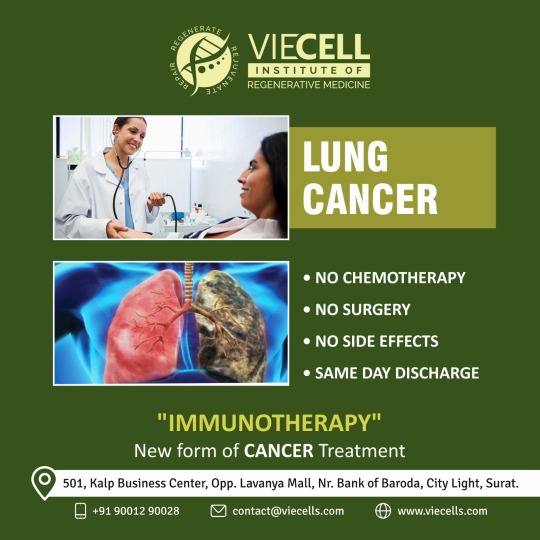
To Know more about Cancer Immunotherapy Please visit: https://www.viecells.com/ Email: [email protected] Ph: +91-9001290028
#cancer#lungscancer#lungs#immunotherapy#NK#NKCells#NKcelltreatment#cancerimmunotherapy#cancertreatment#viecells#gujarati#surat#india
0 notes
Text
Lung Cancer Unveiled: Everything You Need to Know About Causes, Symptoms, and Treatment Options
Lung cancer
Overview
Lung cancer is a type of disease that begins in the lungs and is one of the leading causes of cancer deaths worldwide. The lungs are two vital organs in your chest that take in oxygen and release carbon dioxide. Cell lysis in the lungs is an important source of spread of malignant growth worldwide.
Risk factor
The most important risk factor for lung cancer is smoking, but non-smokers can also develop the disease. The time and amount of cigarettes smoked can affect the likelihood of a lung cell analysis. Why and for what Smoking is the most common cause of lung cancer, but exposure to secondhand smoke can also increase the risk of this disease.
Some lung cancers have an unknown cause, making early detection and prevention difficult.
Types of lung cancer
There are two main types of lung cancer: small cell lung cancer and non-small cell lung cancer. Small cell lung cancer is mostly associated with smokers, while non-small cell lung cancer includes several different types of lung cancer, including adenocarcinoma, squamous cell carcinoma, and squamous cell carcinoma. Lung cancer can cause various complications such as shortness of breath, coughing up blood and pain. If cancer spreads to the central airways, shortness of breath may occur, while coughing up blood may be caused by bleeding from the disease. Pain may also occur if cancer has spread to other parts of the body, such as the bones. Fortunately, there are several treatments available to treat these complications, so it's important to discuss all symptoms with your doctor. Caring Surgery: Surgery is the main treatment option for early stage lung cancer. During the operation, the cancerous tissue is removed along with the surrounding healthy tissue. Radiation therapy: Radiation therapy uses high-energy radiation to destroy cancer cells. It can be used alone or in combination with other treatments. Chemotherapy: Chemotherapy uses drugs to kill cancer cells. It can be given orally or intravenously and is often used in combination with other treatments. Targeted therapy: Targeted therapy uses drugs that target specific genes or proteins in cancer cells to stop their growth. Immunotherapy: Immunotherapy is a newer form of treatment that increases the immune system's ability to recognize and destroy cancer cells. Palliative care: Palliative care focuses on treating symptoms and improving quality of life in patients with advanced lung cancer.
conclusion
lung cancer is a serious disease that affects the lungs and can have many harmful effects on the body. Although smoking is the most common cause of this disease, non-smokers can also develop it. It is very important to be aware of the symptoms of lung cancer and see a doctor immediately if they appear. In addition, early detection and prevention through regular health checks and smoking cessation can help reduce the risk of developing this disease.
For more information visit www.oncorelief.in
#lung cancer#causes#treatment options#smoking#radiation therapy#chemotherapy#surgery#targeted therapy#immunotherapy#palliative care#early detection#symptoms
0 notes
Text
Best Lung Cancer Immunotherapy
Lung Cancer Immunotherapy is a therapy that aims to increase the immune system's response to lung cancer cells. It is a promising treatment that has shown promise in patients with Stage 3 non-small cell lung cancer. Hawaii Oncology have Dr. Ryon Nakasone serves as an Assistant Professor of Medicine at the University of Hawaii. He has also earned his MBA in Healthcare from La Sierra University. His areas of interest are diverse and include such areas as Lung Cancer, Colon Cancer, and Prostate Cancer.
1 note
·
View note
Text
"Doctors have begun trialling the world’s first mRNA lung cancer vaccine in patients, as experts hailed its “groundbreaking” potential to save thousands of lives.
Lung cancer is the world’s leading cause of cancer death, accounting for about 1.8m deaths every year. Survival rates in those with advanced forms of the disease, where tumours have spread, are particularly poor.
Now experts are testing a new jab that instructs the body to hunt down and kill cancer cells – then prevents them ever coming back. Known as BNT116 and made by BioNTech, the vaccine is designed to treat non-small cell lung cancer (NSCLC), the most common form of the disease.
The phase 1 clinical trial, the first human study of BNT116, has launched across 34 research sites in seven countries: the UK, US, Germany, Hungary, Poland, Spain and Turkey.
The UK has six sites, located in England and Wales, with the first UK patient to receive the vaccine having their initial dose on Tuesday [August 20, 2024].
Overall, about 130 patients – from early-stage before surgery or radiotherapy, to late-stage disease or recurrent cancer – will be enrolled to have the jab alongside immunotherapy. About 20 will be from the UK.
The jab uses messenger RNA (mRNA), similar to Covid-19 vaccines, and works by presenting the immune system with tumour markers from NSCLC to prime the body to fight cancer cells expressing these markers.
The aim is to strengthen a person’s immune response to cancer while leaving healthy cells untouched, unlike chemotherapy.
“We are now entering this very exciting new era of mRNA-based immunotherapy clinical trials to investigate the treatment of lung cancer,” said Prof Siow Ming Lee, a consultant medical oncologist at University College London hospitals NHS foundation trust (UCLH), which is leading the trial in the UK.
“It’s simple to deliver, and you can select specific antigens in the cancer cell, and then you target them. This technology is the next big phase of cancer treatment.”
Janusz Racz, 67, from London, was the first person to have the vaccine in the UK. He was diagnosed in May and soon after started chemotherapy and radiotherapy.
The scientist, who specialises in AI, said his profession inspired him to take part in the trial. “I am a scientist too, and I understand that the progress of science – especially in medicine – lies in people agreeing to be involved in such investigations,” he said...
“And also, I can be a part of the team that can provide proof of concept for this new methodology, and the faster it would be implemented across the world, more people will be saved.”
Racz received six consecutive injections five minutes apart over 30 minutes at the National Institute for Health Research UCLH Clinical Research Facility on Tuesday.
Each jab contained different RNA strands. He will get the vaccine every week for six consecutive weeks, and then every three weeks for 54 weeks.
Lee said: “We hope adding this additional treatment will stop the cancer coming back because a lot of time for lung cancer patients, even after surgery and radiation, it does come back.” ...
“We hope to go on to phase 2, phase 3, and then hope it becomes standard of care worldwide and saves lots of lung cancer patients.”
The Guardian revealed in May that thousands of patients in England were to be fast-tracked into groundbreaking trials of cancer vaccines in a revolutionary world-first NHS “matchmaking” scheme to save lives.
Under the scheme, patients who meet the eligibility criteria will gain access to clinical trials for the vaccines that experts say represent a new dawn in cancer treatment."
-via The Guardian, May 30, 2024
#cw cancer#cancer research#cancer#lung cancer#nhs#england#vaccine#cancer vaccines#public health#medical news#good news#hope
1K notes
·
View notes
Text
Immunotherapy for Lung Cancer
Immunotherapy represents a groundbreaking approach in lung cancer treatment, providing significant strides in care. Differing from conventional methods like chemotherapy and targeted therapy, immunotherapy harnesses the body’s immune system to combat cancer cells.
With various types, including immune checkpoint inhibitors, cancer vaccines, and adoptive T cell therapy, it holds promise for improved outcomes. Although side effects exist, recent studies indicate positive impacts on life expectancy, showcasing the transformative potential of immunotherapy in the fight against lung cancer. Consult with your healthcare team for personalized guidance on available immunotherapy options.
Experience groundbreaking Immunotherapy for Lung Cancer at our advanced medical center. Our tailored treatments harness the power of your immune system to target and fight cancer cells effectively. With a patient-centric approach, our expert team delivers personalized care, offering hope and improved outcomes for individuals battling lung cancer. Embrace innovative therapies designed to enhance your body's natural defenses and pave the way for a brighter future. Trust in our comprehensive Immunotherapy solutions to provide you with the strength and resilience needed to overcome the challenges of lung cancer with confidence.
0 notes
Text
Depression linked to deadly inflammation in lung cancer patients
Lung cancer patients with moderate to severe depression are 2 to 3 times more likely to have inflammation levels that predict poor survival rates, a new study found. The results may help explain why a substantial portion of lung cancer patients fail to respond to new immunotherapy and targeted treatments that have led to significantly longer survival for many people with the disease. Photo by…

View On WordPress
0 notes
Link
Dr. Ajay Sharma is famous as top medical oncologist in delhi and providing full treatment through immunotherapy for cancer treatment in delhi; meet best immunotherapy doctor in delhi for immunotherapy for lung cancer in delhi.
#immunotherapy for cancer treatment in delhi#immunotherapy for breast cancer in delhi#immunotherapy for liver cancer in delhi#immunotherapy for lung cancer in delhi#immunotherapy for cervical cancer in delhi#immunotherapy for pancreatic cancer in delhi#top medical oncologist in delhi#best immunotherapy doctor in delhi#best doctor for immunotherapy in delhi
1 note
·
View note
Text
i was diagnosed with stage 3b breast cancer and had 5 months of intense chemo at age 26.
i had a double mastectomy with reconstructive surgery, then an axillary lymph node dissection, then a summer of radiation, then months of oral chemo at 27.
right as i was finishing my oral chemo, it progressed to my lungs and became stage 4. i had more chemo, then a different chemo from the first time, and immunotherapy at 28 and 29.
then it moved to my spine, particularly almost my entire cervical spine, and i started a new chemo regimen that i will stay on as long as it keeps things stable, and in the meantime i had 10 rounds of very intense radiation on my neck that i just finished a week ago at age 30.
i turn 31 in 9 days.
im still alive.
i am still fucking alive.
age 26:

age 30:

22 notes
·
View notes
Text
The Scully Family In-Depth (Part XXI): Faith, Fear, and Scully Symbiosis, Part I

The concluding scene between Scully and her mother is enlightening: not only of their past, present, and future dynamics, but also of the heretical hierarchy she unconsciously erects with her loved ones. There are "other fathers"; but there are also interceding mothers, blind believers, and advocating consciences.
ALL HOPE IS LOST
Scully is lying in bed, wrestling for composure-- swallowing, raising her signature eyebrow-- as the camera pans in, narrowing further and further in on her lost, hopeless, terrified expression. Here, she is aware that the chip has “failed”; and finally believes that death is approaching.
When the door opens and Maggie whispers, “Dana?”, Scully turns abruptly away from the wall, a tear spilling from the corner of one eye.

“Dr. Zuckerman called. He, uh…” her mother rambles, worried and anxious. Catching herself, she affects unaffectedness, approaching with a spring in her step and false smile on her face-- “He said that you wanted to see me?”-- which drops, quickly, when her daughter sits up without a word, visibly troubled. “What is it?”


Scully lunges towards her mother, clinging in shaking horror.


“I’m so sorry,” she wobbles, voice stained with repentance and guilt as she struggles against her fear. “I fight… and I fight and I fight, but I’ve been so stupid." Grieved and shaken, she sniffles back tears clogging her throat.

Lost but relieved at her daughter’s openness, Maggie asks, “What is it?” with a maternal lilt to her voice. (One she might have used to unscramble a weepy confession over some minor infraction, or to unwind the logic behind a particularly challenging math problem.)

Scully pulls back, haunted. “I’ve come so far in my life on simple faith. And now when I need it the most, I just push it away.”

While her admittance explicitly refers to her Catholic beliefs, it also explicitly applies to her partnership and her cancer journey. Scully, despite vowing she would find the answers “for her own reasons” has clung to the hope that, against all the universal laws of science, she would survive terminal brain cancer. Her journey since Memento Mori has been to embrace the fight, to refuse to give up, to insist that she can save herself with her science; or, if push comes to shove, with Mulder’s truth. She likely gave up chemo after Scanlon-- there were no chemo treatments that would cure her, as stated-- and tried immunotherapy treatments instead so she could continue to work, to find answers; and pretended nothing was wrong because everything would be made right, soon. In Elegy, her report came up clean; but she still saw Harold Spuller, which shook her conviction that science was stalling the cancer (post here.) In Gethsemane, she was given a death sentence but refused to accept it; and still did not want her brothers (or Father McCue) to be told-- because deep down, despite her grand stances and "last wishes", she didn't believe she would die (post here.) In Redux I, she escaped a sense of helplessness by working, by trying to prove Mulder right while he plundered the DOJ: she believed he, if anyone, could save her. In Redux II, she panicked when her partner asked if conventional treatment needed to be halted (post here); and was shaken when her doctor admitted the only hope she had left would have to be “unconventional.”
Mulder became her faith: while she was languishing in Scanlon’s facility, she clung to his conviction, drawing upon it to record her defeated thoughts. She used it to rise from Betsy’s deathbed, to move forward with strength, to believe, deep down, that his truth and her faith would cure her. Mulder had doubts in his abilities-- gifting her a keychain in Tempus Fugit, pointing a gun at his head (at his failures) in Demons-- but Scully never did… until Elegy, until he ripped that conviction out from under both their feet. (“The doctor said I’m fine,” she’d said, clinging to shaky ground. “I hope that’s the truth,” he’d replied, showing her there was no ground to cling to.) Scully thought she gave up in Gethsemane, but Bill exposed her to herself (post here)-- “What are you doing at work, getting knocked down? What are you trying to prove? …To this guy, Mulder?” She was trying to prove something: that she hadn’t failed, that she’d done her best. And she felt those efforts had been rewarded by his last-ditch effort to get her a cure… and it had failed. She had failed.
Here, Scully can no longer dodge, run from, or escape the reality of her death: it is before her, again, after being banished in Memento Mori; and it has defeated her (and her partner’s, and her family’s) last hope. With this in mind, she called Maggie first to admit defeat so her mother relay to Mulder, a reversal of Memento Mori’s order of operations. She would rather disappoint her mother than her partner, not after everything they'd been through that year.

Maggie listens, sympathetically and without comment, assuming her daughter will close up if she misplaces a word.
Scully continues, becoming more fervent in her ravaging self-doubt while ripping out the cross from under her hospital gown. “I mean, why… why do I wear this?”


Her mother doesn’t respond, face softly grimacing at the brandished necklace-- possibly over its Ascension connections. At her daughter’s repeated, “Why do I wear this, Mom?”, she wisely keeps silent: the answer that contents her-- a strong belief in God-- wouldn’t, and hasn't, helped her daughter. It’s best to let emotion ride its course, and help Dana settle down afterwards.

“I put something that I don’t even know,” Scully asserts, “or understand under the skin of my neck. I will subject myself to these crazy treatments-- and I keep telling myself that I am doing everything I can. But it’s a lie!” She stops, eyes down, sitting in torment-- a grotesque mask's mockery of happiness-- waiting for her mother to say something, anything.


Maggie doesn’t doubt her daughter: “You have not lost your faith, Dana.”
And Scully hasn’t; but her self doubt is overwhelming her, is providing proof of her inadequacies with each new medical report-- with the final medical report-- and laughing her to scorn.

“I have,” Scully insists, before correcting herself, “in a way. When you, when you asked Father McCue to dinner to minister to my faith, I just closed off to him.”
I’ve discussed before that Melissa Scully acted as the voice of Scully’s conscience (posts here, here, here), and literally as her voice in One Breath. However, this scene in Redux II illustrates the importance of her dynamic with Maggie Scully: her mother acts as Scully’s confessor, just as her father acted as her god. Although Scully took the life of a snake as a little girl, it was Maggie who recalled the story-- in detail so specific that she only could have gotten it directly from Scully. It was Maggie who helped absolve her guilt in The Blessing Way and Wetwired. And most importantly, it was Maggie who patched together Captain Scully and their daughter's relationship; and Maggie who Scully turned to for guidance and reassurance at his funeral (Beyond the Sea) and on her deathbed (Redux II.)
But why? Bill Scully and Melissa didn’t have that relationship with Maggie; and we can assume Charlie falls in the same lines. Yet for Scully, the sun seems to rise and fall on the opinion of her parents. Maggie herself is constantly trying to point Dana to her own path, aware she has no answers that would truly satisfy her daughter: “he was your father” and “you haven’t lost your faith” are truths that she believes are the key to these complicated questions; but knows are not enough, yet.
We see this near deification stems back to Scully’s relationship with her father and extends outward to “other fathers.” But that’s not the whole truth: for every god there is an intermediary; for every Captain there is a wife who gives him “the look” after their daughter’s Christmas dinner (post here.) And for every god and intermediary there is a true believer. And even further, for every true believer there is a conscience that puts into words the deep mysteries of the heart.
And while Scully pedestalized her loved ones-- asking for their opinion on her FBI recruitment, asking for their forgiveness-- then duplicated these structures into other areas of her life-- be it as a disciple of Daniel Waterston's or as an intermediary confessor to (and true believer in) her partner-- her own pedestalized idols pushed back against or regretted their daises. Her father was a man who loved but forgot to translate that love into words, her mother is a woman reliant on her daughter’s strength, her sister was a woman who loved loudly and often overstepped, and her partner is a man who believes deeply in everyone but himself. These people are aware of their faults and voice them constantly to Scully; but she can’t-- or won’t-- see them because she is too afraid to accept their humanity and strike out completely on her own… not until all things, that is.
(Another interesting note: Redux II will later subtly hammer home the “other fathers” connection to Mulder via this convoluted dynamic Scully keeps perpetuating.)

Maggie tightens her mouth, battling relief and bittersweet hope at this confession. Faith in God has lent her strength, and she believes it will give her daughter strength, too. Further, she believes her daughter has been suppressing and choking on denial since the cancer diagnosis; and, while happy Dana is sharing this burden, that joy is marred by the circumstances.
To soothe her own emotions, she begins to put her daughter 'back together'-- a habit Scully seems to have adopted, in adulthood, with her partner. Maggie schools her emotions as best she can while patting her daughter’s hair, delicately combing loose strands back into shape, and smoothing out imaginary wrinkles on her shoulder. “What’s important now,” she mothers, gently but firmly, “is that you save your energy.”




Scully’s face loses its frenetic spark, sinking into hopeless depression. Her mouth is slick with saliva, and her eyes are filling with unshed tears.
This is the real reason she called her mother: “I’m not getting any better, Mom.”

Instantly, the true nature of Maggie’s feelings bubble to the surface: “You don’t know that yet,” she pleads, trying to bargain away her daughter’s finality with a smile and exaggerated head tilt-- a gesture she used, perhaps, when little Dana was distraught or hopeless. Still, her smile fades as Scully's tears continue to well up.


“The PET scan showed no improvement,” Scully confirms, looking up and down to hide from her own and her mother’s pain.


Maggie is crushed, her mouth beginning to warble uncontrollably-- so uncontrollably that Scully's own chin begins to pebble.


Seeing her daughter's distress, Maggie surges forward to hug them together, knowing her child well enough to intuit that emotions are better relieved in privacy.


CONCLUSION
More Scully symbiosis thoughts to come.
Thanks for reading~
Enjoy!
#txf#meta#The Scully Family In-Depth#Faith Fear and Scully Symbiosis Part I#mine#Redux II#S5#In-Depth#cancer arc#xf meta#Scully#Maggie Scully#Mulder#Bill Scully#Captain Scully#Melissa Scully#x-files#xfiles#the x files#thoughts#analysis
30 notes
·
View notes
Text
Patulin (C7H6O4), a mycotoxin produced by several types of fungi, is toxic to a variety of life forms, including humans, mammals, plants, and microorganisms. In particular, environments lacking proper hygienic measures during food production are susceptible to patulin contamination as many of these fungi species tend to grow on damaged or decaying fruits, specifically apples, and even contaminate apple products, such as apple sauce, apple juice, jams, and ciders. Responsible for a wide variety of health hazards, including nausea, lung congestion, ulcers, intestinal hemorrhages, and even more serious outcomes, such as DNA damage, immunosuppression, and increased cancer risk, patulin toxicity is a serious concern worldwide. As a result, many countries have imposed restrictions on the permitted levels of patulin in food products, especially baby foods as infants are more vulnerable to the effects of patulin. Treatment of patulin toxicity include oxygen therapy, immunotherapy, detoxification therapy, and nutrient therapy. However, as prevention is often better than cure, scientists have been on the lookout for efficient ways to mitigate patulin toxicity in food products. To this end, a research team including Associate Professor Toshiki Furuya from Tokyo University of Science (TUS) in Japan, recently screened for soil microorganisms that can potentially help keep patulin toxicity in check. Their study, published in MicrobiologyOpen, was co-authored by Ms. Megumi Mita, Ms. Rina Sato, and Ms. Miho Kakinuma, all from TUS.
Continue Reading
94 notes
·
View notes