#I can’t wait for April so I will be DONE with organisational psych and can just fly off to Ireland & Italy again lol
Explore tagged Tumblr posts
Text


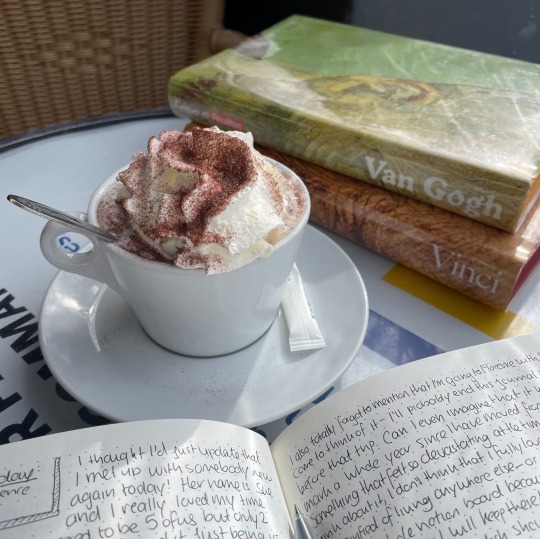

Some moments from this week! I tried fried ice cream with my bf for the first time (cafe isaka in paris!) and took some hot chocolate + journaling breaks from uni work <3
#I can’t wait for April so I will be DONE with organisational psych and can just fly off to Ireland & Italy again lol#studyblr#light academia#cottagecore#studyspo#dark academia#bookblr#uniblr#langblr#study inspiration#France#french#study aesthetic#chaotic academia
3K notes
·
View notes
Note
I'd really like to know a little about the logistics of hospitals adjusting to the current situation - would you be able to tell us a bit about that - how are wards being rearranged, staff being redeployed to different roles etc? It sounds like the hospitals look quite different to how they did several weeks ago if I've understood correctly. I'm glad to hear you're feeling a bit better, hope you're well soon!
Sure, I can try. Changing how we work:We receive regular updates via internal email. First, teaching and group sessions were cancelled. We were warned that some of our shifts would be adjusted - clinic sessions became clerking suspected covid patients. There are now no elective surgeries, no clinics (though some depts like mine can run phone clinics), and a lot of outpatient services are closed. We were soon told leave would probably be cancelled and we’d be likely to have our rotas changed or be redeployed. This was more than a month ago.
In my hospital (and I’m sure many others), they recently cancelled all leave for April, in case they need the staff. Bank holidays are now normal working days - presumably I won’t get time in lieu for the Bank Hols I’m working. I felt that this is risky - you need the staff capacity, but also you don’t want people to fatigue too early, or to become too demoralised. We try to socially distance as much as possible at work - not always easy given most offices are tiny and cramped, and it’s hard to run a ward round miles away from each other. We’re at risk of catching it from each other as well as patients because we’re constantly touching computers and equipment and having to get in close to talk to each other or help patients. We’ve moved where we hold handover, and we try to encourage people to leave if they don’t have to be here. Some ‘bright spark’ took out half the computers in the office to ensure people socially distance, though that just means more waiting for computers.
They’ve redeployed a lot of juniors, particularly from teams (like surgical teams, psych, GP, weird academic jobs where not much was going on) to clerking or the covid-19 wards. Between that and outpatient clinics being cancelled, there are more doctors of every grade of seniority that have been mobilised. It actually meant that when I was on take this week (seeing mostly suspected covid-19, not gonna lie), we were very well staffed. This is great, because it means we have spare capacity to deal with the peak when it comes. Plus I was still dealing with fatigue after my week off for likely covid-19 myself, and it really helped that work was unexpectedly manageable.
They’ve given us some sleep pods, and they’ve made arrangements for more staff to be able to stay over - with transport reduced, and people isolating away from families, more people are choosing to stay in hospital accommodation. We, keep getting donations of food and stuff from people, which is really nice, though I wish it’d go back to how it was before - less donations, but because people were happy. I guess it does improve morale, though. Hospital staff are motivated by food.
Reorganising the hospital:
They’ve basically split my hospital into ‘hot’ and ‘cold’ zones - places where we have patients with suspected covid-19 symptoms, and places for patients with no such symptoms. This means having two ED/A+E departments. Each hot zone has donning and doffing rooms - places to put on and take off PPE. Plenty of places where you have to wash your hands. You have to wear PPE (surgical mask, gloves, gown) even in ’cold’ places.In hot zones all patients wear a mask as a precaution and you usually have to wear more substantive PPE. I hear from friends that their hospitals operate pretty similarly - it’s standard to try to reduce contact between patients who could have covid-19, and those who don’t.
The corridors are quiet and eerie, rather like being oncall at night. Many staff wear masks between departments. Most of the admin staff are now working from home, so there are less employees in hospital than usual. The cafes are all now only take-aways, though you can still sit in the hospital canteen. Given how hard shopping is, it’s a great comfort that you can at least eat at work if the worst comes to the worst. I miss having spaces to sit - I don’t really want to eat my lunch on a covid-19 ward, and it’s important to leave your office to gain some separation from work mentally, for a short while.
They have turned some of the wards (often surgical - as there are now a lot less operations happening) into suspected covid-19 wards. Where our teams had extra capacity (i.e. weren’t at minimal staffing), people were randomly re-allocated to the covid-wards. This happened to me weeks ago. I didn’t mind it, but at the time it was still chaotic because they hadn’t quite formalised a plan for who was being re-allocated there, when. The system is now a lot more slick, at least in my hospital. This kind of thing is unprecedented - we’ve never reorganised entire hospitals or how we work, and certainly not under short notice, and it’s been evolving with the crisis. As it stands, most wards are either hot - suspected covid patients, or cold - patients which tested negative or are not suspected of aving the virus. My regular ward is one of the few cold wards, but we still test and diagnose covid pretty often. For what it’s worth, I feel my hospital have generally done the best job that they can. They have expanded ITU’s capacity extensively, and are coming up with all sorts of ways to ensure they have enough equipment and oxygen.
Almost all outpatient departments have shut, apart from dialysis. We no longer allow as many visitors in hospital - 1 visitor per day for patients who are seriously unwell or dying. Stable patients are not allowed visitors. For people with covid-19, household contacts usually can’t come because they are meant to be self-isolating at home. This means a lot of phone calls to relatives updating them on their loved ones. That’s one of the main ways this has affected us - we’re having a lot more of those “I’m sorry but your loved one is very sick” or resuscitation decision discussions on the phone, and that can be hard.
Equipment and clothes:
In my hospital, I’d say that fit-testing was departmental - it was down to individual departments to organise. And although they said they’d prioritise at risk departments and staff, with re-mobilisation that clearly wasn’t taken into consideration at first. It takes a while to fit test a ton of people - and a some people are failing fit test. I passed, but not necessarily with the kind of mask that’s available. Unfortunately, people like me were on ward cover or on the covid wards pretty early, so I had to do a lot of running around to get myself adequately tested and protected. We have PPE right now, and some clear guidance on a national level, although that doesn’t necessarily line up with PPE guidance in other places. There’s a lot of criticism of PPE policies across hospitals - people fear inadequate protection and inconsistency, and they fear exposure to a virus that can kill them, their loved ones or their patients. Guidance on what kind to use, and when, has changed over the weeks. We try to be sensible with how we use it.
They caved and gave us all scrubs to wear on the wards- 3 pairs each. Unfortunately there are no scrubs that aren’t a size large, so we are all swamped. I’ve bought some comfy but ugly clog type shoes that are easy to clean, and I plan to chuck them when this sorry episode is over. If it’s ever over. My scrubs are far, far too big (they’d be big on my 6′3′‘ dude, so on me they are like a literal tent that has to be rolled up) but I won’t get given an appropriate size when they order more. There was no other way to get scrubs - places like endoscopy or theatres refuse to help people from other departments, even if you literally tell them you’ve been deployed to a covid-19 ward. So it’s either work in tent-like pajamas or your home clothes which may not be as suitable. Dresses and skirts are fine normally, but too flappy in an infection-laden situation. I’m happy to be wearing scrubs, I just wish that they fit. But overall, I feel that we’ve been coping where I am.
6 notes
·
View notes