#EHRS
Explore tagged Tumblr posts
Text
Epic Systems, a lethal health record monopolist

Epic Systems makes the dominant electronic health record (EHR) system in America; if you're a doctor, chances are you are required to use it, and for every hour a doctor spends with a patient, they have to spend two hours doing clinically useless bureaucratic data-entry on an Epic EHR.
How could a product so manifestly unfit for purpose be the absolute market leader? Simple: as Robert Kuttner describes in an excellent feature in The American Prospect, Epic may be a clinical disaster, but it's a profit-generating miracle:
https://prospect.org/health/2024-10-01-epic-dystopia/
At the core of Epic's value proposition is "upcoding," a form of billing fraud that is beloved of hospital administrators, including the "nonprofit" hospitals that generate vast fortunes that are somehow not characterized as profits. Here's a particularly egregious form of upcoding: back in 2020, the Poudre Valley Hospital in Ft Collins, CO locked all its doors except the ER entrance. Every patient entering the hospital, including those receiving absolutely routine care, was therefore processed as an "emergency."
In April 2020, Caitlin Wells Salerno – a pregnant biologist – drove to Poudre Valley with normal labor pains. She walked herself up to obstetrics, declining the offer of a wheelchair, stopping only to snap a cheeky selfie. Nevertheless, the hospital recorded her normal, uncomplicated birth as a Level 5 emergency – comparable to a major heart-attack – and whacked her with a $2755 bill for emergency care:
https://pluralistic.net/2021/10/27/crossing-a-line/#zero-fucks-given
Upcoding has its origins in the Reagan revolution, when the market-worshipping cultists he'd put in charge of health care created the "Prospective Payment System," which paid a lump sum for care. The idea was to incentivize hospitals to provide efficient care, since they could keep the difference between whatever they spent getting you better and the set PPS amount that Medicare would reimburse them. Hospitals responded by inventing upcoding: a patient with controlled, long-term coronary disease who showed up with a broken leg would get coded for the coronary condition and the cast, and the hospital would pocket both lump sums:
https://pluralistic.net/2024/06/13/a-punch-in-the-guts/#hayek-pilled
The reason hospital administrators love Epic, and pay gigantic sums for systemwide software licenses, is directly connected to the two hours that doctors spent filling in Epic forms for every hour they spend treating patients. Epic collects all that extra information in order to identify potential sources of plausible upcodes, which allows hospitals to bill patients, insurers, and Medicare through the nose for routine care. Epic can automatically recode "diabetes with no complications" from a Hierarchical Condition Category code 19 (worth $894.40) as "diabetes with kidney failure," code 18 and 136, which gooses the reimbursement to $1273.60.
Epic snitches on doctors to their bosses, giving them a dashboard to track doctors' compliance with upcoding suggestions. One of Kuttner's doctor sources says her supervisor contacts her with questions like, "That appointment was a 2. Don’t you think it might be a 3?"
Robert Kuttner is the perfect journalist to unravel the Epic scam. As a journalist who wrote for The New England Journal of Medicine, he's got an insider's knowledge of the health industry, and plenty of sources among health professionals. As he tells it, Epic is a cultlike, insular company that employs 12.500 people in its hometown of Verona, WI.
The EHR industry's origins start with a GW Bush-era law called the HITECH Act, which was later folded into Obama's Recovery Act in 2009. Obama provided $27b to hospitals that installed EHR systems. These systems had to more than track patient outcomes – they also provided the data for pay-for-performance incentives. EHRs were already trying to do something very complicated – track health outcomes – but now they were also meant to underpin a cockamamie "incentives" program that was supposed to provide a carrot to the health industry so it would stop killing people and ripping off Medicare. EHRs devolved into obscenely complex spaghetti systems that doctors and nurses loathed on sight.
But there was one group that loved EHRs: hospital administrators and the private companies offering Medicare Advantage plans (which also benefited from upcoding patients in order to soak Uncle Sucker):
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8649706/
The spread of EHRs neatly tracks with a spike in upcharging: "from 2014 through 2019, the number of hospital stays billed at the highest severity level increased almost 20 percent…the number of stays billed at each of the other severity levels decreased":
https://oig.hhs.gov/oei/reports/OEI-02-18-00380.pdf
The purpose of a system is what it does. Epic's industry-dominating EHR is great at price-gouging, but it sucks as a clinical tool – it takes 18 keystrokes just to enter a prescription:
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2729481
Doctors need to see patients, but their bosses demand that they satisfy Epic's endless red tape. Doctors now routinely stay late after work and show up hours early, just to do paperwork. It's not enough. According to another one of Kuttner's sources, doctors routinely copy-and-paste earlier entries into the current one, a practice that generates rampant errors. Some just make up random numbers to fulfill Epic's nonsensical requirements: the same source told Kuttner that when prompted to enter a pain score for his TB patients, he just enters "zero."
Don't worry, Epic has a solution: AI. They've rolled out an "ambient listening" tool that attempts to transcribe everything the doctor and patient say during an exam and then bash it into a visit report. Not only is this prone to the customary mistakes that make AI unsuited to high-stakes, error-sensitive applications, it also represents a profound misunderstanding of the purpose of clinical notes.
The very exercise of organizing your thoughts and reflections about an event – such as a medical exam – into a coherent report makes you apply rigor and perspective to events that otherwise arrive as a series of fleeting impressions and reactions. That's why blogging is such an effective practice:
https://pluralistic.net/2021/05/09/the-memex-method/
The answer to doctors not having time to reflect and organize good notes is to give them more time – not more AI. As another doctor told Kuttner: "Ambient listening is a solution to a self-created problem of requiring too much data entry by clinicians."
EHRs are one of those especially hellish public-private partnerships. Health care doctrine from Reagan to Obama insisted that the system just needed to be exposed to market forces and incentives. EHRs are designed to allow hospitals to win as many of these incentives as possible. Epic's clinical care modules do this by bombarding doctors with low-quality diagnostic suggestions with "little to do with a patient’s actual condition and risks," leading to "alert fatigue," so doctors miss the important alerts in the storm of nonsense elbow-jostling:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5058605/
Clinicians who actually want to improve the quality of care in their facilities end up recording data manually and keying it into spreadsheets, because they can't get Epic to give them the data they need. Meanwhile, an army of high-priced consultants stand ready to give clinicians advise on getting Epic to do what they need, but can't seem to deliver.
Ironically, one of the benefits that Epic touts is its interoperability: hospitals that buy Epic systems can interconnect those with other Epic systems, and there's a large ecosystem of aftermarket add-ons that work with Epic. But Epic is a product, not a protocol, so its much-touted interop exists entirely on its terms, and at its sufferance. If Epic chooses, a doctor using its products can send files to a doctor using a rival product. But Epic can also veto that activity – and its veto extends to deciding whether a hospital can export their patient records to a competing service and get off Epic altogether.
One major selling point for Epic is its capacity to export "anonymized" data for medical research. Very large patient data-sets like Epic's are reasonably believed to contain many potential medical insights, so medical researchers are very excited at the prospect of interrogating that data.
But Epic's approach – anonymizing files containing the most sensitive information imaginable, about millions of people, and then releasing them to third parties – is a nightmare. "De-identified" data-sets are notoriously vulnerable to "re-identification" and the threat of re-identification only increases every time there's another release or breach, which can used to reveal the identities of people in anonymized records. For example, if you have a database of all the prescribing at a given hospital – a numeric identifier representing the patient, and the time and date when they saw a doctor and got a scrip. At any time in the future, a big location-data breach – say, from Uber or a transit system – can show you which people went back and forth to the hospital at the times that line up with those doctor's appointments, unmasking the person who got abortion meds, cancer meds, psychiatric meds or other sensitive prescriptions.
The fact that anonymized data can – will! – be re-identified doesn't mean we have to give up on the prospect of gleaning insight from medical records. In the UK, the eminent doctor Ben Goldacre and colleagues built an incredible effective, privacy-preserving "trusted research environment" (TRE) to operate on millions of NHS records across a decentralized system of hospitals and trusts without ever moving the data off their own servers:
https://pluralistic.net/2024/03/08/the-fire-of-orodruin/#are-we-the-baddies
The TRE is an open source, transparent server that accepts complex research questions in the form of database queries. These queries are posted to a public server for peer-review and revision, and when they're ready, the TRE sends them to each of the databases where the records are held. Those databases transmit responses to the TRE, which then publishes them. This has been unimaginably successful: the prototype of the TRE launched during the lockdown generated sixty papers in Nature in a matter of months.
Monopolies are inefficient, and Epic's outmoded and dangerous approach to research, along with the roadblocks it puts in the way of clinical excellence, epitomizes the problems with monopoly. America's health care industry is a dumpster fire from top to bottom – from Medicare Advantage to hospital cartels – and allowing Epic to dominate the EHR market has somehow, incredibly, made that system even worse.
Naturally, Kuttner finishes out his article with some antitrust analysis, sketching out how the Sherman Act could be brought to bear on Epic. Something has to be done. Epic's software is one of the many reasons that MDs are leaving the medical profession in droves.
Epic epitomizes the long-standing class war between doctors who want to take care of their patients and hospital executives who want to make a buck off of those patients.

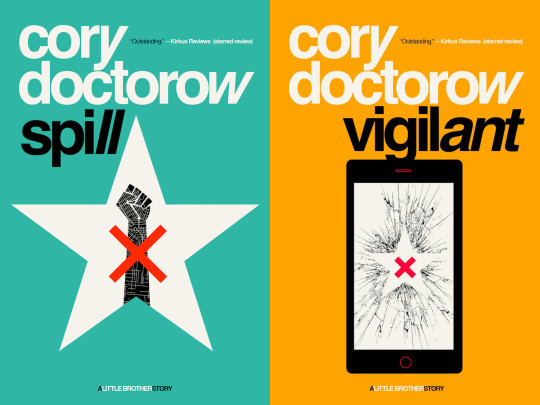
Tor Books as just published two new, free LITTLE BROTHER stories: VIGILANT, about creepy surveillance in distance education; and SPILL, about oil pipelines and indigenous landback.

If you'd like an essay-formatted version of this post to read or share, here's a link to it on pluralistic.net, my surveillance-free, ad-free, tracker-free blog:
https://pluralistic.net/2024/10/02/upcoded-to-death/#thanks-obama

Image: Flying Logos (modified) https://commons.wikimedia.org/wiki/File:Over_$1,000,000_dollars_in_USD_$100_bill_stacks.png
CC BY-SA 4.0 https://creativecommons.org/licenses/by-sa/4.0/deed.en
#pluralistic#ehrs#robert kuttner#tres#trusted research environments#ben goldacre#epic#epic systems#interoperability#privacy#reidentification#deidentification#thanks obama#upcoding#Hierarchical Condition Category#medicare#medicaid#ai#American Recovery and Reinvestment Act#HITECH act#medicare advantage#ambient listening#alert fatigue#monopoly#antitrust
819 notes
·
View notes
Text







Drottning
#lmn#mnh#hjrs#mhrssa#lhjrsses#lhrserlve#mnhnn#lhnn#hnn#ehnn#ahnn#ljnn#arnleronenne#ahl#ehnnemnolen#lhnners#lnn#inn#ann#äåäåäåäåäåäå#enn#ohnn#ehrs
0 notes
Text
2025 Staff Augmentation Trends: EHRS Insights on Bridging Skill Gaps
Explore Exela HR Solutions’ expert take on 2025 staff augmentation trends. Learn how EHRS addresses skill gaps with emerging workforce strategies for business success.
#StaffAugmentation#StaffAugmentationTrends#ITStaffingServices#2025WorkforceSolutions#ExelaHRSolutions#SkillGapManagement#StaffAugmentation Strategies#TemporaryStaffing#StaffAugmentationServices#ITStaffAugmentation#StaffAugmentationSolutions#hr#hrsolutions#hrservices#humanresources#hroutsourcing#hro#ehrs
0 notes
Text
📋✨ Say goodbye to disorganized patient data! Electronic Health Records (EHRs) are here to revolutionize healthcare with seamless coordinated care in multi-clinic systems. From real-time updates to centralized data sharing, EHRs ensure better outcomes for both patients and providers.
Read More - tinyurl.com/28x3rkpc
#ElectronicHealthRecords(EHRs)#Coordinatedcare#multi-clinicsystems#ElectronicHealthRecords#EHR#EHRS#ClinicmanagementsolutioninLaravel#ClinicmanagementappwithLaravelbackend#DoctorclinicmanagementFlutterapp
0 notes
Text
The Evolution of AI in Healthcare: Current Trends and Legal Considerations
Artificial intelligence (AI) is transforming the healthcare landscape, offering innovative solutions to age-old challenges. From diagnostics to enhanced patient care, AI’s influence is pervasive, and seems destined to reshape how healthcare is delivered and managed. However, the rapid integration of AI technologies brings with it a complex web of legal and regulatory considerations that…
#AI#Artificial Intelligence#cancer#COVID-19#Drug Discovery#EHRs#Electronic Health Records#electronic medical records#Health Insurance Portability and Accountability Act#healthcare#heart disease#HIPAA#medications#neurological disorders#Office of Professional Medical Conduct#OPMC#Patient Care#patient information#pharmaceutical#physicians
0 notes
Text
The Promise of Digital Twin Technology in Personalized Healthcare
Healthcare is the fastest and most highly evolving sector in today’s world, along with the birth of different technologies that are playing a vital role in the medical field in terms of solving new problems uniquely and helping professionals provide effective treatments. Digital twin technology is used in many fields and healthcare is one of its applications. DT is one among healthcare technologies and is an innovative approach that uses digital replicas of physical entities to predict various health-related issues. This has become a promising tool that can be used in transforming personalized healthcare. In this article, let us discuss in detail this technology and its prominent role in finding solutions to various health-related problems that are improving patient care.

Defining Digital Twin Technology
Digital twin technology is the process of creating or making virtual models that are replicas of real entities like human organs, systems, physiological acts, or even the entire organism. These virtual models can be used later for simulation, and analysis, and hence we can learn or understand the behavior of an individual in different conditions. This helps medical professionals or specialists to study the particular person in detail which in turn can be more effective and accurate in the diagnosis process.
A DT on creating a virtual model can used to conduct surgeries and oversee the effects virtually that might occur on undergoing the real surgery on the patient’s body. This will help in preventing future harm and suffering from pain. All the virtual replicas are updated regularly with data from different sources like wearable health devices, genetic information, and electronic health records (EHRs) for maintaining accuracy. Thus, by integrating all this information doctors and find valuable insights into a patient’s health conditions and hence can provide personalized diagnoses.
Digital Twin Technology working in healthcare
Digital twin technology mainly works by data integration from different healthcare resources. But it is done in three steps which include the creation of a blueprint, the construction of the first digital twin model, and the third is enhancing its capacity. The data that is integrated will contain the important elements of the patient like medical history, lifestyle, genetic makeup, physical behavior, and emotional factors. All these can be gathered using sensors or wearable medical devices.
Later these digital twins are analyzed using advanced machine learning techniques that can identify and provide meaning or informative patterns, and prediction of future outcomes, and will also give suggestions that can be adopted in personalized treatment plans.
Benefits of Digital Twin Technology
A DT technology can be used as the predicting analysis that showcases the results of your diagnosis without actually doing it on the human body. The process of regular and continuous monitoring of the updated real-time data through virtual twins doctors can detect the symptoms at the early stage and is an alert for professionals so that they can take precautionary measures for patients. With his proactive approach, many diseases can be prevented well before.
It is also a very useful approach to monitoring patients remotely as one need not visit physically to provide or get their health updates. This benefits chronic patients as it gives access to continous support and care by healthcare providers. The major use is to provide personalized care and precision medicines based on the individual’s unique character and genomic factor. Along with this analysis of various scenarios, one can get optimization in treatment depending on the outcome effects with this, doctors can adopt effective and better treatment strategies. Apart from all these DT is a powerful tool for learning drug effects, disease symptoms, and research areas for conducting clinical trials.
Conclusion
To conclude, along with its benefits in various areas of healthcare, certain challenges need to be encountered. The major difficulty is data privacy and security which comes with the major concern of misusing personal and detailed information of the patient. Accuracy may be also an issue as in some cases predictions may go wrong and may cause severe effects. With careful planning and implementation, digital twin technology has the potential to improve patient outcomes and transform the future of healthcare.
Visit More : https://thehealthcareinsights.com/the-promise-of-digital-twin-technology-in-personalized-healthcare/
0 notes
Text
Scrubs and Stadiums
This month’s episode of “News You Can Use” on HealthcareNOWRadio features news from the month of February 2024 News You Can Use with your Hosts Dr Craig Joseph and Dr Nick van Terheyden The show that gives you a quick insight into the latest news, twists, turns and debacles going on in healthcare withmy friend and co-host Craig Joseph, MD (@CraigJoseph) Chief Medical Officer at Nordic Consulting…

View On WordPress
#AI#Ask Me Anything#Bigdata#Blockchain#ChatBots#connectedhealth#Cybersecurity#Digital Health#DigitalHealth#disruption#education#ehealth#ehrs#EMR#fraud#FutureofHealthcare#futurism#HCIT#Healthcare#Healthcare Reform#healthcarecosts#healthdata#HealthIT#healthtech#HIT#hospitals#Incremental#Incremental Healthcare#IncrementalHealth#Innovation
1 note
·
View note
Text
Role of standardized RPO in reshaping manufacturing hiring

Explore the game-changing impact of RPO and its standardized approach to manufacturing hiring. Learn how this strategic shift enhances efficiency & consistency.
#RecruitmentProcessOutsourcing#RPOProviders#HiringProcess#HRServices#ExelaHRSolutions#RecruitmentProcessinManufacturing#RPO#RecruitmentProcessing#HumanResourcesServices#Recruitment#HRSolutions#RPOinManufacturing#EHRS#hroutsourcing#hr#hro#humanresources
0 notes
Text
The Importance of User-Centered Design in Healthcare Product Specifications
Any product's success depends on it being designed to satisfy users' requirements and expectations; this is especially true in the healthcare sector. The demands, preferences, and experiences of users are given top priority during the design process thanks to the design concept known as user-centered (UCD). UCD is crucial in the healthcare industry to guarantee that goods and services satisfy the requirements of patients, carers, and medical professionals.
This essay examines the value of user-centered design in the context of healthcare product specifications. It will go over the advantages of UCD, the difficulties in putting it into practice, and the best methods for creating products from a user-centered perspective.
Benefits of User-Centered Design in Healthcare Product Specifications
Improved patient outcomes
With the development of safe, efficient, and simple-to-use devices, user-centered design can enhance patient outcomes. This may lead to improved patient safety and health outcomes.
Increased patient satisfaction
By developing goods that are catered to their wants and preferences, UCD can raise patient satisfaction. More patient engagement and a better patient experience may result from this.
Reduced risk of errors and adverse events
Usability-centered design (UCD) can lower the possibility of mistakes and unfavourable incidents, which could have detrimental effects on patient safety.
Increased efficiency and productivity
UCD can boost productivity and efficiency by developing products that are simple to use and require little training. Healthcare workers may benefit from time savings and increased production as a result.
Increased adoption and usage
By improving a product's usability and user appeal, UCD can improve adoption and usage. More patient participation and greater health outcomes may arise from this.
Challenges of Implementing User-Centered Design in Healthcare Product Specifications
Budget constraints
By improving a product's usability and user appeal, UCD can improve adoption and usage. More patient participation and greater health outcomes may arise from this. UCD implementation may necessitate the use of extra resources, such as those needed for conducting research, employing specialists, and creating prototypes, which could raise the entire cost of product development.
Time constraints
It might be difficult to develop products quickly in a fast-paced healthcare environment because the UCD process can be time-consuming.
Resistance to change
Stakeholders, including healthcare practitioners, who could feel at ease with conventional procedures and be reluctant to adopt new technologies, can be resistant to change.
Lack of user engagement
It might be difficult to involve users in the design process, especially if they are busy healthcare professionals or patients with serious health problems.
Technical limitations
The capacity to integrate UCD in product development may be constrained by technical issues like the product's complexity or the requirement for regulatory compliance.
Best Practices for Designing Products with a User-Centered Approach
Conduct user research
It's crucial to perform research to comprehend the demands, expectations, behaviours, and preferences of the target market before producing a product. Interviews, surveys, and observational studies may all be a part of this research.
Involve users in the design process
To make sure the product is satisfying their needs, user input should be ongoing throughout the design process. Consumers can test the product, test prototypes, and participate in design decisions.
Use iterative design processes
The product should be continuously improved by designers using an iterative method based on customer feedback. With this strategy, the product may be improved gradually while also guaranteeing that consumer needs are being met.
Consider the entire user experience
The complete user experience, including the pre-and post-use experiences, must be taken into account in a user-centered approach. The context in which the product will be used, the feelings evoked by the experience, and the effect on the user's life should all be taken into account throughout product design.
Test and evaluate products with real users
To make sure that the product satisfies their requirements and expectations, real users must test it. Both before and after the product is released, this testing ought to take place. Usability tests, cognitive walkthroughs, and user satisfaction surveys are all examples of testing methods.
Case Study: Examples of User-Centered Design in Healthcare Product Specifications
Patient portals
Patient portals are online resources that let patients manage their healthcare requirements, receive health information, and get in touch with medical professionals. Patients should have a seamless and intuitive user experience when using patient portals, which include clear and simple-to-understand information, secure communication channels, and personalised features.
Medical devices
Patients regularly use medical equipment like glucose meters, pacemakers, and insulin pumps. For medical equipment to be safe and simple to use for patients, a user-centered design is essential. For instance, to make sure that the devices suit patients' demands, medical device designers employ several techniques to involve patients in the design process, such as focus groups, interviews, and usability testing.
Electronic health records (EHRs)
EHRs are digitised patient health records that healthcare professionals can access. The user interface of EHRs is made to be welcoming and simple to use by using a user-centered design approach. To enhance the user experience, EHRs also include features like individualised patient profiles, tailored data visualisations, and simple search capabilities.
Telemedicine platforms
Platforms for telemedicine enable remote communication between patients and medical professionals. For telemedicine platforms, a user-centered design approach takes user demands into account, taking into account things like simplicity of use, privacy, and security to make the remote care experience for patients as easy and comfortable as possible. Patients can easily access and use services like real-time video chat, secure messaging, and scheduling choices on telemedicine systems, for instance.
Executive Programme in Healthcare Entrepreneurship and Management
The Indian Institute of Technology (IIT) Delhi offers Executive Program in Healthcare Entrepreneurship and Management. The curriculum is made for managers, entrepreneurs, and healthcare professionals who want to improve their entrepreneurship and management abilities.
Healthcare management teaches all the essential practises that need to be understood and followed strictly. The entire program doesn’t take much of your time and makes you eligible for a handsome salary placement. Get yourself enroll in this program and get ready for a new career beginning.
Conclusion
To create healthcare solutions that satisfy the needs of patients, carers, and healthcare professionals, user-centered design (UCD) is essential. UCD makes ensuring that products are reliable, efficient, and simple to use, which enhances patient outcomes, boosts satisfaction, and lowers the possibility of mistakes. Using UCD may provide difficulties, but combining best practises like user research and iterative design methods can assist resolve these difficulties.
UCD is a crucial element of healthcare product design by employing case studies such as patient portals, medical devices, electronic health records (EHRs), and telemedicine platforms. In the end, it takes a user-centered approach to healthcare product design to give consumers high-quality care and enhance their general health results.
0 notes
Text

YOU KNOW S3RK3T TH3Y R34LLY L1K3 YOU AROUND H3R3
YOU SHOULD V1S1T SOM3T1M3, YOUD G3T 4 K1CK OUT OF 1T
4NYW4Y
S33 YOU 4ROUND, 1 GU3SS
#I FORGOT TO POST THIS ONE#I DONT like it that much but I am proud of the Vriska stained glass#I think about their god status on Earth-C a lot#That’s gotta be a crazy thing for them to live with#Vriska is this ancient lost thing#The god that died at the genesis of the world#Or however the mythology’s bloomed over millenia#And Terezi just saw her the other week#She can’t really be gone can she?#She’s coming home? Right? She was just ehre#DO NOT TALK ABOUT BEYOND CANON I dont have anything against it#I am just not familiar#This is not meant to be about beyond canon#It’s just terezi doomed yuri hours#homestuck#homestuck fanart#vriska serket#terezi pyrope#vriska x terezi#vrisrezi#earth-c#Homestuck earth-c#art#digital art#procreate#doodles#HAVE YOU EEEEVERRR STARED DIRECTLY AT THE SUUUUUNNN#HAVE YOU EVER SHARED A CLOSENESS SO EXPOSED AND HAD IT SPIT BACK BY SOMEONE#SO FORGIVE ME IF I JUMP#AT THE RATTLE OF YOUR KEYS
1K notes
·
View notes
Text

They live in my head rent free. Drop your headcanons in the reblogg tags
#uni au where they go to every party and fucking trash it#headcanon that gojo only drinks coke cause one sip and 30 minutes he's lying somewhere striped naked and unconcious#stst bribing shoko into any shinanegan by buying her cigs#shoko drinks them both under the table but suguru actually can keep up with ehr#also weed does weird things to gojo's six eyes 100% confirmed so he is catious#still the loudes mf at the party even if he's sober af#i love them#these three are the best thing that ever happened to me#sashisu#satosho#sugusho#satosugu#stsg#gojo satoru#shoko ieiri#suguru geto#jujutsu kaisen#fanart#satosho weekend#satoshoko#jjk#IPMSSA_Tokyo5!Fanart#IPMSSA_FoundFamily!Fanart#IPMSSA_SaShiSu!Fanart
16K notes
·
View notes
Text

happy christmas or merry holidays <3
i threw symbolism on this thing like glitter on a school diorama.
#uh if u get all of them#ill uhhhh i dunno draw u a joel or smth for funsies >:)#joel smallishbeans#hermitcraft#hermitblr#trafficblr#life series#life smp#wlsmp#wild life smp#i thought all the symbolism talk about joel was the coolest#and since im resident joel nerd i thought id make my own spin on it#if u uh wanna know more send me an ask or smth :)#i dunno if anyone will read the ramblings of a crzed jeremy if i put it on ehre lol#smallishbeans#Hmm nvm I'll drop a couple things in here lol#mars and the moon symbolise a war a clash between emotions and logic#if they are aligned well#it can mean nurturing#but if they are not it can mean aggressiveness and impulsivity and rage. which is very much joel to me. theres a bit of a fire on the mars#theyre being used to drive the chariot. they are still very much fierce#but instead of the lone wolfy ness they're now the loyal best friends type lol.
1K notes
·
View notes
Text
Optimize Operations with Exela HR Solutions for Business Process Services
Discover how Exela HR Solutions streamlines workforce management for Business Process Services. From payroll to compliance, boost efficiency and productivity with EHRS expertise.

#HRSolutionsforBusinessProcessServices#PayrollServicesforHealthcare#HRServicesforHealthcareIndustry#HRSolutions#ExelaHRSolutions#BusinessProcessServices#BPS#BPSEfficiency#HROutsourcingforHealthcare#HRServicesforHealthcare#EHRS
0 notes
Text
Nursing and Technology
Nursing technology has been rapidly advancing over the years, revolutionizing the way nurses provide care to patients. These technologies have greatly improved patient outcomes, reduced medical errors, and increased efficiency in healthcare delivery. Now we will explore some of the newest nursing technologies that are changing the way nurses provide care to patients. With everything, there are…

View On WordPress
#Critical thinking#decision-making#EHRs#Electronic health record#health apps#healthcare providers#Hospital#Nursing#patient outcomes#perceptions#quality of care#registered nurses#Robotics#Technology in healthcare#Telemedicine
0 notes
Text
there is just something about regulus going into absolute shock after harry comes crying to him about breaking something or spilling a glass over and regulus having calmed him down, reassured him and helping him clean up and then staring into space realising maybe he was never his mother's child after all
#anyways im back from the dead#ive offically left school#college ehre i come tf#marauders au#marauders era#the marauders#marauders#harry potter#regulus black#james potter#jegulus
2K notes
·
View notes
Text

just one bite??? 🍎🍬
#WELCOME BACK MAFUEMU. GYAAAHAHSISHAIAHAUAHAHHA#project sekai#mafuemu#pjsk#prsk#emu otori#mafuyu asahina#proseka#emumafu#colorful stage#I SNILED SO SNEETLY MY MAFUEMU MIXED EVENT ITS HEEEERE ITS HEREEEEREERRRE ITS BEEN 80 YEARS.#I LOVEEE EMUS CARD AND HER STUPID LITTLE OUTFIT SHES SO CUTIEPIEEEE#did my best on ehr iutfit from the outfit preview videos the pjsekai jp account pists. i am not downloading jp again.#just the one prison is enough thankyou.#sorry its mikus birthday and im hitting the yuri but in my defence it's what she would want
978 notes
·
View notes