#Clostridioides difficile Research and Development
Explore tagged Tumblr posts
Text




‘Fragile Microbiomes’ by bio-artist Anna Dumitriu
1. SYPHILIS DRESS- This dress is embroidered with images of the corkscrew-shaped bacterium which causes the sexually transmitted disease syphilis. These embroideries are impregnated with the sterilised DNA of the Nichols strain of the bacterium - Treponema pallidum subsp. pallidum - which Dumitriu extracted with her collaborators.
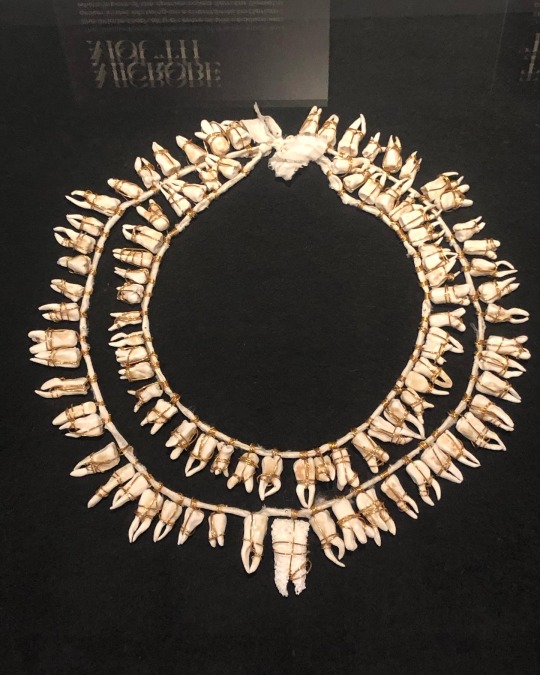
2. MICROBE MOUTH- The tooth at the centre of this necklace was grown in the lab using an extremophile bacterium which is part of the species called Serratia (Serratia N14) that can produce hydroxyapatite, the same substance that tooth enamel is made from.
The handmade porcelain teeth that make up this necklace have been coated with glazes derived from various bacterial species that live in our mouths and cause tooth decay and gum disease, including Porphyromonas gingivalis, which can introduce an iron-containing light brown stain to the glaze.
3. TEETH MARKS: THE MOST PROFOUND MYSTERY- In his 1845 essay “On Artificial Teeth”, W.H. Mortimer described false teeth as “the most profound mystery” because they were never discussed. Instead, people would hide the stigma of bad teeth and foul breath using fans.
This altered antique fan is made from animal bone and has been mended with gold wire, both materials historically used to construct false teeth (which would also sometimes incorporate human teeth). The silk of the fan and ribbon has been grown and patterned with two species of oral pathogens: Prevotella intermedia and Porphyromonas gingivalis. These bacteria cause gum disease and bad breath, and the latter has also recently been linked to Alzheimer’s disease.
4. PLAGUE DRESS- This 1665-style 'Plague Dress' is made from raw silk, hand-dyed with walnut husks in reference to the famous herbalist of the era Nicholas Culpeper, who recommended walnuts as a treatment for plague. It has been appliquéd with original 17th-century embroideries, impregnated with the DNA of Yersinia pestis bacteria (plague). The artist extracted this from killed bacteria in the laboratory of the National Collection of Type Cultures at the UK Health Security Agency.
The dress is stuffed and surrounded by lavender, which people carried during the Great Plague of London to cover the stench of infection and to prevent the disease, which was believed to be caused by 'bad air' or 'miasmas'. The silk of the dress references the Silk Road, a key vector for the spread of plague.
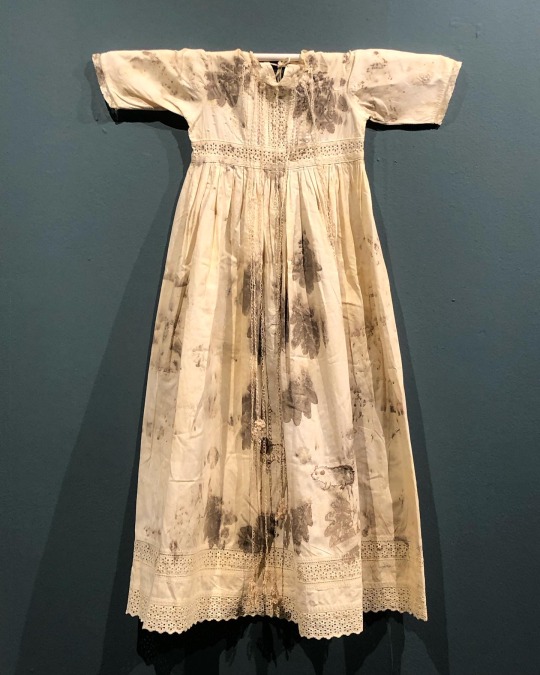
5. BACTERIAL BAPTISM- based on a vintage christening gown which has been altered by the artist to tell the story of research into how the microbiomes of babies develop, with a focus on the bacterium Clostridioides difficile, originally discovered by Hall and O’Toole in 1935 and presented in their paper “Intestinal flora in new-born infants”. It was named Bacillus difficilis because it was difficult to grow, and in the 1970s it was recognised as causing conditions from mild antibiotic-associated diarrhoea to life-threatening intestinal inflammation. The embroidery silk is dyed using stains used in the study of the gut microbiome and the gown is decorated with hand-crocheted linen lace grown in lab with (sterilised) C. difficile biofilms. The piece also considers how new-borns become colonised by bacteria during birth in what has been described as ‘bacterial baptism’.
6. ZENEXTON- Around 1570, Swiss physician and alchemist Theophrastus Paracelsus coined the term ‘Zenexton’, meaning an amulet worn around the neck to protect from the plague. Until then, amulets had a more general purpose of warding off (unspecified) disease, rather like the difference today between ‘broad spectrum’ antibiotics and antibiotics informed by genomics approaches which target a specific organism.
Over the next century, several ideas were put forward as to what this amulet might contain: a paste made of powdered toads, sapphires that would turn black when they leeched the pestilence from the body, or menstrual blood. Bizarre improvements were later made: “of course, the toad should be finely powdered”; “the menstrual blood from a virgin”; “collected on a full moon”.
This very modern Zenexton has been 3D printed and offers the wearer something that genuinely protects: the recently developed vaccine against Yersinia pestis, the bacterium that causes plague.
#my favourite pieces from this exhibition that I visited last month at the Thackray medical museum in Leeds#absolutely fascinating reading about the process and meanings behind these works#mine#anna dumitriu#works
2K notes
·
View notes
Text
Researchers have developed a new antibiotic that reduced or eliminated drug-resistant bacterial infections in mouse models of acute pneumonia and sepsis while sparing healthy microbes in the mouse gut. The drug, called lolamicin, also warded off secondary infections with Clostridioides difficile, a common and dangerous hospital-associated bacterial infection, and was effective against more than 130 multidrug-resistant bacterial strains in cell culture. The findings are detailed in the journal Nature. "People are starting to realize that the antibiotics we've all been taking—that are fighting infection and, in some instances, saving our lives—also are having these deleterious effects on us," said University of Illinois Urbana-Champaign chemistry professor Paul Hergenrother, who led the study with former doctoral student Kristen Muñoz.
Continue Reading.
204 notes
·
View notes
Text
New antibiotic kills pathogenic bacteria, spares healthy gut microbes
Article Date: May 29, 2024
Article Blurb:
Researchers have developed a new antibiotic that reduced or eliminated drug-resistant bacterial infections in mouse models of acute pneumonia and sepsis while sparing healthy microbes in the mouse gut. The drug, called lolamicin, also warded off secondary infections with Clostridioides difficile, a common and dangerous hospital-associated bacterial infection, and was effective against more than 130 multidrug-resistant bacterial strains in cell culture.
[...]
Numerous studies have found that antibiotic-related disturbances to the gut microbiome increase vulnerability to further infections and are associated with gastrointestinal, kidney, liver and other problems.
[...] In a series of experiments, Muñoz designed structural variations of the Lol inhibitors and evaluated their potential to fight gram-negative and gram-positive bacteria in cell culture. One of the new compounds, lolamicin, selectively targeted some “laboratory strains of gram-negative pathogens including Escherichia coli, Klebsiella pneumoniae and Enterobacter cloacae,” the researchers found. Lolamicin had no detectable effect on gram-positive bacteria in cell culture. At higher doses, lolamicin killed up to 90% of multidrug-resistant E. coli, K. pneumoniae and E. cloacae clinical isolates.
When given orally to mice with drug-resistant septicemia or pneumonia, lolamicin rescued 100% of the mice with septicemia and 70% of the mice with pneumonia, the team reported.
Extensive work was done to determine the effect of lolamicin on the gut microbiome.
“The mouse microbiome is a good tool for modeling human infections because human and mouse gut microbiomes are very similar,” Muñoz said. “Studies have shown that antibiotics that cause gut dysbiosis in mice have a similar effect in humans.”
Treatment with standard antibiotics amoxicillin and clindamycin caused dramatic shifts in the overall structure of bacterial populations in the mouse gut, diminishing the abundance several beneficial microbial groups, the team found.
“In contrast, lolamicin did not cause any drastic changes in taxonomic composition over the course of the three-day treatment or the following 28-day recovery,” the researchers wrote.
Many more years of research are needed to extend the findings, Hergenrother said.
[More in Article]
Note: The main scientific journal itself is paywalled (and not yet available in unpaywall nor sci-hub), Nature Journal Link
14 notes
·
View notes
Text
Innovative Approaches to Irritable Bowel Syndrome Treatment

Irritable Bowel Syndrome (IBS) affects millions of people worldwide, and finding the right treatment can be challenging. As research continues to evolve, innovative approaches to irritable bowel syndrome treatment are emerging, offering hope to those who struggle with the condition. These new treatments go beyond traditional methods, focusing on targeting the underlying causes of IBS and improving overall gut health.
Understanding IBS and Its Challenges
Irritable Bowel Syndrome (IBS) is a functional gastrointestinal disorder characterized by chronic abdominal pain, bloating, and altered bowel habits. The exact cause of IBS is not well understood, but it is believed to result from a combination of factors, including genetics, gut microbiome imbalances, and psychological stress.
Traditional treatments for IBS often involve dietary changes, medications, and lifestyle modifications. However, these treatments do not work for everyone, leading to a growing demand for more effective and personalized approaches.
Emerging Treatments for Irritable Bowel Syndrome
Recent advancements in medical research have led to the development of several innovative treatment options for IBS. These treatments aim to address the root causes of the disorder, offering a more targeted approach to managing symptoms.
1. Microbiome Modulation
The gut microbiome plays a crucial role in digestive health, and imbalances in gut bacteria have been linked to IBS. Recent studies have shown that altering the composition of the gut microbiome can improve IBS symptoms. Microbiome modulation involves using probiotics, prebiotics, and even fecal microbiota transplantation (FMT) to restore a healthy balance of gut bacteria.
Probiotics and Prebiotics: Probiotics are live bacteria that can help restore gut health, while prebiotics are non-digestible fibers that promote the growth of beneficial bacteria. Specific strains of probiotics, such as Bifidobacterium infantis, have shown promise in reducing IBS symptoms.
Fecal Microbiota Transplantation (FMT): FMT involves transferring stool from a healthy donor to an IBS patient to restore a balanced microbiome. Although still in the experimental stages for IBS, FMT has shown success in treating other gut conditions like Clostridioides difficile infection.
2. Psychological Therapies
The gut-brain axis, the communication network between the gut and the brain, plays a significant role in IBS. Psychological therapies, such as cognitive-behavioral therapy (CBT) and gut-directed hypnotherapy, have been shown to be effective in managing IBS symptoms by addressing the psychological aspects of the disorder.
Cognitive-Behavioral Therapy (CBT): CBT helps patients identify and change negative thought patterns and behaviors that can exacerbate IBS symptoms. Studies have shown that CBT can reduce IBS symptoms and improve quality of life.
Gut-Directed Hypnotherapy: This therapy involves using hypnosis to achieve a state of focused relaxation, which can help reduce gut sensitivity and improve IBS symptoms. Gut-directed hypnotherapy has been found to be effective for some patients with refractory IBS.
3. Neuromodulation Techniques
Neuromodulation techniques, such as transcutaneous electrical nerve stimulation (TENS) and sacral nerve stimulation (SNS), are emerging as potential treatments for IBS. These techniques involve stimulating specific nerves to regulate gut function and reduce pain.
Transcutaneous Electrical Nerve Stimulation (TENS): TENS involves applying a mild electrical current to the skin overlying the abdominal nerves. It has been found to reduce abdominal pain in IBS patients.
Sacral Nerve Stimulation (SNS): SNS involves implanting a device that sends electrical impulses to the sacral nerves, which control bowel function. While more research is needed, SNS has shown promise in treating IBS-related symptoms.
4. Pharmacological Innovations

New medications are being developed to target specific pathways involved in IBS, offering more targeted and effective treatment options. These include drugs that modulate gut motility, reduce visceral hypersensitivity, and target the gut-brain axis.
Eluxadoline: This medication is a mixed opioid receptor modulator that helps manage diarrhea-predominant IBS (IBS-D). It works by reducing bowel contractions and slowing down the movement of stool.
Rifaximin: An antibiotic that is minimally absorbed into the bloodstream, Rifaximin targets the gut microbiome and has been found to reduce bloating and diarrhea in IBS patients.
FAQs
What are the benefits of using probiotics for IBS? Probiotics can help restore the balance of gut bacteria, potentially reducing symptoms like bloating, gas, and diarrhea.
Is Fecal Microbiota Transplantation (FMT) safe for IBS patients?While FMT is still experimental for IBS, it has shown promise in early studies. It is generally considered safe when performed by qualified professionals.
How do psychological therapies help with IBS? Psychological therapies, such as CBT and gut-directed hypnotherapy, help manage the stress and anxiety that can worsen IBS symptoms, improving overall gut health.
Are neuromodulation techniques effective for IBS?Neuromodulation techniques like TENS and SNS have shown promise in reducing IBS symptoms, particularly abdominal pain, but more research is needed to confirm their effectiveness.
What new medications are available for IBS treatment? New medications like Eluxadoline and Rifaximin target specific aspects of IBS, offering more targeted and effective treatment options for managing symptoms.
Conclusion
Innovative approaches to irritable bowel syndrome treatment are providing new hope for patients struggling with this challenging condition. From microbiome modulation to psychological therapies and neuromodulation techniques, there are now more options than ever for managing IBS symptoms effectively. As research continues to evolve, patients can look forward to even more targeted and personalized treatments in the future.
0 notes
Text
In-Home Enrollment Of Randomized Controlled Trials Finds To Be An Innovative Method Improving Access To Clinical Research
In-Home Enrollment Of Randomized Controlled Trials Finds To Be An Innovative Method Improving Access To Clinical Research
Abstract Introduction: Clostridioides difficile infection is the leading cause of infectious diarrhea in the United States, with substantial morbidity and mortality. Recurrent infection is especially challenging, with each recurrence increasing the likelihood of a successive recurrence, leading to cycles of prolonged symptoms, frequent antimicrobial use, and decreased quality of life. Fecal…
View On WordPress
#Are there C. difficile clinical trials?#C. diff. clinical study#C. difficile clinical trials#Clostridioides difficile Research and Development
0 notes
Link
Close to 3 million people in the United States develop difficult to treat infections caused by drug-resistant bacteria and fungi each year — and about 35,000 die, according to a new government report.
“The modern medicine available to us today may very well be gone tomorrow if we don’t slow the development of antibiotic resistance,” said Robert Redfield, director of the U.S. Centers for Disease Control and Prevention in Atlanta, during a news briefing on November 13.
In its first report on drug-resistant infections in six years, the CDC revised its 2013 report using newly available data including electronic health records from over 700 hospitals. The number of annual deaths from drug-resistant infections at that time is now estimated to have been around 44,000 — almost double the 23,000 deaths previously estimated.
The new report also estimates that currently about 35,000 people die annually from drug-resistant infections, reflecting an 18 percent decrease from the revised number of the 2013 report. That shows there’s been progress in reducing the spread of drug-resistant microbes typically associated with hospitals, a major source of deaths, said Michael Craig, a senior advisor on antimicrobial resistance at the CDC, during the news briefing.

Infections by the fungus Candida auris (shown), which often is resistant to multiple drugs, have proven to be fatal in 30 to 60 percent of cases. C. auris is one of two organisms newly added to the CDC’s list of urgent public health threats.
CREDIT: SHAWN LOCKHART/CDC
Even with the additional data, however, the CDC considers its estimates conservative. In a letter published in Infection Control & Hospital Epidemiology in 2019, researchers from Washington University School of Medicine in St. Louis, using different methodologies, estimate that more than 150,000 people in the United States died from drug-resistant microbes in 2010.
“The CDC’s new numbers represent excellent progress in assessing the burden of antibiotic resistance, but they still likely underestimate its vast impact,” says Greg Frank, director of infectious disease policy for the Biotechnology Innovation Organization, an industry group in Washington, D.C. Deaths due to drug-resistant microbes are often underreported because many patients with these infections also have other health issues that could get recorded as the cause of death, he says.
The latest report also adds two new drug-resistant organisms to the CDC’s list of bacteria and fungi that the agency considers urgent public health threats. The fungus Candida auris and bacteria Acinetobacter that are resistant to the antibiotic carbapenem join the bacteria Clostridioides difficile, drug-resistant Neisseria gonorrhoeae and Enterobacteriaceae that are resistant to carbapenem on the list.
N. gonorrhoeae causes the common, sexually transmitted disease gonorrhea and can cause infertility in women (SN: 12/9/02). Acinetobacter spreads mainly in health care facilities, causing pneumonia and urinary tract infections.
C. auris, which causes severe and often fatal infections in hospitalized patients, is “a pathogen that we didn’t even know about when we put out the last report in 2013,” Craig said. “Since then, it has circumnavigated the globe and has caused a lot of infections and deaths.” Its quick rise from a medically unknown fungus to worldwide health threat may be due to climate change, according to one theory (SN: 7/26/19).
34 notes
·
View notes
Text
Cluster of factors may predict C. difficile infections
Cluster of factors may predict C. difficile infections
A cluster of factors may help predict which patients are likely to develop Clostridioides difficile, a potentially life-threatening disease commonly known as C. difficile or C. diff, a new study has found.
And that could help in efforts to prevent infection, according to the researchers.
Reduced immune function, recent antibiotic use, current or recent hospitalization and prior C. difficile…
View On WordPress
1 note
·
View note
Text
C. Difficile Infection- Ayurvedic Treatment, Diet, Exercises, Research Papers, Yoga & Pranayama
C. Difficile Infection- Ayurvedic Treatment, Diet, Exercises, Research Papers, Yoga & Pranayama
Introduction This is an infectious disease caused by a microbe invasion in the gastro intestinal tract. The bacteria causing this condition, Clostridioides difficile was earlier called Clostridium difficile and often called C. difficile or C. diff. in short. It causes C. difficile infection or C. difficile colitis. This condition develops as the normal healthy gut flora containing good bacteria…

View On WordPress
#C. Difficile Infection-ayurveda-medicines#C. Difficile Infection-ayurvedic-treatment#C. Difficile Infection-herbal-medicines
0 notes
Text
Global Antibiotic Resistance Market Growth, Current Status and Future Scenario of Industry Surveyed in New Research Report 2021-2030
Absolute Markets Insights has announced a statistical data to its extensive repository titled Antibiotic Resistance market. The study comprises of different segments and sub-segments such as type, size, applications, and end-users. One of the many distinctive features of the report is it provides an analytical study of the global Antibiotic Resistance market based on various growth influencing factors. Primary and secondary research techniques have also been used by analysts of the report to study the market. The study also uses information on widespread global regions such as North America, Latin America, Europe, Asia-Pacific, Africa, and India in order to get a better understanding of the competitive landscape. The research report extensively focuses on market size, pricing structures, and shares. The current development patterns of various successful industries have also been mentioned in order to understand effective business strategies.
Vendor Profiling: Antibiotic Resistance Market: Allergan Pharma Co., GlaxoSmithKline PLC., Johnson & Johnson Services Inc., MELINTA THERAPEUTICS - THE ANTIBIOTICS COMPANY, Merck & Co. Inc., Mylan N.V., Nabriva Therapeutics PLC, Otsuka Novel Products GmbH, Pfizer Inc., and Sandoz AG amongst others.
For more information about this report visit: https://www.absolutemarketsinsights.com/reports/Antibiotic-Resistance-Market-2021---2029-876
Key Findings of the Report:
The global antibiotic resistance market was valued at US$ 8417.36 Mn in 2020 growing at a CAGR of 4% over the forecast period (2021 – 2030).
The carbapenem-resistant enterobacteriaceae (CRE) category in the global antibiotic resistance market held the larger market share in 2020. Carbapenem-resistant enterobacteriaceae (CRE) are a family of bacteria that are very difficult to treat due to their highly resistant nature towards antibiotics. They have a reputation of adapting to different types of antibiotic treatments and develop resistance towards them.
The complicated urinary tract infections (cUTI) category in the global antibiotic resistance market held the larger share in 2020. Urinary tract infections (UTIs) are considered to be one of the most common types of infections. According to studies, at least one in two women and one in 10 men experience UTI in their life period.
Antifolates segment occupied the largest market share in the global antibiotic resistance market in 2020. Antifolate drugs are helpful in the treatment of communicable and infectious diseases such as malaria. Many bacteria and viruses that have developed antibiotic resistance spread diseases similar to malaria, such as dengue and other mosquito-borne diseases.
Global Antibiotic Resistance Market: Research Scope
By Resistant Bacteria Type
Pseudomonas Aeruginosa
Clostridioides difficile (C. difficile)
Carbapenem-resistant Enterobacteriaceae (CRE)
Streptococcus pneumoniae (S. pneumoniae)
Acinetobacter
Vancomycin-resistant Enterococci (VRE)
Mycobacterium Tuberculosis (TB)
Neisseria gonorrhoeae (N. gonorrhoeae)
Others
By Disease Indication
Complicated Urinary Tract Infections (cUTI)
Complicated Intra-Abdominal Infections (cIAI)
Community-Acquired Bacterial Pneumonia (CABP)
Acute Skin and Skin Structure Infections (ABSSSI)
Multidrug-Resistant (MDR) and Pulmonary Extensively Drug Resistant (XDR) Tuberculosis (TB) (MDR-TB and XDR-TB)
Sepsis
Clostridium Difficile (C. difficile) Infections
Others
By Drug Class
Antimycobacterials
Fluoroquinolones
Oxazolidinones
Tetracyclines
Penicillins
Antifolates
Combination Treatment
Others
By Route of Administration
Oral
Topical
Intramuscular
Intravenous (IV)
By End Use
Home Care
Healthcare Facilities
Others
By Region
North America
Europe
Asia Pacific
Middle East and Africa
Latin America
Contact Us:
Company: Absolute Markets Insights
Email id: [email protected]
Phone: +91-740-024-2424
Contact Name: Shreyas Tanna
Website: https://www.absolutemarketsinsights.com/
0 notes
Text
Hospital Acquired Infections Therapeutic Market Is Projected To Reach USD 12.5 Billion By 2027
The global hospital acquired infections therapeutic market size is expected to reach USD 12.5 billion by 2027, according to a new report by Grand View Research, Inc. The market is expected to expand at a CAGR of 2.4% from 2020 to 2027. The high prevalence of HAIs, rise in approval and launch of new drugs, and growing hospitalization due to the rise in prevalence of chronic diseases are driving the market.
According to the data published by the New York State Department of Health in November 2019, around 160 hospitals in New York reported total cases of around 1,139 colon SSIs out of 19,732 procedures in 2018, a rate of 5.8 infections per 100 procedures. The same source also states that in 2018, around 15,310 cases of Clostridioides difficile infections (CDI) were reported in acute care hospitals located in New York. Such, high prevalence of hospital-acquired infections is anticipated to significantly raise the demand for its treatment therapies and support the HAIs therapeutics market growth over the forecast period.
Furthermore, key players in the market are involved in extensive R&D initiatives for the development and indication expansion of its already approved drugs for HAI treatment. For instance, in February 2018, the FDA approved Allergan plc’s supplemental New Drug Application (sNDA) and expanded the approval of Avycaz (ceftazidime and avibactam) to include the treatment of HABP/VABP and hospital-acquired bacterial pneumonia.
Request a free sample copy or view report summary: Hospital Acquired Infections Therapeutic Market Report
Hospital Acquired Infections Therapeutic Market Report Highlights
Antibacterial drugs dominated the drug class segment in 2019, owing to the high adoption of antibiotics as the first line of treatment for hospital-acquired infections (HAIs)
The surgical site infections (SSIs) segment held the largest market share in 2019 due to the rising number of surgical procedures and subsequent rising cases of SSIs
The urinary tract infections (UTIs) segment is anticipated to show the fastest growth rate during the forecast period owing to the growing number of UTI cases and rising awareness among people about the disease condition in less-developed countries
The introduction of novel drugs by key players, for instance, Merck to treat ventilator-associated pneumonia has led to a high growth of the market
The high prevalence of HAIs in the European countries is the major factor significantly driving the demand for its medications in this region
Growing awareness levels about various risk factors associated with HAIs in ICU and other emergency care settings is expected to propel market growth in the Asia Pacific region
Hospital Acquired Infections Therapeutic Market Segmentation
Grand View Research has segmented the global hospital acquired infections therapeutic market report on the basis of drug class, infection type, and region:
HAIs Therapeutics Drug Class Outlook (Revenue, USD Million, 2016 – 2027)
Antibacterial Drugs
Antiviral Drugs
Antifungal Drugs
Cell Wall Synthesis Inhibitors
Protein Synthesis Inhibitors
Others
HAIs Therapeutics Infection Type Outlook (Revenue, USD Million, 2016 – 2027)
Urinary Tract Infections
Ventilator-associated Pneumonia
Surgical Site Infections
Bloodstream Infections
Other Hospital Infections
HAIs Therapeutics Regional Outlook (Revenue, USD Million, 2016 – 2027)
North America
Europe
Asia Pacific
Latin America
MEA
U.S.
Canada
Germany
U.K.
Spain
France
Italy
Russia
Japan
China
India
South Korea
Singapore
Australia
Brazil
Mexico
Argentina
South Africa
Saudi Arabia
UAE
List of Key Players of Hospital Acquired Infections Therapeutic Market
Merck & Co., Inc.
Pfizer Inc.
Bayer AG
GlaxoSmithKline Plc.
Daiichi Sankyo Company, Limited
AbbVie Inc.
Abbott Laboratories
F. Hoffmann-La Roche Ltd
Allergan Plc.
About Grand View Research Grand View Research, Inc. is a U.S. based market research and consulting company, registered in the State of California and headquartered in San Francisco. The company provides syndicated research reports, customized research reports, and consulting services. To help clients make informed business decisions, we offer market intelligence studies ensuring relevant and fact-based research across a range of industries, from technology to chemicals, materials and healthcare.
0 notes
Text
PureTech’s Vedanta Biosciences gets federal funding for C. Diff. microbiome therapy

US biotech Vedanta Biosciences has been awarded up to $76.9 million to develop VE303 for high-risk Clostridioides difficile (C. diff.) infection by a US government agency.
The Biomedical Advanced Research and Development Agency (BARDA) will pay $7.4 million up front, plus payments worth up to $69.5 million if the project is successful.
Vedanta is one of PureTech’s stable of companies and this is the first ever BARDA award in the microbiome field.
Funding will support completion of an ongoing phase 2 trial and further clinical development of VE303, an orally-administered live biotherapeutic product (LBP) consisting of eight bacterial strains designed to therapeutically reset a patient’s gut microbiota to stop C. Diff infection.
The product is made from pure, clonal bacterial cell banks, which yield a standardised drug product in powdered form, and could replace the need for faecal transplants and the process of having to find donors.
Products such as this aim to repopulate the gut with harmless bacteria that are resistant against pathogenic bacteria such as C. diff., which can take hold in a patient’s digestive tract after treatment with antiobiotics.
While there are no approved competitors, Ferring Pharma reported positive results from a phase 3 trial of its RBX2660 earlier this year, and other firms working in this area include UK-based Microbiota, working in partnership with Roche.
Vedanta’s ongoing phase 2 study is a multi-centre, randomised, double-blind, placebo-controlled trial designed to evaluate the safety and efficacy of two doses of VE303 compared to placebo in patients with high-risk C. diff. infection.
The study is enrolling patients with a recent confirmed diagnosis of C. Diff. infection who have completed a course of antibiotics but remain at high risk for recurrence. The primary endpoint is prevention of infection recurrence at eight weeks.
Vedanta was founded by PureTech and a global team of scientific co-founders who have expertise in the cross-talk between the microbiome and the immune system.
The post PureTech’s Vedanta Biosciences gets federal funding for C. Diff. microbiome therapy appeared first on .
from https://pharmaphorum.com/news/puretechs-vedanta-biosciences-gets-federal-funding-for-c-diff-microbiome-therapy/
0 notes
Text
$1 billion antibiotic venture fund launched
Antibiotic resistance is a problem. One study from Europe found that in 2015 there were 33,110 deaths attributable to antibiotic resistance; accounting for morbidity as well, antibiotic resistance lead to a a decrease of 874,541 disability-adjusted life years. CDC data show that antibiotic resistant bacteria and fungi caused 35,900 deaths in 2019, 12,800 deaths due to Clostridioides difficile infections.
To fight this trend, large life sciences firms are teaming up with governments and non-governmental organizations to help fund antibiotic research. Endpoints reports:
Pfizer, Eli Lilly, Novo Nordisk, Boehringer Ingelheim, Bayer Pharmaceuticals, Merck KGaA and the American Merck — one of the last giants standing — are teaming up to create a $1 billion for-profit venture to bet on small biotechs developing mid-stage antibiotics, Ed Silverman reported for STAT. Government officials from Germany, Sweden, France and the UK, as well as representatives from Wellcome Trust and Pew Charitable Trusts, will join the companies to announce the initiative on July 9, Silverman wrote. The World Health Organization and the European Investment Bank are also involved in what is being billed as a new solution to the “antibiotic innovation challenge.”
This is welcome news. However, is $1 billion enough? According to Endpoints, they claim the answer is ‘no’.
Considering the number of players and the collective heft they bring — plus the fact that the EIB might contribute as much as 10% — the money isn’t much. By pharma standards, $1 billion won’t even buy you a bolt-on deal, typically in the $2 billion to $5 billion range. It also marks the threshold for blockbuster status that any big cancer drug franchise could easily surpass
While more funding is needed, this is a welcome steps towards addressing a serious public health problem.
$1 billion antibiotic venture fund launched published first on your-t1-blog-url
0 notes
Text
Investigating intestinal bile acids for C. difficile antitoxin development
Clostridioides difficile can cause significant colitis and is a major public health concern. In particular, this bacterium is the most common cause of infectious diarrhea in hospitals and can result in death in severe cases. Two toxins produced by C. difficile, TcdA and TcdB, have been shown to cause disease in animal models, but TcdB is thought to be the primary disease-causing toxin in humans. Previous work has demonstrated that intestinal bile acids can modulate the C. difficile lifecycle, as microbial-derived secondary bile acids, such as deoxycholic acid and lithocholic acid, can inhibit the bacterium’s growth and germination.
SBGrid members Roman Melnyk and Borden Lacy and other researchers have been working to investigate the molecular-level effect of intestinal bile acids on TcdB toxin. The authors demonstrated that primary and secondary bile acids individually bind to TcdB, inhibiting the toxin. More specifically, this binding interaction causes the toxin to change structural conformation such that it is no longer capable of binding to host cell surface receptors. Using this information, they screened bile acid mimetic structures to identify if any could induce comparable conformational changes in TcdB to prevent cell binding, and identified non-steroidal small molecule scaffolds which bind and inhibit this toxin. This could enable the development of C. difficile antitoxins based on this new mechanistic insight.
Read more about this work in PNAS.
#sbgrid#pnas#science#nature#biomedical engineering#structural biology#microbiology#global health#infectious disease#biology#medical#member research
0 notes
Text
Clinical Trial Study Moving Closer to Having Safe and Effective Products to Restore the Gut Microbiome for Patients with Recurrent C. difficile Infections.
Clinical Trial Study Moving Closer to Having Safe and Effective Products to Restore the Gut Microbiome for Patients with Recurrent C. difficile Infections.


Sahil Khanna, M.B.B.S.
A new study published online in the journal ClinicalInfectious Diseases looked at the use of a non-frozen capsule of microbiome restoration therapy for treating patients with recurrent C. difficile infection.
“Patients with C. difficile are typically managed with antibiotics or fecal transplantation for recurrent C. difficile,” says the study’s author, Sahil…
View On WordPress
#C. diff. clinical study#C. difficile clinical trials#Clostridioides difficile Research and Development#Fecal Microbiota Transplantation#FMT#gut microbiome#Mayo Clinic#Microbiome#Sahil Khanna MBBS
0 notes
Text
Fecal microbiota transplants successfully treat patients with C. diff


A new study from the University of Birmingham has shown that Faecal Microbiota Transplants (FMT) are highly successful in treating patients with Clostridioides difficile (C.diff) infection.
Published in EClinical Medicine, results from the first licenced English stool bank, which supplies FMT treatment to patients in the NHS, have shown that in 78% of cases the patient’s diarrhoea had stopped and had not returned in the 90 days after treatment.
Antibiotics can be effective in treating the first episode of C.diff. However, 10-20% of patients don’t respond and the infection then recurs. Success rates of antibiotics in relapsing infection can be as low as 30%.
C.diff infections result from the good gut bacteria being killed by antibiotics given for other infections and causes severe diarrhoea, abdominal pain and may be fatal in elderly patients.
During FMT, the good bacteria in the faeces of a healthy donor are transferred to the gut of a patient with the infection.
The Microbiome Treatment Centre at the University of Birmingham is the first in the UK to be licenced for FMT preparation by the Medicines and Healthcare products Regulatory Agency (MHRA), supplying NHS patients across the country.
Before the dedicated centre was set up, many patients across the UK were unable to access this treatment.
Scientific studies have demonstrated that FMT treatment is better than treatment with special expensive antibiotics for C.diff infections, particularly when the patient’s infection has come back again.
The development of a licenced FMT service at the University of Birmingham will widen the supply and improve equality of access to FMT treatment across the NHS. It will provide critical support for researchers both here in Birmingham and in other centres working on how FMT produces a cure not only in C.diff infection but also conditions such as ulcerative colitis and other diseases which seem to be linked to the gut microbiome.
Lead author Dr Victoria McCune, Consultant Clinical Scientist in Microbiology at South Tees Hospital NHS Foundation Trust, said:
“Our research has successfully shown the benefits of treating recurrent C.diff patients with FMT. Our standardised approach to making FMT will improve the quality and safety of this treatment for many more patients.”
Professor Peter Hawkey, Professor of Clinical and Public Health Bacteriology at the University of Birmingham’s Institute of Microbiology and Infection, said:
“This work has turned an unregulated potentially dangerous method of faecal transplantation into a national service providing rapid, safe regulated, life-saving treatment for a serious disease affecting thousands of patients in the UK.”
###
Notes to editor:
* The University of Birmingham is ranked amongst the world’s top 100 institutions. Its work brings people from across the world to Birmingham, including researchers, teachers and more than 6,500 international students from over 150 countries.
* McCune et al (2020). ‘Results from the first English stool bank using faecal microbiota transplant as a medicinal product for the treatment of Clostridioides difficile infection’. EClinical Medicine.
Disclaimer: We can make mistakes too. Have a nice day.
New post published on: https://www.livescience.tech/2020/03/16/fecal-microbiota-transplants-successfully-treat-patients-with-c-diff/
0 notes
Text
Clostridioides difficile infection flourishes with a high-protein, high-fat diet
Mice fed a high-fat, high-protein diet were more likely to develop and die from antibiotic-driven Clostridioides difficile infections than mice fed a standard diet. In the same study, published in the journal mSystems, a high-carbohydrate diet was protective against severe C. difficile infection–but the researchers suspect that such a diet could produce healthy, asymptomatic carriers that can spread the pathogen. Clostridioides difficile infection flourishes with a high-protein, high-fat diet syndicated from https://triviaqaweb.blogspot.com/
0 notes