#Cellulitis skin infection
Explore tagged Tumblr posts
Text
cellulitis treatment: quick relief | KBK Hospitals

Quick and effective cellulitis treatment at KBK Hospitals. Precise diagnosis, holistic care, and customized plans for fast recovery
#Cellulitis skin infection#Antibiotics for cellulitis#Cellulitis symptoms#cellulitis prevention#cellulitis diagnosis#cellulitis cure#skin infection treatment
0 notes
Text
Acute Bacterial Skin And Skin Structure Infections Market Trends driven by Increasing Antibiotic Resistance
The acute bacterial skin and skin structure infections (ABSSSI) market comprises anti-infective drugs that are used to treat skin infections caused by bacteria. These infections include impetigo, cellulitis, wound infections, and major cutaneous abscesses. The commonly prescribed drugs are antibiotics such as cephalosporins, carbapenems, lipoglycopeptides, oxazolidinones, and tetracyclines. The increasing threat of antimicrobial resistance (AMR) has boosted the demand for effective antibiotic treatments. Growing prevalence of skin infections owing to rising environmental pollution levels and lifestyle changes has also augmented market growth.
Global acute bacterial skin and skin structure infections market is estimated to be valued at USD 3,842.5 Mn in 2024 and is expected to reach USD 5,701.7 Mn by 2031, exhibiting a compound annual growth rate (CAGR) of 5.8% from 2024 to 2031.
Key Takeaways Key players operating in the Acute Bacterial Skin And Skin Structure Infections market are Fresenius SE and Co. KGaA, Pfizer, Inc., Amneal Pharmaceuticals LLC, Intas Pharmaceuticals Ltd., Cadila Healthcare Ltd., Glenmark Pharmaceuticals Ltd, GSK plc, Sun Pharmaceutical Industries Ltd., Aurobindo Pharma Ltd., AbbVie, Inc., Melinta Therapeutics LLC, Accord Healthcare Ltd., Merck and Co., Inc., Teva Pharmaceutical Industries Ltd., Paratek Pharmaceuticals, Inc. The growing prevalence of skin infections across the world coupled with the rising threat of AMR is fueling the demand for effective antibiotic therapies. Leading market players are investing in R&D to develop novel drugs with new mechanisms of action. On the other hand, companies are also undertaking initiatives to expand their presence in emerging economies through strategic partnerships and acquisition activities. The Acute Bacterial Skin And Skin Structure Infections Market Demand rising threat of antimicrobial resistance is a key concern that is augmenting the demand for novel and effective anti-infective treatments for ABSSSIs. According to the WHO, drug-resistant bacteria could cause 10 million deaths annually by 2050 if adequate actions are not taken. Growing awareness regarding antibiotic stewardship practices is reducing the irrational use of antibiotics to some extent. However, further regulatory interventions and strict prescribing guidelines are required to curb the development and spread of resistant pathogens. Market Key Trends One of the major trends witnessed in the acute bacterial skin and skin structure infections market is the rising focus on developing new antibiotic classes with novel mechanisms of action to overcome anti-microbial resistance. Several pipeline drugs under clinical trials employ new mechanisms like inhibition of bacterial DNA/RNA synthesis, cell wall biosynthesis, and protein synthesis. Monoclonal antibodies targeting specific toxins produced by resistant bacteria is another novel area being explored. Fast track approvals and commercialization of path-breaking antibiotic therapies will ensure long-term market sustenance amid growing healthcare costs and stringent pricing control by governments globally.
Porter's Analysis Threat of new entrants: New players find it difficult to enter this market owing to high costs of R&D and regulatory requirements. Bargaining power of buyers: Many buyers have low bargaining power due to lack of alternatives. Bargaining power of suppliers: Suppliers have moderate bargaining power due to availability of substitute sources. Threat of new substitutes: Threat from new substitutes is moderate due to technology developments and increasing investments in alternatives. Competitive rivalry: Fierce competition exists among existing players to gain market share. Geographical Regions North America accounts for the largest share of the global acute bacterial skin and skin structure infections market, in terms of value, followed by Europe. This is attributed to the rapidly growing incidence of skin infections, advanced healthcare infrastructure, favorable reimbursement policies, and high awareness among healthcare professionals and patients regarding diagnosis and treatment. Asia Pacific is expected to witness the fastest growth during the forecast period, primarily driven by improving access to healthcare facilities owing to rising disposable incomes, growing incidence of skin infections due to changing lifestyles, and supportive government policies and initiatives in emerging economies. Rising medical tourism in Asian countries has also boosted the market growth in the region.
Get more insights on Acute Bacterial Skin And Skin Structure Infections Market
Vaagisha brings over three years of expertise as a content editor in the market research domain. Originally a creative writer, she discovered her passion for editing, combining her flair for writing with a meticulous eye for detail. Her ability to craft and refine compelling content makes her an invaluable asset in delivering polished and engaging write-ups.
(LinkedIn: https://www.linkedin.com/in/vaagisha-singh-8080b91)

#Coherent Market Insights#Acute Bacterial Skin And Skin Structure Infections Market#Acute Bacterial Skin And Skin Structure Infections#Cellulitis#Abscess#Skin Abscess#Wound Infection#Erysipelas
0 notes
Text
Cellulitis
Cellulitis may spread rapidly. Affected skin appears swollen and red and may be hot and tender.
0 notes
Text
Cellulitis: A Common and Potentially Serious Skin Infection
Have you ever noticed a red, swollen, and painful area on your skin that feels warm to the touch? If so, you may have cellulitis. Cellulitis is a common bacterial skin infection that can affect anyone at any age. It can spread quickly and cause serious complications if left untreated. In this post, we will explain what cellulitis is, what causes it, how to recognize it, and what to do if you have…

View On WordPress
0 notes
Text
Saw a patient today who had been through a series of medical visits that epitomizes what I hate about multiple different kinds of care providers. Their VA dermatologist took a scoop out of them to remove a basal cell cancer. Fine. I’m not a dermatologist, maybe it needed those wide margins. (If it didn’t, going that deep should mean it was an excisional biopsy and they put in sutures to close it.) They gave the patient and his wife confusing instructions about wound care. They didn’t provide guidance around keeping it covered or moist. It got infected. His wife took him to Urgent Care. The UC doc took a swab of the wound and started antibiotics. They came to see me for a visit we scheduled ages ago for something else.
Here’s the thing. Wounds need to be kept at what I call the Goldilocks moisture level: not too dry and not too wet. If it’s pruny/white/mushy like it’s been in a bathtub, it’s too wet. If it’s cracking, it’s too dry. This is why you can’t say “cover it for X days and then leave it out.��� That would be like telling someone with heart failure and lower extremity edema “take the diuretic for a week and then stop” without any instructions around dry weight, dizziness, etc. It’s more complicated than that.
This wound was too dry. No one had talked to them about keeping it moist. No one had even mentioned Vaseline.
No, they got a wound swab. Want to guess how good a wound swab is for an open wound exposed to the world? Pretty terrible. You can improve it a little bit by making sure you’ve removed some kind of layer and then expressing fluid directly from the wound with the swab, but it’s still bad. The only time I give a shit about what grows from a wound swab is when it was a) collected in the OR (as when the podiatrist gets a sample of osteomyelitic bone in a sterile environment) or b) when it grows pseudomonas. Everything else? I can figure out by looking at it. If it’s skin it’s probably either staph or strep. If it’s staph, it’s either MRSA or MSSA. If it’s MRSA, it’s making a lot of pus, it’s red, it’s hot, it’s painful. This wasn’t. So it was either MSSA or strep. So what are we going to do for systemic antibiotics? Probably the same thing we would have done anyway—Keflex.
And what’s the utility of systemic antibiotics in a skin wound? Not a lot, most of the time. This wasn’t cellulitis proper. It wasn’t red or hot or angry enough. A red border around the wound does not a systemic infection make. And if you don’t care properly for the wound itself, there’s no point in antibiotics, because it still can’t heal. Antibiotics can get where blood goes. Blood does not go into the slough that is the bacterial biofilm covering a wound.
So I sat there with gauze and saline and gently debrided the 100% slough off the wound. It’s yucky and it takes time and attention. It doesn’t get compensated. That’s why no one else had done it yet. The derm had blown it off as “it’s healing, it’s fine.” It wasn’t healing. It was developing rolled edges, where the wound edges couldn’t heal across the slough and so they started to curl back under themselves. If taking off the slough (and keeping it gone by MAINTAINING PROPER CONDITIONS) doesn’t let it heal, I’ll need to get him back in and rough up the edges with a Buck’s curette until it can heal.
Multiple professionals who should have known better tried to make my patient just go away, rather than heal him.
I’m pissed. I’m tired. I think I have a cold. I shouldn’t be doing the work the dermatologist or the UC provider should have done. And because of everything they’d told her, his wife was pissed at me for doing what was correct. “We’ve heard a lot of different things!” Yes, and I’m right. You’ll find out when the wound actually starts healing when we care for it properly.
The value of a model is in what it can predict. Wounds are great about making it clear when your model sucks.
294 notes
·
View notes
Text
Writing Notes: Bites & Stings

References (Dog Bites; Cat; Human; Spider; Bee & Wasp; Snake; Jellyfish)
Bites and stings - puncture injuries inflicted by an animal that penetrate the skin.
DOGS
A typical dog bite results in a laceration, tear, puncture, or crush injury.
Bites from large, powerful dogs may cause fractures and dangerous internal injuries. Dogs trained to attack may bite repeatedly during a single episode.
Infected bites usually cause pain, cellulitis (inflammation of the connective tissues), and a pus-filled discharge at the wound site within 8–24 hours.
Many infections are confined to the wound site, but some of the microorganisms in the mouths of dogs can cause systemic and possibly life-threatening infections.
Rabies is rare among pet dogs in the United States, most of which have been vaccinated against the disease. Tetanus is also rare but can be transmitted by a dog bite if the victim is not immunized.
CATS
The mouths of cats and dogs contain many of the same microorganisms.
Cat scratches and bites are also capable of transmitting the Bartonella henselae bacterium, which can lead to cat-scratch disease, an unpleasant but usually not life-threatening illness.
Cat bites are mostly found on the arms and hands.
Sharp cat teeth typically leave behind a deep puncture wound that can reach muscles, tendons, and bones, which are vulnerable to infection because of their comparatively poor blood supply.
This is why cat bites are much more likely to become infected than dog bites.
Also, people are less inclined to view cat bites as dangerous and requiring immediate attention; the risk that infection has set in by the time a medical professional is consulted is thus greater.
HUMANS
Humans bites result from fights, sexual activity, medical and dental treatment, and seizures. Bites raise the possibility of spousal or child abuse.
Children often bite other children, but those bites are hardly ever severe.
Human bites are capable of transmitting a wide range of dangerous diseases, including hepatitis B, syphilis, and tuberculosis.
Human bites fall into two categories:
Occlusional (true) bites present a lower risk of infection.
Clenched-fist injuries, which are very infectious and can permanently damage the hand, usually result from a fist hitting teeth during a fight.
People often wait before seeking treatment for a clenched-fist injury, with the result that about half of such injuries are infected by the time they are seen by a medical professional.
SPIDERS
As a rule, people rarely see a black widow bite, nor do they feel the bite as it occurs. The first (and possibly only) evidence that a person has been bitten may be a mild swelling of the injured area and two red puncture marks.
Within a short time, some victims begin to experience severe muscle cramps and rigidity of the abdominal muscles. Other possible symptoms include excessive sweating, nausea, vomiting, headaches, and vertigo, as well as breathing, vision, and speech problems.
A brown spider’s bite can lead to necrotic arachnidism, in which the tissue in an area of up to several inches around the bite becomes necrotic (dies), producing an open sore that can take months or years to disappear.
In most cases, the bite simply produces a hard, painful, itchy, and discolored area that heals without treatment in 2–3 days.
The bite may be accompanied by a fever, chills, edema (an accumulation of excess tissue fluid), nausea and vomiting, dizziness, muscle and joint pain, and a rash.
BEES & WASPS
The familiar symptoms of bee and wasp stings include pain, redness, swelling, and itchiness in the area of the sting.
Multiple stings can have much more severe consequences, such as anaphylaxis, a life-threatening allergic reaction that occurs in hypersensitive persons.
SNAKES
Venomous pit viper bites usually begin to swell within 10 minutes and sometimes are painful.
Other symptoms include skin blisters and discoloration, weakness, sweating, nausea, faintness, dizziness, bruising, and tender lymph nodes.
Severe poisoning can lead to tingling in the scalp, fingers, and toes; muscle contractions; an elevated heart rate; rapid breathing; large drops in body temperature and blood pressure; vomiting of blood; and coma.
Many pit viper and coral snake bites (20–60%) fail to poison (envenomate) their victim, or introduce only a small amount of venom into the victim’s body.
The wounds, however, can still become infected by the harmful microorganisms that snakes carry in their mouths.
Coral snake bites are painful but may be hard to see.
One to seven hours after the bite, a bitten person begins to experience the effects of the venom, which include tingling at the wound site, weakness, nausea, vomiting, excessive salivation, and irrational behavior.
Major nerves of the body can become paralyzed for 6–14 days, causing double vision, difficulty swallowing and speaking, respiratory failure, and other problems.
Six to eight weeks may be needed before normal muscular strength is regained.
JELLYFISH
Jellyfish venom is delivered by barbs called nematocysts, which are located on the creature’s tentacles and penetrate the skin of people who brush up against them. Instantly, painful and itchy red lesions usually result.
The pain can continue up to 48 hours.
Severe cases may lead to skin necrosis, muscle spasms and cramps, vomiting, nausea, diarrhea, headaches, excessive sweating, and other symptoms.
In rare instances, cardiorespiratory failure may occur.
Source ⚜ More: Writing Notes & References More: Writing Realistic Injuries ⚜ On Anatomy ⚜ Poison ⚜ Fight Scenes Part 1 2
#writing notes#animals#writeblr#dark academia#spilled ink#literature#writers on tumblr#writing reference#writing prompt#medicine#poets on tumblr#poetry#words#writing inspiration#creative writing#fiction#dogs#writing ideas#thomas gainsborough#writing resources
125 notes
·
View notes
Text

Comfort drawing of Onetrick
I have a skin infection (cellulitis) in my top surgery scars, I'm on antibiotics and have been getting better but I decided to finish this sketch to help me feel better ❤️
#digital art#art#oc artwork#character art#original character#oc#artwork#furry#mlp fanart#mlp#mlp oc#mlp art#mlp oc pony#mlp original character#my little pony#my litte pony friendship is magic#mlp g4#pony oc#pony character#unicorn#sona art
25 notes
·
View notes
Text
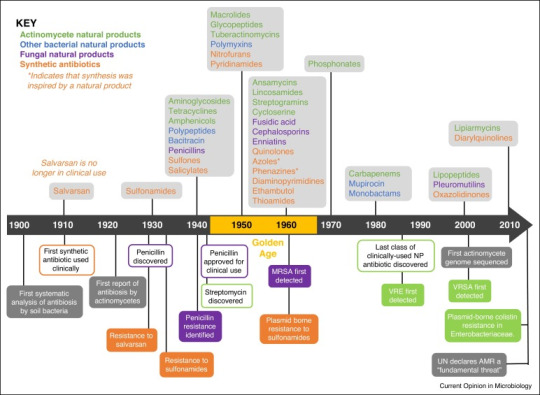
Magic Bullets: The Antibiotic Story
The year was 1907 and a Dr. Alfred Bertheim was trying to make arsenic less toxic to humans.
Why? Because in addition to killing humans, arsenic also kills trypanosomes- single-celled protozoa that cause the life-threatening infection trypanosomiasis. By creating a version of arsenic that still killed the protozoa, but not the human they infected, Dr. Bertheim could create a drug to treat the disease*.
This was not a fully new idea. About 50 years earlier, a drug called Atoxyl had been created in France. About 40 times less toxic than pure arsenic, it had been shown to not only successfully treat trypanosomiasis, but also the equally devastating syphilis infection.
But 40 times less toxic than pure arsenic is still not great. About 2% of people treated even one time with the drug ended up blind, among a myriad of other side effects. It was a start, but not ideal.
And Dr. Bertheim (under the direction of better-known Dr. Paul Ehrlich) was setting out to change that.
And it just so happened that the sixth compound from the sixth group he tried did so. Known as "compound 606", the new Arsphenamine could treat trypanosomiasis, relapsing fever, and syphilis very effectively- and it didn't leave its takers dead or blind.
Most of the time, at least. See, arsphenamine, also known by the brand name salvarsan, was a pain in the ass to administer. It had to be dissolved in several hundred mililiters of water under a nitrogen atmosphere to prepare it for administration. If it touched air, it would rapidly react, causing toxic byproducts that could cause liver failure, severe skin rashes, and even death.
But both trypanosomiasis and syphilis were definitely going to kill you, so it was worth the risk.
And the seed had been planted, so to say. The idea of a chemical able to kill infection-causing agents without killing the host was a true possibility for the future of medicine.
And by 1912, Neosalvarsan, a drug somewhat less effective -but far easier to administer and with significantly fewer side effects- was on the market. Over the next decade, Neosalvarsan would be responsible for a massive drop in syphilis cases worldwide.
But neither of the drugs could treat deadly infections from staph or strep or the hundreds of other bacterial or viral infections that still had no cure in the 1910's and 1920's.
Then came the first of the heavy-hitters. Bayer was a dye company when it started, and in 1932, three and a half decades after switching mostly to pharmaceuticals, chemists at Bayer were testing the company's dyes for anti-infective properties. They went through thousands of trials, finally finding a dye that could kill streptococcal bacteria without killing a mouse host.
Pre-1930s, streptococcal disease was a major problem. It caused strep throat, cellulitis, scarlet fever, childbed (purpural) fever, some forms of toxic shock syndrome, impetigo, necrotizing fasciitis, rheumatic fever, and many others. The skin infections may have been at least somewhat treatable with a hot compress, but the rest were prone to cause blindness, deafness, loss of limbs, and for many, loss of life.
In 1936, sulfonamide antibiotics changed that. Protosil, the first of the sulfonamides, became available to treat many of the infections listed above. These would be used for wound infections throughout WWII. Unfortunately, they would also cause the untimely death of nearly 100 people via the Elixer Sulfanilamide tragedy.
Sulfanilamide was a similar drug to Prontosil and was safe and effective for treating strep infections. However, when mixed with diethylene glycol (now used as standard car antifreeze) to make it into a liquid suspension, it was deadly. See this letter from a doctor who had prescribed the liquid form of the medication, not knowing it was poison:
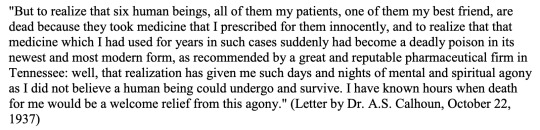
[to read more about the Elixer Sulfanilamide Disaster, see here]
Despite the sulfanilamide tragedy, the race was on for more antibiotics. Three years before they went on the market, researchers had found evidence of bacterial resistance to sulfonamides. What would happen when these new bacteria, that didn't die when exposed to the new wonder drug, made up so much of the bacterial population?
In 1942, the Cocoanut Grove fire in Boston caused over 492 deaths and 130 injuries. The injured were among the first to receive a remarkable new drug called penicillin. The fire and the fate of the victims were publicized throughout the world, and penicillin became a household name overnight. But once again, even before it went on the market in 1943, just in time for the end of the Second World War, there was evidence of resistance.
But fortunately, the fire had been sparked. Over the next 30 years, many dozens of antibiotics would come into clinical use. If you've taken it, it probably came out between 1940 and 1970. Tetracycline, isoniazid, metronidazole, ciprofloxacin, erythromycin, vancomycin, amoxicillin, and dozens more you've never heard of.
And then? Nothing.
Well, not completely nothing, there were a couple that came out in the 1980s and a few in the early 2000s. But nothing like that 30-year golden age.
But now we're running into problems due to drug resistance. About 1.27 million people die annually directly from antibiotic resistant infection, while antibiotic resistance contributes to about 4.95 million more deaths.
The good news is that the drugs that are being made today are directly targeting those antibiotic resistant infections. In fact, as I'm writing this, a new drug (Zosurabalpin) is being tested for a bacteria called Carbapenem-resistant Acinetobacter baumannii, which up until now has had no antibiotic that works against it.
*as you may imagine for the time period, this was not necessarily a benevolent act. See, most of the reason Europeans wanted to treat trypanosomiasis in the first place was because they kept dying of it when they went to colonize Africa. And they wanted something that would give them a leg up on the people who were already there.
107 notes
·
View notes
Text

This is a heads up for my disabled, ADHD, fat, and chronically ill followers that may have to deal with injuries and topical infections! This stuff is awesome for if you have to look after a wound that you can't easily reach or clean multiple times a day.
Gentian Violet is a non-prescription topical antibacterial liquid that contains a blue skin-dying agent. My wound care doctor is fat, and his patients are largely bed-bound, bariatric, or otherwise can't keep up with rigorous wound-cleaning and bandaging routines for stuff like injuries or flareups of cellulitis infections.
This stuff stings pretty bad at first when it's applied and stains your skin a really potent blue color. Once the Gentian dries and dyes your skin, it means that you have a painted-on antibiotic membrane over your wound that you don't have to bandage, and keeps its seal on your wound for TWO DAYS. That includes with regular showering/bathing.
If you have memory issues, this stuff is fantastic. Not only does it stay active and killing bacteria for 2 days, but the reason the stuff is dyed so potently is so you remember to reapply it when the dye fades. When the dye starts to show your regular skin through again? Time too reapply!
If you have motion, mobility, or fatigue problems, this stuff is fantastic. Especially if you're looking after a wound that's in a tricky place to keep clean all the time without having to fully shower, you can literally use cotton swabs (no double-dipping, please! It's not sanitary!!!) to paint the area, and don't have to concern yourself with it again for another couple of days, giving you extra time to rest and heal, and more time to avoid feeling overwhelmed and panicked because you're "not taking good enough care" of it.
If you're allergic to bandage adhesives or get contact dermatitis from wound dressings, this stuff is great. Sometimes an injury or wound needs dressing just for the sake of the healing process rather than avoiding infection, but for ones where that isn't a concern for you, Gentian is a really good alternative for if Stuff That Cuts Off Air To Your Skin gives you problems.
All in all? It stings like hell at first, but my actual doctor told me that he regularly treats patients with full-limb wounds, and they suffer no ill effects for having large portions of their bodies painted with it instead of bandages and gauze.
If it seems like it might be helpful for you, please do talk to your doctor about it. In my state, it's non-prescription and my doctor gave me my bottle for free. Just be careful with using new medical products, and always remember that it's okay to say, "I can't do that easily. I'm disabled. Can you please provide alternatives for me?" when it comes to medical staff pushing you into care regimens that are more destructive than healing for you.
20 notes
·
View notes
Text
day off
Dude was in town for thanksgiving. it was supposed to be all of us but one of my nephews came down with walking pneumonia, which is apparently what all the kids are getting, so we didn't get the family thanksgiving. but dude came out, and programmed the thermostat in my cabin. i still think i'm going to mostly keep it shut off though. i'm getting low on propane and it's worrying me that it'll run out in the middle of the night sometime. it is 20F today though. and I have finally, with help, got my loom all ready and have started to weave the project i got all the stuff for last Christmas.
so i'm hanging out out here even though i could go inside and not be having to heat this space. so i'm like, not heating the space, even though it's slightly uncomfortable. it's up to 50F at the moment so i can't complain too much, the sun is out.
anyway-- I spent some time out here yesterday too and I got a bunch of work done both on the weaving and on the writing. I'm close to having enough of a first draft of the first bit of the tall ships solarpunk bisexuals novel that any of y'all who've expressed interest in reading will have something i can share with you soon. i just need to figure out where i'm heading.
i was going to put up more of the aubreyad fanfic too at some point but it's been so busy and then i just don't have any executive function. it's been rough.
oh also i got cellulitis again. i noticed a weird zit on my leg and in daylight i was like oh. that's an infection. what the fuck. never any broken skin but it managed anyhow. so i just immediately went to urgent care on friday morning when everyone else was meeting up to shop or whatever, and they were like oh well done for coming in this early, and gave me doxycycline. so i'm avoiding dairy for 8 hours a day now but you'd be surprised how much cheese you can eat around that restriction. i'm managing.
i also have to avoid sun but that takes zero actual effort this time of year. only a week of this left. the actual infection site looks fine but i'm of course giving it no quarter. i'm annoyed because i got several little cuts in my hands during all the hell of turkey processing and i was so good and so careful and none of THEM got infected so WTF. ugh.
I guess this season I'm thankful for doxycycline.
now, back to the solarpunk tall ship bisexuals, which keeps taking plot turns i had not anticipated and is not going where i expected. i think i'm also rambling too much but. y'know! we'll see.
the current scene that's rambling on far too long features the main non-sailor character realizing that she's inadvertently taught her nine-month-old to (in sign language) call the computer "daddy" because her father has been away at sea long enough that the child only remembers looking at pictures of him on the computer, and so now she requests screentime by making the sign for father. It is more or less her first word.
18 notes
·
View notes
Text
16 Wound Care Tips
DISCLAIMER: I’m not a doctor. The most medical advice you’re gonna get in here is ‘you should probably see a doctor if you see xyz’. I can’t definitively say if something’s infected or not, nor tell you about your specific circumstances.
TW for references to self-harm, and for somewhat graphic descriptions of wounds.
1. Your skin has 3 layers. The surface-level one is the epidermis; the white stuff beneath that is the dermis; and the yellowish stuff beneath that is the hypodermis. Any wounds that go deeper than the dermis need urgent medical care. Anything that goes deeper than the hypodermis is an emergency.
2. Deeper wounds are more likely to get infected than shallow ones. Unfortunately, deeper infections are also generally more dangerous than shallow ones. General things to look out for that signal infection are: redness; rash; a sense of heat in the wound; inflammation; red lines radiating from the wound; swelling; blistering; crust around the wound; impaired healing; pain; pus; and other discharge. (Note: a healthily healing wound may also produce some translucent-ish discharge. However, if the discharge is very yellow or very opaque, it’s time to see a doctor.)
2.5. One type of infection of the dermis or hypodermis is called cellulitis, and is a Very Bad Thing. As in medical emergency bad. As in will-spread-very-quickly-and-potentially-become-extremely-dangerous bad. Cellulitis usually looks like a red area (with soft borders), and tends to be painful to touch. Cellulitis can turn up anywhere on your body, but is most common on the legs.
2.75. If you have a fever with ANY of the aforementioned symptoms, go straight to hospital. Fever, in this context, tends to signal infection.
3. It’s better to kill an infection before it starts than to wait for symptoms. Wound care is best when it’s preventative. Wash your wounds - yes, even if they’re small - with water + soap, then use a topical antiseptic, such as povidine-iodine or chlorhexidine (that’s bepanthen). You can either get a dropper and drop it directly onto the wound, or get some gauze and swab it on yourself. Generally, covering this with a bandaid is a good idea, as it’ll stop stuff getting into the wound. If it’s relatively shallow, maybe you can get away with leaving it uncovered, but I’d err on the side of caution.
3.5. Do not put rubbing alcohol directly on your wounds - it’ll irritate the skin. However, if you are currently self-harming and seeking to minimise harm, rubbing alcohol can be used to clean any tools. (Clean before AND after, people!)
4. Some antiseptics and antibiotics are provided as creams or ointments. The difference between these is basically how much water they have in ‘em. Creams have more water, so rub into the skin. Ointments have less water, and sit on the wound instead of being rubbed into it. Don’t attempt to rub the ointment in and spread it thin as a result. You can be generous with ointment. Ointment is great, but will stain your clothes - so, it can help to cover it up with a dressing of some kind.
5. Wound dressings are anything you can put on the wound to stop stuff getting in. Wounds will heal faster if you cover them up - no, taking off the bandaid to ‘air it out’ will not, in fact, accelerate healing. Wound dressing options include (but are not limited to): bandages (good for when you need to apply pressure, which is to say anything deep); plasters (good for convenience); gauze + medical tape (more breathable, though I’m not sure of the benefits here). Change wound dressings at least once a day (unless otherwise instructed).
6. Bandaids and medical tape will leave adhesive on your skin. Wash it off with soap and water - otherwise, the sticky stuff builds up, and if you’ve got skin sensitivities, they might get flared up. If wound dressings are causing you continual flare-ups even when you wash the adhesive off, consider using a wound-prep wipe before dressing the wound (but consult with your doctor if it’s infected - I do not know the protocol here). And, for that matter, consult with your doctor anyway if you’re reacting to wound dressings - you might wanna get that checked out.
7. Your dermis contains some blood vessels, nerve endings, and hair follicles. If you hit a blood vessel, it will bleed a lot. So, if you see considerable bleeding:
If it is bright red and it spurts in time with your pulse, this is probably an artery. GO TO HOSPITAL IF YOU SEE THIS KIND OF BLEEDING. IT IS AN EMERGENCY.
If the bleeding is darker but more constant, you’ve probably hit a vein. If this doesn’t stop bleeding in 10 minutes, go to hospital. Put pressure on it in the meantime.
For the record, veins and arteries are not, in fact, bright red and bright blue like they are in textbooks. You will not know that you’re about to hit one until you do. Nerves are similarly difficult to see, but if an injury hits a nerve, it’ll be painful - either it’ll have an electric quality, a burning sensation, or it’ll sting like buggery.
8. The hypodermis contains: more nerves and blood vessels, as well as subcutaneous fat. Fat looks yellow and, uh, bean-like. If you see fat, it’s time to go to urgent care.
8.5. If you go below the hypodermis, go to A&E. I don’t care if it’s small - NOW.
9. Deep wounds may gape - that’s to say that they look, well, open. These wounds will heal quicker if you try to hold them closed to bring the skin walls together - that’s to say that steri-strips and butterfly bandages are your friend. Bear in mind that gaping wounds tend to be deep, so consider getting the wound looked at by a professional before trying to hold it closed at home.
Generally, after 48 hours, it’s unlikely that you’ll be given stitches, even if the wound was deep enough that it ought to have been stitched (that is: hypodermis or deeper). So, if it looks like it’s gonna need stitches (gaping or deep), go get stitches sooner rather than later. A good doctor or nurse will not judge you for whatever reason you’re seeking help.
10. Some skin areas are more prone to infection than others. (See: moist areas; legs; groin/lower abdomen.)
11. Don’t clean your wounds with tissue, paper towel, or toilet paper, as the materials tend to break up, and can leave a fun residue in the wound. Gauze swatches, cotton buds, and clean towels are your friend here.
12. Don’t put makeup on open wounds.
13. For deep wounds: in my experience with dermatillomania, these don’t tend to look like they fill in layer-by-layer so much as they just shrink/thin out. If it looks like it’s filling in in layers/healing slowly or healing in a way that’s incomplete, it’s time to see your doctor. For shallow wounds: if it darkens/goes yellow as it fills in, rather than scabbing, it’s time to see your doctor.
14. If you’re given a course of oral antibiotics, you need to finish the whole damn pack. Yes, even if you seem to have gotten better. Not finishing your dose, unless you’re specifically medically instructed to, may lead to the infection returning. Do not take that risk.
15. If antibiotics seem to be failing to clear things up, it’s time to see a doctor. Many funky things could be at play, but it’s not something you wanna take a risk on.
16. Check when you last had a tetanus shot. If you’re not sure, or if it’s since expired, get another tetanus shot.
6 notes
·
View notes
Text

Chapter 4: Medical Esthetic Procedure Contraindications

So you’re considering getting some medical esthetic procedures done. That’s hot! But before you schedule an appointment or consultation here’s a quick guide of contraindications to be aware of!!

What is a Contraindication?
A contraindication is a condition we look for in the medical field that serves as a reason to not continue forward with a medical treatment due to potential harm the treatment may cause to a patient!
Laser Hair Removal:


Herpes and Cold Sores: Can you get laser hair removal with herpes or cold sores? Yes! But only if there is not an active breakout. We do warn the clients that the lasers we use are powerful enough to cause a herpes or cold sore breakout to occur so please proceed with caution!
Retinol: Use of Retinol’s are a huge no no! It can cause severe damage, burning or scaring if a laser is used! If you are on Retinol please stay off of it for 1 week before your laser hair removal procedure.
Seizures + Epilepsy: If you have a history of epilepsy please refrain from getting any laser or light treatment as it can induce seizures.
Bacterial Skin Infections: Infections can spread to other parts of the body if a laser is used.
Impetigo: This highly contagious superficial skin infection is something we as your medical esthetician should be aware of before continuing with treatment.
Cellulitis: This infection of the dermis and subcutaneous tissue should be cleared before you continue with any laser or light therapy.
Folliculitis: Laser treatments are not performed in areas of folliculitis but several hair removal lasers have been approved by the FDA for pseudofolliculitis barbae treatment.
Fungal Infections: Ringworm and Yeast Infections can not be treated with laser or light therapy until cleared.
Viral Infections: Active viruses are considered major contraindications for laser and light therapy.
Shingles: If there is an active outbreak laser treatment will not be used.
Common Skin Warts (HPV): Although some lasers are used to remove persistent warts, they are still considered contraindications.
Atopic Dermatitis (Eczema): You will not be disqualified as a candidate for laser treatment, unless the outbreak is in an area of proposed treatment.
Open Lesions, Rashes and Sunburns: This includes open lesions from picking at the skin. Any unknown lesions or rashes will be considered contraindications. Sunburns are known to disrupt the skin barrier and are considered contraindications. Any suspicious lesions should always be evaluated by a physician prior to treatment.
Accutane: You must be off of Accutane for at least six months to a year, depending on a physician’s  preference prior to treatment with laser or light therapy.
Immediate Post-Operative Face Lift, Blepharoplasty or Neck Lift: Treatment is avoided for clients who are in post op from these treatments until a physician has given approval for laser or light treatment. 
Pregnancy and Lactation: Pregnancy and lactation are considered contraindications women who are pregnant or lactating, should wait after pregnancy + breastfeeding so a child will not be exposed before beginning or continuing laser or light treatment. 
Laser Tattoo Removal:


Laser tattoo removal shares the same contraindications as laser hair removal.
Red Tattoo Ink: Red tattoo ink is known to be allergenic. If you have experienced an allergic reaction to red tattoo ink, be aware that another allergic reaction may occur if a red ink tattoo is being removed by laser. 
Retinol + Accutane
Pregnancy and Lactation
Bacterial Infections
Viral Infections
Fungal Infections
History of Epilepsy or Seizures
Open Skin Lesions, Sunburns and Rashes
Microneedling:


Herpes + Coldsores: Please wait until an outbreak is fully healed! Estheticians can avoid microneedling the mouth area if you do have an outbreak but it is best to wait until the outbreak is fully healed to avoid any spreading.
Active Acne: Areas of active acne can be skipped over but if there is an all over outbreak it is best to wait.
Rosacea: Clients with vascular rosacea can receive treatment, but not pustular or nodular rosacea wait until the information has settled.
Atopy, Asthma, Hay Fever and Allergies: Any patient with a history of allergies maybe prone to urticaria, after needling due to the release of histamines.
Anticoagulants: Any supplements, known to prolong, bleeding time, may not necessarily be discontinued from treatment, but the risk of bruising increases.
Drugs and Supplements Associated with Photosensitivity: Any drug and supplement that can cause photosensitivity including Accutane is considered a contraindication. 
Fitzpatrick III and Above: Those with darker skin tones are not disqualified from treatment but it should be known that skin will appear puffy, bruising, if present might be visible in thin skinned areas and erythema (skin redness)  when super-imposed on brown, appears much darker. Patience with melasma or post. Inflammatory hyperpigmentation must understand that lesions will appear darker for several months before improving.
PSA: There are certain ingredients to avoid using when it comes to dermal needling. Ingredients to avoid include preservatives, fragrances, emulsifiers, emollient acids, dyes, coloring agents, and UV filters 
Before receiving a dermal needling treatment, you may be asked by your provider about allergy or medication, history, blood pressure/medication, bleeding disorders, eczema, psoriasis, immune system disorders, keloid, scarring, major illnesses, heart conditions, anemia and a lot of other general medical questions.
Body Contouring


Pregnancy and Breast-Feeding
HIV/AIDS
All forms of Cancer
Undergoing Chemotherapy
Immunodeficiency
Lupus
High Blood Pressure
Uncontrolled Diabetes
Keloid Scarring
Excessive Pigmentation
Vein Inflammation
Steroid Medication
Chemical Peels + Laser Resurfacing
Sunburn
Recent Surgery or Scars: Wait 6 months
Open Lesions, Skin Diseases, Inflammation, Varicose Veins, Infection, Metal Implants, Metal Screws, Metal Contraceptive Coil + Prothesis/Silicone Implants: Area will be avoided
Antibiotics: Must wait until completed medication course
Depilatory Creams: Wait 2 weeks
IPL or Laser Treatment: Area that received laser or light therapy must wait 2 weeks before receiving body contouring.
Areas with Botox: Wait 3 months before receiving body contouring.
Areas with Dermal Filler: Wait 2 weeks before receiving body contouring.
Sun Tan: Will be avoided
Chronic Inflammation: Speak with your healthcare provider before proceeding forward with a body contouring treatment.
PSA: Before receiving body contouring, your hydration levels will be checked your body must be 40% or higher for your hydration level. Hydration levels below 40% can cause cat like scratch sensations when receiving body contouring. Which is why low levels of hydration are considered a contraindication and you must wait until your hydration levels are at 40% before receiving treatment.

29 notes
·
View notes
Photo

Looking for a simple way to gift yourself with some self-care? These lavender and cocoa butter bath melts will leave your skin feeling silky smooth while also providing you with aromatherapy benefits. Double a batch and gift some to a friend so they can enjoy these, too! Add a little luxury to the bath with these moisturizing cocoa butter bath melts. They are made with ingredients so natural that you could eat them, and you might just want to! The aroma of cocoa, coconut, and lavender makes my mouth water for what is essentially a gourmet truffle. These truffles, however, are best used in the bath, as the silky soft oils melt in the warm water and soak into your skin, leaving it moisturized and soft. It’s quite easy to make a batch of bath melts, and it only requires a few key ingredients. So let me show you how! These bath melts are scented with lavender and feature dried lavender buds as a topper. What are Bath Melts? After a long day, I like to take some time for myself and give my body a break. A bath is a time for self-love and relaxation, soothing aching and tired muscles. I never have one without adding a little bit of something extra. I have found myself reaching for bath melts more in the winter months as my skin gets dry. Bath melts are a luxurious way to moisturize skin and keep it soft. Made of moisturizing body butters, you pop one in the bath and watch them melt into the water. Then, your skin soaks up the oils from the butters and softens, allowing you to sit and relax in the aromatherapy provided by lavender. I like to use a bath melt when I think my skin needs some extra love and attention. For dry and overworked skin, you can skip taking the time to lotion up your body after the bath. You get two for one with a bath melt! Bath melts are very moisturizing, so you don’t need to add extra lotion after the bath. Why Cocoa Butter is Your Skin’s Best Friend Cocoa butter is the edible fat extracted from the cocoa bean and the main ingredient in chocolate. In fact, the flavour and aroma of chocolate come from cocoa butter, and true chocolate can only be called by that name if it contains 100% rich, smooth cocoa butter. While used to make tasty desserts, cocoa butter is also a prominent ingredient in skin care. It is also full of antioxidants and is so good at moisturizing skin that it is very often used in skincare products. High in fatty acids, it helps to nourish the skin and improve elasticity. The fats create a protective barrier over the skin, helping to really lock in that moisture. Some people have also used cocoa butter to help smooth scars, wrinkles, and stretch marks. When my skin is feeling dry, these bath melts are the first thing I reach for. At room temperature, it is solid, but as you add it to a hot bath, it melts, and the oil disperses into the water and absorbs into your skin while you soak. Cocoa butter is the prime ingredient in these bath melts. What About the Lavender and Coconut Oil? The other half of the moisturizing duo of these bath melts is coconut oil! Coconut oil is made by extracting oil from raw coconuts or coconut kernels. Super rich in saturated fats, it is known to help improve dry skin’s overall moisture content and can help reduce eczema symptoms. The fatty acids also have antimicrobial properties, which makes them safe for skin infections like athlete’s foot, acne, cellulitis, and other bacterial infections. While super moisturizing, there are also some aromatherapy benefits to these bath melts as well. Lavender has always been a favourite with me when it comes to bath time. It is the perfect relaxation herb, promoting calmness, easing stress, and providing anxiety relief. If you like to bathe before bed, lavender has always worked as a wonderful way to ease me into a sleepy mood. All together, cocoa butter, coconut oil, and lavender create the perfect combination for a relaxing hydrating bath melt. Coconut oil is a safe oil to use on most skin types. How to Make Bath Melts If you are looking for a way to inject a little more self-care into your routine or know of someone who could use some pampering, then make up a batch of these luxurious bath melts and turn a hot bath into a heavenly treat. Materials See recipe card below for exact measurements. Jump to Recipe Make It! Melt the oils in the small pot over medium-low heat. Stir constantly and keep a watchful eye on the oils. You want them to just reach the melting point and not overheat. When the oils have melted and combined, add the essential oils and stir well. I like to make small batch items in my Turkish coffee pot, as it makes pouring out the liquid into the mold easier. Immediately pour into silicone molds. I used a silicone ice cube tray, but a candy mold will also work. A small pot with a pour spout makes this job a lot easier. I use this Turkish coffee pot for all of my natural skincare recipes because it is small but tall, has a long handle to keep your hands away from hot oils, and has a spout that makes pouring much easier. Ensure your mold is clean and dry before pouring your heated oil. Sprinkle dried lavender buds on top of the hot oil, dividing the tablespoon up evenly between the bath melts. Use dried lavender buds, not fresh ones. Move the silicone mold to the refrigerator to cool for two hours, and you’re done. Store the finished bath melts in the fridge or a cool place if your house is warm so that they don’t melt before you want to use them! Once fully cooled, bath melts can be removed from the mold. Pop one or two bath melts into a tub filled with hot water and soak for at least twenty minutes. A word of caution: the oils will make your bathtub slippery after you drain it. Be careful when stepping out of the tub. After your soak, be sure to give it a quick clean and wipe so it’s safe and ready to go for the next person. Bath Melt FAQ Can you store bath melts in the freezer? You bet! I like to store mine in the fridge, but you can also store them in the freezer. How do you keep your lavender buds from turning brown? Lavender will often turn gray or brown when it dries. To prevent this, you want to make sure you’re harvesting the lavender at the right time; harvest before the buds flower, not once they’ve finished flowering. It’s also important to limit the dried buds’ exposure to sunlight, so store them in a dark cupboard or drawer. Finally, choose lavender varieties that are known to hold their colour, such as Purple Bouquet and Royal Purple. Can you use shea butter instead of cocoa butter for bath melts? You can try, but I have found that cocoa butter works best. It has a much nicer scent, has a better melting point, and feels lovely on the skin after a bath. Shea butter is heavier, stickier, and better applied directly to the skin. For many, many more natural skincare recipes and gift ideas, check out The Natural Beauty Recipe Book! More Skincare Recipes You’ll Love Lavender and Cocoa Butter Bath Melts Moisturize your skin with luxurious cocoa butter and soak in the aromatherapy of calming lavender during your next bath. This recipe makes 12 bath melts. Melt the oils in the small pot over medium low heat. Stir constantly and keep a watchful eye on the oils. You want them to just reach the melting point and not overheat.When the oils have melted and combined, add the essential oils and stir well.Immediately pour into silicone molds. I used a silicone ice cube tray but a candy mold will also work. A small pot with a pour spout makes this job a lot easier. I use a Turkish coffee pot.Sprinkle dried lavender buds on top of the hot oil, dividing the tablespoon up evenly between the bath melts.Move the silicone mold to the refrigerator to cool for two hours, and you’re done. Store the finished bath melts in the fridge or a cool place if your house is warm so that they don’t melt before you want to use them!Pop one or two bath melts into a tub filled with hot water and soak for at least twenty minutes.The oils will make your bathtub slippery after you drain it. Be careful when stepping out of the tub. After your soak, be sure to give it a quick clean and wipe so it's safe and ready to go for the next person. Source link
#OUTDOOR_LIGHTING#BATH#BUTTER#COCOA#HANDMADE_HOLIDAY_GIFTS#LAVENDER#MELTS#MONTH_JANUARY_WEEK_3#MOTHERS_DAY#NATURAL_BEAUTY#NATURAL_SKINCARE_SERIES#SKIN#SOFT#ULTIMATE#VALENTINES_DAY
2 notes
·
View notes
Text
//
..... think I'm gonna call out for tomorrow's midshift. I already am not feeling great with this evening's closing. Sensory issues are a thing, too, which always seems to be the case when my body is under more strain than usual.
Plus, my boss and supervisor are already aware that I have cellulitis and a skin infection, so it's not like they won't believe me
4 notes
·
View notes
Text
Medical School Journey
Meeting with my advisors, talking about boards 😱
Group study in arthritic diseases and skin/subcut infections 😰
Grabbed sushi for lunch 🍣
Practiced back pain physical therapy 🩻
Legit knocked out without taking my scrubs off when I came home 😴
Woke up to meal prep and make banana bread 🍌
Did chores- mopped, dishes, laundry, dust, scrub kitchen 🧼
Did some flashcards on musculoskeletal disease 💪🦴
Reviewed
Rheumatoid, psoriatic, reactive, osteo and septic arthritis, common derm conditions, cellulitis, fasciitis, gangrene, osteoporosis and osteopetrosis
#plsiamsotired#self improvement#growth#mindset#journal#med student#studyblr#medical school#med studyblr#med school#academia#dark academia
3 notes
·
View notes
Text
11 Skin Conditions You’ve Almost Certainly Never Heard Of

Millions of people in India suffer from at least one skin condition. You’ve probably heard of the more common ones, such as acne, eczema, and rosacea. In fact, there’s a strong possibility you have one yourself.
There are also a number of uncommon skin problems that you may be unaware of. They can range in severity from minor to fatal. They can have an impact on the quality of life of persons who develop them in some situations.
Continue reading for an overview of some of these lesser-known conditions.
Hidradenitis suppurativa
Hidradenitis suppurativa (HS) is a chronic inflammatory disorder that causes lesions to grow on skin-to-skin contact points on the body. The following are the most prevalent locations for breakouts:
underarms, groin, buttocks, upper thighs, and breasts
Although the etiology of HS is uncertain, hormones are likely to play a role in its development because it often begins around puberty.
The illness affects up to 2% of the population. It is especially common in those who are obese or who smoke. Women are more than three times as likely than men to have HS.
Genetics and the immune system are thought to play a role in who gets the condition.
DID YOU KNOW?
People who have hidradenitis suppurativa are more likely to have specific conditions (or comorbidities), such as:
inflammatory bowel disease (IBD) acne
Acne conglobata, dissecting cellulitis of the scalp, and pilonidal sinus disease are all part of the follicular occlusion tetrad (a collection of inflammatory skin disorders).
metabolic disorder
PCOS (polycystic ovarian syndrome)
Type 2 diabetes with squamous cell carcinoma of the afflicted skin
The first signs of HS are outbreaks that resemble pimples or boils. These outbreaks could remain on the skin or fade and recur.
If neglected, more severe symptoms like scarring, infection, and breakouts that rupture and produce a foul-smelling fluid might develop.
There is presently no cure for HS, however there are several therapy options to assist control symptoms. These are some examples:
topical ointments, anti-inflammatory medications, injectable biologics, and hormone therapy
In more severe situations, surgery may be recommended.
Psoriasis inversa
Intertriginous psoriasis is another name for inverse psoriasis. This illness, like HS, causes red sores on regions of the body where skin touches skin. These lesions do not resemble boils. They appear smooth and gleaming.
Many persons who have inverse psoriasis have at least one other type of psoriasis on their body. Experts aren’t clear what causes psoriasis, but genetics and the immune system both play a role.
Psoriasis affects roughly 3% of the world’s population, and 3–7% of those with psoriasis have inverse psoriasis.
Because the skin in high-friction parts of the body is sensitive, treating the condition can be challenging. Steroid creams and topical ointments can be beneficial, but they can also cause unpleasant irritation if used excessively.
People with more severe inverse psoriasis may also require UVB light therapy or injectable biologics to manage their illness.
Harlequin ichthyosis
Harlequin ichthyosis is an uncommon genetic condition that causes children to be born with rough, thick skin covered in diamond-shaped scales.
These plates, which are separated by deep fissures, can shape their eyelids, mouth, nose, and ears. They can also impede limb and chest movement.
Around 200 instances have been recorded around the world. The disorder is caused by a mutation in the ABCA12 gene, which permits the body to produce a protein required for normal skin cell formation.
The mutation hinders lipid transfer to the skin’s top layer, resulting in the scale-like plates. Because of the plates, it is more difficult to:
control water loss
combat illness by regulating body temperature
Harlequin ichthyosis is an autosomal recessive condition caused by faulty genes inherited from both parents.
Because biological carriers rarely show symptoms, genetic testing can detect changes in genes and calculate your risk of developing or passing on genetic illnesses.
A stringent regimen of skin-softening emollients and skin-repairing moisturizers is the most popular treatment for harlequin ichthyosis. Oral retinoids may also be utilized in extreme situations.
Morgellons syndrome
Morgellons disease is an uncommon ailment that causes microscopic fibers and particles to emerge from skin wounds, giving the impression that something is crawling on the skin.
The Morgellons Disease is poorly understood, although it affects nearly 14,000 families, according to the Morgellons Research Foundation.
Morgellons disease is most common in middle-aged Caucasian women. It’s also closely linked to Lyme disease.
Because the symptoms are similar to those of a mental health illness known as delusional infestation, some experts assume it is a psychological issue.
The symptoms are unpleasant but not life-threatening. Typical symptoms include:
weariness anxiety sadness itchy skin rashes or sores black fibrous substance in and on the skin
Lesions only affect one part of the body: the head, trunk, or extremities.
There is no standard treatment option for Morgellons disease because it is still poorly understood.
People suffering with the disease are usually encouraged to maintain close contact with their healthcare team and seek therapy for symptoms such as anxiety and depression.
Elastoderma
Elastoderma is an uncommon disorder characterized by increased skin looseness in particular parts of the body. As a result, the skin sags or hangs down in loose folds.
It can affect any region of the body, but the neck and extremities, particularly the elbows and knees, are the most usually afflicted.
The illness affects less than one in one million persons worldwide. Elastoderma’s actual cause is unknown. It is assumed to be caused by an excess of elastin, a protein that provides structural support to organs and tissues.
Elastoderma has no cure or recommended treatment. Some people will have surgery to remove the problematic area, although the loose skin often returns after the procedure.
Pilonidal sinusitis
Pilonidal sinus illness causes small holes or tunnels at the buttocks’ base or crease. Because symptoms aren’t always clear, most people don’t seek therapy or even recognize the issue until it causes problems.
It is caused when the hair between the buttocks rubs together. The friction and pressure that results pushes the hair inside, causing it to become ingrown.
This minor illness affects 10 to 26 people in every 100,000. The majority of people with this illness are between the ages of 15 and 30, and men are twice as likely as women to have it.
It frequently affects persons who work occupations that demand long periods of sitting. It is often associated with hidradenitis suppurativa (HS).
A few things influence treatment for an infected pilonidal sinus:
signs and symptoms
the size of the abscess, if it is a new or recurring infection
In most cases, treatment entails removing any visible pus from the affected pilonidal sinus. Antibiotics, hot compresses, and topical ointments are also frequently utilized.
If you’re one of the 40% of people with the illness who has reoccurring abscesses, talk to your doctor about other surgical alternatives.
Pemphigus vegetans
Pemphigus is classified as an autoimmune illness by the National Institutes of Health (NIH)Trusted Source. It causes your immune system to target healthy epidermal cells. The epidermis is the top layer of the skin.
Lesions or blisters form where skin naturally meets or rubs together, as in HS. They can also be found in or on the:
mouth, throat, eyes, nose, and genital areas
Pemphigus vulgaris is the most common kind of pemphigus. It affects 0.1 to 2.7 persons in every 100,000.
Pemphigus vegetans, a pemphigus vulgaris variation, accounts for 1 to 2% of pemphigus cases globally.
If untreated, Pemphigus vegetans can be lethal. The treatment focuses on removing the lesions or blisters and preventing them from recurring.
Corticosteroids and other anti-inflammatory steroids are frequently used as the first line of defense. In addition, you can have surgery to remove the lesions or blisters, while also cleaning and dressing the affected area on a daily basis.
Medicated mouthwash or clobetasol, a corticosteroid and ointment used to treat oral problems, are examples of mouth and throat remedies.
Crohn’s disease
Crohn’s disease is an inflammatory bowel disease (IBD) of the digestive tract.
It affects around 780,000 Indians. Every year, approximately 38,000 new cases are reported. Researchers believe that genetics, the immune system, and the environment all have a role in Crohn’s disease development.
Between 20 and 33 percent of persons with Crohn’s disease have skin lesions as a result of the condition. This is referred to as a cutaneous epidemic.
Cutaneous lesions, which resemble genital warts, appear after bowel disease has shown on the skin or another organ outside of the intestinal tract. The eyes, liver, and gallbladder are all included. It might also have an impact on the joints.
If your Crohn’s disease and lesions have metastasized, or spread, they can become painful and potentially lethal. There are currently few therapy options for this stage.
Sneddon-Wilkinson syndrome
Sneddon-Wilkinson illness is characterized by clusters of pus sores on the skin. Subcorneal pustular dermatosis (SPD) is another name for it.
Experts are unsure what is causing it. The disease, which is uncommon and sometimes misunderstood, primarily affects persons over the age of 40, particularly women. As a result, its precise prevalence is uncertain.
Soft, pus-filled pimples occur between skin that rubs together a lot, just like in HS. Skin lesions appear on the body, between skin folds, and in the vaginal area. They “explode” as a result of friction.
This popping of the lesions may be accompanied by an itchy or burning feeling. These feelings are followed by scaling and discolouration of the skin. Despite being chronic and painful, this skin ailment is not lethal.
The antibiotic dapsone is the preferred treatment for this condition, with a daily dose of 50 to 200 milligrams (mg) taken orally.
Lichen planus
Inverse lichen planus pigmentosus is an inflammatory disorder that causes skin fold discolouration and uncomfortable pimples.
Only about 20 cases have been documented worldwide, mostly affecting Asians. Nobody knows what is causing it.
Small clusters of flat lesions, or macules, of discolored skin appear. They don’t normally contain pus, but they do occasionally. Some people’s skin spontaneously clears up with time, whilst others may experience symptoms for years.
This is a mild condition that can be addressed with a topical treatment. Corticosteroids are the most often used treatments for wound healing and can even aid with pigmentation in some situations.
Dowling-Degos syndrome
Dowling-Degos disease is a hereditary illness that causes darker skin, especially in folds such as the armpit, groin, and joint areas.
Pigment changes can also affect the neck, hands, cheeks, and scalp, albeit they are less prevalent.
The majority of the lesions are minor and resemble blackheads, however red areas resembling acne might form around the lips.
Lesions on the scalp might also look as fluid-filled lumps. Itching and burning sensations are possible.
Skin changes, like HS, occur in late childhood or early adolescence.
However, some people do not have breakouts until they reach maturity. Dowling-Degos is not a life-threatening disease, but it can cause distress and worry in those who have it.
This disease presently has no cure. Treatments ranging from laser therapy to topical steroids to retinoids have been tried, but results have been mixed, and nothing has proven to be consistently successful.
Takeaway
If you have a skin issue, pay attention to your body and treat any signs seriously.
Consult your doctor who can assist you in obtaining a diagnosis and determining the best treatment options for your specific problems.
2 notes
·
View notes