#Cardiac surgical procedures
Explore tagged Tumblr posts
Text
Things to Keep in Mind While Choosing the Right Cardiac Surgeon

There is nothing more worrisome than discovering you have a heart issue. It's no secret that acting promptly is crucial, especially with cardiac problems that can quickly become serious. Fortunately, today, advanced technology and expert cardiologists make high-quality cardiac care easily accessible when it's most needed.
However, according to cardiac specialists at United Hospital, recognized as the Best Cardiology Hospital in Bangalore, say that finding the right cardiac surgeon for you is quite a challenge
Here are some important factors you can keep in mind.
Choosing the Best Cardiac Surgeon
According to Bangalore’s Best Cardiologist operating at United Hospital, the skill sets Of your operating surgeon play a huge role especially when complicated cardiac surgeries are to be performed. Therefore, it's crucial to choose your cardiac surgeon wisely.
ReferralsSeeking recommendations from your friends, family and other healthcare professionals can be very useful while searching for a professional cardiac surgeon. Though you have a reference, assess your surgeon by communicating with him freely.
Review his credentialsAs the patient in question, you have every right to study your cardiac surgeon’s credentials with respect to his qualifications and certifications. It is a good choice to connect with hospitals whom your surgeon is associated with and study his records.
Consider the Surgeon’s experienceSuccess percentages of the surgeon are of paramount importance when deciding on engaging a cardiac surgeon. The more experience with a particular condition or procedure a cardiac surgeon has, the better your results are likely to be. If possible, get in touch with patients whom the surgeon in question has treated to understand his approach.
Research Hospital QualityChoose a hospital which has all the advanced surgical facilities and more importantly, rehabilitation facilities as the duration of your hospital stay after surgery depends upon how quickly you respond to treatment post-surgery. Hence, choose a hospital which has a good track record for cardiac care as well as convenient to travel for frequent checkups.
CommunicationCommunication Skills and Confidence levels of your surgeon are equally important. It is good to engage a surgeon who can communicate freely and instil confidence in you especially if the surgery is tricky and communicated. At the same time, he should be able to understand if you have any budget constraints and suggest the best possible approach which does not deprive you of quality treatment.
Cardiac surgeries can be stressful for patients and their loved ones. Therefore, choosing a hospital and surgeon who makes you feel comfortable from the beginning is essential. If you're seeking a Good Heart Hospital in Bangalore with an experienced cardiac team, consider reaching out to United Hospital.
#cardiology hospital near me#Bangalore best cardiologist#heart specialist hospital in Bangalore#best cardiology hospital in Bangalore#good heart hospital in Bangalore#best heart failure treatment hospitals in Bangalore#Cardiac surgeon#Cardiothoracic surgeon#Cardiac surgical procedures#Minimally invasive heart surgery#Coronary artery bypass graft (CABG)#Valve replacement surgery#Congenital heart defect surgery#Cardiac transplant surgeon#Cardiac care specialist#Cardiac surgery recovery
0 notes
Text
Choosing the Right Sternum Saw: Key Features and Best Practices for Surgeons

Selecting the right sternum saw is crucial for ensuring successful surgical outcomes, particularly in complex cardiac and thoracic surgeries. As the largest and most trusted manufacturer, supplier, and exporter of sternum saws worldwide, Mercury Healthcare is at the forefront of innovation, providing high-quality surgical tools that meet the needs of modern healthcare professionals. In this article, we explore the key features surgeons should consider when choosing a sternum saw and why Mercury Healthcare is the preferred choice for healthcare providers globally.
Key Features to Look for in a Sternum Saw
Precision and Control In critical surgeries, precise cutting is essential to minimize trauma and ensure patient safety. A sternum saw must offer excellent control, allowing surgeons to perform procedures with accuracy. Mercury Healthcare's S1 Sternum Saw is designed with a clear line of sight and lightweight construction, providing surgeons with exceptional control during surgeries. The precision of our saws ensures efficient cutting, reducing the risk of complications and enhancing patient recovery times.
Ergonomics and Lightweight Design Long surgical procedures can be physically demanding for surgeons. A well-designed sternum saw should be lightweight and ergonomically crafted to reduce hand fatigue and allow surgeons to operate comfortably for extended periods. Mercury Healthcare prioritizes surgeon comfort, and our sternum saws are built with a balanced, lightweight design that enhances both maneuverability and ease of use.
Sterilization Compatibility Fast and efficient sterilization is crucial in surgical settings to prevent infections. Our S1 Sternum Saw can be ETO sterilized or autoclaved, ensuring a quick turnaround between procedures. This feature is especially beneficial in busy operating rooms where time is critical, helping medical teams maintain optimal cleanliness without sacrificing efficiency.
Convenience and Safety Features Safety features are a must for any surgical instrument. Mercury Healthcare's sternum saws are equipped with quick-release blades and a patented retention system, making blade changes seamless and reducing downtime during operations. Additionally, the tapered blade protector helps deflect underlying tissues from contact with the blade, minimizing the risk of tissue damage during surgery. These features make our saws both convenient and safe, allowing surgeons to focus on what matters most — patient care.
Durability and Reliability A reliable sternum saw must withstand the demands of frequent use in high-stakes surgical environments. Mercury Healthcare's sternum saws are made from high-grade materials that ensure durability and longevity. Whether performing routine procedures or complex surgeries, our saws provide consistent performance, making them the trusted choice for surgeons worldwide.
Best Practices for Using a Sternum Saw
To maximize the performance of a sternum saw, surgeons should follow these best practices:
Regular Maintenance: Proper cleaning and maintenance after each use will ensure the saw's longevity and precision.
Blade Replacement: Always use sharp, sterile blades, and replace them as necessary to avoid unnecessary pressure on the sternum.
Operator Training: Surgeons and surgical teams should undergo proper training to ensure the correct and safe use of the sternum saw, reducing risks and improving surgical outcomes.
Why Choose Mercury Healthcare?
At Mercury Healthcare, we are committed to delivering high-quality, innovative surgical equipment that meets the demands of healthcare professionals around the globe. As the leading manufacturer and exporter of sternum saws, we combine cutting-edge technology with a deep understanding of surgical needs. Our focus on precision, safety, and reliability has earned us the trust of surgeons worldwide, making Mercury Healthcare the go-to provider for advanced medical tools.
Our sternum saws are not only built for superior performance but also designed with the future of healthcare in mind. As we continue to innovate and set new industry standards, we remain dedicated to improving patient outcomes and enhancing the surgical experience for healthcare providers.
#Best sternum saw for cardiac surgery#Top features of surgical sternum saws#How to choose the right sternum saw for surgeons#Benefits of lightweight sternum saw for surgery#Leading sternum saw manufacturer for cardiac procedures#High-precision sternum saw for thoracic surgery#Trusted sternum saw supplier for surgeons worldwide#Autoclavable sternum saw for safe surgeries#Best sternum saw for healthcare professionals#Most reliable sternum saw for surgical use#Ergonomic sternum saw for long surgeries#ETO sterilized sternum saw for quick turnaround#Sternum saw with quick-release blades#Durable sternum saw for frequent surgical use#Safe and reliable sternum saw for medical procedures
0 notes
Text
──── 𝑻𝒂𝒄𝒉𝒚𝒄𝒂𝒓𝒅𝒊𝒂


To see the well-versed, experienced cardiac surgeon in such a state of distress was a sight you were not keen to experience again, and even at the cost of your shared secret, you would do anything to soothe him and bring him down from the adrenaline high.

𝐏𝐀𝐈𝐑𝐈𝐍𝐆 ── Zayne x Scrub Nurse!F!Reader 𝐖𝐎𝐑𝐃 𝐂𝐎𝐔𝐍𝐓 ── 2.1k 𝐓𝐀𝐆𝐒 ── Smut, fluff, pet names, secret relationship, power imbalance, innappropriate use of an on-call room, Greyson is so sick of Zayne's shit ➺ Wall, public, desperate sex, creampie, praise, uniform, size kink 𝐁𝐄𝐓𝐀 ── @smutconnoisseur (my absolute saviour, thank you for buckling in with my utterly insane rambles) 𝐀𝐍𝐓𝐇𝐄𝐌𝐒 ── Keep It Down by Migrant Motel 𝐀𝐎𝟑 ── HERE 𝐀𝐔𝐓𝐇𝐎𝐑 𝐍𝐎𝐓𝐄 ── My first smut I have written in a year, oi vey.

─── 𝑳𝑨𝑫𝑺 𝑴𝒂𝒔𝒕𝒆𝒓𝒍𝒊𝒔𝒕 ───



The atmosphere was tense — not unlike any other time within the bustling halls of the surgery floor, but this time, the air was thick with apprehension, a dash of uncertainty for what laid behind the double doors of the operating room.
As though you could feel the gaze of those above in the observation window, you shivered from nerves beneath the countless layers you wore. The shirt you wore was form fitting, as all scrub wear was, but it felt somehow even tighter, closing in around your throat even with the deep-necked collar.
In front of you were the immovable and ever-focused figures of your superiors. Both were skilled surgeons and almost indistinguishable while gowned in endless layers, but one stood out in particular — he was straight-backed and intently homed in on the chest cavity of his patient while his deft fingers moved with purpose, going from scalpel to scissors, to thread and needles. The occasional, clear command of: “Suction,” came every few seconds to every minute.
“Doctor,” a voice spoke, clear and kind in tone.
“We’re almost finished–” Snip.
Footsteps shuffled around you as a few team members re-emerged in new places to better accommodate the final stages of surgery. This singular procedure had been in the pipeline for months, and naturally, they called upon the most skilled surgeon to undertake it, the chief of surgery himself, Zayne.
Few knew of the intimate relationship between the chief surgeon of Akso hospital and his dedicated scrub nurse — a secret you desperately hoped to maintain.
Time seemed to melt away in a haze of stolen glances and lingering touches, your history together blurring into an intoxicating mix of professional respect and burning desire. A shiver ran down your spine as Zayne declared the surgery complete, his commanding voice sending a familiar heat through your core.
He stepped back from the patient, his scrubs marked with evidence of his skilled work — crimson streaks and surgical fluids that somehow made him look even more imposing, more powerful.
“Sir,” you said quietly, outstretching your hands to meet him halfway. Your own gloved hands carefully pulled the soiled gloves from his hands to reveal the scrub cuffs of his shirt.
Zayne strode silently toward the sliding, pressurized door leading to the preparation room. A large metal basin gleamed under the harsh downlights. You watched with concern as he gripped its edge, his wrists shaking from strain.
The door slid shut with an ominous, loud click, leaving you alone with him in the preparation room.
Your heart raced as you stepped closer, closing the distance between you both. The fingers on your outstretched hand trembled slightly as you reached for the ties of his surgical gown, and the fabric rustled beneath your touch as you slowly undid the knots at his upper back, then lower, each movement deliberate and charged with tension.
The scrub gown fell away from his broad shoulders, and your breath caught at your proximity to him while you helped him shrug it off.
With quick, almost desperate movements, you discarded both his soiled gown and your own into the waste bin, the sudden lack of barriers between you making the air feel electric.
The metal of the basin began to creak under his grip, and his shoulders heaved slightly. “Zayne?” you whispered, resting a hand on the back of his bicep. “Are you all right?”
It happened in a whirl — one moment you were standing beside the trembling figure of your lover, and then, the next moment your feet scrambled to keep you upright against the sudden tug of Zayne’s hand gripping your elbow. “Wait, wait, Zay– What’s wrong?” The question sounded sharp to your ears, and he only huffed in reply.
His footsteps echoed harshly in the eerily deserted corridor outside of the surgery suite, and the sight seemed to bring his mind back into focus. “Come with me.”
“Where?” you rushed, still jogging to keep up with his long strides. The determined pull of his brow and set line of his lips stirred something deep within you, but you shoved that thought down with extreme force — you were at work, you scolded silently. “They– Won’t they need you back–?”
“No, Greyson will handle it.” His pace increased, as did the rustle of his slacks. The sound caught your attention, but before you could glance down to make sure he wasn’t leaving the OR suite with contaminated clothes, fingers gripped your chin and forced your face upwards.
You gulped, the flush of heat that coursed through you had nothing to do with nerves or exertion within the operating room. Deep, hazel eyes bore into your own, and his mouth opened around a few words that made your stomach swoop. “I need you.”
The outline of his face grew blurry, and you blinked. “I– Uh, okay, um–”
“Now.”
The force of his pull made a squeak of surprise slip past your tight lips, and you were tugged toward the closest on-call room. “But we’re at work–!”
“I don’t care,” Zayne grit out through clenched teeth. The door slammed open, and you rushed inside, him following right behind you. You noticed his grip was still trembling, the twitch of his arm far more noticeable now that his shirt left nothing to your imagination.
“But– Oh, shit, Zayne!” Your feet were lifted from the ground, and your hands carded through his hair to ground yourself. The sheer volume of your shout made a sense of fear tear through your middle; being caught in such a compromising situation with your superior would spell disaster. “Wait, wait, baby,” you begged, panting against his lips, but he was not deterred.
While one hand gripped the swell of your ass to keep you in the air, the other moved towards your neck. “No,” Zayne grunted, tilting your head back with his thumb beneath your chin. His lips trailed from your jaw to your collarbone and back up again. “The only way that I will wait,” he continued, his voice lowering into a husked rasp. “Is if you were to tell me you didn’t want this.”
“No, no I do, please–” The hand pushing your head back vanished, and you lowered your chin to capture his lips with yours — to tease him even further, you nibbled on his bottom lip and grinned as he groaned low in his throat, a silent curse escaping in a sigh.
“Be quiet for me then, darling.”
You giggled and shifted in his grip to help pull down the scrub pants you wore, and they fell to your ankles with ease. The sheer strength needed to make such a move made you swoon, a rush of light headedness forcing you to gasp for air. “How can you–?”
“I need you,” Zayne repeated in a low growl. “I need this—need to feel you.”
The pressure of his hand on your ass increased, and you felt the flutter of fabric against the back of your thigh, followed by the quiet clink of his belt. “Zayne, please,” you breathed, staring at him through half-lidded eyes. Fabric rustled as the waistband of his slacks shifted and fell to his hips.
"I know," he whispered. His fingers traced along your clothed cunt, drawing a soft gasp from your lips. A knowing smirk curved his mouth as he felt your arousal. "I can feel how much you want this, already so wet for me, my darling girl, hm? Who knew you were so eager."
The sudden sound of muffled footsteps made you both freeze, your attention now front and center on the fact you were currently half-way up the wall of an on-call room, legs wrapped around Zayne’s tense middle while he teased your clit with the pads of his fingers. Shocks of pleasure shot up your spine as he circled your clit with precision, and his other hand hastily closed your parted mouth. “Shh, keep quiet, darling. You don’t want them to know how well you take it, do you?”
“Shut up and kiss me,” you hissed, the words muffled by his palm.
Zayne chuckled and stepped closer, the tip of his cock pressing against your clit. “Easy, darling,” he cooed, finally moving his hand away from your mouth. "Open up for me, sweetheart," Zayne murmured, his breath warm against your ear. "Let yourself feel everything–” The push of his cock made your eyes squeeze shut. “Yes, just like that, perfect."
A hitched whine caught in your throat as the pressure grew. “Ha– Oh, my god.” Your forehead fell to his shoulder, and your hands moved from his hair to his broad shoulders. “Don’t– Don’t you dare stop–”
“I don’t plan to, but you have to let me in, baby,” Zayne rasped, his breath hot over the shell of your ear. “You can do it—be a good girl for me.”
Shuddering with the onslaught of sensation, you took a deep breath. The gentle coaxes and praise from Zayne made it easier to breathe, and after several, slow inhales, you nodded slightly. “M’kay.”
A soft brush of Zayne’s lips against your temples made you smile dazedly, and you moaned softly as you felt him withdraw, then gasped at the delicious pressure as he pushed back in. “You must’a been all pent up,” you breathed.
“You have no idea,” he grunted, and then you felt his resolve snap.
The pitch of your moans increased as Zayne lost himself in you, the slide of the plaster wall while the force of his thrusts kept moving you up the wall behind you pulled at your shirt and exposed your lower stomach — the feeling of his own shirt against the strip of bare skin only made the intensity of your pleasure burn hotter. “Za– Ohmygod, you feel–”
“How you can be so tight, baby,” he growled, his forehead now resting against your sternum. “I can’t last– Fuck, I can’t.”
The outward curse made you gasp, your heart raced to keep up with the rush of pleasure he gave you. “Give it to me, please—I need it, Zayne, ohgod–”
“You’ll have it.”
Your scrub shirt rustled and you squeaked as you were pulled back down the wall, now eye to eye with him. “I want to watch you, see how pretty my darling is when she loses herself over my cock.”
“Don’t–”
“Don’t what?” The few strands of hair that brushed against the very top of his glasses now stuck to his forehead. “I cannot help but be greedy for what’s mine.”
“Oh– Zayne, Zayne,” you chanted, the sudden burn all consuming as the coil in your stomach grew unbearably taut. “Please, ‘m so close, please!”
The sounds and mewls of pleasure that fell from your parted lips were silenced by his own, a kiss that was all teeth and tongue — the feeling of being consumed from the inside out by him blurred your vision around the edges with its intensity.
“Give it to me, baby. Give it all to me, come on,” he coaxed, voice rough against your lips, and his harsh pants for air only added to the litany of sensations. “Come apart for me, that’s it–”
“Zayne!”
Waves of pleasure crashed over you as your senses overloaded — blood rushed in your ears, your thighs trembled uncontrollably against his sides, and your toes curled in your shoes. Your fingers desperately sought anchor; one hand gripped his broad shoulder while the other tangled in his hair, pulling him closer as ecstasy consumed you completely.
“Fuck, oh god, fuck,” Zayne groaned deeply, his hips stuttering to a stop as your walls clenched around him. “I’m going to–” His words cut off with a guttural moan as he came, flooding you with warmth that triggered another wave of pleasure through your oversensitive body. Each subtle movement of his cock inside you drew out more delicious aftershocks.
“Please,” you hoarsely begged, putting your arms around his shoulders to pull him closer. He moaned in reply and tucked his face into your neck, all while rocking in place to ride out what pleasure was left.
The room filled with your shared breaths and soft moans as you squeezed around him deliberately, making him press even closer. “You're quite unprofessional,” he rumbled against your neck, his smile evident in his voice. “And such a troublemaker too.”
You let out a wicked laugh, ignorant of the footsteps outside in the corridor, and squeezed around him deliberately, delighting in the strangled gasp that escaped his throat. “Oh, that's rich coming from the one who just had to have me against a wall at work. So much for being professional, Doctor.”
“Hush.” His hands slid from your hips to your waist as he let out a breathless chuckle. "If I were you, I would be more careful with that mouth of yours, darling. We still have half a shift to get through." The warning in his voice held a playful edge that made you shiver with anticipation for when he would drive you home.



𝐄𝐕𝐄𝐍𝐓𝐒 ── Medical Edition Bingo (@fandom-free-bingo) ⠄⠂⠁⠁⠂⠄⠄ Playful Growls • O5 ── MASTERLIST ── Gingerbread Bingo (@fandom-free-bingo) ⠄⠂⠁⠁⠂⠄⠄ Finally Kissing Them • G3 ── MASTERLIST ⠄⠂⠁⠁⠂⠄⠄ "Please." • B4 ⠄⠂⠁⠁⠂⠄⠄ Hospital AU • I5 ⠄⠂⠁⠁⠂⠄⠄ Desperate Kiss • O4 ── MASTERLIST ⠄⠂⠁⠁⠂⠄⠄ Public Sex • I5 ── MASTERLIST ── Any Fandom AU Bingo (@anyfandomaubingo) ⠄⠂⠁⠁⠂⠄⠄ Hospital AU • I3 ── MASTERLIST ── Under The Sea Bingo (@seasonaldelightsbingo) ⠄⠂⠁⠁⠂⠄⠄ nuzzling their partner's neck like a cat • G4 ── MASTERLIST

#zayne x you#zayne x reader#zayne x female reader#zayne smut#zayne fic#l&ds x reader#lads zayne x reader#love and deepspace#love and deepspace x reader#love and deepspace smut#love and deepspace drabbles#l&ds smut#li shen x reader#li shin smut#l&ds zayne#lnds smut#lads smut#love & deepspace x reader#lnds x reader#lads x reader#l&ds x you#lads x you#love and deepspace x you#lads zayne#zayne l&ds#lnd zayne#li shen#love and deepspace zayne#zayne love and deepspace#love and deepspace scenarios
539 notes
·
View notes
Text
WIP Hospital: Surgery

*Meredith Grey monologue voice* Writers really batter their characters and sometimes the damage is so great that they have to be seen to by the professionals and if you've really messed them up, they may need surgery.
Before Surgery

Before any surgery, the patient must be prepared for the procedure. They will be prepped by nurses and doctors but there are things every patient must go through before the surgery especially if they undergo general anesthesia.
No drink/food for a set period of time before the surgery.
Removal of necessary hair
Possible enema but not always necessary
Thoroughly bathed and cleansed, the patient should not use any makeup, nail varnish or perfume
Tests maybe run prior to surgery such as blood tests
All piercings, protesthetics
The preparation of advance directives such as DNRs and wills etc
What is in an OR?

OR or operating room is where operations take place - or would be if your character was having surgery at hospital (they aren't, are they?)
Surgical Lights: Surgeons have to see why they are doing so high powered lighting is used to illuminate the patient and cavity.
Operating Tables: Operating tables are where the patient lies while the surgeons are trying to save their life. also known as surgical tables, are essential to any operating room.
Surgical Displays: These are screens that magnify the cavity for the OR, sort of like tvs that allow everyone a view of what's going on.
Blanket Warmers: Or warming cabinets. These are where the IV fluids, linens, and blankets are kept.
Scrub Sinks: This is where the surgeons abd nurses and technicians get washed up, sterilised and gowned.
Vital Signs Monitor: This is a machine that tracks the patient's heart rate, oxygen saturation, breathing rate and blood pressure.
Ventilator: A ventilator helps the patient breathe while on anesthesia.
Anesthesia Machine: This machine delivers anesthesia to the patient and monitors the level.
Diathermy or Electrocautery Machine: This is used to cut tissue and control bleeding
The Surgical Team

These are the people present in the OR besides the patient. It is up to them to keep the patient alive of course but to also ensure that safety and cleanliness are upheld.
Surgeon: Is the lead of the team and responsible for the planning and cutting of the patient. Most surgeons are specialists.
Surgical Assistant: They work alongside the surgeon, helping the surgeon.
Scrub Nurse: Scrub nurses are in charge of making sure everything stays sterile. They sterilise the surgical instruments and are in charge of minimalising contamination.
Anesthesiologist: The doctor who specialises in anesthesia who monitors the use of anaesthesia.
Circulating Nurse: Circulating nurses manage supplies, equipment and may run messages if needed outside the OR.
Observer: Sometimes med students or other surgeons will observe the surgery. They aren't essential.
General Surgerical Tools

These are just a few tools used with surgeries.
Scalpel – These are the blades used to cut into tissue.
#10: Scalpel with a large curved edge used for making large incisions.
#11: Scalpel with a triangular blade used to make short, shallow cuts.
#12: A small, crescent-shaped blade used to cut sutures
#15: used for short, precise cuts because of its small blade. Ideal for making short, precise incisions because of its small, curved cutting edge. Mostly used in cardiac surgery.
#17: Flat, chisel-like blade for narrow cuts
#18: Narrow, chisel blade for deep cuts and scraping
#20: Large curved blade, used when making a puncture or cut.
#21: Large curved blade, for slicing tissue and puncturing. commonly used for cutting tissue and other procedures that require a puncture or cut.
#22: Like the #10, it is flat and curved cutting edge, used on thick skin.
#23: Large blade that is slightly narrower but pointier
#24: Wide, flat blade with an angle used to make cuts at the corner, used to trim and strip
Forceps - are a gripping tool. Not to be confused with hemostats.
Allis Forceps: Have little teeth running along in them and are for firm tissue such as fascia.
Babcock Forceps: Smooth ended jawed forceps that are used for delicate tissue.
Dunhill Forceps: Small curved, serrated forceps used to hold vessels before ligation.
Lane Tissue Forceps: Forceps with interlocking teeth used to hold tough tissue
Littlewood Forceps: These forceps have blunt teeth, used for tough tissue as well as gaining entry through the umbilicus in laparoscopic surgery.
Sawtell Forceps: curved serrated forceps with a serrated end used to grip vessels
Spencer Wells: Can be curved or straight. They are used to clamp medium/large vessels before ligation
Debakey Forceps: Smooth forceps used for many things but used to grip tissue
Lanes Forceps: Toothed forceps used to grasp most tissues but not the bowel.
Gillies Forceps: Narrow forceps with teeth used on skin.
Scissors - are used to cut sutures and snip things during surgery.
Mayo Scissors: Heavy scissors with blunt ends, either curved or straight, used to cut thick tissue and sutures.
McIndoe Scissors: Curved scissors used to cut/dissect tissue
Hemostats - these are used to clamp vessels to prevent blood flow into the cavity the the surgeons are working in.
Adson Forceps: Can be straight or curved, with either semi-serrated tips or toothed tips, used to clamp vessels and tissues.
Artery Undermining Forceps: Toothed forceps, with ratchetted ringlets. Can be straight or angled, used to hold thick tissues during cardiothoracic surgeries
Bainbridge Forceps: Forceps with long jaws with serrated tips, used to clamp the bowel.
Crile Forceps: A clamp with horizontal, serrated jaws, that can be curved or straight. These are used in laparoscopical practices, for clamping tissue and vessels for cauterization and ligation.
Dandy Forceps: These forces are curved, with half-serrated jaws. Used to control the flow of blood.
Ferguson Angiotribe Forceps: Interlocking blades, curved or straight, used to clamp vessels to control blood flow.
Gemini Mixter Forceps: Curved and serrated, used to hold damaged and delicate vessels during cardiothoracic surgery.
Hartman Forceps: These are narrow, serrated, straight or curved but used primarily for left-handed surgeons. They are used to clamp small vessels.
Jacobson Forceps: Forceps with serrated curved jaws. Used for closing a wound or in tonsillectomies.
Kelly Forceps: Forceps with half-serrated jaws, either curved and straight. They are used for clamp
Kocher Hemostatic Forceps: Has serrated jaws and toothed tips. Used for grasping large blood vessels to control blood flow and holding dense tissue.
Lovelace Forceps: Forceps with fully serrated jaws, used for clamping vessels in gynecologic procedures.
Mikulicz Forceps: Half-serrated jaws with curved tips. Used for clamping the peritoneal sac during abdominal wall closure and the peritoneal tissues in the pelvic cavity.
Mixter Forceps: Right-angled jaws with longitudinal serrations, straight, curved patterns which can be half and fully-serrated. These are used for hard to reach places, used to hold tissue, blood vessels and stitches.
Mosquito Forceps: Short, serrated jaws used for incisions and thin tissues, usually before cauterization.
Rochester Carmalt Forceps: Long, wide serrated jaws. Used for grasping blood vessels.
Rochester Ochsner Forceps: These are used to objects and blood vessels during orthopedic procedures.
Retractors - used to pull back the flesh so the surgeon has better view
Langenbeck Retractor: Hook-shaped retractor, used to separate the edges of wounds. They can come in different sizes depending how deep you want the wound tract.
Norfolk and Norwich Retractor: This retractor is self-retaining, used to keep deep wounds open.
Travers Retractor: Also a self-retaining retractor, but used for much shallower wounds
Other Tools
Cauterization device: used to cauterizate blood vessels to prevent bleeding.
Needle Holder: Used for holding needles while suturing, it looks like a pair of scissors
Rampley Sponge Holding: used to store sponges and gauze
Towel clips: Used to keep towels and drapes in the place
Suction: This machine is sort of like a hose that sucks up blood and other fluids.
Surgical Stapler: Sort of what it says on the tin, a device that staples wounds together quickly.
Laparotomy Sponge/Lap Pad: Is an absorbent pad used to keep the cavity free of excess blood and fluid or to prevent too much bleeding.
Drapes: This is the cloth used to cover the patient and the operating table.
What to Wear to Surgery?

In surgery, contamination is always a fear so the surgeons and their team must dress accordingly in the OR. Most times the patient is draped or wearing a hospital gown.
Protective Cap: This is a cap that covers the hair. Worn by everyone.
Surgical Masks: Worn over the mouth and nose. Usually worn just by the surgical team.
Protective Eyewear: To shield the eyes from blood and debris. Usually worn just by the surgical team.
Gloves: Worn by the surgical team.
Gowns: These are long gowns worn over the scrubs. Worn by the surgical team.
Protective Shoe Covers: Worn over shoes of the surgical team.
Phrases used in the OR

Operations are high stress situations. Often communication is shortened to quick phrases.
Scalpel: Give me a scalpel
Clamp: Give me a clamp
Suction: Suck up this blood/liquid for me.
Retract: Hold back the tissue
Bovie: Give me the cautery equipment
Sponge count: Count the sponges and towels in case we left one in this here guy
Close: Stitch up the patient
Irrigation: Wash out the wound with water
Intubate: Insert a tube in the patient's throat to help them breath
Extubate: Remove the breathing tube
Airplane: Tilt the bed to expose a lateral portion or change the patient’s hemodynamics.
Donut: A support for the patient’s head after anesthesia.
Jump Room: Another OR prepped and waiting for the surgeon for another surgery
Types of Surgery

Surgeons don't just perform every kind of surgery. Most surgeons stick to a practicular specialty.
General Surgery: General surgery focuses on the abdominal organs.
Cardiothoracic Surgery: Deals with everything in the chest, eg. heart and lungs.
Orthopedic Surgery: Focuses on bones and muscle
Neurosurgery: This surgery focuses on the brain, spinal cord, and nervous system.
Plastic and Reconstructive Surgery: This surgery focuses on cosmetic surgery but also reconstructive procedures.
Pediatric Surgery: For babies, children and teenagers.
Vascular Surgery: Focuses on arteries and veins, everything on the vascular system.
Urology: Focuses on the urinary tract and male reproductive organs.
Otolaryngology (ENT): The ears, nose, and throat.
Gynecologic Surgery: Surgery focusing on the female reproductive system.
Examples of surgery

There are thousands of kinds of surgery but I've just listed a few well known ones here.
Appendectomy: Removal of the appendix
Cholecystectomy: Removal of the gallbladder
Coronary Artery Bypass Grafting (CABG): Bypass surgery performed to improve blood flow to the heart
Cesarean Section (C-section): The removal of a baby from the womb surgically.
Hysterectomy: Removal of the uterus.
Mastectomy: Removal of one or both breasts
Tonsillectomy: Removal of the tonsils.
Biopsy: Removal of tissue for examination.
Carotid Endarterectomy: Removal of blockages from in the arteries.
Debridement: Surgical removal of skin that is damaged or infected.
Dilation and Curettage (D&C): Removal of tissue from within the uterus.
Skin Graft: The planting of healthy skin over areas of damaged skin
Spinal Fusion: Joining two or more vertebrae
Rhinoplasty: Surgery to reconstruct or reshape the nose
Prostatectomy: Removal of the prostate gland
Hernia Repair: The repair of a hernia
Total Knee Replacement: The replacement of the knee with artificial components
Hip Replacement: Replacement of hip with artificial components.
Heart Valve Replacement and Repair: The repair of valves in the heart.
Aortic Aneurysm Repair: Repair of enlarged aorta to prevent rupture.
Pacemaker Installation: The installation of a pacemaker to regulate heartbeat.
Craniotomy: Opening up the skull to treat the brain for tumors, aneurysms or repairing damage.
Spinal Decompression: The relieving of pressure on the spinal cord.
Deep Brain Stimulation (DBS): This is the treatment of the brain with electrical pulses.
Breast Augmentation and Reconstruction: The implantion of artificial breasts for cosmetic reasons or to replace them after trauma or removal.
Liposuction: The removal of excess fat in the body.
Ovarian Cystectomy: Removal of ovarian cysts.
Endometriosis Surgery: Removal of endometrial tissue outside the uterus.
Nephrectomy: Removal of kidney
Ureteroscopy: Removal of obstruction in urinary tract
Vasectomy: The clipping of the male reproductive tracts to prevent fertility.
Colectomy: Partial or total removal of the colon.
Gastrectomy: Partial or total removal of the stomach.
Esophagectomy: Partial or total removal of the esophagus
Septoplasty: The correction of a deviated or damage septum.
Cochlear Implantation: Surgery to grant the hard of hearing or deaf to hear without hearing aids due to an implanted device.
The Winchester Method
Let's be honest your character is likely not going to hospital for their needed surgery. That bullet is going to be removed elsewhere and that appendix is coming out on the run. We're writers, we sort of use medicine like a fucking jump rope. THIS IS FOR FICTIONAL PURPOSES ONLY. The basic needs of make your own surgerical tools:
Sterilisation: You need something to sterilise your "tools". You can use alcoholic spirits or boiling water or open fire.
Needle and thread: You have to close yourself up, both need to be sterilised. See my post on stitches.
Cauterization: You need may need something to cauterise the wounds or stop bleeding. Something hot, sterile and metal like the flat of a knife can work short term.
Scalpel: You will need a sharp knife, sterilised and appropriately sized like a small paring knife or the blade of a Swiss army knife.
Bandages and towels: Something to soak up blood and cover. Torn up clothes or sheets can be used but most be sterilised.
Anesthesia/Pain Management: Something for the pain. Strong drink can be used to dull the pain but so can over the counter meds.
#I might have been watching a lot of medical dramas recently#I haven't done a wip hospital post in a while#Wip hospital#Wip hospital Surgery#writing#writeblr#writing resources#writing reference#writing advice#writer#spilled words#writer's problems#writer's life#Writing help#Writing research#writeblr community#wtwcommunity#Wtw#Medical au#Hospital au
101 notes
·
View notes
Text
Some Cardiology Vocabulary

for your next poem/story
Ablation – Elimination or removal.
Annulus – The ring around a heart valve where the valve leaflet merges with the heart muscle.
Arrhythmia – (or dysrhythmia) An abnormal heartbeat.
Autologous – Relating to self. For example, autologous stem cells are those taken from the patient’s own body.
Bruit – A sound made in the blood vessels resulting from turbulence, perhaps because of a buildup of plaque or damage to the vessels.
Cardiac – Pertaining to the heart.
Cardiomegaly – An enlarged heart. It is usually a sign of an underlying problem, such as high blood pressure, heart valve problems, or cardiomyopathy.
Carotid artery – A major artery (right and left) in the neck supplying blood to the brain.
Claudication – A tiredness or pain in the arms and legs caused by an inadequate supply of oxygen to the muscles, usually due to narrowed arteries or peripheral arterial disease (PAD).
Commissurotomy -A procedure used to widen the opening of a heart valve that has been narrowed by scar tissue.
Digitalis – A medicine made from the leaves of the foxglove plant. Digitalis is used to treat congestive heart failure (CHF) and heart rhythm problems (arrhythmias).
Endocardium – The smooth membrane covering the inside of the heart. The innermost lining of the heart.
Infarct – The area of heart tissue permanently damaged by an inadequate supply of oxygen.
Jugular veins – The veins that carry blood back from the head to the heart.
Maze surgery – A type of heart surgery that is used to treat chronic atrial fibrillation by creating a surgical “maze” of new electrical pathways to let electrical impulses travel easily through the heart. Also called the Maze procedure.
Myocardium – The muscular wall of the heart. It contracts to pump blood out of the heart and then relaxes as the heart refills with returning blood.
Palpitation – An uncomfortable feeling within the chest caused by an irregular heartbeat.
Pericardium – The outer fibrous sac that surrounds the heart.
Regurgitation – Backward flow of blood through a defective heart valve.
Septal defect – A hole in the wall of the heart separating the atria or in the wall of the heart separating the ventricles.
Sources: 1 2 3 4 ⚜ More: Word Lists
#cardiology#terminology#word list#spilled ink#writing reference#dark academia#writeblr#studyblr#langblr#linguistics#literature#creative writing#writing inspiration#writing inspo#writing ideas#writers on tumblr#writing prompt#poetry#poets on tumblr#writing resources
88 notes
·
View notes
Text

Hello! Today I started playing with AI, this is what I came up with, I hope you enjoy it !
Isabelle was 26 years old when her life took an unexpected turn. Since childhood, she had always been an active and energetic woman. She loved running in the park, practicing yoga, and spending hours exploring the city with her friends. But everything changed one summer day when she began to feel a persistent pain in her right side. At first, she thought it was just a muscle strain, a consequence of her busy schedule and long hours at the gym.
However, the pain did not go away. After several medical consultations and tests, she received a devastating diagnosis: kidney cancer. The news hit her with overwhelming force. The idea of facing such a serious illness at her age was terrifying. Despite the tears and anguish, Isabelle gathered her courage and prepared for what lay ahead. She knew she had to undergo surgery to remove the affected kidney.
On the day of the operation, Isabelle arrived at the hospital with a mix of nerves and hope. She was greeted by a medical team that reassured her and prepared her for the procedure. In a private cubicle, she changed into a surgical gown, feeling the cold fabric against her skin. Clara, a kind nurse, placed a hair cap on her head and explained the importance of the compression stockings, which were put on her to aid circulation during the surgery. Despite her discomfort, Isabelle felt a bit more at ease.
When it was time for anesthesia, Dr. Martínez placed an intravenous line and explained that she would feel a little dizzy. As the medication took effect, Isabelle felt the world slowly fade away, leaving behind her worries. However, what no one expected was that the surgery would become complicated.
Hours passed, and the medical team realized that something was wrong. As the operation dragged on, a growing fear filled the operating room. Suddenly, alarms began to sound. Isabelle had gone into cardiac arrest. “She’s going into arrest!” shouted a nurse. In an instant, the room became a whirlwind of activity.
Dr. López, the lead surgeon, moved quickly, directing the team with precision. Dr. Martínez adjusted the anesthesia and administered emergency medications. Every second counted as the team fought to stabilize her. After several attempts, they finally managed to restore her pulse. The operating room, once filled with tension, was flooded with a sigh of relief.
With Isabelle’s heart beating again, the team continued the surgery, this time with renewed determination. Finally, after hours of hard work, Dr. López announced that they had finished. Isabelle was transferred to the recovery room, where she began to awaken. Her body felt heavy and confused, but the sound of the monitors reminded her that she had overcome a great battle.
As she regained consciousness, she found herself in a calm silence. When she opened her eyes, she saw a nurse approaching, who explained what had happened and assured her that she was okay. Over time, Isabelle began to understand what she had experienced. Although she had faced an overwhelming challenge, she had come through it.
Her recovery was a gradual process. With each passing day, her strength returned, along with her determination to live fully. She joined support groups, shared her experience on social media, and became a health advocate. Her story resonated with others facing similar situations, inspiring them to keep fighting.
A year after the surgery, Isabelle signed up for a charity 5K run, a goal she had set for herself before her diagnosis. On the morning of the race, she felt a mix of emotions. As she ran, each step reminded her of her struggle and the life she had regained. Crossing the finish line brought tears to her eyes, but this time they were tears of joy and gratitude. She had faced her fear and emerged victorious.
Isabelle had not only survived an illness; she had learned to live again, with a new perspective and a deep appreciation for each day. Her story became a testament to resilience, reminding others that even in the darkest moments, there is always a light at the end of the tunnel.
92 notes
·
View notes
Note
Ok but just imagine :
Surgeon!Damian Wayne and Surgical intern/resident!reader. Or the reader could be an attending idk? But it’s so enemies to lovers coded! The tension??!???!!!!! Damian is the scary attending and the reader doesn’t dower like the rest? Or the reader is sunshine and the complete opposite of Damian’s personality. It’s a very scrambled idea but I just thought you might like to work with it?
Enemies to lovers? sign me tf up
Also, istg I had no idea what a surgical resident was before this. For those who don't know, they spend about five-ish years in a hospital and are usually under direct supervision of a more senior resident or an attending surgeon, attending for short.
Masterlist
Surgeon!Damian Wayne x Surgical Resident!reader
Part One, Part Two
You’re not stressed, you’re just… very close to breaking down. Or breaking a law. Or breaking someone’s nose “accidentally”. Or breaking… it didn’t matter what you broke, you just needed to break it.
Two years in to your internship at Gotham General hospital and you couldn’t be more of a wreck. In the bathroom stall no less- getting yelled at by the chief resident after not knowing what some extremely rare condition was (he didn’t even know it himself) and getting called one or two slurs by a senior resident wasn’t something you were used to and yet you knew it was normal.
Taking in a deep breath, you exit the stall and wash your hands and face before making your way to the OR, muttering positive phrases in your mind that were not helping at all.
With one more nod to yourself for reassurance, you open the door and are immediately greeted by the one face you didn’t want to see.
Dr. Wayne had a very prominent reputation for being less than friendly, for giving any resident- no matter how experienced- mental breakdowns and most importantly for being one of the best cardiac surgeons in Gotham. You exchange a nervous glance with another second-year resident, but only for as long as you dared.
Somehow, you were walking on eggshells without even taking a step.
The patient required a maze procedure, where the surgeon creates a pattern of scar tissue that allows the heart’s rhythm to return to normal.
You try sneaking a glance or two to the attending surgeon, but he glares back at you in warning before you can deduce his mood. Although that was probably a good tell.
The patient finally drifts off to sleep, you shift your attention right back to the attending as he begins the procedure with an incision on the patient’s chest.
Two hours later and maybe a bit too much yelling, the surgery was complete. The other residents begin leaving, but Dr. Wayne stays. You’re about to leave too when a low voice fills the silent space.
“That was the District Attorney,” Dr. Wayne says, and you pause all thought. You did everything right, didn’t you? You didn’t really do much, honestly, but what you did was correct, right? “And I can’t have a day-one intern screw up and jeopardize his health. He’s had a heart surgery before.”
“Do you want me to-”
“Yes,” he snaps.
“What do I tell the-”
“Chief resident? Tell him it’s not his problem.”
You nod and awkwardly leave the OR as fast as possible, not risking another moment in the same room as the man who is known for biting people’s heads off. Not literally.
You hope.
Not wanting to take any chances with the attending surgeon, you manage to find a space just near the DA’s ward that allows you to do paperwork while also being able to easily see the patient every five or ten minutes.
It went on like this for an hour and a half without problem and a snack in between before you exited the DA’s ward yet again, only this time loud and angry steps echoed through the hallway.
Your head whips around and your heart immediately drops to your feet. Your blood runs cold as the chief resident storms down the hall, eyes deadset on you.
You open the door to his office and politely gesture for him to walk inside. The chief resident, Langley, stops, glares and despite his temper, he agrees. You follow him in and swallow nervously, heart pounding in your ears.
“Before you get mad-”
“I already am mad,” Langley seethes, slamming his meaty hand on the small desk. “You abandoned all of your duties to- to what, to suck up to the District Attorney?”
“No sir-”
“Other patients need care and we’re already short on staff without some fucking idiot thinking that they can do whatever the fuck they want-”
“Dr. Wayne specifically requested me to do post-operation patient care-”
Your voices had risen to the point of shouting. You wouldn’t be surprised if the DA could hear it or even the other staff in the nearby wards and hallways.
“He doesn’t need a FUCKING NANNY.” the chief resident cried, and in one swift movement, he grabs a binder and slams it into the side of your face. “And who gives a fuck what that stuck-up WAYNE SURGEON wants?”
“Who gives a fuck on what I want?” a calmer, lower and yet far more terrifying voice states behind you. The hairs on the back of your neck raise and Langley’s eyes go wide. “Certainly not you. And here’s the thing, Langley,” the surgeon moves you aside in the already crowded space, more gently than you expected as he steps towards the chief resident, broad shoulders blocking your view, “that’s a problem. I could have your future ruined with a simple phone call or complaint and you decide to simply not respect authority?”
“That bitch-”
“Did exactly what I wanted her to,” Dr. Wayne replies in the same condescending tone. “Maybe you could learn a thing or two.”
Silence, apart from Langley’s ragged breathing. The ear that was hit rings loudly and when you softly touch you cheek, you can feel a bruise forming.
“You won’t apologize? That’s fine,” the surgeon says with an innocent shrug. “Consider your career gone.”
You certainly weren’t expecting that, and neither did Langley. He sputters in an attempt to right the course of a train that’s already fallen off the cliff, his eyes no doubt as wide as his steadily shrinking ego.
Was Dr. Wayne serious? You were confident that he could ruin someone’s career in a single phone call- he’s the best cardiac surgeon in the state, maybe even the country, and a Wayne, for crying out loud- but would he really just ruin someone’s career so quickly?
“You can show yourself out, by the way.” The surgeon raises an arm in a mocking gesture, beckoning the chief resident to leave and never return. “Security can, too.”
With no options left, Langley huffs and pushes past Dr. Wayne. You can still hear his angry footsteps, like a stampede of bison, as he storms down the hall.
“Thank you,” you murmur to the surgeon as he slowly turns around, inspecting the blow you took by carefully holding your chin and jaw in his large hands. You couldn’t tell if your heart was beating faster when Langley started ripping into you or right now, in this very moment, when you’re forced to stare in to green eyes so close you can make out every speck of dark gold within them.
“Don’t worry about it.” You swear on God’s good graces that the man smiled, just a twitch of his lips. “And please, call me Damian.”
With that, he lets go of your jaw and exits your makeshift office, leaving you flustered and confused.
He wanted you to call him by his first name?
397 notes
·
View notes
Text
“Dottie Roe,” 30 (USA 1965)
“Dottie” was a New Yorker seeking medical attention because she had started bleeding in the second trimester. She had suffered two miscarriages in the past and likely feared that she might lose this baby too. Unfortunately, the doctor’s dubious course of action would end her baby’s life and her own.
The medical journal that recorded Dottie’s case does not specify what the diagnosis was, but the doctor decided to put Dottie through a hysterotomy abortion and a tubal ligation. This was a questionable course of action considering that hysterotomy abortion is associated with a very high maternal mortality rate. But since it qualified under the health exemption (“life of the mother” exception), it was completely legal.
The report of Dottie’s death raises questions. She was under general anesthesia for the abortion and tubal ligation, but would never wake up. The journal states that “Cardiac arrest ensued during the procedure, and the patient expired following completion of a tubal ligation, never having regained consciousness.”
Later research found that the risk of hysterotomy abortion concurrent with surgical sterilization was unjustified even in someone perfectly healthy. Today, medical knowledge has advanced beyond the antiquated approach of abortion for pregnancy complications— the recommendation that failed Dottie and her child.
Other pre-Roe legal abortions that were meant as “life/health of the mother” exceptions and killed the patient instead include:
“Carolyn” and “Caroline Roe”: Both died in North Carolina in 1970 or 1971 after abortions for “health indications”
“Bonnie Roe”: Put through an abortion because her heart condition, then died because of drugs for the abortion that were contraindicated in heart patients
“Molly Roe”: Her killers were rebuked by a maternal health committee for a saline abortion that was more dangerous to the young lupus patient than her pregnancy
“Rita Roe”: A cardiac patient who died from multiple pulmonary emboli after an abortion at 12 weeks pregnant
Caro Lena Grasso: An Italian immigrant with a chronic respiratory illness who died of infection caused by the abortion meant to stabilize her
Erika Charlotte Wullschleger: At 28, she was in a tank respirator at Scripps Memorial Hospital. She was just starting to get better before dying from the abortion that her husband, not she, signed the consent forms to.
Barbara Riley: After a doctor told her to have an abortion instead of giving birth again, she reluctantly underwent the highly dangerous saline abortion that took both lives.
(Sources below)


New York State Medical Journal, January 1974
#pregnant people deserve better#pre roe legal#pro life#unsafe yet legal#unidentified victim#tw abortion#tw ab*rtion#tw murder#abortion#abortion debate#death from legal abortion
9 notes
·
View notes
Note
Hi! Just found your blog and I think I’m in love, this is my new holy grail.
Could you give me a quick rundown of procedures that have to do with bone marrow? What are they, why are they done, etc.
PS: is there any niche topic you’ve been wanting to mention but have never been asked about? If so, now’s your chance to nerd out! :)
- 🦾
Oh dear anon, you've just activated me like a sleeper agent... I've already done a ton of research on bone marrow procedures for a whumpy daydream, and I just learned about it in school. Little did you know, this is the niche topic that I could talk about for days.
Bone marrow, baby!
So bone marrow in the innermost part of the bones and is most abundant in the long bones (femurs, humeruses, radiuses, ulnas, tibias, and fibulas) and pelvis. The primary function of bone marrow is to produce blood cells, including erythrocytes (red blood cells [RBCs]), leukocytes (white blood cells [WBCs]), and platelets). RBCs carry oxygen, WBCs fight infections, and platelets clump together to form clots and stop bleeding. The bone marrow cells that produce these blood cells are called hematopoietic [he-MAT-o-po-EE-tic] stem cells.
Bone marrow dysfunction can manifest in clinical disorders such as anemias (sickle cell, beta thalassemia, aplastic), malignancies (leukemia, myeloma, lymphoma, polycythemia vera), and other non-anemia deficiencies (leukopenia [deficiency of WBCs], neutropenia [deficiency of neutrophils, a type of WBC], thrombocytopenia [deficiency of platelets]). These disorders can co-occur and result from each other. Some medications like chemotherapy and some anti-infectives can also suppress the bone marrow.
Procedures involving the bone marrow include aspiration and biopsy, donation, and transplant.
Bone marrow aspiration and biopsy: This is a procedure to take a sample of the bone marrow for the purposes of diagnosing any of the above disorders. It is not performed if the patient has bleeding disorders like hemophilia. This is usually an outpatient procedure done in an interventional radiology (procedures are guided by x-ray or other imaging methods) unit. The patient will be admitted to the unit and asked to change into a gown, then will get an IV and have a full set of vitals taken (temperature, heart rate, respiratory rate, blood pressure, oxygen saturation). They will be asked to sign a consent form after the procedure and its risks and benefits have been explained. When it's time for their procedure, the patient will be wheeled in a hospital bed to the procedure room (see the image below) by a nurse.

All staff involved in the procedure will be wearing lead-lined aprons, surgical masks, and goggles. In the procedure room, they will move from the bed to a table, or will be assisted if needed, and positioned on their stomach with a pillow under their hips. They will be hooked up to a cardiac monitor and put on an end-tidal CO2 sampling nasal cannula (see the image below).

They may or may not be given fentanyl and midazolam (Versed) through their IV for pain relief and mild sedation. They will still be awake and aware during the procedure. I've seen people make small talk with the staff for their entire procedures. The patient will then be draped everywhere except for the site (over one of the iliac crests of the pelvis) of the procedure. The radiologist will inject lidocaine into the skin around the site and clean it with betadine (a disinfectant similar to iodine). The radiologist will then make a small incision at the site and insert a needle containing a fine tube down to the bone (see the image below).
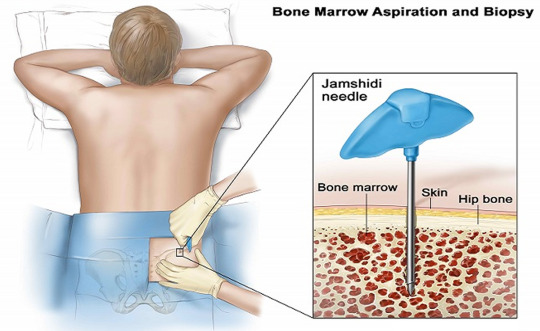
The radiologist will work the needle into the bone with a twisting motion. The patient won't feel pain, but some people have said that the sensation of the needle twisting into the bone can be uncomfortable. When the needle penetrates the marrow, it will be removed, leaving the tube to which a syringe will be attached and marrow drawn up. Patients have reported feeling an uncomfortable sucking sensation during this part. Once this is done, the tube will be removed and a biopsy needle (see the image below) will be inserted into the same incision to take a separate sample.

A twisting motion is also used here. The radiologist will then put a pressure dressing on the site. After the radiological equipment has been turned off and the patient disconnected from the monitoring equipment, the staff will move them back to the hospital bed and the nurse will wheel them back to their cubicle in the unit. They will be positioned so that their weight is on the incision to maintain pressure and control bleeding. The patient will stay at the hospital for a few hours while the meds wear off and the nurses monitor them for bleeding, after which they will be discharged with instructions to call the doctor if they experience any excessive bleeding. They should have someone else drive them home.
Bone marrow donation: To be a bone marrow donor, a person has to be between 18 and 35 years old; not have HIV/AIDs, rheumatoid arthritis, systemic autoimmune diseases, bleeding disorders, brain injury, cancer or prior cancer treatments within 5 years of the donation, chronic pain that is treated with medications, chronic Lyme disease, diabetes that requires insulin, heart disease, hepatitis B/C, or kidney disease; and be a match to the intended recipient's human leukocyte antigen (HLA) and blood type. (Note: people can donate to bone marrow banks and be matched anonymously to recipients with their same HLA type) HLA types are different from blood types and are most commonly matched between people of the same ethnic background and family members, especially siblings. The donor will have to undergo extensive tests to ensure that they are healthy enough to undergo the procedure and for their bone marrow to be used for transplant; these include blood tests, tests for all types of infections, an electrocardiogram, and a chest x-ray. Bone marrow stem cells may be harvested from a regular blood donation or from bone marrow aspiration. The procedure for donation is the same as for aspiration, only the patient may be put under general anesthesia and intubated and the doctor will pull off about 1-2 pints of bone marrow. The patient may have to stay in the hospital overnight.
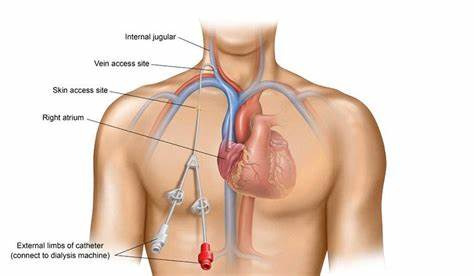
Bone marrow transplant: This is officially called a hematopoietic stem cell transplant (HSCT) and is usually done for leukemia, lymphoma, myeloma, polycythemia vera, aplastic anemia, severe immunodeficiency disorders, sickle cell anemia, beta thalassemia, and other disorders of the bone marrow or immunity. Stem cells can be taken from the recipient before their illness became serious, a related or unrelated donor, or umbilical cord blood. It is often a last resort treatment due to its high cost (up to $500,000) and potential for graft rejection. Before transplantation, the patient will receive high-dose radiation and chemotherapy (myeloablative therapy) to destroy their existing bone marrow. Once the myeloablative therapy has been completed, stem cells will be infused through a central venous catheter (see the image below), which the patient will certainly already have if they have cancer.
Ideally, the cells will seed in the bones and multiply to fill them (engraftment). This can take 2-4 weeks, or may never occur. The patient may not achieve full immunity for months or years. The patient may be in the hospital from the start of myeloablative therapy to 100 days after the transplant. Following the transplant, the patient will be on a regimen of medications to suppress their immune system to avoid graft-versus-host disease (GVHD; rejection of the donor stem cells resulting in a systemic inflammatory reaction). The patient may or may not be on this regimen for the rest of their life; if they never experience GVHD, they may not. They will have to be on the lookout for signs of graft rejection and secondary cancers (due to the myeloablative therapy) for the rest of their life.
Thanks for letting me nerd out and happy whumping!
#whump#hospital whump#anon ask#🦾#bone marrow aspiration and biopsy#bone marrow donation#bone marrow transplant
5 notes
·
View notes
Text
What are the Different Types and Treatments of Arthritis?

Leading a beautiful life doesn’t come without challenges. Our body goes through a lot of stress and grind in the process and there comes a stage when it needs more attention and care than ever before.
The Best Orthopedic Doctor in Bangalore at United Hospital explains that the wear and tear, our body is subjected to, leads to pain in the ankles and knees. Sometimes, it can get pretty hard to walk!
Are we welcoming Arthritis in this case?! Well, in the worst case, unfortunately, we may be. However, experts indicate that there is no need to panic. With rapid advancements in medical science, there is not just hope, but more confidence that we can defeat Arthritis.
It is all about being aware of what Arthritis exactly is and taking precautions at the right time that could be the best beginning to arrive at a successful solution.
Understanding Arthritis?
Experts at United Hospital, a dedicated Orthopedic Centre in Bangalore focusing on Arthritis care, explain that Arthritis is a medical condition involving swelling and tenderness of one or more joints. It may worsen with age and is a prevalent cause of discomfort among senior citizens
Types of Arthritis
Arthritis can affect individuals of any age, but the elderly are more vulnerable.
Some of the common forms of Arthritis are:
Osteoarthritis - It is a condition that affects joints in your Hands, Knees, Hips and Spine.
Psoriatic Arthritis - This a condition that develops in people due to a very challenging skin disease called Psoriasis.
Reactive Arthritis – This causes joint pain and swelling triggered by an infection in prominent parts of your body — most often your intestines, genitals or urinary tract.
Rheumatoid Arthritis – This is a chronic inflammatory disorder which can affect more than just joints including premier organs like lungs, heart, eyes and blood vessels.
Some of the other conditions faced notably by the elderly include Ankylosing Spondylitis.
Symptoms of Arthritis
The most common signs and symptoms of arthritis involve the joints. Hence, it is important to seek an expert opinion if you observe one or more of the following symptoms:
Pain in the joints.
Stiffness felt in the joints.
Swelling observed in or around the joints.
Redness observed in the joints.
Difficulty in moving.
Treatment for Arthritis
Arthritis, if untreated, can be a really painful thing to handle. However, what really matters is the right type of medical attention at the right time and from the right source. Your treatment is based on how severe is your condition and can include:
Medications
Depending upon the type of Arthritis diagnosed, your medications may include:
Non-steroidal anti-inflammatory drugs.
Creams and Ointments.
Steroids
Physical therapies and exercises.
Surgical Interventions
In case you do not get any relief from the above medications your doctor might recommend surgical interventions to bring you back to your routine lifestyles in quick time. Some of the types of surgeries performed include,
Joint Repairs
Joint Replacements
Joint fusions
Let’s say Goodbye to Arthritis forever and welcome a painless life. For many of us, life may begin at 40, but so does Arthritis! Hence, if you are wondering as to, “Which is the Best Orthopaedic Clinic near me to treat Arthritis”? feel free to connect with United Hospital.
#Cardiac surgeon#Heart surgeon#Cardiothoracic surgeon#Cardiac surgery#Heart surgery#Cardiac surgical procedures#Open-heart surgery#Minimally invasive heart surgery#Coronary artery bypass graft (CABG)#Valve replacement surgery#Aortic surgery#Congenital heart defect surgery#Pediatric cardiac surgeon#Cardiac transplant surgeon#Cardiac care specialist#Cardiac surgery recovery#cardiology hospital near me#Bangalore best cardiologist#heart specialist hospital in Bangalore#best cardiology hospital in Bangalore#good heart hospital in Bangalore#best heart failure treatment hospitals in Bangalore
0 notes
Text
Robotic Heart Surgery in Rajasthan, India
Robotic heart surgery is a cutting-edge, minimally invasive technique that offers precision, faster recovery, and reduced complications for heart patients. In Rajasthan, India, this advanced procedure is transforming cardiac care, providing safer and more effective treatment options.
With expert cardiologists and state-of-the-art technology, Robotic heart surgery in Rajasthan, India, is becoming a preferred choice for patients seeking high-quality cardiac treatment. This technique enhances surgical accuracy, reduces pain, and shortens hospital stays.
For the best Robotic heart surgery in Rajasthan, India, visit www.drlalitmalik.com to consult top heart specialists and ensure expert care for a healthier heart.
#Robotic heart Surgery in Rajasthan#India#BesSurgery t Robotic Heart in Rajasthan#Top Cardiac Surgeons for Robotic Surgery in Rajasthan
2 notes
·
View notes
Text
Prompt: Surgery (Escapril Day 28)
Procedure:
Dissection of a desolate cadaver with special focus on the physiological impact of emotional distress
Introduction:
The said procedure aims to explore the anatomical structures of an agonized cadaver with a focus on understanding the physiological manifestations of a heartbreak.
Equipments:
i. A desolate cadaver: A cadaver with a history of chronic heartbreak and acute agony.
ii. Dissection instruments: scalpel (sharpened by an apathetic tongue), scissors (ready to snap at any instant) , forceps (multi functioning i.e grasping truth from the windpipe, retracting false accusations, manipulating sutures of empty consolation), gauze bandages (to fill the void of heart) and other surgical tools.
iii. Dissection table: A sterile table (any empty casket will do) equipped with enough darkness and suffocation particles.
Method:
i. A midline scalp incision was made by the tongue-sharpened scalpel, extending from the forehead to the occipital region.
ii. A craniotomy was performed with high-speed derogatory remarks to create a bone flap in shape of a crushed soul, over the frontal, parietal and temporal lobes.
iii. The dura mater was then incised with utmost neglect to expose the wilting brain tissue.
iv. The brain was then thoroughly laughed at with special attention to the limping limbic system and paranoid prefrontal cortex. Tissue samples were then collected for histological analysis to assess the impact of emotional distress for future guinea pigs.
v. Next, a midline incision was made through the worn sternum using the same scalpel infused with misery.
vi. The torn pericardium curtain was removed to expose the fractured heart.
vii. The heart was then examined for any intact cardiac chambers or other decently performing arteries. The heart was then shattered by the rhythmical hammering of a regular sized taunt.
viii. The heart was then ruthlessly excised in one piece and the cracks were sutured with delusion to put it up for auction.
ix. The cadaver was then abandoned to breathe and walk.
Reflection:
The findings of the following procedure suggest that — active exposure of victim's brain and heart to continuous emotional distress, allows the offender to shape them into malfunctioning masses.
Conclusion:
In conclusion, the following procedure was a success and more such breathing cadavers are currently undergoing the same procedure to ensure the triumph of this groundbreaking surgery.
note: no cadaver was harmed in the following process, all mentioned criteria and procedures are a work of fiction.
— circadeacademia
#scribbles#prose poem#writers and poets#poems and quotes#quotes#spilled ink#poetry#poetic#writeblrcafe#spilled thoughts#escapril#napowrimo#april prompts#national poetry month#writing prompts#female writers#creative writing#am writing#original writing#button poetry#writers on tumblr#writerscafe#poets on tumblr#my poetry#prose poetry#poetic prose#poetry and prose#writeblr#writeaway#original poem
9 notes
·
View notes
Text
Heart Care Centre In Gorakhpur
When it comes to maintaining overall health, few things are as vital as taking care of your heart. As the heart continues to be one of the most critical organs in our body, any issues related to it must be taken seriously. In Gorakhpur, the demand for quality heart care services has risen significantly, as people are becoming more aware of the importance of cardiovascular health. Fortunately, Gorakhpur is home to some of the best heart care centre, where patients can receive expert treatment and guidance on managing heart conditions.
In this blog, we’ll explore the best heart care centre in Gorakhpur, the services they offer, and why you should choose them for your heart health needs.

Heart diseases continue to be one of the leading causes of death worldwide. In India, the rise of lifestyle diseases such as hypertension, diabetes, and high cholesterol has contributed to an increase in heart-related problems. Early diagnosis and intervention are key to managing heart conditions effectively. This is where a good heart care centres comes into play. Heart care centres are equipped with advanced technology, skilled cardiologists, and modern facilities to provide accurate diagnosis, treatment, and preventive care for a wide range of heart diseases.
Services Offered at Heart Care Centres in Gorakhpur
Heart care centres in Gorakhpur provide a variety of services, ranging from preventive care to advanced treatment options. Here are some of the key services you can expect:
1. Cardiology Consultations
A heart care centre begins with consultations with experienced cardiologists who assess your symptoms, medical history, and risk factors. These consultations often involve a thorough examination and may be followed by diagnostic tests to understand the root cause of any heart issues.
2. Comprehensive Diagnostic Tests
Accurate diagnosis is the first step toward effective treatment. Heart care centres in Gorakhpur offer state-of-the-art diagnostic tools such as:
Electrocardiogram (ECG)
Echocardiogram (ultrasound of the heart)
Stress tests
Holter monitoring
Angiography and angioplasty
These tests help identify underlying conditions like heart disease, arrhythmias, blocked arteries, and more.
3. Cardiac Surgery and Interventions
For patients with severe heart conditions, heart care centres in Gorakhpur offer surgical interventions such as:
Coronary Artery Bypass Grafting (CABG)
Valve replacement or repair
Angioplasty and stent placement
These procedures are performed by expert cardiac surgeons who specialize in heart-related surgeries, ensuring the best outcomes for patients.
4. Preventive Care and Health Monitoring
Heart care centres emphasize preventive care to help individuals avoid heart disease. They provide services like:
Routine health check-ups
Blood pressure and cholesterol monitoring
Lifestyle counseling (diet, exercise, stress management)
Weight management and smoking cessation programs
By focusing on prevention, these centres help patients lower the risk of heart disease and maintain a healthy lifestyle.
5. Cardiac Rehabilitation
After a heart attack or surgery, patients require a rehabilitation program to recover fully. Cardiac rehabilitation involves supervised exercise, diet counseling, and psychological support to help individuals regain strength and reduce the risk of further complications.
Why Choose a Heart Care Centre in Gorakhpur?
1. Expert Cardiologists
Heart care centres in Gorakhpur are staffed by experienced and qualified cardiologists who specialize in diagnosing and treating a wide range of heart conditions. Whether you’re dealing with high blood pressure, irregular heartbeats, or more severe conditions like coronary artery disease, these professionals provide the best possible care.
2. State-of-the-Art Facilities
The heart care centres in Gorakhpur are equipped with the latest technology, including high-resolution imaging systems, advanced cardiac monitoring tools, and cutting-edge surgery equipment. This allows doctors to provide accurate diagnoses and offer effective treatment options for heart patients.
3. Personalized Care
Each patient is unique, and heart care centres understand the importance of providing personalized care. From the first consultation to post-treatment care, cardiologists work with patients to create tailored treatment plans that suit their individual needs and health goals.
4. Comprehensive Approach
These centres offer a comprehensive range of services under one roof, ensuring that all aspects of heart health are addressed. From diagnostic tests and treatment options to preventive care and rehabilitation, you can count on the heart care Centres in Gorakhpur to support your heart health journey.
Best Heart Care Centre in Gorakhpur.
Gupta Heart Care Centre in Gorakhpur
This Centre are well-known for their experienced team of cardiologists, use of advanced medical technology, and focus on patient well-being.
Conclusion
Taking care of your heart is an essential aspect of living a long and healthy life. If you're experiencing any symptoms of heart disease or if you simply want to ensure your heart health is in check, it’s time to consult a trusted heart care centres in Gorakhpur. With world-class doctors, top-notch facilities, and comprehensive treatment options, you can rest assured that your heart is in safe hands.
Remember, early detection and intervention can save lives. Don’t wait for symptoms to worsen—schedule a consultation at one of Gorakhpur’s leading heart care centres today.
Call to Action: If you or someone you know is concerned about their heart health, don't delay. Contact a reliable Heart Care Centre in Gorakhpur for an assessment and start your journey toward a healthier heart today
2 notes
·
View notes
Text
Top 5 Most Needed Equipment in a Hospital
Hospitals are the cornerstone of healthcare, playing a crucial role in saving lives and improving the quality of care. To deliver optimal treatment, hospitals must be equipped with the latest and most essential medical devices. These tools not only enhance diagnostic accuracy but also ensure patient safety and efficient operations. In this article, we’ll explore the top 5 most needed equipment in a hospital, detailing their importance and functionality. If you’re looking to procure high-quality devices, consider exploring options to buy medical supplies online, where convenience meets affordability.
1. Diagnostic Imaging Systems
Diagnostic imaging systems are indispensable in modern medicine, allowing doctors to view and analyze internal structures of the body. Equipment such as X-ray machines, CT scanners, and MRI machines provide critical insights into a patient’s condition.
Why They’re Needed:
Enable early and accurate diagnosis.
Help in planning surgical procedures.
Monitor the effectiveness of ongoing treatments.
Investing in reliable diagnostic imaging systems ensures better patient outcomes and streamlines the treatment process. High-quality imaging devices are widely available through medical supplies online platforms, offering advanced technology at competitive prices.
2. Patient Monitoring Systems
Patient monitoring systems are essential for tracking vital signs such as heart rate, blood pressure, oxygen saturation, and temperature. These systems are particularly crucial in intensive care units (ICUs) and operating rooms.
Key Features:
Continuous monitoring of patient health.
Real-time alerts for any abnormalities.
Integration with hospital information systems for data storage and analysis.
Modern patient monitors are equipped with wireless capabilities, enabling remote monitoring. This feature is invaluable, especially during emergencies or in telemedicine settings.
3. BPL ECG Machine
An electrocardiogram (ECG) machine records the electrical activity of the heart and is essential for diagnosing various cardiac conditions. Among the top-rated ECG machines, the BPL ECG machine stands out for its precision and user-friendly design.
Benefits of BPL ECG Machines:
High accuracy in detecting arrhythmias and heart abnormalities.
Easy-to-use interface for healthcare professionals.
Portability, making it ideal for both hospital and home use.
Cardiac health is a critical aspect of patient care, and a dependable ECG machine ensures timely intervention. Purchasing a BPL ECG machine from trusted sources online guarantees authenticity and quality.
4. Surgical Instruments and Equipment
No hospital can function without a comprehensive range of surgical instruments. From scalpels and forceps to advanced robotic surgical systems, these tools are vital for performing both minor and major surgeries.
Must-Have Surgical Equipment:
Sterilizers to ensure a contamination-free environment.
Laparoscopic tools for minimally invasive procedures.
Advanced anesthesia machines for patient safety during operations.
To maintain high standards of patient care, hospitals must regularly update and replace their surgical instruments. Many healthcare facilities prefer sourcing these items through medical supplies online, ensuring timely delivery and cost-effectiveness.
5. Ventilators and Respiratory Equipment
Ventilators and other respiratory equipment have become indispensable, especially in the wake of the COVID-19 pandemic. These devices provide critical support for patients who struggle to breathe independently.
Importance of Ventilators:
Assist patients with respiratory failure.
Play a crucial role in ICUs and emergency care units.
Provide life-saving support during severe illnesses or post-surgical recovery.
Modern ventilators come with advanced settings to customize airflow and pressure, catering to the unique needs of each patient. Hospitals can explore various models and price ranges by purchasing these devices from medical supplies online platforms.
Why Choose Medical Supplies Online?
The healthcare industry is evolving rapidly, and so is the way hospitals procure equipment. Buying medical supplies online offers several advantages, including:
Wide Range of Options: From basic tools to advanced machinery, online platforms provide a comprehensive selection of medical equipment.
Cost Efficiency: Competitive pricing and frequent discounts make online shopping more affordable.
Convenience: Avoid the hassle of visiting multiple vendors; place orders with just a few clicks.
Authenticity: Reputable platforms ensure that all products meet international quality standards.
2 notes
·
View notes
Note
Lofty, im curious.
If you'd care to share, are you an EMT Basic, Intermediate or Paramedic?? I just learned there was a difference haha
YOU KNOW THE DIFFERENCE :D
Intermediate is an old level that’s being phased out, though I have a coworker who is an intermediate. The national standard levels in the USA are EMT (basic), Advanced EMT, and Paramedic. I’m an advanced 👍🏻 The difference between me and a medic is I don’t do cardiac drugs (which is highly ironic considering I’m a cardiac ICU nurse and I play with cardiac drugs all the time at my nursing job lol), I don’t medically sedate people, and I can’t do certain procedures like intubation, needle decompression thoracotomy, or surgical airways (cricothyrotomy). I can start IVs and give most of the meds in our drug boxes, I can do IO and blind airways and CPAP. That kind of stuff.
I don’t usually call for a medic all that often, it has to be pretty freaking dire. I think the last time I called for one was because we were about to code a baby (baby was fine in the end, don’t worry).
#you ask skye answers#lovely anon#Idk if any of the things I said will make sense to anyone but I’m short on time and wanted to answer this one#So if you don’t know some of the terms I used feel free to ask :)
22 notes
·
View notes
Text
World's first fully robotic heart transplant performed

🔹A groundbreaking achievement in medical technology has been made at King Faisal Specialist Hospital and Research Centre in Riyadh, Saudi Arabia, where the world’s first fully robotic heart transplant was successfully performed. The operation, lasting about two and a half hours, was conducted on a 16-year-old patient suffering from end-stage heart failure, who specifically requested that his chest remain unopened during the procedure.
🔹The surgery was led by cardiovascular surgeon Feras Khaliel, who prepared meticulously with his team, conducting seven training sessions over three days to ensure everything went smoothly. This rigorous preparation highlights the complexity and innovation involved in performing such a pioneering operation.
🔹Majid Al Fayyad, the CEO of the medical center, praised the accomplishment as a significant advancement in healthcare, drawing parallels to the historical significance of the first heart transplants conducted in the 1960s. The fully robotic approach marks a new era in surgical procedures, emphasizing precision and minimally invasive techniques.
🔹This landmark surgery not only showcases the capabilities of robotic technology in medicine but also sets a precedent for future procedures. It represents a major step forward in cardiac care, offering hope for improved outcomes in patients requiring heart transplants.
2 notes
·
View notes