#Buy PrEP HIV Pill
Explore tagged Tumblr posts
Text
A federal appeals court panel appeared skeptical on Tuesday of calls to impose a nationwide freeze on Obamacare’s rules for no-cost coverage of preventive care while litigation continues — a move the Biden administration warned would threaten access to a range of services for millions of people on employer-sponsored insurance and Obamacare’s individual market.
Both sides in the case agreed that the individual Texas businesses that sued over the mandate should be shielded from it while the case makes its way through the courts. But they split on whether more harm would be caused by keeping the current coverage rules intact for everyone else in the country or by suspending them nationwide.
Attorneys representing the Texas employers and individual workers challenging the policy argued that because
the United States Preventive Services Task Force is made up of outside experts who are not Senate-confirmed or overseen by Senate-confirmed government employees, their recommendations of what preventive services should be covered by insurance — from syphilis tests to depression screenings — must be “set aside” and can’t be enforced.
Their suit also claims the Obamacare requirement for insurance to cover the pre-exposure prophylaxis pill used to prevent transmission of HIV — known as PrEP — violates the religious rights of the challengers. In their legal briefs, they equated covering the highly effective medication with encouraging homosexuality and promiscuity.
The merits of those legal arguments didn’t come up in Tuesday’s hearing before the 5th U.S. Circuit Court of Appeals in New Orleans, which focused squarely on whether the nationwide freeze of the Obamacare mandate a lower court ordered in March went too far.
That ruling, Justice Department attorney Alisa Klein told the court, was a “legal error” that “extinguished the rights of about 150 million people who are not parties to the case.”
Klein urged the appeals court judges to consider the “balance of equities,” arguing that there would be no harm done to the already-protected plaintiffs by putting the nationwide injunction on hold, but great harm done to everyone else if they failed to do so.
“It can’t be overstated how important the guarantee of cost-free access is when patients go to get their mammograms and colonoscopies,” she said. “We’re talking about 50 different types of care.”
The attorney for the conservative challengers, Jonathan Mitchell, responded that the nationwide ruling was appropriate because “agency actions must be set aside if they are unlawful.”
Mitchell — the architect of the six-week abortion ban Texas imposed before Roe was overturned — attempted to reassure the judges that imposing a nationwide injunction wouldn’t cause harm because insurers are unlikely to drop coverage of preventive care services while the case is still in process.
The judges on the appeals court panel seemed unconvinced.
Leslie Southwick — an appointee of former President George W. Bush — called that assertion “speculative” and said it was “very unusual” to be asked to rule on “our sense of how insurance companies would react.”
“I’m not sure what we have to go on,” he said.
The judges also grilled Mitchell on whether a win for his side would solve his clients’ problem — a legal threshold known as “redressability.” When Mitchell argued that individual workers he represents who are refusing to buy insurance because of the PrEP coverage requirement would be able to get covered if the mandate were lifted, Judge Stephen Higginson noted that the workers’ own affidavits “don’t say that.”
Higginson — an appointee of former President Barack Obama — pointed out that only one of the four workers came anywhere close to making that claim, and that he expressed “a desire to buy insurance, not a specific intent.”
Mitchell acknowledged that there’s no “iron-clad guarantee” his clients would buy health insurance if courts blocked the Obamacare mandate.
In closing, the judges urged both him and the DOJ to try to broker a compromise that would more narrowly tailor the nationwide ruling without infringing on the rights of the plaintiffs.
Tuesday’s hearing was the latest in a months-long saga over the preventive care mandate that’s been in place for more than a decade.
Texas District Court Judge Reed O’Connor — the author of several rulings against pieces of Obamacare — issued a nationwide ruling in March for the challengers, striking down all of the decisions made by the United States Preventive Services Task Force since 2010 about what insurers must cover without cost sharing.
In May, the 5th Circuit Court issued an administrative stay of that lower court ruling — keeping the current coverage rules in place while the case proceeds.
Public health groups warn of serious consequences if O’Connor’s ruling is upheld — citing research showing that even small out-of-pocket costs deter many people from seeking preventive care, leading to sicker patients and more costly treatments. Medical experts are particularly worried that coverage rollbacks would exacerbate already record rates of sexually transmitted diseases by making testing and treatment services unaffordable for vulnerable populations.
Many major insurers have pledged to maintain preventive care at no cost to patients for the time being no matter what courts decide, but experts fear that patients could eventually be hit with out-of-pocket charges should the 5th Circuit and Supreme Court side with the challengers.
The case also throws more than two-dozen new recommendations the federal task force is currently weighing in jeopardy, rules that could expand coverage of everything from prenatal care to speech therapy to osteoporosis.
3 notes
·
View notes
Text
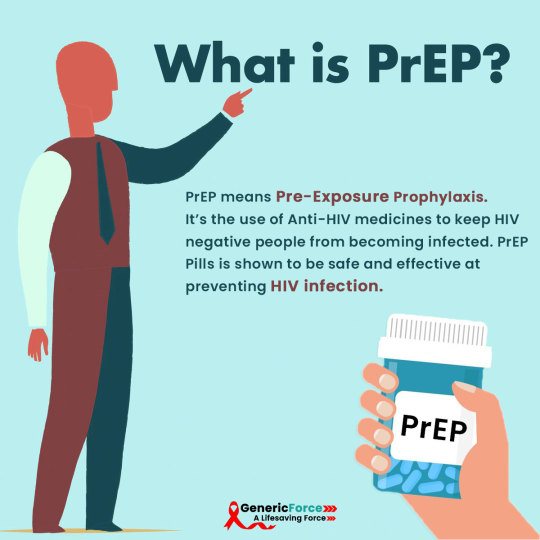
What is PrEP?
PrEP means Pre-Exposure Prophylaxis. It’s the use of anti-HIV medicines to keep HIV negative people from becoming infected. PrEP Pills is approved by the FDA and has been shown to be safe and effective at preventing HIV infection.
Truvada is currently the only drug approved for use as PrEP HIV Pills. Truvada prep is a single pill that is a combination of two anti-HIV drugs, tenofovir, and emtricitabine. Truvada is the brand name for PrEP, but generic forms of PrEP HIV are available, which contain the same active drugs.
PrEP is different from PEP (Post-exposure prophylaxis), which is an emergency treatment for HIV taken after possible exposure to the virus. PrEP greatly reduces the risk of HIV. PrEP Medicine for HIV is a powerful prevention tool and can help reduce anxiety and stress for people at risk of contracting HIV.
PrEP Medication for HIV:
Tenvir EM Tablet
Viraday Tablet
Tenvir 300 Mg
Tafero Em Tablet
Tavin Em
Where can I Buy PrEP Medicine?
We are GenericForce, one of the most trusted generic drugstores in the world today. From allover the world come to us to buy all kinds of medicines and healthcare products. https://www.genericforce.com/
#Genericforce#HIV infection#Truvada#PrEP HIV#PrEP HIV medicine#how does PrEP work#PrEP HIV infection#how effective is PrEP#PrEP online#PrEP medicine#PrEP medicine for hiv#truvada cost#truvada PrEP#truvada PrEP dosage#truvada PrEP pill#truvada PrEP price#Buy Tenvir EM#tenvir tablet use#tenvir em prep#what is tenvir-em used for#Tenvir EM#Tenvir EM Tablet#Tenvir 300 Mg Tablet#Viraday#Tafero Em Tablet#Tavin Em#PrEP
0 notes
Text
Treating HIV Infection with Tenvir EM Tablet
Tenvir-EM tablet (Tenofovir / Emtricitabine) is an antiviral medicine used to treat patients suffering from human immunodeficiency virus (HIV). It operates by stopping the reproduction of virus cells allowing the immune system to naturally control the infection.
What is Tenvir-EM (Tenofovir / Emtricitabine)?
Tenvir EM Tablet is a generic version of Truvada. Tenvir 300 mg prevents the multiplication of HIV virus in human cells, thus stopping HIV virus from producing new infections. Tenvir-EM Tablet is a combination drug consisting of two antiretroviral drugs, Tenofovir and Emtricitabine, used in the treatment of HIV. It can be used as pre-exposure prophylaxis against HIV. Visit this site www.himsedpills.com for more information.
What is Tenvir EM prescribed for?
HIV infection:
Tenvir-EM is used in the treatment of Human Immunodeficiency Virus (HIV) infection.
Pre-exposure prophylaxis:
This medication is used in combination with safe-sex practices to reduce the risk of sexually acquired HIV infection in adults at high risk.
How should I use Tenvir-EM?
Always follow your physician's instructions while using the Tenvir L Tablets to get the safest and most effective results from treatment. One tablet is usually taken once daily. As HIV treatment, Truvada must be used in combination with other HIV medicines. As PrEP, Truvada should be used in combination with risk-reduction counseling, correct and consistent condom use, regular HIV testing, and treatment of other sexually transmitted infections.

How Tenvir-Em Tablet Works?
Tenvir-EM Tablet is a combination of two anti-HIV medicines Emtricitabine and Tenofovir disoproxil fumarate. They prevent HIV from multiplying, thereby reducing the amount of virus in your body.
Basic facts about HIV
People with HIV can enjoy a long and healthy life by taking antiretroviral treatment, which is effective and available to all.
Regular testing for HIV is important to know your status. HIV is found in semen, blood, vaginal and anal fluids, and breastmilk.
Using external (or male) condoms or internal (or female) condoms during sex is the best way to prevent HIV and other sexually transmitted infections.
If you’re pregnant and living with HIV, the virus in your blood could pass into your baby’s body during birth or afterward through breastfeeding. Taking HIV treatment and becoming undetectable eliminates this risk.
Stages of HIV Infection
Weight loss
Chronic diarrhea
Night sweats
Fever
Persistent cough
Mouth and skin problems
Regular infections
Serious illness or disease.
Dosage of Tenvir EM Tablet?
Adult Dose: One tablet once a day with or without food. Each tablet contains 300 mg tenofovir disoproxil fumarate + 200 mg emtricitabine.
What are the side effects of Tenvir-EM?
Headaches
Dizziness
Nausea or diarrhea
Depression
Mild skin irritation
Changes in location or shape of body fat
Tenvir-Em Tablet Related Warnings?
Pregnancy:
Tenvir-EM Tablet is generally considered safe to use during pregnancy.
Driving:
Tenvir-EM Tablet may decrease alertness, affect your vision or make you feel sleepy and dizzy. Do not drive if these symptoms occur.
Kidney:
Tenvir-EM Tablet should be used with caution in patients with kidney disease. Dose adjustment of Tenvir-EM Tablet may be needed. Please consult your doctor.
The Best Way to Buy Tenvir EM tablet?
Tenofovir is the treatment of serious hepatitis b virus infection and HIV attacks. Tenvir EM is two antiretroviral drugs namely emtricitabine and tenofovir, which are only effective against RNA viruses such as Human beings Immunodeficiency Virus (HIV).
#Tenvir EM#Tenvir EM Tablet#truvada cost#GenMedicare#truvada prep#truvada prep dosage#truvada prep pill#truvada prep price#Buy Tenvir EM#tenvir tablet use#tenvir em prep#what is tenvir-em used for#Truvada#PrEP hiv#prep hiv medicine#how does prep work#prep HIV infection#how effective is prep#prep online#prep medicine#prep medicine for hiv#Himsedpills
0 notes
Text
Right to Medicine
Access to medicine is a fundamental element of the right to health, which is an essential human right and is necessary for living a life in dignity. The right to access medicine should be regardless of one’s economic, social, cultural, religious, or political background according to the United Nations.
However, millions of people are unable to access medicine of good quality in a timely fashion, which is also affordable. This problem is especially prominent in developing countries, but also people in Europe are often unable to afford essential medical treatments or drugs. According to the UN, access to medicine is linked with the principles of equality and non-discrimination, transparency, participation, and accountability. So why is such an essential human right violated to an extent that the WHO declared it as a global issue?
The introduction of systems such as patents and SPC’s, which came into place to allow companies to re-earn the money they lost in the developmental face of a drug, has big negative impacts. Due to the monopoly a company can hold on to a drug for up to 25 years, the prices of such drugs skyrocket, which limits the access of many people as they simply cannot afford to buy it. It also leads to a medicine shortage in many countries, as they are unable to afford to buy the essential drug, limiting the access of medicines such as PrEP in entire countries.
According to a recent study, improving the access to essential medicines could save up to 10 million people each year. Essential for this, is holding pharmaceutical companies accountable for their human right’s responsibility and highlighting the social costs unfair pricing can include.
Especially the inability to afford and access PrEP’s due to the monopoly Gilead has on Truvada comes at a high cost. Many people have to resort to DIY Prep, which can include Pill sharing or smuggling. The reason why people would go to such lengths is to ensure that they are protected is to allow themselves to be at ease during sex. Sexual health is a state of physical, mental, and social well-being in relation to sexuality, and being scared of being infected with HIV can have negative influences on one’s mental health. Studies show that increasing sexual health leads to the reduction of anxiety and depression among the population.
Overall, ensuring access to essential medicine is a human right everyone should be able to have, and the failure to provide it leads to enormous social costs including the suffering and the decrease of mental well being among the population.
4 notes
·
View notes
Text
HIV(AIDS)
HIV stands for human immunodeficiency virus. It is a virus that attacks cells that help the body fight infection, specifically the white blood cells called CD4 cells. HIV destroys these CD4 cells (T cells), making a person more vulnerable to other infections and diseases such as tuberculosis and some cancers. It is spread by contact with certain bodily fluids of a person with HIV, most often spreads through unprotected sex (without a condom or HIV medicine to prevent or treat HIV) with a person who has HIV. It may also spread by sharing drug needles or through contact with the blood of a person who has HIV. Women can give it to their babies during pregnancy or childbirth. First identified in 1981, HIV is the cause of one of humanity’s deadliest and most persistent epidemics.
The human body can’t get rid of HIV and no effective HIV cure exists. So, once you have HIV, you have it for life. However, by taking HIV medicine (called antiretroviral therapy or ART), people with HIV can live long and healthy lives and prevent transmitting HIV to their sexual partners. In addition, there are effective methods to prevent getting HIV through sex or drug use, including pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP).
Without treatment, the infection might progress to an advanced disease stage where it reduces the number of CD4 cells (T cells) in the body, making the person more likely to get other infections or infection-related cancers. Over time, HIV can destroy so many of these cells that the body can’t fight off infections and disease, this stage is called AIDS (acquired immunodeficiency syndrome). However, modern advances in treatment mean that people living with HIV in countries with good access to healthcare very rarely develop AIDS once they are receiving treatment.
Causes:
Scientists identified a type of chimpanzee in Central Africa as the source of HIV infection in humans. Scientists suspect the simian immunodeficiency virus (SIV) jumped from chimps to humans when people consumed infected chimpanzee meat or when they came into contact with their infected blood. Studies show that HIV may have jumped from apes to humans as far back as the late 1800s. Over decades, the virus slowly spread across Africa over the course of several decades and later into other parts of the world. We know that the virus has existed in the United States since at least the mid to late 1970s.
To become infected with HIV, infected blood, semen or vaginal secretions must enter your body. This can happen by having sex, you may become infected if you have any kind of sex with an infected partner whose blood, semen or vaginal secretions enter your body. By sharing needles, sharing contaminated IV drug paraphernalia (needles and syringes) puts you at high risk of HIV and other infectious diseases, such as hepatitis. The risk of HIV transmitting through blood transfusions is extremely low in countries that have effective screening procedures in place for blood donations. Infected mothers can pass the virus on to their babies during pregnancy or delivery or through breast-feeding. Mothers who are HIV-positive and get treatment for the infection during pregnancy can significantly lower the risk to their babies.
How HIV doesn't spread
You can't become infected with HIV through ordinary contact. That means you can't catch HIV or AIDS by hugging, kissing, dancing or shaking hands with someone who has the infection. HIV doesn't spread through the air, water nor insect bites.
Symptoms:
After the first month or so, HIV enters the clinical latency stage. This stage can last from a few years to a few decades. Some people don’t have any symptoms during this time, while others may experience a flu-like illness within 2 to 4 weeks after infection (Stage 1 HIV infection). But some people may not feel sick during this stage. Flu-like symptoms include fever, chills, rash, night sweats, muscle aches, sore throat, fatigue, swollen lymph nodes, or mouth ulcers. Other symptoms may include dark splotches under the skin or inside the mouth, nose, or eyelids, sores, spots, or lesions of the mouth and tongue, genitals, or anus, bumps, lesions, or rashes of the skin, recurrent or chronic diarrhea, rapid weight loss, neurologic problems such as trouble concentrating, memory loss, and confusion, and anxiety and depression.
HIV symptoms at this stage may come and go, or they may progress rapidly. This progression can be slowed substantially with treatment. With the consistent use of this antiretroviral therapy, chronic HIV can last for decades and will likely not develop into AIDS, if treatment was started early enough.
For the most part, infections by other bacteria, viruses, fungi, or parasites cause the more severe symptoms of HIV. These conditions tend to progress further in people who live with HIV than in individuals with healthy immune systems. A correctly functioning immune system would protect the body against the more advanced effects of infections, and HIV disrupts this process.
As with the early stage, HIV is still infectious during this time even without symptoms and can be transmitted to another person. However, the only way to know for sure whether you have HIV is to get tested. If someone has these symptoms and thinks they may have been exposed to HIV, it’s important that they get tested.
For the most part, symptoms of HIV are similar in men and women. However, symptoms they experience overall may differ based on the different risks men and women face if they have HIV. Both men and women with HIV are at increased risk of sexually transmitted infections (STIs). However, women may be less likely than men to notice small spots or other changes to their genitals. In addition, women with HIV are at increased risk of recurrent vaginal yeast infections, other vaginal infections, including bacterial vaginosis, pelvic inflammatory disease (PID), menstrual cycle changes, and human papillomavirus (HPV), which can cause genital warts and lead to cervical cancer.
Diagnosis:
The only way to know for sure if you have HIV is to get tested. Knowing your status is important because it helps you make healthy decisions to prevent getting or transmitting HIV. Testing is relatively simple. You can ask your health care provider for an HIV test. Many medical clinics, substance abuse programs, community health centers, and hospitals offer them too. You can also buy a home testing kit at a pharmacy or online, however, such results should only be considered as a full diagnosis following review and confirmation by a qualified health worker.
Knowledge of one’s HIV-positive status has two important benefits. People who test positive can take steps to get treatment, care and support before symptoms appear, which can prolong life and prevent health complications for many years. And people who are aware of their status can take precautions to prevent the transmission of HIV to others.
HIV can be diagnosed through blood or saliva testing. Available tests include, antigen/antibody tests. These tests usually involve drawing blood from a vein. Antigens are substances on the HIV virus itself and are usually detectable in the blood within a few weeks after exposure to HIV. Antibody tests. These tests look for antibodies to HIV in blood or saliva. Most rapid HIV tests, including self-tests done at home, are antibody tests. Antibody tests can take three to 12 weeks after you're exposed to become positive. Nucleic acid tests (NATs). These tests look for the actual virus in your blood (viral load). They also involve blood drawn from a vein. If you might have been exposed to HIV within the past few weeks, your doctor may recommend NAT. NAT will be the first test to become positive after exposure to HIV. Talk to your doctor about which HIV test is right for you. If any of these tests are negative, you may still need a follow-up test, weeks to months later to confirm the results.
Treatment:
Currently, there's no cure for HIV/AIDS. Once you have the infection, your body can't get rid of it. However, there are many medications that can control HIV and prevent complications. These medications are called antiretroviral therapy (ART). Everyone diagnosed with HIV should be started on ART, regardless of their stage of infection or complications. A person living with HIV can reduce their viral load to such a degree that it is no longer detectable in a blood test. After assessing a number of large studies, the CDC concluded that individuals who have no detectable viral load “have effectively no risk of sexually transmitting the virus to an HIV-negative partner.” Medical professionals refer to this as undetectable = untransmittable (U=U). The person still has HIV, but the virus is not visible in test results. However, the virus is still in the body. And if that person stops taking antiretroviral therapy, the viral load will increase again and the HIV can again start attacking CD4 cells. People living with HIV generally take a combination of medications called highly active antiretroviral therapy (HAART) or combination antiretroviral therapy (cART). This approach has the best chance of lowering the amount of HIV in the blood. There are many ART options that combine three HIV medications into one pill, taken once daily.
There are a number of subgroups of antiretrovirals, such as:
- Protease inhibitors, protease is an enzyme that HIV needs to replicate. These medications bind to the enzyme and inhibit its action, preventing HIV from making copies of itself. These include:
o atazanavir/cobicistat (Evotaz)
o lopinavir/ritonavir (Kaletra)
o darunavir/cobicistat (Prezcobix)
- Integrase inhibitors: HIV needs integrase, another enzyme, to infect T cells. This drug blocks integrase. These are often the first line of treatment due to their effectiveness and limited side effects for many people.
o elvitegravir (Vitekta)
o dolutegravir (Tivicay)
o raltegravir (Isentress)
o Nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs)
- This class of drugs, also referred to as “nukes,” interfere with HIV as it tries to replicate:
o abacavir (Ziagen)
o lamivudine/zidovudine (Combivir)
o emtricitabine (Emtriva)
o tenofovir disproxil (Viread)
o Non-nucleoside reverse transcriptase inhibitors (NNRTIs) that work in a similar way to NRTIs, making it more difficult for HIV to replicate.
There are also emergency HIV pills, or post-exposure prophylaxis
If an individual believes they have been exposed to the virus within the last 3 days, anti-HIV medications, called post-exposure prophylaxis (PEP), may be able to stop infection. Take PEP as soon as possible after potential contact with the virus. PEP is a treatment lasting a total of 28 days, and physicians will continue to monitor for HIV after the completion of the treatment.
People will often use a combination of these drugs to suppress HIV. A medical team will adapt the exact mix of drugs to each individual. HIV treatment is usually permanent, lifelong, and based on routine dosage. A person living with HIV must take pills on a regular schedule. Each class of ARVs has different side effects, but possible common side effects include:
nausea
fatigue
diarrhea
headache
skin rashes
When people get HIV and don’t receive treatment, they will typically progress through three stages of disease. Treatment can slow or prevent progression from one stage to the next. Also, people with HIV who take HIV medicine as prescribed and get and keep an undetectable viral load have effectively no risk of transmitting HIV to an HIV-negative partner through sex.
Stage 1: Acute HIV infection
Within 2 to 4 weeks after infection with HIV, people may experience a flu-like illness, which may last for a few weeks. This is the body’s natural response to infection. When people have acute HIV infection, they have a large amount of virus in their blood and are very contagious. But people with acute infection are often unaware that they’re infected because they may not feel sick right away or at all. To know whether someone has acute infection, either an antigen/antibody test or a nucleic acid (NAT) test is necessary. If you think you have been exposed to HIV through sex or drug use and you have flu-like symptoms, seek medical care and ask for a test to diagnose acute infection.
Stage 2: Clinical latency (HIV inactivity or dormancy)
This period is sometimes called asymptomatic HIV infection or chronic HIV infection. During this phase, HIV is still active but reproduces at very low levels. People may not have any symptoms or get sick during this time. For people who aren’t taking medicine to treat HIV, this period can last a decade or longer, but some may progress through this phase faster. People who are taking medicine to treat HIV (ART) as prescribed may be in this stage for several decades. It’s important to remember that people can still transmit HIV to others during this phase. However, people who take HIV medicine as prescribed and get and keep an undetectable viral load (or stay virally suppressed) have effectively no risk of transmitting HIV to their HIV-negative sexual partners. At the end of this phase, a person’s viral load starts to go up and the CD4 cell count begins to go down. As this happens, the person may begin to have symptoms as the virus levels increase in the body, and the person moves into Stage 3.
Stage 3: Acquired immunodeficiency syndrome (AIDS)
AIDS is the most severe phase of HIV infection. People with AIDS have such badly damaged immune systems that they get an increasing number of severe illnesses, called opportunistic illnesses.
Source: x x x x x x
6 notes
·
View notes
Text
How to buy generic PrEP online in the UK?

PrEP (Pre-Exposure Prophylaxis) reduces the risk of contracting HIV by over 99% and multiple studies have shown that PrEP is the most effective tool for bringing new HIV transmission rates down to zero. To buy PrEP in the UK, you need to go online. PrEP is not available directly from pharmacies. Simply ensure you take the necessary tests before starting PrEP and buy PrEP online to start getting round-the-clock protection from HIV.
What is PrEP and why one should use it?
PrEP is short for pre-exposure prophylaxis which is a biochemical combination of antiretroviral drugs. These drugs are best for those who are at higher risk of being exposed to HIV infection. Taking one pill daily will keep the stress and anxiety of HIV infection at bay. There are also other dosing options which you can look in to.
How does it work?
PrEP is a combination of two antiretroviral drugs tenofovir disoproxil fumarate and emtricitabine. It is important that you take a pill daily or follow a recognised dosing regime so that the presence of these medications in your bloodstream can block HIV infection. According to reports, daily usage of PrEP is over 99% effective in preventing HIV infection. That’s more than condoms.
Benefits of taking PrEP
PrEP is the best decision one can make to avoid HIV infection. People who are at higher risk of getting infected should consider buying generic PrEP online or finding a clinic to supply this. If one of the partners is tested HIV positive then the other partner must buy PrEP as soon as possible to reduce the risk of infection. Taking the PrEP medication daily at the same time has a success rate of over 99%.
It is beneficial for HIV negative people. With a daily dose of PrEP they can stay relaxed and assured about the proactive control over HIV infection. HIV positive people can also get peace of mind by knowing that their partner taking PrEP is well protected.
Who is eligible to take PrEP?
In the UK it is legal to buy or import PrEP. There are free clinics and support facilities that can help you get your HIV tests done in the most confidential way. When you get clinically assessed for your eligibility to take the HIV prevention pills, the next step is to ask yourself “where can I find PrEP?”
How to buy PrEP?
People who are not on clinical trials can buy PrEP online for delivery to the UK. You can find the most reliable and affordable website selling generic PrEP online. The generic PrEP contains exactly the same medication as the brand product. Also, it is legal to buy PrEP in London online.
Top tips to get PrEP online
Online PrEP providers are officially authorized to help people who want to buy PrEP in the UK. You can find online stores selling generic PrEP at the best price. Make sure that the website you are using to order PrEP is producing the genuine drug or importing the drug with adherence to the customs laws in the UK.
When you get PrEP from an overseas seller it is important to order at least one month in advance. Timely delivery is always assured by reputable providers, but still, it is beneficial to buy PrEP before you run out of your dose.
Always try to order from online PrEP stores that deal directly with the manufacturer. The company that is sourcing directly often assures to give the safest and most affordable products.
There are lots of websites that list genuine online pharmacies to buy PrEP in the UK. These online sources are trusted and verified by authorities, so you can be assured that the PrEP you are going to order is totally safe and not fake at all.
Conclusion
PrEP is the best HIV infection prevention method. Sexually active people who are at high risk of HIV infection must get their tests done before buying PrEP. Affordable and generic PrEP can easily be found online. It is legal to buy PrEP in the UK via an online PrEP provider. YThe tips mentioned in this post solve questions like how to buy PrEP and where to buy it in London and the UK.
1 note
·
View note
Text
10 Things You Should Know About Condoms for National Condom Month
The American Sexual Health Association (ASHA) recognizes February as National Condom Month. Condom awareness and education is always important, but it seems especially timely right now given that rates of condom use appear to have dropped during the COVID-19 pandemic. In this post, I’ve compiled a set of 10 facts and statistics worth knowing about condoms.
1.) With perfect use, condoms are 98% effective at preventing pregnancy. However, perfect use isn’t often achieved in the real world due to human error. When we consider typical use—what happens in reality—the effectiveness rate drops to 82%. What this means is that, in practice, 18 out of 100 women who use condoms regularly over the course of a year will end up pregnant.
2.) If you’re surprised by the 82% typical use rate, you’re not alone. Research suggests that most people overestimate the effectiveness of condoms at preventing pregnancy, which is why we need educational efforts like National Condom Month.
3.) One of the biggest reasons condoms aren’t as effective as people think they are is because many of us don’t always use them correctly or consistently. For instance, studies of college students have found that as many as 38% report having waited until after starting intercourse to put a condom on, and as many as 14% report having taken a condom off before intercourse was over. For more on common condom use errors, check out this infographic. To learn about proper condom use techniques, check out this handy page from the CDC.
4.) In addition to making condom use errors, another reason for the low typical use effectiveness rate is that people sometimes use condoms that don’t fit them well. Many fail to realize that condoms are not a “one-size-fits-all” device. Research has found that poor-fitting condoms are linked to a greater risk of breakage and of people with penises forgoing condoms altogether. Keep in mind that condoms come in different sizes and thicknesses, so shop around for one that fits you (or your partner) well.
5.) Buying condoms that fit well and learning how to use them correctly can reduce the risk of error; however, remember that even with perfect use, condoms aren't 100% effective. If unintended pregnancy is a concern for you or your partner, consider using multiple methods of birth control simultaneously, such as combining condoms with the pill or another hormonal contraceptive. In doing so, you can also capitalize on the STI-preventative benefits of condoms at the same time.
6.) Although condoms are often lamented for reducing sensation, some studies suggest that they don’t necessarily have to take all of the fun out of sex. Research has found that, on average, condom users and non-users report no difference in how pleasurable their most recent sexual event was or in their likelihood of reaching orgasm. That said, if you find that condoms do reduce sensation for you, you might consider experimenting with different types of condoms and/or adding a drop of lubricant inside the condom before slipping it on.
7.) Condoms aren’t used during most acts of sexual intercourse today. In a national U.S. survey in which participants were asked to report their condom use rates during their last 10 experiences with vaginal and anal intercourse, overall usage rates were 25% for men and 22% for women during vaginal sex, and 26% for men and 13% for women during anal sex. Keep in mind that these are overall rates and that they vary somewhat across different groups. For example, rates are higher among adolescents and unmarried adults compared to older adults and those who are married.
8.) Rates of condom use have dropped in recent years. For example, among teens, the number who reported using a condom the last time they had intercourse dropped from 59% to 54% between the years 2013 and 2017. During the same time period, condom use rates also declined among adult men who have sex with men, but this group experienced an even steeper drop. What accounts for the decline? There are probably several factors at play, including increased usage of long-lasting reversible contraceptives, the rise of HIV prevention drugs like PrEP, and changes in overall sexual activity patterns. To learn more about the factors that might be contributing to lower rates of condom use, check out this article.
9.) In the past, animal intestines were the most popular material used for making condoms. Today, some condoms are still made from this (e.g., Naturalamb); however, these condoms have largely fallen out of favor because they are costlier to produce than latex. Plus, while they may be effective at preventing pregnancy, animal membranes are too porous to serve as an effective barrier to most STIs. Learn more about the history of condoms in this video.
10.) Some people don’t realize this, but in addition to the traditional condom that goes over the penis (often referred to as the “male condom”), there is also an internal condom that lines the interior of the vagina or anus. This product was formerly known as the “female condom”; however, it was recently rebranded as the “internal condom” to make it gender neutral and to reflect the fact that it can be used for both vaginal and anal sex.
Want to learn more about Sex and Psychology? Click here for more from the blog or here to listen to the podcast. Follow Sex and Psychology on Facebook, Twitter (@JustinLehmiller), or Reddit to receive updates. You can also follow Dr. Lehmiller on YouTube and Instagram.
Image Source: 123RF/place4design
You Might Also Like:
Nonconsensual Condom Removal: How Common is “Stealthing?”
Why You Should Take Your Time When Putting On A Condom
Things Guys Say To Avoid Using Condoms
5 Common Myths About Sexually Transmitted Infections
from Meet Positives SMFeed 8 https://ift.tt/3cXbh15 via IFTTT
0 notes
Text
10 Things You Should Know About Condoms for National Condom Month
The American Sexual Health Association (ASHA) recognizes February as National Condom Month. Condom awareness and education is always important, but it seems especially timely right now given that rates of condom use appear to have dropped during the COVID-19 pandemic. In this post, I’ve compiled a set of 10 facts and statistics worth knowing about condoms.
1.) With perfect use, condoms are 98% effective at preventing pregnancy. However, perfect use isn’t often achieved in the real world due to human error. When we consider typical use—what happens in reality—the effectiveness rate drops to 82%. What this means is that, in practice, 18 out of 100 women who use condoms regularly over the course of a year will end up pregnant.
2.) If you’re surprised by the 82% typical use rate, you’re not alone. Research suggests that most people overestimate the effectiveness of condoms at preventing pregnancy, which is why we need educational efforts like National Condom Month.
3.) One of the biggest reasons condoms aren’t as effective as people think they are is because many of us don’t always use them correctly or consistently. For instance, studies of college students have found that as many as 38% report having waited until after starting intercourse to put a condom on, and as many as 14% report having taken a condom off before intercourse was over. For more on common condom use errors, check out this infographic. To learn about proper condom use techniques, check out this handy page from the CDC.
4.) In addition to making condom use errors, another reason for the low typical use effectiveness rate is that people sometimes use condoms that don’t fit them well. Many fail to realize that condoms are not a “one-size-fits-all” device. Research has found that poor-fitting condoms are linked to a greater risk of breakage and of people with penises forgoing condoms altogether. Keep in mind that condoms come in different sizes and thicknesses, so shop around for one that fits you (or your partner) well.
5.) Buying condoms that fit well and learning how to use them correctly can reduce the risk of error; however, remember that even with perfect use, condoms aren't 100% effective. If unintended pregnancy is a concern for you or your partner, consider using multiple methods of birth control simultaneously, such as combining condoms with the pill or another hormonal contraceptive. In doing so, you can also capitalize on the STI-preventative benefits of condoms at the same time.
6.) Although condoms are often lamented for reducing sensation, some studies suggest that they don’t necessarily have to take all of the fun out of sex. Research has found that, on average, condom users and non-users report no difference in how pleasurable their most recent sexual event was or in their likelihood of reaching orgasm. That said, if you find that condoms do reduce sensation for you, you might consider experimenting with different types of condoms and/or adding a drop of lubricant inside the condom before slipping it on.
7.) Condoms aren’t used during most acts of sexual intercourse today. In a national U.S. survey in which participants were asked to report their condom use rates during their last 10 experiences with vaginal and anal intercourse, overall usage rates were 25% for men and 22% for women during vaginal sex, and 26% for men and 13% for women during anal sex. Keep in mind that these are overall rates and that they vary somewhat across different groups. For example, rates are higher among adolescents and unmarried adults compared to older adults and those who are married.
8.) Rates of condom use have dropped in recent years. For example, among teens, the number who reported using a condom the last time they had intercourse dropped from 59% to 54% between the years 2013 and 2017. During the same time period, condom use rates also declined among adult men who have sex with men, but this group experienced an even steeper drop. What accounts for the decline? There are probably several factors at play, including increased usage of long-lasting reversible contraceptives, the rise of HIV prevention drugs like PrEP, and changes in overall sexual activity patterns. To learn more about the factors that might be contributing to lower rates of condom use, check out this article.
9.) In the past, animal intestines were the most popular material used for making condoms. Today, some condoms are still made from this (e.g., Naturalamb); however, these condoms have largely fallen out of favor because they are costlier to produce than latex. Plus, while they may be effective at preventing pregnancy, animal membranes are too porous to serve as an effective barrier to most STIs. Learn more about the history of condoms in this video.
10.) Some people don’t realize this, but in addition to the traditional condom that goes over the penis (often referred to as the “male condom”), there is also an internal condom that lines the interior of the vagina or anus. This product was formerly known as the “female condom”; however, it was recently rebranded as the “internal condom” to make it gender neutral and to reflect the fact that it can be used for both vaginal and anal sex.
Want to learn more about Sex and Psychology? Click here for more from the blog or here to listen to the podcast. Follow Sex and Psychology on Facebook, Twitter (@JustinLehmiller), or Reddit to receive updates. You can also follow Dr. Lehmiller on YouTube and Instagram.
Image Source: 123RF/place4design
You Might Also Like:
Nonconsensual Condom Removal: How Common is “Stealthing?”
Why You Should Take Your Time When Putting On A Condom
Things Guys Say To Avoid Using Condoms
5 Common Myths About Sexually Transmitted Infections
from MeetPositives SM Feed 4 https://ift.tt/3cXbh15 via IFTTT
0 notes
Text
PrEP Made HIV Prevention Easier—and It’s Getting Even Simpler - WIRED
New Post has been published on https://newsprofixpro.com/theeyesofthe/2019/07/31/prep-made-hiv-prevention-easier-and-its-getting-even-simpler-wired-2/
PrEP Made HIV Prevention Easier—and It’s Getting Even Simpler - WIRED

Theres a very successful little blue pill on the market. Its highly effective, it benefits thousands of people, and it can transform your love life. No, its not Viagra. Its Truvada, also known as pre-exposure prophylaxis (PrEP), and it is 99 percent effective… Read More

Buy Now



Price: $634.99
Item specifics
Condition:
New: A brand-new, unused, unopened, undamaged item in its original packaging (where packaging is
Model:
ec77
Brand:
bestmassage
Country/Region of Manufacture: United States

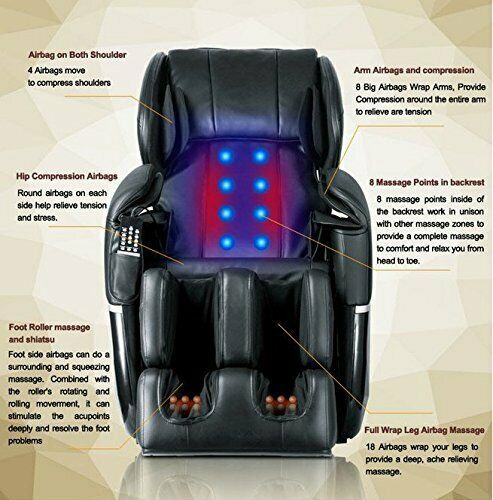



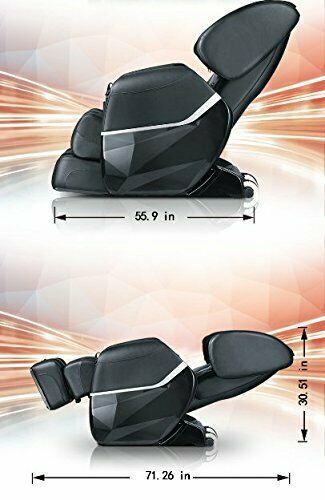





$634.99 End Date: Monday Aug-26-2019 18:52:40 PDT Buy It Now for only: $634.99 Buy It Now | Add to watch list
0 notes
Link

#Genericforce#HIV infection#Truvada#PrEP HIV#PrEP HIV medicine#how does PrEP work#PrEP HIV infection#how effective is PrEP#PrEP online#PrEP medicine#PrEP medicine for hiv#truvada cost#truvada PrEP#truvada PrEP dosage#truvada PrEP pill#truvada PrEP price#Buy Tenvir EM#tenvir tablet use#tenvir em prep#what is tenvir-em used for#Tenvir EM#Tenvir EM Tablet#Tenvir 300 Mg Tablet#Viraday#Tafero Em Tablet#Tavin Em#PrEP#What is PrEP#Buy PrEP HIV Pill#PrEP HIV Prevention
0 notes
Text
PrEP Made HIV Prevention Easier—and It’s Getting Even Simpler - WIRED
New Post has been published on https://newsprofixpro.com/tekamedia/2019/07/31/prep-made-hiv-prevention-easier-and-its-getting-even-simpler-wired/
PrEP Made HIV Prevention Easier—and It’s Getting Even Simpler - WIRED

Theres a very successful little blue pill on the market. Its highly effective, it benefits thousands of people, and it can transform your love life. No, its not Viagra. Its Truvada, also known as pre-exposure prophylaxis (PrEP), and it is 99 percent effective… Read More

Buy Now



Price: $0.99
Item specifics
Condition:
New: A brand-new, unused, unopened, undamaged item in its original packaging (where packaging is
Brand:
Unbranded
Country/Region of Manufacture: China MPN:
Does Not Apply
UPC:
Does not apply











$0.99 End Date: Tuesday Aug-6-2019 0:18:47 PDT Buy It Now for only: $0.99 Buy It Now | Add to watch list
0 notes
Text
At last, a Brexit dividend – shame it’s for the pedlars of fake medicine
Some crimes are just worse than others. When I tell people I research the market for fake and substandard medicines, their most common reaction is: “Fake cancer medicines? That’s horrible. Why would anyone do that?”
The World Health Organization reported earlier this month that fake leukaemia medicine, packaged for the UK market to look like the genuine drug Iclusig, was circulating in Europe and the Americas. The short answer to why anyone would do something as morally awful as this, is of course: to make money. The fake leukaemia drug, containing mostly paracetamol, is being sold for $13,500 a pack – $450 a pill – in the US, or £5,000 a pack in the UK. There is now a far larger market for legal medicines than there is for illegal drugs, such as heroin or cocaine, and there’s a much smaller chance of getting caught. The (genuine) pills are for seriously sick people, so if a patient doesn’t blossom back to health after taking (fake) treatments, doctors generally blame the tumour, not the pill.
Drug dealers are apparently figuring this out – researchers have found traces of ecstasy and Viagra ingredients in pills posing as antimalarial medicine. Falsifiers monitor worried posts on patient forums, clock shortages of specific drugs, weigh up what the most anxious might pay for an online sale, how distracted the national regulator might be, and move in opportunistically to fill the gap.
On all counts, people in the UK are vulnerable right now. The criminals’ business model depends on patients taking risks. And desperate patients will buy medicines from dodgy sources for lots of reasons, our research shows. If the medicine you need isn’t covered by your insurance or health service, you turn to the internet (think of the HIV-prevention pill PrEP in England and Wales, for example). If you’re embarrassed to ask for a prescription, or you don’t have time to go and queue at the surgery, or you distrust the generic medicine on offer at the hospital and would rather buy a well-known brand, or you were redirected to an online pharmacy while self-diagnosing a nasty rash – all these are reasons to step away from the really very safe supply chains that the NHS and most bricks-and-mortar pharmacies in the UK provide.
Recently patients in the UK have mentioned yet another reason for drifting away from safe sources for their medicines: the threat of a no-deal Brexit. Patients are reported to be buying essential medicines wherever they can, stockpiling because they fear shortages after Brexit. It’s a very legitimate fear.
At the moment,EU governments work together through the European Medicines Agency (EMA) to license medicines for use throughout the 28 nations. But there’s no clear legal provision for the circulation in the UK of products authorised by the EMA after 29 March. The UK’s Medicines and Healthcare products Regulatory Agency (MHRA) is doing its best to re-establish itself as an independent regulator; it has cobbled together a 188-page draft amendment to current medicines regulations to stave off the worst effects of crashing out of Europe’s effective regulatory structures. That, together with a diplomatically apocalyptic “explanatory memorandum” is sitting in parliament’s inbox, along with a zillion other pieces of urgent legislation, itching to be reviewed and signed before exit from the EU.
If it doesn’t get signed in time, the fallout may be dire. In 2018, the UK imported close to 15m kg of medicine a month from other EU countries on average, according to HMRC customs figures, some 5m more than it exported to them. That’s an awful lot of products to be in sudden limbo, leaving an awful lot of patients in potential need.
Even if an orderly exit deal is done, delays related to paperwork and border checks will threaten smooth supply, possibly leading to gaps on pharmacy shelves. Though there is every indication that the MHRA is bending over backwards to minimise disruption to companies, shelves will grow even emptier if the regulator is pressured to “take back control” by requiring UK-specific product registration. Some companies will decide the number of patients in the UK doesn’t justify the cost of registering products for rare conditions here; they’ll forgo UK sales, and UK patients may forgo longer or healthier lives. Expensive product registration also pushes up prices, increasing pressure on the NHS and perhaps restricting wide access to expensive new medicines for all Britons.
All of these things would mean even more patients turning to the internet for an affordable version of something they want or need and can’t easily get from their local pharmacy through the NHS. And that, in turn, will make the UK a more lucrative market for criminals flogging fake cures over the internet.
0 notes
Text
“I Still Haven’t Found What I’m LOOKING For”
March 25, 2015 at 4:01pm
You ever get the feeling that something is too good to be true? Well, after watching the first couple of episodes of HBO's "Looking", I finally felt like we finally had a realistic look at the gay community…..well, the white gay community. For a storyline about characters in present day San Francisco, the show didn't have a very diverse cast of characters. I loved that it had some older gay characters and that it involved a group of diverse ages. That's real…..unlike "Queer As Folk" which seemed like a gay fairytale in comparison.
If you have not heard…."Looking" has been officially cancelled. Many are going to say that the interview controversy with openly gay cast member Russell Tovey was the final nail in the coffin…..that his flippant comment about being glad that he was happy his character was more masculine and not feminine like some of the others really shined a bad light on the show.
Yes…that was not a good move, but I don't think that killed the show. It just polarized those who loved the show and those who were on the fence. But in actuality, HBO says that it didn't bring in a large enough audience.
It's my theory that the Tovey controversy made the producers and network "look" at the power of what the show represents and how hungry the gay community is for more stories about their lives. And like the brilliant Kerry Washington said in her GLAAD Award acceptance speech "We need more diverse stories about our lives to be told."
It's a shame that the show has been cancelled because the writing was just getting into some real issues…..aging, losing your best friend, dating someone who is HIV+, PREP, monogamy and Grindr in a relationship. But I think that all of these issues were too close to reality. I posted a few times about the show on facebook and was surprised by a lot of the comments by the 20s to early 30s demographic. Many said they didn't like the show. Some complained about the casual sex. Some felt the storyline didn't move fast enough like "Queer As Folk". Some didn't care about the characters at all because they were living the show.
It's probably going to surprised many why I believe that the show is being cancelled.
Because it is a little too real in content, I think they cancelled "Looking" because an election year is coming. I have a facebook friend who doesn't believe that a TV show can have an effect on politics. For example….SNL, The Daily Show and The Colbert Report (in my opinion) really played a huge part in the 2008 presidential election as well as many daily news issues. Their humor and satire really skewed people like Sarah Palin and John McCain. John Stewart and Stephen Colbert really educated many people about veteran issues and much more over the years.
With the 2016 election approaching, perhaps a TV show that takes a realistic look at our lives would be too big of a responsibility. If folks got up in arms about an opinion on what type of guy man is acceptable, many are going to differ on where we go on the Gay Marriage fight and other issues that gay men face today. Imagine tackling PrEP. That's a tough one to take a stance on. For those who don't know what PREP is, Pre-Exposure Prophylaxis is a drug you can take like a "Morning After Pill" to prevent you from contracting the HIV virus. Sounds like a great prevention pill, huh? Well. some gay men are abusing it so they can just go out and bareback whenever they want. I think this is only going to lead to a nightmare.
Remember a few years ago when there was news of a "Super Strain" of the HIV virus? How did that strain happen? It happened because of the virus had mutated and became resistant to most drugs. With guys abusing PrEP, this could all happen again and be even worst than the last time. Then we have an epidemic on our hands.
PrEP is a great thing to have around if you can afford it. But most don't know the difference between PrEP and PEP. One is a daily treatment to prevent and the other is a treatment to be given shortly after exposure to the virus. For example….I know a bartender who broke up a fight and help one of the guys who was bleeding all over the place. PEP probably saved this bartender's life if that person was HIV+. That's what PrEP is for. It seems really irresponsible for privileged gay men who can afford this drug to be abusing it when this drug could be used in countries where it could save lives.
So, why would HBO want to be responsible for telling that kind of story? I wouldn't want that responsibility! And with the Gay Marriage Supreme Court judgement coming, would you want the responsibility of telling the story if it doesn't pass?
And with the uncertainty of who is running and what will happen in the next election, it is too much weight being put on our images and shows. The Gay Vote is going to be very important in the next election. If for some ungodly reason the US elects a Republican for president (which with all the money being poured into this next election is really possible), it will be many dark days for gays, minorities and the economy.
So, to refer back to Ms. Washington's acceptance speech….."So, when I hear black people say they don't believe in gay marriage…." I really can't believe that many black people are buying into the divisive rhetoric that Right Wingers are spewing. Divide and concur has always worked. Kerri spoke about how they pit women, people of color and the LGBT against each other to keep them all in check. If you don't think that someone else's struggle is not yours, YOU ARE FOOLISH! No one is free or has rights until we all do! So, when someone suffers in the Middle East it effects you just like if it was happening in your neighborhood next door. When a gay man is publicly murdered because of who they are in Uganda, it is just like you being discriminated against because you are black or latino. When a young girl is denied access to an education is just like when a woman only makes 78 cents for every dollar that a man makes.
So….I don't blame HBO for walking away from "Looking". Wouldn't it be great if our so called gay channel, LOGO actually produced and promoted actual shows that told our stories instead of the filler like "Drag Race" and "5 Gays and 1 Girl". But they can't. They don't produce anything. They are owned by VIACOM and I bet if you look real deep into the finances you'll find that it is Republican owned and operated (kinda like FOX which produces most of the top shows on network television).
Dangle the carrot and then take it away…….checkmate!
1 note
·
View note
Text
What happens if a coronavirus vaccine is never developed? It has happened before
New Post has been published on https://apzweb.com/what-happens-if-a-coronavirus-vaccine-is-never-developed-it-has-happened-before/
What happens if a coronavirus vaccine is never developed? It has happened before
As countries lie frozen in lockdown and billions of people lose their livelihoods, public figures are teasing a breakthrough that would mark the end of the crippling coronavirus pandemic: a vaccine.
But there is another, worst-case possibility: that no vaccine is ever developed. In this outcome, the public’s hopes are repeatedly raised and then dashed, as various proposed solutions fall before the final hurdle.
Instead of wiping out COVID-19, societies may instead learn to live with it. Cities would slowly open and some freedoms will be returned, but on a short leash, if experts’ recommendations are followed. Testing and physical tracing will become part of our lives in the short term, but in many countries, an abrupt instruction to self-isolate could come at any time. Treatments may be developed — but outbreaks of the disease could still occur each year, and the global death toll would continue to tick upwards.
It’s a path rarely publicly countenanced by politicians, who are speaking optimistically about human trials already underway to find a vaccine. But the possibility is taken very seriously by many experts — because it’s happened before. Several times.
“There are some viruses that we still do not have vaccines against,” says Dr. David Nabarro, a professor of global health at Imperial College London, who also serves as a special envoy to the World Health Organization on COVID-19. “We can’t make an absolute assumption that a vaccine will appear at all, or if it does appear, whether it will pass all the tests of efficacy and safety.
“It’s absolutely essential that all societies everywhere get themselves into a position where they are able to defend against the coronavirus as a constant threat, and to be able to go about social life and economic activity with the virus in our midst,” Nabarro tells CNN.
Most experts remain confident that a COVID-19 vaccine will eventually be developed; in part because, unlike previous diseases like HIV and malaria, the coronavirus does not mutate rapidly.
Many, including National Institute of Allergy and Infectious Diseases director Dr. Anthony Fauci, suggest it could happen in a year to 18 months. Other figures, like England’s Chief Medical Officer Chris Whitty, have veered towards the more distant end of the spectrum, suggesting that a year may be too soon.
But even if a vaccine is developed, bringing it to fruition in any of those timeframes would be a feat never achieved before.
“We’ve never accelerated a vaccine in a year to 18 months,” Dr. Peter Hotez, dean of the National School of Tropical Medicine at Baylor College of Medicine in Houston, tells CNN. “It doesn’t mean it’s impossible, but it will be quite a heroic achievement.
“We need plan A, and a plan B,” he says.
WHEN VACCINES DON’T WORK
In 1984, the US Secretary of Health and Human Services Margaret Heckler announced at a press conference in Washington, DC, that scientists had successfully identified the virus that later became known as HIV — and predicted that a preventative vaccine would be ready for testing in two years.
Nearly four decades and 32 million deaths later, the world is still waiting for an HIV vaccine.
Instead of a breakthrough, Heckler’s claim was followed by the loss of much of a generation of gay men and the painful shunning of their community in Western countries. For many years, a positive diagnosis was not only a death sentence; it ensured a person would spend their final months abandoned by their communities, while doctors debated in medical journals whether HIV patients were even worth saving.
The search didn’t end in the 1980s. In 1997, President Bill Clinton challenged the US to come up with a vaccine within a decade. Fourteen years ago, scientists said we were still about 10 years away.
The difficulties in finding a vaccine began with the very nature of HIV/AIDS itself. “Influenza is able to change itself from one year to the next so the natural infection or immunization the previous year doesn’t infect you the following year. HIV does that during a single infection,” explains Paul Offit, a pediatrician and infectious disease specialist who co-invented the rotavirus vaccine.
“It continues to mutate in you, so it’s like you’re infected with a thousand different HIV strands,” Offit tells CNN. “(And) while it is mutating, it’s also crippling your immune system.”
HIV poses very unique difficulties and Covid-19 does not possess its level of elusiveness, making experts generally more optimistic about finding a vaccine.
But there have been other diseases that have confounded both scientists and the human body. An effective vaccine for dengue fever, which infects as many as 400,000 people a year according to the WHO, has eluded doctors for decades. In 2017, a large-scale effort to find one was suspended after it was found to worsen the symptoms of the disease.
Similarly, it’s been very difficult to develop vaccines for the common rhinoviruses and adenoviruses — which, like coronaviruses, can cause cold symptoms. There’s just one vaccine to prevent two strains of adenovirus, and it’s not commercially available.
“You have high hopes, and then your hopes are dashed,” says Nabarro, describing the slow and painful process of developing a vaccine. “We’re dealing with biological systems, we’re not dealing with mechanical systems. It really depends so much on how the body reacts.”
Human trials are already underway at Oxford University in England for a coronavirus vaccine made from a chimpanzee virus, and in the US for a different vaccine, produced by Moderna.
However, it is the testing process — not the development — that holds up and often scuppers the production of vaccines, adds Hotez, who worked on a vaccine to protect against SARS. “The hard part is showing you can prove that it works and it’s safe.”
PLAN B
If the same fate befalls a COVID-19 vaccine, the virus could remain with us for many years. But the medical response to HIV-AIDS still provides a framework for living with a disease we can’t stamp out.
“In HIV, we’ve been able to make that a chronic disease with antivirals. We’ve done what we’ve always hoped to do with cancer,” Offit says. “It’s not the death sentence it was in the 1980s.”
The groundbreaking development of a daily preventative pill — pre-exposure prophylaxis, or PrEP — has since led to hundreds of thousands of people at risk of contracting HIV being protected from the disease.
A number of treatments are likewise being tested for Covid-19, as scientists hunt for a Plan B in parallel to the ongoing vaccine trials, but all of those trials are in very early stages. Scientists are looking at experimental anti-Ebola drug remdesivir, while blood plasma treatments are also being explored. Hydroxychloroquine, touted as a potential “game changer” by U.S. President Donald Trump, has so found been found not to work on very sick patients.
“The drugs they’ve chosen are the best candidates,” says Keith Neal, Emeritus Professor in the Epidemiology of Infectious Diseases at the University of Nottingham. The problem, he says, has been the “piecemeal approach” to testing them.
“We have to do randomized controlled trials. It’s ridiculous that only recently have we managed to get that off the ground,” Neal, who reviews such tests for inclusion in medical journals, tells CNN. “The papers that I’m getting to look at — I’m just rejecting them on the grounds that they’re not properly done.”
Now those fuller trials are off the ground, and if one of those drugs works for COVID-19 the signs should emerge “within weeks,” says Neal. The first may already have arrived; the U.S. Food and Drug Administration told CNN it is in talks to make remdesivir available to patients after positive signs it could speed up recovery from the coronavirus.
The knock-on effects of a successful treatment would be felt widely; if a drug can decrease a patient’s average time spent in ICU even by by a few days, it would free up hospital capacity and could therefore greatly increase the willingness of governments to open up society.
But how effective a treatment is would depend on which one works — remdesivir is not in high supply internationally and scaling up its production would cause problems.
And crucially, any treatment won’t prevent infections occurring in society — meaning the coronavirus would be easier to manage and the pandemic would subside, but the disease could be with us many years into the future.
WHAT LIFE WITHOUT A VACCINE LOOKS LIKE
If a vaccine can’t be produced, life will not remain as it is now. It just might not go back to normal quickly.
“The lockdown is not sustainable economically, and possibly not politically,” says Neal. “So we need other things to control it.”
That means that, as countries start to creep out of their paralyses, experts would push governments to implement an awkward new way of living and interacting to buy the world time in the months, years or decades until Covid-19 can be eliminated by a vaccine.
“It is absolutely essential to work on being COVID-ready,” Nabarro says. He calls for a new “social contract” in which citizens in every country, while starting to go about their normal lives, take personal responsibility to self-isolate if they show symptoms or come into contact with a potential COVID-19 case.
It means the culture of shrugging off a cough or light cold symptoms and trudging into work should be over. Experts also predict a permanent change in attitudes towards remote working, with working from home, at least on some days, becoming a standard way of life for white collar employees. Companies would be expected to shift their rotas so that offices are never full unnecessarily.
“It (must) become a way of behaving that we all ascribe to personal responsibility … treating those who are isolated as heroes rather than pariahs,” says Nabarro. “A collective pact for survival and well-being in the face of the threat of the virus.
“It’s going to be difficult to do in poorer nations,” he adds, so finding ways to support developing countries will become “particularly politically tricky, but also very important.” He cites tightly packed refugee and migrant settlements as areas of especially high concern.
In the short term, Nabarro says a vast program of testing and contact tracing would need to be implemented to allow life to function alongside COVID-19 — one which dwarfs any such program ever established to fight an outbreak, and which remains some time away in major countries like the U.S. and the U.K.
“Absolutely critical is going to be having a public health system in place that includes contact tracing, diagnosis in the workplace, monitoring for syndromic surveillance, early communication on whether we have to re-implement social distancing,” adds Hotez. “It’s doable, but it’s complicated and we really haven’t done it before.”
Those systems could allow for some social interactions to return. “If there’s minimal transmission, it may indeed be possible to open things up for sporting events” and other large gatherings, says Hotez — but such a move would not be permanent and would continually be assessed by governments and public health bodies.
That means the the Premier League, NFL and other mass events could go ahead with their schedules as long as athletes are getting regularly tested, and welcome in fans for weeks at a time — perhaps separated within the stands — before quickly shutting stadiums if the threat rises.
“Bars and pubs are probably last on the list as well, because they are overcrowded,” suggests Neal. “They could reopen as restaurants, with social distancing.” Some European countries have signaled they will start allowing restaurants to serve customers at vastly reduced capacity.
Restrictions are most likely to come back over the winter, with Hotez suggesting that COVID-19 peaks could occur every winter until a vaccine is introduced.
And lockdowns, many of which are in the process of gradually being lifted, could return at any moment. “From time to time there will be outbreaks, movement will be restricted — and that may apply to parts of a country, or it may even apply to a whole country,” Nabarro says.
The more time passes, the more imposing becomes the hotly debated prospect of herd immunity — reached when the majority of a given population, around 70% to 90%, becomes immune to an infectious disease. “That does to some extent limit spread,” Offit says — “although population immunity caused by natural infection is not the best way to provide population immunity. The best way is with a vaccine.”
Measles is the “perfect example,” says Offit — before vaccines became widespread, “every year 2 to 3 million people would get measles, and that would be true here too.” In other words, the amount of death and suffering from COVID-19 would be vast even if a large portion of the population is not susceptible.
All of these predictions are tempered by a general belief that a vaccine will, eventually, be developed. “I do think there’ll be vaccine — there’s plenty of money, there’s plenty of interest and the target is clear,” Offit says.
But if previous outbreaks have proven anything, it’s that hunts for vaccines are unpredictable. “I don’t think any vaccine has been developed quickly,” Offit cautions. “I’d be really amazed if we had something in 18 months.”
Source link
0 notes
Text
New California Law May Expand Use Of HIV Prevention Drugs, With Caveats
SACRAMENTO, Calif. — Kellen Willhite was 24 when he learned he’d been exposed to HIV. What followed was, as he describes it, a second trauma: trying to obtain the drugs that could save him before it was too late.
In 2016, a day after Willhite and his then-boyfriend had engaged in unprotected sex, they visited the small offices of Golden Rule Services, a nonprofit community clinic about 7 miles south of the state Capitol.
“I had a gut feeling,” Willhite said. He wanted his boyfriend to be tested. The test result came back positive for HIV, and Willhite learned that he needed to start taking a medication known as post-exposure prophylaxis, or PEP.
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
Sign Up
Please confirm your email address below:
Sign Up
“I was terrified. I was crying because the clock was ticking. You have to start PEP within 72 hours of exposure,” Willhite said. A counselor at Golden Rule advised him about the drug and sent him to an emergency room, where he waited for a long time before being redirected to his primary care doctor for a prescription. The doctor was not in his office.
Eventually, Willhite got his prescription for the full month-long course of treatment, and later he moved to daily doses of anti-HIV pre-exposure prophylaxis, or PrEP. But he remembers the process as “a nightmare.”
A new California law, the first of its kind in the nation, is designed to avoid precisely the kind of stress Willhite endured after learning of his HIV exposure — and to eliminate obstacles for people looking for longer-term protection against the virus.
The law, SB-159, eliminates mandatory doctor visits and bars insurance companies from requiring prior authorization for the drugs. Pharmacists who take a special training course can dispense PEP and PrEP directly to patients without a physician’s prescription, beginning in July.
In signing the bill last month, California Gov. Gavin Newsom applauded the state legislature for “getting us close to ending HIV and AIDS for good.”
Among people working to halt the epidemic, the response has been more guarded. They say bypassing the prescription process is a welcome development, but it does not address all the barriers to access. Unless it is accompanied by cost control, education and relentless outreach to at-risk residents, they argue, it may not make the difference the bill’s supporters hope to see.
“We view this [bill] as one part of a broader access issue,” said Courtney Mulhern-Pearson, director of policy and strategy at the San Francisco AIDS Foundation. “It’s a piece of the puzzle.”
PrEP, marketed and sold by Foster City, Calif.-based Gilead Sciences under the brand name Truvada, is a single pill which, when taken daily, is up to 99% effective at reducing the risk of contracting HIV through sex, according to the Centers for Disease Control and Prevention. The prevention rate on PrEP among those who inject drugs is 74%. (The U.S. Department of Health and Human Services says that PEP, a combination of several different oral drugs, is very effective at preventing HIV infection post-exposure, but “not 100%.”)
Despite PrEP’s effectiveness, fewer than 40,000 of the estimated 220,000 to 240,000 state residents who could use it are taking the medication, according to the California Health Benefits Review Program, which analyzed the state law.
It estimated that PrEP and PEP usage would increase by 2% in the first year of the new law but, after that, barriers such as lack of reimbursement for patient counseling and lab tests could limit increases in its use.
Medical professionals who work with HIV pose tough questions about the law’s potential limitations: How many pharmacies will undertake the training necessary to act as dispensaries, and will they be evenly distributed around the state? What about people who can’t afford it? What will patients do when their maximum allowed prescription-free PrEP dosage — 60 days — runs out?
The 60-day limit was a compromise that induced the California Medical Association and other lobbies to drop their opposition to the legislation. It means those who wish to continue the regimen will have to make primary care visits before their 60-day supply runs out. Doctors say it’s important for people on Truvada to be monitored anyway, given the drug’s potential side effects on kidney and liver function and bone density.
State Sen. Scott Wiener (D-San Francisco), a co-sponsor of the law who revealed in 2014 that he uses PrEP every day to remain HIV-negative, noted that there are places in California where getting a prompt doctor’s appointment can be difficult. Being able to start PrEP or PEP without a prescription at least buys some time, he said.
One thing the law cannot address is how to get the drugs to the people at the highest risk: black and Latino men who have sex with men. Those two groups have the highest rates of new HIV cases nationally.
As the executive director of a nonprofit that offers free HIV testing, Clarmundo Sullivan says he works consistently with clients who aren’t even aware of the anti-HIV drug regimens PrEP and PEP, much less how to access them. (Mark Kreidler for California Healthline)
“This legislation is really, really important, but it’s slightly negligent in its approach,” said Clarmundo Sullivan, executive director of Golden Rule Services, where Kellen Willhite first learned he’d been exposed to HIV. “We have to do a better job of educating and reaching out to that high-risk community, to demystify what PrEP is. We’re still seeing very low uptake among people of color.”
An important factor behind the low use, and not just for people of color, is the cost of PrEP. The full price for Truvada is nearly $20,000 a year, and although Gilead and many states have programs in place to help defray the cost, a lot of people still have trouble affording it.
Willhite, who initially had a copay of $40 for PrEP with insurance he got through his mother, now has similar copays on an employer plan — and he knows he’s lucky. “I know people who are paying hundreds of dollars a month,” said Willhite, who now works at Golden Rule, three years after he first walked in there worried about HIV.
The month-long regimen of PEP runs between $600 and $1,000 without insurance.
Another financial hindrance, one built into the law, is a requirement to show you have tested negative for HIV within the past seven days before you can obtain PrEP without a prescription.
Golden Rule Services tests patients for free, as do many nonprofit clinics and county health departments in California. “But how many people in the community even know that?” Sullivan said. “Some of our clients are sharing with us that it’s costing them up to $250 to get an HIV test at certain places.”
There are other potential obstacles. A California Department of Insurance investigation found this year that some life, disability and long-term care insurance companies were denying coverage to people on PrEP, or hiking their premiums, which could have a chilling effect on its use.
In the end, said Golden Rule’s Sullivan, only aggressive outreach will lead to wider use of HIV-prevention medications. “It takes time, it takes money, it takes vulnerability, because you’re sharing very, very sensitive information,” he said. “The bureaucracy that’s involved has frustrated a lot of people.”
This KHN story first published on California Healthline, a service of the California Health Care Foundation.
from Updates By Dina https://khn.org/news/new-california-law-may-expand-use-of-hiv-prevention-drugs-with-caveats/
0 notes
Text
Trump’s bid to wipe out AIDS will take more than a pill
New Post has been published on https://thebiafrastar.com/trumps-bid-to-wipe-out-aids-will-take-more-than-a-pill/
Trump’s bid to wipe out AIDS will take more than a pill
President Donald Trump’s plan to eradicate HIV transmission will require extending access to the most vulnerable Americans. | Chris Jackson/Getty Images
health care
People who are still at risk have complex, unmet social needs.
COLUMBIA, SOUTH CAROLINA — If President Donald Trump’s ambitious plan to wipe out HIV transmission in America by 2030 is to have any chance of success, it will have to reach people like Kwanna Dingell’s mother.
In April,she walked into an emergency room in rural South Carolina seven times — and seven times she was refused care. That final time, the hospital called the police, who put the homeless woman in jail. From there, she went back to the same hospital, where she spent 18 days in the psychiatric ward.
Story Continued Below
Frantic, Dingell finally tracked her mother down with help from the police, only to find that a hospice nurse was also looking for her, wanting to alert the hospital that Dingell’s mother had HIV. She had kept it a secret — from her daughter, from her community and from health care providers, who may have treated her quite differently had they known she was probably suffering from HIV-related dementia.
Public health now has the tools to eradicate HIV — medicines to protect people from getting the virus, to prevent those who have it from infecting others, and to prolong lives by decades. But it takes a lot more than a pill to reach the “hard to reach” populations, people who 40 years into the epidemic are still most at risk of contracting and spreading HIV/AIDS. These are the stigmatized, the marginalized, the poor, the homeless, the afraid, the addicted and the mentally ill, in rural communities and urban cores.
Unlike the 1980s, the faces of the AIDS crisis in 2019 are not found so much in San Francisco’s Castro district or New York’s Greenwich Village. They are disproportionately black men, and increasingly black women. Some are gay or bisexual and closeted in hostile communities. Many are at risk because of drug addiction and mental illness, in small rural southern towns or in troubled inner cities like Baltimore. Coping with HIV is one of only many challenges in their difficult, chaotic lives.
Eradicating the virus will need to look less like a science experiment and more like a broad social welfare program.
In his budget for fiscal 2020, Trump requested an additional $291 million for his AIDS program and plans to start some work even sooner by drawing about $30 million from the Minority AIDS Initiative fund.
But many doing HIV/AIDS prevention work worry that the approach may not be broad enough, and that rules on spending public funds may not be flexible enough. That’s particularly the case given a trend in some areas, like South Carolina, of moving away from community-based organizations that provide outreach, education and support services like van rides for rural patients who need to travel long distances to get to a clinic. Instead, the money and energy are going to a narrower medical approach.
Wiping out HIV does require pills — affordable pills. And getting people to take the pills and keep taking them day after day also requires support services. It would ideally involve a full-scale attack on poverty, racial, economic and educational inequalities and long-held stigmas against people who have acquired a disease associated with sex, drugs, and risky behavior.
“In some ways we’ve skimmed off the easiest [HIV] populations to take care of,” said Kyle Murphy of AIDS United, a nonprofit that has focused on getting grant money into hard to reach communities where, he said, people still in need of HIV services require more and different kinds of assistance.
The people that the U.S. is missing for HIV care now aren’t so obvious because they’re often not interacting with the health system or proactively reaching out for care, saidAmanda Rosecrans, who directs Baltimore City Health Department’s HIV and hepatitis C sexually transmitted disease clinics. These patients are hard to find and hard to keep in care.
Baltimore recently started up a mobile STD clinic that it sends out with the city’s needle exchange vans. Most people who come to the clinic are using drugs, engaged in commercial sex work or both. Many have never had health insurance (though they may be eligible now for free or subsidized coverage under the Affordable Care Act) and haven’t had health care in a long time, Rosecrans said.
The clinic has helped reach them but has not always enabled the consistent, ongoing relationships needed to keep them on AIDS meds for years. “It’s been really hard to keep those people engaged,” she said. “All of the patients who we’ve tried to do HIV treatment on the vans so far, we’ve sort of lost contact with for one reason or another — incarceration, folks that are homeless.” The city is starting to think of some ideas it could test to stay in contact with these people, like giving them mobile phones, but government grants that let them buy pills don’t necessarily let them buy phones.
Given recent biomedical and public health advances, the Trump administration sees the time as ripe for an audacious plan to slash new HIV infections in the U.S. by 75 percent within five years, and by 90 percent within 10. Medicines, if made affordable and taken correctly, can suppress the virus to undetectable levels, reducing transmission. Pre-exposure prophylaxis, or “PrEP,” drugs can prevent infection in people at high risk. New tools let public health officials pinpoint transmission hot spots, and swoop in where HIV infections are spreading most rapidly.
“Today, we have the right data, the right tools and the right leadership, to end the HIV epidemic,” HHS Secretary Alex Azar said at the National HIV Prevention Conference in March.
But for many in rural South Carolina or hard-hit parts of Baltimore — two of the areas specifically targeted in the Trump plan because of high rates of new infections — fancy science isn’t the silver bullet that Washington bureaucrats count on.
“A lot of our clients … are below the poverty level, well below the poverty level. Most are zero-income and a lot of their issues are bigger than HIV,” said Selena Lowery, the lead case manager at the South Carolina HIV Council’s Wright Wellness Center in Columbia, South Carolina, which has been helping the Dingell family. Like her counterparts in Baltimore, she can get people into HIV treatment — but keeping them there means also addressing transportation, employment, and often underlying drug addiction or mental illness.
“If you had to think about, ‘Am I going to go to the doctor or go stand on line for day labor,’ I’m going to go to day labor because I have to eat, and I have to have some place to lay my head tonight,” she said. “If we’re not treating the whole person it’s not going to work.”
But money is limited for HIV-focused organizations — community-based organizations, not just medical clinics — to address these larger needs. The federal Ryan White program mandates that grantees spend 75 percent of their money on core services like doctor’s visits and medication. That leaves 25 percent for emergency financial assistance, transportation or food. Lowery said it’s not enough.
Lenatte Henry, the Wright Wellness Center’s outreach specialist, who spends a lot of her time trying to get the 20 to 30 percent of clients who drop out of HIV treatment back into care, says the main reasons people stop treatment are addiction, homelessness and general financial troubles. Everyday struggles leave little room for keeping track of pills and getting to appointments.
When Wright runs mobile testing clinics in and around Columbia, at sites like a rundown motel where sex workers or people recently released from prison stay, the people who show up are more motivated by the offer of a $5 or $10 gift card — enough for food for a day — than learning about their HIV status.
Even when people are identified as high-risk, getting them on PrEP is hard — only about one in five of the estimated 1.1 million eligible people are taking Gilead’s drug, which costs $20,000 a year. And the racial gap is huge. Black men and women account for about 40 percent of Americans who should be offered PreP, but make up only about 11 percent of current users. White Americans make up about a fourth of those who should be offered PrEP but comprise nearly 70 percent of those who get it.
Gilead in May announced it would donate enough PrEP medicine to treat 200,000 at-risk people for a decade. But critics fear the largess may slow down the adoption of cheaper generics. They contend that Gilead — whose high profits were just the subject of a critical House oversight hearing — could do a lot more to wipe out HIV simply by lowering its drug prices. The company was dogged by similar criticism for its high-priced hepatitis C medications. The PrEP drug Gilead sells for $1,600 a month in the U.S. goes for just hundreds of dollars a month in Europe. Many countries already have access to cheaper generics.
Money is only one obstacle to broad adoption of PrEP. The federal Ryan White program, which serves low-income and uninsured people with the HIV virus, does include wraparound services like emergency housing or mental health. But that law went into effect about 30 years ago to help people infected with the virus; it hasn’t been modified to help those who are high-risk but HIV negative.
Baltimore’s Rosecrans also wants federal funding to be more flexible, so clinics aren’t so boxed in by a patient’s HIV status. Her clinics can’t provide wraparound services for PrEP patients, nor, under current rules, can she combine services all on one site, which would eliminate obstacles for patients who traipse from one place to another to get health care, support and assistance.
And government funding has moved away from AIDS education and efforts to combat stigma, on the theory that the country has largely gotten the basic facts about HIV treatment and transmission. But in wide swathes of the country that’s not the case. People still think AIDS is an untreatable, fatal disease that can be spread through casual contact.
“It’s like going back in time,“ Dingell said of her mother’s community. “They look at it like it’s still the 1980s. They don’t know that there are resources there, that there’s education, that they can live a healthy life. They have no idea, and unfortunately my mother is one of those people.“ Her aunt, she added, always Lysol-ed the bathroom each time her mother visited, afraid of catching the virus. She was one of the few in the family who either knew, or at least suspected, that the woman had AIDS.
Similar anecdotes abound in support groups run by the Wright clinic for HIV-positive women and among gay, bisexual and transgender men. They tell of being shunned by their churches, and of being told, inaccurately, that AIDS is a death sentence and that they should not have babies because they too will die. One woman, Susan Kitchens, said her physician kicked her out of his office a few years ago for fear his other patients would drop him if word got out that he had treated her. Many said their doctors had never heard about PrEP.
“I’ve literally heard physicians say, ‘If that’s the lifestyle you want to live, why do I care if you live or die,’” said one man, who asked to use only his first name, Stephen, because of the stigma he still endures.
The Wright Center has found that stigma, while detrimental to all, has a higher impact on blacks than on whites. Whites feared social isolation; people of color worried about all that plus basic economic survival and losing their jobs, said Wright’s executive director, Bambi Gaddhist.
For children it can be worse. Some have been “cast out of their home” for being gay or bisexual or transgender. They can’t even begin to talk about HIV/AIDS, she said. The abstinence-only education that dominates schools leaves a lot unsaid about HIV prevention and treatment, and there isn’t much funding for what Gaddhist terms AIDS “Basic 101,” based in trusted community settings.
Similar fears play out in Baltimore; people travel across the city to visit an STD clinic to avoid being recognized.
Going directly to the community can make a big difference, Rosecrans said.
“A lot of times patients have had really negative experiences with health care settings, especially if going to an emergency room and getting labeled a drug user. … So, they come to us and we’re nice to them and it keeps them coming back over time,” she said.
But in South Carolina and among HIV workers there are fears that community outreach is being increasingly decimated, not built up.
In recent years South Carolina has cut off funding for Wright’s work with churches; the CDC no longer lets the organization use its grants to lease vans to transport patients to keep them in HIV treatment. There’s a broader shift of funding away from community-based organizations focused on prevention, unless they directly provide medical care. Grant applications often exclude rural jurisdictions because they don’t have the density of disease necessary to get the “bang for the buck” the federal government wants, added Nic Carlisle, the executive director of the Southern AIDS Coalition.
“We have to be really careful,” said Carlisle. “There’s a lot of talk about using federally qualified health centers and the whole medical model,” but the Trump plan is silent on support services that are often better managed by smaller community-based organizations.
“They are nimble, they end up doing more with less, they end up looking more like the communities they are trying to serve. … Unfortunately I think the emphasis on this sort of medical model or medicalization has really disadvantaged them,” he said.
In a recent conversation, Dingell said her mother was still in the hospital. She was barely eating; Dingell wasn’t sure how much longer she would survive. Like many in South Carolina, Dingell had not heard of Trump’s plan to eradicate HIV and was skeptical of how her mother’s community would react. More awareness and services like housing could eventually make a difference. But it’s likely too late for her family.
In an ideal world, “if she took her medicine and didn’t have a stigma around this disease she could have lived a healthy life, she wouldn’t be in this situation. And you know, if they treated her with dignity and treated her as if she was a person with rights to be treated medically,” she said. “But that’s not her reality.”
Read More
0 notes