#Biliary System
Explore tagged Tumblr posts
Text
#Gallbladder Function#Gallstones#Cholecystectomy#Bile Production#Bile Storage#Liver and Gallbladder#Gallbladder Disease#Cholecystitis#Gallbladder Pain#Fatty Liver#Gallbladder Removal#Ultrasound Gallbladder#Digestive Health#Biliary System#Cholelithiasis#Gallbladder Infection#Post-surgery Gallbladder Care#Gallbladder Polyps#Jaundice and Gallbladder#Gallbladder Function Tests#health & fitness
1 note
·
View note
Text
The average weight of a gallbladder in a healthy adult ranges from 2 to 3 ounces (50 to 85 grams). Situated beneath the liver, this small organ plays a vital role in digestion by storing bile, which aids in breaking down fats. Factors like age, gender, and overall health can influence gallbladder weight. Surgical removal, or cholecystectomy, is a common intervention for issues like gallstones. Understanding the normal weight of the gallbladder provides insights into digestive system health, and variations may indicate underlying conditions impacting this essential organ's function.
#Gallbladder Health#Digestive System#Cholecystectomy#Bile Function#Gallstones#Organ Weight#Biliary System
0 notes
Text
MCQS Biliary Tract & Gallbladder/ Medical Exam/Medical Student Exam/ Mrcs/FRCS/ USMLE Qs / No1doctor
#Gallbladder #Biliary_Tract #bile #biliary #infection #surgery #MCQs #Exam #medical #doctor #medical_exam #medical_student #no1doctor #dratef #Mrcs #frcs #usmle Please Subscribe to our Channel Like ,Share our Videos Press Alarm Button Free Medical Android applications Follow Us At Social Media Accounts Join our Telegram Group Free Medical Applications can gallbladder problems cause gas, can your…

View On WordPress
#a biliary stricture#biliary apex#biliary apparatus anatomy#biliary atresia#biliary atresia baby#biliary atresia in pediatrics#biliary atresia nursing#biliary atresia osmosis#biliary atresia ultrasound#biliary biliary akha#biliary brush biopsy#biliary brushing#biliary bypass procedure#biliary cirrhosis#biliary colic#biliary drain#biliary system#biliary tract#biliary tree#biliary tree anatomy#dratef#Exam#frcs#medical exam#Mrcs#no1doctor#surgery#usmle
0 notes
Text

Gall Bladder Cancers Treatment in Ludhiana
Get advanced gall bladder cancer treatment in Ludhiana with expert diagnosis and personalized care. Dr. Nitin Behl specializes in cutting-edge therapies for better recovery and health outcomes.
#Gallbladder cancer specialist#Liver and pancreas care#Oncology expert#Tumor treatment#Biliary tract cancer#Endoscopic surgery#Hepatologist in Ludhiana#Minimally invasive cancer treatment#Digestive system cancer#Gastrointestinal oncology
0 notes
Text
The CDC has quietly changed who should AVOID the MMR vaccine.
https://www.cdc.gov/vaccines/vpd/mmr/public/index.html
They now state that ANYONE that “Has a parent, brother or sister with a history of immune system problems” should AVOID THE MMR VACCINE!
What exactly is an 'immune system problem?" Every autoimmune disorder.
* Achalasia
* Addison’s disease
* Adult Still's disease
* Agammaglobulinemia
* Alopecia areata
* Amyloidosis
* Amyotrophic lateral sclerosis (Lou Gehrigs)
* Ankylosing spondylitis
* Anti-GBM/Anti-TBM nephritis
* Antiphospholipid syndrome
* Autoimmune angioedema
* Autoimmune dysautonomia
* Autoimmune encephalomyelitis
* Autoimmune hepatitis
* Autoimmune inner ear disease (AIED)
* Autoimmune myocarditis
* Autoimmune oophoritis
* Autoimmune orchitis
* Autoimmune pancreatitis
* Autoimmune retinopathy
* Autoimmune urticaria
* Axonal & neuronal neuropathy (AMAN)
* Baló disease
* Behcet’s disease
* Benign mucosal pemphigoid
* Bullous pemphigoid
* Castleman disease (CD)
* Celiac disease
* Chagas disease
* Chronic inflammatory demyelinating polyneuropathy (CIDP)
* Chronic recurrent multifocal osteomyelitis (CRMO)
* Churg-Strauss Syndrome (CSS) or Eosinophilic Granulomatosis (EGPA)
* Cicatricial pemphigoid
* Cogan’s syndrome
* Cold agglutinin disease
* Congenital heart block
* Coxsackie myocarditis
* CREST syndrome
* Crohn’s disease
* Dermatitis herpetiformis
* Dermatomyositis
* Devic’s disease (neuromyelitis optica)
* Discoid lupus
* Dressler’s syndrome
* Endometriosis
* Eosinophilic esophagitis (EoE)
* Eosinophilic fasciitis
* Erythema nodosum
* Essential mixed cryoglobulinemia
* Evans syndrome
* Fibromyalgia
* Fibrosing alveolitis
* Giant cell arteritis (temporal arteritis)
* Giant cell myocarditis
* Glomerulonephritis
* Goodpasture’s syndrome
* Granulomatosis with Polyangiitis
* Graves’ disease
* Guillain-Barre syndrome
* Hashimoto’s thyroiditis
* Hemolytic anemia
* Henoch-Schonlein purpura (HSP)
* Herpes gestationis or pemphigoid gestationis (PG)
* Hidradenitis Suppurativa (HS) (Acne Inversa)
* Hypogammalglobulinemia
* IgA Nephropathy
* IgG4-related sclerosing disease
* Immune thrombocytopenic purpura (ITP)
* Inclusion body myositis (IBM)
* Interstitial cystitis (IC)
* Juvenile arthritis
* Juvenile diabetes (Type 1 diabetes)
* Juvenile myositis (JM)
* Kawasaki disease
* Lambert-Eaton syndrome
* Leukocytoclastic vasculitis
* Lichen planus
* Lichen sclerosus
* Ligneous conjunctivitis
* Linear IgA disease (LAD)
* Lupus
* Lyme disease chronic
* Meniere’s disease
* Microscopic polyangiitis (MPA)
* Mixed connective tissue disease (MCTD)
* Mooren’s ulcer
* Mucha-Habermann disease
* Multifocal Motor Neuropathy (MMN) or MMNCB
* Multiple sclerosis
* Myasthenia gravis
* Myositis
* Narcolepsy
* Neonatal Lupus
* Neuromyelitis optica
* Neutropenia
* Ocular cicatricial pemphigoid
* Optic neuritis
* Palindromic rheumatism (PR)
* PANDAS
* Parkinson's disease
* Paraneoplastic cerebellar degeneration (PCD)
* Paroxysmal nocturnal hemoglobinuria (PNH)
* Parry Romberg syndrome
* Pars planitis (peripheral uveitis)
* Parsonage-Turner syndrome
* Pemphigus
* Peripheral neuropathy
* Perivenous encephalomyelitis
* Pernicious anemia (PA)
* POEMS syndrome
* Polyarteritis nodosa
* Polyglandular syndromes type I, II, III
* Polymyalgia rheumatica
* Polymyositis
* Postmyocardial infarction syndrome
* Postpericardiotomy syndrome
* Primary biliary cirrhosis
* Primary sclerosing cholangitis
* Progesterone dermatitis
* Psoriasis
* Psoriatic arthritis
* Pure red cell aplasia (PRCA)
* Pyoderma gangrenosum
* Raynaud’s phenomenon
* Reactive Arthritis
* Reflex sympathetic dystrophy
* Relapsing polychondritis
* Restless legs syndrome (RLS)
* Retroperitoneal fibrosis
* Rheumatic fever
* Rheumatoid arthritis
* Sarcoidosis
* Schmidt syndrome
* Scleritis
* Scleroderma
* Sjögren’s syndrome
* Sperm & testicular autoimmunity
* Stiff person syndrome (SPS)
* Subacute bacterial endocarditis (SBE)
* Susac’s syndrome
* Sympathetic ophthalmia (SO)
* Takayasu’s arteritis
* Temporal arteritis/Giant cell arteritis
* Thrombocytopenic purpura (TTP)
* Tolosa-Hunt syndrome (THS)
* Transverse myelitis
* Type 1 diabetes
* Ulcerative colitis (UC)
* Undifferentiated connective tissue disease (UCTD)
* Uveitis
* Vasculitis
* Vitiligo
* Vogt-Koyanagi-Harada Disease
Wonder how many doctors are paying attention?
~shared from Jodi Wilson
33 notes
·
View notes
Text
How Does The Drug Got Excreted / Eliminated From The Body?
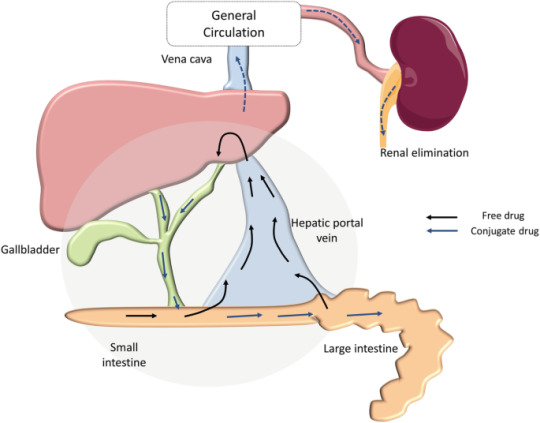
Drug excretion is an important process in pharmacology, encompassing the elimination of pharmaceutical substances from the body. While the ultimate elimination of all drugs is inevitable, the specific pathways involved can vary significantly. Some drugs undergo extensive metabolic transformations before being excreted, while others are expelled from the body in their original form.
The kidneys play a central role in excreting water-soluble substances, effectively filtering them from the bloodstream. Meanwhile, the biliary system handles drugs that remain unabsorbed from the gastrointestinal tract, providing an alternative route for elimination. Although excretion through auxiliary channels such as the intestines, saliva, sweat, breast milk, and lungs is typically minimal, certain volatile anesthetics and residual drug traces in breast milk can have notable impacts, particularly on vulnerable populations such as infants.
Renal excretion constitutes a significant portion of drug elimination, accounting for approximately 20% of the plasma that is filtered through the glomeruli. While most water and electrolytes are reabsorbed back into circulation, polar compounds like drug metabolites are excreted predominantly in urine. However, it’s important to note that renal excretion tends to decrease with age, necessitating careful dosage adjustments for elderly patients to mitigate potential adverse effects.
Numerous factors influence the process of renal excretion, including the extent of protein binding, the degree of drug ionization affecting reabsorption rates, fluctuations in urine pH that can alter excretion dynamics, and the impact of metabolic inhibitors on tubular secretion mechanisms.
Biliary elimination, on the other hand, occurs when drugs traverse the biliary epithelium via active transport mechanisms. However, this process is not without limitations, as transporter saturation can impose constraints on drug excretion rates. Typically, larger molecules containing polar and lipophilic groups are excreted through bile, while smaller molecules tend to favor renal elimination pathways.
In addition to renal and biliary routes, drugs may also be eliminated to varying extents through auxiliary pathways such as saliva, tears, feces, sweat, and exhalation. While the quantities eliminated through these routes are generally minimal, drug excretion in breast milk can pose significant concerns for lactating mothers, potentially exposing nursing infants to pharmacological agents.
Understanding the pharmacokinetic parameters governing drug excretion is paramount for optimizing therapeutic regimens and minimizing the risk of adverse effects. Key parameters include the rate of elimination, clearance, elimination rate constant, and biologic half-life for drugs undergoing first-order elimination kinetics.
In conclusion, drug excretion represents a broad process influenced by a myriad of factors, necessitating comprehensive consideration to ensure the safe and efficacious use of pharmacotherapy.
For medical students navigating the complexities of their studies, Expert Academic Assignment Help serves as a beacon of professionalism and expertise. With a steadfast dedication to excellence and competency, our team provides invaluable support and guidance tailored to your academic needs. Do not hesitate to reach out to us for assistance on your academic journey, email: [email protected]
Your excellence our pride.
#assignment help#medical students#healthcare#nursing school#nursing student#medicine#medication#health and wellness#health#homework help#do your homework#university student#medical school#online writing#academic assignments#academic writing#grad school#pharmacy student#pharmacology#pharmacy technician#pharmacy
24 notes
·
View notes
Text
health update letsgooo:
UGHH i think my fourth procedure of this month was finally 100% successful, which means there will be no more complications!!!! (hopefully!!) 😩 i also think i can finally get rid of the drainage tubes too soon!! 🥰🤞i apparently also got 15 staples across my abdomen and four more down another incision site, so that's fun. it's healing well tho. no more 8/10 pain!! :)
moral of the story? (a little disclaimer/PSA 🥰): all of these complications (drainage tubes, 4 hour long open abdominal surgery, 2 endoscopic procedures, opioid withdrawal from 24/7 use) were 100% my fault. i ignored my gallbladder issues for literal years and ruined my biliary system in the process. all for the purpose of avoiding surgery in the first place 😀 (don't do what i did. don't ignore your health if you are able to treat it PLEASE I'M NOT JOKING LMAO)
i have been in the hospital for 20 days 🙂
#i am finally feeling better now :) mentally and physically yay#tw surgery#tw medical#tw health problems#tw possible sh?? i didn't do anything here for that purpose but i'm adding this to be careful
11 notes
·
View notes
Text
How Phloroglucinol 150 + Trimethylphloroglucinol 150 Suppositories Work in Treating Gastrointestinal Disorders
Gastrointestinal disorders affect millions of people worldwide, causing discomfort, pain, and disruption to daily life. Among the effective treatments for these conditions are phloroglucinol 150 + Trimethylphloroglucinol 150 suppositories, which have gained prominence for their antispasmodic properties. As a leading phloroglucinol 150 + trimethylphloroglucinol 150 suppository manufacturer in Senegal, Centurion Healthcare Pvt. Ltd. is proud to shed light on how these suppositories work and their role in managing gastrointestinal health.

Understanding Phloroglucinol and Trimethylphloroglucinol
Phloroglucinol and trimethylphloroglucinol are active ingredients widely used to relieve spasms in smooth muscles. Together, they form a potent combination that addresses various gastrointestinal issues by reducing spasmodic pain and improving patient comfort.
Key Properties of the Active Ingredients
Phloroglucinol: A spasmolytic agent that relaxes smooth muscles, especially in the gastrointestinal tract. It works by targeting hyperactive muscles, thus reducing contractions.
Trimethylphloroglucinol: A derivative of Phloroglucinol that enhances its efficacy and provides prolonged relief from spasms.
Mechanism of Action
The suppository form of Phloroglucinol 150 + Trimethylphloroglucinol allows for direct absorption into the bloodstream, offering faster relief compared to oral medications. Here is how it works:
Inhibits Muscle Spasms: The active ingredients block the calcium channels in smooth muscle cells, preventing excessive contractions.
Reduces Pain: By relaxing the muscles, the suppositories alleviate pain caused by cramping or spasms.
Targets Specific Disorders: Conditions like irritable bowel syndrome (IBS), colitis, and biliary colic benefit significantly from this treatment.
Applications of Phloroglucinol 150 + Trimethylphloroglucinol Suppositories
Irritable Bowel Syndrome (IBS): IBS is characterized by abdominal pain, bloating, and irregular bowel movements. The antispasmodic action of Phloroglucinol 150 + Trimethylphloroglucinol suppositories helps reduce abdominal discomfort and improve bowel function.
Renal and Biliary Colic: These conditions involve severe pain due to spasms in the urinary or biliary tract. The suppositories provide rapid relief by relaxing the affected smooth muscles.
Postoperative Spasms: Following abdominal surgeries, patients often experience spasms in the gastrointestinal tract. These suppositories are effective in minimizing such discomfort and speeding up recovery.
Why Choose Suppositories?
Suppositories offer several advantages over other forms of medication:
Rapid Absorption: The rectal route bypasses the digestive system, ensuring faster onset of action.
Minimized Side Effects: Unlike oral medications, suppositories reduce the risk of gastrointestinal irritation.
Convenience for Patients with Nausea: Patients unable to take oral medications due to vomiting or nausea benefit significantly from suppositories.
Centurion Healthcare Pvt. Ltd.: A Trusted Partner in Pharmaceuticals
Centurion Healthcare Pvt. Ltd. stands out as a leading name in the pharmaceutical industry in India, renowned for its commitment to quality and innovation. As one of the top pharmaceutical companies in India, we specialize in manufacturing and exporting high-quality medications, including Phloroglucinol 150 + Trimethylphloroglucinol 150 suppositories.
Our Expertise
Phloroglucinol 150 + trimethylphloroglucinol 150 suppository exporter in Senegal: We ensure timely delivery and adherence to international quality standards for our global clients.
State-of-the-Art Facilities: Our advanced manufacturing units adhere to stringent GMP guidelines, ensuring the highest quality products.
Comprehensive Solutions: From research and development to manufacturing and distribution, we cover every aspect of the pharmaceutical value chain.
The Role of Indian Pharma Companies in Global Healthcare
India has established itself as a global leader in the pharmaceutical sector, supplying affordable and high-quality medicines worldwide. Pharmaceutical companies in India, like Centurion Healthcare Pvt. Ltd., are at the forefront of this success story. Here is why:
Affordable Innovation: Indian pharma companies combine innovation with cost-efficiency, making medications accessible to millions.
Global Reach: As a prominent phloroglucinol 150 + trimethylphloroglucinol 150 suppository supplier in Senegal, we exemplify the international presence of Indian pharmaceuticals.
Diverse Product Range: From generics to specialized medications, Indian pharma manufacturing companies in India cater to diverse healthcare needs.
Challenges in Gastrointestinal Health and the Need for Effective Solutions
Gastrointestinal disorders are on the rise globally due to factors like poor diet, stress, and sedentary lifestyles. These conditions require effective and targeted treatments to improve patient quality of life. Phloroglucinol 150 + Trimethylphloroglucinol suppositories address this need by:
Providing Quick Relief: Their rapid absorption ensures faster alleviation of symptoms.
Enhancing Patient Compliance: Easy-to-administer and effective, these suppositories are a preferred choice for many patients.
Reducing Healthcare Costs: By preventing complications and hospitalizations, they offer cost-effective solutions for gastrointestinal care.
Centurion Healthcare Pvt. Ltd.: A Leader among Pharmaceutical Companies
As one of the top 10 pharmaceutical companies in India, Centurion Healthcare Pvt. Ltd. is dedicated to improving global healthcare through innovative products. Our pharma companies in India are known for their commitment to excellence, making us a trusted partner for healthcare providers and patients alike.
Why Partner with Us?
Global Expertise: We have a strong presence in international markets, including Senegal, where we are recognized as a leading phloroglucinol 150 + trimethylphloroglucinol 150 suppository manufacturer in Senegal.
Quality Assurance: Our products undergo rigorous quality checks to meet the highest standards.
Customer-Centric Approach: We prioritize the needs of our clients and patients, ensuring effective and reliable solutions.
The Future of Gastrointestinal Treatment
The pharmaceutical industry is constantly evolving, with new advancements shaping the future of healthcare. As a leader in the pharmaceutical industry in India, Centurion Healthcare Pvt. Ltd. is committed to staying at the forefront of innovation.
Key Trends to Watch:
Personalized Medicine: Tailored treatments based on individual patient needs.
Advanced Drug Delivery Systems: Innovations like sustained-release formulations and targeted therapies.
Global Collaboration: Strengthening ties between Indian pharma companies and international healthcare providers.
Conclusion
Phloroglucinol 150 + Trimethylphloroglucinol 150 suppositories represent a significant advancement in the treatment of gastrointestinal disorders. Their effectiveness in relieving spasms and improving patient outcomes makes them a vital tool in modern healthcare.
As a trusted phloroglucinol 150 + trimethylphloroglucinol 150 suppository exporter in Senegal and one of the top pharmaceutical companies in India, Centurion Healthcare Pvt. Ltd. is proud to contribute to global health through high-quality products. Partner with us to access reliable and innovative solutions for your healthcare needs.
#Pharma manufacturing companies in India#Pharmaceutical companies in India#Pharma companies in India#Phloroglucinol 150 +trimethylphloroglucinol 150 suppository manufacturer#Phloroglucinol 150 +trimethylphloroglucinol 150 suppository exporter#Phloroglucinol 150 +trimethylphloroglucinol 150 suppository supplier#Top pharmaceutical companies in India#Top 10 pharmaceutical companies in India
4 notes
·
View notes
Text
home and so, so tired... 🫠 medical stuff under cut
i got diagnosed with many-a-thing! gallstones, biliary colic, PUD, and pancreatitis. sighs
they gave me morphine and it barely helped. in fact, bc ive never had morphine before, the initial shock of it flushing through my system made me cry lmao. i did Nawt feel better--until i vommed. then i felt much better for a bit, but now i'm not doing well again. but it's not as bad fortunately
3 notes
·
View notes
Text

Renewal Noticed
The gall bladder and bile ducts and associated small glands are a part of the digestive system, distinct from the liver, known as the extrahepatic biliary tree. This study reveals the mechanisms underlying how, like the gut, these components constantly renew their lining cells (epithelium)
Read the published research paper here
Image from work by Serrena Singh and colleagues
Section of Digestive Diseases, Department of Internal Medicine, Yale University School of Medicine, New Haven, CT, USA
Image originally published with a Creative Commons Attribution 4.0 International (CC BY 4.0)
Published in Developmental Cell, October 2023
You can also follow BPoD on Instagram, Twitter and Facebook
#science#biomedicine#immunofluorescence#biology#stem cells#neurons#genetics#liver#bile ducts#galbladder#epithelium#cells#digestion
9 notes
·
View notes
Text
Causes and risk factors in Chronic pancreatitis
Title: Understanding the Causes and Risk Factors of Chronic Pancreatitis
Chronic pancreatitis is a debilitating condition characterized by inflammation and irreversible damage to the pancreas. While the exact cause of chronic pancreatitis can vary from person to person, several factors contribute to its development. By understanding these causes and risk factors, individuals can take proactive steps to minimize their risk and manage the condition effectively.
1. Alcohol Consumption: Chronic alcohol abuse is one of the leading causes of chronic pancreatitis. Excessive alcohol consumption over a prolonged period can damage pancreatic cells, leading to inflammation and scarring. It's essential to moderate alcohol intake and seek help if struggling with alcohol dependence.
2. Genetics: Genetic factors play a significant role in predisposing individuals to chronic pancreatitis. Certain genetic mutations, such as mutations in the PRSS1, SPINK1, and CFTR genes, can increase the risk of developing the condition. Family history of pancreatitis or other pancreatic disorders also elevates the risk.
3. Smoking: Smoking is a well-established risk factor for chronic pancreatitis. The harmful chemicals in tobacco smoke can damage the pancreas and impair its function over time. Quitting smoking is crucial for reducing the risk of developing chronic pancreatitis and improving overall health.
4. Gallstones: Gallstones, which are hardened deposits in the gallbladder, can obstruct the pancreatic duct and lead to inflammation of the pancreas. This condition, known as biliary pancreatitis, can progress to chronic pancreatitis if left untreated. Managing gallstones promptly through medication or surgical removal can help prevent complications.
5. Autoimmune Diseases: Autoimmune conditions such as autoimmune pancreatitis (AIP) can cause chronic inflammation of the pancreas. In AIP, the body's immune system mistakenly attacks the pancreatic tissue, triggering inflammation and scarring. Proper diagnosis and treatment are essential for managing autoimmune-related pancreatitis effectively.
6. Hereditary Factors: In some cases, chronic pancreatitis can be inherited as a familial disorder. Individuals with a family history of the condition are at an increased risk of developing it themselves. Genetic counseling and screening may be recommended for those with a family history of chronic pancreatitis.
7. Hypertriglyceridemia: Elevated levels of triglycerides in the blood, a condition known as hypertriglyceridemia, can contribute to the development of chronic pancreatitis. High triglyceride levels can lead to pancreatic inflammation and damage. Managing triglyceride levels through diet, exercise, and medication can help reduce the risk.
8. Other Risk Factors: Obesity, certain medications, such as corticosteroids and diuretics, and certain medical conditions, such as cystic fibrosis and hypercalcemia, can also increase the risk of chronic pancreatitis. Identifying and addressing these risk factors early on is crucial for prevention and management.
Conclusion: Chronic pancreatitis is a complex condition with multiple contributing factors. By understanding the causes and risk factors associated with the disease, individuals can make informed lifestyle choices and seek appropriate medical care to reduce their risk and manage the condition effectively. It's essential to adopt a holistic approach to health, including maintaining a healthy weight, avoiding excessive alcohol consumption, quitting smoking, and addressing underlying medical conditions, to promote pancreatic health and overall well-being.
#chronic illness#chronic pancreatitis#health#causes and riskfactors#blog posting#health blog#pain management#prevention strategies
2 notes
·
View notes
Text
Trusted Oncological Care With Trusted Hands

It is but natural that the best cancer hospital in Delhi is the right place to find the best oncologist in Delhi. Equipped with the highest qualifications and ably assisted by an efficient support staff, the oncologists at the world-class Indraprastha Apollo Hospital provide cancer patients the best care possible. The top-end facilities, equipment and techniques available to a cancer specialist here go a long way in strongly backing the healing process of every patient.
Besides qualifications and experience, empathy and compassion are equally important qualities to look for in the best oncologist in Delhi. At the Indraprastha Apollo Hospital, each member of the Apollo Cancer Institute is committed to providing cancer patients with every life-saving treatment available. For example, Image Guided Radiotherapy (IGRT), Stereotactic Body Radiotherapy (SBRT), Frameless Stereotactic Radiosurgery (SRS), 3D Conformal Radiotherapy, Intensity Modulated Radiotherapy (IMRT), and High Dose Rate (HDR) Brachytherapy are offered here for early detection of cancer and advanced surgical technology known as da Vinci robotical surgical system help cancer surgeons perform complicated surgeries with ease ensuring best outcome. In addition, the Tumour Board and Group Tumour Board meetings foster discussions between surgical, medical and radiation oncologists as do the Cancer Awareness Programs and counselling sessions offered at the Apollo Cancer Institute.
Follow-up constitutes an important component of treatment and is an integral part of the management protocols carried out by the Apollo Cancer Institute. Early detection and timely management of recurrence is the principle objective of follow-up in cancer management. The best oncologist in Delhi firmly believes this not only enhances survival but improves quality of life of patients.
Take a look at some of the top cancer specialists at Indraprastha Apollo Institute, who would each qualify to be the best oncologist in Delhi:
Dr Anil D’Cruz
MBBS, MS, DNB, FRCS (HON.
With over three decades of experience, Dr D’Cruz is a renowned surgical oncologist focusing primarily on head and neck cancers. His major areas are management of neck metastasis, conservative laryngeal surgery, cancers of the oral cavity, thyroid, quality of life issues and global health.
Dr Manish Singhal
MBBS, MD, DM(AIIMS)ECMO
Dr Singhal’s career spans over twenty years, largely covering all types of chemotherapy, intensive protocols, immunotherapy, hormonal therapy in addition to dealing with oncological emergencies, including medical care of patients.
Dr Dipanjan Panda
MBBS, MD, DM
One of the best medical oncologists in Delhi, Dr Panda’s area of expertise lies in gastrointestinal and hepatic pancreatico biliary malignancy, breast and gynaecological malignancy, lung and head neck cancer, genito-urinary malignancy, lymphoma and myeloma (haematological malignancy) and rare tumours like neuroendocrine tumours.
Dr Shuaib Zaidi
MBBS, MS (SURGERY), DNB (SURGERY), MCH (SURGICAL ONCOLOGY)
The Academic Coordinator and Senior Consultant in the Department of Surgical Oncology, Dr Zaidi has over twenty years of experience as a surgical oncologist. He specialises in the treatment of thoractic cancer, gastrointestinal cancer, PIPAC (Pressurised Intraperitoneal Chemotherapy), breast cancer and complex gynaecologic oncology.
Dr Praveen Garg
MBBS, M.S.(GEN.SURGERY), M.CH.(ONCOSURGERY)
Dr Garg specialises in the diagnosis, treatment and surgical management of malignant conditions in various parts of the body, and has advanced training in parathyroid and thyroid cancer surgeries, breast conservation surgeries, mastectomies and breast tissue reconstructions.
Dr Ruqaya Ahmed Mir
MBBS, DNB
Trained in robotic surgery, Dr Mir routinely performs major oncological resectional surgical procedures for head and neck cancers, lung and oesophageal cancers, major gastrointestinal malignancies, breast and gynaecological malignancies and soft tissue sarcomas.
To get in touch with the best oncologist in Delhi, contact Indraprastha Apollo Hospital
2 notes
·
View notes
Text
Prioritizing Your Liver Health: Finding the Right Specialist in Ludhiana

The liver is a vital organ responsible for numerous crucial functions in the body, from detoxification and metabolism to producing essential proteins. When liver-related issues arise, seeking expert medical attention from a specialized doctor is paramount for accurate diagnosis and effective management. If you reside in Ludhiana or the surrounding region and are looking for a Liver and Pancreas Specialist in Ludhiana or a dedicated Gastro and Liver Diseases Doctor in Ludhiana, understanding the importance of their expertise is the first step towards safeguarding your liver health.
A liver specialist, also known as a hepatologist, is a physician who has undergone specialized training in the diagnosis and treatment of diseases affecting the liver, gallbladder, biliary tree, and pancreas. While gastroenterologists often manage a broad range of digestive system disorders, a specialist with a focus on the liver and pancreas possesses in-depth knowledge and experience in handling complex conditions related to these specific organs. This specialized expertise is crucial for accurate diagnosis, which may involve advanced imaging techniques, blood tests, and sometimes liver biopsies.
Seeking a skilled Liver and Pancreas Specialist in Ludhiana is essential if you experience symptoms indicative of liver problems. These can include jaundice (yellowing of the skin and eyes), abdominal pain and swelling, fatigue, dark urine, pale stools, nausea, vomiting, and a tendency to bruise or bleed easily. These symptoms could point towards various liver conditions such as hepatitis (viral or autoimmune), fatty liver disease (non-alcoholic or alcohol-related), cirrhosis, liver cancer, primary biliary cholangitis, and other less common liver disorders. Timely consultation with a specialist can lead to early diagnosis and intervention, significantly improving treatment outcomes.
The pancreas, although a separate organ, is closely linked to the liver and biliary system in terms of function. Therefore, specialists who focus on liver diseases often have expertise in pancreatic disorders as well. If you experience symptoms like severe abdominal pain (often radiating to the back), nausea, vomiting, and weight loss, it's important to consult a Liver and Pancreas Specialist in Ludhiana who can evaluate both organ systems and identify the underlying cause. Pancreatic conditions can include pancreatitis (acute or chronic), pancreatic cysts, and pancreatic cancer, all of which require specialized management.
Finding the right Gastro and Liver Diseases Doctor in Ludhiana ensures that you receive comprehensive care that considers the intricate relationship between the digestive system and these vital organs. While some gastroenterologists have a particular interest and expertise in liver diseases, a dedicated liver specialist often possesses a more focused understanding of the nuances of liver and pancreatic disorders. They are typically up-to-date with the latest advancements in hepatology and pancreatology, including cutting-edge diagnostic techniques and treatment modalities.
When searching for a liver specialist in Ludhiana, consider factors such as their qualifications, board certifications, years of experience, and patient testimonials. Consulting your primary care physician for referrals can be a valuable step. Additionally, researching online and seeking recommendations from trusted sources can help you identify a Liver and Pancreas Specialist in Ludhiana who aligns with your specific needs. Choosing a doctor with whom you feel comfortable and who communicates effectively is also crucial for a positive treatment experience. Prioritizing your liver health by seeking timely and expert care from a qualified specialist is an investment in your long-term well-being.
#Liver Health#Liver Specialist#Ludhiana Doctor#Gastroenterologist#Dr. Nitin Behl#Liver Treatment#Hepatitis Care#Liver Checkup#Fatty Liver Disease#Digestive Wellness
0 notes
Text
The Physiology Of The Liver
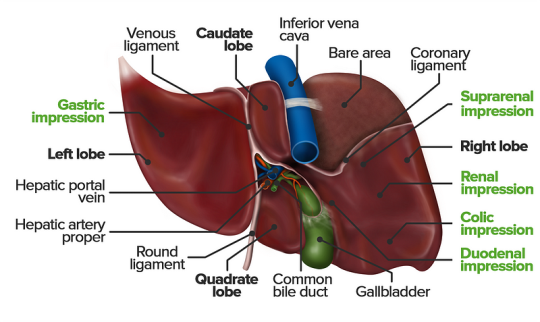
The liver is a vital organ responsible for numerous functions including metabolism, immunity, digestion, detoxification, and vitamin storage. It weighs around 2% of an adult’s body weight and is unique due to its dual blood supply from the portal vein (75%) and the hepatic artery (25%).
Cellular Structure
The liver’s functional unit is the lobule, which is hexagonal in shape. Each corner of the hexagon has a portal triad consisting of the portal vein, hepatic artery, and bile duct. The lobule is composed mainly of hepatocytes, which have distinct apical and basolateral membranes. Hepatocytes are categorized into three zones based on their function and blood supply:
Zone I (periportal region): Closest to the blood supply, involved in oxidative metabolism (e.g., gluconeogenesis, bile formation).
Zone II (pericentral region): Sits between Zones I and III.
Zone III: Farthest from the blood supply, primarily involved in detoxification and biotransformation.
Blood and bile flow in opposite directions within the liver. The space of Disse, between the hepatocytes and the sinusoidal lumen, contains Kupffer cells (macrophages) and Ito cells (fat-storing stellate cells).
Development
The liver develops from endodermal cells of the foregut as the hepatic diverticulum around the fourth week of embryonic development. It undergoes complex differentiation influenced by various pathways (e.g., Wnt/β-catenin, FGF). By the sixth week, the liver participates in hematopoiesis, and hepatocytes begin bile production by the 12th week.
Organ Systems and Functions
The liver interacts with multiple body systems:
Digestive and Metabolic Roles: Aids in digestion, stores fat-soluble vitamins, and handles cholesterol.
Hematological Functions: Produces clotting factors and proteins.
Detoxification: Metabolizes drugs and other xenobiotics through phase I (oxidation, reduction, hydrolysis) and phase II (conjugation) reactions.
Bilirubin Metabolism: Converts heme to unconjugated bilirubin, then conjugates it for excretion.
Hormonal and Protein Synthesis: Involved in thyroid hormone activation and synthesis of nearly all plasma proteins.
Related Testing
Liver function tests (LFTs), including ALT, AST, bilirubin, alkaline phosphatase, and gamma-glutamyl transpeptidase (GGT), help assess liver health. Imaging techniques like ultrasound, CT, and MRI are also employed to identify liver abnormalities.
Pathophysiology
Cirrhosis results from chronic liver injury (e.g., due to alcoholism, hepatitis B and C), leading to fibrosis and necrosis. It causes symptoms like portal hypertension, coagulopathy, and jaundice. Hepatitis viruses (A, B, C, D, E), autoimmune diseases (e.g., primary biliary cholangitis), and metabolic conditions (e.g., non-alcoholic fatty liver disease) also contribute to liver pathology.
Clinical Significance
Understanding liver physiology helps manage conditions like viral hepatitis, alcoholic liver disease, benign liver lesions, and liver cancers. Early detection through appropriate testing and management strategies is essential for preventing end-stage liver disease and improving patient outcomes
As academic students and researchers navigate the challenges of their assignments and research endeavors, Expert Academic Assignment Help stands ready to provide professional guidance and assistance. Whether you require support with assignment writing, research paper assistance, or essay help, our team of experts is dedicated to helping you achieve academic excellence. Reach out to us today at [email protected] and let us support you on your academic journey. We wish you success and professional excellence.
#medical students#healthcare#nursing school#nursing student#medicine#medical help#academic assignments#university student#medical university#university life#university#studying#study motivation#study blog#studyblr community#study inspiration#studyspo#studyblr#student#study aesthetic#medical student#aesthetic#medical school#case study
2 notes
·
View notes