#Abnormal Smear And HPV
Explore tagged Tumblr posts
Note
Hello, hello! I have a few HPV questions that are kind of convoluted and I've never been given a straight answer, I'm hoping you can help (or at least point me in the right direction).
Is there a definitive pos/neg test for HPV, such as a blood test?
Can someone with one strain of HPV pass it to someone where it then becomes a different strain? For example, my ex had genital warts, which I did not get, but then I went on to have an abnormal pap, and as far as I'm aware it is two different strains of HPV that cause GW and cervical cancer.
If that can't happen, is it possible for someone to pass more than one strain to you where you're only symptomatic for one of them?
And lastly, since I never had GW, had my abnormal cells removed, and haven't been sexually active with anyone since my ex (close to 10 years ago), is it possible that I could have a GW outbreak now? I'm sort of worried about it but I also think it's probably fordyce spots.
Thank you!
hi anon,
thanks for the HPV questions!
for people with a cervix, an HPV test can be performed using cells gathered from the cervix. for people with a penis and prostate there isn't strictly a designated test to detect HPV, but visual inspections can be performed to find abnormalities, and people who have had anal sex can sometimes be tested with an anal Pap smear.
strains of HPV don't turn into different strains. there are nearly 200 stains of HPV, nearly all of which are harmless, but there are 2 that can (but don't always) cause genital warts and 13 that can (but don't always) cause cancers of the cervix, anus, vagina, vulva, penis, and throat. the genital warts strain and the cervical cancer strains do not overlap.
yes, you can have multiple concurrent HPV infections of different strains. not all will be symptomatic; it's possible that none of them will be. most people with HPV will be asymptomatic for the duration of their infection.
after ten years, it's unlikely that you still have HPV. most infections are resolved within about two years, and it sounds as if you haven't had an opportunity to pick up an infection from anyone else.
52 notes
·
View notes
Text
A Primer on Cancer Screenings For Trans People
rebloggable on its own now, hooray. I'm a healthcare quality guy, a preventive care navigator, and I've worked with trans health for almost a decade at this point. I anticipate this info will be harder to get shortly, so go forth, own it, spread it to your elders, etc
for transmascs and trans men:
- if you have not had top surgery or have only had a reduction, you should get mammograms as recommended for cis women. if you are at average risk, this is every 2 years starting at age 40.
- if you have not had top surgery / only reduction and you are at HIGH risk of breast cancer (for example, you have a BRCA mutation, received significant radiation to the chest, or a strong family history of breast cancer), ask your doctor. they will likely want you to start earlier, go more often, and/or get a breast MRI in addition to your mammogram. if you are interested in top surgery, please also talk to your surgeon! if you're at sufficiently high risk, especially if you have a BRCA mutation, it might change the way they do the surgery or the way your results look.
- if you have had top surgery that is NOT a risk-reducing mastectomy, your risk of breast cancer is reduced but not 100% eliminated. (if you have to ask, or if you haven't already discussed this all with your doctor, you didn't get a risk-reducing mastectomy.) it is not usually possible to do a mammogram on someone after masculinizing top surgery because of the limited amount of breast tissue remaining, and it might not be worth it given the reduced risk (not much data out there), so just keep a casual eye out for any lumps and ask your doctor if something pops up.
- if you have a cervix, you should get cervical cancer screening (Pap smears or HPV testing or both) as recommended for cis women. I recognize that pelvic exams suck for trans men for various reasons - if you find them difficult due to pain or dysphoria, consider asking your doctor if you can self-collect the sample, or if they can order just an HPV test so you only have to test every five years. another fun thing about pap smears: if you've been on testosterone for awhile, it may be challenging to interpret pap results - the cells can atrophy the longer you're on T.
- if you have had your cervix surgically removed and you have no history of abnormal pap smears, you no longer need cervical cancer screening - congrats! if you DO have a history of abnormal paps, you will need to continue getting smears of the cuff / vaginal vault left behind until you have three normal tests in a row. then you're free!
for transfems and trans women:
- if you have breasts, you will likely need breast cancer screening. if you are at average risk, as of 2016, the guidelines circulating were a mammogram every 2 years starting at age 50 after being on estrogen for 5 years or more. however, these are old guidelines, and the starting age for cis women was pushed back to age 40 (from 50) after they were released. I've also seen some interesting data that breast cancer risk increases from cis male levels relatively quickly after starting HRT, so
- my personal recommendation is that trans women and transfems, after a length of HRT determined by you and your doctor (5 years seems probably reasonable for average risk, maybe shorter for high risk), roughly follow guidelines for cis women. throw that Dutch study I just linked at them if they complain. trans women may also have a higher incidence of dense breast tissue, which is more challenging to image - make sure you're regular on screening so your medical team can better monitor changes.
- prostate cancer screening should be a discussion between you and your doctor because the risks may not outweigh the benefits for everyone. if you are at average risk and choose to be screened, you should get a PSA test (just a blood test) starting at age 55 and discontinuing at age 70. practically nobody does a digital rectal exam (the physical exam where they stick fingers up you) anymore because the evidence just isn't there for it and a PSA test is easier.
for everyone:
- colorectal cancer screening is so important. especially for Black people and other people of color, who are at higher risk, but for everyone! screening should start at age 45-50 and can be a colonoscopy every 10 years or a FIT (stool sample) test every year.
- you may need other tests depending on other risk factors you might have, your mileage may vary.
- your insurance might complain about paying for a screening that isn't "congruent" with your gender marker. trans women may benefit from strategically changing their gender marker with insurance to F, if it is possible. trans men may benefit from strategically leaving theirs as F, if it is possible and desirable (altho, if you follow my next step, may not be desirable... your mileage may vary). a doctor's office competent in trans care probably knows how to argue your case successfully to insurance in any case.
- in preparation for the possibility that insurance stops covering HRT for trans people, you may wish to ask your doctor to prescribe your HRT under a diagnosis code that is NOT "gender dysphoria." this was commonly done in the past to get hormones covered by insurance. happy to provide some possible codes for you on request, but would prefer not to blast my strategies all over the internet for obvious reasons.
- stop smoking cigarettes, damn it! that is one of the best things you can do to reduce your cancer risk. I know they look cool and they're a way to soothe yourself from the horrors, but get a vape if you must continue using tobacco. (also, most surgeons want you to quit before you have surgery, so if you want surgeries in the future there's no time like the present.)
10 notes
·
View notes
Text
Small health update under the cut!
A little over three weeks ago, I went through a conization surgery due to abnormal cells being found on my cervix (degree CIN3). In the procedure, they removed four pieces of my cervix to try to remove the abnormal cells. The pieces were then sent to a lab to be analyzed for potential cancerous cells, and I just got the results: No cancer cells, and they successfully removed all the abnormal cells!
So now I need to have another Pap smear done in 6 months to make sure that there are no new abnormal cells, and that the HPV infection that caused it is all gone. If that turns out to be all clear, I can go back to having regular Pap smears every 3 years.
This is a massive relief from something that has been stressing me out since I got the results of my last Pap smear back in May (after having the actual Pap smear done in February), and I cannot stress this enough: If you have a uterus, please, please, please don't skip your Pap smears! They are so important and can literally save your life. ❤️
15 notes
·
View notes
Note
what advice would you give to a trans person who is terrified of getting health checks such as pap smears? I'm generally rather touch-averse and that doubled with the dysphoria makes it very scary to think about.
Hi Anon,
This is a topic close to my heart, because I myself am touch-averse and have a trauma response to pelvic examinations. I also want to make sure everyone understands why it's important to get pap smears!
Let's start with what pap smears are, why they're important, and who they are for. Maybe understanding that will be the first step in finding the strength and courage to go through with them.
QUICK ANATOMY & PHYSIOLOGY LESSON - THE PAP SMEAR
What is a pap smear for?
Your cervix is the gateway to your uterus, sitting atop the vagina. It's a thick ring of muscle that is normally closed, opening just a tiny bit for menses to escape (the sensation of the muscle opening is what causes cramps).
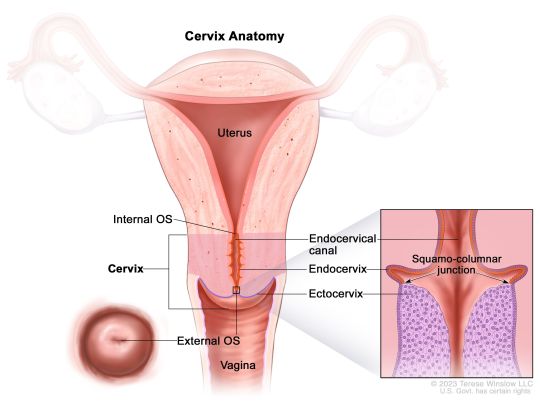
Now, the trouble comes when cervical cells have been infected with a virus called human papillomavirus (or HPV) - especially certain "high-risk" strains. HPV is very common in the human population - almost everyone sexually active has had it at some time, with about 50% of infections being a high-risk type. Most people just clear the virus themselves and never even know. But sometimes, this viral infection will start a process of dysplasia (basically growing weird cells), which can be the start of cervical cancer.
The job of a pap smear is to check the cervical cells for dysplastic changes that indicate things might progress towards cancer, or for the virus itself. (What it looks for specifically depends on your age and previous results, but the process is the same for you). When lesions are found early, they are VERY easily treatable. The pap smear saves thousands of lives every year by preventing cervical cancers.
How is a pap smear performed?
A device called a speculum will need to be inserted into your vagina to hold open the walls of the vagina and allow the provider to visualize the cervix. Once this is in place, a soft brush-like device is passed up through the vagina, pressed against the cervix, and swirled around several times to collect cells. This may feel weird or uncomfortable, but shouldn't cause pain. Most people don't feel it at all, the speculum being the worst part. The whole thing takes about one minute.
Separate from the pap smear, the provider may also perform a bimanual exam, which is when they insert fingers from one hand into the vagina while pressing down on the abdomen, to look for masses, abnormalities or tenderness.

Who needs a pap smear?
CURRENTLY (as of 2023), everyone with an intact cervix who is 21 or older is recommended to get pap smears, regardless of gender identity, sexual orientation, or sexual history. Between ages 21-29, you should go every 3 years, and after age 30, every 5 years (depending on results - if you get a positive, you would need more frequent observation).
If you are older than 21 and have never had any kind of sexual contact with anyone at all (including hands, mouths, or sharing toys!), you can discuss with your provider to see if a modified schedule may make sense based on your risk level.
Note: The HPV vaccine may change these recommendations in the future! I strongly recommend getting the vaccine if you have not already!
---
OK, Anon. With that public service announcement out of the way, let's talk about the real meat of your question.
The best thing I can recommend is to take the time to find a provider you vibe with. Someone with whom you feel safe, with whom you have mutual respect. See if your local LGTBQIA+ support group has recommendations, or if any clinics in your area have providers that specialize in LGTBQIA+ or trauma-informed care. Call and ask providers questions about how they handle people who struggle with pelvic exams. Generally, avoid crusty old men.
A good provider will warn you before ever touching any part of your body, go slowly, and ask permission each time, and stop the second you tense up. A GREAT provider will make you feel in control the whole time - they may let you insert the speculum yourself and not make you use stirrups if they're triggering for you. Medical consent is the same as sexual consent - just because you're disrobed in that room doesn't mean you need to let anyone touch you. You do not have to undergo a pap smear with a provider you don't trust. You are allowed to walk away.
Other things to try:
You can ask for a short-acting anti-anxiety medicine, like Xanax, to take before the visit, provided you've got a ride.
You can bring a companion, or ask for a nurse to hold your hand.
Chat nonstop, tell stupid jokes, or listen to music on headphones, whatever kind of distraction works best for you.
Meditate, practice belly breathing, really focus on full body relaxation, especially of the pelvic muscles
Remind yourself that it's one minute every few years for the piece of mind that you won't get cancer.
Be open to the possibility that it won't be as bad as you're fearing.
Know that you are brave and strong. You can do hard things. You can do anything for one minute.
If any other trans folx out there want to share tips with Anon for how to navigate gynecologic exams, please share!
#reproductive health#sex education#midwifery#gynecologic care#pap smear#pelvic exams#gender affirming care#lgtbqia+#transgender#trans health care
16 notes
·
View notes
Text
this is your sunday reminder to always, always book your routine pap smear if you're due. ya girl is finally hpv negative after being positive and high-risk of cervical cancer for six years because of it. getting tested annually has been uncomfy and nerve-wrecking, but it's also meant any time i had abnormal cells, they were tested immediately. thankfully, none ever went cancerous and i am now officially back to three year routines due to the virus clearing itself. i've also been bumped back down to low risk. these aren't fun, but they're super important. and don't ever be ashamed of your diagnosis! it's also always worth checking with your doctor if you're eligible for the hpv vaccine if you weren't offered it as a kid.
#out of character. ⸻ hope speaks.#tw personal#tw cervical cancer#it might be tmi and non rp related#bt the message is IMPORTANT n ill spread it anywhere i can <3
8 notes
·
View notes
Text
Just when I'm in a good place, life brings me back down.
My smear test results came in today. High-risk HPV was present. My cells are abnormal. "Mild changes," the letter said. I have to go for a colposcopy for further screening.
In a weird way, I'm not surprised. I've spoken here about my menstrual issues. I knew something was wonky in the womb area. I knew the moment I touched the letter what it would say... I just didn't think it actually would.
I'm 29. My last smear was normal. And I've been ignored about my concerns with my periods for 3 years. I only got this smear because someone finally listened and I had the coil fitted. My dr asked since I'd be there with my legs akimbo anyway. I was overdue by a few months because of my period issues. It was pure chance she asked.
And... I'm absolutely fucking terrified.
If you are someone who prays... maybe you would be so kind to include my cervix in them.
And please, for the love of God, go and get your smear test.
#smear test#hpvawareness#go and get your fucking smear test#psa i will be using dark humour to get through this
29 notes
·
View notes
Text
i just realised that i'm probably due for my first cervical screening and was like 'ugh....' but i totally forgot, as of september last year, instead of getting a smear, you can get a swab test from the doctor and do it yourself at home and give it to a lab to evaluate (we have a ton of labs around where we either get referred to to have tests of all sorts done, or if it's an at home sample collection, to give the sample in).
this method is only really recommended if your family has no history of cervical cancer, you have never had abnormal cells, or you've never had high risk of exposure to hpv; it doesn't test for abnormal cells, but it tests for cancer causing hpv strains themselves. and once that is found, then you do the regular cell scrape smear from then on.
so next time i go to the doc, i'll just ask for one of those tests.
7 notes
·
View notes
Text
Cervical Cancer: Understanding the Disease, Prevention, and Treatment

Introduction:
Cervical cancer is a significant health concern affecting women worldwide. It is a type of cancer that develops in the cervix, the lower part of the uterus. In this blog, we will explore the key aspects of cervical cancer, including its causes, risk factors, prevention strategies, early detection methods, and treatment options.
Causes and Risk Factors:
The primary cause of cervical cancer is persistent infection with high-risk types of human papillomavirus (HPV), a sexually transmitted infection. Other risk factors include smoking, a weakened immune system, long-term use of oral contraceptives, multiple sexual partners, and a history of sexually transmitted infections. Understanding these risk factors can help individuals make informed choices to reduce their chances of developing cervical cancer.
Prevention Strategies:
Prevention is key when it comes to cervical cancer. Vaccination against HPV is a crucial preventive measure and is recommended for both males and females before they become sexually active. Regular cervical cancer screenings, such as Pap tests and HPV tests, are vital for early detection and intervention. Practising safe sex, maintaining good sexual health, and quitting smoking are additional preventive strategies that can significantly reduce the risk of developing cervical cancer.
Early Detection and Screening:
Regular cervical cancer screenings are essential for early detection and treatment. Pap tests, also known as Pap smears, involve collecting cells from the cervix and examining them for abnormal changes. HPV tests detect the presence of high-risk HPV strains in cervical cells. These screenings can identify precancerous changes or early-stage cervical cancer when it is most treatable.
Treatment Options:
The choice of treatment for cervical cancer depends on various factors, such as the stage of cancer, the individual's age, and overall health. Treatment options may include surgery, radiation therapy, chemotherapy, or a combination of these modalities. Surgery aims to remove the cancerous tissue, while radiation therapy uses high-energy X-rays to kill cancer cells. Chemotherapy employs drugs to destroy cancer cells or stop their growth. The treatment plan is personalised to each individual's unique situation and is determined by a team of healthcare professionals specialising in gynecologic oncology.
Conclusion:
Cervical cancer is a preventable and treatable disease when detected early. Understanding the causes, risk factors, and preventive strategies are crucial steps in reducing the incidence of cervical cancer. Regular screenings and vaccinations are fundamental in early detection and intervention. If diagnosed, various treatment options are available to manage the disease effectively. By raising awareness, promoting preventive measures, and encouraging regular screenings, we can strive towards a future where cervical cancer becomes a rarity. Together, we can make a significant impact in the fight against cervical cancer and improve women's health worldwide.
For more details click on the link 👇🏻 https://bit.ly/3osreVo
#HopeAgainstCancer#ICANWIN#YESITSRAM#FightAgainstCancer#CancerAwarenessMatters#TogetherAgainstCancer#CancerWarriorsUnite#EmpoweredByHope#RaisingCancerAwareness#IgniteTheFight#ConquerCancerTogether#InspireHopeForSurvivors#CancerFreeFuture#CancerAwareness#CancerSupport#CancerSurvivor#CancerFighter#CancerCommunity#CancerResearch#CancerPrevention#CancerFree#EndCancer#StandUpToCancer#CancerJourney#CancerWarrior#CancerAware#CancerThrive#NoOneFightsAlone
26 notes
·
View notes
Text
My ex-wife did not give me cancer.
I realize that most people who get divorced dont get cancer from their ex-partner but I spent 6 months thinking that she might have. She gave me HPV and I had an abnormal pap smear, then an abnormal biopsy, then finally they scraped all the abnormal cells away and tested them. I do not have cancer. I have been holding on to my last shred of sanity by the skin of my teeth and now I have a slightly firmer grip. I don't have cancer. I keep saying it so that I can slowly start to believe it. Months of crying, screaming, and then numbness have finally left me here. I hate her. I hate her even more than the man who traumatized me as a child and I thought that wasn't possible. I don't think she understands what the last 6 months have done to me and I doubt she cares but some part of me wants her to finally face some consequences for her actions. So far I am the only one who has faced consequences and it was for her actions, not mine. How do you make someone without empathy understand the gravity of my absolute terror these last 6 months? She gets to move on and live with her lovers and I am stuck with medical debt, less faith in humanity, and so much rage. How does she face justice?
4 notes
·
View notes
Note
hello witch person, i'm a transmasc who's on a waitlist for getting my uterus chopped, however I have read that HPV could still infect me and live happily in my vagina (and cause problems there). I am the first trans man my GP has treated so she's unsure about how a pap smear will work when I have no uterus and I'd like to know if they do them/how they work to ease my anxiety (I'm very young so possibly my first one will be with already no uterus). I can and will ask the doctor at the trans clinic in our next appointment, but those have a long waitlist and it's worrying me, so I'd appreciate any info you have on this
hi anon,
doing a Pap smear will depend on whether or not you have a cervix, since a Pap involves scraping the cervix for samples to search for abnormalities that could be a warning of cervical cancer caused by HPV. it's usually standard practice to leave the cervix in place after a hysterectomy, so that's something to check in with your surgeon about!
45 notes
·
View notes
Text
How Lady Gynecologist Can Help Educate Females About The Importance Of Regular Checkups
Women’s health is an essential aspect of overall well-being, and regular gynecological checkups play a pivotal role in ensuring early detection of health issues and maintaining reproductive health. A Lady gynecologist in Thane is a female medical professional specializing in women’s reproductive health and holds a unique and vital role in educating and empowering women to prioritize their health. Here’s an overview of how a lady gynecologist can help educate females about the importance of regular checkups.

Creating a Safe and Comfortable Environment: One of the primary advantages of a lady gynecologist is the ability to create a safe and comfortable environment for women. Many women find it easier to discuss sensitive health topics, such as menstrual health, sexual health, or menopause, with a female doctor who may share a similar perspective or experience.
Promoting Preventative Healthcare: One of the primary responsibilities of a lady gynecologist is to educate women about preventative health care. Gynecologists often advocate for regular checkups, including routine screenings like Pap smears, pelvic exams, breast exams, and blood pressure monitoring, which are crucial in identifying potential health issues early.
Addressing Common Myths and Misconceptions: There are many myths and misconceptions surrounding women’s health, particularly in reproductive care. A lady gynecologist has a critical role in debunking these myths and providing evidence-based medical information.
Empowering Women with Knowledge About Their Bodies: Education is empowering, and a key aspect of a lady gynecologist's role is to help women understand their bodies better. By offering information about menstrual cycles, sexual health, fertility, and menopause, a gynecologist empowers women to take charge of their health.
Encouraging Early Detection and Regular Screening: A major focus for a lady gynecologist is encouraging women to engage in early detection practices, which can significantly improve health outcomes. Screening tests, such as mammograms, HPV tests, and ultrasound exams, can detect abnormalities before they develop into more serious health problems.
Building Trust and Encouraging Long-Term Health Habits: A key aspect of a gynecologist’s role is building trust with female patients, making them feel comfortable enough to come back for regular checkups. By fostering this relationship, a lady gynecologist can encourage women to make regular visits a part of their routine, just like seeing a general practitioner for checkups.
For the Best Gynecologist in Thane, you can connect with them without any delay.
About Dr. Vidya Shetty
Dr. Vidya Shetty is one of the leading names because she is offering everyone excellent quality gynecology treatment at economical prices. For treatment and expert advice, you can book your appointment today.
0 notes
Text
why did noone show me what they used to put in my cervix???? (now there's cool vaginal swab tests for HPV and they only poke u in the cervix if you have a history of abnormal smears or if you test positive for HPV it's nice)
I need to share this pure joy with everyone. I don’t have any money but if I did I’d blaze this post with it because everyone deserves to see this.
I have several doctor friends and this is usually a good source of entertaining medical stories but today it was a source of Art.
My friends had a teen patient ask them for all their expired Pap smear swabs (which are apparently called cervical brooms). For those unfamiliar, they look like this

She then took them home and came back on her next visit with this

It’s… a peacock. A work of art. Made of expired vaginal swabs, paper, and a plastic hanger.

He has a bow tie and glasses.
I cannot comprehend his magnificence. He’s called Rupert.
5K notes
·
View notes
Text
Best Female Cancer Specialist in Delhi | Comprehensive Gynecologic Oncology
Gynecological cancers require professional care from a highly qualified specialist with in-depth knowledge of the intricacies of the female reproductive tract. Dr. Sarita Kumari, an illustrious gynecological oncologist in Delhi, is committed to delivering complete cancer care for women diagnosed with ovarian, cervical, uterine, vaginal, and vulvar cancers. Through her patient-centered approach and state-of-the-art medical skills, she guarantees the optimal form of treatment and recuperation for each patient.
If you or someone you love is looking for first-rate gynecologic cancer care, Dr. Sarita provides individualized treatment, such as minimally invasive robotic procedures, targeted therapy, and integrative post-treatment care, making recovery comfortable and successful.
What is Gynecologic Oncology?
Gynecologic oncology is a dedicated branch of medicine that deals with the prevention, diagnosis, and treatment of cancer in the organs of the female reproductive system. The most frequent forms are:
Ovarian Cancer – Also known as the "silent killer" because of its nonspecific symptoms that result in late-stage diagnosis.
Cervical Cancer – Primarily caused by the Human Papillomavirus (HPV) and can be prevented through regular screening and vaccination.
Uterine (Endometrial) Cancer – Associated with hormonal disturbances, obesity, and genetic predisposition.
Vaginal & Vulvar Cancer – Rare cancers that need specialized diagnosis and treatment.
By remaining proactive and getting regular screenings, women can greatly lower their risk and enhance their opportunity for early detection, which enhances treatment results.
Why Dr. Sarita Kumari for Gynecologic Cancer Treatment?
Long Experience – Decades of experience in diagnosing and treating gynecologic cancers with high success rates.
Minimally Invasive Procedures – Expert in robotic-assisted and laparoscopic surgeries, allowing for quicker recovery and less scarring.
Advanced Treatment Choices – Offering focused therapy, immunotherapy, and HIPEC (Heated Intraperitoneal Chemotherapy) for better cancer management.
Patient-Centric Care – Each treatment plan is specifically designed according to the patient's individual needs.
Thorough Post-Treatment Care – For long-term well-being, prevention of cancer recurrence, and emotional support.
Comprehensive Gynecologic Oncology Services
Early Detection & Diagnosis
The sooner cancer is diagnosed, the higher the success rate of treatment. Dr. Sarita employs the most advanced diagnostic equipment to provide accurate and timely diagnosis:
Pap Smear & HPV Testing – Crucial for identifying early symptoms of cervical cancer.
Pelvic Ultrasound & MRI Scans – High-resolution scans to identify abnormalities in the uterus and ovaries.
Biopsy & Genetic Testing – Determines cancer type and genetic susceptibility.
CA-125 & Other Tumor Markers – Blood tests utilized to track the advancement of ovarian cancer.
Advanced Cancer Therapies
Dr. Sarita offers the most recent developments in gynecologic cancer therapies with accuracy, efficiency, and reduced discomfort for her patients.
Surgical Oncology – Accuracy-Based Cancer Removal
Radical Hysterectomy – Surgical removal of the cervix and uterus for advanced stages.
Cytoreductive Surgery – Shrinks the tumor to enhance the efficacy of chemotherapy.
Fertility-Sparing Surgery – Enables younger patients with early-stage cancer to maintain the capability of getting pregnant.
Robotic & Laparoscopic Surgery – Low-invasive surgery for faster recovery.
Chemotherapy & Targeted Therapy
Intravenous & Intraperitoneal Chemotherapy – Eliminates cancer cells and helps avoid recurrence.
Targeted Therapy (PARP Inhibitors, Bevacizumab) – Targets cancer cells while leaving the healthy tissues intact.
Immunotherapy & Hormonal Therapy – Activates the body's immune system to combat gynecologic cancers.
HIPEC – Heated Intraperitoneal Chemotherapy
HIPEC is a sophisticated method that infuses heated chemotherapy directly into the abdominal cavity following tumor removal surgery, specifically targeting remaining cancer cells.
Recovery & Post-Treatment Support
Cancer treatment isn't merely about eliminating the disease – it's about restoring patients' health, confidence, and quality of life. Dr. Sarita offers extensive post-treatment care to promote long-term wellness:
Regular Follow-Ups & Imaging Tests – Regular check-ups to identify any recurrence signs.
Diet & Lifestyle Counseling – Dietary and physical training to enhance immunity and recuperation.
Mental & Emotional Support – Counseling facilities and support groups to assist the patients in dealing with the emotional burdens of cancer treatment.
Real Stories, Real Hope – Patient Testimonials
"Dr. Sarita helped me through my ovarian cancer therapy with professionalism and empathy. Now, I am cancer-free and thankful for her remarkable care." – Meera S.
"Finding out that I had cervical cancer was petrifying, but Dr. Sarita's encouragement and accurate treatment regimen instilled hope in me. Because of her, I am now living a healthy life." – Priya R.
0 notes
Text
Anal Pap smear
What is the male version of a Pap smear?
AI Overview
The male equivalent of a Pap smear is an anal Pap smear. It's a procedure that collects cells from the anus to check for abnormalities that could lead to cancer.
How it's performed
A doctor collects cells from the anus
The cells are then checked for abnormalities in a lab
When it's recommended
Some doctors recommend anal Pap tests for gay and bisexual men, who are at higher risk of anal cancer
You can contact your primary care provider to ask if this test applies to your personal situation
Why it's important
Some types of human papillomavirus (HPV) can cause anal cancer
Screening for abnormal anal cells can help remove them before they develop into cancer
Vaccination against HPV before initial sexual exposure can reduce the risk of anal cancer
Other HPV tests for men
Men are typically screened clinically with a visual inspection to check for lesions (such as warts)
Male urethral smears have also been used as a screening tool for detecting HPV infection
0 notes
Text
Planning for a Cancer Checkup in Chennai? Key Information You Must Know!
One of the biggest health issues in the globe is cancer. For treatment and recovery to be successful, early discovery is essential. A cancer health checkup in Chennai helps identify potential risks and detect cancer at its earliest stages. Even before symptoms appear. A Cancer Screening Checkup in Chennai further aids in early diagnosis, improving treatment outcomes. If you are considering a cancer checkup. Here’s everything you need to know about its importance. Available tests. And where to get screened.

Why is a Cancer Checkup Important?
Regular cancer checkups help detect abnormal cell growth before it develops into a serious condition. Many types of cancer. Such as breast. Cervical. Lung. Prostate. And colorectal cancer. May not show symptoms initially. Screening allows for timely medical intervention. improving survival rates and raising the likelihood that therapy will be successful.Cancer checkups are particularly beneficial for individuals with. ⦁ A family history of cancer. ⦁ Exposure to risk factors like smoking. Alcohol. Or harmful chemicals. ⦁ Age-related risks. Above 40. ⦁ Pre-existing health conditions that may increase cancer susceptibility.
Common Tests in a Cancer Screening Checkup
⦁ Blood Tests & Tumor Markers – Identifies substances produced by cancer cells. ⦁ Mammogram – Detects breast cancer in women. ⦁ Pap Smear & HPV Test – Screens for cervical cancer. ⦁ PSA Test – Checks for prostate cancer in men. ⦁ Colonoscopy – Detects colorectal cancer. ⦁ Low-Dose CT Scan (LDCT) – Screens for lung cancer. Especially for smokers. ⦁ MRI & CT Scans – Helps visualize abnormal growths.
These screenings help in early detection. Allowing doctors to recommend preventive measures or immediate treatments if needed.
Who Should Get a Cancer Screening Checkup?
Cancer screening is recommended for individuals who. ⦁ Have a family history of cancer. ⦁ Are above 40 years old. ⦁ Have lifestyle risk factors like smoking. Alcohol consumption. Or obesity. ⦁ Experience unexplained symptoms like fatigue. Weight loss. Or persistent pain. ⦁ Work in environments with chemical exposure.
Regular screenings help in early diagnosis. Preventing the disease from reaching advanced stages.
Where to Get a Cancer Screening Checkup in Chennai?
Several hospitals and diagnostic centers in Chennai provide cancer screening services. However. If you are looking for a convenient and hassle-free option. Asto Labs offers a comprehensive cancer checkup. With free home sample collection.
Why Choose Asto Labs for Your Cancer Checkup?
⦁ Get tested in the convenience of your own home with home sample collection.. ⦁ Accurate & Reliable Reports – Lab-certified results you can trust. ⦁ No Travel Required – Avoid long waiting hours at hospitals. ⦁ Tailored Screening Plans – Based on your age. Gender. And medical history.
With Asto Labs. You can undergo a cancer screening checkup in Chennai without stepping out of your home.
How to Book a Cancer Checkup in Chennai?
Booking a cancer screening test is quick and simple.
⦁ Consult a Doctor – Identify the right screening tests based on your risk factors. ⦁ Schedule an Appointment – Contact Asto Labs for free home sample collection. ⦁ Sample Collection – A trained professional will visit your home to collect the required samples. ⦁ Receive Reports – Get your test results via email or WhatsApp. ⦁ Follow-Up Consultation – Discuss your results with a healthcare expert if needed.
Conclusion:Take Charge of Your Health Today!
By prioritizing regular screenings, individuals can take proactive steps toward early cancer detection and prevention. Advanced diagnostic methods, including a Cancer Health Checkup in Chennai, help identify risks before symptoms appear, ensuring timely medical intervention. Asto Labs offers comprehensive and reliable cancer checkups, making early detection more accessible and convenient. Regular checkups not only improve treatment success rates but also contribute to overall well-being. Taking charge of your health today with Asto Labs can lead to a healthier and more secure future.
#cancer checkup in Chennai#full body cancer check up in Chennai#cancer health check up in Chennai#blood cancer check up in Chennai
0 notes
Text
Please get your smear, it really can prevent a lot of suffering later. My partner tested positive for HPV (which means I have it too, of course), this was followed up with a colposcopy which identified high-risk abnormal cells. One loop exclusion later, she's clear. Had she not been having regular smears, she wouldn't have known unless it had become cancerous in the future, and then it might have been too late.
Attn: People With Cervixes!

When was your last Pap smear?
Because I am tired of seeing young people (think 40 year olds!) die horribly of an almost completely preventable disease, and I haven't seen the obligatory Tumblr PSA about it, so I'm making my own.
1. CERVICAL CANCER IS REALLY BAD
Cancers that have a good prognosis are usually cancers that can be caught early--like skin cancer, which is easily seen, and therefore usually treated very early. Cervical cancer does not give you symptoms until you have very advanced disease, which means unless someone is regularly testing your cervix, you will likely not be diagnosed early. More than half of people diagnosed with cervical cancer present with advanced disease. 75% of them will be dead within 5 years. For comparison, when caught in the earliest stage, there is a 90% 5 year survival rate. Treatment for those diagnosed is chemo and radiation, and believe me, those are not fun. If you do happen to be in the lucky 25% of survivors, if your cancer comes back, you have an 85% chance of dying within a year. Also! We think of cancer as something that happens to old people, but the average age of diagnosis for cervical cancer is 50.
2. WHO GETS CERVICAL CANCER?
Cervical cancer used to be the most common cause of cancer-related death in women in America, but at this point it's basically a disease of People Without Pap Smears--developing countries, immigrants, low socioeconomic status, BIPOC, rural communities, LGBTQ, etc.
3. HOW DO PAP SMEARS SAVE YOUR LIFE?
A Pap smear is a screening test for two things: HPV, and your cervical cells. HPV is the most common sexually transmitted disease in the world. Literally half of the people in America have some strain of HPV on their body. Most HPV infections go away on their own (in people with healthy immune systems), but some strains are Very Bad, and some people are just Very Unlucky, and the HPV starts causing your cervical cells to turn cancerous. 91% of all cervical cancers are caused by HPV. So a Pap smear looks to see if your have HPV, and if so, is it one of the bad ones? And also, do you have any cancerous cells hanging about in your cervix? And! It takes 10-30 years for HPV to turn those cells into cancer, which means you have a really really long time to catch it before it becomes cancer and cut those pre-cancer cells out!
4. WHAT ABOUT THAT VACCINE?
The thing my dad said I shouldn't get because it might make me a slut. Yes! There is an HPV vaccine! You should get it! It protects you against the nine most common cancer-causing types of HPV. It's recommended starting at age 11, and you can get it up to age 45 now! (It used to be 26, but as of 2020, it's now extended.)You can get it from most primary care doctors, or from Planned Parenthood, CVS, Walgreens, etc. If you get the vaccine you still need Pap smears.
5. I HEARD YOU CAN ONLY GET THE VACCINE IF YOU'RE A VIRGIN
Fake news. While the vaccine does not treat old infections of HPV, it does prevent new ones, so while the benefits are theoretically decreased in those who have already been sexually active, it does not mean you will not benefit from having it!
6. WHO GETS PAP SMEARS?
Everyone with a cervix starting at age 21, until you lose your cervix or until you're 65. You should get them every 3-5 years (depending on your exact age and what test your doctor does).
7. BUT I GOT THE VACCINE
Nice! You still need Pap smears.
8. I HAD ONE AND IT WAS HORRIBLE/I'M SCARED OF THE EXAM
Talk to your doctor about this in advance! Good gynecologists (and other providers) will work with you to minimize discomfort as much as possible. They can use a small speculum and lots of gel, prescribe anti-anxiety medications to take in advance, and some people will even use numbing creams and/or laughing gas.
9. BUT I DON'T HAVE/CAN'T SEE A GYN
Most primary care physicians can do them! So do a lot of urgent care centers!
10. BUT I'M A LESBIAN
HPV can be transmitted through oral/genital contact, hand/genital, and even hand-to-hand-then-genital, so you still need Pap smears.
11. BUT I'M A VIRGIN/ASEXUAL
You still need Pap smears. HPV can be transmitted not just through penetrative sex, but also through oral/genital, hand/genital, and hand-to-hand-then-genital, and also 9% of cervical cancers are not caused by HPV.
12. BUT I'M A TRANSGENDER MAN
If your cervix was removed, then congrats! You do not need Pap smears. Otherwise, unfortunately, you are still at risk for cervical cancer and need to be screened.
13. BUT I'M A TRANSGENDER WOMAN
Neovaginas do not need Pap smears! Congrats! Consider getting the vaccine, though, to prevent spreading HPV to others.
14. BUT I'M A CIS-GENDERED MAN
Congrats! You do not need Pap smears! You should still consider the vaccine though, not only to prevent the spread of HPV to others, but also because HPV causes 50% of all penile cancers as well.
In summary: please please please go get your pap smear. Go get vaccinated. The spread of HPV can be prevented, and cervical cancer can be caught and treated before it even becomes cancer.
DON'T FEAR THE SMEAR
57K notes
·
View notes