#ALSO YEAH BACK TO TOPIC- I do feel like I improved my VP a bit- not as Much as the start ofc but a lil bit a lil bit
Explore tagged Tumblr posts
Text


━ 2021, July
━━ 2021, September
━━━ 2023, July
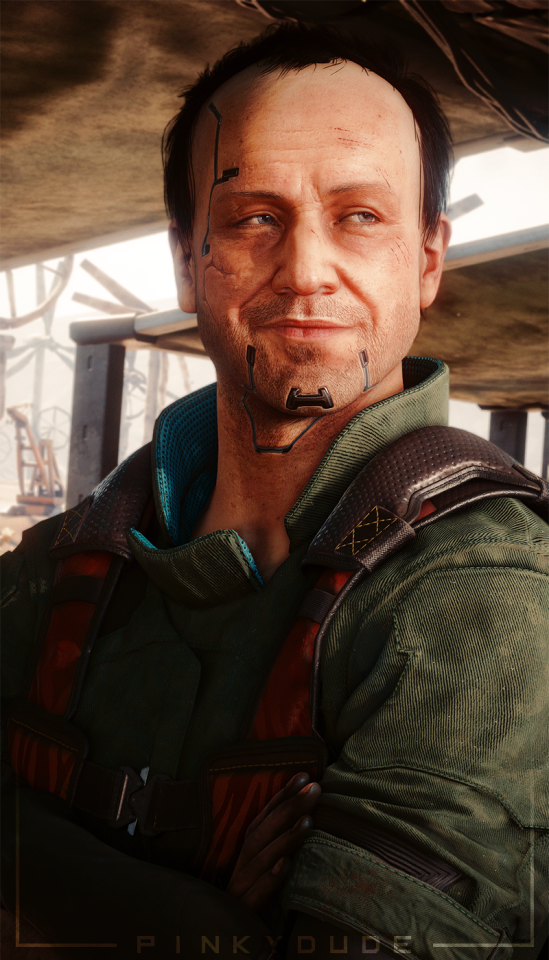
Mitch Anderson | 259/?? Evolution - With a little help from my friends
#Cyberpunk 2077#Mitch Anderson#Aldecaldos#Screenshot#Virtual Photography#hhhhhhhhh pinky try not to get emo over Mitch challenge (failed)#I'm mad at myself for not taking as much pics of him in 2022 hgfhhgf if at all like-#ALSO YEAH BACK TO TOPIC- I do feel like I improved my VP a bit- not as Much as the start ofc but a lil bit a lil bit#god I love him so much uwu his lil cheeky face
21 notes
·
View notes
Text
RHR: A Three-Step Plan to Fix Conventional Healthcare
In this episode we discuss:
The patient case that inspired the book
Who is this book for?
The mismatch between our medical paradigm and chronic disease
Drug companies and conflicts of interest
How clinicians can help create a new paradigm
The three core problems and how to solve them
What this new paradigm looks like
How do we pay for this? Is it scalable?
How allied providers are the key
Show notes:
Unconventional Medicine by Chris Kresser
Special offer for RHR podcast listeners - get the audiobook free if you buy the book by November 12th.
NaturalForce.com - use coupon “unconventional” and get $10 plus free shipping
[smart_track_player url="http://ift.tt/2yiM0Yd" title="A Three-Step Plan to Fix Conventional Healthcare" artist="Chris Kresser" ]
youtube
Chris Kresser: Hey, everybody, Chris Kresser here. Welcome to another episode of Revolution Health Radio. Today we’re going to do something a little different. I am bringing on a guest host, Tony Federico, he’s the VP of marketing for Natural Force Nutrition, a physiology editor for the Journal of Evolution and Health, and a longtime contributor to Paleo Magazine, and also at Paleo f(x), which is where I met Tony, I think, originally, and I have interacted with him the most. And he’s moderated several panels that I’ve been on and I’ve always been impressed with the way he’s done that, the intelligent questions that he asks and just his balanced perspective on ancestral health and Functional Medicine, and this movement overall. Today is the day that my new book, Unconventional Medicine, comes out. It’s now available on Amazon, and I wanted to ask Tony to come take over the podcast and talk with me about the book because I know he’s really interested in all these topics and he’s read quite a bit of the book himself, and I thought it would be more interesting to have a conversation about it than for me to just sit here and do a monologue. So Tony welcome to the show and thanks for being here. Tony Federico: Yeah, thanks for inviting me on, Chris. It’s always fun, when we’ve had the chance to chat, as you said. Whether in person or on podcast, I’m always happy to jump in and dish on health with you. Chris: Fantastic. So, you have read a little bit of the book and we chatted a little bit about it via email, so let’s dive in. Let’s talk a little bit about this book. And for me it was really, it felt like the most important next step that I could take in order to get this message out about ending chronic disease. Tony: Yeah, I got my copy of Unconventional Medicine a couple days ago. I just so happened to have some time off yesterday, and the next thing I knew I was 80 pages in. Chris: Nice. Tony: So, I have to say that, as somebody who’s been in the trenches, I worked as a personal trainer for 10 years, I could really relate to a lot of the things that you were saying in the book, and we’ll get into why a little bit later on in the interview. But you know I just am really impressed with what you put together here, Chris. So let's just, let's get into it, and the first thing that I actually wanted you to maybe tell me a little bit about was how you open the book, which I think is a really great story about a patient named Leo. So I wanted to talk a little bit about Leo and his story and kind of how that inspired you to go down this particular path of unconventional medicine.
The patient case that inspired the book
Chris: Sure, yeah. So, Leo was an eight-year-old boy that I treated in my clinic a few years back, and I wanted to start with his story because it's, unfortunately, a typical story, much more common than, of course, we would like. And it was powerful for me, it was a powerful experience. It's what actually led to me writing this book. So, like way too many other kids of his age, he was suffering from a number of behavioral issues. He was initially diagnosed on the autism spectrum. Eventually they settled on OCD and sensory processing disorder. He would throw these just crazy tantrums where he'd end up crying or screaming inconsolably, writhing on the floor, and this would happen for seemingly the simplest of reasons. Like trying to get his shoes tied as they were going out the door, not cutting the crust off his sandwich in just the right way or getting a stain on his favorite T-shirt. And he was really rigid around his behavior and its environment, everything had to be just right, just the way he wanted it to be, or else he would fly off the handle.
Is a new healthcare paradigm affordable? Scalable? You bet.
His diet was extremely limited, he only ate a handful of foods, pretty much all of which were processed and refined. So crackers, bread, toaster waffles, that sort of thing, and this is part of the kind of OCD-like tendencies. And any time his parents would try to introduce new food, he would go totally ballistic. And they were worried about nutrient deficiency, but they didn't feel like they ... they were just worn down. Any parent who has a kid like this will understand that. It's just they didn’t feel like they had the resources to battle him at every meal. And they took him to a bunch of doctors locally, and that’s where they got those diagnoses. Initially they were kind of relieved to have those, but then after a while they realized that they were just simply labels for symptoms. And when they asked what the treatment was, you can probably guess the answer: medication. Tony: Something to do with drugs. Chris: Something to do with drugs. Yeah. And when they asked how long he would be on that treatment, you can probably also guess the answer. Tony: The rest of your life. Chris: Yeah. Shrug of the shoulders, indefinitely, maybe he'll grow out of it, that sort of thing. And they weren't excited about the idea of of medicating their son, but they were also aware of how much he was suffering, and they were suffering, frankly, too. They decided to give them a try, starting with Adderall, and then they progressed to Ritalin and then antidepressants. And certainly the drugs did seem to help with at least some of the symptoms, but there were a couple issues. Number one, they also caused some very intractable side effects like headache, abdominal pain, irritability, and most significantly, severe sleep disruption. And they had a couple of other kids that were younger than Leo. So they were not happy about the sleep disruption. Nobody was because it was brutal for them and also brutal for Leo. Kids need a lot of sleep, and if they’re waking up throughout the night, that’s going to make ... So that was in some ways worse than the original symptoms they were trying to treat. And then Leo's mom had done quite a bit of research on the effects of these medications and she was scared. Particularly for children and adolescents, some of these drugs have some pretty scary side effects and long-term risks. So what really stood out to me, and I mentioned this in the book, is that not once during this entire process of seeing all these different doctors, primary care provider, psychiatrist, eventually behavioral disorder specialists, did anybody even hint at the possibility that something in Leo's diet or some other underlying issue like a gut problem or nutrient deficiency or heavy metal toxicity or something like that could be contributing to his symptoms. It wasn't even broached as a possibility at any time. Fortunately, Leo's mom, one of her friends followed my work and sent her a couple of articles from my blog. One was on the gut–brain–axis, and I think the other one was on the underlying root causes of behavioral disorders. And so that's what led them to bring Leo to see me, and long story short, we were able to ... we did a bunch of testing, found issues that you might guess at. So, disrupted gut microbiome, SIBO, fungal overgrowth, gluten intolerance, but also intolerance of soy and corn and rice and buckwheat, which were major ingredients in a lot of the processed and refined food products that he ate, and arsenic toxicity because rice milk was the only other beverage he would drink aside from water. And we know that rice products can be high in arsenic. So, we, over several months, it definitely wasn't easy to address these problems because of his OCD-like tendencies and his picky eating habits. But after several months he was like a different kid. His teacher even called home and was like, “What have you done with Leo and who’s this kid that you’re sending in?” Because it was a big issue for her. They often had to come to school and pick him up early because of the behavioral problems. And his diet expanded; he was eating foods he would've thrown against the wall just months before, he was more tolerant of disorder, more relaxed in his environment. They were able to travel for the first time in a long time because he wasn't so anxious in unfamiliar environments. His physical symptoms had improved significantly. So they were just over the moon. They couldn't believe it, and toward the end of our treatment together, she said something that really struck me, which was there’s so many kids out there that are like Leo and they’re suffering, they’re not finding help in the conventional system. Tony: Sure. Chris: And their doctors and parents are not even thinking about this stuff. Like it’s not even in most people’s consciousness that if a kid has a behavioral disorder that you should look at these physiological issues. It’s not, for 99 percent of people they don't even go there because they don't know. Tony: Yeah, I mean I think that that was—reading about Leo and reading about a story and certainly there's people that I've known, myself included, who have had very similar experiences—I think it's great to have a narrative like this that you can really connect to because then when you tease it apart, all the pieces really make sense. It makes sense why having doctors treat symptoms has failed, it makes sense why a lack of communication between the health provider network that was supposed to be serving Leo failed. It makes sense why it didn't work when you actually start to tease it out. But then we’re still all, well not all, but most of us are still going down this path and it's an exercise in futility, really. You have an eight-year-old kid who's on powerful stimulant medications, he’s on antidepressants, and it was bad enough for his parents to reach out and to seek those interventions as solutions, and then the side effects are even worse. And that’s just something that just gets you right in the heart. And like you said, he’s not the only one, he’s not the only kid. His parents are not the only parents. And frankly, his doctors are not the only doctors because I can guarantee you that that probably doesn’t really feel good for the practitioner, for the healthcare provider to not get results as well. And they’re working with what they’ve got. Chris: Absolutely. Tony: And trying to use the tools they have. Chris: Yeah, I mean, let’s be clear about this. Everybody is doing the best they can in this situation. The parents are doing the best they can, in the vast majority of situations, parents just love their kids and do everything possible that they can to help their kids thrive. I’m a parent, I know that that’s how I relate to my kid. I know that every parent I know, that’s how they relate to their kids. And I would even, I would say that’s true for doctors too. The vast majority of them are trying to do the best they can with the tools that they have and in the system that they’re working within. And that’s the rub. Tony: Right. Chris: It’s like most doctors I’ve seen have been caring and they’ve wanted to do the right thing, but the question is, can they do the right thing in the conventional medical system as it exists today? And, of course, that’s largely what the book is about.
Who is this book for?
Tony: Yeah, so let’s kind of speak to that specifically. And we’re talking about doctors, we’re talking about medical professionals, we’re talking about patients, and then we didn’t mention it, but where I fit into this formula or potential formula as an allied healthcare provider, as a personal trainer/health coach, is that your audience for this book, do you really see that kind of triad is who you're speaking to here? Chris: Yeah, definitely. I think if you look at the cover of the book, the subtitle is “join the revolution to reverse chronic disease, reinvent healthcare, and create a practice you love.” So that last bit would suggest that it's mostly for practitioners, but that's not true. It is really for anybody that is interested in the ideas of reinventing healthcare and reversing chronic disease. And, in fact, I would argue that that change is going to be initiated by people, primarily by people that are not practitioners. So it's like a grassroots, bottom-up approach, where a good example is with my training program, my ADAPT training program, now that we've been training practitioners in this approach for the last couple years, we always ask people how they learned about my work or how they learned about the training program. And in a surprising number of cases, the answer is from their patients. So these doctors or other practitioners, their patient brings an article in that I wrote or brings something in, tells them about me, and to their credit they’re open-minded enough to go and check it out. And then they like what they see and they end up taking the next step. So people even who have no intention of ever becoming a healthcare practitioner, I think would really benefit from this book if they're interested in these ideas. And then certainly, as you mentioned, licensed healthcare providers like medical doctors or nurse practitioners or physician assistants that are currently working within the conventional paradigm but have already seen its limitations and want to do something different but don't yet know what that might look like. And then people who are outside of the conventional paradigm but are already practitioners, so acupuncturists, chiropractors, naturopathic physicians, etc., in many cases they’re already well aware of the limitations of conventional medicine, which is why they chose to go down a different path. But speaking personally as an acupuncturist myself, I also saw some limitations in the traditional Chinese medicine approach, or at least some differences in the way that I wanted to practice it. I was looking for something that could incorporate modern diagnostic testing and create a more systematic approach that included ancestral diet and lifestyle and some of the other things we talk about in the book. So, I think many of those practitioners can benefit from the book from that perspective. And then you have the growing and already large number of people like yourself who are personal trainers, health coaches, nutritionists, etc., who I really think are going to play an increasingly important role in this revolution to reinvent healthcare. Tony: Yeah, it so important now for people to really, for patients to be their own advocate, and I don't think we’re living in a time where I remember with my grandparents—if your doctor said something, it was basically gospel and you didn’t question it and you didn't think about it. Now, the first thing people do when they experience a symptom, it's Dr. Google first. So it's super important to equip and arm patients with good information, which I think this book does. Here's a path, here's a path forward for you as a patient. But then it's respectful of the role of doctors, and you highlight many situations where conventional medicine is great. If you break your arm or get in a car accident or have a heart attack or whatever the case may be, yeah, you need a doctor, and you need to go to an emergency room and you need those types of interventions. But it's really in this kind of gray area, it’s really not gray, it’s actually quite clear. And we could probably specify a little bit more, but there’s this middle zone where somebody’s not acutely injured, they’re not acutely in a disease state. They’re in a chronic disease state, or they’re just unwell. And it’s hard for a system that is all about pharmacological interventions, surgical interventions, to deal with a more subtle approach. And that’s where that whole middle ground and acupuncturists and massage therapists and everybody who's in that middle zone. I had clients constantly when I was actively training, constantly asking me questions where I was like, you know what? This is really something they maybe should be taking to their doctor. But guess what? The doctor only has 15 minutes under pressure to see as many patients as they can. I had a friend who was a physician in France. And he was telling me about their medical model, and he would spend tons of time with his patients. And it was actually incentivized for prevention. And here we see some maybe misplaced incentives, and perhaps you can speak a little bit more about that.
The mismatch between our medical paradigm and chronic disease
Chris: Yeah, so, going back to your original comments, I think that the most important thing for people to understand is that our medical model, when it comes to our medical paradigm, is that it evolved during a time when acute problems were the biggest issues. So in 1900, the top three causes of death were all infectious diseases, tuberculosis, typhoid, and pneumonia. And the other reasons people would see the doctor were among those you mentioned, like a broken bone or a gallbladder attack or appendicitis. Tony: War. Chris: Right, injuries, trauma, etc. And so the treatment for that's pretty straightforward. It wasn't always successful, of course, but it was straightforward. You know, if the bone was broken, you set it in a cast. If the gallbladder was swelling, you would take it out. If someone was having appendicitis, you’d remove the appendix. So that's pretty ... it's one problem, one doctor, one treatment. Pretty straightforward. But you fast-forward to today, it's a totally different healthcare landscape. Seven of the top 10 causes of death are chronic disease rather than acute problems now, and 86 percent of the healthcare dollars we spend go toward treating chronic disease. And unlike acute problems, chronic diseases are expensive, difficult to manage and usually last for a lifetime. They don't lend themselves to that one doctor, one problem, one treatment kind of approach. The average chronic disease patient requires multiple doctors, usually one for every different part of the body in our system, and is taking ... Tony: Specialists. Chris: Right, specialists, they’re taking multiple medications in many cases, and they're going to be taking those medications for the rest of their life. So far, it's really, our conventional medical system is amazing for these acute problems. But it's the wrong tool for the job for chronic problems. So that's one issue, and it’s really important to point that out, because we just went through the whole healthcare debate again with the Affordable Care Act and the current administration’s proposal for a replacement, which has not come to fruition. But throughout that entire discussion, it really bothered me that there was an elephant in the room. All the discussion was around insurance. Like, who gets insurance and who doesn’t. And that’s important, it’s important to talk about that. But we have to recognize that health insurance is not the same thing as healthcare. Tony: Yeah. Chris: Health insurance is a method of paying for healthcare. And that’s really crucial to get that difference. Because my argument in the book is that there is no method of paying for healthcare, whether it’s the government, corporations, or individuals, that will be adequate and will be sustainable under the pressure of growing prevalence of chronic disease. It will bankrupt all of us. Government, the corporations, individuals, whoever is responsible for paying for the care will not be able to do it unless we can actually prevent and reverse chronic disease instead of just slapping Band-Aids on it. Tony: I think the analogy you gave in the book was rearranging the deck chairs on the Titanic. “Making a few small tweaks to our current system and expecting that to work is like rearranging the deck furniture on the Titanic as it inexorably sinks into the ocean. Too little, too late.” Chris: Yeah, exactly. That’s the argument about insurance. As the whole ship goes under, sinks under. The other problems you mentioned are very real also. So we have a misalignment of incentives, like the insurance industry, for example, doesn't benefit when the cost of care shrinks because they only make more money when the overall expenditures rise. So it's actually not in their best interest necessarily to seek out the most cost-effective solutions.
Drug companies and conflicts of interest
Chris: And then of course, we have drug companies. People are pretty well aware of the conflicts of interest there. It’s in their interest to sell drugs, and even when that’s not in the interests of the general public or the patients or the doctors. In many cases, it’s not in their interest either. So the best example of this is a recent one. We’re in the midst of an opioid crisis, the worst we’ve ever seen by far, and the DEA has been wanting to create new regulations that restrict a pharmacy’s ability to sell opioids in ways that will protect people. So, for example, there was a pharmacy in West Virginia in a town that was tiny. It had like 30,000 people in this town, and they had ordered something like nine million opioid pills in the last year. It was clearly a front, like there’s clearly something shady going on there. There's no way that 30,000 people in that town needed nine million opioid pills, and yet there are no regulations to actually prevent that from happening. And so, the DEA had proposed some regulations to just safely protect people from that kind of thing. And the Big Pharma lobby basically shut that down and they played a big role in writing a law that limits the DEA's ability to do that kind of regulation in the midst of the worse opioid crisis ever. And to put this in perspective, we hear a lot about the gun lobbies and their control. They spend about $10.5 million lobbying Congress, I think, per year. And Big Pharma, they spent $250 million. Tony: Wow. Chris: Twenty-five-fold higher. Tony: It's really tragic. I actually, I don’t think we’ve ever talked about this, but I grew up in South Florida, which was kind of ground zero for the opioid epidemic. And I remember in high school down in Miami and West Palm Beach, and kids would get a hold of a contact or whatever, somebody that had a prescription and basically would end up being a de facto drug dealer vis-à-vis a pill mill, etc. The kid across the street from me died, multiple kids in my high school died, multiple kids went into in-treatment programs, some of them battled addictions for decades. Some of them got out of it. Very few got out of it. Some of them didn't and have continued to be plagued with either switching from pharmaceuticals to street drugs like heroin, etc., and then we can see what's happening there. And that's just one example. If we look at drug consumption in the United States, is it that Americans are just that much sicker and we’re in that much more pain than people in other countries? Because we’re consuming far and away more painkillers than any other country on the planet. And I would venture to guess that you could say the same about antidepressants or ADD medication. It's very much a case of misaligned incentives. And incentives are working in the sense of the pharmaceutical companies are doing very well. Chris: Yeah. Who are they working for is the question. Tony: Exactly. Chris: We’re the only country aside from New Zealand that allows direct-to-consumer drug advertising, and I think that's a big part of the problem. But it's not just Big Pharma. We also have conflicts in medical research that, of course, are related to Big Pharma because they pay for two-thirds of all medical research. We have broken payment models, where there's no real incentive or reward for good performance, and in fact, you could argue it's the other way around because doctors are compensated for, usually based on the number of procedures they order and the number of patients they see. So to your point about the doctor in France who is actually incentivized to prevent, rather than just treat disease, we don't have that at all, it's the opposite. And so there are a lot of deeply entrenched issues that we certainly need to address, and that's not essentially what this book is about. There are other books that cover that material really well, and frankly many of those issues are outside of our individual control as clinicians or practitioners.
How clinicians can help create a new paradigm
Chris: We can work toward addressing them, and I think we should, but the good news is that I think that the bigger changes that we need to focus on individually and collectively are addressing the medical paradigm which we’ve talked about, creating a medical paradigm that’s better suited to tackle chronic disease. Addressing the mismatch between our modern diet and lifestyle, and our genes and our biology, which we've, of course, talked a lot about on the show before. And then creating a new way of delivering healthcare that actually supports this new medical paradigm and this more preventative approach. Because those things are all within our control as clinicians. Tony: Yeah. I like how you posed the question, and it was kind of a cool little, I think it was, not Hiroshi, but the person who is in charge of cooking at a Buddhist monastery. And basically a young monk comes up to this older man. He’s like, why are you doing the grunt work, basically washing rice out in the courtyard? And he says, it was like, what was it? “If not me, who? And if not now, when?” And I think that that’s really kind of the core of setting all this stuff up. Talking about the problem is really in the service of pivoting to the solution, and I’m a big believer in thinking globally, thinking big, but acting locally, hyper-locally, like yourself. Chris: Yeah. Tony: And then the people around you and who you can touch and impact. That’s ultimately where the power comes from. So let’s talk about that. What is in people’s power. And you started to describe some of those pillars of a new model. And you describe it as the ADAPT framework. And I don’t know how much you get into this on your regular podcast episodes, but to just kind of lay it out, ADAPT from a big-picture perspective. How does that actually address some of these systemic issues from an individually empowered stance? Chris: Yeah, great question, and before I even go into that, I just want to say I agree that I think the change is going to happen on different levels. So, because a lot ... we’ve talked about this stuff at conferences or even some people who’ve already read the book. They say, oh, this is fantastic. I’m so excited. But how are we going to deal with Big Pharma and the insurance industry and these misaligned incentives and all of that? And can we ever deal with that? The answer is we’re not going to deal with that overnight and it’s going to take a while to unwind those things. Tony: It’s the chronic disease, is what you call... Chris: Exactly, exactly. And I use that analogy in the book. But the good news is that changes can happen very quickly on an individual and local level. And there’s already a lot of evidence of that happening. So my own clinic, CCFM, tripled in size in the last three years alone. We have Cleveland Clinic Center for Functional Medicine, launched by Dr. Mark Hyman, has just blown up like crazy. I mean they started in this tiny space. Now their 17,000-square-foot space, it takes up the whole second floor of the Glickman Tower at Cleveland Clinic. They've got a waitlist of 2,500 patients from nine countries around the world. This is really exciting! The Cleveland Clinic is always on the forefront of the newest trends in medicine, and the fact that they've invested that much money in this speaks volumes. Then we have groups like Iora Health, an organization based in the Rocky Mountain area that’s reversing diabetes using health coaches. So there are lots of really interesting produced concepts, and there's going to be more and more of these. Like we’re doing a pilot program with the Berkeley Fire Department where we’re working with their new recruits to help, we’re implementing a wellness program. Tony: That’s awesome. Chris: To reduce injuries and help with recovery and optimize their performance. And if that goes well, there’s been interest from the wider fire department and in the city of Berkeley as a whole. Robb Wolf’s done some incredible work with Reno that we’ve talked about before. So I think the change is going to happen more quickly on this local grassroots level, and then that's going to start to get the attention of people on a state and federal level. And then it will start to get really interesting.
The three core problems and how to solve them
To answer your question, in my book I basically lay out three core fundamental problems with the healthcare system in the US. And these, I argue, go even deeper than the misaligned incentives and Big Pharma and all of that stuff, although they’re, of course, connected. The first is that there is a profound mismatch between our genes and our biology and our modern diet and lifestyle. And I'm not going to say more about that now because almost everyone listening to this podcast knows exactly what I mean. The second problem is the mismatch between our medical paradigm and chronic disease, which we just talked about. We need a new medical paradigm that is better suited for chronic disease. And then the third is that the way we deliver care in this country is also, it's not set up to support the most important interventions. And we’ve touched on that too, where the average visit with the primary care provider is just actually eight to 12 minutes. Tony, you were talking about 15 minutes. That’s luxurious in our current model. The average amount of time a patient gets to speak before they’re interrupted by the doctor is 12 seconds. Tony: Wow. Chris: So I think it’s pretty clear that if a patient has multiple chronic diseases, which one in four Americans now do, one in two has one chronic disease, and they show up to the doctor’s office and they're on multiple medications, and they had been presenting with a whole set of new symptoms, there’s absolutely no way to provide high-quality care in a 10-minute visit. So we have to change our, not only the paradigm, but also the way that care is delivered. So that was my premise. So it follows then that my solution would address, I would hope at least those three points, right? Each of those three deficiencies. So the ADAPT framework combines an ancestral diet and lifestyle, which addresses that mismatch between our genes and biology in our modern diet and lifestyle. And then Functional Medicine is the new paradigm of medicine that is based on addressing the root cause of health problems, so we can prevent and reverse them instead of just suppressing symptoms. And then the third component is what I call a collaborative practice model, which links licensed providers like medical doctors, nurse practitioners, with what I call allied providers, which include folks like yourself, Tony, health coaches, nutritionists, personal trainers, etc., to provide a much, much higher level of care than what doctors are able to provide on their own. So, again, we're not trying to replace doctors in any, or even conventional medicine. We need people to do colonoscopies and remove cancerous tumors and use all of the incredible amount of training and expertise and skill that they’ve acquired over a lifetime of practice and study. We absolutely want that, but we need to add stuff to that that's not available now. Tony: What that really says to me is, emphasize the importance of community, of connection, of collaboration. We’re social creatures, we’re tribal by nature. That’s another kind of Paleo/ancestral health part of the puzzle. And it would be foolish to think that we can dissect out and silo out all these different aspects of our lives without consequence. I really like this idea of bringing everybody into the fold, and it’s not saying that you can go to just the naturopath, or you can go to just the health coach. Because like I mentioned already, I certainly would’ve been ill-equipped to handle plenty of issues that a client would’ve brought to mind or brought up in conversation during a training session. But it would’ve been really great to say, ah, here's the Functional Medicine practitioner that I recommend you speak with, and to have a good relationship with that person and to be able to, as a health coach, help my clients better by getting them in touch with the right person. And that’s having this network that can really support people throughout their health journey whether it’s just feeling better and more energy, or addressing something like diabetes or hypertension. Which certainly there’s a place for all the players in that kind of scenario.
What this new paradigm looks like
Chris: Absolutely. And let’s use an example just to bring this to life for people. So, imagine you go to the doctor and they do some blood testing for your annual physical. And they find that your fasting blood sugar is 96 or 97. Your hemoglobin A1c is 5.5, and you’ve got triglycerides that are 110, 120, maybe 130. Currently, what would happen is nothing, usually. Tony: You’re not sick enough yet. Chris: Yeah, all of your markers are within the lab range, they say, and that means you’re normal, and so you might get some vague advice about make sure to exercise and follow a good diet. And thank you very much, that’s it. Certainly there are exceptions to the rule, of course. There’s some practitioners who can get a lot more proactive about that. But I can’t tell you how many people, patients I’ve had that have been given that basic line with those kinds of lab results. What could happen is this. The doctor says, “Well, you know, if we think of blood sugar disorders on a spectrum, on the left you’ve got perfect blood sugar. On the right you’ve got full-fledged type 2 diabetes. You’re not on the right yet, you don’t have type 2 diabetes or even technically prediabetes, but you’re progressing along that spectrum. And what we know from a lot of research is that if we don’t intervene now, that you’re going to continue progressing. And in fact, we have studies that show that the average patient who has prediabetes, will progress to full-fledged type 2 diabetes in just five years if it’s not addressed.” So what we want to do is be proactive here. We want to intervene now because it’s much easier to prevent a disease before it occurs than it is to treat it after it’s already occurred. So here’s what we’re going to do. We’re going to set you up with our staff health coach, and they’re going to give you all the support you need to adopt a better diet. They’re actually even going to take you shopping, they’re going to come to your house and clean out your pantry with you, and they're going to give you recipes and meal plans and give you ... totally hold your hand and do everything that they need to to get you on this diet. Because we know that information is not enough. We’ve got lots of studies. I can tell you as a doctor, go eat a healthy diet, and hey, we know that that’s probably not going to happen. Most people know what they should be doing, but they’re not doing it, and it’s not because of lack of information. It’s because they need support, and we’re here to support you. We’ve got this health coach. Furthermore, we've got this great personal trainer named Tony. We’re going to set you up with him and we’re also going to set you up with a gym membership. And the good news is, your insurance is going to pay for all this. They’re going to pay for the health coach, they’re going to pay for the gym membership, they’re going to pay for your sessions with Tony. And in six months’ time, you’re going to come back here and we’re going to retest your blood markers and I can almost guarantee that if you stick with the program, you’re going to have normal blood sugar by that time. And throughout that period you’re going to have weekly check-ins with a health coach, you’re going to have training sessions. And not only will your blood sugar be normal, you’re going to lose weight, your energy levels are going to go up, your sleep’s going to get better, you’re going to feel more confident and empowered because you’re making these changes, and you’re going to feel like a different person. Now that’s totally possible.
How do we pay for this? Is it scalable?
Chris: I can hear some people saying, “Oh, how are we going to pay for that? That’s ridiculous.” Tony: Is it scalable? Chris: The question we should be asking is, is treating type 2 diabetes scalable? Because I mentioned this in the book, it costs $14,000 a year to treat a single patient with type 2 diabetes. So let’s imagine that this patient progresses. We don’t intervene, five years later they have type 2 diabetes. All of a sudden the healthcare system is spending $14,000 a year paying for that person’s care. And let’s say that that person gets diagnosed at age 40, which is still reasonable these days. The age of diagnosis is dropping more and more, and then let’s say that they live until they’re 85 years old, which is also possible because of our heroic medical interventions that keep people alive a lot longer than they might have been otherwise. So 45 years living with type 2 diabetes, that’s a cost of almost $650,000 for one patient to the healthcare system. Tony: And that doesn’t even touch on the lost wages, cost to employers, when someone’s on leave, loss of productivity. And then the cost to the family members. Chris: Absolutely. Tony: People that are actually, are helping the patient, their health is going to be going down too. Chris: Yeah. Nor does it touch on the qualitative aspects. Being immobilized, not being able to play with your grandkids, all of that stuff. But let’s just even forget about that for a second—$650,000, okay? And then the CDC recently came out with statistics saying that 100 million Americans have either prediabetes or diabetes, and 88 percent of people with prediabetes don’t even know that they have it. Which means they're almost certainly going to progress, right? If you do the math and you multiply 100 million people times even $14,000 for one year, you get a number that’s so large, I don’t even know what it is. It’s like a google something. It’s like, it has so many zeros after it, I don’t even know how to characterize it. But then if you multiply 100 million times like 20 or 30 years, it’s more money than there is in the world. It's like it's not going to happen. Tony: Not sustainable, not scalable. Chris: Not sustainable, not scalable. So let’s say in our example that we ... the healthcare system spends $10,000, which is way more than would be necessary, but let’s even say we buy the person’s groceries for three months. And their gym membership and their trainer, and their health coach, and those weekly, let’s say we spend $10,000. We’re just super generous and we spend $10,000 for that six-month period. Again, the research and my clinical experience indicates with near certainty that if the person is at that stage of not even prediabetic and we intervene, there’s like almost no chance that it’s not going to, we’re not going to be able to normalize that person’s blood sugar. And if they do that and they stick with it and they are able to do that because they now have support rather than just information, we’ve just saved the healthcare system $640,000 over the course of that patient’s lifetime. And that’s a conservative estimate, as you say. We're not including even the indirect costs. Tony: Right, right. Chris: I think that this is not only possible, it's going to become necessary. And whether we get there with a proactive approach where we decide to move in this direction and we make these changes or whether we get there because we absolutely have no choice, we’re going to get there. Tony: Yeah. I mean it really sounds like we can’t afford to not do this. Chris: Exactly. Tony: And if we get to that point where we continue down the reactive path and we wait until there’s a total collapse, it might be too late, just to put it frankly. And it’s going to come out at a huge, not just financial cost, a huge human cost. Chris: Yeah, it’s going to be, we can use the chronic disease metaphor again, it’s a lot easier to prevent a problem or reverse it at an earlier stage than it is to wait until the patient is essentially on life support or the healthcare system is on life support. It’s harder to reverse it at that time. And that’s of course why I’m writing the book now because I want to get this message out as far and wide as I can. Tony: Yeah. If not now, when? If not you, who? Go right back to there.
How allied providers are the key
Chris: Exactly. And one more thing about that is the amazing thing, the beauty of this is that it takes about eight years and hundreds of thousands of dollars to train a doctor. And it takes a certain kind of personality and a certain kind of comfort level with science, and a lot of prerequisites. It’s not for everybody. And there’s a ... already we have a shortage of doctors, and that’s predicted to get worse. I’ve seen estimates that suggest by 2025 we’ll have a shortage of 52,000 primary care physicians. So that’s a big deal. [insert image] So we already don’t have enough doctors, it’s already going to get worse, but if you think of healthcare as like a ... I have something in the book called the healthcare population pyramid. And you were referring to it earlier, Tony, where at the very top of that pyramid you’ve got 5 percent of people who are in really acute situations. So they’re in the hospital or they’re in an intensive outpatient care setting. They need the conventional medicine paradigm as it exists, and it’s fantastic for those situations. Then you’ve got another 25 percent of people in that kind of high middle of the pyramid who are dealing with some pretty serious chronic health challenges. So they require more regular care, but they’re not sick enough to be in the hospital or in any kind of ... they’re living their lives, but they’re struggling a lot. A Functional Medicine practitioner/clinician usually working in concert possibly with the conventional specialist of some kind is a really great option for that 25 percent of the pyramid. But then you’ve got the 70 percent at the bottom. So these are people who do, may have health issues, but they’re more minor, so they might have skin problems, or a little bit of brain fog, some difficulties sleeping, some GI issues. And these can be definitely debilitating and total pain, but they’re not at the level of that 25 percent. My argument is that in many cases these people could be very well served by a health coach or nutritionist with good training. And possibly seeing a Functional Medicine provider once or twice a year, or something like that. And the thing is, we can train people in a year or two without an extensive science background to be very, very objective in this role. Because they’re mostly working with patients on changing their behavior. If you think about it, most of the risk factors for chronic disease come down to the wrong behaviors. Eating the wrong diet, not getting enough sleep, not exercising, or exercising too much, or any number of things that come down to choices that we’re making. And so if a skilled health coach who’s trained in things like motivational interviewing and coaching to strengths and other evidence-based principles of facilitating behavior change which we have a ton of research on, they can be incredibly effective for that 70 percent of the population. That's the majority of the population. So we’re totally underutilizing these practitioners, and my argument is that they’re going to play a huge role in this future of medicine. And that's of course one reason why we're launching an ADAPT Health Coach Training Program next year to complement the practitioner training program that we've been doing. Because I want to create this ecosystem we've been talking about where you have all of these different types of practitioners working to the maximum of their training and ability and scope of practice and supporting each other and therefore providing the highest level of care to patients. Tony: That certainly kind of perks my ears up hearing about the ADAPT health coach option and something that I’m personally interested in. So who knows? Maybe I can get in on that. We can talk about it again in the future. Chris: Yeah, for sure. For sure. Tony: So, for this particular book, for Unconventional Medicine, people are fired up, they’re hearing about it, they’re like, “Okay, this resonates with me. I’m a practitioner, I’m an allied health provider, I’m a patient, I’m ready. Now’s the time. This is it. We’re going to do this.” What’s the best way for people to get their hands on this thing? Chris: Well not surprisingly, Amazon. They have the best way to get your hands on anything. So it’s available in paperback, Kindle, and audiobook. We’re hoping [the audiobook] is going to be out today, the day this podcast is released. But it might be another two or three days. They’re just taking their sweet time to approve it. I narrated the audiobook myself. So you podcast listeners, I figured you might be into that, since you like to listen. Tony: They know your voice. Chris: Yeah, and just listening to something instead of reading it perhaps. So to that end, we have a special offer for podcast listeners, because I appreciate your support and I know many of you are already part of this movement, and some are wanting to get involved. So if you buy that paperback or Kindle version between now and Sunday night, you’ll get some really cool bonuses. The first is a free copy of the audiobook. So again, we wanted to include that for podcast listeners, since we figured you guys and gals are probably interested in audio. But there are two other things that are really, I think, fantastic. And one, they’re both tools to help you be more confident and persuasive and factual when you share your passion for Functional Medicine and an ancestral diet and lifestyle. Because we’ve had a lot of questions from people, both practitioners and non-practitioners alike. They say, “Oh, how do I talk about this stuff to my sister at Thanksgiving?” Tony: “Isn’t that that caveman diet?” Chris: Yeah, exactly. All of our ancestors died when they were 30, so why should we even care? How do you respond to those arguments? Or if you start talking about Functional Medicine and maybe one of your conventional medicine colleagues says, “Oh, that’s just, I saw something on Science-based Medicine that said that was all just hooey. There’s nothing to it. How do you respond to that?” So what we wanted to do is give people the ammunition they needed in a respectful way. You know, this isn’t about getting the better of somebody. It’s about responding in a factual and convincing but respectful way. So we’ve got two different, we’re calling these the Power Packs. And one is for practitioners, so clinicians, health coaches, nutritionists, trainers, etc., and these are facts, research that you can reference and persuasive reasons for your clients or patients or colleagues to consider this Functional Medicine and ancestral diet and lifestyle approach. And then we have one for non-practitioners called the Supporter Power Pack. And these are smart answers and compelling comebacks, again respectful, for those common objections that you hear when you start talking about this stuff with your friends and family. So these bonuses are available until Sunday night [November 12, 2017] at 11:59 p.m. Pacific Time. So you’ve got a few days to act on that, and you can go to ... we set up a special link for you to get these and that’s Kresser.co/bonus. That’s Kresser.co/bonus. So head over there to get your Power Packs and your free audiobook, and that’s after you purchase either the paperback or Kindle. There’ll be a place where you enter your order number and we ask for some information just to verify, and I hope you enjoy those and get a lot out of them. Because they were actually really fun to put together. Tony: Yeah, I think the audiobook is huge. I like to listen to audiobooks when I’m driving around town or outside getting some exercise. Chris: Yeah. Tony: So, no excuses when you make it that easy. Chris: Yeah, yeah. So, Tony, thanks so much for doing this. This has been really fun to talk to you, as it always is. And I appreciate it. Tony: Actually, I wanted to throw in one extra little special thing, as we mentioned, at the top of the show. I spent 10 years as a personal trainer in the trenches, I was involved with Paleo Magazine for many, many years, going to all the events, and for me kind of an evolution in my professional life was, how do I impact more people? How do I help more people? And at first I was working one on one, and then it was as a facility manager helping other trainers and coaches get better. And then I was able to scale it up that way. And last year I had an opportunity to join the team over at Natural Force, which is all-natural, nutritional products, and I basically said, “You know what? I’m going to go all in on this because if I can touch a million people through really good, high-quality nutrition, that’s me maximizing my impact and really kind of living my purpose.” So one of the things I wanted to do today is put it out there for anyone listening who maybe uses collagen or MCT oil or whey protein. We really bend over backwards to source the best ingredients in the world, no additives, all that stuff. Everything is as clean as we can possibly make it. It takes a lot of work, working with manufacturers. Kind of like what you were saying, how patients have to know how to talk to their doctor. I don’t think people really realize, and I didn’t realize until I got on the inside, how much work it is for a brand to work with their manufacturers to convince them to get outside of the conventional mold. So it’s the kind of unconventional nutrition is really what we’re pushing here. So I set up a discount code for any Revolution Health listeners. Go to NaturalForce.com, use coupon code “unconventional” and get $10 off plus free shipping on your order. So I just want to put that out there as just a little extra bonus for anybody, and I would certainly love to help in that way and really get some good, high-quality nutrition into people’s hands. Chris: Awesome. Yeah, and there’s so many ways people can help, and I ... at Paleo f(x) we’ve see the growth of companies that are serving this space, and it's amazing. Like the products that are available now. I had breakfast this morning, I had some eggs and kale and parsley and a little bit of bacon in a couple of cassava flour tortillas. Breakfast burritos. Whoever thought I’d be having a breakfast burrito again? Tortillas are made from completely cassava flour. They’re autoimmune friendly and they’re grain-free tortillas. It’s incredible. Tony: I think I might have some of those in my fridge as well. Chris: Yeah. I mean there’s so many things. And these people, they’re serving this movement with that kind of work. So it’s great to see. Tony: It takes a village, man. Chris: It does. Thanks again, Tony. I really appreciate it. Thank you, everybody. So again, Kresser.co/bonus to pick up your free audiobook and the other bonuses, and I hope you can all join me in this revolution to reinvent healthcare. We need you, whatever your background and goals. Take care, everybody.
Source: http://chriskresser.com November 08, 2017 at 04:12PM
1 note
·
View note
Text
My MAcc Experience: A Guest Post by Ben Ma, MAcc
Ello, I am not Annie. She asked me to write a lil bit about my experience in MAcc. I am her not-imaginary boyfriend/supplier of stuffed animals. A lil intro about me, for those of you that don’t know, my name is Ben Ma, I recently completed both the MAcc program at UWaterloo and the CFE. I’m starting work as a Taxation Analyst at CIBC. Some of you may know me as:
Former VP Education of AFSA.
One of the Tax Mentors at UWAFSA’s Tax Clinic.
The Textbook Guy.
I have an unhealthy obsession about puns, mangoes and the Canadian Tax system (I kid you not).
I’m going to preface this post with a few notes:
I haven’t taken all the courses, and obviously my discussion isn’t necessarily representative of an MAcc discussion.
I’m a self-proclaimed tax geek, so almost all the courses I took were tax electives. Some I recommend for all people, tax or otherwise, some I don’t recommend at all.
I’m going to say a lot of bad puns. Deal with it.
I’m going to break this down into two sections – the courses, and the MAcc experience.
♛ MACC EXPERIENCE ♛
I am going to say this upfront: You don’t learn any new content in MAcc. What you learn in MAcc isn’t so much new information, but more so of a new way to approach a situation, and learn how to write cases, and present information in such a way that it would be useful to a user. You’ll have already learned everything you needed before in an undergrad course- now you need to … Master that knowledge.
There’s also no homework that you technically need to do. Same as undergrad, you could probably not do assignments/cases and just coast on by. But you are going to suffer a LOT if you don’t prepare for class. Because MAcc is just so case-based, not doing the cases takes out at least 50% of the learning. For the love of God, if you didn’t prepare for class before, now is the time to do it.
If you thought you did well in undergrad and none of this advice applies to you, get your head out of your ass. I went into MAcc with an 88% average, and I still managed to get a 28% on a final exam. Now’s the time to start preparing for class, reviewing, and for the love of God, start showing your work. In MAcc your final answer doesn’t really matter that much unlike in undergrad. I struggled in the beginning because I would just go straight to the answer. But now what’s important is your process. You could be completely off base with your final answer, but if you showed your work 90% of the way, you can probably get 90% of the answers.
♛ COURSES ♛
Considering how the MAcc program is really just a substitute for a PEP program, and is really just a super prep course for the CFE, I think it would be reasonable to talk about how well the course prepares you for the CFE, and how interesting/useful it is.
MANDATORY COURSES
ACC 611: Financial Reporting
One of your mandatory courses for the first term. Ya know all those X91 courses in AFM? Here’s a situation and now let’s do parts A B C of the question? Yeah, I don’t think you can count on those courses anymore.
ACC 611 is really one of your big exposures to CFE style cases, and it’s a huge change from the way undergrad wanted you to present information. Now the focus isn’t so much on the solution, but on the process that you used to approach the situation. This course also put a much bigger focus on actually knowing the accounting standards. I really struggled in this course (this is the one I bombed the exam on) because I didn’t have a structure, and I essentially guessed my way around the exam. Thankfully I ended up fixing this before the CFE. A big part of how to improve and prepare in this course is just a LOT of practice. After a while, you start becoming more familiar with the standards, and how to approach the problem. A big thing that helped me fix up my approach was starting to use a case writing structure.
Outline the issue
Discuss the standard if applicable
Apply case facts to the standard
Recommend corrections if necessary.
ACC 680: Managerial Accounting
Remember AFM 211? Welcome back to it. This course is essentially a more difficult version of AFM 211. You’ll become very familiar with how to structure a DCF in this course. Thankfully that’s really the only thing that’ll happen in this course, a few variations on how to do a DCF, it’s really quite … manageable. I usually found this course to be a lot more straightforward than the other courses, what they usually want is the same: one quantitative analysis and a qualitative analysis, and provide a recommendation based on that. A lot of how to prepare for this class is really do a lot of practice cases until DCFs are ingrained in your mind.
CPA ELECTIVE COURSES
The CPA elective courses are supposed to represent the four elective roles that you can take in the CFE: Audit, Tax, Finance and Performance Management. Each course will teach you how to achieve depth in that particular area. I only took Tax and Finance myself.
ACC 607: Tax
This course is essentially AFM 462 intensified. You’ll do a case every single week, and they’re not going to be easy, it’s quite…taxing and you may or may not have to remember obscure tax facts. Here’s the thing about tax though, you’re never expected to have a perfect answer. In addition, any case in ACC 607 will be twice as hard as any case in the CFE. I honestly believe that the ACC 607 course overprepares you for the CFE, to the extent that you’ll be very comfortable doing the tax role if you decide to do it.
For this class, again, you should at least attempt the practice problems. In this case you’re always going to miss something though. I think it’d be more helpful to do these cases in a group setting, and make sure you take very detailed notes in class, this is the one class where notes in class are very important. I find tax to inherently be very reliant on technical aspects, more so than the other electives – note taking is imperative as a result.
ACC 690: Finance
This is one course I don’t recommend. Yes, it does provide you the information you need for the CFE, but I honestly feel like the course is just a rehash from some undergrad courses. Some of the slides are the same as 3rd year AFM 373... typos included. It’s also the only one of the elective courses that doesn’t test you on a case based exam. It’s not hard to prepare for this course either, you can’t really exceed or do poorly in it. All in all, compared to the other CPA Elective courses, it’s not as well designed or structured in my opinion.
If I had to recommend 2 courses that you should take, I would recommend Audit and Tax. Lame standard choices I know. But I think that the things you learn in these courses are harder to pick up on your own, whereas the things you learn in the other courses can be learned through practice or common sense. Needless to say, you should also choose electives that match the role you’re planning on taking for the CFE.
MACC ELECTIVE COURSES
ACC 605: International Tax
If you are not a fan of tax, this is not the course for you. This is a very tax research-heavy course that will discuss the implications of taxes in multiple jurisdictions and how the Canadian Tax system accounts for it. Though this is a great way to understand how tax works, I have to admit, this will not be useful for the CFE. At all. It’s unlikely you’re going to use this in work either, as it’s a very complex topic and requires a lot of expertise and research, unless you’re going into some international tax advisory role. Definitely not a course to take if you want a bird course. But if you have a passion for tax, I highly recommend this course. It’s hard, but satisfying when you understand it.
ACC 662: Tax Policy
I didn’t take this course, but I’ve talked to a lot of classmates about it. You know how I said International Tax was tax research-heavy? This one is even heavier. This is a course that teaches you why and how policymakers develop taxes, and you’ll write some essays on particular topics. Again, not an easy course, and not for those who don’t like tax. But if you’re considering a PhD in the future, or a future in academia, or even tax policy, this is highly recommended, as this will literally walk you through what you need to do when researching tax.
ACC 690: Tax for the CFO
I cannot recommend this course enough, especially if you’re entering a tax role in industry. This course teaches you how companies actually prepare tax provisions and it’ll give you a very good understanding of IAS 12 (Taxes), combining accounting and taxes in a comprehensive way. It’s useful for the CFE, as it’ll teach you IAS 12 very thoroughly, and adjustments to reach taxable income if tax is your weak point. I’m currently in a taxation role at CIBC, and what I did in this course is going to be directly transferable to my role.
ACC 606: Business Valuations
I also highly recommend this course. One of the major parts that you can be tested on in Finance is valuations. This course teaches you how to approach a valuation, and is incredibly useful for the CFE if you are weak in Finance. If you’re a Finance person, this course also moves you directly to the second exam for the CBV designation if you’re interested.
♛
Well, that’s pretty much my overview of what I thought about courses and how to prepare for them. If you have any other questions, feel free to reach out to me. I can be reached by Facebook, Twitter, summoning through the Dark Arts, or smoke signals.
2 notes
·
View notes
Text
Increase Traffic by 88% With a New Keyword Research Strategy Ft. Emily Maxie of Very (Inbound Success Ep. 78)
How can a simple change in your keyword research approach dramatically increase traffic, leads and revenue?
Emily Maxie
This week onThe Inbound Success Podcast I spoke with Emily Maxie, VP of Marketing at software development company Very, and Stacy Willis, Emily's strategist at IMPACT, about the incredible results they got by focusing on pillar content and topic clusters.
The two of them shared how they worked together to revamp Very's SEO strategy and why the new approach they used for keyword research at Very has inspired Stacy to change how she carries out keyword research for all of IMPACT's clients.
The results of this work are impressive - an 88% quarter over quarter increase, and 1100% year over year increase, in website traffic, along with notable improvements in the quality of the company's leads.
This week's episode of The Inbound Success Podcast is brought to you by our sponsor, IMPACT Live, the most immersive and high energy learning experience for marketers and business leaders. IMPACT Live takes place August 6-7, 2019 in Hartford Connecticut and is headlined by Marcus Sheridan along with keynote speakers including world-renowned Facebook marketing expert Mari Smith and Drift CEO and Co-Founder David Cancel.
Inbound Success Podcast listeners can save 10% off the price of tickets with the code "SUCCESS".
Click here to learn more or purchase tickets for IMPACT Live
Some highlights from my conversation with Emily and Stacy include:
Very is a software development company that focuses on IoT and machine learning.
The company was doing digital marketing and while it was successful in driving traffic to its site, it was the wrong kind of traffic and the leads were unqualified.
Working with her strategist, Stacy Willis of IMPACT, Emily identified three key topic areas that all fit within service offerings that would be the right fit for Very, and developed a pillar content and topic cluster strategy aimed at building credibility in those areas.
For those three main topic areas, Stacy and Emily used SEMRush to identify the related keywords that had the highest search volume and lowest competition.
Pillar content needs to be at least 4,000 words long and to gain immediate traction while her team worked on creating that long form content, Emily started by publishing blogs that were focused on her subtopic keywords.
Emily makes it easy for her team to produce content on highly technical subject matter by interviewing her company's subject matter experts and then writing the blogs herself, but giving them an opportunity to review the articles for accuracy before they are published. Her big tip? Don't "write past what you understand."
Emily began posting the subtopic blogs at a pace of three articles per week in June of 2018 and before she could even publish her pillar content, the company saw an 88% quarter over quarter increase in website traffic.
As of this January, the company's year over year traffic increase has been 1100%.
Very is now also ranking number one for "IoT application development" and for "IoT app development" - two of its target keywords.
Stacy shared that the experience with Very has been so positive that it has inspired her and the team at IMPACT to change the way we approach keyword research, and now they focus exclusively on keywords that are related to their pillar content topics.
Resources from this episode:
Save 10% off the price of tickets to IMPACT Live with promo code "SUCCESS"
Visit verypossible.com
Check out the Very blog and resource center
Connect with Emily Maxie on LinkedIn or follow her on Twitter
Connect with Stacy Willis on LinkedIn
Check out two of Stacy's favorite keyword research tools: SEMRush and Answer the Public
IMPACT's pillar content on website redesign
For great examples of companies and people doing inbound marketing really well, check out Emily's recommendations, Women Who Code and Harvard Business Review, and Stacy's recommendation, Invision.
To stay on top of the latest changes and trends in the startup world, check out Emily's recommendation, the Reboot Podcast.
Listen to the podcast to learn more about the changes that Emily and Stacy made, and get the specifics of their new keyword research and SEO strategy.
Transcript
Kathleen Booth (Host):Welcome back to the Inbound Success Podcast. This week on the Inbound Success podcast, I have two guests. One is Stacy Willis, who is a strategist with IMPACT. And the other is Emily Maxie, who's the VP of marketing with Very. Welcome to the podcast.
Emily Maxie (Guest): Thanks. It's great to be here.
Emily, Kathleen and Stacy recording this episode
Kathleen: Stacy's been on the podcast before. She's a familiar name. You haven't been on before. Tell my listeners a little bit about yourself, your background, and also about Very.
About Emily Maxie and Very
Emily: Yeah, absolutely. So, my long ago background, I went to school thinking I was going to be a journalist, and graduated the year that the iPad came out. And all newspapers were laying people off. And so I worked at a newspaper for about a year, but ended up pivoting into marketing pretty quickly. And landed doing marketing at a technology company, and just really love doing marketing at tech companies because it's kind of the fact based very analytical side of journalism that I love.
But it's also an ability to be creative, and it's much more in demand than print journalism is. And yeah, it's just kind of my niche, and it's something I love. And then Very is a software development company that focuses on IoT and machine learning. And we have been around for about seven years. I've been with them for about a year and a half.
Kathleen: And IoT, for anyone listening, is the Internet of Things. Which I feel like I want to ask you to define that, but I also know that that's an incredibly hard thing to define. So I don't know, are up for it?
Emily: That's like the Pandora's box right there, right? Yeah. I can give kind of ... I'm sure this isn't the official definition and it might make our technologists cringe, but for the marketers out there, any devices that you have that are connected to the internet is the Internet of things. So we've seen the refrigerators that are connected to the internet and you can see inside of them from your cell phone or things like that.
We recently created a connected fish tank where you could turn the lights on and off, and check the water temperature from your phone. So all of those interactions between our physical world and the internet is what Internet of Things is.
Kathleen: That's so cool. Well good definition. All I could think as I was listening to you say that is the last thing I want to be able to do is see inside my refrigerator, unless I absolutely have to because it's gross.
Emily: Yeah, yeah.
Stacy: And that refrigerator that can tell you when something's gone bad. That's great.
Yeah, or if you're out of milk.
Kathleen: I saw something in People Magazine the other day and it was Ryan Seacrest's refrigerator, and I'm not kidding, it looked ... There's no way they cook in that house. And he had baskets with ribbons on them inside of his refrigerator. And I think the only food in there was like spirulina shots.
If I had that fridge I would be fine looking at it all day.
Stacy: Of course.
A Keyword Strategy for Very
Kathleen: So interesting. So the reason that I was excited to talk to you guys, the two of you, is that you worked together on a really interesting effort to revisit the keyword strategy for Very, and it had some really impactful results.
So let's rewind the clock and start with really what ... First of all, obviously Very is doing digital marketing. That's what you're focused on. What are your goals? What type of clients are you looking to bring in? And what types of keywords were you targeting?
Emily: Yeah. So really our goals ... I came in a year and a half ago being the first marketer that Very had ever had. They'd been in business for seven years and never had any marketing. And it all had just been the partners out there hustling and using their personal network, some things like that. And the first time that we had someone reach out to us through the website, it was like magic to them. They were just like, "What? This is so much easier."
After that happened I was really able to kind of not only grow the marketing budget, but I think elevate marketing within the company as more than just fixing the website or making things look pretty, stuff like that.
So really, our goal with marketing this year is to drive millions of dollars of revenue for the company. Last year marketing drove 2.2 million for the company, and that was our first year actually doing marketing.
So I'm really excited about 2019, and the keywords that we were focused on. Well, we spent about a year focusing on the wrong target segment. So we now rank really highly for a lot of blockchain related keywords, which is not a segment that we're going after anymore. So it might be something that we go after in the future, but we just really found that ... You think Internet of things is hard to explain, try explaining blockchain.
And also just there was a lot of immaturity in the market. People didn't really know what they were buying or what they wanted. There was this gold rush with initial coin offerings where people got money overnight and then they were spending it very recklessly and it was just not the type of client that we wanted to work with for now. But that was really what we were focused on, with kind of a secondary focus on IoT and machine learning, which are now the core tenants of our business.
Kathleen: So if I'm hearing you correctly, it sounds like what you're saying is that you understood that they were the wrong keywords mostly because the type of client you were getting was a poor fit. Is that accurate?
Emily: Yes. We understand now that they were the wrong keywords because we ... And SEO and AdWords were not the only things we were doing, we're also sponsoring conferences. And so we were doing huge push across the board for these types of clients. And we kept getting people raising their hands and saying, "I have a project." And then they would move through the sales cycle and then, "Oh, I don't actually have funding." Or they'd get to the end of the sale cycle and then we'd just never hear from them again.
We should have pivoted faster away from it, we should have seen it faster, but we have a pretty long sales cycle so it took us awhile to identify. Yes, we're getting tons of interest from this, but it's not the right fit for our business.
Kathleen: Yeah, that's really interesting. I think that's definitely a situation I see a lot. And I've seen it with a lot of clients we've had at IMPACT and when I had my own agency, we saw it too. Inbound marketing can work really well, and you can be getting lots of leads and still not feeling like it's right. And that's a familiar refrain to me. So you recognized that you were driving leads but they were not the right kinds of leads. And at the time you were working with Stacy, correct?
Emily: Yep.
Kathleen: So you guys sat down, and how did you approach the challenge of determining what is the best way to attract the right kind of lead?
Emily: Go ahead, Stacy.
Kathleen: I'll let you start. Or you want me? Okay. You want me to jump right in?
Emily: Yeah. Go for it.
Stacy: What we wanted to do when we were looking to put together a holistic keyword strategy was to not isolate ourselves so far down one path, but to make sure that we were building credibility on a number of topics that all fit within service offerings that would be the right fit for Very. So full disclosure, at the time that we created this, we still weren't 100% sure that blockchain was the wrong one. So it is one of the three topic areas we did cover.
But what we did was we created a bit more breadth, and made sure that we had three major topic areas we were going after. And organize these into a topic cluster kind of keyword strategy. So I'm sure that most people hearing this will probably be familiar with what pillar content is. But if you're not, it's the organization around a high level topic area, and then you'll have subtopics that are highly related.
So the example that we always use from our own website is website redesign. And separately, a subtopic from that might be how much does the website redesign cost? It's a really specific area of that main topic. And so we wanted to go ahead and create a wholistic strategy for Very. That worked to give us coverage over three topic areas instead of just a single one.
Kathleen: And what were those three topic areas?
Stacy: So at the time that we created it, it was blockchain, IoT, and machine learning, were the three.
Kathleen: And how did you ... And knowing the situation you had previously with that wrong type of client, how did you approach this in a way that you felt would eliminate that same issue from happening?
Emily: So just to clarify, we realized that maybe two months ago and we did this keyword strategy probably five or six months ago. So it was after we did this keyword strategy, we got a ton of volume in the door, and then we were able to see, okay, two hits, one miss. And we're able to kind of eliminate blockchain from the bunch. But at the time of developing this, we were still very focused on blockchain. And in fact, it was the one that we're most focused on.
Kathleen: Wow. That is so interesting to me because that, what it says to me is that the new strategy worked really quickly if you were able to see that fast.
Emily: Definitely.
Kathleen: And it worked in the sense that it did deliver leads, but they were the wrong leads and you realized it. So that's so interesting. All right, so let's go back to before you knew that you didn't want to target those.
Stacy: Naive little Emily.
Kathleen: Yeah. And no, I mean I don't think if there's anything naive about it, I mean I think this is just the reality in marketing is you have to try things and you have to watch them, and recognize quickly when they're not working and pivot. And so kudos to you for doing that.
Pillar Content and Topic Clusters
Kathleen: So going back, you identified these three big topics that you wanted to build clusters around that Stacy described. Walk me through the process that the two of you used to determine what those subtopics would be.
Stacy: So I was lucky. Emily just gave them to me. She knew what her team was really, really good at, which I think is really important. So I'll let her speak to that.
Emily: Yeah, I basically went to the team because we are a services company, we are very dependent on what our team's capabilities are. And because we're technical services company, it's not just, okay, we do blockchain, which we no longer do, but it's, we do blockchain, we build smart contracts. We don't work on this framework or that framework, we do work on these.
And so it got down in the very specific nitty gritty and the technical. And so I kind of gave Stacy a list of here's what I think, I have no idea what the search volume is. And then she curated that list, and said, "Okay, here are some of the keywords related to these that we should be going for."
Kathleen: Okay. And Stacy, so Emily delivered this list to you. How did you go about evaluating that and coming back with those recommendations?
Stacy: Well, I'm a giant nerd. So I enjoy diving into really, really specific data. So not everybody may get as super excited about this as I do, but-
Emily: No, we must both be giant nerds then, 'cause this is what I like to talk about every week. So-
Stacy: Oh, that's good, that's good.
Emily: Yeah.
Stacy: So then nobody's gonna hold it against me as I talk about it at length right now. Excuse me. Apologies, I'm fighting a little bit of a cold so I might cough throughout this.
Kathleen: Oh, there is something going around.
Stacy: Especially if I get more excited. Yeah.
Kathleen: There's something going around and these were the times when I'm happy that I can podcast over zoom so that I don't get your cold.
Stacy: Darn, I wanted to give it to you.
But what we did internally is we went and dove into a tool called SEMrush, which is possibly one of my favorite tools of all time because it gives you access to the greatest level of data on keywords that's out there. What we did is took the areas in which we knew that the team was really good at delivering, so those three topic areas, and said, "What are the combination of the terms that have the highest search volume?" So that's the most number of people out there looking for those terms.
And the lowest competition. Essentially not that many other websites are competing with you trying to rank for the same term. And what bubbled to the top throughout all this research of keywords that were related to these areas, keywords that were maybe variations of ways to say this.
The example that I can put there is machine learning and artificial intelligence, kind of ended up being synonymous terms. But they're very different terms when you're thinking about search, right? They have no words in common, but they're highly related. So it really helps to know which way people are referring to it to find you, right?
And so what we did is we looked at all of those kinds of related terms and bubbled up to the top those that had the best potential based on that search volume and competition crossover. And we organized them into a structure that looked like we talked about what these topic clusters were.
There was a high level keyword which is our big very general topic area that had a very high search volume. And then we connected all of the smaller subtopics that we found that were the best crossover of that high search volume, low competition, that are more specific.
And some of the tools that we use when we're trying to get a little more specific with our keywords or things like Answer the Public.
Kathleen: I love that one.
Stacy: That's one of my favorite. Yeah. It-
Kathleen: They also have the best website home page experience with that grumpy-
Stacy: Oh my gosh. I sometimes will sit there and watch his face for about 30 seconds because I'm like ...
Kathleen: Same.
Stacy: I just need someone to be mad at me for about 5 seconds.
Kathleen: He's mesmerizing. So if you're listening and you've never gone to answer the public, check it out and there's this super grumpy older man on the home page, and it's awesome.
Stacy: Yeah. It's great. He's judging you for how fast you're typing in your keyword. It's hilarious.
Kathleen: Okay, so you used to answer the public.
Stacy: Yeah. So we pulled the data out of SEMrush, we bubbled up the best opportunities, and then we go to answer the public to say, "What questions are people asking about these terms that we want to be answering?"
And so what we did was we actually started building out all of our subtopic blogs before we even started on our pillars. So pillar content is typically 4,000 words and above. So we're talking pretty hefty material that takes a little while to get all of the content put together that get maybe the subject matter experts you need on board and get something out the door.
So we didn't want to hold that up. So we put together the full editorial calendar of all the subtopic blogs and started diving into those first. And I can let Emily share how she worked with her team to get those moving and forward because I think that's probably her journalism career coming out. I've never had a client that's been so great at getting content out the door.
Creating Content for a Highly Technical Industry
Kathleen: Ooh, Emily, I need to hear about this because this is the universal challenge that all marketers face. So talk to us.
Emily: Yeah. Well, first of all, I've never been at a company where I have had such a responsive team of experts. We're small company and we are completely remote, which means we all have to be really good communicators. And so everyone in the company is just great at getting back to me. And so that is one thing that really helps.
Another secret weapon thing of mine too is I'll interview them for a blog post on a topic. I'll write it up and then I'll tell them, "Hey, here it is. You can preview it. It's going live on this date. Please get your feedback to me before then."
And so it's not leaving it to them of a question like, do you have any edits? Is this approved? It's just saying, "This is happening." And I always give them their respectful amount of time. I'm always very respectful of the fact that they have a job to do. And there's been times where someone has been like, "Oh, I had edits, and it went live." And I'm like, "That's okay, it's the internet. You can go and you can make edits."
So that's kind of my sneaking enjoy of getting things out the door.
The other thing I'll say is just having a writing background. I write a lot of it myself. And then just get them to sign off. So for a lot of the topics I would just go and become a subject matter expert on whatever it was by doing research and things like that. And then running it by our internal subject matter expert. And they'd say, "Here, this wording isn't quite right. But other than that it's good to go." And that's-
Kathleen: I am impressed because it's ... I , it's one thing ... I've had lots of clients from lots of different industries over the years, so it's very funny and random, but I mean I know a weird amount about commercial landscaping and insurance. It's one thing to become an expert on commercial landscaping, it is entirely another to do research and make yourself into a subject matter expert on IoT machine learning and natural language processing. So I mean how do you do that? How much time does that take? And-
Emily: It's very time consuming. Yeah. So it is very time consuming, but again, the journalism background, really they taught me. I mean I had classes where they would say, "Go attend this event and deliver us an article about it within the hour." Because that's the type of thing you have to do if you're a journalist.
And so it's really kind of like going in, understanding as much as you can, not writing past where you understand. Don't go beyond what your understanding is.
But just doing a ton of research and not getting hung up on, is this perfect? And I think that's one thing that is really difficult for a lot of people. It's difficult for me. You want everything that goes out to be perfect and the best that it can be, but sometimes just getting something out, especially if it's a timely topic or something that is a new term that no one's ranking for, is getting something out is better than getting nothing out. And then you can go back and refine it in the future.
But at that point I was doing a lot more of that. Now I've moved into ... So I was director of marketing then, I'm VP of marketing now. And since being promoted I've been doing a lot more strategic work. And so I've offloaded a lot of that copywriting to IMPACT. And they're working with our internal subject matter experts on blog posts. But yeah, at the time I was writing a lot myself.
And in fact, this morning, I spent about an hour writing a blog post about something that the fun thing about being able to be a marketer and a writer is we can have a client who has a question, and I can just write something about it, and get it on the blog post that day, and have our sales team send it over to the client. And potentially win that deal because I'm just able to be very responsive and nimble.
Kathleen: That's fantastic. We have one of the partners at IMPACT is Marcus Sheridan, who's fairly well known in the marketing world. And he is adamant when he works with companies that they have an in house content manager. And he specifically tells them to hire journalism students. And I think it's for the reasons that you outlined, which is that they tend to be well trained in how to get the story out.
And I loved what you said about not writing past what you know, because I think that that definitely is a trap that marketers fall into. And sometimes it's because you want to sound smart. And there's lots of reasons for it, but I think understanding your limitations and sticking within the guard rails you have is a really good lesson. And I love that you give people those deadlines and say, "I'm putting it up. If I don't hear from you, it's going up regardless." Very smart.
Emily: Yeah. We also have just a great working culture at Very. And a very much a fail fast culture, and an agile, nimble, get out the MVP type culture. And so there are other companies that I've been at where there was a lot more bureaucracy around what goes out the door and who sees it, and the checks and balances and all of that. And here it's really just me, and I love that. I really find that interesting and engaging.
Kathleen: Yeah, the startup world is not for every marketer. Some absolutely love it and wouldn't have it any other way. And some don't need a ton of resources.
So I'm curious. Alright, you identified all these subtopics, you built out the themes you wanted for the articles. It sounds like you started writing as the pillar was being developed. Can you talk me through, how much content was this? And in what amount of time? How many articles did you put up?
Emily: That's a really good question.
Stacy: You guys were on pace for at least three a week for an entire quarter, is what the cadence is that we'd look like in terms of blogs.
Yeah.
Kathleen: Okay. Go ahead.
Emily: We're not still at that cadence. But that's what we were for a while.
Kathleen: Okay. And this started when?
Emily: This would be, we were looking at the launch of this strategy around June of 2018.
Kathleen: Okay. So that's when the articles started going up, or that's when you finished the strategy?
Emily: So that's when the articles started going up. So the really interesting thing about this is we built this strategy knowing that the capstone is the pillar, right? The pillar pages was gonna tie everything together. But what we found is because over the course of the quarter is when we were going to even get the first pillar out. So we were like, "We'll just tackle the subtopic blogs first, then they'll all be there ready for our pillar when the pillow goes live," right?
The Results of Very's Pillar Content Strategy
Emily: Well, before the pillar even went live, our traffic went through the roof. So it was really telling in terms of how we should overall be structuring keyword strategies going forward.
Stacy: And the results of this which had originally been, let's just put together three pillar content strategies, was now let's change the way we do keyword strategies as a whole for our clients at IMPACT. So that was what came out of this.
Kathleen: So when you say the traffic went through the roof, put some numbers behind that for me. What was it at and what did it go to?
Emily: So we saw an 88% quarter over quarter increase in traffic.
Kathleen: 88?
Emily: 88%, yeah. It went from 8,800 range of organic businesses, just organic, to 16,600 for the quarter.
Kathleen: In one quarter.
Emily: Yeah. So that's quarter two compared to quarter three.
Kathleen: Wow.
Emily: And the crazy thing about that is that in May of 2017 this was a brand new domain with zero SEO juice. When I came in, it was a 100 percent brand new domain.
Kathleen: Wow.
Emily: So our year over year growth this past year, January nine to January nine, compared to the previous period was 1100 percent gross.
Kathleen: Oh my gosh. And do you have any numbers around what happened to your lead generation? What was the growth there? And I know some of it is growth, but some of it is also just the quality of the leads. I'd be curious to know more about what you saw.
Emily: Yeah. So the really interesting thing is, obviously we dabbled in and in blockchain for a while, but we were also working on building up the topics around machine learning in IoT, and we have started to get in really, really high caliber clients. I wish that I could mention their names because they're names that you would recognize, but they're still in our pipeline and I definitely shouldn't.
But we have gotten through organic really high quality leads coming to us and saying, "You are obviously the experts in facial recognition." Or, "You're obviously the experts in building internet connected products."
And the content speaking for itself, we're ranking number one for IoT application development and for IoT app development. Several of those key words that if you'd asked us a year ago, it would've just been, no, that's not a thing that's possible. Maybe in five years or something like that. So yeah, we're definitely seeing the results in terms of business as well.
Kathleen: And how long is the typical article that you're producing? Are these 800 words, 1600 words? Do you have any kind of guideline around that?
Emily: I don't have any guidelines. I like to say right until the topic tells you to stop. Because again, it's kind of like getting too far out in front of your skis or getting to a point where you feel like you're just saying things just to say them. So I don't have any guidelines. If I had to guess, I would guess it's between 800 and 1600 words for the ones we're producing.
Stacy: And I'd say on average the ones that you've outsourced to IMPACT, probably run around the 1,200 range.
Emily: Yeah, that makes sense.
Kathleen: Now when did you wind up getting the actual pillar content up?
Stacy: That's a good question because it wasn't even in the quarter. No, where we grabbed all these results from, which is why it was so exciting. And we're like, "okay, all keyword strategies have to be done differently from now on." The blockchain one, I believe, Emily, was the first one to go up?
Emily: It was, and it was created in September.
Kathleen: And when that went live, did you see, again, any sort of a boost? I know that you wind up kind of shifting the focus away from that, so I don't know if that's the best one to use as an example. But I'm curious to know if that had an impact on the traffic as well.
Emily: Yeah. But not as much as I kind of thought. So we got about 300 views to that pillar page. But compared to the blog posts, it's nothing. And so I think really the thing that shines about this or thing that stands out about this strategy is the strategy itself. And I think the ... At least, I don't know what you've experienced with other clients, but for us the pillar page is kind of like an afterthought, and it's more of the strategy behind it. Yeah.
Kathleen: Well, it makes sense because if you have the more niche topics covered in the blogs, I think that tends to be what people are searching. So that does seem logical.
Emily: Yeah. And quite honestly with every pillar strategy, it's the combination of all of the pieces is what really drives the traffic. There's not really any one piece that you'd say, "Hey, this is the only thing that matters." It's really the fact that all of them are connected together.
Stacy: And Kathleen, we've seen this on the IMPACT website with our website redesign pillar.
The traffic boost that it's given all of the blogs that it's been connected to has been far greater than the traffic boost to the actual pillar itself.
Kathleen: Yeah, that's absolutely right. Interesting. So now at this point, fast forward to today, do you have all three pillars and clusters completely up? Or are you still working on some of 'em?
Emily: No, we're still working on the content for IoT and for machine learning. And really it's not because we've been slow on the marketing side, but our business has been figuring out exactly where we want to play. And within, we say we do IoT and machine learning, well both of those are huge umbrellas. That's like saying we're a marketing agency.
Well for who? And what do you do? And what technologies do you use? And so I'm still in the process of a couple of things. So first is working really closely with our sales team to do customer interviews and prospect interviews to figure out service market theft. And then the other thing is just publishing a lot of blog posts that could be potential pillar content reference material and seeing how they perform before going too deep into one.
A New Approach to Keyword Research
Kathleen: Interesting. And what would you say ... Stacy, I'll throw this one out to you. You talked about how this experience kind of inspired you to say we really have to change the way we do keyword research now and content strategies. If you had to distill this down into what was the biggest change that you made, the before versus the after, how would you describe that?
Stacy: Yeah. So the way that we use to deliver keyword strategies was, here's a list of keywords that are completely ... We're not even considering how they're related to each other. We're looking at each keyword on an individual basis and its own performance, which is still important. But what this has done is now involved a layer deeper where we're actually grouping our keywords that we're recommending clients target into groups of related clusters.
So if we ever are presenting a keyword strategy to a client and there's a single keyword, they're saying, "Go after this keyword," and there's nothing else related to it, that's not gonna happen anymore, essentially.
So that was kind of the old way, that you know, it's been the way since inbound became a thing. It's get your long tail keywords and write a blog. And you just think about that one keyword at one time for one page, as opposed to thinking of it more holistically across your website, of how many keywords do I have in this group that can all lead up to the same topic area?
And so now we're making sure that if we are putting together a keyword strategy or an editorial calendar that we are grouping topics together into groups like that. Because when we saw that even before we had all of the pillar built up together, that was a signal to Google that we were a topic area expert. And they rewarded us greatly for it.
Kathleen: That's interesting. Now have you seen that ... What is the pace of growth look like since that first big jump? Has it been fairly steady, or?
Emily: Yeah. Yeah, it's been pretty steady. I would say that we have some months that it looks like, "Oh, it's not growing quite as fast" and part of that is just we have backed off on the content creation to focus really hard on the business strategy. So that then we can go back and go hard, and know that we're making the right bet so that we don't make the same mistake again that we made with focusing on blockchain.
Kathleen: It is so interesting how literally as you scale up and scale back content publication, it's like turning the faucet on and off. You can really see a direct correlation to traffic and leads-
Stacy: Definitely.
Kathleen: And that's fascinating. Interesting. So if somebody wants to check out your site and see some of this content that you're talking about and get a sense for what you guys are doing, where can they find it online?
Emily: Yeah. Our URL is verypossible.com. And you can go to our blog or you can go to /resources, which is the place where we have a lot of videos and white papers and things like that. And you can find the pillar page there as well.
Kathleen: By the way, I love your domain name.
Emily: Oh, thank you.
Kathleen: Yeah.
Emily: Yeah, talk about SEO Challenge when your brand name is Very, forget about branding traffic.
Kathleen: Yeah, that's tough.
Kathleen's Two Questions
Kathleen: Well before we wind up, I do have two questions I always ask my audience. And I'll start with you, Emily. Company or individual, who do you think is doing inbound marketing really well right now?
Emily: So I'm going to be a terrible marketer and just let you know that I don't keep up with other marketers because I'm really occupied keeping up with technology so that I can be really good at my job where I'm at. And that's one reason I work with Impact is because I need people to help me who are keeping up with the latest trends and things like pillar content and stuff like that.
Kathleen: So my question for you is - and I love that answer because I actually am more fascinated to hear about your experience as a consumer of content - so you just said you try to keep up with technology. Is there a technology website or blog that you think is doing a really great job?
Emily: Yeah.
Kathleen: Who do you like to read?
Emily: I love Women Who Code. I love reading HBR, Harvard Business Review. Yeah, Women Who Code is really my favorite newsletter because they keep up with both women and tech stuff, but also just trends in the industry and things like that.
And we're also ... Another thing that I'm just passionate about is women in tech, and we're really trying to recruit female developers. And so I'm looking at not just how are other tech marketing themselves, but how are they marketing themselves as an employer brand. And so figuring that out and kind of seeing what other people are doing.
Kathleen: Ooh, I'll have to check that out because I'm kind of curating my own list of really good email newsletters. So that sounds like a good one to add to it.
Emily: Yeah.
Kathleen: And I love examples from outside of the marketing world.
Emily: I also love the Reboot podcast, which is just a very grounded and thoughtful podcast about being in a startup and kind of keeping your head on straight while you're at a startup. So that's a really good one too.
Kathleen: Ooh, that sounds like a good one. And it sounds like I already got my answer to my second question from you, which is, with digital marketing changing so quickly, how do you stay up to date? And it sounds like what you said is for you at least it's relying on an agency to kind of keep you up to date.
Emily: Absolutely.
Kathleen: Yeah.
Emily: Yeah. I'm a one person marketing team, and I do events and the website content. I'm now an interim head of sales for a little bit and covering for someone while they're on leave. And so I have a thousand hats. And being able to stay up on marketing is something that is so important, but I just don't have the time to do. And so that's the biggest reason that I work with IMPACT.
Kathleen: Great. And Stacy, I interviewed you recently and I got your answers. Any new tidbits to add to what we talked about last time?
Stacy: Yeah. Um, I'll just throw out that I've also very recently been super impressed with Invision. Their content production engine is amazing. Not only to people who aren't users, but their community for designers and the way in which they engage people to use their tools successfully.
So they have great examples of how you can use this part of their program or things like that I think probably go a whole heck of a long way in keeping their users satisfied and more engaged with their product over time, which is still a function of marketing, although we don't always think of it as such when we're really focused on bringing in new leads. But I've been really, really impressed with what they do.
Kathleen: Oh, that's a good one. I'll definitely check that one out. Well, thank you both. This was so interesting.
How to Reach Emily
Emily: Emily, if somebody wants to find you personally online, what's the best way for them to connect with you?
Emily: You can find me on Twitter @EmilyMaxie, M-A-X-I-E. Or on LinkedIn. The awesome thing about having a super weird last name is I'm the only Emily Maxie. So-
Kathleen: Perfect.
Emily: Just Google Emily Maxie and come find me. Yeah, I would love to connect and geek out about marketing or technology or whatever it may be.
Kathleen: I love it, and Stacy, what's the best way for somebody to connect with you?
Stacy: So directly through IMPACT's website is the easiest way to get to me, or on LinkedIn. And you can find my LinkedIn profile through the Impact website, which is probably easier 'cause Stacy willis is not a very unique name.
Kathleen: Well and I'll include links in the show notes to all of your various profiles.
Stacy: Awesome.
Kathleen: Thank you both. It's been fascinating. I'm really excited to check out some of the content, Emily, and just get a sense for what you guys did to get these great results. But I appreciate you joining me.
You Know What To Do Next...
Kathleen: If you are listening and you learned something new or you enjoyed this episode, you know what to do. I would love it if you would give us a review on Apple podcasts or the platform of your choice.
And if you know someone doing kick ass inbound marketing, tweet me @WorkMommyWork because I would love to interview them. Thank you, Stacy, and thank you, Emily.
Stacy: Thank you.
Emily: Thanks.
Stacy: Have a good one.
Want to stay updated when the podcast is released?
Drop us your name and email address below and we’ll send you the show notes every Monday!
from Web Developers World https://www.impactbnd.com/blog/increase-website-traffic-keyword-research-emily-maxie
0 notes
Text
RHR: A Three-Step Plan to Fix Conventional Healthcare
In this episode we discuss:
The patient case that inspired the book
Who is this book for?
The mismatch between our medical paradigm and chronic disease
Drug companies and conflicts of interest
How clinicians can help create a new paradigm
The three core problems and how to solve them
What this new paradigm looks like
How do we pay for this? Is it scalable?
How allied providers are the key
Show notes:
Unconventional Medicine by Chris Kresser
Special offer for RHR podcast listeners - get the audiobook free if you buy the book by November 12th.
NaturalForce.com - use coupon “unconventional” and get $10 plus free shipping
[smart_track_player url="http://traffic.libsyn.com/thehealthyskeptic/RHR_-_A_Three-Step_Plan_to_Fix_Conventional_Healthcare.mp3" title="A Three-Step Plan to Fix Conventional Healthcare" artist="Chris Kresser" ]
youtube
Chris Kresser: Hey, everybody, Chris Kresser here. Welcome to another episode of Revolution Health Radio. Today we’re going to do something a little different. I am bringing on a guest host, Tony Federico, he’s the VP of marketing for Natural Force Nutrition, a physiology editor for the Journal of Evolution and Health, and a longtime contributor to Paleo Magazine, and also at Paleo f(x), which is where I met Tony, I think, originally, and I have interacted with him the most. And he’s moderated several panels that I’ve been on and I’ve always been impressed with the way he’s done that, the intelligent questions that he asks and just his balanced perspective on ancestral health and Functional Medicine, and this movement overall. Today is the day that my new book, Unconventional Medicine, comes out. It’s now available on Amazon, and I wanted to ask Tony to come take over the podcast and talk with me about the book because I know he’s really interested in all these topics and he’s read quite a bit of the book himself, and I thought it would be more interesting to have a conversation about it than for me to just sit here and do a monologue. So Tony welcome to the show and thanks for being here. Tony Federico: Yeah, thanks for inviting me on, Chris. It’s always fun, when we’ve had the chance to chat, as you said. Whether in person or on podcast, I’m always happy to jump in and dish on health with you. Chris: Fantastic. So, you have read a little bit of the book and we chatted a little bit about it via email, so let’s dive in. Let’s talk a little bit about this book. And for me it was really, it felt like the most important next step that I could take in order to get this message out about ending chronic disease. Tony: Yeah, I got my copy of Unconventional Medicine a couple days ago. I just so happened to have some time off yesterday, and the next thing I knew I was 80 pages in. Chris: Nice. Tony: So, I have to say that, as somebody who’s been in the trenches, I worked as a personal trainer for 10 years, I could really relate to a lot of the things that you were saying in the book, and we’ll get into why a little bit later on in the interview. But you know I just am really impressed with what you put together here, Chris. So let's just, let's get into it, and the first thing that I actually wanted you to maybe tell me a little bit about was how you open the book, which I think is a really great story about a patient named Leo. So I wanted to talk a little bit about Leo and his story and kind of how that inspired you to go down this particular path of unconventional medicine.
The patient case that inspired the book
Chris: Sure, yeah. So, Leo was an eight-year-old boy that I treated in my clinic a few years back, and I wanted to start with his story because it's, unfortunately, a typical story, much more common than, of course, we would like. And it was powerful for me, it was a powerful experience. It's what actually led to me writing this book. So, like way too many other kids of his age, he was suffering from a number of behavioral issues. He was initially diagnosed on the autism spectrum. Eventually they settled on OCD and sensory processing disorder. He would throw these just crazy tantrums where he'd end up crying or screaming inconsolably, writhing on the floor, and this would happen for seemingly the simplest of reasons. Like trying to get his shoes tied as they were going out the door, not cutting the crust off his sandwich in just the right way or getting a stain on his favorite T-shirt. And he was really rigid around his behavior and its environment, everything had to be just right, just the way he wanted it to be, or else he would fly off the handle.
Is a new healthcare paradigm affordable? Scalable? You bet.
His diet was extremely limited, he only ate a handful of foods, pretty much all of which were processed and refined. So crackers, bread, toaster waffles, that sort of thing, and this is part of the kind of OCD-like tendencies. And any time his parents would try to introduce new food, he would go totally ballistic. And they were worried about nutrient deficiency, but they didn't feel like they ... they were just worn down. Any parent who has a kid like this will understand that. It's just they didn’t feel like they had the resources to battle him at every meal. And they took him to a bunch of doctors locally, and that’s where they got those diagnoses. Initially they were kind of relieved to have those, but then after a while they realized that they were just simply labels for symptoms. And when they asked what the treatment was, you can probably guess the answer: medication. Tony: Something to do with drugs. Chris: Something to do with drugs. Yeah. And when they asked how long he would be on that treatment, you can probably also guess the answer. Tony: The rest of your life. Chris: Yeah. Shrug of the shoulders, indefinitely, maybe he'll grow out of it, that sort of thing. And they weren't excited about the idea of of medicating their son, but they were also aware of how much he was suffering, and they were suffering, frankly, too. They decided to give them a try, starting with Adderall, and then they progressed to Ritalin and then antidepressants. And certainly the drugs did seem to help with at least some of the symptoms, but there were a couple issues. Number one, they also caused some very intractable side effects like headache, abdominal pain, irritability, and most significantly, severe sleep disruption. And they had a couple of other kids that were younger than Leo. So they were not happy about the sleep disruption. Nobody was because it was brutal for them and also brutal for Leo. Kids need a lot of sleep, and if they’re waking up throughout the night, that’s going to make ... So that was in some ways worse than the original symptoms they were trying to treat. And then Leo's mom had done quite a bit of research on the effects of these medications and she was scared. Particularly for children and adolescents, some of these drugs have some pretty scary side effects and long-term risks. So what really stood out to me, and I mentioned this in the book, is that not once during this entire process of seeing all these different doctors, primary care provider, psychiatrist, eventually behavioral disorder specialists, did anybody even hint at the possibility that something in Leo's diet or some other underlying issue like a gut problem or nutrient deficiency or heavy metal toxicity or something like that could be contributing to his symptoms. It wasn't even broached as a possibility at any time. Fortunately, Leo's mom, one of her friends followed my work and sent her a couple of articles from my blog. One was on the gut–brain–axis, and I think the other one was on the underlying root causes of behavioral disorders. And so that's what led them to bring Leo to see me, and long story short, we were able to ... we did a bunch of testing, found issues that you might guess at. So, disrupted gut microbiome, SIBO, fungal overgrowth, gluten intolerance, but also intolerance of soy and corn and rice and buckwheat, which were major ingredients in a lot of the processed and refined food products that he ate, and arsenic toxicity because rice milk was the only other beverage he would drink aside from water. And we know that rice products can be high in arsenic. So, we, over several months, it definitely wasn't easy to address these problems because of his OCD-like tendencies and his picky eating habits. But after several months he was like a different kid. His teacher even called home and was like, “What have you done with Leo and who’s this kid that you’re sending in?” Because it was a big issue for her. They often had to come to school and pick him up early because of the behavioral problems. And his diet expanded; he was eating foods he would've thrown against the wall just months before, he was more tolerant of disorder, more relaxed in his environment. They were able to travel for the first time in a long time because he wasn't so anxious in unfamiliar environments. His physical symptoms had improved significantly. So they were just over the moon. They couldn't believe it, and toward the end of our treatment together, she said something that really struck me, which was there’s so many kids out there that are like Leo and they’re suffering, they’re not finding help in the conventional system. Tony: Sure. Chris: And their doctors and parents are not even thinking about this stuff. Like it’s not even in most people’s consciousness that if a kid has a behavioral disorder that you should look at these physiological issues. It’s not, for 99 percent of people they don't even go there because they don't know. Tony: Yeah, I mean I think that that was—reading about Leo and reading about a story and certainly there's people that I've known, myself included, who have had very similar experiences—I think it's great to have a narrative like this that you can really connect to because then when you tease it apart, all the pieces really make sense. It makes sense why having doctors treat symptoms has failed, it makes sense why a lack of communication between the health provider network that was supposed to be serving Leo failed. It makes sense why it didn't work when you actually start to tease it out. But then we’re still all, well not all, but most of us are still going down this path and it's an exercise in futility, really. You have an eight-year-old kid who's on powerful stimulant medications, he’s on antidepressants, and it was bad enough for his parents to reach out and to seek those interventions as solutions, and then the side effects are even worse. And that’s just something that just gets you right in the heart. And like you said, he’s not the only one, he’s not the only kid. His parents are not the only parents. And frankly, his doctors are not the only doctors because I can guarantee you that that probably doesn’t really feel good for the practitioner, for the healthcare provider to not get results as well. And they’re working with what they’ve got. Chris: Absolutely. Tony: And trying to use the tools they have. Chris: Yeah, I mean, let’s be clear about this. Everybody is doing the best they can in this situation. The parents are doing the best they can, in the vast majority of situations, parents just love their kids and do everything possible that they can to help their kids thrive. I’m a parent, I know that that’s how I relate to my kid. I know that every parent I know, that’s how they relate to their kids. And I would even, I would say that’s true for doctors too. The vast majority of them are trying to do the best they can with the tools that they have and in the system that they’re working within. And that’s the rub. Tony: Right. Chris: It’s like most doctors I’ve seen have been caring and they’ve wanted to do the right thing, but the question is, can they do the right thing in the conventional medical system as it exists today? And, of course, that’s largely what the book is about.
Who is this book for?
Tony: Yeah, so let’s kind of speak to that specifically. And we’re talking about doctors, we’re talking about medical professionals, we’re talking about patients, and then we didn’t mention it, but where I fit into this formula or potential formula as an allied healthcare provider, as a personal trainer/health coach, is that your audience for this book, do you really see that kind of triad is who you're speaking to here? Chris: Yeah, definitely. I think if you look at the cover of the book, the subtitle is “join the revolution to reverse chronic disease, reinvent healthcare, and create a practice you love.” So that last bit would suggest that it's mostly for practitioners, but that's not true. It is really for anybody that is interested in the ideas of reinventing healthcare and reversing chronic disease. And, in fact, I would argue that that change is going to be initiated by people, primarily by people that are not practitioners. So it's like a grassroots, bottom-up approach, where a good example is with my training program, my ADAPT training program, now that we've been training practitioners in this approach for the last couple years, we always ask people how they learned about my work or how they learned about the training program. And in a surprising number of cases, the answer is from their patients. So these doctors or other practitioners, their patient brings an article in that I wrote or brings something in, tells them about me, and to their credit they’re open-minded enough to go and check it out. And then they like what they see and they end up taking the next step. So people even who have no intention of ever becoming a healthcare practitioner, I think would really benefit from this book if they're interested in these ideas. And then certainly, as you mentioned, licensed healthcare providers like medical doctors or nurse practitioners or physician assistants that are currently working within the conventional paradigm but have already seen its limitations and want to do something different but don't yet know what that might look like. And then people who are outside of the conventional paradigm but are already practitioners, so acupuncturists, chiropractors, naturopathic physicians, etc., in many cases they’re already well aware of the limitations of conventional medicine, which is why they chose to go down a different path. But speaking personally as an acupuncturist myself, I also saw some limitations in the traditional Chinese medicine approach, or at least some differences in the way that I wanted to practice it. I was looking for something that could incorporate modern diagnostic testing and create a more systematic approach that included ancestral diet and lifestyle and some of the other things we talk about in the book. So, I think many of those practitioners can benefit from the book from that perspective. And then you have the growing and already large number of people like yourself who are personal trainers, health coaches, nutritionists, etc., who I really think are going to play an increasingly important role in this revolution to reinvent healthcare. Tony: Yeah, it so important now for people to really, for patients to be their own advocate, and I don't think we’re living in a time where I remember with my grandparents—if your doctor said something, it was basically gospel and you didn’t question it and you didn't think about it. Now, the first thing people do when they experience a symptom, it's Dr. Google first. So it's super important to equip and arm patients with good information, which I think this book does. Here's a path, here's a path forward for you as a patient. But then it's respectful of the role of doctors, and you highlight many situations where conventional medicine is great. If you break your arm or get in a car accident or have a heart attack or whatever the case may be, yeah, you need a doctor, and you need to go to an emergency room and you need those types of interventions. But it's really in this kind of gray area, it’s really not gray, it’s actually quite clear. And we could probably specify a little bit more, but there’s this middle zone where somebody’s not acutely injured, they’re not acutely in a disease state. They’re in a chronic disease state, or they’re just unwell. And it’s hard for a system that is all about pharmacological interventions, surgical interventions, to deal with a more subtle approach. And that’s where that whole middle ground and acupuncturists and massage therapists and everybody who's in that middle zone. I had clients constantly when I was actively training, constantly asking me questions where I was like, you know what? This is really something they maybe should be taking to their doctor. But guess what? The doctor only has 15 minutes under pressure to see as many patients as they can. I had a friend who was a physician in France. And he was telling me about their medical model, and he would spend tons of time with his patients. And it was actually incentivized for prevention. And here we see some maybe misplaced incentives, and perhaps you can speak a little bit more about that.
The mismatch between our medical paradigm and chronic disease
Chris: Yeah, so, going back to your original comments, I think that the most important thing for people to understand is that our medical model, when it comes to our medical paradigm, is that it evolved during a time when acute problems were the biggest issues. So in 1900, the top three causes of death were all infectious diseases, tuberculosis, typhoid, and pneumonia. And the other reasons people would see the doctor were among those you mentioned, like a broken bone or a gallbladder attack or appendicitis. Tony: War. Chris: Right, injuries, trauma, etc. And so the treatment for that's pretty straightforward. It wasn't always successful, of course, but it was straightforward. You know, if the bone was broken, you set it in a cast. If the gallbladder was swelling, you would take it out. If someone was having appendicitis, you’d remove the appendix. So that's pretty ... it's one problem, one doctor, one treatment. Pretty straightforward. But you fast-forward to today, it's a totally different healthcare landscape. Seven of the top 10 causes of death are chronic disease rather than acute problems now, and 86 percent of the healthcare dollars we spend go toward treating chronic disease. And unlike acute problems, chronic diseases are expensive, difficult to manage and usually last for a lifetime. They don't lend themselves to that one doctor, one problem, one treatment kind of approach. The average chronic disease patient requires multiple doctors, usually one for every different part of the body in our system, and is taking ... Tony: Specialists. Chris: Right, specialists, they’re taking multiple medications in many cases, and they're going to be taking those medications for the rest of their life. So far, it's really, our conventional medical system is amazing for these acute problems. But it's the wrong tool for the job for chronic problems. So that's one issue, and it’s really important to point that out, because we just went through the whole healthcare debate again with the Affordable Care Act and the current administration’s proposal for a replacement, which has not come to fruition. But throughout that entire discussion, it really bothered me that there was an elephant in the room. All the discussion was around insurance. Like, who gets insurance and who doesn’t. And that’s important, it’s important to talk about that. But we have to recognize that health insurance is not the same thing as healthcare. Tony: Yeah. Chris: Health insurance is a method of paying for healthcare. And that’s really crucial to get that difference. Because my argument in the book is that there is no method of paying for healthcare, whether it’s the government, corporations, or individuals, that will be adequate and will be sustainable under the pressure of growing prevalence of chronic disease. It will bankrupt all of us. Government, the corporations, individuals, whoever is responsible for paying for the care will not be able to do it unless we can actually prevent and reverse chronic disease instead of just slapping Band-Aids on it. Tony: I think the analogy you gave in the book was rearranging the deck chairs on the Titanic. “Making a few small tweaks to our current system and expecting that to work is like rearranging the deck furniture on the Titanic as it inexorably sinks into the ocean. Too little, too late.” Chris: Yeah, exactly. That’s the argument about insurance. As the whole ship goes under, sinks under. The other problems you mentioned are very real also. So we have a misalignment of incentives, like the insurance industry, for example, doesn't benefit when the cost of care shrinks because they only make more money when the overall expenditures rise. So it's actually not in their best interest necessarily to seek out the most cost-effective solutions.
Drug companies and conflicts of interest
Chris: And then of course, we have drug companies. People are pretty well aware of the conflicts of interest there. It’s in their interest to sell drugs, and even when that’s not in the interests of the general public or the patients or the doctors. In many cases, it’s not in their interest either. So the best example of this is a recent one. We’re in the midst of an opioid crisis, the worst we’ve ever seen by far, and the DEA has been wanting to create new regulations that restrict a pharmacy’s ability to sell opioids in ways that will protect people. So, for example, there was a pharmacy in West Virginia in a town that was tiny. It had like 30,000 people in this town, and they had ordered something like nine million opioid pills in the last year. It was clearly a front, like there’s clearly something shady going on there. There's no way that 30,000 people in that town needed nine million opioid pills, and yet there are no regulations to actually prevent that from happening. And so, the DEA had proposed some regulations to just safely protect people from that kind of thing. And the Big Pharma lobby basically shut that down and they played a big role in writing a law that limits the DEA's ability to do that kind of regulation in the midst of the worse opioid crisis ever. And to put this in perspective, we hear a lot about the gun lobbies and their control. They spend about $10.5 million lobbying Congress, I think, per year. And Big Pharma, they spent $250 million. Tony: Wow. Chris: Twenty-five-fold higher. Tony: It's really tragic. I actually, I don’t think we’ve ever talked about this, but I grew up in South Florida, which was kind of ground zero for the opioid epidemic. And I remember in high school down in Miami and West Palm Beach, and kids would get a hold of a contact or whatever, somebody that had a prescription and basically would end up being a de facto drug dealer vis-à-vis a pill mill, etc. The kid across the street from me died, multiple kids in my high school died, multiple kids went into in-treatment programs, some of them battled addictions for decades. Some of them got out of it. Very few got out of it. Some of them didn't and have continued to be plagued with either switching from pharmaceuticals to street drugs like heroin, etc., and then we can see what's happening there. And that's just one example. If we look at drug consumption in the United States, is it that Americans are just that much sicker and we’re in that much more pain than people in other countries? Because we’re consuming far and away more painkillers than any other country on the planet. And I would venture to guess that you could say the same about antidepressants or ADD medication. It's very much a case of misaligned incentives. And incentives are working in the sense of the pharmaceutical companies are doing very well. Chris: Yeah. Who are they working for is the question. Tony: Exactly. Chris: We’re the only country aside from New Zealand that allows direct-to-consumer drug advertising, and I think that's a big part of the problem. But it's not just Big Pharma. We also have conflicts in medical research that, of course, are related to Big Pharma because they pay for two-thirds of all medical research. We have broken payment models, where there's no real incentive or reward for good performance, and in fact, you could argue it's the other way around because doctors are compensated for, usually based on the number of procedures they order and the number of patients they see. So to your point about the doctor in France who is actually incentivized to prevent, rather than just treat disease, we don't have that at all, it's the opposite. And so there are a lot of deeply entrenched issues that we certainly need to address, and that's not essentially what this book is about. There are other books that cover that material really well, and frankly many of those issues are outside of our individual control as clinicians or practitioners.
How clinicians can help create a new paradigm
Chris: We can work toward addressing them, and I think we should, but the good news is that I think that the bigger changes that we need to focus on individually and collectively are addressing the medical paradigm which we’ve talked about, creating a medical paradigm that’s better suited to tackle chronic disease. Addressing the mismatch between our modern diet and lifestyle, and our genes and our biology, which we've, of course, talked a lot about on the show before. And then creating a new way of delivering healthcare that actually supports this new medical paradigm and this more preventative approach. Because those things are all within our control as clinicians. Tony: Yeah. I like how you posed the question, and it was kind of a cool little, I think it was, not Hiroshi, but the person who is in charge of cooking at a Buddhist monastery. And basically a young monk comes up to this older man. He’s like, why are you doing the grunt work, basically washing rice out in the courtyard? And he says, it was like, what was it? “If not me, who? And if not now, when?” And I think that that’s really kind of the core of setting all this stuff up. Talking about the problem is really in the service of pivoting to the solution, and I’m a big believer in thinking globally, thinking big, but acting locally, hyper-locally, like yourself. Chris: Yeah. Tony: And then the people around you and who you can touch and impact. That’s ultimately where the power comes from. So let’s talk about that. What is in people’s power. And you started to describe some of those pillars of a new model. And you describe it as the ADAPT framework. And I don’t know how much you get into this on your regular podcast episodes, but to just kind of lay it out, ADAPT from a big-picture perspective. How does that actually address some of these systemic issues from an individually empowered stance? Chris: Yeah, great question, and before I even go into that, I just want to say I agree that I think the change is going to happen on different levels. So, because a lot ... we’ve talked about this stuff at conferences or even some people who’ve already read the book. They say, oh, this is fantastic. I’m so excited. But how are we going to deal with Big Pharma and the insurance industry and these misaligned incentives and all of that? And can we ever deal with that? The answer is we’re not going to deal with that overnight and it’s going to take a while to unwind those things. Tony: It’s the chronic disease, is what you call... Chris: Exactly, exactly. And I use that analogy in the book. But the good news is that changes can happen very quickly on an individual and local level. And there’s already a lot of evidence of that happening. So my own clinic, CCFM, tripled in size in the last three years alone. We have Cleveland Clinic Center for Functional Medicine, launched by Dr. Mark Hyman, has just blown up like crazy. I mean they started in this tiny space. Now their 17,000-square-foot space, it takes up the whole second floor of the Glickman Tower at Cleveland Clinic. They've got a waitlist of 2,500 patients from nine countries around the world. This is really exciting! The Cleveland Clinic is always on the forefront of the newest trends in medicine, and the fact that they've invested that much money in this speaks volumes. Then we have groups like Iora Health, an organization based in the Rocky Mountain area that’s reversing diabetes using health coaches. So there are lots of really interesting produced concepts, and there's going to be more and more of these. Like we’re doing a pilot program with the Berkeley Fire Department where we’re working with their new recruits to help, we’re implementing a wellness program. Tony: That’s awesome. Chris: To reduce injuries and help with recovery and optimize their performance. And if that goes well, there’s been interest from the wider fire department and in the city of Berkeley as a whole. Robb Wolf’s done some incredible work with Reno that we’ve talked about before. So I think the change is going to happen more quickly on this local grassroots level, and then that's going to start to get the attention of people on a state and federal level. And then it will start to get really interesting.
The three core problems and how to solve them
To answer your question, in my book I basically lay out three core fundamental problems with the healthcare system in the US. And these, I argue, go even deeper than the misaligned incentives and Big Pharma and all of that stuff, although they’re, of course, connected. The first is that there is a profound mismatch between our genes and our biology and our modern diet and lifestyle. And I'm not going to say more about that now because almost everyone listening to this podcast knows exactly what I mean. The second problem is the mismatch between our medical paradigm and chronic disease, which we just talked about. We need a new medical paradigm that is better suited for chronic disease. And then the third is that the way we deliver care in this country is also, it's not set up to support the most important interventions. And we’ve touched on that too, where the average visit with the primary care provider is just actually eight to 12 minutes. Tony, you were talking about 15 minutes. That’s luxurious in our current model. The average amount of time a patient gets to speak before they’re interrupted by the doctor is 12 seconds. Tony: Wow. Chris: So I think it’s pretty clear that if a patient has multiple chronic diseases, which one in four Americans now do, one in two has one chronic disease, and they show up to the doctor’s office and they're on multiple medications, and they had been presenting with a whole set of new symptoms, there’s absolutely no way to provide high-quality care in a 10-minute visit. So we have to change our, not only the paradigm, but also the way that care is delivered. So that was my premise. So it follows then that my solution would address, I would hope at least those three points, right? Each of those three deficiencies. So the ADAPT framework combines an ancestral diet and lifestyle, which addresses that mismatch between our genes and biology in our modern diet and lifestyle. And then Functional Medicine is the new paradigm of medicine that is based on addressing the root cause of health problems, so we can prevent and reverse them instead of just suppressing symptoms. And then the third component is what I call a collaborative practice model, which links licensed providers like medical doctors, nurse practitioners, with what I call allied providers, which include folks like yourself, Tony, health coaches, nutritionists, personal trainers, etc., to provide a much, much higher level of care than what doctors are able to provide on their own. So, again, we're not trying to replace doctors in any, or even conventional medicine. We need people to do colonoscopies and remove cancerous tumors and use all of the incredible amount of training and expertise and skill that they’ve acquired over a lifetime of practice and study. We absolutely want that, but we need to add stuff to that that's not available now. Tony: What that really says to me is, emphasize the importance of community, of connection, of collaboration. We’re social creatures, we’re tribal by nature. That’s another kind of Paleo/ancestral health part of the puzzle. And it would be foolish to think that we can dissect out and silo out all these different aspects of our lives without consequence. I really like this idea of bringing everybody into the fold, and it’s not saying that you can go to just the naturopath, or you can go to just the health coach. Because like I mentioned already, I certainly would’ve been ill-equipped to handle plenty of issues that a client would’ve brought to mind or brought up in conversation during a training session. But it would’ve been really great to say, ah, here's the Functional Medicine practitioner that I recommend you speak with, and to have a good relationship with that person and to be able to, as a health coach, help my clients better by getting them in touch with the right person. And that’s having this network that can really support people throughout their health journey whether it’s just feeling better and more energy, or addressing something like diabetes or hypertension. Which certainly there’s a place for all the players in that kind of scenario.
What this new paradigm looks like
Chris: Absolutely. And let’s use an example just to bring this to life for people. So, imagine you go to the doctor and they do some blood testing for your annual physical. And they find that your fasting blood sugar is 96 or 97. Your hemoglobin A1c is 5.5, and you’ve got triglycerides that are 110, 120, maybe 130. Currently, what would happen is nothing, usually. Tony: You’re not sick enough yet. Chris: Yeah, all of your markers are within the lab range, they say, and that means you’re normal, and so you might get some vague advice about make sure to exercise and follow a good diet. And thank you very much, that’s it. Certainly there are exceptions to the rule, of course. There’s some practitioners who can get a lot more proactive about that. But I can’t tell you how many people, patients I’ve had that have been given that basic line with those kinds of lab results. What could happen is this. The doctor says, “Well, you know, if we think of blood sugar disorders on a spectrum, on the left you’ve got perfect blood sugar. On the right you’ve got full-fledged type 2 diabetes. You’re not on the right yet, you don’t have type 2 diabetes or even technically prediabetes, but you’re progressing along that spectrum. And what we know from a lot of research is that if we don’t intervene now, that you’re going to continue progressing. And in fact, we have studies that show that the average patient who has prediabetes, will progress to full-fledged type 2 diabetes in just five years if it’s not addressed.” So what we want to do is be proactive here. We want to intervene now because it’s much easier to prevent a disease before it occurs than it is to treat it after it’s already occurred. So here’s what we’re going to do. We’re going to set you up with our staff health coach, and they’re going to give you all the support you need to adopt a better diet. They’re actually even going to take you shopping, they’re going to come to your house and clean out your pantry with you, and they're going to give you recipes and meal plans and give you ... totally hold your hand and do everything that they need to to get you on this diet. Because we know that information is not enough. We’ve got lots of studies. I can tell you as a doctor, go eat a healthy diet, and hey, we know that that’s probably not going to happen. Most people know what they should be doing, but they’re not doing it, and it’s not because of lack of information. It’s because they need support, and we’re here to support you. We’ve got this health coach. Furthermore, we've got this great personal trainer named Tony. We’re going to set you up with him and we’re also going to set you up with a gym membership. And the good news is, your insurance is going to pay for all this. They’re going to pay for the health coach, they’re going to pay for the gym membership, they’re going to pay for your sessions with Tony. And in six months’ time, you’re going to come back here and we’re going to retest your blood markers and I can almost guarantee that if you stick with the program, you’re going to have normal blood sugar by that time. And throughout that period you’re going to have weekly check-ins with a health coach, you’re going to have training sessions. And not only will your blood sugar be normal, you’re going to lose weight, your energy levels are going to go up, your sleep’s going to get better, you’re going to feel more confident and empowered because you’re making these changes, and you’re going to feel like a different person. Now that’s totally possible.
How do we pay for this? Is it scalable?
Chris: I can hear some people saying, “Oh, how are we going to pay for that? That’s ridiculous.” Tony: Is it scalable? Chris: The question we should be asking is, is treating type 2 diabetes scalable? Because I mentioned this in the book, it costs $14,000 a year to treat a single patient with type 2 diabetes. So let’s imagine that this patient progresses. We don’t intervene, five years later they have type 2 diabetes. All of a sudden the healthcare system is spending $14,000 a year paying for that person’s care. And let’s say that that person gets diagnosed at age 40, which is still reasonable these days. The age of diagnosis is dropping more and more, and then let’s say that they live until they’re 85 years old, which is also possible because of our heroic medical interventions that keep people alive a lot longer than they might have been otherwise. So 45 years living with type 2 diabetes, that’s a cost of almost $650,000 for one patient to the healthcare system. Tony: And that doesn’t even touch on the lost wages, cost to employers, when someone’s on leave, loss of productivity. And then the cost to the family members. Chris: Absolutely. Tony: People that are actually, are helping the patient, their health is going to be going down too. Chris: Yeah. Nor does it touch on the qualitative aspects. Being immobilized, not being able to play with your grandkids, all of that stuff. But let’s just even forget about that for a second—$650,000, okay? And then the CDC recently came out with statistics saying that 100 million Americans have either prediabetes or diabetes, and 88 percent of people with prediabetes don’t even know that they have it. Which means they're almost certainly going to progress, right? If you do the math and you multiply 100 million people times even $14,000 for one year, you get a number that’s so large, I don’t even know what it is. It’s like a google something. It’s like, it has so many zeros after it, I don’t even know how to characterize it. But then if you multiply 100 million times like 20 or 30 years, it’s more money than there is in the world. It's like it's not going to happen. Tony: Not sustainable, not scalable. Chris: Not sustainable, not scalable. So let’s say in our example that we ... the healthcare system spends $10,000, which is way more than would be necessary, but let’s even say we buy the person’s groceries for three months. And their gym membership and their trainer, and their health coach, and those weekly, let’s say we spend $10,000. We’re just super generous and we spend $10,000 for that six-month period. Again, the research and my clinical experience indicates with near certainty that if the person is at that stage of not even prediabetic and we intervene, there’s like almost no chance that it’s not going to, we’re not going to be able to normalize that person’s blood sugar. And if they do that and they stick with it and they are able to do that because they now have support rather than just information, we’ve just saved the healthcare system $640,000 over the course of that patient’s lifetime. And that’s a conservative estimate, as you say. We're not including even the indirect costs. Tony: Right, right. Chris: I think that this is not only possible, it's going to become necessary. And whether we get there with a proactive approach where we decide to move in this direction and we make these changes or whether we get there because we absolutely have no choice, we’re going to get there. Tony: Yeah. I mean it really sounds like we can’t afford to not do this. Chris: Exactly. Tony: And if we get to that point where we continue down the reactive path and we wait until there’s a total collapse, it might be too late, just to put it frankly. And it’s going to come out at a huge, not just financial cost, a huge human cost. Chris: Yeah, it’s going to be, we can use the chronic disease metaphor again, it’s a lot easier to prevent a problem or reverse it at an earlier stage than it is to wait until the patient is essentially on life support or the healthcare system is on life support. It’s harder to reverse it at that time. And that’s of course why I’m writing the book now because I want to get this message out as far and wide as I can. Tony: Yeah. If not now, when? If not you, who? Go right back to there.
How allied providers are the key
Chris: Exactly. And one more thing about that is the amazing thing, the beauty of this is that it takes about eight years and hundreds of thousands of dollars to train a doctor. And it takes a certain kind of personality and a certain kind of comfort level with science, and a lot of prerequisites. It’s not for everybody. And there’s a ... already we have a shortage of doctors, and that’s predicted to get worse. I’ve seen estimates that suggest by 2025 we’ll have a shortage of 52,000 primary care physicians. So that’s a big deal. [insert image] So we already don’t have enough doctors, it’s already going to get worse, but if you think of healthcare as like a ... I have something in the book called the healthcare population pyramid. And you were referring to it earlier, Tony, where at the very top of that pyramid you’ve got 5 percent of people who are in really acute situations. So they’re in the hospital or they’re in an intensive outpatient care setting. They need the conventional medicine paradigm as it exists, and it’s fantastic for those situations. Then you’ve got another 25 percent of people in that kind of high middle of the pyramid who are dealing with some pretty serious chronic health challenges. So they require more regular care, but they’re not sick enough to be in the hospital or in any kind of ... they’re living their lives, but they’re struggling a lot. A Functional Medicine practitioner/clinician usually working in concert possibly with the conventional specialist of some kind is a really great option for that 25 percent of the pyramid. But then you’ve got the 70 percent at the bottom. So these are people who do, may have health issues, but they’re more minor, so they might have skin problems, or a little bit of brain fog, some difficulties sleeping, some GI issues. And these can be definitely debilitating and total pain, but they’re not at the level of that 25 percent. My argument is that in many cases these people could be very well served by a health coach or nutritionist with good training. And possibly seeing a Functional Medicine provider once or twice a year, or something like that. And the thing is, we can train people in a year or two without an extensive science background to be very, very objective in this role. Because they’re mostly working with patients on changing their behavior. If you think about it, most of the risk factors for chronic disease come down to the wrong behaviors. Eating the wrong diet, not getting enough sleep, not exercising, or exercising too much, or any number of things that come down to choices that we’re making. And so if a skilled health coach who’s trained in things like motivational interviewing and coaching to strengths and other evidence-based principles of facilitating behavior change which we have a ton of research on, they can be incredibly effective for that 70 percent of the population. That's the majority of the population. So we’re totally underutilizing these practitioners, and my argument is that they’re going to play a huge role in this future of medicine. And that's of course one reason why we're launching an ADAPT Health Coach Training Program next year to complement the practitioner training program that we've been doing. Because I want to create this ecosystem we've been talking about where you have all of these different types of practitioners working to the maximum of their training and ability and scope of practice and supporting each other and therefore providing the highest level of care to patients. Tony: That certainly kind of perks my ears up hearing about the ADAPT health coach option and something that I’m personally interested in. So who knows? Maybe I can get in on that. We can talk about it again in the future. Chris: Yeah, for sure. For sure. Tony: So, for this particular book, for Unconventional Medicine, people are fired up, they’re hearing about it, they’re like, “Okay, this resonates with me. I’m a practitioner, I’m an allied health provider, I’m a patient, I’m ready. Now’s the time. This is it. We’re going to do this.” What’s the best way for people to get their hands on this thing? Chris: Well not surprisingly, Amazon. They have the best way to get your hands on anything. So it’s available in paperback, Kindle, and audiobook. We’re hoping [the audiobook] is going to be out today, the day this podcast is released. But it might be another two or three days. They’re just taking their sweet time to approve it. I narrated the audiobook myself. So you podcast listeners, I figured you might be into that, since you like to listen. Tony: They know your voice. Chris: Yeah, and just listening to something instead of reading it perhaps. So to that end, we have a special offer for podcast listeners, because I appreciate your support and I know many of you are already part of this movement, and some are wanting to get involved. So if you buy that paperback or Kindle version between now and Sunday night, you’ll get some really cool bonuses. The first is a free copy of the audiobook. So again, we wanted to include that for podcast listeners, since we figured you guys and gals are probably interested in audio. But there are two other things that are really, I think, fantastic. And one, they’re both tools to help you be more confident and persuasive and factual when you share your passion for Functional Medicine and an ancestral diet and lifestyle. Because we’ve had a lot of questions from people, both practitioners and non-practitioners alike. They say, “Oh, how do I talk about this stuff to my sister at Thanksgiving?” Tony: “Isn’t that that caveman diet?” Chris: Yeah, exactly. All of our ancestors died when they were 30, so why should we even care? How do you respond to those arguments? Or if you start talking about Functional Medicine and maybe one of your conventional medicine colleagues says, “Oh, that’s just, I saw something on Science-based Medicine that said that was all just hooey. There’s nothing to it. How do you respond to that?” So what we wanted to do is give people the ammunition they needed in a respectful way. You know, this isn’t about getting the better of somebody. It’s about responding in a factual and convincing but respectful way. So we’ve got two different, we’re calling these the Power Packs. And one is for practitioners, so clinicians, health coaches, nutritionists, trainers, etc., and these are facts, research that you can reference and persuasive reasons for your clients or patients or colleagues to consider this Functional Medicine and ancestral diet and lifestyle approach. And then we have one for non-practitioners called the Supporter Power Pack. And these are smart answers and compelling comebacks, again respectful, for those common objections that you hear when you start talking about this stuff with your friends and family. So these bonuses are available until Sunday night [November 12, 2017] at 11:59 p.m. Pacific Time. So you’ve got a few days to act on that, and you can go to ... we set up a special link for you to get these and that’s Kresser.co/bonus. That’s Kresser.co/bonus. So head over there to get your Power Packs and your free audiobook, and that’s after you purchase either the paperback or Kindle. There’ll be a place where you enter your order number and we ask for some information just to verify, and I hope you enjoy those and get a lot out of them. Because they were actually really fun to put together. Tony: Yeah, I think the audiobook is huge. I like to listen to audiobooks when I’m driving around town or outside getting some exercise. Chris: Yeah. Tony: So, no excuses when you make it that easy. Chris: Yeah, yeah. So, Tony, thanks so much for doing this. This has been really fun to talk to you, as it always is. And I appreciate it. Tony: Actually, I wanted to throw in one extra little special thing, as we mentioned, at the top of the show. I spent 10 years as a personal trainer in the trenches, I was involved with Paleo Magazine for many, many years, going to all the events, and for me kind of an evolution in my professional life was, how do I impact more people? How do I help more people? And at first I was working one on one, and then it was as a facility manager helping other trainers and coaches get better. And then I was able to scale it up that way. And last year I had an opportunity to join the team over at Natural Force, which is all-natural, nutritional products, and I basically said, “You know what? I’m going to go all in on this because if I can touch a million people through really good, high-quality nutrition, that’s me maximizing my impact and really kind of living my purpose.” So one of the things I wanted to do today is put it out there for anyone listening who maybe uses collagen or MCT oil or whey protein. We really bend over backwards to source the best ingredients in the world, no additives, all that stuff. Everything is as clean as we can possibly make it. It takes a lot of work, working with manufacturers. Kind of like what you were saying, how patients have to know how to talk to their doctor. I don’t think people really realize, and I didn’t realize until I got on the inside, how much work it is for a brand to work with their manufacturers to convince them to get outside of the conventional mold. So it’s the kind of unconventional nutrition is really what we’re pushing here. So I set up a discount code for any Revolution Health listeners. Go to NaturalForce.com, use coupon code “unconventional” and get $10 off plus free shipping on your order. So I just want to put that out there as just a little extra bonus for anybody, and I would certainly love to help in that way and really get some good, high-quality nutrition into people’s hands. Chris: Awesome. Yeah, and there’s so many ways people can help, and I ... at Paleo f(x) we’ve see the growth of companies that are serving this space, and it's amazing. Like the products that are available now. I had breakfast this morning, I had some eggs and kale and parsley and a little bit of bacon in a couple of cassava flour tortillas. Breakfast burritos. Whoever thought I’d be having a breakfast burrito again? Tortillas are made from completely cassava flour. They’re autoimmune friendly and they’re grain-free tortillas. It’s incredible. Tony: I think I might have some of those in my fridge as well. Chris: Yeah. I mean there’s so many things. And these people, they’re serving this movement with that kind of work. So it’s great to see. Tony: It takes a village, man. Chris: It does. Thanks again, Tony. I really appreciate it. Thank you, everybody. So again, Kresser.co/bonus to pick up your free audiobook and the other bonuses, and I hope you can all join me in this revolution to reinvent healthcare. We need you, whatever your background and goals. Take care, everybody.
0 notes
Text
RHR: A Three-Step Plan to Fix Conventional Healthcare
In this episode we discuss:
The patient case that inspired the book
Who is this book for?
The mismatch between our medical paradigm and chronic disease
Drug companies and conflicts of interest
How clinicians can help create a new paradigm
The three core problems and how to solve them
What this new paradigm looks like
How do we pay for this? Is it scalable?
How allied providers are the key
Show notes:
Unconventional Medicine by Chris Kresser
Special offer for RHR podcast listeners - get the audiobook free if you buy the book by November 12th.
NaturalForce.com - use coupon “unconventional” and get $10 plus free shipping
[smart_track_player url="http://traffic.libsyn.com/thehealthyskeptic/RHR_-_A_Three-Step_Plan_to_Fix_Conventional_Healthcare.mp3" title="A Three-Step Plan to Fix Conventional Healthcare" artist="Chris Kresser" ]
youtube
Chris Kresser: Hey, everybody, Chris Kresser here. Welcome to another episode of Revolution Health Radio. Today we’re going to do something a little different. I am bringing on a guest host, Tony Federico, he’s the VP of marketing for Natural Force Nutrition, a physiology editor for the Journal of Evolution and Health, and a longtime contributor to Paleo Magazine, and also at Paleo f(x), which is where I met Tony, I think, originally, and I have interacted with him the most. And he’s moderated several panels that I’ve been on and I’ve always been impressed with the way he’s done that, the intelligent questions that he asks and just his balanced perspective on ancestral health and Functional Medicine, and this movement overall. Today is the day that my new book, Unconventional Medicine, comes out. It’s now available on Amazon, and I wanted to ask Tony to come take over the podcast and talk with me about the book because I know he’s really interested in all these topics and he’s read quite a bit of the book himself, and I thought it would be more interesting to have a conversation about it than for me to just sit here and do a monologue. So Tony welcome to the show and thanks for being here. Tony Federico: Yeah, thanks for inviting me on, Chris. It’s always fun, when we’ve had the chance to chat, as you said. Whether in person or on podcast, I’m always happy to jump in and dish on health with you. Chris: Fantastic. So, you have read a little bit of the book and we chatted a little bit about it via email, so let’s dive in. Let’s talk a little bit about this book. And for me it was really, it felt like the most important next step that I could take in order to get this message out about ending chronic disease. Tony: Yeah, I got my copy of Unconventional Medicine a couple days ago. I just so happened to have some time off yesterday, and the next thing I knew I was 80 pages in. Chris: Nice. Tony: So, I have to say that, as somebody who’s been in the trenches, I worked as a personal trainer for 10 years, I could really relate to a lot of the things that you were saying in the book, and we’ll get into why a little bit later on in the interview. But you know I just am really impressed with what you put together here, Chris. So let's just, let's get into it, and the first thing that I actually wanted you to maybe tell me a little bit about was how you open the book, which I think is a really great story about a patient named Leo. So I wanted to talk a little bit about Leo and his story and kind of how that inspired you to go down this particular path of unconventional medicine.
The patient case that inspired the book
Chris: Sure, yeah. So, Leo was an eight-year-old boy that I treated in my clinic a few years back, and I wanted to start with his story because it's, unfortunately, a typical story, much more common than, of course, we would like. And it was powerful for me, it was a powerful experience. It's what actually led to me writing this book. So, like way too many other kids of his age, he was suffering from a number of behavioral issues. He was initially diagnosed on the autism spectrum. Eventually they settled on OCD and sensory processing disorder. He would throw these just crazy tantrums where he'd end up crying or screaming inconsolably, writhing on the floor, and this would happen for seemingly the simplest of reasons. Like trying to get his shoes tied as they were going out the door, not cutting the crust off his sandwich in just the right way or getting a stain on his favorite T-shirt. And he was really rigid around his behavior and its environment, everything had to be just right, just the way he wanted it to be, or else he would fly off the handle.
Is a new healthcare paradigm affordable? Scalable? You bet.
His diet was extremely limited, he only ate a handful of foods, pretty much all of which were processed and refined. So crackers, bread, toaster waffles, that sort of thing, and this is part of the kind of OCD-like tendencies. And any time his parents would try to introduce new food, he would go totally ballistic. And they were worried about nutrient deficiency, but they didn't feel like they ... they were just worn down. Any parent who has a kid like this will understand that. It's just they didn’t feel like they had the resources to battle him at every meal. And they took him to a bunch of doctors locally, and that’s where they got those diagnoses. Initially they were kind of relieved to have those, but then after a while they realized that they were just simply labels for symptoms. And when they asked what the treatment was, you can probably guess the answer: medication. Tony: Something to do with drugs. Chris: Something to do with drugs. Yeah. And when they asked how long he would be on that treatment, you can probably also guess the answer. Tony: The rest of your life. Chris: Yeah. Shrug of the shoulders, indefinitely, maybe he'll grow out of it, that sort of thing. And they weren't excited about the idea of of medicating their son, but they were also aware of how much he was suffering, and they were suffering, frankly, too. They decided to give them a try, starting with Adderall, and then they progressed to Ritalin and then antidepressants. And certainly the drugs did seem to help with at least some of the symptoms, but there were a couple issues. Number one, they also caused some very intractable side effects like headache, abdominal pain, irritability, and most significantly, severe sleep disruption. And they had a couple of other kids that were younger than Leo. So they were not happy about the sleep disruption. Nobody was because it was brutal for them and also brutal for Leo. Kids need a lot of sleep, and if they’re waking up throughout the night, that’s going to make ... So that was in some ways worse than the original symptoms they were trying to treat. And then Leo's mom had done quite a bit of research on the effects of these medications and she was scared. Particularly for children and adolescents, some of these drugs have some pretty scary side effects and long-term risks. So what really stood out to me, and I mentioned this in the book, is that not once during this entire process of seeing all these different doctors, primary care provider, psychiatrist, eventually behavioral disorder specialists, did anybody even hint at the possibility that something in Leo's diet or some other underlying issue like a gut problem or nutrient deficiency or heavy metal toxicity or something like that could be contributing to his symptoms. It wasn't even broached as a possibility at any time. Fortunately, Leo's mom, one of her friends followed my work and sent her a couple of articles from my blog. One was on the gut–brain–axis, and I think the other one was on the underlying root causes of behavioral disorders. And so that's what led them to bring Leo to see me, and long story short, we were able to ... we did a bunch of testing, found issues that you might guess at. So, disrupted gut microbiome, SIBO, fungal overgrowth, gluten intolerance, but also intolerance of soy and corn and rice and buckwheat, which were major ingredients in a lot of the processed and refined food products that he ate, and arsenic toxicity because rice milk was the only other beverage he would drink aside from water. And we know that rice products can be high in arsenic. So, we, over several months, it definitely wasn't easy to address these problems because of his OCD-like tendencies and his picky eating habits. But after several months he was like a different kid. His teacher even called home and was like, “What have you done with Leo and who’s this kid that you’re sending in?” Because it was a big issue for her. They often had to come to school and pick him up early because of the behavioral problems. And his diet expanded; he was eating foods he would've thrown against the wall just months before, he was more tolerant of disorder, more relaxed in his environment. They were able to travel for the first time in a long time because he wasn't so anxious in unfamiliar environments. His physical symptoms had improved significantly. So they were just over the moon. They couldn't believe it, and toward the end of our treatment together, she said something that really struck me, which was there’s so many kids out there that are like Leo and they’re suffering, they’re not finding help in the conventional system. Tony: Sure. Chris: And their doctors and parents are not even thinking about this stuff. Like it’s not even in most people’s consciousness that if a kid has a behavioral disorder that you should look at these physiological issues. It’s not, for 99 percent of people they don't even go there because they don't know. Tony: Yeah, I mean I think that that was—reading about Leo and reading about a story and certainly there's people that I've known, myself included, who have had very similar experiences—I think it's great to have a narrative like this that you can really connect to because then when you tease it apart, all the pieces really make sense. It makes sense why having doctors treat symptoms has failed, it makes sense why a lack of communication between the health provider network that was supposed to be serving Leo failed. It makes sense why it didn't work when you actually start to tease it out. But then we’re still all, well not all, but most of us are still going down this path and it's an exercise in futility, really. You have an eight-year-old kid who's on powerful stimulant medications, he’s on antidepressants, and it was bad enough for his parents to reach out and to seek those interventions as solutions, and then the side effects are even worse. And that’s just something that just gets you right in the heart. And like you said, he’s not the only one, he’s not the only kid. His parents are not the only parents. And frankly, his doctors are not the only doctors because I can guarantee you that that probably doesn’t really feel good for the practitioner, for the healthcare provider to not get results as well. And they’re working with what they’ve got. Chris: Absolutely. Tony: And trying to use the tools they have. Chris: Yeah, I mean, let’s be clear about this. Everybody is doing the best they can in this situation. The parents are doing the best they can, in the vast majority of situations, parents just love their kids and do everything possible that they can to help their kids thrive. I’m a parent, I know that that’s how I relate to my kid. I know that every parent I know, that’s how they relate to their kids. And I would even, I would say that’s true for doctors too. The vast majority of them are trying to do the best they can with the tools that they have and in the system that they’re working within. And that’s the rub. Tony: Right. Chris: It’s like most doctors I’ve seen have been caring and they’ve wanted to do the right thing, but the question is, can they do the right thing in the conventional medical system as it exists today? And, of course, that’s largely what the book is about.
Who is this book for?
Tony: Yeah, so let’s kind of speak to that specifically. And we’re talking about doctors, we’re talking about medical professionals, we’re talking about patients, and then we didn’t mention it, but where I fit into this formula or potential formula as an allied healthcare provider, as a personal trainer/health coach, is that your audience for this book, do you really see that kind of triad is who you're speaking to here? Chris: Yeah, definitely. I think if you look at the cover of the book, the subtitle is “join the revolution to reverse chronic disease, reinvent healthcare, and create a practice you love.” So that last bit would suggest that it's mostly for practitioners, but that's not true. It is really for anybody that is interested in the ideas of reinventing healthcare and reversing chronic disease. And, in fact, I would argue that that change is going to be initiated by people, primarily by people that are not practitioners. So it's like a grassroots, bottom-up approach, where a good example is with my training program, my ADAPT training program, now that we've been training practitioners in this approach for the last couple years, we always ask people how they learned about my work or how they learned about the training program. And in a surprising number of cases, the answer is from their patients. So these doctors or other practitioners, their patient brings an article in that I wrote or brings something in, tells them about me, and to their credit they’re open-minded enough to go and check it out. And then they like what they see and they end up taking the next step. So people even who have no intention of ever becoming a healthcare practitioner, I think would really benefit from this book if they're interested in these ideas. And then certainly, as you mentioned, licensed healthcare providers like medical doctors or nurse practitioners or physician assistants that are currently working within the conventional paradigm but have already seen its limitations and want to do something different but don't yet know what that might look like. And then people who are outside of the conventional paradigm but are already practitioners, so acupuncturists, chiropractors, naturopathic physicians, etc., in many cases they’re already well aware of the limitations of conventional medicine, which is why they chose to go down a different path. But speaking personally as an acupuncturist myself, I also saw some limitations in the traditional Chinese medicine approach, or at least some differences in the way that I wanted to practice it. I was looking for something that could incorporate modern diagnostic testing and create a more systematic approach that included ancestral diet and lifestyle and some of the other things we talk about in the book. So, I think many of those practitioners can benefit from the book from that perspective. And then you have the growing and already large number of people like yourself who are personal trainers, health coaches, nutritionists, etc., who I really think are going to play an increasingly important role in this revolution to reinvent healthcare. Tony: Yeah, it so important now for people to really, for patients to be their own advocate, and I don't think we’re living in a time where I remember with my grandparents—if your doctor said something, it was basically gospel and you didn’t question it and you didn't think about it. Now, the first thing people do when they experience a symptom, it's Dr. Google first. So it's super important to equip and arm patients with good information, which I think this book does. Here's a path, here's a path forward for you as a patient. But then it's respectful of the role of doctors, and you highlight many situations where conventional medicine is great. If you break your arm or get in a car accident or have a heart attack or whatever the case may be, yeah, you need a doctor, and you need to go to an emergency room and you need those types of interventions. But it's really in this kind of gray area, it’s really not gray, it’s actually quite clear. And we could probably specify a little bit more, but there’s this middle zone where somebody’s not acutely injured, they’re not acutely in a disease state. They’re in a chronic disease state, or they’re just unwell. And it’s hard for a system that is all about pharmacological interventions, surgical interventions, to deal with a more subtle approach. And that’s where that whole middle ground and acupuncturists and massage therapists and everybody who's in that middle zone. I had clients constantly when I was actively training, constantly asking me questions where I was like, you know what? This is really something they maybe should be taking to their doctor. But guess what? The doctor only has 15 minutes under pressure to see as many patients as they can. I had a friend who was a physician in France. And he was telling me about their medical model, and he would spend tons of time with his patients. And it was actually incentivized for prevention. And here we see some maybe misplaced incentives, and perhaps you can speak a little bit more about that.
The mismatch between our medical paradigm and chronic disease
Chris: Yeah, so, going back to your original comments, I think that the most important thing for people to understand is that our medical model, when it comes to our medical paradigm, is that it evolved during a time when acute problems were the biggest issues. So in 1900, the top three causes of death were all infectious diseases, tuberculosis, typhoid, and pneumonia. And the other reasons people would see the doctor were among those you mentioned, like a broken bone or a gallbladder attack or appendicitis. Tony: War. Chris: Right, injuries, trauma, etc. And so the treatment for that's pretty straightforward. It wasn't always successful, of course, but it was straightforward. You know, if the bone was broken, you set it in a cast. If the gallbladder was swelling, you would take it out. If someone was having appendicitis, you’d remove the appendix. So that's pretty ... it's one problem, one doctor, one treatment. Pretty straightforward. But you fast-forward to today, it's a totally different healthcare landscape. Seven of the top 10 causes of death are chronic disease rather than acute problems now, and 86 percent of the healthcare dollars we spend go toward treating chronic disease. And unlike acute problems, chronic diseases are expensive, difficult to manage and usually last for a lifetime. They don't lend themselves to that one doctor, one problem, one treatment kind of approach. The average chronic disease patient requires multiple doctors, usually one for every different part of the body in our system, and is taking ... Tony: Specialists. Chris: Right, specialists, they’re taking multiple medications in many cases, and they're going to be taking those medications for the rest of their life. So far, it's really, our conventional medical system is amazing for these acute problems. But it's the wrong tool for the job for chronic problems. So that's one issue, and it’s really important to point that out, because we just went through the whole healthcare debate again with the Affordable Care Act and the current administration’s proposal for a replacement, which has not come to fruition. But throughout that entire discussion, it really bothered me that there was an elephant in the room. All the discussion was around insurance. Like, who gets insurance and who doesn’t. And that’s important, it’s important to talk about that. But we have to recognize that health insurance is not the same thing as healthcare. Tony: Yeah. Chris: Health insurance is a method of paying for healthcare. And that’s really crucial to get that difference. Because my argument in the book is that there is no method of paying for healthcare, whether it’s the government, corporations, or individuals, that will be adequate and will be sustainable under the pressure of growing prevalence of chronic disease. It will bankrupt all of us. Government, the corporations, individuals, whoever is responsible for paying for the care will not be able to do it unless we can actually prevent and reverse chronic disease instead of just slapping Band-Aids on it. Tony: I think the analogy you gave in the book was rearranging the deck chairs on the Titanic. “Making a few small tweaks to our current system and expecting that to work is like rearranging the deck furniture on the Titanic as it inexorably sinks into the ocean. Too little, too late.” Chris: Yeah, exactly. That’s the argument about insurance. As the whole ship goes under, sinks under. The other problems you mentioned are very real also. So we have a misalignment of incentives, like the insurance industry, for example, doesn't benefit when the cost of care shrinks because they only make more money when the overall expenditures rise. So it's actually not in their best interest necessarily to seek out the most cost-effective solutions.
Drug companies and conflicts of interest
Chris: And then of course, we have drug companies. People are pretty well aware of the conflicts of interest there. It’s in their interest to sell drugs, and even when that’s not in the interests of the general public or the patients or the doctors. In many cases, it’s not in their interest either. So the best example of this is a recent one. We’re in the midst of an opioid crisis, the worst we’ve ever seen by far, and the DEA has been wanting to create new regulations that restrict a pharmacy’s ability to sell opioids in ways that will protect people. So, for example, there was a pharmacy in West Virginia in a town that was tiny. It had like 30,000 people in this town, and they had ordered something like nine million opioid pills in the last year. It was clearly a front, like there’s clearly something shady going on there. There's no way that 30,000 people in that town needed nine million opioid pills, and yet there are no regulations to actually prevent that from happening. And so, the DEA had proposed some regulations to just safely protect people from that kind of thing. And the Big Pharma lobby basically shut that down and they played a big role in writing a law that limits the DEA's ability to do that kind of regulation in the midst of the worse opioid crisis ever. And to put this in perspective, we hear a lot about the gun lobbies and their control. They spend about $10.5 million lobbying Congress, I think, per year. And Big Pharma, they spent $250 million. Tony: Wow. Chris: Twenty-five-fold higher. Tony: It's really tragic. I actually, I don’t think we’ve ever talked about this, but I grew up in South Florida, which was kind of ground zero for the opioid epidemic. And I remember in high school down in Miami and West Palm Beach, and kids would get a hold of a contact or whatever, somebody that had a prescription and basically would end up being a de facto drug dealer vis-à-vis a pill mill, etc. The kid across the street from me died, multiple kids in my high school died, multiple kids went into in-treatment programs, some of them battled addictions for decades. Some of them got out of it. Very few got out of it. Some of them didn't and have continued to be plagued with either switching from pharmaceuticals to street drugs like heroin, etc., and then we can see what's happening there. And that's just one example. If we look at drug consumption in the United States, is it that Americans are just that much sicker and we’re in that much more pain than people in other countries? Because we’re consuming far and away more painkillers than any other country on the planet. And I would venture to guess that you could say the same about antidepressants or ADD medication. It's very much a case of misaligned incentives. And incentives are working in the sense of the pharmaceutical companies are doing very well. Chris: Yeah. Who are they working for is the question. Tony: Exactly. Chris: We’re the only country aside from New Zealand that allows direct-to-consumer drug advertising, and I think that's a big part of the problem. But it's not just Big Pharma. We also have conflicts in medical research that, of course, are related to Big Pharma because they pay for two-thirds of all medical research. We have broken payment models, where there's no real incentive or reward for good performance, and in fact, you could argue it's the other way around because doctors are compensated for, usually based on the number of procedures they order and the number of patients they see. So to your point about the doctor in France who is actually incentivized to prevent, rather than just treat disease, we don't have that at all, it's the opposite. And so there are a lot of deeply entrenched issues that we certainly need to address, and that's not essentially what this book is about. There are other books that cover that material really well, and frankly many of those issues are outside of our individual control as clinicians or practitioners.
How clinicians can help create a new paradigm
Chris: We can work toward addressing them, and I think we should, but the good news is that I think that the bigger changes that we need to focus on individually and collectively are addressing the medical paradigm which we’ve talked about, creating a medical paradigm that’s better suited to tackle chronic disease. Addressing the mismatch between our modern diet and lifestyle, and our genes and our biology, which we've, of course, talked a lot about on the show before. And then creating a new way of delivering healthcare that actually supports this new medical paradigm and this more preventative approach. Because those things are all within our control as clinicians. Tony: Yeah. I like how you posed the question, and it was kind of a cool little, I think it was, not Hiroshi, but the person who is in charge of cooking at a Buddhist monastery. And basically a young monk comes up to this older man. He’s like, why are you doing the grunt work, basically washing rice out in the courtyard? And he says, it was like, what was it? “If not me, who? And if not now, when?” And I think that that’s really kind of the core of setting all this stuff up. Talking about the problem is really in the service of pivoting to the solution, and I’m a big believer in thinking globally, thinking big, but acting locally, hyper-locally, like yourself. Chris: Yeah. Tony: And then the people around you and who you can touch and impact. That’s ultimately where the power comes from. So let’s talk about that. What is in people’s power. And you started to describe some of those pillars of a new model. And you describe it as the ADAPT framework. And I don’t know how much you get into this on your regular podcast episodes, but to just kind of lay it out, ADAPT from a big-picture perspective. How does that actually address some of these systemic issues from an individually empowered stance? Chris: Yeah, great question, and before I even go into that, I just want to say I agree that I think the change is going to happen on different levels. So, because a lot ... we’ve talked about this stuff at conferences or even some people who’ve already read the book. They say, oh, this is fantastic. I’m so excited. But how are we going to deal with Big Pharma and the insurance industry and these misaligned incentives and all of that? And can we ever deal with that? The answer is we’re not going to deal with that overnight and it’s going to take a while to unwind those things. Tony: It’s the chronic disease, is what you call... Chris: Exactly, exactly. And I use that analogy in the book. But the good news is that changes can happen very quickly on an individual and local level. And there’s already a lot of evidence of that happening. So my own clinic, CCFM, tripled in size in the last three years alone. We have Cleveland Clinic Center for Functional Medicine, launched by Dr. Mark Hyman, has just blown up like crazy. I mean they started in this tiny space. Now their 17,000-square-foot space, it takes up the whole second floor of the Glickman Tower at Cleveland Clinic. They've got a waitlist of 2,500 patients from nine countries around the world. This is really exciting! The Cleveland Clinic is always on the forefront of the newest trends in medicine, and the fact that they've invested that much money in this speaks volumes. Then we have groups like Iora Health, an organization based in the Rocky Mountain area that’s reversing diabetes using health coaches. So there are lots of really interesting produced concepts, and there's going to be more and more of these. Like we’re doing a pilot program with the Berkeley Fire Department where we’re working with their new recruits to help, we’re implementing a wellness program. Tony: That’s awesome. Chris: To reduce injuries and help with recovery and optimize their performance. And if that goes well, there’s been interest from the wider fire department and in the city of Berkeley as a whole. Robb Wolf’s done some incredible work with Reno that we’ve talked about before. So I think the change is going to happen more quickly on this local grassroots level, and then that's going to start to get the attention of people on a state and federal level. And then it will start to get really interesting.
The three core problems and how to solve them
To answer your question, in my book I basically lay out three core fundamental problems with the healthcare system in the US. And these, I argue, go even deeper than the misaligned incentives and Big Pharma and all of that stuff, although they’re, of course, connected. The first is that there is a profound mismatch between our genes and our biology and our modern diet and lifestyle. And I'm not going to say more about that now because almost everyone listening to this podcast knows exactly what I mean. The second problem is the mismatch between our medical paradigm and chronic disease, which we just talked about. We need a new medical paradigm that is better suited for chronic disease. And then the third is that the way we deliver care in this country is also, it's not set up to support the most important interventions. And we’ve touched on that too, where the average visit with the primary care provider is just actually eight to 12 minutes. Tony, you were talking about 15 minutes. That’s luxurious in our current model. The average amount of time a patient gets to speak before they’re interrupted by the doctor is 12 seconds. Tony: Wow. Chris: So I think it’s pretty clear that if a patient has multiple chronic diseases, which one in four Americans now do, one in two has one chronic disease, and they show up to the doctor’s office and they're on multiple medications, and they had been presenting with a whole set of new symptoms, there’s absolutely no way to provide high-quality care in a 10-minute visit. So we have to change our, not only the paradigm, but also the way that care is delivered. So that was my premise. So it follows then that my solution would address, I would hope at least those three points, right? Each of those three deficiencies. So the ADAPT framework combines an ancestral diet and lifestyle, which addresses that mismatch between our genes and biology in our modern diet and lifestyle. And then Functional Medicine is the new paradigm of medicine that is based on addressing the root cause of health problems, so we can prevent and reverse them instead of just suppressing symptoms. And then the third component is what I call a collaborative practice model, which links licensed providers like medical doctors, nurse practitioners, with what I call allied providers, which include folks like yourself, Tony, health coaches, nutritionists, personal trainers, etc., to provide a much, much higher level of care than what doctors are able to provide on their own. So, again, we're not trying to replace doctors in any, or even conventional medicine. We need people to do colonoscopies and remove cancerous tumors and use all of the incredible amount of training and expertise and skill that they’ve acquired over a lifetime of practice and study. We absolutely want that, but we need to add stuff to that that's not available now. Tony: What that really says to me is, emphasize the importance of community, of connection, of collaboration. We’re social creatures, we’re tribal by nature. That’s another kind of Paleo/ancestral health part of the puzzle. And it would be foolish to think that we can dissect out and silo out all these different aspects of our lives without consequence. I really like this idea of bringing everybody into the fold, and it’s not saying that you can go to just the naturopath, or you can go to just the health coach. Because like I mentioned already, I certainly would’ve been ill-equipped to handle plenty of issues that a client would’ve brought to mind or brought up in conversation during a training session. But it would’ve been really great to say, ah, here's the Functional Medicine practitioner that I recommend you speak with, and to have a good relationship with that person and to be able to, as a health coach, help my clients better by getting them in touch with the right person. And that’s having this network that can really support people throughout their health journey whether it’s just feeling better and more energy, or addressing something like diabetes or hypertension. Which certainly there’s a place for all the players in that kind of scenario.
What this new paradigm looks like
Chris: Absolutely. And let’s use an example just to bring this to life for people. So, imagine you go to the doctor and they do some blood testing for your annual physical. And they find that your fasting blood sugar is 96 or 97. Your hemoglobin A1c is 5.5, and you’ve got triglycerides that are 110, 120, maybe 130. Currently, what would happen is nothing, usually. Tony: You’re not sick enough yet. Chris: Yeah, all of your markers are within the lab range, they say, and that means you’re normal, and so you might get some vague advice about make sure to exercise and follow a good diet. And thank you very much, that’s it. Certainly there are exceptions to the rule, of course. There’s some practitioners who can get a lot more proactive about that. But I can’t tell you how many people, patients I’ve had that have been given that basic line with those kinds of lab results. What could happen is this. The doctor says, “Well, you know, if we think of blood sugar disorders on a spectrum, on the left you’ve got perfect blood sugar. On the right you’ve got full-fledged type 2 diabetes. You’re not on the right yet, you don’t have type 2 diabetes or even technically prediabetes, but you’re progressing along that spectrum. And what we know from a lot of research is that if we don’t intervene now, that you’re going to continue progressing. And in fact, we have studies that show that the average patient who has prediabetes, will progress to full-fledged type 2 diabetes in just five years if it’s not addressed.” So what we want to do is be proactive here. We want to intervene now because it’s much easier to prevent a disease before it occurs than it is to treat it after it’s already occurred. So here’s what we’re going to do. We’re going to set you up with our staff health coach, and they’re going to give you all the support you need to adopt a better diet. They’re actually even going to take you shopping, they’re going to come to your house and clean out your pantry with you, and they're going to give you recipes and meal plans and give you ... totally hold your hand and do everything that they need to to get you on this diet. Because we know that information is not enough. We’ve got lots of studies. I can tell you as a doctor, go eat a healthy diet, and hey, we know that that’s probably not going to happen. Most people know what they should be doing, but they’re not doing it, and it’s not because of lack of information. It’s because they need support, and we’re here to support you. We’ve got this health coach. Furthermore, we've got this great personal trainer named Tony. We’re going to set you up with him and we’re also going to set you up with a gym membership. And the good news is, your insurance is going to pay for all this. They’re going to pay for the health coach, they’re going to pay for the gym membership, they’re going to pay for your sessions with Tony. And in six months’ time, you’re going to come back here and we’re going to retest your blood markers and I can almost guarantee that if you stick with the program, you’re going to have normal blood sugar by that time. And throughout that period you’re going to have weekly check-ins with a health coach, you’re going to have training sessions. And not only will your blood sugar be normal, you’re going to lose weight, your energy levels are going to go up, your sleep’s going to get better, you’re going to feel more confident and empowered because you’re making these changes, and you’re going to feel like a different person. Now that’s totally possible.
How do we pay for this? Is it scalable?
Chris: I can hear some people saying, “Oh, how are we going to pay for that? That’s ridiculous.” Tony: Is it scalable? Chris: The question we should be asking is, is treating type 2 diabetes scalable? Because I mentioned this in the book, it costs $14,000 a year to treat a single patient with type 2 diabetes. So let’s imagine that this patient progresses. We don’t intervene, five years later they have type 2 diabetes. All of a sudden the healthcare system is spending $14,000 a year paying for that person’s care. And let’s say that that person gets diagnosed at age 40, which is still reasonable these days. The age of diagnosis is dropping more and more, and then let’s say that they live until they’re 85 years old, which is also possible because of our heroic medical interventions that keep people alive a lot longer than they might have been otherwise. So 45 years living with type 2 diabetes, that’s a cost of almost $650,000 for one patient to the healthcare system. Tony: And that doesn’t even touch on the lost wages, cost to employers, when someone’s on leave, loss of productivity. And then the cost to the family members. Chris: Absolutely. Tony: People that are actually, are helping the patient, their health is going to be going down too. Chris: Yeah. Nor does it touch on the qualitative aspects. Being immobilized, not being able to play with your grandkids, all of that stuff. But let’s just even forget about that for a second—$650,000, okay? And then the CDC recently came out with statistics saying that 100 million Americans have either prediabetes or diabetes, and 88 percent of people with prediabetes don’t even know that they have it. Which means they're almost certainly going to progress, right? If you do the math and you multiply 100 million people times even $14,000 for one year, you get a number that’s so large, I don’t even know what it is. It’s like a google something. It’s like, it has so many zeros after it, I don’t even know how to characterize it. But then if you multiply 100 million times like 20 or 30 years, it’s more money than there is in the world. It's like it's not going to happen. Tony: Not sustainable, not scalable. Chris: Not sustainable, not scalable. So let’s say in our example that we ... the healthcare system spends $10,000, which is way more than would be necessary, but let’s even say we buy the person’s groceries for three months. And their gym membership and their trainer, and their health coach, and those weekly, let’s say we spend $10,000. We’re just super generous and we spend $10,000 for that six-month period. Again, the research and my clinical experience indicates with near certainty that if the person is at that stage of not even prediabetic and we intervene, there’s like almost no chance that it’s not going to, we’re not going to be able to normalize that person’s blood sugar. And if they do that and they stick with it and they are able to do that because they now have support rather than just information, we’ve just saved the healthcare system $640,000 over the course of that patient’s lifetime. And that’s a conservative estimate, as you say. We're not including even the indirect costs. Tony: Right, right. Chris: I think that this is not only possible, it's going to become necessary. And whether we get there with a proactive approach where we decide to move in this direction and we make these changes or whether we get there because we absolutely have no choice, we’re going to get there. Tony: Yeah. I mean it really sounds like we can’t afford to not do this. Chris: Exactly. Tony: And if we get to that point where we continue down the reactive path and we wait until there’s a total collapse, it might be too late, just to put it frankly. And it’s going to come out at a huge, not just financial cost, a huge human cost. Chris: Yeah, it’s going to be, we can use the chronic disease metaphor again, it’s a lot easier to prevent a problem or reverse it at an earlier stage than it is to wait until the patient is essentially on life support or the healthcare system is on life support. It’s harder to reverse it at that time. And that’s of course why I’m writing the book now because I want to get this message out as far and wide as I can. Tony: Yeah. If not now, when? If not you, who? Go right back to there.
How allied providers are the key
Chris: Exactly. And one more thing about that is the amazing thing, the beauty of this is that it takes about eight years and hundreds of thousands of dollars to train a doctor. And it takes a certain kind of personality and a certain kind of comfort level with science, and a lot of prerequisites. It’s not for everybody. And there’s a ... already we have a shortage of doctors, and that’s predicted to get worse. I’ve seen estimates that suggest by 2025 we’ll have a shortage of 52,000 primary care physicians. So that’s a big deal. [insert image] So we already don’t have enough doctors, it’s already going to get worse, but if you think of healthcare as like a ... I have something in the book called the healthcare population pyramid. And you were referring to it earlier, Tony, where at the very top of that pyramid you’ve got 5 percent of people who are in really acute situations. So they’re in the hospital or they’re in an intensive outpatient care setting. They need the conventional medicine paradigm as it exists, and it’s fantastic for those situations. Then you’ve got another 25 percent of people in that kind of high middle of the pyramid who are dealing with some pretty serious chronic health challenges. So they require more regular care, but they’re not sick enough to be in the hospital or in any kind of ... they’re living their lives, but they’re struggling a lot. A Functional Medicine practitioner/clinician usually working in concert possibly with the conventional specialist of some kind is a really great option for that 25 percent of the pyramid. But then you’ve got the 70 percent at the bottom. So these are people who do, may have health issues, but they’re more minor, so they might have skin problems, or a little bit of brain fog, some difficulties sleeping, some GI issues. And these can be definitely debilitating and total pain, but they’re not at the level of that 25 percent. My argument is that in many cases these people could be very well served by a health coach or nutritionist with good training. And possibly seeing a Functional Medicine provider once or twice a year, or something like that. And the thing is, we can train people in a year or two without an extensive science background to be very, very objective in this role. Because they’re mostly working with patients on changing their behavior. If you think about it, most of the risk factors for chronic disease come down to the wrong behaviors. Eating the wrong diet, not getting enough sleep, not exercising, or exercising too much, or any number of things that come down to choices that we’re making. And so if a skilled health coach who’s trained in things like motivational interviewing and coaching to strengths and other evidence-based principles of facilitating behavior change which we have a ton of research on, they can be incredibly effective for that 70 percent of the population. That's the majority of the population. So we’re totally underutilizing these practitioners, and my argument is that they’re going to play a huge role in this future of medicine. And that's of course one reason why we're launching an ADAPT Health Coach Training Program next year to complement the practitioner training program that we've been doing. Because I want to create this ecosystem we've been talking about where you have all of these different types of practitioners working to the maximum of their training and ability and scope of practice and supporting each other and therefore providing the highest level of care to patients. Tony: That certainly kind of perks my ears up hearing about the ADAPT health coach option and something that I’m personally interested in. So who knows? Maybe I can get in on that. We can talk about it again in the future. Chris: Yeah, for sure. For sure. Tony: So, for this particular book, for Unconventional Medicine, people are fired up, they’re hearing about it, they’re like, “Okay, this resonates with me. I’m a practitioner, I’m an allied health provider, I’m a patient, I’m ready. Now’s the time. This is it. We’re going to do this.” What’s the best way for people to get their hands on this thing? Chris: Well not surprisingly, Amazon. They have the best way to get your hands on anything. So it’s available in paperback, Kindle, and audiobook. We’re hoping [the audiobook] is going to be out today, the day this podcast is released. But it might be another two or three days. They’re just taking their sweet time to approve it. I narrated the audiobook myself. So you podcast listeners, I figured you might be into that, since you like to listen. Tony: They know your voice. Chris: Yeah, and just listening to something instead of reading it perhaps. So to that end, we have a special offer for podcast listeners, because I appreciate your support and I know many of you are already part of this movement, and some are wanting to get involved. So if you buy that paperback or Kindle version between now and Sunday night, you’ll get some really cool bonuses. The first is a free copy of the audiobook. So again, we wanted to include that for podcast listeners, since we figured you guys and gals are probably interested in audio. But there are two other things that are really, I think, fantastic. And one, they’re both tools to help you be more confident and persuasive and factual when you share your passion for Functional Medicine and an ancestral diet and lifestyle. Because we’ve had a lot of questions from people, both practitioners and non-practitioners alike. They say, “Oh, how do I talk about this stuff to my sister at Thanksgiving?” Tony: “Isn’t that that caveman diet?” Chris: Yeah, exactly. All of our ancestors died when they were 30, so why should we even care? How do you respond to those arguments? Or if you start talking about Functional Medicine and maybe one of your conventional medicine colleagues says, “Oh, that’s just, I saw something on Science-based Medicine that said that was all just hooey. There’s nothing to it. How do you respond to that?” So what we wanted to do is give people the ammunition they needed in a respectful way. You know, this isn’t about getting the better of somebody. It’s about responding in a factual and convincing but respectful way. So we’ve got two different, we’re calling these the Power Packs. And one is for practitioners, so clinicians, health coaches, nutritionists, trainers, etc., and these are facts, research that you can reference and persuasive reasons for your clients or patients or colleagues to consider this Functional Medicine and ancestral diet and lifestyle approach. And then we have one for non-practitioners called the Supporter Power Pack. And these are smart answers and compelling comebacks, again respectful, for those common objections that you hear when you start talking about this stuff with your friends and family. So these bonuses are available until Sunday night [November 12, 2017] at 11:59 p.m. Pacific Time. So you’ve got a few days to act on that, and you can go to ... we set up a special link for you to get these and that’s Kresser.co/bonus. That’s Kresser.co/bonus. So head over there to get your Power Packs and your free audiobook, and that’s after you purchase either the paperback or Kindle. There’ll be a place where you enter your order number and we ask for some information just to verify, and I hope you enjoy those and get a lot out of them. Because they were actually really fun to put together. Tony: Yeah, I think the audiobook is huge. I like to listen to audiobooks when I’m driving around town or outside getting some exercise. Chris: Yeah. Tony: So, no excuses when you make it that easy. Chris: Yeah, yeah. So, Tony, thanks so much for doing this. This has been really fun to talk to you, as it always is. And I appreciate it. Tony: Actually, I wanted to throw in one extra little special thing, as we mentioned, at the top of the show. I spent 10 years as a personal trainer in the trenches, I was involved with Paleo Magazine for many, many years, going to all the events, and for me kind of an evolution in my professional life was, how do I impact more people? How do I help more people? And at first I was working one on one, and then it was as a facility manager helping other trainers and coaches get better. And then I was able to scale it up that way. And last year I had an opportunity to join the team over at Natural Force, which is all-natural, nutritional products, and I basically said, “You know what? I’m going to go all in on this because if I can touch a million people through really good, high-quality nutrition, that’s me maximizing my impact and really kind of living my purpose.” So one of the things I wanted to do today is put it out there for anyone listening who maybe uses collagen or MCT oil or whey protein. We really bend over backwards to source the best ingredients in the world, no additives, all that stuff. Everything is as clean as we can possibly make it. It takes a lot of work, working with manufacturers. Kind of like what you were saying, how patients have to know how to talk to their doctor. I don’t think people really realize, and I didn’t realize until I got on the inside, how much work it is for a brand to work with their manufacturers to convince them to get outside of the conventional mold. So it’s the kind of unconventional nutrition is really what we’re pushing here. So I set up a discount code for any Revolution Health listeners. Go to NaturalForce.com, use coupon code “unconventional” and get $10 off plus free shipping on your order. So I just want to put that out there as just a little extra bonus for anybody, and I would certainly love to help in that way and really get some good, high-quality nutrition into people’s hands. Chris: Awesome. Yeah, and there’s so many ways people can help, and I ... at Paleo f(x) we’ve see the growth of companies that are serving this space, and it's amazing. Like the products that are available now. I had breakfast this morning, I had some eggs and kale and parsley and a little bit of bacon in a couple of cassava flour tortillas. Breakfast burritos. Whoever thought I’d be having a breakfast burrito again? Tortillas are made from completely cassava flour. They’re autoimmune friendly and they’re grain-free tortillas. It’s incredible. Tony: I think I might have some of those in my fridge as well. Chris: Yeah. I mean there’s so many things. And these people, they’re serving this movement with that kind of work. So it’s great to see. Tony: It takes a village, man. Chris: It does. Thanks again, Tony. I really appreciate it. Thank you, everybody. So again, Kresser.co/bonus to pick up your free audiobook and the other bonuses, and I hope you can all join me in this revolution to reinvent healthcare. We need you, whatever your background and goals. Take care, everybody. RHR: A Three-Step Plan to Fix Conventional Healthcare published first on https://chriskresser.com
0 notes