autistic/disabled/mental illness blog for organizing and gathering information, mostly on autism, avpd, adhd, and depression. this is a side blog so I can't follow back with this blog.
Don't wanna be here? Send us removal request.
Note
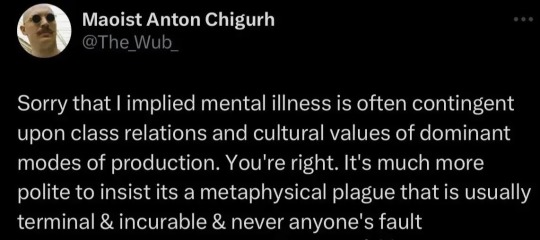
Can u tell us the differences between someone who has AVPD and SZPD?
Here is a copy-paste from Treatment of Schizoid Personality by Zachary Wheeler.
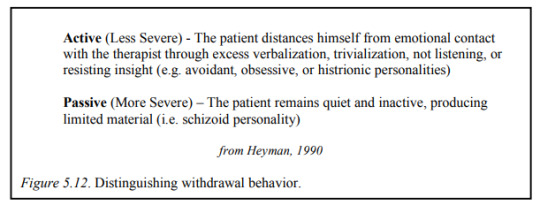
Avoidant pathology reflects active detachment from a desired closeness with others, while Schizoid pathology usually reflected a passive detachment indicative of limited interest in relationships
Patients that most frequently qualify for an Avoidant diagnosis are often in touch with their neediness for others, but often run from opportunities for intimacy because they fear rejection, feelings of inadequacy, abandonment and failure in these situations
Accordingly Avoidant individuals often experience high levels of depression and anxiety in their lives, and a good deal of shame, embarrassment, and feelings of inferiority in relationship to other. Only to a limited degree in Schizoid and Schizotypal presentations where neediness for others is deeply denied or split off, and fears of rejection and embarrassment do not often materialize because relationships are avoided and the emotional implications of interpersonal associations are dismissed. Anxiety and depression do occur, but usually only arise when connection to others is in some way unavoidable.
The Avoidant personality differs mainly in that these individuals are capable of warming up to others once an accepting relationship has been established, whereas the Schizoid and Schizotypal presentations tend to experience strong anxiety within relationships that does not easily abate
In general, Avoidant presentations are those Schizoid patients that tend to be seen as outwardly suffering. In particular, these patients often report loneliness and longing for relationships that are not usually present in pure Schizoid types.
But Avoidant PD and Schizoid PD are more similar than not:
The difficulty of using the DSM to adequately assess the Schizoid personality is covered extensively elsewhere (Akhtar 1992; Gabbard 1994), as is the large diagnostic overlap between Avoidant and Schizotypal disorders with Schizoid personality (Livesley, West, & Tanney, 1986; Shedler & Westen, 2004).
Avoidant is also sometimes referred to as High Schizoid.
Schizoid without (or with minimal) Avoidant traits is sometimes referred to as Pure Schizoid.
My Opinion:
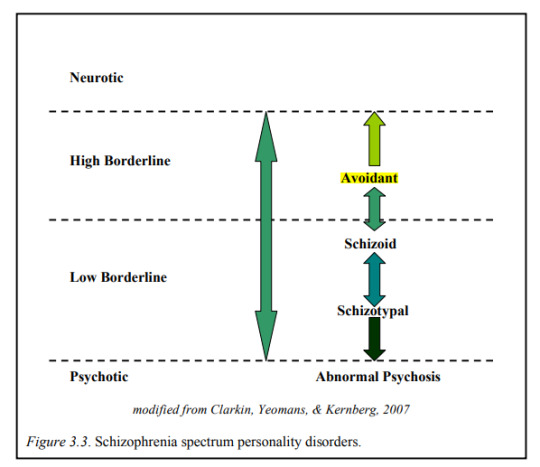
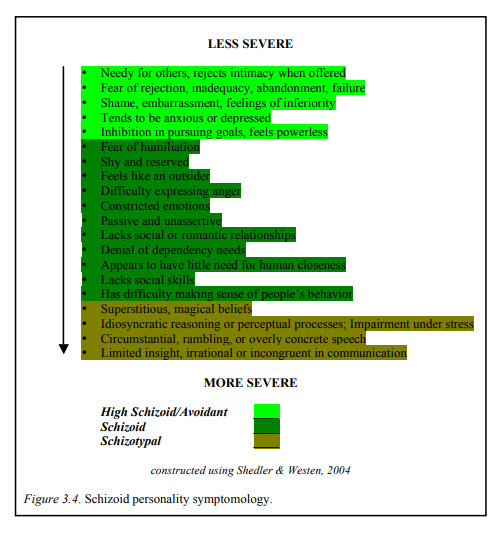
I view them as being on the same spectrum rather than completely separate disorders, as seen on figure 3.4. I think most people on the schizoid, avoidant, schizotypal spectrums have a mixture of these symptoms and don't usually fit into only one box. Avoidant and schizoid traits often overlap, and a large amount of schizotypals also have avoidant and schizoid traits.
144 notes
·
View notes
Text
my frustration with “going nonverbal/nonspeaking” (as a fully nonverbal person)
transcript: my frustration with “going nonverbal/nonspeaking” (as a fully nonverbal person)
this written for instagram because of this post. but thought tumblr may like it too. “you” means general you, no one specific.
the instagram post and this on wordpress
this disclaimer is for instagram but also for anyone new to this discussion:
in full honestly, don’t know how to write this. am tired, language and complex ideas too much at time of writing, and general exhaust at having to argue same thing over and over again and justify own existence. tired of being minority within minority, wish there are others to do these work for me so i don’t have to do it all by self, singlehandedly advocate for everyone (not to mention problem with that—i can’t speak for everyone).
so honestly, if you don’t have anything nice to say, especially if you speaking (yes, even if you lose speech. include you), just don't say anything at all. move on.
online actually autistic community (AAut) dominated by white, lower support needs. level 1, speaking, late diagnosed, high masking autistics. find people like you is great, what not great is you treat your very narrow community as “voice of all autistic” and your experience as ultimate autistic experience. i write plenty about that, many more elaborate than this, if you not familiar with this concept.
many people in this community experience times when cannot speak, sometimes because overwhelm, shutdown, dissociate, or anxiety (situational mutism), but do not struggle with act of speaking rest of time (some struggle with speech all the time but still can speak - more on that later). the community call “going nonverbal/nonspeaking,” or even “when i am nonverbal nonspeaking” (not talking about those nonverbal as child and verbal now older), after clinical term “nonverbal” (nonverbal autism) and term coined by apraxic nonspeaking autistics “nonspeaking.”
both of which talk about it as an “all the time” experience.
when i search nonverbal or nonspeaking because i want community too, want see people like me too, two category i see: 1) parents of nonverbal nonspeaking children, whom can’t relate to because age, who can’t write own experience because their age and developmental ability. and 2) overwhelming amount of speaking autistic talk about going nonverbal going nonspeaking.
and the very very few fully nonverbal nonspeaking voices. drowned out. cannot find anyone.
nonverbal used to be term to describe us, people who can’t speak or cannot functionally speak beyond few words. medical term, alright, so some of us don’t like. so some of us reject that and create term all of our own, called nonspeaking. created by nonspeaking autistics with severe apraxia and brain body disconnect, describe their own experience of able to think in words able to spell out words (with great dedication and work and support), just cannot do that with mouth. their term. they create.
and you take it? without knowing context? without reading anything by those same nonspeaking coiners?
when is last time you purposely seek out nonverbal nonspeaking voices? when is last time you accidentally came across us? can you name any nonverbal nonspeaking advocate that talk about their experiences? one? two? three? a BIPOC person, a (specifically) Black person? a Black woman? a trans person? a physically disabled person? a person not from western world?
same narrative over and over. “i can speak for nonverbal autistic i understand their experience because i am autistic i can’t talk sometimes” no you cannot. as someone who was able to speak when young who lose speech (”go nonverbal”) but now have no speech to lose because full time nonverbal. no the experience not the same. not comparable. you gain it back. i don’t. you can explain with mouth words what happen when you get out. i can’t, i only have AAC. countless nonverbal nonspeaking people without AAC or sign cannot, at all. you never experience daily small and big struggle of casually being nonverbal all the time.
your experience of lose speech unique from my nonverbal. but if you so insist to compare and equate, you only guest to my experience, my daily life.
“when i go nonverbal and no one understand so have to force to speak” i cannot force words out. know you don’t mean to say this, and not saying you at fault for this, but nevertheless accidental perpetuate and reinforce idea that anyone who don’t speak can just be forced to speak if try hard enough. but often not how it works. and this exact harmful rhetoric devoid and delays nonverbal nonspeaking people given access to AAC, because “need try to force words out first, AAC unnatural so last resort.”
this may be new concept for you. new concept to instagram, to tiktok. to other places. it may seem i only one with this problem, “i once saw a nonspeaking person’s account and they don’t have problem.”
yeah, because we are not monolith. some nonverbal nonspeaking people don’t care. some nonverbal nonspeaking people may even welcome “go nonverbal nonspeaking” or “when i am nonverbal nonspeaking.”
but don’t be fooled into believe i only one. have many nonverbal/nonspeaking and/or higher support needs friends on tumblr, who talk about this who have been saying this for years. *years*. years before i joined. i am not creator, i only bring message here, because many of us are too high support needs too disabled to do anything else. many of us only stay on our small corner of tumblr because it most peaceful, because at least some listen, because least hostile, because need to defend our experience against our own community the least. (but it happens less doesn’t mean it doesn’t happen, we still exhausted.) many of us only stay on our small corner of tumblr because that all we can handle, or because we not allowed or shouldn’t be on other social media because age or abilities or both.
i cannot handle conflict i do not do well and i shouldn’t be here. but if not me, who else? if i don’t do it, who else is going to?
some nonverbal nonspeaking people and parents of them may question, why you start debate about useless term when so many nonverbal nonspeaking people don’t even have access to communicate, real problems. to that i say i do those work too. and to that i say this is real problem too, because am autistic so online actually autistic community should also be my space too but it not. but it hostile. because am lonely because seeing yourself so crucial because don’t know anyone in person like me don’t have any friends in person like me, so i go online to find people like me and i cannot because no own term to search and what used to be term many people without similar experience insist they understand and can speak for me because they say we have similar experience. because this aloneness and the unique difficulty from being full time nonverbal and the struggle of future and the unique mistreatment from both outside but also inside community have drove me over edge many times and it is presence and knowing their presence of my tumblr nonverbal nonspeaking / higher support needs friends that gave me hope to stay. because so many people don’t listen and instead speak over. terminology only a symptom of problem. address roots, sure, but part of address roots is address symptoms.
‘well nonverbal people are never around” maybe it because you don’t make it welcome for us to join.
“fully nonverbal rare anyway” estimated 30% of us nonverbal nonspeaking, which this statistic probably only count those nonverbal since birth. even more are minimally speaking or without full functional communication, abilities limited to requests. sure, 30% still not majority. but significant amount never the less. speaking lower support needs autistic without intellectual disability not majority anyway too but your experience still deserve heard. ours too.
“see less nonverbal people because they don't have ability to communicate and use social media” yes, many nonverbal nonspeaking people not given access to communication (like AAC), forced to live in silence (because body language communication not enough alone!). silence from birth to teenage years, to adulthood, even until they die. some cannot understand social media or AAC because intellectual disability or cognitive ability. some not allowed on there because safety, some not allowed on because presumed incompetent and abused. all true. do you advocate for them too? or is it just talking point against me, pretend you care?
but not all of us, we exist. some of us thankfully supportive parents all along, parents given resources, us given resources, so we access to AAC since beginning. some of us became nonverbal later in life (which not same experience as those early in life, i acknowledge). some of us after years of forced silence, finally given access to AAC and can now communicate and advocate! some of us on social media - do you listen?
but you see none of us in your community anyway. maybe one token person.
you can go nonverbal. i cannot go verbal. see difference? you can come close to my experience, but i never will have (future) ability to go to yours.
it frustrate that have to specify am nonverbal **all the time** when write this, because if don’t do that will be assumed otherwise. frustrate that when in neurodivergent space stranger see me AAC they assume i can speak because they only know part time users (know part time users frustrate too because people assume they cannot speak and get surprised when they do. me being assumed automatic part time is not fault of part time AAC users.)
even been told am privileged to be nonverbal nonspeaking, privilege over speaking autistic who lose speech because in their mind it mean i get all support i need i get all recognition get all the representation. which. couldn’t be farther from truth.
all that. is fraction of reason i frustrate at “going nonverbal nonspeaking” and “when i was nonverbal nonspeaking.”
so many other words. lose speech. intermittent speech.
just want have own sub community where can find people similar experience.
6K notes
·
View notes
Note
Do you have any tips on how to recover from a meltdown? I've had several in the past few months and I haven't had all that many before, so I don't have much experience and I never what to do to take care of myself and recover afterwards.
The absolute best thing would be to figure out what's causing them and try to do things to minimise the possibility of them happening. What has changed in the past few months that might be causing them or exacerbating any stresses you already had? This can be difficult to do, of course, and can sometimes involves having to be more forceful in self-advocating if you need more adjustments at a place of work or even with family, but it would save a lot of pain and exhaustion in the long-run. Sometimes quite simple changes can make a huge difference!
As for recovery afterwards:
It's probably mostly going to be a case of needing some time to rest (and a restful environment - resting won't be as effective if it involves sitting and chill in a room filled with people and noise).
Meltdowns are exhausting, so try to get some sleep. Hydrate. Maybe have a snack.
You might need a lack of sensory input. I treat meltdowns a bit like a migraine. I need dark and quiet, and solitude. Basically a break from any outside stimuli that I need to process or that I am even less able to cope with than usual. If you need the same, but it's hard to achieve because of your living arrangements or where the meltdowns occur, you can always adjust; use noise cancelling headphones/ear plugs/ear defenders to block out noise, and close your eyes to block out light or other visuals.
If I can't sleep, or I have already slept and feel better but drained, I'll often watch a programme I like (it's light and 'silly', is easy to watch, a nice distraction, and can even cheer me up a bit).
I also tend to feel a bit flu-ey after a meltdown and so having some painkillers and juice can make me feel a bit better. Putting something cool on my forehead can also help as I often feel a little feverish and find it soothing.
If there is someone around who can help you, maybe let them know in advance what things might be helpful for them to do. Having someone get you a drink if you're too exhausted or 'stuck', for example. But ideally it would involve them being able to pre-empt the things that might help you, rather than having to ask (as it might be difficult to make decisions or communicate needs).
To figure out what best works for you, think about how you feel after a meltdown. Do you feel exhausted? Do you have a headache? A sore throat? Or do you feel wired and irritable? Do your sensory issues tend to be worse?
Then think about what things tend to work for you when in that state. What best helps you relax or calm down? What things might make you feel better (so come up with ways to address the things that are causing problems - water and painkillers for headaches, water/some honey for a sore throat, an eye mask or dark room for light sensitivity, etc).
I hope this helps!
Ko-Fi
155 notes
·
View notes
Link
“Often, disabled white people invest in white supremacy because whiteness is the only privilege they are able to exercise. At the same time, they use their disability identity to escape any criticism or calls for self-reflection.“
71 notes
·
View notes
Note
i was wondering if hand flapping is exclusively an autistic trait (for lack of better words)? as far as i know, i’m neurotypical but whenever i get really excited i tend to do a hand flapping motion. i don’t do it to mock, i do it bc it helps me get out the energy/excitement. also is stimming an exclusively neurodivergent trait? sorry for the long question!
No, hand flapping is not an exclusively autistic trait. In fact I know many NT people who hand flap when excited, and it’s also pretty common for NT people to hand flap when upset (many NT people fan their own faces when upset).
Also, everybody stims. People bite their nails, bounce their legs, play. with jewellery. You might know someone who is always chewing gum, or playing with a lighter. ND stimming can often look a bit different to NT stimming (more obvious for example), and is more pathologised (an autistic person rocking is somehow unsightly, if an autistic person hand flaps whilst seeming to *not* be experiencing any big emotion it worries people) but if an NT plays with their necklace, or fiddles with a ring, or even bounces and hand flaps because they’re really excited, it hardly registers with the people around them (although I suppose NT hand flapping is often perceived as effeminate and could therefore gain some negative attention depending on who’s doing it and who sees them).
23 notes
·
View notes
Note
Do you think kids with autism should be allowed to have free therapy dogs like blind and deaf people do?
This is actually quite a complicated question because there’s a lot of different things to consider.
Guide dogs and Hearing dogs are not therapy dogs. They’re assistance dogs. They are disability aids. Not all blind or d/Deaf people need, want, or have assistance dogs.
There are organisations that provide assistance dogs for autistic children. Not all autistic children will need/will benefit from having an assistance dog, or be suitable as a handler (although usually the parent is the handler), and there are certain tasks that ‘Autism dogs’ seem to be used for that I personally don’t agree with - I don’t think it’s the safest thing to have a child tethered to a dog, for either the child or the dog). I’m not sure whether any/all organisations that provide Autism dogs charge for them.
For a long time it seemed that no organisations would provide dogs for autistic adults (at least in the UK), when I think that adult autistic handlers makes more sense. Children have their parents to help them navigate the world, whereas adults might benefit from an assistance dog to help them be more independent.
Whether an assistance dog is suitable for someone is always going to be on a case by case basis. Aspects of being an assistance dog handler can also cause difficulties (such as dealing with members of the public who insist on touching or distracting the dog, challenge you on whether you are allowed to be somewhere with the dog, or even just talk to you when you’d rather they didn’t). Animals are also a huge responsibility.
It’s possible to owner-train an assistance dog, although obviously they still have to have the same high level of training to be considered an assistance dog and to have access to public spaces (where dogs are otherwise not allowed to be).
12 notes
·
View notes
Text
on the serotonin “chemical imbalance” claim
Antidepressants are supposed to work by fixing a chemical imbalance, specifically, a lack of serotonin in the brain. Indeed, their supposed effectiveness is the primary evidence for the chemical imbalance theory. But analyses of the published data and the unpublished data that were hidden by drug companies reveals that most (if not all) of the benefits are due to the placebo effect. Some antidepressants increase serotonin levels, some decrease it, and some have no effect at all on serotonin. Nevertheless, they all show the same therapeutic benefit. Even the small statistical difference between antidepressants and placebos may be an enhanced placebo effect, due to the fact that most patients and doctors in clinical trials successfully break blind. The serotonin theory is as close as any theory in the history of science to having been proved wrong. Instead of curing depression, popular antidepressants may induce a biological vulnerability making people more likely to become depressed in the future.
Irving Kirsch. 2015. “Antidepressants and the Placebo Effect”. Zeitschrift für Psychologie 222 (3): 128–134. PMCID: PMC4172306. https://doi.org/10.1027/2151-2604/a000176.
A decade ago, we published an article in PLoS Medicine about the serotonin deficiency theory of depression (Lacasse & Leo, 2005). We transposed the psychiatric literature on serotonin and depression with what pharmaceutical companies had been claiming in their consumer advertisements for years—that a chemical imbalance (serotonin deficiency) caused depression and this imbalance was corrected by selective serotonin reuptake inhibitor (SSRI) drugs. For instance, advertisements for fluoxetine (Prozac) had stated:
When you’re clinically depressed, one thing that can happen is the level of serotonin (a chemical in your body) may drop. So you may have trouble sleeping. Feel unusually sad or irritable. Find it hard to concentrate. Lose your appetite. Lack energy. Or have trouble feeling pleasure…to help bring serotonin levels closer to normal, the medicine doctors now prescribe most often is Prozac® (Eli Lilly, 1998)
We knew that such advertisements did not accurately reflect the scientific status of the serotonin theory in the psychiatric research community (see Table 1; we have modified the original table to integrate new material that came to our attention since 2005). Some advertisements were more tentative or clever in their wording than others, but it seemed obvious that the drug companies were at least pushing the boundaries. We thought several of them were going over the line, in plain sight of the Food and Drug Administration (FDA), which ostensibly regulates direct-to-consumer advertising. Our goal was to illustrate the clear disconnect between the existing psychiatric science and what the public was being told in these advertisements, and we argued that the FDA should issue warning letters to pharmaceutical companies (Lacasse, 2005; Lacasse & Leo, 2005). Of course, there were ramifications for clinicians—if it was illegal to claim this in advertisements, wasn’t it also an unacceptable thing to be telling vulnerable clients?
After the publication of the paper, we were interviewed by numerous journalists. Several of them thought our work was provocative and that we were “attacking” a well-accepted theory. If it was an attack, it was an inside job, as our sources included NIMH-funded scientists, an award-winning biological psychiatrist, and a popular psychiatric textbook. Anyone familiar with the history of serotonin research would find our argument unremarkable (e.g., Healy, 1997, 2004; Moncrieff, 2008; Valenstein, 1998). In the United Kingdom, psychiatrist David Healy has been making this point for decades (e.g., Healy, 1987, 1997, 2004, 2012, 2015). But the questions from journalists reminded us that the enormous marketing campaigns promoting SSRI drugs (and surely many of the physicians prescribing them) had convinced the U.S. public that the serotonin theory of depression was firmly grounded in science. This wasn’t just an issue of misleading advertising. Instead, the incredulity seemed fueled by the significant number of mental health clients who had heard the chemical imbalance explanation from their prescribers.
link to Lacasse and Leo 2005 added. Jeffrey R. Lacasse and Jonathan Leo. 2015. “Antidepressants and the Chemical Imbalance Theory of Depression: A Reflection and Update on the Discourse”, with rejoinders by Ronald Pies and Daniel Carlat. the Behavior Therapist 38 (7): 206–213.
Biomedical causal explanations of depression, principally the “chemical imbalance” theory, have been vigorously promoted in recent decades to reduce public stigma and facilitate pharmacotherapy (Lacasse & Leo, 2005). As a result, the chemical imbalance theory has become the dominant cultural understanding of depression in the United States (France, Lysaker, & Robinson, 2007). Anti-stigma initiatives by the National Alliance for Mental Illness (NAMI) portray depression as a “chronic medical illness” (NAMI, 2013). Characterizing depression in biomedical terms is assumed to reduce stigma according to attribution theory, which predicts that attributing a mental disorder to an uncontrollable cause reduces blame among observers (Corrigan, 2000). However, increased public endorsement of the chemical imbalance explanation has not resulted in improved attitudes toward depressed individuals (Pescosolido et al., 2010). Indeed, research findings suggest that biomedical causal explanations for depression do not reliably reduce blame and may worsen perceptions of dangerousness and unpredictability (Kvaale, Gottdiener, & Haslem, 2013).
Biomedical explanations for mental disorders may produce essentialist thinking, in which biological causes suggest inherent differences in the nature of sufferers (Boysen & Gabreski, 2012; Haslam, 2000, 2011; Phelan, 2005). An essentialist perspective views biologically-based mental disorders as deep-seated, immutable defects which make an individual categorically distinct from others. One predicted consequence of this perspective is prognostic pessimism, the belief that the problem is unlikely to respond to remedial action (Dar-Nimrod & Heine, 2011; Haslam, 2011). In studies of public attitudes toward individuals with mental disorders, prognostic pessimism appears to be worsened by biomedical causal explanations (e.g., Bennett, Thirlaway, & Murray, 2008; Phelan, 2005; Phelan, Yang, & Cruz-Rojas, 2006). Although studies of the attitudes of laypersons are necessary to inform efforts to reduce public stigma, such research does not address a question of critical importance to clinicians: how do biomedical causal explanations affect how individuals with mental disorders view their own symptoms?
as Kemp, Lickel, and Deacon state in the abstract:
This experiment examined the impact of chemical imbalance test feedback on perceptions of stigma, prognosis, negative mood regulation expectancies, and treatment credibility and expectancy. Participants endorsing a past or current depressive episode received results of a bogus but credible biological test demonstrating their depressive symptoms to be caused, or not caused, by a chemical imbalance in the brain. Results showed that chemical imbalance test feedback failed to reduce self-blame, elicited worse prognostic pessimism and negative mood regulation expectancies, and led participants to view pharmacotherapy as more credible and effective than psychotherapy. The present findings add to a growing literature highlighting the unhelpful and potentially iatrogenic effects of attributing depressive symptoms to a chemical imbalance.
Joshua J. Kemp, James J. Lickel, and Brett J. Deacon. 2014. “Effects of a Chemical Imbalance Causal Explanation on Individuals’ Perceptions of Their Depressive Symptoms”. Behaviour Research and Therapy 56:47–52. https://doi.org/10.1016/j.brat.2014.02.009.
900 notes
·
View notes
Link
“Modern evidence reveals that there is little difference between antidepressants and placebo for the treatment of depression. This is the message of Khan and Brown’s review (1) of antidepressant research. In fact, older studies came to the same conclusion. In 1969, the authors of a comprehensive review commissioned by the U.S. National Institute of Mental Health concluded that “in well-designed studies, the differences between the effectiveness of antidepressant drugs and placebo are not impressive” (2), p. 19).
Problems with the evidence for antidepressants go even deeper than Khan and Brown suggest, however. Not only does this evidence show that these drugs are little different from placebo, but also that there are no grounds to believe they have specific effects that would justify their classification as “antidepressants”.
Like other drugs used for mental health problems, drugs classed as antidepressants are psychoactive substances. Psychoactive substances are drugs that enter the brain and by doing so modify normal thoughts, emotions and behaviours. Recreational drugs have psychoactive properties that some people find pleasant or exciting, but other drugs – including antipsychotics, anticonvulsants and antidepressants – have psychoactive effects that are less appealing. The psychoactive effects of individual antidepressants vary in strength and character, with the effects of some, such as the selective serotonin reuptake inhibitors (SSRIs), being weak and subtle, whereas the effects of others are more profound (e.g., the tricyclics).
The fact that antidepressants are psychoactive substances has major implications for the interpretation of placebo-controlled trials. Firstly, the use of a psychoactive substance will inevitably impact on the experiences and emotions captured by depression rating scales. The sedative effects of antidepressants, such as the tricyclics and newer drugs like mirtazapine, for example, are likely to reduce the degree of agitation, anxiety and insomnia experienced by people with depression. These symptoms feature strongly in measurement scales. Changes in sleep alone can account for up to 6 points on the Hamilton Rating Scale for Depression, for example, whereas typical antidepressant-placebo differences are around 2 to 3 points (3,4). Moreover, psychoactive effects may impact in varied ways on thoughts.
Secondly, the psychoactive effects of antidepressants, along with the physical modifications they produce (both commonly referred to as “side effects”, although this is misleading since an independent, therapeutic effect has not been established), will infringe the double blind design. Some of the participants allocated to the active drug will be able to detect that they have received the real drug because of the physical or mental changes the drug produces, especially since they are provided with detailed information on possible side effects. Thus, it has been shown in many placebo-controlled trials of drugs used for mental health problems that participants can guess what they have received better than chance (5). In this situation, people allocated to the active drug are likely to have enhanced expectations of the effectiveness of therapy, and people who suspect they are taking placebo may have unduly negative expectations. Both of these factors may create or exaggerate a difference between antidepressants and placebo.
Unless the psychoactive effects of antidepressants are somehow discounted, differences between antidepressants and placebo cannot be interpreted as providing evidence that those drugs have a specific “antidepressant” effect. Indeed, it transpires that most drugs with psychoactive effects – including many antipsychotics, benzodiazepines, stimulants, buspirone and opiates (6) – produce the same changes as so-called antidepressants in randomized trials in people diagnosed with depression. Moreover, antidepressants themselves come from a wide array of chemical classes, and produce diverse pharmacological effects. Unsurprisingly, it seems that the experience of taking some sort of mind-altering substance produces a slightly different result from taking an inert placebo, when you attempt to measure people’s thoughts and feelings (7,8).
If we accept this model, we need to ask whether the psychoactive effects that antidepressants or other drugs produce might logically be useful in people with depression. There may, for example, be a role for temporary use of drugs with sedative properties to manage insomnia, anxiety and agitation in people who experience these symptoms, balancing proper evidence of benefits against adverse effects, including risks of dependence.
There has been some debate as to whether the SSRIs and related antidepressants produce a state of emotional suppression or disengagement. Antipsychotics are well known for dulling emotions, but the effects of SSRIs are likely to be more subtle. Evidence from converging sources now suggests that SSRIs and other newer antidepressants do have this property, and that it is associated with recognized side effects, such as loss of libido and sexual impairment (9–11). Many people dislike this state of emotional numbing but, in theory, some may find it useful to manage an intense emotional crisis. Again, we need evidence to explore whether this particular effect produces any tangible improvement in people suffering from depression, and whether people find it acceptable or not.
For decades now people have been told that depression is a chemical imbalance and that antidepressants work by correcting that imbalance. This view is not supported by evidence, and is misleading as to the nature and effects of antidepressant drugs. We need to recognize that antidepressants are psychoactive substances, we need more data on the nature of the varied psychoactive effects they produce, and we need to explore whether giving drugs that produce an artificially altered emotional state is a useful and acceptable intervention for people with depression.”
42 notes
·
View notes
Link
“Although the early antidepressant trials which included severely ill and hospitalized patients showed substantial drug-placebo differences, these robust differences have not held up in the trials of the past couple of decades, whether sponsored by pharmaceutical companies or non-profit agencies. […] As of now, antidepressant clinical trials have an effect size of 0.30, which … is less than impressive.”
10 notes
·
View notes
Text
lots of messages asking about antidepressants so i’ll invite anyone who wants to to search “antidepressants” on my blog and you’ll get more results than you care to :) here’s my distilled take: if meds are helping you, who cares what some lady on the internet thinks?? truly, unfollow me if you’re doing well w meds and this discourse is unproductively upsetting to you. psych meds are complicated, as are the dynamics around their administration. we don’t know exactly how they “work” (it’s certainly not in the way that’s popularly conveyed in the chemical imbalance model), and long term risks are also not well understood or publicized. some people have very bad experiences w these meds, and with withdrawal and beyond. the star*d trial gave the strongest evidence to date that antidepressants are only a little more effective than placebos, and mainly for people with severe depression. i like a good placebo effect, tho!! if i’ve weighed its risks! and i like what helps us get thru the days. i value sustaining life above all else. and again, who even cares what i think? your body, your choice.
118 notes
·
View notes
Note
What is the oldest that Autism can develop? The latest age of early childhood? I'm aware you're not professionals, but I thought that you may have knowledge of this.
You can’t develop autism. Autistic people are autistic from birth.
50 notes
·
View notes
Text
“Diagnostic manuals such as the DSM were created to provide a common diagnostic language for mental health professionals and attempt to provide a definitive list of mental health problems, including their symptoms.
The main findings of the research were:
• Psychiatric diagnoses all use different decision-making rules
• There is a huge amount of overlap in symptoms between diagnoses
• Almost all diagnoses mask the role of trauma and adverse events
• Diagnoses tell us little about the individual patient and what treatment they need
The authors conclude that diagnostic labelling represents ‘a disingenuous categorical system’.
Lead researcher Dr Kate Allsopp, University of Liverpool, said: “Although diagnostic labels create the illusion of an explanation they are scientifically meaningless and can create stigma and prejudice. I hope these findings will encourage mental health professionals to think beyond diagnoses and consider other explanations of mental distress, such as trauma and other adverse life experiences.”
Professor Peter Kinderman, University of Liverpool, said: “This study provides yet more evidence that the biomedical diagnostic approach in psychiatry is not fit for purpose. Diagnoses frequently and uncritically reported as ‘real illnesses’ are in fact made on the basis of internally inconsistent, confused and contradictory patterns of largely arbitrary criteria. The diagnostic system wrongly assumes that all distress results from disorder, and relies heavily on subjective judgments about what is normal.””
#everyone that gets diagnosed with everythign under the sun knows this already but its worth putting here#antipsychiatry#articles
17K notes
·
View notes
Note
You mentioned in one of your replies that you heard that cbt wasn't always that helpful for autistic people. Do you know why that is? I've always disliked cbt (and it's variants), but it's always pushed on me as some sort of gold standard
In my case, one of the biggest reasons was my communication difficulties.
I struggle with people, so having to meet a stranger causes a lot of stress and anxiety, being expected to communicate wholly face-to-face with that stranger, the lay-out of the rooms that therapies are usually delivered in (chairs facing each other, no desk in between to block the other person). I don’t think I have ever managed to communicate anything of importance to any professional, and usually the more significant information is provided by whoever is accompanying me (so any sessions I ‘go alone’ tend to seem like a waste of time). When I heard that it wasn’t always very helpful for autistic people in general, I can’t recall whether there was any explanation as to why this was, and if so what it was!
From the NHS site:
Cognitive behavioural therapy (CBT) is a talking therapy that can help you manage your problems by changing the way you think and behave.It’s most commonly used to treat anxiety and depression, but can be useful for other mental and physical health problems.
So for me, that in itself is strike one! Talking therapies aren’t always accessible for people, and it can be difficult for various reasons to get around this. For example, needing an interpreter or facilitator to support, or struggling with AAC in pressured/stressful situations.
How CBT worksCBT is based on the concept that your thoughts, feelings, physical sensations and actions are interconnected, and that negative thoughts and feelings can trap you in a vicious cycle.
Many autistic people can struggle to recognise how they are feeling, physically and emotionally, or might struggle to recall how they felt during a situation prior to the therapy session, and/or to communicate their feelings, which will likely hinder the process. Remembering what advice was given, recognising when to apply it, being able to do so under other stressors (during times of sensory overload, for example, or alongside trying to process a social interaction) or whilst combating executive dysfunction, etc… (and then having to report back to the therapist during your next session) are all other challenges, are all things that might make it especially hard for autistic people. Here are the pros and cons as listed on the NHS website:
Pros and cons of CBT
Cognitive behavioural therapy (CBT) can be as effective as medicine in treating some mental health problems, but it may not be successful or suitable for everyone.
Some of the advantages of CBT include:
it may be helpful in cases where medicine alone has not worked
it can be completed in a relatively short period of time compared with other talking therapies
the highly structured nature of CBT means it can be provided in different formats, including in groups, self-help books and apps (you can find mental health apps and tools in the NHS apps library)
it teaches you useful and practical strategies that can be used in everyday life, even after the treatment has finished
Some of the disadvantages of CBT to consider include:
you need to commit yourself to the process to get the most from it – a therapist can help and advise you, but they need your co-operation
attending regular CBT sessions and carrying out any extra work between sessions can take up a lot of your time
it may not be suitable for people with more complex mental health needs or learning difficulties, as it requires structured sessions
it involves confronting your emotions and anxieties – you may experience initial periods where you’re anxious or emotionally uncomfortable
it focuses on the person’s capacity to change themselves (their thoughts, feelings and behaviours) – this does not address any wider problems in systems or families that often have a significant impact on someone’s health and wellbeing
Some critics also argue that because CBT only addresses current problems and focuses on specific issues, it does not address the possible underlying causes of mental health conditions, such as an unhappy childhood.
It may well be that CBT can be effective if it is adapted to suit the autistic person’s needs (is made accessible). However, it very often seems that there is a ‘one size fits all’ approach to most things.
#I'm encountering this problem in counseling now so I can attest to this#autism#actuallyautistic#cbt
92 notes
·
View notes
Text
There’s a website where you can learn ASL (American Sign Language) on your own, free and it’s a 31 Day program! The woman on there, her name is Rochelle Barlow, she runs the site and she actually is a homeschool teacher and teaches ASL. I am passing this on to some of you guys cause most of y’all on here is open-minded and curious and it is something important to learn.
I truly believe this site is helpful for some people who can not afford to going to ASL classes, or someone like me that just enjoys learning something new. This site will help with that. Once you sign up you will put in your email address and Rochelle sends you emails on tips on how to sign, gives you practice sheets, and gives you your weekly videos. And its all online. No need to paying for anything. (Unless if you want to she has something very different to this program)
IMO and yes, this site is really amazing and is important because you never know if someone who is deaf or HOH needs help, if you end up losing your hearing ability this is something you will at least have on the back of your head, and it is just like any other language and should be taught.
153K notes
·
View notes
Photo




This is the most accurate description I’ve ever found, thought it was worth spreading ❀
186K notes
·
View notes
Photo







@actuallyadhd
[Image Descriptions:
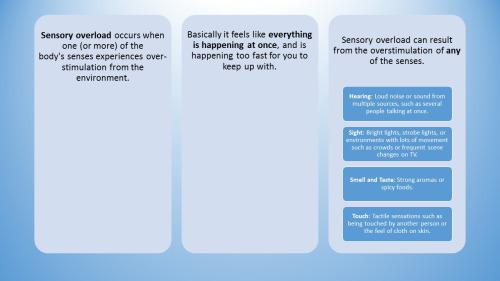
All slides have a light blue background, and the text is written in blue rectangles with rounded corners.
Slide 1: The title is in white text inside a dark blue circle that is centred in the slide.
Sensory Overload And how to cope
Slide 2: The header is in a dark blue rectangle and white text, and the body is in a pale blue rectangle and black text.
Sensory overload has been found to be associated with disorders such as:
Fibromyalgia (FM)
Chronic Fatigue Syndrome (CFS)
Post Traumatic Stress Disorder (PTSD)
Autistic spectrum disorders
Generalized Anxiety Disorder (GAD)
Synesthesia
Slide 3: The text is in three pale blue rectangles that go horizontally across the slide. All use black text. The last rectangle has four smaller dark blue rectangles with white text inside it for the four points. The text is centred in all of the rectangles.
Sensory overload occurs when one (or more) of the body’s senses experiences over-stimulation from the environment.
Basically it feels like everything is happening at once, and is happening too fast for you to keep up with.
Sensory overload can result from the overstimulation of any of the senses.
Hearing: Loud noise or sound from multiple sources, such as several people talking at once.
Sight: Bright lights, strobe lights, or environments with lots of movement such as crowds or frequent scene changes on TV.
Smell and Taste: Strong aromas or spicy foods.
Touch: Tactile sensations such as being touched by another person or the feel of cloth on skin.
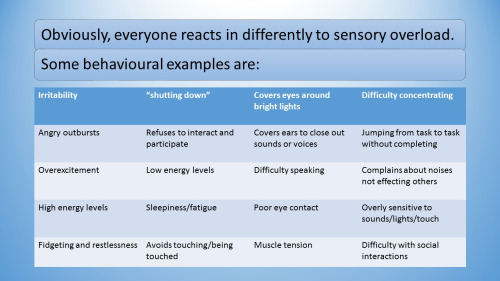
Slide 4: A heading in two light blue rectangles with black text, followed by a table with a dark blue first row that has white text, and then alternating pale blue and white rows with black text. (The table is not really a table, it is just a four-column list.)
Obviously, everyone reacts in differently to sensory overload.
Some behavioural examples are:
Irritability — “Shutting down” — Covers eyes around bright lights — Difficulty concentrating Angry outbursts — Refuses to interact and participate — Covers ears to close out sounds or voices — Jumping from task to task without completing Overexcitement — Low energy levels — Difficulty speaking — Compains about noises not effecting others High energy levels — Sleepiness/fatigue — poor eye contact — Overly sensitive to sounds/lights/touch Fidgeting and restlessness — Avoids touching/being touched — Muscle tension — Difficulty with social interactions
Slide 5: The header is in a dark blue box with pointy corners and white text. The body is in a pale blue box with pointy corners and black text.
There are two different methods to prevent sensory overload: avoidance and setting limits:
Create a more quiet and orderly environment - keeping the noise to a minimum and reducing the sense of clutter.
Rest before big events.
Focus your attention and energy on one thing at a time.
Restrict time spent on various activities.
Select settings to avoid crowds and noise.
One may also limit interactions with specific people to help prevent sensory overload.
Slide 6: This looks the same as the last slide except the text in the header is black.
It is important in situations of sensory overload to calm oneself and return to a normal level.
Remove yourself from the situation.
Deep pressure against the skin combined with proprioceptive input that stimulates the receptors in the joints and ligaments often calms the nervous system.
Reducing sensory input such as eliminating distressing sounds and lowering the lights can help.
Calming, focusing music works for some.
Take an extended rest if a quick break doesn’t relieve the problem.
Slide 7: Four light blue rectangles with rounded corners, stacked one above the other, with black text.
What if someone you know is experiencing sensory overload?
Recognize the onset of overload. If they appear to have lost abilities that they usually have, such as forgetting how to speak, this is often a sign of severe overload.
Reduce the noise level. If they are in a noisy area, offer to guide them somewhere more quiet. Give time to process questions and respond, because overload tends to slow processing. If you can control the noise level, for example by turning off music, do so.
Do not touch or crowd them. Many people in SO are hypersensitive to touch - being touched or thinking they are about to be touched can worsen the overload. If they are seated or are a small child, get down to their level instead of looming above them.
Slide 8: Similar to previous slide, only with three rectangles instead of four.
Don’t talk more than necessary. Ask if you need to in order to help, but don’t try to say something reassuring or get them talking about something else. Speech is sensory input, and can worsen overload.
If they have a jacket, they may want to put it on and put the hood up. This helps to reduce stimulation, and many people find the weight of a jacket comforting. If their jacket is not within reach, ask them if they want you to bring it. A heavy blanket can also help in a similar way.
Don’t react to aggression. Don’t take it personally. It is rare for someone who is overloaded to cause serious harm, because they don’t want to hurt you, just get out of the situation. Aggression often occurs because you tried to touched/restrained/blocked their escape.
Slide 9: Similar to previous slide, only with two rectangles instead of three.
When they have calmed down, be aware that they will often be tired and more susceptible to overload for quite awhile afterwards. It can take hours or days to fully recover from an episode of sensory overload. If you can, try to reduce stress occurring later on as well.
If they start self-injuring, you should usually not try to stop them. Restraint is likely to make their overload worse. Only intervene if they are doing something that could cause serious injury, such as hard biting or banging their head. It’s a lot better to deal with self-injury indirectly by lowering overload.
Slide 10: The header is in a dark blue rectangle with white text, and the other text is in a row of five dark blue circles with white text. The text is centred in all shapes.
To summarise - Remember the 5 R’s
Recognise The symptoms of overload
Remove Yourself from the situation
Reduce the stimulus causing the overload
Relax Your body and calm yourself down
Rest Yourself as you will most likely feel fatigue.]
16K notes
·
View notes