#you check for brachial pulse
Explore tagged Tumblr posts
Text
Why is this Shoto coded to me lol
For the record, the average person often struggles to do it correctly even when taught in a CPR class. Which is why we teach laypersons not to spend more than about 5 seconds trying before starting CPR (people will sit there trying to find the pulse instead of proceeding with life saving bc they’re panicked and not thinking straight).
There is also an opposite phenomenon which is this…
Shoto: *searches for pulse with his thumb*
Shoto: He’s alive!
Aizawa: No, he’s dead. That’s your own pulse.

#if you’re curious#you should take the pulse on the side of the neck you are next to#don’t reach across the body#in an infant you don’t check for carotid pulse in the neck#you check for brachial pulse#on the inside of the upper arm#and use your index and middle finger#bc the thumb can make you falsely feel your own pulse not theirs
4K notes
·
View notes
Text
Ripples (Hen, Tommy) - 1400wd
AN ~ i am obsessed with sweet, sweet platonic content and the hentommy moment we may never get, so i'm giving us one.
In the middle of a building collapse (because of course they are), Hen and Tommy catch up. Read on AO3 (~1500wd)
-
It's coming down!
The ear-shattering screech of steel and concrete is the only thing Hen can hear for a long moment after she throws herself forward into the hallway. The roof is holding out here, although the concrete dust isn't helping as the air is becoming dangerously smokey. A torn electrical line spits out aimless sparks. But she's okay.
Grimacing against the oncoming headache, she gets to her feet and takes stock.
“Ravi, you okay?”
“Partial floor collapse back here when the ceiling came down,” Ravi reports from somewhere out of sight. He coughs. “I'm down a floor, but I'm okay.”
“Kinard?”
Nothing.
“Tommy? Come in.”
“Hen?”
His voice is weak, but she's not just hearing it through the comms. Hen turns back to the pile of rubble, sifting through sheets of ceiling plaster and trying to pinpoint where it's coming from. Soon enough, she sees a hand wave.
“Got you,” she assures him. “How you feeling?”
He groans. She frowns as she clears the last of the lighter debris, and can see why, because of course he's not been lucky enough to catch a bit of plaster and plywood. He's stuck face-down, the whole back half of his body pinned under probably a half a tonne of rubble.
“My leg,” he advises. “Right's okay I- I think. Left is really- oh, Christ, I think it's twisted up pretty bad. At least it was. I can't- I don't think I can feel it anymore.”
Tommy's breath shakes like he's fighting off a panic attack as Hen requests assistance. Possible spinal. Even when she manages to get both of their halligans under there and relieve some of the pressure, there's only so much that can be seen from here of his bloody mess of a knee. She can only confirm that it's highly unlikely his toes are actually moving. And sure, it means maybe nothing but maybe it means a pinched nerve or amputation or permanent paralysis or, or, or – in other words; no more being a firefighter, no more being a pilot, no more of a lot of other things too probably and that hurts so much more than the fact that half his body's being pulverised into the floor.
“Come on now,” Hen challenges gently. “You know better than to take it to the worst case scenario.”
He nods as best he can down here. He's starting to feel cold and shake and it's got to be some kind of stress response. Is he going into shock?
“I also know better,” he manages, “than putting myself on the call roster for the craziest firehouse in LA.”
“Yeah, well. We all do stupid things for pretty boys, hm?”
He can picture it, the smirk on her face; equal parts compassion and mischievousness. It makes him feel warmer and stop clenching his jaw. He hadn't even realised he was doing that. But she's right, and she's picked a hell of a time to bring it up, and it's working: thinking of Evan and his boyish smile and his big blue eyes brings his heart rate down, steadies his breathing...
Hen settles in beside him. She's close enough to check his brachial pulse, or grab him and yank him forward – possible spinal be damned - if anything else goes down, but as it is, they wait.
After a few breaths of reassuringly collapse-sounds-free silence, Tommy asks:
“So, how's Karen and Denny?”
It almost makes her laugh. He's still face down and bleeding under a roof and for his tone, they could be stood free and clear around an average office water cooler. Ah, the life of a firefighter.
“They're good,” Hen assures him. “Great, actually. You know, Denny's almost fourteen?”
“Wow. Way to make me feel old.”
“Tell me about it.”
“Evan tells me you guys have a daughter now too?”
“Mara,” Hen updates him. “She's nine. Came to us through foster. She's been through a lot but we're getting there. She's really strong, and she's working really hard, you know, to heal.”
“Good, that's good. Sounds like she's got a bright future ahead of her,” Tommy congratulates. Then a more sombre tone settles into his voice. “Sounds like someone else I know.”
It's something about having your whole life and livelihood hanging in the balance that brings out this sort of confessional in people, Hen knows. She's both always wary of it, and also sort of addicted to the kind of radical honesty that constantly spilling your literal actual guts tends to inspire. So even as she tries to get out - “Tommy, we don't have to do this,” - she braces herself to accept whatever is about to come next as if it's the last thing he'll ever get to say.
“I'm sorry I was such a dick to you,” he says, “back in the day. I wish I could say I just got caught up in the machismo and stuff but honestly I- I didn't know any better. And I didn't really want to try. But you, and Chim, you're some of the best firefighters out there and I didn't give you guys your due and I'm sorry.”
Tears prick at Hen's eyes, and it doesn't help the sweat and smoke and concrete dust that's still settling all around them. She'd patched over these wounds a long time ago but it feels nice all the same, freeing in a way she hadn't anticipated, to get an apology she was never going to ask for.
“You know,” Tommy continues, softer now. “I think you saved my life.”
“Uh, pretty sure I'm up to about six counts of that,” she jests, because she can feel it coming;
“I'm not talking about in the field.”
There it is.
Hen's breath catches in her throat as Tommy finds the courage to recount it. She's felt it coming for a long time now, maybe even years, but certainly since he'd strode into Chim's hospital room all giddy and covered with soot and with Buck she'd kind of wondered. Wondered what her crying and demanding to be seen in the middle of the firehouse floor all those years ago might have actually done. It had done a lot for her, but she'd never quite be ready to hear, let alone to contemplate, what those words might have done for a man who'd grown up in a military family under don't ask don't tell – the same policy that had kept Karen's dream out of reach until it was too late. For a man who'd not grown up having and valuing marginalised experiences; not having a bad-ass, butch as hell mother who'd always taught her to speak her truth, even if that truth was something said mother had struggled to deal with at first. He'd been taught how to be a man and a gentleman and a soldier and not much else. He'd never realised what intimacy could actually be like, what love could actually be like; he'd thought he'd scared off every girl he'd ever had because there was something abnormal about him. Something fundamentally unloveable.
“... Bits and pieces, looking back – you know how it is. I'd just always sort of thought there was something wrong with me. I'd never really seen any other possibility. Until you. So. I know I'm late to the party, but for what it's worth – I see you now, Hen. And I am honoured to call you Captain.”
Hen nods, trying to swallow the lump in her throat as some of those tears splash down her cheeks. In spite of herself she feels something reach back in time and touch her fierce, heartbroken younger self; a promise that it's going to be worth it one day.
“It's worth a lot, Tommy,” she manages. “Thank you.”
Then, the radio crackles back to life.
“Cap,” Eddie reports, “Ambulances from the 133 pulling up. 118 should be on you now.”
Footsteps clamour down the hall toward them, as Ravi, Buck and Chim rush in, backboard and hydraulic jack in hand. Chim pushes the morphine, Ravi pushes the pain point of the rubble away, Buck and Hen slide Tommy out and even though he yelps and moans Buck can't hide the joy and relief that breaks out on his face as they flip him onto his back and slide him onto the backboard in swift, perfectly matched unison like a well-oiled machine.
“We've got you,” Buck promises, squeezing one of Tommy's trembling hands with a sweaty, giddy smile. He glances over at Hen, and checks in - “You good?”
What do you think it is? he'd asked her once. The secret to happiness?
He's in the middle of a burning building, and it looks like it's pouring out of him now.
“I'm great,” she replies. “Let's move.”
27 notes
·
View notes
Text
Learning
Today in school I learned how to take vital signs and decided to make this cute little one shot where Halstead Sister practices on Jay.
"okay, so I'm just going to first try to find your pulse on your brachial artery" you said while setting down your stethoscope and blood pressure cuff. You had just come back from class and coincidentally both your brothers were home and you had convinced Jay to allow you to take a set of vitals on him for practice.
Jay extended his arm and your began palpating the area, above, below, and around on either side of his upper arm trying to feel his pulse. Every time you looked up to try and focus on feeling if there was a pulse, you watched as your brother's face scrunched with confusion. After about 2 minutes of not locating the pulse, you exclaimed, "huh, I can't seem to find it. Like it'll jump and then I won't be able to feel it" "Y/N, he's a living breathing person, you must be able to feel it. Try moving his bicep muscle" called Will, who was starting a pot of water for pasta. "Oh, that's a good idea" you stated while pushing Jay's muscle out of the way and trying to feel for it again. "Got it!" You shouted! "I guess all that working out has made that harder, hmm good to know" Jay noted while allowing you to wrap the blood pressure cuff on his arm. Rolling your eyes, you began inflating the cuff, "Let me know if I'm hurting you" you said while watching for the systolic number. Slowly you began to deflate the cuff while trying to find the diastolic and once it was fully deflated you began writing down your findings on your "Vitals Sheet" "So, what's the verdict doc? High blood pressure or low blood pressure?" joked Jay while ripping the cuff off his arm and placing it on the table. "I got 130/80, so not the best but not bad either." "Sounds good to me" shrugged Jay. "Are you going to practice gathering any other vital signs Y/N/N or are you done?" asked Will while adding spaghetti to the bowling water. "hmm, could I try getting your heart rate manually? I was about to get a reading of that on myself in class today, but then I got called into the hallway to practice lifting the stretcher with the heavy dummy on it" "Sure, why not" shrugged Jay while handing over his arm. Grabbing the pulse near the side of his wrist near his thumb, you looked at your watch and began counting. "uh, Will, I got 26" Dropping the spoon and turning off the stove, Will ran over, "Move out of the way" As you moved, Jay looked at Will with concern written on his face, "why did you run over here so fast?" "Our sister has pained me long enough, I'm going to show her how the professionals do it!" Will stated while swiftly grabbing his brother's wrist. He located the pulse in no time flat, checking his watch, he counted. "43, which if we multiplied by 2, which we are supposed to do, would equal out to 86" "Which is? Good or bad Will?" probed Jay. "Y/N, care to answer?" nudged Will while looking at you. "In normal range!" you mumbled. It wasn't your fault you weren't fast at this or even good at locating a pulse on someone else. The only practice of locating a pulse you've had before this was on yourself and some times at night when you couldn't sleep so you would feel for your wrist pulse to help lull you to sleep. "Good job, now I think you've had enough practice for one day" concluded Will while getting up to tend to the pasta. As you went to clean up your supplied, Jay nudged you. When you turned to face him, he stated, "Hey, you're learning still. It takes time to get as fast as Will. But the fact that you're trying and willing to make mistakes shows you are going to be a great EMT"
#chicago pd imagine#jay halstead imagine#will halstead imagine#halstead sister imagine#halstead sister#halstead sister x halstead brothers#halstead brothers#halstead brothers imagine#one chicago imagine
73 notes
·
View notes
Text
Diabetes Lecture
Dr. Samaan
8/23/23
HgbA1c 5.7%-6.4% is prediabetes
HgbA1c 6.5% is diabetic
Normal HgbA1c 4.8-5.6% is normal
DM: A1c 6.5%, BG 126, random BG >200 with symptoms
The A1c has to be a lab draw in order for you to use it to make the diagnosis. So a POC HgbA1c doesn’t count to make the diagnosis.
Screen everyone age 40-70 who are overweight or have risk factors; younger than 40 and obese with risk factor; screen q1-3 years. Risk factors: HDL<35, TG >250, depression, on atypical antipsychotics, high risk populations (non-white), OSA/sleep issues, HIV+ for 15+ years on meds. Old HIV meds caused endocrine issues. Newer HIV meds don’t unless they’ve been on them for a long time.
You don’t need to be fasting to check HgbA1c. Not covered as screening by CMS. A1c not accurate in GDM, renal failure, anemias, renal failure, liver disease.
Prediabetes: 5-7% weight loss will cut the risk of progressing to diabetes by 1/2! Moderate exercise: of 150 minutes a week (e.g., brisk walking 3+ mph), water aerobics, bicycling 10 mph or less, tennis (doubles), gardening—OR 75 minutes of vigorous intensity exercise a week.
Metformin started in prediabetics decreases progression by 31%! Shown to decrease CVD risk. Works best for BMI>35. Metformin can cause low B12. We should use “med monitoring” code annually in pts on metformin. Diarrhea is a common adverse effect. If pt can’t leave the house because of the diarrhea, try the extended release form.
GLP1 agonists and SGLT2 inhibitors could be used in prediabetics. It’s in the works.
If A1c of 9 and BG >200, you will have less fatigue, polyuria, blurred visions, skin infections.
A1c <7.5 à improved quality of life and increased productivity at work
Goal A1c is <7%
Tighter control in younger pts is ok.
Older pts can have A1c goal of 8.0%; avoid hypoglycemia and side effects of increased meds.
Metformin and lifestyle modifications are first line management.
You can start with something other than metformin, but insurance might not cover it.
DM education can help drop A1c by 0.6% or more. WDH and PRH have diabetes education classes.
Diabetic Benchmarks/Screenings:
Statins! All diabetics over 40 should be on moderate to high intensity statin. Under 40 if additional CVD risk factors.
Pts with DM have increased number of small LDL particles which tend to be more associated with ASCVD.
DM is the leading cause of CKD. Check urine microalbumin yearly. ACE/ARB is HTN and proteinuria, urine Cr >300. Go yearly for dilated eye exam. DM is the #1 cause of blindness in the US.
Nerve damage causes the fat pad on the sole of the foot to move, leaving decreased cushioning which predisposes to diabetic foot ulcers. Foot exam should be every visit if loss of sensation. Should do a foot exam annually. Check the skin, document hammer toe, charcot foot, bunion, pes planus.
Get an Ankle Brachial Index (ABI) if you cannot palpate a pulse. Get Toe Brachial Index (TBI) if ABI is not accurate.
Document presence of diabetic neuropathy. Assess for B12 deficiency, TSH, metals, etc.
Metformin, statin, annual vision screen and urine microalbumin, foot exams, diabetes education.
Sulfonylureas (e.g., glipizide) have no long-term benefits, cause hypoglycemia.
3 notes
·
View notes
Text
How to Perform Basic Life Support (BLS) in an Emergency
Basic Life Support (BLS) is a crucial set of medical procedures used to help individuals experiencing life-threatening emergencies, such as cardiac arrest, respiratory failure, or choking. BLS focuses on maintaining an open airway, ensuring breathing, and supporting circulation through cardiopulmonary resuscitation (CPR). Knowing how to perform BLS can make the difference between life and death in critical situations.
In this comprehensive guide, we will break down the essential steps of performing BLS in an emergency, equipping you with the knowledge and confidence to act effectively.

Understanding the Basics of BLS
BLS is typically performed by first responders, healthcare professionals, and trained individuals. The key components of BLS include:
Assessing the Situation: Ensuring the environment is safe before providing assistance.
Checking for Responsiveness: Determining whether the individual is conscious or unresponsive.
Activating Emergency Services: Calling for medical help as soon as possible.
Performing High-Quality CPR: Providing effective chest compressions and rescue breaths.
Using an Automated External Defibrillator (AED): Applying an AED when available.
Now, let’s go through these steps in detail.
Step 1: Assess the Situation
Before intervening in a medical emergency, it is essential to ensure your own safety. Approach the victim carefully and look around for hasards such as fire, electrical dangers, or traffic. If the scene is unsafe, do not put yourself at risk—call emergency services and wait for professional help.
If the area is safe, proceed to check the individual’s condition.
Step 2: Check for Responsiveness
Gently tap the person on the shoulder and loudly ask, “Are you okay?” If there is no response, the individual is unresponsive and may need immediate medical attention.
For infants, tap the bottom of their foot to check for responsiveness.
Step 3: Activate Emergency Services
If the person is unresponsive, immediately call emergency services or instruct someone nearby to call. In most countries, you can dial 911 (USA), 000 (Australia), or 112 (Europe).
When calling emergency services, provide the following information:
Your location
The nature of the emergency (e.g., unconscious person, not breathing)
Any steps you have taken (e.g., starting CPR, using an AED)
If possible, put the phone on speaker mode so you can continue assisting the person while receiving guidance from the dispatcher.
Step 4: Check for Breathing and Pulse
Look for chest movements to see if the person is breathing.
Listen for breath sounds by placing your ear close to their nose and mouth.
Feel for a pulse on the side of the neck (carotid artery in adults, brachial artery in infants).
If the person is not breathing or has irregular breathing (e.g., gasping), you must start CPR immediately.
Step 5: Perform High-Quality CPR
For Adults and Children:
Positioning: Lay the person on their back on a firm surface.
Hand Placement: Place the heel of one hand in the center of the chest (on the lower half of the sternum). Put your other hand on top and interlock your fingers.
Chest Compressions: Push hard and fast, aiming for a depth of at least 2 inches (5 cm) in adults and about 2 inches in children.
Compression Rate: Perform 100–120 compressions per minute (think of the beat of "Stayin’ Alive" by the Bee Gees).
Allow Full Recoil: Let the chest fully rise between compressions.
For Infants:
Two-Finger Technique: Use two fingers (index and middle) in the center of the chest.
Compression Depth: About 1.5 inches (4 cm).
Compression Rate: Same as adults—100–120 compressions per minute.
**If two rescuers are present, use the “two-thumb encircling technique” for better efficiency.
Rescue Breaths:
After 30 compressions, provide 2 rescue breaths if trained to do so.
Tilt the head back slightly to open the airway.
Pinch the nose shut and give a breath into the mouth until you see the chest rise.
Each breath should last about 1 second.
If breaths do not make the chest rise, reposition the head and try again.
Continue CPR cycles (30:2 ratio) until medical professionals arrive or the person starts breathing.
Step 6: Use an Automated External Defibrillator (AED)
An AED is a portable device that delivers a controlled shock to restore normal heart rhythm. If an AED is available:
Turn it on and follow the voice prompts.
Attach the electrode pads to the person's bare chest as instructed.
Analyse the heart rhythm: The AED will determine if a shock is needed.
Deliver the shock: If advised, ensure no one is touching the person and press the shock button.
Resume CPR immediately after the shock and continue as needed.
Step 7: Post-Resuscitation Care
If the person regains consciousness, place them in the recovery position (lying on their side) to prevent choking. Continue monitoring their breathing and be prepared to resume CPR if necessary until professional help arrives.
Special Considerations
Choking: If the person is choking but still conscious, perform the Heimlich maneuver (abdominal thrusts) for adults and back slaps and chest thrusts for infants.
Drowning Victims: Provide rescue breaths before starting compressions.
Pregnant Women: Perform compressions slightly higher on the chest.
Trauma Cases: If spinal injury is suspected, avoid excessive head tilting.
Conclusion
Knowing how to perform Basic Life Support (BLS) can save lives. Emergencies can occur anywhere, and quick, effective action is crucial. By following the steps outlined above—assessing the situation, calling for help, checking breathing and pulse, performing CPR, and using an AED—you can provide critical assistance until professional help arrives.
Consider taking an accredited BLS certification course to practice these skills in a supervised setting. The more people trained in BLS, the more lives can be saved.
Stay informed, stay prepared, and be ready to act when needed!
0 notes
Text
How to Do a Home Heart Rate Check
What factors influence heart rate?
Numerous variables and factors can affect your heart rate, which is not consistent. These consist of physical activity, stress, drugs, and underlying medical issues. Understanding these factors is essential since they may have an impact on your general health. One dynamic metric that can fluctuate during the day is your heart rate. A number of things can affect it:
Work out
One of the strongest heart rate stimulants is physical activity. Your heart rate rises during activity in order to provide your muscles more oxygen and nourishment.
Anxiety and Stress
Your heart rate may increase as a result of psychological and emotional causes including stress and anxiety. Your heart rate rises in reaction to the “fight or flight” response, which primes your body for action.
Drugs
Your heart rate may be impacted by some drugs, such as stimulants or drugs that affect the cardiovascular system. Knowing the possible negative effects of any medications you’re taking is crucial. underlying medical conditions: Abnormal heart rates can result from medical diseases such as thyroid abnormalities, arrhythmias, or hypertension. To keep a healthy heart rate, these conditions must be managed.
How to Measure Your Heart Rate
We’d like to introduce you to Asto Labs, a dependable and accurate heart rate monitoring system that helps streamline this process, before getting into the exact techniques for taking your heart rate. You can easily monitor your heart rate using Asto Labs’ sophisticated capabilities.
The radial pulse
Taking your radial pulse is one of the main ways to determine your heart rate. This method involves feeling the pulse in your wrist. It’s an easy and practical approach to keep an eye on your heart rate. Understanding how to measure your radial pulse and its significance can help you stay in tune with your cardiovascular health.
To measure your radial pulse:
Sit down and rest for a few minutes to establish a baseline. Locate the radial artery on your wrist by feeling for the pulse on the thumb side of your wrist, just below the base of your thumb. Use your index and middle fingers to gently press down on the artery. In 60 seconds, count how many beats you feel. This is your heart rate. The radial pulse is a reliable way to monitor your heart rate, and it’s a technique that’s easy to perform regularly. Keep in mind that it’s best to measure your radial pulse when you’re at rest.
Carotid pulse
Checking your heart rate through the carotid pulse, located in your neck, is another valuable technique. We’ll detail the process for you and explain its importance. Knowing how to measure your carotid pulse is especially useful in situations where you need a quick and accurate assessment of your heart rate.
To measure your carotid pulse:
Sit down and rest for a few minutes. Locate your carotid artery by gently pressing your fingers on the side of your neck, just below your jawline. In a minute, count how many beats you feel. This is your heart rate. The carotid pulse is often used in emergency situations or when a quick assessment of heart rate is needed. Remember to be gentle when pressing on your carotid artery to avoid discomfort.
Pedal and brachial pulse
In addition to the radial and carotid pulses, you can also measure your heart rate using the pedal and brachial pulses. These methods offer alternative locations for assessing your heart rate, and we’ll cover how to perform these measurements and discuss their relevance.
Measuring the Pedal Pulse:
Take a few minutes to sit or lie down to relax.. To locate the pedal pulse, you’ll need to feel the top of your foot, just below your ankle bone. Gently press your fingers to this area. Count the beats for 60 seconds to determine your heart rate. ind a comfortable seated position. The brachial pulse is located inside your upper arm, near your bicep muscle. Use your fingers to apply gentle pressure and count the number of beats in 60 seconds. These alternative methods can be particularly helpful for individuals with wrist or neck issues that may affect the accuracy of radial or carotid pulse measurements. Knowing how to check your heart rate using different pulse points provides you with flexibility and reliability.
0 notes
Text
From Symptoms to Solutions: Navigating Peripheral Artery Disease

Peripheral Artery Disease (PAD) is a common but often overlooked condition that affects millions of people worldwide. It occurs when arteries in the legs become narrowed or blocked, reducing blood flow. If left untreated, this could cause major issues. Understanding the symptoms, diagnosis, and treatment options for PAD is essential for anyone concerned about their vascular health.
What is Peripheral Artery Disease?
PAD is a circulatory problem where narrowed arteries reduce blood flow to the limbs, most often the legs. The primary cause of PAD is atherosclerosis, where fatty deposits (plaque) build up in the artery walls. This narrowing can lead to serious health issues, including heart attack and stroke. Risk factors include age, smoking, diabetes, high blood pressure, and high cholesterol levels. People over 50, especially those with these risk factors, should be particularly aware of PAD.
Recognizing the Symptoms
Knowing the symptoms of PAD is crucial for early detection and treatment. Common symptoms include:
Leg Pain or Cramping: Many people experience pain, cramping, or heaviness in the legs or buttocks during physical activities, such as walking or climbing stairs. This condition is known as intermittent claudication and usually eases with rest.
Weak or Absent Pulses: You may notice weak or absent pulses in your legs or feet, indicating poor blood flow.
Numbness or Weakness: Some people may have weakness or numbness in their legs, which makes walking challenging.
Coldness in the Lower Leg or Foot: If one leg or foot feels colder than the other, it could be a sign of reduced blood flow.
Color Changes: Legs or feet may appear pale, bluish, or have a shiny appearance, indicating circulation issues.
If you notice any of these symptoms, it’s essential to consult a peripheral artery disease specialist for a proper evaluation.
Diagnosis of PAD
PAD diagnosis requires a few stages. An extensive medical history and physical examination are the first steps a healthcare professional will take. In addition to evaluating your general health, they might check the pulse in your legs and feet.
The ankle-brachial index (ABI) test is a frequently used diagnostic tool for PAD. The blood pressure in your arm and ankle are compared during this test. Your ankle pressure may be lower than your arm pressure, which could be a sign of PAD. Further testing, including angiography or ultrasounds, can help see how blood flows through your arteries and spot obstructions.
For those in the Vasai area, seeking diagnosis at the best diagnostic center in Vasai can ensure accurate results and prompt referrals to specialists.
Treatment Options
If diagnosed with PAD, there are various treatment options available to improve your symptoms and overall health. Here are some common approaches:
1. Lifestyle Modifications
Making healthy lifestyle changes is often the first step in managing PAD. Here are some tips:
Healthy Diet: Eating a balanced diet low in saturated fats and high in fruits, vegetables, whole grains, and lean proteins can help lower cholesterol and improve overall health.
Regular Exercise: Engaging in regular physical activity is crucial for managing PAD. Walking, swimming, and cycling can improve circulation and reduce symptoms. A healthcare provider may recommend a supervised exercise program to help you start.
Smoking Cessation: One of the best strategies to enhance your vascular health is to give up smoking. Smoking raises the risk of problems and destroys blood vessels.
2. Medications
In addition to lifestyle changes, your doctor may prescribe medications to help manage PAD. Common medications include:
Blood Thinners: These medications help prevent blood clots, improving blood flow.
Cholesterol-Lowering Drugs: Statins and other cholesterol-lowering medications can help reduce plaque buildup in the arteries.
Medications to Improve Symptoms: Certain medications may be prescribed to help alleviate pain and improve walking distance.
3. Surgical Interventions
If lifestyle changes and medications are not sufficient, surgical options may be considered. These include:
Angioplasty: a process that involves inserting a tiny balloon into the constricted artery and inflating it to make it wider. To maintain the artery open, a stent — a tiny mesh tube — may occasionally be inserted.
Bypass Surgery: In more serious situations, bypass surgery can be required. This entails utilizing a vein or synthetic material to create a new channel for blood to flow around the clogged artery.
For patients seeking specialized care, visiting a peripheral artery disease specialist at facilities like Midas Care Clinic can provide tailored treatment options and expert guidance.
Living with PAD
Managing life with PAD involves regular follow-ups with your healthcare provider. It’s essential to monitor your symptoms and make adjustments to your treatment plan as needed. Staying active, following a heart-healthy diet, and keeping a positive attitude can significantly improve your quality of life.
Conclusion
Peripheral Artery Disease is a serious condition that affects many people, but it doesn’t have to control your life. By recognizing the symptoms early and seeking proper diagnosis and treatment, you can manage PAD effectively. Remember, awareness and proactive measures are your best allies in navigating this condition. If you suspect you have PAD, don’t hesitate to reach out to a healthcare professional or visit the best diagnostic center in Vasai for evaluation. A healthier tomorrow can result from actions taken now.
0 notes
Text

Authored by Java Barker. 4.11.24.
Before CPR make sure that:
The victim and you are safe and you know your location. If the victim is an adult, call 911 before CPR. If the victim is a child/infant, initiate CPR and perform 5 reps of 30 compressions with 2 rescue breaths or 2 minutes of CPR, then call 911.
The following condition warrants immediate CPR:
Victim is Unconscious.
Victim is not Breathing.
Victim has No Pulse.
If one or more of these symptoms is present, perform CPR as soon as possible.
Timeline for brain death/permanent damage after the heart has stopped beating:
0 to 4 minutes after exhibiting symptoms. Chances of Brain Damage Minimal.
4 to 6 minutes after exhibiting symptoms. Chances of Brain Damage Possible.
6 to 10 minutes after exhibiting symptoms. Chances of Brain Damage Likely.
Greater than 10 minutes. Chances of Brain Death Likely
CPR:
C-Compressions, after checking for pulse via carotid artery or brachial artery for infant, perform 30 compressions, interrupted by two mouth to mouth breaths, one second each; repeat until emergency services arrive
A-Airway, Clear the airway and check for any obstructions;
B-Breathing, perform 2 rescue breaths 1 second each;
Recommended position for performing CPR is to have victim lying flat on his back
Recommended rate for effective compressions for adult/child is 100 to 120 compressions per minute
When performing compressions, make sure the chest returns to its original position
When performing adult CPR the depth of the compressions should be at least 2 inches deep (but not greater than 2.4 inches)
When performing child CPR, make sure your compressions are 1/3 of the depth of the chest or 2 inches deep
When performing infant CPR, make sure your compressions are 1/3 of the depth of the chest or 1 1/2 inches deep
For a child, depending on the size, you can use one or two hands
For an infant, use two fingers
If not comfortable performing mouth to mouth, call 911, but at least administer external chest compressions until help arrives. Note, conventional CPR is still advised for pediatric victims.
Key points, if performing Chest Compressions ONLY:
Chest compressions should be performed at a rate of 100 to 120 per minute
Increase the depth of chest compressions to 2 inches (but not greater than 2.4 inches) for adults/children and 1.5 inches for infants
Continue with chest compressions for as long as possible or until help arrives
There has been a change in the recommended sequence for the lone rescuer to initiate chest compressions before giving rescue breaths (C-A-B rather than A-B-C).
Before proceeding with General CPR:
Assess the environment to make sure you and the victim are not in danger
Make sure you are aware of your location to help emergency responders locate you
Assess the surroundings for anyone who can help
Avoid moving the victim unless there is an immediate danger to you or the victim
Determine if the victim is conscious or unconscious by positioning yourself next to the victim, tapping him/her on the shoulder and shouting "Are you OK? Are you Ok?"
Assess for no breathing or only gasping and check pulse. This should be performed simultaneously in less than 10 seconds.
Immediately ask someone to call 911 and then have the person report back to you. If no one is available, call 911 yourself prior to beginning CPR and leave the phone next to the victim.
To perform CPR, remember the basic steps of CPR administration called CAB. C for compressions, A for airway, and B for breathing.
The proper ratio is 30 chest compressions to 2 rescue breaths. Keep interruptions to less than 10 seconds. Continue administering compressions at a rate of 100-120/min with 2 rescue breaths until emergency services arrive.
Infant CPR (younger than 1 year)
The steps for performing CPR for infant are slightly different to adult and child.
Difference 1: Administration of CPR prior calling 911. Perform 5 reps of 30 compressions with 2 rescue breaths in between. Once done, then call 911.

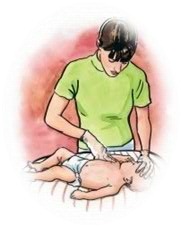
Difference 4: Chest Compressions. When performing compressions, place 2 fingers on the breastbone (see video for more detail) -- just below the nipples and make sure not to press at the very end of the breastbone. Keep your other hand on the infant's forehead, keeping the head tilted back.
Difference 5: Depth of Compressions. Press down on the infant's chest so that it compresses about 1/3 of the depth of the chest, about 1 1/2 inches.
Before proceeding with Infant CPR:
Assess the environment to make sure you and the victim are not in danger
Make sure you are aware of your location to help emergency responders locate you
Assess the surroundings for anyone who can help
Avoid moving the victim unless there is an immediate danger to you or the victim
Determine if the victim is conscious or unconscious by positioning yourself next to the infant, and determine if the infant is responsive by tapping/flicking the victim on the foot several times.
Assess for no breathing or only gasping and check pulse. This should be performed simultaneously in less than 10 seconds.
If unconscious and help is available, immediately ask someone to call 911 and report back to you. If alone, (Difference 1) initiate CPR and perform 5 reps of 30 compressions with 2 rescue breaths in between, then call 911. Leave the phone next to the victim.
.XO-JB.
0 notes
Text
Aditi Jagtap Pune : Why Can You Feel Your Pulse In Your Stomach

According to Dr Ranjit Jagtap News, feeling pulse rate in some parts of the body is considered completely normal, how in this blog we are going to uncover. It’s completely normal to feel a pulse in certain parts of your body other than the chest area. To check through pulse rate, doctors sometimes press the stomach area. Pulse rate in general terms measures heart rate, with the total number of times your heart pounds per minute. When enthusiasm in your heart pumps, arteries in your body expands and contract calmly. That’s the pulse. Pulse in general terms, determines heart rate, or the number of times a heart beats in a minute.
When professionals like Dr Ranjit Jagtap check your pulse rate, they check the strength and rhythmic beat of your heart which reveals whether the blood is hard or soft. Pulse points are the spot, where one can detect pulse, Certainly, there are some numbers of pulse point present in the body, few of them includes,
Temporal Artery: On temple in front of ear
Carotid Artery: On one side of your neck
Brachial Artery: On the upper arm, closer to elbow
Radial And Ulnar Artery: On the wrist
Femoral Artery: Located in the inner thigh
Popliteal Artery: On the top of the knee, can be seen once the knee is bent
Dorsalis pedis Artery: On top of the foot
Posterior Tibial Artery: Placed in the middle of an ankle.
One can feel a pulse point on these spots, an artery runs way closer to the skin, way below the hardest structure. This is the reason why a pulse is taken either on the wrist or on the neck.
So, how will you check the pulse?
According to Dr Ranjit Jagtap Daughter, If you’ve never done a test before, it’s very easy to track your own pulse. Aditi Jagtap Pune sharesBelow mentioned are the three steps to check the carotid pulse.
> Step number one, use your index and middle finger to press soft groove gently, on either side of the neck, closest to the windpipe.
> Step two, Use a watch or stopwatch, to count the total number of beats you feel in 30 seconds.
> Add the number.
For a healthier adult, normal beat count is between 60 to 100 per minute. Your pulse must feel steady with a constant gap between the beats. If your heart feels an extra beat or a beat is skipped, that’s common and harmless. Talk to the doctor about potential irregularity.
How One May Feel Heartbeat In Stomach
It’s common to feel a pulse in your stomach. What you’re picking up on is a pulse present in your stomach. Aorta is the most essential artery which carries blood, from heart to other body parts, It normal to carry the pulse rate,
Out of three section in the day, you can feel pulse rate in the stomach,
Within the course of during/eating
While lying down
During pregnancy
When you start munching, your heart pumps extra blood to the stomach and small intestines. It helps in digesting food and absorbing nutrients. This temporary surge can build a profound pulse in your heart.
Once you lie down you can feel the pulse rate, and raise the knee. And say, if you don’t have an abdominal pulse rate, you may also spot a stomach pulse.
The amount of blood flowing in the body increases, during the time of pregnancy. Increased amount of blood is pumped with increased heartbeat, making pulse more noticeable.
Dr ranjit jagtap daughter, shares In very few cases, picking pulse in your stomach could be a signal of something serious. Always give attention, if you get sudden symptoms, involving pain in the abdomen either on side or back. This becomes extremely important when you carry a:
A Blood Vessel Disease
Higher Blood Pressure
A History of Aortic Infection
A family history of abdominal aortic aneurysm
Recent Traumatic Injury
Conclusion:
At Dr Ranjit Jagtap clinic, heart patients or anyone looking for a heart checkup, can pay a visit, and get medication, treatments, or diagnostic profiles accordingly. For the past 50 years, the specialist has treated patients on a global scale. Ranjit Jagtap Clinic, have collectively contributed towards cardiac care setup in Pune. Professional has performed more than 30,000 heart operations till the end date.
#aditi jagtap pune#dr ranjit jagtap#dr ranjit jagtap daughter#dr. ranjit jagtap news#dr. ranjit jagtap clinic
0 notes
Text
5 Fundamentals Of CPR Training As Well As Certification

CPR is actually a crucial life-saving skill that can create a substantial difference in emergencies. Whether you're a health care expert, a first -responder, or an anxious citizen, Ottawa first aid cpr training as well as license outfit you with the understanding as well as peace of mind to act quickly as well as successfully during the course of important scenarios.
5 Crucial Fundamentals Of Cardiopulmonary Resuscitation Training And Also Certification
Knowing CPR's Function
Cardiopulmonary resuscitation is actually performed to maintain blood stream flow and oxygenation in people experiencing cardiac arrest. In the course of heart attack, the heart quits pumping blood successfully, causing a shortage of air source to crucial body organs, consisting of the brain. CPR intends to bring back blood stream circulation and oxygenation to these body organs until advanced clinical help gets here.
Mastering Compression Strategies
Central to CPR is breast compressions, which aid mimic the heart's pumping action. Effective compression procedure entails placing the heel of one hand on the center of the prey's trunk (generally in between the nipples) and interlocking the various other possession on leading. The rescuer should at that point position their shoulders straight over their hands and also do squeezings to a deepness of at least 2 ins for adults as well as adolescents, and also regarding 1.5 ins for infants as well as children. Squeezings ought to be actually conducted at a rate of 100 to 120 compressions per moment, permitting comprehensive trunk recoil between compressions to make certain ample blood circulation.
Mastering Rescue Breathing
Aside from chest squeezings, CPR involves providing saving breathing spells to the prey to provide oxygen to their lungs. For adults as well as adolescents, saviors conduct mouth-to-mouth breathing, securing the victim's nostrils with their palm and also giving 2 breaths right into the victim's oral cavity, enjoying for chest growth. For little ones as well as youngsters, the mouth-to-mouth method is actually slightly tweaked, with the savior covering both the sufferer's mouth as well as nostrils with their mouth as well as supplying gentle breaths ideal for the target's dimension. It is actually important to preserve an accessible air passage as well as make sure appropriate ventilation during the course of rescue breathings.
Recognizing the Signs of Cardiac Arrest
Motivate identification of cardiac arrest is necessary for starting Ottawa first aid cpr training successfully. Common indicators of heart attack consist of the abrupt reduction of responsiveness, absence of breathing, as well as no pulse. Saviors need to immediately evaluate the victim's cooperation by touching and yelling, checking out for typical breathing, and also emotion for a pulse on the carotid artery for grownups as well as youngsters or the brachial vein for little ones and children. If the sufferer is actually unresponsive, certainly not taking a breath commonly, and has no rhythm, CPR must be actually started promptly. If you prefer to learn further information on cpr, you have to sneak a peek at www.ottawafirstaidcpr.ca website.
Seeking Certification and Regular Training
While any person may discover CPR rudiments, formal license gives thorough instruction as well as examination of capabilities. CPR license training programs, used through institutions such as the American Heart Association (AHA) and the Red Cross, cover a variation of topics, consisting of essential life assistance (BLS), automated exterior defibrillator (AED) use, as well as strangling alleviation. Accreditation commonly includes a mix of on the internet knowing elements, hands-on skills technique, as well as a last analysis. It's vital to restore CPR accreditation on a regular basis, commonly every one to pair of years, to ensure that abilities continue to be up-to-date and reliable.
In final thought, CPR instruction as well as certification are invaluable resources for anyone looking for to be gotten ready for emergencies. Through knowing the objective of CPR, grasping compression as well as breathing strategies, acknowledging indications of heart apprehension, as well as seeking official license and regular instruction, individuals can with confidence react to heart emergencies as well as likely spare lives. In a realm where every 2nd matters, being actually geared up with CPR skills can easily produce all the difference in an individual's opportunity of survival.
Ottawa First Aid CPR
1061 Merivale Rd Unit#204, Ottawa, ON K1Z 6A9
613-682-0142
0 notes
Text
youtube
डायबिटीज ( Diabetes ) से होता है Leg Attack जानिए कैसे?
Diabetic Foot Need Professional Care
Hello friends, I am Dr. Virendra Sheorain, a #vascularspecialist . Today we will discuss diabetic foot and #diabeticulcer also referred as wound in the foot. So, this video is for those patients whose feet, fingers, and toes have #wounds and these wounds are not healed by any medicine or dressing. What should they do?
This #disease is known as "#diabeticfoot " in layman's terms, and it is not necessary that it will affect only diabetes patients. It can affect patients who are heavy smokers, #patients who have diabetes from smoking, or patients who have simple #diabetes with uncontrolled blood sugar levels. What happens is that people who have had diabetes for a long time or who smoke begin to notice changes in their arteries. With time, these arteries get blocked, and just like blockage of the arteries of the heart can cause a heart attack, blockage of the brain's arteries can cause a brain attack. Similarly, a blockage of the leg arteries can result in a leg attack. After these attacks, wounds start to develop.
We get patients from various economic strata: villages, cities, high class, low class economically, and there are different reasons for these wounds' development. Some patients say that I went to a wedding and a shoe bite caused the wound, but they fail to understand that it is caused by blockage of arteries. I am telling you this so that when you see or hear this kind of wound information from your surrounding people, you can suggest that they visit a peripheral vascular surgeon instead of a cardiologist or thoracic surgeon, as this is a very common mistake.
Its diagnosis is very simple. The #doctors has to just check for the pulse in the leg to see if it is normal or not. If there is a slight doubt, then it is better to send the patient to a good radiologist or nearby radiologist for a color Doppler. If the test shows that your arteries have less blood flow or a deviation from their normal pattern, that means your arteries have problems.
For these wounds in the leg, no matter what medicine you apply, it won’t help, and this wound will keep spreading to other parts of the leg, and one day you will lose your leg. Some people initially lose their heels and toes, and later their legs need to be amputated below the knee. So now, let me tell you about the treatment of this wound. When you visit a vascular surgeon, they perform some basic tests like an arterial doppler and an ankle-brachial index (ABI). These are basic tests, and you don’t have to know details for them. But the surgeon who is performing these tests gets to know the condition of your arteries and can then advise you on the treatment of the disease.
In today's world, the #treatment is very simple. Earlier, there used to be big bypasses, big incisions, artificial veins, or even grafts that had a high chance of infection failure. Now we have hybrid operating rooms in every big hospital. An angiography machine is installed in every hybrid operating theater. Your closed veins are opened by modern technology through angiography, angioplasty, or stenting, just like the heart, your legs are also treated. A hybrid bypass can be done if needed with the help of a small incision. How can it be avoided? Well, if you keep your diabetes under control, stop smoking, and take the medicines given to you by your doctor honestly and on time.
So if you still have any related questions, many patients ask us: "once the artery is treated, how many days will it last?" I have to say that the arteries that we open last for a long time if you take the medicine regularly, quit smoking, and keep diabetes under control.
Still, if you have any questions related to diabetes foot, or not able to understand anything related to it, or have someone in your neighborhood with diabetic foot, please message us at the below-described website link or WhatsApp number. You can consult us; we will be very happy to help you out and give you a second opinion. I will be glad. Thank you.
1 note
·
View note
Note
Hey, I have a question prompted by a fic I'm working on. How would a (medically trained and unwell) character check (or rather, get an idea of) their blood-pressure when they don't have any access to instruments? My understanding (which is very patchy) is that you can get a sense of blood-pressure when taking the radial pulse, but I don't know if that's correct or reliable, or if there are other ways. Thanks for everything you do!
If your character is afraid their blood pressure is particularly low, they can take their pulses. Typically as long as the systolic (top number) is 90 and the diastolic (bottom number) is above 30, blood is getting to the brain. You can get a decent idea of whether or not blood is getting to the brain with which pulses are still intact.
There are more pulses than just the radial (wrist) pulse. You can get a pulse on top of the foot (dorsalis pedis), the inside of the ankle (posterior tibial), on the back of the knee (popletel), the groin (inguinal), the inside of the upper arm (brachial), the neck (carotid), and over the heart (apical, or point of maximal impulse/PMI).
As blood pressure drops to inadequately low levels, pulses start to disappear at the furthest points of the body. As long as you have the radial (wrist) pulse, you know the top number is at least 90, and that enough blood is getting to the brain.
Conditions where BP might get too low include injuries that cause blood loss to the point where the body can no longer compensate, and really anything else that could cause shock (severe allergic reaction, life threatening infection, life threatening dehydration, etc...).
Now, obviously this would not work if they were afraid their blood pressure was too high. However, if they have a blood pressure cuff, they can get a good idea of what their systolic (top number) blood pressure is by doing the following:
Place the cuff around the top of their arm.
Find the radial pulse
Pump the cuff up while feeling for the radial pulse to disappear.
The point at which the pulse disappears is the systolic blood pressure, which will give them a good idea of if their blood pressure is so high they need to go to an emergency department (pretty much anything over 180/x would be dangerously high).
Now, in an emergency where the patient did not already have a condition they knew about where their blood pressure went high, really the only reason their BP would go that high is if they had been poisoned with a stimulant or had a head injury that was causing an increase in pressure inside the head (the body increases BP to be able to force blood into the brain in this case, but there are usually symptoms way before this).
28 notes
·
View notes
Note
Once again, I'm filling your inbox with my dumb requests... I can't stop thinking of Nurse!Kylo inspecting me with a whole array of medical equipment while I'm drugged and groggy and strapped to a hospital bed 🥵
So I’m gonna do some thots instead of a one shot (:
Tags: is this crackfic? maybe a little. medical terminology which makes me laugh. his scrubs are obvs black, duh. finger sucking. blatant malpractice (why is this a theme of mine?). i skipped popliteal pulses bc to me they do not exist (:
You’d wake up from your procedure in the post-anesthesia care unit. Your surgery was the last of the day so you knew you’d be alone in the open room.
There would be a few flashes of memory before you were at least half awake, remembering the face of the most handsome nurse you’d ever laid eyes on, a face that warmed your cheeks.
You’d panic when nobody was there, alone in this too-bright, freezing room.
Nurse Ren would come into view on a swivel stool, rolling up to your side, assuring you everything is fine, looking at you with a wicked glint behind his eyes.
He’d bring you a warm blanket and you’d relax back into bed.
Although you could hear the beeps of the monitors connected to you via 5 leeds the pre-op nurse had placed, he would still insist on checking your heart rhythm himself, explaining with a wink that he wants to be “extra thorough” for his favorite patient.
When he was leaning over you, lifting your surgical gown, you’d sink into the heat falling from his body to yours, an unbidden throb coming to your core.
He smelled so good, but fresh, not like cologne. A lock of his hair would brush your face when he was listening to your apical pulse rate.
He’d stay close but turn to face you while his hand was still under your gown, he’d smirk and say “don’t be nervous, I feel it too.”
This would bring your eyes to blink rapidly and your pulse to heighten further, the monitors beeping incessantly now.
Keeping your stare he would gather the stethoscope in one hand, you’d notice the prominent veins, and keep one on your chest, finger tips now just barely grazing the sensitive flesh.
As you hadn’t expected this, his touch would cause your thighs to clamp together, the sudden movement catching on your gown and cluing him further into how turned on you are.
His face would twitch in such a way to signal how purposeful this all was.
In your sleepy state he’d take his hand, and it’s accompanied gloved warmth, from you. This would bring a shiver.
He’d whip out a pen light and ask you to stare at his eyes as he examined your response, checking for PERRLA. His eyes were so beautiful, lust striking you again, suddenly your dry mouth becoming extremely obvious.
He’d go to examine your oral mucosa, placing two long, heavy, demanding fingers over your tongue. At this point you begin to feel slick collecting on your thighs.
Maybe a little too brave, you’d close your lips around his fingers and suck on the purple nitrile gloves, watching his lips part.
Nurse Ren would pull them away and move to sit with you in the bed, his hips next to yours.
He’d floor you with a darkened gaze and say “I’m checking your pulses now.”
First he’d place one large hand over your neck, feeling both your carotids at the same time, pressing down harder than necessary and earning a head rush.
Keeping your stare he’d trace both hands parallel down your arms and grasp your elbows, feeling your brachial arteries, then down to your wrists.
Here he would let your hands fall into his, the sight dizzying seeing the contrast of your from his.
He stands again and walks to your feet, feeling first your pedal pulses.
That same darkness still resides in him as he leads gloved hands up both your legs, the blanket and gown collecting over his forearms.
He’d crawl into bed with you, hands searching blindly for your femoral pulses, his fingers leaving your breathless while he pressed into the pliant area.
“Just one more, then I’ll leave to document my assessment”
Even groggily you knew his intentions, hips half bucking while your legs spread to allow him better... access.
He hasn’t dropped your gaze this whole time, seeing every fluctuating in your features he’s earned.
A thumb trails over your mound and dips into your slit, first just barely grazing over your clit and drawing a stifled moan from parted, parched lips.
Another smirk would light, pressure applying further as he passes over the electric flesh.
Another buck into his hand and he’d chuckle under his breath, a killer smile forming in his features.
He’d remove his hand, his touch, and cover you back up, crawl off your bed, and leave you wanting.
“You should be out of here soon. Let me know if you.... need anything.”
#kylo ren#thots#kylo ren imagine#kylo ren x reader#crackfic#dr. rockhard has been summoned#kylo ren x you#ask#clumsycopy#nurse!kylo
59 notes
·
View notes
Note
hmmmm prompt 11 “heartbeat” for 4mg Ativan maybe ? <3
CW: dermatillomania, anxiety attacks, self injury stims
This is short idk how I feel about it but <3
***
There are many places one should be able to feel their own pulse normally, Ava knows them all by heart. Carotid pulses are the strongest, a heavy pressure against the jugular that is the go to for checking someone’s heart rate. Radial pulse is next, easy to feel if you slip your first two fingers down the inside of your opposite wrist. Pedal pulse isn’t as common, most instances only call for this when checking for blood flow to lower extremities. Still, Ava knew if she pressed two fingers to the top of her foot she would be able to feel her heartbeat through that artery. Brachial pulse is only used for young children, it's much harder to check the pulse on an adult from their inner elbow. Of course if one tried they would eventually be able to feel the rhythmic beating of their heart in that spot as well. Not to mention the five different areas on the chest to place a stethoscope, all areas where the different frequencies sound the loudest. Aortic, pulmonic, ERB’s, tricuspid, mitral.
Doctor Bekker knew all these by heart, could calculate her own heart rate or anyone else’s in approximately twenty seconds. It was second nature to her, yet sometimes her anxiety overtook the logical part of her brain and all of that knowledge was forgotten. When she was anxious Ava could feel her heart everywhere, even though she knew it wasn’t how things worked anatomically, it was everywhere in those moments.
Her heart pounding in her ears when she woke up from a nightmare, tears streaming down her cheeks before she was even awake enough to realize she was sobbing. Unable to hear Sarah over her racing heart and the horrible thoughts flooding her mind. It surrounded her in that moment, too distracting for Ava to notice when Sarah wrapped her in a gentle embrace and tried to calm her down.
The times where she couldn’t lay down because she felt her heartbeat radiating through her back, amplified as if it only made the pulse echo through her body. These moments were the worst because they usually occurred alongside the sensation of bugs everywhere. It was those times where Ava would sit on the floor in the bathroom and cry, exhausted but unable to sleep. Her dermatillomania and anxiety fighting within her brain, heart feeling like it was about to burst through her ribcage through her back. Even if that wasn’t possible, in those moments it was all Ava could feel.
When her anxiety was bad Ava could only feel her heart. Even when her hands were numb from scrubbing them raw because they didn’t feel clean, when her feet had fallen asleep, and her arms should be aching from the way her nails dug into the skin. Her eyes should hurt after crying for hours and her head must be pounding from when she had a meltdown and hit herself repeatedly. All of those sensations didn’t even register in the moment, the only feeling she could recognize was the haunting feeling of her heart everywhere.
Ava had dedicated her career to hearts, amazed by their mechanics and enjoying fixing them. She had spent her whole university experience fixated on the organ, knowing its functions by heart and able to dissect and repair one by memory. She loved hearts, she did, but there were times when all Ava wanted was for her own to stop. Not because she wanted to die, not at all; she just wanted to be able to feel something — anything — else.
12 notes
·
View notes
Text
it’s hard to breathe sometimes
AO3 Link
A/N: for @buckleystrand for this post :D hope you enjoy!
Eddie’s in the middle of drafting a petition letter to the city to ban gas stoves from homes in his head when it all goes to shit.
They had been on hour twenty of a twenty-four-hour shift that had been steady but uneventful when the alarm went off. It was just after four in the morning and apparently someone hadn’t turned the gas for their stove off all the way. One thing leads to another, hot burner catches dishtowel on fire, owner’s out on a morning jog—boom. House fire.
The team had the flames mostly under control in terms of not spreading to other houses nearby, but inside was a whole other story. The gas line had only just been shut off when Eddie and Buck were sent inside, so whatever lingering gas was still in the pipes only added fuel to the literal fire. It would likely be under control soon, since there wouldn’t be anymore gas adding to the issue, but it was still risky.
Buck and Eddie were only in here because the homeowner wasn’t sure if her daughter had left for work yet. She took the bus according to the mother, so checking the garage was pointless, and was not answering her phone.
Poking his head into the last room on his side of the second floor, Eddie peered through the smoky haze and called out.
“LAFD, anybody in here?”
No response, nobody on the floor, under or in the bed, or in the closet.
Ducking from the room, Eddie made for the stairs, nearly colliding with Buck as they met up.
“Find anything?” Buck called over the roaring flames and groaning framework.
“Nobody,” Eddie confirmed. “You?”
“Empty as far as I found.”
Eddie is about to suggest they check the kitchen and living room one more time when their radios crackle simultaneously. Bobby’s voice filters through a second later.
“Buckley, Diaz, we got a response from the daughter. She’s at work already. Get out of there and we’ll get this fire put out and wrap up.”
“Copy that, Cap,” Eddie responds for them both. “On our way.”
He sends Buck down the stairs ahead of him, far more content to have eyes on his impulsive partner. The steps creak with ominous protest under their weight, and Eddie can feel his heart like a lump in his throat as his heartbeat thunders in his ears. What if the steps give out? Will he be able to push Buck to safety before they both go down? What if the stairs give out under Buck first? Will he be able to grab Buck in time?
He finds something new to fret about with every step they take down until they’re only three or four steps from the bottom. Eddie glances to his right on instinct, knowing that the kitchen is just down a short hallway—the heart of the inferno.
Buck gets to the bottom of the stairs and steps to one side to make sure Eddie gets down too.
Eddie gets to the bottom of the stairs. He looks to Buck and finds a familiar grin through the haze.
The stairs creak ominously, the wall chimes in. The ceiling roars its way into the melody as the trapped heat engulfs the drywall.
The next few seconds are a blur Eddie will never be able to untangle. He thinks Buck screams his name; he definitely sees the first moment of the rafters breaking through the ceiling. Then it’s just wood and flame, heat and jarring impact.
Everything spins for a moment, there’s roaring all around him. Bobby’s voice is a static, garbled alarm near Eddie’s ear.
Buck lies beside him on the ground. There’s something flashing on Buck’s turnout coat, a red light. Eddie knows it’s important, but he’s struggling to remember why.
God…it’s burning in here.
Everything snaps back into place with a sudden clarity that leaves Eddie dizzy. He sucks in a strangled breath and scrambles to his feet. That light is Buck’s oxygen indicator, and the red means it’s compromised. A quick glance of the situation gives Eddie everything he needs to know, and his heart rapidly descends from his throat to his stomach.
The beams in the ceiling had given way under the heat of the flare, and probably would have come down on top of them both if Buck hadn’t shoved them out of the way. But by putting himself between the falling debris and Eddie, it looks like one of the heavier beams caught Buck’s tank of oxygen.
Thankfully, Buck doesn’t seem pinned. Eddie isn’t sure if Buck himself got struck by anything, but he doesn’t have time to make that assessment here. With practiced ease, Eddie tamps down on every single emotion trying to rear its head and hauls Buck over his shoulders.
They exit the burning structure just as Bobby seems to instruct Chimney to head in after them.
“Cap!” Hen calls, rushing to meet them.
The team is on Eddie and Buck in seconds. Chimney and Bobby had the forethought to bring a gurney, so Hen helps Eddie deposit Buck as carefully as possible onto it. Hen tugs Buck’s helmet off the firefighter’s head and passes it off to Bobby. Chimney secures a c-collar around Buck’s neck seconds later. Hen’s already giving rapid-fire instructions to Chimney to grab an oxygen mask as she works Buck’s ruined tank off his back.
“Hen, take Eddie in the ambulance with you,” Bobby interrupts, face set in a neutral expression. They all know him better, though; know how worried he is. “He needs to get checked out, too. Contact me when you get there and I’ll meet you later.”
Bobby claps a hand down on Eddie’s shoulder as Chimney and Hen rush Buck’s gurney towards the waiting ambulance. The Captain gives Eddie a significant look before letting him limp after the rest of the team.
Chimney swings himself into the driver’s seat as Hen flits around the back over Buck. By the time Eddie climbs in and shuts the doors behind him, she’s already got an oxygen mask fitted over Buck’s face and is prepping other materials. She glances up at Eddie and gestures to the bench.
“Get your turnout gear off, okay? I need to check you over.”
Eddie’s quick to remove his helmet and oxygen tank, having nearly forgotten both were still on. Shedding his turnout coat and gloves, he glances up in time to watch Hen finish manipulating Buck’s coat away from his chest and arm. She attaches a line and slings the bag up onto a free shelf so she can keep working.
Buck blinks awake less than a minute later as Eddie helps Hen attach the ECG leads to Buck’s chest. He wheezes weakly into the oxygen mask and his eyes loll around in a daze before he blinks into focus.
“Hey there,” Eddie says, managing a grin down at Buck’s tired expression. “Welcome back, Buck. How ya feeling?”
“Smokey,” Buck whispers, sounding like hell. He looks a little pale, and Eddie is about to comment on his pallor when the machine registers the leads and starts giving them a reading. Hen frowns at the machine, and as Eddie scans over the numbers, he does too.
“Your heart rate’s a little high and pressure a little low there, Buckaroo,” Hen murmurs, placing a gloved hand on his shoulder. She looks down at Buck and gives his shoulder a careful squeeze. “Anything feeling off?”
“My arm hurts,” Buck rasps, eyelids drooping.
“Which arm, Buck?” Hen says, already shifting back into action. He manages a weak indication to his right arm, the one without the line in it. Eddie reaches to tap at Buck’s cheek as Hen works at Buck’s turnout coat again to expose his arm.
“Eyes open, Buck,” Eddie says, raising his voice a little. “You know the drill, bud. We’re almost at the hospital, stay awake.”
Chimney’s racing through the near empty streets. There are scarce few cars out with them at just shy of five in the morning and thus eliminating the worry of traffic impeding them. Eddie sends up a quiet thanks to the universe for small mercies.
His thanks are abruptly cut off when Hen curses beside him.
Buck’s right arm is exposed, now she’s got the coat pulled away, and it’s soaked in blood. The dark, loose fabric had hidden the slash and the spreading blood from them until now.
“His brachial artery got nicked, he’s loosing too much blood,” Hen says even as she scrambles to grab a wrap for a tourniquet. “He’s going to need a transfusion when we get to the hospital, we don’t know how long that’s been bleeding. Eddie, can you—”
She’s cut off by the sound of the AED pack alarm.
Eddie looks down at Buck’s face, only to find him pale, still, and his eyes closed.
“We lost the pulse,” Hen says, voice strangled. “Chim, drive faster!”
Eddie throws himself into action as Hen starts aggressively tying off the tourniquet on Buck’s arm. His movements are on autopilot, repetitive hours of CPR classes take over as he fits one hand over the other and positions himself over Buck’s chest. He’s dimly aware of Hen moving away from Buck’s arm and grabbing an Ambu-bag and replacing the oxygen mask with it over Buck’s face.
The ambulance rattles and the sirens wail as Chimney picks up speed.
Eddie counts out his pulses against Buck’s motionless chest and begs the universe he had just been thanking to give Buck back.
He pulls his hands back after thirty and gives a breathless, “check,” to Hen. Eddie’s eyes take in Buck’s slack features, barely hearing Hen’s frantic denial.
Eddie’s back to pushing on Buck’s chest before he even thinks about it, muttering under his breath as he counts in his head. A steady, mindless litany he whispers like liturgy, like it might yield him something other than faith.
“C’mon Buck,” he says. “Come on, man, don’t do this. We need you. I need you, Chris needs you.”
Repeatedly, muttering in time to the thrust of his hands against Buck’s sternum. Eddie feels a rib give way under his fingers and chokes on a sob in the middle of his pleas. But he’s back to his whispers a moment later, a new warble to his tone.
“Still no pulse, get clear,” Hen’s voice cuts through Eddie’s mounting hysteria. She’s pressing shock pads to Buck’s chest with practiced proficiency even before he’s backed away.
“Charging,” Hen calls to the ambulance as Eddie sits back with shaking limbs. “Clear!”
Buck’s torso arches off the gurney as electricity courses through him. The AED takes a moment to read before instructing Hen to shock Buck again. She calls the same cues and Eddie dimly realizes his hands are numb and he’s unable to look away from Buck’s face.
Eddie’s ears are ringing as he watches Buck’s body seize up with the second shock.
They wait as the machine registers.
The AED beeps once, twice.
“We’ve got a pulse!” Hen cries.
The ambulance lurches to a stop and there’s suddenly a flurry of movement as the doors fling open. Noise and scrambling are the prelude, then equipment adjustments made, and then the gurney carrying Buck whisks away. Eddie’s still sitting on the bench in the ambulance, his gear scattered beside him and ears ringing with the sudden silence. The ghostly sensation of Buck’s ribs breaking under Eddie’s hands lingers in his aching knuckles.
“Eddie?” Hen.
“You with us, man?” Chimney.
He thinks they’re on either side of him, coaxing him to his feet so he can sit on the floor with his legs hanging out the back. They’re checking him over, hands careful and methodical. Eddie thinks they give him an all clear, but he’s not sure how much time has passed. He feels stuck in a loop of those few seconds where he realized Buck had slipped away under his hands.
“Eddie,” Hen tries again, but he cuts her off with a hoarse voice.
“He was gone.” Hen and Chimney share a look around him as Eddie continues. “He wasn’t there…and I almost lost him.”
“You know Buck’s a stubborn fighter, Eddie,” Hen murmurs. “He’s back, and they’re not going to let him leave again. None of us will.”
“Buck’s come back from a lot worse, Eddie,” Chimney says with a confidence Eddie wishes he had right now. “Knowing him, he’ll be running around the fire house sooner rather than later.”
Eddie nods numbly, wishing he believed their words as much as they did.
“Let’s head inside, Eds,” Chimney says, he and Hen tugging with careful coaxing at his arms. “We need to call Cap, and we’ll be there for Buck when he wakes up.”
When. Eddie clung to that word. Not if. When.
He glimpses the brightening horizon as they lead him into the waiting room and hopes it’s a good sign.
---------------------------
He’s really starting to hate hospitals. Eddie was never fond of them to begin with, but the amount of times Buck had landed himself in a hospital bed in the past year only amplified that hatred. The machines were redundant, the steady beeping of the heart monitor, the click and whir of the oxygen line, the paced inflation and deflation of the blood pressure cuff, and the ever so subtle drip from the IV were a reliable descant. One Eddie was far too familiar with and all too tired of hearing—like an overplayed pop song on the morning radio.
Bobby had come through about fifteen minutes prior, bearing coffee and a bland hospital breakfast pastry for Eddie. The Captain had taken one look at Buck laid up in the bed and sighed like the world lay upon his shoulders. Eddie could have sworn he watched Bobby age another five years in front of him.
“You kids are going to give me stress ulcers one of these days,” Bobby had said, running his fingers through Buck’s dirty hair.
Eddie hadn’t responded, and it was obvious Bobby hadn’t been expecting an answer.
“Take the day off, Eddie,” Bobby had said, patting Eddie’s shoulder on the way out. “Call us when he wakes up, okay? The rest of us are going in because I couldn’t get anyone to cover on such short notice. But we’ll come running if you need us.”
Eddie thinks he might have managed a strained acknowledgement, but he honestly can’t remember. The coffee cup sits cold in his hand now as he stares at Buck’s sleeping face. The pastry is all but forgotten on the table beside the bed.
Running a hand down his face, Eddie heaves out a heavy breath and reminds himself to call Carla later. She had already been taking Chris to school that morning, but he had called earlier to ask if she wouldn’t mind picking him up, too. Carla—the angel she is—had agreed even before Eddie explained the situation. He needed to keep her updated, along with the team.
“Eddie?”
His head snapped up, eyes wide, heart racing.
Buck’s eyelids were heavy, but they were open. Eddie was out of his chair and on the edge of Buck’s bed in a heartbeat, coffee set aside.
“Hey, Buck,” Eddie said breathlessly.
“What happened?”
“You took a nasty hit when the ceiling came down in that house fire yesterday morning. Doctor said you were unconscious so long because of the blood loss, but it’s good to see you awake, man.”
Buck’s brow furrowed, nodding wearily as he flinched a little, hand drifting towards his chest.
“Ah, shit,” Buck hisses out. “Did I break a rib?”
“I did,” Eddie whispers, fingers aching with the memory. “You flat lined in the ambulance on the way here.”
“Oh,” Buck says after a moment, looking a little lost with the information. “I’m sorry.”
Eddie looks at Buck like he’s grown a second head, and Buck just stares at where his hands are resting on the bed. His fingers pick with idle attention at the tap securing his IV line and Eddie suppresses the urge to slap Buck.
“Did,” Buck looks up as Eddie falters. “Did you just apologize for flat lining?”
Buck doesn’t seem to have an answer, looking a little bewildered by the question.
“Because I’m sure I misheard you,” Eddie continues in lieu of Buck’s silence. “There’s no way you are apologizing for something you had no control over, right? I mean that just makes it seem like you think it was a burden for me to bring you back to life like I wouldn’t do it again in a heartbeat. Right, Buck?”
Buck, looking properly chastised, and fighting a tiny smile, nods.
“Good,” Eddie says, taking Buck’s hand in his own, running his thumb over Buck’s knuckles. A few of them are bruised from the tumble they took, and Eddie keeps his touch careful. His own knuckles still bear a phantom ache from breaking Buck’s ribs, but it’s easier to ignore that now Buck is up and talking.
Eddie catches Buck glancing at the coffee and pastry at the bedside table. He watches a knowing smirk quirk up the corner of Buck’s mouth.
“The team knows now, don’t they?”
“Oh, absolutely,” Eddie says without hesitation.
“How much do you think Hen won from that?”
“Considering that I’m pretty sure Bobby already knew, I think they’ll be splitting the pot.”
Buck huffs a brief laugh, careful of his ribs, and squeezes Eddie’s hand.
“How long do you think they’ll tease us for?”
“Longer than necessary,” Eddie chuckles, brushing his lips across Buck’s knuckles. He doesn’t care what the team thinks, he’s just glad he has Buck here in front of him. They can handle whatever comes their way.
69 notes
·
View notes
Text
Basic CPR requires that you assess:
C-Circulation (need for chest compressions)
A-Airway
B-Breathing
...or "C-A-B" before beginning resuscitation efforts.
Tap the infant's foot to see if he responds.
Check for breathing and simultaneously check for a pulse in the brachial artery for no more than 10 seconds.
If he is unresponsive and not breathing (or only gasping) but has a pulse >60 bpm, begin rescue breaths. If his pulse is <60 or undetectable within 10 seconds, begin chest compressions as well.
The respiratory rate and effort, pulse oximetry, heart rate, perfusion, and strength of pulses will direct whether you give oxygen or proceed with CPR.
To review pediatric resuscitation in depth, link to 2015 guidelines for cardiopulmonary resuscitation and emergency cardiovascular care published by the American Heart Association.
I think they update this every 5 years, so there must be new guidelines for this year.
3 notes
·
View notes