#wound care & hyperbaric medicine
Explore tagged Tumblr posts
Text
Website: https://www.wattshbot.com/
Address: Las Vegas, Nevada, USA
From small single chamber clinics to huge multiple chamber mega clinics for humans and/or animals, we are your partner. We are here to walk beside you as you grow through the hyperbaric clinic creation process. Your success is our success! Get in touch now to see how we can assist you with your best hyperbaric outcome!
Who We Are:
Since 2006, We’ve been providing various levels of non- hospital based hyperbaric clinic consulting services to clients from the US and overseas. From assisting with the basic selection of various hyperbaric chambers to the complete build-out of the hyperbaric medicine clinic itself. Our newest enterprise is outfitting small animal veterinary clinics and hospitals with the best animal hyperbaric chamber options. Our primary focus has always been on facility and client safety. We believe in fostering an overall safe practice environment. This will enhance the facility return on investment. We look forward to walking beside you as you enter this new and exciting realm of medical speciality.
Consulting Services:
We work with clients, providing exceptional consulting services that are catered specifically to their hyperbaric needs. Get in touch to explore your hyperbaric possibilities.
Human Hyperbaric Clinic Consulting:
We are here to guide and assist you with your journey into Hyperbaric Medical clinic operations for humans. From curiosity to complete implementation.
Veterinary Hyperbaric Clinic Consulting:
There are just over one hundred Veterinary Hyperbaric clinics in the country. Modern Veterinary practices are beginning to utilize this amazing new and growing field of Veterinary Medicine to provide the best possible outcome to their Veterinary clients. As the costs of providing effective care continues to grow, this field of Veterinary Medicine will continue to experience greater growth, as well.
Keywords: hyperbaric medicine hyperbaric medicine physician hyperbaric medicine near me hyperbaric clinic hyperbaric oxygen clinic hyperbaric chamber veterinary hyperbaric consult hyperbaric oxygen therapy veterinary hyperbaric oxygen therapy veterinary medicine hyperbaric veterinary medicine veterinary hyperbaric oxygen therapy veterinary hyperbaric oxygen therapy near me burn hyperbaric medicine hyperbaric medicine and wound care wound care & hyperbaric medicine hyperbaric chamber clinic near me hyperbaric clinic near me hyperbaric medicine clinic hyperbaric oxygen clinic near me hyperbaric wound care clinic hyperbaric wound clinic hvm hyperbaric veterinary medicine veterinary hyperbaric chamber veterinary hyperbaric oxygen hyperbaric medicine consultants hyperbaric chamber veterinary medicine hyperbaric oxygen chamber veterinary hyperbaric oxygen therapy in veterinary medicine hyperbaric veterinary medicine chamber sechrist hyperbaric chamber veterinary veterinary hyperbaric veterinary hyperbaric chamber near me veterinary hyperbaric medicine veterinary hyperbaric oxygen therapy cost veterinary hyperbaric society veterinary hyperbaric therapy veterinary medicine hyperbaric therapy convergent hyperbaric consulting services hyperbaric consultant hyperbaric consulting solutions hyperbaric medicine consultants hyperbaric consultant hyperbaric oxygen therapy for animals animal hyperbaric oxygen chamber anxiety hyperbaric oxygen animation
#hyperbaric medicine#hyperbaric medicine physician#hyperbaric medicine near me#hyperbaric clinic#hyperbaric oxygen clinic#hyperbaric chamber veterinary#hyperbaric consult#hyperbaric oxygen therapy veterinary#hyperbaric oxygen therapy veterinary medicine#hyperbaric veterinary medicine#veterinary hyperbaric oxygen therapy#veterinary hyperbaric oxygen therapy near me#burn hyperbaric medicine#hyperbaric medicine and wound care#wound care & hyperbaric medicine#hyperbaric chamber clinic near me#hyperbaric clinic near me#hyperbaric medicine clinic#hyperbaric oxygen clinic near me#hyperbaric wound care clinic#hyperbaric wound clinic#hvm hyperbaric veterinary medicine#veterinary hyperbaric chamber#veterinary hyperbaric oxygen#hyperbaric medicine consultants
1 note
·
View note
Text
Also preserved on our archive
Some interesting science analyzed
BY BROOKS LEITNER
Imagine lying back in an enclosed chamber where you bask for 90 minutes in a sea of pure oxygen at pressures two to three times that felt at sea level. This is the world of hyperbaric oxygen therapy (HBOT), a technology that’s been around for decades and is now being explored as a possible treatment for Long COVID.
"The silence on the inside is deafening at first,” says John M.,* who has undergone dozens of HBOT treatments for his persistent Long COVID symptoms. Fortunately, there is a television outside the chamber in view, and it is easy to communicate with the provider if needed. While the potential protocol is still being refined, patients may undergo up to 40 HBOT sessions to address some of the most problematic, lingering symptoms of this complex condition.
HBOT is a therapeutic process that has been widely used to treat such conditions as decompression sickness in scuba divers, carbon monoxide poisoning, and diabetic foot ulcers. In HBOT, the body is exposed to 100% oxygen, a significant increase from the 21% oxygen concentration we typically breathe. The therapy takes place in an enclosed chamber where the air pressure is elevated above normal levels. The combination of high-pressure and high-oxygen conditions enhances the amount of oxygen that can reach the body's tissues. The hope is that this therapy can provide the same relief and healing to people with Long COVID that it does for those with other conditions.
According to John M., HBOT was the first treatment that helped with his sleep and reduced his heart palpitations. “At one point after hospitalization, my Long COVID symptoms were so bad that I could barely walk or talk. HBOT was a great tool that really assisted with my recovery,” he said. John added that he hopes the medical community will achieve a better understanding of how HBOT can help relieve suffering for patients with Long COVID and that more research will increase access to this innovative therapy.
Does HBOT improve Long COVID symptoms? One key observation from the work of Inderjit Singh, MBChB, an assistant professor at Yale School of Medicine (YSM) specializing in pulmonary, critical care, and sleep medicine, is that Long COVID patients often experience debilitating fatigue. Based on Dr. Singh’s previous Long COVID research, the exhaustion is thought to be linked to the muscles’ inability to efficiently extract and utilize oxygen.
To picture how HBOT might work, you can think of your muscles as engines sputtering, struggling to get the fuel they need. If oxygen is the gas that fuels the muscles, it’s as if you are trying to complete your daily routine while the gas tank is running on “empty.” By aiming to directly address this oxygen utilization impairment, HBOT may be a potential solution.
A systematic review by researchers at the China Medical University Hospital noted that HBOT could tackle another major factor in the Long COVID puzzle: oxidative stress. This relates to the body's struggle to maintain balance when harmful molecules, known as free radicals, run amok, causing chronic inflammation.
Research co-authored by Sandra K. Wainwright, MD, medical director of the Center for Hyperbaric Medicine and Wound Healing at Greenwich Hospital in Connecticut, suggests that HBOT, with its high-oxygen environment, might dampen this chronic inflammation by improving mitochondrial activity and decreasing production of harmful molecules. Other potential benefits of HBOT in the treatment of Long COVID may include restoration of oxygen to oxygen-starved tissues, reduced production of inflammatory cytokines, and increased mobilization of hematopoietic stem cells—primary cells that transform into red blood cells, white blood cells, and platelets.
HBOT for Long COVID: Current and ongoing research Several small-scale reports have indicated that HBOT is safe for patients with Long COVID.
To address this question, a trial that followed the gold standard of modern medical research—a randomized, placebo-controlled, double-blind design—assigned 73 Long COVID patients to either receive 40 sessions of HBOT or a placebo of only 21% oxygen. The study observed positive changes in attention, sleep quality, pain symptoms, and energy levels among participants receiving HBOT. In a longitudinal follow-up study published in Scientific Reports, the authors at the Tel Aviv University found that clinical improvements persisted even one year after the last HBOT session was concluded. In a second study, the same authors focused on heart function, measured by an echocardiogram, and found a significant reduction in heart strain, known as global longitudinal strain, in patients who received HBOT.
In another study, 10 patients with Long COVID underwent 10 HBOT treatments over 12 consecutive days. Testing showed statistically significant improvement in fatigue and cognitive function. Meanwhile, an ongoing trial at the Karolinska Institute in Sweden has reported interim safety results wherein almost half of the Long COVID patients in the trial reported cough or chest discomfort during treatment. However, it was unclear whether HBOT exacerbated this symptom or if this adverse effect was due to the effort of participation by patients suffering from more severe Long COVID symptoms.
Is HBOT currently available as a treatment for Long COVID? For HBOT to become a mainstream treatment option for Long COVID, several critical priorities must be addressed. First, there is currently no established method for tailoring HBOT dosages to individual patients, so researchers must learn more about the specific features or symptoms that indicate potential benefits from HBOT. At the same time, we need to identify factors that may be associated with any adverse outcomes of HBOT. And finally, it’s important to determine how long these potentially beneficial effects last in a larger cohort. Will just a few HBOT trials be enough to restore patients to their baseline health, or will HBOT become a recurring component of their annual treatment regimen?
For now, HBOT remains an experimental therapy—and as such is not covered by insurance. This is a huge issue for patients because the therapy is expensive. According to Dr. Wainwright, a six-week course of therapy can run around $60,000. That’s a lot to pay for a therapy that’s still being studied. In the current completed studies, different treatment frequencies and intensities have been used, but it’s unclear how the treatment conditions affect the patient’s outcome.
“I have had some patients notice improvements after only 10 or 15 treatments, whereas some others need up to 45 treatments before they notice a difference,” notes Dr. Wainwright. “I think that HBOT is offering some promising results in many patients, but it is probably a strong adjunctive treatment to the other spectrum of things Long COVID patients should be doing, like participating in an exercise, rehab, and nutritional program.”
Dr. Singh notes that “a major challenge for research is the heterogeneity of Long COVID. It is hard to determine which symptoms to treat and enroll patients into trials based on them.”
Perhaps treatments that target multiple issues caused by Long COVID, like HBOT, may help overcome this challenge.
*Not his real name.
Brooks Leitner is an MD/PhD candidate at Yale School of Medicine.
The last word from Lisa Sanders, MD: Hyperbaric oxygen therapy (HBOT) is just one of the many existing treatments that are being looked at to treat Long COVID. We see this with many new diseases—trying to use a treatment that is effective in one set of diseases to treat another. And there is reason for optimism: We know that HBOT can deliver high levels of oxygen to tissues in need of oxygen. That’s why it’s used to treat soft tissue wounds. If reduced oxygen uptake is the cause of the devastating fatigue caused by Long COVID, as is suggested by many studies, then perhaps a better delivery system will help at least some patients.
Studies referenced:
bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-023-08002-8
www.ncbi.nlm.nih.gov/pmc/articles/PMC8806311/
www.nature.com/articles/s41598-024-53091-3
www.nature.com/articles/s41598-022-15565-0
www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2024.1354088/full
www.ncbi.nlm.nih.gov/pmc/articles/PMC11051078/#:~:text=Proposed%20Mechanism%20of%20HBOT%20o
#long covid#hbottherapy#HBOT#hyperbaric oxygen therapy#mask up#covid#pandemic#wear a mask#public health#covid 19#still coviding#wear a respirator#coronavirus#sars cov 2
12 notes
·
View notes
Text
Hyperbaric Medicine (HBO)
I'm sorry, what is that?

I have a side hustle as a hyperbaric medicine provider and I am here to give you the down and dirty!
Sometimes referred to as HBO (hyperbaric oxygen), hyperbaric or dive medicine is a specialty that utilizes oxygen at high pressure to treat a variety of conditions, primarily things involving wounds. We place a patient in a chamber, deliver 100% oxygen to them, pressurize the chamber, and keep them in there for about 120 minutes. Since oxygen is the number one thing you need to heal a wound, we use a lot of it to try and speed up the process.
The Basics
Wait - what? HOW? Try not to have PTSD from your days in chemistry, but remember these?

The treatment physiology of hyperbarics relies on gas laws. Recall that it takes a lot of pressure to dissolve a gas into a liquid.
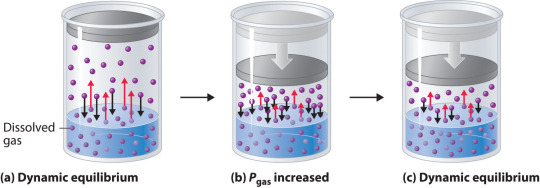
We use pressure to force oxygen into the blood stream at high rates to facilitate wound healing. For reference, most of your oxygen content is bound to hemoglobin (~98%). You do have dissolved oxygen in your blood, represented by your PaO2/PvO2 in a blood gas. However, this makes up a fraction of O2 content (~2%: if you want a clinical soap box, you should hear me talk about blood gases to students lol). A normal ABG would have a PaO2 of 65-100. An ABG acquired during hyperbaric treatment would be well over 2,000.
As an aside, recall that ambient air is 21% oxygen. Also, as a reminder, we exist at 1.0 ATA of pressure (one atmosphere).
How is it done?
Delivering oxygen this way requires delivery of a lot of pressure. We utilize dive chambers for this purpose. There are two types of chambers:
Monoplace: literally looks like a class coffin. Holds one patient and delivers oxygen at pressure through the entire chamber. These are very popular at wound centers.

Multiplace: literally looks like a submarine. Holds 2+ patients and delivers oxygen at pressure to individual patients hooked up to hoods or masks. These are found at tertiary care/academic medical centers.

Literally, the multiplace hoods make you look like a silly space person.

The reason oxygen is delivered this way in a multiplace chamber is to reduce the risk of fire. Oxygen at pressure can go boom. Having an entire chamber full of O2 is a big risk. So, we deliver the gas individually to each patient.
How did it start?
Dinking around with gases at pressure has been a thing for 400 years. However, it didn't become a more focused endeavor until the first dive suits started to be a thing in the 1870s. The specialty itself is relatively new, developed in the 1930s due to advent of decompression illness with divers. Things really progressed in the 1950s.
One pivotal study was "Life without Blood" in 1959. Dr. Boerema proved that he could keep a pig alive with HBO alone. The ethics of this experiment are questionable but he exsanguinated a pig under hyperbaric conditions (3.0 ATA, 100% FiO2). Plasma was left behind. By doing this, he proved that, at pressure, an organism does not need hemoglobin to live. Kind of a radical thing to prove! Don't worry, the pigs did get their blood back and recovered without issue.
What is treated with HBOT? (hyperbaric oxygen therapy)
Anything related to wound healing can be treated with HBOT. We also treat carbon monoxide poisoning, air gas embolism, and decompression sickness with HBOT. I'll start with those since they are (imo), the most clinically interesting. ;-D
Carbon monoxide poisoning: The physiology of using HBOT to treat CO poisoning is based on the binding affinity of CO to hemoglobin. CO has 200 x the binding affinity for hemoglobin than O2 or CO2 does. Because the binding sites are taken up by CO, hemoglobin cannot pick up O2. It also can't offload whatever O2 is already bound. The goal with HBOT is to bombard the blood with massive amounts of O2 to force CO off.

For reference, it would take about 6 hours for CO to offload on its own from hemoglobin on room air. It would take half as long at 100% FiO2 delivered at standard air pressure (1.0 ATA). CO is rapidly forced off within 30 minutes with HBOT. With very severe CO poisoning, particularly in cases of LOC, this is vital for limitation of hypoxia and neurological sequelae of exposure. Treatment is 1-3 "dives" depending on clinical context. The patient is treated at 2.8 ATA (60 feet of sea water) for about 120 minutes.
Air gas embolism: This occurs when gas is accidentally introduced into circulation. It can either be venous or arterial. The venous system has much more flexibility in tolerance for air bubbles. 15 cc or less of gas introduction is probably not going to result in symptoms. Higher volumes go to the lungs and can result in local lung infarction.
The real danger with this is air introduced into arterial circulation. Depending on where it is introduced, it can go directly to the heart causing an MI, or to the brain causing a stroke. Any volume of air introduced into arterial circulation is bad news bears. Treatment is usually 1 "dive" but could be more based on the context. The patient is treated at 2.8 ATA for 30 minutes and then the ascent is extremely slow. The whole dive takes about 5 hours. Why so long? If we ascend too quickly, the air bubble will reform.
Decompression sickness: This occurs primary with scuba divers who ascended too quickly. Scuba divers generally breath mixed gas, most commonly air (21% O2, ~79% N2) or nitrox (35% O2, ~65% N2). As someone is diving, the nitrogen they breath is also dissolved into their blood since they are at a pressure greater than 1.0 ATA. If a diver ascends too quickly, the nitrogen dissolved in the blood will rapidly reform air bubbles in the blood. We just mentioned how that is problematic.
Since air bubbles can go everywhere in circulation, the symptoms are variable ranging from headache, vertigo, nausea, joint pain, chest pain, stroke symptoms, loss of bowel/bladder function, etc. The treatment for this is to recompress the patient and very slowly ascend in the HBO chamber. Treatment is usually 1 dive but could be more based on the context. The patient is treated at 2.8 ATA for 30 minutes and then the ascent is extremely slow. The whole dive takes about 5 hours. Why so long? Again, if we ascend too quickly, the air bubble will reform.
Wound related conditions: there are roughly 15 approved diagnoses for HBO by Medicare in the USA. This is important to mention because if a condition is not covered, paying out of pocket is extremely cost-prohibitive. Insurance is billed $6,000 per treatment! Some of the most common conditions treated are osteoradionecrosis, soft-tissue radionecrosis, irradiation cystitis with hematuria, and refractory chronic osteomyelitis. Wounds created from radiation exposure have the best evidence to support the use of HBOT. These are considered outpatient conditions so patients come to be treated Monday-Friday. We dive to 2.4 ATA for 120 minutes. At minimum, patients are prescribed 20 dives but most treatment protocols for radiation induced injuries is at least 40 dives.
As you can see, this is a HUGE commitment for the patient. One dive is not enough for these wound related conditions. As a hyperbaric provider, I can say that we have patients with such significant symptom relief from HBO. For example, irradiation cystitis with hematuria is extremely debilitating. Patients are fatigued from chronic blood loss, deal with painful bladder spams and pelvic pain, pain with urination, and increased frequency. The blood can clot and obstruct their urethra or foley catheter. Symptoms like this limit quality of life. HBOT makes a huge difference for them.
Benefits
Anyone who has barriers to wound healing can benefit from HBO. Barriers include vascular disease, CKD, COPD, DM, heart failure, and immunocompromised status. The goal is symptom resolution/improvement or healing of the wound. Some patients get approved for far more treatments than we typically do. Usually the maximum insurance will cover is 60. However, in some situations, the clinical benefit of continued treatments is recognized by insurance and treatment is extended.
As a provider, I get to know these patients pretty well. They show up every day that I am staffing in HBO and it is rewarding to see them improve. Compared to my critical care role, this is a nice change of pace.
Adverse Reactions and Risks
There are risks and side effects to HBO. The most common are barotrauma, pneumothorax, seizure, temporary worsening of cataracts/vision, and abdominal distention.
Barotrauma of the ears and sinuses is by the most common issue we face in HBOT. If patients are not able to clear their ears as they descend ("pop" their ears), they can rupture their ear drums. Patients that cannot descend without extreme pain may need myringotomy tubes (ear tubes) to assist with equalizing pressure.
Seizure is a risk of HBOT and that primarily comes from oxygen reducing the seizure threshold. We mitigate this with "air breaks". These are 5 minutes intervals of the treatment where the patient is receiving air rather than 100% O2. Example, we treat at 100% for 30 minutes, have a 5 minute air break, repeat x 2. Obviously the people at highest risk are those with epilepsy or taking seizure threshold reducing medications.
HBOT can worsen cataracts and vision temporarily. The mechanism of this is poorly understood but we know it is reversible. Distance vision is affected the most.
Contraindications
The only absolute contraindication to HBOT is an untreated pneumothorax. There are many relative contraindications that require a risk benefit analysis. An example of this is pregnancy. HBOT has not been thoroughly studied in pregnancy and is not recommended EXCEPT in cases of CO poisoning where we know that the CO concentration is higher in fetal circulation than maternal. Always treat a pregnant person with CO poisoning.
Other potential contraindications include use of certain chemotherapy agents, COPD with blebs/bullae, severe heart failure, epilepsy, sinus/HEENT disease, claustrophobia, certain implanted devices, or active infection.
With certain chemo agents, they can lower the seizure threshold putting patients at higher risk of seizure in the chamber. People with COPD and blebs are at risk of those blebs popping under pressure and causing acute respiratory distress. People with heart failure can experience flash pulmonary edema after an HBO treatment. If people are claustrophobic, obviously spending time in a monoplace chamber can trigger panic attacks. At my center, we sometimes have people referred to our multiplace chamber for exactly that reason.
Most implanted medical devices are HBOT compliant. Generally, pacers and other devices are tested at 4.0 ATA of pressure. We double check with the manufacturer that the device is compliant. If it isn't, we cannot safely treat and have to deny the consult.
Obviously, if someone is sick, we don't want them in the chamber. Particularly colds, severe allergies, fever, or anything that is affecting HEENT. People with acute sinus infection are unable to clear sufficiently to dive. Even if they can clear, they feel miserable. No need to go through that.
Safety Issues
I mentioned that high O2 environments are at risk for explosion. Safety is the number one concern with any chamber. The goal is to reduce risk of fire by removing fabrics that create static (anything synthetic), removing electronic devices that are not HBOT approved, and going through multiple levels of safety checks for patients and for chamber preparation.
At our chamber, only 100% cotton is allowed in the chamber. All patients have special scrubs that they wear during treatment. No electronic devices can be brought in the chamber which includes phones, tablets, laptops, e-readers, watches, pagers, etc. We do have HBOT approved IV pumps and radio headsets that we use. These have been tested at 4.0 ATA. The radio headsets are for the attendant (staff member) who is in the chamber and this is also for safety purposes. Since we have a mulitplace chamber, a staff member is always in the chamber with the patient(s).
One thing I do want to address is that some people are concerned about putting a patient with active cancer into the chamber. There is concern that the high O2 environment will "feed" the cancer. There is simply not data to support this. Active cancer is not a contraindication to HBOT.
And there you have it! The down and dirty of HBOT! Hopefully you learned something cool. If you think you have a patient who would benefit, find your local HBOT provider. We are always happy to talk with you about the process. If you care about a soapbox of how insurance companies suck, see below. :-D
Soapbox: I will say, I have definitely been frustrated with insurance companies. They are the gatekeepers of this treatment. You can have several providers supporting the use of treatment and an insurance company can still say "no". Very frustrating.
A prime example of this are patients who have avascular necrosis that is steroid or chemotherapy induced. These are often younger patients (late teens, early 20s) who have/had leukemia of some kind. They end up having necrosis at a joint, usually the femoral head, that will likely result in complete joint replacement at a young age. No orthopedic surgeon wants to replace joints on a young person. It comes will all kind of problems and always needs revision later in life.
Insurance companies will say "we only cover radiation induced necrosis" because that is what the literature supports. Yes, they are correct that the vast majority of studies support HBOT for radiation induced injury. However, the pathophysiology of the tissue destruction, while a little different, ends up with the SAME problem. There are studies that support HBOT use in these situation but not nearly as many as radiation induced injury. The result is that patients suffer, get a joint replacement they could have avoided (or postponed until they are fully developed), and generally are shafted.
*end soapbox*
#pablr#medblr#nurblr#pharmblr#physician assistant#physician associate#doctor#physician#hyperbaric medicine#hbot#hbo#medicine#oxygen therapy
6 notes
·
View notes
Text
Brain Science: Election Day +2, 2024 Personal, Congressional, and National Accountability

"Democracy is the only system that persists in asking the powers that be whether they are the powers that ought to be." - Sydney J. Harris The sky hasn't fallen. But this isn't about politics, though nothing these days seems to be free of tough choices amidst competing interests and "truth." This is a reflection on choices we as a country face with respect to medicine, specifically brain wounds, mental health, and modern alternatives and supplements to standards of care that are outdated. Consider: Compared to most of medicine, Brain Science is in its infancy. A quick review of the historical record shows the recent rush of new science: Early-history: Trephination, an early form of brain surgery, was used to treat a variety of conditions, including: Relieving pressure in the skull, Treating symptoms of epilepsy and sinusitis, and curing supernatural or otherworldly conditions. Remains of the brothers, who lived during the Bronze Age between 1550 BC and 1450 BC, were found with holes in their skulls during an excavation of a tomb in the ancient city of Tel Megiddo. The Incas beat Europeans to it, but fossils show that brain surgery may have begun around 2.5 million years ago, during the late Paleolithic period. Pre-modern: Al-Zahrawi performed surgical treatments for head injuries, skull fractures, and other conditions in Al-Andalus from 936 to 1013 AD. Simple neurosurgery was performed on King Henri II in 1559 after a jousting accident. He didn't survive. 18th century: The Industrial Revolution led to economic and technological growth, which in turn led to medical progress. 19th century: Scientists made discoveries and inventions that helped identify and prevent illnesses, and understand how bacteria and viruses work. Anesthetics were developed, and medical training improved. Cushing ushers in modern neurosurgery in 1895. 20th century: Research focused on infectious diseases and how they spread. Many pathogenic organisms were discovered and classified, including viruses, which cause diseases like polio, measles, and mumps. 1950s: Antibiotics were discovered, and the mechanisms of metabolic diseases were understood. 1960s and 1970s: The scientific method became more important than tradition and authority. Treatments had to be shown to be effective through statistically sound techniques. 1980s to 2000: Robot-assisted surgery, Vaccine for Hepatitis “B”; MRI scanner; Statins; Laser Cataract Surgery; Gamow bag (hyperbaric bag for treating altitude sickness); tiny camera on a pill; Radiosurgery (for epilepsy and malignant tumors); Viagra. 2000 to present: Human Genome completed; CRISPR; worldwide BRAIN projects; Nobel prize for importance of oxygen, discovery of the glymphatic system, (re)discovery of translational/functional/ alternative medicine. In 2024, "invisible wounds" are no longer invisible. Brain scanning and sophisticated biomarker techniques can reveal brain wounds and provide hints for interventions to cure those wounds. And we continue to discover many of the mechanisms of action that impede brain health, and how HBOT addresses conditions like inflammation, oxygen delivery, proliferation of stem cells, healing, restoration of brain functions necessary for health, and ageing. The glymphatic system, an undiscovered body system until 2012, helps the brain clear metabolic waste, excess fluid, and proteins. It's thought that glitches in the glymphatic system may contribute to the buildup of harmful waste in the brain, which could lead to conditions like Alzheimer's disease, stroke, and Parkinson's disease. HBOT, by reducing inflammation and growing new blood vessels, restores glymphatic system regularity. Consider the impact of the 2019 Nobel Prize in Physiology or Medicine on our understanding of brain mechanics. The prize was awarded to William G. Kaelin Jr., Sir Peter J. Ratcliffe, and Gregg L. Semenza for their discoveries about how cells sense and adapt to oxygen levels. The scientists' work revealed the molecular machinery that regulates gene activity in response to oxygen levels. This process is essential for hypoxia-inducible factor (HIF). Dr. Shai Efrati, a veteran HBOT researcher, has recently published BEYOND NORMAL, How the new Science of Enhanced Medicine Elevates Peak Performance and Repairs Brain Injury. In it, he speaks directly to the power of Hyperbaric Oxygenation, coupled with HIF, to restore brain function. His ground-breaking work provides remarkable insights about oxygen delivery for Stroke, Concussion, PTSD, Fibromyalgia, neurologic disorders like Alzheimers's, peak physical performance, and the science of "reverse ageing." Bottom line: new advances in medicine have escaped many medical school graduates who have never heard of HBOT, the glymphatic system, or HIF. Sadly, medicine and insurance rules make it difficult for doctors to really listen to patients to do proper diagnoses, The lack of time to read outside their discipline means doctors are uninformed. Victims of brain wounds are underserved and often unknowing about safe, effective, available, and less costly interventions to deal with their mis- or mal-diagnosed TBI/PTSD/Concussion. In the midst of a complex and often contentious healthcare landscape, we find ourselves grappling with critical choices that directly impact the lives of countless individuals suffering from brain injuries and mental health challenges. The urgency for modern alternatives to outdated care standards has never been more pronounced, as we witness the heartbreaking epidemics of suicide, concussions, and mental health issues affecting veterans and civilians alike. At TreatNOW, we are committed to illuminating the path forward by educating key stakeholders—Congress, the Department of Defense, and the general public—about the proven benefits of innovative treatments like Hyperbaric Oxygen Therapy (HBOT). Our efforts are driven by a deep compassion for those struggling with the aftermath of brain wounds and a resolute belief in the power of timely intervention to facilitate healing. As we tirelessly advocate for policy changes that will enhance access to effective treatments, we invite you to join us in championing this vital mission. Together, we can break the logjam and ensure that those in need receive the care they deserve. ****************************** The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help end symptoms of PTSD, get patients off most of their drugs, and heal brain wounds to end the effects of BLAST injury, mild TBI Persistent Post Concussive Syndrome, and polytrauma from AHI and Burn Pits. Diabetic Foot Ulcers have become a major emphasis. www.treatnow.org Heal Brains. Stop Suicides. Restore Lives. TreatNOW Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made. Read the full article
#brainhealth#braininjury#brainscience#brainwound#brainwounds#chambertreatment#concussion#HBOT#HBOTTreatment#hyperbaricchamber#HyperbaricOxygentherapy#PTSD#TBI#traumaticbraininjury
0 notes
Text
Diabetic Foot Ulcer Care in Hyderabad: Best Treatments Without Amputation

Diabetic foot ulcers are a serious complication affecting individuals with diabetes, leading to persistent wounds that are slow to heal. These ulcers require immediate medical attention to prevent further complications, including infections and, in severe cases, amputations. Fortunately, patients in Hyderabad have access to innovative and effective treatments that focus on preserving the foot. This guide will explore the best options for diabetic foot ulcer treatment in Hyderabad, including non-amputation methods that allow patients to heal while maintaining mobility and quality of life.
In recent years, advances in medicine have introduced non-amputation treatment options that prioritize healing and limb preservation. Here are some of the highly effective approaches available in Hyderabad:
Debridement Debridement involves removing dead skin and tissue from the ulcer, allowing the body’s natural healing processes to work more effectively. This procedure helps to reduce infection risk and is typically performed under the care of an experienced wound care specialist.
Advanced Dressings and Wound Care Using specialized dressings can accelerate the healing of diabetic foot ulcers. These dressings create an optimal environment for healing, keeping the wound moist while protecting it from bacteria. Some advanced wound care centers in Hyderabad offer dressings with antibacterial properties, which can further prevent infection.
Hyperbaric Oxygen Therapy (HBOT) HBOT is a treatment that delivers high levels of oxygen to the wound area, improving blood circulation and promoting tissue repair. This therapy has been effective in reducing the need for amputations and is available at select clinics in Hyderabad.
Stem Cell Therapy Stem cell therapy is an emerging treatment that uses stem cells to regenerate damaged tissues, helping to speed up the healing of chronic ulcers. It’s a specialized procedure that offers significant promise for those looking to heal without the threat of amputation.
Negative Pressure Wound Therapy (NPWT) NPWT, or vacuum-assisted closure, applies negative pressure to the wound, which can help remove fluids and stimulate blood flow. This therapy has shown great results for non-healing ulcers and is available at leading diabetic foot treatment centers in Hyderabad.
The Best Treatment for Diabetic Foot Ulcers in Hyderabad
Finding the best treatment for diabetic foot ulcers depends on individual needs, the ulcer’s severity, and any underlying health issues. Consulting with top-rated specialists in Hyderabad can provide access to personalized treatment plans tailored for optimal recovery without amputation.
0 notes
Text
How Hyperbaric Chamber Oxygen Therapy is Revolutionizing Recovery in San Antonio

In recent years, hyperbaric chamber oxygen therapy in San Antonio has gained significant attention for its ability to accelerate healing and recovery across a range of medical conditions. From athletes recovering from injuries to patients with chronic conditions, many are turning to this innovative treatment to boost their recovery process. In this blog, we’ll dive into how hyperbaric oxygen therapy works, the science behind its success, and why it’s becoming a popular choice for residents of San Antonio.
Understanding Hyperbaric Oxygen Therapy (HBOT)
Hyperbaric oxygen therapy involves placing a patient in a specialized chamber where they breathe in pure oxygen at increased atmospheric pressures. This process allows more oxygen to be dissolved into the bloodstream, enhancing the body’s natural healing processes. The high oxygen levels can penetrate areas of the body where blood flow may be restricted, delivering much-needed oxygen to tissues and cells.
Why Choose Hyperbaric Chamber Oxygen Therapy in San Antonio?
San Antonio is home to a growing number of medical facilities offering hyperbaric chamber oxygen therapy. Here’s why more people are choosing this treatment:
Advanced Medical Facilities: San Antonio boasts several advanced medical facilities equipped with the latest hyperbaric chambers, ensuring patients receive top-quality care.
Expert Medical Staff: Trained professionals and specialists in hyperbaric medicine ensure that the therapy is conducted safely and effectively.
Personalized Treatment Plans: Many clinics in San Antonio offer personalized treatment plans tailored to the specific needs of the patient, whether it’s for wound healing, injury recovery, or managing chronic conditions.
The Science Behind Hyperbaric Oxygen Therapy
The effectiveness of hyperbaric chamber oxygen therapy is backed by science. Here’s how it works:
Increased Oxygen Delivery: Under normal conditions, oxygen is carried through the body by red blood cells. In a hyperbaric chamber, oxygen is dissolved directly into all the body’s fluids, including plasma, lymph, and cerebrospinal fluids, which can then be delivered to areas where circulation is poor.
Promotes Angiogenesis: The high levels of oxygen promote the growth of new blood vessels, a process known as angiogenesis, which is crucial for healing wounds and regenerating tissues.
Reduces Inflammation and Swelling: Increased oxygen levels can reduce inflammation and swelling, a common issue in various injuries and chronic conditions, facilitating faster recovery.
Conditions Treated with Hyperbaric Oxygen Therapy
Hyperbaric chamber oxygen therapy in San Antonio is utilized to treat a wide array of conditions, including:
Diabetic Foot Ulcers: These non-healing wounds can significantly benefit from the increased oxygen, which promotes faster tissue repair and reduces the risk of amputation.
Sports Injuries: Athletes recovering from fractures, muscle tears, or ligament injuries use HBOT to accelerate recovery time and reduce downtime.
Chronic Pain and Fatigue: Patients suffering from conditions like fibromyalgia or chronic fatigue syndrome may experience pain relief and increased energy levels.
Radiation Injury Recovery: HBOT is also used to treat radiation-induced injuries, promoting healing in tissues damaged by radiation therapy.
Benefits of Hyperbaric Chamber Oxygen Therapy for Recovery
Speeds Up Healing Process: For acute injuries and chronic conditions alike, hyperbaric oxygen therapy can significantly speed up the healing process, allowing patients to return to their normal activities more quickly.
Non-Invasive Treatment: Unlike surgeries or other invasive procedures, HBOT is non-invasive, making it a safer option for many patients.
Enhances Quality of Life: By reducing symptoms and speeding up recovery, hyperbaric oxygen therapy can improve the overall quality of life for patients dealing with chronic pain or injury.
Potential Cost Savings: Faster recovery times can lead to fewer medical appointments and potentially lower overall healthcare costs.
What to Expect During Hyperbaric Oxygen Therapy
For those considering hyperbaric chamber oxygen therapy in San Antonio, here’s what you can expect:
Initial Consultation: A consultation with a hyperbaric medicine specialist will determine if you are a good candidate for HBOT. They will review your medical history and current condition.
Therapy Sessions: Each session typically lasts between 60 to 90 minutes. You’ll be placed in a hyperbaric chamber, where you’ll breathe pure oxygen while the pressure is gradually increased.
Post-Therapy: After the session, you can resume your daily activities. Some people might feel a bit tired, but this usually passes quickly.
Frequently Asked Questions (FAQs)
Q: How many sessions of hyperbaric oxygen therapy will I need? A: The number of sessions varies depending on the condition being treated and individual patient needs. Your healthcare provider will create a personalized treatment plan for you.
Q: Is hyperbaric oxygen therapy covered by insurance? A: Coverage varies by insurance plan and condition being treated. It’s best to check with your insurance provider to determine if hyperbaric chamber oxygen therapy in San Antonio is covered under your plan.
Q: Are there any side effects? A: While side effects are rare, some individuals may experience ear discomfort, sinus pressure, or temporary vision changes. Severe side effects are uncommon but should be discussed with your healthcare provider.
Q: Can children undergo hyperbaric oxygen therapy? A: Yes, children can undergo HBOT, but it should be recommended and closely monitored by a pediatric specialist.
Q: How do I prepare for a hyperbaric oxygen therapy session? A: It’s generally advised to wear comfortable clothing and avoid using perfumes, deodorants, or lotions before the session. Your provider will give you specific instructions based on your treatment plan.
Conclusion
Hyperbaric chamber oxygen therapy in San Antonio is revolutionizing recovery for many patients, offering a non-invasive, effective way to enhance healing and improve overall well-being. Whether you’re dealing with a chronic condition, recovering from an injury, or looking to boost your overall health, this therapy could be a game-changer. Always consult with a qualified healthcare provider to see if HBOT is right for you and to develop a tailored treatment plan that meets your specific needs.
0 notes
Text
A Deep Dive into HBOT in Nepal: What Patients Should Know
Hyperbaric Oxygen Therapy (HBOT) is an innovative treatment that has garnered significant attention worldwide, and Nepal is no exception. As more people seek alternative therapies for various health conditions, HBOT stands out for its potential to promote healing, enhance recovery, and improve overall well-being. This article will provide an in-depth look at HBOT in Nepal, exploring its benefits, applications, and what patients need to know before considering this therapy.
What is HBOT?
Hyperbaric Oxygen Therapy involves breathing pure oxygen in a pressurized chamber. This process increases the amount of oxygen your blood can carry, which helps to speed up the body’s natural healing processes. The therapy is typically used to treat a variety of medical conditions, from chronic wounds to radiation injuries, and is gaining popularity for its potential benefits in sports recovery and wellness.
Benefits of HBOT
1. Accelerated Healing
One of the most significant benefits of HBOT is its ability to speed up the healing process. The increased oxygen levels in the blood can enhance tissue repair and regeneration, making it particularly effective for wounds that are slow to heal, such as diabetic foot ulcers or radiation-induced injuries.
2. Reduced Inflammation
HBOT has been shown to reduce inflammation, which can be beneficial for conditions such as arthritis, sports injuries, and other inflammatory diseases. By decreasing swelling and promoting blood flow, HBOT helps to alleviate pain and improve mobility.
3. Enhanced Immune Function
The therapy also strengthens the immune system, helping the body fight off infections more effectively. This is especially useful for patients with compromised immune systems or those recovering from surgery.
4. Improved Brain Function
There is growing evidence to suggest that HBOT can improve cognitive function, particularly in patients with brain injuries, strokes, or neurological disorders. The increased oxygen supply to the brain can aid in the recovery of damaged brain cells and improve overall mental clarity.
HBOT in Nepal: The Current Scenario
Nepal is gradually embracing HBOT as a viable treatment option for various medical conditions. While the therapy is still relatively new in the country, a growing number of medical facilities are offering HBOT services. These centers are equipped with state-of-the-art hyperbaric chambers and are staffed by trained professionals who ensure that patients receive safe and effective treatment.
Availability of HBOT in Nepal
In major cities like Kathmandu and Pokhara, HBOT is becoming increasingly accessible. Clinics and hospitals that offer HBOT are typically associated with specialized medical care, including wound care centers, sports medicine facilities, and wellness clinics. The therapy is often recommended by healthcare providers for patients who have not responded to traditional treatments or those looking to enhance their recovery process.
Cost of HBOT in Nepal
The cost of HBOT in Nepal can vary depending on the location and the number of sessions required. On average, a single session can range from NPR 5,000 to NPR 15,000. While this may seem expensive, many patients find the investment worthwhile due to the potential health benefits and the ability to avoid more invasive treatments.
What to Expect During an HBOT Session
Patients considering HBOT in Nepal should be aware of what the treatment entails. Each session typically lasts between 60 to 90 minutes, during which the patient will be placed in a hyperbaric chamber. The chamber is then pressurized to a level higher than normal atmospheric pressure, and the patient breathes in pure oxygen. The process is painless, though some patients may experience slight discomfort in their ears due to the change in pressure, similar to the sensation during an airplane takeoff.
Safety Considerations
HBOT is generally safe when administered by trained professionals in a controlled environment. However, like any medical treatment, there are some risks involved. Patients with certain conditions, such as lung disease, ear problems, or those who are pregnant, should consult their doctor before undergoing HBOT. It’s essential to follow the medical provider’s instructions carefully to minimize any potential risks.
FAQs about HBOT in Nepal
1. What conditions can HBOT treat?
HBOT is used to treat a variety of conditions, including chronic wounds, radiation injuries, carbon monoxide poisoning, decompression sickness, and certain infections. It is also used in sports medicine to aid in the recovery of injuries and improve athletic performance.
2. How many HBOT sessions are needed?
The number of sessions required depends on the condition being treated. Acute conditions may only require a few sessions, while chronic or more severe conditions may necessitate 20 to 40 sessions or more.
3. Is HBOT covered by insurance in Nepal?
Insurance coverage for HBOT in Nepal varies. Some insurance providers may cover the therapy for specific conditions, while others may not. It’s advisable to check with your insurance company before beginning treatment.
4. Are there any side effects of HBOT?
While HBOT is generally safe, some patients may experience temporary side effects such as ear discomfort, fatigue, or mild dizziness. Serious side effects are rare but can include oxygen toxicity or damage to the lungs.
5. Can HBOT be combined with other treatments?
Yes, HBOT is often used in conjunction with other treatments, such as wound care, physical therapy, and medication. It can enhance the effectiveness of these treatments by improving oxygen delivery to damaged tissues.
6. Who should not undergo HBOT?
Patients with certain medical conditions, such as untreated pneumothorax (collapsed lung), severe claustrophobia, or certain types of ear infections, may not be suitable candidates for HBOT. It’s essential to undergo a thorough medical evaluation before starting treatment.
Conclusion
Hyperbaric Oxygen Therapy is a promising treatment option that is gaining traction in Nepal. With its potential to accelerate healing, reduce inflammation, and improve overall health, it offers a viable alternative for patients seeking to enhance their recovery from various medical conditions. As with any medical treatment, it’s crucial to consult with a healthcare professional to determine if HBOT is the right option for you.
Whether you’re dealing with chronic health issues or looking to boost your recovery after surgery or injury, HBOT in Nepal could be the solution you’ve been searching for.
Source Link: https://terasworld.com/a-deep-dive-into-hbot-in-nepal-what-patients-should-know/
0 notes
Text
Comprehensive Wound Care Solutions in San Antonio: Vayu Advanced Wound Clinic & Hyperbarics

When dealing with wounds that refuse to heal, specialized care becomes crucial. At Vayu Advanced Wound Clinic & Hyperbarics in San Antonio, Texas, Dr. Manjulatha Badam, MD, CWSP, UHM, leads a dedicated team offering advanced wound care services designed to promote healing and improve outcomes.
Advanced Wound Care Services
Vayu Advanced Wound Clinic & Hyperbarics specializes in treating chronic wounds and ulcers through a variety of advanced techniques. Dr. Badam, a Certified Wound Specialist Physician (CWSP) with expertise in Undersea and Hyperbaric Medicine (UHM), provides comprehensive evaluations and personalized treatment plans tailored to each patient's specific needs.
One of the key treatments offered at Vayu is hyperbaric oxygen therapy (HBOT). This therapy involves breathing pure oxygen in a pressurized room or chamber, which increases the amount of oxygen in the bloodstream. HBOT has been proven effective in promoting the healing of wounds that have not responded to traditional therapies. By enhancing oxygen delivery to tissues, HBOT stimulates the formation of new blood vessels and accelerates the healing process for stubborn wounds.
Conditions Treated
The clinic specializes in managing a wide range of chronic wounds, including diabetic ulcers, pressure sores, venous stasis ulcers, and wounds related to vascular insufficiencies. These conditions often require specialized care to address underlying issues contributing to the wound’s persistence. Dr. Badam and her team focus on identifying the root cause of the wound and implementing targeted treatments to achieve optimal healing outcomes.
Expertise and Compassionate Care
Dr. Manjulatha Badam brings a wealth of experience and expertise to Vayu Advanced Wound Clinic & Hyperbarics. As a board-certified physician in Wound Care and Hyperbaric Medicine, she is committed to delivering compassionate care that prioritizes patient well-being. Her approach emphasizes not only treating the wound but also addressing the holistic needs of each individual, ensuring comprehensive and personalized care throughout the healing process.
Patient-Centered Approach
At Vayu Advanced Wound Clinic & Hyperbarics, patient satisfaction and comfort are paramount. The clinic’s team understands the physical and emotional challenges associated with chronic wounds and strives to create a supportive environment for every patient. From the moment you schedule your initial consultation to your follow-up appointments, you can expect attentive care and clear communication regarding your treatment plan.
Why Choose Vayu Advanced Wound Clinic & Hyperbarics?
Choosing Vayu Advanced Wound Clinic & Hyperbarics means choosing specialized care that makes a difference. Here’s what sets them apart:
Specialized Expertise: Dr. Manjulatha Badam’s specialized training and certifications ensure that you receive the highest standard of care for complex wound issues.
Advanced Technology: The clinic is equipped with state-of-the-art facilities, including hyperbaric chambers, to deliver effective treatments tailored to your needs.
Comprehensive Care: Beyond treatment, the clinic offers education and support to help patients and their families understand wound care management and prevention strategies.
Proven Results: Many patients have experienced significant improvements in wound healing and quality of life under the care of Dr. Badam and her team.
Schedule Your Evaluation Today
If you or a loved one is struggling with a non-healing wound, take the first step towards healing by scheduling an evaluation at Vayu Advanced Wound Clinic & Hyperbarics. Conveniently located in San Antonio, their clinic provides accessible and compassionate care focused on achieving positive outcomes for every patient.
To schedule your appointment, feel free to call us. Whether you require hyperbaric oxygen therapy or other advanced wound care treatments, Vayu Advanced Wound Clinic & Hyperbarics is here to support you on your journey to recovery.
To Schedule an Appointment Call Us:+1 210-651-1112
Address: 8666 Huebner Rd., Suite 220 San Antonio, TX 78240.
0 notes
Text
What is the common use of oxygen in hospitals?
Oxygen is commonly used in hospitals for a variety of essential medical purposes, primarily to support patients with respiratory issues. Oxygen therapy helps maintain adequate oxygen levels in the blood, ensuring that tissues and organs function properly. Overall, oxygen is an indispensable component of hospital care, playing a crucial role in both acute and chronic medical treatments to ensure patients receive the necessary support for their respiratory needs.

Oxygen therapy: Administered to patients with respiratory conditions like chronic obstructive pulmonary disease (COPD), pneumonia, asthma, and heart failure to maintain adequate blood oxygen levels.
Surgical support: Provided to patients undergoing surgery to ensure stable oxygen levels while under anesthesia.
Emergency medicine: Used to treat patients who have experienced trauma, heart attacks, or strokes, where rapid oxygen delivery is crucial for survival.
Neonatal care: Essential for premature infants with underdeveloped lungs, supporting their breathing and development.
Hyperbaric oxygen therapy (HBOT): Used to treat decompression sickness (common in divers), serious infections, and non-healing wounds due to diabetes or radiation injury by delivering oxygen at high pressure.
Chronic conditions management: Helps manage long-term respiratory diseases, ensuring patients can maintain their oxygen levels and improve their quality of life.
Critical care: Integral in intensive care units (ICUs) for patients with severe illnesses or injuries requiring continuous monitoring and oxygen support.
0 notes
Text
Addressing Non-Healing Wounds: Insights into Oxygen Wound Therapy for Enhanced Healing
Dealing with non-healing wounds can be challenging, but innovative therapies like oxygen wound therapy offer promising solutions. Explore the dynamics of non-healing wounds and the benefits of oxygen wound therapy in promoting effective healing.

Understanding Non-Healing Wounds
1. Challenges in Healing:
Non healing wound, often associated with conditions like diabetes or poor circulation, face challenges in the normal healing process, leading to chronicity.
2. Contributing Factors:
Factors such as infection, impaired blood flow, or underlying health issues may contribute to the persistence of non-healing wounds, requiring targeted intervention.
3. Wound Types:
Non-healing wounds can take various forms, including pressure ulcers, diabetic foot ulcers, or venous leg ulcers, each requiring a specific approach to achieve successful healing.
4. Impact on Quality of Life:
Chronic wounds not only impact physical health but can also significantly affect the overall quality of life, emphasizing the importance of effective treatment.
Oxygen Wound Therapy: A Breath of Fresh Healing
1. Enhanced Oxygen Delivery:
Oxygen wound therapy, also known as hyperbaric oxygen therapy (HBOT), involves delivering high levels of oxygen to the wound site, promoting improved cellular function and healing.
2. Microbial Control:
Oxygen-rich environments are inhospitable to many bacteria, aiding in the control of infections and creating a favorable setting for wound healing.
3. Stimulation of Angiogenesis:
Increased oxygen levels stimulate the formation of new blood vessels (angiogenesis), enhancing blood flow to the wound and promoting tissue regeneration.
4. Reduced Inflammation:
Oxygen therapy helps reduce inflammation, a critical factor in chronic wound healing, creating an environment conducive to the natural healing process.
Collaborative Care for Optimal Results
1. Comprehensive Wound Assessment:
Thoroughly assess the wound's characteristics, underlying causes, and any contributing factors to tailor an effective treatment plan.
2. Multidisciplinary Approach:
Collaborate with a multidisciplinary team, including wound care specialists, hyperbaric medicine experts, and primary care providers, to optimize care and outcomes.
3. Patient Education:
Educate patients on wound care practices, lifestyle modifications, and the importance of adherence to the prescribed treatment plan to achieve successful healing.
Empowering Healing with Oxygen Wound Therapy
Non-healing wounds can be challenging, but with advancements like oxygen wound therapy, there's hope for enhanced healing. Consult with healthcare professionals to explore whether oxygen wound therapy is a suitable option for your specific situation. Together, we can empower healing and improve the overall well-being of individuals dealing with non-healing wounds.
#diabetic foot ulcer#venous stasis ulcer#wound care ulcer#wound healing and diabetes#non healing wound#leg infection in diabetic#pressure ulcer care#diabetic foot infection#ulcers on feet#oxygen wound therapy
0 notes
Text
What is the best way to treat diabetes foot ulcers?
The best way to treat diabetes foot ulcers involves caring for the wound and managing diabetes properly. Here's a simplified explanation with a focus on readability:

Treating Diabetes Foot Ulcers:
Clean and Protect the Wound: Gently wash the sore with mild soap and water. Put on special cream and cover it with a clean bandage to keep it safe from germs.
Relieve Pressure: Try not to put too much weight on the sore foot. You can use special shoes, cushions, or casts to reduce the pressure. This helps the wound heal without more harm.
Control Blood Sugar: Keep your blood sugar levels in check. Follow your doctor's advice about taking medicines, eating well, and staying active to manage diabetes properly.
Take Antibiotics: If the sore gets infected, your doctor may prescribe antibiotics to fight the infection. Make sure to take them exactly as your doctor tells you.
Remove Dead Tissue: Sometimes, a healthcare professional will need to remove dead tissue from the sore to help it heal. This is called "debridement."
Hyperbaric Oxygen Therapy: In special cases, you might need to breathe pure oxygen in a chamber to speed up healing.
Visit Your Doctor: Regularly see your doctor to check how the sore is doing. They'll ensure it's getting better and not worse.
Learn About Foot Care: Get educated on how to take care of your feet. Check them every day, wear proper shoes, and keep them clean.
Change Your Habits: If you smoke, quitting can make a big difference. Smoking harms blood flow, making it harder for the sore to heal.
Remember, early and careful treatment of Diabetes Foot Ulcers is crucial. Always follow your doctor's advice, and if you have any concerns or problems, don't wait – seek help promptly. Properly managing diabetes is key to preventing future ulcers and keeping your feet healthy.
#diabetic foot ulcer cure#diabetic foot ulcer management#health#nutrition#medicine#diabetic foot infection treatment#hospital#diabetic foot ulcer#diabetic foot care#diabetes#actually diabetic
0 notes
Text
Breathing New Life: Exploring the Healing Wonders of Hyperbaric Oxygen Chambers
CRYO-SCIENCE has steadfastly remained at the forefront of innovative wellness and healing technologies, consistently pioneering approaches that harmonize advanced science with health. In a world where we are continually seeking new ways to enhance our wellbeing, optimize recovery, and uphold our health, the emphasis has shifted toward exploring scientific marvels that enable these pursuits. A shining example of this exploration is the fascinating world of Hyperbaric Oxygen Chambers.
The science behind Hyperbaric Oxygen Chambers is as captivating as the myriad of health benefits they promise. These chambers are designed to immerse an individual in an environment where atmospheric pressure is significantly increased, typically about 1.5 to 3 times the normal pressure. Within this encapsulating space, the air is enriched, teeming with 100% pure oxygen, contrasting significantly with the 21% encountered under standard atmospheric conditions. But what are the intricate details of how a Hyperbaric Oxygen Chamber truly contributes to our healing and wellness?
A Voyage Into Enhanced Oxygenation
Upon entering a Hyperbaric Chamber, the body is enveloped by this high-pressure, pure oxygen environment. The elevated pressure causes the blood to assimilate more oxygen than it typically would, thereby supercharging the body's capability to transport oxygen to cells, tissues, and organs. This advanced method of delivering higher oxygen levels to where it is needed accelerates the body’s natural healing processes and augments the function of cells and tissues.
The hyperbaric environment essentially amplifies the body's ability to repair and regenerate. When injuries or infections occur, certain areas may require more oxygen to initiate and sustain the healing process. The oxygen-rich blood derived from Hyperbaric Oxygen Chamber therapy permeates areas where circulation might be diminished or blocked, fostering a more optimal healing environment and instigating various physiological healing processes.
CRYO-SCIENCE: Pioneering Hyperbaric Innovations
Dedication to authentic science and genuine care for enhancing human recovery and wellness are the pillars that guide CRYO-SCIENCE. The company has judiciously harnessed the power and potential of Hyperbaric Oxygen Chambers, melding scientific prowess with an unwavering commitment to health.
In the realm of regenerative medicine, this technology is not merely a tool; it is a vessel that propels healing, recovery, and wellness into new dimensions. CRYO-SCIENCE, with its lineage of expertise, ensures that the potential of the Hyperbaric Chamber is fully unlocked, providing an experience that is not only therapeutically profound but also meticulously safe and carefully tailored to individual needs.
Bridging Recovery and Innovation
Delving deeper, one discovers that Hyperbaric Oxygen Chambers serve as a bridge, connecting innovative scientific technology with the primordial power of oxygen, the life-giving element. Oxygen is crucial for the production of energy in our bodies, pivotal in generating adenosine triphosphate (ATP). A boost in oxygen levels can facilitate enhanced ATP production, thus optimizing energy availability and utilization within the body.
It's essential to recognize that the benefits of Hyperbaric Oxygen Chamber therapy are multi-faceted, encompassing an array of medical and wellness realms. From assisting in the healing of wounds, managing chronic conditions, enhancing recovery post-surgery, to even fostering overall wellness and vitality, the applications are impressively extensive.
Real-Life Impact: Testimonials and Triumphs
Numerous accounts illustrate the tangible impact and triumphs associated with Hyperbaric Chamber therapy. From athletes who have expedited their recovery timelines to individuals navigating the complexities of chronic conditions, the stories are both inspirational and reflective of the vast potential housed within these chambers of healing.
Indeed, for those who have experienced enhanced recovery and revitalization, the Hyperbaric Oxygen Chamber serves as more than a technological marvel; it is a sanctuary where their bodies are empowered to initiate and amplify their inherent healing capabilities.
The Future of Healing with CRYO-SCIENCE
As we gaze into the future, the integration of Hyperbaric Oxygen Chamber technology within health and wellness practices is not merely a possibility; it is an inevitable evolution, propelled by the promising results and the relentless pursuit of innovations like those from CRYO-SCIENCE.
In an era where the synergy between technological advancements and healthcare is more pivotal than ever, companies like CRYO-SCIENCE are not just participants; they are trailblazers, contributing to the dawn of a new age in wellness and recovery.
Through rigorous research, continuous innovation, and a deep-seated commitment to enhancing quality of life, CRYO-SCIENCE is not merely administering Hyperbaric Oxygen Chamber therapy. It is masterfully orchestrating a symphony of science, technology, and health, creating harmonies that echo through the realms of healing, wellness, and beyond.
In essence, the Hyperbaric Chamber, under the esteemed guardianship of entities like CRYO-SCIENCE, is breathing new life into our collective journey towards optimized health, redefining the boundaries, and expanding our horizons in the enthralling universe of scientific wellness.
0 notes
Text
HBOT's Cutting-Edge Approach to Diabetic Foot Wound Treatment

Introduction:
In the realm of modern medical advancements, Hyperbaric Oxygen Therapy (HBOT) has emerged as a cutting-edge approach with immense potential in the field of diabetic foot wound treatment. With the year 2023 ushering in new possibilities and discoveries, it's crucial to delve into the latest insights regarding HBOT and its transformative impact on addressing diabetic foot wounds. Let us explore the key advancements, benefits, and implications of utilizing HBOT for diabetic foot wound care.
The Diabetic Foot Wound Challenge: A Growing Concern in 2023
The rising prevalence of diabetes worldwide has contributed to an increase in diabetic foot wounds, a complex issue that requires effective interventions. According to recent data from authoritative sources, diabetic foot ulcers affect millions globally, and the challenge is further exacerbated by potential complications such as infections and amputations.
HBOT Unveiled: A New Horizon in Diabetic Foot Wound Care
Amid this healthcare landscape, advanced wound care and hyperbaric medicine shines as a beacon of hope. HBOT involves the administration of pure oxygen in a pressurized chamber, facilitating the delivery of oxygen to damaged tissues. Studies suggest that heightened oxygen levels can stimulate cellular repair, boost the immune system, and enhance blood flow to expedite wound healing. This approach has shown remarkable promise in addressing diabetic foot wounds.
Embracing Innovation: HBOT's Unique Mechanism for Healing
How does HBOT work its magic on diabetic foot wounds? Within the hyperbaric chamber, patients experience an increased oxygen concentration, promoting the formation of new blood vessels and improved circulation to the wound site. This process aids in reducing inflammation, combating infection, and nurturing tissue regeneration, pivotal factors in diabetic foot wound recovery.
The 2023 Outlook: Integrating Science and Technology for Optimal Outcomes
This year, the integration of science and technology has paved the way for enhanced precision in administering HBOT. Advanced monitoring systems ensure that patients receive the right dosage of oxygen, while innovative hyperbaric chamber designs guarantee a comfortable and safe experience. These advancements amplify HBOT's effectiveness in treating diabetic foot wounds while minimizing potential risks.
The Path Forward: Empowering Patients with HBOT
As the year progresses, the medical community recognizes that empowering patients with knowledge is integral to their healing journey. HBOT not only offers a groundbreaking approach to diabetic foot wound treatment but also encourages patients to actively participate in their recovery. With its potential to expedite healing, prevent complications, and potentially reduce the need for invasive procedures, HBOT stands as a beacon of hope for individuals battling diabetic foot wounds.
Conclusion: Charting New Frontiers in Diabetic Foot Wound Care
In this era of medical innovation, HBOT's cutting-edge approach is redefining the landscape of diabetic foot wound treatment. The confluence of scientific understanding, technological advancements, and patient empowerment has led to a new chapter in healthcare, one where diabetic foot wounds are met with targeted solutions that foster healing and improve quality of life. As we progress through, the potential of HBOT offers a glimmer of hope for a healthier future for individuals navigating the challenges of diabetic foot wounds.
NexGen Hyperbaric, LLC
Hyperbaric Room, 2205 Cordillera Way, Edwards, CO 81632
+18885674302
0 notes
Text
A Half-Truth is a Whole Lie

** I'm from the government and I'm here to help. ** We're doing everything humanly possible to get your better. ** I have nothing but your best interests in mind. ** All men are created equal. ** Secretary of Defense McNamara's and Vice President Cheney's justifications for going to war. ** To care for him who shall have borne the battle, and for his widow, and his orphan. Let’s confront an obvious “truth” facing us: despite obvious differences of opinion about the “best” way forward as a society, we are generally in agreement that we can fix problems. Scientists have split problems into “tame” and “complex” and “wicked.” “Tame” problems have a clear definition, and it is easy to identify the point at which they are solved . Complex problems have a clear agreement on the nature of the problem, but not on the solutions . In contrast, wicked problems lack agreement on both their definition and their solution. They are people problems, not math or science problems. A wicked problem is a social or cultural issue or concern that is difficult to explain and inherently impossible to "solve." Examples of wicked problems today include things like education standards, tax policy, health care, climate change, affirmative action, when to go to war, and immigration. And, of course, how to treat and heal brain wounds. Even the definition of “brain wound” is a wicked problem when doctors aren’t trained in the new science. Wicked problems never have straight-forward solutions. By their very nature, wicked problems are human problems. When elevated in the political arena, wicked problems can’t be solved, only managed. It’s that old dilemma: do you want to make a statement, or do you want to make progress? Unless people who disagree really want to make progress, there’s no managing a wicked problem: there’s only a dialogue of the deaf that results in continued suffering, lack of progress, accusations, prevarication, finger-pointing, and resentment. Let’s face it: politics is more and more running from wicked problems. Even tame problems like seat belt use started out as am wicked problem which eventually was tamed by resort to math, engineering, and economics and gradual demonstrations of results. Lately, polarized politics turns all problems into wicked problems. Thus, politics has become a series of half-truths dressed up as policy statements that become rallying cries and wish lists. The HARD work of compromise is necessary to turn wicked problems into a series of small steps toward legislative compromise and lasting change. Not a solution, but a series of manageable steps and compromises that equal progress and positive change. Concerning Veterans, four half-truths that have become whole lies are instructive. One, service members have been told that there’s little that can be done for Traumatic Brain Injury (TBI) other than pass through a variety of palliative care facilities: the NICoE, DVBIC, Intrepid Spirit Centers, PREP programs, specialized care, and a seemingly endless set of appointments for drug distribution, talk therapy, physical and occupational and various therapies designed to allow patients to learn new ways to live with the new, sub-standard normal. Current reports from the DVBIC at Walter Reed belie the advertisements: “The underlying goal of DVBIC is to ensure that active duty military and veterans with brain injury receive the best evaluation, treatment, and follow-up.” It is at best only half true. More and more patients report unwillingness to properly diagnose TBI, choosing “mental health” or PTSD as the diagnosis. Treatments ignore a proven, safe, and effective use of Hyperbaric Oxygen Therapy (HBOT). The VA and Military medicine continue in their ignorance about the proven science, including ignoring positive results with patients using HBOT after leaving Walter Reed. Two, Veterans with Diabetic Foot Ulcers (DFUs) are rarely told that they can probably avoid lower limb amputations if only the VA would routinely use an on-label, proven, insured, and widely available use of HBOT. There is an implied promise that VA doctors will use EVERY means available to avoid amputations. The VA’s malignant behavior in NOT informing patients about the availability of HBOT outside the VA means that patients get a half truth: we are following a healing protocol where the ultimate path may be amputation. Since the protocol does not include HBOT as an option, the VA reports the following harrowing numbers: 796,340 Veterans have died from Diabetic Foot Ulcer (DFU) and Lower Limb Amputation (LLA) in the past 22-years, more than all the Veterans KIA in all the U.S. Wars (623,982) since the beginning of World War I. Approximately 94% were not offered HBOT treatments. Three, numerous Veterans and other USG employees have been victimized by Havana Syndrome (aka Anomalous Health Incidents or AHI). The overwhelming majority of those who have come forward have not been properly diagnosed for the injuries they experienced. A widening gulf between promises from the USG related to care, insurance, treatments and support are honored in the breach. Leaving aside the politics of the origins, methods, timing, responsibility, and continuing attacks, the victims have been mistreated and effectively told that they are no longer worthy of honorable treatment and care. Instead of adequate treatment of what appears to be traumatic brain injuries in a majority of the cases, victims receive limited care, limited financing of care, abuse during care, and a cold shoulder from parent agencies as their lives and careers go downhill. Imagine being told that your headaches, migraines, fatigue, balance, mental abilities, hearing loss, memory, anger, depression and more are in all probability a result of a mass psychogenic illness or, worse, an attempt to get increased disability payments? One struggles to find the half-truth in the on-going saga of a government abandoning its very best. Four, service members affected by BLAST overpressure are receiving renewed interest as a result of work in the Senate Armed Services Committee. A parade of government witnesses continues to affirm that they are doing everything humanly possible, even though it is common knowledge that DOD is not doing enough to prevent injuries. Here’s a half truth: DOD and the VA claim to be learning from their own research about BLAST overpressure. The other part of the equation that is a whole lie is that neither DoD nor the VA will use HBOT to heal the brain wounds resulting from BLAST overpressure. This is especially onerous since doctors inside Marine units prescribe HBOT for TBIs, allowing not-for-profit HBOT clinics and foundations to pay for the brain wounds. Despite the successes in the TreatNOW Coalition clinics, TBIs have not even been adequately diagnosed in service members committing suicide from the very units called out by the New York Times as suffering inordinate numbers of brain casualties. The validity of using HBOT for wound healing to the brain is validated in the most recent research. Unsurprisingly, delivering oxygen under pressure safely and economically leads to effective wound healing. The FDA already approves HBOT for wound healing. That statement is true. What would make it even more true is if medicine recognized that "invisible wounds" should be treated as wounds. HBOT is essentially already on-label when the new science of brain wounding is taken into account. Numerous other interventions for brain wounds with comorbid maladies have a much better chance of effectiveness when the concussion cascade is interrupted, healed, and reversed. That statement is also generally true. The half-truth and, thus, whole lie, is that medicine in the DoD and the VA claim to be keeping up with the new science in their Centers of Excellence. Yet they disdain and ignore the Mechanisms of Action of brain wounding, and the interventions in use around the world that are healing those wounds. The sad fact is also that the VA and DoD persist in continuing to repeat the lies that their research proves that HBOT is unproven, unsafe, ineffective, costly, risky, or worse. The rest of the world and over 31,000 satisfied HBOT patients -- among them over 12,000 active duty and Veterans -- know the truth revealed in over 21 peer-reviewed clinical trials. ****************************** The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help end symptoms of PTSD, get patients off most of their drugs, and heal brain wounds to end the effects of BLAST injury, mild TBI Persistent Post Concussive Syndrome, and polytrauma from AHI and Burn Pits. Diabetic Foot Ulcers have become a major emphasis. www.treatnow.org Heal Brains. Stop Suicides. Restore Lives. TreatNOW Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made Read the full article
#blastinjury#brainhealth#braininjury#brainwounds#DFU#HBOT#HBOTTreatment#HealingwithHyperbarics#hyperbaricchamber#PTSD#TBI#traumaticbraininjury#TraumaticBrainInjury#Veterans
0 notes
Text
https://delhi.apollohospitals.com/blog/hyperbaric-medicine/
Delhi Apollo Hospital is a renowned healthcare provider offering advanced medical care in various specialties. It is one of the leading hospitals in India and has been providing world-class healthcare services for more than two decades. It is a multi-speciality hospital with a wide range of treatments and services in the field of cardiology, neurology, urology, nephrology, gastroenterology, orthopaedics and many more.
The hospital is renowned for its Hyperbaric Medicine department, which is one of the best in the country. Hyperbaric Medicine is a specialized form of medical treatment which uses a chamber filled with pressurized oxygen to increase the amount of oxygen in the body. This helps in the healing of various conditions such as traumatic brain injury, decompression sickness, carbon monoxide poisoning, and other serious medical conditions. It is also used in combination with other treatments such as chemotherapy and radiation therapy. At Delhi Apollo Hospital, the Hyperbaric Medicine department is equipped with the latest technology and has a team of highly experienced and well-trained experts who provide the highest level of medical care. The department is dedicated to providing the best possible medical care and treatment to its patients.
The team of experts provide a comprehensive range of treatments and therapies for a variety of medical conditions. The Hyperbaric Medicine department at Delhi Apollo Hospital offers a variety of treatments including hyperbaric oxygen therapy (HBOT), wound care, and hyperbaric chamber maintenance. The team of experts have a wealth of experience and knowledge in the field of Hyperbaric Medicine and can provide customized solutions to meet the individual needs of each patient. Delhi Apollo Hospital also provides research and education on Hyperbaric Medicine. The staff at the department are regularly involved in various research projects to improve patient outcomes and advance the field of Hyperbaric Medicine.
The hospital also hosts workshops, seminars, and conferences to spread awareness about the benefits of Hyperbaric Medicine. At Delhi Apollo Hospital, the Hyperbaric Medicine department provides the highest quality of care and treatment to its patients. The team of experts is committed to providing the best possible care and treatment to its patients. The hospital is well-equipped to handle any medical emergency and provides a supportive environment for its patients. Delhi Apollo Hospital is the perfect place for patients looking for quality Hyperbaric Medicine treatments. The hospital provides the best possible medical care and treatment to its patients and ensures that they get the best possible outcome from the treatment.
#Hyperbaric Medicine#best hospital in delhi#cardiologist in delhi#best heart hospital in delhi#gastroesophageal reflux disease#best cancer hospital in delhi#delhi heart hospital#what is robotic surgery#robotic surgery in india
0 notes
Text
Amniotic Membrane Market: Significance & Global Performance
Amniotic membrane or amnion, a thin membrane on the inner side of the fetal placenta and composed of the epithelium, has emerged as an ideal source for tissue transplantation. Moreover, amnion has an array of biological properties, making it attractive for use in various surgical procedures, including ocular surface reconstruction and tissue engineering.
The advancements in anatomy have triggered significant investments in research and development of amniotic membrane applications. While AM has shown beneficial results in burn injuries, the upsurge in R&D investments has increased its use in eye surgery, cell therapy, stem cell research, and more, boosting the amniotic membrane market growth prospects.

In fact, the identification of new stem cells has increased the membrane’s potential, making it ideal for developing regenerative medicines. For instance, Organogenesis Holdings Inc, a leading regenerative medicine company, gained approval from the US FDA for ReNu, a cryopreserved amniotic suspension allograft, to manage symptoms related to knee osteoarthritis.
Amniotic Membrane Market - Global & Regional Trends
As per estimates, the global amniotic membrane market will display revenue growth at a CAGR of 7.01% during the forecast period 2022-2028.
Considering the evolving healthcare sector, the amniotic membrane market is expected to witness tremendous growth in the Asia-Pacific nations. Estimates suggest that approximately half a billion people in the region will be 65 or older by 2025. This change in demographics, in addition to a shift in consumer expectations, will widen the market’s scope. In this regard, the growing demand for chronic care management will expand amnion application in ophthalmology, burn injuries, and cosmetic surgeries, among others.
Additionally, amniotic membrane transplantation has gained momentum in various conjunctival and corneal diseases, signaling opportunistic growth for players in the APAC region. Considering its growth in North America, amnions have proven advantageous in treating limbal stem cell deficiency, providing support and protection to transplanted limbal tissues and stem cells. Recently, in Canada, numerous techniques have been developed to dehydrate amnion while preserving the wound-healing properties to formulate a temperature-stable allograft.
Furthermore, the United Kingdom is the center of research and development of amniotic membrane applications in Europe. Several hospitals, such as NuVision, have gained expertise in providing AM treatments. Amniotic membrane treatments are gaining center stage across the nation, given the technological advancements. For instance, in November 2021, several ophthalmologists shared their innovations of AM application in treating ocular surface conditions through a webinar sponsored by NuVision Biotherapies Ltd.
Market by Application – Expert Outlook
Surgical Wounds: Human amniotic membrane has been used for treating acute and chronic wounds, decreasing infection and pain while accelerating the healing time. The surgical wound segment dominates the overall market and is expected to maintain its stronghold till 2028. Although a plethora of wound dressings are available, chronic wounds remain a major medical concern. As a result, chronic wounds awareness programs largely support amnion application. For instance, the Wound Healing and Hyperbaric Center at Carteret Health Care, a Healogic Network member, is engaged in raising awareness of chronic wounds, providing advanced therapies.
Ophthalmology: The rise in chronic and infectious diseases has resulted in a global rise in surgeries, boosting the market’s potential. Amniotic membrane is rapidly used in ophthalmic surgeries to initiate faster recovery and decrease inflammation. Amnion has become crucial in eye treatments, given its anti-scarring and anti-inflammatory properties. For instance, Bio Tissue Inc offers AmnioGraft to treat ocular surface indications like corneal ulcers, dry eye, chemical burns, etc. Besides, AM is highly preferred in developing regions since it is cheaper than allografts.
Competitive Analysis
For any company, acquisitions and agreements ensure expansion in business footings. Acquisitions, for instance, are quicker, cheaper, and less risky compared to other methods to extend volume sales. On the other hand, agreements are crucial to eliminating disagreements, confusion, or changes that may transpire during the course of the business period.
Notable acquisitions and agreements that support the market’s development:
In February 2021, Katena Products Inc, a leading provider of premium ophthalmic instruments and devices, announced the acquisition of ASICO LLC to expand the ophthalmic surgical product line and lead in the innovation of new products.
Integra LifeSciences Corporation, in January 2021, acquired ACell Inc and its proprietary MatriStem UMB to offer comprehensive wound management solutions.
Celularity Inc and Oncternal Therapeutics Inc entered into a research partnership in September 2021 to examine placental-derived cellular treatments.
Celularity also collaborated with Imugene Ltd in August 2021 to employ Imugene’s CD19 oncolytic virus technology and its CD19 CYCART-19 to remedy solid tumors.
In Conclusion,
The amniotic membrane market has shown rapid and promising results in healing damaged tissues. From chemical burns to ulcers to the cornea, amnions have emerged as suitable membranes in wound care management. This indicates that the use of AM in medicine and therapies is expanding in various branches of medicine.
#Amniotic Membrane Market#amniotic membrane#healthcare and wellness#healthcare#lifesciences#market research reports#market research report#triton market research
0 notes