#what worsens parkinson's disease
Explore tagged Tumblr posts
Text
Effective Treatment for Parkinson's Disease - Know Here
Parkinson's disease is a common problem that affects many people around the world. It makes it hard to move, causes shaking, and makes the body feel stiff.
These symptoms can make everyday activities difficult. But there are ways to deal with Parkinson's disease and make life better. Learning about the treatments available and making small changes in your daily life can really help.
In this blog, we'll talk about the different treatments you can try for Parkinson's disease and how making simple changes in your daily routines can make a big difference.
There are lots of things you can do to help with the symptoms, like taking medicine or trying different therapies.
Also, knowing what makes Parkinson's symptoms worse and being careful about what you eat can really help manage the condition.
By understanding the different stages of Parkinson's disease and working with top psychiatrist in Patna who know a lot about it, you can feel more confident about dealing with it and hope for a better quality of life.
What causes Parkinson's disease
Parkinson's disease starts when brain cells that produce dopamine, an important chemical, begin to function poorly. Experts believe that a mix of genetics and environmental factors plays a big role.
Getting older, having family members with Parkinson's, or being exposed to certain chemicals can increase the chances of getting the disease.
The problem begins when the cells making dopamine start to die off, causing issues with how the brain communicates with itself. This results in symptoms like shaking and difficulty in moving smoothly.
Being older than 60, having family members with Parkinson's, or being exposed to certain chemicals can raise the risk of getting it. Knowing about these things helps doctors find ways to treat and prevent it from getting worse.
Parkinson's disease stages
Parkinson's disease moves through different stages, each with its own challenges.
At first, the signs might not stand out and could be missed easily. But as time goes on, people may notice clearer symptoms, both physical and non-physical.
Doctors need to know about these stages so they can help at the right time. In the beginning, someone with Parkinson's might just have a bit of shaking or stiffness.
But as the disease gets worse, they may have more trouble moving around and thinking clearly. Doctors can change treatments based on these shifts to help handle symptoms and make life better.
Having regular check-ups and adjusting medications and therapies are crucial as Parkinson's progresses. Understanding how Parkinson's changes over time helps people and their families get ready for what's ahead and make sure they get the help they need.
Additionally, to understand what makes Parkinson's disease worse, it's important to watch what you eat, especially when it comes to foods to avoid with Parkinson's disease.
Some foods can make symptoms worse and lead to problems with moving and more inflammation.
These might be foods with lots of sugar, saturated fats, or processed stuff. It's a good idea to eat these kinds of foods in small amounts to help control symptoms.
Also, think about other things that can make Parkinson's symptoms worse, like stress or not getting enough sleep.
Eating a balanced diet with plenty of fruits, veggies, and lean meats can help keep you healthy while dealing with Parkinson's. Making smart choices about what you eat can help make symptoms better and improve your life if you have Parkinson's disease.
Parkinson's disease medication
When I was diagnosed with Parkinson's disease, I started exploring ways to treat it. Alongside the medicines my doctor prescribed, I also tried other treatments and adjusted my lifestyle. With guidance from my doctors, I created a plan for taking my medications that made me feel less sick and more comfortable.
Being diagnosed also helped me to understand my condition better and what might happen in the future. By taking an active role in my treatment and learning about Parkinson's disease, I took charge of my health journey and improved a lot.
By using a combination of medicines and lifestyle changes, I achieved a level of health I didn't think was possible before.
Conclusion
In conclusion, even though dealing with Parkinson's disease is tough, but there are ways to make life better. Finding the right treatment and support from experts like a psychiatrist in Patna or a top psychiatrist in Patna is crucial.
Talking to experienced doctors, including Parkinson's disease specialists, making healthy lifestyle changes, and keeping up with new treatments can give hope and help people take control of their journey with Parkinson's.
By actively participating in their treatment, making positive changes to how they live, and staying informed, individuals can face the challenges with confidence and strength, leading to a satisfying life despite the difficulties caused by the condition.
#psychiatrist in patna#Top Psychiatrist in Patna#i cured my parkinson's disease#parkinson's disease medication#what worsens parkinson's disease#foods to avoid with parkinson's disease#parkinson's disease stages#parkinson's disease specialists#what causes parkinson's disease#parkinson's disease diagnosis
0 notes
Text
Per one single request (and that is all I need to carry on) here is an expansion of my tags on this post
What even is dementia?
Basically, it's an umbrella term. It describes a set of common symptoms, primarily worsening cognitive loss.
It's kind of like saying you have a cold. A cold is not a diagnosis, it's a grouping of different illnesses, like rhino virus (the most common), influenza, covid, the list goes on.
So, you can have dementia and Alzheimer's, but you wouldn't describe yourself as having both. You'd say "I have a type of dementia, Alzheimer's disease." In the same way you'd say, "I have a cold, I think it's just a rhino virus but it's a whopping my ass."
So why'd you pick Alzheimer's for that example?
Well, Alzheimer's disease is the most common type of dementia. It's where all the stereotypes you'd know about it come from. This is gonna be a text heavy post, so have a graph

University of Queensland
Before I talk about them in more detail though, what's a brain?
Your brain is made up of segments that control different specific bits of your body.
I always knew that if you hit the back of your head you might go blind, cos the eye and sight stuff happens at the back of the head. This is true.
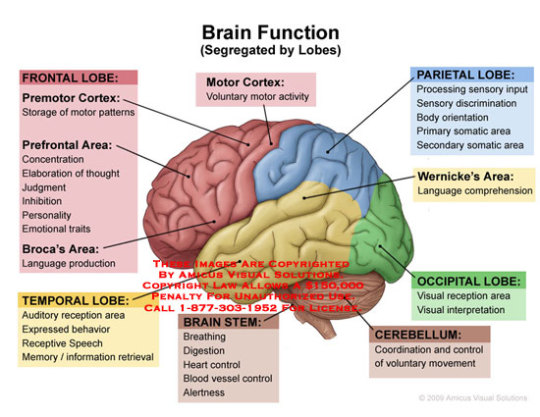
I love a copyright warning on a photo. This post constitutes personal use
Alright! An important thing about dementia is that it moves through the brain steadily, going piece by piece. It doesn't do it all at once. So you have a starting spot, and a progressive loss of cognition as it kills your neurons. We figure out the dementia type by the symptoms, cos the brain is so defined
So if you hit the back of your head, the green occipital lobe in that picture, you mess with your sight. If you lose cognition in the back of your head your eyes are seeing fine, but your cognition loss makes you process that sight incorrectly. What you see can be completely different to what other people see. This is posterior cortical atrophy, and I bring it up because we know someone who died from it, this is Terry Pratchett's dementia subtype

It's not on the above graph cos it's quite a rare type
Where's Alzheimer's start?
In the kinda middle bit, the temporal lobe. Memory, ya know. And once it takes your memory it'll move on, but it's not always the same, so people living with Alzheimer's disease will developed varying symptoms as the disease progresses, which takes many years. Sometimes people get a diagnosis of mixed dementia cos it's doing a few lobes at once. Or they have another quite different type of dementia at the some time
I'm not gonna talk about Alzheimer's much cos if you know anything about how dementia goes, you probably know it from Alzheimer's disease.
Let's go through a few others
Vascular dementia is the next biggie!
It's a curious one, this is stroke related. So, when you get a stroke you often lose cognition in the affected area of the brain. That's not dementia, that's a stroke!
But if you get lots and lots of strokes, constantly, that's a type of dementia. Cos you're getting steadily cognitively worse
(this is a good time to remind people that dementia is not a diagnosis or even a type of illness like cancer, it is a descriptive umbrella of common symptoms. The underlying causes can be wildly different)
Vascular dementia doesn't follow our moves steadily though the brain model, cos the strokes can and do happen anywhere. It's rough
What am I talking about, they're all rough. It'll get rougher
Lewy bodies dementia
Often cross diagnosed with Parkinson's disease dementia, it just depends if you get the physical or cognitive symptoms first.
Lewy bodies doesn't tend to have any memory loss. I know, no one thinks that's possible! But this is a dementia without memory loss! Cognitive loss is not the same thing as memory loss, theres other cognitive thing you can lose. That's why they're different words I guess
Of course, in all dementias eventually everything goes. Cos it's progressive, it keeps progressing
Lewy bodies is more likely to cause physical impacts like shaking and shuffling gait. You'll also hallucinate, have delusion, sleep badly, and experience mood swings.
From a care perspective, the people living with Lewy bodies disease are vastly more likely to be violent than any other person living with dementia
Robin Williams had this one, but he never knew. They confirmed via autopsy. So I'm gonna add a fun gif of him cos he was lovely

There's a lot of other disease/illness induced dementias
Huntington's turns into dementia eventually. HIV too. If you have down syndrome you have an extra gene that will always turn into dementia if you live long enough (that's one of our few 100% rates). Alcohol related dementia. So on and so forth. There's a shit tonne of types
Anyway, thats enough about disease progression. I'll talk out a few more common misunderstandings and then post
Is dementia fatal?
Sure is. Most people will die of something else while they have dementia, cos age often comes with comorbidities, but if the only thing you have is Alzheimer's disease it will still kill you. It's taking out your brain cells, eventually you'll forget how to swallow and choke.
Honestly tho it's more likely you'll die 'by accident' due to doing something you didn't realise was dangerous, like going for a walk wearing nothing at night and developing hypothermia. That is a dementia-caused death, I think we can all see that, but it'll be written down as hypothermia. So reported deaths are lower than what's true
Alzheimer's takes 10 - 30 years for the neuron loss to be extreme enough to kill you outright. Lewy bodies is more like 5 - 7 years. There's a range and the ranges are poorly defined, quiz your GP if this ever comes up in your life
It's an old person disease, right?
Overwhelmingly yes. It's considered younger onset if you're less than 65. But from the graph above you can see that's a big enough proportion to get its own slot
But kids don't get it
Sure they do, childhood dementia is a whole thing. It's awful. People are born with it. Again, dementia isn't an illness type, it's a symptom grouping. Kids can be born with progressive, worsening cognitive loss. So while it's not Alzheimer's disease, it is dementia. It's like 1 in 3000 kids have some kind of childhood dementia, and most die before they reach adulthood.
It's untreatable
It is incurable (but they keep researching!) but we have treatments for the early stages. If you or a loved one is experiencing confusion and memory loss, get moving early and you might be able to delay the worsening of symptoms for a few years. It's not a cure, but it's better than nothing. And it's all we've got
How do you, op, know?
I have a master's degree in dementia, and I work in the field. Not naming my job cos I'm not speaking for them rn, I'm just presenting what I know personally

Gonna end the post there. Send me asks or questions or whatever, I'll try and answer. If I get enough asking the same thing I'll do another post expanding on that ❤️❤️❤️
168 notes
·
View notes
Text
Also preserved on our archive
By Julia Doubleday
Last week, Jason Gale of Bloomberg put out an excellent piece about post-COVID brain damage, titled “What We Know About Covid’s Impact on Your Brain.”
The piece is broad and draws on dozens of studies to paint a concerning picture of Your Brain on COVID. It’s not the first piece to do so in the mainstream press, but it’s one of a small handful over nearly half a decade. Gale’s piece gathers evidence pointing to increased risks of dementia, Parkinson’s disease, cognitive impairment, worsening of previous psychiatric conditions, and significant drops in IQ.
The piece goes on to mention viral persistence, immune system disruption and blood clots as linked to the cognitive impacts of COVID- all three are key targets of ongoing research into Long COVID. It’s a wonderful summary to help people get a picture of the enormous amount of research pointing to brain damage following COVID.
It also begs the question: why is the public learning potentially life-altering information about a virus they’ve almost certainly contracted multiple times now from the economics section of Bloomberg? (Or from The Gauntlet, for that matter?)
As politicians pushed us all “back to normal”, a common refrain from the top was that we “had the tools” to deal with COVID, and that individuals could now make their own decisions about what sorts of risks they were comfortable taking.
I’ve written at length about the absurdity of attempting to individualize what is a collective problem. What was once a libertarian, far-right wing idea - disease control should be the territory of individuals, not society at large- was first promoted by Republicans, then mainstreamed by liberals in order to paint Biden’s failed vaccine-only herd-immunity strategy as a success.
As we settled into a cycle of endless waves of disease driven by rapidly evolving new variants, our government and public health bodies continued to promote the fantasy that everyone can make their own decisions about whether or not to get infected.
Of course, anyone who does make the “risk assessment” that catching COVID is unsafe for them is functionally shut out of society. It’s hardly a choice freely made, as the social and economic punishments for failing to “return to normal” continue to intensify.
But it wasn’t enough to snatch away free tests, vaccines and COVID treatments, all but eliminate the isolation period for active infections, and push people to view disease control as a personal responsibility. Along with instructing people to make their own “risk assessments” about COVID, our government also downplays, minimizes, and flat out denies the risks of recurrent infections.
For example: COVID causes cognitive damage. That seems like an important piece of information to give the American public while you encourage them to make risk assessments about whether to contract it every year, does it not?
What about parents deciding to send their kids back to schools with zero precautions?
Should they be warned that COVID carries a significant risk of brain damage following infection, before deciding whether it’s a good idea to let their children catch it twice a year?
And if that information is quite deliberately kept from the public by the same bodies failing to provide collective mitigations, are you asking people to make “risk assessments”, or are you just pushing them to catch COVID?
Let’s review what the public has been told about cognitive damage after COVID by the CDC, the President, the administration, and prominent media figures.
The CDC’s twitter account has never tweeted the words “cognitive damage” or “brain damage” in reference to COVID. On March 23, 2023, the CDC twitter account posted its only reference to “brain fog”:
"Common symptoms of Long COVID include fatigue, shortness of breath, fast heartbeat, & brain fog. If several weeks have passed since you had #COVID19 & you still have symptoms that interfere with your daily activities, talk to your doctor."
The current CDC Director, Mandy Cohen, has never tweeted the words “cognitive damage,” “brain damage” or “brain fog.” Neither has former CDC Director Rachelle Walensky.
In interviews, Mandy, like the rest of the administration, likes to keep it vague. Brain damage is certainly not on the talking points menu; no specific outcomes are. We are “living with COVID”. We “have the tools”. She encourages vaccinations and not masks, the tool that can actually prevent infection. In a 2023 media tour about “rebuilding trust” with the public, she repeatedly refers to the pandemic in the past tense although the pandemic is ongoing according to the WHO.
Here’s an interesting one: former White House COVID-19 Response Coordinator Ashish Jha has tweeted about COVID brain damage once: on June 17, 2021, ten months before he joined the administration. He’s since become a prominent minimizer who calls masking “fringe” and downplays post-COVID immune system dysregulation, but here’s what he had to say in June 2021:
"Important study out of UK
Worth your time
Researchers examined brain MRIs of people before and after they got COVID, matched with controls
What did they find?
Substantial loss of grey matter in those who had gotten but recovered from COVID
www.medrxiv.org/content/10.1101/2021.06.11.21258690v1 "
Wow! Seems like the kind of thing the White House COVID-19 Response Coordinator would want to share with people, rather than never mention again.
And of course, the most subtle propaganda the Administration, fellow politicians, and CDC leaders employ is their refusal to mask or appear to mitigate COVID in any way. If each COVID infection carries a risk of brain damage, surely the Director of the CDC wouldn’t constantly show up in public spaces - including airport terminals- maskless?
The President famously wouldn’t even mask after testing positive for COVID, shortly before dropping out of his re-election campaign. He, certainly, has never talked about COVID’s effects on the brain (if indeed, he’s aware of them), instead using airtime to brag about defeating disease mitigation tools. “The pandemic is over,” he incorrectly stated in the fall of 2022, “if you notice, no one is wearing masks,” he went on to say, correctly identifying his success at stigmatizing COVID prevention.
Perhaps no single outlet is more responsible for the dishonest normalizing of continual COVID reinfections than the New York Times newsletter The Morning in the hands of David Leonhardt. During the mass death event of Omicron Wave 1, Dave was the main party responsible for the “omicron is mild” narrative (a lie) that spread round the world. This February, he “both sides’d” vaccinating children because, quote, “children are extremely unlikely to become seriously ill from Covid”. As recently reported by CBS News, up to 5.8 million kids have Long COVID.
Of course, it’s fantastic that CBS News is reporting on the damage that has been done to children by returning them to classrooms without upgraded ventilation or other mitigations. It would have been better if major media outlets had conveyed this risk before millions of children were disabled.
It’s also great that Bloomberg is reporting about the brain damage that can follow COVID, deep diving the research and putting forward three of the most compelling explanations for Long COVID. But how many people, nearly five years into the crisis, know anything about this topic? How many people who are three, four, five infections in, consented to these risks when they took their masks off?
Who is responsible for this ignorance? Is it not the public health bodies and politicians charged with responding to the virus?
In interviews and speeches, it’s not only cognitive damage that our elected leaders and public health officials fail to mention. President Biden has said the words “Long COVID” a handful of times publicly. Vice President Harris has never said them. Is this not bizarre to anyone who expects the Democratic party to convey scientific facts about the pandemic to the public? Is it not clearly an attempt to hide those harmed by the ongoing “let it rip” strategy from view?
When tens of millions of Americans are disabled by a virus on your watch, never uttering the name of the disease they have is deliberate, and leaves sufferers of Long COVID struggling with stigmatization in their personal lives. By enforcing silence around Long COVID at the top of the Biden Administration, in the CDC, and among media talking heads, the public is encouraged to doubt and dismiss the condition entirely.
If this administration is so certain the public would freely choose to ignore the millions suffering from Long COVID, the risks of infection including brain damage, the high rates of transmission in our communities, and continue to opt out of mitigations and mask wearing, why do they work so hard to hide all of the above?
Why do they, along with most other electeds on the Hill, pretend they have never heard the words Long COVID, refuse to acknowledge the ongoing toll of mass infection, and continue to push testing and data out of reach? Is this the behavior of leaders who are confident that the public has freely chosen to cruelly and deliberately abandon millions of people to long-term chronic illness, and to repeatedly risk joining them?
Or is it the behavior of leaders who know they are on borrowed time, sweeping the ever-growing body of evidence and ever-higher pile of victims under the rug while stubbornly repeating that “nobody is wearing masks”?
Scientists, advocates and reporters face an uphill battle getting information about the risks of repeated COVID infections to the public. It is uphill not because of the lack of studies, resources, victims, or voices, but because those who could do the most good continue to use their platforms to do the most harm. As long as the public receives the message from our leaders that recurrent COVID infections aren’t dangerous, the truth has a high wall of propaganda to hurdle.
Nevertheless, the truth continues to emerge via studies, articles, the people who’ve been harmed, and those who care. It’s unfortunate that our public health officials and politicians will be remembered for hiding the facts about COVID, rather than disseminating them.
#mask up#covid#pandemic#covid 19#wear a mask#public health#sars cov 2#coronavirus#still coviding#wear a respirator
21 notes
·
View notes
Text






Happy 92nd Birthday veteran Scottish actress Phyllida Law, born on May *8th 1932 in Glasgow.
Wiki has 8th July on the first line of their page on Phyllida, but on the side panel has May 8th, so who knows!?
There is very little about her early life except she was born in Glasgow, the daughter of Megsie “Meg” and William Law, a journalist. She said once of he Glasgow upbringing “When you grow up in Glasgow with a Glaswegian granny, you’re taught that pride is a wicked thing. I still feel a bit like that.“ Phyllida grew up in Glasgow’s west end, just off Great Western Road, but war broke out when she was just seven and she found herself evacuated to places such as Lenzie, in Dunbartonshire, and Skelmorlie, Ayrshire.
That gave her a love for the Scots countryside which means she now splits her life between her home in London and a family cottage in Argyll. Phyllida would fit in well with the Scottish & Proud ethos, in an interview she says:
“I’m passionate about my Scots heritage. How could I not be? I can’t live without it. There’s no way I could live without those hills and it’s got to be the west coast. “I sometimes travel to Edinburgh then go up to Pittenweem or somewhere and I think to myself, ‘This isn’t Scotland.’ It’s a wonderful coastline but it’s not Scotland for me.
“When my parents lived in Glasgow they were always looking for a cottage to which they could retire. They found one in Ardentinney, so I visit that a lot.
She joined the Bristol Old Vic in 1952, from what I can gather she was first in the wardrobe department, the first pic shows her standing, from a 1952 photo. Heron screen acting credits start in 1958 and are very extensive, the pick of them are Dixon of Dock Green and a stint as the storyteller in the great children’s show Jackanory in the 60’s. It must have been during her time in the BBC’s children’s TV department she met her husband to be The Magic Roundabout narrator Eric Thompson, She has previously stated that the character of Ermintrude the cow was modelled on her.
Angels in the 70’s and of course Taggart in the 80’s as well Thomson, the variety series hosted by actress Emma Thompson in 1988, Emma just happens to be her daughter. Heartbeat, Hamish Macbeth and Dangerfield in the 90’s, Waking the dead and Doctors in the noughties has kept her busy, now in her 86th year she has still been appearing on the small screen, in The Other Wife and New Tricks during the past 8 years. Film roles include She is known for her work on Much Ado About Nothing , The Time Machine and The Winter Guest.
Phyllida spends most of her time in Argyll in a house she shares with her daughter Emma. who is spending more time looking after her mother, as she was diagnosed with Parkinson's Disease in 2915.
Phyllida constantly needs the support of a wheelchair and even assistance when washing due to the effect the condition is having on her.
Due to the progressive nature of the condition, symptoms tend to gradually worsen over time. It is common for individuals to struggle both with walking and talking at the height of the condition.
Phyllida herself spoke about the burdens of looking after an infirm parent, she looked after her mother, Meg who suffered with Alzheimer’s disease. Mego died in 1994 aged 93 after almost 20 years of being cared for by Ms Law at her mother's home in the village of Ardentinny on the west coast, near Dunoon.
Emma said of her mother “Mum is quite lame so it's a case of taking her out in a wheelchair, and making sure she takes her medication. The meds are amazing."
38 notes
·
View notes
Text
What Are the Symptoms of a Neurological Disorder?
Neurological disorders are complex conditions that affect the brain, spinal cord, and nervous system. These disorders can range from mild issues like migraines to severe conditions such as Parkinson’s disease or multiple sclerosis. Understanding the symptoms of neurological disorders is crucial for early diagnosis and treatment. In this article, we'll explore the common symptoms, causes, and how Fakeeh University Hospital can provide expert care to those affected.
Common Symptoms of Neurological Disorders
Neurological disorders can manifest in a variety of ways, depending on the area of the nervous system affected. Below are some of the most common symptoms:
1. Chronic Headaches
Headaches, especially those that occur frequently or last for extended periods, may be a sign of a neurological disorder. Migraines, cluster headaches, and tension headaches all fall into this category. If over-the-counter medication doesn't provide relief, it could be a signal that further medical evaluation is needed.
2. Seizures
Seizures are sudden, uncontrolled electrical disturbances in the brain. They can cause changes in behavior, movements, and consciousness. If you or someone you know experiences seizures, it may indicate epilepsy or another neurological issue.
3. Tingling or Numbness
Unexplained tingling, numbness, or a pins-and-needles sensation, particularly in the hands or feet, could signal peripheral nerve damage or conditions like multiple sclerosis.

4. Difficulty Speaking
Speech problems, such as slurred speech or difficulty finding the right words, are common symptoms of neurological conditions like stroke or brain injury. Immediate medical attention is often required in these cases.
5. Weakness or Loss of Coordination
Weakness in one part of the body or overall difficulty with balance and coordination may indicate issues with the brain, spinal cord, or nerves. These symptoms are often seen in conditions like Parkinson’s disease and multiple sclerosis.
6. Memory Loss and Confusion
Cognitive symptoms, such as memory loss, confusion, or difficulty concentrating, can be early signs of Alzheimer’s disease, dementia, or other degenerative neurological disorders.
7. Tremors
Tremors, or unintentional shaking of a body part, are often associated with conditions like Parkinson’s disease. If the tremors are persistent or worsen over time, it is crucial to seek medical evaluation.
8. Chronic Pain
Chronic pain that doesn’t seem to have an obvious cause, particularly in the back or limbs, can be linked to nerve damage or other neurological conditions like neuropathy.
9. Vision Problems
Blurry vision, double vision, or sudden loss of vision may indicate a neurological problem, particularly if these issues occur suddenly.
Causes of Neurological Disorders
Neurological disorders can have various causes, including:
Genetic factors: Some neurological disorders, like Huntington's disease, are inherited.
Infections: Conditions like meningitis or encephalitis are caused by infections that affect the brain.
Injury: Traumatic brain injuries (TBI) or spinal cord injuries can lead to long-term neurological problems.
Autoimmune disorders: Conditions like multiple sclerosis are the result of the immune system attacking the nervous system.
Lifestyle factors: Poor diet, lack of exercise, and exposure to toxins may increase the risk of developing certain neurological disorders.
Aging: The natural aging process can contribute to conditions like Alzheimer’s and Parkinson’s disease.
When to Seek Medical Attention
If you or a loved one experiences any of the symptoms listed above, it's essential to seek medical advice. Neurological disorders can progress rapidly, and early diagnosis is key to managing and treating these conditions effectively.
Comprehensive Neurological Care at Fakeeh University Hospital Dubai
Our Neurology Department offers comprehensive care for a wide range of neurological disorders, serving both pediatric and adult patients. Whether you're looking for a neurologist near me or a specialized clinic, we offer tailored neurological services to meet every patient’s needs.
Additionally, our neurology department is equipped with the latest technology to treat conditions affecting the central and peripheral nervous systems, including nerve and muscle disorders.
How Fakeeh University Hospital Can Help?
Fakeeh University Hospital in Dubai, we offer world-class treatment for a wide range of neurological disorders. Our team of experienced neurologists and healthcare professionals uses advanced diagnostic tools and cutting-edge treatments to ensure the best possible outcomes for our patients.
Here’s why you should choose Fakeeh University Hospital for neurological care:
Comprehensive Diagnosis: Our hospital is equipped with state-of-the-art diagnostic equipment, including MRI, CT scans, and neurophysiological testing, ensuring that we can accurately diagnose even the most complex neurological conditions.
Expert Neurologists: Our team includes leading neurologists in Dubai who specialize in conditions like epilepsy, stroke, multiple sclerosis, and more. With years of experience, they provide the best care tailored to each patient’s needs.
Customized Treatment Plans: We understand that each patient is unique. Our specialists create personalized treatment plans that may include medication, physical therapy, and lifestyle changes to manage neurological conditions effectively.
Advanced Neurological Care: We offer a range of non-surgical treatment options, helping patients recover and regain their quality of life through rehabilitation programs and ongoing care.
Holistic Care: Fakeeh University Hospital, our approach to neurological care includes not only medical treatments but also emotional and psychological support for patients and their families.

Why Choose Fakeeh University Hospital for Neurology Care?
Fakeeh University Hospital is one of the top neurology hospitals in the UAE, offering world-class care for a wide range of neurological disorders. Here are some reasons why patients choose us:
Expert Neurologists: Our team includes some of the best neurologists in Dubai, with specialists in areas such as migraine treatment, spinal disorders, and multiple sclerosis.
Comprehensive Neurological Services: We provide treatments for everything from nerve conduction studies to neurological rehabilitation, ensuring that you receive complete care under one roof.
Advanced Facilities: Our neurological care clinic is equipped with state-of-the-art technology, making us a leader in providing accurate diagnoses and effective treatments.
Patient-Centered Care: We prioritize personalized treatment plans that address each patient's specific needs, ensuring compassionate and tailored care at every step.
If you're searching for the best neurologist in Dubai, Fakeeh University Hospital is your go-to choice for high-quality neurological care. Contact us today to schedule your consultation.
Conclusion
Neurological disorders can affect every aspect of a person's life, but early detection and treatment can make a significant difference. If you're experiencing any symptoms of a neurological disorder, don’t delay in seeking professional help. At Fakeeh University Hospital in Dubai, we are dedicated to providing you with the highest level of care.
Book an appointment today to consult with our expert neurologists and take the first step toward managing your neurological health.
2 notes
·
View notes
Text
OOC // Mun's Notification
I'll be slowly going through my drafts this week. My response rate will still be slow due to my full-time job, my mental state after work, and my family situation (which I'll explain below).
Thank you for your patience!
Last week, my father was admitted to the emergency room with unknown symptoms. His strength had completely diminished, his tremors were severe, and his speech was sluggish. Initially, the doctors suspected a significant worsening of his Parkinson's disease.
Fortunately, or unfortunately, they discovered that his symptoms were actually caused by COVID.
He’s doing much better and has been moved to a rehab facility to regain strength. However, my family and I are considering whether it’s time for him to move to a nursing facility. He’s showing signs of dementia and Alzheimer’s and has bad mobility.
A nursing facility might be better for his overall health than staying at home... but it all depends on whether we can find an available facility that meets his needs, is a decent place, and costs.
So yeah, that's what's going on in a nutshell.
6 notes
·
View notes
Text
Beyond Hope chapter 1
Here is the sequel to my Daniel and Lestat fic, Beyond Metaphor.
The days pass and Lestat tells Daniel his story. Daniel challenges him every step of the way, uncaring that he’s an immortal killer that could easily snuff him out. What does that matter, when he’s already dying?
The only people who fear death are those who have something to live for.
That doesn’t mean Daniel is going to let Lestat violate him; he told him if he bit him again he could write his own damn book. Lestat had agreed that he wouldn’t bite Daniel without his permission. Daniel didn’t plan to give it, so he agreed.
At first, they stuck to Lestat’s tale. His past, his history, his version of events from the time in Rue Royale. Within two weeks, Daniel has the entire story recorded and his questions asked. He just has to write the book.
To his surprise, Lestat keeps showing up. He says to ‘supervise’ his book, but he rarely even looks at what Daniel is writing. Yet he’s there, almost every night.
“You know, I may croak before I finish this,” Daniel says from the kitchen. He’s been using the kitchen instead of his office lately to work, there’s more room and it’s easier to hobble back to the couch to take a rest.
Lestat strolls in, damp from the rain outside. The light reflecting off the moisture on his hair makes something like a halo effect. And Lestat does look more angel than devil, doesn’t he? Especially when he comes bearing gifts.
“Don’t be so morbid, mon ami,” Lestat says, sitting down the bag of Chinese take-out. It’s got a yellow smiley-face staring at Daniel. “Eat, you must keep up your strength.”
He’s said similar to Louis in the past. Almost like he cares.
Lestat catches the thought and flashes him a grin. “I’ve grown quite fond of you, Daniel.”
“Lucky me,” Daniel says dryly and pushes his laptop aside to eat. His hands have been getting tremors today, so it’s not like he’s gotten much done.
Lestat sits across from him and watches. Daniel says nothing for a second, then lets out a deep sigh, “What?”
“I noticed your tremor is back.”
“Your powers of observation astound me.”
Lestat grins, and Daniel can see fang poking out. “You resort to sarcasm when you’re afraid.”
“Afraid of what? You?” Daniel says and jabs into his low-mein. He’s provoking Lestat and he knows it, but it’s better than a talk about his frail mortality.
Lestat ignores the bait. “I accessed the internet today-”
“Welcome to the 21st century.”
Lestat continues like he didn’t speak, “I told the lovely librarian that I needed information on Parkinson’s disease. She was very helpful when I told her of my poor sick uncle.”
“Trying to gauge how much of your book you’ll have to finish yourself when I croak?” he brings his hand to his mouth as he speaks, but a tremor causes him to drop his fork.
Lestat watches it hit the table and brings his eyes up to meet Daniel’s. “Your tremor has worsened. Your movements are slower and your balance is off.”
“I noticed.”
“As did I,” Lestat says and cocks his head. He looks at Daniel for a moment, then says, “My blood could alleviate your symptoms. Not heal you, but it will help.”
Daniel drops his fork again, this time from shock. “Are you offering?”
“I told you, Daniel. I’m fond of you.”
Without thinking, Daniel’s hand comes to the amulet around his neck. He’s never had the blood from anyone besides Armand. It feels like a betrayal of sorts, to take Lestat’s. He must catch the thought because he laughs. “Still his minion after all these years?”
Daniel’s face flushes red. “I’m not-”
“Not what? In love with him?”
“No.”
Lestat smiles. “I can read minds, cher. You can’t hide from me.”
“Stay out of my head.”
Lestat holds his hands up in a mockery of surrender. “If you insist.”
After he eats, he goes back to the living room. Lestat has already wandered in and started up True Blood. Vampire media fascinates him, and he’s already forced Daniel to start multiple vampire shows and movies. He put his foot down when Lestat tried The Vampire Diaries. He’s not watching teeny-bopper melodrama, even if the cast all look like supermodels.
This is how he spends his nights. Hanging out with a vampire.
It strikes him that Lestat may be his only friend. And isn’t that just a kick in the face?
Daniel sits beside Lestat on the couch. Lestat is caught up in watching Sookie and one of her love interests suck face. Daniel can’t keep track of their names; he only watches because Lestat wants to. The absurdity of it hits him, and he wants to laugh. He’s dying; and here he is spending his last days shooting the shit with an honest to god vampire.
“Why do you keep coming around? What’s in it for you?” Daniel asks, because he has to know.
Lestat looks over to Daniel and there’s a weariness in his eyes Daniel isn’t used to seeing. Lestat smiles sadly. “Because you are my only friend as well.”
“You know I’m dying, right?” Daniel says. How will Lestat take that, if he really is his only friend?
Lestat pauses the show and looks at him intently. “You don’t have to. I would give you the dark gift, if you wanted it.”
And live forever like this? Alone and bitter for all of time. No, to live forever you need something to live for and Daniel has nothing. But the thought of death…
It terrifies him. Daniel doesn’t believe in anything, in any sort of higher power or afterlife. You live, you die, you rot. That’s all there was to it. Once it was over, it’s over. You just cease to exist.
Why wouldn’t he avoid that, if he could? The scared, desperate part of his brain says to say yes. But Daniel isn’t sure. He wanted this once. But that had been when there was Armand. When he had a reason to live forever.
Except, he doesn’t have to be alone. Lestat is his friend. If he can make friends with him, he can find others. There’s hope.
“Let me think about it.”
4 notes
·
View notes
Text
What to Expect When Diagnosed with Parkinson’s Disease

Parkinson’s disease occurs when cells in the brain that produce dopamine stop working or die, which affects coordination of body movements.
The early signs of Parkinson's disease can be subtle, including tremors, rigidity, slowness of movement, postural instability, and masked face.
Symptoms worsen over time, progressing through five stages. While there is currently no cure, treatment options include medication, physical therapy, occupational therapy, speech therapy, surgery, and lifestyle changes.
It's important to work closely with a healthcare professional to develop an individualized treatment plan that addresses specific symptoms and needs.
While Parkinson’s disease is a life-long condition, it usually takes time to get worse, and most people still have a normal life span with this condition.
4 notes
·
View notes
Text
Effective Frozen Shoulder Treatment at Kapadia Multispeciality Hospital, Mumbai
Frozen shoulder, also known as adhesive capsulitis, is a painful condition that limits shoulder movement and affects daily activities. If you're experiencing stiffness, pain, or restricted mobility in your shoulder, it's essential to seek expert medical care. At Kapadia Multispeciality Hospital in Mumbai, we provide comprehensive frozen shoulder treatment to help you regain movement and live pain-free.
What Is A Frozen Shoulder?
Frozen shoulder occurs when the tissues around the shoulder joint become inflamed and stiff, leading to pain and reduced mobility. The condition typically progresses through three stages:
Freezing Stage: Gradual onset of pain and stiffness, worsening over time.
Frozen Stage: Severe restriction in movement, but pain may slightly reduce.
Thawing Stage: Improvement in mobility as the shoulder heals.
Causes and Risk Factors
While the exact cause of frozen shoulder is unknown, several factors increase the risk:
Diabetes: Common among diabetic patients.
Injury or Surgery: Immobilization of the shoulder can lead to stiffness.
Age & Gender: More common in individuals aged 40-60, especially women.
Medical Conditions: Thyroid disorders, heart disease, and Parkinson’s disease.
Advanced Frozen Shoulder Treatment at Kapadia Multispeciality Hospital
At Kapadia Multispeciality Hospital, our team of expert doctors and physiotherapists provide a personalized approach to frozen shoulder treatment using the latest medical advancements.
Non-Surgical Treatments
🔹 Medications: Pain relievers and anti-inflammatory drugs to reduce discomfort.
🔹 Physical Therapy: Customized exercises to restore shoulder mobility.
🔹 Steroid Injections: Targeted relief from inflammation and pain.
🔹 Hydrodilatation: A minimally invasive procedure to stretch the joint capsule.
Surgical Options (For Severe Cases)
🔹 Shoulder Manipulation: Performed under anesthesia to break adhesions.
🔹 Arthroscopic Release: A minimally invasive procedure to remove scar tissue.
Why Choose Kapadia Multispeciality Hospital for Frozen Shoulder Treatment?
Expert Specialists: Highly experienced orthopedic doctors and physiotherapists.
Comprehensive Diagnosis: Advanced imaging and personalized treatment plans.
State-of-the-Art Facilities: Equipped with modern medical technology.
Patient-Centric Care: Compassionate support throughout recovery.
Regain Shoulder Mobility Today!
If you're struggling with a frozen shoulder, don’t wait for the pain to worsen. Get expert frozen shoulder treatment at Kapadia Multispeciality Hospital in Mumbai and start your journey toward recovery.
Take the first step to pain-free movement with Kapadia Multispeciality Hospital – Your trusted partner in healthcare!
0 notes
Text
How Early Detection Can Transform Outcomes in Neurological Conditions
Neurological conditions encompass many disorders that affect the brain, spinal cord, and nervous system. These conditions, if not detected early, can significantly impact a person's quality of life. Early detection plays a crucial role in improving outcomes, reducing complications, and offering better treatment options.
At GS Hospital, recognized as one of the Best Neuro Hospital in Ghaziabad and among the Top 10 Private Hospitals in Uttar Pradesh, we prioritize early diagnosis and advanced treatment for neurological conditions. In this article, we'll explore how early detection can transform neurological outcomes, the importance of timely medical intervention, and the role GS Hospital plays in offering exceptional neurological care.

Understanding Neurological Conditions:
Neurological conditions refer to disorders that affect the brain, spinal cord, and nerves. Some common examples include:
Stroke
Epilepsy
Parkinson's Disease
Multiple Sclerosis
Alzheimer's Disease
Brain Tumors
Each condition comes with its set of symptoms, complications, and treatment options. However, what remains constant is the importance of detecting these conditions at the earliest stages.
Why Early Detection Matters in Neurological Conditions:
Early detection of neurological disorders plays a crucial role in improving patient outcomes, enhancing quality of life, and minimizing long-term complications. Neurological conditions, such as Alzheimer's disease, Parkinson's disease, epilepsy, multiple sclerosis, and stroke, often progress silently before noticeable symptoms emerge. Identifying these conditions in their early stages offers significant advantages across multiple dimensions.
1. Improved Treatment Options:
Early diagnosis allows for timely initiation of treatment plans tailored to the patient’s condition.
Many neurological disorders respond better to early therapeutic interventions, reducing the severity of symptoms.
Less invasive and more effective treatments are often available in the early stages.
2. Prevention of Disease Progression:
Progressive neurological disorders, such as Parkinson's and Alzheimer's, worsen over time.
Early intervention can delay or slow disease progression, preserving cognitive and motor functions.
Preventing complications reduces the need for advanced care or surgical interventions.
3. Better Quality of Life:
Managing symptoms in the early stages can significantly improve day-to-day functioning.
Patients are more likely to maintain independence and mobility with early symptom control.
Psychological benefits, including reduced anxiety and improved emotional well-being, are significant outcomes of early diagnosis.
4. Cost-Effective Care:
Early detection often reduces the financial burden associated with long-term treatments and hospitalizations.
It minimizes the need for complex surgical procedures or intensive therapies in advanced stages.
Preventive care and early symptom management contribute to better resource utilization in healthcare settings.
5. Enhanced Support Systems:
Early diagnosis allows patients and families to plan for the future more effectively.
Access to support groups, counseling services, and rehabilitation programs can be initiated early.
Caregivers can receive timely training and guidance for managing the condition at home.
Common Warning Signs of Neurological Disorders:
Recognizing the early warning signs of neurological disorders is essential for timely diagnosis and treatment. Neurological conditions can affect the brain, spinal cord, and nervous system, leading to a wide range of physical, cognitive, and emotional symptoms. Prompt medical attention can significantly improve outcomes, prevent complications, and enhance the quality of life for those affected.
1. Persistent Headaches:
Frequent or severe headaches, especially if they worsen over time.
Headaches accompanied by nausea, vomiting, or sensitivity to light and sound.
Sudden and intense headaches that feel different from usual migraines.
2. Vision Problems:
Sudden loss of vision or blurred and double vision.
Difficulty focusing on objects or seeing flashes of light.
Changes in peripheral vision or unexplained visual disturbances.
3. Speech and Communication Issues:
Difficulty speaking clearly or slurred speech.
Struggling to find the right words or construct coherent sentences.
Problems in understanding spoken or written language.
4. Muscle Weakness or Numbness:
Weakness in one or more limbs, often on one side of the body.
Persistent tingling, numbness, or a "pins and needles" sensation.
Difficulty holding objects, buttoning a shirt, or performing fine motor tasks.
5. Loss of Balance and Coordination:
Trouble walking steadily or frequent loss of balance.
Unexplained dizziness or vertigo-like sensations.
Sudden inability to perform coordinated movements.
6. Cognitive and Memory Issues:
Persistent memory loss or forgetfulness beyond normal aging.
Confusion about time, place, or identity of people.
Difficulty with concentration, planning, or problem-solving.
7. Seizures or Involuntary Movements:
Sudden, uncontrollable jerking or twitching movements.
Episodes of blackouts or loss of consciousness.
Recurring seizures or tremors without an obvious cause.
8. Chronic Fatigue or Sleep Disturbances:
Extreme fatigue even after adequate rest.
Difficulty falling asleep or staying asleep.
Excessive daytime sleepiness or unrefreshing sleep.
The Importance of Early Detection in Neurology:
Early detection of neurological disorders is a critical factor in preventing severe complications, improving outcomes, and preserving quality of life. Neurological conditions such as Alzheimer's disease, Parkinson's disease, epilepsy, and multiple sclerosis often present subtle early symptoms that can go unnoticed without proper evaluation. At GS Hospital, recognized as one of the 10 Best Neurology Hospitals in Uttar Pradesh, early diagnosis is prioritized through cutting-edge diagnostic technologies and expert neurological care.
Key Benefits of Early Detection in Neurological Disorders:
1. Better Prognosis:
Slower Disease Progression: Timely intervention can decelerate the advancement of progressive diseases such as Parkinson’s or Alzheimer’s.
Prevent Irreversible Damage: Early treatment minimizes the risk of permanent brain or nerve damage.
Enhanced Recovery Rates: Early interventions increase the chances of partial or full recovery in conditions like stroke.
2. Improved Quality of Life:
Symptom Management: Early diagnosis allows for better control of symptoms, reducing their impact on daily activities.
Preserving Independence: Prevents severe disabilities that can limit mobility, communication, and cognitive functions.
Psychological Well-being: Patients and families are better prepared emotionally and mentally to handle the condition.
3. Cost-Effective Treatment:
Lower Long-Term Costs: Early intervention reduces the financial burden of prolonged hospital stays and complex treatments.
Reduced Dependency on Advanced Therapies: Conditions detected early often respond to non-invasive therapies, minimizing surgical interventions.
Avoiding Emergency Situations: Timely diagnosis prevents complications that could lead to costly emergency care.
4. Enhanced Treatment Options:
Wider Range of Therapies: Many treatments are more effective in the early stages of neurological diseases.
Personalized Care Plans: Early detection allows for tailored treatment strategies suited to the patient's unique condition.
Proactive Symptom Control: Preventing symptoms from becoming unmanageable improves patient outcomes.
Role of Advanced Diagnostics in Early Detection of Neurological Disorders:
Early detection of neurological disorders is crucial for effective treatment and improved patient outcomes. At GS Hospital, one of the Top Neurology Hospitals in Uttar Pradesh, we prioritize early diagnosis through state-of-the-art diagnostic tools and technologies. Our advanced diagnostic infrastructure ensures accurate identification of neurological conditions, enabling targeted and timely interventions.
1. MRI (Magnetic Resonance Imaging):
High-Resolution Imaging: Provides detailed images of the brain, spinal cord, and nervous system.
Early Abnormality Detection: Identifies tumors, strokes, multiple sclerosis, and structural brain abnormalities.
Non-Invasive Procedure: Safe and effective with no exposure to radiation.
Functional MRI (fMRI): Measures brain activity by detecting changes in blood flow.
2. CT (Computed Tomography) Scans:
Quick and Effective Imaging: Delivers rapid imaging results, especially in emergency situations.
Detailed Cross-Sectional Images: Helpful for detecting brain hemorrhages, traumatic injuries, and tumors.
Guidance for Procedures: Used to guide surgical interventions and biopsies.
3. Electroencephalography (EEG):
Brain Activity Monitoring: Records electrical activity in the brain to detect irregularities.
Seizure Diagnosis: Effective in identifying epilepsy and other seizure disorders.
Sleep Disorders: Helps diagnose neurological sleep-related issues.
Non-Invasive Procedure: Safe and painless diagnostic method.
4. Electromyography (EMG):
Nerve and Muscle Function Assessment: Measures electrical activity in muscles and nerve cells.
Neuromuscular Disorders Diagnosis: Detects conditions like ALS, peripheral neuropathy, and muscular dystrophy.
Real-Time Results: Provides immediate feedback for accurate diagnosis.
5. Lumbar Puncture (Spinal Tap):
Cerebrospinal Fluid Analysis: Helps detect infections, bleeding, or autoimmune diseases affecting the nervous system.
Diagnosis of Meningitis and Encephalitis: Essential in identifying inflammation or infection in the brain and spinal cord.
Measurement of Pressure Levels: Assesses intracranial pressure and cerebrospinal fluid abnormalities.
6. Advanced Neuro-Imaging Techniques:
PET (Positron Emission Tomography): Identifies changes in brain metabolism.
SPECT (Single Photon Emission Computed Tomography): Evaluates blood flow and brain function.
Transcranial Doppler Ultrasound: Measures blood flow in brain arteries.
Advantages of Advanced Diagnostics at GS Hospital:
Early and Accurate Detection: Enables precise diagnosis of complex neurological disorders.
Personalized Treatment Plans: Diagnostics guide customized treatment strategies.
Minimized Risk of Complications: Early identification reduces the chances of disease progression.
State-of-the-Art Technology: Access to the latest diagnostic equipment ensures top-quality care.
Why Choose GS Hospital for Neurological Diagnostics?:
Expert Neurologists: Highly experienced specialists in neurological diagnostics.
Comprehensive Testing Facilities: All major diagnostic tools under one roof.
Patient-Centric Approach: Ensuring comfort and care throughout diagnostic procedures.
Accurate Reporting: Reliable and timely diagnostic reports for better treatment outcomes.
Comprehensive Treatment Options for Neurological Conditions at GS Hospital:
At GS Hospital, recognized as one of the Best Neurosurgery Hospitals in UP, we are dedicated to providing personalized and evidence-based treatment plans for a wide range of neurological disorders. Our team of highly qualified neurologists, neurosurgeons, and rehabilitation specialists collaborates to deliver holistic care that addresses both the root causes and symptoms of neurological conditions.
1. Medication Management:
Targeted Therapies: Customized medications for conditions such as epilepsy, Parkinson’s disease, and multiple sclerosis.
Symptom Control: Effective management of pain, tremors, and muscle stiffness.
Preventive Medications: To reduce the risk of seizures, stroke, or disease progression.
Regular Monitoring: Ongoing assessment to adjust dosages and minimize side effects.
2. Surgical Interventions:
For conditions that do not respond to medications, surgical procedures offer life-changing results.
Brain Tumor Surgery: Removal of benign or malignant brain tumors with precision techniques.
Deep Brain Stimulation (DBS): Used for Parkinson’s disease and movement disorders.
Spinal Surgeries: Addressing spinal cord injuries, disc herniation, and spinal stenosis.
Minimally Invasive Techniques: Faster recovery, smaller incisions, and reduced hospital stays.
3. Rehabilitation Therapies:
Rehabilitation plays a critical role in helping patients regain independence and improve their quality of life.
Physical Therapy: Improves mobility, balance, and coordination.
Occupational Therapy: Helps patients adapt to daily activities.
Speech Therapy: Assists with speech, swallowing, and cognitive impairments.
Cognitive Rehabilitation: Enhances memory, problem-solving, and focus.
4. Lifestyle Modifications:
Lifestyle changes can significantly impact neurological health and prevent disease progression.
Balanced Diet: A diet rich in antioxidants, omega-3 fatty acids, and essential nutrients.
Regular Exercise: Improves brain function, blood circulation, and stress management.
Stress Reduction Techniques: Mindfulness, meditation, and adequate rest.
Avoidance of Neurotoxins: Limiting alcohol consumption and avoiding harmful substances.
5. Advanced Therapies and Cutting-Edge Technologies:
Neurostimulation Therapies: Used for chronic pain and neurological dysfunctions.
Botox Injections: Effective for managing muscle spasticity and chronic migraines.
Telemedicine Services: Remote consultations for follow-up care and early intervention.
Multidisciplinary Care: Collaboration between neurologists, neurosurgeons, therapists, and counselors.
6. Patient Education and Support Programs:
Condition Awareness: Educating patients and families about their condition.
Self-Management Techniques: Equipping patients with strategies for symptom control.
Support Groups: Emotional and psychological support for patients and caregivers.
Follow-Up Care: Regular check-ups to monitor progress and adjust treatment plans.
Why Choose GS Hospital for Neurological Care?:
Expert Team: Experienced neurologists, neurosurgeons, and therapists.
State-of-the-Art Infrastructure: Equipped with advanced diagnostic and surgical tools.
Holistic Approach: Focus on physical, emotional, and cognitive well-being.
Patient-Centric Care: Personalized treatment plans tailored to individual needs.
Comprehensive Facilities: All services under one roof for seamless care.
Conclusion:
Early detection is a game-changer in the management of neurological conditions. Timely intervention can prevent complications, offer effective treatments, and improve the patient's quality of life. At GS Hospital, one of the Best Neurosurgery Hospitals in UP, we are committed to providing exceptional neurological care with advanced facilities and an expert team.
If you or your loved ones are experiencing any neurological symptoms, don't delay seeking help. Early action can make all the difference in transforming outcomes.
#Best Neuro Hospital in Ghaziabad#Top 10 private hospitals in Uttar Pradesh#10 Best Neurology Hospitals in Uttar Pradesh#Best Neurosurgery Hospitals in UP
0 notes
Text
What are phantom smells a sign of - Google Search
Phantom smells, also known as phantosmia, can be a symptom of many conditions, including:
Upper respiratory infections: Colds, allergies, and COVID-19 can all cause phantom smells
Brain-related conditions: These include brain tumors, stroke, epilepsy, and Alzheimer's disease
Other conditions: These include head trauma, Parkinson's disease, and certain medications
Endocrine disorders: Hypothyroidism, a deficiency of thyroid hormones, can cause phantom smells
Psychiatric conditions: Mood disorders and schizophrenia can involve phantom smells
Phantom smells can be caused by a number of different things, including:
Overactive neurons
Problems in the nasal passageway, such as polyps
Smoking
Frequent sinus infections
Phantom smells can improve, worsen, or disappear over time, and treatments aren't always effective. If you have phantom smells that last more than a few weeks, you should see a healthcare provider to determine the cause and get treatment.
0 notes
Text
The Importance of Early Detection in Neurological Disorders
Neurological disorders, ranging from chronic headaches to life-altering conditions like brain tumors and epilepsy, can have a profound impact on an individual's quality of life. While advanced treatments and cutting-edge technology have improved outcomes significantly, the importance of early detection cannot be overstated. Timely diagnosis is often the first step in effective management and recovery.

What Are Neurological Disorders?
Neurological disorders encompass a wide range of conditions affecting the nervous system, including the brain, spinal cord, and nerves. These conditions can manifest in various ways, such as cognitive impairments, motor dysfunction, and sensory deficits. Common neurological disorders include:
Stroke: Sudden disruption of blood flow to the brain.
Parkinson’s Disease: A progressive disorder affecting movement and coordination.
Multiple Sclerosis: A condition in which the immune system attacks the protective sheath of nerves.
Epilepsy: Characterized by recurrent seizures.
Understanding the signs and symptoms of these conditions is crucial for early detection and intervention.
Why Is Early Detection Crucial?
The prognosis of neurological disorders often hinges on how soon they are diagnosed. Here’s why early detection plays such a pivotal role:
Prevention of Disease Progression: Conditions like multiple sclerosis and Parkinson’s disease are progressive, meaning they worsen over time. Early intervention can slow the progression and maintain a better quality of life.
Improved Treatment Outcomes: For disorders like stroke, timely diagnosis can be the difference between recovery and permanent disability. Treatments like clot-busting medications are most effective when administered within a critical time window.
Cost-Effective Management: Early diagnosis often means fewer complications, leading to reduced healthcare costs over time.
Better Quality of Life: Prompt treatment helps individuals manage symptoms effectively, enabling them to lead a more fulfilling life.
Signs to Watch For
Early detection relies on recognizing the warning signs of neurological issues. Common symptoms include:
Persistent headaches or migraines.
Sudden loss of vision, balance, or coordination.
Memory lapses or confusion.
Muscle weakness or tingling sensations.
Unexplained seizures.
If you or a loved one experience these symptoms, it’s essential to seek medical advice promptly.
The Role of Medical Professionals in Early Detection
Specialists like Dr. Aditya Gupta, renowned for his expertise in neurology, emphasize the importance of regular check-ups and advanced diagnostic tools. Imaging technologies like MRI and CT scans, coupled with thorough neurological exams, are instrumental in identifying disorders at an early stage.
Moreover, public awareness campaigns and health screenings are vital in educating individuals about the importance of early detection.
Conclusion
Early detection of neurological disorders is a lifesaving measure that ensures timely treatment and better outcomes. By being vigilant about the warning signs and seeking prompt medical advice, individuals can take proactive steps toward managing their health effectively.
For expert guidance and cutting-edge treatment options, consulting a specialist like Dr. Aditya Gupta can make all the difference in navigating the complexities of neurological health.
0 notes
Text
Dry Mouth Remedies: What’s New in 2025?

Dry mouth, or xerostomia, is a common condition affecting millions of people worldwide. It’s not just an uncomfortable feeling – it can also impact oral health by increasing the risk of cavities, gum disease, and difficulty speaking or swallowing. If you've struggled with dry mouth, you're not alone, and new remedies in 2025 may offer fresh hope. At Limegreen Dental Care, we’re excited to share the latest treatments and innovations designed to alleviate dry mouth symptoms and improve your quality of life.
Understanding Dry Mouth: The Basics
Dry mouth occurs when your salivary glands don't produce enough saliva, which is crucial for maintaining oral health. Saliva helps to rinse away food particles, neutralize acids, and fight harmful bacteria in your mouth. Several factors contribute to dry mouth, including:
Medications: Many prescription and over-the-counter drugs, such as antihistamines and antidepressants, can reduce saliva production.
Health conditions: Diabetes, Sjögren’s syndrome, and Parkinson’s disease are among the conditions that can cause dry mouth.
Dehydration: Not drinking enough water or excessive alcohol/caffeine consumption can leave your mouth feeling parched.
Aging: As we age, salivary production naturally decreases.
Fortunately, in 2025, new remedies and innovations are changing how we address dry mouth. Here’s a look at the latest treatments and tips.
1. Saliva Stimulants: Newer Medications and Devices
For years, the go-to medication for dry mouth has been pilocarpine (Salagen) and cevimeline (Evoxac), both of which help stimulate saliva production. However, in 2025, there are more advanced alternatives entering the market that offer better results with fewer side effects.
A promising development is the new artificial saliva sprays and gels that now feature improved formulations, providing longer-lasting moisture. These products often combine natural ingredients like aloe vera or glycerin to help soothe dry mouth. Look for those that are free from alcohol and preservatives, as these can actually worsen the condition over time.
2. Smart Hydration Systems
One of the most innovative breakthroughs in 2025 is the rise of smart hydration technology. New gadgets are available that monitor your hydration levels throughout the day and alert you when it’s time to drink more water. Some devices are designed to pair with apps on your phone, providing reminders to stay hydrated and track your fluid intake.
These systems are especially helpful for individuals with medical conditions that cause chronic dry mouth, like diabetes or certain autoimmune diseases. By staying on top of hydration, you can naturally improve your saliva production and keep dry mouth at bay.
3. Probiotics for Oral Health
Probiotics, known for supporting gut health, are now being explored for their potential in treating dry mouth. In 2025, new probiotic formulations are specifically designed to balance the oral microbiome. This can help reduce the harmful bacteria that thrive in dry conditions and encourage the growth of beneficial bacteria that contribute to saliva production.
Research has shown that oral probiotics can support a healthy oral environment by improving saliva flow and preventing the bad breath and cavities often associated with dry mouth. These probiotics come in the form of lozenges, powders, or chewable tablets, and they work to maintain moisture and a healthy balance in the mouth.
4. Hydrating Oral Care Products
Traditional toothpaste and mouthwashes can sometimes aggravate dry mouth, but 2025 has seen the emergence of specialized oral care products designed to hydrate. Look for moisturizing toothpastes and mouth rinses that include hydrating agents like xylitol, glycerin, or hyaluronic acid, which help promote moisture retention and reduce the feeling of dryness.
These products often contain a blend of soothing ingredients that not only prevent dryness but also help to rebuild and repair damaged oral tissues. Some formulas even have antibacterial properties to reduce plaque buildup, which is a common issue for people with dry mouth.
5. Bioelectric Stimulation Therapy
One of the most exciting advancements in 2025 is the use of bioelectric stimulation to promote saliva production. These devices, which are typically worn on the skin near the salivary glands, use electrical impulses to stimulate the nerves and encourage saliva flow. Clinical studies have shown that this therapy can provide significant relief for individuals suffering from chronic dry mouth, especially those undergoing radiation therapy for cancer.
While still emerging, bioelectric stimulation therapy offers a non-invasive and effective alternative to traditional treatments, especially for those who do not respond well to medications or other interventions.
6. Lifestyle Adjustments: Simple Yet Effective
While medical treatments are essential, lifestyle changes play a crucial role in managing dry mouth. In 2025, experts continue to emphasize simple habits that can make a big difference:
Chewing sugar-free gum or sucking on lozenges: Stimulates saliva production naturally.
Avoiding caffeine, alcohol, and tobacco: These substances can dry out the mouth further.
Using a humidifier: Keeping the air moist, especially at night, can prevent your mouth from becoming too dry while you sleep.
Drinking plenty of water: It’s still one of the most effective ways to combat dry mouth.
7. Collaboration with Your Dentist
At Limegreen Dental Care, we encourage regular communication between our patients and their healthcare providers to manage dry mouth effectively. Dentists play a crucial role in identifying and addressing the root causes of dry mouth, offering tailored recommendations and treatments to alleviate symptoms. With new advancements in 2025, we're more equipped than ever to provide comprehensive care and support.
Conclusion
As we move into 2025, new treatments and technologies are revolutionizing the way we manage dry mouth. From saliva stimulants to smart hydration systems and bioelectric therapies, the options are expanding, providing hope for those struggling with this uncomfortable condition. At Limegreen Dental Care, we’re committed to staying ahead of the curve and providing our patients with the latest in oral health innovations.If you’re experiencing dry mouth, don’t wait to get the relief you deserve. Schedule an appointment with us today to explore the latest treatments and take control of your oral health in 2025 and beyond.
0 notes
Text
What We Know About Covid’s Impact on Your Brain - Published Sept 13, 2024
By Jason Gale
Scientists are worried that persisting cognitive issues may signal a coming surge of dementia and other mental conditions
Many of Covid’s earliest and most alarming effects involve the brain, including a lost sense of smell, sluggish thinking, headaches, delirium and strokes. More than four years after the pandemic began, researchers are recognizing the profound impacts Covid can have on brain health, as millions of survivors suffer from persistent issues such as brain fog, depression and cognitive slowing, all of which hinder their ability to work and otherwise function. Scientists now worry that these symptoms may be early indicators of a coming surge in dementia and other mental conditions, prolonging the pandemic’s societal, economic and health burden.
What Studies Show In 2021, UK researchers reported early results from a study comparing brain scans taken before and after the pandemic began. They discovered signs of damage and accelerated aging in the brain, particularly in the region responsible for smell, even in patients who had experienced mostly mild cases of Covid months earlier.
How Does Covid-19 Impact the Brain? Research has since shown that Covid-related cognitive deficits can persist for years, especially in older adults and those who suffered more severe cases. For instance, a study of seniors hospitalized during China’s first Covid wave showed that 2 1/2 years later, 40% developed cognitive impairment, compared with just 14% of their uninfected spouses. A 2024 UK study of people hospitalized for Covid treatment revealed a significant worsening of psychiatric and cognitive symptoms three years after discharge. Half experienced moderate to severe depression, a quarter suffered severe cognitive decline, and one in nine showed a loss of mental function equivalent to a 30-point drop on the IQ scale, where a score of 100 is average.
For patients already battling Alzheimer’s disease, Covid can exacerbate brain inflammation, damage immune cells, and accelerate the memory-robbing disease itself, studies indicate. Even previously healthy older adults face an increased risk of cognitive impairment and new-onset dementia after infection. Mild Covid cases in younger adults have also been linked to brain issues affecting memory and thinking. These symptoms may be permanent but typically fluctuate and tend to worsen after physical or mental exertion, often impairing the ability of individuals to work and socialize.
Younger Americans Report More Cognitive Disability A February study of nearly 113,000 people found greater deficits in memory and executive function among people who had been infected at some point compared with those who had never had the SARS-CoV-2 virus. Those struck later in the pandemic had smaller deficits compared with those infected with the original strain or the alpha variant, the first new version of the virus to come to researchers’ attention. The study also noted a slight cognitive benefit for people who received two or more vaccinations.
Even mild cases of Covid led to cognitive decline, equivalent to an average 3-point drop in IQ. For those with unresolved symptoms such as persistent shortness of breath or fatigue, the decline amounted to a 6-point decrease in IQ.
Some evidence suggests the infection may increase the risk of Parkinson’s disease. This link is supported by the rise in cases of parkinsonism — a collection of symptoms such as tremors, slow movement, stiffness and balance issues — following Covid.
How Covid Harms the Brain The effects of a SARS-CoV-2 infection on the brain are the focus of intense research and remain only partially understood. Studies suggest that during acute infection, the virus may damage nerves, particularly in the olfactory bulb — which houses the nerves that transmit smell impulses to the brain — leading to problems that can persist for years. In some cases, the virus may infect the brain through this pathway, altering the organ’s structure and resulting in impaired cognition and fatigue.
Persistent viral remnants or the initial infection itself may trigger neuroinflammation and disrupt the immune system, causing antibodies and T cells to mistakenly attack healthy brain cells, damage blood vessels, and harm the blood-brain barrier. Additional research points to blood clots that may drive immune activation, restricting the supply of oxygen and nutrients to the brain, and altered levels of key hormones cortisol and dopamine that may be linked to changes in gut health.
Possible Economic Impact While the long-term effects of Covid on conditions such as Parkinson’s disease and dementia remain uncertain, the stakes are high. These are both lifelong, incurable, progressive illnesses with a profound societal impact, affecting not only those diagnosed but also their families, caregivers, and the broader healthcare system.
Already, there are significant economic repercussions globally from the enduring prevalence of long Covid, a loosely defined umbrella term to describe new, returning or ongoing health problems of varying severity that occur after a case of SARS-CoV-2 infection. By the end of 2023, long Covid had affected an estimated 400 million people worldwide. Analysts have put the annual economic toll at between $864 billion to $1.04 trillion in developed nations alone – roughly 1% of the global economy. Much of the impact arises from the ongoing disability and illness experienced by sufferers, with persistent fatigue and concentration problems among the most common.
#long covid#covid is not over#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#sars cov 2#still coviding#wear a respirator#covid conscious#covid is airborne
30 notes
·
View notes
Text







Happy Birthday veteran Scottish actress Phyllida Law, born on May 8th 1932 in Glasgow.
There is very little about her early life except she was born in Glasgow, the daughter of Megsie “Meg” and William Law, a journalist. She said once of he Glasgow upbringing “When you grow up in Glasgow with a Glaswegian granny, you’re taught that pride is a wicked thing. I still feel a bit like that.“ Phyllida grew up in Glasgow’s west end, just off Great Western Road, but war broke out when she was just seven and she found herself evacuated to places such as Lenzie, in Dunbartonshire, and Skelmorlie, Ayrshire.
That gave her a love for the Scots countryside which means she now splits her life between her home in London and a family cottage in Argyll. Phyllida would fit in well with the Scottish & Proud ethos, in an interview she says:
“I’m passionate about my Scots heritage. How could I not be? I can’t live without it. There’s no way I could live without those hills and it’s got to be the west coast. “I sometimes travel to Edinburgh then go up to Pittenweem or somewhere and I think to myself, ‘This isn’t Scotland.’ It’s a wonderful coastline but it’s not Scotland for me.
“When my parents lived in Glasgow they were always looking for a cottage to which they could retire. They found one in Ardentinney, so I visit that a lot.
She joined the Bristol Old Vic in 1952, from what I can gather she was first in the wardrobe department, the first pic shows her standing, from a 1952 photo. Heron screen acting credits start in 1958 and are very extensive, the pick of them are Dixon of Dock Green and a stint as the storyteller in the great children’s show Jackanory in the 60’s. It must have been during her time in the BBC’s children’s TV department she met her husband to be The Magic Roundabout narrator Eric Thompson, She has previously stated that the character of Ermintrude the cow was modelled on her.
Angels in the 70’s and of course Taggart in the 80’s as well Thomson, the variety series hosted by actress Emma Thompson in 1988, Emma just happens to be her daughter. Heartbeat, Hamish Macbeth and Dangerfield in the 90’s, Waking the dead and Doctors in the noughties has kept her busy, now in her 86th year she has still been appearing on the small screen, in The Other Wife and New Tricks during the past 8 years. Film roles include She is known for her work on Much Ado About Nothing , The Time Machine and The Winter Guest.
Phyllida spends most of her time in Argyll in a house she shares with her daughter Emma. who is spending more time looking after her mother, as she was diagnosed with Parkinson's Disease in 2915.
Phyllida constantly needs the support of a wheelchair and even assistance when washing due to the effect the condition is having on her.
Due to the progressive nature of the condition, symptoms tend to gradually worsen over time. It is common for individuals to struggle both with walking and talking at the height of the condition.
Phyllida herself spoke about the burdens of looking after an infirm parent, she looked after her mother, Meg who suffered with Alzheimer’s disease. Mego died in 1994 aged 93 after almost 20 years of being cared for by Ms Law at her mother's home in the village of Ardentinny on the west coast, near Dunoon.
20 notes
·
View notes
Text
Experience the Benefits of Houston Medical Marijuana

As medical marijuana continues to gain popularity across the United States, Houston has emerged as a key player in offering relief for patients with various medical conditions. With increasing acceptance and a growing number of studies highlighting its potential benefits, Houston medical marijuana has become a viable option for those seeking alternative treatment solutions. In this blog, we’ll take a closer look at how to access medical marijuana in Houston, its potential benefits, and how to consult with a medical marijuana doctor to get started.
Navigating the Legal Landscape of Houston Medical Marijuana
The legalization of medical marijuana in Texas has been a significant development for patients seeking relief from chronic pain, anxiety, insomnia, and other health conditions. However, many individuals still face challenges in accessing medical marijuana due to strict regulations and the need for a certified Texas medical marijuana doctor.
The process of obtaining a medical marijuana prescription in Houston can be confusing and time-consuming. You may be unsure where to begin, how to find a licensed provider, or what conditions qualify for medical marijuana treatment. With all these questions, it can be overwhelming to navigate the legal and medical aspects of accessing medical marijuana.
The Consequences of Delayed Access to Treatment
Delaying access to medical marijuana treatment can lead to worsening symptoms and reduced quality of life. Many individuals living with chronic pain, anxiety, or other qualifying conditions often find traditional medications ineffective or riddled with unpleasant side effects. Without proper access to medical marijuana, patients may experience prolonged discomfort, decreased functionality, and even worsening health issues.
For those who are eligible for medical marijuana treatment, waiting too long can mean enduring unnecessary pain and suffering. Additionally, missing out on early access to medical marijuana could result in the need for stronger medications or more invasive treatments in the future. The delay can also affect your mental health, with some patients experiencing anxiety or frustration from not being able to access the treatment they need.
Houston Medical Marijuana – How to Access and Benefits
Fortunately, the process of accessing medical marijuana is becoming more streamlined, thanks to an increasing number of certified Texas medical marijuana doctors and dispensaries. Let’s break down the key steps to accessing medical marijuana in Houston, the benefits it offers, and how a Texas medical marijuana doctor can guide you through the process.
1. How to Access Medical Marijuana
The first step in obtaining medical marijuana in Houston is obtaining a prescription from a licensed Texas medical marijuana doctor. These doctors are certified by the state to recommend medical marijuana to patients suffering from qualifying medical conditions. Once you’ve been evaluated and approved by a qualified doctor, you can apply for the Texas Compassionate Use Program (CUP).
Here’s an overview of how to proceed:
Step 1: Schedule an appointment with a certified Texas medical marijuana doctor. The doctor will assess your condition and medical history to determine if medical marijuana is appropriate for you.
Step 2: If approved, the doctor will register you in the Compassionate Use Program (CUP), which allows you to legally access medical marijuana in Texas.
Step 3: Visit a licensed dispensary to purchase your medical marijuana. Texas law requires that only registered dispensaries provide medical marijuana, so it’s essential to choose a licensed location.
2. Qualifying Conditions for Houston Medical Marijuana
In Texas, medical marijuana is available to patients suffering from a range of qualifying conditions. These include chronic pain, cancer, epilepsy, multiple sclerosis, Parkinson’s disease, and anxiety, among others. Your Texas medical marijuana doctor will evaluate your condition to see if you meet the requirements for treatment.
It's important to note that while medical marijuana is approved for many health conditions, it is still heavily regulated. Only licensed doctors can recommend marijuana as a treatment option, ensuring that patients receive appropriate care.
3. Benefits of Houston Medical Marijuana
Medical marijuana offers a variety of benefits to those dealing with chronic conditions. While its effectiveness varies depending on the individual and condition, many patients report significant improvements in their health and quality of life. Some of the key benefits include:
Pain Relief: One of the most common reasons people seek medical marijuana is to relieve chronic pain. Studies show that marijuana can help alleviate pain caused by conditions like arthritis, back pain, and cancer.
Reduced Anxiety: Many patients use medical marijuana to manage anxiety and stress. Some strains of medical marijuana have been shown to have calming effects, helping to reduce symptoms of anxiety and depression.
Improved Sleep: Medical marijuana can also help patients suffering from insomnia and other sleep disorders. Certain strains promote relaxation and can assist with falling asleep and staying asleep.
Nausea and Vomiting Relief: For patients undergoing chemotherapy or those with chronic conditions, medical marijuana can help reduce nausea and vomiting, making treatments more tolerable.
Appetite Stimulation: Some patients find that medical marijuana helps stimulate appetite, which is particularly beneficial for those with conditions like cancer or AIDS, where loss of appetite is common.
4. Consulting with a Texas Medical Marijuana Doctor
To begin your journey with Houston medical marijuana, consulting with a Texas medical marijuana doctor is the first and most crucial step. These doctors specialize in assessing whether medical marijuana is a suitable treatment option for your specific condition. During your consultation, the doctor will review your medical history, discuss your symptoms, and determine if you meet the criteria for medical marijuana.
Once you’ve been approved, the doctor will guide you through the next steps, including registering for the Compassionate Use Program and finding a licensed dispensary. The doctor will also help you understand the different forms of medical marijuana, such as oils, tinctures, and capsules, and how to use them safely and effectively.
5. Texas Medical Marijuana Doctor’s Role in Your Treatment
The role of a Texas medical marijuana doctor goes beyond simply prescribing marijuana. They provide valuable guidance on dosage, strain selection, and potential side effects. Their goal is to ensure that you receive the most effective treatment while minimizing any risks. Moreover, they will monitor your progress and adjust your treatment plan as needed to optimize your results.
Conclusion
Medical marijuana offers a promising alternative for patients seeking relief from chronic conditions. Whether you suffer from pain, anxiety, or sleep disorders, medical marijuana can provide significant benefits when used correctly. To get started, consulting with a certified Texas medical marijuana doctor is essential to ensure that you meet the qualifications and understand the treatment options available.
Ready to explore Houston medical marijuana? Schedule a consultation with a certified Texas medical marijuana doctor today to see if you qualify for the compassionate care you need!
0 notes