#vascular disease devices
Explore tagged Tumblr posts
Text
Varicose Veins Treatment in Karimnagar
At Karimnagar, we understand that every patient is unique, which is why we take a personalized approach to each individual's care plan. We offer a comprehensive range of services, including routine foot care, wound care, vascular ultrasounds, and more, to help diagnose and treat a variety of conditions. Our state-of-the-art facility is equipped with the latest technology and equipment to ensure that you receive the best possible care.
Glue Treatment For Varicose Veins in Karimnagar Glue Treatment For Varicose Veins: Glue treatment, also known as VenaSeal, is a minimally invasive treatment for varicose veins. It involves the use of a medical adhesive, which is injected into the affected vein. The glue seals the vein, and blood is rerouted to healthier veins. The procedure is painless and requires no anesthesia.
Laser Treatment For Varicose Veins in Karimnagar Laser Treatment For Varicose Veins:Laser treatment is another minimally invasive procedure used to treat varicose veins. It involves the use of a laser to heat and seal the affected vein, causing it to collapse and eventually fade away. The procedure is performed under local anesthesia, and most patients can return to normal activities within a day.
Microsclerotherapy Treatment in Karimnagar Microsclerotherapy for Cosmetic Purpose:Microsclerotherapy is a cosmetic treatment used to remove spider veins or small varicose veins. It involves the injection of a sclerosing agent directly into the affected vein, causing it to collapse and fade away. The procedure is minimally invasive and requires no anesthesia.
Peripheral Artery Bypass Treatment in Karimnagar Peripheral Artery Bypass/Angioplasty/Stenting:Peripheral artery bypass, angioplasty, and stenting are procedures used to treat peripheral artery disease. They involve the use of a catheter to insert a balloon or stent into the blocked artery, allowing blood flow to be restored. The procedure is performed under local anesthesia and requires a short hospital stay.
Aortic Aneurysm center in Karimnagar Aortic Aneurysm Stenting/Open Surgery:Aortic aneurysm stenting and open surgery are procedures used to treat an aneurysm in the aorta. Stenting involves the insertion of a stent into the weakened section of the artery to support and reinforce it. Open surgery involves the surgical repair or replacement of the damaged portion of the artery. The procedure requires general anesthesia and a hospital stay.
Diabetic Foot Treatment in Karimnagar Diabetic Foot / Podiatric Surgery:Diabetic foot and podiatric surgery are procedures used to treat foot problems related to diabetes. They involve the removal of damaged tissue, the correction of deformities, and the treatment of infections. The procedures may be performed under local or general anesthesia, depending on the complexity of the surgery.
Day Care Surgeries in Karimnagar Day Care Surgeries:Day care surgeries are minor procedures that can be performed in an outpatient setting. They include procedures such as skin biopsies, mole removal, and minor laceration repairs. The procedures are performed under local anesthesia and patients can return home the same day.
Varicose vein treatment in Karimnagar Varicose vein treatment by Endovenous Ablation: Our clinic offers a minimally invasive treatment option for varicose veins known as endovenous ablation. This treatment is performed using a laser or radiofrequency energy to heat and close the affected veins, allowing blood to reroute through healthier veins. The procedure is quick, effective, and virtually painless with no scarring, allowing patients to return to their daily activities almost immediately.
Diabetic foot ulcers and Non-healing ulcer Management in Karimnagar Diabetic foot ulcers and Non-healing ulcer Management: Our clinic specializes in the management of diabetic foot ulcers and non-healing ulcers. Our expert team of vascular surgeons offers comprehensive treatment options to promote wound healing and prevent further complications. We use a multidisciplinary approach, including wound care, offloading, infection control, and vascular interventions to help patients recover quickly.
Peripheral bypasses, DVT management in Karimnagar Peripheral bypasses, DVT management: We offer advanced treatment options for peripheral arterial disease and deep vein thrombosis. Peripheral bypass surgery involves redirecting blood flow around a blocked artery using a graft, and we provide expert care for this procedure. Our team also offers specialized care for deep vein thrombosis, including anticoagulation therapy, compression stockings, and thrombectomy if necessary.
Aortic Aneurysm Treatment in Karimnagar Aortic Aneurysm Endovascular repair: Our clinic provides endovascular repair for aortic aneurysms, a less invasive alternative to traditional open surgery. The procedure involves inserting a stent-graft through a small incision, allowing us to repair the aneurysm without major surgery. This procedure offers faster recovery times, less pain, and fewer complications than traditional open surgery.
for more info:
#varicoseveins#varicoseveintreatment#vascularsurgery#vascular#hvc#deepveinthrombosis#hyderabadvascularcenter#stoptheclot#deep vein thrombosis#dvt#venousthromboembolism#vascular disease#vascular surgery#vascularhealth#ai vascularity#peripheral vascular devices market#vascular surgeon
0 notes
Text
https://justpaste.it/9gd4n
The Vascular Disease Devices Market in 2023 is US$ 32.21 billion, and is expected to reach US$ 54.19 billion by 2031 at a CAGR of 6.70%.
#Vascular Disease Devices Market#Vascular Disease Devices Market Trends#Vascular Disease Devices Market Growth
0 notes
Text
The Hidden Dangers of Peripheral Arterial Disease
Peripheral Arterial Disease (PAD) often lurks unnoticed, overshadowed by more commonly discussed health issues. Yet, its impact on the circulatory system and overall health is profound. Dr. Sumit Kapadia, a renowned name in vascular health, delves into the hidden dangers and lesser-known symptoms of this disease.

Understanding PAD
PAD is a condition marked by the narrowing of arteries in the legs due to atherosclerosis. This plaque buildup hampers blood flow, leading to a range of symptoms. While leg pain during physical activities is a known symptom, PAD also manifests in subtler signs like temperature changes in the legs, skin colour changes, slower growth of toenails, and even erectile dysfunction in men, especially those with diabetes.
The Importance of Early Detection
With advancements in medical science, including new treatments for PAD in 2023, recognizing these symptoms early has become crucial. Dr. Kapadia utilizes several diagnostic tests such as the Ankle-Brachial Index (ABI) and Doppler Ultrasound Imaging, which are instrumental in detecting PAD early and preventing its progression.
Conclusion
Understanding and recognizing the lesser-known symptoms of PAD are vital for early intervention. With advanced peripheral artery disease treatment and angioplasty options available, effectively managing PAD under the guidance of experts like Dr. Kapadia is more achievable than ever.
#vascular surgeon#dr. sumit kapadia#vascular surgery#varicose veins#endovascular specialist#varicose vein treatment#laser treatment#veintreatment#peripheral arterial disease#peripheral vascular devices market
0 notes
Link
#market research future#peripheral artery disease#peripheral vascular disease#peripheral vascular device#peripheral stent market
0 notes
Text

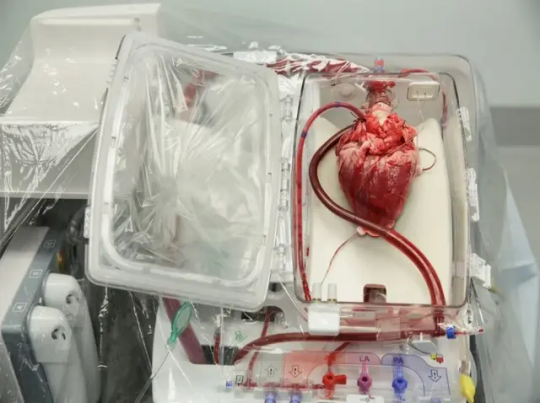
Groundbreaking Pig Heart Transplant is Performed for the Second Time
For the second time ever, a pig heart has been transplanted into a living human recipient, the University of Maryland Medical Center announced on Friday.
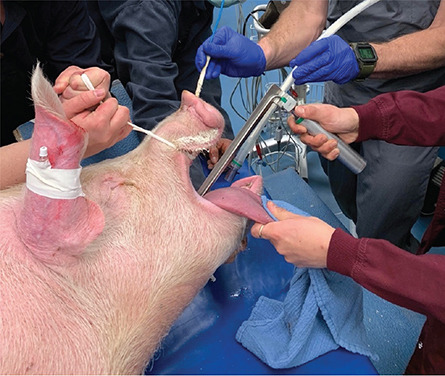
The groundbreaking surgery was done on September 20 at UMMC by the same transplant team that preformed the first such experimental surgery in 2022.
In a news release, the hospital said the recipient, 58-year-old Lawrence Faucette, “is currently breathing on his own, and his heart is functioning well without any assistance from supportive devices.”
Faucette had end-stage heart disease. He had pre-existing peripheral vascular disease and complications with internal bleeding making him ineligible for a traditional heart transplant, the hospital said in the release. He was admitted to UMMC on September 14 after experiencing symptoms of heart failure.
“My only real hope left is to go with the pig heart, the xenotransplant,” Faucette told the hospital in an internal interview several days before the surgery.
The experimental xenotransplant surgery was green lit under the US Food and Drug Administration’s “compassionate use” program. According to the FDA, the program is “a potential pathway for a patient with a serious or immediately life-threatening disease or condition to gain access to an investigational medical product (drug, biologic, or medical device) for treatment outside of clinical trials when no comparable or satisfactory alternative therapy options are available.”


The pig heart used came from a genetically modified pig from Revivcor, a subsidiary the United Therapeutics Corporation. The pig had 10 genes edited, including three genes “knocked out” or inactivated to eliminate the alpha gal sugar in the pig’s blood cells, which can trigger a severe reaction in the human immune system, causing organ rejection. An additional pig gene was modified to control for the growth of the pig’s heart while 6 human genes were added into the pig’s genome to increase acceptance by the immune system. The FDA first approved the gene edited pigs in 2020 for potential therapeutic use and consumption.
Doctors are also treating Faucette with an experimental antibody treatment to further suppress the immune system and prevent rejection. He will be closely monitored for any signs of rejection or any development of pig related viruses. The donor pig was also closely screened for any signs of virus or pathogens.

“We are once again offering a dying patient a shot at a longer life, and we are incredibly grateful to Mr. Faucette for his bravery and willingness to help advance our knowledge of this field,” said Dr. Bartley Griffith, in the release. Griffith is the surgeon who performed the transplant and is a professor of surgery at the University of Maryland School of Medicine.
The hospital said Faucette fully consented to the experimental treatment and was informed of all the risks. In addition, he underwent a full psychiatric evaluation and discussed his case with a medical ethicist.
According to the hospital’s news release, Faucette is a married father of two from Frederick, Maryland and a 20-year Navy veteran who had most recently worked as a lab technician at the National Institutes of Health before retiring.
“We have no expectations other than hoping for more time together,” said his wife Ann Faucette, in the release. “That could be as simple as sitting on the front porch and having coffee together.” There are currently no clinical trials that utilize pig organs for transplants in living human beings. The University of Maryland performed the first such experimental surgery on 57-year-old David Bennett in January 2022. Bennett died two months following the surgery.
While there were no signs of rejection in the initial weeks following the transplant, an autopsy concluded that Bennett ultimately died of heart failure from “a complex array of factors,” including Bennett’s condition prior to the surgery. Bennet had already been hospitalized and kept on a heart lung bypass machine for 6 weeks prior to the transplant. However, a case study by the doctors published in the Lancet also noted there was evidence of pig virus that had not been identified previously.
According to the federal government, there are more than 113,000 people on the organ transplant list, including 3,354 people in need of a heart. The group Donate Life America says that 17 people die each day waiting for a donor organ.
By Nadia Kounang,


#Groundbreaking Pig Heart Transplant is Performed for the Second Time#The University of Maryland Medical Center#Lawrence Faucette#heart#pig heart#heart transplant#organ transplant#xenotransplant#animals#strange#stranger things#science#science news
20 notes
·
View notes
Text
Prevention and rehabilitation in Middle Ages by Prof. Francesco Carelli in Journal of Clinical Case Reports Medical Images and Health Sciences
Italian hospitals in the late Middle Ages already offered much more than a simple reception and care. In a work that can be consulted in the Laurentian Library in Florence, datable about 1300, painter Gaddi shows a series of hospitalized people. Already the representation is not very sad perhaps due to the lack of modern white walls and patients appear regularly placed in beds with acts of assistance and care. The two couples in the foreground completely decline an idea of health that we moderns tend to, even though we have not yet reached it. In fact, therapy is combined with education and prevention. The disease in question is a chronic vascular sore, a subject not resolved at by us moderns and a source of great health care costs. One of the reasons for these costs is to be fund in the lack of attention of moderns to preventive and educational activities. In the foreground on the right the therapeutic act is portrayed, in which it is evident a doctor performing a cleaning, disinfection and dressing of a vascular sore. But the great news that is incredible in the so – called dark ages, is portrayed on the left. The doctor, recognizable by the red headdress, gives a stick, that is a device to improve, encourage and facilitate the ambulatory exercise by his patient. We also note that he spends time on an explanation to the patient who is portrayed as he listens to medical advice with interest. The rehabilitation intentions are proven by the fact the patient wears a rudimentary orthopaedic brace which surrounds widely the neck. The device allows the patient to walk keeping the arm hanging from the neck, unable to move perhaps following a trauma. In the hospitals of the Middle Ages, therefore, education and adapted motor activity were carried out which, today, together with food, is considered the basis of disease prevention.
#Prevention#rehabilitation#chronic vascular sore#dark ages#jcrmhs#Journal of Clinical Case Reports Medical Images and Health Sciences predatory Case Reports in clinical Medicine#orthopaedic
5 notes
·
View notes
Text
Medical Professionals and Etymology
Thinking out aloud here.
Sometimes I wonder if doctors and medical professionals(maybe scientists as well) have a better grasp on the English language and etymology than the general person, being that they have to learn so many medical terms that are based in Latin and have clear, direct meanings from their Latin bases.
Here are some examples:
Adrenal: From "ad-" (near) and "renes" (kidneys), referring to the glands located near the kidneys.
Antibiotic: "Anti-" (against) and "biotic" (life), indicating substances that fight against life, particularly microorganisms.
Cardiovascular: "Cardio-" (heart) and "vascular" (blood vessels), relating to the heart and blood vessels.
Dermatology: "Derma" (skin) and "-ology" (study of), the study of skin and its diseases.
Glycogenesis: "Glyco-" (sugar) and "-genesis" (creation), the formation of glycogen from glucose molecules.
Orthopedics: "Ortho-" (straight) and "-pedics" (child), originally referring to the treatment of skeletal deformities in children but now encompassing the treatment of musculoskeletal disorders in general.
And going off on a wild tangent here, I also wonder if Chinese-speakers have a clear understanding of what a thing is, being that Chinese characters for things are usually compound words of other real things.
For example:
Television is 电视机, literally translates back into English as "electric view device".
Soap is 肥皂, literally translates into "fat construct", which is what soap is, made from fat.
5 notes
·
View notes
Text
This gets INCREDIBLY LONG, so a little tl;dr here for you: I decided to become a healthy volunteer for clinical research studies in order to fill a hole I thought I had in my fetish dreams, but got addicted to being a test subject. Because it was SO MUCH FUN.
I'm not on here much because this is a secretive place for me (much like a lot of you) and I don't have a lot of alone time.
I just got back from a trip recently and haven't been able to parse my feelings about it. I need to share my fun experiences with SOMEONE because not many people in my life appreciate the feelings I have for them like a lot of you will.
Clearly, by the reposts and likes, I have a medical fetish. Strongest for EKGs, blood pressure cuffs, catheters, oxygen masks. But also for most things medical related. I have ton of equipment that I've used on myself and others.
My wife is a wonderful supporter of anything that turns me on more and has been a fantastic patient for me. But she doesnt have the appreciation for medical equipment, she doesn't love the feeling of a mask over her nose and mouth, the light touch of wires across her chest, like I do.
As I've gotten older, I've needed to figure out more about myself and why I have these feelings. I've always liked being the patient, always wanted to be the experiment.
An idea came to me while I was involved in biometrics screening at work and I wondered why I had never thought of it before: why not volunteer as a healthy subject for clinical research?
I dove head first into it, checking out all the available research programs in my area (there were a lot), but what I began to realize is I didn't just want to be pumped full of experimental drugs and to find out what they do (even though most of those studies would involve the equipment I enjoyed). I wanted something more...basic. Something less experimental, but more intimate.
I found the perfect study, one that still required vitals monitoring (my reason for interest), but also helped further science in a way that interested me personally. A venous occlusion and distension study that looked at the effect NSAIDs have on veins to potentially help patients with Periferal Arterial Disease (PAD). I was nervous to tell my wife about it (just as nervous in fact as when I told her about my fetish initially). But she was perfectly OK with it, mentioning that clinical volunteers are a needed commodity.
With that, I sent off a message to the clinical research coordinator. And I waited. And waited. And waited.
It took about a week of nervous anticipation before she responded with a phone call. She explained the procedure, how they would measure the volume of my arm, hook up an IV retrograde into the forearm, wrap blood pressure-like cuffs around my wrist, forearm, and bicep to force the blood out of my arm for the occlusion portion. Heartrate would be monitored via a 3-lead EKG, BP would be taken periodically on my other arm, as well as continual BP measured via a device wrapped around my wrist and finger called a finometer. She asked if all that sounded ok.
Yes. 1000% yes.
We set up an appointment for a few weeks later and my sex drive went into overdrive at the prospect. My wife was a bit wary of this at first, but eventually warmed up to the idea and reaped the benefits of my overactive imagination.
The day of the experiment, I drove to the medical center, walking briskly past all the patients milling about the general hospital area, past the cancer center, and on toward the cardiac and vascular institute. God, it was such a rush feeling like I belonged there, but for a fun reason, not because I was sick. That sterile hospital smell, the sounds, the lights, the doctors and nurses passing me in their scrubs, going about their business.
I arrived outside of the clinical research floor and was immediately met by the clinical coordinator, no time to get my bearings, no more sitting and waiting. It was finally go time.
She whisked me past receptionists, then past equipment strewn in the hallways, doors leading to open rooms with beds in the middle, until we arrived at "my" room.
I tried not to stare as we entered. It was REALLY HARD. My quick glance took in the table in the middle of the room, the racks of monitoring equipment on the left wall, baskets with wires and tubes hanging out the tops, a large ultrasound machine to the right of the table, a roller tray with what I knew was an IV kit as well as several other syringes in sterile packaging.
I followed the coordinators instruction to sit and fill out my pre-procedure paperwork while she went over all the things that would happen to me (like I needed to hear it again, I'd read the paperwork at least 20 times throughout the prior weeks). Then she took my height and weight, and listened to my lungs and heart. I was a nervous wreck, so my heartrate was a bit high. She chocked it up to dehydration and got me a cup of ice water. Next we measured my arm volume by dunking it in a long tube of water and noting the displacement. Then I was sent to the bathroom before the start of the procedure while she retrieved the other members of the clinical team.
I had a few precious moments to myself in the cramped room once I got back to take everything else in. The computers by the back right corner. The windows out to look over a helipad, as we were on the fourth floor. Just how much juicy equipment lay on the racks on the far wall. None of this was helping my heartrate to slow down.
The coordinator came back in with a tech in tow and told me to hop up on the table in the center so she could get baseline BP, and get me hooked up to the EKG and get my IV placed.
I padded over after taking my shoes and socks off and used the stool to sit down on the table. The tech began wrapping the oh so familiar dark blue cuff around my right arm, while the coordinator pulled over the tray with the syringes and IV kit. At the coordinators request the BP cuff inflated as I sat there trying to calm my thumping heart. She remarked a mostly normal BP, much to my surprise, 125/85, only slightly on the high side for me. She had me lay down and we took it again two more times! God it felt amazing to just have someone so interested in my blood pressure.
The fun was just beginning, though. The coordinator took my left arm in her hands and pulled it over to the tray. Getting gloves on and cracking open the IV kit, she set about cleaning my arm and wrapping a band around my bicep, a steady stream of questions about my family, my job, and answers to my questions back. General banter while she looked down at my arm with such scrutiny, poking the inside of my elbow to confirm a good vein, then a quick jab as the IV entered and was dressed in a flash. I've had flu shots that hurt more, she was such a pro.
The banter continued as she dug around in a bag for three sticky electrodes, tenting my loose tshirt to reach just below my left side ribs, and my left and right shoulders. The tech helped her get the wires attached and I soon turned to see the delicious green line on the screen spiking up and down to a fair 110 bpm. The coordinator remarked again about my higher heartrate, but I informed her it was probably just nerves from my first visit and that I had a naturally high heartrate (I usually sit in the high 80s).
We continued onward, another male tech coming in, as well as the lead clinical physician who would be doing the ultrasound on my arm during the occlusion and infusion. They all busied themselves with various tasks, noting my HR, my BP, or prepping the occlusion cuffs.
The primary clinical physician asked if he could bring in a student intern, as a petite asian girl, probably half my age in her first few years of college shuffled in from the hall. "Of course" was my only response, the more the merrier. Good GOD was I trying so hard not to be turned on by all the extra staff and the entire situation.
Things moved quickly from here. The techs wrapped a cuff around my wrist, my forearm underneath the IV, and around my bicep.
The coordinator lifted my arm up and gave me a roll of gauze to squeeze. After squeezing for a few seconds she said "Five, four, three, two, one, cuff one up" and with the signature puff of air, the cuff around my wrist inflated, incredibly tight. "Five, four, three, two, one, cuff two up", and the second cuff on my forearm tightened, pushing the pooled blood in my forearm away even further (the pressure felt so odd on the retrograde IV at my elbow). "Five, four, three, two, one, cuff three up", and with that the last cuff around my bicep inflated, tighter than I'd ever pumped up a BP cuff during my own play, cutting off circulation to my entire left arm.
The tingling started in earnest as the coordinator told me I could relax my arm and the primary physician set about my forearm with cold gel and the ultrasound probe. I thought perhaps I'd lose more feeling in that arm, but I could feel the lightest touch from the physician, the push and pull of the probe as he clicked keys to zero in on the veins he was looking to image. He talked quietly with his intern, pointing to the screen, to my arm. She would nod and note things as well, also motioning to whatever they saw on the monitor.
The rest of the techs also milled about, the coordinator asking for time to be marked and noting my heartrate. I'd forgotten the monitor, as I was so focused on my left arm. Turning my neck I saw my HR had shot up to 144 bpm! My BP was also much higher as well topping at 155/100. Guess having an extra arms worth of blood rushing around my body sure changed my biometrics.
We waited for some time, taking new baseline statistics of my body's functions. 10 minutes passed, me simply lying there with my arm going numb, the continual squeeze of the finometer on my finger giving me an indication of my pulse.
Next up the coordinator sidled up next to my head, dragged the tray back over and set about getting the first syringe ready. She informed me there were 50ml, separated into 5 different syringes. "They may have doses of Ketorelac, or it may simply be saline, based on randomized trial".
As she began the first infusion, the primary physician and his intern were back on the ultrasound, probing and watching the spot where the IV entered my arm. I could feel the gentle caress of the probe as cold liquid filled my veins, again surprised at how much I could still feel despite 15 full minutes of cut off circulation.
The coordinator hooked up the next syringe and asked how I was feeling.
"I'm great!" I replied promptly.
"Alright, there's four more of these, so just let me know if the pressure gets to be too much in your arm."
She hooked up the next and pushed the plunger slowly down. My arm felt cold now, the liquid going in fluctuating between warm and cool, an odd sensation. The physician continued talking to his intern. The techs and the coordinator would talk amongst themselves as well.
"See this here as it's infused"
"Which one is that, the second?"
"We're on 17 minutes"
"Heartrates up, BP is a little higher as well"
"Still doing OK? I'm going to start the next, just let me know if it begins to be too much."
It was...so much. All of it. A pleasant buzzing whir in my mind, like ASMR but stronger, dominated my brain. All I could do was feel the sensations of my body and listen to the researchers as they talked about my body's functions and what they were doing to me like I wasn't a person to them. Like I was this enigma, this puzzle that needed solving. Just a subject, an experiment for them to run.
Once the infusions were all in place, and another 5 minutes had passed, the cuff was released and warmth and stabbing pins and needles filled my veins and arteries again.
More vitals were taken to confirm changes in my blood pressure, but after the release it was simply a matter of cleaning up. And just like that it was over.
I was cleaned up, given a meal card to use at the cafeteria, told how much my help was appreciated and sent on my way.
I've just come back from my fifth time (first time back since the pandemic), some of the studies have taken place in the MRI center (MRIs are relaxing and I love the idea of my brain being scanned).
And now i just feel the looming emptiness inside. There is so much anticipation and excitement each time I set up dates to go be a research subject. So much feeling. And when I'm there, when I'm being worked on and monitored, when I'm being watched over and dolled upon, I feel so good and right.
It's addictive, like a drug. I want more. I want to go back every week so they can poke me with more needles, watch my heartrate take off at the inflation of a cuff.
Anyway. If you've read this far, congrats on seeing a bit of my not so normal psyche. Glad there are plenty of people out there to volunteer who, like me, don't mind the uncomfortable and invasive parts of medical advancement.
If you think you can control yourself (I actually did a pretty good job in the end of keeping my lust under control), you may want to consider being a healthy volunteer as well. It's definitely an experience you'll never forget.
Feel free to ask questions and such, I'll answer them when I can.
17 notes
·
View notes
Text
Abdominal aortic aneurysm – Abdominal aortic aneurysm (AAA) is a common and potentially life-threatening condition. Approximately 7000 deaths per year are attributed to ruptured AAA in the United States. Without repair, ruptured AAA is nearly uniformly fatal. For asymptomatic patients, elective repair of the aneurysm is the most effective management to prevent rupture.
●Asymptomatic small AAA – For most patients with asymptomatic infrarenal AAA <5.5 cm, we recommend conservative management (watchful waiting) rather than elective AAA repair (Grade 1A). The risk of aneurysm rupture does not exceed the risk of repair until the aneurysm diameter reaches 5.5 cm. However, there are situations for which elective repair of asymptomatic AAA <5.5 cm may also be appropriate. These may include rapidly expanding AAA (>0.5 cm in six months or >1 cm per year), coexistent aneurysm/peripheral artery disease, and female sex.
●Conservative management – Conservative management consists of periodic clinical evaluation and imaging surveillance to identify AAA that exceeds the threshold for repair or is rapidly expanding. Medical therapies for patients with AAA focus on the management of modifiable risk factors for AAA and cardiovascular disease with the goals of reducing the need for intervention due to aneurysm expansion or rupture, reducing morbidity and mortality associated with AAA repair, and reducing cardiovascular morbidity and mortality.
•Smoking cessation – For patients with AAA who smoke, we recommend smoking cessation (Grade 1A). Smoking is strongly associated with AAA expansion and rupture and is the most important modifiable risk factor. Even though reduced aneurysm expansion and rupture risk have not been clearly demonstrated among those who have stopped smoking, smoking cessation has other clear benefits.
•No medical therapies proven to limit AAA expansion – Although many pharmacologic therapies aimed at limiting AAA expansion and preventing rupture have been tried, no therapy has been proven successful at achieving these goals, and as such, we suggest not implementing any of the pharmacologic therapies discussed above for the sole purpose of treating AAA (Grade 2C).
●Asymptomatic large AAA – For good-risk surgical candidates (open or endovascular repair) with AAA >5.5 cm, we recommend elective AAA repair (Grade 1A). For patients with AAA >5.5 cm who have a short life expectancy (<2 years) due to advanced comorbidities, particularly cardiopulmonary disease or malignancy, we suggest no repair over endovascular aneurysm repair (Grade 2B). For these patients and others who elect not to undergo repair, ongoing AAA surveillance is not needed. The patient should be encouraged to create an advanced directive detailing their wishes for no repair of any kind in the event of rupture. Family members or other caretakers should be made aware of these wishes, given that the patient may not be able to report their wishes at the time of aneurysm rupture.
●AAA repair – The primary goals of aneurysm repair are to prevent rupture while minimizing morbidity and mortality associated with repair. We agree with guidelines from major medical and surgical societies that emphasize an individualized approach when choosing between an open or endovascular approach to AAA repair, accounting for aortic anatomy, patient age, life expectancy, and risk factors for perioperative morbidity and mortality. For patients with favorable anatomy for endovascular repair (as defined by the instructions for use of a given device) and a high level of perioperative risk, we recommend endovascular repair, rather than open surgical repair (Grade 1B).
●Surveillance schedule for unrepaired AAA – The optimal surveillance schedule for patients who are not undergoing AAA repair is not known for certain. The Society for Vascular Surgery (SVS) recommends surveillance every 6 to 12 months using ultrasound or CT for medium-sized aneurysms (4 to 5.4 cm in diameter) but less frequent intervals for smaller aneurysms. We frequently perform surveillance on small aneurysms annually to minimize imaging variability and alleviate patient anxieties. Annual clinical examination and risk reduction assessment can also be performed concurrently with AAA surveillance.
4 notes
·
View notes
Text
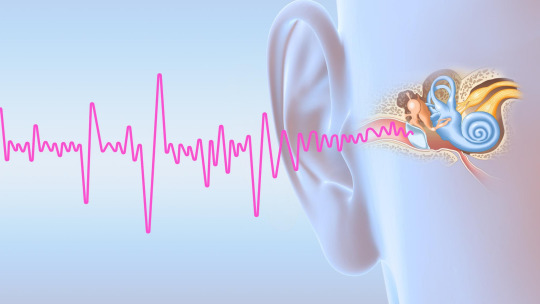
Tinnitus is a medical term that refers to a noise generated inside the head rather than in the environment. It is a common problem that affects millions of people around the world. Statistics say that 36 million people suffer from tinnitus in the United States, so it can be considered a fairly common condition. Other studies conducted in different countries also show that the prevalence of tinnitus ranges from 5% to 15% of the adult population.
Tinnitus can originate from various places in the body, including the ear or the brain itself, and along the path between the ear and the brain. The noise can be of different types, such as a whistle, a buzz, a hiss, or a roar. It can be constant or intermittent, and can vary in intensity and frequency.
There are two main types of tinnitus: non-pulsatile (subjective) and pulsatile (objective). Non-pulsatile tinnitus is caused by abnormal activity in the auditory cortex of the brain responsible for sound processing. It is often the result of hearing loss, exposure to loud noises, or ear related disorders. Pulsatile tinnitus is vascular in nature and involves noise from the blood vessels near the ear. It is often caused by abnormal blood vessels or abnormal vasculature problems, such as tumors.
For most people, tinnitus is temporary and goes away quickly. But for some people, tinnitus is chronic and can significantly affect quality of life. Tinnitus can affect people's lives in many ways, depending on the intensity, frequency and type of noise they hear. Some possible consequences of tinnitus in people's lives are: Physical and mental health problems, such as fatigue, stress, changes in sleep and concentration, memory problems, depression, anxiety, or irritability. Hearing problems, such as difficulty hearing real sounds, understanding speech, or locating the source of sounds. Communication problems, such as difficulty holding a conversation, participating in social or professional activities, or isolating yourself from others. Emotional well-being problems, such as low self-esteem, frustration, anger or hopelessness.
To prevent tinnitus, it is important to avoid or reduce the factors that can cause or aggravate the problem. Some prevention measures you can take are: Limit exposure to loud noises, which can damage the hearing cells in the inner ear. If you can't get away from loud sounds, use appropriate hearing protection, such as earplugs or earmuffs. Lower the volume of electronic devices such as television, radio, or headphones, and avoid prolonged use of these devices. Let your ear rest from time to time. Have your ears cleaned regularly by a professional to prevent the accumulation of substances that can clog the external auditory canal. Properly treat ear infections, which can cause inflammation and irritation in the auditory system. Avoid excessive intake of medications, alcohol, and caffeine, which can have ototoxic effects or alter blood circulation in the ear. Avoid smoking, which can impair vascular health and increase the risk of tinnitus. Controlling cardiovascular diseases, such as hypertension or atherosclerosis, which can affect blood flow in the ear and cause pulsatile tinnitus. Take care of mental health by avoiding stress and seeking psychological support if necessary. Stress can make tinnitus worse and cause anxiety, depression, or irritability.
#Excellent Review#health tips#create your best version#Have a healthy body Healthy body and mind#How to have a healthier body#Caring for your body#how to be more productive#nutrition tips#improve your life#cortexi#revisão do cortexi#resenhas de córtexi#cortexi funciona#suplemento cortexi#comprar cortexi#gotas de cortexi#zumbido do córtex#cortexi customer review#revisão honesta do cortexi#efeitos colaterais do cortexi#o cortexi é legítimo#cortexi revelado
3 notes
·
View notes
Text
The Vascular Disease Devices Market in 2023 is US$ 32.21 billion, and is expected to reach US$ 54.19 billion by 2031 at a CAGR of 6.70%.
#Vascular Disease Devices Market#Vascular Disease Devices Market Trends#Vascular Disease Devices Market Growth
0 notes
Link
0 notes
Text
Body Composition: What It Is and How to Measure

Body composition analysis involves a series of tests to measure the ratio of different tissues that our bodies are currently made up of – including muscles tissue , fat, bones and percentage of water in the body. Now, we can see Why is body composition important for health?
Body composition is a critical aspect of overall health because it provides a detailed understanding of the different components that make up the body, primarily fat, muscle, bone, and water.
Better Indicator than Weight: Unlike weight or BMI alone, body composition offers a more comprehensive view of an individual’s health status. It differentiates between muscle, fat, and bone mass.
Disease Risk Assessment: Higher body fat percentages, particularly visceral fat, are associated with increased risk of chronic diseases such as heart disease, diabetes, and certain cancers.
Strength and Endurance: A higher muscle mass relative to fat mass typically correlates with better strength, endurance, and overall physical performance.
Functional Mobility: Maintaining a healthy muscle-to-fat ratio can enhance functional mobility and reduce the risk of falls and injuries, especially in older adults.
What are the benefits of having a healthy body composition?
Having a healthy body composition, which typically means a higher ratio of lean body mass (muscles, bones, and organs) to fat mass, offers numerous benefits for overall health and well-being. Here are some key advantages:
Reduced Risk of Chronic Diseases: A healthy body composition lowers the risk of developing chronic diseases such as heart disease, type 2 diabetes, and certain cancers. Excess body fat, especially around the abdomen, is linked to increased inflammation and insulin resistance.
Improved Cardiovascular Health: A balanced ratio of lean mass to fat mass helps maintain healthy blood pressure, cholesterol levels, and blood sugar levels, reducing the strain on the heart and vascular system.
Enhanced Metabolic Rate: Lean body mass, particularly muscle, is metabolically active tissue. This means that individuals with more muscle mass have a higher resting metabolic rate, which helps in maintaining a healthy weight and burning more calories even at rest.
Better Physical Functioning: A healthy body composition improves overall strength, endurance, and flexibility, making everyday activities easier and reducing the risk of injuries.
Stronger Immune System: Proper muscle mass and a balanced diet support a robust immune system, helping the body fend off infections and illnesses more effectively.
Alfarsi.me provides the BIODY XPERT Analyzer in Muscat, Oman for body composition analysis in Muscat, Oman which can be used to determine fat mass and hydration levels. It’s a multi-frequency device that doesn’t require any wires or consumables. It is an interconnected object that takes advantage of cutting-edge technology and can be used anywhere.
0 notes
Text
Body Composition: What It Is and How to Measure
Body composition analysis involves a series of tests to measure the ratio of different tissues that our bodies are currently made up of – including muscles tissue , fat, bones and percentage of water in the body. Now, we can see Why is body composition important for health?
Body composition is a critical aspect of overall health because it provides a detailed understanding of the different components that make up the body, primarily fat, muscle, bone, and water.
Better Indicator than Weight: Unlike weight or BMI alone, body composition offers a more comprehensive view of an individual’s health status. It differentiates between muscle, fat, and bone mass.
Disease Risk Assessment: Higher body fat percentages, particularly visceral fat, are associated with increased risk of chronic diseases such as heart disease, diabetes, and certain cancers.
Strength and Endurance: A higher muscle mass relative to fat mass typically correlates with better strength, endurance, and overall physical performance.
Functional Mobility: Maintaining a healthy muscle-to-fat ratio can enhance functional mobility and reduce the risk of falls and injuries, especially in older adults.
What are the benefits of having a healthy body composition?
Having a healthy body composition, which typically means a higher ratio of lean body mass (muscles, bones, and organs) to fat mass, offers numerous benefits for overall health and well-being. Here are some key advantages:
Reduced Risk of Chronic Diseases: A healthy body composition lowers the risk of developing chronic diseases such as heart disease, type 2 diabetes, and certain cancers. Excess body fat, especially around the abdomen, is linked to increased inflammation and insulin resistance.
Improved Cardiovascular Health: A balanced ratio of lean mass to fat mass helps maintain healthy blood pressure, cholesterol levels, and blood sugar levels, reducing the strain on the heart and vascular system.
Enhanced Metabolic Rate: Lean body mass, particularly muscle, is metabolically active tissue. This means that individuals with more muscle mass have a higher resting metabolic rate, which helps in maintaining a healthy weight and burning more calories even at rest.
Better Physical Functioning: A healthy body composition improves overall strength, endurance, and flexibility, making everyday activities easier and reducing the risk of injuries.
Stronger Immune System: Proper muscle mass and a balanced diet support a robust immune system, helping the body fend off infections and illnesses more effectively.
Alfarsi.me provides the BIODY XPERT Analyzer in Muscat, Oman for body composition analysis in Muscat, Oman which can be used to determine fat mass and hydration levels. It’s a multi-frequency device that doesn’t require any wires or consumables. It is an interconnected object that takes advantage of cutting-edge technology and can be used anywhere.
0 notes
Text
Finding the Best Cardiologist in Jaipur Heart Health with the Right Care
Dr. Amit Gupta (Cardiology Doctor in Jaipur) is a young and talented Interventional Cardiologist in Jaipur. He is currently associated with CK Birla Hospital, Jaipur as a Senior Additional Director in the Cardiology Department. His training in cardiology and cardiac intervention is from the most esteemed cardiac center in India (G. B. Pant Hospital, MAMC, New Delhi). He is equally competent in Pacemaker, ICD, CRT implantation, Balloon Valvoplasty, Peripheral angioplasty, Percutaneous ASD, PDA device closure, and diagnostic Electrophysiology study. He very well performs percutaneous treatment of vascular injuries, aneurysms, malformations, and uterine fibroids by coiling and stent graft.
The heart is one of the most vital organs in our body, tirelessly working to keep us alive. When it comes to taking care of your heart, it's crucial to find the right specialist who can provide expert advice and treatment. For those living in Jaipur, a city renowned for its quality healthcare services, there are numerous options available for consulting a cardiologist. This article discusses why it's essential to see a heart doctor, how to find the best cardiologist in Jaipur, and the importance of selecting a heart clinic in Jaipur that best suits your health needs.
Why Consult a Cardiologist?
Heart health is a serious matter that affects millions worldwide. From genetic predispositions to lifestyle choices, many factors contribute to heart-related problems. Regular check-ups with a cardiologist are crucial to identifying any potential issues early on. A cardiologist specializes in diagnosing and treating heart conditions, including hypertension, coronary artery disease, arrhythmias, and heart attacks. Whether you're experiencing symptoms like chest pain, shortness of breath, or irregular heartbeats, or simply want to monitor your heart health, consulting a heart doctor near you is highly recommended.
Finding the Right Cardiologist in Jaipur
When looking for a cardiologist in Jaipur, it’s essential to consider a few key factors to ensure you’re receiving the best care:
Experience and Specialization: Cardiologists have different areas of expertise, so it’s best to select one who specializes in the specific heart issue you may be facing. For example, some may focus on interventional cardiology (like angioplasty), while others might be experts in heart rhythm disorders or heart failure management.
Reputation and Credentials: It’s helpful to look into the credentials, training, and reviews of cardiologists in Jaipur. Board-certified cardiologists with a history of successful treatments are often a safer choice. Referrals from family and friends or searching online for a heart specialist in Jaipur can also be a good starting point.
Location and Accessibility: Having a heart clinic in Jaipur close to you can make a significant difference, especially during emergencies. By finding a reputable heart clinic nearby, you’ll ensure that you have quick access to quality care whenever needed.
Hospital Affiliations: Cardiologists who are associated with well-known hospitals or heart clinics can offer additional benefits, such as access to advanced technology, comprehensive diagnostic tools, and specialized support staff.
Heart Clinics in Jaipur
Jaipur is home to several highly reputed heart clinics that provide a range of cardiovascular treatments. These clinics are equipped with the latest technology for diagnosis and treatment, offering services such as:
Echocardiography: A crucial test for assessing heart function and structure.
Electrocardiogram (ECG): Essential for detecting heart rhythm issues.
Stress Tests: Help in determining how well your heart functions under physical exertion.
Angiography and Angioplasty: For patients who need intervention for blocked arteries.
Cardiac Rehabilitation: Programs aimed at helping patients recover from heart attacks or surgeries.
Visiting a reputable heart clinic in Jaipur can be particularly beneficial because these clinics often employ a team-based approach to heart care, where cardiologists, nurses, and other healthcare professionals work together to provide personalized treatment plans.
Tips for Choosing a Heart Doctor Near You
If you’re looking for a heart doctor near you in Jaipur, it’s essential to do thorough research before deciding. Here are some tips to help guide you in your search:
Check Reviews and Testimonials: Reviews from other patients can provide insight into the doctor’s expertise, bedside manner, and the quality of care they provide.
Consultation Style: Some patients prefer a more hands-on, detailed consultation style, while others may want a quicker, straightforward approach. You can learn more about a cardiologist’s approach through patient feedback or during an initial consultation.
Availability: Choose a cardiologist who is accessible and can provide support in case of an emergency. It’s comforting to know that your doctor is readily available or that the clinic has emergency support around the clock.
Maintaining Heart Health: Preventative Care
Seeing a cardiologist in Jaipur isn't just for those already experiencing heart issues. Preventive care, including regular check-ups, blood pressure monitoring, and maintaining healthy cholesterol levels, is critical to sustaining heart health. Cardiologists can offer lifestyle advice, suggest dietary adjustments, and provide exercise recommendations tailored to individual needs. They may also recommend routine tests, like cholesterol screenings, blood pressure checks, and ECGs, to detect potential issues before they escalate.
Finding a heart specialist in Jaipur who aligns with your health needs and preferences can make a profound difference in managing your heart health. Regular visits to a cardiologist and choosing the right heart clinic nearby can help detect potential issues early, improve quality of life, and possibly even save your life. If you’re concerned about heart health, don’t wait until a symptom escalates; make an appointment with a reliable heart doctor near you to ensure peace of mind and a healthier heart.
0 notes
Text
Finding an Ultrasound Test Near You: What to Expect and How to Choose the Right Facility

If you’re looking for an “ultrasound test near me,” you’re not isolated. Ultrasound imaging has evolved into one of the most generally used diagnostic tools in healthcare, offering a safe, non-invasive way to view the body. Whether you’re pregnant, marketing with a medical situation, or sharing unexplained signs, an ultrasound test delivers clear pictures of organs, tissues, and blood flow. Here’s what you ought to learn about discovering and training for an ultrasound test about you.
What is an Ultrasound Test?
An ultrasound test, also known as sonography, utilizes high-frequency sound locks to create real-time pictures of systems within the body. Unlike X-rays, which use radiation, ultrasounds are typically safe and can be used repeatedly. This makes them ideal for various uses, including monitoring fetal growth during gestation, diagnosing diseases involving the liver, kidneys, and other organs, and guiding systems like biopsies.
How to Find an Ultrasound Test Near You
Research Online: The easiest way to find an ultrasound building nearby is by exploring online. Keywords like “ultrasound test near me” will provide a list of nearby imaging centers, clinics, and clinics that offer these services. Check websites, ratings, and reviews to ensure you’re choosing a respected facility.
Ask Your Doctor for Recommendations: Your physician can often supply referrals to trusted ultrasound providers. They might also advise on what type of ultrasound is best suited for your specific requirements, as some hospitals may specialize in certain types of ultrasounds, like obstetric or vascular.
Check Insurance and Cost: Make sure the facility accepts your insurance or offers affordable rates for self-paying patients. Ultrasound prices vary depending on the type of test and location, so it’s important to confirm these details in advance.
What to Expect During an Ultrasound Test
Ultrasound tests are quick and easy. During the test, a technician applies a gel on the skin and uses a device called a transducer to send sound waves into the body. These sound waves bounce around, making images of the inner systems on a monitor. Most ultrasound exams take about 30 to 45 minutes.
Why Choosing the Right Facility Matters
When it comes to diagnostic imaging, quality matters. Choosing a respected ultrasound center ensures accurate results and reliable service. Look for accredited facilities with experienced radiologists and advanced equipment, as this can make a significant difference in the accuracy of your diagnosis and therapy.
Final Thoughts
Probing for an “ultrasound test near me” is the first step in taking charge of your health. By choosing a trusted facility, preparing for the test, and knowing what to expect, you can make the procedure smooth and stress-free. Whether for regular monitoring or diagnosing a new condition, an ultrasound test is a useful tool in modern medicine.
0 notes