#treatment for Nephrotic
Text
Why Reducing Sodium and Fluid Intake is Crucial for Kids with Nephrotic Syndrome
Did you know that about 12 in every 100,000 children in India are affected by nephrotic syndrome each year? Nephrotic syndrome is a kidney disorder that can cause significant health problems if not managed properly. One of the most important steps in managing this condition is reducing sodium and fluid intake. This might sound simple, but it can make a big difference in a child's health. Additionally, consulting with the best nephrologists in India can provide expert guidance and tailored treatment plans to ensure the best possible outcomes for affected children.
Engaging Stat:
Approximately 12 in 100,000 children in India are diagnosed with nephrotic syndrome annually, highlighting the importance of dietary management for better health outcomes.
The Importance of Dietary Changes:
Nephrotic syndrome causes the kidneys to leak protein into the urine, leading to swelling, especially in the legs and around the eyes. High sodium intake can worsen this swelling, making the condition harder to manage. Excess fluid intake can also increase swelling and blood pressure, putting extra strain on the kidneys. By reducing sodium and fluid intake, children with nephrotic syndrome can prevent these complications and improve their overall health.
Understanding the Benefits:
Lowering sodium and fluid intake helps control swelling and blood pressure, reducing the burden on the kidneys. This can lead to fewer hospital visits and a better quality of life for children. Parents might worry about how to limit these elements in their child's diet. However, many resources and recipes are available to make this transition easier. Choosing fresh fruits and vegetables over processed foods can significantly reduce sodium intake.
Making Healthier Choices:
Parents and children must work together to choose healthier options. Reducing sodium and fluid doesn't mean bland food or constant thirst. Many delicious, low-sodium recipes can be both satisfying and nutritious. It's also essential to teach children about the importance of these dietary changes. By making them part of the decision-making process, kids are more likely to stick to the guidelines.
Five Steps for a healthier you:
Start by gradually reducing the amount of salt in your child's diet. Replace high-sodium snacks with fruits, vegetables, and homemade treats. Encourage your child to drink water instead of sugary drinks and limit their intake of soups and sauces that are often high in sodium. Regularly check food labels to make informed choices.
Gradually Reduce Salt: Start by slowly decreasing the amount of salt in your child's diet. This helps their taste buds adjust to less salty flavors over time.
Choose Healthy Snacks: Replace high-sodium snacks like chips and processed foods with healthier options such as fresh fruits, vegetables, and homemade treats.
Encourage Water Consumption: Promote drinking water instead of sugary drinks, which can contain hidden sodium and extra calories.
Limit High-Sodium Foods: Reduce your child's intake of foods like soups and sauces, which are often high in sodium. Opt for low-sodium or homemade versions whenever possible.
Check Food Labels: Regularly read food labels to identify and avoid high-sodium products. Look for items labeled as "low sodium" or "no added salt."
Conclusion:
In India, managing nephrotic syndrome is a significant challenge, but with the right dietary changes, children can lead healthier lives. Reducing sodium and fluid intake plays a crucial role in controlling symptoms and preventing complications. About 12 in every 100,000 children in India struggle with this condition each year. By making simple yet effective changes to their diet, families can help their children feel better and avoid hospital visits. Have you considered how these dietary adjustments could benefit your child? With the right approach, managing nephrotic syndrome becomes much more manageable. Additionally, seeking advice from the best doctors for nephrotic syndrome treatment in India can provide valuable guidance and ensure that your child receives the most effective care.
FAQ’s:
Q1: What is nephrotic syndrome?Nephrotic syndrome is a kidney disorder that causes the body to excrete too much protein in the urine, leading to swelling, especially in the legs and around the eyes.
Q2: Why is reducing sodium important for children with nephrotic syndrome?Reducing sodium helps to control swelling and lower blood pressure, making it easier for the kidneys to function properly.
Q3: How can I reduce sodium in my child’s diet?You can reduce sodium by avoiding processed and packaged foods, using fresh ingredients, and seasoning foods with herbs and spices instead of salt.
#best nephrologists in india#best nephrologists online consultation#online nephrologists consultation#best doctors for Nephrotic Syndrome treatment india
0 notes
Text
Nephrotic Syndrome Treatment in Homeopathy
Nephrotic Syndrome Treatment in Homeopathy A Gentle Path to Kidney Health Nephrotic Syndrome is a kidney disorder characterized by excessive protein loss in the urine, low blood protein levels, high cholesterol levels, and swelling, particularly in the legs and feet. Homeopathy offers a holistic approach to treating Nephrotic Syndrome by focusing on the individual's overall health and specific symptoms rather than just the disease itself. This treatment aims to stimulate the body's natural healing processes through highly diluted natural substances, tailored to each patient's unique condition. Homoeopathy strives to reduce proteinuria, manage swell, and improve kidney function while minimizing side effects, providing a gentle and personalized path to better kidney health and overall well-being.
0 notes
Text
Nephrotic syndrome treatment
Nephrotic syndrome is a kidney disorder characterized by increased protein levels in the urine, low blood protein levels, high cholesterol levels, and swelling (edema) in various parts of the body. The treatment of nephrotic syndrome aims to reduce proteinuria, manage symptoms, and prevent complications. Here are common treatment approaches:
Medications:
Corticosteroids: The first-line treatment for nephrotic syndrome is usually corticosteroids, such as prednisone. They help reduce inflammation in the kidneys and decrease protein leakage into the urine. A high dose may be prescribed initially, followed by a gradually decreasing maintenance dose.
Immunosuppressive drugs: If corticosteroids alone are ineffective or not well-tolerated, additional immunosuppressive medications like cyclophosphamide, mycophenolate mofetil, or rituximab may be prescribed to further suppress the immune system and reduce proteinuria.
Diuretics: Diuretic medications like furosemide or spironolactone may be used to manage edema by increasing urine output and reducing fluid retention.
Dietary and lifestyle modifications:
Sodium restriction: Limiting sodium intake can help manage edema by reducing fluid retention. This often involves avoiding processed foods and adding less salt to meals.
Low-fat, low-cholesterol diet: A diet low in saturated fats and cholesterol may be recommended to control high cholesterol levels often seen in nephrotic syndrome.
Adequate protein intake: In some cases, protein intake may need to be adjusted to ensure a balance between maintaining protein levels and minimizing proteinuria. This is best determined by a healthcare professional or registered dietitian.
Blood pressure control:
Angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs): These medications are often prescribed to control blood pressure and reduce proteinuria in nephrotic syndrome.
Management of complications:
Blood clot prevention: Nephrotic syndrome increases the risk of blood clots. Medications like anticoagulants (blood thinners) may be prescribed to prevent clot formation.
Vaccinations: It is important for individuals with nephrotic syndrome to stay up to date with vaccinations, particularly for pneumococcal infections and influenza, as they are more susceptible to infections.
Regular follow-up appointments with a healthcare provider are essential to monitor the response to treatment, adjust medication dosages, and address any emerging complications. In some cases, if the underlying cause of nephrotic syndrome is a specific kidney disease, additional treatments such as immunosuppressive therapies or plasmapheresis may be considered.

0 notes
Text
In this article, we will explore the various Ayurvedic Nephrotic Syndrome treatment and their effectiveness. We will also discuss how these cures work.
#ayurvedic nephrotic syndrome treatment#best kidney failure ayurvedic treatment#ayurvedic polycystic kidney disease treatment#kidney problem treatment#ayurvedic clinic#yoga center#ayurvedic treatment#renal stones ayurvedic treatment
0 notes
Text
#Ayurvedic treatment for proteinuria#Proteinuria ayurvedic treatment#Ayurveda treatment for fixing proteinuria#Protein loss in urine treatment in ayurveda#Ayurvedic medicine for proteinuria#Acute kidney disease treatment in ayurveda#Acute kidney failure treatment in ayurveda#Chronic kidney disease treatment in ayurveda#Nephrotic syndrome ayurvedic medicine#Nephrotic syndrome ayurvedic treatment#Ayurvedic medicine for kidney cyst
0 notes
Text
Oedema - pitting vs non-pitting
Oedema is swelling due to excess fluids in tissues.
In pitting oedema, pressing on the affected area leaves an indentation (that persists after removing the pressure). In non-pitting oedema, the area feels firm to touch and does not form indentations.
Pitting oedema:
The excess fluid is mainly composed of water
Commonly caused by heart failure, venous insufficiency, or nephrotic syndrome
Non-pitting oedema:
The excess fluid consists of water WITH protein and salts
Usually indicates a condition of the thyroid / lymphatic system
Different types:
Lymphoedema is due to a build-up of lymphatic fluid (e.g. due to a tumour blocking lymphatic flow / after removal of lymph nodes).
Myxoedema occurs in hypothyroidism and often affected the pretibial or periorbital area.
Angioedema is localised swelling of the skin and is usually due to allergic reactions. It typically affects the face, tongue, larynx, abdomen, arms, and legs. When the larynx is affected, it may affect breathing, which is an emergency!
Lipoedema is when fat accumulates in subcutaneous tissues - it usually affects the legs/buttocks and almost exclusively occurs in postpubertal females (not the same as cellulite!)
If patients present with oedema, it's always important to test if it's pitting or non-pitting as this helps to determine the cause and correct treatment!
#med school#medical student#medicine#revision#medspo#medblr#dermatology#renal#cardiology#oedema#pitting#non-pitting#heart failure
33 notes
·
View notes
Text
*Dr. Smita Goel Homeopathy Clinic*
www.thehomeopathyclinic.co.in
Everyone has protein in their blood. The main protein in your blood is called albumin. Proteins have many important jobs in your body, such as helping to build your bones and muscles, prevent infection and control the amount of fluid in your blood.
Healthy kidneys remove extra fluid and waste from your blood, but let proteins and other important nutrients pass through and return to your blood stream. When your kidneys are not working as well as they should, they can let some protein (albumin) escape through their filters, into your urine. When you have protein in your urine, it is called proteinuria (or albuminuria). Having protein in your urine can be a sign of nephrotic syndrome, or an early sign of kidney disease.
Anyone can have protein in their urine. You may be more at risk for having it if you have one or more of the risk factors for kidney disease, such as:
• Diabetes
• High blood pressure
• Family history of kidney disease
When your kidneys are first starting to have problems, and you do not have a lot of protein in your urine, you will not notice any symptoms. The only way to know if you have protein in your urine is to have a urine test. The test for protein in the urine measures the amount of albumin in your urine, compared to the amount of creatinine in your urine. This is called the urine albumin-to-creatinine ratio (UACR). A UACR more than 30 mg/g can be a sign of kidney disease.
When your kidney damage gets worse and large amounts of protein escape through your urine, you may notice the following symptoms:
• Foamy, frothy or bubbly-looking urine when you use the toilet
• Swelling in your hands, feet, abdomen or face
If you are having these symptoms, your kidney damage may already be severe. Talk to your health care provider immediately about what may be causing your symptoms and what treatment is best for you.
If you have diabetes or high blood pressure, the first and second most common causes of kidney disease, it is important to make sure these conditions are under control by homeopathy.

#greater noida#best homeo clinic in indirapuram#homeopathy for ibs#ghaziabad#homeopathy clinics#homeopathy cold treatment in indirapuram#homeopathy doctor#best skin doctor in ghaziabad#homeopathy#homeopathy medicine#best homeopathy clinic in indirapuram#best homeopathy doctor#homeopathy skin allergies treatment in indirapuram#homeopathy skin allergies treatment in noida#homeopathy specialist in indirapuram#homeopathy treatment#laser treatment in indirapuram#skin specialist in indirapuram#indirapuram#child doctor in noida#child specialist in noida#noida news#nursery school in greater noida#greater noida west#noida#ghaziabad latest news#ghaziabadnews#ayurvedic doctor in ghaziabad#wave city ghaziabad#best schools in ghaziabad
2 notes
·
View notes
Text
Dr. Sidharth Sethi — Delhi’s Trusted Name in Pediatric Kidney Care

Dr. Sidharth Sethi — Delhi���s Trusted Name in Pediatric Kidney Care
When it comes to pediatric kidney care, choosing the right specialist is of utmost importance. In the bustling city of Delhi, one name consistently stands out for delivering exceptional care to children with kidney disorders — Dr. Sidharth Sethi. Recognized as the Best Pediatric Nephrologist in Delhi, Dr. Sethi’s dedication to treating young patients has earned him immense trust and admiration from both medical professionals and families alike.
Expertise in Pediatric Nephrology
Dr. Sidharth Sethi is well-known for his comprehensive approach to diagnosing and treating a wide array of pediatric kidney conditions. From chronic kidney disease and nephrotic syndrome to rare genetic disorders affecting kidney function, Dr. Sethi’s skill set is unmatched. His use of the latest medical technologies and treatments, combined with his compassionate care, has made him the Best Pediatric Nephrologist in Delhi for families seeking expert treatment.
Compassionate and Patient-Centered Care
Parents consistently commend Dr. Sidharth Sethi for his empathetic approach to pediatric care. He ensures that both children and their families fully understand the medical conditions they are facing, which is crucial in managing long-term treatments. This patient-centered focus has made him a go-to choice for those looking for the Best Pediatric Nephrologist in Delhi. His ability to balance medical expertise with a warm, reassuring demeanor is what sets him apart from others.
Why Choose Dr. Sidharth Sethi?
Comprehensive Treatment Plans: Dr. Sethi tailors his approach to the unique needs of each patient, ensuring that treatment is not only effective but also minimally invasive where possible.
State-of-the-Art Facilities: As the Best Pediatric Nephrologist in Delhi, Dr. Sethi practices in some of the best healthcare facilities in the city, offering cutting-edge treatments for complex kidney conditions.
Reputation for Excellence: Dr. Sidharth Sethi’s years of experience and his consistent track record of successful treatments make him the top choice for pediatric kidney care.
A Trusted Name in Pediatric Kidney Care
Parents want the very best for their children, especially when it comes to health. Dr. Sidharth Sethi’s reputation as the Best Pediatric Nephrologist in Delhi is built on his commitment to providing exceptional care, his dedication to staying at the forefront of medical advances, and his ability to form strong, trusting relationships with his patients and their families. If you are searching for a specialist to treat your child’s kidney issues, you can feel confident placing your trust in Dr. Sethi.
To schedule an appointment With the Best Child Kidney Doctor in India, please contact:
Name: Dr. Sidharth Sethi (Best Child Kidney Doctor in India)
Address: Division of Pediatric Nephrology, Kidney Institute, Medanta, The Medicity, Gurgaon, Haryana, India, 122001
Phone: 0124–4141414
Website: www.pediatricnephrologyindia.com
1 note
·
View note
Text
Rare Kidney Diseases Market To Witness High Growth Owing To Increasing Government Support For Rare Disease Research

The rare kidney diseases market has witnessed a significant growth owing to the rise in government initiatives to support rare disease research. Rare kidney diseases are a subset of rare diseases affecting the kidneys, which includes conditions like cystic kidney disease and nephrotic syndrome. These conditions severely impact kidney functioning and require lifelong treatment. The increasing focus on development of novel treatment options has resulted in growth of this market.
The Rare Kidney Diseases Market is estimated to be valued at US$ 3.9 Bn in 2024 and is expected to exhibit a CAGR of 11% over the forecast period 2024-2031.
Key Takeaways
Key players operating in the rare kidney diseases are Seres Therapeutics, Inc.,Enterome,4D pharma plc,International Flavors & Fragments Inc.,OptiBiotix Health Plc. These players are engaging in new product launches and research collaborations to expand their offerings in the market.
The growing prevalence of rare kidney disorders is a major factor driving the demand for treatment and management of these conditions. As per estimates, rare kidney diseases affect over 12 million people worldwide each year. The lack of approved treatment options also presents lucrative opportunities for market players.
Technological advancements like development of gene and cell therapies hold potential to revolutionize the treatment of rare kidney diseases. Several clinical trials are ongoing to evaluate the therapeutic potential and safety of novel treatment approaches like CRISPR for genetic rare kidney diseases.
Market Trends
Growing focus on precision medicine: Researchers are actively exploring ways to develop more personalized and targeted treatment approaches for rare kidney diseases based on patient genetics and biomarkers. This includes development of molecular biomarkers for early disease diagnosis and precision therapeutics.
Increasing clinical trial activity: A large number of phase 2 and phase 3 clinical trials are being conducted to evaluate new products in conditions like primary hyperoxaluria and nephrotic syndrome. The successful development of these pipeline drugs can drive revenue generation in the coming years.
Market Opportunities
Orphan drug designation: Regulatory agencies provide incentives like market exclusivity to support development of drugs for rare diseases. Many companies are leveraging these benefits by obtaining orphan drug status for pipeline candidates.
Partnerships and collaborations: Establishing strategic collaborations is one of the focus areas of companies to access advanced research capabilities and technologies for developing innovative therapies. Both large and small players are actively partnering for product development.
Impact Of COVID-19 On Rare Kidney Diseases Market
The COVID-19 pandemic had a significant impact on the rare kidney diseases market. During the initial outbreak and lockdowns imposed worldwide, disrupted supply chains hampered the manufacturing and distribution of drugs and medical devices used for treating rare kidney diseases. This led to shortages and delays in treatment for many patients. Telemedicine saw increased adoption as visiting hospitals became risky. However, virtual consultations could not replace in-person monitoring and treatment needed by many rare kidney patients. Research and clinical trials also faced delays due to delayed approvals, non-availability of participants and investigators, etc. The economic slowdown impacted fund raising for pharmaceutical companies and startups working on drug development for rare kidney conditions.
As restrictions have eased in 2022, the market is recovering slowly. Manufacturing and supply chains have stabilized while maintaining necessary safety protocols. Although telemedicine continues to play a supportive role, most patients have resumed visiting hospitals and care centers for treatment. Drug developers are making efforts to recover lost time by fast-tracking certain clinical trials. Governments and private organizations are providing funding support to help accelerate research. It is expected that the market will regain its pre-pandemic growth levels by 2024. However, risks of future waves persist and the long-term impact of the pandemic on this market remains uncertain.
The rare kidney diseases market in North America holds the largest share globally, both in terms of value and volume. This is due to high awareness, favorable reimbursement policies, presence of major pharmaceutical companies and advanced healthcare facilities in the US and Canada. Europe is the second largest market. The Asia Pacific region is witnessing fastest growth and rising cases of rare kidney diseases are driving market growth in countries like India, China and Japan. Africa and Latin America are expected to offer emerging opportunities with economic development and expanding healthcare access in the future.
The rare kidney diseases market in China is growing at the fastest rate globally. This is owing to China's huge population size which increases the patient pool for rare diseases, rising healthcare spending, growing medical tourism and strong government support for the biopharmaceutical industry. Other dynamic Asian markets include India and Japan due to their large generics manufacturing base and rapidly aging demographics respectively. Government schemes for rare disease treatment are boosting market growth in India.
Get more insights on this topic: https://www.pressreleasebulletin.com/rare-kidney-diseases-market-to-register-significant-growth-due-to-advances-in-microbiome-therapeutics/
Author Bio:
Alice Mutum is a seasoned senior content editor at Coherent Market Insights, leveraging extensive expertise gained from her previous role as a content writer. With seven years in content development, Alice masterfully employs SEO best practices and cutting-edge digital marketing strategies to craft high-ranking, impactful content. As an editor, she meticulously ensures flawless grammar and punctuation, precise data accuracy, and perfect alignment with audience needs in every research report. Alice's dedication to excellence and her strategic approach to content make her an invaluable asset in the world of market insights. (LinkedIn: www.linkedin.com/in/alice-mutum-3b247b137 )
What Are The Key Data Covered In This Rare Kidney Diseases Market Report?
:- Market CAGR throughout the predicted period
:- Comprehensive information on the aspects that will drive the Rare Kidney Diseases's growth between 2024 and 2031.
:- Accurate calculation of the size of the Rare Kidney Diseases and its contribution to the market, with emphasis on the parent market
:- Realistic forecasts of future trends and changes in consumer behaviour
:- Rare Kidney Diseases Industry Growth in North America, APAC, Europe, South America, the Middle East, and Africa
:- A complete examination of the market's competitive landscape, as well as extensive information on vendors
:- Detailed examination of the factors that will impede the expansion of Rare Kidney Diseases vendors
FAQ’s
Q.1 What are the main factors influencing the Rare Kidney Diseases?
Q.2 Which companies are the major sources in this industry?
Q.3 What are the market’s opportunities, risks, and general structure?
Q.4 Which of the top Rare Kidney Diseases companies compare in terms of sales, revenue, and prices?
Q.5 Which businesses serve as the Rare Kidney Diseases’s distributors, traders, and dealers?
Q.6 How are market types and applications and deals, revenue, and value explored?
Q.7 What does a business area’s assessment of agreements, income, and value implicate?
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it
#Rare Kidney Diseases Market Trend#Rare Kidney Diseases Market Size#Rare Kidney Diseases Market Information#Rare Kidney Diseases Market Analysis#Rare Kidney Diseases Market Demand
0 notes
Text
Pediatric Kidney Care: Specialized Treatment for Children
Kidney health is vital for overall well-being, and this is especially true for children. Pediatric kidney care focuses on diagnosing, treating, and managing kidney-related conditions in children. Specialized treatment ensures that young patients receive the appropriate care tailored to their unique physiological and developmental needs.
Importance of Pediatric Kidney Care
1. Early Diagnosis: Children are at risk of developing various kidney conditions, some of which may be congenital (present at birth) or acquired later in childhood. Early diagnosis is crucial for effective treatment and preventing long-term complications.
2. Growth and Development: Kidney health plays a significant role in a child's growth and development. Proper kidney function is essential for maintaining fluid and electrolyte balance, blood pressure, and overall metabolism. Any disruption in kidney function can impact these processes and, consequently, the child's development.
Common Pediatric Kidney Conditions
1. Congenital Abnormalities:
Polycystic Kidney Disease (PKD): A genetic disorder characterized by the growth of numerous cysts in the kidneys.
Hydronephrosis: Swelling of a kidney due to a build-up of urine, often caused by a blockage in the urinary tract.
Vesicoureteral Reflux (VUR): A condition where urine flows backward from the bladder to the kidneys.
2. Acute Kidney Conditions:
Acute Kidney Injury (AKI): A sudden decline in kidney function, often caused by dehydration, infection, or medications.
Nephrotic Syndrome: A disorder that causes the kidneys to leak large amounts of protein into the urine.
3. Chronic Kidney Conditions:
Chronic Kidney Disease (CKD): A long-term condition characterized by gradual loss of kidney function.
Glomerulonephritis: Inflammation of the kidney's filtering units, which can lead to kidney damage.
Specialized Treatment Approaches
1. Multidisciplinary Care: Pediatric kidney care often involves a team of specialists, including pediatric nephrologists, urologists, dietitians, and social workers. This multidisciplinary approach ensures comprehensive care addressing all aspects of the child's health.
2. Diagnostic Tools: Advanced diagnostic tools are used to accurately diagnose kidney conditions in children. These may include:
Ultrasound: Imaging to detect structural abnormalities.
Blood Tests: To assess kidney function and detect any underlying conditions.
Urine Tests: To check for protein, blood, and other abnormalities.
3. Medical Management:
Medications: Depending on the condition, various medications may be prescribed, including diuretics, antihypertensives, and immunosuppressants.
Dietary Modifications: Nutrition plays a crucial role in managing kidney conditions. A dietitian can help create a diet plan that supports kidney health and addresses specific dietary needs.
4. Surgical Interventions: Some kidney conditions may require surgical intervention. Pediatric surgeons specialize in procedures such as:
Correction of urinary tract obstructions
Repair of congenital abnormalities
Kidney transplantation for severe cases of kidney failure
Support for Families
1. Education: Educating families about their child's kidney condition and treatment options is crucial. Understanding the condition helps parents and caregivers make informed decisions and provide better support for their child.
2. Emotional Support: Dealing with a chronic or severe kidney condition can be challenging for both the child and the family. Emotional support, including counseling and support groups, can help families cope with the stress and anxiety associated with the condition.
3. Ongoing Monitoring: Regular follow-up appointments and monitoring are essential to track the child's progress and adjust treatment plans as needed. This ensures that any changes in the child's condition are promptly addressed.
Conclusion
Pediatric kidney care requires specialized treatment tailored to the unique needs of children. Early diagnosis, a multidisciplinary approach, and ongoing support for families are crucial components of effective pediatric kidney care. By providing comprehensive and specialized care, healthcare professionals can help children with kidney conditions lead healthier, more fulfilling lives.
Credits : https://chennaikidneycare.com/
#best urology doctor#pediatric urology#urology doctor#urology specialist#urologist surgeon#best urology hospital in chennai#best urologists in chennai#urinary incontinence#urinary tract infection
0 notes
Text
Understanding the Link Between Hepatitis B and Nephrology: A Comprehensive Overview
Introduction
Hepatitis B, a viral infection that affects the liver, is a significant global health concern. Nephrology, the medical specialty focusing on kidney health, may seem unrelated at first glance. However, the interplay between Hepatitis B and kidney health is crucial and warrants deeper understanding. This blog aims to explore the intricate relationship between Hepatitis B and nephrology, shedding light on how this liver infection can impact kidney function and the role of nephrologists in managing affected patients.
What is Hepatitis B?
Hepatitis B is caused by the Hepatitis B virus (HBV), which leads to liver inflammation. It's transmitted through contact with infectious body fluids, such as blood, semen, and vaginal secretions. The infection can be acute or chronic. Chronic Hepatitis B can lead to severe liver conditions, including cirrhosis and liver cancer. According to the World Health Organization (WHO), an estimated 296 million people were living with chronic Hepatitis B infection in 2019, highlighting its widespread impact.
Call for Online Speaker /Poster
Participate at the CME/CPD accredited 14th World Gastroenterology, IBD & Hepatology Conference from December 17-19, 2024, in Dubai, UAE & Virtual.
WhatsApp us: https://wa.me/442033222718?text=
Virtually Registration Here: https://gastroenterology.universeconferences.com/virtual-registration/

The Connection Between Hepatitis B and Kidney Health
Glomerulonephritis: One of the primary ways Hepatitis B impacts kidney health is through glomerulonephritis, a condition characterized by inflammation of the kidney's filtering units (glomeruli). HBV-associated glomerulonephritis can result from the deposition of immune complexes (HBV antigens and antibodies) in the glomeruli, leading to kidney damage. Symptoms include proteinuria (excess protein in urine), hematuria (blood in urine), and in severe cases, nephrotic syndrome.
Membranous Nephropathy: Chronic Hepatitis B can lead to membranous nephropathy, a type of glomerulonephritis. This condition is marked by the thickening of the glomerular basement membrane due to immune complex deposition, causing proteinuria and edema. Early diagnosis and management are critical to prevent progression to chronic kidney disease (CKD).
Polyarteritis Nodosa (PAN): PAN is a systemic vasculitis that can be associated with HBV. It affects small and medium-sized arteries, including those supplying the kidneys, leading to renal ischemia, hypertension, and renal insufficiency. PAN requires prompt treatment to prevent severe renal and systemic complications.
Role of Nephrologists in Managing Hepatitis B-Related Kidney Conditions
Nephrologists play a pivotal role in the management of kidney diseases associated with Hepatitis B. Their responsibilities include:
Early Detection: Identifying renal involvement in patients with Hepatitis B through regular screening for proteinuria, hematuria, and renal function tests.
Diagnosis: Utilizing renal biopsy when necessary to diagnose the specific type of glomerulonephritis or other renal pathologies linked to HBV.
Treatment: Implementing antiviral therapy to reduce HBV viral load, which can help alleviate renal symptoms. Common antiviral agents include tenofovir and entecavir. In addition, immunosuppressive therapy might be required for conditions like membranous nephropathy.
Monitoring: Regularly monitoring kidney function and adjusting treatments as needed to prevent progression to CKD or end-stage renal disease (ESRD).
Collaboration: Working closely with hepatologists and infectious disease specialists to provide comprehensive care to patients with HBV and renal involvement.
Preventive Strategies
Preventing Hepatitis B and its complications is critical. Strategies include:
Vaccination: The Hepatitis B vaccine is highly effective and recommended for all infants, unvaccinated adults at risk, and healthcare workers.
Safe Practices: Avoiding the sharing of needles, practicing safe sex, and ensuring blood products are screened for HBV.
Regular Health Checks: Routine screening for HBV in high-risk populations can lead to early detection and treatment, reducing the risk of renal complications.
Call for Online Speaker /Poster
Participate at the CME/CPD accredited 14th World Gastroenterology, IBD & Hepatology Conference from December 17-19, 2024, in Dubai, UAE & Virtual.
WhatsApp us: https://wa.me/442033222718?text=
Virtually Registration Here: https://gastroenterology.universeconferences.com/virtual-registration/

Avoiding Hepatitis B and its potential impact on kidney health requires a combination of preventive measures, lifestyle choices, and regular medical check-ups. Here are some strategies to help you avoid Hepatitis B and maintain kidney health:
Preventing Hepatitis B
Vaccination:
Get Vaccinated: The Hepatitis B vaccine is the most effective way to prevent the infection. It is typically given as a series of three to four shots over six months. Ensure you and your family members, especially newborns, are vaccinated.
Safe Practices:
Avoid Sharing Needles: Do not share needles or syringes. This includes not just illicit drug use but also any medical or cosmetic procedures involving needles.
Safe Sex: Use condoms during sexual activity, especially with partners whose HBV status is unknown. Limit the number of sexual partners.
Blood Safety: Ensure any blood transfusions or organ transplants come from HBV-screened donors.
Personal Items: Do not share personal items like razors, toothbrushes, or nail clippers, as they might have blood on them.
Healthcare Settings:
Infection Control: Ensure that healthcare providers follow standard precautions, including the use of gloves and sterilized equipment.
Tattoos and Piercings: Choose reputable facilities that follow strict hygiene and sterilization protocols.
Maternal Transmission:
Prenatal Care: Pregnant women should be screened for HBV. If positive, appropriate measures can be taken to prevent transmission to the newborn.
Maintaining Kidney Health
Hydration:
Drink Plenty of Water: Staying hydrated helps your kidneys function properly by flushing out toxins from your body.
Healthy Diet:
Balanced Diet: Eat a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Reduce salt intake to prevent high blood pressure, which can damage the kidneys.
Limit Protein Intake: Excessive protein can strain the kidneys. Consult with a healthcare provider to determine an appropriate protein intake.
Regular Exercise:
Stay Active: Regular physical activity helps maintain a healthy weight, lowers blood pressure, and improves overall kidney function.
Avoid Toxins:
Limit NSAIDs: Overuse of nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can harm the kidneys. Use these medications sparingly and under medical supervision.
Avoid Smoking and Excessive Alcohol: Both smoking and heavy alcohol use can damage the kidneys.
Monitor Health Conditions:
Blood Pressure and Diabetes: Keep blood pressure and blood sugar levels under control. Hypertension and diabetes are major risk factors for kidney disease.
Regular Check-ups: Routine medical check-ups can help detect early signs of kidney problems. If you have a family history of kidney disease, more frequent monitoring may be necessary.
Manage Chronic Conditions:
Treat Infections Promptly: Any infections, especially urinary tract infections, should be treated promptly to prevent kidney damage.
Medication Management: If you have chronic conditions like diabetes or hypertension, follow your treatment plan diligently and take medications as prescribed.
Combining Efforts for Overall Health
Regular Screenings:
HBV Screening: Get tested for Hepatitis B if you are at risk. Early detection allows for better management and reduces the risk of transmission.
Kidney Function Tests: Regular tests like serum creatinine and urine albumin can help monitor kidney health.
Education and Awareness:
Stay Informed: Educate yourself and others about Hepatitis B and kidney health. Awareness can lead to better prevention and early intervention.
Call for Online Speaker /Poster
Participate at the CME/CPD accredited 14th World Gastroenterology, IBD & Hepatology Conference from December 17-19, 2024, in Dubai, UAE & Virtual.
WhatsApp us: https://wa.me/442033222718?text=
Virtually Registration Here: https://gastroenterology.universeconferences.com/virtual-registration/

Conclusion
The relationship between Hepatitis B and kidney health underscores the importance of a multidisciplinary approach in managing affected patients. Nephrologists, with their expertise in kidney diseases, are essential in diagnosing, treating, and monitoring renal conditions associated with HBV. Through collaborative care, early intervention, and preventive measures, the adverse renal outcomes of Hepatitis B can be effectively managed, improving patient outcomes and quality of life.
0 notes
Text
Turmeric: A Promising Aid for Nephrotic Syndrome
Discover the potential of Turmeric as a game-changer in the battle against Nephrotic Syndrome. Explore the benefits of Turmeric's natural remedies for Nephrotic Syndrome, including its role in reducing the need for albumin infusion. Uncover the quest for a permanent cure and the best treatment options available for Nephrotic Syndrome. Unlock the power of nature in treating this condition. Take the first step towards a healthier you with Turmeric's promising aid. Embrace a holistic approach to Nephrotic Syndrome management today. Click now to learn more and embark on your journey to a brighter, healthier future.
https://www.ayurvedickidneycare.com/nephrotic-syndrome-ayurvedic-treatment
#albumin infusion in nephrotic syndrome#nephrotic syndrome permanent cure.#best treatment for nephrotic syndrome#natural remedies for nephrotic syndrome#nephrotic syndrome natural treatment
0 notes
Text
Nephrotic Syndrome Treatment
The two basic types of the glomerular disease include nephritic and nephrotic, but with some diseases, the two types can overlap.
Nephritic disease ("glomerulonephritis") is defined by the presence of blood (Hematuria) and protein (Proteinuria) in the urine and the presence of hypertension clinically. There may or may not be significant impairment of kidney function. Sometimes, a person suffering from glomerulonephritis may not exhibit any symptoms, and their condition may go unnoticed until blood and protein are discovered during a routine urinalysis.
Hematuria and impaired kidney function are common in people with the more severe nephritic disease. Urine testing may also reveal high protein levels, as well as edema (swelling in the lower legs) or high blood pressure.
Examples of conditions that may cause glomerulonephritis include:Immunoglobulin A (IgA) nephropathy
Systemic Lupus Erythematosis (SLE)
Vasculitis
Certain bacterial and viral infections (post infectious glomerulonephritis)
Mixed cryoglobulinemia
Alport syndrome
IgA vasculitis (Henoch-Schönlein purpura)
C3 glomerulopathy
Nephrotic syndrome — People with nephrotic syndrome have protein in the urine (proteinuria) but, often, little to no blood in the urine (hematuria). Kidney function may worsen if nephrotic syndrome progresses with time.
Examples of conditions that may cause nephrotic syndrome include:
Focal segmental glomerulosclerosis
Membranous nephropathy (including lupus)
Diabetic nephropathy
Post infectious glomerulonephritis (later stage)
IgA nephropathy
Primary amyloidosis or the related disorder light chain deposition disease

0 notes
Text
Ayurvedic Nephrotic Syndrome Treatment with Doctor consultation! Get the complete process of Treatment and medicines.
#nephrotic syndrome ayurvedic treatment#best kidney failure ayurvedic treatment#kidney failure treatment#protein urea treatment#ayurvedic clinic#ayurvedic treatment#Renal stones ayurvedic treatment#yoga center#ayurveda yogashram
0 notes
Text
How Does Kidney Disease Cause Hypertension?
How Does Kidney Disease Cause Hypertension?
Hypertension is also known as high blood pressure. This can lead to serious health complications and an increased risk of cardiovascular disease, stroke, chronic kidney disease, and sometimes death. Blood pressure is the force that a person’s blood exerts on the walls of blood vessels, which affects how the heart works. Many people suffer from this chronic disease without knowing that they have…

View On WordPress
#Acute kidney disease treatment in ayurveda#Acute kidney failure treatment in ayurveda#Ayurveda treatment for fixing proteinuria#Ayurvedic treatment for proteinuria#Chronic kidney disease treatment in ayurveda#Nephrotic syndrome ayurvedic medicine#Nephrotic syndrome ayurvedic treatment#Polycystic kidney disease ayurvedic treatment#Polycystic kidney disease treatment in ayurveda#Protein loss in urine treatment in ayurveda#Proteinuria ayurvedic treatment
0 notes
Text
Antithrombin Market Size, Trend, Analysis and Forecast (2021-2027)
The antithrombin market is anticipated to grow at a CAGR of approximately 5% during the forecast period. Antithrombin, a protein produced by the liver and present in blood, plays a crucial role in inhibiting blood clotting by inactivating thrombin. Deficiency in antithrombin can arise from conditions such as nephrotic syndrome, liver failure, severe trauma, metastatic tumors, and genetic mutations. Additionally, advancements in drug administration technology and an increase in blood clotting disorders are fueling market growth. Antithrombin deficiency heightens the risk of thromboembolism, which can lead to excessive bleeding during surgeries. Antithrombin III is commonly used for extracorporeal membrane oxygenation (ECMO) during cardiopulmonary bypass. According to the National Institutes of Health (NIH), approximately 310 million surgeries are performed annually in the U.S.
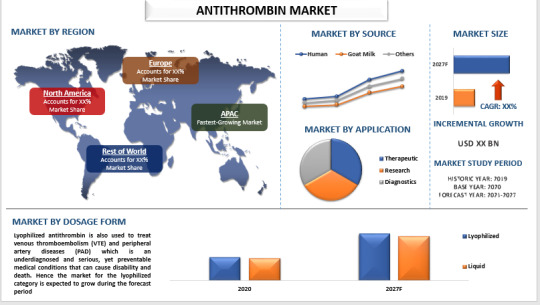
Market Segmentation by Application
The antithrombin market is segmented into therapeutic, research, and diagnostics. In 2020, the therapeutic segment is expected to experience significant growth, driven by the rising number of cardiac surgeries, ongoing drug research and development, and increasing prevalence of heart-related diseases such as atrial fibrillation and heart failure. The demand for antithrombin in therapeutic applications is on the rise, as antithrombic drugs and treatments are crucial for managing heart diseases. For example, the Centers for Disease Control and Prevention (CDC) estimates that 12.1 million people in the U.S. will have atrial fibrillation (AFib) by 2030.
For a comprehensive analysis of the market drivers, visit: https://univdatos.com/report/antithrombin-market/
Market Segmentation by Source
The antithrombin market is categorized into human, goat milk, and others. The goat milk segment is projected to see substantial growth due to its proven medical efficacy. Goat milk is a significant external source of antithrombin, capable of producing as much antithrombin in a year as 90,000 blood donations. Factors such as increasing cases of blood clotting, high blood pressure, high cholesterol, and cardiac surgeries are driving this market segment. Key market players are also launching new products to address antithrombin deficiency.
Market Segmentation by Dosage Form
The market is divided into lyophilized and liquid forms. The lyophilized segment held a significant market share and is expected to grow considerably, primarily due to its use in treating thrombin deficiency and coronary heart diseases (CAD). According to the CDC, around 18.2 million adults have coronary artery disease. Additionally, lyophilized antithrombin is used to treat venous thromboembolism (VTE) and peripheral artery diseases (PAD), serious yet preventable conditions that can cause disability and death. This segment is expected to see continued growth.
Regional Market Analysis
The report provides a comprehensive analysis of major regions, including North America (U.S., Canada, Rest of North America); Europe (Germany, U.K., France, Spain, Italy, Rest of Europe); Asia-Pacific (China, India, Japan, Australia, South Korea, Rest of Asia-Pacific); and the Rest of the World. In 2020, North America held a significant market share, driven by the high prevalence of heart disease, a large population, availability of skilled healthcare professionals, and major pharmaceutical companies. The region also sees a high incidence of blood clots, further contributing to market growth. According to the CDC, as many as 100,000 people in the U.S. die from blood clots each year, costing the nation up to $10 billion annually.
For a sample report, visit: https://univdatos.com/get-a-free-sample-form-php/?product_id=23070
Major Companies
Key players in the antithrombin market include Grifols S.A., Octapharma AG, LFB USA Inc., CSL Limited, Takeda Pharmaceuticals, Axis-Shield Plc, Siemens AG, Thermo Fisher Scientific, Lee Biosolutions Inc., and BDI Pharma Inc.
Contact Us:
UnivDatos Market Insights
Email - [email protected]
Contact Number - +1 9782263411
Website -www.univdatos.com
#Antithrombin Market#Antithrombin Market Size#Antithrombin Market Report#Antithrombin Market Forecast
0 notes