#third party payer
Explore tagged Tumblr posts
Text
There should literally be no such thing as an "insurance denial." If a doctor prescribes something for their patient, a third party payer should not have any authority to deny that.
Their job is to hold the money & to dole it out for medical needs. It's not their job to decide what those medical needs are. That's a doctor's job.
And not just any doctor's job. That's specifically just your doctor's job. The person whom you authorized to actually evaluate you directly.
Once you go to a doctor and your doctor says "ok you need This Medical Thing" that should be the end of the conversation. The insurer simply is tasked with dispensing the check accordingly.
If our healthcare system wasn't just an inhumane cash grab perpetuated by heartless ghouls, it would operate like this. And also it would be guaranteed to everyone, but I digress.
161 notes
·
View notes
Text
...I feel like when people end up griping about how others say "both parties are the same" in the context of US politics, in pushing back against that sentiment they kinda overlook what's animating a decent part of it.
Cause, like, the parties are in fact very different, given one's the Unhinged Fascist Khorne Cult Party and the other is Everyone Else, but I've noticed that at the root of the complaint that the parties are the same; especially on the left; it's rooted in less what they do and more in what they won't do.
IE, the policies that would actually help them are so far outside of the Overton Window due to a combo of right-wing dominance and the Dems being bitch-ass cowards and brown-nosers, that they feel that the parties are interchangable because the results in terms of things that will get done for them is the same, IE jack shit.
Like, the big one is single-payer healthcare, but I think we can cite other examples, we've all seen 'em.
And like, y'all know me, I'm super critical of anti-electoralism, if only because we're not doing shit to solve my big issue (copyright being Too Fucking Long and Too Fucking Much) without engaging at least a bit with the electoral system, and ditto for a lot of other issues.
Instead of nonvoting or trying to brute-force third parties in a system designed to crush them, I generally believe in stuff like Ranked Choice Voting, the Interstate Voting Compact and murdering the filibuster as better levers to push so we can kill the two-party system and get shit done that isn't "blow up civillians overseas" or "pass yet another censorship bill"
But I feel like acting like people saying "both parties are the same" is nihilism and not a statement of feeling underrepresented aren't really helping, and comes off as apologizing for the assholes who failed them because they cared more about lobbyist money or institutionalism than human fucking life.
And it does so in a way that definitely isn't gonna get people to vote or; more importantly; isn't gonna help at getting those people on your side to do things to create a world where they actually are represented.
#voting#parties#this is where monopolies lead#two party system bad#representation#democracy#us politics
34 notes
·
View notes
Note
Hey I want to understand
What are your current economic beliefs and ideology?
Cynical independent voter, unaligned. My economic/class position and race/gender are probably important too, but really, that just tells you more about where my self-interest is located, not if I am following it.
Seriously though, I can’t really say no honestly to almost any “are you now or have you ever been” because I’ve been most things for at least five minutes, and have taken something of value from most of them. I mostly have a lot of things that don’t work. Also, my particular location irt economic/class position and race/gender is pretty much “you’re not exactly any team’s target demographic, you’re screwed by both sides while both claim to represent your interests. Also you will be in the second or third wave of people up against the wall When The Revolution Comes/Day of the Rope at best due to things you cannot change, so better hope neither of those happen.” Like, I am on both teams’ long lists of people that will get stern visits at minimum due to family members’ affiliations, anything else aside.
I have become more and more cynical about anything other than raw self-interest, in-group preference, and the vicious righteous joy of the hunt at acceptable targets. Raw self-interest is frequently a counterbalance on the last two, and what qualifies as in-group is malleable, and righteous urge to punish is just “justice” when in moderation and under control of law rather than mob lynching, so none of those motivations are entirely bad… but they’re also absolutely not entirely good either.
To be more detailed, I was raised in a Blue state in a single party Democratic area in a politically involved fundamentalist Christian religious right Republican family, then started looking into anarchism and libertarianism basically as soon as I was free to make my own choices. I was already aware of the absurdity of communists through college professors who said things like “nobody ever starved to death under communism” in class, so it always seemed like a nonstarter of an ideology to people who cared about truth and not doing genocides/famines.
Economically… I am not going to give you an option on the gold standard or the interest rate because I don’t have one. I voted for Bernie every time he was an option… and I voted Libertarian in 2016. I would like to own a house or even an apartment, but I understand why people like me (not a STEMlord/STEMdigger/boomer) will never be allowed to own capital, and that again, there’s no real political will to change that. Being very explicitly denied the literal privilege of buying into the system rather puts me off it, but any alternative is almost certainly worse for me.
Also I like eating and being clothed and receiving healthcare sometimes and grew up poor enough that I know that not getting enough of those things is like. I don’t want to starve or not receive healthcare, and I don’t really want those things to happen to others either. But I also understand that food doesn’t come from grocery stores and healthcare isn’t spontaneously generated either.
I believe that single payer healthcare would be a significant improvement in efficiency in the United States, but it is unlikely that it will happen due to the ludicrous amount of GDP that is being skimmed, and the fact that the rest of the world benefits from it, so the forces against it are extremely strong.
I would like free speech, freedom of religion, all that Rockwell shit for everyone, but I am starting to have doubts about the practicality of that in an internet age.
Oh yeah also I believe that human beings are animals and that there is no god, afterlife, or spiritual dimension, but it’s psychologically helpful for many people to believe that there is, because life is hard and people need to believe that they will be with their dead loved ones again in the afterlife and it all means something and justice prevails in the end. And I am not into damaging other people psychologically because of ideology alone, also this belief doesn’t exactly make me happy or more pro social so I don’t really go around trying to convince others to stop believing in god if it’s working for them and not causing problems for others.
#oh geez I can tag asks now#cynical#it’s the economy stupid#class in the us#american politics#race and class#housing crisis#self interest#I have more to lose than my chains bro#the wreckage of my anarchism#the wreckage of my christianity#the wreckage of my atheism
15 notes
·
View notes
Text
Hi there. I'm back with theory #3 for Sylus' myth. Which....might be less evidence-heavy than the first two and really just me talking out of my ass. I started writing at midnight because that's just on brand clown behavior of me 🙃 ANYWAY...
People who haven't read Rafayel, Xavier, and Zayne's myths, please tread carefully, because I will touch upon them briefly and allude to events in their myths.
Quick recap from first post:
Theory 1: Sylus and MC must have been destined lovers in a past life, but due to whatever conflict, Sylus decided to break his bond with her for her protection and accept any punishment that comes with it, which could mean to be ruler of a place he has no desire for, an imprisonment of sort.
Theory 2: Destined lovers, but perhaps a third party interfered out of jealousy or spite. Could Sylus have been caught and framed of a crime and been literally imprisoned, thus forcing him and MC to separate?
So...I half-joked in a post that my new theory is that Sylus sold his soul to the devil. Or, you know, maybe he is the devil himself. This is partly stemmed from the Long-Awaited Revelry trailer, which has the word "demon" over a shot of him and later in the same trailer, one of Sylus' companion forms is aptly titled "Otherworldly Visitor". Make of that as you will.


And with the new trailer for No Defense Zone, we see that Sylus' right eye glows in a demonic way, similar to his in the LAR trailer. Even the atmosphere in both scenes seem a bit supernatural. Now....I didn't want to go there, but, um................do you suppose he is an incubus? 😭😭😭 The shot after "demon" has the word "desire," which can have a sexual connotation.
For those who don't know, an incubus is a male demon who preys on women sexually.......it would explain his kinky behavior in NDZ 💀 but I digress.......
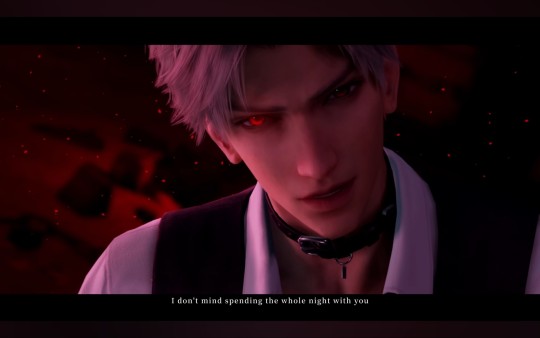

Some of the first lines we hear from Sylus:
"Even if you wanted to sell your soul, you still have to find someone who can pay the price."
"Want some help? Yes? No? Maybe so?"
These lines reinforce the idea of "deal with the devil". In the new theme song, Visions opposées, the singer also sings this line: "Mais c'est le prix à payer" (But that's the price to pay). It could just be figurative, or it could hold some literal truth, because I found it interesting how that verse overlaps with Sylus' scenes. I doubt it's a coincidence since the devs are so good at planting seeds.
From the chorus, in order, we hear:
[MINOR RAFAYEL, XAVIER, & ZAYNE SPOILERS]
"But that's the price to pay / o'love" - Rafayel, God of the Sea, is separated by MC. His price? His civilization.
"Stars will always shine / But with pain" - Xavier and MC are separated (side note: I don't have the second half of Xavier's first myth yet, so I can't elaborate too much. But I've seen enough references to understand the scene depicted in the MV)
"Though separated / Hearts cling on" - Zayne (The Foreseer) is separated from MC in many lifetimes. The memories of their love are tied to the jasmine flowers even if they forget.
[END SPOILERS]
"That's the price to pay / Yet lovers endure forevermore"
This is the verse that plays over Sylus' scene. What is his price? Does the following verse mean that he and MC must always endure something? Hardship? Misfortune?
When the chorus repeats a second time near the end, all of the above verses coincide with the intended love interest. It absolutely can be argued that all four love interests paid a price for their love, and not just Sylus. This whole tangent was brought up to follow with the whole "deal with the devil" aspect. As stated previously, I wouldn't be surprised if the devs and songwriters intended for the lyrics to have layers upon layers of meaning in relation to the stories.
Also take into consideration the lyrics from the song in Sylus' first official trailer, Tangible Shackles:
The outlaw again celebrates this encounter in fate It's time to break the seal they set in mind It's time they will have to pay the price
To me, though, in this song, the verse sounds very vengeful. It sounds almost vindictive, as if someone must be punished for whatever wrongdoing done against Sylus.
Watching the interview for Visions opposées, it seems the LADS team has shared enough of the intended stories for the songwriters to understand and pen the songs we hear. I trust that there will be complete clarity to the lyrics once we're able to understand Sylus' myth.
Love is the privilege of mortals
A gift the gods covet in vain
Astra, you ass, is that you
Now remember the first official trailer for Sylus? Yeah. Long-Awaited Revelry. Do you know what "revelry" mean? 'Cause I sure as heck didn't and kept wanting to read it as rivalry
revelry. noun. a situation in which people are drinking, dancing, singing, etc. at a party or in public, especially in a noisy way. — Cambridge Dictionary
To put it simply, "long-awaited party," which with the new knowledge of the timeline of scenes shown, we can clearly see a scene of MC entering a ballroom where Sylus is at in the trailer.

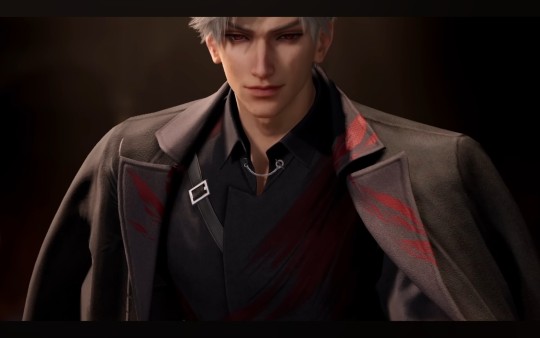
What type of party is this? Long-awaited? Maybe an engagement? In the MV, you can catch a brief glimpse of guests in the background watching MC enter. It seems almost like Sylus is waiting to show her off. The dance they share also seem intimate, and Sylus' expression is very soft and tender.
Previously, I alluded that it looks like MC and Sylus' wrist are bounded by a thread, similar to the Red Thread of Fate, but afterwards, I had my doubts, and if in keeping with the theme of being trapped, perhaps they were actually cuffed? I have previously mentioned that handcuffs have shown up often in the trailers.
To be cuffed together makes it seem like it wasn't a choice for one or both people. Kind of pondering if maybe MC might have sold her soul to Sylus, thus becoming bounded to him?

I have also made a lot of references to the myth of Hades and Persephone previously (still holding onto it with every fiber of my being tbqh), BUT for the sake of this third theory, let's revise the above scene to mean...
Sylus, a demonic creature, is trapped on the dark side while MC is a mortal on the light side (mortal realm). He knows their love can never be, so he forces whatever bond they made together to break, setting her free to remain in the mortal realm while he remains trapped in the Underworld.
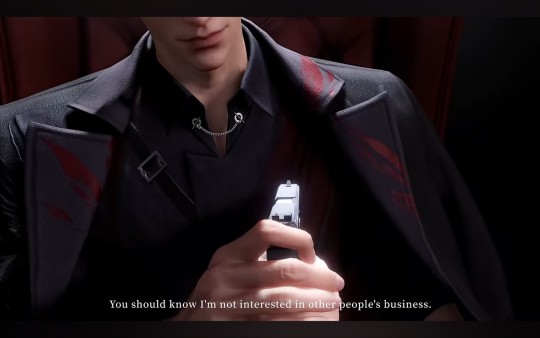

Interestingly, Sylus conjures up a gun, pressing it to his chest where his heart would be. And he makes MC shoot him. ....thus breaking their bond? Or killing him idk man
This appears to be the following appearance of him after he is shot in his chair:

I'm sorry if this seems out of left field and my mind works in a weird way, but.....the scene above kind of made me think of the Roman/Greek myth for Cupid/Eros and Psyche. Rather, I was thinking of the scene where after her jealous sisters manipulated her and planted seeds of doubts, Psyche betrays her husband's trust and broke her promise to not view his face and learn of his identity. She carries a dagger with the intention of killing him.
In the aforementioned myth, Psyche does journey into the Underworld during a final trial set forth by Cupid/Eros' mother, Venus/Aphrodite. Other than that, there might not be many other correlations I can make in regard to the scene depicted in Visions opposées.
Speaking of Cupid (Roman name, but aka Eros in Greek mythology), however, it's also worth noting that Cupid was described as a "demon of fornication" by some mythographers. Take this part with a grain of salt since this was due to adapting the Roman myth for Christian usage. I do, however, vaguely recalled in some Greek/Roman myths, Eros/Cupid was viewed as devious by the other gods due to him being able to make both mortals and the gods fall in love depending on his whims, be it out of mischievousness or malice.
So....Cupid....God of desire....erotic love.............that earlier incubus comment I made?? 😭 This part I am definitely pulling out of my ass. 💀 Let's just wrap this post up. 🫠
If we look at the myth from the angle that Sylus is a demon, then....
Theory 3: Sylus is a demon who has come across MC, and for whatever reason, she is desperate to make a deal with a demon, thus bounding herself to him. Perhaps over time, Sylus grows to adore her, but maybe MC betrays his trust, whether it be intentional or at the manipulation of others? Could he have tested her when he made her shoot him? Was he willing to die for her, even if it's at her hands?
Uhhhh.....yeah. This theory seems more far-fetched. 🫠 Well, thanks for your time! If any of the crumbs I've presented stirred any theories from you all, I'd love to hear it! Bye. 💕
#love and deepspace#love and deepspace sylus#lnds analysis#lnds ramblings#i have got to stop writing things after midnight#🗿#i still think there is a heavy borrowing of greek mythology#yes i was that child that went through a greek myth geek phase and devoured everything i could#i will do a follow up post after reading the myth to see how far off i was lol
41 notes
·
View notes
Text
Excerpt from this story from Inside Climate News:
Gov. Glenn Youngkin vetoed two bills for the development of small solar projects and energy storage that had won bipartisan votes and support from Dominion Energy, environmental groups and farm and forestry representatives.
The bills would have encouraged private homes and companies to initiate solar projects and bolstered the existing utility’s efforts to capture electricity from renewable sources for later use. Dominion said in April, in an application to purchase electricity from third-party suppliers, that enhanced solar production and its own plans to store electricity would result in billions of dollars of fuel savings through 2035.
Youngkin has described himself as an “all-of-the-above” energy supporter with plans to support fossil fuel sources as well as renewable technologies. Critics said the vetoes last week raise questions about his commitment to clean energy and illustrate his disdain for the state’s landmark decarbonization law, the Virginia Clean Economy Act (VCEA).
The Republican governor, enthusiastic about the development of data centers in the state, has in the past year supported a proposed natural gas peaker plant and renewable sources to encourage such development. But Youngkin rejected the current legislation over his concern that ratepayers for existing utilities, which are reliant on fossil fuel, would bear in part the cost of increased solar production, according to a statement released Tuesday.
“He does not support legislation that puts rate payers at risk,” Peter Finocchio, Youngkin’s press secretary, said in an email.
Regarding battery storage efforts, Youngkin said that he was relying on market forces. “Long-duration energy storage is an expensive technology and if utilities believed it to be the best technology to meet demand, they would actively be seeking permission to build them. We must be vigilant to limit cost increases to Virginia’s residents,” he said in a “veto explanation” released on a state website.
2 notes
·
View notes
Text
commissioned art with a premise I Hate: do you block the artist who after all is a third party just interested in the cash, or figure out who the unnamed payer is and just block them
3 notes
·
View notes
Text
Why You Need to Outsource Medical Billing Services to a Third-Party Medical Billing Company
In today's complex healthcare landscape, managing medical billing can be a daunting task for healthcare providers. From coding and claims submission to payment posting and denial management, the intricacies of medical billing can significantly impact a practice's revenue cycle. Outsource medical billing services to a third-party medical billing company can streamline operations, improve efficiency, and ultimately boost your bottom line.
Benefits of Outsourcing Medical Billing Services
Enhanced Efficiency: A dedicated medical billing company has the expertise and resources to streamline your billing processes. They can automate tasks, reduce errors, and accelerate claim processing, leading to faster payments.
Increased Revenue: By outsourcing, you can ensure accurate and timely claims submission, minimizing denials and maximizing reimbursement. A specialized billing company can identify and recover lost revenue, optimizing your revenue cycle.
Reduced Administrative Burden: Offloading medical billing tasks to a third-party company allows your staff to focus on patient care and other core competencies. This frees up valuable time and resources, improving overall productivity.
Compliance Adherence: Staying up-to-date with ever-changing healthcare regulations can be challenging. A reputable medical billing company has the knowledge and experience to ensure compliance with HIPAA, ICD-10, and other relevant regulations, mitigating legal and financial risks.
Improved Cash Flow: Timely claim processing and efficient payment collection can significantly improve your cash flow. A dedicated billing company can optimize your revenue cycle, ensuring you receive payments promptly.
Challenges of In-House Medical Billing
High Staffing Costs: Hiring and retaining qualified billing staff can be expensive, especially in competitive markets.
Complex Regulations: Keeping up with the ever-evolving healthcare regulations requires specialized knowledge and ongoing training, which can be a significant burden.
Time-Consuming Tasks: Manual data entry, claim submission, and follow-up can be time-consuming and prone to errors.
Limited Expertise: In-house staff may lack the specialized expertise to handle complex billing scenarios and appeals processes effectively.
Services Offered by a Medical Billing Company
Claims Submission: Accurate and timely submission of claims to payers.
Coding and Billing: Correct coding of medical services and procedures.
Payment Posting: Efficient posting of payments and adjustments.
Denial Management: Effective handling of denied claims, including appeals and resubmissions.
Follow-up on Claims: Timely follow-up on outstanding claims to expedite payment.
Financial Reporting: Detailed financial reports to track revenue and expenses.
Staffing Cost Savings
By outsourcing medical billing, you can significantly reduce staffing costs. You won't need to hire and train in-house billing staff, saving you money on salaries, benefits, and overhead expenses.
Overhead Cost Savings
Outsourcing can also help you save on overhead costs. You won't need to invest in billing software, hardware, and other infrastructure. Additionally, you can reduce office space requirements, further lowering your overhead expenses.
How Right Medical Billing LLC Can Save Your Money and Time
Right Medical Billing LLC is a leading medical billing company that can help you streamline your revenue cycle and improve your bottom line. Our experienced team of billing experts offers a comprehensive range of services, including:
Expert Billing Services: Our team stays up-to-date with the latest industry regulations and coding guidelines to ensure accurate and timely claims submission.
Advanced Technology: We leverage cutting-edge technology to automate tasks, reduce errors, and accelerate the billing process.
Dedicated Account Managers: You'll have a dedicated account manager to oversee your billing operations, ensuring smooth communication and timely resolution of issues.
Improved Cash Flow: Our efficient follow-up and denial management processes help you collect payments faster, improving your cash flow.
Reduced Administrative Burden: By outsourcing your medical billing, you can free up your staff to focus on patient care, leading to increased productivity and patient satisfaction.
Why Choose Right Medical Billing LLC?
By choosing Right Medical Billing LLC, you can:
Increase Revenue: Our expertise in coding, billing, and claims submission can help you maximize reimbursement.
Improve Efficiency: Our streamlined processes and advanced technology can significantly reduce turnaround time for claims.
Enhance Compliance: Our team ensures adherence to all relevant regulations, mitigating legal and financial risks.
Reduce Costs: Our cost-effective solutions can help you save money on staffing, technology, and overhead expenses.
Improve Patient Satisfaction: By freeing up your staff to focus on patient care, you can enhance patient satisfaction and loyalty.
In conclusion, outsourcing medical billing services to a reputable company like Right Medical Billing LLC can provide numerous benefits, including increased efficiency, improved revenue, reduced administrative burden, and enhanced compliance. By partnering with us, you can streamline your operations, improve your cash flow, and focus on what matters most: providing quality patient care.
2 notes
·
View notes
Note
I'm so glad to find another woman on this site who is happy that Kamala lost and that Trump's team won. My immediate family, my church, and even my county are very relieved, but I haven't seen much of that relief here. Unsurprisingly so, because I know how pro choice tumblr is, even compared to the US population. I know a lot of pro life activists have been saying that neither candidate was going to further the pro life movement, but Kamala's campaign was outright hostile to the pro life movement, whereas Trump at least has some pro lifers on his team. Trump also allows individual states to ban abortions, whereas Kamala would probably try to legalize it everywhere.
Yes, exactly. Neither side is perfect, but I wasn’t about to let perfect be the enemy of good when making my decision to vote. Trump has always said he wants to leave the abortion issue up to the states, and frankly, he’s the President who appointed some of the Supreme Court Justices responsible for overturning Roe in the first place. Since he won this election, there’s a very good chance he will have more SC picks that could tip the odds further in our favor in the future, too. As a pro-lifer, this was the most desirable outcome of the two, as there was a very real danger of President Harris signing federal abortion access into law if it was brought to her desk, trying to push through executive orders favoring abortion, making tax payers pay for abortions, appointing Justices who would be sympathetic to the pro-choice cause, and more. Trump has not tried and will not try to do any of those things. There was no way I could stomach voting third party or abstaining from voting with the crossroads we were at.
4 notes
·
View notes
Text
"Although DSM III considerably expanded the range of behaviors defined as markers of mental disorder, the manual never actually defined what exactly qualified these behaviors as mental disorders. The creation of a classification system in which symptoms signified and thus qualified as markers of a mental or emotional disorder now pathologized a wide range of behaviors. For example, “oppositional disorder” (coded 313.81) is defined “as a pattern of disobedient, negativistic, and provocative opposition to authority figures,” “histrionic personality disorder” (coded 301.50) occurs when individuals are “lively and dramatic and always drawing attention to themselves,” and “avoidant and personality disorder” (coded 301.82) is characterized by “hypersensitivity to potential rejection, humiliation, or shame and unwillingness to enter into relationships unless given unusually strong guarantees of uncritical accep-tance.” With the attempt to carefully codify and classify pathologies, the category of mental disorder became very loose and very wide, including behaviors or personality traits that merely fell outside the range of what psychologists postulated was “average.” Behaviors or personality features that might have been previously categorized as “having a bad temper” were now in need of care and management and were henceforth pathologized. Herb Kutchins and Stuart Kirksuggest that the codification of pathologies is related to the close connection between mental health treatment and insurance coverage. DSM III grew out of the need to make the relationship between diagnosis and treatment tighter so that insurance companies (or other payers) could process claims more efficiently. As Kutchins and Kirk put it, “DSM is the psychotherapist’s password for insurance reimbursement.” DSM—which provides the code numbers to be listed on the claims for insurance reimbursement—is the bridge connecting mental health professionals and such large money-giving institutions as Medicaid, Social Security Disability Income, benefit programs for veterans, and Medicare. Not only is it used by the majority of mental health clinicians, but it is increasingly used by third parties such as “state legislatures, regulatory agencies, courts, licensing boards, insurance companies, child welfare authorities, police, etc.” In addition, pharmaceutical industries have an interest in the expansion of mental pathologies that can then be treated with psychiatric medications. As Kutchin and Kirk eloquently put it, “For drug companies, . . . unlabeled masses are a vast untapped market, the virgin Alaskan oil fields of mental disorder.” Thus the DSM, willfully or not, helps label and chart new mental health consumer territories, which in turn help expand pharmaceutical companies. Hence the expansion of the category of mental illness, dysfunction, or emotional pathology is related to the professional and financial interests of mental health professionals and drug companies. It is also related to the increasing use of psychological categories to claim benefits, compensations, or extenuating circumstances in courts. In this process, the DSM has clearly considerably enlarged the scope of psychologists’ authority, who now legislate over such questions as how much anger may be appropriately expressed, how much sexual desire one should have, how much anxiety one should feel, and which emotional behaviors should be given the label of “mental disease.”" -Saving the modern soul: Therapy, emotions and the culture of self-help by Eva Illouz
17 notes
·
View notes
Text
Consulting firm McKinsey & Co has agreed to pay $78 million to resolve claims by U.S. health insurers and benefit plans that it fueled an epidemic of opioid addiction through its work for drug companies including OxyContin maker Purdue Pharma. The settlement was disclosed in papers filed on Friday in federal court in San Francisco. It marked the last in a series of settlements McKinsey has reached resolving lawsuits over the U.S. opioid epidemic. Plaintiffs accused McKinsey, one of the leading global consulting firms, of contributing to the deadly drug crisis by helping drug manufacturers including Purdue Pharma design deceptive marketing plans and boost sales of painkillers. McKinsey previously paid $641.5 million to resolve claims by state attorneys general and another $230 million to resolve claims by local governments. It has also settled cases by Native American tribes. Friday’s class action settlement, which requires a judge’s approval, resolves claims by so-called third-party payers like insurers that provide health and welfare benefits.
4 notes
·
View notes
Text
Dumbest Thing I've Ever Heard: 7/31/2023
Fifth Place: Erick Erickson
On 7/30/2023, Mr. Erickson tweeted the following:
Starting to see more and more progressives demand public swimming pools. Get ready for the next entitlement program.
Not public swimming pools! Anything but public swimming pools!
By the way, the top reply is somebody pointing out that the city Erickson lives in--has multiple public swimming pools:
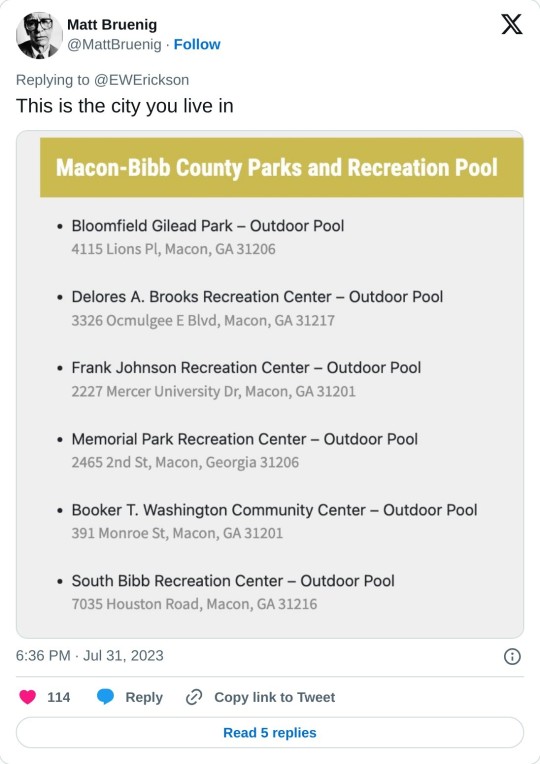
I'm sorry, I can't get over this: Erickson is seriously concerned that progressives are going to--what exactly? Use tax payer dollars to make the community better? That's really something you view as a concern? As one Twitter user put it:
i like that the worst thing this guy can imagine is americans collectively deciding to use the wealth they produce and the taxes they pay to give themselves something nice
Fourth Place: Stephen Strang
Right-wing watch posted a clip of him on Friday talking about allowing drag queens to read to children, he says "They would not let someone dressed up in a Nazi uniform go in and read stories to children."
First off, who exactly is the "they" in this case? Second off, there is obviously no comparison between the ideology of the most genocidal and murderous regime of the twentieth century and people dressing in drag, and the fact that you think these two things are on even remotely the same level shows there is something wrong with you.
Third Place: Donald Trump
NBC reached out to forty-four of Trump's former cabinet officials to see how many of them would support his 2024 run for re-election--only four did. Those four, for those curious, are Mark Meadows, Ric Grenell, Matthew Whitaker, and Russ Vought. A Tea Party holdover who played a key role in the Freedom Caucus until he was made Trump's Chief of Staff and who appeared in a debunked creationist propaganda film, a small time ambassador who once got into a fight with Nick Fuentes over if he was immoral for being a homosexual, a failed Congressional candidate turned Attorney General, and a man who is only known for hindering Biden's transition to the Presidency, respectively.
What I find funny though is not that this group of nitwits have endorsed Trump's re-election, but that they are the only ones who worked with Donald Trump to have done so. If so few of the people who were around Donald feel comfortable giving him a second term, what should that say to the rest of us?
Second Place: Jonathan Chait
What's wrong with this picture?

If you said the fact that it implies the corruption of a Supreme Court Justice is on the same level as the corruption of the son of the President despite one actually having the power to impact people's lives and the other not, you'd be correct. However, this false comparison is the entire basis of New York Magazine's article "The Sleaze Problem: How Democrats can clean up the Supreme Court and address the Hunter Biden affair." Why Democrats need to address the Hunter Biden affair--which is little more than trumped up charges against a private system--I'm not sure.
The column even sees its author admitting that nothing Hunter Biden did was illegal while also accepting the incorrect notion that nothing Clarence Thomas did was illegal.
The article proposes that Democrats should propose an ethics code for the Supreme Court while aiming for Republican support through also creating a stricter ethics code around the actions of family members of politicians. Of course, Chait admits this wouldn't actually work because doing so would indict the Trump kids even more than Hunter Biden--but on the bright side, at least the Democrats now have an answer for the irrational and nonsensical charges against Hunter Biden. If only Democrats would play into GOP talking points, that would show them.
Winner: Samuel Alito
Did you know that nothing in the Constitution gives Congress the power to regulate the Supreme Court? Well that's what Samuel Alito thinks--of course, it isn't actually true. Congress specifically has the power to stop courts from ruling on specific issues, to determine who is on the Supreme Court, and various other forms of regulation--but Alito doesn't want to mention that, because that could get in the way of his power grab.
Samuel Alito, you've said the dumbest thing I've ever heard.
2 notes
·
View notes
Text
TDS Return Filing Online: Everything You Must Know in 2025
Introduction
Navigating the world of TDS Return Filing Online can seem daunting, especially with the evolving tax regulations in 2025. This comprehensive guide will walk you through every aspect of the process, ensuring you stay compliant, avoid penalties, and make the most of digital filing. Whether you’re a business owner, a salaried individual, or a tax professional, this post will answer all your questions about TDS Return Filing Online.
What is TDS?
Tax Deducted at Source (TDS) is a mechanism by which the government collects tax at the source of income generation. When certain payments, such as salary, interest, rent, or professional fees, are made, the payer deducts a specified percentage as tax and remits it to the government on behalf of the payee. This ensures timely tax collection and reduces tax evasion.
Why is TDS Return Filing Online Important?
TDS Return Filing Online is not just a legal obligation but also a critical part of transparent financial management. Filing TDS returns online:
Ensures compliance with the Income Tax Act.
Helps avoid hefty penalties and interest.
Provides a digital record for future reference.
Enables quick processing of refunds and credits. It is mandatory for most deductors, including businesses and government entities.
Who Must File TDS Returns Online?
The following entities are required to file TDS returns online:
Companies and government deductors.
Individuals and HUFs (Hindu Undivided Families) are subject to tax audits
Businesses making specified payments (salary, rent, professional fees, etc.).
Anyone who has deducted TDS during a financial year.
Types of TDS Return Forms
Choosing the correct form is crucial for TDS Return Filing Online. The form depends on the nature of the payment and the deductee:
Form
Purpose
Form 24Q
TDS on salaries paid to resident employees
Form 26Q
TDS on payments other than salaries to resident Indians
Form 27Q
TDS on payments to non-resident Indians and foreign companies
Form 26QB
TDS on payment for the purchase of immovable property
Form 26QC
TDS on rent payments exceeding ₹50,000 per month
Form 27EQ
TCS (Tax Collected at Source) on specified goods and services
Documents Required for TDS Return Filing Online
Before you begin the TDS Return Filing Online process, gather the following documents:
TAN (Tax Deduction and Collection Account Number)
PAN details of the deductor and deductee
Details of TDS deducted and deposited (Challan details)
Nature and amount of payment
Valid Digital Signature Certificate (DSC) or Electronic Verification Code (EVC)
Correct TDS return form (24Q, 26Q, 27Q, etc.)
Bank details for refund (if applicable)
Step-by-Step Guide to TDS Return Filing Online
Filing your TDS return online is straightforward if you follow these steps:
Step 1: Register on the Income Tax Portal
Visit the official income tax e-filing portal.
Register using your TAN and other required details.
Step 2: Download the Return Preparation Utility (RPU)
Download the latest RPU from the TRACES portal or use approved third-party software.
Prepare your TDS return by entering all required details (deductor, deductee, challan, etc.).
Step 3: Validate the Return
Use the File Validation Utility (FVU) to check for errors.
The FVU will generate a .fvu file, which is the final version for submission.
Step 4: Upload the TDS Return
Log in to the e-filing portal with your TAN.
Go to the TDS section and select ‘Upload TDS’.
Attach the .fvu file and sign with DSC or EVC as required.
Step 5: Acknowledgement
After a successful upload, you will receive an acknowledgment receipt.
Save or print this for your records.
TDS Return Filing Due Dates for FY 2025-26
Timely TDS Return Filing Online is essential to avoid penalties. Here are the due dates for FY 2025-26:
Quarter
Period
TDS Return Due Date
Q1
1st April – 30th June 2025
31st July 2025
Q2
1st July – 30th September 2025
31st October 2025
Q3
1st October – 31st December 2025
31st January 2026
Q4
1st January – 31st March 2026
31st May 2026
Note: TDS must be deposited by the 7th of the following month for each deduction.
Penalties for Late or Incorrect TDS Return Filing Online
Failing to file your TDS return on time or submitting incorrect information can result in severe penalties:
Late Filing Fee (Section 234E): ₹200 per day until the return is filed, up to the amount of TDS.
Incorrect Filing Penalty (Section 271H): Ranges from ₹10,000 to ₹1,00,000 for non-filing or incorrect filing.
Interest on Late Payment: Additional interest may be charged for delayed TDS deposit.
Example: If your TDS amount is ₹5,000 and you delay filing by 30 days, the penalty is ₹200 x 30 = ₹6,000, but you will pay only ₹5,000 as the penalty cannot exceed the TDS amount.
Common Mistakes to Avoid in TDS Return Filing Online
Using the wrong TDS return form.
Entering incorrect PAN or TAN details.
Failing to validate the return with FVU.
Missing the due date for filing or payment.
Not verifying the return with DSC or EVC.
Ignoring error reports after validation.
Avoiding these mistakes ensures smooth TDS Return Filing Online and prevents unnecessary penalties.
FAQs on TDS Return Filing Online
Q1: Can I revise a TDS return after filing?
Yes. If you discover errors after filing, you can submit a revised TDS return with the correct details. You’ll need a consolidated file and a justification report for the revision.
Q2: Is it mandatory to file TDS returns online?
Yes, for all companies, government deductors, and those subject to tax audit. Others may file manually, but online filing is recommended for accuracy and convenience.
Q3: What happens if I miss the TDS return due date?
You will be liable for a late filing fee of ₹200 per day (up to the TDS amount) and may also face additional penalties for non-filing or incorrect filing.
Q4: Which form should I use for TDS on salary?
Use Form 24Q for TDS deducted from salaries paid to resident employees.
Conclusion
TDS Return Filing Online in 2025 is a streamlined, efficient process, provided you understand the requirements, deadlines, and penalties. By following the correct steps, using the right forms, and staying updated with the latest regulations, you can ensure full compliance and avoid costly mistakes. Make sure to file your TDS returns on time, validate your data, and keep all acknowledgments for future reference. For hassle-free compliance, consider using professional services or trusted online platforms.
Stay proactive, stay compliant, and make TDS Return Filing Online a seamless part of your financial routine in 2025!
0 notes
Text
Why Your Practice Requires an Expert Infusion Billing Company
The infusion therapy market keeps expanding at a rapid rate due to the management of chronic illnesses, oncology, and diabetes. The complexity regarding infusion billing also increases with this rapid expansion. Now, infusion billing companies have become an absolute necessity at the moment. The global infusion billing market has already exceeded USD 9 billion in 2023 and is predicted to reach a volume of USD 17 billion by the next 5 years (i.e., 2030) with an 8.4% CAGR. In the meantime, the global market for infusion management software should exceed USD 35 billion by 2033 because of the use of smart, connected pumps and digital tools.
The rapid and large-scale expansion represents the need for fully integrated infusion billing programs that would be capable of maintaining fine timing, code hierarchy, prior authorizations, denial management, and special payer-driven compliance.
Market momentum and innovation trends
Connected infusion pumps and IOT: EMR integration along with smart pumps with barcode scanning, IOT connectivity has reduced drug errors by up to 44% and increased coding accuracy.
Emerging tech boosting RCM accuracy: AI-based applications and live dashboards have helped cut the standard errors and denials in billing and allowed accelerating reimbursements, respectively.

The main industry trends in infusion billing
Cloud and Automation
The world is moving towards an immense shift towards cloud-based programs and automation. These systems offer security, central access to data, and real-time updates. They also provide some AI-powered functions such as coding, denial tracking, and claim follow-up- minimizing mistakes and improving efficiency.
Artificial Intelligence and analytics
Infusion billing AI-powered technology has eliminated close to 35% of denials and cut down processing time by half. Predictive analytics predetermine the actions of the payer and make it possible to correct and streamline the revenue cycle.
Regulatory and value-based models
With the ever-growing and ever-complex regulatory intricacy, healthcare is leaning more towards expert infusion billing outsourcing to ensure compliance. The shift towards value-based care also requires more nuanced and complex workflows, entailing specialized vendor expertise.
Recovery of post covid backlog
Following the backlog of claims that were caused by the pandemic, infusion billing organizations contributed so much to the aged claims. The resuming of elective procedures is one of the factors that led to the surge in demand for outsourced billing services.
Patient Engagement
Patient portals have become part of the newest infusion billing solutions for better billing visibility and payments. This helps improve accuracy and enhance patient satisfaction.
Benefits vs. Challenges
Advantages of Outsourcing
Almost 30-40% of operational expenses are being reduced with the help of outsourcing.
Most (approx. 80%) medical bills contain errors, and with the aid of outsourcing, the risk of any errors is majorly cut down, and the risk is thus minimized.
By outsourcing the infusion billing, the claims are handled in a swifter manner. Often, the claims that took months to process are completed within weeks by outsourcing.
Challenges and Restraints
One of the major concerns is data security. Statistics state that almost 80% of healthcare breaches happen by a third party.
Vendor transparency is sometimes lacking, as many providers have reported hidden errors and a lack of visibility in outsourced models.
The costs can be pretty variable, and the fees often range from 3-10% of collections for outsourced partners.
Future Forecast
The innovations in the world of infusion billing will continue through AI, cloud, and strict data governance. In the near future, integration with EHR and real-time analytics will become the basic expectations for infusion billing providers.
The landscape of infusion billing companies is now richer than ever. It is only going to become more competitive as time goes by. Your practice will only thrive when you select the vendors diligently and follow up with the vendor after the selection and in line with the trends of digital transformation. As we continue moving through 2025, we witness that the best infusion billing solutions will lead to the charge.
0 notes
Text
See Vaccine Recommendations Backed by Science in These Handy Charts
We are in the era of DIY public health, since the government will no longer do it. Jen Christiansen, Meghan Bartels via Scientific American. However, it’s not that easy to simply do what’s wise in this sphere. Medicare, Medicaid and other third-party payers use the brain dead official vaccine recommendations coming from Trump’s clown RFK as a basis for deciding which vaccinations will be paid…
0 notes
Text
There's supposedly over 161 million registered voters in the U.S., in 2024 (it was 168 million in 2020, apparently about 7 million people died or got taken off the registration, which might be voter suppression) a total of about 141 million votes have been counted for both Harris and Trump so far.
And there's millions more citizens who are eligible to vote but have never been registered.
Trump won the popular vote by about 5 million this time, but there's still about 20 million people on the voter rolls who evidently aren't part of the Democrat+Republican totals. Those 20 million (and, votes are still being counted, so the final total might be less, though I did round the Trump total up to 73 million and the Harris total up to 68 million, for my convenience) either didn't vote (at least for the presidency) or voted third party.
Since the electoral college is what decides who the president is, though, it does depend on where those 20 million live. And I'm doing this on my phone, and don't have the time or energy to do that statistical breakdown for every single state, how many registered voters per state vs. how many people did or didn't vote in that state.
Harris got about as many votes as Clinton in 2016, maybe a few million more, Trump got about as many votes as he got in 2020, if a little less.
A lot of the swing states that went for Trump, did have Abortion initiatives and other progressive initiatives on the ballot, many of which passed, and a few of them supposedly had local elections that went blue, even when the counties themselves still went for Trump, or the district voted for a republican for a congressional seat.
And, like, that's odd, honestly. Like, a possible explanation is that, progressive voters turned up, voted for a democratic mayor or state senator or governor or abortion rights or whatever, then left all the federal selections blank. Because while state legislatures and governors can't actually do a lot about foreign policy, they can, in fact, do things to people in their states and cities.
But for that to be true it would require a big difference between the vote totals for Trump+Harris in those states and the vote totals for those down-ballot races, and. There doesn't seem to be, at first glance? It seems like otherwise democratic voters, or voters who voted for progressive ballot initiatives. Voted for Trump anyway. And 20 million registered voters just didn't turn up.
And, to be cynical for a moment? It isn't like the Israel/Palestine conflict started on October 7th. Palestinians have suffered wrongdoing by the government of Israel since the modern state of Israel's founding, and Israel has had better weaponry and American support for a very long time and they've definitely dropped bombs before. And they've also had the illegal settlements in the West Bank for years.
And all of that was also already true in 2020, and Biden supported Israel back then too. His political stance on Israel didn't change between then and now. Biden already said he would never support Medicare for all, or single-payer healthcare, everyone knew he was moderate/conservative, right-wing, on a lot of issues. Biden in 2020 had some support from some "never Trump" Republicans who endorsed him as well.
And Biden could be associated with Obama and Obama's handlings of the wars in Iraq and Afghanistan, as Obama's VP. And the U.S. armed forces who actually answered to Obama were the ones doing war crimes and drone and missile strikes for that.
But it seems like Biden was able to get away with it and get 10 million more people to vote for him, very possibly, because he was a white guy. The same complaints had a harder time. Sticking.
Its not like nobody had complaints about the Biden campaign's mismanagement. His history of gaffes, the time he was in a basement and nobody saw him for weeks.
Then again, maybe Biden just got lucky that Covid happened, and Trump clearly and obviously mismanaged it. And Harris, in turn, got associated with the slow economic recovery from Covid, lead by the Biden Admin, and with all the wars in Ukraine and Israel/Palestine that Biden evidently didn't do well enough resolving.
Wars that, again, had already been happening, going back to when Putin's Russia annexed Crimea back in 2014, and, again, the very long history of the Israel-Palestine conflict. But I guess people don't care as much when it isn't in their news feeds or their social media timelines.
...Honestly. The thing that gets me about the popular vote totals is that. Trump went from 63 million in 2016, to over 74 million in 2020, and he's still at almost 73 million now.
So, yeah, there's 20 million people who didn't vote this year, aside from the millions who aren't registered, but. 10 million more people voted for him than voted for him the first time he won.
And. That's a lot scarier to me, in all honesty.
"I don't want to see anyone blaming abstaining voters for this!"
Of course you don't. The entire idea of abstaining was that you could pretend this didn't involve you. Not getting blamed was more important to you than doing any kind of damage control, more important than protecting any of the people you said you wanted to protect. And in this moment, I don't really care what you want. Of course, this isn't entirely your fault. Of course other people made this worse. But if you're going to pretend you had nothing to do with this, forgive me if I ignore you.
9K notes
·
View notes
Text
6 Ways to Optimize Billing Efficiency in Anesthesia

Anesthesia practices face unique challenges in billing and coding due to the complex nature of services, time-based reporting, and ever-changing compliance standards. To stay profitable and efficient, these practices must focus on optimizing their billing processes. This guide outlines key strategies to help anesthesia groups streamline operations, maximize reimbursements, and maintain compliance using effective medical billing services and revenue cycle management techniques.
1. Understand the Nuances of Anesthesia Billing
Unlike most specialties, anesthesia billing is time-based and requires accurate documentation of start and end times, modifiers, and ASA (American Society of Anesthesiologists) physical status codes. Anesthesia providers must also consider concurrency and medical direction rules. Failing to capture these details can lead to claim denials or underpayments. Utilizing medical billing services for anesthesia that specialize in these nuances can help practices avoid costly errors.
2. Leverage Technology for Efficient Revenue Cycle Management
Investing in robust billing software designed specifically for anesthesia can significantly enhance revenue cycle management. These platforms automate claim submission, verify insurance eligibility, track denials, and generate real-time reports. By streamlining the entire billing process, practices can reduce administrative burdens and focus more on patient care while improving cash flow.
3. Outsource to Specialized Medical Billing Services
Many anesthesia groups benefit from partnering with third-party medical billing services that understand the intricacies of their field. These services often offer dedicated teams for coding, billing, and compliance management, which ensures accurate and timely claim processing. Outsourcing also reduces overhead costs and allows staff to concentrate on clinical duties, which is key to optimize medical billing for anesthesia practices.
4. Focus on Accurate Coding and Documentation
Accurate documentation and coding are the foundation of any successful billing process. Anesthesia-specific CPT codes, modifiers (e.g., QX, QK, QY, QZ), and ASA crosswalks must be applied correctly. Regular training for coders and providers ensures that coding reflects the services rendered. Medical billing services for anesthesia often include certified coders who stay updated on regulatory changes, which reduces compliance risks and denials.
5. Monitor Key Performance Indicators (KPIs)
To optimize medical billing for anesthesia practices, it is essential to track KPIs such as denial rates, days in A/R (accounts receivable), claim submission lag time, and collection rates. Regular KPI analysis helps identify bottlenecks and implement targeted improvements. Advanced revenue cycle management systems can automatically generate KPI dashboards, providing actionable insights to decision-makers.
6. Stay Compliant with Evolving Regulations
Regulatory changes in healthcare, such as updates in Medicare policies, ICD-10 codes, and HIPAA requirements, can significantly impact billing practices. Anesthesia providers must ensure compliance to avoid audits, fines, or claim rejections. Partnering with knowledgeable medical billing services for anesthesia helps ensure compliance with federal and payer-specific guidelines.
To thrive in a competitive healthcare landscape, anesthesia practices must implement efficient billing strategies that reduce errors, enhance compliance, and improve collections. Whether through in-house improvements or outsourcing to expert medical billing services, the key to success lies in mastering revenue cycle management and adapting to the unique demands of the specialty. By doing so, practices can truly optimize medical billing for anesthesia practices and achieve long-term financial health.
0 notes