#they said translation in 2025 but you know the track record
Explore tagged Tumblr posts
Text
dandelion is indeed the worst but if he’s not present in the next book i would legitimately be sorrowful as the whole thing will become a slog . you basically cannot have the “short stories” era-of-the-timeline iteration of geralt without dandelion, it would be like eating unbuttered bread.
though it’s not like season of storms did them dirty, i wasn’t disappointed with it (… with regards to them), but since it’s literally been over 20 years since the saga was finished i’m trying to prepare for any potential reality
#however i will accept an absence of dandelion IN THE CASE OF we get to see geralt and yennefer living together in vengerberg#but if it’s regular geralt day in the life then if dandelion’s not there it’s gonna suuuuuccckk#i mean as in geralt’s life sucks without him. badly#and it also? sucks with him. good-ly.#it’s august and we don’t have a title yetttt 🥲 and they said 2024 … hmhm sure#i just feel like rupaul ‘and don’t fuck it up’.gif#like i’m excited but also wtf? new witcher book? are we on punk’d?#it’s not going to be the best but i’m hoping it will be at least as good as season of storms. not a high bar ok!#this from the person who was optimistic about the n*tflix show. don’t trust me i like to believe in the future#i was going to say ‘and i trust sapkowski more than i trust n*tflix’ and then i laughed.#i don’t trust him—i don’t even trust the version of him from the 90s and 00s!#one side of me can’t believe i’m still here after the guardswomen of kerack. and the ‘well i’m only gay for clout’ villain motivations#the other side of me is intensely curious wtf geralt will get up to this time and how witcher could maybe even denigrate further#but season of storms ending was actually good and = well it’s not like sapkowski forgot what it was about#then again it’s been 10 years and a bad adaptation since then so im biting my nails#all i ask : please stick with the naming convention of the other books. i don’t want to write an absurdly long or short name or acronym out#sooooo weird that in a few months i will be saying: there are 9 witcher books.#actually rn i just say there’s 7 and discount season of storms as a legitimate heir but mention it as footnote lol#i just hope i can survive until this new book and until its translation LOLLLL#they said translation in 2025 but you know the track record#new book: *releases winter 2024* | english translation: coming 2045!#jk i think they finally figured out that witcher is a money printer so they will be eager to translate it now and not waffle around#they kicked their butts into gear with the hussite trilogy so ! and they made new hardcovers.#the elbow-high diaries#new book 2024
24 notes
·
View notes
Note
I have seen your tweets about the spin off. You seem really positive that Melissa is coming back, but I'm so confused by it? Why do you feel so hopeful? I don't want to get my hopes up and be heartbroken all over again.
I wouldn't say I'm "hopeful" I just think for me looking at all the evidence it seems very likely. Other people think differently and that's absolutely okay for them. But if you want to know WHY I think the evidence is in favour, I shall detail it so you can make up your own mind.
So, yesterday Angela Kang commented this
And she's right, when she said "we've all" she meant it. Most of the people involved in the show have said Melissa will be back, though most have not specified the show.
Gimples quote is the one most alluding to non-Caryl stuff:
However, the others are more about Caryl together:
(THIS IS A LONG IMAGE HEAVY POST WITH LOTS OF INFO!)

Nicotero hinted very strongly at Carol going after Daryl:

And then of course there's Norman. He has literally staked his reputation (such as it is) on them reuniting and promised until he's blue in the face that is happening.
Of course he could be lying, however how would that serve him? It would make him more obviously a liar, make those who do still trust him lose that trust and just anger his already thinning fanbase.
And most importantly, Melissa herself said she would be back:

This was only the first step of evidence that has been ever evolving since. The main one of course being Joao on YouTube. The Brazilian youtuber has a very solid track record of spoilers - he had several call sheets from season 11. I can't find the translation of his video, but Hanna summed it up here: https://mcbride.tumblr.com/post/702367502037057536/daryl-spinoff-carol-rumorsspoilers The gist being that Melissa would return to the spin-off either at the end of s1 or start of s2, and that season 2 would have her as a main character, and s2 would start filming back to back with s1 in March 2023.
Many didn't believe Joao, however over time all he's said is proving true.
The showrunner's WGA page shows he is showrunning 2 seasons and employed at least until 2025:

And now, Duane Manwiller has confirmed that yes they are filming the seasons back to back:
And the info we have fits with Joao saying the season 2 filming starts in March.
Early casting calls for returning characters had them listed until Feb:
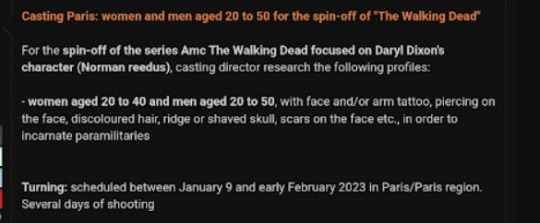

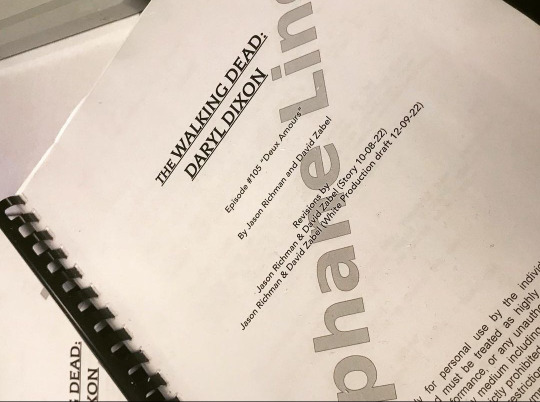
That seems to indicate one story ending in Feb and another starting in March. We know they are still filming s1 in February from this:
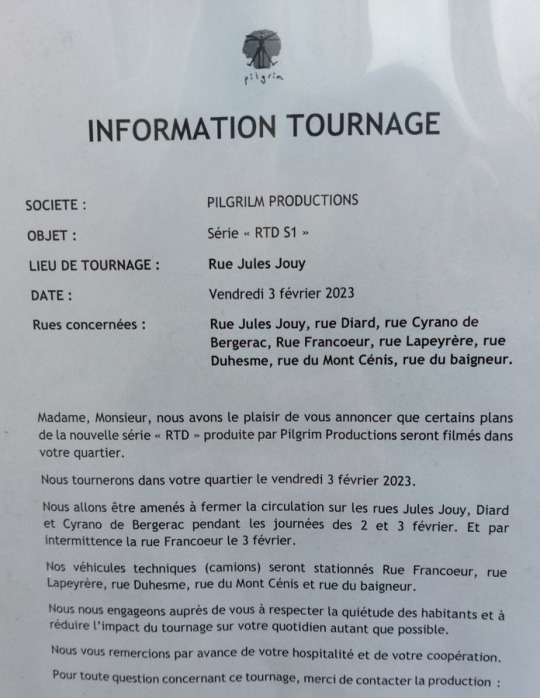
And it looks like they are reaching the end of the season by mid-Feb as those casting calls suggested, given episode 5 appeared to start filming on 20 Jan:
We also now have casting calls for March, and a filming location for 4 week. Given eps are normally filmed over 2 weeks (or so) that does scream of a s1 cliffhanger and s2 resolution:

So given ALL the information that Joao gave in his video about the timing and season 2 has now been proven correct, stands to reason it makes it MUCH more likely the connected information - that Melissa is returning - is also correct.
Now in terms of the negatives, or questions I have seen people posting which make them think it can't be true, here's my answers.
If Melissa can come to France to film now, why couldn't she before?
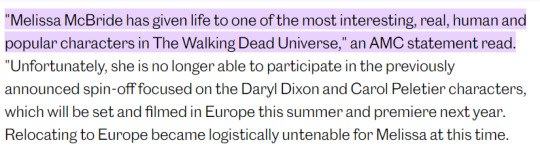
Two key phrases to note here - 1) "at this time" 2) "filmed in Europe this summer". Filming was delayed by at least 4 months, and while Melissa may not have been able to travel to Europe then, she very well could be NOW. It very much appears from this statement - which she would have approved - that it was a timing/logistics issue.
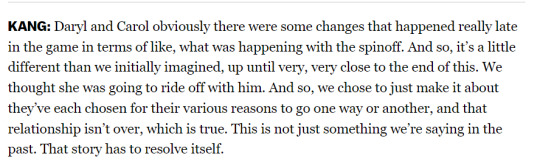
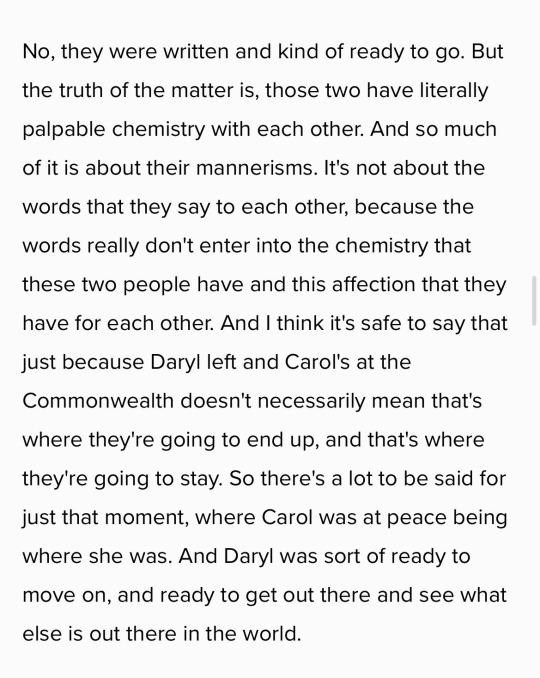
This seems backed up by this phrasing from Kang, which also agrees with Joao's statement that it was always the plan to get her back:

"Were", past tense.
Also, it's entirely possible that neither she, nor the production will be STAYING in France.
Early on in production, a crew member's partner said they'd be in France until March/April:

(Source: DearTvShow)
If they are just filming season 1 final mid-Feb, it seems highly unlikely they are going to complete a second season by April. Thus, it seems likely they are only filming a couple of episodes of s2 in France.
It's very possible then that Melissa can do s2 because it WON'T be filmed entirely in France.
2) If Melissa is returning why haven't AMC announced it?
Well, that is a question, and obviously I don't know the answer. Yes, I agree it would make more sense if they did. BUT I can see logical reasons why they might not:
they might be gun shy in announcing anything until Melissa's filming is in the can, after what previously happened
they might not want to overshadow Norman's "epic" solo first season
they might think that a surprise appearance by Carol is a bigger impact
And they have precedence for this, when Morgan returned in season 5, it was kept totally secret and Lennie James went to great lengths to remain hidden - traveling under a false name, staying in a different town etc: https://youtu.be/UParJyrTqIg
3) If Melissa is returning, why haven't we seen her filming yet?
Have you met Melissa? LOL We know Melissa has ALWAYS been the queen ninja of filming. Even location shooting like the beach from 10x01, where fans ONLY saw Norman and Lauren Ridloff interacting and never saw Melissa.
But also, she wouldn't have been filming until this week anyway, as it seems likely they just NOW are getting to the s1 finale. And whose to say she isn't on set now, filming, hidden away and using a pseudonym?

40 notes
·
View notes
Link
Even before the coronavirus pandemic, telemedicine was gaining popularity. In 2018 and 2019, online searches for telemedicine increased nearly 25 percent. Healthcare organizations had already turned to telemedicine to deliver care and increase accessibility. In a March 2020 survey, 41 percent of healthcare providers said that they were using telemedicine technology, an increase from 22 percent in 2018. When the coronavirus pandemic hit, healthcare providers and patients alike looked to telemedicine to minimize the spread of disease while still providing and obtaining care. For instance, before COVID-19, only 8 percent of consumers in Massachusetts were using telemedicine; afterward, usage surged to 21 percent.

Telemedicine isn’t new. For years, registered nurses (RNs) have answered patients’ questions by phone, either from a doctor’s office or on an RN hotline. Say you call your doctor’s office to tell them that you’ve been getting headaches since you started your new medication. When the RN or doctor calls you back and tells you to take a smaller dose, that’s telemedicine. But with today’s advances in technology, telemedicine can be done online, and it encompasses more than just phone calls or video conferencing. It can include monitoring patients remotely through connected devices as well as conducting virtual visits. These visits can cover anything from triage to determine if you need to be seen by a doctor to counseling. This guide will discuss what telemedicine is, as well as the terms related to telemedicine, how to start offering telemedicine services, how to evaluate telemedicine tools, and how telemedicine can be a safer option for medical care during a pandemic.
Just so you know You’ve got your medical toolkit ready to help those in need — but what about your telemedicine toolkit? With JotForm’s HIPAA-compliant telehealth platform, you can easily create online medical forms that keep sensitive health data safe.
What does telemedicine include?
Telemedicine first came on the radar in 1879, when an article in the Lancet discussed using the telephone to reduce office visits. In 1925, Science and Invention magazine suggested that radio could be a way to diagnose patients. And we’ve all likely called the doctor’s office to discuss symptoms and find out if we should come in or just take some aspirin and ride it out. While telemedicine and related services were first created to help people who don’t have ready access to medical services, a study found that low-income and rural patients are the least likely to use it, possibly because they lack access to providers that use telemedicine. However, usage is increasing rapidly among physicians and patients thanks to the availability of smartphones with video conferencing capabilities.
Telemedicine is booming
The market for telemedicine services is expected to more than double by 2025, up to $55.6 billion from $25.4 billion in 2020. But given the explosion in demand due to the coronavirus pandemic, with some telemedicine companies seeing a 50 percent increase in visit volumes, that could be a low figure. Prior to the coronavirus, many providers hadn’t yet embraced telemedicine because Medicaid and private insurers restricted reimbursement. However, most have since increased coverage, with the Centers for Medicare and Medicaid Services (CMS) leading the charge to reimburse providers and restrict the spread of the coronavirus. This increased acceptance by insurance providers may boost the number of providers offering telemedicine, even after the pandemic passes. A staggering 90 percent of the $3.5 trillion spent annually on healthcare in the U.S. is to care for people with chronic conditions. Telemedicine can reduce those costs while still providing patients with the care they need.
Online intake forms
With the rise in telemedicine visits, online intake is essential. Some medical practices are already using online intake forms and asking new patients to fill them out before a visit. These forms give telemedicine providers information that’s crucial to treating patients.

In addition to online intake forms, telemedicine patients can use forms to self-report data, like side effects, symptoms, and blood pressure readings. It’s vital for healthcare providers to keep this data safe in order to comply with the Health Insurance Portability and Accountability Act (HIPAA). A total of 81 percent of Americans own a smartphone, more than those who own a desktop or laptop computer, at less than 75 percent. Because many patients will likely use smartphones to fill out these forms, they need to be mobile-friendly.
Online consultation and telemedicine
How an online consultation is conducted may vary by provider. For example, some doctors may use a video conferencing platform specifically designed for telemedicine, like Doxy.me. Others may be part of a larger telehealth network like MDLive. Telemedicine also includes remote monitoring of patients, such as through Bluetooth-connected devices. For instance, a patient with diabetes could be sent home with a blood glucose monitor that automatically uploads readings and sends alerts to their physician if the readings are abnormal. Other types of telemedicine include transmitting imaging, like radiology images, to radiologists for review, as well as consulting with a specialist via video conference in the referring physician’s office. It can also include telepsychiatry, or visits with a mental health professional, through video calls.
Telehealth
Mobile apps that educate patients about their health are types of telehealth, a broader category that includes telemedicine. For example, a consumer app like MyFitnessPal, where users log their food intake and weight and get information on the calories and macros of their meals, is one type of telehealth app. Online educational courses, for both medical professionals and patients, are another example of telehealth. An RN might take an online course to keep up with their continuing education, or a patient could take an online class in diabetes management.
Telemedicine pros and cons
There are advantages and disadvantages to using telemedicine. Not only does it reduce costs for healthcare providers and patients, it also makes healthcare more accessible and convenient, particularly to those living in rural areas. Patients have access to more specialists as well. It’s easier for a patient with a thyroid condition, for instance, to see an endocrinologist who can monitor their medication. Patients can also be more engaged in their care. For example, a patient who uses a remote monitoring device for their blood glucose might also have an app on their smartphone that lets them see the trends in their blood glucose levels and how those levels change when they do things like going for a walk or eating. However, telemedicine does have its downsides. When you’re using a platform from an on-demand telemedicine service that matches you with a random physician, you’re not getting care continuity. This doctor may not be able to treat you as effectively because they don’t have your full record. Additionally, reimbursement for providers may be an issue if insurance companies and the CMS decide to go back to the old models for reimbursement. There may also be a technology challenge for providers and patients as they learn to use HIPAA-compliant video conferencing platforms or figure out how to submit their copays. Telemedicine, however, is still cost-effective, and during a global pandemic, a safe way to provide care for patients.
Telemedicine and other related terms
When people discuss telemedicine, they might also use the term “telehealth.” These terms are often used interchangeably, but they have subtly different meanings. “Telemedicine” refers specifically to clinical services, like online doctor visits in real time, while “telehealth” includes clinical services but also refers to things like online continuing education and mobile apps that patients can use to track their health. Telemedicine is a subset of telehealth. The following are the most common terms and services related to telemedicine.
Telenursing
One type of telemedicine that you might already be familiar with is telenursing. This has actually been around for decades, and you’ve probably used it many times. Telenursing is when you call either your doctor’s office or a hotline staffed with registered nurses (RNs) to get information about your symptoms. For example, you might wake up one morning with a stuffy nose and cough. Before you head to the doctor’s office, you could call and speak to a nurse, who would ask about your symptoms and decide if you need to come in, or if you could take some cold medicine and wait it out. Telenursing is just one subset of telemedicine, however. A lot of different specialties translate well to video and other remote technology, including psychiatry, radiology, and even dermatology, among others.
Telepsychiatry
Perhaps the best fit for telemedicine is telepsychiatry. The basic definition of telepsychiatry is a visit with a psychiatrist or psychiatric nurse over the telephone or via video conference to conduct a session, most likely for medication management.

In many cases, telepsychiatry makes mental health care more accessible to patients, particularly those whose conditions make it difficult to travel for appointments. It also allows providers to serve patients in areas where there aren’t mental health professionals nearby; over half of the counties in the U.S. don’t have a psychiatrist, for example. There are several guidelines that can help make telepsychiatry successful. But telepsychiatry does have its downsides. Often, mental health professionals use nonverbal cues and body language to help treat a patient, and that can’t easily be seen through a video conference. Some patients may not be good candidates for telepsychiatry because they have difficulty complying with their existing treatment plans or tend to engage in drug-seeking behaviors. For example, a patient with a substance abuse problem may not be forthright about their use of an existing prescription for anxiety. Additionally, the Ryan Haight Online Consumer Protection Act of 2008 prevents providers from prescribing controlled substances through telemedicine visits. For example, patients with Attention Deficit Hyperactivity Disorder (ADHD), who are typically treated with controlled substances, would need an initial in-person visit.
Teletherapy
Telepsychiatry also extends to real-time virtual appointments with licensed social workers, psychologists, marriage and family therapists, speech and language therapists, and other health professionals. This is known as teletherapy. This subset of telemedicine lends itself particularly well to virtual visits. While the therapist may not be able to pick up on all body language cues, they can pick up on facial expressions and voice variances as the patient works with them. This can help therapists provide better treatment while allowing both the patient and the therapist more flexibility.
Teleradiology
As Baby Boomers age, there may be an increase in the need for radiologists to diagnose and treat conditions like Alzheimer’s. As it stands now, employment is expected to grow by 9 percent from 2018 to 2028. By using teleradiology, which transmits images electronically for radiologists to review remotely, more of these MRIs and x-rays can be read in less time. And radiologists can review the transmitted images and provide their interpretation of the results to the physician that ordered them electronically as well.
Teledermatology
The demand for physicians and surgeons, including dermatologists, is expected to grow by 7 percent from 2018 to 2028, according to the Bureau of Labor Statistics. Teledermatology makes it easier for dermatologists to treat patients, particularly those who live far from the nearest provider. One use for teledermatology includes triaging conditions. For example, you might describe a strange-looking patch of skin to your dermatologist and show it to them over a video conference, and they could ask you questions about how it’s responding to treatment with over-the-counter medications. If that isn’t working, they might want you to see a doctor in person to find out if you need a prescription. Teledermatology can also be used to treat chronic conditions, particularly those that require multiple appointments per week. A patient with severe psoriasis could video conference with their provider and describe how the cream is working, as well as discuss more aggressive treatment options like oral medication.
Telepathology
Radiologists aren’t the only medical professionals who can read lab results remotely. Increasingly, pathologists are viewing slides using remotely operated microscopes or high-quality static images to diagnose diseases. For example, a healthcare professional could load a tissue sample into a robotic, remote-controlled microscope. The pathologist could remotely zoom in and pan to view the tissue sample for abnormalities, then discuss the findings with the referring physician.
Telerehabilitation
Closely tied to teletherapy, telerehabilitation lets healthcare professionals like occupational therapists and physical therapists deliver care remotely. Sometimes this is done using connected devices to assess the patient’s movement and provide cues. Other times, therapists use telerehabilitation to assess how well the patient is adapting to their environment, particularly after a medical incident like a stroke. A big benefit of telerehabilitation is that these patients are often constrained in how far they can travel. Telemedicine visits allow therapists to customize patients’ care plans and monitor their progress without requiring them to come in for frequent visits. Not all telemedicine services are delivered in real time, like teleradiology and telepathology, but the majority are. This makes it easier for patients to get care and for healthcare professionals to deliver services, not only directly to patients but also in consultation with other providers. Knowing the terms related to telemedicine can help both providers and patients navigate the types of services offered.
Telemedicine and HIPAA
Complying with the Health Insurance Portability and Accountability Act (HIPAA) is a must for medical institutions. The fines for not being HIPAA-compliant are hefty. Accidental violations cost $100–$50,000 per incident, with a yearly maximum of $25,000. And if you willfully break the rules, you could be hit with a penalty of up to $1.5 million. Since HIPAA was first enacted in 1996, the Office for Civil Rights (OCR) at the U.S. Department of Health and Human Services (HHS) has received over 231,968 reports of potential violations. Many of the cases just required corrective action, but in 75 cases it investigated, gross violations occurred. The total dollar amount for those fines was over $116 million dollars. The OCR can and has referred cases to the Department of Justice (DOJ) for criminal prosecution.

Since telemedicine practices are technically medical practices, HIPAA compliance applies to them, too. While the OCR has temporarily relaxed enforcement for telemedicine in response to the coronavirus pandemic, sensitive patient information must still be protected.
Basic HIPAA compliance, even during the pandemic
Relaxed enforcement doesn’t mean that the OCR won’t go after medical practices that aren’t careful. They’ve opened up consumer-grade video conferencing services to healthcare providers, like FaceTime, Facebook Messenger, and Skype. However, you’re still required to let patients know about potential privacy risks from these services. Additionally, you still need to follow basic HIPAA guidelines, such as with information sharing. HIPAA allows you to share protected health information (PHI) without authorization in certain circumstances. For example, if a patient has signed a waiver, you can share PHI with family members or caregivers. But you still can’t share PHI with employers. There are also several circumstances when you can share PHI without authorization and still be HIPAA-compliant:
If it will help treat your patient. For example, if you consult with another physician who may be able to provide guidance, that’s allowed under HIPAA.
With public health authorities like the Centers for Disease Control (CDC) or a state or local health department during a public health emergency. For example, if you share information about a patient who has recovered from COVID-19 with the city’s health department, that’s allowed.
To confirm the health status of a publicly identifiable figure, like a politician. If a reporter is asking whether Mayor Smith has contracted the coronavirus, you can answer yes or no. You’ll obviously want to be cautious about sharing any other information.
Protecting patient information
Even in a pandemic, healthcare organizations need to protect PHI. While fines for HIPAA violations may not be imposed, patients trust you to keep their data safe at all times. The importance of basic information security protocols at this time cannot be overstated. For example, some consumer-grade applications used for video conferencing, like Facebook Messenger, are not encrypted by default. If you’re going to use a consumer service like this, you need to make sure messages are encrypted and that you can turn on this feature. You need to vet any technology you may use, which we’ll cover in the next chapter. For example, if you start storing patient data in a cloud storage service, you need to know what type of encryption that service uses.
Securing personal devices
Your smartphone, tablet, or laptop also needs to be secured, particularly if you’re using a personal device. Ideally, you’ll already have a device policy in place, including a Bring Your Own Device (BYOD) policy for personal devices. If you don’t, make sure you have some basic measures in place to protect your patient’s data if you’re accessing it from one of these devices. For example, installing a program that allows you to remotely disable or wipe the device if you lose it can prevent the wrong person from accessing PHI. If you log into your electronic health record (EHR) software from remote locations, you should use a virtual private network (VPN) on your device. This software encrypts your data as it travels back and forth between your device and your EHR or another system you’re using remotely.
Responding to breaches
Under HIPAA, you must report breaches of PHI. For example, if your computer system gets hacked, you have to notify your patients that this has happened, as well as what information was compromised and what you’re doing to mitigate the damage. If a breach occurs, you must let the person whose information was compromised or their personal representative, like their parent or guardian, know within 60 days. You also have to let HHS know about the breach. If less than 500 people are affected, you can wait until up to 60 days after the end of the calendar year. But if more than 500 people are affected, you have to let HHS — and local media — know at the same time you notify the patients. Moving forward, you should first assess how this breach happened and how you can tighten controls around PHI. For example, if the breach occurred because someone clicked on a link in an email spoofing or “spear phishing” attack, conduct information security training for all employees.
Conducting risk assessments
To help ensure that you’re HIPAA compliant, make sure you conduct regular risk assessments, both with your staff and with your systems. To make this easier, the Office of the National Coordinator for Health Information Technology (ONC) developed an SRA tool with the OCR and the HHS Office of the General Counsel (OGC). This tool will take you through a series of questions to assess whether you’re at risk of noncompliance. You can also use the paper-based version of the tool to conduct your risk assessment. Using the SRA tool will help you identify any weak points in how you handle PHI and provide information on the potential impact to your healthcare organization if you don’t meet the requirements. If you use the downloadable tool, it won’t send your data anywhere. Ultimately, telemedicine deals with sensitive patient information but in a new way that could pose problems for organizations that don’t pay close attention to HIPAA requirements. By treating telemedicine as you would in-office visits, you can reduce your risk of running afoul of regulators.
How to start a telemedicine practice
Telemedicine naturally requires online tools to treat and diagnose patients. While it may be tempting to use consumer-grade products like FaceTime or Skype for telemedicine, laying the foundation now for a HIPAA-compliant telemedicine practice will make it easier to continue providing services after the coronavirus pandemic. The first thing you need to do is find out whether or not your technology providers will sign a business associate agreement (BAA). This document will protect you if your technology provider accidentally breaches HIPAA. You should also investigate their information security procedures. The Health Information Technology for Economic and Clinical Health (HITECH) Act provides guidelines for healthcare providers to secure protected health information (PHI). Knowing the ins and outs of this law can help you choose telemedicine software that’s HIPAA compliant.

Here are some tips related to specific products you’ll be using as part of a telemedicine practice.
HIPAA-compliant video conferencing
Video conferencing software is extremely important for telemedicine. This is where you’ll conduct virtual visits with your patients. Their privacy and security is paramount. You don’t want to use software that stores their information insecurely — or lets someone who isn’t supposed to be on the call log in. For example, video conferencing provider Zoom entered the spotlight during the coronavirus pandemic when many people started using it for business and personal meetings. However, the platform quickly came under fire for security issues, including the ability for hackers to “Zoombomb,” or join a call that they weren’t invited to. Users also raised concerns about encryption issues. Your best bet for HIPAA-compliant video conferencing may be a provider that creates software specifically for healthcare organizations. Doxy.me, Secure Telehealth, and VSee are all standalone video conferencing platforms for the healthcare industry. Zoom has also created a product for healthcare, Zoom for Healthcare, that should resolve some security concerns. 
HIPAA-compliant cloud storage
To access patient information from anywhere, you need a HIPAA-compliant cloud storage provider. HITECH has set forth guidelines about what you should look for, including a permission-based system that limits the likelihood of unauthorized access to PHI. The system should also provide access monitoring, audit trails, and data encryption while the data is in transit and being stored. The good news is, there are five big cloud storage providers that will all enter into a BAA and meet HITECH requirements. Dropbox, Google Drive, Microsoft OneDrive, Amazon Web Services (AWS) storage service, and Box are all HIPAA compliant. The one you choose will depend on your storage needs and budget.
HIPAA-compliant hosting
Your practice’s website will also need to be HIPAA compliant. Web hosting handles electronic data, including PHI, when a patient accesses their records, so look closely at how your web hosting provider limits unauthorized access and safeguards data. When you’re researching web hosts, look for providers that offer solutions specifically for healthcare. These have likely conducted third-party audits to ensure they’re following HITECH guidelines for electronic data. Some providers that offer HIPAA-compliant hosting include Liquid Web, Rackspace, AWS, and Microsoft Azure.
HIPAA-compliant email
While some practices have embraced patient portals, others use email to communicate with patients. HIPAA allows electronic communications with patients, including email, but you must ensure you’re following regulations. You’ll need a HIPAA-compliant email provider like HIPAA Vault. Another way to make sure your email is HIPAA compliant is to use an add-on to your existing system that encrypts your emails. Services like Virtru, Paubox, NeoCertified, and Protected Trust all offer extensions that sit on top of existing email programs like Outlook or Gmail, and protect data in transit and at rest.
HIPAA-compliant CRM
Using a customer relationship management (CRM) system can help you stay in touch with your patients. It pulls together different sources of data like clinical, financial, and contact information so that you can remind patients of appointments or help engage them in their healthcare plan. A HIPAA-compliant CRM solution is a must so that your patients’ PHI isn’t compromised. If you’re looking for a standalone CRM platform that’s HIPAA compliant, there are several options. Zendesk has been HIPAA compliant since 2015, and Salesforce, a popular choice among many companies, can be configured to be HIPAA compliant.
HIPAA-compliant online forms
As part of your medical practice, you’ll likely use intake forms for patients to self-report their medical histories. Data must be protected as it’s collected and transmitted, which means you need a HIPAA-compliant online form provider. JotForm not only offers a BAA but also provides templates for healthcare forms. You can schedule appointments, send intake forms to patients before their appointments, and have them sign agreements using electronic signatures. You can even embed payment into the forms so they can securely submit their copays.
The importance of staff training
You must train your staff on HIPAA compliance for telemedicine. According to an IDG study, 98 percent of IT leaders agree that humans are the weakest link in cybersecurity. They’re the ones most likely to click on a link in an email or accidentally provide PHI to the wrong person. When you use a lot of different online systems, it’s even more critical to educate staff on HIPAA and cybersecurity risks. In addition to making sure they use virtual private networks (VPNs) to access any PHI, teach them not to click on any links in emails from people they don’t know. While it’s impossible to come up with every possible scenario, creating a written policy and guidelines can help to educate employees. Focus on the most likely issues, like sharing information online, using strong passwords, and being cautious about email links.
HIPAA and social media
A lot of patients are willing to share PHI over social media, but social media isn’t HIPAA compliant if it involves PHI. Additionally, healthcare providers should never post anything that could identify a patient on social media, including pictures with their faces blurred out or gossip about patients, even if the patient’s name isn’t mentioned. HIPAA does have a marketing exception, but you need to get permission in writing to use the patient’s information. For example, if you’re a dermatologist, you might want to show a patient’s skin before and after treatment. You need to get a signed release, which you can do using a HIPAA-compliant form.
Patient education
One of the roadblocks you may encounter in telemedicine is patients’ inability to use some of the tools. For example, they may be confused about video conferencing and whether or not they need a computer. Your patients will need at least some basic tech knowledge so they can log in. Spending time on patient education can help. You can post instructions to your website, as well as send them via email to patients prior to their appointments, perhaps when you send an intake form. This will help them get up to speed before the visit. Choosing HIPAA-compliant and easy-to-use tools now will help you build the foundation for a telemedicine practice. Always check the security policies and protocols of any provider you’re considering, and make sure it’s possible to get a BAA before you start using them.
Managing a telemedicine practice
Once you’ve got your telemedicine practice up and running, you’ll need to manage it. A telemedicine practice has a lot in common with a brick-and-mortar clinical practice, so the way you manage it will be similar. However, introducing additional technology means you’ll have to manage your online tools and your staff differently. Whereas in a traditional practice you might only need someone to manage your electronic health record (EHR) software, email system, and computer systems, in a telemedicine practice, you’ll have a lot of other products to maintain, like video conferencing tools and cloud storage services.

The main difference between telemedicine and traditional medicine
In a traditional medical practice, you can do almost everything in person. For example, you can triage a patient to determine the severity of their symptoms. You can also test a blood sample that the phlebotomist drew. But many medical practices are turning to online technologies to make patient care more efficient and to provide greater access to specialists. For instance, instead of sending a physical slide with a sample from a patient’s tissue to a pathologist, they might use telepathology to have a medical professional digitally review the slide for abnormalities. In a telemedicine practice, you’ll be doing almost everything online. Triage will be conducted via video conference or over the phone. The only time you’ll see patients in person is if you have to do lab work or if their symptoms are severe enough for an examination.
Collecting payments
Collecting payments for telemedicine services can pose a challenge. Even with parity laws that require insurance companies to reimburse you for telemedicine services just as they’d reimburse for an in-person office visit, you may need to collect copays. In addition, if you see private pay patients, you’ll need to collect payment from them directly. There are a few ways you can do this. Some practices that have been using a credit card reader with a keyboard input may be able to take payments over the phone, but this can be difficult if you’re running your practice remotely. You may not have access to the card reader, for example. Using a form can be a much easier and safer way to collect payment for telemedicine services. Some of the video conferencing software providers, like Doxy.me, have this feature integrated in their premium plans, and it’s fully compliant with the Payment Card Industry Data Security Standard (PCI DSS). However, if you want to choose your payment provider or send the form ahead of time to your patient, it might be better to use a standalone form solution like JotForm. You can set up your own form with custom fields and embed a payment gateway to a provider you choose, like PayPal, Square, and Stripe. JotForm is fully PCI DSS compliant as well.
Reimbursement
In addition to collecting payment for telemedicine services, make sure to use the right billing codes so that the insurance company will reimburse you. The policies for reimbursement vary by provider, so double-check to make sure you’re using the right Current Procedural Terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS) codes. CPT and HCPCS codes may change as new services are accepted for reimbursement, so it’s important to pay attention to any changes. For example, during the coronavirus pandemic, two new HCPCS codes (U0001 and U0002) and one new CPT code (87635) were added for coronavirus-related testing services. If you’re billing Medicare, you can reference an online fact sheet they’ve provided for the codes that should be used. In almost all cases, the codes can vary depending on whether you’re treating a new or established patient and how long the visit lasts.
Maintaining records
In addition to collecting payment, you’ll also have to maintain patient records. When you conduct telemedicine visits, you have to document them just as you would an in-person visit. That includes things like the evaluation you’re doing, their signed informed consent form, evaluation results, diagnosis, and recommendations for further treatment. Online forms can also help you with this. For example, you can send an informed consent form to the patient using JotForm and embed an e-signature widget so the patient can sign the form. If you need to get information from a patient before a visit, like an update on their condition, you can also use online forms.
Patient confidentiality
Another important part of managing a telemedicine practice is maintaining confidentiality. When you’re dealing with computer systems, there’s always a possibility that hackers could gain access to your patients’ information. However, if you’ve chosen your software providers carefully, this becomes less of an issue. As discussed in a previous chapter, humans tend to be the weakest link in any security chain. When your staff is working remotely, it’s important that they know what they can and can’t disclose so that they can keep patient information protected and stay HIPAA compliant. One way to do this is to require staff members to sign confidentiality agreements. If they’re not able to come into the office, you can have them sign online agreements that detail their responsibilities. Additionally, if you need to release a patient’s information to another provider or a family member, you can send them a form to sign electronically and easily add it to their record. While managing a telemedicine practice can seem very different from managing a traditional brick-and-mortar clinic, you can use best practices from a physical setting for an online practice. The only big difference is that you’ll have to adapt to an online world, which means choosing tools that let you do things like collect consent and payment virtually.
How telemedicine can be the best option during a pandemic
COVID-19 has taught healthcare organizations a lot about telemedicine. While telemedicine has historically been slow to catch on because of reimbursement issues and patient hesitation, the pandemic has necessitated virtual visits to slow the spread of the disease. In-person visits could actually pose a danger to patients and providers alike, as carriers of COVID-19 can be asymptomatic and contagious for approximately 14 days after exposure. During a time when doctors are needed more than ever, healthcare providers rapidly adopted telemedicine, and insurance companies and Medicaid stepped up to provide reimbursement.

For example, in California, Stanford Children’s Health had 35 daily telemedicine visits before COVID-19. But after the pandemic hit the state, the organization logged 500 in just one day.
Telemedicine lessons from the COVID-19 pandemic
The biggest lesson that both patients and providers have learned during the COVID-19 pandemic is that telemedicine is not only possible, but it’s a viable option for treatment. Going forward, telemedicine may be adopted even more widely. A survey found that 60 percent of adults are willing to use telemedicine due to the pandemic. This can open the door for more types of telemedicine and expand the types of care that can be provided remotely. A secondary lesson is that telemedicine conducted via video conferencing is only the tip of the iceberg. As discussed in previous chapters, there are so many types of telemedicine that can be used to provide care, including the use of connected devices. For instance, connected blood pressure monitors can upload data to an electronic health record (EHR), which can then alert the provider if the reading is abnormal. This makes patient monitoring easier because they don’t have to travel to a doctor’s office.
Technology makes telemedicine possible
The widespread availability of high-speed internet and smartphones has made telemedicine available to people who would otherwise need to be seen in person for routine care. During the COVID-19 pandemic, internet provider backbone networks didn’t show signs of congestion, suggesting a mature infrastructure that can handle the additional load. There are also a plethora of technology tools available, which makes it much easier for providers to introduce and leverage telemedicine. Video conferencing, cloud storage, CRM, HIPAA-compliant forms, and other online tools have removed some of the biggest barriers to entry. Online forms are more critical than ever right now, as healthcare providers need up-to-date information on patient symptoms, as well as releases and informed consent forms to be signed electronically. JotForm offers customizable, HIPAA-compliant forms to collect data for healthcare organizations, including templates that can be customized for different practices.
Coronavirus Responder Program
Recognizing the need for telemedicine on the front lines of the COVID-19 pandemic, JotForm quickly rolled out the Coronavirus Responder Program. This program provides free, unlimited, HIPAA-compliant JotForm accounts to first responders, healthcare providers, nonprofits, and government organizations. This program can provide a lot of benefits to those trying to stop the spread of COVID-19. It includes templates that can assist with creating forms to collect data from patients and other clients.
Telemedicine toolkit
JotForm has also created a toolkit for medical practices that contains the online medical forms necessary to collect patient data while keeping it safe. This includes a way to capture electronic signatures on consent forms, schedule appointments, collect payments, and conduct patient intake.  In addition, the toolkit helps telemedicine practices provide ways for patients to upload files, like videos, documents, and photos. For example, a patient could upload a photo of their reaction to a particular product for a doctor to evaluate. Providers can more easily provide a diagnosis with the JotForm Draw on Image widget, which lets patients draw on a diagram to show where their pain is, such as their left knee or lower back. This information can help medical professionals assess how treatment is progressing and provide suggestions to alleviate pain or discomfort. These forms integrate with HIPAA-compliant tools like Dropbox, Google Drive, and Google Sheets, along with other telemedicine software. You can also generate password-protected PDF files to send to patients, securing the documents so that they’re for patients’ eyes only. Finally, the ability to use JotForm’s HIPAA-compliant telemedicine tools on mobile devices will allow healthcare professionals to treat and diagnose patients remotely. For instance, they can assign forms to other staff members, who can respond using their mobile devices. During a pandemic, telemedicine can, in some cases, be a better option to provide care to patients. It enables providers to triage and diagnose from a distance, allowing patients to remain in the safety of their homes while receiving treatment.
Conclusion
While telemedicine has come into the spotlight because of the COVID-19 pandemic, it isn’t new. Providers were slow to adopt it because of reimbursement issues, but Medicare’s newly adopted rules and insurers’ recent acceptance of telemedicine has made it more commonplace. As a result, many healthcare providers have turned to telemedicine to provide care during this time. They can remotely diagnose and treat patients, as well as conduct maintenance visits, which is safer for both them and their patients.

There are many different types of telemedicine, all of which must comply with HIPAA. Whether it’s sending radiological images to be read digitally or conducting a video doctor visit, these methods allow providers and patients to connect regardless of location. Starting a telemedicine practice requires selecting tools carefully, including video conferencing, CRM, cloud storage, web hosting, and data-collection tools. You’ll also need to train staff and educate patients on how to use these tools and on best practices for protecting patient information.The COVID-19 pandemic has taught healthcare providers and patients alike that telemedicine is a viable healthcare option. Using technology, including JotForm’s HIPAA-compliant forms, can expand access to care and make the process more convenient for patients.
0 notes