#the greater your risk of permanent vision loss in the affected eye.
Explore tagged Tumblr posts
Text
What is Retinal Detachment?

Retinal detachment describes an emergency situation in which a thin layer of tissue (the retina) at the back of the eye pulls away from its normal position.
Retinal detachment separates the retinal cells from the layer of blood vessels that provides oxygen and nourishment to the eye. The longer retinal detachment goes untreated, the greater your risk of permanent vision loss in the affected eye.
Warning signs of retinal detachment may include one or all of the following: reduced vision and the sudden appearance of floaters and flashes of light. Contacting an eye specialist (ophthalmologist) right away can help save your vision.
For more information, consult Dr. Vaidya Eye Centre the Best Retina Specialist in Mumbai.
#Retinal detachment describes an emergency situation in which a thin layer of tissue (the retina) at the back of the eye pulls away from its#Retinal detachment separates the retinal cells from the layer of blood vessels that provides oxygen and nourishment to the eye. The longer#the greater your risk of permanent vision loss in the affected eye.#Warning signs of retinal detachment may include one or all of the following: reduced vision and the sudden appearance of floaters and flash#For more information#consult Dr. Vaidya Eye Centre the Best Retina Specialist in Mumbai.
0 notes
Text
Top 5 Reasons to Consult a Retina Specialist in Greater Noida for Eye Health
EYES ARE indeed the windows to one's health, and a Retina Specialist in Greater Noida is one of them as keeping the retina healthy is important for maintaining good vision. A retina specialist identifies several conditions that lead to retinal diseases that could, possibly affect one's eyesight. If you have no clue about when it's time to go see a retina specialist, here are the top five reasons to make an appointment,

1. Diabetic Retinopathy
Diabetic retinopathy is one of the common complications of people with diabetes and, if not treated, may lead to vision loss. An eye specialist in Greater Noida can diagnose the early stages of this disease and use treatments such as laser treatment or injections to prevent damaging effects on your eyes. For any diabetic person, regular check-ups are important to keep your eyes healthy.
2. Age-Related Macular Degeneration (AMD)
One of the primary reasons for loss of vision in geriatric patients, AMD affects the central area of the retina. Early detection is highly crucial in the treatment of AMD and its progression rate. Retina specialists in Greater Noida take utmost care to provide superior treatment options that preserve vision and provide quality of life to those afflicted by this medical condition.
3. Retinal Detachment
Retinal detachment is a condition that requires immediate care for emergencies. Sometimes flashes of light, floaters, or shadows cast over the visual field may point out the requirement to see a Retina Specialist in Greater Noida as early as possible. In this case, prompt treatment can save one from permanent vision loss.
4. Treatment for Eye Injuries
Traumatic eye injuries will often cause either retinal tears or detachments, requiring special attention. A retina specialist is trained to manage such emergencies and performs surgical interventions as indicated to preserve vision.
5. Multi-disciplinary care for complex eye conditions
A Retina Specialist in Greater Noida can address a range of complex conditions that involve macular holes, uveitis, and inherited retinal diseases. Patients are assured of getting broad, state-of-the-art care in an environment tailored to their particular need.
Regular visitations with a Retina Specialist in Greater Noida are necessary for maintaining long-term eye health, especially among people at risk for retinal conditions. Don't wait till the condition worsens—come now to seek the best care for your eyes and your future.
0 notes
Text

Retinal Detachment describes an emergency situation in which a thin layer of tissue (the retina) at the back of the eye pulls away from its normal position. The longer retinal detachment goes untreated, the greater your risk of permanent vision loss in the affected eye.
Warning signs of retinal detachment may include one or all of the following: - reduced vision - sudden appearance of floaters - flashes of light. Contacting an eye specialist (ophthalmologist) right away can help save your vision.
Consult our specialists from 9:00AM to 8:00PM!!
📞 Call to book your appointments.
https://chandanhospital.in/
#StayHealthy #StaySafe #ChandanHospitalCares #ChandanHospital #MultiSpecialityHospital #Surgeon #BestSurgeons #Health #BestTreatment #Healthcare #BestHospitalInLucknow #Lucknow #BestHospitalInUttarPradesh #EyeSurgery #Ophthalmology #Retina
#best cardiac hospital in lucknow#best ivf hospital in lucknow#best ivf centre in lucknow#cancer treatment in lucknow#best cardiac hospital
0 notes
Text
Preserving Sight: Understanding Age-Related Macular Degeneration
Macular degeneration (AMD), also referred to as age-related macular degeneration, is a progressive eye condition affecting millions of people globally and one of the primary causes of vision loss among individuals aged 50 or over. Understanding its causes, symptoms and available treatments is vital in order to early detect and effectively manage this debilitating disease.

What Is Macular Degeneration?
The macula is a small yet highly sensitive area located at the center of our retinas at the back of our eyes that provides clear, detailed vision for activities such as reading, driving and recognising faces. Macular degeneration occurs when this vital structure begins deteriorating slowly over time causing central vision loss while leaving peripheral vision unaffected.
Types of Macular Degeneration: There are two primary forms of macular degeneration, dry AMD and wet AMD.
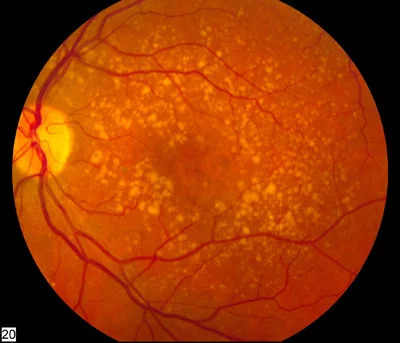
Dry AMD: Dry AMD accounts for an estimated 90% of cases. It typically progresses slowly, as deposits called drusen accumulate over time in the macula, leading to gradual vision loss over time. If left untreated, dry AMD could become permanent.
Wet AMD: Although less common and severe than its dry counterpart, Wet AMD can still have devastating results. It occurs when abnormal blood vessels form beneath the retina and leak blood and fluid onto it, leading to scarring and macula damage which leads to significant vision loss quickly and unexpectedly.
Although its exact causes remain unknown, certain risk factors increase your likelihood of macular degeneration:
Age: Macular degeneration typically affects people aged 50 or above. After 50, their risk significantly increases.
Genes: Macular degeneration runs in families, making the likelihood of developing it greater.
Smoking: Studies have conclusively linked smoking with an increased risk of macular degeneration.
Race and Ethnicity: Caucasians of European descent are more prone to macular degeneration than people from other races or ethnic backgrounds.
Macular degeneration often does not present with noticeable symptoms in its early stages; however, as the condition worsens individuals may notice the following:
Blurred or distorted central vision
difficulty reading or recognising faces
reduced color perception
If you notice dark or empty areas in the center of your vision, it is crucial that you seek medical advice as soon as possible. Regular comprehensive eye exams - with dilation - can aid in early detection and diagnosis of macular degeneration.
Treatment and Management:
Regular treatments are not effective for Macular Degeneration. One of the most effective ways to treat Macular Degeneration is Sanjeevan Netralaya’s Advanced Ayurvedic Eye Care. At Sanjeevan Netralaya, every patient is given special individual care and is provided unique treatments that is suited to their bodies and condition instead of a generic line of treatment. This ensures effective care as well as makes sure that the patient does not go through any painful or harmful side effects.
Macular degeneration is an eye condition that can significantly impede an individual's quality of life, so understanding its causes, symptoms, and available treatment options are vital in early diagnosis and successful management. Scheduling regular eye exams at clinics like Sanjeevan Netralaya, adopting healthy lifestyle choices, seeking professional help for vision preservation as well as living life with macular degeneration are key strategies in adapting to life with macular degeneration and adapting accordingly. By raising awareness and funding research efforts on macular degeneration we can work toward an eventual prevention.
#sanjevan netralaya#macular degeneration cure#wet macular degeneration#amd#retina centers#eyesight#eyes#retina#eyes ayurvedic treatment#ayurvedic treatment for glaucoma#glaucoma treatment in ayurveda#diabetic retinopathy
0 notes
Text
The Benefits of Retinal Photography
Digital Retinal Photography is Now at Tatum Eyecare!
Digital Retinal Photography is a very effective way to photograph of the interior surface of the eye, including the retina, optic nerve and macula. As one of the newest innovations in the eye health care industry, digital retinal photography helps optometrists, ophthalmologists and other trained medical professionals diagnose eye disorders and diseases, as well as monitor disease progression with greater accuracy than ever before.
Being one of the newer kids on the block, digital retinal photography is lauded by some people, while other people remain skeptical. At Tatum EyeCare, we understand digital retinal photography is a smart choice for diagnostic and preventative purposes regardless of any existing eye disorders and diseases you have, or that you might knowingly be at risk for. Why do we feel this way? Well, if you keep reading we will tell you!
What Eye Disorders and Diseases Are Detected?
Some of the eye disorders and diseases digital retinal imaging can detect include:
Macular Degeneration
Glaucoma
Cataracts
Retinal Tears or Detachments
Occlusion
Even Diabetes and High Blood Pressure
The pictures we take help us assess the health of your retina, and help us to detect and manage the aforementioned eye disorders and diseases. Finding retinal disorders as early as possible is critical for preventing serious disease progression and even vision loss.
In addition to helping detect eye disorders and diseases early, digital retinal photography provides a permanent historical record of changes in your eye. Images can be compared side-by-side, year after year, to discover even subtle changes that may adversely affect your health.
Digital Retinal Imaging vs Dilation
There is still some debate about Digital Retinal Imaging vs Dilation. Let’s take a moment to discuss the benefits of digital retinal imaging vs. dilation. Some of them include:
Expediency. It takes us seconds to take a retinal image vs 45 minutes to 1 hour to complete the dilation process
Comfort. Taking a retinal image is painless vs dilation, which is notoriously uncomfortable and has effects lasting several hours after the drops are placed in each eye
Coverage. This is one of the biggest benefits of digital retinal imaging vs dilation. Dilation only lets us see about 15% of your eye, while digital retinal photography increases that to 95%!
As you can see, the digital retinal imaging vs dilation debate is not really a debate at all!
Is Taking a Retina Image Safe?
Yes it is. Taking a retina image is very safe. In fact, the only potential complaints we ever get when we take a retinal image are about the technology itself…. as patients have to lean in and keep their eyes close to the imaging machine for about 30 seconds. Contrast this with eye drops that irritate your senses while blurring your vision for hours, and a retina image seems like the much better choice of the two options!
A Digital Retinal Scan Educates Everyone
Finally, a digital retinal scan provides us with a host of images we can review together with you. As a result, we can point out the various structures of the retina and explain treatment options for any conditions revealed by the pictures. We believe the more you know about eye disorders and diseases, the more likely you will be to understand and follow an eye doctor’s recommendations for treatment and prevention. in this way, a digital retinal scan is an educative tool we can explore together that will help increase your education, awareness and active investment in the longevity of your healthy sense of sight.
The Best Optometrists in North Phoenix
When you choose Tatum EyeCare for you vision health and fashion needs, you are choosing optometrists in North Phoenix who are invested in our clients and community. We are happy to answer any other questions you have about retinal imaging, or to schedule your appointment with one of our optometrists today. We’ve proudly served the Valley of the Sun for over 20 years. Stop in to view our extensive eyewear collection, and see for yourself how Tatum EyeCare reframes customer service and optical expertise for everyone!
Contact Tatum eyecare
#tatum eyecare#eyewear#eyecare center#eyecare clinic#eyeexam#eyeglasses#best optometrist#Retinal Photography
0 notes
Text
Retina Treatment In Mumbai

Retina is like the film in a camera. Retina is the third and inner coat of the eye which is a light-sensitive layer of tissue. When the focused light hits the retina, a picture is created and sent to the brain through the optic nerve (the nerve of the eye), thus giving us vision. Sometimes part of the retina either tears, pulls away or detaches from the back of the eye; when this occurs that part of the retina cannot gather light ans results in vision loss.
Diseases and conditions of the retina
Age-Related Macular Degeneration
Diabetic Retinopathy
Retinal tear
Retinal Detachment
Age-Related Macular Degeneration
What causes in AMD?
During normal aging, yellowish deposits, called drusen, form under the retina, which is the light-sensitive layer of tissue at the back of the eye that provides clear, sharp images.
As drusen increase in size and number, they can interfere with proper functioning of the retina, damaging or killing the light-sensitive cells of the macula.
Because the macula’s light-sensitive cells provide the ability to have sharp, detailed vision, the results can be blurring of central vision and a devastating impact on the ability to enjoy activities of daily life, such as reading, driving, or even recognizing the face of a friend or family member.
This form of age-related macular degeneration is called dry AMD. Dry AMD can be a precursor to wet AMD.
Wet AMD occurs when abnormal blood vessels behind the retina start to grow under the macula. These blood vessels often leak blood and fluid, damaging or killing light-sensitive cells—loss of vision occurs quickly.
Although approximately 80 percent of patients with age-related macular degeneration have dry AMD, wet AMD is responsible for 80 to 90 percent of severe loss of vision with this disease.
Life with AMD : what you should know but din’t
AMD may be a difficult condition, but it is not as devastating as people fear when they are diagnosed and only rarely leads to complete blindness. Millions of people actually live healthy, independent lives, despite having age-related macular degeneration.
It is important to learn about the disease and work with a retina specialist, who will put a treatment plan in place. These physicians have the ability, training, and experience to treat all medical and surgical aspects of AMD and other diseases of the retina.
A retina specialist can also suggest access to rehabilitation options like low vision aids which includes a variety of tools and resources that can make everyday living with AMD a little bit easier.
Symptoms
The earliest signs of AMD in the retina can be detected by a retina specialist before you have any vision loss, but those who have had the disease for some time may notice changes in vision which are symptomatic of dry and wet AMD.
Dry AMD symptoms
Need for brighter light when reading
Difficulty adapting to low light levels
Increased blurriness of printed words
Decrease in brightness of colors
Blurred spot in the center of the field of vision
Blank or black spot in the field of vision (spot will start small and grow over time, possibly leading to blindness
Wet AMD
Early stage wet AMD
End stage wet AMD with scarringWet AMD Symptoms
Sudden painless decline in central vision
Visual distortions, such as straight lines appearing wavy, or objects appearing larger or smaller than they are
Well-defined blind spot in the center of vision
It is important to pay close attention to any decline in central vision—both near and distant. If you notice any of these signs or symptoms, schedule an examination with a retina specialist.
Risk factors
Many people ask if age-related macular degeneration can be prevented. Like most things in life, there is no easy answer.
The primary risk factor for AMD is age—the older you are, the greater your risk. Also, people with a family history of AMD are at higher risk, as are women and people of European descent.
Some lifestyle factors are also known to increase your risk for AMD:
Cigarette smoking
Obesity
Hypertension (high blood pressure)
Excessive sun exposure
Diet deficient in fruits and vegetables
Diagnostic tests
The best way to detect AMD is an examination by a retina specialist. The following are some typical methods he/she will use to check for AMD.
Dilated eye exam
In this examination, a physician uses eye drops to dilate, or widen, the pupil to examine the retina. Regular dilated eye exams are important, especially for those who are at a higher risk for developing AMD.
If you are over age of 50, it is a good idea to schedule an periodic eye examination to look for the earliest signs of AMD before any vision loss has occurred.
Ocular coherence tomography
The physician may suggest an optical coherence tomography (OCT) exam. This test provides cross-sectional images of the retina that show its thickness, helping determine whether fluid has leaked into retinal tissue and other changes that happen with AMD.
Amsler grid
Another way to detect AMD is by using an Amsler grid test. In this test, the patient covers one eye at a time and stares at the black dot at the center of the grid. If the straight lines appear broken, crooked, wavy, bent, or distorted, the patient may have AMD.
It is important to note that this test is hardly sufficient to rule out the possibility of AMD, as many people with the disease may see no abnormalities on an Amsler grid.
Visual acuity test
Because AMD affects visual acuity, an eye chart can also be an indicator of the development of AMD.
Treatment and drugs
There is no known cure for AMD, but early detection and proper treatment can protect vision from further deterioration.
Dry AMD treatments
Currently, no medical treatments exist for dry AMD, but the retina specialist will suggest strategies to slow its progression—taking vitamin or mineral supplements, for example.
If you have Dry AMD, it is extremely important to follow your retina specialist’s eye examination schedule.
Biweekly Amsler’s grid self examination
Also, if you experience new symptoms or your notice any deterioration in vision, see your retina specialist right away.
Retinal Tear / Detachment
Tears or detachment results from aging, an eye-injury, or another eye problem.
A retinal detachment occurs when fluid leaks through the tear and separates the retina from the back of the eye.
Symptoms of Retinal Tear:
Floaters (specks or threads in your vision).
Flashes (lights, stars or streaks in your vision).
Sudden blurry vision.
Treatment of Retinal Tear is mainly surgical this involves :
Pneumatic retinopexy- Sealing a tear:
This procedure can be used to treat retinal detachment if the tear is small and easy to close. A small gas bubble is injected into the eye (specifically into the clear, gel-like substance between the lens and the retina), where it then rises and presses against the retina, closing the tear. A laser or cryopexy can then be used to seal the tear.
Each of these treatments seals the retina to the back of the eye, and prevents progressive deterioration of the tear.
Symptoms of Retinal Detachment:
Flashes of light
Seeing “floaters” (small flecks or threads)
Darkening of your peripheral (side) vision
Treatment for Retinal Detachment :
Laser Treatment of the Retina : Laser is usually performed to decrease leakage in the retina, treat abnormal blood vessel growth, or create a beneficial scarring effect that can help prevent a retinal detachment. It is a non invasive procedure .
Scleral Buckle : This treatment for retinal detachment involves surgically sewing a silicone band (buckle) around the white of the eye (called the sclera) to push the sclera toward the tear until the tear heals. This band is not visible and remains permanently attached. Laser or cryo treatment may then be necessary to seal the tear.
Vitrectomy : A sophisticated microsurgical technique in which the vitreous gel is removed from inside the eye with a small, specialized cutting device, an operating microscope to look into the eye, and microsurgical instruments.
Depending on the complexity of the retinal detachment, various combinations of vitrectomy, buckle, laser and gas bubble may be used to repair the retina.
Diabetic Retinopathy
Diabetic retinopathy is a diabetes complication that affects eyes. It’s caused by damage to the blood vessels of the light-sensitive tissue at the back of the eye (retina). The cells in persons with diabetes mellitus have difficulty using and storing sugar properly. When blood sugar gets too high, it can damage the blood vessels in the rear of the eyes. This damage may lead to diabetic retinopathy. It can lead to vision loss or blindness. You already may have diabetic retinopathy, or be at risk for it. But you can take steps to reduce your risk of vision loss from this condition.
Symptoms
Spots or dark strings floating in your vision (floaters)
Blurred vision
Fluctuating vision
Impaired color vision
Dark or empty areas in your vision
Vision loss
Diabetic retinopathy usually affects both eyes
Causes
The primary cause of diabetic retinopathy is diabetes—a condition in which the levels of glucose (sugar) in the blood are too high. Elevated sugar levels from diabetes can damage the small blood vessels that nourish the retina and may in some cases block them completely. As a result, the blood supply to the retina from these damaged blood vessels is cut off and vision is affected.
In response to the lack of blood supply, the eye may create growth factors that lead to diabetic macular edema, which can lead to decreased vision, or proliferative diabetic retinopathy, which can lead to retinal detachment and vision loss.
Complications
Complications can lead to serious vision problems:
Vitreous hemorrhage : The new blood vessels may bleed into the clear, jelly-like substance that fills the center of your eye. If the amount of bleeding is small, you might see only a few dark spots (floaters). In more-severe cases, blood can fill the vitreous cavity and completely block your vision.
Vitreous hemorrhage by itself usually doesn’t cause permanent vision loss. The blood often clears from the eye within a few weeks or months. Unless your retina is damaged, your vision may return to its previous clarity.
Retinal detachment.The abnormal blood vessels associated with diabetic retinopathy stimulate the growth of scar tissue, which can pull the retina away from the back of the eye. This may cause spots floating in your vision, flashes of light or severe vision loss.
New blood vessels may grow in the front part of your eye and interfere with the normal flow of fluid out of the eye, causing pressure in the eye to build up (glaucoma). This pressure can damage the nerve that carries images from your eye to your brain (optic nerve).
Eventually, diabetic retinopathy, glaucoma or both can lead to complete vision loss.
Development & Types Of Diabetic Retinopathy
Diabetes damages the blood vessels of the Retina & as a result, they may leak fluid, proteins or fats or they may rupture & cause haemorrhage (bleeding) or they may get blocked. This is seen in Background Diabetic Retinopathy.
In the more severe cases, as the blood vessels get blocked, the subsequent loss of nutrition & oxygen to the retina promotes the growth, i.e. proliferation of new, fragile abnormal vessels on the optic disc or elsewhere which easily rupture & use cause large haemorrhage & severe visual loss or blindness. This is seen in Proliferative Diabetic Retinopathy.
When there is involvement of the central vision with difficulty in near vision affecting the most part of the retina called Macula it is known as Diabetic maculopathy.
Detection & Prevention Of Vision Loss
The problem with diabetic retinopathy is that there are no symptoms in the early stages. During the time when retinopathy is most easily treated, the diabetic will not notice visual changes. In fact, more than 50% of patients with proliferative retinpathy may have good vision for 5 years or more. When visual symptoms start, it is often too late. Therefore, consider the following steps:
Routine eye examination – Eyes should be checked periodically as advised by your eye doctor
Diabetes Control
Control of blood pressure (hypertension) and cholestrol
Stop smoking & alcohol intake.
Investigations
Diabetic retinopathy is best diagnosed with a dilated eye exam.
During the exam, the eye doctor looks for:
Abnormal blood vessels
Swelling, blood or fatty deposits in the retina
Growth of new blood vessels and scar tissue
Bleeding in the clear, jelly-like substance that fills the center of the eye (vitreous)
Retinal detachment
Abnormalities in optic nerve
In addition to this exam, there are 3 other diagnostic tools eye specialist use to detect and manage diabetic retinopathy:
Fundus Photograph : This involves taking images of retina using a specialized non contact fundus camera.
Fundus Fluorescein Angiography (FFA): By injecting dye into one of the peripheral veins, severity of retinopathy can be picked up for treatment depending on the pattern of dye leakage.
Optical Coherence Tomography (OCT): is non-invasive as compared to FFA (no needle) & with fundus photography, it provides accurate screening for diabetic retinopathy severity. We have installed the latest 3D OCT at Ojas for enhanced imaging quality.
In addition, the eye doctor may:
Check vision
Measure eye pressure to test for glaucoma
Look for evidence of cataracts
Treatment
Laser photo-coagulation: Diabetic retinopathy is a treatable condition by laser photocoagulation. The Laser beam energy is absorbed by the ocular tissues/retina where it is directed & it is then changed to heat energy which coagulates the tissue by burning. Thus the Laser is used to spot weld the leaking point in the retina. We can prevent the complications of retinopathy such as haemorrhage, fibrous scar tissue formation & retinal detachment.
Intravitreal injections : these are the more recent means of treating diabetic retinopathy. Like Lasers they are not particularly painful, can be more effective than laser itself in most cases.
Surgery : with Microincisional (keyhole) Stitchless Vitrectomy surgery, diabetic retinopathy complications like bleeding & retinal detachment can be easily treated without opening up tissues of the eye or taking stitches.
Are you looking for Retina Treatment in Mumbai, Bandra and Kandivali City?
We at Ojas have Best Eye Surgeon In Mumbai for Retina treatment and surgery. At Ojas Eye Hospital, one of the best eye care hospital in Mumbai all kinds of Retinal diseases like Diabetic Retinopathy, Age Related Macular Degeneration, Retinal tear and Retinal Detachment are treated.
Contact Ojas Eye Hospital today for all your Retina Treatment in Mumbai City at Call us (+91) 9137462795.
Tags = Retina Treatment In Mumbai, Retina Specialist in Mumbai, Retina treatment in India, Retina Specialist in India, Retina Surgery In Mumbai, best Retina hospital In Mumbai, Retina surgeon in Mumbai, Best Eye Hospital in Mumbai
#Retina Treatment In Mumbai#Retina Specialist in Mumbai#Best Laser Eye Treatment in Mumbai#Best Eye Hospital in Mumbai#Eye Hospital in Mumbai
3 notes
·
View notes
Text
Retinal Detachment: Symptoms, Risk Factors, Treatment and Prevention-Mr Harish Jagtani
The retina is a thin, light-sensitive tissue present at the back of the eye where an image is formed by the eye lens. A healthy retina along with a healthy cornea, lens and other eye parts is necessary for a person to see clearly.
When the retina separates from the back of the eye, the condition is known to be retinal detachment which can further lead to partial or complete vision loss. Retinal detachment is a medical emergency since retinal cells may get critically deprived of oxygen, therefore, one should immediately contact a healthcare expert, eye specialist or our Harish Jagtani hospital, in case sudden vision changes are experienced.
A study conducted with 40,965 people aged 40 years or older in Kinshasa showed that retinal diseases are common among Congolese adults. Also, retinal conditions were found to be a major cause of low vision and blindness.
Read on to know more about the condition.
Retinal Detachment: Symptoms
No pain is experienced in usual cases of retinal detachment, however, a person may observe one or more of the below-mentioned symptoms before the retina detaches completely.
Blurry vision
Partial loss of vision
Sudden and brief flashes of light when the eye moves sideways; the condition is also known as photopsia
Sudden and significant increase in floaters (bits of debris which appear as strings, rods or black flecks)
Heaviness in the eye
Other vision problems such as the curved appearance of straight lines or an appearance of a shadow in the peripheral vision
Retinal detachment: Risk Factors
While the condition may affect people of all ages and health status, certain factors are known to increase the risk. These include:
Family history of retinal detachment (i.e. genetic factors)
Prior history of retinal detachment
Advancing age
Eye injury or trauma to the eye
Extreme nearsightedness
Previous cataract surgery that led to complications
Posterior vitreous detachment (a common condition in the elderly)
Poorly managed diabetes mellitus
If you find yourself at a greater risk of retinal detachment, consult your doctor at the earliest to seek preventive treatment.
Retinal Detachment: Surgery
The treatment options for retinal detachment include several kinds of surgery. Without surgery, there is a high risk of complete loss of vision. Commonly used surgical procedures for the treatment of retinal detachment are:
Laser surgery (photocoagulation)
Cryosurgery
Vitrectomy
Scleral buckling
Pneumatic retinopexy
Doctors analyse various factors to find the right type of surgical procedure for a patient.
Retinal Detachment: Prevention
Retinal detachment cannot be prevented altogether by any means, however, one can reduce the chances of developing this condition by taking several steps:
People with diabetes should keep their blood sugar levels under check.
People who often participate in sports or work with tools should wear protective eyewear to prevent injury or trauma to the eye.
People at a higher risk of developing retinal detachment should get eye exams twice a year.
The Bottom Line
Retinal detachment is one of the critical eye conditions and can lead to permanent loss of vision if left untreated or if the treatment is delayed. Therefore, it is necessary to stay aware of its symptoms and risk factors to identify them and seek medical attention at the earliest. Harish Jagtani Hospitals houses a state-of-the-art ophthalmology department to bring world-class healthcare facilities to your proximity. Schedule an appointment now to get a complete eye check-up.
0 notes
Text
The Effects of Diabetes on Eyes

The Effects of Diabetes on Eyes People with diabetes are at greater risk for the development of glaucoma, a condition that damages the optic nerve, which provides sharp vision. This disease is caused by increased blood glucose, which damages the tiny blood vessels in the retina. Moreover, the high glucose levels in the blood can cause cataracts, which are cloudy lenses in the eye. These conditions can severely impact sight, and if not treated early, they can lead to irreversible blindness. People with diabetes are also more likely to develop cataracts, which cause blurred vision. These problems may develop at a young age and get worse over time. The good news is that cataract surgery is available. This procedure involves replacing the cloudy lens in the eye with an artificial one. The process requires a surgeon to remove the cloudy lens and replace it with an artificial one. While most people with diabetes don't notice any symptoms, proliferative retinopathy can lead to a permanent loss of vision, which is irreversible. A person with diabetes needs to monitor their blood sugar levels regularly. If the levels are too high, the retinal tissue cannot change its shape. The lens in the middle of the eye is damaged and cannot heal. Often, diabetics have blurred vision because their blood sugar changes too quickly. In such cases, it is important to have regular eye exams so the doctor can identify any problems before they get worse. However, if this does occur, the damage is irreversible. As diabetes progresses, the blood sugar levels in the eye will increase, and the pressure within the eye will make it harder to see clearly. This will lead to vision loss and further complications. To prevent this, it is necessary to get regular dilated eye exams and control other health conditions. If your blood glucose levels are too high, the ophthalmologist will recommend you take measures to control your diabetes. By managing the condition properly, you can protect your eyes from future damage. In the long term, diabetes affects the eyes and leads to the development of retinopathy, which is the most common cause of blindness in adults aged 20-74. In addition to retinopathy, the other effects of diabetes on eyes include glaucoma, retinopathy, and a change in vision. Although diabetics can improve blood sugar levels by avoiding these conditions, it is important to monitor their eye health on a regular basis. In the long run, diabetes can lead to a variety of eye complications. Dry eyes, for example, can result in impaired vision. While you can manage your diabetes and prevent it from causing these problems, it is important to monitor your sugar levels so that you can avoid developing diabetic retinopathy. If left untreated, it can cause serious problems, including blindness. Even simple symptoms, such as dry eyes, can be serious, such as a sensitivity to light. visit at website -https://www.aarogyalab.com/blog/The-Effects-of-Diabetes-on-Eyes Office Address G-3/48, 3rd floor, sector 15, Rohini New Delhi 110089 India
0 notes
Text
Important Things that Patients Should Know About Carotid Artery Disease
Heart stroke is among the most feared medical ailments. In most cases, it could lead to paralysis or even death. If you have been detected with CAD or Carotid Artery Disease, then here are the top essential things that you should know about the condition:
Restricts the flow of blood to your brain
The carotid artery is present on either side of the neck and facilitates blood flow to the head and the brain. Usually, when the vascular doctor in Bangalore at the vascular clinic touches the side of the neck to check the pulse, they touch to feel the carotid artery. The disease happens when there is an accumulation of plaque or fatty deposits in the artery that blocks the carotid artery, thus, restricting the flow of blood to your brain.
This results in the slow degeneration of the brain and may eventually give rise to various severe symptoms and complications. The vascular doctor in Bangalore can help you to effectively detect and treat the deadly disease.
Transient Ischemic Attack
A TIA or Transient Ischemic Attack is the first symptom of CAD. This disease grows gradually and might not even have any noticeable signs until the patient experiences a TIA or a stroke. The TIA is usually identified as a temporary blockage of the flow of blood to your brain.
The different symptoms of TIA include:
Slurred speech or difficulty in speaking
Weakness or numbness on either side of the body
Dizziness
The trouble with vision both or one of the eyes
Loss of balance or difficulty walking
The signs of TIA are very identical to a heart stroke, but it does not last for that long. If the patient experiences any symptoms of TIA, then they should immediately seek medical help even if they feel better after some time.
Increases the chances of a stroke
CAD stops or restricts the flow of blood to your brain. This dramatically increases the chances of a stroke. The restriction in the blood flow greatly impacts the supply of oxygen to your brain. This may permanently cause brain damage or even death within a few minutes. Carotid artery disease is among the leading causes of death and brain damage around the world.
There are two ways in which this disease could cause a heart stroke. A piece from the plaque could either break off and get lodged or settle in the blood vessels of the brain, resulting in embolism. Sometimes, the carotid artery disease could become very severe and lead to the permanent and complete blockage of the carotid artery. Vascular doctors near me can effectively detect the condition and provide comprehensive treatment.
Increased chance of developing carotid artery disease
Various hazardous factors could enhance the chances of developing CAD. A few of the factors are health-related to hereditary, while many others are correlated to the lifestyle choice of the patient. They include:
Smoking: It increases the heart rate and blood pressure. This could irritate the lining of the arteries, which causes damage and can lead to plaque formation.
High blood pressure: High blood pressure enhances the pressure in the walls of the artery, which causes damage or weakness to the artery and leads to CAD.
High cholesterol: Higher cholesterol levels are the leading risk factor that causes carotid artery disease.
Diabetes: Diabetes affects the natural ability of the body to process fats and blood sugar. This puts a person at greater risk of developing plaque accumulation and high blood pressure.
Obesity: Obesity enhances the chances of diabetes, increased blood pressure, and CAD.
Age: Ageing causes the arteries to weaken or stiffen and make them more liable to get damaged. This could enhance the chance of carotid artery disease.
Family history: Genetic conditions inherited from the family can also put you at a greater risk of the disease.
Lifestyle changes to prevent CAD
By introducing some changes to your daily lifestyle, you can help considerably lower the chances of the disease. These steps include:
Quit smoking: If you are smoking, then it is high time that you quit it now because chain-smoking or even occasional smoking can lead to CAD.
Regular exercise: Physical inactivity can make you obese and overweight, which increases the chances of the disease. Do regular exercise daily for at least 30 minutes to keep your body healthy and to keep your body weight under check.
Balanced diet: Eat a balanced diet of vegetables and fruits. This will help you to keep your body healthy and to manage your weight. Avoid eating oily food or junk food.
Reduce your consumption of alcohol: Alcohol consumption can contribute to CAD.
Limit your cholesterol and fat: Check your cholesterol levels and reduce your bad cholesterol while improving the good cholesterol levels in your body. Also, maintain your fat levels.
Manage your health conditions: If you have chronic ailments such as high cholesterol. High blood pressure, or diabetes, then you should take the necessary steps to manage these conditions to prevent them from escalating into significant situations.
If you are searching for the best vascular clinic or vascular doctors near me, you must visit the Vascular Centre Bangalore today.
0 notes
Text
Symptoms and Treatment of Brain Stroke: A Complete Guide

Stroke is also known as brain stroke is a medical condition where the blood supply to a part of the brain decreases or gets severely interrupted.
It is a medical condition where the cells of the brain start dying within minutes of being deprived of nutrients and oxygen due to the restriction of blood supply. The inability of brain cells to regenerate results in permanent damage and irreversible results.
The human brain is a complex organ that relies on a continuous blood supply. A disruption in blood flow can cut important oxygen and glucose to the brain and lead to brain death within a couple of minutes.
Signs and symptoms of stroke include:
If you or someone you're with maybe having a stroke, pay special attention to the time the symptoms began. Some treatment options are most effective when given early after a stroke begins in humans. Compared to men, women are more likely to get a brain stroke.
Trouble in speaking and understanding what other people are saying. You might experience confusion, slur your words or have difficulty understanding speech and words.
Paralysis or numbness in the face, arm, and leg. You might develop sudden numbness, weakness, or paralysis in your face, arm or leg. This often affects just only one side of your body part. Try to raise your both arms over your head at the same time. If one arm begins to fall, you might be having a stroke. Also, one side of your mouth might droop when you try to smile and speak.
Problems seeing in one or both eyes. You may suddenly have blurred or blackened vision in your eyes, or you may see double.
Headache. A sudden, severe headache, that can be accompanied by vomiting, dizziness, or altered consciousness, might indicate that you're having a stroke.
Trouble walking. You may stumble or lose your balance while walking. You might also have sudden dizziness or a loss of coordination.
Risk factors for brain stroke and how can brain stroke be prevented?
Many of the risk factors for brain stroke are related to a poor and bad lifestyle. Some of these are:
Obesity
Sedentary and stressful living
Chronic alcoholism
Addictive drug abuse like cocaine
Uncontrolled high blood pressure, diabetes, and cholesterol
Tobacco chewing and smoking
Disorders of sleep like obstructive sleep apnea
Cardiovascular diseases like heart failure
Changes in lifestyle and habits can help in the prevention of brain stroke. Depending upon your risk factors, your neurosurgeon or cardiologist may advise medications for brain stroke prevention, if required.
A brain stroke is a medical problem. Quick diagnosis and prompt care from a trained emergency team of the best neurosurgeons, vascular surgeons, cardiologists, and neurologists can save one from a disability or fatal consequences.
Time to see a doctor
Seek early medical attention if you notice any signs or symptoms of a brain stroke, even if they seem to come and go or they disappear completely. Also, you can visit the best neurosurgeon in your area to get early treatment. Think "FAST" and do the following:
Face. Ask the person to smile. Does one side of the face droop?
Arms. Ask the person to raise both arms. Does one arm drift downward? Or is one arm unable to rise?
Speech. Ask the person to repeat a simple phrase or words. Is his or her speech slurred or strange seems?
Time. If you notice any of these signs, call emergency medical help immediately.
Call top neurosurgeon or your local emergency number right away. Don't wait to see if symptoms stop and fine. The longer a brain stroke goes untreated, the greater the amount of brain damage and disability.
Batish Neurosurgery: Best Neurologist in Panchkula
Batish Neurosurgery is a place where we treat all kinds of neurological conditions. Dr. V.K Batish and Dr. Aman Batish, are among the renowned neurologists in Chandigarh, Mohali, and Panchkula.
If you're with someone you suspect is having a brain stroke or some symptoms, Book an appointment and start a happy journey towards a healthy brain.
0 notes
Text
What is Retinal Detachment?

Retinal detachment describes an emergency situation in which a thin layer of tissue (the retina) at the back of the eye pulls away from its normal position.
Retinal detachment separates the retinal cells from the layer of blood vessels that provides oxygen and nourishment to the eye. The longer retinal detachment goes untreated, the greater your risk of permanent vision loss in the affected eye.
Warning signs of retinal detachment may include one or all of the following: reduced vision and the sudden appearance of floaters and flashes of light. Contacting an eye specialist (ophthalmologist) right away can help save your vision.
For more information, consult Dr. Vaidya Eye Centre the Best Retina Specialist in Mumbai.
0 notes
Text
MEETSUN Blue Light Blocking Glasses, Anti Eye Strain Headache (Sleep Better),Computer Glasses UV400 Transparent Lens
MEETSUN Blue Light Blocking Glasses, Anti Eye Strain Headache (Sleep Better),Computer Glasses UV400 Transparent Lens
Price: (as of – Details) Product Description SAY GOODBYE TO EYESTRAIN & HEADACHES Why do we need the blue light filter glasses? Eye Strain Too much blue light exposure can cause eye strain, headaches, and blurred vision,affect your learning and working efficiency. Permanent Eye Damage Long term exposure to blue light has been linked to a greater risk for vision loss. Headaches Cause poor…

View On WordPress
0 notes
Text
Diabetic Retinopathy Treatment In Ghatkopar
Diabetic retinopathy is a form of eye disease caused by chronically high or variable blood sugar that is associated with diabetes. If left untreated, diabetic retinopathy can lead to vision loss and blindness. The condition develops slowly throughout many years; therefore, it is essential to undergo regular eye tests when you have Diabetes. Retinopathy is basically impaired blood vessels in the retina which is the thin inner light-sensitive layer situated in the back of the eyes. In some cases, these vessels will swell up (macular oedema) and leak fluid into the rear of the eye. In other cases, abnormal blood vessels will grow on the surface of the retina.
Diabetic retinopathy occurs in three stages:
Background retinopathy - Background retinopathy is said to occur if you have developed microaneurysms on your retina. Microaneurysms are when there is a swelling of the capillaries (very small blood vessels) that feed the retina. It is an early warning sign that your diabetes has lead to some damage of the small blood vessels of your retina.
Diabetic maculopathy - The macula is the part of the eye that helps to provide us with our central vision. Diabetic maculopathy is when the macula sustains some form of damage. One such cause of macular damage is from diabetic macular oedema whereby blood vessels near to the macula leak fluid or protein onto the macula.
Proliferative retinopathy - If a significant number of blood vessels on the retina become damaged, your body will respond by releasing a growth hormone known as Vascular Endothelial Cell Growth Factor (VEGF). The growth hormone stimulates the growth of new blood vessels. However, these new blood vessels are particularly weak and prone to leaking. Proliferative retinopathy is the body’s attempt to save its retina but it can often lead scarring of the retina and can cause the retina to detach, leading to blindness.
Symptoms
You might not have any signs of diabetic retinopathy until it becomes serious. When you do have symptoms, you might notice:
Loss of central vision, which is used when you read or drive
Not being able to see colors
Blurry vision
Holes or black spots in your vision
Floaters, or small spots in your vision caused by bleeding
Poor night vision
Risk factors
Anyone who has diabetes can develop diabetic retinopathy. Risk of developing the eye condition can increase as a result of:
Duration of diabetes — the longer you have diabetes, the greater your risk of developing diabetic retinopathy
Poor control of your blood sugar level
High blood pressure
High cholesterol
Pregnancy
Tobacco use
Being African-American, Hispanic or Native American
Detection and diagnosis of diabetic retinopathy
Diabetic retinopathy can be detected by undergoing a comprehensive eye examination that emphasizes on the evaluation of specifically the retina and macula. Such a test may include:
Visual acuity measurements – measuring a patient’s ability to see at different distances.
Patient history – to determine the presence of diabetes, vision impairments and other general health issues that may affect vision.
Tonometry – Measuring pressure within the eye.
Refraction – to establish whether a prescription for new glasses is required.
Pupil dilation – evaluation of eye structures, including assessment of the retina and optic nerve through a dilated pupil.
Supplementary testing may be required which include:
Retinal tomography or photography – In this test retina’s current status is documented.
Fluorescein angiography test - During this test, your doctor will inject a dye into your arm, allowing them to track how the blood flows in your eye. They’ll take pictures of the dye circulating inside of your eye to determine which vessels are blocked, leaking, or broken.
An optical coherence tomography (OCT) exam - It is an imaging test that uses light waves to produce images of the retina. These images allow your doctor to determine your retina’s thickness. OCT exams help determine how much fluid, if any, has accumulated in the retina.
Treatment
Treatment of diabetic retinopathy depends on the extent of the disease.
Eye Injections - Eye Medications called vascular endothelial growth factor (VEGF) inhibitors can be used to help stop the growth of new blood vessels and improve vision. Most people who receive these injections will need to get them for at least three months. Over time, some people may need to get them less often or may no longer need them at all, but others will need to continue in order to protect their vision.
Focal laser surgery - This surgery attempts to stop or reduce the leaking of blood or fluid into the eye by burning and sealing the damaged blood vessels.
Photocoagulation - This is usually done in your doctor’s office as an outpatient procedure during a single session. The procedure may or may not restore your vision to normal, but it should prevent your condition from worsening.
Scatter laser surgery - This surgery uses lasers to burn the damaged blood vessels so that they shrink. This procedure may require more than one application, and your vision may be blurry for a day or more after each session. You may also experience loss of peripheral vision or night vision after the procedure.
Vitrectomy - This surgery is done under general anesthesia and involves making a tiny incision in the eye to remove blood from the vitreous fluid, as well as any scar tissue that may cause retinal detachment.
Complications
Diabetic retinopathy involves the abnormal growth of blood vessels in the retina. Complications can lead to serious vision problems:
Vitreous hemorrhage - The new blood vessels may bleed into the clear, jelly-like substance that fills the center of your eye. If the amount of bleeding is small, you might see only a few dark spots (floaters). In more-severe cases, blood can fill the vitreous cavity and completely block your vision. Vitreous hemorrhage by itself usually doesn't cause permanent vision loss. The blood often clears from the eye within a few weeks or months. Unless your retina is damaged, your vision may return to its previous clarity.
Retinal detachment - The abnormal blood vessels associated with diabetic retinopathy stimulate the growth of scar tissue, which can pull the retina away from the back of the eye. This may cause spots floating in your vision, flashes of light or severe vision loss.
Glaucoma - New blood vessels may grow in the front part of your eye and interfere with the normal flow of fluid out of the eye, causing pressure in the eye to build up (glaucoma). This pressure can damage the nerve that carries images from your eye to your brain (optic nerve).
Blindness - Eventually, diabetic retinopathy, glaucoma or both can lead to complete vision loss.
How can I reduce my risk of Retinopathy?
You can reduce your risk of developing diabetic retinopathy, or help prevent it getting worse, by:
Controlling your blood sugar, blood pressure and cholesterol levels
Taking your diabetes medication as prescribed
Attending all your screening appointments
Getting medical advice quickly if you notice any changes to your vision
Maintaining a healthy weight, eating a healthy, balanced diet, exercising regularly and stopping smoking.
Tags~ cataract surgery in ghatkopar best eye specialist in ghatkopar Lasik Eye Surgery in Ghatkopar
0 notes
Text
Retinal Detachment Disorder Market Size, Share, Trends, Epidemiology and Market Forecast 2030
Retinal Detachment Disorder defines a condition wherein a thin layer of tissue (retina) at the back of the eye pulls far away from its ordinary position. Retinal Detachment Disorder separates the retinal cells from the layer of blood vessels that provides oxygen and nourishment. The longer Retinal Detachment Disorder goes untreated, the greater your risk of permanent vision loss inside the affected eye.

Retinal Detachment Disorder Causes
There are many causes of Retinal Detachment Disorder, but the most common causes are growing old or eye injury. There are three types of Retinal Detachment Disorder such as rhegmatogenous, tractional, and exudative. Each type happens due to a one-of-a-kind problem that causes your retina to move away from the back of your eye.
Retinal Detachment Disorder Signs and Symptoms
Retinal detachment disorder itself is painless. However, caution signs nearly seem before it occurs or has advanced, such as the sudden occurrence of many floaters — specks that appear to drift through your field of vision, flashes of light in one or both eyes, blurred vision, gradually diminished side (peripheral) vision, a curtain-like shadow over your visual field.
Retinal Detachment Disorder Epidemiology
Retinal detachment disorder is a common retina-associated disorder caused due to various factors and is more prevalent after the age of 50s. Retinal Detachment Disorder is more common among men as compared to women. In Europe, the highest number of Retinal Detachment Disorder was among males aged 60 to 79 years, whereas TRD was amongst females at the same age.
The Retinal traction detachment epidemiology has not been reported in large-scale studies, mainly because of its multifactorial etiology.
A study by Poulson et al. reported the incidence of primary Retinal Detachment Disorder In southern Denmark to be 1.25 per 100 000 inhabitants per year. In this study, out of all patients with RTD, 48.7% were male, and 51.4% were female. The median age was 59.3 years.
Retinal Detachment Disorder Treatment Options
Surgery is nearly constantly used to repair a retinal tear, hole, or detachment. Various techniques are available. Your eye care provider will consider treatment options with you. You may need a combination of treatments for the best outcomes. Treatments include Laser therapy or cryopexy (freezing), Pneumatic retinopexy, Scleral buckle, Vitrectomy.
Retinal Detachment Disorder Market
The Retinal Detachment Disorder market is segmented by product type, and by the end-user. The Retinal Detachment Disorder market is highly diversified with a huge number of products available in the market and the presence of major players such as Alcon Inc among others. The expanding prevalence of eye-associated disorders and the growing geriatric population are a few driving factors of the Retinal Detachment Disorder market.
Among 7MM countries, the United States accounts for XX% of the overall Retinal Detachment Disorder market size in 2019.
#retinal detachment disorder market#retinal detachment disorder market share#retinal detachment disorder market size#retinal detachment disorder market research report#retinal detachment disorder epidemiology#retinal detachment disorder pipeline#retinal detachment disorder key companies
0 notes
Text
Diabetic Retinopathy Treatment In Ghatkopar - Dr. Jatin Ashar
Diabetic retinopathy
is a form of eye disease caused by chronically high or variable blood sugar that is associated with diabetes. If left untreated, diabetic retinopathy can lead to vision loss and blindness. The condition develops slowly throughout many years; therefore, it is essential to undergo regular eye tests when you have Diabetes. Retinopathy is basically impaired blood vessels in the retina which is the thin inner light-sensitive layer situated in the back of the eyes. In some cases, these vessels will swell up (macular oedema) and leak fluid into the rear of the eye. In other cases, abnormal blood vessels will grow on the surface of the retina.
Diabetic retinopathy occurs in three stages:
Background retinopathy - Background retinopathy is said to occur if you have developed microaneurysms on your retina. Microaneurysms are when there is a swelling of the capillaries (very small blood vessels) that feed the retina. It is an early warning sign that your diabetes has lead to some damage of the small blood vessels of your retina.
Diabetic maculopathy - The macula is the part of the eye that helps to provide us with our central vision. Diabetic maculopathy is when the macula sustains some form of damage. One such cause of macular damage is from diabetic macular oedema whereby blood vessels near to the macula leak fluid or protein onto the macula.
Proliferative retinopathy - If a significant number of blood vessels on the retina become damaged, your body will respond by releasing a growth hormone known as Vascular Endothelial Cell Growth Factor (VEGF). The growth hormone stimulates the growth of new blood vessels. However, these new blood vessels are particularly weak and prone to leaking. Proliferative retinopathy is the body’s attempt to save its retina but it can often lead scarring of the retina and can cause the retina to detach, leading to blindness.
Symptoms
You might not have any signs of diabetic retinopathy until it becomes serious. When you do have symptoms, you might notice:
Loss of central vision, which is used when you read or drive
Not being able to see colors
Blurry vision
Holes or black spots in your vision
Floaters, or small spots in your vision caused by bleeding
Poor night vision
Risk factors
Anyone who has diabetes can develop diabetic retinopathy. Risk of developing the eye condition can increase as a result of:
Duration of diabetes — the longer you have diabetes, the greater your risk of developing diabetic retinopathy
Poor control of your blood sugar level
High blood pressure
High cholesterol
Pregnancy
Tobacco use
Being African-American, Hispanic or Native American
Detection and diagnosis of diabetic retinopathy
Diabetic retinopathy can be detected by undergoing a comprehensive eye examination that emphasizes on the evaluation of specifically the retina and macula. Such a test may include:
Visual acuity measurements – measuring a patient’s ability to see at different distances.
Patient history – to determine the presence of diabetes, vision impairments and other general health issues that may affect vision.
Tonometry – Measuring pressure within the eye.
Refraction – to establish whether a prescription for new glasses is required.
Pupil dilation – evaluation of eye structures, including assessment of the retina and optic nerve through a dilated pupil.
Supplementary testing may be required which include:
Retinal tomography or photography – In this test retina’s current status is documented.
Fluorescein angiography test - During this test, your doctor will inject a dye into your arm, allowing them to track how the blood flows in your eye. They’ll take pictures of the dye circulating inside of your eye to determine which vessels are blocked, leaking, or broken.
An optical coherence tomography (OCT) exam - It is an imaging test that uses light waves to produce images of the retina. These images allow your doctor to determine your retina’s thickness. OCT exams help determine how much fluid, if any, has accumulated in the retina.
Treatment
Treatment of diabetic retinopathy depends on the extent of the disease.
Eye Injections - Eye Medications called vascular endothelial growth factor (VEGF) inhibitors can be used to help stop the growth of new blood vessels and improve vision. Most people who receive these injections will need to get them for at least three months. Over time, some people may need to get them less often or may no longer need them at all, but others will need to continue in order to protect their vision.
Focal laser surgery - This surgery attempts to stop or reduce the leaking of blood or fluid into the eye by burning and sealing the damaged blood vessels.
Photocoagulation - This is usually done in your doctor’s office as an outpatient procedure during a single session. The procedure may or may not restore your vision to normal, but it should prevent your condition from worsening.
Scatter laser surgery - This surgery uses lasers to burn the damaged blood vessels so that they shrink. This procedure may require more than one application, and your vision may be blurry for a day or more after each session. You may also experience loss of peripheral vision or night vision after the procedure.
Vitrectomy - This surgery is done under general anesthesia and involves making a tiny incision in the eye to remove blood from the vitreous fluid, as well as any scar tissue that may cause retinal detachment.
Complications
Diabetic retinopathy involves the abnormal growth of blood vessels in the retina. Complications can lead to serious vision problems:
Vitreous hemorrhage - The new blood vessels may bleed into the clear, jelly-like substance that fills the center of your eye. If the amount of bleeding is small, you might see only a few dark spots (floaters). In more-severe cases, blood can fill the vitreous cavity and completely block your vision. Vitreous hemorrhage by itself usually doesn't cause permanent vision loss. The blood often clears from the eye within a few weeks or months. Unless your retina is damaged, your vision may return to its previous clarity.
Retinal detachment - The abnormal blood vessels associated with diabetic retinopathy stimulate the growth of scar tissue, which can pull the retina away from the back of the eye. This may cause spots floating in your vision, flashes of light or severe vision loss.
Glaucoma - New blood vessels may grow in the front part of your eye and interfere with the normal flow of fluid out of the eye, causing pressure in the eye to build up (glaucoma). This pressure can damage the nerve that carries images from your eye to your brain (optic nerve).
Blindness - Eventually, diabetic retinopathy, glaucoma or both can lead to complete vision loss.
How can I reduce my risk of Retinopathy?
You can reduce your risk of developing diabetic retinopathy, or help prevent it getting worse, by:
Controlling your blood sugar, blood pressure and cholesterol levels
Taking your diabetes medication as prescribed
Attending all your screening appointments
Getting medical advice quickly if you notice any changes to your vision
Maintaining a healthy weight, eating a healthy, balanced diet, exercising regularly and stopping smoking
Important Reminder: This information is only intended to provide guidance, not a definitive medical advice. Please consult eye doctor about your specific condition. Only a trained, experienced board certified eye doctor can determine an accurate diagnosis and proper treatment.
For more information or make an appointment for consultation with Dr. Jatin Ashar, please visit - https://www.mumbaieyecare.com/
Tag = eye specialist in Ghatkopar, Dry Eye Treatment In Ghatkopar, eye specialist in ghatkopar east, cornea surgery in ghatkopar, Child Eye clinic in ghatkopar
#eye specialist in Ghatkopar#Dry Eye Treatment In Ghatkopar#eye specialist in ghatkopar east#cornea surgery in ghatkopar#Child Eye clinic in ghatkopar
0 notes
Text
Original Levitra Tablets For Men`s In faisalabad |03000023915|
Levitra® Tablets Price in Pakistan PKR 2000/-
Levitra 20mg Tablets in Pakistan
Original Levitra Tablets EtsayDaraz.com Never walk away from sexual tension with Levitra 20 mg Tablets in Pakistan. You must have surely heard of many pills, which counteract the erectile dysfunction problems in the market. But did you know that almost all of those have been created using synthetic products which hinder the possibility of your sexual performance in the long run? Levitra Tablets in Pakistan ensures that you can pop the tablets whenever you find yourself sexually aroused without sparing a thought for other stimulants.
Levitra Tablets Price in Pakistan Levitra is one of the best sexual enhancement products which is imported by USA. And now available in Pakistan with low price. This is manufacturer to treat men sexual functions problem. Levitra Tablets Price in Pakistan The precious and natural herbs ingredient in LEVITRA works specifically on the chain of events that occurs in the penis during arousal. When two large chambers in a man’s penis fill with blood. Levitra Tablets in Pakistan If you see how a single tablet heightens your sexual desire in a few moments. Levitra Tablets Price in Pakistan Tablets balance your needs so that even a small dosage of 10 mg would be able to increase your stamina level throughout the entire night. Levitra Tablets Price in Pakistan Levitra is the combination with sexual stimulation that increasing blood flow to the penis to help a man get and keep an erection.
Levitra® 20mg (Vardenafil)
Levitra 20 mg Tablets in Pakistan: Your full evidence path to a thicker and firmer penis! Levitra 20mg Tablets in Pakistan adjusts your needs so that even a little measurement of 10 mg would have the option to help your stamina through the whole night. The phosphodiesterase type 5 inhibitors in these tablets actuates the blood stream to your penis during the hours of sexual movement. All said and done, this tablet would not bomb your trust once. The little bundling guarantees that you can convey it consistently without anybody monitoring your blameworthy mystery. Levitra Tablets in Pakistan The strength of the medication can be surely known whether you perceive how a solitary tablet increases your sexual want in no time flat. LEVITRA (vardenafil HCl) is a FDA-affirmed oral physician recommended prescription for the treatment of erectile brokenness (ED) in men. It has a place with a class of medications called "PDE5 inhibitors".Original Levitra Tablets in Pakistan It works by expanding blood stream to the penis to help improve erectile capacity. Usage of Levitra Tablets Vardenafil is utilized to treat male sexual capacity issues (ineptitude or erectile brokenness ED). In mix with sexual incitement, vardenafil works by expanding blood stream to the penis to enable a man to get and keep an erection. This medication doesn't ensure against explicitly transmitted ailments, (for example, HIV, hepatitis B, gonorrhea, syphilis). Levitra Timing Tablets in Pakistan Practice "safe sex, for example, utilizing latex condoms. Counsel your primary care physician or drug specialist for more subtleties. Step by step instructions to utilize Levitra Peruse the Patient Information Leaflet gave by your drug specialist before you start taking vardenafil and each time you get a top off. On the off chance that you have any inquiries, ask your primary care physician or drug specialist. Accept this prescription by mouth as coordinated by your primary care physician, generally as required. Take vardenafil, with or without nourishment, around 1 hour before sexual movement. Best Levitra in Pakistan Try not to take more than once day by day. Portions ought to be dismantled at any rate 24 hours. The measurements depends on your ailment, reaction to treatment, and different meds you might be taking. Make certain to educate your primary care physician and drug specialist concerning every one of the items you use (counting professionally prescribed medications, nonprescription medications, and home grown items). Abstain from eating grapefruit or drinking grapefruit juice while utilizing this drug except if your primary care physician or drug specialist says you may do so securely. Grapefruit can build the opportunity of symptoms with this prescription.Levitra Tablets in Karachi Approach your primary care physician or drug specialist for more subtleties.
Ingredients of Levitra Tablets: LEVITRA (vardenafil hydrochloride) is administered orally for the treatment of erectile dysfunction.Levitra Tablets in Islamabad This mono hydrochloride salt of vardenafil is a selective inhibitor of cyclic guanosine monophosphate (cGMP)-specific phosphodiesterase type 5 (PDE5).
Vardenafil HCl is designated chemically as piperazine, 1-[[3-(1,4-dihydro-5-methyl-4-oxo-7-propylimidazo[5,1-f][1,2,4]triazin-2-yl)-4-ethoxyphenyl]sulfonyl]-4-ethyl-, monohydrochloride and has the following structural formula: LEVITRA® (vardenafil hydrochloride) Structural Formula Illustration Vardenafil HCl is a nearly colorless, solid substance with a molecular weight of 579.1 g/mol and a solubility of 0.11 mg/mL in water. LEVITRA is formulated as orange, round, film-coated tablets with “BAYER” cross debossed on one side and “2.5”, “5”, “10”, and “20” on the other side corresponding to 2.5 mg, 5 mg, 10 mg, and 20 mg of vardenafil, respectively. In addition to the active ingredient, vardenafil HCl, each tablet contains microcrystalline cellulose, crospovidone, colloidal silicon dioxide, magnesium stearate, hypromellose, polyethylene glycol, titanium dioxide, yellow ferric oxide, and red ferric oxide Benefits of Levitra Tablets: Levitra Tablets Price In Pakistan balances your needs so that even a small dosage of 10 mg would be able to carry your stamina through the entire night. The phosphodiesterase type 5 inhibitors in these tablets activates the blood flow to your penis during the times of sexual activity. All said and done, this tablet would not fail your trust once.Levitra Tablets Price In Lahore The small packaging ensures that you can carry it at all times without anyone being aware of your guilty secret. Levitra Tablets in Pakistan The potency of the drug can be well understood if you see how a single Levitra Tablets Price In Islamabad heightens your sexual desire in a few moments. LEVITRA (vardenafil HCl) is an FDA-approved oral prescription medication for the treatment of erectile dysfunction (ED) in men. It belongs to a class of drugs called "PDE5 inhibitors". It works by increasing blood flow to the penis to help improve erectile function.The active ingredient in LEVITRA works specifically on the chain of events that occurs in the penis during arousal, when two large chambers in a man’s penis fill with blood.Levitra Pills Price In Pakistan
How Long Does It Take For Levitra To Take Effect?
About 30 Minutes How Long Does It Take Erectile Dysfunction Medication To Work? Viagra And Levitra Take About 30 Minutes To Work, And The Effects Last For About 4 Hours After You Take The Pill. You Should Take Cialis At Least 2 Hours Before You Plan To Have Sex.
What Are The Side Effects Of Taking Levitra?
Side-Effects of Levitra Tablets Headache, flushing, stuffy/runny nose, or dizziness may occur. Vision changes such as increased sensitivity to light, blurred vision, or trouble telling blue and green colors apart may also occur. If any of these effects persist or worsen, tell your doctor or pharmacist promptly.Levitra Tablets in Pakistan To reduce the risk of dizziness and lightheadedness, get up slowly when rising from a sitting or lying position.Levitra Tablets in Pakistan Remember that your doctor has prescribed this medication because he or she has judged that the benefit to you is greater than the risk of side effects. Many people using this medication do not have serious side effects.Sexual activity may put extra strain on your heart, especially if you have heart problems. If you have heart problems and experience any of these serious side effects while having sex, stop and get medical help right away: severe dizziness, fainting, chest/jaw/left arm pain, nausea.Levitra Tablets in Multan Rarely, sudden decreased vision, including permanent blindness, in one or both eyes (NAION) may occur.Levitra Tablets in Pakistan If this serious problem occurs, stop taking vardenafil and get medical help right away. You have a slightly greater chance of developing NAION if you have heart disease, diabetes, high cholesterol, certain other eye problems ("crowded disk"), high blood pressure, if you are over 50, or if you smoke. Rarely, a sudden decrease or loss of hearing, sometimes with ringing in the ears and dizziness, may occur. Stop taking vardenafil and get medical help right away if these effects occur.Levitra Tablets in Pakistan In the rare event you have a painful or prolonged erection lasting 4 or more hours, stop using this drug and get medical help right away, or permanent problems could occur.Levitra Tablets in Pakistan Get medical help right away if you have any very serious side effects, including: fast/irregular heartbeat, seizures, temporary memory loss. A very serious allergic reaction to this drug is rare.Levitra Tablets in Pakistan However, get medical help right away if you notice any symptoms of a serious allergic reaction, including: rash, itching/swelling (especially of the face/tongue/throat), severe dizziness, trouble breathing.This is not a complete list of possible side effects. If you notice other effects not listed above, contact your doctor or pharmacist. Precautions of Levitra Tablets In Pakistan: Prior to taking vardenafil, tell your primary care physician or drug specialist in the event that you are adversely affected by it;Levitra Tablets in Pakistan or on the off chance that you have some other sensitivities. This item may contain latent fixings, which can cause unfavorably susceptible responses or different issues. Converse with your drug specialist for more subtleties. Prior to utilizing this medicine,Levitra Tablets in Pakistan tell your primary care physician or drug specialist your therapeutic history, particularly of: heart issues, (for example, cardiovascular failure or dangerous unpredictable heartbeat in the previous a half year, chest torment/angina, cardiovascular breakdown), stroke in the previous a half year, kidney infection (dialysis), liver ailment, high or low circulatory strain, an extreme loss of body water (lack of hydration), penis conditions, (for example, angulation, fibrosis/scarring, Peyronie's illness), history of agonizing/delayed erection (priapism), conditions that may expand the danger of priapism, (for example, sickle cell paleness, leukemia, numerous myeloma), eye issues, (for example, retinitis pigmentosa, unexpected diminished vision, NAION), draining issue, dynamic stomach ulcers. Vardenafil may cause a condition that influences the heart cadence (QT prolongation). QT prolongation can seldom cause genuine (infrequently deadly) quick/unpredictable heartbeat and different side effects,Levitra Tablets in Pakistan (for example, serious unsteadiness, swooning) that need medicinal consideration immediately. The danger of QT prolongation might be expanded on the off chance that you have certain ailments or are consuming different medications that may cause QT prolongation. Prior to utilizing vardenafil, tell your PCP or drug specialist of the considerable number of medications you take and on the off chance that you have any of the accompanying conditions: certain heart issues (cardiovascular breakdown, slow heartbeat, QT prolongation in the EKG), family ancestry of certain heart issues (QT prolongation in the EKG, unexpected cardiovascular demise). Low degrees of potassium or magnesium in the blood may likewise build your danger of QT prolongation. This hazard may increment in the event that you utilize certain medications, (for example, diuretics/"water pills") or on the off chance that you have conditions, for example, serious perspiring, looseness of the bowels, or retching. Converse with your primary care physician about utilizing vardenafil securely. Levitra 20mg Tablets in Pakistan This medication may make you bleary eyed or cause vision changes. Liquor or pot (cannabis) can make you increasingly woozy.Original Levitra 20mg Tablets in Pakistan Try not to drive, use hardware, or do whatever necessities readiness or clear vision until you can do it securely. Breaking point mixed refreshments. Converse with your primary care physician on the off chance that you are utilizing weed (cannabis). Before having medical procedure,Original Levitra 20mg Tablets in Bahawalpur enlighten your primary care physician or dental specialist regarding every one of the items you use (counting doctor prescribed medications, nonprescription medications, and natural items). More established grown-ups might be increasingly touchy to the reactions of this medication, particularly QT prolongation (see above). This medicine isn't generally utilized in ladies.Levitra Tablets in Pakistan Accordingly, it is probably not going to be utilized during pregnancy or bosom sustaining. Counsel your primary care physician on the off chance that you have any inquiries regarding this medicine.
0 notes