#self administered serotonin
Explore tagged Tumblr posts
Text



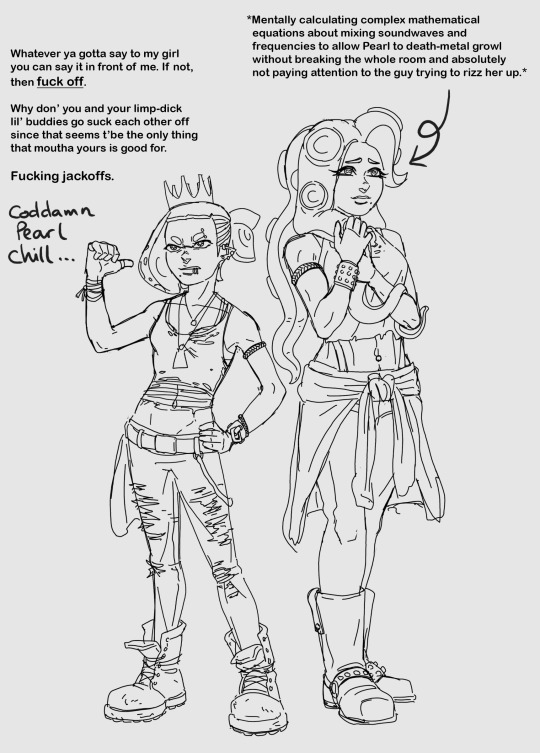



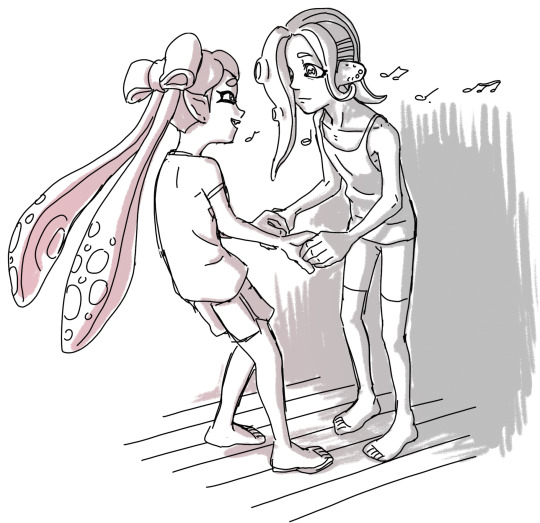
They're supposed to be monochrome, but I still put them in so much color...
I couldn't decide how to color the background, so I did a clean version and a colored version which makes them look like they're at a disco.
Eight, once they find out Iso Padre made it to the surface, is so excited to introduce him to her friends.
As for Acht, Marina introduces them to Callie as a roomate to help them adjust to the surface after being trapped in the Deep Sea Metro for so long. Callie discovers that gently singing to Acht is the best way to coax them to come to breakfast.
#splatoon#pearlina#pearl houzuki#marina ida#off the hook#side order#agent 8#callie cuttlefish#acht mizuta#acht dedf1sh#iso padre#frye onaga#my art#self administered serotonin
2K notes
·
View notes
Text
[Transcript] Fallen Angels
FALL OUT BOY'S ULTRA-AMBITIOUS NEW ALBUM WILL MAKE THEM ONE OF THE WORLD'S BIGGEST BANDS. SO HOW COME PETE WENTZ IS STILL SO DEPRESSED?
source: x the other page missing ;-;
2007 Kerrang! No.1142

PETE WENTZ is an hour late.
Because of this the first thing you learn about Fall Out Boy is that nothing happens without him. His three other bandmates - singer and guitarist Patrick Stump, guitarist Joe Trohman and drummer Andy Hurley - sit waiting. They're in a conference room on the first floor of the Marriott Hotel in Lowell, Massachusetts, a pretty, vanilla flavoured town 60 minutes north of Boston. The reason the group are here is because in three hours they're due to play four songs in front of 8,000 people gathered to watch the local radio station's Christmas concert. But first they're forced to wait. Because picturing Fall Out Boy without Pete Wentz is like imagining a motorway without traffic.
"See, that's not right," says Patrick Stump. Stump is wearing a small frown and an indulgent smile. It's been said that he has no ego. As you hear him now he's checking out his own entry page on Wikipedia. "No, see, they've got that wrong...
We don't have much time. Fall Out Boy landed at Roston's Logan airport at 4pm. This lunchtime they were in Chicago; by dawn they'll be in Manhattan. The band's ride pulled up in Lowell an hour ago. It's now 6:30. At 9:25, they're due onstage. Before that they need to pose for photographs and answer questions.
"Pete's in his room," someone says. Andy Hurley goes downstairs to the toilet, taking a security guard with him. Fall Out Boy have two security men: one for Pete Wentz, one for the others.
Wentz calculates that he spends 40 minutes out of every hour on the phone. He receives up to a 100 emails a day. He owns a film production company. He's a published author. He owns his own record label. He owns his own clothing line. He's modelled for Gap. He'd be modelling for us if he could be bothered to be here.
But Pete is in his room, laid low with depression. He's sat on the floor "calling random people from [his] home town [Wilmette, Illinois]", people whom he believes will "understand [him]". Problem is, when they pick up the phone he "can't think of a thing to say". All the while it's getting later and later. He feels self-conscious about how to time his entry, aware that he might be thought of as "the asshole American guy in a band". Even now, two and a half hours later, these feelings are still resident in his mind. "It's weird," he'll say. "Although I'm functioning, half of my head is in another place.
Do you see how people might look at you, see your wealth and your privilege and your opportunities, and think: you ungrateful son of a bitch?
"Of course," he says. "I think that all the time. But you asked me about depression and so I'm talking about it. It's the culture we live in."
You don't seem to mind talking about it. "The only problem I have with it is that I don't want people to read this article and go, 'lt'd be so amazing to be depressed! That'd be cool!'. I don't want to create an industry of misery."
These days, Pete Wentz has prescriptions for Xanax, Praxil, Prozac and Ativan. To compliment this, he's taking serotonin reuptake inhibitors (more anti-depressants). In the past, he's been administered anti psychotics. If Wentz were to die tomorrow his coffin would need to be fitted with a child-proof lid.
"Sorry I'm late," he says, entering the conference room, shaking hands. "I'll be your self-conscious rock star for the day." Paul Harries, Kerrang!'s photographer, tells the bassist that we don't have much time. Pointing the lens at his face he tells him it'll need to see his full repertoire of poses. The subject understands precisely what the photographer means, and as the flash lights zap before him he gives him just that. The camera loves Pete Wentz, even if at the moment Pete Wentz hates himself.
He's depressed. You'd never know.
"NOT TO beat up on the press," says Joe Trohman. "But they do tend to take one look at our band and and say, Pete Wentz is Fall Out Boy." Trohman is answering a question as to whether it grates on his nerves that the band's bass player is the one who garners most of the public attention. "Not at all, no. Pete is the public face of the band because we want him to be the public face of the band.
Would you be screwed without him?
61 notes
·
View notes
Text
Psychedelics, Ketamine, and MDMA in the Treatment of Mental Health Disorders
Abstract: Mental illness is a serious and widespread issue affecting approximately 59.3 million adults in the US alone. Many more around the world suffer from it, with many cases going undiagnosed and untreated.
This paper aims to discuss alternative treatment methods for three mental health diagnoses that all involve depressive symptoms: major depressive disorder, post-traumatic stress disorder, and borderline personality disorder. Major depressive disorder has very high prevalence rates around the world, namely in America, with more than 8% of American adults being diagnosed with it each year—that’s 21 million people.
SSRI (selective serotonin reuptake inhibitor) antidepressants are the most common course of treatment for major depressive disorder. SNRI’s (selective norepinephrine reuptake inhibitors) are also prescribed when necessary. The problem with these medications is that they take quite a while to reach full effect. One of the most commonly prescribed SSRI’s is sertraline, better known by its brand name Zoloft. It needs 4 to 6 weeks to “build up” in the system enough to become fully therapeutic. This range is also true for other antidepressants. Now imagine there was a way to quickly alleviate symptoms much more dramatically than previously seen with traditional psychiatric medication. Instead of up to 6 weeks, imagine it could work instantly and markedly. We don’t have to imagine; the future of treatment-resistant depression is here, and it comes in an unconventional (and to some, controversial) form. Esketamine (administered as a nasal spray under the brand name Spravato), lysergic acid (LSD), MDMA (3,4-methylenedioxymethamphetamine), and psilocybin found in “magic mushrooms”—all of these have one thing in common: they can treat certain mental illness. When administered professionally in a clinical setting at a therapeutic dose, these substances can have profound and lasting positive effects on mental health. According to a clinical trial done by Charles Raison et al., 2023, “Psilocybin treatment was associated with a clinically significant sustained reduction in depressive symptoms and functional disability, without serious adverse events. These findings add to increasing evidence that psilocybin-when administered with psychological support-may hold promise as a novel intervention for MDD.” The concept of the brain being malleable aligns with these findings. Because of neuroplasticity, these alternative treatment options “…appear to work by encouraging the growth of new connections between neurons in the brain,” according to the National Institutes of Health, 2023. This is promising not only for MDD, but PTSD as well. Psychedelics can decrease amygdala reactivity during emotion processing, which may reverse the heightened amygdala reactivity typically observed in PTSD. Furthermore, we see positive results in the clinical trials that have been conducted thus far.
How Psychedelics Affect the Brain
Psychedelics offer a novel way to treat mental health disorders in patients who are not responding to other treatment options. It is more powerful than traditional psychiatric medication, and could set the stage for recovery. A person could undergo psilocybin-assisted therapy and then start a regimen of psychiatric medication as “maintenance”. The psilocybin would’ve just provided that initial “push” to promote neuroplasticity. Typically, the brain creates strong repetitive thought patterns as a defense mechanism against unpleasant events, including psychological trauma. Some individuals might develop a trauma response to certain stimuli. Without processing the trauma, the brain may create a defense mechanism in the form of a deeply ingrained habit. One such habit may be to “check” objects over and over again in an attempt to self-soothe (commonly seen in obsessive-compulsive disorder), or to always avoid the offending stimuli, at any cost. It will protect the body from perceived danger and alleviate anxiety in the short-term; however, now the body has a normative thought pattern to obsessively “check” certain objects or to be extremely avoidant of certain situations. Psilocybin turns these processes off, so to speak. It blocks the synapses in that part of the brain. Once it’s turned off, the active mind can begin forming new beliefs, potentially even processing the trauma. This takes advantage of neuroplasticity and quickens the process of creating new healthy thought patterns. The patient could then continue to work on their recovery in psychotherapy.
Researchers have found that “psilocybin temporarily disrupts a brain network involved in creating a person's sense of self. The findings help explain the neurobiology of psychedelic experiences and give insight into harnessing the potential therapeutic effects of psychedelic drugs.” (National Institute of Health, 2024). Moreover, a single dose of psilocybin “can cause acute distortions of space–time perception and ego dissolution, producing rapid and persistent therapeutic effects in human clinical trials. In animal models, psilocybin induces neuroplasticity in cortex and hippocampus.” (Siegel et al, 2024).
Furthermore, low doses of ketamine have been shown to improve depression in patients with MDD. Spravato (esketamine) is a nasal spray administered clinically twice a week during weeks 1-4 in the induction phase. Following that, maintenance treatment is once weekly during weeks 5-8, and then finally, every 2 weeks or once weekly from week 9 forward. Esketamine is a part of ketamine. Ketamine has two components called enantiomers that can be used to achieve different outcomes. The esketamine component is thought to be more effective for treating depression, which is why doctors use the esketamine formulation known as Spravato. The complete mechanism of action of esketamine is unknown. Clinical studies have shown that it helps treat depressive symptoms by targeting different neural receptors in the brain, not unlike traditional psychiatric medication. However, it has been shown to be more effective than traditional medication alone. It targets opioid receptors; some research suggests that activation of opioid receptors is partially involved in ketamine’s and esketamine’s antidepressant effect. It also targets the NMDA (N-methyl-D-asparate) receptor, which manages synaptic plasticity (keeping your synapses pliable and able to retain information). Ketamine and esketamine block NMDA receptors in the brain and thereby increase levels of glutamate, the most abundant chemical messenger in the brain. Blocking NMDA receptors also activates AMPA receptors to release other molecules that help brain cells communicate with each other along new pathways. Known as synaptogenesis, this process likely affects mood, thought patterns, and cognition, including memory. And finally, AMPA (Alpha-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid) receptor is also targeted. This receptor also uses glutamate, similarly to the NMDA receptor. The AMPA receptor manages and mediates fast-acting synaptic activity, such as memory and learning abilities. AMPA receptor abnormalities can contribute to mental and behavioral health disorders.
Adverse Effects
These drugs substantially alter brain activity, so there’s a possibility they could cause seizures in someone who has epilepsy. With Spravato, common side effects are nausea, hypertension, dizziness, and sedation. Sometimes dissociation (depersonalization and derealization) can also occur, as ketamine (of which esketamine is derived) belongs to a class of substances called “dissociatives”. As for psilocybin, there were research findings that showed “A minority of participants in the psilocybin and escitalopram conditions showed clinically significant symptom-worsening (9.7% and 10.3%, respectively),” according to Otto Simonsson et al., 2023. Escitalopram (brand name Lexapro) is one of those aforementioned SSRI’s. It is common for traditional antidepressant medication to be prescribed alongside the psychedelic-assisted therapy. So, some individuals did indeed react negatively to the treatment.
Specifically in borderline personality disorder, will the treatment of depressive symptoms with MDMA lead to the worsening of other BPD symptoms such as intense, inappropriate outbursts of anger? If the person with BPD had comorbid bipolar disorder, would the MDMA treatment trigger mania or hypomania? “Despite extensive research showing evidence that treatment for borderline personality disorder (BPD) is effective, almost half of BPD individuals will never fully recover over their lifetime.” (Videler et al., 2019). Thus, the need for adjunct treatment is important, as dialectical behavioral therapy on its own is not enough for some individuals. BPD is a serious mental health condition that requires intensive treatment, and the use of alternative treatment proves promising. However, we must address the question of if MDMA in particular could worsen some of the symptoms of BPD. The studies are very new, and not a lot of data has been recorded yet. It could be hypothesized that other symptoms of BPD could worsen, but the depressive symptoms would most likely greatly improve. According to Traynor et al., “…researchers have also found MDMA-AP–related changes in personality structure by way of decreased neuroticism and increased openness, which are two personality traits shown to have significant genetic correlations with borderline personality disorder in a recent study.” Also mentioned by Traynor et al. is the suggestion to add specific interventions so that the experience will be a positive one. “Additionally, similar to the structure of interventions for comorbid borderline personality disorder and PTSD (in which patients are taught skills to support adequate experiential immersion into exposures), skills to cope with avoidance behaviors, impulsive urges, suicidal ideation, and dissociation (e.g., mindfulness, distress tolerance, and anti-dissociation skills) may be taught before MDMA dosing sessions to support immersion into the experience and to cope with any distress that may arise.” It’s also important to note that MDMA is one of the few drugs that acts on oxytocin, which is the bonding “love” hormone produced by skin contact or sex. Those with BPD have been demonstrated to have very low levels of oxytocin, which might partially explain their pronounced issues with attachment and relationships. Oxytocin is what binds mothers to their infants, and it is thought that the brains of those with BPD do not properly regulate it because of past psychological trauma (trauma which often contributes majorly to the development of BPD). Also of note is that “MDMA’s effects on neurotransmission have been well characterized both in rodents and in humans as promoting neurotransmitter release, inhibiting monoamine reuptake transporters, acting directly or indirectly upon downstream receptors, and modulating several neurohormones, all contributing to its characteristic subjective and physiological effects.” (Zaretsky et al., 2023). We can see how this “neurotransmitter release” would promote better overall mood, leading to the diminished effect of things like depression, lack of motivation, and anhedonia.
Long-term positive effects
The medical literature has demonstrated that the positive effects of these treatments are long-lasting. According to the McLean Hospital, “Participants in psychedelic therapy trials have reported positive effects that have lasted long after treatment ended.” This information was pulled from a prospective 12-month follow-up study demonstrating the lasting positive effects. “Significant, large-magnitude, and sustained decreases in depression from pretreatment across the five follow-up assessments occurred with the two patient-rated depression assessment questionnaires (QIDS and BDI-II). (Gukasyan et al, 2022). A graph of the findings is shown below:

At the 12-month mark, using the BDI-II depression rating scale, remission rate for participants was at 75%. That is clinically significant. Using the QIDS, the remission rate was at 67%.
As for safety: According to Gukasyan et al, “Although psilocybin treatment of MDD appears promising, little is known about long-term efficacy and safety.” This means that over the course of the next few years, we will see more conclusive data emerge as clinical trials continue and more medical information is found.
With regard to borderline personality disorder and MDMA, not enough data has been collected to conclusively say that the positive effects are long-lasting. Conversely, not enough information has been found on adverse effects.
The Biological Basis of Mental Illness
What, then, causes these depressive symptoms, biologically speaking? Which neurotransmitters are involved in creating purported “chemical imbalances”?
Well, “The monoamine-deficiency theory posits that the underlying pathophysiological basis of depression is a depletion of the neurotransmitters serotonin, norepinephrine or dopamine in the central nervous system.” (Hasler, 2010). In particular, the serotonin receptors are classified as whole as “5HT”. There are subsets such as 5HT-A and 5HT-2. Sertraline, better known as Zoloft like we mentioned earlier, can cause desensitization of the 5HT-2 receptor, thereby altering brain chemistry, as a prolonged influx of serotonin can cause this desensitization. Then there’s dopamine levels. According to the Cleveland Clinic, “Dopamine is associated with rewards and motivation, while serotonin is associated with happiness, focus, and calmness. Dopamine and serotonin share involvement in some mental health conditions, including depression and mood disorders.” “Dopamine receptors are a variety of receptors that can either increase or decrease cyclic adenosine monophosphate levels in the brain. They are classified into different subtypes as well, including D1, D2, D3, D4, and D5 receptors.” (Perez de la Mora, 2020). Finally, we have norepinephrine, which also plays a role in depression, hence why we have SNRI medications to treat depression symptoms as well as SSRI’s. These neurotransmitters being dysregulated has been long-believed to be the cause of most mental health disorders.
Conclusion
These alternative treatment methods play on these key receptors, but in much different ways than traditional psychiatric medication, and can produce much quicker results; some instantaneously. Because of this instant effect, the social attitude is shifting toward these “unconventional” methods. They usher in an age of hope for those with mental health conditions such as major depressive disorder, post-traumatic stress disorder, and borderline personality disorder. The research will only grow from here.
References:
Fuentes, J. J., Fonseca, F., Elices, M., Farré, M., & Torrens, M. (2020). Therapeutic Use of LSD in Psychiatry: A Systematic Review of Randomized-Controlled Clinical Trials. Frontiers in psychiatry, 10, 943. https://doi.org/10.3389/fpsyt.2019.00943
Gukasyan N, Davis AK, Barrett FS, et al. (2022). Efficacy and safety of psilocybin-assisted treatment for major depressive disorder: Prospective 12-month follow-up. Journal of Psychopharmacology. 2022;36(2):151-158. https://doi.org/10.1177/02698811211073759
Hasler G. (2010). Pathophysiology of depression: do we have any solid evidence of interest to clinicians? World psychiatry: official journal of the World Psychiatric Association (WPA), 9(3), 155–161. https://doi.org/10.1002/j.2051-5545.2010.tb00298.x
Inouye, A., Wolfgang, A., & Philhower, L. (2024). MDMA-assisted dialectical behavioral therapy for borderline personality disorder: A qualitative study of mental health clinicians. Journal of Psychedelic Studies. 8(1), 92–105.
Molla, H., Lee, R., Lyubomirsky, S., & de Wit, H. (2023). Drug-induced social connection: Both MDMA and methamphetamine increase feelings of connectedness during controlled dyadic conversations. Nature News. https://www.nature.com/articles/s41598-023-43156-0
Perez de la Mora, M. Hernandez-Mondragon, C., Crespo-Ramirez, M., Rejon-Orantes, J., O. Borroto-Escuela, D., Fuxe, K.
Conventional and Novel Pharmacological Approaches to Treat Dopamine-Related Disorders: Focus on Parkinson’s Disease and Schizophrenia.
Neuroscience.
Volume 439, 2020,
Pages 301-318,
ISSN 0306-4522,
https://doi.org/10.1016/j.neuroscience.2019.07.026.
Raison, C. L., Sanacora, G., Woolley, J., Heinzerling, K., Dunlop, B. W., Brown, R. T., Kakar, R., Hassman, M., Trivedi, R. P., Robison, R., Gukasyan, N., Nayak, S. M., Hu, X., O'Donnell, K. C., Kelmendi, B., Sloshower, J., Penn, A. D., Bradley, E., Kelly, D. F., Mletzko, T., Griffiths, R. R. (2023). Single-Dose Psilocybin Treatment for Major Depressive Disorder: A Randomized Clinical Trial. JAMA, 330(9), 843–853. https://doi.org/10.1001/jama.2023.14530
Simonsson, O., Carlbring, P., Carhart-Harris, R., Davis, A. K., Nutt, D. J., Griffiths, R. R., Erritzoe, D., & Goldberg, S. B. (2023). Assessing the risk of symptom worsening in psilocybin-assisted therapy for depression: A systematic review and individual participant data meta-analysis. Psychiatry research, 327, 115349. https://doi.org/10.1016/j.psychres.2023.115349
Siegel, J.S., Subramanian, S., Perry, D. et al. Psilocybin desynchronizes the human brain. Nature 632, 131–138 (2024). https://doi.org/10.1038/s41586-024-07624-5
Traynor, J. M., Roberts, D. E., Ross, S., Zeifman, R., & Choi-Kain, L. (2022). MDMA-Assisted Psychotherapy for Borderline Personality Disorder. Focus (American Psychiatric Publishing), 20(4), 358–367. https://doi.org/10.1176/appi.focus.20220056
Vargas M.V., Dunlap L.E., Dong C, Carter S.J., Tombari R.J., Jami S.A., Cameron L.P., Patel S.D., Hennessey J.J., Saeger H.N., McCorvy J.D., Gray J.A., Tian L, Olson D.E. (2023). Psychedelics promote neuroplasticity through the activation of intracellular 5-HT2A receptors. Science. Feb 17;379(6633):700-706. https://doi.org/10.1126/science.adf0435
Videler, A. C., Hutsebaut, J., Schulkens, J. E. M., Sobczak, S., & van Alphen, S. P. J. (2019). A life span perspective on borderline personality disorder. Current Psychiatry Reports, 21(7), 51. https://doi.org/10.1007/s11920-019-1040-1.
Zaretsky, T. G., Jagodnik, K. M., Barsic, R., Antonio, J. H., Bonanno, P. A., MacLeod, C., Pierce, C., Carney, H., Morrison, M. T., Saylor, C., Danias, G., Lepow, L., & Yehuda, R. (2024). The Psychedelic Future of Post-Traumatic Stress Disorder Treatment. Current neuropharmacology, 22(4), 636–735. https://doi.org/10.2174/1570159X22666231027111147
#heeeere is another one of my papers I've written#I plan to add more even though I already turned it in and the semester's over lol. but...I like it so far#mental health#mental illness#txt
6 notes
·
View notes
Text
Is Ibogaine Safe? Separating Myth from Medical Facts

Is Ibogaine safe? This article dives into the facts behind Ibogaine Treatment, dispelling the common myths and highlighting the real medical benefits of Ibogaine Treatment— particularly when administered in a medically safe clinical environment. Discover how ibogaine offers a powerful path to healing addiction and trauma at the root.
When it comes to treating todays powerful addictions and mental health conditions, many are searching for a more effective and comprehensive solution t outdated traditional methods. They are seeking something deeper—a therapy that delves inwardly to address the root causes of their suffering. Enter Clinical Ibogaine Treatment, an alkaloid found in the Tabernanthe Iboga plant of Western Africa.
But as promising as Ibogaine may sound, improper administration of the molecule has surrounded it by controversy, confusion, and conflicting opinions. Is it as effective as some clinic’s claim? Is it dangerous? Or is it somewhere in between?
In this article, we’ll separate myths from medical facts and take an honest look at the Benefits Of Ibogaine Treatment, how it works to generate neuroplasticity in the brain and reduce or eliminate withdrawal symptoms and cravings, and, most importantly, whether ibogaine is safe.
Understanding Ibogaine: What Is Ibogaine, Really?
Ibogaine is a naturally occurring psychoactive compound with the molecular formula C20H26N2O. It is derived from the root bark of the Tabernanthe iboga plant native to Western Africa and has been traditionally used for centuries by the Bwiti tribal people for ceremonial healing and rite of passage purposes. Over the last many years, ibogaine has gained attention in the Western world for its powerful ability to interrupt addiction cycles—and has been particularly touted for its impressive ability to eliminate, or drastically reduce, acute and post-acute withdrawal systems connected to opioid addiction. Ibogaine has also show high effectiveness at treating alcohol dependency as well as addictions to stimulants.
Unlike traditional medications that often require repetitive and structured use, Ibogaine Treatment is dosed in a single-session. During the treatment, individuals enter a deep, introspective state—often described as a waking dream—where they process traumas, repressed emotions, and gain insight into the roots of their drug and/or alcohol use. Ibogaine metabolizes through the liver into its active metabolite “Noribogaine” (also known as 12-hydroxyibogamine). Noribogaine remains in the body for for a prolonged period, typically 8-16 weeks, and serves as a strong serotonin reuptake inhibitor that helps to stabilize brain chemistry, produce mood stabilizing effects, and stifle cravings for drugs and alcohol. This two to four months following ibogaine treatment provides a crucial window of opportunity for the patient to deeply assess their past drug and/or alcohol use and learn and implement new strategies, lifestyle choices, and behaviors that support long-term sustainable recovery.
The Benefits of Ibogaine Treatment vs. Traditional Detox
One of the most compelling benefits of Ibogaine Treatment is its ability to reduce or even fully eliminate withdrawal symptoms during detox. For individuals coming off of opioids, this is a major game-changer.
But the benefits go well beyond the physical detox. Ibogaine has been shown to:
• Interrupt addictive thought patterns by resetting the brain’s reward system
• Drastically reduce cravings and compulsive behaviors
• Shift the patients perspective in how they view and process trauma and emotional pain
• Create deep psychological insights and restored self-awareness
• Encourage spiritual renewal and purpose
People often describe feeling as if they’ve experienced several years of emotional psychotherapy in a single treatment session. However, as extraordinary as ibogaine may sound to many, questions and myth’s regarding safety have trailed closely behind and hampered ibogaines progress into mainstream medical practice.
Myth #1: Ibogaine Is Just A Dangerous Psychedelic
Fact: Ibogaine is not a drug that can or would be desired to be used recreationally in any way. Unlike substances such as LSD and psilocybin, Ibogaine is used 100% medicinally and properly administered within a structured clinical setting with a strong therapeutic focus.
While Ibogaine is indeed considered the most powerful of all hallucinogens, at clinic’s such as the Avante Ibogaine Institute, patients are placed under strict cardiac monitoring by trained professionals. Furthermore, pre-treatment clinical assessments, lab work and EKG’s are performed at the Avante Ibogaine Institute to ensure patient candidacy and preparedness prior to treatment. When these proper clinical protocols are followed, the risks are significantly minimized if not eliminated.
Myth #2: Ibogaine Is Too Risky to Be Considered Safe
Fact: Like any powerful medical intervention, Ibogaine does come with risks—particularly given that many patients have experienced extended terms of chronic drug and alcohol abuse. Certain individuals with heart conditions, liver issues, or pre-existing mental health disorders may not qualify for treatment.
However, these risks are well-documented and manageable when appropriate safety screenings are performed. In fact, when done correctly, Ibogaine Treatment is safer than many long-term prescription drug protocols used in conventional addiction treatment—many of which come with their own list of side effects, dependency issues, and limited long-term results.
Myth #3: There’s No Scientific Evidence Behind Ibogaine
Fact: Research on Ibogaine is ongoing and growing rapidly. While it’s not yet approved for use in the United States, studies from Europe, Mexico, Brazil, and New Zealand have shown promising results and Texas passed a $50 million research bill on June 11, 2025 to further investigate the flood of anecdotal evidence that has been reported by the Avante Ibogaine Institute and other reputable clinical ibogaine providers over the past decade and beyond.
Some key findings include:
• Significant reduction in withdrawal symptoms and cravings
• Far lower relapse rates compared to traditional rehab
• Improved mood and mental clarity in patients with PTSD and depression
• Increased neuroplasticity and stimulation of brain growth factors
Ibogaine is also being studied for its potential in treating traumatic brain injuries, PTSD, and other neurological disorders—adding to the expanding list of benefits of Ibogaine Treatment.
What Makes Ibogaine Treatment Safe?
At the Avante Ibogaine Institute, safety is the top priority. The facility follows strict medical protocols before, during, and following treatment to ensure the patient’s optimal safety, treatment effectiveness, and overall well-being.
Here’s how the Avante Ibogaine Institute keeps the Ibogaine treatment process safe:
• Comprehensive medical screening: Pre-Treatment cardiac evaluations (EKG), liver function, blood work, and psychological assessments
• On-site medical supervision: Medical Professionals (Physicians and ACLS nurses) monitor patients 24/7 during treatment
• Controlled dosage: Ibogaine is administered in carefully measured doses, specific to each patient’s medical profile and safety tolerance level
• Post-treatment integration: Emotional supportive therapy helps patients to process and apply their clinical ibogaine experience
This level of care is crucial to the safety and effectiveness of the experience.
Who Should NOT Take Ibogaine?
While Ibogaine can offer tremendous benefits, it’s not right for everyone. People with the following conditions are generally not considered candidates:
• Heart arrhythmias or cardiovascular disease
• Liver failure or severe hepatic conditions
• Psychiatric conditions such as schizophrenia
• Active suicidal ideation
• Use of certain prescription medications that Avante’s clinical assessment finds may be toxic or interact negatively with Ibogaine
• Pregnant women
When considering clinical ibogaine treatment, proper screening is paramount to success and choosing a reputable ibogaine treatment clinic such as the Avante Institute is essential.
Separating the Truth from the Hype
Ibogaine is not a magic pill, and it’s not without risks. However, it is one of the most promising therapeutic tools available for individuals who are determined to end a dependency on drugs or alcohol. Clinical Ibogaine Treatment is also highly beneficial for those suffering from PTSD and depression as it offers deep healing—both physical and emotional—that many traditional treatments fail to deliver.
It's also important to remember that Ibogaine is just one part of the journey. Integration therapy, lifestyle changes, and ongoing support are vital to making the transformation last.
Conclusion: Is Ibogaine Safe? Yes—When Done the Right Way
To answer the question simply: Yes, Ibogaine Treatment is a safe and effective therapy when administered in the proper setting, under professional medical care, and with proper pre-treatment screening.
When it comes to treating addiction, PTSD, and trauma at the root level—not just the symptoms—The Benefits of Ibogaine Treatment are hard to ignore. For those seeking lasting change, it offers not only hope but a truly transformative path forward.
If you or someone that you care about is struggling, it may be time to look beyond the surface and contact with Avante Ibogaine Institute —and explore a deeper way to heal with clinical ibogaine treatment.
1 note
·
View note
Text
The Transformational Journey of an Ayahuasca Ceremony: Unlocking the Mind
Ayahuasca, a sacred drink derived from plants that is used for spiritual awakening and healing, has been used to administer the indigenous ceremonies in the Amazon. Many seekers have turned to shamanic retreats in search of firsthand experience with the profound effects of psychedelic therapy because of the growing interest in holistic psychedelic therapy. The purpose of this article is to discuss what an Ayahuasca ceremony is, the science behind its use, and the outcomes that attendees should anticipate.
What is the Ayahuasca ceremony?
The consumption of a potent beverage made by Amazonian indigenous people from the Ayahuasca vine, Psychotria viridis leaves, and DMT in an Ayahuasca ceremony is a traditional healing practice. Typically, this spiritual journey is led by a shaman. At this ceremony, everything has been planned to take its time, including calming the mind for extended reflection, healing, and immediate personal development.
Participants are expected to get rid of any negative or haunting experiences that might affect their growth by going through such vivid examples and emotional evaporation. In point of fact, it has evolved into a sacred ceremony, and right now, attention is being paid to these relatives who possess healing power and the potential for spiritual insight.
The Scientific Basis for Psychedelic Treatment
Through evidence of its efficacy as a treatment for mental health disorders, ayahuasca therapy has received significant scientific validation. Ayahuasca's active ingredient, DMT, links serotonin receptors in the brain and prompts an investigation into a clearly defined emotional environment.
Through increased neuroplasticity and an experience of connectedness with other people, research suggests that Ayahuasca can lessen symptoms of depression, PTSD, and addiction. As a result, its growing role in the integration of psychedelics and therapy has earned it the right to provide psychological healing.
What a Shamanic Retreat Does
In many people's minds, an Ayahuasca ceremony is the option for profound healing and personal development that can be found in shamanic retreats that provide an authentic and controlled environment. These retreats make ritual, intention, and setting a big deal, making it safe and meaningful to travel.
To encourage openness, participants frequently adhere to dietary restrictions and meditate. Support, emotional healing, and integration practices help people process their experiences within the framework of the retreat.
What to Expect During the Ayahuasca Experience
Every person who participates in the Ayahuasca ceremony has a unique experience because of the highly personal nature of the experience. The visions may include vivid imagery or profound reflections on life and existence. Deep feelings and repressed traumas can be brought to light for healing.
Common physical effects include nausea and vomiting, which is thought to be a form of purging or cleansing from negative energies and a release of them. However, once purging stops, we experience permanent transformation, inner peace, and increased awareness.
Conclusion
There is a lot more to an Ayahuasca ceremony than just getting high. Opportunities for serious personal development are presented by the spiritual and therapeutic aspects. One can safely and purposefully navigate this powerful ritual with the assistance of the shamanic retreat. Ayahuasca presents a real opportunity for self-healing and discovery, with research confirming its benefits. The few attracted to embracing its transformative power should consider a well-guided retreat along this changing pathway.
0 notes
Text
Treatments of Bulimia Nervosa THE BEST OPTION Evaluation of Combined Therapy for Bulimia Nervosa Description and Significance Bulimia nervosa, simply bulimia or BN, refers to uncontrolled overeating or binging and then eliminating what has been eaten (SJH, 2012; Grange et al., 2004). Recent reports show alarming increases in the incidence, which now adolescents and pre-adolescents. The latest population statistics say that about 27.3 of the U.S. population is between 12 and 19 years old. BN affects up to 3% of these young people 15-18 years old at peak (SJH, Grange et al.). Brief Description of BN BN consists of eliminating or purging ingested food through induced vomiting, inappropriate use of laxatives or diuretics, fasting or extreme exercise to control weight (SJH 2012; Grange et al., 2004). The exact cause or causes are still unknown. But some factors are believed to contribute to it. These are cultural ideals and social attitudes about body appearance, self-evaluation on the basis of body weight and shape and family problems. Self-consciousness, especially about physical appearance, is most common and strongest in adolescence (SLH, Grange et al.). The common symptoms indicative of BN include low or normal body weight viewed as overweight, recurring binge eating and the fear of not stopping it, self-induced vomiting, excessive fasting, excessive exercising, ritualistic and peculiar eating habits, inappropriate laxative use, irregular or no menstruation, anxiety, depression, scares at the back of the fingers from induced vomiting and over-achieving behavior (SJH 2012; Grange et al., 2004). Usual treatment is through a combination of individual therapy, family therapy, behavior change and nutritional adjustment. Treatment is decided after an evaluation of the person and his or her family. Additional medication may be prescribed or administered if depression is also present. Parents are counseled to be supportive of the patient. Hospitalization may also be required if case of complications like weight loss and malnutrition (SLH, Grange et al.). Recent evidence suggests fluoxetine as the only USFDA-approved selective serotonin-reuptake inhibitor or SSRI for BN in adolescents and pre-adolescent persons (Blake & Rich, 2008). It is also more effective and beneficial than placebo. In combination with cognitive behavioral therapy or CBT, it is even better and superior to fluoxetine alone, CBT alone or placebo, according to trial results. Other drugs are citalopram or escitalopram, sertraline, paroxetine, and venlafaxine (Blake & Rich). Relevance to Clinical Care and Nursing The increase of BN incidence and prevalence among adolescents and pre-menarchial adolescents are specifically alarming to the health care profession (Grange et al., 2004). Partial eating syndromes add to the alarming situation. Community samples suggest that 10-50% of them develop BN yet diagnostic tests revealed that only 1-5% of the girls who responded reflected the BN condition. This meant that there are those whose symptoms have not been recognized and recorded in the statistical manual. These partial eating syndromes are likely to grow and become full-blast (Grange et al.). Randomized Clinical Trials 1. Solomando et al. (2008) summarized recent evidence drawn from the clinical guidelines of the National Institute for Health and Clinical Excellence and high-quality systematic reviews on the use of CBT for treating children and adolescents with mental health problems, such as BN. The synthesis was limited to systematic reviews in identifying and examining the most reliable evidence available. The outcomes yielded the most reliable evidence of potential benefit or the lack of it for CBT. Data drawn from the meta-analyses of randomized controlled trials offered the best evidence for CBT in treating children and adolescents with generalized mental disorders, such as generalized anxiety disorder, depression, obsessive-compulsive disorder and post-traumatic disorder. There is limited evidence in efficacy for ADHD and other antisocial behavior, psychotic and related disorders, substance misuse, self-harm behavior and eating disorders (Solomando et al.). This is level-1 evidence, which is systematic and can be generalized for mental health problems but not for eating disorders like BN. 2. Goodyer S. et al. (2007) performed a randomized controlled superiority trial in order to determine the effectiveness of SSRIs and CBT in the short-term as compared with an SSRI and clinical care alone in adolescents with moderate to severe major depression, as co-occurring in BN. The team surveyed 208 adolescents, aged 11-17, from 6 outpatient clinics in Manchester and Cambridge. They were diagnosed with major or probable major depression and unresponsiveness to a brief initial intervention. Included were adolescents with suicidal tendencies, depressive psychosis, and conduct disorders. The team administered SSRI and routine care to 103 respondents and SSRI, routine care and CBT to 105 for 12 weeks and maintenance for 16 weeks. Secondary measures were change in scores on moods and feelings through a questionnaire, the revised children's rating scale, the children's global assessment scale, and the clinical global impression improvement scale. Results yielded no evidence of efficacy of combined CBT and SSRIs with routine clinical care on short-term as contributing to improvement by 28 weeks for the respondents. This was in comparison with routine clinical care and SSRI alone (Goodyer et al.). This is a Level-2 evidence of a single experimental study, which can be generalized for short-term generalization. 3. The TADS Team (2007) performed randomized controlled trial on the effectiveness of a combination of treatments on adolescents with major depressive disorder. These treatments were fluoxetine hydrochloride therapy, CBT and their combination. The RCT was conducted on 320 participants, aged 12-17, in 13 academic community sites for 36 weeks. The team, an independent evaluator, used the Children's Depression Rating Scale. CBT and combination therapies were not masked but placebo and fluoxetine therapies were double blind for 12 weeks. The treatments were un-blinded afterwards. The placebo group was excluded in these analyses. Findings showed that treatment with fluoxetine alone or in combination with CBT sped up the rate of improvement. The addition of CBT increased safety levels. The combination appeared superior to either in treating depression, which frequently accompanies BN. This is level-1 evidence, which can be generalized for depression (TADS Team). 4. Brent (2008) and his team, in a separate RCT, found that the combination of CBT and a change of SSRIs would raise clinical response for adolescents with depression who were unresponsive to SSRI as an initial treatment. The team's aim was to evaluate and compare the effectiveness of four treatment alternatives on 334 patients, aged 12-18, from 6 U.S. academic and community clinics from 2000-2006. The team switches between SSRIs and CBT and compared the treatments for 12 weeks. Venlafaxine with CBT was also tested. The outcome measures used were the Clinical Global Impressions-Improvement Scale and the Children's Depression Ration Scale (Brent et al.). This is a Level -3 evidence as it was quasi-experimental. 5. Walkup (2008) and his team similarly concluded that both CBT and SSRI reduced severe anxiety symptoms in children and adolescents to a superior level. They conducted an RCT to explore the relative or combined efficacy of these treatments on 488 participants, aged 7-17 with varying diagnoses of anxiety disorders. The participants went through 14 CBT sessions and received the SSRI sertraline, a combination of CBT and sertraline or a placebo for 12 weeks. The team used categorical and dimensional ratings at baseline in weeks 4, 8 and 12. Results showed a high 80% of improvement from combination therapy, according to the Clinician Global Impression Improvement test. The Pediatric Anxiety Rating Scale yielded a similarly high pattern of response, particularly for the combination therapy. Other symptoms associated with CBT, such as insomnia, fatigue, sedation and restlessness, were also reduced (Walkup et al.). This is level-2 evidence, which can be generalized for anxiety, which often accompanies BN. 6. Hay (2008) and his associates conducted 26 systematic reviews, RCTs and observational studies on the effectiveness of treatments on young BN patients. These were retrieved from Medline, Embase, The Cochrane Library, among others, up to June 2007. They used a GRADE evaluation in assessing the quality of evidence. The team found 17 interventions for BN. Summary of results showed that up to 1% of young women, who are body conscious, develop BN; they were of normal weight; half of them would have fully recover in 10 years' time; CBT alone could produce improvement compared with no treatment; CBT is comparably effective as other treatment in reducing symptoms; the efficacy of other psychological therapies remained unknown; and some SSRIs can work against symptoms better than can placebos (Hay et al.). This is a level-1 evidence that can be generalized. 7. Dubicka et al. (2010) attempted to resolve the conflicting findings from RCTs on the efficacy of SSRIs combined with CBT. In determining whether CBT produces additional benefits to SSRI treatment on adolescents suffering from depression, the team performed a meta-analysis of RCT s on new lines of SSRIs in combination with CBT on sample adolescents. These participants, aged 11-18, were diagnosed with depression as defined by DSM-IV. They were given a new type of SSRI in combination with CBT and the results were compared with those with SSRI without CBT. The focus was on depression and impairment scores, overall improvement, suicidality, and adverse effects. Results showed on significant benefit from the combined treatment on depression symptoms. A significant advantage was computed for impairment in the short-term of 12 weeks only. The combination, therefore, was found to produce limited advantage due to the varied sampling and methodology. Future research should focus on predictors of response and clinical components (Dubicka et al.). This is level-1 evidence, which can be generalized. 8. A single-site study, conducted by Riggs and her team (2007) aimed at comparing the effect of fluoxetine hydrochride against that of placebo in treating depression and related disorders in adolescents. They performed a randomized controlled trial from May 2001 to August 2004 on 126 adolescent volunteers, aged 13-19, from the community and according to the requirements of DSMMD for 16 weeks. Measures used were the Childhood Depression Rating Scale-Revised and Clinical Global Impression Improvement and self-reported symptoms for the past 30 days. The results showed that fluoxetine with CBT appeared to be similarly safe and effective for depression in participants with substance use disorder and those depressed but not into substance use. The researchers surmised that CBT may have produced the higher-then-expected response and thus blur the efficacy result (Riggs et al.). This is level-2 evidence, which can be generalized. 9. Hall (2008) and her team conducted multiple consistent RCTs to determine the most effective treatment or treatments for BN in adolescents. The group used a Cochrane review of 40 RCTs of 1-220 patients at a mean of 60 for 16 weeks median and a follow up median of 7.5 months. At that time of the test, CBT was considered the most effective. It confirmed that, compared with no treatment, CBT substantially improved symptoms. CBT also proved more significantly efficacious than other forms of psychotherapy in inducing eating abstinence. Guided self-help alone did not reduce binge and purge episodes. Results of this test and other case-control studies provided evidence that pharmacotherapy with anti-depressants are effective in treating BN. The combination is even more effective when psychotherapy is added. Remission rates were low but long-term follow-up data were limited (Hall et al.). 10. Schmidt (2007) and his associates conducted a randomized control trial of family therapy and CBT guided self-care for participating adolescents diagnosed with Bulimia Nervosa and related disorders. Their objective was to compare the effectiveness and cost-effectiveness of these two types on 85 respondents from the United Kingdom. Of the total, 41 were assigned at random to the family therapy group and 44 to CBT guided self-care. The primary measures used were abstinence from binge eating and vomiting for 6 months and then at 12 through interviews. The secondary measures included the symptoms and costs of care. The primary hypothesis was that family therapy would induce higher rates of abstinence and induced vomiting at treatment and follow-up. The secondary hypothesis was that guided self-care would be more inexpensive than family therapy. Results showed that CBT-guided self-care had a slight advantage over family therapy. It induced faster reduction of bingeing, cost less and was more acceptable to adolescents with BN (Schmidt et al.). This is level-2 evidence and can be generalized. Synthesis Of the 10 RTCs, 7 confirm the effectiveness of CBT in treating the symptoms of Bulimia Nervosa in combination with SSRIs. The combination is superior but only in the short-term (Boodyet et al., 2007). It accelerates improvement with SSRIs as well as raises the safety level (The TADS Team, 2007). The combination is better than simply switching SSRIs without the combination (Brent et al., 2008). Walkup (2008) and his team agree. Hay (2008) and his team also say that CBT alone will work on BN. Riggs (2007) and team that the combination will work. And Schmidt (2007) say the combination is more effective than family therapy. Of the 7 who confirm the benefits of CBT, 5 agree that the combination of CBT and SSRIs is the best treatment for BN. Recommendation CBT has been described as a talking therapy, which endeavors to solve emotional or behavioral problems and behaviors through a systematic approach (Osterhout, 2012). It appears best to manage BN through an interdisciplinary approach. This will involve and include a primary care provider, a psychiatrist, a psychotherapist, and a dietitian. It is preferable for the psychiatrist or psychotherapist to possess expertise in managing eating disorders. The dietitian should review and oversee the patient's nutritional rehab. A dentist and other health experts may also be needed. The overall aims should be to reduce or eliminate binge eating and purging, treat the complications, prevent them and enhance her overall health. BIBLIOGRAPHY Blake, J. G and Rich, J. (2008). Which drugs are most effective for moderate to severe depression in adolescents? Vol 57 # 5 The Journal of Family Practice: Quadrant Health Com. Inc. Retrieved on February 29, 2012 from http://www.jfponline.com/Pages.asp?AID-6182 Brent et al. (2008). Switching to another SSRI or to Venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression. The Journal of the American Medical Association: American Medical Association. Retrieved on February 29, 2012 from http://www.jama.ama-assn.org/content/299/8/901.full?linkType=FULL&journalCode=jama&resid=299/8/901 Dubicka, B. et al. (2010). Combined treatment with cognitive-behavioral therapy in adolescent depression: meta-analysis. Vol 197, The British Journal of Psychiatry: The Royal College of Psychiatrists. Retrieved on February 29, 2012 from http://www.bjp.rcpsych.org/content/197161433.full Goodyer, S., et al. (2007). Selective serotonin reuptake inhibitors and routine specialist care with and without cognitive behavior therapy in adolescents with major depression: randomized controlled trial. British Medical Journal: BMJ Publishing Group Ltd. Retrieved on February 29, 2012 from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1925185 Grange, D. le, et al. (2004). Bulimia nervosa in adolescents: a disorder in evolution? Vol 158 Archives of Pediatric and Adolescent Medicine: University of Chicago. Retrieved on February 29, 2012 from http://www.archipedi.ama-assn.og/cgi/reprit/158/5/478.pdf Hall, M.N. et al. (2008). Treatment of Bulimia Nervosa. Vol 77 (11) American Family Physician: Family Physicians Inquiries Network. Retrieved on March 4, 2012 from http://www.aafp.org/afp/2008/0601/p1588.html Hay, P.J., et al. (2008). Bulimia nervosa. Clinical Evidence: BMJ Publishing Group Lt. Retrieved on February 29, 2012 from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2907970 Osterhout, C. (2012). Bulimia Nervosa treatment and management. Medscape News:P Medscape: WebMD LLC. Retrieved on March 6, 2012 from http://www.emedicine.medscape.com/article/286485-treatment Riggs, P. d., et al. (2007). A randomized controlled trial of fluoxetine and cognitive behavioral therapy in adolescents with major depression, behavior problems, and substance use disorders. Vol 161 (11) Archive Pediatric and Adolescent Medicine: American Medical Association. Retrieved on February 29, 2012 from http://www.archpedi.ama-assn:org/cgi/content/161/11/1026 Schmidt, U. et al. (2007). A randomized controlled trial of family therapy and cognitive behavior therapy guided self-care for adolescents with Bulimia Nervosa and related disorders. Vol 164 (4) American Journal of Psychiatry: American Psychiatric Association. Retrieved on March 3, 2012 from http://www.ajp.psychiatryonline.org/article.aspx?volume=164&page=591&journalID=13 Solomando, A.M., et al. (2008). Cognitive behavioral therapy for children and Adolescents. 21 (4) Current Opinion in Psychiatry: Lippincott Williams & Wilkins. Retrieved on February 29, 2012 from http://www.medscape.com/viewarticle/575409 SJH (2012). Bulimia nervosa in adolescents. St. Joseph's Hospital and Medical Center: Catholic Healthcare West. Retrieved on February 29, 2012 from http://www.stjosephs-phx.org/Medical_Services/Adolescent_Medicine/221179 TADS Team, The (2007). The treatment for adolescents with depression study. Vol 64 (10) Archives in General Psychiatry: American Medical Association. Retrieved on February 29, 2012 from http://www.archpsych.ama-assn.org/cgi/content/full/64/10/1132 Walkup, J.T., et al. (2008). Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. New England Journal of Medicine: Massachusetts Medical Society. Retrieved on February 29, 2012 from http://www.nejm.org/doj/full/10.1056/NEJMoa0804633 Read the full article
0 notes
Text
Tramadol and Dormicum: Uses, Effects, and Risks

Tramadol and Dormicum are two commonly used pharmaceutical drugs, each serving distinct medical purposes. While Tramadol is an opioid analgesic primarily used for pain relief, Dormicum (Midazolam) is a benzodiazepine used for sedation and anxiety relief. Despite their effectiveness, both drugs tramadol come with potential risks and side effects that require careful consideration.
What is Tramadol?
Tramadol is a centrally acting opioid analgesic prescribed for moderate to severe pain management. It works by binding to opioid receptors in the brain and altering pain perception. Tramadol also increases serotonin and norepinephrine levels, which contribute to its analgesic effects.
Uses of Tramadol
Pain Management: Used for post-surgical pain, chronic pain conditions, and injury-related pain.
Neuropathic Pain: Sometimes prescribed for nerve pain conditions such as diabetic neuropathy and fibromyalgia.
Side Effects of Tramadol
While effective, Tramadol may cause side effects such as:
Nausea and vomiting
Dizziness and drowsiness
Constipation
Respiratory depression (in high doses)
Risk of addiction and dependence with prolonged use
Precautions: Tramadol should be used with caution in patients with a history of substance abuse, seizures, or respiratory conditions. It should not be combined with alcohol or other central nervous system depressants.
What is Dormicum?
Dormicum, the brand name for Midazolam, is a benzodiazepine used for its sedative, hypnotic, and anxiolytic properties. It enhances the effects of gamma-aminobutyric acid (GABA), a neurotransmitter that induces relaxation and sedation.
Uses of Dormicum
Pre-Surgical Sedation: Administered before surgeries to reduce anxiety and induce sleep.
Treatment for Insomnia: Used in certain cases where short-term sleep aid is necessary.
Seizure Control: Effective in managing seizures and convulsions in emergency settings.
Side Effects of Dormicum
Some potential side effects include:
Drowsiness and confusion
Reduced coordination
Memory impairment
Respiratory depression
Risk of dependence and withdrawal symptoms with prolonged use
Precautions: Dormicum should not be taken with alcohol or other depressants as it may lead to life-threatening respiratory issues. It should be used under medical supervision, especially in elderly patients and those with respiratory disorders.
Risks and Potential for Abuse
Both Tramadol and Dormicum have the potential for misuse and addiction. Tramadol, although a weaker opioid, can still lead to dependency, especially when taken in high doses or for extended periods. Dormicum, like other benzodiazepines, poses a risk of addiction, particularly when used for sleep disorders without medical supervision.
Conclusion
Tramadol and Dormicum serve valuable medical purposes when used correctly under a doctor’s supervision. However, their potential for side effects, dependency, and misuse makes it crucial to use them responsibly. Patients should always follow their healthcare provider’s instructions and avoid self-medication to prevent adverse effects and complications.
0 notes
Text
Understanding Treatment Resistant Depression
Treatment Resistant Depression (TRD) is a significant clinical challenge, characterized by a lack of response to standard antidepressant therapies. Individuals suffering from TRD may find that their symptoms persist despite trying multiple treatment options, leading to prolonged distress and impairment in daily functioning. Recognizing and addressing TRD is crucial for providing effective care and improving the quality of life for those affected.
What is TRD?
TRD is generally defined as a major depressive episode that does not adequately respond to at least two different classes of antidepressant medications taken at an adequate dose and duration. The complexities of TRD can stem from various factors, including genetic predispositions, the severity of the illness, comorbid conditions, and the patient's unique brain chemistry.
Treatment Options for Resistant Depression
1. Medication Adjustments:
Augmentation Strategies: Adding a second medication, such as atypical antipsychotics or mood stabilizers, can enhance the efficacy of current treatments.
Switching Medications: Transitioning to a different class of antidepressants, such as serotonin-norepinephrine reuptake inhibitors (SNRIs) or monoamine oxidase inhibitors (MAOIs), may yield better results.
2. Psychotherapy:
o Cognitive Behavioral Therapy (CBT): A structured, goal-oriented therapy focusing on modifying negative thought patterns and behaviors associated with depression.
o Interpersonal Therapy (IPT): Aimed at improving interpersonal relationships and communication skills, which can significantly impact mood and self-esteem.
3. Advanced Therapeutic Approaches:
o Transcranial Magnetic Stimulation (TMS): A non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain, offering an alternative for those who do not respond to conventional treatments.
o Ketamine Infusions: Administered under medical supervision, ketamine has shown rapid antidepressant effects, even in individuals with severe TRD.
4. Electroconvulsive Therapy (ECT):
o A highly effective treatment for severe depression, particularly in cases where immediate response is necessary or when other treatments have failed.
Treatment Resistant Bipolar Depression
Bipolar disorder can also present challenges in treatment when depressive episodes prove resistant. Treatment resistant bipolar depression requires a comprehensive approach that often includes mood stabilizers, atypical antipsychotics, and psychotherapeutic interventions tailored to the individual's needs. Collaborative care among psychiatrists, psychologists, and primary care providers is essential to ensure optimal management and recovery.
Dealing with Treatment ResistantDepression is a complex journey that requires a personalized and multifaceted approach. By exploring various treatment avenues, including medication adjustments, psychotherapy, and advanced therapies, individuals can find relief from their symptoms. If you or a loved one is struggling with TRD, seek help from a qualified mental health professional who can guide you toward effective treatment options and a path to recovery.
Get Help TodayDon’t let Treatment Resistant Depression define your life. Contact us for a consultation, and let’s work together to find the treatment that suits your needs. Your mental health matters, and support is available.
Schedule an appointment: https://healthymindssj.com/appointment/
Call us: 856-751-4116
Visit: www.healthymindssj.com
#healthy mind psychiatry#psychiatrist cherry hill#healthy minds psychiatry#psychiatry cherry hill nj#psychiatrist south jersey#psychiatrist for depression nj#depression therapy cherry hill#depression counseling cherry hill#best psychiatrist in nj#psychiatrist near me for depression
0 notes
Text
What Is Psilocybin Therapy? A Detailed Scientific Guide to Psilocybin Approach for Mental Health

buy here buy here buy here buy here
Psilocybin therapy involves the use of psilocybin, a naturally occurring psychedelic compound found in certain mushrooms, as a treatment for mental health conditions. This therapy is gaining attention for its potential to alleviate symptoms of various mental health disorders, including depression, anxiety, PTSD, and substance use disorders.
buy here buy here buy here buy here
Overview of Psilocybin
Chemical Structure: Psilocybin is converted in the body to psilocin, which interacts with serotonin receptors in the brain, particularly the 5-HT2A receptor.
Effects: The compound can induce alterations in perception, mood, and cognition, often described as a mystical or transcendent experience.
Mechanism of Action
Psilocybin's therapeutic effects are thought to arise from several mechanisms:
Neuroplasticity: Psilocybin promotes neuroplasticity, allowing the brain to form new neural connections, which can lead to improved emotional regulation and cognitive flexibility.
Default Mode Network (DMN): Psilocybin decreases activity in the DMN, a network associated with self-referential thoughts and rumination, which could be beneficial for conditions like depression.
Emotional Processing: The substance may enhance emotional processing and introspection, allowing individuals to confront and work through past traumas or negative thought patterns.
Therapeutic Applications
Research into psilocybin therapy has shown promise for several mental health conditions:
Major Depressive Disorder (MDD): Studies indicate significant reductions in depressive symptoms following psilocybin treatment, often lasting weeks or months.
Anxiety Disorders: Psilocybin may help reduce anxiety, particularly in terminal illness patients, providing relief from existential distress.
Post-Traumatic Stress Disorder (PTSD): Preliminary studies suggest psilocybin can facilitate trauma processing and reduce PTSD symptoms.
Substance Use Disorders: Psilocybin has been explored as a treatment for addiction, showing potential to disrupt habitual patterns associated with substance abuse.
Treatment Protocol
Psilocybin therapy typically follows a structured protocol:
Preparation: Patients undergo psychological assessment and preparation sessions to establish a therapeutic alliance and set intentions for the experience.
Dosing Sessions: A trained therapist guides the patient through one or more sessions where psilocybin is administered in a controlled setting.
Integration: Post-session integration therapy helps patients make sense of their experiences and apply insights to their lives.
Safety and Considerations
Risks: While psilocybin is generally considered safe, it can cause adverse effects, such as anxiety or panic during the experience. Individuals with a personal or family history of psychosis may be at higher risk.
Legality: The legality of psilocybin varies by region. Research settings often operate under strict regulatory conditions.
Current Research and Future Directions
Ongoing clinical trials are investigating the efficacy and safety of psilocybin for various conditions. As research expands, we may see more standardized protocols and guidelines for its use in therapeutic settings.
Conclusion
Psilocybin therapy represents a promising frontier in mental health treatment. While still under investigation, its potential to transform therapeutic practices for mental health disorders is becoming increasingly recognized, with many advocating for its integration into mainstream clinical practice. As research continues, it is essential to approach psilocybin therapy with careful consideration of its benefits and risks.
1 note
·
View note
Text
Unlocking Tranquility: A Closer Look at Ketamine Infusion in Rancho Mission Viejo
Introduction:
In the serene community of Rancho Mission Viejo, the pursuit of mental well-being is taking on innovative dimensions, with ketamine infusion clinic in Rancho Mission Viejo emerging as a topic of exploration. This closer look into Ketamine infusion aims to unravel its mechanisms, clinical applications, patient experiences, challenges, and the potential impact it holds for unlocking tranquility in the realm of mental health.

I. Understanding Ketamine Infusion Therapy:
Ketamine, originally recognized for its anesthetic properties, has garnered attention for its potential as a transformative mental health treatment. In the context of Rancho Mission Viejo, Ketamine infusion therapy involves administering the drug intravenously in controlled settings to address conditions such as depression, anxiety, and post-traumatic stress disorder (PTSD). The unique aspect of Ketamine lies in its rapid-acting antidepressant effects, setting it apart from traditional treatments.
II. Mechanisms of Ketamine:
To unlock tranquility with Ketamine, it is crucial to comprehend its mechanisms. Unlike conventional antidepressants that primarily target neurotransmitters like serotonin, Ketamine acts on the glutamate system. Specifically, it antagonizes N-methyl-D-aspartate (NMDA) receptors, leading to increased synaptic connections and triggering cascades that result in rapid mood improvement. This distinctive mechanism offers a promising avenue for individuals in Rancho Mission Viejo seeking relief from persistent mental health challenges.
III. Clinical Applications:
Ketamine infusion therapy demonstrates versatility in addressing various mental health conditions, making it a subject of interest in Rancho Mission Viejo.
a. Depression: Clinical studies have shown that Ketamine infusion produces rapid and robust antidepressant effects, especially for individuals with treatment-resistant depression. The quick onset of action distinguishes Ketamine as a potential lifeline for those in acute distress.
b. Anxiety Disorders: Ketamine's anxiolytic properties make it a candidate for treating various anxiety disorders. Individuals in Rancho Mission Viejo experiencing debilitating anxiety may find relief through the calming effects induced by Ketamine infusion.
c. Post-Traumatic Stress Disorder (PTSD): Emerging research suggests that Ketamine infusion may be beneficial for individuals struggling with PTSD. By disrupting maladaptive memory processes, Ketamine could potentially alleviate the emotional distress associated with traumatic memories.
IV. Patient Experiences:
An essential aspect of Ketamine infusion therapy is the reported transformative experiences of patients in Rancho Mission Viejo.
a. Dissociative State and Insights: During Ketamine sessions, individuals may enter a dissociative state, fostering a unique introspective experience. Patients often report gaining insights into their thoughts, emotions, and life experiences, contributing to a profound sense of self-awareness.
b. Rapid Relief and Improved Mood: One of the notable features of Ketamine infusion is the rapid relief of symptoms. Many patients in Rancho Mission Viejo report an almost immediate improvement in mood, offering a stark contrast to the delayed onset often associated with traditional antidepressants.
c. Holistic Well-Being: Beyond symptom relief, Ketamine infusion therapy is reported to contribute to holistic well-being. Patients describe a sense of clarity, improved motivation, and an enhanced ability to engage in therapy and self-care practices.
V. Challenges and Considerations:
While the potential benefits of Ketamine infusion therapy are promising, challenges and considerations exist.
a. Access and Availability: The availability of trained professionals and specialized clinics for Ketamine infusion may be limited in Rancho Mission Viejo. This raises concerns about access and the need for expanded availability to meet the growing interest in this innovative treatment.
b. Financial Considerations: The cost of Ketamine infusion therapy can be a barrier for some individuals, as insurance coverage varies, and out-of-pocket expenses may pose challenges. Ensuring affordability and exploring financial assistance options are considerations for those seeking this treatment.
c. Long-Term Effects and Safety: The long-term effects and safety of repeated Ketamine infusions require further research. While short-term benefits are evident, ongoing studies aim to address concerns related to the extended use of Ketamine for mental health conditions.
VI. Community Perspectives:
The reception of Ketamine infusion therapy in Rancho Mission Viejo reflects a mix of curiosity, hope, and cautious optimism. Mental health advocates emphasize the importance of exploring alternative treatments, particularly for individuals facing persistent challenges. However, there are also considerations about the need for further research, education, and awareness to ensure responsible and informed use of Ketamine in mental health care.
Conclusion:
As Rancho Mission Viejo explores the potential of Ketamine infusion therapy in unlocking tranquility for mental health challenges, a nuanced understanding of its mechanisms, clinical applications, patient experiences, and associated challenges is crucial. The reported rapid relief, transformative insights, and holistic well-being experienced by patients underscore the potential impact of Ketamine in the mental health landscape.
While challenges such as access, affordability, and safety considerations persist, the exploration of Ketamine infusion therapy signifies a potential paradigm shift in mental health care in Rancho Mission Viejo. By fostering open dialogue, increasing awareness, and addressing concerns responsibly, the community has the opportunity to navigate this innovative path towards unlocking tranquility for individuals seeking effective and transformative mental health interventions.
0 notes
Text
GOLDEN RULES FOR NURSES
NURSES
Golden Points to Remember
➥ Antiemetic drugs prevent vomiting.
➥ Intraosseous injections are given into the bone marrow.
➥ Intrathecal injections are given into the spinal cavity.
➥ Intramuscular injections should be given on 90° angle.
➥ Subcutaneous injections should be given on 45° angle.
➥ Intradermal injections should be given on 15° angle.
➥ Blood group ‘AB’ is known as universal recipient and blood group ‘O is known as universal donor.
➥ Mercury is used in thermometer because mercury is very sensitive to little change in temperature.
➥ For giving enema, left lateral position should be given.
➥ Air cushion is used to prevent bed sores.
➥ Hey’s test is performed for identify bile salts in urine
➥ Smith’s test is performed to found out presence of bile pigments in urine.
➥ Components of Total parenteral nutrition (TPN) are carbohydrates (glucose), amino acids, lipids,vitamins, minerals, and electrolytes.
➥ Insulin may be added to TPN to offset the high concentration of glucose and heparin may be added to limit the formation of a fibrous clot at the tip of the catheter.
➥ The bones in the forearm act as a natural splint by providing support to an I.V. access site.
➥ Don’t select an I.V. site on a paralyzed or traumatized arm.
➥ The basilica vein is normally used for a peripherally inserted central catheter (PICC) line.
➥ Because the insertion of a PICC line is below the level of the heart, an air embolism isn’t an expected occurrence.
➥ If a client has a high temperature, notify the physician before administering any blood product.
➥ No solution or product other than normal saline should be added to blood or blood product.
➥ Maslow’s hierarchy of needs must be met in the following order: physiologic (oxygen, food, water,sex, rest, and comfort), safety and security, love and belonging, self-esteem and recognition, and self- actualization.
➥ To avoid staining the teeth, the client should take a liquid iron preparation through a straw.
➥ Fluid oscillation in the tubing of a chest drainage system indicates that the system is working properly.
➥ The type of assessment that includes data related to a client’s biological, cultural, spiritual and social need is called Comprehensive Assessment.
➥ The Vital Signs are: 1. Temperature, 2. Pulse, 3.Respiration, 4. Blood pressure, and 5. Pain.
➥ Heat loss due to contact with circulating air movement is known as Convection.
➥ The range of marking in glass/clinical thermometer is 95-110° F and 35-43.3°C.
➥ Normal Rectal temperature is 99.6° F (37°C) (1°F ) higher than oral temperature).
➥ Rectal temperature is the most reliable.
➥ Relapsing fever: Fever episodes are separated by intervals of normal temperature for days or weeks.
➥ Rigor: Sudden rise in body temperature with shivering as seen in malaria.
➥ Increased depth of breathing with normal respiratory rate is called Hyperpnea.
➥ Cheyne-Stokes Respiration is characterized by altered period of Tachypnea and Apnea.
➥ Pulse deficit refers to the difference between apical pulse and radial pulse.
➥ A Blood Pressure Cuff that is too large will give falsely low reading of BP.
➥ Beneficence: Doing good for clients and providing benefit balanced against risk.
➥ Isotonic solutions allow free movement of water across the membrane without changing concentration of solutes on either side. E.g. 0.9% NaCl.
➥ Hypertonic solution: Fluids with solutes more concentrated than in cells, e.g. 5% dextrose.
🛑 Explanation
1. Antiemetic drugs prevent vomiting.
Antiemetic drugs are medications used to prevent or treat nausea and vomiting. They work by targeting different receptors in the body, including those in the gastrointestinal tract and the central nervous system.
There are several types of antiemetic drugs available, including:
1. Serotonin antagonists: These drugs block the action of serotonin, a neurotransmitter involved in nausea and vomiting. Examples include ondansetron, granisetron, and dolasetron.
2. Dopamine antagonists: These drugs block the action of dopamine, a neurotransmitter involved in nausea and vomiting. Examples include metoclopramide and prochlorperazine.
3. Histamine antagonists: These drugs block the action of histamine, a neurotransmitter involved in nausea and vomiting. Examples include dimenhydrinate and meclizine.
4. Cannabinoids: These drugs work by activating cannabinoid receptors in the body, which can help to reduce nausea and vomiting. Examples include dronabinol and nabilone.
Other types of antiemetic drugs include benzodiazepines, which can help to reduce anxiety and nausea, and corticosteroids, which can help to reduce inflammation and swelling that can contribute to nausea and vomiting.
Antiemetic drugs may be prescribed for a variety of conditions, including chemotherapy-induced nausea and vomiting, postoperative nausea and vomiting, and motion sickness, among others. It is important to note that antiemetic drugs may have side effects, and should only be taken as directed by a healthcare professional.
GOLDEN POINTS FOR NURSES
2. Intraosseous injections are given into the bone marrow.
Intraosseous injections are given directly into the bone marrow, typically of the long bones such as the femur, tibia, and humerus.
This route of administration is used when intravenous access is not feasible or when a more rapid onset of action is needed, such as in emergency situations.
Intraosseous injections are commonly used in pediatric patients, as well as in adult patients in emergency and critical care settings.
The technique involves using a specialized needle to penetrate the bone and access the marrow cavity, where medications or fluids can be injected directly into the bloodstream.
GOLDEN POINTS FOR NURSES
3. Intrathecal injections are given into the spinal cavity.
Intrathecal injections are given directly into the spinal cavity, specifically into the subarachnoid space surrounding the spinal cord.
This route of administration is used to deliver medications or other substances directly to the central nervous system, bypassing the blood-brain barrier. Intrathecal injections may be used to treat conditions such as chronic pain, spasticity, and certain types of cancer, among others.
The technique involves using a specialized needle to puncture the spinal canal and access the subarachnoid space, where medications or other substances can be injected. Because of the risks associated with this procedure, including infection, bleeding, and damage to the spinal cord or nerves, it is typically performed under strict sterile conditions by trained medical professionals.
Golden rules for NURSES
4. Intramuscular injections should be given on 90° angle.
The angle at which an intramuscular injection should be given can vary depending on the size of the needle and the location of the injection site. In general, a 90-degree angle is appropriate for most adult patients receiving intramuscular injections.
However, for patients who have less subcutaneous tissue or who are receiving injections in areas with less muscle mass, such as the deltoid muscle in the upper arm, a 45-degree angle may be more appropriate. It is important to follow proper injection technique and to consult with a healthcare provider if you have any questions or concerns about administering an intramuscular injection.
Golden rules for NURSES
5. Subcutaneous injections should be given on 45° angle.
The angle at which a subcutaneous injection should be given can vary depending on the size of the needle and the location of the injection site. In general, a 45-degree angle is appropriate for most adult patients receiving subcutaneous injections.
However, for patients who have less subcutaneous tissue or who are receiving injections in areas with less fat, such as the abdomen, a 90-degree angle may be more appropriate. It is important to follow proper injection technique and to consult with a healthcare provider if you have any questions or concerns about administering a subcutaneous injection.
Golden rules for NURSES
6. Intradermal injections should be given on 15° angle.
Yes, that's correct. Intradermal injections are administered at a shallow angle, typically between 5 and 15 degrees, into the dermis layer of the skin.
The angle used for an intradermal injection is much shallower than for an intramuscular or subcutaneous injection, as the goal is to inject the medication just under the surface of the skin.
This type of injection is commonly used for skin testing, such as for tuberculosis or allergies, and is typically given on the inner forearm or upper back. It is important to follow proper injection technique and to consult with a healthcare provider if you have any questions or concerns about administering an intradermal injection.
Golden rules for NURSES
7. Blood group ‘AB’ is known as universal recipient and blood group ‘O is known as universal donor.
Yes, that's correct. Blood group AB is known as the universal recipient because individuals with this blood type can receive blood from any other blood type without experiencing an adverse immune reaction. This is because they have both A and B antigens on the surface of their red blood cells, and therefore do not produce antibodies against either antigen.
On the other hand, blood group O is known as the universal donor because individuals with this blood type can donate blood to individuals with any other blood type without causing an adverse immune reaction. This is because they do not have A or B antigens on the surface of their red blood cells, and therefore do not produce antibodies against these antigens. However, individuals with blood group O can only receive blood from other individuals with blood group O, as their immune system will recognize the A and B antigens as foreign and produce antibodies against them.
Golden rules for NURSES
8. Mercury is used in thermometer because mercury is very sensitive to little change in temperature.
Yes, that is correct. Mercury is often used in thermometers because it is a liquid metal that has a high coefficient of thermal expansion, which means that it expands and contracts in response to changes in temperature. This makes it very sensitive to even small changes in temperature and allows for accurate temperature readings.
In addition, mercury has a low freezing point and a high boiling point, which means that it remains in a liquid state over a wide range of temperatures. This allows it to be used in both low-temperature and high-temperature applications.
However, it is important to note that mercury is a toxic substance and can be harmful if ingested or inhaled. For this reason, many countries have banned the use of mercury in thermometers and other consumer products, and alternative substances such as alcohol or digital thermometers are often used instead.
Golden rules for NURSES
9. For giving enema, left lateral position should be given.
Yes, the left lateral position is commonly used for administering an enema. This position helps to promote the flow of the enema solution into the rectum and prevents it from flowing back out.
To assume the left lateral position for an enema, the patient should lie on their left side with their left leg straight and their right knee bent slightly. They should bring their right knee up towards their chest to further open the rectal area. This position helps to straighten out the rectum and makes it easier to insert the enema tip.
It is important to follow proper enema administration technique and to use sterile equipment to minimize the risk of infection or injury. A healthcare provider should be consulted if you have any questions or concerns about administering an enema.
Golden rules for NURSES
10. Air cushion is used to prevent bed sores.
Air cushions can be used as part of a preventative strategy to help reduce the risk of bed sores, also known as pressure ulcers. Pressure ulcers can occur when there is prolonged pressure on a particular area of the skin, often caused by immobility or being in a seated or lying position for an extended period of time.
Air cushions are designed to distribute pressure evenly over the surface of the cushion, which can help reduce pressure on any particular area of the body. This can help to prevent the development of pressure ulcers and also provide greater comfort for the person sitting or lying on the cushion.
However, it is important to note that air cushions are just one component of a comprehensive pressure ulcer prevention plan. Other strategies may include repositioning the patient regularly, maintaining good skin hygiene, and providing adequate nutrition and hydration. It is important to work with a healthcare provider to develop an individualized care plan for preventing pressure ulcers in each patient.
Golden rules for NURSES
11. Hey’s test is performed for identify bile salts in urine
Hey's test is a laboratory test used to detect the presence of urobilinogen in urine, not bile salts. Urobilinogen is a colorless substance that is produced in the liver during the breakdown of bilirubin, a yellowish substance that is formed when old red blood cells are broken down.
Hey's test involves adding a chemical reagent to a urine sample, which causes any urobilinogen present to oxidize and turn pink or red in color. The intensity of the color change is used to determine the concentration of urobilinogen in the urine.
While Hey's test is not used specifically to identify bile salts in urine, elevated levels of urobilinogen in the urine can be an indication of liver disease or other medical conditions affecting the liver or biliary system, which can lead to the accumulation of bile salts in the urine. It is important to consult with a healthcare provider for proper diagnosis and treatment of any medical condition.
Golden rules for NURSES
12. Smith’s test is performed to found out presence of bile pigments in urine.
No, Smith's test is not used to detect the presence of bile pigments in urine. Smith's test is a laboratory test used to detect the presence of protein in urine.
Bile pigments, such as bilirubin and urobilinogen, may be present in urine in certain medical conditions affecting the liver or biliary system. However, there are other laboratory tests that are more commonly used to detect these substances in urine, such as the bilirubin test or the urobilinogen test.
It is important to consult with a healthcare provider for proper diagnosis and treatment of any medical condition that may be affecting the urinary system or other organ systems in the body.
Golden rules for NURSES
13. Components of Total parenteral nutrition (TPN) are carbohydrates (glucose), amino acids, lipids,vitamins, minerals, and electrolytes.
Yes, that is correct. Total parenteral nutrition (TPN) is a form of nutrition therapy that delivers all of the necessary nutrients, including carbohydrates (glucose), amino acids, lipids, vitamins, minerals, and electrolytes, directly into the bloodstream through a vein. TPN is typically administered when a patient is unable to obtain adequate nutrition through the gastrointestinal tract, such as in cases of severe malabsorption, intestinal obstruction, or other medical conditions.
The specific components and concentrations of TPN are tailored to the individual patient's needs based on factors such as age, weight, medical condition, and laboratory values. TPN is typically administered in a hospital setting and requires close monitoring by a healthcare provider to ensure proper dosing and to monitor for any potential complications or side effects.
Golden rules for NURSES
14. The bones in the forearm act as a natural splint by providing support to an I.V. access site.
Yes, that is correct. The bones in the forearm, specifically the radius and ulna, can act as a natural splint by providing support and stability to an IV access site. When an IV catheter is inserted into a vein in the arm, it can be secured in place using a dressing or tape to prevent movement or dislodgement. However, the bones in the forearm can also provide additional support and stability to the IV catheter, which can help to prevent accidental dislodgement or complications such as infiltration or extravasation.
It is important to ensure that the IV catheter is properly placed and secured, and to monitor the IV site for signs of complications such as swelling, redness, pain, or leakage. If any of these signs are present, it is important to notify a healthcare provider immediately.
Golden rules for NURSES
15. Don’t select an I.V. site on a paralyzed or traumatized arm.
Yes, that is correct. When selecting an IV site, it is important to avoid areas that are paralyzed or traumatized. A paralyzed limb may have reduced blood flow and sensation, which can increase the risk of complications such as infiltration or extravasation. Additionally, a traumatized limb may have damaged blood vessels or tissues, which can also increase the risk of complications.
When selecting an IV site, healthcare providers typically look for a site that has good blood flow, easy access, and minimal risk of complications. The most common sites for IV access are the veins in the arms, but other sites such as the hands or feet may be used if necessary. Factors such as the patient's medical condition, age, and overall health may also be taken into consideration when selecting an IV site.
It is important to properly assess the patient's veins and select the most appropriate site for IV access, while also considering the patient's comfort and safety. Proper insertion and maintenance of the IV catheter, as well as monitoring for signs of complications, can help to ensure optimal outcomes for the patient.
Golden rules for NURSES
16. Don’t select an I.V. site on a paralyzed or traumatized arm.
It is important to avoid selecting an intravenous (IV) site on a paralyzed or traumatized arm. There are several reasons for this:
Risk of further injury: If the arm is already traumatized or paralyzed, there is a risk of further injury or damage to the arm if an IV is inserted in that area. This can result in nerve damage, muscle damage, or other complications.
Difficulty monitoring: If the arm is paralyzed, it may be difficult to monitor for signs of infection or other complications at the IV site. This can lead to delayed diagnosis and treatment of any problems that may arise.
Reduced blood flow: A paralyzed or traumatized arm may have reduced blood flow, which can affect the delivery of fluids and medications through the IV. This can result in poor IV access or incomplete delivery of medication.
In general, it is important to choose a site for IV insertion that is healthy, well-vascularized, and free from any injuries or abnormalities. If a patient's arm is paralyzed or traumatized, it is best to select a different site for the IV. This can help ensure that the IV is placed safely and effectively, without causing any further harm to the patient.
Golden rules for NURSES
17. The basilica vein is normally used for a peripherally inserted central catheter (PICC) line.
The basilic vein is one of the veins that can be used for a peripherally inserted central catheter (PICC) line. A PICC line is a long, thin tube that is inserted through a peripheral vein (usually in the arm) and passed through to the larger veins near the heart. This type of catheter is often used for patients who require long-term intravenous (IV) access for medications, fluids, or other treatments.
The basilic vein is located on the medial (inner) side of the upper arm, and it runs from the elbow to the axilla (armpit). It is one of the larger veins in the arm, making it a good candidate for a PICC line insertion. Other veins that can be used for a PICC line include the cephalic vein and the brachial vein.
When a PICC line is inserted, the healthcare provider will use ultrasound guidance to locate the basilic vein and insert the catheter through the skin and into the vein. The catheter is then advanced through the vein and into the larger veins near the heart. Once the catheter is in place, it can be used for the administration of medications, fluids, or other treatments.
It is important to note that while the basilic vein is a common choice for a PICC line insertion, the healthcare provider will consider several factors when choosing the best vein for each patient. These factors may include the patient's medical history, the size and condition of the veins, and the specific needs of the patient's treatment plan.
Golden rules for NURSES
18. Because the insertion of a PICC line is below the level of the heart, an air embolism isn’t an expected occurrence.
While it is true that the insertion of a peripherally inserted central catheter (PICC) line is typically done below the level of the heart, an air embolism can still occur during the insertion process or while the catheter is in place.
An air embolism occurs when air bubbles enter the bloodstream and block the flow of blood to vital organs. While air embolisms are rare, they can be life-threatening if not promptly recognized and treated.
During the insertion of a PICC line, there is a risk of air entering the catheter or the bloodstream. Healthcare providers take precautions to minimize this risk by carefully priming and flushing the catheter and using specialized techniques to insert and position the catheter.
However, even with these precautions, it is still possible for air to enter the bloodstream. This can happen if the catheter becomes disconnected or if the patient experiences a sudden change in position that allows air to enter the catheter.
To minimize the risk of air embolism, healthcare providers carefully monitor patients during and after PICC line insertion. They may use ultrasound or other imaging techniques to confirm proper catheter placement and check for any signs of air in the bloodstream.
If an air embolism is suspected, immediate treatment is required. This may include stopping the infusion, administering supplemental oxygen, and positioning the patient in a way that prevents the air from traveling to the heart or lungs. In severe cases, more advanced treatments may be necessary, such as hyperbaric oxygen therapy or surgery.
Golden rules for NURSES
19. If a client has a high temperature, notify the physician before administering any blood product.
If a client has a high temperature, it is important to notify the physician before administering any blood product. This is because a high temperature can be a sign of infection or another underlying condition that may be exacerbated by the administration of blood products.
Blood products are typically used to treat a variety of conditions, including anemia, bleeding disorders, and immune system disorders. While these products can be life-saving, they also carry certain risks, such as infection, allergic reactions, and transfusion reactions.
One of the key steps in ensuring the safe administration of blood products is to carefully screen patients for any underlying conditions or risk factors that may increase their risk of complications. This includes monitoring for signs of infection, such as a high temperature, before administering any blood products.
If a client has a high temperature, the physician may want to delay or modify the administration of blood products until the underlying cause of the fever can be identified and treated. This may involve further testing or evaluation to determine if the client has an infection or other condition that could increase their risk of complications from the blood product.
By notifying the physician of any signs of infection or other concerns before administering blood products, healthcare providers can help ensure the safe and effective use of these important treatments.
Golden rules for NURSES
20. No solution or product other than normal saline should be added to blood or blood product.
It is generally recommended that no solution or product other than normal saline should be added to blood or blood products. This is because the addition of other substances can increase the risk of adverse reactions and other complications.
Normal saline, also known as 0.9% sodium chloride, is a sterile solution of salt and water that is used to replace lost fluids and restore electrolyte balance in the body. It is often used as a diluent for blood and blood products because it is compatible with these substances and does not increase the risk of adverse reactions or complications.
Adding other solutions or products to blood or blood products can alter their composition and increase the risk of adverse reactions, such as transfusion reactions, allergic reactions, or infections. For example, adding medications or other substances to blood products can increase the risk of medication errors and other complications.
In some cases, healthcare providers may need to add a medication or other substance to blood or blood products to meet the specific needs of the patient's treatment plan. When this is necessary, it is important to carefully follow established protocols and guidelines to minimize the risk of adverse reactions or other complications.
Overall, the addition of any solution or product to blood or blood products should only be done under the direction of a healthcare provider with appropriate training and expertise in transfusion medicine.
Golden rules for NURSES
21. Maslow’s hierarchy of needs must be met in the following order: physiologic (oxygen, food, water,sex, rest, and comfort), safety and security, love and belonging, self-esteem and recognition, and self- actualization.
Maslow's hierarchy of needs is a theory that suggests that human needs can be organized into a hierarchy, with lower-level needs taking priority over higher-level needs. According to Maslow's theory, the hierarchy of needs must be met in a specific order, with lower-level needs needing to be met before higher-level needs can be addressed.
The hierarchy of needs includes the following levels, in order from lowest to highest:
Physiological needs: These are the most basic needs, including the need for oxygen, food, water, shelter, sleep, and other bodily needs.
Safety needs: Once physiological needs are met, individuals have a need for safety and security, including physical safety, financial security, and stability.
Love and belonging needs: After safety needs are met, individuals have a need for love, affection, and a sense of belonging, including relationships with family, friends, and community.
Esteem needs: Once the need for love and belonging is met, individuals have a need for self-esteem and recognition from others, including achievement, status, and respect.
Self-actualization needs: Once all of the other needs are met, individuals have a need for self-actualization, including personal growth, self-fulfillment, and realizing their full potential.
In order to meet higher-level needs, lower-level needs must first be met. For example, an individual who is hungry and thirsty will not be able to focus on safety needs until their basic physiological needs are met. Similarly, an individual who is struggling to find a sense of belonging may have difficulty focusing on self-esteem needs until they feel a sense of connection with others.
By understanding Maslow's hierarchy of needs, healthcare providers can better understand the needs and priorities of their patients and develop treatment plans that address their most pressing needs first. This can help promote better outcomes and improve patient satisfaction.
Golden rules for NURSES
22. To avoid staining the teeth, the client should take a liquid iron preparation through a straw.
To avoid staining the teeth, it is recommended that the client take a liquid iron preparation through a straw. Iron supplements can cause staining of the teeth, which can be unsightly and difficult to remove. By using a straw to take the supplement, the liquid can bypass the teeth and reduce the risk of staining.
In addition to using a straw, there are other strategies that can help minimize the risk of staining from iron supplements. For example, the client can rinse their mouth with water after taking the supplement to help remove any residual liquid from the teeth. They may also want to avoid brushing their teeth immediately after taking the supplement, as this can actually spread the iron around and increase the risk of staining.
If the client does experience staining from the iron supplement, there are several options for addressing the issue. One approach is to switch to a different form of iron supplement, such as a tablet or capsule, which may be less likely to cause staining. Alternatively, the client may be able to use a whitening toothpaste or receive professional teeth whitening treatment to help remove the stains.
Overall, while liquid iron preparations can be an effective treatment for iron deficiency, they can also cause staining of the teeth. By using a straw and taking other steps to minimize the risk of staining, clients can help ensure that they receive the benefits of iron supplementation without experiencing unwanted side effects.
Golden rules for NURSES
23. Fluid oscillation in the tubing of a chest drainage system indicates that the system is working properly.
Fluid oscillation in the tubing of a chest drainage system does not necessarily indicate that the system is working properly. In fact, fluid oscillation can be an indication of a problem with the system that requires attention from healthcare providers.
A chest drainage system is typically used to remove excess air or fluid from the pleural space in the chest. The system consists of a drainage tube, a collection chamber, and a series of tubing that connects the drainage tube to the collection chamber. The tubing is often clear, allowing healthcare providers to observe the movement of fluid and air through the system.
Fluid oscillation refers to the movement of fluid back and forth in the tubing of the chest drainage system. While some oscillation is normal and can indicate that the system is functioning properly, excessive oscillation can be a sign of a problem. For example, if there is a blockage in the tubing or collection chamber, fluid may be unable to flow freely and can cause increased oscillation. Similarly, if the drainage tube is not properly inserted into the pleural space, air may be drawn into the tubing and cause oscillation.
If a healthcare provider observes excessive fluid oscillation in a chest drainage system, they may need to take steps to address the underlying issue. This may involve adjusting the placement of the drainage tube, clearing any blockages in the tubing or collection chamber, or replacing a malfunctioning component of the system.
Overall, while some fluid oscillation in the tubing of a chest drainage system can be normal, excessive oscillation can be a sign of a problem that requires attention from healthcare providers.
Golden rules for NURSES
24. The type of assessment that includes data related to a client’s biological, cultural, spiritual and social need is called Comprehensive Assessment.
The type of assessment that includes data related to a client's biological, cultural, spiritual, and social needs is indeed called a comprehensive assessment.
A comprehensive assessment is a holistic approach to assessing a client's health status that takes into account various aspects of their life, including their physical health, cultural background, spiritual beliefs, and social environment. By gathering information on these different factors, healthcare providers can gain a more complete understanding of the client's health status and develop a care plan that addresses all of their needs.
In a comprehensive assessment, healthcare providers may gather data through a variety of methods, including interviews, physical exams, laboratory tests, and observation of the client's behavior and interactions with others. They may also use standardized assessment tools to gather information on specific aspects of the client's health, such as their mental health status or their risk for falls.
Overall, a comprehensive assessment is an important tool for healthcare providers in understanding their clients' needs and developing an effective care plan that addresses all aspects of their health and well-being.
Golden rules for NURSES
25. The Vital Signs are: 1. Temperature, 2. Pulse, 3.Respiration, 4. Blood pressure, and 5. Pain.
The vital signs are indeed a set of important measurements that healthcare providers use to assess a client's overall health status. The five vital signs are:
Temperature: The measurement of the body's core temperature. Normal body temperature ranges from 97.7°F to 99.5°F (36.5°C to 37.5°C).
Pulse: The measurement of the heart rate, or the number of times the heart beats per minute. A normal pulse rate for adults is between 60 to 100 beats per minute.
Respiration: The measurement of the breathing rate, or the number of breaths taken per minute. A normal respiration rate for adults is between 12 to 20 breaths per minute.
Blood pressure: The measurement of the force of blood against the walls of the arteries as the heart pumps blood throughout the body. Blood pressure is expressed in two numbers, with the systolic pressure (the top number) indicating the pressure when the heart beats, and the diastolic pressure (the bottom number) indicating the pressure when the heart is at rest. A normal blood pressure reading for adults is typically around 120/80 mmHg.
Pain: The subjective experience of discomfort or distress. Pain is assessed using various scales, such as the numeric rating scale (NRS) or visual analog scale (VAS).
Overall, the vital signs are important indicators of a client's overall health status, and healthcare providers regularly assess these measurements to monitor changes in the client's condition and develop an effective care plan.
Golden rules for NURSES
26. Heat loss due to contact with circulating air movement is known as Convection.
Yes, that is correct. Convection is the transfer of heat from a surface to a fluid (e.g. air or water) that is moving. When air moves over a surface, it carries away heat, causing the surface to cool.
This is why we feel cooler when there is a breeze or wind blowing, even if the air temperature is the same.
Convection is an important factor to consider when designing heating and cooling systems, as well as in understanding the behavior of the atmosphere and oceans.
Golden rules for NURSES
27. The range of marking in glass/clinical thermometer is 95-110° F and 35-43.3°C.
Glass or clinical thermometers typically have a range of markings from 95-110°F (Fahrenheit) and 35-43.3°C (Celsius), which is the normal range of human body temperature.
The thermometer works by using a liquid, usually mercury, that expands or contracts as it is heated or cooled.
The length of the liquid column inside the thermometer changes depending on the temperature, and this is what is used to determine the temperature reading.
It is important to use the thermometer correctly and to read the markings accurately to get an accurate measurement of body temperature.
Golden rules for NURSES
28. Normal Rectal temperature is 99.6° F (37°C) (1°F ) higher than oral temperature)
The normal rectal temperature is generally considered to be about 1°F (0.6°C) higher than the normal oral temperature, which is typically around 98.6°F (37°C).
This is because the rectum is a more accurate indicator of core body temperature, as it is located closer to the internal organs and is not affected by external factors such as food or drink.
However, rectal temperature measurement is generally reserved for medical purposes and is not recommended for routine temperature checks at home.
Oral temperature measurement is a more convenient and less invasive method that can provide a good approximation of core body temperature.
Golden rules for NURSES
29. Rectal temperature is the most reliable
Rectal temperature is generally considered to be the most reliable method of measuring body temperature because it provides a more accurate reflection of core body temperature.
This is because the rectum is located in the central part of the body, close to the internal organs which generate heat, and is not affected by external factors such as food or drink.
However, rectal temperature measurement may not be suitable for all individuals, especially for those who are uncomfortable with the procedure, those who have certain medical conditions, or those who have undergone rectal surgery.
Oral temperature measurement is a convenient and non-invasive alternative that can provide a good approximation of core body temperature for most people.
Other methods of temperature measurement include axillary (underarm) measurement, ear measurement, and forehead measurement, which may be suitable for certain populations or situations.
Golden rules for NURSES
30. Relapsing fever: Fever episodes are separated by intervals of normal temperature for days or weeks
Relapsing fever is a type of fever caused by certain bacterial infections, such as Borrelia species.
The fever episodes in relapsing fever are characterized by sudden onset of high fever, chills, headache, muscle aches, and other flu-like symptoms.
These episodes typically last for several days to a week or more, and are then followed by a period of normal temperature, which can last for days or weeks.
During the periods of normal temperature, the patient may feel completely well and may not have any symptoms.
However, the fever episodes can recur, often with different symptoms or severity, leading to a relapsing pattern of illness.
Treatment for relapsing fever typically involves antibiotics, such as doxycycline or penicillin, and may require several courses of treatment to fully eradicate the bacteria.
Golden rules for NURSES
31. Rigor: Sudden rise in body temperature with shivering as seen in malaria.
Rigor is a medical term used to describe a sudden onset of fever with chills and shivering. In the context of malaria, rigor is a common symptom that occurs during the febrile (fever) episodes, which are a hallmark of the disease.
Malaria is a parasitic infection caused by Plasmodium species, which are transmitted to humans by the bite of infected mosquitoes.
The febrile episodes in malaria are typically cyclical, with sudden onset of high fever, rigor, and other flu-like symptoms such as headache, muscle aches, and fatigue.
The fever may last for several hours to a few days, and is then followed by a period of normal or subnormal temperature.
The cyclical nature of the fever episodes is a key diagnostic feature of malaria, and helps to distinguish it from other febrile illnesses.
Treatment for malaria typically involves antimalarial medications, such as chloroquine, artemisinin-based combination therapy (ACT), or other drugs depending on the species of Plasmodium involved and the location of the infection.
Golden rules for NURSES
32. Increased depth of breathing with normal respiratory rate is called Hyperpnea.
Hyperpnea is an increase in the depth and intensity of breathing, without an increase in the respiratory rate.
It is often seen during exercise or other physical activity, as the body needs more oxygen to meet the increased demand.
It can also occur in response to certain medical conditions, such as metabolic acidosis or congestive heart failure.
Golden rules for NURSES
33. Cheyne-Stokes Respiration is characterized by altered period of Tachypnea and Apnea.
Cheyne-Stokes respiration is a type of abnormal breathing pattern that is characterized by a cycle of alternating periods of tachypnea (rapid breathing) and apnea (temporary cessation of breathing).
The cycle typically lasts between 30 seconds to 2 minutes, and can be seen in patients with various medical conditions, such as heart failure, stroke, and traumatic brain injury.
It is caused by an abnormality in the respiratory centers in the brain, which affects the regulation of breathing.
Golden rules for NURSES
34. Pulse deficit refers to the difference between apical pulse and radial pulse.
Pulse deficit is a condition where there is a difference between the apical pulse (the heartbeat heard through a stethoscope over the apex of the heart) and the radial pulse (the pulse felt at the wrist).
It occurs when some of the heartbeats are not transmitted to the peripheral arteries, leading to a discrepancy between the apical and radial pulse rates.
Pulse deficit can be caused by various medical conditions, such as atrial fibrillation, premature ventricular contractions, and heart block. It is often an indication of an underlying heart problem and should be evaluated by a healthcare provider.
Golden rules for NURSES
35. A Blood Pressure Cuff that is too large will give a falsely low reading of BP.
No, that is not correct.
A blood pressure cuff that is too large will actually give falsely high readings of blood pressure.
This is because the cuff will not be able to adequately compress the artery, leading to an overestimation of the blood pressure.
Conversely, a cuff that is too small will give falsely low readings of blood pressure, as it will compress the artery too much, leading to an underestimation of the blood pressure.
It is important to use the appropriate size of blood pressure cuff for accurate readings of blood pressure.
Golden rules for NURSES
36. Beneficence: Doing good for clients and providing benefits balanced against risk.
Beneficence is one of the four main ethical principles in healthcare, which refers to the obligation of healthcare providers to do good and to promote the well-being of their clients.
This principle requires that healthcare providers act in the best interests of their clients and provide care that maximizes benefits and minimizes risks.
Beneficence also requires that healthcare providers make decisions that are based on the best available evidence and that they continually seek to improve the quality of care that they provide.
Balancing the benefits of treatment against the risks is an important aspect of beneficence, as healthcare providers must weigh the potential benefits of a particular treatment against the potential risks and side effects in order to make informed decisions about the best course of action for their clients.
Golden rules for NURSES
37. Isotonic solutions allow free movement of water across the membrane without changing concentration of solutes on either side. E.g. 0.9% NaCl.
An isotonic solution is a solution that has the same concentration of solutes as the fluid inside the cells of the body.
When an isotonic solution is administered, water moves freely across the cell membrane in both directions, without changing the concentration of solutes on either side of the membrane.
This is because the concentration of solutes in the isotonic solution is equal to the concentration of solutes inside the cells, so there is no gradient to drive the movement of water in one direction or the other.
One example of an isotonic solution is 0.9% NaCl (normal saline), which is commonly used for intravenous fluid administration to replace lost fluids and electrolytes in the body.
Golden rules for NURSES
38. Hypertonic solution: Fluids with solutes more concentrated than in cells, e.g. 5% dextrose.
No, that is not entirely correct.
A hypertonic solution is a solution that has a higher concentration of solutes than the fluid inside the cells of the body. When a hypertonic solution is administered, water moves out of the cells and into the extracellular fluid, causing the cells to shrink.
This is because the concentration of solutes in the hypertonic solution is greater than the concentration of solutes inside the cells, creating a gradient that drives the movement of water out of the cells.
An example of a hypertonic solution is 3% saline, which is used to treat hyponatremia (low sodium levels). 5% dextrose is actually an isotonic solution, because dextrose (a form of glucose) is rapidly metabolized by the body, leaving only water and a small amount of electrolytes in the solution. When 5% dextrose is administered, it initially acts as an isotonic solution, but once the dextrose is metabolized, the remaining fluid becomes hypotonic (lower concentration of solutes than inside the cells).
It is important to note that the effects of hypertonic and hypotonic solutions on the body depend on the concentration of the solutes in the solution, as well as the rate and volume of administration. Administration of hypertonic or hypotonic solutions must be carefully monitored to avoid adverse effects on the body.

2 notes
·
View notes
Text
Unlocking the Mind: The Transforming Journey of an Ayahuasca Ceremony
The Amazon indigenous ceremonies have been administered by Ayahuasca, a sacred drink from plants for spiritual awakening and healing. Such growing interest in psychedelic therapy, directed by holistic interest, has led many seekers to shamanic retreats for the first-hand experience of deep effects. This article looks into what an Ayahuasca ceremony is, the science behind the use, and what the participants should expect from the experience.
What Is the Ceremony of Ayahuasca?
Ayahuasca ceremony is a traditional healing practice where a potent brew is consumed, made from Ayahuasca vine, Psychotria viridis leaves, and DMT, by Amazonian indigenous people. Usually, there is a shaman to guide along this spiritual journey. All the intentions which have been put to make things take their time at this ceremony include quieting the mind for long introspection, healing, and immediate personal development.
Participants endure such vivid examples and emotional evaporation, which are expected to rid the individual of any negative or haunting experiences that might affect an individual's growth. Actually, it has become a sacred ceremony, and now, attention is being given to these relatives with remedy power and possible spiritual insight.
The Science Behind Psychedelic Therapy
Ayahuasca therapy has received significant scientific validation through evidence of treatment efficacy for mental health disorders. DMT, the active ingredient in Ayahuasca, serves to link serotonin receptors in the brain and trigger an inquiry into a well-defined emotional environment.
According to research, Ayahuasca can lessen depressive symptoms and symptoms of PTSD and/or addiction via increased neuroplasticity and connectedness-with-others experience. This has thus given birth to its ever-growing place in the integration of psychedelics with therapy, making it worthy of offering psychological healing.
The Role of a Shamanic Retreat
An Ayahuasca ceremony takes place in many individuals' minds as the option for deep healing and personal growth, found in shamanic retreats that provide an authentic and controlled environment. These retreats place great importance on ritual, intention, and setting, thus enabling a safe and meaningful journey.
Participants often engage in dietary restrictions and meditative practices to facilitate openness. The retreat provides the structure within which support, emotional healing, and integration practices assist individuals in their processing of experiences.
The Ayahuasca Experience: What to Expect
The Ayahuasca encounter can be described as very personal, ensuring the experience is different for everyone who attends. The visions may present anything from vivid imagery to deep contemplations about life and existence. Emotions can be deeply felt; repressed traumas can be awakened for healing.
Physical effects such as nausea and vomiting are common; vomiting is considered a kind of purging or cleansing from any negativity and a release of bad energies. Nevertheless, once purging stops, we then have greater awareness, inner peace, and permanent transformation.
Conclusion
An Ayahuasca ceremony encompasses much more than a psychedelic experience. The spiritual and therapeutic aspects usher in opportunities for some serious personal development. With the help of the shamanic retreat, one can sufficiently navigate this powerful ritual safely and intentionally. With research validating its advantages, Ayahuasca provides a real opportunity for healing and self-discovery. The few attracted to embracing its transformative power should consider a well-guided retreat along this changing pathway.
0 notes
Text
Treatments of Bulimia Nervosa THE BEST OPTION Evaluation of Combined Therapy for Bulimia Nervosa Description and Significance Bulimia nervosa, simply bulimia or BN, refers to uncontrolled overeating or binging and then eliminating what has been eaten (SJH, 2012; Grange et al., 2004). Recent reports show alarming increases in the incidence, which now adolescents and pre-adolescents. The latest population statistics say that about 27.3 of the U.S. population is between 12 and 19 years old. BN affects up to 3% of these young people 15-18 years old at peak (SJH, Grange et al.). Brief Description of BN BN consists of eliminating or purging ingested food through induced vomiting, inappropriate use of laxatives or diuretics, fasting or extreme exercise to control weight (SJH 2012; Grange et al., 2004). The exact cause or causes are still unknown. But some factors are believed to contribute to it. These are cultural ideals and social attitudes about body appearance, self-evaluation on the basis of body weight and shape and family problems. Self-consciousness, especially about physical appearance, is most common and strongest in adolescence (SLH, Grange et al.). The common symptoms indicative of BN include low or normal body weight viewed as overweight, recurring binge eating and the fear of not stopping it, self-induced vomiting, excessive fasting, excessive exercising, ritualistic and peculiar eating habits, inappropriate laxative use, irregular or no menstruation, anxiety, depression, scares at the back of the fingers from induced vomiting and over-achieving behavior (SJH 2012; Grange et al., 2004). Usual treatment is through a combination of individual therapy, family therapy, behavior change and nutritional adjustment. Treatment is decided after an evaluation of the person and his or her family. Additional medication may be prescribed or administered if depression is also present. Parents are counseled to be supportive of the patient. Hospitalization may also be required if case of complications like weight loss and malnutrition (SLH, Grange et al.). Recent evidence suggests fluoxetine as the only USFDA-approved selective serotonin-reuptake inhibitor or SSRI for BN in adolescents and pre-adolescent persons (Blake & Rich, 2008). It is also more effective and beneficial than placebo. In combination with cognitive behavioral therapy or CBT, it is even better and superior to fluoxetine alone, CBT alone or placebo, according to trial results. Other drugs are citalopram or escitalopram, sertraline, paroxetine, and venlafaxine (Blake & Rich). Relevance to Clinical Care and Nursing The increase of BN incidence and prevalence among adolescents and pre-menarchial adolescents are specifically alarming to the health care profession (Grange et al., 2004). Partial eating syndromes add to the alarming situation. Community samples suggest that 10-50% of them develop BN yet diagnostic tests revealed that only 1-5% of the girls who responded reflected the BN condition. This meant that there are those whose symptoms have not been recognized and recorded in the statistical manual. These partial eating syndromes are likely to grow and become full-blast (Grange et al.). Randomized Clinical Trials 1. Solomando et al. (2008) summarized recent evidence drawn from the clinical guidelines of the National Institute for Health and Clinical Excellence and high-quality systematic reviews on the use of CBT for treating children and adolescents with mental health problems, such as BN. The synthesis was limited to systematic reviews in identifying and examining the most reliable evidence available. The outcomes yielded the most reliable evidence of potential benefit or the lack of it for CBT. Data drawn from the meta-analyses of randomized controlled trials offered the best evidence for CBT in treating children and adolescents with generalized mental disorders, such as generalized anxiety disorder, depression, obsessive-compulsive disorder and post-traumatic disorder. There is limited evidence in efficacy for ADHD and other antisocial behavior, psychotic and related disorders, substance misuse, self-harm behavior and eating disorders (Solomando et al.). This is level-1 evidence, which is systematic and can be generalized for mental health problems but not for eating disorders like BN. 2. Goodyer S. et al. (2007) performed a randomized controlled superiority trial in order to determine the effectiveness of SSRIs and CBT in the short-term as compared with an SSRI and clinical care alone in adolescents with moderate to severe major depression, as co-occurring in BN. The team surveyed 208 adolescents, aged 11-17, from 6 outpatient clinics in Manchester and Cambridge. They were diagnosed with major or probable major depression and unresponsiveness to a brief initial intervention. Included were adolescents with suicidal tendencies, depressive psychosis, and conduct disorders. The team administered SSRI and routine care to 103 respondents and SSRI, routine care and CBT to 105 for 12 weeks and maintenance for 16 weeks. Secondary measures were change in scores on moods and feelings through a questionnaire, the revised children's rating scale, the children's global assessment scale, and the clinical global impression improvement scale. Results yielded no evidence of efficacy of combined CBT and SSRIs with routine clinical care on short-term as contributing to improvement by 28 weeks for the respondents. This was in comparison with routine clinical care and SSRI alone (Goodyer et al.). This is a Level-2 evidence of a single experimental study, which can be generalized for short-term generalization. 3. The TADS Team (2007) performed randomized controlled trial on the effectiveness of a combination of treatments on adolescents with major depressive disorder. These treatments were fluoxetine hydrochloride therapy, CBT and their combination. The RCT was conducted on 320 participants, aged 12-17, in 13 academic community sites for 36 weeks. The team, an independent evaluator, used the Children's Depression Rating Scale. CBT and combination therapies were not masked but placebo and fluoxetine therapies were double blind for 12 weeks. The treatments were un-blinded afterwards. The placebo group was excluded in these analyses. Findings showed that treatment with fluoxetine alone or in combination with CBT sped up the rate of improvement. The addition of CBT increased safety levels. The combination appeared superior to either in treating depression, which frequently accompanies BN. This is level-1 evidence, which can be generalized for depression (TADS Team). 4. Brent (2008) and his team, in a separate RCT, found that the combination of CBT and a change of SSRIs would raise clinical response for adolescents with depression who were unresponsive to SSRI as an initial treatment. The team's aim was to evaluate and compare the effectiveness of four treatment alternatives on 334 patients, aged 12-18, from 6 U.S. academic and community clinics from 2000-2006. The team switches between SSRIs and CBT and compared the treatments for 12 weeks. Venlafaxine with CBT was also tested. The outcome measures used were the Clinical Global Impressions-Improvement Scale and the Children's Depression Ration Scale (Brent et al.). This is a Level -3 evidence as it was quasi-experimental. 5. Walkup (2008) and his team similarly concluded that both CBT and SSRI reduced severe anxiety symptoms in children and adolescents to a superior level. They conducted an RCT to explore the relative or combined efficacy of these treatments on 488 participants, aged 7-17 with varying diagnoses of anxiety disorders. The participants went through 14 CBT sessions and received the SSRI sertraline, a combination of CBT and sertraline or a placebo for 12 weeks. The team used categorical and dimensional ratings at baseline in weeks 4, 8 and 12. Results showed a high 80% of improvement from combination therapy, according to the Clinician Global Impression Improvement test. The Pediatric Anxiety Rating Scale yielded a similarly high pattern of response, particularly for the combination therapy. Other symptoms associated with CBT, such as insomnia, fatigue, sedation and restlessness, were also reduced (Walkup et al.). This is level-2 evidence, which can be generalized for anxiety, which often accompanies BN. 6. Hay (2008) and his associates conducted 26 systematic reviews, RCTs and observational studies on the effectiveness of treatments on young BN patients. These were retrieved from Medline, Embase, The Cochrane Library, among others, up to June 2007. They used a GRADE evaluation in assessing the quality of evidence. The team found 17 interventions for BN. Summary of results showed that up to 1% of young women, who are body conscious, develop BN; they were of normal weight; half of them would have fully recover in 10 years' time; CBT alone could produce improvement compared with no treatment; CBT is comparably effective as other treatment in reducing symptoms; the efficacy of other psychological therapies remained unknown; and some SSRIs can work against symptoms better than can placebos (Hay et al.). This is a level-1 evidence that can be generalized. 7. Dubicka et al. (2010) attempted to resolve the conflicting findings from RCTs on the efficacy of SSRIs combined with CBT. In determining whether CBT produces additional benefits to SSRI treatment on adolescents suffering from depression, the team performed a meta-analysis of RCT s on new lines of SSRIs in combination with CBT on sample adolescents. These participants, aged 11-18, were diagnosed with depression as defined by DSM-IV. They were given a new type of SSRI in combination with CBT and the results were compared with those with SSRI without CBT. The focus was on depression and impairment scores, overall improvement, suicidality, and adverse effects. Results showed on significant benefit from the combined treatment on depression symptoms. A significant advantage was computed for impairment in the short-term of 12 weeks only. The combination, therefore, was found to produce limited advantage due to the varied sampling and methodology. Future research should focus on predictors of response and clinical components (Dubicka et al.). This is level-1 evidence, which can be generalized. 8. A single-site study, conducted by Riggs and her team (2007) aimed at comparing the effect of fluoxetine hydrochride against that of placebo in treating depression and related disorders in adolescents. They performed a randomized controlled trial from May 2001 to August 2004 on 126 adolescent volunteers, aged 13-19, from the community and according to the requirements of DSMMD for 16 weeks. Measures used were the Childhood Depression Rating Scale-Revised and Clinical Global Impression Improvement and self-reported symptoms for the past 30 days. The results showed that fluoxetine with CBT appeared to be similarly safe and effective for depression in participants with substance use disorder and those depressed but not into substance use. The researchers surmised that CBT may have produced the higher-then-expected response and thus blur the efficacy result (Riggs et al.). This is level-2 evidence, which can be generalized. 9. Hall (2008) and her team conducted multiple consistent RCTs to determine the most effective treatment or treatments for BN in adolescents. The group used a Cochrane review of 40 RCTs of 1-220 patients at a mean of 60 for 16 weeks median and a follow up median of 7.5 months. At that time of the test, CBT was considered the most effective. It confirmed that, compared with no treatment, CBT substantially improved symptoms. CBT also proved more significantly efficacious than other forms of psychotherapy in inducing eating abstinence. Guided self-help alone did not reduce binge and purge episodes. Results of this test and other case-control studies provided evidence that pharmacotherapy with anti-depressants are effective in treating BN. The combination is even more effective when psychotherapy is added. Remission rates were low but long-term follow-up data were limited (Hall et al.). 10. Schmidt (2007) and his associates conducted a randomized control trial of family therapy and CBT guided self-care for participating adolescents diagnosed with Bulimia Nervosa and related disorders. Their objective was to compare the effectiveness and cost-effectiveness of these two types on 85 respondents from the United Kingdom. Of the total, 41 were assigned at random to the family therapy group and 44 to CBT guided self-care. The primary measures used were abstinence from binge eating and vomiting for 6 months and then at 12 through interviews. The secondary measures included the symptoms and costs of care. The primary hypothesis was that family therapy would induce higher rates of abstinence and induced vomiting at treatment and follow-up. The secondary hypothesis was that guided self-care would be more inexpensive than family therapy. Results showed that CBT-guided self-care had a slight advantage over family therapy. It induced faster reduction of bingeing, cost less and was more acceptable to adolescents with BN (Schmidt et al.). This is level-2 evidence and can be generalized. Synthesis Of the 10 RTCs, 7 confirm the effectiveness of CBT in treating the symptoms of Bulimia Nervosa in combination with SSRIs. The combination is superior but only in the short-term (Boodyet et al., 2007). It accelerates improvement with SSRIs as well as raises the safety level (The TADS Team, 2007). The combination is better than simply switching SSRIs without the combination (Brent et al., 2008). Walkup (2008) and his team agree. Hay (2008) and his team also say that CBT alone will work on BN. Riggs (2007) and team that the combination will work. And Schmidt (2007) say the combination is more effective than family therapy. Of the 7 who confirm the benefits of CBT, 5 agree that the combination of CBT and SSRIs is the best treatment for BN. Recommendation CBT has been described as a talking therapy, which endeavors to solve emotional or behavioral problems and behaviors through a systematic approach (Osterhout, 2012). It appears best to manage BN through an interdisciplinary approach. This will involve and include a primary care provider, a psychiatrist, a psychotherapist, and a dietitian. It is preferable for the psychiatrist or psychotherapist to possess expertise in managing eating disorders. The dietitian should review and oversee the patient's nutritional rehab. A dentist and other health experts may also be needed. The overall aims should be to reduce or eliminate binge eating and purging, treat the complications, prevent them and enhance her overall health. BIBLIOGRAPHY Blake, J. G and Rich, J. (2008). Which drugs are most effective for moderate to severe depression in adolescents? Vol 57 # 5 The Journal of Family Practice: Quadrant Health Com. Inc. Retrieved on February 29, 2012 from http://www.jfponline.com/Pages.asp?AID-6182 Brent et al. (2008). Switching to another SSRI or to Venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression. The Journal of the American Medical Association: American Medical Association. Retrieved on February 29, 2012 from http://www.jama.ama-assn.org/content/299/8/901.full?linkType=FULL&journalCode=jama&resid=299/8/901 Dubicka, B. et al. (2010). Combined treatment with cognitive-behavioral therapy in adolescent depression: meta-analysis. Vol 197, The British Journal of Psychiatry: The Royal College of Psychiatrists. Retrieved on February 29, 2012 from http://www.bjp.rcpsych.org/content/197161433.full Goodyer, S., et al. (2007). Selective serotonin reuptake inhibitors and routine specialist care with and without cognitive behavior therapy in adolescents with major depression: randomized controlled trial. British Medical Journal: BMJ Publishing Group Ltd. Retrieved on February 29, 2012 from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1925185 Grange, D. le, et al. (2004). Bulimia nervosa in adolescents: a disorder in evolution? Vol 158 Archives of Pediatric and Adolescent Medicine: University of Chicago. Retrieved on February 29, 2012 from http://www.archipedi.ama-assn.og/cgi/reprit/158/5/478.pdf Hall, M.N. et al. (2008). Treatment of Bulimia Nervosa. Vol 77 (11) American Family Physician: Family Physicians Inquiries Network. Retrieved on March 4, 2012 from http://www.aafp.org/afp/2008/0601/p1588.html Hay, P.J., et al. (2008). Bulimia nervosa. Clinical Evidence: BMJ Publishing Group Lt. Retrieved on February 29, 2012 from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2907970 Osterhout, C. (2012). Bulimia Nervosa treatment and management. Medscape News:P Medscape: WebMD LLC. Retrieved on March 6, 2012 from http://www.emedicine.medscape.com/article/286485-treatment Riggs, P. d., et al. (2007). A randomized controlled trial of fluoxetine and cognitive behavioral therapy in adolescents with major depression, behavior problems, and substance use disorders. Vol 161 (11) Archive Pediatric and Adolescent Medicine: American Medical Association. Retrieved on February 29, 2012 from http://www.archpedi.ama-assn:org/cgi/content/161/11/1026 Schmidt, U. et al. (2007). A randomized controlled trial of family therapy and cognitive behavior therapy guided self-care for adolescents with Bulimia Nervosa and related disorders. Vol 164 (4) American Journal of Psychiatry: American Psychiatric Association. Retrieved on March 3, 2012 from http://www.ajp.psychiatryonline.org/article.aspx?volume=164&page=591&journalID=13 Solomando, A.M., et al. (2008). Cognitive behavioral therapy for children and Adolescents. 21 (4) Current Opinion in Psychiatry: Lippincott Williams & Wilkins. Retrieved on February 29, 2012 from http://www.medscape.com/viewarticle/575409 SJH (2012). Bulimia nervosa in adolescents. St. Joseph's Hospital and Medical Center: Catholic Healthcare West. Retrieved on February 29, 2012 from http://www.stjosephs-phx.org/Medical_Services/Adolescent_Medicine/221179 TADS Team, The (2007). The treatment for adolescents with depression study. Vol 64 (10) Archives in General Psychiatry: American Medical Association. Retrieved on February 29, 2012 from http://www.archpsych.ama-assn.org/cgi/content/full/64/10/1132 Walkup, J.T., et al. (2008). Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. New England Journal of Medicine: Massachusetts Medical Society. Retrieved on February 29, 2012 from http://www.nejm.org/doj/full/10.1056/NEJMoa0804633 Read the full article
0 notes
Photo

The High Priestess. Art by Cristy C. Road, from Next World Tarot.
When your energy centers are aligned and your trauma is suddenly unfamiliar, you experience awakening, and evidence of your personal power sprawls before your world of wilted books and half-written love letters. The High Priestess protects the threshold between self-doubt and enlightenment. She is self-preserving. Understanding that her powers are sacred — doubted by colonizers, but revered by her family and the ghosts of her ancestors. She speaks through her intuition and holds space to decipher whether we need to administer a public outcry or quietly cultivate a long term solution.
The High priestess exists between the familiarity of her tropical roots, the abundance and fertility of an organic harvest, and the light of the moon. She is cultivated and awoken. Harnessing her higher self in the comfort of her own safety. The High priestess holds these solutions in her third eye, nestled in a crevice behind the Hypothalamus, on the Pineal Gland.
The Pineal Gland is a small pine cone shaped organ that releases melatonin and serotonin (responsible for emotional states of well-being), and DMT — the spirit molecule. While humans are born with a strong sense of connection to the pre-colonial practice of knowing the spirit without its commercialized decline; the pineal gland's function can go awry by adolescence, considering the toxins present in food and hygiene products that humans consume.
The pineal gland is an endangered portal to intuition — the 6th Chakra, the third eye, the perception of metaphysical realities and energetic wisdom. This is felt through the gut; as thunder when we experience truth and agency, or as a swarm of butterflies who speak for your heart when you are scared or in love. Intuition is a glowing inner knowledge that makes you cry, keeps you warm, or makes you cringe. The High Priestess asks you to seek knowledge behind these sensations; trust them and honor them, as they are literally your inner truth.
#Cristy C. Road#Next World Tarot#The High Priestess#Major Arcana#Tarot#Tropical#Favorites#Racial Diversity
21 notes
·
View notes
Text
#22: Black Widow [Marvel]

Hey there, my dearies! It's been a while. I have no excuse, it was just a low-serotonin time of year.
Yes, I know I teased Claude last time, but since we've had Marvel Studios return to the silver screen with Black Widow, I thought we might take a shot at building the leading lady of the movie: Natalia Alianovna Romanova, also known as Natasha Romanoff, also known as the main Black Widow. We're going to build her according to the comic book main universe, Earth-616.
Next Time: We conClaude the Fire Emblem request, I promise.
Let's see what is needed for this spider to bite into D&D:
International Super Spy... SUPER SPY: Natasha is trained in the art of espionage, intelligence gathering and disguise. We need to be able to blend easily with any crowd and act as if we belong everywhere.
Soviet Super Soldier: While not as strong and effective as Captain America and the Red Guardian, Natasha had been administered a Red Room version of the Super-Soldier Serum, which enhanced her physical attributes to the peak of human potential.
Jacqueline-of-All-Trades: As part of her spy training, Natasha had to become proficient in many skills, included but not limited to: dancing, acting, linguistics, hacking, and acrobatics.
---
As she's enhanced, we can easily categorize Natasha as a Variant Human. We get a +1 to two abilities of our choice (Dexterity and Strength), we know how to speak Common and one other language of our choice, we gain proficiency in one skill of our choice (Acrobatics), and we get to pick a feat. The Linguist feat gives us a +1 to our Intelligence, lets us learn three more languages of our choice, and we can create codes and ciphers that cannot be decrypted unless one beats the DC of [our Intelligence score (not modifier) + our proficiency bonus] or uses magic.
For our background, we shall erase our true self and assume a new identity with the Faceless background from Baldur's Gate: Descent into Avernus. We get proficiency in Deception and Intimidation skills, and with the Disguise Kit. We also learn one more language. Our background feature, Dual Personalities, lets us create an alter-ego which we use when interacting with people around. We can even introduce ourselves as our alter-ego to our own party members in order to ensure our anonymity.
ABILITY SCORES
Dexterity will be our primary ability. We're nimble, we're slick, we can fight in heels. Charisma is next, we're a great seductress and we can even trick the Trickster God into revealing his plans. Follow that up with Constitution, Black Widow is known to take hits and heal pretty fast.
Intelligence will be next, we're a learned individual and we need the Big Brain for all those languages and cipher-making skills. Strength is a little lower than I want to, especially since Natasha in the comics is capable of lifting 500 lbs) but we can fix it later. Finally, we're dumping Wisdom; we're not silly, we just need other abilities more.
CLASS
I think this one's pretty obvious, there is a very obvious way to make a spy in D&D, but I'm going to try and spice it up a little:
Level 1 - Rogue: Starting with the sneakiest class! Rogues get the d8 Hit Dice, [8 + our Constitution modifier] initial Hit Points, and get proficiency with light armour, simple weapons, hand crossbows, longswords, rapiers, shortswords, and thieves' tools. Our saving throws are Dexterity and Intelligence, and we get to pick four skills from the Rogue skill list (Investigation, Persuasion, Sleight-of-Hand, and Stealth). For Natasha, I suggest going with regular leather armour, daggers, and a hand crossbow to simulate Widow's Bite (ask your DM if it can be flavoured as a wrist-mounted crossbow device).
Rogues begin with Expertise - we get to choose two skills we're proficient in and double our proficiency bonus for any checks involving those skills. Let's get better with Acrobatics and Sleight-of-Hand.
We also know Thieves' Cant, a special system of phrases and symbol used by Rogues to contact other Rogues without being discovered.
Finally, we know how to perform Sneak Attack. Despite the name, we don't need to be sneaky when executing it. Whenever we attack with an advantage on our turn (or the target is within 5 feet of another creature hostile to it), we can add extra 1d6 damage to our strike. It can be only done with a ranged weapon, or one with Finesse property.

Level 2 - Rogue: We get Cunning Action. Our agility allows us to shorten the time we need to perform certain tasks. We can now use the Dash, Disengage, and Hide action as a bonus action.
Level 3 - Rogue: Our Sneak Attack bonus damage becomes 2d6 now. We also get to pick our subclass, our Roguish Archetype. While Assassin seems like a very obvious choice, Natasha isn't really a killer exclusively. Instead, we're going to go with the Scout Archetype from Xanathar's Guide to Everything, as it embodies the "survival and stealth" approach to playing a Rogue.
Starting with Skirmisher, we can use a reaction to move up to half of our speed when the enemy finishes its turn within 5 feet of us. Doing so does not provoke attacks of opportunity. Survivalist gives us proficiency in Nature and Survival skills, and our proficiency bonus is doubled for all checks involving those (effectively giving us more Expertise).
Additionally, if your DM allows it, you can pick up the Steady Aim optional feat from Tasha's Cauldron of Everything. As a bonus action, we can get an advantage on an attack roll, provided we sacrifice our movement for the current turn. Afterwards, our speed becomes 0 until the end of the turn.
Level 4 - Rogue: Time for our first Ability Score Improvement of the build. Let's raise our Constitution and Intelligence this time. We'll focus on unarmed combat a little later down the build.
Level 5 - Rogue: Our Sneak Attack bonus becomes 3d6. We get Uncanny Dodge, which lets us take half damage of any attack that hits us and that we can see.
Level 6 - Fighter: Time to show that CQC some love. When we multiclass into a Fighter, we get proficiency in light armour, medium armour, shields, simple weapons, and martial weapons. We get to pick our Fighting Style, and since we already have a Dexterity-based style with daggers, and a ranged style with our Widow's Bite, let's get Unarmed Fighting for times where we need to go into action without our toys. Our unarmed strikes now deal [1d6 + our Strength modifier] bludgeoning damage. If we aren't wielding a weapon or a shield, the d6 becomes d8. Additionally, if we are grappling a creature, we can deal 1d4 bludgeoning damage at the start of each of our turn.

We also get Second Wind, which represents Natasha's accelerated healing capabilities. Once per short or long rest, we can restore [1d10 + our Fighter level] Hit Points on our turn.
Level 7 - Fighter: We get Action Surge. Once per short or long rest, we can take one additional Action on our turn.
Level 8 - Rogue: Moving back into the sneaky super-spy territory, we get some extra Expertise. We can select two more skills we're proficient with to double our proficiency bonus. Let's get Deception and Investigation.
Level 9 - Rogue: Our Sneak Attack bonus becomes 4d6. We now get Evasion, which in my opinion is one of the better skills in the entire game. If we're within range of an AoE spell (such as Fireball) and a successful saving throw would make us take half damage, we instead take no damage (and we take half damage instead of full damage if we fail the throw).
Level 10 - Rogue: Halfway through the build and we get another Ability Score Improvement. Let's raise our Strength and, to start removing the negative modifier, Wisdom.
Level 11 - Rogue: Our Sneak Attack bonus becomes 5d6. We also get our first subclass upgrade: Superior Mobility. Our speed increases permanently by 10 feet.
Level 12 - Rogue: Another ASI! Let's bump our Dexterity by 2 points to get some better AC and Initiative.
Level 13 - Rogue: Our Sneak Attack becomes 6d6. We also unlock Reliable Talent, another very powerful skill. Whenever we must make a skill check related to a skill we're proficient with, any roll of 9 and lower becomes 10. Depending on a DM, this effectively removes a possibility of Natural 1s for our best skills.
Level 14 - Rogue: One more ASI. We can finally eliminate the negative modifier for Wisdom, and let's get one more point in Strength.
Level 15 - Rogue: Our Sneak Attack bonus becomes 7d6, and we get another subclass feature: Ambush Master. We have an advantage on Initiative rolls. Additionally, the first creature we hit during the first round of combat becomes an easy target; attacks against it have an advantage until the end of our next turn.

Level 16 - Rogue: We get Blindsense, which is yet another great feature... Man, Rogues really get some good stuff. We are now aware of any invisible or hiding creatures within 10 feet of us.
Level 17 - Rogue: Our Sneak Attack bonus becomes 8d6, and with Slippery Mind we get proficiency in Wisdom saving throw.
Level 18 - Rogue: Time for our final ASI of the build. Let's cap our Dexterity to 20.
Level 19 - Rogue: Our Sneak Attack bonus becomes 9d6. We also get our final subclass upgrade: Sudden Strike. If we use the Attack action on our turn, we can make one more attack as a bonus action. This second attack can benefit from our Sneak Attack, even if we used it before, but we cannot Sneak Attack the same target twice on the same turn.
Level 20 - Rogue: Our capstone is Rogue 18, and we end this build with the Elusive feature. While we aren't incapacitated, no attack made against us can get an advantage.
---
And that's Natasha the Black Widow. Let's see what we got:
I'm gonna confidently say, we've made a pretty good infiltrator. With multiple languages, disguise kit, and 9 proficient skills out of 18 available (with 6 with Expertise), we've elevated the Red Room training into anime protagonist levels.
With a standard leather armour our AC is 16, we got a +5 to our Initiative, and we've 142 Hit Points on average.
We are not exactly a frontline fighter, though. It is better if we take the behind-the-scenes approach to combat. Utilizing covers and making sure we're not targetted by the heavy hitters.
---
Ah, this was fun. A nice warm-up before coming back to our regularly scheduled program. I hope you guys enjoyed this, and I'll see you for the next one!
- Nerdy out!
#marvel#mcu#avengers#black widow#natasha romanoff#dnd#d&d 5e#d&d build#dungeons and dragons#rogue#scout#fighter
14 notes
·
View notes
Text
Esketamine for Anxiety: A Novel Approach to Treatment
Introduction:
Anxiety disorders affect millions of people worldwide, leading to significant impairment in daily functioning and quality of life. Traditional treatments such as psychotherapy and selective serotonin reuptake inhibitors (SSRIs) have been the mainstay for managing anxiety, but not all individuals respond adequately to these interventions. Esketamine, a relatively recent addition to the psychiatric pharmacopeia, has emerged as a promising alternative for those with treatment-resistant anxiety. This article explores the use of esketamine in the context of anxiety disorders, shedding light on its mechanisms, efficacy, and potential impact on the future of anxiety treatment.
Understanding Esketamine:
Esketamine is a derivative of ketamine, a dissociative anesthetic that has been used for decades in medical and veterinary settings. Ketamine gained attention in the psychiatric community when researchers discovered its rapid and robust antidepressant effects, particularly in individuals who did not respond to traditional antidepressants. Esketamine is the S-enantiomer of ketamine and is the active component responsible for its psychoactive effects.
Mechanism of Action:
The exact mechanism of esketamine's action in treating anxiety is not fully understood, but it is believed to involve the modulation of glutamate, the most abundant neurotransmitter in the brain. Unlike traditional antidepressants that primarily target serotonin, norepinephrine, or dopamine, esketamine works on the glutamatergic system. It acts as an N-methyl-D-aspartate (NMDA) receptor antagonist, leading to increased synaptic glutamate levels.
The rapid onset of action seen with esketamine is one of its distinguishing features. While traditional antidepressants may take weeks to produce therapeutic effects, esketamine can induce noticeable improvements within hours or days. This swift response is particularly valuable for individuals experiencing acute anxiety or those at risk of self-harm due to severe symptoms.
Clinical Trials and Efficacy:
Clinical trials have been conducted to evaluate the efficacy of esketamine in various anxiety disorders, including generalized anxiety disorder (GAD), social anxiety disorder (SAD), and post-traumatic stress disorder (PTSD). Results have shown promise, especially in individuals who did not respond adequately to conventional treatments.
In a landmark study, researchers investigated the use of esketamine nasal spray in patients with treatment-resistant depression and comorbid anxiety. The study demonstrated significant reductions in anxiety symptoms, suggesting that esketamine might be a viable option for individuals with both depressive and anxiety disorders.
Safety and Side Effects:
While Esketamine For Anxiety has shown efficacy, concerns about safety and side effects exist. Common side effects include dissociation, dizziness, and increased blood pressure. Dissociation is a temporary state where individuals may feel disconnected from their surroundings or have altered perceptions of reality. This effect is usually short-lived and tends to resolve on its own.
To mitigate potential risks, esketamine is administered in a controlled setting, typically in a healthcare provider's office. Patients are monitored closely during and after administration to ensure their safety. Additionally, individuals with a history of psychosis or certain medical conditions may not be suitable candidates for esketamine treatment.
Challenges and Future Directions:
Despite the promising results, esketamine faces challenges that warrant further investigation. The long-term safety profile, optimal dosing strategies, and potential for abuse are areas that require careful consideration. Ongoing research aims to address these concerns and refine the understanding of esketamine's role in anxiety treatment.
The future of esketamine in anxiety management also hinges on its accessibility. Currently, esketamine is administered in supervised settings, limiting its availability to certain populations. As research progresses, efforts to develop more user-friendly formulations or alternative delivery methods may broaden its reach and impact.
Conclusion:
Esketamine represents a paradigm shift in the treatment of anxiety disorders, offering a novel approach for individuals who do not respond to traditional interventions. Its rapid onset of action and distinct mechanism make it a valuable addition to the therapeutic arsenal for mental health professionals. As research continues, a more comprehensive understanding of esketamine's long-term effects, optimal use, and broader implications for anxiety treatment will emerge, potentially reshaping the landscape of psychiatric care.
0 notes