#mkpx
Explore tagged Tumblr posts
Photo

📽from the bali |a r c h i v ę s| with my gem, @mkpx . www.flowergypsies.com #flowergypsies #flowercrown #wanderlust (at Bali, Indonesia)
0 notes
Text
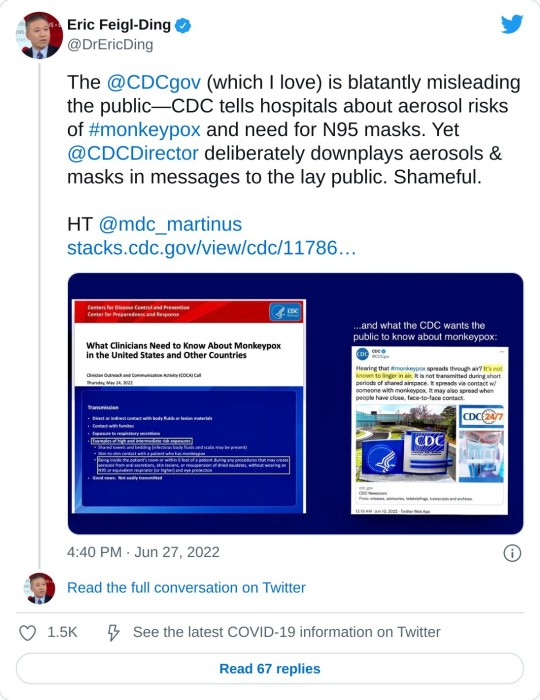
>2) Sometimes in life you have to call the CDC out and admit that the beloved world renowned public health agency you grew up loving, @CDCgov, is a mere shadow of its former self.@CDCDirector cannot tell lay public one thing & then tell clinicians something else on #monkeypox


#twitter#eric feigl ding#monkeypox#mkpx virus#mkpx#cdc corruption#gaslighting#pandemic#monkeypox pandemic#masking#world health organization
68 notes
·
View notes
Text
Medical experts and some pundits are raising alarm about the spread of monkeypox, a far more containable disease than Covid. But apparently because the public has been told to get used to endemic Covid, it’s supposed to resign itself to endemic Covid. A fresh report from IM Doc illustrates how appalling state of public health in America.
A little background courtesy Twitter:
From IM Doc at the start of the week:
Today a gay patient in his 30s showed up in the office. He is healthy and very athletic. He is a “boy” to another older gay man. They travel the world and are into serious gay fetish play. Spanking, bondage, discipline etc. Patient has had fever and chills and horrible headache for 3 days. A reticulonodular rash has developed but no vesicles yet. They have been playing in clubs, parties, and orgies in 4 major cities the past 2 weeks. There are so many things in that diagnostic differential but of course monkeypox is right up there. And of course NO TESTING IS AVAILABLE. I called all levels of health department and even CDC today. The CDC is voice mail hell. Never talked to a human. It took several hours for a health dept human but by then the patient was already gone potentially spreading the wealth everywhere. They are acting as if I was talking about the Martian Flu. Again, we have known about this two months now, and it was like I was asking for the Holy Grail. Testing? “I need to call so and so……not sure…..but I’ll get right back to you……..”. And don’t get me started about their handling of the quarantine. I have no idea if he is really a case. Multiple tests are pending. But not monkeypox. There is apparently no blood test for that. You have to swab the vesicles. But what if we do not have vesicles yet? Or if a patient may be past the vesicular stage? Crickets. I would like to think there is a baseline competence. But that is too much an ask right now. Again two months all over the news and this is what we have. We are a completely unserious nation.
Remember that IM Doc is in a wealthy destination in Flyover. Apparently the local public health officials not only think that monkeypox is exclusively a gay STD, but also that they can’t have it locally because there are no gay men in their part of the world. Did they miss Brokeback Mountain? Or the private jet landing schedule?
On top of that, the local public health officials appear unable to use a search engine. In fact, there are monkeypox tests, but as IM Doc did correctly infer, they can’t be used before the vesicles stage, which is 2-4+ days after lesions start forming. Oh, and monkeypox patients are contagious as soon as they start having lesions and potentially also during the prodome period, before rash starts.
From the CDC:
Persons with monkeypox will develop an early set of symptoms (prodrome). A person may sometimes be contagious during this period.
The first symptoms include fever, malaise, headache, sometimes sore throat and cough, and lymphadenopathy (swollen lymph nodes).
Lymphadenopathy is a distinguishing feature of monkeypox from smallpox.
This typically occurs with fever onset, 1–2 days before rash onset, or rarely with rash onset.
Lymph nodes may swell in the neck (submandibular & cervical), armpits (axillary), or groin (inguinal) and occur on both sides of the body or just one.
And the disease progression:
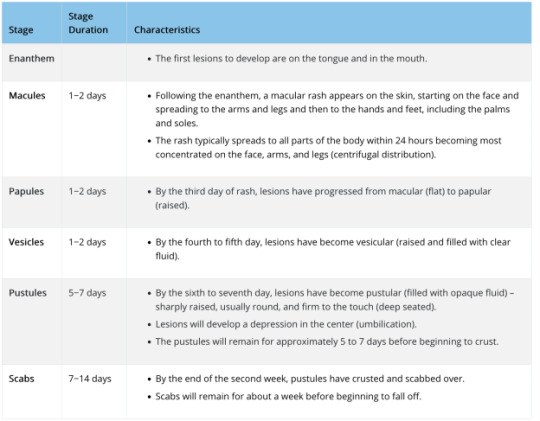
So let us return to IM Doc’s predicament. Yes, the CDC has been announcing that various labs are now testing for monkeypox. For instance, from a July 13 press release:
Starting today, Quest Diagnostics will begin testing for monkeypox. The company has developed a real-time polymerase chain reaction (PCR) test that uses patient swab specimens to qualitatively detect non-variola orthpoxviruses and monkeypox virus DNA. The test is now available to healthcare providers nationwide (except in New York)*…. Quest will offer monkeypox virus testing at the company’s advanced laboratory in San Juan Capistrano, Calif. and can accept specimens from anywhere in the country.* Quest’s testing will continue to increase the current capacity provided through CDC’s Laboratory Response Network (LRN), Labcorp, and Mayo Clinic Laboratories, providing testing capacity of up to 60,000 specimens per week by the end of July. On June 22, HHS announced that five commercial laboratory companies would soon begin offering monkeypox testing. Since then, CDC has shipped the tests to the laboratories and their employees have been trained on their administration, among other steps. Anyone with a rash that should talk to their healthcare provider about whether they need to get tested, even if they don’t think they had contact with someone who has monkeypox. Healthcare providers can order monkeypox virus testing from Quest as they normally would order other tests. People seeking testing for monkeypox must consult with their healthcare provider first; they cannot separately go to a Quest lab, submit a specimen, and request testing
This sounds easy-peasy, right? Except it isn’t. From the CDC Monkeypox: Preparation and Collection of Specimens (boldface ours):
Effective communication and precautionary measures between specimen collection teams and laboratory staff are essential to maximizing safety when manipulating specimens suspected to contain monkeypox virus…. Procedures and materials used for collecting specimens may vary depending on the phase of the rash (i.e., swab of lesion surface or crust from healing lesion). For initial laboratory testing of monkeypox virus specimens at Laboratory Response Network (LRN) laboratories or authorized commercial laboratories, the recommended specimen type is skin lesion material. Specifics on the acceptable specimen type accepted within these laboratories may vary.Please contact the appropriate public health department or commercial laboratory to determine acceptable specimens. For further characterization of the specimen at CDC, dry swabs of lesion material, swabs of lesion material in VTM, or crusts are acceptable. To ensure specimens are stored and shipped within the required timeframe, consultation with the CDC is suggested. Personnel who collect specimens should use personal protective equipment (PPE) in accordance with recommendations for healthcare settings. Specimens should be collected in the manner outlined below. When possible, use a plastic, sterile, leak-proof container rather than glass materials for specimen collection. Two swabs from each lesion should be collected for testing. Using two sterile synthetic swabs (including, but not limited to polyester, nylon, or Dacron) with a plastic, wood, or thin aluminum shaft, swab the lesion vigorously to collect adequate DNA. Do not use cotton swabs. It is not necessary to de-roof the lesion before swabbing. Break off the end of each swab’s applicator into a 1.5-or 2-mL screw-capped tube with O-ring or place the entire swab in a sterile container that has a gasket seal and is able to be shipped under the required conditions. Two swabs from each lesion should be collected, preferably from different locations on the body or from lesions which differ in appearance. Swabs and other specimens should each be placed in different containers. If using transport media, only VTM is accepted at CDC at this time; do not use universal or other transport media. Specimen collection, storage, and shipping of human specimens is subject to CLIA restrictions. Specimens being sent to CDC for testing should be stored refrigerated (2-8°C) or frozen (-20°C or lower) within an hour of collection. CDC 50.34 form must be included for each specimen. When possible, ship specimens on dry ice. Specimens received outside of acceptable temperature ranges will be rejected. Laboratory testing has indicated that the current monkeypox outbreak is associated with the West African clade of monkeypox virus. The U.S. government does not consider the West African clade of monkeypox virus as meeting the definition of Category A infectious substance under the Hazardous Materials Regulations (HMR). Therefore, specimens and material suspected or confirmed to contain the West African clade of monkeypox virus can be shipped as UN 3373 Biological Substance, Category B. See U.S. Department of Transportation’s (DOT) Transporting Infectious Substances Safely and Managing Solid Waste Contaminated with a Category A Infectious Substance (pg. 94) for further guidance. Refer to the Poxvirus Serology test on the CDC Test Directory for further specimen storage, packaging, and shipping instructions. For current information on the Molecular Detection test, please contact the CDC at [email protected] for details on collection, storage, packaging, and shipping of specimens.
Now perhaps this sort of specimen collection and shipment is routine for many small hospitals like IM Doc’s. But the repeated “Call the CDC for instruction” suggests otherwise. So even if IM Doc’s patient had monkeypox-looking pustules that could have been sampled and tested, neither the CDC nor the local health department did a damned thing to help.
From a later message, after I had informed IM Doc that there were monkeypox tests, but only of vesicles (as he’d inferred):
Is it not a sad state of affairs that you are able to find this and the public health dept did not know the first thing about this? I am thinking they are probably able to assist now after this incident yesterday, but it is the total lack of preparedness that is very disturbing. They did not know the first thing about testing. And from what I am told this PCR testing is on the vesicle swabs only. My questions remain. What if the patient is in a prodrome of fever and rash but no vesicles? What if the patient has already convalesced through the vesicles? What do we swab in those instances? Are we certain that every single monkeypox patient will have vesicles? What do we do when this is highly suspected and the patient is already having a high fever and pain and rash but no vesicles? And most importantly, should any of the examples above be placed into quarantine until further notice? The fact that none of these questions could be answered and still are not today, especially the quarantine of highly suspected patients, is of the most concern to me. These are simple obvious issues that any clinician would raise and it is as if they have never been thought of before. The patient from yesterday, for example, has been reported. Multiple blood tests for many other things done. Most of which are pending. I still do not know for sure his diagnosis, and he has no vesicles when I followed up with him today. And there is no quarantine at all. This just does not jive well in my opinion with the level of fear they are exhibiting about this getting out of control. This is what I have been talking about for the past two years. In the past, the CDC would have been all over making sure every primary care doctor in the USA knew exactly what the protocol was. I have heard or seen nothing. I go over my email daily. I have found nothing on their website that is more than simple platitudes. Certainly nothing that would guide me through the above questions. And to my disappointment, the health department personnel were in no better shape than I was. Just like Ebola, COVID, and West Nile virus, monkeypox is something no one of us has ever handled. I would have expected after two months for the entire system to be on the ball, and after our first scare in my area, it is clear we are nowhere near prepared. Acute public health issues like this are only as strong as the weakest link, and we failed yesterday. This departure from past behavior from the CDC has been the most difficult for us old docs to stomach.
And to add an additional point: the fact that there is a monkeypox test of some sort suggests that the CDC is in mission accomplished mode and isn’t pushing for the development of a blood test, which would enable clinicians to find the infection earlier (and perhaps later) than the skin-sampling ones do, and would also be less nasty to administer from the patient and practitioner perspective.
So we are well on the way to having monkeypox be as bad as it could be. Scientist GM added:
We actually have no idea how bad monkeypox is right now. Notice that there are no statistics released on how many of the cases are hospitalized, how many in ICU, etc. We had that reporting system fairly quickly with COVID back in 2020. And it is being rolled back now, with the move to weekly reporting in many places, likely to be followed by no reporting at all eventually (other than some quarterly or annual retrospective summaries) So the lessons – that if you don’t control infections, you need to control information – have been learned. And it is very much possible that people have died of monkeypox in the West but it is not reported yet. So far 3 people have officially died of monkeypox in the last two months, all in Africa. And Africa has reported very few cases in that period, i.e. the CFR there is in line with what it has been historically. Now it is certain that they have always missed cases there, but I also have doubts it is the same undercount ratio that it is for COVID, as monkeypox is a rather visible disease that drags for longer than COVID and the pain is serious. Which means that we have the following possibilities: 1) Mortality is low in western hospitals but high in Africa where hospitals are less well equipped. That sounds attractive on the surface, but if you think about it, it doesn’t really make that much sense – it would if there were a lot of people in ICU on their death bed and we in the West are doing miracles to save them that they don’t have the resources for in Africa. But we are not hearing about that. 2) The people it is hitting right now are a lot less susceptible to dying. I doubt that though, as this isn’t a disease known to exhibit drastic differences in CFR across different populations…. 3) The virus has mutated on its way to the growing pandemic outside Africa and is less pathogenic now. Meanwhile those 3 people who died in Africa got the ancestral Nigerian strain (with the 3-4% CFR, while the Congo strain with the 10% CFR hasn’t been exported at all) and this is why they died 4) We aren’t told the truth. We will unfortunately know more in the coming months. Once schools reopen and community-wide transmission has ramped up even more, there should be massive outbreaks in children, from where it will infect parents, etc. And then there will be serious pressure on hospitals. This will likely coincide with yet another major COVID wave and your guess is as good as mine about what will happen then…
Remember that GM’s gloomy-seeming calls on Covid most of the time weren’t pessimistic enough. So take that as a warning.
And while we are at it, CDC delanda est.
#mkpx#mkpx virus#monkeypox#monkeypox pandemic#center for disease control and prevention#cdc corruption#cdc#naked capitalism
12 notes
·
View notes
Text
A plague upon both your houses
The Democrats "ended" Covid in spite of the ongoing pandemic because focus group testing told them it would be popular. In spite of over a million dead already and hundreds more dying every day, they continue on with business as usual. Part of it is because their masters want things to go back to normal, but the other part is for the sake of electoral popularity. The mask mandates, lockdowns, and quarantines were "unpopular", so they stopped them believing it would boost them in the midterms.
I think that handily explains the non-response to monkeypox. Putting a stop to it would mean going through that all over again. It would mean lockdowns, quarantines, mask mandates, more disruptions to "normalcy," and--worst of all, the little people would expect all the things that Trump gave them before: eviction protection, covid relief, work from home, paycheck protection, etc. For them, the "cure" would be "worse than the disease." It doesn't help either that the political "wisdom" is that you don't get credit for averting a crisis, only in fixing one.
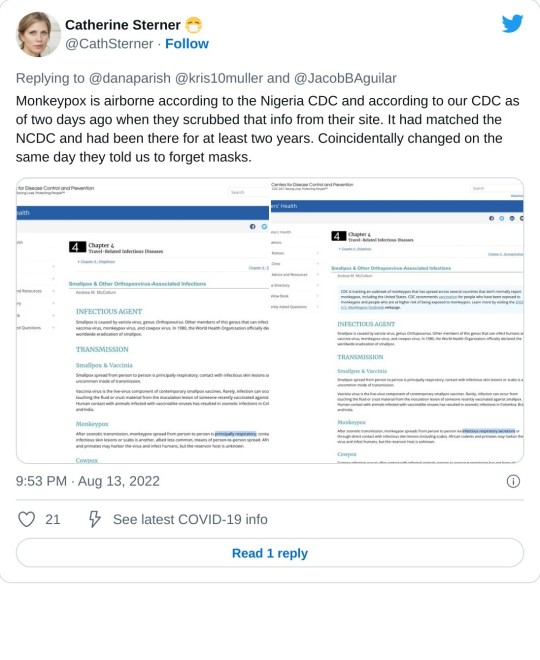
So unfortunately that means that Monkeypox is going to remain a "gay disease" until after midterms at the earliest. That is assuming it remains under the radar, which there's really no telling, especially with the CDC scrubbing the fact that it's an airborne disease from its web pages.
Things are quiet right now because so far they've managed to keep a lid on it, but I don't doubt that in the current climate of "personal risk assessment", the moment that it becomes politically convenient, mask off. Gay men are going to be thrown under the bus as morally depraved, hedonistic fags and it's their fault that they're catching and spreading this disease, because it's spread by intimate contact and of course they should know better by now.
Perversely, the only thing that might save us is that unlike covid, it's not an "invisible" disease. The sociopaths in DC can get covid, buy their monoclonal antibody treatments, and continue acting like everything is normal, like it's just a bad cold. I wonder if the bourgeois antipathy towards masking will change once their faces start becoming disfigured by pustules.
6 notes
·
View notes
Text
CDC Rigs Its Own Monkeypox Case Reports by Not Including Questions on Airborne Transmission
CDC Rigs Its Own Monkeypox Case Reports by Not Including Questions on Airborne Transmission
By Lambert Strether of Corrente.
This short and sweet post will have two parts. First, I will show that the CDC Monkeypox case report form omits amy questions about airborne transmission. Then I will show why that’s a bad idea, inexplicable given CDC’s previous documentation on this point.
Caveat: I am not saying that “Monkeypox is airborne.” To my knowledge, we don’t have epidemiological studies of the same quality we have with Covid; the kind with seat charts and diagrams of airflow (as in the famous Skagit Valley chorus study, but with many others); that is the kind of evidence I rate highest, most of all because such studies show me how to imagine the ground and what to do. However, we do have sufficient information not to rule out airborne transmission altogether, as I will show. That CDC does this a priori — and at the start of what we all hope is not the start of another global pandemic on the order of Covid — is mind-boggling, or would be mind-boggling if we had not, by this time, had plenty of experience with how “The Centers for Disease” operates. They have form. * * *
First, let’s look at the CDC case report, “OMB No. 0920-1011.” We have the “Short Form,” designed to be filled out by state or local health officials. We also have the “Data Dictionary Codebook” (same OMB number), which documents the database fields that will be populated by Short Form data entry. Both are embedded in the Appendix to this post. (The name “Short Form” suggests the existence of a “Long Form,” probably populating database fields unused by the Short Form, but if such a form exists, I haven’t seen it.
From transmission, the key section in the Short From is “History of Possible Exposures.” Here it is:
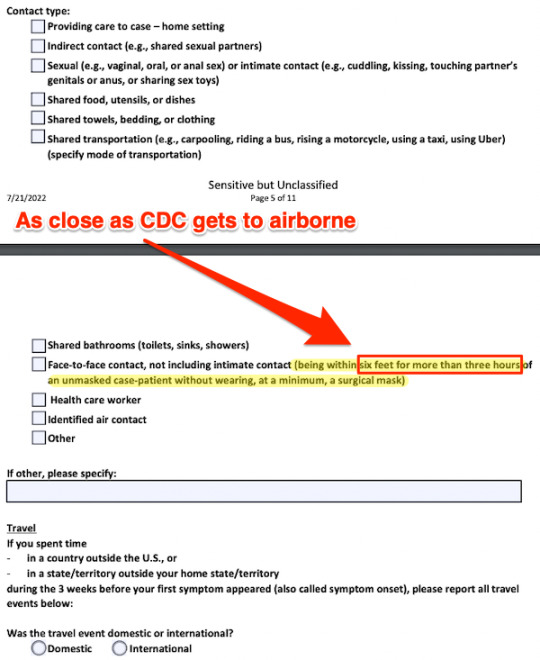
As you can see, the structured portion of the form (i.e. checkboxes and radio buttons) does not permit any representation of airborne transmission (certainly not a “fleeting contact” such as has occurred with Covid); airborne tranmission is ruled out a priori[1].
An interviewer desperate to somehow cram information about airborne transmission into the form could use the following text fields (“location of exposure,” “additional details”):
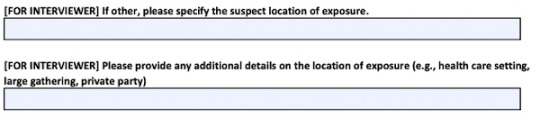
However, exactly because such data would be unstructured and unstandardized, it’s not likely to make it into any reports generated from the database.
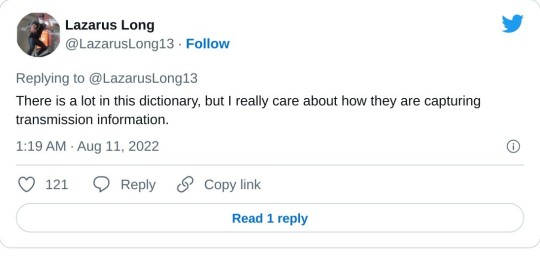
We now turn to the Data Dictionary Codebook. As you can see, fields on the Short Form are mapped to fields in a database. Here is an example of how the documentation is structured:
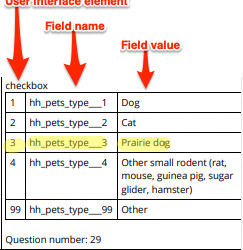
As you can see, the basic structure is a series of field/value pairs, mutually exclusive (ORed radio buttons) or not (ANDed checkboxes). Hilariously, I found this field while searching for “air” (“prairie”); no such luck. “Prairie Dog” strongly suggests that the Data Dictionary dates from no later than 2003, when “All people infected with monkeypox in this outbreak became ill after having contact with pet prairie dogs. The pets were infected after being housed near imported small mammals from Ghana. This was the first time that human monkeypox was reported outside of Africa.” But no doubt our thinking, and our fields, have been updated since that time.
We can also see from this example that the CodeBook contains many fields that are not used in the Short Form. Here is another example:
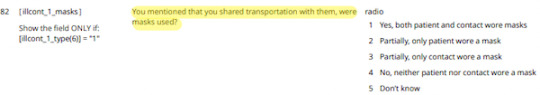
The word “mask” does not appear in the Short Form.
I scanned the entire codebook, and I can’t find any fields that would store data relevant to airborne transmission in the general case. (You can check my work in the Appendix.) For example, the famous Japanese 3Cs — closed spaces (with poor ventilation), crowded places (with many people nearby), and close-contact settings (such as close-range conversations), are highly structured and would lend themselves well to representation in a database. Here are more suggestions:
We can conclude, then, that CDC simply is not enquiring into airborne transmission of Monkeypox. They have ruled it out, a priori. However, if you go by existing literature — including from the CDC itself — there’s plenty of reason consider it a real possibllity. To that literature we now turn. * * *
First, from KHN, “CDC Posts, Then Deletes, Guidance On Airborne Risks Of Monkeypox“:
The Centers for Disease Control and Prevention says it removed the recommendation that travelers worried about monkeypox should wear a mask because it was causing confusion. Although public health officials have been linking many of the cases in this outbreak to close sexual contacts, monkeypox can also be spread through the air for short distances.
This is one of KHN’s handy wrap-ups. From the New York Times, “Monkeypox Can Be Airborne, Too.” So why not collect data on airborne transmision of monkeypox, if only to rule it out?
Then there’s Nature, “How does monkeypox spread? What scientists know.” What we “know” seems solid:
Several studies… show that few people contract the disease from an infected household member with whom they didn’t have sexual contact. This finding, paired with the data about viral load, suggests that respiratory droplets and airborne particles probably aren’t the primary transmission route… If corroborated by further research [which CDC has decided not to do, because reasons], it could call into question whether people should isolate for the entire duration of infection, which might be difficult because the illness seems to take up to a month to resolve, she adds.
But what we “know” melts into air:
Even if the virus can be sexually transmitted, it’s unclear how large of a role this mode of transmission has, compared with simply being in close, skin-to-skin contact with a person or inhaling their respiratory particles [gawd, they can never say “aerosols”] — which also occur during sex.
Put more pointedly, during sex — hear me out — people share air, so any theory of skin-to-skin contact has an enormous confounding factor. So why not collect data on airborne transmision of monkeypox, if only to rule it out?
Now let’s do a (frankly cursory) review of the literature on airborne transmission of monkeypox.
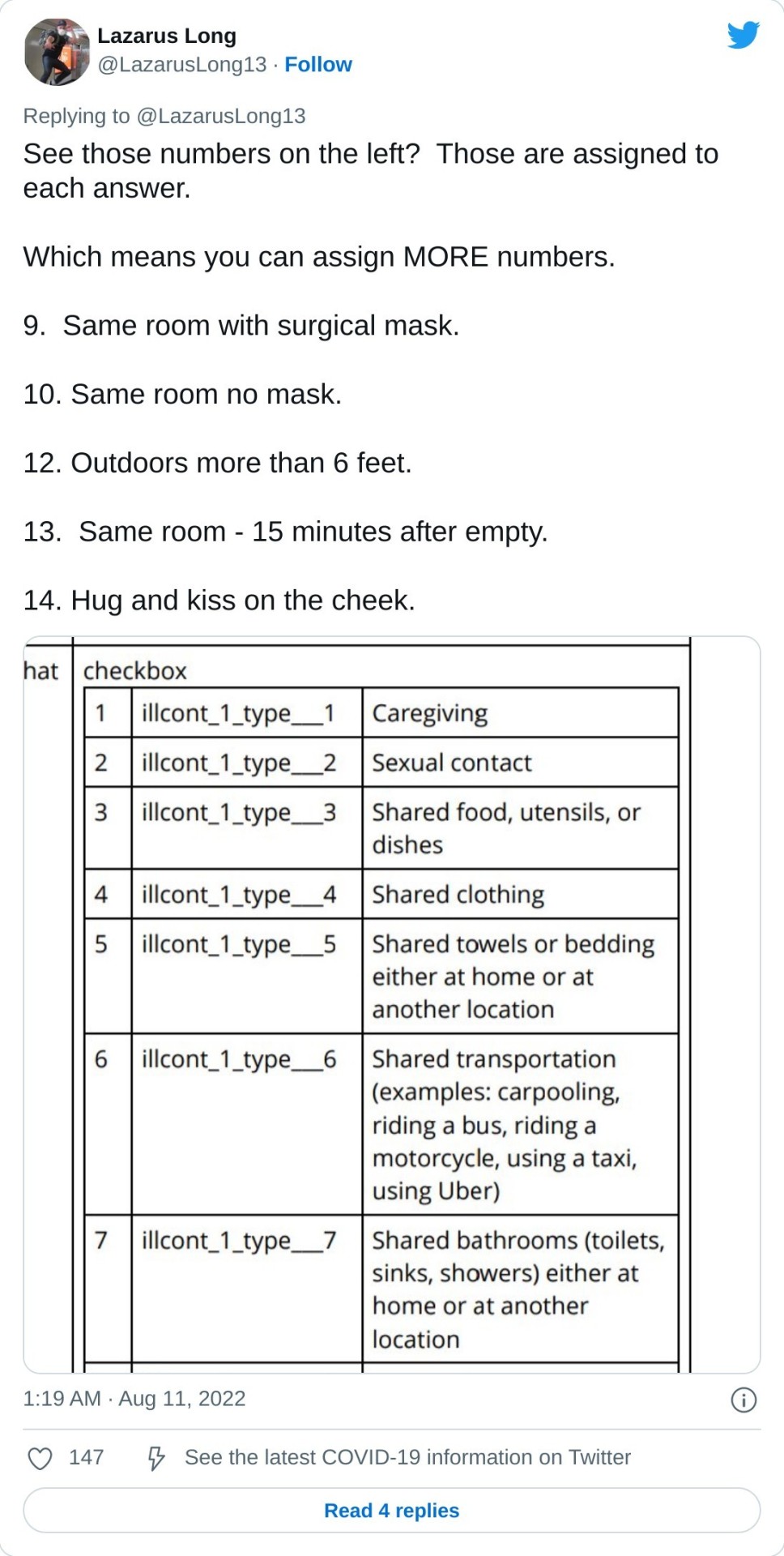
CDC, “Smallpox & Other Orthopoxvirus-Associated Infections.” Here is CDC scrubbing it:
CDC, “Hospital Respiratory Protection Program Toolkit“:
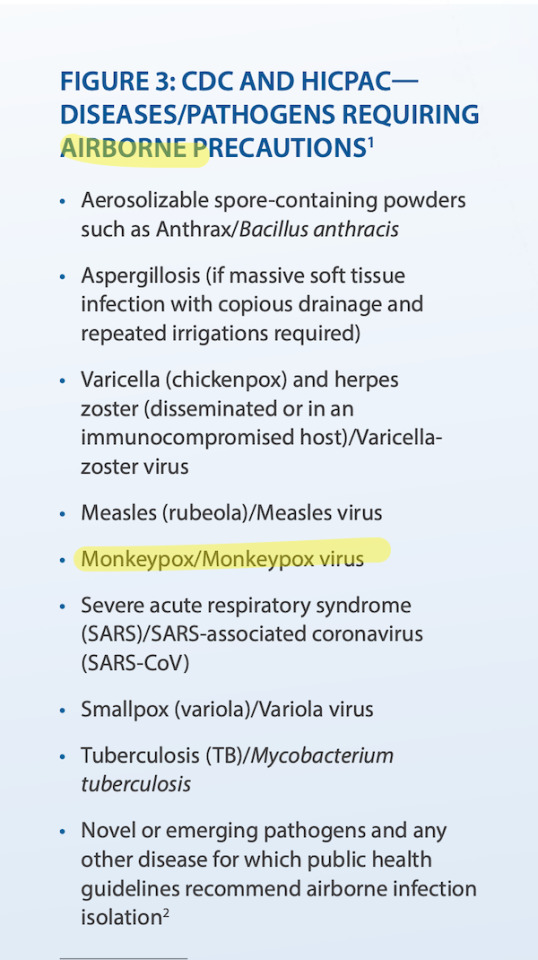
CDC, “Potential Exposure to Person with Confirmed Human Monkeypox Infection” (via):
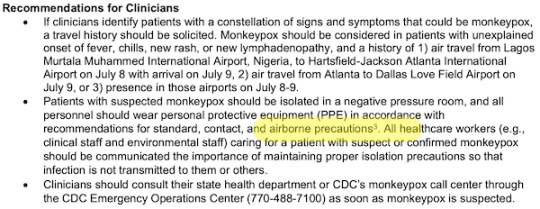
CDC, “Monkeypox in the Democratic Republic of the Congo“:

Coughing and sneezing is possibly droplets (loogies, ballistic). Talking (like singing) certainly includes aerosols, i.e. transmission is airborne.
But wait, there’s more from the CDC:
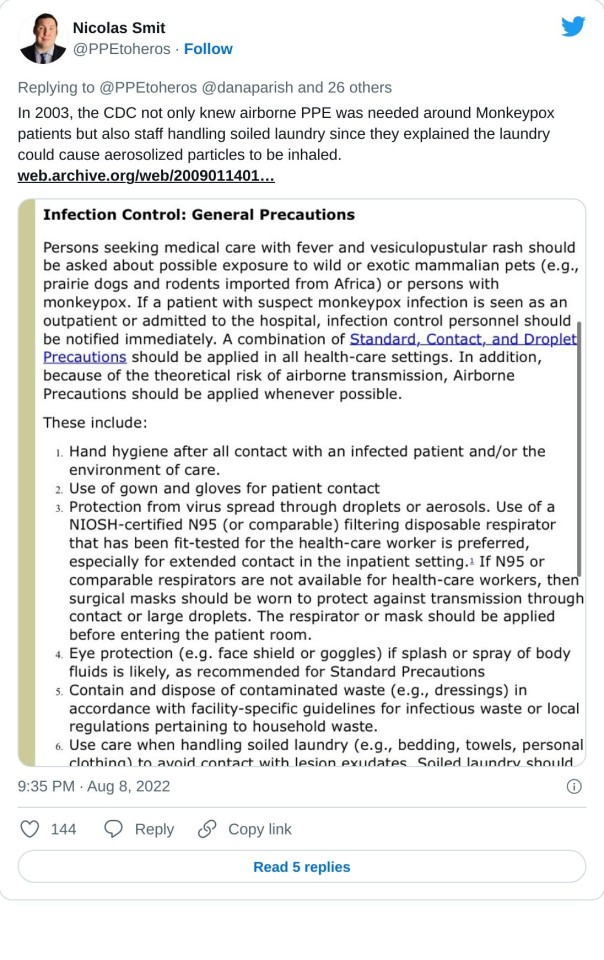
GOV.UK, “High consequence infectious diseases (HCID)“:

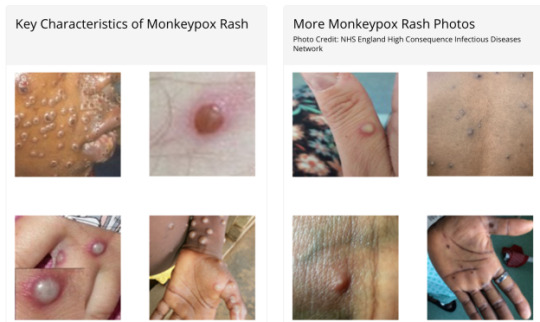
And finally, Clinical Infectious Diseases, “The Clinical Characteristics of Human Monkeypox, and Risk Factors for Severe Disease.” Figure 1 lists the upper and lower respiratory tract symptoms — arguably related to breathing, not touch — the researchers studied.:

Oddly, the CDC’s “Short Form” has eliminated all these symptoms, even coughing:
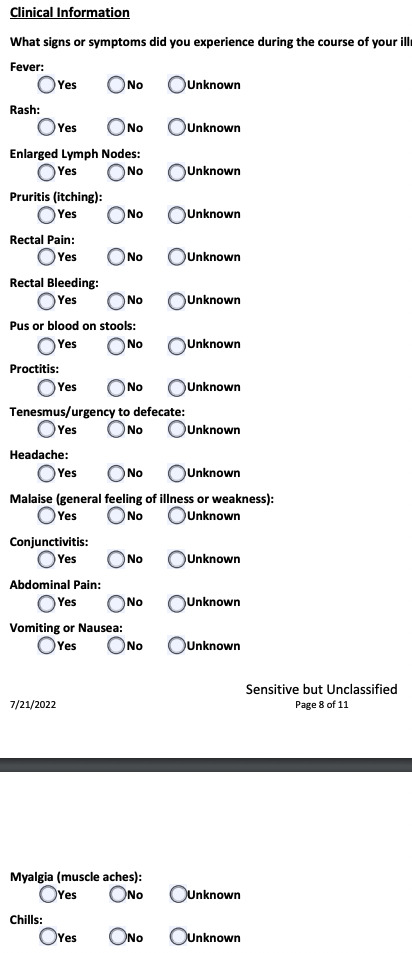
Again, why not collect data on airborne transmision of monkeypox, if only to rule it out?
* * *
In list form:
1) Why won’t CDC collect data on airborne transmission of monkeypox, if only to rule it out?
2) Why won’t CDC collect data on airborne transmission of monkeypox, if only to rule it out?
3) Why won’t CDC collect data on airborne transmission of monkeypox, if only to rule it out?
4) Why won’t CDC collect data on airborne transmission of monkeypox, if only to rule it out?
5) Why won’t CDC collect data on airborne transmission of monkeypox, if only to rule it out?
6) Why won’t CDC collect data on airborne transmission of monkeypox, if only to rule it out?
7) Why won’t CDC collect data on airborne transmission of monkeypox, if only to rule it out?
8) Why won’t CDC collect data on airborne transmission of monkeypox, if only to rule it out?
9) Why won’t CDC collect data on airborne transmission of monkeypox, if only to rule it out?
10) Why won’t CDC collect data on airborne transmission of monkeypox, if only to rule it out?
And so forth. One hesitates to use the word “farce” for CDC”s “science” here, if only because stronger words come to mind.
NOTES
[1] CDC might not be so strong on transmission, but hoo boy! Did they lavish attention on data structures for gender and race (although not, naturally, proxies for class like income or education level).
#center for disease control and prevention#cdc#monkeypox#mkpx virus#pandemic#monkeypox pandemic#public health#late stage capitalism#social murder#class warfare
20 notes
·
View notes
