#laura edwards-leeper
Explore tagged Tumblr posts
Link




Florida House of Representatives Office of the Speaker
Paul Renner Speaker
MEMORANDUM
To: The Honorable Randy Fine, Chair, Health & Human Services Committee From: Paul Renner, Speaker Date: April 23, 2023 RE: Authorization to Commence Investigation
Dear Chair Fine,
According to correspondence from the Florida Chapter of the American Academy Of Pediatrics (FCAAP) to the Florida Board of Medicine, “gender-affirming care is the widely accepted standard of care for treating transgender adolescents with gender dysphoria.” Many medical organizations are said to endorse “gender-affirming care,” although FCAAP’s statement indicates that the standards of care are actually developed by just two organizations — the Endocrine Society and the World Professional Association for Transgender Health (WPATH).
Last year, Florida’s Agency for Health Care Administration (AHCA) adopted a rule excluding from Medicaid coverage certain treatments for gender dysphoria. That rule is the subject of ongoing litigation in federal court, where the plaintiffs rely extensively on WPATH’s and the Endocrine Society’s standards of care and guidelines and describe them as “widely accepted best practices.” AHCA sought to probe that assertion by serving subpoenas on those entities and others that endorse “gender-affirming care” for minors in order to determine whether this purported medical consensus was truly the result of an intellectually rigorous and open process — as any medical consensus should be. Those entities — including WPATH, the Endocrine Society, the American Academy of Pediatrics, and the American Psychiatric Association — responded by fighting vigorously to avoid any meaningful inquiry or disclosure. And they did so notwithstanding their knowledge (and likely, their intent) that their own standards and endorsements are being cited in litigation as a basis to effectively veto state law.
Similarly, in an ongoing legal challenge to Alabama’s Vulnerable Child Compassion and Protection Act, which prohibits the use of puberty blockers, hormone treatments, and surgical interventions as “gender-affirming care” for minors, the plaintiffs have likewise relied extensively on WPATH’s guidelines. But when the State of Alabama sought discovery regarding WPATH’s development of those guidelines, WPATH’s response once again was to seek judicial protection from any disclosure. When the federal court ordered WPATH last month to respond to Alabama's subpoena, WPATH’s reaction was to seek extraordinary appellate review rather than comply.
Dr. Laura Edwards-Leeper, the first psychologist at what has been described as the first major gender clinic in the U.S. (at Boston Children’s Hospital), has publicly expressed concern about the “irresponsible” treatment being administered to minors with gender dysphoria. Referring to her fellow practitioners, she stated that “everyone is very scared to speak up because we’re afraid of not being seen as being ‘affirming.’” And Dr. Marci Bowers, a transgender gynecologic surgeon who has performed more than 2,000 “sex-change” operations and who served as president of WPATH, has commented regarding the state of open discourse and debate: “There are definitely people who are trying to keep out anyone who doesn't absolutely buy the party line that everything should be affirming and that there's no room for dissent.”
Although these leading practitioners (and others) have sounded alarm bells regarding contemporary treatment of minors with gender dysphoria, organizations including FCAAP apparently maintain that there is medical consensus that “gender-affirming care” is the appropriate treatment. The foregoing (and other) indicia of widespread self-censorship in the medical profession suggest that the purported consensus may be little more than a mirage.
WPATH's own published standards of care at least acknowledge what we all know through common experience to be true: that the human brain continues to develop well into early adulthood, that “adolescence is often associated with increased risk-taking behaviors,” and that adolescence is commonly characterized by “a heightened focus on peer relationships, which can be both positive and detrimental.” Dr. Erica Anderson — a transgender psychologist, a former president of WPATH’s United States chapter (USPATH), and a member of the American Psychological Association (APA) task force that writes the APA guidelines for transgender care — has publicly acknowledged that “teenagers influence each other” and that “to flatly say there couldn't be any social influence in formation of gender identity flies in the face of reality.” Concluding that “it's gone too far,” Dr. Anderson asked rhetorically, “What happens when the perfect storm — of social isolation, exponentially increased consumption of social media, the popularity of alternative identities — affects the actual development of individual kids?” It appears that those responsible for developing and endorsing the purported consensus of gender-affirming care for minors may not have engaged with that question in any serious way. And it appears that they wish to avoid any inquiry into their possible failures to do so.
As our courts and the Supreme Court have long recognized, “sunlight is said to be the best of disinfectants.” Yet it appears that the medical organizations who create and endorse guidelines on a contentious issue fraught with scientific uncertainty have gone to great lengths to avoid scrutiny and to keep the public (and their duly elected representatives) in the dark regarding the process by which these "consensus" guidelines were developed.
Therefore, I now authorize and direct the Health and Human Services Committee to investigate whether the adoption and endorsement of “gender-affirming care” as the standard of care for minors have been the result of rigorous medical and scientific analysis and consideration, or whether the integrity of the medical profession has been compromised by a radical gender ideology that stands to cause permanent physical and mental harm to children and adolescents. As part of this investigation, the Committee may look into any relevant matter within the scope of the House's constitutional investigative powers. The Committee may also issue any necessary subpoenas for documents and testimony, including from Florida-based organizations that recommend, endorse, or otherwise promote the standard of care described herein.
Respectfully,
Paul M. Renner, Speaker of the House
cc: Kathleen Passidomo, Senate President Ron DeSantis, Governor
#transphobia#Randy Fine#Paul Renner#Florida#Ron DeSantis#wpath#aap#fcaap#erica anderson#laura edwards-leeper#marci bowers
10 notes
·
View notes
Text
in last week's b&r katie mentioned that the whole "would you rather have a dead son or an alive daughter" line of manipulation is being pushed not just by the kids but by the clinicians
when does that cross into outright extortion
"i’m not saying you have to buy lupron from me, i’m just saying that if you don’t, something bad may or may not happen to your son, capisce?"
9 notes
·
View notes
Text
By: Ben Appel
Published: Jun 13, 2023
As a gay man, I have no pride in Pride month. Radical LGBT bullies have captured it – and threaten to 'fix' us by medicalizing and transitioning us. But gay people will NOT be erased again.
Everywhere around me, I see Pride flags. 'It's time to celebrate the LGBT community!' I'm told. But, this year, as a gay man, I'm not proud of my so-called 'community.'
In fact, I'm horrified by it.
Two decades ago, when I attended my first Pride parade, the LGBT world truly needed it. Pride is the opposite of shame. And for decades, even centuries, gay people had been told to be ashamed of ourselves, of our same-sex attraction, and our supposed inability to behave like 'normal' people.
We were harassed and oppressed. Homosexuality was criminalized. If a man was convicted of having consensual sex with another adult man, he was given two options: imprisonment or chemical castration.
Gays were forced to be something we were not. We were erased.
And that's why I am so heartbroken that 20 years later, the LGBT community supports a new practice that threatens to erase gay people.
It is benignly called 'gender-affirming care.'
Today, LGBT Pride marches arm in arm with radical ideologues who contend there is no such thing as biological sex.
Their extreme doctrine claims that men can simply decide to become women, and, most disturbingly of all, that children can actually change their sex.
Educators, policymakers and physicians are telling young boys that if they like wearing dresses or playing with dolls, they might be girls; young girls are told that if they prefer football to ballet, they might be boys; and that with some experimental pills and high-risk surgeries, they can all finally be 'normal.'
Magically transformed, forever.
But what if a young person struggling to be 'normal' is not trans, but gay? What would have happened to me?
In the course of research for my forthcoming memoir, 'Cis White Gay,' I interviewed a wide range of experts and people within the LGBT community on this troubling, evolving ideology.
I spoke with Dr. Laura Edwards-Leeper, the founding psychologist for the first hospital-based pediatric gender clinic in the U.S.
'There are definitely cases when I strongly suspect sexuality is the issue with young teens,' Dr. Edwards-Leeper explained of her work with gender diverse and transgender people. 'I wonder about it with children, too.'
I told Dr. Edwards-Leeper about my own gender-nonconformity in childhood and my concern that if I were growing up today, I would have been erroneously affirmed as a transgender girl. 'I'm sure you would have,' she said.
Dr. Erica Anderson, a transgender clinical psychologist who treats children, shares the same fear.
'I'm afraid too often, [gay boys are] consuming social media that says, "If you are uncomfortable in your body when you hit puberty, if you don't quite fit with your age mates, well, maybe you're trans,"' she told me. 'I think it's a terrible message to kids, that there's no place for variance. And I think it is the foundation under which, in some circles, there is some transing of the gay.'
Can the LGBT community truly be proud of this?
I cannot overlook the devastating reality that the same pills offered to distressed adolescent boys to feminize their bodies and stave off male adulthood are the same pills, just decades ago, that were used to render gay men asexual.
I cannot turn a deaf ear to the words of former gender clinicians at a U.K. clinic, who told The Times U.K. in 2019 about a dark joke among staff, that soon 'there would be no gay people left,' that what happened in their clinic felt like 'conversion therapy for gay children,' or that 'for some families, it was easier to say, this is a medical problem, "here's my child, please fix them!"'
'Fix them'? 'Fix' children?
I also cannot ignore the testimonies of the detransitioners — adult gay men who sought escape from homophobia in a trans identity and have come to regret it. Some tell me that they were coerced to believe that their atypical femininity meant that they were trapped in the wrong bodies.
'Michael' told me, 'The reason why I felt so happy [after transition] was because I got a break from being seen as a gay guy; I was just this normal, hetero-appearing girl.'
Brian confessed that, 'With estrogen, my libido just kind of died, and it felt so great because I always viewed my sexuality as something bad, and [transgenderism] kind of appealed to me because my dad always hated gay people.'
'Steven' said, 'I felt like I'd rather be a trans woman than a gay man because that was like the lowest and most disgusting thing you could be.'
There are lesbian, gay, bisexual, and transgender people who are horrified by what is being done.
So, we write, we talk, we tweet. We phone our friends and our relatives and neighbors. We tell them that what is being done to children is medical malpractice.
We explain that recklessly administered 'gender-affirming care' is nothing less than the experimental medicalization of homosexuality that carries significant risks. It leads to infertility and loss of sexual function, and no child can adequately consent to it.
To advocates of these practices, I ask you: Is this what you mean when you say you're on 'the right side of history?'
I cannot shrug off the feeling that in the name of the so-called 'LGBT community' a great injustice may be happening before our eyes. But when gay people speak out – we're called bigots.
Lesbians are told they're hateful if they don't want to date males, who identify as women. And gays are told they're hateful if they don't want to date females, who identify as men.
I've had the term 'cis' spat at me with the same venom that I was once called homophobic slurs on the playground, all because I am 'cisgender.'
I am a male that is exclusively attracted to other males. Is that no longer allowed?
Is this what my 'community' has become – the bullies that we once fought against?
If I am proud of anything this Pride Month, it is my new 'community' of LGBT heretics.
Those of us who stand up in the face of ridicule to say: This is not us. This is not who we are.
I am proud every time we're shouted down by authoritarian activists. I remain proud even as we're called 'evil,' 'right-wingers,' or 'transphobes.'
To that community, I say: Happy Pride.
==
Note: links added by me to preempt deniers: "LiTeRaLLy nO oNe iS sAyInG tHaT!" "tHaT nEvEr hApPeNs!"
#Ben Appel#gay conversion therapy#gay conversion#anti gay#homophobia 2.0#homophobia#gender ideology#queer theory#woke homophobia#Pride#pride month#happy pride#chemical castration#LGBT#LGBTQIAlphabet#Alphabet Mafia#LGBTQIAQWERTY#is it over yet?#religion is a mental illness
29 notes
·
View notes
Text

lead author kinnon mackinnon's work and quotes were pivotal to this reuters report from december 2022 pushing the narrative that detransitioners are being silenced by trans people but that detransition is on the rise, particularly among those with 'complex mental health', feat. the usual suspects (laura edwards-leeper, kc miller, chloe cole, &c) and gesturing toward the idea that transition ought to be more gatekept and delayed, particularly for minors, in order to 'protect' vulnerable people
detransition and retransition and non-linear transition do all happen and there's nothing wrong with that or with talking about it. however, i would be extremely cautious about engaging with any project or study led by mackinnon specifically, given that he seems to have no compunction about his work being used to bolster reactionary fear and disgust about trans people (someone might change their body in a way they later feel differently about! oh my god the horror!) and right-wingers' consequent attempts to restrict access to transition healthcare
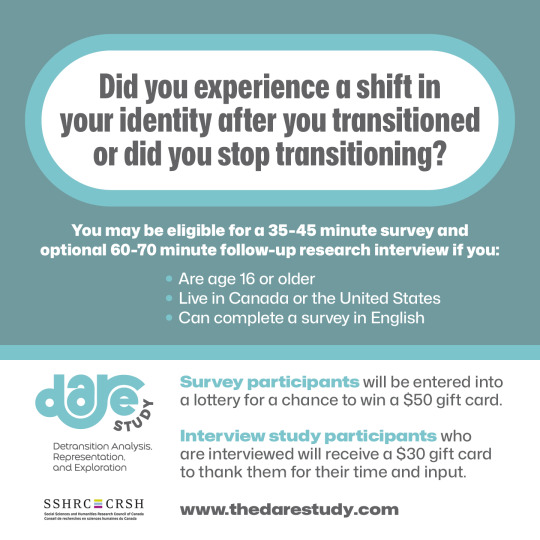
Have you experienced shifts in your identity after transitioning? You may be eligible for a study conducted by a team of LGBTQ researchers.
Participants must meet the following eligibility criteria:
-aged 16 and older
-living in the United States or Canada
-have ever discontinued a gender transition* or detransitioned
-desiring to detransition but feel unable to take steps
*We define gender transition as social, legal, and/or medical interventions used to affirm a trans/nonbinary identity. People who have desisted are eligible to take the survey.
The survey is available at: thedarestudy.com
777 notes
·
View notes
Text
I'm remembering my therapist's office and the view out the window. I can hear her voice and feel the texture on the couch. The stacks of books on the windowsill and the clocks are still in the same place. The painting of the crane is still on the wall and there's boxes of tea by the door again. I miss her, like a long time friend who moved away. She quite honestly saved my life and I don't know how to thank her besides living my best life.
1 note
·
View note
Quote
Earlier this month the High Court in London looked at the case of one detransitioner, Keira Bell, who had brought a judicial review against the Tavistock clinic, England’s only specialist youth gender-identity centre. She claimed that the clinic should not have allowed her to take puberty blockers and later undergo testosterone treatment and a double mastectomy. The court ruled that it was “highly unlikely” that a 13-year-old and “doubtful” that 14- and 15-year-olds are mature enough to consent to such a procedure, and that doctors treating 16- and 17-year-olds may also need to consult a judge before starting. Trans activists argue that a long-marginalised group is now finding its voice in popular culture. Their critics retort that vulnerable teenagers are losing themselves in an online world which adulates anyone who comes out as trans. --- Society is struggling to strike a balance. Some children who feel they are in the wrong body will always feel that way and might benefit from altering their bodies. Others will change their minds—many of these will simply turn out to be gay. No medical test can tell these two groups apart. --- Plenty of doctors fail to observe even WPATH’s guidelines. Laura Edwards-Leeper, a professor of psychology at Pacific University in Oregon who helped found America’s first transgender clinic for children and teens in Boston, says she gets many emails from parents “desperate to find a therapist who will not just blindly affirm that their child is trans”. Ideally, she said, an adolescent with gender dysphoria would have been regularly seeing a therapist, who encouraged them to explore other possible causes for their feelings and had a comprehensive psychological assessment before being put on blockers or hormones. “It is very rare that even one of these things happens,” she says.
“An English ruling on transgender teens could have global repercussions”
0 notes
Text
A new push to ban medical treatments for transgender children

Feb 1st 2020
WASHINGTON, DC
JAMES YOUNGER’S mother believed he should wear dresses and grow his hair long because he considered himself a girl. His father claimed the seven-year-old was perfectly content with trousers, short hair and being a boy. Almost every detail of the couple’s vicious custody battle was fought over their child’s gender identity. After his mother won, culture warriors piled in.
Ted Cruz, a senator from Texas, said the child was “a pawn in a left-wing political agenda”. A host of Republican politicians shared posts from a #ProtectJamesYounger social-media campaign. In October a judge awarded James’s parents joint custody, barring them from speaking publicly about the case. Since then its effects have rippled beyond one unhappy family. Lawmakers in a number of states say the Youngers’ row has prompted them to try to pass laws banning medical interventions that bring transgender children closer to the sex with which they identify.
On January 29th South Dakota became the first state to vote for such a bill in its lower chamber. It needs to be approved by the Senate and governor to become law. At least five others have drawn up bills which would make it illegal to perform gender-reassignment surgery on children and to prescribe puberty blockers and cross-sex hormones for them.
The chief motivation of such lawmakers is political. Some cite the Texan custody case as an inspiration for their bans. But no seven-year-old child is prescribed puberty blockers or undergoes gender-reassignment surgery. To suggest as much—as some right-wing commentators have—is more rallying cry than reality check.
The danger of making trans rights an issue in the culture wars is that it prevents a discussion of the dangers of prescribing blockers and sex hormones for children who suffer from gender dysphoria, the distress caused by feeling that one’s sex at birth and gender identity do not match.
Data on all aspects of transgender medical interventions are poor. No one knows how many children have been prescribed these drugs. Little is known about how they have fared since. But in the past decade there has been a surge in the number of children treated as trans. Clinics serving them have mushroomed. In 2007 there was one. Today there are perhaps 50. Waiting lists at many are long and lengthening.
Anecdotal evidence suggests that standards of care have failed to keep pace. The biggest concern is that children put on blockers—first prescribed between the ages of 9 and 14 to suppress the action of sex hormones—and later, testosterone or oestrogen, do not first undergo sufficiently comprehensive evaluations.
Guidelines from the World Professional Association for Transgender Health say such interventions should follow “extensive exploration of psychological, family and social issues”. That seems elementary. There is no medical test for gender dysphoria. Research suggests that most children who identify as the other sex eventually grow out of it. They are also more likely to suffer from anxiety and depression. Untangling all of this and establishing whether a child is likely to go on feeling that they are in the wrong body—a guess, at best—poses significant challenges for children, parents and their doctors.
Laura Edwards-Leeper, a professor of psychology at Pacific University in Oregon who helped found America’s first transgender clinic for children in Boston, reckons the “vast majority” of children on blockers or sex hormones have not undergone proper assessments. This, she says, is because of a shortage of mental-health professionals with the necessary training and the desire of doctors to provide care for a group that has long been denied it.
This carries the obvious risk that patients will regret transitioning. No one knows how many people fall into this category. A small number of those put on blockers and sex hormones have since “detransitioned”. The most outspoken among them are lesbians who say that had they been encouraged to explore gender non-conformity—the idea, for instance, that women can be butch—rather than transgenderism, they would not have taken testosterone. Others say mental-health problems caused their gender dysphoria and cross-sex hormones were prescribed as the solution.
A second, related problem concerns the way blockers are sold to patients and their families. Developed in the 1980s to treat premature puberty, they have transformed transgender health care since they were first used for this purpose in the late 1990s. Doctors attest that they save adolescents who feel desperate about developing the “wrong” sex characteristics from enormous distress. Blockers can forestall more traumatic interventions later: the removal of breasts, or the shaving of an Adam’s apple. Their effects are largely reversible. Doctors who prescribe them routinely refer to blockers as a “conservative” measure.
Yet few children seem to step off the treatment path that blockers set them on. The great majority go on to sex hormones. Given the inadequacy of many pre-treatment evaluations, this seems unlikely to be wholly the result of sound diagnoses.
Puberty blockers also have other side-effects. Over time, they can affect bone density. This means that doctors are keen to move patients who want to continue treatment onto sex hormones within a few years. But many of the effects of these are irreversible, including infertility. Paul Hruz, an endocrinologist at Washington University School of Medicine in St Louis, says interrupting puberty may have other harmful effects. A surge of hormones during puberty may help put adolescents at ease with their birth gender. Puberty blockers would prevent that process.
Few doctors worried by these problems are prepared to speak about them openly. That is unsurprising given how inflammatory the issue has become. When Lisa Littman, a professor of behavioural and social sciences at Brown University, published a paper in 2018 in which she noted that most transgender children were teenage girls with no history of gender dysphoria—a phenomenon she called “rapid-onset gender dysphoria”—she was denounced as transphobic.
In such a polarised environment, bills proposing blanket bans of puberty blockers are likely to be counterproductive. They may push advocates for early intervention to further extremes. A better approach would be twofold. A neutral assessment of the existing data on the use of blockers, hormones and their effects would help patients and their families make decisions. Most existing research has been undertaken by those working in the field. At the same time, clinics should ensure that children in transgender clinics undergo comprehensive mental-health evaluations.
For all this to happen there needs to be an acknowledgment of the dangers of starting children on often irreversible treatments. At present, that is unimaginable.■
This article appeared in the United States section of the print edition under the headline "A new push to ban medical treatments for transgender children"
https://ift.tt/2tRVcpz
0 notes
Link
Therapists are taking notice, too, of the increasing prevalence of people detransitioning and going back their birth sex, and suggesting a need for comprehensive psychological assessments, rather than fast-tracking children to transition. An article in The Atlantic shares interviews with Scott Leibowitz, a psychiatrist who treats children and adolescents in Columbus, Ohio, and Laura Edwards-Leeper, a psychologist at Pacific University and Oregon's Transgender Clinic. Both believe as Edwards-Leeper shares, "that comprehensive assessments are crucial to achieving good outcomes for TGNC [transgender and gender non-conforming] young people, especially those seeking physical interventions, in part because some kids who think they are trans at one point in time will not feel that way later on."
0 notes
Text
Red-voting conservative father of transgender child embraces changes
Red-voting conservative father of transgender child embraces changes
LEXIE CANNES STATE OF TRANS — And in the embracing of their transgender daughter Lynne, the parents, Albert and Leigh, relocated to Portland, Oregon primarily for the resources offered to trans kids in the area.
The family’s story is told in an in-depth article in Portland’s Willamette Week titled “Transgender at 10″. While I did share this story on my social media sites, I wanted to make note of…
View On WordPress
#Jenn Burleton#Karin Selva#KATE WILLSON#Laura Edwards-Leeper#Lynne#oregon#portland#Randall Children’s Hospital#T-Clinic#trans kids#trans youth#transactive#Transgender At 10#Willamette Week
0 notes
Text
By: Benjamin Ryan
Published: Oct 31, 2024
Boston Children’s Hospital slashed the time slated for psychologists to assess and write a report on children seeking gender-transition treatment from 20 hours to under 3 hours, alarming experts.
The world-renowned Boston Children’s Hospital is being denounced by leading psychologists for drastically reducing the time it allocates for mental-health professionals to determine whether children identifying as transgender should receive gender-transition treatment. Shocked and dismayed by the hospital’s policy, these experts in pediatric-gender medicine have called the shortened assessment period woefully inadequate — considering the complexity of gender-related distress in minors and the fact that these medications are life-altering and, in the case of testosterone and estrogen, cause irreversible effects.
During the second half of the 2010s, leaders at the pediatric gender clinic at Boston Children’s first cut in half, and ultimately slashed by eightfold, the time they typically scheduled for in-house psychologists to assess gender-distressed children before determining whether they should be referred to endocrinologists to begin a treatment path that includes puberty blockers and cross-sex hormones.
By about 2018, the gender clinic’s assessment policy was to provide these minor-age patients only a one-hour appointment with a psychologist, plus one hour with that provider and their family. This is according to three staff psychologists and the clinic’s director.
“It’s shocking,” Laura Edwards-Leeper, a former Boston Children’s psychologist who helped found its gender clinic, told the Sun of the dramatic reduction in time allotted for such assessments.
This reported sea change in clinic policy came to light thanks to a lawsuit brought by a fired psychologist that is now being heard in Suffolk County Superior Court in Boston. Amy Tishelman, 68, has accused Boston Children’s Hospital of age- and gender-based discrimination and of retaliation. The hospital terminated her in 2021, alleging she violated a patient-privacy law; she had filed her initial discrimination suit against the institution the year prior.
Dr. Tishelman, who is widely recognized as a leader in pediatric gender medicine, on Thursday testified that when she began working for Boston Children’s gender clinic in 2013, administrators allotted her 20 hours, and sometimes longer, to assess whether a child should be referred for gender treatments; this included her time to write the report on the patient.
A few years into her tenure at the gender clinic, the hospital had cut that period to 10 hours, she said. Then, by early 2018, it had slashed the time again.
“I didn’t feel like that was doable at all,” Dr. Tishelman said from the stand. She denounced as “reckless” the clinic’s policy it adopted over six years ago of allotting just two hours of assessment-appointment time and a half hour for report writing.
Speaking to the complex calculus involved in considering whether gender-distressed adolescents should receive powerful medications to alter their puberty, Dr. Tishelman continued: “There’s a lot of things to think about in the long- and short-run. It’s not like taking an aspirin. It’s a big deal.”
That it has taken so many years for these specific policies at Boston Children’s to be laid bare lends weight, critics suggested to the Sun, to the persistent allegations that pediatric gender care, a controversial medical specialty, is lacking in transparency.
The associated political stakes are substantial. During the presidential campaign’s home stretch, President Tru.mp has relentlessly hammered Vice President Kamala Harris for her past support of taxpayer funded gender-transition treatments for prisoners, including detainees who are undocumented migrants. His campaign has funneled tens of millions of dollars into attack ads on this issue.
Dr. Tishelman alleged in court that her supervisor at Boston Children’s, Dr. Yee-Ming Chan, was threatened by her success and had long subjected her to sexist and ageist treatment. Dr. Chan, who denies these claims, is a pillar in the field of pediatric gender medicine in his own right. He is a co-principal investigator of an ongoing and multipronged $10 million National Institutes of Health–spon.sored research endeavor of the care transgender youth, including studies of the use of puberty blockers and cross-sex hormones to treat gender-related distress.
Republican members of Congress last week pledged to launch an investigation into the federal grant funding this study. They were inspired to do so after The New York Times reported that the research project’s leading investigator, Dr. Johanna Olson-Kennedy of Children’s Hospital Los Angeles, said that she had refrained, expressly for political reasons, from publishing the team’s study finding that puberty blockers were not tied to psychological benefits.
The Boston trial has also shone a harsh light on a substantial blind spot in pediatric gender medicine: the crucial question of how those who medically transition as minors fare as adults.
By stripping Dr. Tishelman of her right to see patients in the gender clinic in 2019, she and her attorney alleged in court, Boston Children’s compromised her vital research into the care of transgender children. By firing her outright two years later, she said, the hospital terminated, among other research, her effort to establish a comprehensive database of all the patients the gender clinic had ever seen and to follow up with those who had reached adulthood.
“We were the first clinic to see transgender kids in the United States, and we don’t know whatever happened to them and how they’re doing,” Dr. Tishelman testified about the hundreds of former patients who have aged out of the clinic’s care.
“It’s damning that an institution like that, which has all those esteemed affiliations with major universities, would put the kibosh on an area of research that’s so desperately needed and would have informed their administrative decisions had they allowed it,” Erica Anderson, a psychologist and former head of the U.S. division of the World Professional Association for Transgender Health, or WPATH, told the Sun.
Boston Children’s is most prominently affiliated with Harvard Medical School.
Dr. Anderson, who is transgender, said that the assessment-related testimony from multiple Boston Children’s employees in Dr. Tishelman’s trial — who gave no indication that the drastically shortened assessment time is anything but a long-standing clinic policy — suggested a “fall from grace” for the prestigious hospital. The institution, she said, has “capitulated to the medicalization of children in a way that is reckless.”
“When people like Amy Tishelman are forced to draw a line in the sand and say, ‘no,’ and institutions come down hard on someone like her, we’re in deep trouble in America,” Dr. Anderson said.
A leader in the field, a challenge to that reputation
The gender clinic housed at Boston Children’s, called the Gender Multispecialty Service, or GeMS, is a pioneer and considered to be among the pre-eminent clinics of its kind in the United States. Consequently, the news that GeMS will approve children for gender-transition treatment at a pace multiple leading gender-medicine psychologists told the Sun was alarmingly hasty will likely deal a blow not only to the hospital’s reputation, but to this controversial and besieged medical field as a whole.
Opponents and skeptics of prescribing puberty blockers and cross-sex hormones to treat gender-related distress in minors frequently characterize the nation’s pediatric gender clinics as engaging in sloppy, rushed care. These critics, who include many Republican lawmakers as well as a few vocal insiders like Dr. Anderson, often assert that doctors routinely place vulnerable adolescents suffering from myriad mental health problems on powerful, life-altering drugs without engaging in proper due diligence.
Given the nation’s fractured health care system and a prevailing lack of routine patient-data collection in this field, as well as an evident reticence by gender-medicine researchers to publish unflattering research findings, comprehensive information about actual assessment practices at these clinics has remained fairly elusive.
The expositions that have emerged at Dr. Tishelman’s trial consequently shed crucial light onto the practices of a medical field that has become increasingly insular and secretive as it has faced mounting political and public scrutiny, lawsuits and, for Boston Children’s in particular, even threats of violence.
The hospital sustained waves of bomb threats in 2022 after the influential conservative social-media account LibsOfTikTok focused its criticism on the Boston gender clinic and others like it. The account, run by Chaya Raichik, circulated videos that Boston Children’s had published, and ultimately deleted, advertising its gender-transition services, including surgeries it indciated it would perform on minors.
Evidently concerned, at least in part, by the potential for further threats of violence, attorneys for Boston Children’s have sought to keep shielded from public view allegations about GeMS’s practices that were included in exhibits Dr. Tishelman submitted for her lawsuit. In an October 2023 filing successfully requesting that the judge overseeing the case seal portions of those exhibits the attorneys wrote:
“Public disclosure of these allegations will add fuel to an already highly charged public debate over the care of gender diverse youth and could cause serious, irreversible harm to the Hospital and the practitioners who Plaintiff now, for the first time, accuses of providing substandard care to this already at-risk population.” The attorneys further asserted: “GeMS practitioners provide individualized, safe, and affirmative care.”
A representative for Boston Children’s declined to answer questions from the Sun, saying the hospital could not comment on pending litigation.
How Boston Children’s began the U.S. pediatric gender-medicine revolution
In 2007, Boston Children’s became the first U.S. clinic to import a pediatric gender-transition treatment protocol pioneered by researchers in the Netherlands. The Dutch model, as it’s known, observed strict criteria that only prescribed puberty blockers and cross-sex hormones to minors who had consistent cross-sex identification from early childhood, supportive parents, and no major other psychiatric problems. The model also discouraged prepubescent social transitions.
According to a 2014 paper regarding 55 of the first Dutch youths to receive gender-transition treatment and surgeries under the protocol, their outcomes by young adulthood were generally favorable. The notable exception was one participant who died from complications from a vaginoplasty.
During the transformative decade since then, diagnoses of gender dysphoria — meaning distress stemming from a misalignment between a person’s biological sex and their gender identity — in young people have soared across the Western world. In response, scores of gender clinics nationwide have opened, following Boston Children’s lead.
Concurrently, the profile of the typical patient presenting at pediatric gender clinics has shifted profoundly from the makeup of the original Dutch cohort. Today’s gender-dysphoric minors are more likely to be natal females and to only express gender dysphoria after puberty’s onset. They also have a higher rate of other psychiatric conditions and autism.
In tandem, U.S. gender-medicine practitioners have become known worldwide for their particularly eager abandonment of the Dutch model’s guardrails. In their place, clinics such as Boston Children’s have adopted a philosophy known as gender-affirming care.
The gender-affirmative ethos has been propagated and popularized in particular by a policy statement published by the American Academy of Pediatrics in 2018. The statement encourages care providers to observe deference to a child’s self-perception of their gender and essentially let the child take much of the lead in their own care. The document is now the subject of a medical-malpractice lawsuit and a recent probing letter from Republican state attorneys general.
Recent analyses of national medical-claims data provide at least some sense of how common pediatric gender care has become. The nonprofit Do No Harm recently conservatively estimated that at least 14,000 U.S. minors received gender-transition medications, surgeries, or both between 2019 and 2023. And the Manhattan Institute estimated, also conservatively, that 5,300 to 6,300 minors—as young as 12 years old—received gender-transition mastectomies between 2017 and 2023.
Boston Children’s, Do Not Harm found, provided such services to at least 300 children, accounting for nearly half the cases that the analysis identified in Massachusetts.
According to GeMS’s website, the clinic has cared for more than 1,000 families. The site states: “We believe in a gender-affirmative model of care, which supports transgender and gender diverse youth in the gender in which they identify. This is a standard of care grounded in scientific evidence, demonstrating its benefits to the health and well-being of transgender and gender diverse youth.”
Recent systematic literature reviews—the gold standard of scientific evidence—have cast serious doubt on assertions that the evidence base behind pediatric gender-transition treatment is robust and reliable. These reviews have all found that such medical interventions are based on shaky and uncertain research findings.
The broad adoption of the gender-affirming care method and the concurrent surge in gender-transition treatment prescriptions have helped fuel a furious backlash among state-house Republicans. Since 2021, 26 states have passed laws banning pediatric gender-transition treatment; all but two of them ban transition surgeries for minors as well. In December, the Supreme Court will hear oral arguments over whether Tennessee’s treatment ban violates the Constitution.
Gary Click, a Republican state representative from Ohio, marshaled that state’s ban into law. In an email to the Sun, he responded to news from Dr. Tishelman’s trial, specifically that Boston Children’s assesses gender-dysphoric minors in just two hours of appointment time, by criticizing the pediatric gender-transition treatment advocates with whom he has clashed.
“While I consistently advocated for mental-health over medical interventions, I was frequently and falsely accused of denying psychological care,” Mr. Click said of such advocates. “I’ve since discovered they are usually guilty of what they accuse us of doing. Now it appears that they are in a rush to medicate children before they have a chance to heal emotionally and choose a normal life.”
An employment lawsuit affords a rare view inside a top gender clinic
Dr. Tishelman, who is an expert in child maltreatment and trauma, worked at Boston Children’s for nearly three decades. In 2013, she was appointed the director of clinical research at GeMS. Prior to her termination, she was a senior attending psychologist at the hospital and an assistant professor at Harvard Medical School.
In addition to her research duties, Dr. Tishelman spent a relatively small portion of her overall schedule conducting the psychological assessments of gender-dysphoric patients who were potential candidates for gender-transition treatment.
WPATH guidelines advise that gender clinics conduct a comprehensive assessment of such pediatric patients prior to prescribing them gender-transition drugs.
Today, Dr. Tishelman is a research associate professor in psychology at Boston College. Her 2021 amended legal complaint, filed after she was fired in March of that year, charts what it claims was a fraught relationship between her and the Boston Children’s pediatric endocrinologist Dr. Yee-Ming Chan. Her complaint states that Dr. Chan, who is over a decade her junior, became her supervisor at GeMS in 2014.
Dr. Chan repeatedly disputed in his testimony on Monday that he was indeed her official supervisor at the gender clinic.
The legal complaint alleges that Dr. Chan subjected Dr. Tishelman to “a ceaseless sexist and ageist campaign of denigrations, accusations and recriminations” that created a hostile work environment and was driven by his “professional jealousy.”
Dawn Solowey, an attorney for Boston Children’s of the law firm Seyfarth Shaw, asserted during her opening statement on Oct. 21 that Dr. Chan sought to foster a productive and copacetic working relationship with Dr. Tishelman. During his testimony, he denied Dr. Tishelman’s accusations of mistreatment.
Both Psychologist Kerry McGregor, who is now the associate director of GeMS, and Francie Mandel, a senior clinical social worker supervisor at the clinic, testified favorably about Dr. Chan’s character and professionalism and cast those qualities of Dr. Tishelman in a negative light.
There remain several days of additional testimony in the trial that might flesh out the details of all the contrasting accounts.
Dr. Tishelman testified that other GeMS employees reacted with jealousy to the news in late 2017 of her appointment by WPATH as the lead author of the revision to its guidelines on care for prepubescent children with gender dysphoria. However, many professionals throughout the national field congratulated her, she said.
Soon after the WPATH appointment, Dr. Tishelman testified, GeMS doubled her clinical work, demanding that she see far more gender dysphoric patients than her schedule permitted. Others testified that this shift was unrelated to the news regarding WPATH.
“When I started, there were 20 hours,” Dr. Tishelman said of the time allotted for patient assessments. “And now they were asking me to do them in two-and-a-half hours.”
The assessments, she said, were meant to address a litany of complex needs and concerns. The original 20 hours included the time for Dr. Tishelman to speak with a gender-distressed child and their family; conduct scoring of major mental-health and neurodivergence markers; assess for suicidality; and determine the family’s concerns about infertility, which is a major risk of pediatric gender-transition treatment. Additionally, she might secure permission to confer with the patient’s outside therapist or school counselor. The time allotted also factored in her effort to write a detailed report on whether the child was a proper gender-transition treatment candidate and what other types of support they might need.
“Kids can be confused about what they want to do,” she said on the stand. “It’s a collaborative process to try to work with kids and their families to try to figure out what’s best for them, knowing the benefits and risks—being informed about the choices.”
Dr. Tishelman testified that by early 2018, GeMS administrators eliminated from the assessments a screening measure for autism. She alleged that despite what she characterized as the degradation of the assessments’ quality by that time, GeMS would include in various reports about the clinic’s work that its staffers followed WPATH’s trans-care guidelines.
“Shortening evaluations” at GeMS “eventually became a big concern” among her research collaborators nationwide, Dr. Tishelman testified. “People would complain to me about my protocol from outside,” she said in reference to those national colleagues.
Dr. Tishelman specified that Dr. Robert Garofalo, a leading pediatrician at the gender clinic at Lurie Children’s Hospital in Chicago, expressed a concern to her at around this time regarding GeMS excluding from the assessments a measure of family acceptance and support of transgender patients. Along with Dr. Chan, Dr. Garofalo is a co-principal investigator on the long-running NIH-funded study of which Dr. Olson-Kennedy is the research lead.
“I would try to tell people that I was not in charge of the protocol,” Dr. Tishelman testified.
Dr. Garofalo responded to an email seeking comment by asserting that the Sun’s initial characterization of Dr. Tishelman’s testimony about him was incorrect. But after the Sun then clarified her words about him, he did not respond further.
Dr. Edwards-Leeper was a coauthor under Dr. Tishelman of the WPATH guidelines chapter revision on prepubescent children and also co wrote the accompanying adolescent chapter. Having left GeMS in 2011, Dr. Edwards-Leeper now practices in Ohio. She reported that she faced similar pressure to assess patients faster from an employer in the interim.
She refused.
“There was no possible way I could cut corners,” she said. Today, in private practice, she directly assesses gender-dysphoric adolescents and their parents for at least 10 hours and ultimately writes a 20- to 30-page report on them.
Dr. Edwards-Leeper, who was on the team that first imported the Dutch protocol to Boston Children’s, told the Sun that she only relatively recently learned that GeMS had progressively slashed its assessment time period during the late 2010s.
“When Amy first shared that with me, I was just in disbelief,” said Dr. Edwards-Leeper, expressing concern that the system of patient oversight she had helped establish at GeMS — one in which she said that, as Dr. Tishelman testified, psychologists spent about 20 hours on the assessment process all told and produced a 15- to 20-page report — had been compromised.
On Tuesday, Dr. McGregor testified that the clinic had allotted four hours of “face-to-face time” with patients for assessments when she started at GeMS in 2016 and ultimately cut this to two hours. The day prior, Dr. Jeremi Carswell, director of GeMS, also testified that the assessment appointment time had been cut from four hours to two hours.
“My understanding is that some were unhappy about it,” Dr. McGregor said about the time reduction, specifying Dr. Tishelman and GeMS psychologist Peter Hunt in particular. “I thought it was appropriate. But some people wished they’d had that time.”
Further asked by a Boston Children’s attorney about why the assessment time was reduced, Dr. McGregor said: “I think that four hours was too much time. If you ever try and get an adolescent to pay attention to you for four hours straight, it’s a little bit difficult. And also we were able to get all the information in much less time. So, in order to see our growing patient population, it made sense to make that time more efficient.”
Dr. McGregor, who said she spent about 15 to 45 minutes writing her assessment reports, with the aid of a template she created, continued: “And we also could always ask for more time if we needed to. So I’ve met for a second session with patients. It’s pretty rare, but I do it if I need it.”
Asked if two hours was typically sufficient to perform what the attorney called “a hormone-readiness assessment,” Dr. McGregor replied that it was. And asked for greater specifics about occasions when she said this was not sufficient time, she said, “Very rarely, but usually if someone has extreme social anxiety, they don’t want to talk, it takes a while to warm them up, maybe they’re on the autism spectrum, things like that, it might make sense to have a second session.”
Dr. Tishelman’s attorney, Patrick Hannon, of Hartley Michon Robb Hannon, asked Dr. McGregor about the videos that GeMS put out advertising their services. She referred to one in which she suggested that, as she recalled in her testimony, “a lot of parents share that some of their children seem to know seemingly from the womb as if they come out kind of knowing who they are,” meaning transgender.
“There’s no scientific research that would support the assertion that kids know whether they’re transgender as soon as they come out of the womb, right?” Mr. Hannon asked Dr. McGregor.
“I don’t know how we would do that scientific research, so no,” she replied.
What is typical practice in this field?
It is evident that many of the nation’s pediatric gender clinics do engage in lengthy and circumspect assessments of gender-dysphoric minors seeking puberty blockers. But WPATH’s recommendation on this measure notwithstanding, it is also apparent that there is no uniformly upheld standard across this medical field and that assessment times and thoroughness vary dramatically.
Some American mental-health providers, for example, advertise that they will write a letter recommending a gender-dysphoric child for puberty blockers after only a single visit.
Dr. Edwards-Leeper has defended the value of robust assessments in the face of a burgeoning movement across the pediatric gender medicine field to question their utility.
The most comprehensive data set detailing assessment times comes not from America, but from Britain. A major analysis of pediatric gender medicine, called the Cass Review, that was published in April included information from an audit of discharge data regarding some 3,300 patients cared for by England’s pediatric gender clinic, known as GIDS.
The children from this cohort who were ultimately referred to endocrinology received the go-ahead after an average of just under seven assessment appointments. However, a substantial proportion of these children were referred after only three or four assessment appointments.
Anna Hutchison, a psychologist who worked for GIDS between 2013 and 2017, reflected on the prospect of being asked to assess a child and their family in only two appointments, as became the practice at GeMS in 2018. “What can you realistically achieve in that time?” Dr. Hutchinson said.
Dr. Hutchinson ultimately publicly protested policies at GIDS that she said resulted in incautious, unethical care. In an interview, she conjectured that the Boston clinic might have been under mounting demands similar to those that, across the Atlantic, caused the inadequately resourced GIDS to buckle. As the population of gender-dysphoric British children seeking care swelled, Dr. Hutchinson recalled, systemic pressure pushed her and her colleagues to spend less time assessing each child — even as the rate of other psychiatric conditions among the patients steadily increased.
“There are risks in changing what we do clinically based only on resources,” said Dr. Hutchinson. Referring to the increasing demand for services from increasingly troubled children, she said, “Because numbers are going up, complexity is going up, and the amount of time per patient her family goes down.”
“We essentially became an assessment and medication service,” she said of GIDS during her tenure.
Ms. Solowey, the attorney for Boston Children’s, suggested in court last week that GeMS also could not keep up with demand, saying that the clinic “had a really long waiting list.”
Ms. Mandel testified that the reduction, six years back, in appointment hours allotted for individual patient assessments at GeMS was driven not by clinical factors but by billing-related concerns.
As for insights into American practices, in October 2022, Reuters published an investigation of pediatric gender clinics in which it reported: “Seven of the clinics said that if they don’t see any red flags and the child and parents are in agreement, they are comfortable prescribing puberty blockers or hormones based on the first visit, depending on the age of the child.”
Nearly two dozen medical-malpractice lawsuits have been filed by detransitioners – people who medically transitioned and then regretted it, stopping treatment and reverting to identifying as their birth sex – against health and mental health providers over the past two years. Central to many of those suits are claims that minors or young adults suffering from multiple other psychiatric conditions were prescribed gender-transition treatment for dysphoria after only a cursory assessment that failed to meet the WPATH standard.
Jordan Campbell, a partner at Campbell Miller Payne, a Dallas firm that represents many of these plaintiffs, told the Sun: “Dr. Tishelman’s testimony squares with what we see and hear from every single one of our clients: a general sense to rush patients into life-altering medicalization with very little — frequently even less than two hours — assessment, if any.”
In Feb. 2023, Jamie Reed famously blew the whistle on her employer, The Washington University Transgender Center at St. Louis Children’s Hospital, where she had been a case manager. Ms. Reed has accused the since-shuttered clinic of shirking its responsibility to provide comprehensive aid to a population of vulnerable children with very complex needs. (An internal university investigation found the clinic followed “appropriate policies and procedures according to the accepted standards of care.”)
“I long suspected that the sloppy care Wash U. provided would be found across the country,” Ms. Reed told the Sun. During her time at the St. Louis clinic, she said, “I was often unable to refer patients to high-quality psychological assessment, and our clinicians were also limited to scheduling only two sessions to complete an assessment—matching Dr. Tishelman’s account.”
Dr. Tishelman’s downfall
Attorneys for Boston Children’s have asserted in court that the hospital stripped Dr. Tishelman of permission to see GeMS patients in 2019 as a consequence of her chronic delinquency in turning in her patient reports; Ms. Mandel confirmed in her testimony that some reports were late. At that time five years ago, Dr. Tishelman testified, she had six delinquent reports.
The hospital claims that it fired Dr. Tishelman outright in 2021 for violating federal patient privacy laws by viewing, without authorization, records of hundreds of patients not under her care. The hospital alleged that she secretly accessed those files in 2019 in hopes of defending herself by identifying other delinquent psychologist colleagues.
Dr. Tishelman testified that the deadlines for her reports were deliberately unreasonable, given how GeMS administrators had burdened her with an excessive workload. She asserted that the clinic singled her out and “set me up to fail.”
Dr. Edwards-Leeper and Erica Anderson were among the dozens of major figures in pediatric gender medicine who signed a letter of protest to Boston Children’s over Dr. Tishelman’s firing.
In his opening statement, Mr. Hannon said that the patient-privacy-related infraction was a “tru.mped up” pretext for Dr. Tishelman’s termination. Dr. Tishelman ultimately testified that the GeMS patient population was considered communal among the staff psychologists and that it was common practice to discuss one another’s cases and review related medical records at staff meetings. Dr. Tishelman said that Dr. Chan knew in mid-2019 that she had recently reviewed other clinic psychologists’ reports and that he made no objection at the time.
Dr. Tishelman said Dr. Chan confirmed to her during that meeting that the other psychologist at GeMS she had identified as delinquent – Kerry McGregor –was making recommendations regarding gender-transition treatment for children despite omitting key information meant to be in the reports.
“You can’t really write the report without using all the information we’re gathering to put together to understand these people,” Dr. Tishelman testified. “Otherwise why would we even collect that information in the first place?”
Dr. McGregor testified that records indicated her reports were not actually delinquent. She said that at that time there were “some addended scores that I had not placed for the assessment report” – an oversight that she said she quickly rectified.
She further testified that she was alarmed when she learned in 2019 that Dr. Tishelman had accessed her patient records; the following year, she determined that this included files pertaining to over 200 children. Dr. McGregor recalled that Dr. Carswell relayed to her in mid-2019 that the legal department at Boston Children’s found there were some legitimate reasons for Dr. Tishelman to have accessed those records and that her having done so was not cause for concern.
Two years later, however, Dr. Tishelman was terminated from the clinic.
#Benjamin Ryan#Amy Tishelman#Boston Children's Hospital#medical scandal#medical corruption#medical malpractice#religion is a mental illness
0 notes