#hyperbaric centers
Explore tagged Tumblr posts
Text
BRO having empathy sucks!!
#i can hear the disappointment and the bargaining and the frustration through the phone#and i can’t do SHIT to help her and i feel awful#<- context: a client of ours had his cancer return and his wife is trying to see what membership and payment plans she can get#also i work at a wellness center. just to clarify. but we do iv drips and hyperbaric therapies but we dont know if that’s gonna help him#i just hate that i can’t help i’m literally just a message man between this woman and my manager#and i want to just make it easier on her and him and their children like GOD this fucking sucks i hate what this family is going through :(#shut up chelsea
9 notes
·
View notes
Text
Revolutionize Healing with Tesla Med Beds at Atlanta Hyperbaric Center
Discover the future of wellness with Tesla Med Beds from Atlanta Hyperbaric Center. Our advanced med beds promote rapid recovery, cellular rejuvenation, and enhanced overall health. Experience cutting-edge technology designed to accelerate healing naturally. Visit our Tesla Med Beds page to transform your wellness journey today!
Read More :
0 notes
Text
Hyperbaric medicine center in Mumbai
0 notes
Text
Breathing New Life HBOT Oxygen therapy near Glendale CA Services Available

Hyperbaric Oxygen Therapy (HBOT) near Glendale, CA, could be the solution. Discover the benefits of HBOT, how it works, and where to access these services nearby. Explore the transformative potential of HBOT oxygen therapy near Glendale CA for your well being.
Understanding HBOT:
HBOT entails inhaling pure oxygen within a chamber that's pressurized. This helps your body absorb more oxygen than usual, which can promote healing and wellness.
Benefits of HBOT:
Faster Healing:
HBOT can speed up your body's natural healing processes, making it great for wounds, injuries, and recovery after surgery. Reduced Swelling: By delivering oxygen to areas with inflammation, HBOT can help decrease swelling and pain from conditions like arthritis and sports injuries.
Better Brain Function:
Increased oxygen levels can improve your thinking and memory, making HBOT helpful for conditions like stroke and brain injuries. Stronger Immune System: HBOT supports your immune system, making it easier for your body to fight off infections and sickness.
Overall Wellness:
Many people feel refreshed and energized after HBOT sessions, even if they don't have any specific health issues. Services Available Near Glendale: Several places near Glendale offer HBOT services tailored to your needs. These services typically include:
Consultations with experts to figure out the best HBOT plan for you. Comfortable and safe hyperbaric chambers for your sessions. Friendly staff to guide you through the process and answer your questions. Adaptable scheduling choices to accommodate your hectic lifestyle.
Choosing a Provider:
Make sure to choose a trustworthy HBOT provider near Glendale. Look for places that focus on patient care, have trained professionals, and keep their facilities clean and safe.
Conclusion:
HBOT is a promising way to boost your health and wellness. With services available near Glendale, you have access to a natural approach to healing and rejuvenation. Whether you're recovering from an injury or just want to feel better overall, HBOT could be the solution you've been looking for.
#Top Neurologist in Glendale CA#socal hyperbaric oxygen center#neurologist glendale#neurologist in glendale#neurologist in glendale ca#hbot oxygen therapy near Glendale CA#functional neurology la#best neurologist treatment in glendale ca#neurological in glendale#neurological services Glendale#brain and spine center#Vestibular Rehabilitation Glendale#neurological care Glendale#Glendale Neurological Care#spine center glendale#socal brain and spine specialist#Neurological Rehab in Glendale#socal brain and spine#Functional Neurology in Glendale
1 note
·
View note
Text



Supernatural is your go-to destination in Hamilton for an integrated biohacking approach to inner and outer wellbeing. We offer a range of cutting-edge therapies, including IV therapy Hamilton, cryotherapy Hamilton, red light Hamilton treatments, PEMF Hamilton (Pulsed Electromagnetic Field) therapy, and access to a hyperbaric chamber Hamilton. Our programs are designed to optimize your mind and body, addressing everything from skin and hair to bone, gut, and hormone health. We empower you to take control of your aging process, recharge physically and mentally, recover faster, age better, live longer, and unlock your full potential. Explore the world of wellness at Supernatural today!
0 notes
Text
Also preserved on our archive
Some interesting science analyzed
BY BROOKS LEITNER
Imagine lying back in an enclosed chamber where you bask for 90 minutes in a sea of pure oxygen at pressures two to three times that felt at sea level. This is the world of hyperbaric oxygen therapy (HBOT), a technology that’s been around for decades and is now being explored as a possible treatment for Long COVID.
"The silence on the inside is deafening at first,” says John M.,* who has undergone dozens of HBOT treatments for his persistent Long COVID symptoms. Fortunately, there is a television outside the chamber in view, and it is easy to communicate with the provider if needed. While the potential protocol is still being refined, patients may undergo up to 40 HBOT sessions to address some of the most problematic, lingering symptoms of this complex condition.
HBOT is a therapeutic process that has been widely used to treat such conditions as decompression sickness in scuba divers, carbon monoxide poisoning, and diabetic foot ulcers. In HBOT, the body is exposed to 100% oxygen, a significant increase from the 21% oxygen concentration we typically breathe. The therapy takes place in an enclosed chamber where the air pressure is elevated above normal levels. The combination of high-pressure and high-oxygen conditions enhances the amount of oxygen that can reach the body's tissues. The hope is that this therapy can provide the same relief and healing to people with Long COVID that it does for those with other conditions.
According to John M., HBOT was the first treatment that helped with his sleep and reduced his heart palpitations. “At one point after hospitalization, my Long COVID symptoms were so bad that I could barely walk or talk. HBOT was a great tool that really assisted with my recovery,” he said. John added that he hopes the medical community will achieve a better understanding of how HBOT can help relieve suffering for patients with Long COVID and that more research will increase access to this innovative therapy.
Does HBOT improve Long COVID symptoms? One key observation from the work of Inderjit Singh, MBChB, an assistant professor at Yale School of Medicine (YSM) specializing in pulmonary, critical care, and sleep medicine, is that Long COVID patients often experience debilitating fatigue. Based on Dr. Singh’s previous Long COVID research, the exhaustion is thought to be linked to the muscles’ inability to efficiently extract and utilize oxygen.
To picture how HBOT might work, you can think of your muscles as engines sputtering, struggling to get the fuel they need. If oxygen is the gas that fuels the muscles, it’s as if you are trying to complete your daily routine while the gas tank is running on “empty.” By aiming to directly address this oxygen utilization impairment, HBOT may be a potential solution.
A systematic review by researchers at the China Medical University Hospital noted that HBOT could tackle another major factor in the Long COVID puzzle: oxidative stress. This relates to the body's struggle to maintain balance when harmful molecules, known as free radicals, run amok, causing chronic inflammation.
Research co-authored by Sandra K. Wainwright, MD, medical director of the Center for Hyperbaric Medicine and Wound Healing at Greenwich Hospital in Connecticut, suggests that HBOT, with its high-oxygen environment, might dampen this chronic inflammation by improving mitochondrial activity and decreasing production of harmful molecules. Other potential benefits of HBOT in the treatment of Long COVID may include restoration of oxygen to oxygen-starved tissues, reduced production of inflammatory cytokines, and increased mobilization of hematopoietic stem cells—primary cells that transform into red blood cells, white blood cells, and platelets.
HBOT for Long COVID: Current and ongoing research Several small-scale reports have indicated that HBOT is safe for patients with Long COVID.
To address this question, a trial that followed the gold standard of modern medical research—a randomized, placebo-controlled, double-blind design—assigned 73 Long COVID patients to either receive 40 sessions of HBOT or a placebo of only 21% oxygen. The study observed positive changes in attention, sleep quality, pain symptoms, and energy levels among participants receiving HBOT. In a longitudinal follow-up study published in Scientific Reports, the authors at the Tel Aviv University found that clinical improvements persisted even one year after the last HBOT session was concluded. In a second study, the same authors focused on heart function, measured by an echocardiogram, and found a significant reduction in heart strain, known as global longitudinal strain, in patients who received HBOT.
In another study, 10 patients with Long COVID underwent 10 HBOT treatments over 12 consecutive days. Testing showed statistically significant improvement in fatigue and cognitive function. Meanwhile, an ongoing trial at the Karolinska Institute in Sweden has reported interim safety results wherein almost half of the Long COVID patients in the trial reported cough or chest discomfort during treatment. However, it was unclear whether HBOT exacerbated this symptom or if this adverse effect was due to the effort of participation by patients suffering from more severe Long COVID symptoms.
Is HBOT currently available as a treatment for Long COVID? For HBOT to become a mainstream treatment option for Long COVID, several critical priorities must be addressed. First, there is currently no established method for tailoring HBOT dosages to individual patients, so researchers must learn more about the specific features or symptoms that indicate potential benefits from HBOT. At the same time, we need to identify factors that may be associated with any adverse outcomes of HBOT. And finally, it’s important to determine how long these potentially beneficial effects last in a larger cohort. Will just a few HBOT trials be enough to restore patients to their baseline health, or will HBOT become a recurring component of their annual treatment regimen?
For now, HBOT remains an experimental therapy—and as such is not covered by insurance. This is a huge issue for patients because the therapy is expensive. According to Dr. Wainwright, a six-week course of therapy can run around $60,000. That’s a lot to pay for a therapy that’s still being studied. In the current completed studies, different treatment frequencies and intensities have been used, but it’s unclear how the treatment conditions affect the patient’s outcome.
“I have had some patients notice improvements after only 10 or 15 treatments, whereas some others need up to 45 treatments before they notice a difference,” notes Dr. Wainwright. “I think that HBOT is offering some promising results in many patients, but it is probably a strong adjunctive treatment to the other spectrum of things Long COVID patients should be doing, like participating in an exercise, rehab, and nutritional program.”
Dr. Singh notes that “a major challenge for research is the heterogeneity of Long COVID. It is hard to determine which symptoms to treat and enroll patients into trials based on them.”
Perhaps treatments that target multiple issues caused by Long COVID, like HBOT, may help overcome this challenge.
*Not his real name.
Brooks Leitner is an MD/PhD candidate at Yale School of Medicine.
The last word from Lisa Sanders, MD: Hyperbaric oxygen therapy (HBOT) is just one of the many existing treatments that are being looked at to treat Long COVID. We see this with many new diseases—trying to use a treatment that is effective in one set of diseases to treat another. And there is reason for optimism: We know that HBOT can deliver high levels of oxygen to tissues in need of oxygen. That’s why it’s used to treat soft tissue wounds. If reduced oxygen uptake is the cause of the devastating fatigue caused by Long COVID, as is suggested by many studies, then perhaps a better delivery system will help at least some patients.
Studies referenced:
bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-023-08002-8
www.ncbi.nlm.nih.gov/pmc/articles/PMC8806311/
www.nature.com/articles/s41598-024-53091-3
www.nature.com/articles/s41598-022-15565-0
www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2024.1354088/full
www.ncbi.nlm.nih.gov/pmc/articles/PMC11051078/#:~:text=Proposed%20Mechanism%20of%20HBOT%20o
#long covid#hbottherapy#HBOT#hyperbaric oxygen therapy#mask up#covid#pandemic#wear a mask#public health#covid 19#still coviding#wear a respirator#coronavirus#sars cov 2
20 notes
·
View notes
Text
Jiara Pregnancy Season 5 (Rumors, Interviews, Theories)
Could Kiara Be Pregnant in Outer Banks Season 5?

As Outer Banks fans eagerly anticipate the fifth and final season, one theory has gained traction: Could Kiara be pregnant? While it may seem like a far-fetched plot twist, a closer look at the narrative and character developments throughout the show reveals several subtle hints that could suggest this storyline. In this think piece, we’ll explore the reasons why a potential pregnancy for Kiara might not be as unlikely as it seems.
1. The Emotional Connection Between Kiara and JJ (Pre-Death)
One of the most significant developments in Outer Banks Season 4 is the deepening bond between JJ and Kiara, culminating in their intimate moment in the hyperbaric chamber. Their relationship has always been a fan-favorite, but the intensity of this scene cannot be overlooked. As fans noticed, the pair were sweaty and emotionally charged, which, along with other physical cues, implied that something more than just a kiss occurred .
This scene marked a turning point in their relationship, and with their growing emotional closeness, it’s reasonable to speculate that their connection could have lasting consequences. A pregnancy would not only serve as a dramatic turn in their story but would also deepen the stakes for both characters, particularly following the emotional weight of JJ’s eventual death . The possibility of Kiara carrying JJ’s child could represent a bittersweet legacy and a continuation of his spirit.
2. Kiara’s Parents’ Warning in Season 2
In an earlier season, Kiara’s parents expressed concern about her association with the Pogues, warning her that she could end up pregnant by one of them. This line, although delivered in a judgmental manner, has taken on new significance as Kiara’s relationship with JJ has evolved. Fans have revisited this moment as a subtle hint, suggesting that the writers may have planted the seed for this storyline well in advance .
If Kiara were to find out she’s pregnant, it would not only bring this warning full circle but would also offer an opportunity to explore her relationship with her parents in a more profound way. The pregnancy could lead to tension with them, adding to Kiara’s internal conflict between her loyalties to the Pogues and the expectations placed on her by her family.
3. The Impact of JJ’s Death
The death of JJ in the Season 4 finale could serve as a catalyst for a number of emotional arcs in Season 5. Fans have speculated that Kiara’s potential pregnancy could be a way for the writers to honor JJ’s legacy, providing a sense of continuity even after his tragic end. A child would serve as a poignant reminder of their bond and the love they shared in their final moments. It would also give the Pogues an emotional anchor as they navigate the challenges of the final season .
4. The Pregnancy Theory vs. Sarah’s Pregnancy
Another factor complicating the potential for Kiara’s pregnancy storyline is the confirmation of Sarah’s pregnancy in Season 5. This development could make the writers cautious about introducing another pregnancy arc, as it might feel repetitive. However, if handled differently, Kiara’s pregnancy could still stand apart. While Sarah’s storyline might focus on the joy and challenges of motherhood, Kiara’s pregnancy could explore themes of grief, legacy, and survival—giving her character a unique narrative that contrasts with Sarah’s .
5. Fan Speculation and Thematic Depth
The theory of Kiara being pregnant has sparked a significant amount of fan speculation, with many viewers revisiting key moments from previous seasons, particularly Season 4, where JJ and Kiara’s connection was front and center. The idea of Kiara potentially being pregnant fits well within the show’s larger thematic exploration of family, loss, and coming-of-age struggles. It would provide another layer of emotional depth to an already complex character, forcing Kiara to reconcile her adventurous spirit with the responsibilities of parenthood.
Conclusion
While there is no official confirmation that Kiara will be pregnant in Outer Banks Season 5, the theory remains compelling for several reasons. The growing bond between JJ and Kiara, combined with the hints dropped in earlier seasons and the potential for emotional conflict, makes the possibility of a pregnancy plausible. With Season 5 set to explore deeper emotional arcs, Kiara’s potential pregnancy could be a way for the writers to highlight themes of legacy, love, and loss, while adding an additional layer of drama to the final season.
As we await more details, it’s clear that the theory resonates with many fans, and whether it comes to fruition or not, it speaks to the enduring investment viewers have in Kiara’s journey—and the fate of the Pogues.
12 notes
·
View notes
Text
At his rally on Sunday at New York City’s Madison Square Garden, former president and Republican presidential nominee Donald Trump said that if elected he would allow wellness conspiracist and anti-vaccine activist Robert F. Kennedy Jr. to “go wild on health.” Kennedy, a former Democrat and scion of the famous political family, initially ran as an independent third-party and potential spoiler candidate, and has spent the better part of two decades spreading conspiracy theories that would likely inform the policies of a Trump administration.
In August, Kennedy suspended his presidential campaign and threw his weight behind Trump. (Both the Trump and Kennedy campaigns received support from billionaire donor Timothy Mellon.) There were early indications that he might have a place in a possible Trump administration, particularly in some areas focused on health. Kennedy himself even created a spinoff of Trump’s MAGA slogan with his own Make America Healthy Again, or MAHA. But Trump’s speech seems to indicate that Kennedy would indeed have a place in the cabinet, perhaps running Health and Human Services (HHS).
Kennedy has since hit the campaign trail stumping for Trump alongside another former Democrat and conspiracy theorist, Tulsi Gabbard.
Kennedy has spent years spreading health mis- and disinformation, particularly about vaccines. In 2014, Kennedy joined Children’s Health Defense (CHD) as a member of its board. CHD pushes debunked conspiracy theories linking conditions like autism with vaccines and other environmental factors. In 2021, Meta banned Kennedy’s Instagram account for spreading disinformation about the Covid-19 vaccine, and he was named by the Center for Countering Digital Hate (CCDH) as one of 12 people responsible for 65 percent of vaccine disinformation across Instagram, Facebook, and Twitter. Thanks to the Covid-19 pandemic, Kennedy’s own profile, as well as that of CHD, began to rise. CHD raised more money in 2021 than it ever had before.
Meta reinstated Kennedy’s Instagram account last year when he announced his run for the presidency, and it remains up, despite the fact that he is no longer running for office. CHD remains banned from Meta’s platforms. More recently, Kennedy has echoed unfounded conspiracies that could undermine faith in the integrity of the 2024 elections.
During his presidential campaign, Kennedy tried to distance himself from the anti-vax movement. Still, he continued to spread disinformation, like falsely saying that the Biden administration had violated the Nuremburg Code by mandating vaccines. And his vision for making America healthy again is drastic. Last Friday, he posted on X to warn the Food and Drug Administration (FDA) that its “aggressive suppression of psychedelics, peptides, stem cells, raw milk, hyperbaric therapies, chelating compounds, ivermectin, [and] hydroxychloroquine” was about to end.
The Department of Health and Human Services oversees 13 agencies, including the FDA and the National Institutes of Health (NIH). In an interview with NBC News while he was still running for president, Kennedy said he would gut those agencies, which he has said are now captured by corporations. He would also impose more testing on already existing vaccines, which health experts told NBC would result in many children being unable to get vaccinated. (Trump, for his part, has claimed he would withhold funding from schools that require vaccination.) Kennedy’s plan would also include dismissing scientists at the NIH who study infectious diseases, focusing instead on the environmental factors and vaccines that he believes cause illnesses.
During his campaign, he held a health policy roundtable with doctors that pushed fake Covid-19 treatments.
Trump campaign spokesperson Steven Cheung told WIRED that “President Trump announced a Trump-Vance transition leadership group to initiate the process of preparing for what comes after the election. But formal discussions of who will serve in a second Trump Administration is [sic] premature.”
8 notes
·
View notes
Text
17 || CHS

Pairing: Vernon x f.reader
Genre: Hurt/Comfort, Friends to Lovers, First Love, Fluff, Slice of life
WC: 1k
Summary: On your wedding day to Vernon, you flashback to the day you first met him, back when you were classmates in school & how you fell in love at first sight. This chronicles your fluffy, at times angsty love story from your meet cute till the day of your wedding.
A/N: True Story (almost), inspired by the song 17 by Pink Sweat$ & SVT 🌊🌙⭐️
Prologue
Walking down the aisle in a white gown while keeping my eyes trained on my groom, was as easy as breathing in a hyperbaric chamber. But it shouldn't have been, not when I hated being the center of attention, not when I wore high heels that threatened to break my fall, not when breathing itself was hard with me being an asthmatic, yet against all odds, he made everything easier by simply being present. Being in love is often described as having your breath taken away but with him, it was like he gave me the breath of life. Chwe Hansol was like a breath of fresh air in my suffocating existence. Every time, I'd been gasping for air, he'd been there, keeping me alive, I still remembered the first time we'd met like it was yesterday.
"I wanna love you as strong, when we're 92 the same as 17."
Chapter 1 - 17
Shifting to a new school was something I'd always dreaded. But I had the practice, given that my dad had a job that kept sending him on projects across the world and this was my 7th school in many years. But this one mattered more than the rest, this is where I'd do my high school, that part of my school life that was romanticized beyond my imagination. But it was nothing like the books, movies, songs had told me it would be.
Shifting to a new country meant no one spoke in English, everyone spoke in Korean even though the teaching took place in English in this so called fancy international school in Seoul which I'd been assured was the best of the best. But here I was, back to crying in bathroom stalls, eating lunch alone and being bullied and excluded by the class for being an outsider. They hated me for scoring straight A's without realizing that studying was my only constant in a childhood where I kept shifting cities and losing friends, for not being beautiful enough as per Korean standards without understanding what steroids do to a child suffering from a chronic illness and they hated me because all the adults loved me, not knowing that when they praised me for being so mature for a child my age, I didn't take it as a compliment but a consequence of having lived through trauma.
So naturally, I did the only thing that made sense to me, I studied through the day, cried myself to sleep at night. If it wasn't bad enough that I was being troubled by the students, there was a teacher who took pleasure in making my life harder. The swim coach made it her life's mission to humiliate me because I couldn't swim in the deep end like the others, though she refused to give any instructions in English, I had to not only try to comprehend and follow her Korean instructions but it also meant I couldn't explain my asthma to her because she wouldn't give me any time of her day. I was trying my best to pick up swimming, to push myself to my best but it was never enough for her. Until the day when it time for the swim practicals and despite my many refusals, she wanted everyone to swim from the deep end. None of the students helped me as I tried to explain in my broken Korean that I couldn't pull this off and the coach assumed I was just being lazy and making excuses. She ended up doing what she did with any student who she thought needed to learn a lesson, she pushed me unsuspectingly into the pool, expecting me to just swim my way out of it. And I tried, I promise you I did. But it simply wasn't enough, and sure enough I started drowning somewhere around the 9ft mark.
At first, I started flailing reflexively but somewhere in the back of my mind, the thought that it wouldn't be so bad to give up made it's home and I stopped trying. I hated my life, I wanted the pain to stop so this wasn't a bad idea was it? It would be so easy to just let go. Except just as I made up my mind to give up, I felt an iron clad grip on my wrist, refusing to let go. Next thing I knew I was coughing up water & back on dry land, the first thing I heard was his deep voice arguing with the teacher in Korean, I could barely get the gist but turned out that he was defending me in front the teacher. He seemed to have put 2 & 2 together from the class in panic had confessed that they knew I had asthma but refused to tell the teacher this because they thought it would've been fun to watch me suffer. I couldn't explain the surge of warmth I felt at the fact that someone was finally standing up for me, when I couldn't. But the next thing he did, made me break down entirely, I didn't believe in love at first sight but I was a goner right then & there.
He turned to me with his tender gaze, "Are you okay? I'm so sorry about what happened. I promise I'll speak to my father about it, he's on the school board. You'll be okay, but for now let's just get you to the school nurse okay? Do you feel okay to stand up?? Can you walk?" At first, I thought the lack of oxygen had messed up my brain, he was just speaking in fluent Korean then how was I understanding him so perfectly? Until, it struck me that he'd switched to english, the words slipping off his tongue like it was second nature. I couldn't believe it, finally, I had someone who understood me, someone who saw me for who I was. Nothing felt better than telling him, "Thank you, thank you for saving my life." Because he had, not just literally but even metaphorically. And in that moment, I could already picture our future- shaking hands and becoming friends at the nurse's office, library study hangs that soon became date nights, our first kiss after he scored the winning goal at the football match, dancing under the stars during prom night as the DJ played, "17 by Pink Sweats & SVT" and recreating that moment by playing the same song, as I walked down my wedding aisle a decade later.
"We'll be dancing the same groove, when we're 92, the same as 17."
To Be Continued... 🌊🌙⭐️
#vernon#hansol vernon chwe#chwe vernon#chwe hansol x reader#chwe hansol#vernon svt#vernon fic#seventeen#seventeen fic#svt carat#svt x reader#Spotify
12 notes
·
View notes
Text
Laura Bassett at Men's Health:
LESS THAN A year after launching his independent campaign for president, Robert F. Kennedy Jr. began shopping around his endorsement—and the loyalty of his small but significant base—to both major political parties in exchange for a cabinet position. Kamala Harris reportedly rejected a meeting with him outright. Donald Trump, however, has taken him up on the offer, announcing that in exchange for Kennedy’s endorsement, he’d let the anti-vaccine candidate “go wild” on health, food, and medicine if he wins a second term. Kennedy says Trump has promised him control of multiple government agencies, including the Department of Health and Human Services (HHS)—which includes the Food and Drug Administration (FDA) and Centers for Disease Control and Prevention (CDC)—and the Department of Agriculture (USDA). Therefore, a hybrid anti-vax and Make America Great Again (MAGA) movement was born: MAHA, short for “Make America Healthy Again.”
Supporting this movement to push Kennedy voters toward Trump is the MAHA Alliance, a Super PAC led by Del Bigtree, former communications director for the Kennedy campaign and CEO of the anti-vax group Informed Consent Action Network. The operation appears to be widely geared towards men, partnering with right-wing influencers like Russell Brand and Jordan Peterson who champion traditional masculinity, and aims to combine “the health-conscious, independent-minded voters with Trump’s proven ability to disrupt the status quo,” according to its mission statement. “This includes prioritizing regenerative agriculture, preserving natural habitats, and eliminating toxins from our food, water, and air.”
Some of MAHA’s goals sound pretty great in theory—especially during a time when public trust in the medical system and American food safety are so low. Incentivizing sustainable farming, improving soil health, protecting natural habitats, and cleaning up our air, water, and food are goals everyone should be able to get behind, paired with a viable policy strategy and leaders who are actually willing to take on the big oil and big agriculture lobbies to address our systemic environmental problems.
[...]
Meanwhile, other ideas being pushed by the movement and by Kennedy himself—like eroding public trust in vaccines and peddling pseudoscientific alternatives to vaccines—are downright dangerous to public health. In an October 25 post on X, Kennedy threatened to dismantle the entire FDA if Trump is elected, accusing the agency of “aggressive suppression of psychedelics, peptides, stem cells, raw milk, hyperbaric therapies, chelating compounds, ivermectin, hydroxychloroquine, vitamins, clean foods, sunshine, exercise, nutraceuticals and anything else that advances human health and can’t be patented by Pharma.”
Many of these buzzwords he’s using—ivermectin and hydroxychloroquine in particular—are just snake oil alternatives to the Covid vaccine that don’t work, and in some cases, actually kill people. Jennifer Nuzzo, Ph.D., Professor of Epidemiology and Director of the Pandemic Center at Brown University School of Public Health, told me that Kennedy’s tweet “is straight from the anti-vaxxers' playbook that aims to sow doubt about credible medical approaches in order to sell and profit from unproven alternative approaches.”
[...]
Encouraging people to drink raw milk is another very dangerous health trend being promoted by supporters of the movement. Rep. Marjorie Taylor Greene (R-Fla.) recently waded into this one, tweeting a glass of unpasteurized milk with the caption, “Raw milk does a body good. Make America Healthy Again!” The problem is, by skipping the process of killing off harmful bacteria in milk, we are leaving it potentially contaminated with lethal pathogens. “Pasteurization has been one of the most effective public health measures ever, essentially ending the illnesses that used to come from drinking tainted milk,” explains Dr. Nestle. “Infectious diseases used to be the leading causes of death and disability among Americans. Public health measures effectively ended them. It makes no sense to bring them back.”
One thing MAHA gets somewhat right is addressing the serious health harms of microplastics and “forever chemicals,” which have been linked to chronic disease, heart attack, and stroke. It’s great that we’re starting to pay attention to those. Unfortunately, though, the Trump administration created a loophole during his final few months in office that allows companies to dodge having to report how many forever chemicals they’re discharging into the environment.
Laura Bassett wrote in Men’s Health what the MAHA movement gets right and wrong (and it’s mostly wrong) about our state of health.
#Robert F. Kennedy Jr.#MAHA#Donald Trump#Make America Healthy Again#2024 Presidential Election#Public Health#Processed Foods#MAHA Alliance#Del Bigtree#Food Safety#Food#Ultra Processed Foods#Ivermectin#Coronavirus Vaccines#Hydroxychloroquine#Big Pharma#Raw Milk#Forever Chemicals
6 notes
·
View notes
Text
me: i dont really autoship and outside of the silly lil ana-sonny ship i have buried in my back pocket i dont exactly ship any of the kiddos together by default
also me: part of danny's story centers around the ocean, alot of his aesthetics stem from the deeper waters & storm-torn seas, his post-house work & trade is literally shipyard & hyperbaric welding that puts him under in deep waters and its ridiculously dangerous and pays high due to it. so many little parts of my danny connect to the ocean and its in part because subconsciously its still danny-julie to me sorry gun youre wrong yet again but also because he would more than happily move & live wherever his partner wants to be, he's a roamer / nomad / wanderer / etc and hyperbaric welding pulls them to all different places depending on the job & contract so he'd happily settle wherever he aint picky and for julie in particular he'd live anywhere coastal so she can enjoy the beaches nearby if she wanted that
.
#also theres quite a few songs in his playlists that have ocean-themes in some capacity and i just. yeah-#again chemistry IS big to me but i cant say i subconsciously still tie them together lmao#[ ♡ ] ── * raphael a-o. / 𝘭𝘰𝘳𝘦.
5 notes
·
View notes
Text
i just saw the most beautiful act of love. gonna be sappy in the tags real quick :’)
#okay so some background: i work in a wellness center that has a good handful of medical services along with our other ones and one of the#medical services we offer is hyperbaric oxygen therapy?? <- in case you don't know what that is it's basically like a sleeping bag that we#zip you up in and give you a nasal canal with 90% oxygen and we pressurize the bag so it's similar to going up in an airplane. it's good fo#mental clarity and also for getting better sleep. like 1 hour in there is equivalent to 4 hours of REM sleep. super cool!!#also we use walkie-talkies to communicate with you since you're all sealed up in there and it takes like 10 minutes to pressurize up n down#however!! one of the other benefits is that it can help with symptoms of dementia. i've seen people with brain injuries come in before but#today was my first time seeing someone do it for dementia. and he brought his wife in with him for support#i just walked over and saw her sitting on the floor beside the chamber he was in and she was smiling and staring at him through the window#she was speaking into the walkie and laughing with him and i just. the idea of her wanting to be with him in these hard moments 🥺#she's now reading a book but still sitting right there on the ground beside him. my nurse offered her a chair but she's not leaving his sid#i just i can't y'all i love love.#chelsea speaks
4 notes
·
View notes
Text
Hyperbaric Medicine (HBO)
I'm sorry, what is that?

I have a side hustle as a hyperbaric medicine provider and I am here to give you the down and dirty!
Sometimes referred to as HBO (hyperbaric oxygen), hyperbaric or dive medicine is a specialty that utilizes oxygen at high pressure to treat a variety of conditions, primarily things involving wounds. We place a patient in a chamber, deliver 100% oxygen to them, pressurize the chamber, and keep them in there for about 120 minutes. Since oxygen is the number one thing you need to heal a wound, we use a lot of it to try and speed up the process.
The Basics
Wait - what? HOW? Try not to have PTSD from your days in chemistry, but remember these?

The treatment physiology of hyperbarics relies on gas laws. Recall that it takes a lot of pressure to dissolve a gas into a liquid.
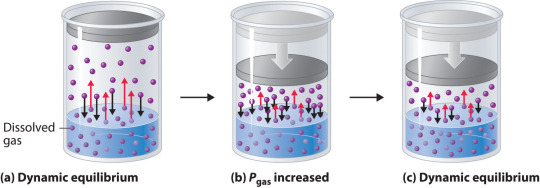
We use pressure to force oxygen into the blood stream at high rates to facilitate wound healing. For reference, most of your oxygen content is bound to hemoglobin (~98%). You do have dissolved oxygen in your blood, represented by your PaO2/PvO2 in a blood gas. However, this makes up a fraction of O2 content (~2%: if you want a clinical soap box, you should hear me talk about blood gases to students lol). A normal ABG would have a PaO2 of 65-100. An ABG acquired during hyperbaric treatment would be well over 2,000.
As an aside, recall that ambient air is 21% oxygen. Also, as a reminder, we exist at 1.0 ATA of pressure (one atmosphere).
How is it done?
Delivering oxygen this way requires delivery of a lot of pressure. We utilize dive chambers for this purpose. There are two types of chambers:
Monoplace: literally looks like a class coffin. Holds one patient and delivers oxygen at pressure through the entire chamber. These are very popular at wound centers.

Multiplace: literally looks like a submarine. Holds 2+ patients and delivers oxygen at pressure to individual patients hooked up to hoods or masks. These are found at tertiary care/academic medical centers.

Literally, the multiplace hoods make you look like a silly space person.

The reason oxygen is delivered this way in a multiplace chamber is to reduce the risk of fire. Oxygen at pressure can go boom. Having an entire chamber full of O2 is a big risk. So, we deliver the gas individually to each patient.
How did it start?
Dinking around with gases at pressure has been a thing for 400 years. However, it didn't become a more focused endeavor until the first dive suits started to be a thing in the 1870s. The specialty itself is relatively new, developed in the 1930s due to advent of decompression illness with divers. Things really progressed in the 1950s.
One pivotal study was "Life without Blood" in 1959. Dr. Boerema proved that he could keep a pig alive with HBO alone. The ethics of this experiment are questionable but he exsanguinated a pig under hyperbaric conditions (3.0 ATA, 100% FiO2). Plasma was left behind. By doing this, he proved that, at pressure, an organism does not need hemoglobin to live. Kind of a radical thing to prove! Don't worry, the pigs did get their blood back and recovered without issue.
What is treated with HBOT? (hyperbaric oxygen therapy)
Anything related to wound healing can be treated with HBOT. We also treat carbon monoxide poisoning, air gas embolism, and decompression sickness with HBOT. I'll start with those since they are (imo), the most clinically interesting. ;-D
Carbon monoxide poisoning: The physiology of using HBOT to treat CO poisoning is based on the binding affinity of CO to hemoglobin. CO has 200 x the binding affinity for hemoglobin than O2 or CO2 does. Because the binding sites are taken up by CO, hemoglobin cannot pick up O2. It also can't offload whatever O2 is already bound. The goal with HBOT is to bombard the blood with massive amounts of O2 to force CO off.

For reference, it would take about 6 hours for CO to offload on its own from hemoglobin on room air. It would take half as long at 100% FiO2 delivered at standard air pressure (1.0 ATA). CO is rapidly forced off within 30 minutes with HBOT. With very severe CO poisoning, particularly in cases of LOC, this is vital for limitation of hypoxia and neurological sequelae of exposure. Treatment is 1-3 "dives" depending on clinical context. The patient is treated at 2.8 ATA (60 feet of sea water) for about 120 minutes.
Air gas embolism: This occurs when gas is accidentally introduced into circulation. It can either be venous or arterial. The venous system has much more flexibility in tolerance for air bubbles. 15 cc or less of gas introduction is probably not going to result in symptoms. Higher volumes go to the lungs and can result in local lung infarction.
The real danger with this is air introduced into arterial circulation. Depending on where it is introduced, it can go directly to the heart causing an MI, or to the brain causing a stroke. Any volume of air introduced into arterial circulation is bad news bears. Treatment is usually 1 "dive" but could be more based on the context. The patient is treated at 2.8 ATA for 30 minutes and then the ascent is extremely slow. The whole dive takes about 5 hours. Why so long? If we ascend too quickly, the air bubble will reform.
Decompression sickness: This occurs primary with scuba divers who ascended too quickly. Scuba divers generally breath mixed gas, most commonly air (21% O2, ~79% N2) or nitrox (35% O2, ~65% N2). As someone is diving, the nitrogen they breath is also dissolved into their blood since they are at a pressure greater than 1.0 ATA. If a diver ascends too quickly, the nitrogen dissolved in the blood will rapidly reform air bubbles in the blood. We just mentioned how that is problematic.
Since air bubbles can go everywhere in circulation, the symptoms are variable ranging from headache, vertigo, nausea, joint pain, chest pain, stroke symptoms, loss of bowel/bladder function, etc. The treatment for this is to recompress the patient and very slowly ascend in the HBO chamber. Treatment is usually 1 dive but could be more based on the context. The patient is treated at 2.8 ATA for 30 minutes and then the ascent is extremely slow. The whole dive takes about 5 hours. Why so long? Again, if we ascend too quickly, the air bubble will reform.
Wound related conditions: there are roughly 15 approved diagnoses for HBO by Medicare in the USA. This is important to mention because if a condition is not covered, paying out of pocket is extremely cost-prohibitive. Insurance is billed $6,000 per treatment! Some of the most common conditions treated are osteoradionecrosis, soft-tissue radionecrosis, irradiation cystitis with hematuria, and refractory chronic osteomyelitis. Wounds created from radiation exposure have the best evidence to support the use of HBOT. These are considered outpatient conditions so patients come to be treated Monday-Friday. We dive to 2.4 ATA for 120 minutes. At minimum, patients are prescribed 20 dives but most treatment protocols for radiation induced injuries is at least 40 dives.
As you can see, this is a HUGE commitment for the patient. One dive is not enough for these wound related conditions. As a hyperbaric provider, I can say that we have patients with such significant symptom relief from HBO. For example, irradiation cystitis with hematuria is extremely debilitating. Patients are fatigued from chronic blood loss, deal with painful bladder spams and pelvic pain, pain with urination, and increased frequency. The blood can clot and obstruct their urethra or foley catheter. Symptoms like this limit quality of life. HBOT makes a huge difference for them.
Benefits
Anyone who has barriers to wound healing can benefit from HBO. Barriers include vascular disease, CKD, COPD, DM, heart failure, and immunocompromised status. The goal is symptom resolution/improvement or healing of the wound. Some patients get approved for far more treatments than we typically do. Usually the maximum insurance will cover is 60. However, in some situations, the clinical benefit of continued treatments is recognized by insurance and treatment is extended.
As a provider, I get to know these patients pretty well. They show up every day that I am staffing in HBO and it is rewarding to see them improve. Compared to my critical care role, this is a nice change of pace.
Adverse Reactions and Risks
There are risks and side effects to HBO. The most common are barotrauma, pneumothorax, seizure, temporary worsening of cataracts/vision, and abdominal distention.
Barotrauma of the ears and sinuses is by the most common issue we face in HBOT. If patients are not able to clear their ears as they descend ("pop" their ears), they can rupture their ear drums. Patients that cannot descend without extreme pain may need myringotomy tubes (ear tubes) to assist with equalizing pressure.
Seizure is a risk of HBOT and that primarily comes from oxygen reducing the seizure threshold. We mitigate this with "air breaks". These are 5 minutes intervals of the treatment where the patient is receiving air rather than 100% O2. Example, we treat at 100% for 30 minutes, have a 5 minute air break, repeat x 2. Obviously the people at highest risk are those with epilepsy or taking seizure threshold reducing medications.
HBOT can worsen cataracts and vision temporarily. The mechanism of this is poorly understood but we know it is reversible. Distance vision is affected the most.
Contraindications
The only absolute contraindication to HBOT is an untreated pneumothorax. There are many relative contraindications that require a risk benefit analysis. An example of this is pregnancy. HBOT has not been thoroughly studied in pregnancy and is not recommended EXCEPT in cases of CO poisoning where we know that the CO concentration is higher in fetal circulation than maternal. Always treat a pregnant person with CO poisoning.
Other potential contraindications include use of certain chemotherapy agents, COPD with blebs/bullae, severe heart failure, epilepsy, sinus/HEENT disease, claustrophobia, certain implanted devices, or active infection.
With certain chemo agents, they can lower the seizure threshold putting patients at higher risk of seizure in the chamber. People with COPD and blebs are at risk of those blebs popping under pressure and causing acute respiratory distress. People with heart failure can experience flash pulmonary edema after an HBO treatment. If people are claustrophobic, obviously spending time in a monoplace chamber can trigger panic attacks. At my center, we sometimes have people referred to our multiplace chamber for exactly that reason.
Most implanted medical devices are HBOT compliant. Generally, pacers and other devices are tested at 4.0 ATA of pressure. We double check with the manufacturer that the device is compliant. If it isn't, we cannot safely treat and have to deny the consult.
Obviously, if someone is sick, we don't want them in the chamber. Particularly colds, severe allergies, fever, or anything that is affecting HEENT. People with acute sinus infection are unable to clear sufficiently to dive. Even if they can clear, they feel miserable. No need to go through that.
Safety Issues
I mentioned that high O2 environments are at risk for explosion. Safety is the number one concern with any chamber. The goal is to reduce risk of fire by removing fabrics that create static (anything synthetic), removing electronic devices that are not HBOT approved, and going through multiple levels of safety checks for patients and for chamber preparation.
At our chamber, only 100% cotton is allowed in the chamber. All patients have special scrubs that they wear during treatment. No electronic devices can be brought in the chamber which includes phones, tablets, laptops, e-readers, watches, pagers, etc. We do have HBOT approved IV pumps and radio headsets that we use. These have been tested at 4.0 ATA. The radio headsets are for the attendant (staff member) who is in the chamber and this is also for safety purposes. Since we have a mulitplace chamber, a staff member is always in the chamber with the patient(s).
One thing I do want to address is that some people are concerned about putting a patient with active cancer into the chamber. There is concern that the high O2 environment will "feed" the cancer. There is simply not data to support this. Active cancer is not a contraindication to HBOT.
And there you have it! The down and dirty of HBOT! Hopefully you learned something cool. If you think you have a patient who would benefit, find your local HBOT provider. We are always happy to talk with you about the process. If you care about a soapbox of how insurance companies suck, see below. :-D
Soapbox: I will say, I have definitely been frustrated with insurance companies. They are the gatekeepers of this treatment. You can have several providers supporting the use of treatment and an insurance company can still say "no". Very frustrating.
A prime example of this are patients who have avascular necrosis that is steroid or chemotherapy induced. These are often younger patients (late teens, early 20s) who have/had leukemia of some kind. They end up having necrosis at a joint, usually the femoral head, that will likely result in complete joint replacement at a young age. No orthopedic surgeon wants to replace joints on a young person. It comes will all kind of problems and always needs revision later in life.
Insurance companies will say "we only cover radiation induced necrosis" because that is what the literature supports. Yes, they are correct that the vast majority of studies support HBOT for radiation induced injury. However, the pathophysiology of the tissue destruction, while a little different, ends up with the SAME problem. There are studies that support HBOT use in these situation but not nearly as many as radiation induced injury. The result is that patients suffer, get a joint replacement they could have avoided (or postponed until they are fully developed), and generally are shafted.
*end soapbox*
#pablr#medblr#nurblr#pharmblr#physician assistant#physician associate#doctor#physician#hyperbaric medicine#hbot#hbo#medicine#oxygen therapy
6 notes
·
View notes
Text
youtube
Dr Alfred Vaughn Jackson in Knoxville, TN is an ER physician working at multiple locations as staff ED physician as well as ER director role at Jamestown Regional Medical Center. Dr Alfred Jackson is the director of the Hospitalist department at Westbrook Medical Center treating admitted patients as well as wound care specialist, with the additional treatment using Hyperbaric Oxygen therapy. Dr Alfred Jackson brings real ER and hospitalist experience into the primary care role allowing the hospital to care for more complex disease conditions.
Dr Alfred Jackson Westbrook Medical Center 930 Adell Ree Park Ln #2543 Knoxville, TN 37909 865-769-2600 https://www.westbrookmed.com/ https://www.linkedin.com/in/vaughn-j-68736883 https://www.doximity.com/pub/alfred-jackson-md-8e7a
#Dr Alfred Vaughn Jackson#Dr Alfred Jackson#Alfred Vaughn Jackson#Knoxville#TN#Westbrook Medical Center#Acute Care Clinic#Jamestown#Tennessee#University Of Tennessee Medical Center#Youtube
2 notes
·
View notes
Text
BRAIN WOUND UPDATE #10: AVIV Clinic Press Release: Review of Scientific Basis of HBOT for TBI

BRINGING YOU CURRENT INFORMATION ABOUT HOW TO HELP TREAT AND HEAL BRAIN WOUNDS: CONCUSSIONS, TBI, PTSD ORLANDO, Fla., Aug. 01, 2023 (GLOBE NEWSWIRE) -- Aviv Clinics, one of the most advanced brain clinics in the world, shares the results of a new comprehensive literature review that shows hyperbaric oxygen therapy (HBOT) should be recommended as an effective therapy for patients suffering with chronic mild traumatic brain injury (TBI). Chronic mild traumatic brain injury occurs when symptoms from a mild traumatic brain injury are prolonged and last for more than six months. The literature review, The efficacy of hyperbaric oxygen therapy in traumatic brain injury patients: literature review and clinical guidelines, was conducted by the Sagol Center for Hyperbaric Medicine and Research at Shamir Medical Center, Tel Aviv University and University of Pittsburgh Medical Center’s neurosurgery department, and published in the official journal of the European Society of Medicine, Medical Research Archives. The literature review evaluated articles and human clinical trials data from 1969 to April 2023 that provided detailed information on the type of HBOT treatment and clinical outcomes. The articles were categorized into acute-subacute traumatic brain injury and chronic traumatic brain injury and evaluated by HBOT experts and esteemed research leaders Dr. Shai Efrati, director of the Sagol Center and co-founder of Aviv Scientific; Dr. Amir Hadanny, chief medical officer at Aviv Scientific and chief medical research officer at the Sagol Center; and Dr. Joseph Maroon, vice chairman of the Department of Neurological Surgery at the University of Pittsburgh Medical Center. The literature review concluded that HBOT should be recommended for chronic traumatic brain injury for a selected group of patients suffering from prolonged post-concussion syndrome (PPCS) who have clear evidence of metabolic dysfunctional brain regions and who have been properly evaluated by standardized cognitive tests and functional brain imaging. Evidence involved in the review, including seven randomized controlled trials and six prospective studies, suggested significant improvement in cognitive function, symptoms and quality of life in patients with chronic mild traumatic brain injury. For acute moderate-severe TBI, the review concluded that HBOT may be recommended as a treatment but explained that further studies are needed to both evaluate outcomes and determine the optimal treatment protocols. Evidence in the review, including nine randomized controlled trials, one meta-analysis and two prospective studies evaluating the clinical effects of hyperbaric oxygen therapy in patients suffering from acute and subacute traumatic brain injuries, showed mortality was significantly reduced but mixed results for favorable functional outcomes in survivors. “This literature review scoured an immense amount of data related to HBOT as a therapy for traumatic brain injury, and the evidence that HBOT is effective against chronic traumatic brain injury is clear,” said Dr. Amir Hadanny, Chief Medical Officer at Aviv Scientific and Chief Medical Research Officer at the Sagol Center. “When looking at the comprehensive data over a larger stretch of time, we’re seeing the quality of studies have improved, and it’s exciting to see HBOT research heading further in the right direction. Many people are dealing with symptoms of chronic traumatic brain injury, and the current rehabilitation methods are limited in their efficacy. The science behind how HBOT can be effective is evident, and there is hope for those who are suffering.” HBOT is a medical treatment in which 100% oxygen is administered at an increased environmental pressure. Aviv’s unique HBOT protocol, the hyperoxic-hypoxic paradox, fluctuates oxygen levels during treatment and is being used to repair and regenerate damaged brain tissue in several types of brain injuries including traumatic brain injury, stroke, PTSD, long COVID and age-related cognitive decline among others. Previous studies from the research team at the Sagol Center for Hyperbaric Medicine and Research have demonstrated the efficacy of HBOT as a treatment for persistent post-concussion syndrome (PPCS), suggesting that HBOT improves cognitive function, behavioral function and quality of life in both adult and pediatric patients suffering from PPCS at the chronic stage, even years after their injury. Aviv Clinics offers an advanced treatment program with a multidisciplinary team of medical experts providing patients with top-line care and the opportunity to improve their quality of life. The Aviv Medical Program includes an in-depth assessment of the patient’s physical and neurological condition to assess the fit for the program. For patients that meet the criteria, the Aviv team will then prepare a comprehensive treatment schedule combining HBOT with personal cognitive training, and physical and dietary coaching, for a holistic approach to patient health. The HBOT sessions are conducted in state-of-the-art multiplace chambers that are comfortable, safe and allow for medical staff to accompany patients during the treatment. The elevated pressure in the HBOT chamber creates an optimal oxygenation condition, ultimately encouraging damaged brain and body tissues to regenerate and heal. The full study is available here. For more on Aviv Clinics, visit aviv-clinics.com Aviv Clinics is the leader in the research and treatment of age-related cognitive and functional decline and novel applications of hyperbaric oxygen therapy (HBOT) to maximize human performance. Based on an exclusive partnership with the world’s largest hyperbaric medicine and research facility, the Sagol Center at Shamir Medical Center in Israel, Aviv is introducing a global network of clinics delivering the most effective evidence-based treatment of the aging related decline – the Aviv Medical Program. The three-month regimen, designed to improve the aging-related decline in healthy adults, was developed based on over a decade of research and thousands of patients treated worldwide under the scientific leadership of Shai Efrati, M.D., chair of Aviv Scientific’s Medical Advisory Board and director of the Sagol Center. Media Contact: Ellie Holt [email protected] ########## The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can help heal the symptoms and effects of acute concussion/TBI/PTSD by helping heal brain wounds. Heal Brains. Stop Suicides. Restore Lives. TreatNOW Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made. Read the full article
#acutemoderate-severeTBI#AvivClinics#brainhealth#braininjured#braininjury#brainwound#chronictraumaticbraininjury#concussion#concussionprotocol#ConcussionSymptoms#concussiontreatment#HBOT#HBOTTreatment#HealingwithHyperbarics#hyperbaric#HyperbaricOxygentherapy#hyperoxic-hypoxicparadox#mildtraumaticbraininjury#stroke#TBI#TBItreatment#traumaticbraininjury
2 notes
·
View notes
Text
Understanding Hyperbaric Chamber Costs: A Complete Guide

Explore the factors that determine hyperbaric chamber cost with Life Force MedBed. Learn about pricing for purchase or rental, whether for personal use or wellness centers. Discover how these advanced chambers can enhance healing and well-being while making an informed investment tailored to your needs.
Visit Now https://medium.com/@lifeforcemedbed/understanding-the-cost-of-hyperbaric-chambers-a-comprehensive-guide-b09e77eec3c2
0 notes