#heart and vascular Institute
Text
Best Heart Hospital in Mohali-ACEHearinstitute
These days, heart diseases are a pretty regular occurrence. Heart illness must be treated with great care and in a holistic manner to be effectively treated. Make an appointment with the best heart hospital in Mohali if you suffer any of the following symptoms. The greatest care is available at ACE Heart & Vascular Institute.

#ACE Heart & Vascular Institute#Heart Hospital#Cardiology#Lithotripsy Treatment#interventional cardiology#pediatric cardiology
0 notes
Text
COVID-19's long-term effects on the body: an incomplete list
COVID’s effect on the immune system, specifically on lymphocytes:
NYT article from 2020 (Studies cited: https://www.biorxiv.org/content/10.1101/2020.05.18.101717v1, https://www.biorxiv.org/content/10.1101/2020.05.20.106401v1, https://www.unboundmedicine.com/medline/citation/32405080/Decreased_T_cell_populations_contribute_to_the_increased_severity_of_COVID_19_, https://www.medrxiv.org/content/10.1101/2020.06.08.20125112v1)
https://www.biorxiv.org/content/10.1101/2022.01.10.475725v1
https://www.science.org/doi/10.1126/science.abc8511 (Published in Science)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9057012/
https://www.forbes.com/sites/williamhaseltine/2022/04/14/sars-cov-2-actively-infects-and-kills-lymphoid-cells/
https://www.cleveland.com/news/2022/10/in-cleveland-and-beyond-researchers-begin-to-unravel-the-mystery-of-long-covid-19.html
SARS-CoV-2 infection weakens immune-cell response to vaccination: NIH-funded study suggests need to boost CD8+ T cell response after infection
https://www.merckmanuals.com/professional/hematology-and-oncology/leukopenias/lymphocytopenia
https://thetyee.ca/Analysis/2022/11/07/COVID-Reinfections-And-Immunity/
Dendritic cell deficiencies persist seven months after SARS-CoV-2 infection
https://www.frontiersin.org/articles/10.3389/fimmu.2022.1034159/full
https://www.n-tv.de/politik/Lauterbach-warnt-vor-unheilbarer-Immunschwaeche-durch-Corona-article23860527.html (German Minister of Health)
Anecdotal evidence of COVID’s effects on white blood cells:
https://twitter.com/DrJohnHhess/status/1661837956875956224
https://x.com/TristanVeness/status/1661565201345564673
https://twitter.com/TristanVeness/status/1689996298408312832
Much more if you speak to Long Covid patients directly!
Related information of interest:
China approves Genuine Biotech's HIV drug for COVID patients
COVID as a “mass disabling event” and impact on the economy:
https://www.ctvnews.ca/health/report-says-long-covid-could-impact-economy-and-be-mass-disabling-event-in-canada-1.6306608
https://x.com/inkblue01/status/1742183209809453456?s=20
COVID’s impact on the heart:
https://www.dailystar.co.uk/news/world-news/deadly-virus-could-lead-heart-31751263 (Research from: Japan's Riken research institute)
https://www.brisbanetimes.com.au/national/queensland/unlike-flu-covid-19-attacks-dna-in-the-heart-new-research-20220929-p5bm10.html
https://www.mdpi.com/2077-0383/12/1/186
https://medicalxpress.com/news/2023-04-mild-covid-effects-cardiovascular-health.html
https://publichealth.jhu.edu/2022/covid-and-the-heart-it-spares-no-one
https://www.bhf.org.uk/informationsupport/heart-matters-magazine/news/coronavirus-and-your-health/is-coronavirus-a-disease-of-the-blood-vessels (British Heart Foundation)
COVID’s effect on the brain and cognitive function:
https://www.openaccessgovernment.org/article/brain-infection-by-sars-cov-2-lifelong-consequences/171391/
https://www.cidrap.umn.edu/covid-19/study-shows-covid-leaves-brain-injury-markers-blood
https://www.theguardian.com/world/2020/jul/08/warning-of-serious-brain-disorders-in-people-with-mild-covid-symptoms
Cognitive post-acute sequelae of SARS-CoV-2 (PASC) can occur after mild COVID-19
Neurologic Effects of SARS-CoV-2 Transmitted among Dogs
https://journals.lww.com/nsan/fulltext/2022/39030/neurological_manifestations_and_mortality_in.4.aspx
https://www.salon.com/2023/06/17/new-evidence-suggests-alters-the-brain--but-the-extent-of-changes-is-unclear/
https://www.scientificamerican.com/article/covid-virus-may-tunnel-through-nanotubes-from-nose-to-brain/
https://neurosciencenews.com/post-covid-brain-21904/
https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(22)00260-7/fulltext
https://medicalxpress.com/news/2022-08-covid-infection-crucial-brain-regions.html
https://news.ecu.edu/2022/08/04/covid-parkinsons-link/
Covid as a vascular/blood vessel disease:
https://www.salon.com/2020/06/01/coronavirus-is-a-blood-vessel-disease-study-says-and-its-mysteries-finally-make-sense/
https://www.salon.com/2023/12/27/brain-damage-caused-by-19-may-not-show-up-on-routine-tests-study-finds/
https://www.nih.gov/news-events/news-releases/sars-cov-2-infects-coronary-arteries-increases-plaque-inflammation
https://www.mdpi.com/2077-0383/12/6/2123
https://www.sciencedaily.com/releases/2021/10/211004104134.htm (microclots)
Long Covid:
Post-COVID-19 Condition in Canada: What we know, what we don’t know, and a framework for action
https://www.ctvnews.ca/health/coronavirus/more-than-two-years-of-long-covid-research-hasn-t-yielded-many-answers-scientific-review-1.6235227
https://www.cbc.ca/news/canada/london/cause-of-long-covid-symptoms-revealed-by-lung-imaging-research-at-western-university-1.6504318
https://www.cbc.ca/news/canada/montreal/long-covid-study-montreal-1.6521131
https://news.yale.edu/2023/12/19/study-helps-explain-post-covid-exercise-intolerance
Other:
- Viruses and mutation: https://typingmonkeys.substack.com/p/monkeys-on-typewriters
Measures taken by the rich and world leaders
Heightened risk of diabetes
https://jamanetwork.com/journals/jama/fullarticle/2805461
https://www.nature.com/articles/d41586-022-00912-y
Liver damage:
https://timesofindia.indiatimes.com/city/mumbai/46-of-covid-patients-have-liver-damage-study/articleshow/97809200.cms?from=mdr
tl;dr: covid is a vascular disease, not a respiratory illness. it can affect your blood and every organ in your body. every time you're reinfected, your chances of getting long covid increase.
avoid being infected. reduce the amount of viral load you're exposed to.
the gap between what the scientific community knows and ordinary people know is massive. collective action is needed.
#putting this somewhere at least as reference for... somebody hopefully#covid#disability#y'all. it is bleak out there but some very good people are doing their best to help#we need as many people aware and helping as possible
464 notes
·
View notes
Text
Beyond breathing: How COVID-19 affects your heart, brain and other organs - Published Jan 16, 2024
It's easy to be complacent about COVID-19. Most people experience only mild issues – fever and coughing, maybe congestion and shortness of breath.
But the coronavirus is capable of causing much more than a simple respiratory illness, affecting organs throughout the body, experts say.
"We see people have symptoms from almost head to toe in terms of how they feel, how they function and what they can do," said Dr. Adrian Hernandez, a cardiologist who is director of the Duke Clinical Research Institute in Durham, North Carolina.
The new year started with an increase in COVID-19 hospitalizations in the U.S., prompting Hernandez and other experts to advise caution, especially for those at high risk.
While the short-term effects of COVID-19 can be flu-like, even mild cases can lead to long COVID – a constellation of problems that can persist for weeks or months. More than 200 symptoms have been linked to long COVID, said Hernandez, who has overseen many COVID-19 studies.
Because COVID-19 typically affects breathing and can lead to problems such as pneumonia, many people may think it's primarily a lung disease. It's not that simple, said Dr. Nisha Viswanathan, director of the long COVID program at the David Geffen School of Medicine at the University of California, Los Angeles.
"I would argue that COVID-19 is not a disease of the lungs at all," she said. "It seems most likely that it is what we call a vascular and neurologic infection, affecting both nerve endings and our cardiovascular system."
It's no surprise that experts say SARS-CoV-2 – the name of the virus that causes COVID-19 – is complex, with many of its pathways just beginning to be understood. But some things are becoming clear. One of the best reviews of long COVID symptoms, Viswanathan said, appeared last January in Nature Reviews Microbiology. It detailed the disease's effects throughout the body, including the pancreas, blood vessels and reproductive system.
"SARS-CoV-2 is excellent at triggering your immune system to go from zero to 100," said Dr. Lindsay McAlpine, a neurologist who is director of the Yale NeuroCovid Clinic in New Haven, Connecticut. That revving of the immune response leads to both a "wide swath of inflammation" and excessive blood clotting, she said.
"Perhaps the viral replication is going on in the lungs and nasopharynx (the area at the top of the throat that connects the nose to the respiratory system). But the inflammation that the virus triggers is systemic," McAlpine said.
Here are some parts of the body significantly affected by COVID-19...
Full text, Spanish translation, and more avaliable at our archive
#coronavirus#wear a respirator#sars cov 2#mask up#public health#wear a mask#pandemic#covid#covid 19#still coviding#covid conscious#covid cautious#covid is airborne#covid isn't over#the pandemic isn't over#covid pandemic#covidー19#long covid
23 notes
·
View notes
Note
Since the Doctor isn't Gallifreyan but still has two hearts, having two hearts is not just a Gallifreyan trait then?
Do other species have two hearts?
The Institute couldn't possibly speculate on the origins of individual Time Lords, but a binary cardiovascular system isn't exclusive to Gallifreyans—many species have two hearts.
💕 Species with Dual Hearts
Various Species in the Mutter’s Spiral: Within the Milky Way, some humanoid, monopod, and drone species naturally have binary vascular systems.
Dulcians
Apalapucians
Skale Inhabitants
The Kulan
The Kirithons: Genetically engineered to have two hearts.
The Meep
Word Lords
Earth Leeches: Although not technically hearts as humans define them, leeches have a segmented structure with regions that function similarly to two hearts.
🏫 So ...
A binary vascular system isn't exclusive to Galifreyans. It's quite rare to see a specifically two-hearted species on Earth, but out in the wide Universe, it's not so uncommon and by no means defines a Gallifreyan.
Although it is super interesting that leeches and the Yssgaroth/Vampires are both blood-suckers, and some posit the Time Lords gained their abilities through the 'Yssgaroth taint', isn't that fun?
Related:
Factoid: Could a Gallifreyan survive if they lost a heart?
What would a Human/Gallifreyan child be like?: Developmental expectations of a hybrid.
Could a Word Lord and a Time Lord loom a child together?: If Word Lords and Time Lords could reproduce, and what the result would be.
Hope that helped! 😃
More content ...
→📫Got a question? | 📚Complete list of Q+A and factoids
→😆Jokes |🩻Biology |🗨️Language |🕰️Throwbacks |🤓Facts
→🫀Gallifreyan Anatomy and Physiology Guide (pending)
→⚕️Gallifreyan Emergency Medicine Guides
→📝Source list (WIP)
→📜Masterpost
If you're finding your happy place in this part of the internet, feel free to buy a coffee to help keep our exhausted human conscious. She works full-time in medicine and is so very tired 😴
#doctor who#gil#gallifrey institute for learning#dr who#dw eu#gallifrey#gil biology#gallifreyans#gallifreyan biology#whoniverse#time lord biology#ask answered
16 notes
·
View notes
Text

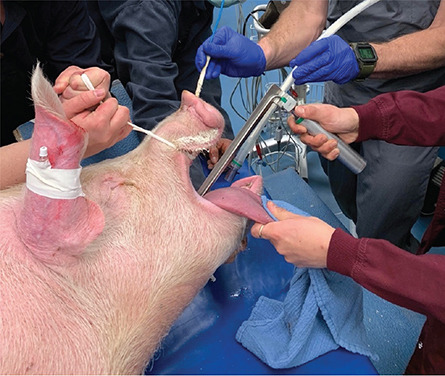
Groundbreaking Pig Heart Transplant is Performed for the Second Time
For the second time ever, a pig heart has been transplanted into a living human recipient, the University of Maryland Medical Center announced on Friday.
The groundbreaking surgery was done on September 20 at UMMC by the same transplant team that preformed the first such experimental surgery in 2022.
In a news release, the hospital said the recipient, 58-year-old Lawrence Faucette, “is currently breathing on his own, and his heart is functioning well without any assistance from supportive devices.”
Faucette had end-stage heart disease. He had pre-existing peripheral vascular disease and complications with internal bleeding making him ineligible for a traditional heart transplant, the hospital said in the release. He was admitted to UMMC on September 14 after experiencing symptoms of heart failure.
“My only real hope left is to go with the pig heart, the xenotransplant,” Faucette told the hospital in an internal interview several days before the surgery.
The experimental xenotransplant surgery was green lit under the US Food and Drug Administration’s “compassionate use” program. According to the FDA, the program is “a potential pathway for a patient with a serious or immediately life-threatening disease or condition to gain access to an investigational medical product (drug, biologic, or medical device) for treatment outside of clinical trials when no comparable or satisfactory alternative therapy options are available.”


The pig heart used came from a genetically modified pig from Revivcor, a subsidiary the United Therapeutics Corporation. The pig had 10 genes edited, including three genes “knocked out” or inactivated to eliminate the alpha gal sugar in the pig’s blood cells, which can trigger a severe reaction in the human immune system, causing organ rejection. An additional pig gene was modified to control for the growth of the pig’s heart while 6 human genes were added into the pig’s genome to increase acceptance by the immune system. The FDA first approved the gene edited pigs in 2020 for potential therapeutic use and consumption.
Doctors are also treating Faucette with an experimental antibody treatment to further suppress the immune system and prevent rejection. He will be closely monitored for any signs of rejection or any development of pig related viruses. The donor pig was also closely screened for any signs of virus or pathogens.

“We are once again offering a dying patient a shot at a longer life, and we are incredibly grateful to Mr. Faucette for his bravery and willingness to help advance our knowledge of this field,” said Dr. Bartley Griffith, in the release. Griffith is the surgeon who performed the transplant and is a professor of surgery at the University of Maryland School of Medicine.
The hospital said Faucette fully consented to the experimental treatment and was informed of all the risks. In addition, he underwent a full psychiatric evaluation and discussed his case with a medical ethicist.
According to the hospital’s news release, Faucette is a married father of two from Frederick, Maryland and a 20-year Navy veteran who had most recently worked as a lab technician at the National Institutes of Health before retiring.
“We have no expectations other than hoping for more time together,” said his wife Ann Faucette, in the release. “That could be as simple as sitting on the front porch and having coffee together.” There are currently no clinical trials that utilize pig organs for transplants in living human beings. The University of Maryland performed the first such experimental surgery on 57-year-old David Bennett in January 2022. Bennett died two months following the surgery.
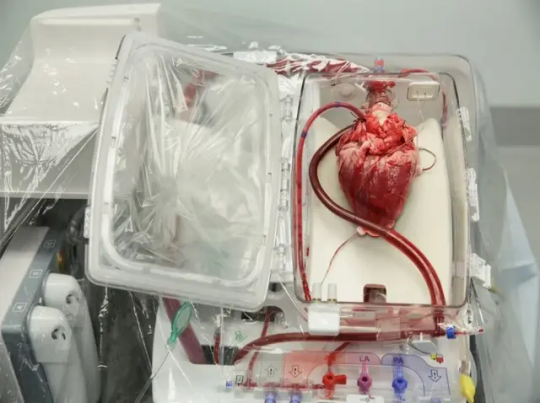
While there were no signs of rejection in the initial weeks following the transplant, an autopsy concluded that Bennett ultimately died of heart failure from “a complex array of factors,” including Bennett’s condition prior to the surgery. Bennet had already been hospitalized and kept on a heart lung bypass machine for 6 weeks prior to the transplant. However, a case study by the doctors published in the Lancet also noted there was evidence of pig virus that had not been identified previously.
According to the federal government, there are more than 113,000 people on the organ transplant list, including 3,354 people in need of a heart. The group Donate Life America says that 17 people die each day waiting for a donor organ.
By Nadia Kounang,


#Groundbreaking Pig Heart Transplant is Performed for the Second Time#The University of Maryland Medical Center#Lawrence Faucette#heart#pig heart#heart transplant#organ transplant#xenotransplant#animals#strange#stranger things#science#science news
20 notes
·
View notes
Text
New method enables fast, accurate estimates of cardiovascular state to inform blood pressure management
New Post has been published on https://thedigitalinsider.com/new-method-enables-fast-accurate-estimates-of-cardiovascular-state-to-inform-blood-pressure-management/
New method enables fast, accurate estimates of cardiovascular state to inform blood pressure management


If patients receiving intensive care or undergoing major surgery develop excessively high or low blood pressures, they could suffer severe organ dysfunction. It’s not enough for their care team to know that pressure is abnormal. To choose the correct drug to treat the problem, doctors must know why blood pressure has changed. A new MIT study presents the mathematical framework needed to derive that crucial information accurately and in real time.
The mathematical approach, described in a recent open-access study in IEEE Transactions on Biomedical Engineering, produces proportional estimates of the two critical factors underlying blood pressure changes: the heart’s rate of blood output (cardiac output) and the arterial system’s resistance to that blood flow (systemic vascular resistance). By applying the new method to previously collected data from animal models, the researchers show that their estimates, derived from minimally invasive measures of peripheral arterial blood pressure, accurately matched estimates using additional information from an invasive flow probe placed on the aorta. Moreover, the estimates accurately tracked the changes induced in the animals by the various drugs physicians use to correct aberrant blood pressure.
“Estimates of resistance and cardiac output from our approach provide information that can readily be used to guide hemodynamic management decisions in real time,” the study authors wrote.
With further testing leading to regulatory approval, the authors say, the method would be applicable during heart surgeries, liver transplants, intensive care unit treatment, and many other procedures affecting cardiovascular function or blood volume.
“Any patient who is having cardiac surgery could need this,” says study senior author Emery N. Brown, the Edward Hood Taplin Professor of Medical Engineering and Computational Neuroscience in The Picower Institute for Learning and Memory, the Institute for Medical Engineering and Science, and the Department of Brain and Cognitive Sciences at MIT. Brown is also an anesthesiologist at Massachusetts General Hospital and a professor of anesthesiology at Harvard Medical School. “So might any patient undergoing a more normal surgery but who might have a compromised cardiovascular system, such as ischemic heart disease. You can’t have the blood pressure being all over the place.”
The study’s lead author is electrical engineering and computer science (EECS) graduate student Taylor Baum, who is co-supervised by Brown and Munther Dahleh, the William A. Coolidge Professor in EECS.
Algorithmic advance
The idea that cardiac output and systemic resistance are the two key components of blood pressure comes from the two-element Windkessel model. The new study is not the first to use the model to estimate these components from blood pressure measurements, but previous attempts ran into a trade-off between quick estimate updates and the accuracy of estimates; methods would either provide more erroneous estimates at every beat or more reliable estimates that are updated at minute time scales. Led by Baum, the MIT team overcame the trade-off with a new approach of applying statistical and signal processing techniques such as “state-space” modeling.
“Our estimates, updated at every beat, are not just informed by the current beat; but they incorporate where things were in previous beats as well,” Baum says. “It’s that combination of past history and current observations that produces a more reliable estimate while still at a beat-by-beat time scale.”
Notably, the resulting estimates of cardiac output and systemic resistance are “proportional,” meaning that they are each inextricably linked in the math with another co-factor, rather than estimated on their own. But application of the new method to data collected in an older study from six animals showed that the proportional estimates from recordings using minimally invasive catheters provide comparable information for cardiovascular system management.
One key finding was that the proportional estimates made based on arterial blood pressure readings from catheters inserted in various locations away from the heart (e.g., the leg or the arm) mirrored estimates derived from more invasive catheters placed within the aorta. The significance of the finding is that a system using the new estimation method could in some cases rely on a minimally invasive catheter in various peripheral arteries, thereby avoiding the need for a riskier placement of a central artery catheter or a pulmonary artery catheter directly in the heart, the clinical gold standard for cardiovascular state estimation.
Another key finding was that when the animals received each of five drugs that doctors use to regulate either systemic vascular resistance or cardiac output, the proportional estimates tracked the resulting changes properly. The finding therefore suggests that the proportional estimates of each factor are accurately reflecting their physiological changes.
Toward the clinic
With these encouraging results, Baum and Brown say, the current method can be readily implemented in clinical settings to inform perioperative care teams about underlying causes of critical blood pressure changes. They are actively pursuing regulatory approval of use of this method in a clinical device.
Additionally, the researchers are pursuing more animal studies to validate an advanced blood pressure management approach that uses this method. They have developed a closed-loop system, informed by this estimation framework, to precisely regulate blood pressure in an animal model. Upon completion of the animal studies, they will apply for regulatory clearance to test the system in humans.
In addition to Baum, Dahleh and Brown, the paper’s other authors are Elie Adam, Christian Guay, Gabriel Schamberg, Mohammadreza Kazemi, and Thomas Heldt.
The National Science Foundation, the National Institutes of Health, a Mathworks Fellowship, The Picower Institute for Learning and Memory, and The JPB Foundation supported the study.
#Anesthesia#Animals#approach#arm#arteries#author#beats#Biomedical engineering#blood#blood pressure#Brain#Brain and cognitive sciences#computer#Computer Science#data#Disease#drug#drugs#Electrical Engineering&Computer Science (eecs)#engineering#experimental#factor#Foundation#framework#gold#harvard#Health#Health care#Health sciences and technology#heart
4 notes
·
View notes
Text
More on Ohio corruption. 👇

Then this happens 👇

Puppet pushes experimental inoculations 👇

Say What? 👇

The deeper I go down this Rabbit Hole 🐇 the uglier it gets. I'm now discovering that Ohio is involved BIG time in organ harvesting. 👇

One man's story👇
I lived in Cincinnati for 42 years. We had a business right next to Union Terminal. In 1993 I was headed into work on my motorcycle, early morning. Some kid ran a stop sign right there at the Terminal underpass and broadsided me. If not for my helmet and full leathers I wouldn’t be alive. It was out-of-body for me. I watched the cops let the kid drive off. Then one cop jerked my helmet off and threw it way down the underpass. They tried to say that I didn’t have a helmet on. The ambulance was there very quickly. My wife and family could not find me for more than 12 hours. I was taken to University Hospital. It just happened that we had a friend that worked there and she heard that someone from near Union Terminal had been brought in. This was much later in the day. She said they were calling me a Donor Cyclist. She finally called my Brother/Business Partner to see if I was missing. That’s the only way anyone found me. I’m pretty sure I was supposed to be parted out. The kid that hit me and the car were never to be seen again. Needless to say, that experience has changed my life.

Ohio Treasurer Josh Mandel made this purchase! The largest single government purchase of Israel Bonds ever in the US!
Who is this guy? 👇

Tri Health...a Cincinnati health care system of hospitals, inc 1 near UCMC, Good Samaritan, recently joined with Cleveland Clinics Heart, Vascular and Thorastic Institute. The only one associated in the region. 🤔
The CEO of Trihealth is very woke!
Btw....geographically Cincinnati is most southern city...borders KY.
Cleveland is most Northern city.

We really have to question what's going on 🤔
The news is fake... The war is real...
We Are The News Now!!!
#pay attention#educate yourself#educate yourselves#reeducate yourself#knowledge is power#reeducate yourselves#think for yourself#think for yourselves#think about it#do your homework#do your research#do your own research#question everything#ask yourself questions#ask yourself#ohio#truthful news#political news#real news#news#we are the news#digital soldier
28 notes
·
View notes
Photo







Interesting and beautiful photo-collages of Mohd Azlan Mam Mohd Latib (or AzlanMAM08)
http://www.azlanmam08.com/
"Born in Balik Pulau, Penang, Malaysia in 1974. Studied at College of Medical Imaging, graduated in Medical Imaging, majoring in Intervention Radiological and Cardiac procedures. Azlan had worked in Radiology Department, University Malaya Medical Centre , National Heart Institute , HealthScan Malaysia and currently working as CTA Clinician/Deputy Manager of CT Scan Unit in Cardiac Vascular Sentral Kuala Lumpur (CVSKL ), a private diagnostic and medical centre , specializing in Multi Slice CT Coronary Angiogram and Coronary Imaging .
In addition he had a formal education in Fundamentals , Basics and Principles in Photography during his undergraduate study at College of Medical Imaging. Now he is interested in Risograph printmaking on self-made caffeinated paper , Medium Format / Analogue photography / Experimental shots and Alternative hand tinting , collage and printmaking."
10 notes
·
View notes
Text
The In Vivo Imaging Market is projected to grow from USD 2915 million in 2024 to an estimated USD 3880.233 million by 2032, with a compound annual growth rate (CAGR) of 3.64% from 2024 to 2032.The in vivo imaging market is a dynamic and rapidly expanding sector in the healthcare industry, playing a pivotal role in preclinical and clinical research. In vivo imaging refers to the visualization of biological processes and structures within a living organism. This technology is instrumental in understanding disease progression, evaluating therapeutic efficacy, and accelerating drug development. The demand for non-invasive, high-resolution, and real-time imaging solutions is propelling the growth of this market across the globe. This article explores the key drivers, technologies, and trends shaping the in vivo imaging market.
Browse the full report at https://www.credenceresearch.com/report/in-vivo-imaging-market
Key Market Drivers
1. Growing Preclinical Research and Drug Development:
In vivo imaging techniques have become a cornerstone in preclinical research, particularly in the pharmaceutical and biotechnology sectors. As the demand for new drug development and personalized medicine increases, researchers rely on imaging technologies to visualize the biological effects of therapeutic candidates in real-time. This accelerates the drug development pipeline by providing critical data on safety, efficacy, and pharmacokinetics.
2. Advances in Molecular Imaging:
Molecular imaging technologies, such as positron emission tomography (PET), single-photon emission computed tomography (SPECT), and optical imaging, are increasingly being used to study biological pathways at the molecular and cellular levels. These advancements enable researchers to detect diseases earlier, monitor treatment responses, and even predict outcomes in preclinical models. The precision offered by these tools has further driven their adoption in research institutions and pharmaceutical companies.
3. Rising Prevalence of Chronic Diseases:
The increasing global incidence of chronic diseases such as cancer, cardiovascular diseases, and neurological disorders has underscored the need for effective diagnostic and therapeutic monitoring tools. In vivo imaging systems are critical in detecting tumors, assessing cardiovascular health, and tracking neurological changes in conditions like Alzheimer's and Parkinson's disease. This surge in chronic diseases directly boosts the demand for advanced imaging solutions.
4. Technological Innovations:
Significant strides in imaging technologies have been made in recent years. Innovations such as hybrid imaging systems (e.g., PET-CT and PET-MRI), which combine different imaging modalities, have enhanced image resolution, accuracy, and functional data acquisition. These technologies offer a more comprehensive understanding of biological processes, helping clinicians make better-informed decisions.
5. Increased Government and Private Funding:
Government and private sector investments in healthcare research and innovation are providing significant financial support to the in vivo imaging market. Research initiatives focusing on cancer, cardiovascular diseases, and other critical health concerns are leading to increased utilization of advanced imaging technologies.
Types of In Vivo Imaging Technologies
1. Magnetic Resonance Imaging (MRI):
MRI is one of the most commonly used in vivo imaging techniques due to its ability to generate high-resolution images of soft tissues. It is particularly useful in neurology and cardiology research for imaging the brain, heart, and vascular structures.
2. Positron Emission Tomography (PET):
PET imaging is crucial for studying metabolic processes and is widely used in cancer research and neurology. It allows for the real-time assessment of cellular and molecular activity, providing valuable data on tumor metabolism and brain function.
3. Optical Imaging:
Optical imaging techniques such as bioluminescence and fluorescence imaging are extensively used in preclinical studies. These non-invasive methods are ideal for monitoring gene expression, protein-protein interactions, and tracking disease progression in animal models.
4. Computed Tomography (CT):
CT scanning provides detailed cross-sectional images of bones, organs, and tissues, making it an important tool for studying skeletal structures, lung diseases, and cardiovascular conditions in animal models.
5. Ultrasound Imaging:
Ultrasound is widely used in cardiovascular and obstetric research for real-time imaging of blood flow, heart function, and fetal development. It is favored for its non-invasive nature and cost-effectiveness.
Challenges Facing the In Vivo Imaging Market
Despite its rapid growth, the in vivo imaging market faces several challenges. High costs associated with advanced imaging systems, the need for specialized training to operate complex technologies, and ethical concerns regarding animal research are some of the major hurdles. Additionally, integrating these imaging technologies into clinical practice remains a significant challenge, particularly in low-resource settings where access to advanced equipment is limited.
Market Trends and Future Outlook
The future of the in vivo imaging market is promising, with several key trends emerging:
1. Artificial Intelligence (AI) Integration:
AI-powered imaging systems are becoming increasingly popular for automating image analysis and improving diagnostic accuracy. Machine learning algorithms are enabling researchers to extract more information from imaging data, leading to better predictive models and personalized treatment plans.
2. Expansion of Optical and Hybrid Imaging:
The integration of optical imaging with other modalities like MRI and PET is expected to continue, offering improved sensitivity and resolution for preclinical research. This trend is likely to expand the applications of imaging technologies beyond oncology and neurology into fields like immunology and infectious diseases.
3. Increased Adoption of Imaging in Drug Development:
As pharmaceutical companies continue to adopt imaging for drug discovery and development, the market is poised to see increased demand. Imaging will play an increasingly important role in evaluating drug safety and efficacy, reducing the time and cost associated with clinical trials.
Key Player Analysis:
Aspect Imaging Ltd. (Israel)
Biospace Lab (France)
Bruker (U.S.)
CMR Naviscan (U.S.)
FUJIFILM Holdings America Corporation (Canada)
General Electric (U.S.)
Guerbet (France)
Hitachi, Ltd. (Japan)
Koninklijke Philips N.V (Netherlands)
LI-COR, Inc. (U.S.)
Mediso Ltd. (U.S.)
MILabs B.V. (Netherlands)
Miltenyi Biotec (Germany)
MR Solutions (U.K.)
PerkinElmer Inc. (U.S.)
SCANCO Medical AG (Switzerland)
Siemens (Germany)
Takara Bio Inc. (Japan)
Trifoil Imaging (U.S.)
Segmentation:
By Modality:
Optical imaging,
Nuclear imaging,
Magnetic resonance imaging (MRI),
Ultrasound,
Others
By Reagents:
Bioluminescent and fluorescent labels,
Radioisotopes,
Nanoparticles,
Others
By Technique:
Radiography,
Optical imaging,
Magnetic resonance imaging,
Others
By End User:
Hospitals and clinics,
Research institutions,
Pharmaceutical and biotechnology companies,
Others
By Region
North America
The U.S
Canada
Mexico
Europe
Germany
France
The U.K.
Italy
Spain
Rest of Europe
Asia Pacific
China
Japan
India
South Korea
South-east Asia
Rest of Asia Pacific
Latin America
Brazil
Argentina
Rest of Latin America
Middle East & Africa
GCC Countries
South Africa
Rest of Middle East and Africa
Browse the full report at https://www.credenceresearch.com/report/in-vivo-imaging-market
About Us:
Credence Research is committed to employee well-being and productivity. Following the COVID-19 pandemic, we have implemented a permanent work-from-home policy for all employees.
Contact:
Credence Research
Please contact us at +91 6232 49 3207
Email: [email protected]
Website: www.credenceresearch.com
0 notes
Text
What are the top hospitals for cardiac surgery in chennai

Here is a list of some of the best hospitals for cardiac surgery in Chennai, which is among the leading medical hubs within the country:
Apollo Hospitals
Known for: Advanced cardiac care includes heart transplantation, bypass surgery, and minimally invasive procedures.
Specialties: CABG, coronary artery bypass grafting; valve repair and replacement; treatment of arrhythmias are the few examples.
MIOT International Hospital
Known for: It provides comprehensive cardiac care, along with state-of-the-art facilities and accomplished surgeons.
Specialties: Heart transplantation, cardiopulmonary bypass grafting, repair techniques of the valves and children cardiac surgery in India.
Global Hospitals
Known for:Advanced cardiac care, including robotic-assisted surgery, along with other advanced interventional cardiology procedures.
Specialties: CABG, valve repair, and replacement; arrhythmia treatment.
Sri Ramachandra Medical Centre
Known for: It offers a comprehensive range of cardiac care with all available surgical and non-surgical treatments.
Specialties: Heart Heart transplant, bypass surgery, cardiac valve repair, and medical treatment of an arrhythmia.
Related Post: (Best Cardiologist in Chennai)
Fortis Malar Hospital
Known for: Advanced cardiac care, with the focus on patient-centered, excellent outcomes.
Specialties: CABG, valve repair, and replacement; treatment of arrhythmias.
Kauvery Hospital
Known For: Comprehensive cardiac care by a wide team of cardiologists and cardiac surgeons.
Specialties include heart transplantation, cardiac bypass grafting, valve repair, and arrhythmia treatment.
Prashanth Superspeciality Hospital
Known for: Advanced cardiac care, with the emphasis on minimally invasive techniques, has safety of the patient in the foreground.
Specialties: CABG, valve repair and replacement, arrhythmia treatment.
Gleneagles Global Health City
Known for: Comprehensive cardiac care, offering all available surgical and non-surgical treatments.
Specialties include heart transplant, cardiac bypass surgery, valve repair, and arrhythmia treatment.
Chennai Vascular Clinic & Teertam Clinic
Known for: Specialized vascular care, including treatment of peripheral arterial disease and aortic aneurysms.
Specialized care in cardiology, with emphasis on prevention and early diagnosis.
Medway Heart Institute
Known for: Specialized cardiac care, with a focus on prevention and early diagnosis.
Specialties: Cardiac catheterization, angioplasty, and arrhythmia treatment.
Specialties include cardiac catheterization, angioplasty, and arrhythmia therapy. Specialties: Vascular surgery, interventional cardiology.
#Paediatric Cardiac Surgery In India#cardiac surgery Chennai#top hospitals for cardiac surgery Chennai#best cardiac surgeons Chennai#heart transplant Chennai#bypass surgery Chennai#valve replacement Chennai#arrhythmia treatment Chennai
0 notes
Text
Multimodal Imaging Market: Advancing Diagnostic Precision
The Multimodal Imaging market is revolutionizing medical diagnostics by combining multiple imaging techniques to provide comprehensive insights into patient conditions. This integrated approach enhances diagnostic accuracy and treatment planning, driving significant growth in the imaging industry. This article delves into the latest trends, market segmentation, key growth drivers, and leading companies in the multimodal imaging sector.
Market Overview
According to SkyQuest’s Multimodal Imaging Market report, the market is valued at USD 2.26 billion in 2023 and is expected to grow at a CAGR of 4.3% during the forecast period. The rise in chronic diseases, advancements in imaging technology, and increasing demand for precise diagnostics are propelling market expansion.
Request Your Free Sample: - https://www.skyquestt.com/sample-request/multimodal-imaging-market
Market Segmentation
By Modality:
PET/MRI: Combines Positron Emission Tomography (PET) with Magnetic Resonance Imaging (MRI) for detailed anatomical and functional information.
PET/CT: Integrates PET with Computed Tomography (CT) to offer comprehensive imaging for oncology and cardiology.
SPECT/CT: Merges Single Photon Emission Computed Tomography (SPECT) with CT for enhanced diagnostic capabilities in nuclear medicine.
Others: Includes hybrid modalities like PET/MR and PET/CT in various combinations for specific diagnostic needs.
By Application:
Oncology: Utilizes multimodal imaging for accurate tumor detection, staging, and treatment planning.
Cardiology: Enhances the assessment of cardiac conditions and evaluation of heart diseases.
Neurology: Provides detailed brain imaging for diagnosing neurological disorders and monitoring disease progression.
Orthopedics: Assists in the diagnosis and treatment of musculoskeletal conditions.
Others: Includes applications in trauma care, vascular imaging, and preoperative planning.
By End-User:
Hospitals: Major users of multimodal imaging systems for comprehensive diagnostic and treatment services.
Diagnostic Imaging Centers: Specialized facilities offering advanced imaging services to patients.
Research Institutions: Engage in the development and validation of new imaging technologies and applications.
Others: Includes outpatient clinics and specialized medical centers.
Read More at: - https://www.skyquestt.com/report/multimodal-imaging-market
Key Growth Drivers
Technological Advancements: Innovations in imaging technology, such as hybrid imaging systems and software, are driving market growth.
Rising Prevalence of Chronic Diseases: Increased incidence of cancer, cardiovascular diseases, and neurological disorders fuels the demand for advanced diagnostic solutions.
Growing Focus on Precision Medicine: The shift towards personalized healthcare requires detailed imaging for accurate diagnosis and tailored treatment plans.
Increase in Healthcare Spending: Enhanced investment in medical infrastructure and advanced diagnostic tools supports market expansion.
Leading Companies in the Market
SkyQuest’s report highlights key players in the Multimodal Imaging market, including:
Siemens Healthineers
GE Healthcare
Philips Healthcare
Canon Medical Systems
Hitachi Medical Systems
Toshiba Medical Systems Corporation
Hologic, Inc.
Fujifilm Holdings Corporation
Medtronic Plc
Esaote S.p.A.
Take Action Now: Secure Your Report Today - https://www.skyquestt.com/buy-now/multimodal-imaging-market
Challenges and Opportunities
The multimodal imaging market faces challenges such as high costs associated with advanced imaging systems and the need for specialized training for operators. However, opportunities lie in developing cost-effective solutions, expanding applications across various medical fields, and integrating AI to enhance imaging accuracy and efficiency.
Future Outlook
The Multimodal Imaging market is poised for robust growth, driven by continuous technological advancements and an increasing emphasis on precision medicine. Companies that innovate with new imaging modalities and focus on expanding their service offerings will lead the market. For a comprehensive analysis and strategic insights, consult SkyQuest’s Multimodal Imaging Market report.
The Multimodal Imaging market is crucial for advancing diagnostic capabilities and improving patient outcomes. As technology evolves and healthcare needs grow, multimodal imaging will play an increasingly significant role in medical diagnostics. Decision-makers in the healthcare industry should leverage these advancements to stay ahead in this dynamic market. For more detailed information, refer to SkyQuest’s in-depth Multimodal Imaging Market report.
0 notes
Text
Study Reveals How COVID-19 Infection Can Cause or Worsen Diabetes - Published Sept 13, 2024
Researchers from Weill Cornell Medicine have used a cutting-edge model system to uncover the mechanism by which SARS-CoV-2, the virus that causes COVID-19, induces new cases of diabetes, and worsens complications in people who already have it. The team found that viral exposure activates immune cells that in turn destroy beta (β) cells, the pancreatic cells that produce insulin. The study was published Sept. 2 in Cell Stem Cell.
“There has long been a hypothesis in the field that certain viral infections may trigger type 1 diabetes," said co-corresponding author Dr. Shuibing Chen, director of the Center for Genomic Health, the Kilts Family Professor of Surgery and a member of the Hartman Institute for Therapeutic Organ Regeneration at Weill Cornell Medicine. “But we were able to show how this happens in the context of COVID-19 infection.”
“When someone has severe COVID-19, of course the first priority is to treat the life-threatening symptoms,” said co-corresponding author Dr. Robert Schwartz, an associate professor of medicine at Weill Cornell Medicine and a gastroenterologist and hepatologist at NewYork-Presbyterian/Weill Cornell Medical Center. “But moving forward, there may be a way to develop clinical therapeutics that help avoid later injury to organs like the pancreas.”
Dr. Liuliu Yang and Dr. Yuling Han, who were postdoctoral fellows in the Department of Surgery, and Dr. Tuo Zhang, an instructor in microbiology and immunology at Weill Cornell Medicine, were co-first authors of the paper.
From the early days of the COVID-19 pandemic, doctors caring for sick patients observed that the virus affected a number of organ systems, including not only the lungs, but also the heart, liver, colon and pancreas. For the current work, the researchers started with samples of pancreatic tissue from autopsies of people who had died of COVID-19. They observed that the pancreatic islets, the parts of the pancreas that generate the insulin to regulate blood sugar, were damaged.
They then used an analysis technique called GeoMx to study the samples in more detail. This revealed the presence of immune cells called proinflammatory macrophages in the tissues. The job of these macrophages is to kill off pathogens, but they sometimes cause collateral damage to healthy tissues.
To learn more about this activity, the team used a model system developed in the Chen Lab that had never been used before; pancreatic islet organoids (mini organs) that included both a vascular system and immune cells. “If we want to use organoids to study how a disease progresses, it’s important to be able to include components of the immune system in these models,” said Dr. Chen. In this case, after infecting the organoids with SARS-CoV-2, they found the macrophages appeared to be killing off the β cells through a type of cell death called pyroptosis.
The team also used the organoids to study how the pancreas responds to infection with another infectious virus — coxsackievirus B4, which has been implicated in the onset of type 1 diabetes. They found a similar macrophage response. “Moving forward, this organoid system is going to be useful for looking at other viruses as well,” Dr. Schwartz said.
Further research on the signaling molecules that activate the macrophages also suggested potential interventions for protecting β cells from damage in patients with severe infections. Although it is too early to begin testing any treatments, this is something that may be possible in the future. This work could also help shed light on the underlying causes of long COVID, a condition that is believed to affect more than 15 million people in the United States.
Many Weill Cornell Medicine physicians and scientists maintain relationships and collaborate with external organizations to foster scientific innovation and provide expert guidance. The institution makes these disclosures public to ensure transparency. For this information, see profiles for Dr. Shuibing Chen and Dr. Robert Schwartz.
The research reported in this story was supported by the National Institute of Diabetes and Digestive and Kidney Diseases, part of the National Institutes of Health, through grant numbers R01DK137517, R01DK124463, R01DK130454, R01DK121072. The study also used data acquired from the Human Pancreas Analysis Program (HPAP-RRID:SCR_016202) Database), a Human Islet Research Network consortium (UC4-DK-112217, U01-DK-123594, UC4-DK-112232, and U01-DK-123716); and the Integrated Islet Isolation and Distribution Program (IIDP), NIH grant UC4DK098085.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Study Link: www.cell.com/cell-stem-cell/fulltext/S1934-5909(24)00293-5
#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#sars cov 2#still coviding#wear a respirator#diabetes#long covid
4 notes
·
View notes
Text
Nurse Practitioner - Heart and Vascular Institute of Texas near San Antonio, TX - Westover Hills - (San Antonio, Texas, United States)
Nurse Practitioner – Heart and Vascular Institute of Texas near San Antonio, TX – Westover Hills – (San Antonio, Texas, United States)
Heart and Vascular institute of Texas
3011 W Loop 1604 N Suite 102
San Antonio, TX 78251
Summary
Provide direct patient care services; augment a physician’s ability to provide medical services to patients; perform diagnostic and therapeutic procedures, order lab…
0 notes
Text
Finding the Top Heart Specialist in Hyderabad -TX Hospitals

Introduction:
When it comes to heart health, finding the right specialist is crucial for receiving high-quality care and effective treatment. Hyderabad, known for its advanced medical facilities, is home to several esteemed heart specialists who are renowned for their expertise in diagnosing and treating various cardiac conditions. Here’s a guide to some of the top heart specialists in Hyderabad and how you can easily book an appointment with them.
1. Dr. K. Sarat Chandra - Leading Heart Specialist
Dr. K. Sarat Chandra is recognized as one of the leading heart specialists in Hyderabad. His impressive qualifications include an MBBS, MD, and DM in Cardiology, with additional fellowships from prestigious institutions such as the American College of Cardiology (FACC), the European Society of Cardiology (FESC), and the Cardiological Society of India (FCSI). Dr. Chandra’s extensive experience and comprehensive approach to cardiology make him a top choice for those seeking expert care for their heart health.
Book Now: To schedule an appointment with Dr. K. Sarat Chandra, call 9089489089 or book your visit through TX Hospitals.
2. Dr. Sumeet Sinha - Expert Cardiologist
Dr. Sumeet Sinha is a highly regarded cardiologist in Hyderabad, known for his expertise in both preventive and interventional cardiology. With an MBBS, MD in General Medicine, and a DM in Cardiology, Dr. Sinha provides thorough diagnostic and treatment services for a wide range of heart conditions. His patient-focused approach ensures that each individual receives personalized care tailored to their specific needs.
Book Now: For a consultation with Dr. Sumeet Sinha, contact 9089489089 or arrange your appointment through TX Hospitals.
3. Dr. Deepak Saha - Specialist in Cardiology
Dr. Deepak Saha is a distinguished cardiology specialist in Hyderabad, known for his extensive training and expertise. His qualifications include an MD in Medicine, DNB in Cardiology, and fellowships from the Society for Cardiovascular Angiography and Interventions (FSCAI) and the European Society of Cardiology (FESC). Dr. Saha’s advanced skills in managing complex cardiac issues make him a top specialist in the field.
Book Now: Schedule your appointment with Dr. Deepak Saha by calling 9089489089 or visiting TX Hospitals.
4. Dr. Pruthvi Gattu - Renowned Heart Specialist
Dr. Pruthvi Gattu, with his MBBS, MD in General Medicine, and DM in Cardiology, is well-regarded for his proficiency in diagnosing and treating various heart diseases. His expertise and commitment to providing high-quality care make him one of the leading heart specialists in Hyderabad.
Book Now: To consult Dr. Pruthvi Gattu, call 9089489089 or book through TX Hospitals.
5. Dr. V. Chandrakanth - Top Cardiac Doctor
Dr. V. Chandrakanth is a top cardiac doctor in Hyderabad, known for his thorough diagnostic skills and effective treatment plans. With an MBBS and DM in Cardiology, Dr. Chandrakanth is dedicated to helping patients manage their heart conditions and improve their overall cardiovascular health.
Book Now: For an appointment with Dr. V. Chandrakanth, contact 9089489089 or schedule your visit at TX Hospitals.
6. Dr. Avinash Dal - Leading Cardiothoracic & Vascular Surgeon
Dr. Avinash Dal is a highly skilled cardiothoracic and vascular surgeon in Hyderabad. With qualifications including an MBBS, MS in General Surgery, and MCh in Cardiothoracic & Vascular Surgery, Dr. Dal specializes in complex heart surgeries and vascular procedures. His advanced surgical techniques and comprehensive care make him a leading choice for patients needing specialized cardiac surgery.
Book Now: Contact Dr. Avinash Dal by calling 9089489089 or book your consultation through TX Hospitals.
7. Dr. Sohail Sayyad - Expert Cardiothoracic Surgeon
Dr. Sohail Sayyad is an expert in cardiothoracic surgery with qualifications including an MBBS, DNB in General Surgery, and MCh in Cardiothoracic Surgery from NIMS. His extensive training and experience in performing intricate cardiac surgeries make him a top choice for patients requiring surgical interventions.
Book Now: To arrange a consultation with Dr. Sohail Sayyad, call 9089489089 or schedule your appointment at TX Hospitals.
8. Dr. Shashi Janjirala - Best Cardiac Surgeon
Dr. Shashi Janjirala, holding an MBBS, MD, and DM in Cardiology, is known for his exceptional skills in cardiac surgery. His expertise in handling complex surgical cases and his dedication to patient care make him one of the best cardiac surgeons in Hyderabad.
Book Now: For a consultation with Dr. Shashi Janjirala, contact 9089489089 or book through TX Hospitals.
Finding the right heart specialist can significantly impact your overall health and treatment outcomes. Hyderabad offers a range of top-notch cardiologists and cardiac surgeons who are committed to providing exceptional care. To schedule an appointment with any of these leading specialists, call 9089489089 or book through TX Hospitals.
#heart specialist in hyderabad#best cardiac doctor in hyderabad#best doctor for open heart surgery in hyderabad#top 10 cardiology doctors in hyderabad#heart transplant doctor in hyderabad
0 notes
Text
Pazopanib HCL: A Powerful Tyrosine Kinase Inhibitor for Cancer Treatment
Pazopanib HCL is a cutting-edge medication used in the treatment of advanced renal cell carcinoma (RCC) and soft tissue sarcoma. As a tyrosine kinase inhibitor, it plays a crucial role in managing these challenging cancers by targeting the mechanisms that enable tumor growth and spread.
What is Pazopanib HCL?
Pazopanib HCL is an effective tyrosine kinase inhibitor that helps manage advanced renal cell carcinoma and soft tissue sarcoma. This medication works by inhibiting key tyrosine kinases involved in cancer progression, thus hindering tumor growth and metastasis.
Buy Pazopanib HCL to access this powerful treatment option and take a step towards managing your cancer effectively.
Mechanism of Action
Pazopanib HCL works by blocking multiple tyrosine kinases, including:
Vascular Endothelial Growth Factor Receptors (VEGFRs)
Platelet-Derived Growth Factor Receptors (PDGFRs)
Fibroblast Growth Factor Receptors (FGFRs)
By inhibiting these receptors, pazopanib disrupts angiogenesis, the process through which tumors develop their blood supply. This disruption reduces the growth and spread of tumors, leading to decreased tumor vascularity and increased necrosis.
Benefits and Advantages
Here’s why buying pazopanib HCL could be a valuable choice for managing advanced RCC and soft tissue sarcoma:
Broad-Spectrum Inhibition: Pazopanib targets multiple pathways involved in tumor growth and angiogenesis, offering a comprehensive approach to cancer treatment.
Convenient Oral Administration: Its oral formulation makes it easy to take, improving patient compliance and convenience.
Effective Symptom Management: By slowing cancer progression and reducing tumor size, pazopanib helps improve patients' quality of life and potentially extends survival.
Side Effects and Risks
While pazopanib is effective, it can cause side effects that need monitoring:
Hypertension: Elevated blood pressure may occur, requiring careful management to avoid cardiovascular issues.
Hepatotoxicity: Liver toxicity, indicated by elevated liver enzymes, may necessitate regular monitoring of liver function.
Cardiac Toxicity: Potential cardiac side effects include QT interval prolongation, arrhythmias, and heart failure, particularly in those with preexisting cardiovascular conditions.
Gastrointestinal Issues: Pazopanib may cause diarrhea, nausea, and vomiting, which might require supportive care or dose adjustments.
About MedicaPharma
MedicaPharma is a leading distributor of high-quality active pharmaceutical ingredients (APIs), providing products to hospitals, pharmacies, research institutes, and universities worldwide. When you buy pazopanib HCL from us, you are choosing a supplier committed to excellence in pharmaceutical quality and safety.
Why Choose MedicaPharma?
At MedicaPharma, we pride ourselves on supplying GMP-certified products with logistics that comply with GDP regulations. This ensures that when you buy pazopanib HCL, you receive a product of the highest standard, supporting your treatment journey effectively.
Request a Quote Today
If you’re interested in buying pazopanib HCL, contact us for a quote and more information about how our high-quality products can meet your needs. Let MedicaPharma assist you in accessing this essential medication for managing advanced renal cell carcinoma and soft tissue sarcoma.
Choose MedicaPharma for reliable, high-quality pharmaceutical solutions and take control of your cancer treatment with confidence.
0 notes
Text
Engineering and matters of the heart
New Post has been published on https://thedigitalinsider.com/engineering-and-matters-of-the-heart/
Engineering and matters of the heart


Before she had even earned her bachelor’s degree, MIT professor and biomedical engineer Ellen Roche was gaining research experience in the medical device industry. In her third year at the National University of Ireland at Galway, Roche participated in a biomedical engineering program in which students worked at companies developing new devices for patient care.
“I worked on cardiovascular implants during my placement and loved it,” says Roche, an associate professor at MIT’s Institute for Medical Engineering and Science (IMES) and Department of Mechanical Engineering. “For me, early experience in the medical device industry was very influential because it showed me the elaborate process of what happens from the time a technology is designed at the bench, as it is developed into a meticulously tested and reliable device that will actually be implanted in a human.”
In graduate school, a similar program led Roche first to Mednova Ltd. in Galway and then to its sister company, Abbott Vascular in California, initially for a six-month stay. Roche enjoyed the work so much that she ended up staying three and a half years. While at Mednova and Abbott, she worked on a carotid artery filter designed to prevent stroke during the procedure when a stent is implanted. She also investigated coating parts of the stents with drugs that prevent arteries from becoming occluded.
Roche, who earned tenure at MIT in July 2023, directs the Therapeutic Technology Design and Development Lab, which incorporates soft robotics, advanced fabrication methods, and computational analysis tools to develop novel devices that help to heal the heart, lungs, and other tissues. Some of the devices her team designs are intended for implantation into patients, such as a soft robotic ventilator, while others, such as a 3D-printed replica of a patient’s heart, enable research and testing of other therapies.
She encourages her students to find ways to collaborate and be flexible — and to get some kind of industry experience while still in school. She says she tells them, “Be open to accepting good opportunities as they arise, work with like-minded people, and work hard at what you are doing, but readapt when you need to.”
“There’s so much that’s very hard to even imagine until you spend some time in industry, including regulatory submissions, quality control, clinical studies, manufacturing considerations, sterilization, reliability, packaging, labeling, distribution, and sales. It really is a concerted effort of many teams with many skills to get a device to first-in-human studies,” Roche says. “Having said that, it’s one of the most rewarding.”
Born in Galway, the daughter of a civil engineer father and a mother who was a radiographer, Roche always loved math, science, and building things, and was drawn to medicine as well. She says she chose biomedical engineering because of its interdisciplinary nature and its potential for impacting society.
Roche says her mother had a “huge influence” on her career choices.
“She brought me to the hospital to meet with people using various medical devices, and introduced me to one of my mentors in industry,” she says. “She had taught herself, as the local girls’ school she attended did not teach advanced (or honors) math.”
After working at Abbott, Roche says she found she wanted to expand her studies and learn new technologies that could be applied to medical devices. She returned to school, enrolling in a bioengineering master’s program at Trinity College in Dublin. While earning her degree, she also worked at Medtronic, where she helped develop a replacement valve for the aorta that was brought all the way from conception to clinical application in humans, a process she says she was fortunate to experience firsthand.
She also studied medicine at the Royal College of Surgeons in Ireland before being awarded at Fulbright Scholarship to pursue her PhD.
“Receiving the Fulbright Science and Technology award solidified my plans to pursue graduate study in the U.S.,” she says. She chose as PhD advisors David Mooney, a professor of bioengineering, and Conor Walsh, a professor of engineering and applied sciences, at Harvard University. “They were (and still are) amazingly supportive of my personal and professional development,” she says.
Roche has worked on a number of medical devices, including the soft, implantable ventilator; a mechanism that prevents the buildup of scar tissue; and the robotic heart, created by using 3D printing. For the robotic heart, Roche and her team start with an MRI scan of a patient’s heart and, using a soft material, print a replica of the heart, matching the anatomy, including any defects. With such a realistic model, the researchers can then apply different treatments, such as prosthetic valves or other implantable devices, in order to test them and learn more about the biomechanics that are involved.
“We can look at various devices and tune the heart, depending on what we’re trying to test,” Roche said in the “Curiosity Unbounded” podcast with MIT President Sally Kornbluth.
The 3D-printed heart, and other medical simulators Roche has worked on, greatly facilitate and improve the testing of patient interventions — and may one day also be used as implantable devices in humans.
“You can envision the people who are at end-stage heart failure, who are waiting for a transplant and on these long lists, could actually have a printed, entirely synthetic, beating heart,” Roche told Kornbluth.
Roche’s work has garnered many awards, including a National Science Foundation CAREER award in 2019, and boosts to her entrepreneurship. Her medical device startup, Spheric Bio, which is developing a minimally invasive heart implant aimed at preventing strokes, won the Faculty Founders Initiative Grand Prize in 2022 and the Lab Central Ignite Golden Ticket, which supports startup founders from traditionally underrepresented groups in biotechnology.
Meanwhile, in a dual faculty appointment in mechanical and medical engineering, Roche won the Thomas McMahon Mentoring Award in 2020, which each year goes to a person who “through the warmth of their personality, inspires and nurtures [Harvard-MIT Program in Health Sciences and Technology] students in their scientific and personal growth.” She also received the Harold E. Edgerton Faculty Achievement Award in 2023, in recognition of exceptional teaching, research, and service.
The current research advances that excite Roche most, she says, include treatments and devices that can be customized to be patient-specific, such as in silico trials and digital twins where computational approaches can facilitate the investigation various interventions and prediction of their outcomes.
Roche’s expanding research on physical biorobotic simulators and computational models has attracted interest from industry and clinical teams. She was recently approached by a local hospital to build models for training heart surgeons on how to select which pump or ventricular assist device to use depending on a patient’s particular case. The models allow the surgeons to explore the efficacy of the assist devices at work.
Roche has three young daughters, whom she often brings to work, where “they love the environment, the students, and the lab,” she says.
Somehow, she also finds time to do triathlons, travel, and sample some of the local brews of New England. She’s currently planning to participate in a triathlon with her two PhD co-advisors, Mooney and Walsh. Luckily, she says she does her best thinking while running, biking, or swimming — or late at night.
Active and successful in so many realms, Roche provides seemingly simple advice to her students who want to have an impact on the world: “Find a way to combine what you love, what you are good at, and what will help others.”
#2022#2023#3d#3D printing#Advice#Analysis#Anatomy#arteries#bioengineering#Bioengineering and biotechnology#Biomechanics#Biomedical engineering#biotechnology#Born#Building#career#collaborate#college#Companies#curiosity#Design#development#devices#digital twins#drugs#Edgerton#Engineer#engineering#Environment#Fabrication
1 note
·
View note