#gmfcs
Explore tagged Tumblr posts
Text

🔰 Fellows' Academic Rounds
⭐ Art and Science of Paediatric Orthopaedic Clinical Examination
📚 Session 1
🗓️ Date: Saturday, 21st September 2024 🕗 Time: 8:00 to 9:00 am IST
🔆Click to Watch : https://tinyurl.com/OrthoTV-Orthokids-75
🎗️ Topic & Faculty :
🔹How do I examine a child with cerebral palsy? Dr. Gaurav Gupta
🔹Fellows quiz on GMFCS & visual gait analysis Dr. Joyance James
👨⚕️ Moderator
Dr. Maulin Shah Dr. Preksha Vijay
🤝 OrthoTV Team Dr. Ashok Shyam, Dr. Neeraj Bijlani
📺 Streaming live on OrthoTV: www.orthotvonline.com
▶️ Join OrthoTV - https://linktr.ee/OrthoTV
#PaediatricOrthopaedics #FellowsAcademicRounds #CerebralPalsy #ClinicalExamination #GMFCS #GaitAnalysis #OrthopedicEducation #OrthoTV #Orthokids #LiveWebinar #PediatricSurgery #OrthoTVGlobal #FellowsQuiz #OrthopedicRounds #CerebralPalsyExamination #OrthopedicSurgeons #OrthopedicTraining
0 notes
Photo

Скалодром зацепы производство , тестирование и продажи как для обычных детей так и для детей с ограниченными возможностями . Если вам необходимо подобрать скалодром зацепы под определенные особенности вашего ребенка , компания скалодромы Жужа будет рада помочь в этом вопросе . Мы помогаем создавать в малых пространствах комфортную среду для детей с ограниченными возможностями , что позволяет им более эффективно и быстрее социализироваться. #детиовз #рас #дцп #аутизм #адаптивныйфитнес #адаптивныйскалодром #детскийсад #GMFCS ##занятиясдетьми #дцпангел #дцпреабилитация #дцпдети #лфк #физическаятерапия #особенныеродители #особоедетство (at Скалодромы Жужа) https://www.instagram.com/p/B5xWpgUB_HA/?igshid=1059chr4nnctq
#детиовз#рас#дцп#аутизм#адаптивныйфитнес#адаптивныйскалодром#детскийсад#gmfcs#занятиясдетьми#дцпангел#дцпреабилитация#дцпдети#лфк#физическаятерапия#особенныеродители#особоедетство
0 notes
Text
MY FAVORITE FOUNDATION CHANGED THEIR FORMULA GRRR

#gmfc Tarte why you gotta do this to me#I’ve been using this foundation for 8 YEARS#I have to make the tube I have count 😭#what is with all my favorite things changing formula lately
0 notes
Text
A free medical camp for underpriviliged children suffering from Cerebral Palsy and Pediatric Orthopaedic disorders was organised by Dr. Easwar T.R and the administrative team at ICCONS, Shoranur, Kerala on 24th, May,2018.
A gamut of problems commonly seen in children with Cerebral Palsy was observed in OPD. While some parents had the good fortune of seeking medical care and intervention early in course of disease and others were not so fortunate. Lack of parental knowledge, distance / accessible care, financial cruch, normal siblings to care for and single parent challenges were the most important issues observed on casual data collection.
The medical camp was followed by an awareness class for parents, therapists and other care givers by Dr. Easwar T.R on the various aspects of Cerebral Palsy.
Custom wheel chair and mobility solutions for needy patients was discussed with Physiotherapists and low cost solutions for the same identified. Mobility solutions continue to be a major challenge for children in rural areas with poor roads, small homes with narrow doors and steps inside homes especially with outdoor toilets.
Flat foot in Cerebral Palsy
Cerebral Palsy child with widestance and flat foot
A child with dislocated hip due to poor posturing
Pediatric Orthopedic Camp at ICCONS
In front of Dr. Easwars office
Outpatient Department at ICCONS
Flat foot in Cerebral Palsy
Cerebral Palsy child with widestance and flat foot
A child with dislocated hip due to poor posturing
In front of Dr. Easwars office
Outpatient Department at ICCONS
Outpatient Department at ICCONS
In front of Dr. Easwars office
Pediatric Orthopedic Camp at ICCONS
A child with dislocated hip due to poor posturing
Cerebral Palsy child with widestance and flat foot
Flat foot in Cerebral Palsy
Cerebral Palsy Medical Camp at Shoranur, Kerala A free medical camp for underpriviliged children suffering from Cerebral Palsy and Pediatric Orthopaedic disorders was organised by Dr.
0 notes
Text
Tragic accident in Atchutapuram SEZ, reactor blast at pharma company causes panic
This morning, a tragic accident took place in the Atchutapuram Special Economic Zone (SEZ) near Visakhapatnam, where a reactor blast occurred at a pharma company. According to the preliminary reports, one person died on the spot, and three others were reported to be heavily injured in the accident. The reactor blast at the GMFC Labs Pvt Ltd triggered a huge explosion leading workers and the…
View On WordPress
0 notes
Text
From Diagnosis to Recovery: The Comprehensive Cerebral Palsy Care at Upright Kids Ortho with Paediatric Orthopaedic Surgeon Bangalore | Dr. Jayanth S Sampath

Cerebral palsy (CP) is a disorder that affects muscle tone, movement, and motor skills (the ability to move in a coordinated and purposeful way).
Cerebral palsy can also lead to other health issues, including vision, hearing, and speech problems, and learning disabilities.
CP is usually caused by damage to parts of the brain before or during a child’s birth, or during the first 2 years of a child’s life.
There is no cure for CP, but treatments such as physical therapy, splints or orthotics, medications such as Botulinum injections and Orthopaedic Surgery will help a child who is living with the condition.
It is worthwhile pointing out that majority of common human ailments such as diabetes, high blood pressure, stroke, heart attack, kidney failure, etc are also incurable conditions. But, treatment of these conditions is essential to prevent complications. Cerebral palsy is no different in that it does not have a cure but treatment is essential.
How does Cerebral Palsy work At Upright Kids Ortho?
What are the symptoms and signs of cerebral palsy?
Paediatric Orthopaedic Surgeon Bangalore | Dr. Jayanth S Sampath says the predominant symptoms and signs of cerebral palsy are related to difficulties with movements of the legs and arms.
The extent and severity of the brain lesion is the leading factor in the magnitude of the motor deficit. For example, developmental motor delay, gait disorders, poor fine and gross motor coordination, swallowing disorders, or speech delay are all the result of the basic movement problem. The way they present varies from child to child. For that reason, it is difficult to describe a clinical picture that will satisfy every child with cerebral palsy. The clinical presentation, even though with many common features, is very much unique for a particular child. In addition, the comorbid conditions add more to the uniqueness of the presentation of the child with cerebral palsy. For example, some children may be blind, while others may have normal vision; some children may have a severe cognitive delay while others may have a normal or near normal cognitive level.
What are the types of cerebral palsy?
Based upon the form of motor impairment, cerebral palsy can be divided into types:
Spastic cerebral palsy
Dyskinetic cerebral palsy (according to the predominant symptoms dyskinetic CP may be either dystonic or choreo-athetoid) which includes ataxic cerebral palsy
Hypotonic cerebral palsy.
These categories are not rigid, and the majority of patients most probably have a mixture of them.
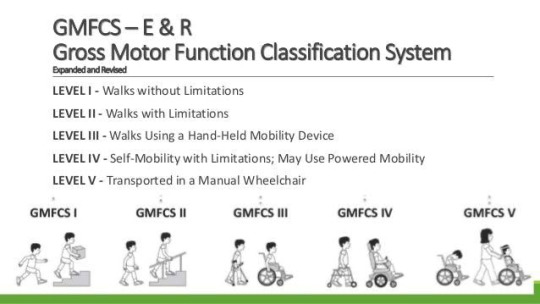
Cerebral palsy can also be classified into different types depending on the mobility level of the child. This system is called GMFCS (Gross Motor Functional Classification System) and is the most widely used classification system to describe children with cerebral palsy. The figure below easily illustrates the different types from Level I to Level V. Kindly note that the mobility level changes slightly as the child goes through the teenage years and pubertal growth spurt.
This is a well-described aspect of the natural history of cerebral palsy. Children who were walking with support until the age of 8 – 10 years lose some or all of their walking ability during early adolescence. This has been attributed to a reduction in the power: weight ratio of children. As muscles become bigger, they also become weaker relative to their weight.
Causes of CP
Paediatric Orthopaedic Surgeon Bangalore | Dr. Jayanth S Sampath says There is no identifiable cause in some children with cerebral palsy.
Typical causes to look for include
Problems occurring before birth (e.g. exposure to radiation, infection, inadequate brain development),
Problems during birth such as asphyxia before birth, hypoxia (poor oxygen supply) of the brain, and birth trauma during labor and delivery
Premature and low birth weight babies
Complications occurring some time after birth or during childhood.
Genetic causes
In the modern context, many premature babies (babies born earlier than 36 weeks and/ or less than 1.5 kg in weight at birth) can be saved thanks to advances in neonatal care but premature babies have an increased risk of CP. Many of the children that we see in our practice have spent some time in the NICU (neonatal intensive care unit). Fortunately, premature babies have spasticity as their predominant movement disorder, most will walk independently and their gait problems can be corrected by orthopaedic surgery.
In the past, conditions such as kernicterus (uncontrolled jaundice in newborn babies causing damage to parts of the brain) were quite common. This group of disorders caused dyskinetic type of CP that was not readily amenable to surgery and prognosis for walking was poor. Due to early detection of jaundice in most neonates and prompt treatment, the incidence of Kernicterus is on the decline.
Why do premature babies develop CP?
Premature infants are vulnerable, in part because their organ systems and control mechanisms are not fully developed, increasing the risk of reduced oxygen supply to the brain that may manifest later as CP.
It is sometimes difficult to differentiate between cerebral palsy caused by damage to the brain that results from inadequate oxygenation and CP that arises from brain damage which occurs when the baby is still in the womb that then precipitates premature delivery. From the point of view of treatment, this distinction is academic and not of much relevance. MR scan of the brain may help in diagnosing this further but in terms of treatment, diagnostic tests such as MR scans do not help with orthopaedic treatment.
After birth (postnatal), other causes include toxins, severe jaundice, lead poisoning, physical brain injury, shaken baby syndrome, incidents involving hypoxia to the brain (such as near drowning), and encephalitis or meningitis.
The three most common causes of asphyxia in the young child are: choking on foreign objects such as toys and pieces of food, poisoning, and near drowning.
In general, postnatal causes of CP (damage to the brain after birth) result in a more severe form of the condition with extreme muscle tone and postures, severe cognitive impairment and the prognosis for walking is less certain compared to CP caused by prematurity.
Diagnosis of Cerebral Palsy:
The initial suspicion of CP is typically raised by family members or noticed by the parents as a failure to achieve motor milestones. The child may not achieve head control by 6 months, sitting may be delayed or mild abnormalities in walking may be noticed.
The child’s paediatrician is usually the first person to raise the possibility of CP. As mentioned earlier, cerebral palsy is NOT a condition resulting from a single cause. It is a clinical diagnosis made by doctors when a child has a number of different problems such as problems with walking, speech, hearing, sight, balance, co-ordination and fine motor control (using the hands for delicate tasks such as writing).
No single factor can confirm or refute the diagnosis of CP. Rather; it is combination of various factors that taken together will help the doctor make the diagnosis of CP.
For instance, a 2 year old child who has not yet started walking; was a premature baby born at 7 months with a birth weight of 1kg may turn out to have cerebral palsy.
Though tests such as an MR scan of the brain are quite commonly done in the process of making the diagnosis of CP, there is no single test which will confirm the diagnosis. As the causes of CP are highly varied, a series of investigations (tests) may need to be carried out.
Who makes the diagnosis?
According to Paediatric Orthopaedic Surgeon Bangalore | Dr. Jayanth S Sampath, Any qualified clinician with experience in the area of child development can make a diagnosis of cerebral palsy. Typical clinicians who may see children with a potential diagnosis of CP include paediatricians, physiotherapists, paediatric orthopaedic surgeons, developmental specialists, and paediatric neurologists, amongst others.
Once the possibility of CP has been raised, it is prudent to seek the opinion of
A paediatric neurologist (to confirm the diagnosis) and
A paediatric orthopaedic surgeon (to discuss treatment options).
It is advisable to seek expert advice early so that parents can be correctly counselled about the particular treatment options suitable for their child.
Clinicians unfamiliar with the modern management of CP are a source of misinformation to parents. Words such as “untreatable” are sometimes used, causing uncertainty and distress to parents. CP is very much treatable with modern scientific methods and good outcomes are routinely obtained in the majority of children.
Treatment for CP
There are several factors which influence choice of treatment for a particular child. The principal among these are:
Age of the child
The age of the child is the single most important factor which influences treatment planning. Cerebral palsy is a “static” encephalopathy, meaning that the primary problem in the brain does NOT change over time. It does not get better or worse. However, bones, muscles and joints of the legs can develop abnormalities due to growth.
Any intervention such as physiotherapy, Botox injection or surgery should be employed after a thorough understanding of the natural history of cerebral palsy. Thanks to the pioneering work of Prof Rosenbaum and co-workers (from CanChild Centre for Childhood Disability Research, McMaster University, Canada), we have a detailed understanding of how children with CP develop in the first few years of life. Similar findings were seen in an independent Swedish study (Developmental Medicine & Child Neurology 2007, 49: 751–756).
The graph below shows that children with GMFCS Level I and II CP (children with independent walking ability) reach their peak motor ability around the age of 6 to 7 years. This NATURAL improvement occurs due to the maturation of brain function. It, therefore, stands to reason that any intervention such as orthopaedic surgery should be performed after the age of 7 years.
The Ontario Motor Growth Study
The Motor Growth Curves report patterns of gross motor development in children with cerebral palsy, classified according to each of the five levels of the Gross Motor Function Classification System (GMFCS) (Palisano et al., 1997). Children in this study were followed longitudinally for several years. The findings were published in a paper entitled ‘Prognosis for Gross Motor Development in Cerebral Palsy. Creation of Motor Growth Curves’, Rosenbaum et al., JAMA 2002; 288; 1357-63.
In the first few years of life, most children with CP will benefit from supportive treatments such as physiotherapy and orthotics. Once the child reaches his or her maximum motor potential (typically between the ages of 8 and 10 years) and achieves a steady state in terms of growth, consideration can be given to whether orthopaedic surgery will be beneficial.
The graph below illustrates common interventions undertaken at different ages in children with CP.
It can be seen that peak age for non-surgical treatments is around 5 years and the peak age for surgery is around 10 years.
GMFCS Level:
The walking ability of the child determines his/ her GMFCS level. Children with GMFCS levels I and II and some children with Level III CP may benefit from Gait Improvement Surgery (also called Single Event Multi-level Surgery or SEMLS).
Children with GMFCS Levels IV and V CP do not benefit from surgery to release contractures or muscle tightness in the legs, as the children in this category are unlikely to gain the ability to walk even with surgery. However, children with GMFCS Levels IV and V CP have a high risk of gradual dislocation of the hip joint. This will require careful monitoring through regular hip x-rays.
Movement Disorder:
Spasticity is the most common movement disorder seen in CP. Muscles affected by spasticity feel tight when stretched suddenly. Slow and gentle stretching of the muscle does not evoke spasticity.
Children with spasticity as their predominant movement disorder and who are able to walk either independently or with support have a better overall prognosis with regard to walking/ standing ability compared to children with other types of movement disorders.
Children with dyskinetic movement disorders such as Dystonia, Athetosis, chorea, ataxia or hypotonia DO NOT show a predictable response to surgery.
Scientific publications also advocate non-surgical treatment options in children with Dystonia. Dyskinetic movements are caused by damage to parts of the brain (called basal ganglia). Performing orthopaedic surgery by muscle releases and tendon lengthening cannot change the damaged area in the brain.
It is highly likely that children with dyskinetic movement patterns will remain unchanged even after orthopaedic surgery. Any minor improvements noted after surgery are likely to be due to the physiotherapy provided post-operatively and these improvements will reverse once the intensive physiotherapy is stopped.
Spasticity is caused by damage to nerve fibres leaving the higher centres of the brain (cerebral cortex). Therefore, spasticity does not change after muscle release surgery. What orthopaedic surgery corrects is the permanent muscle stiffness which occurs as a consequence of spasticity. In fact, some experts believe that spasticity is beneficial in that it maintains muscle strength to a certain extent.
Orthopaedic surgery is therefore recommended only in those children who have permanent shortening of the muscle rather than pure spasticity. If regular physiotherapy and other treatments are provided at an early stage, muscle shortening does not typically develop in younger children (less than 6 years of age). Even in those younger children where contractures do develop, this can be managed without the need for surgery, through the use of Botox, serial casting, physiotherapy and use of splints.
There are treatments such as Botulinum toxin injection; Selective Dorsal Rhizotomy and Intrathecal Baclofen pump which directly reduce spasticity. More information about these anti-spasticity treatments is provided in a later section.
As the child grows, bones and muscles normally grow in almost perfect synchrony.
In children with CP, muscle growth is unable to keep up with bone growth. Therefore, muscles become progressively shorter over time. This causes joint tightness and eventually contractures (permanent joint tightness).
Bones can develop abnormal twists (called torsional problems) in children with CP.
When babies develop inside the mother’s womb, bones of the legs develop with an inward twist. This is normal and happens in all children. Typically developing children start walking by the age of 1 year. The forces applied to the legs during walking causes the inwardly twisted bones to straighten out. When walking is delayed (in conditions such as CP), the embryonic alignment of the leg bones persists. Persistent femoral anteversion and internal tibial torsion together contribute to intoeing gait (feet turned inwards) in children with CP.
The main orthopaedic issues in children with CP are:
Muscle shortening
Joint contractures
Bony torsion
Medications
Medications that can lessen the tightness of muscles may be used to improve functional abilities, treat pain and manage complications related to spasticity. It’s important to talk about the risk of drug treatments with your doctor and discuss whether medical treatment is appropriate for your child’s needs. The selection of medications depends on whether the problem affects only certain muscles (isolated) or the whole body (generalized).
Focal spasticity
Generalized spasticity
Therapies
A variety of nondrug therapies can help a person with cerebral palsy to enhance functional abilities. These include the following:
Physical therapy: Muscle training and exercises may help your child’s strength, flexibility, balance, motor development and mobility. Braces or splints may be recommended for your child. Some of these supports are used to help with function, such as improved walking. Others may stretch stiff muscles to help prevent contractures.
Occupational therapy: Using alternative strategies and adaptive equipment, occupational therapists work to promote your child’s independent participation in daily activities and routines in the home, the school and the community.
Speech therapy: Speech therapists help improve your child’s ability to speak clearly or to communicate using sign language. They can also teach your child to use special communication devices — such as a board covered with pictures of everyday items and activities. Sentences can be constructed by pointing to the pictures. Speech therapists may also address difficulties with muscles used in eating and swallowing.
Surgical or other procedures
Surgery may be needed to lessen muscle tightness or correct bone abnormalities caused by spasticity. These treatments include:
Orthopaedic surgery: Children with severe contractures or deformities may need surgery on bones or joints to place their arms and legs in their correct positions. Surgical procedures can also lengthen muscles and tendons that are proportionally too short because of severe contractures. These corrections can lessen pain, improve mobility, and make it easier to use a walker, braces or crutches.
Severing nerves: In some severe cases, when other treatments haven’t helped, surgeons may cut the nerves serving the spastic muscles. This relaxes the muscle and reduces pain, but can also cause numbness.
For more information visit- https://www.uprightkidsortho.com/blog/managing-cerebral-palsy-in-children-a-doctor-explains/
Our website - https://www.uprightkidsortho.com/
Our other treatment-
Perthes disease- https://www.uprightkidsortho.com/perthes-disease/
Clubfoot – https://www.uprightkidsortho.com/clubfoot-or-congenital-talipes-equinovarus/
Leg length discrepancy- https://www.uprightkidsortho.com/leg-length-discrepancy/
#orthopedics #orthopedicsurgery #orthopedics #orthopedicsurgeon #surgery #surgeon #Doctorjayanth #Drjayanth #Doctorjayanthwhitefield
#orthopedics#orthopedicsurgery#orthopedicsurgeon#surgery#surgeon#Doctorjayanth#Drjayanth#Doctorjayanthwhitefield#drjayanth#doctorjayanth#bangalore#doctorjayanthwhitefield#pediatric
0 notes
Text
#51 GMFCS – Gross Motor Function Classification System
El sistema de la clasificación de la función motora gruesa (GMFCS) para la parálisis cerebral está basado en el movimiento auto-iniciado por el paciente con énfasis en la sedestación (control del tronco), las transferencias y la movilidad.
Como se califica?
el sistema de clasificación de cinco niveles, nuestro principal criterio es que la diferencia entre cada uno de estos niveles sea significativo para la vida diaria.
Nivel 1: Camina sin restricciones
Nivel 2: Camina con limitaciones
Nivel 3: camina utilizando dispositivo manual auxiliar de la marcha
Nivel 4: Auto movilidad limitada, es decir movilidad motorizada
Nivel 5: transportado en silla de ruedas
Antes del 2 cumpleaños
Nivel 1: el bebé entra y sale de la posición sentada, gatea sobre las manos y las rodillas, tira para ponerse de pie y da pasos agarrándose de los muebles. Los bebés caminan entre los 18 meses y los 2 años de edad sin necesidad de ningún dispositivo de ayuda a la movilidad.
Nivel 2 : sentado en el suelo pero usa las manos para apoyarse. Gatea sobre manos y rodillas. Puede jalar para ponerse de pie y dar pasos agarrándose de los muebles.
Nivel 3: sentado en el suelo con la parte inferior de la espalda apoyada. Se arrastra hacia adelante sobre el estómago.
Nivel 4: Los bebés tienen control de la cabeza, pero se requiere soporte del tronco para sentarse en el suelo. Los bebés pueden rodar hacia atrás y pueden rodar hacia el estómago.
Nivel 5: las deficiencias limitan el control voluntario del movimiento. Necesita ayuda con el control de la cabeza y el tronco al sentarse.
Entre 2 y 4 cumpleaños
Nivel 1: Entrar y salir del suelo sentado y de pie sin ayuda. Niños capaces de caminar.
Nivel 2: Entrar y salir del suelo sentado y de pie sin ayuda. Capaz de jalar para pararse en una superficie estable. Navegue apoyándose en los muebles y camine con un dispositivo de asistencia.
Nivel 3: Los niños se arrastran boca abajo o gatean sobre las manos y las rodillas. Puede tirar para ponerse de pie y recorrer distancias cortas. Puede caminar distancias cortas con un andador y la supervisión de un adulto.
Nivel 4: Los niños se sientan cuando se colocan y necesitan manos para apoyarse. Necesita equipo para sentarse y pararse. Se arrastra sobre el estómago o se arrastra por distancias cortas.
Nivel 5: Los niños necesitan equipo adaptable para sentarse y pararse. No tienen medios de movimiento independiente y algunos usan sillas de ruedas eléctricas.
Entre 4 y 6 cumpleaños
Nivel 1 : Entrar y levantarse de la posición sentada sin apoyarse en las manos. Los niños caminan adentro y afuera y suben escaleras. Empezar a correr y saltar.
Nivel 2 : Capaz de sentarse en una silla. Capaz de pasar del piso a estar de pie, pero requiere una superficie para impulsarse. Capaz de caminar distancias cortas en terreno estable. Capaz de subir escaleras con la ayuda de una barandilla. Sin correr ni saltar.
Nivel 3 : los niños pueden sentarse en una silla pero pueden necesitar algo de apoyo. Camine con un dispositivo de movilidad de mano. Sube escaleras con ayuda.
Nivel 4 : Los niños necesitan apoyo en el tronco cuando están sentados. Use un andador para distancias cortas. Puede lograr la automovilidad usando una silla de ruedas.
Nivel 5 : Todas las áreas de la función motora están limitadas. No hay medios de movimiento independiente.
Entre los 6 y los 12 años
Nivel 1 : Los niños caminan en casa, en la escuela, al aire libre y en la comunidad. Los niños pueden correr y saltar, pero el equilibrio es limitado.
Nivel 2 : Los niños caminan en la mayoría de los entornos. Dificultad en terreno irregular. Puede caminar al aire libre y en la comunidad con ayuda. Capacidad mínima para correr y saltar.
Nivel 3 : Los niños caminan usando un dispositivo de movilidad manual. Necesita una silla de ruedas cuando viaja largas distancias. Puede ser capaz de subir y bajar escaleras utilizando una barandilla.
Nivel 4 : Los niños requieren asistencia para sentarse y asistencia con las transferencias. En casa, los niños ruedan, gatean o caminan distancias cortas con ayuda o usan una silla de ruedas. Para distancias más largas, los niños usan una silla de ruedas manual o eléctrica.
Nivel 5 : Los niños son transportados en silla de ruedas manual en todos los escenarios. Los traslados requieren asistencia física completa.
Entre los 12 y los 18 años
Nivel 1 : Capaz de caminar en el hogar, la escuela, al aire libre y en la comunidad. Capaz de correr y saltar. El saldo es limitado.
Nivel 2 : Capaz de caminar en la mayoría de los entornos. En la escuela o el trabajo, utilizan dispositivos de movilidad portátiles por seguridad. Al aire libre y en la comunidad, utilizan una silla de ruedas para largas distancias. Capaz de subir y bajar escaleras usando una barandilla.
Nivel 3 : Los jóvenes caminan usando un dispositivo de movilidad manual. En la escuela y en la comunidad utilizan una silla de ruedas manual o eléctrica. Puede subir y bajar escaleras usando una barandilla.
Nivel 4 : Los jóvenes utilizan la movilidad con ruedas en la mayoría de los entornos. Necesita 1 o 2 ayudantes para las transferencias. Puede usar una silla eléctrica. Puede caminar distancias cortas en interiores usando un andador.
Nivel 5 : Los jóvenes se transportan en una silla de ruedas manual en todos los entornos. Los jóvenes tienen una capacidad limitada para mantener las posturas de la cabeza y el tronco y controlar los movimientos de los brazos y las piernas. Se requiere asistencia física de 1 o 2 personas o un elevador mecánico para los traslados.
(_ApplicationFrame, 2017)
Cuando se creo?
su creación fue en el 2007
El objetivo de la GMFCS es determinar cuál nivel representa mejor las habilidades y limitaciones del niño y joven sobre su funcionamiento motor grueso.
ARTICULOS Y REFERENCIAS https://canchild.ca/system/tenon/assets/attachments/000/000/079/original/GMFCS-ER_Translation-Spanish.pdf https://www.cambridge.org/core/journals/developmental-medicine-and-child-neurology/article/abs/gross-motor-function-classification-system-impact-and-utility/76E4E01AA59277DC7543CE7E7CFE5DC7 https://www.childrensmn.org/educationmaterials/childrensmn/article/17180/gross-motor-function-classification-system/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5406689/ _ApplicationFrame. (2017, 4 agosto). Children’s Minnesota. https://www.childrensmn.org/educationmaterials/childrensmn/article/17180/gross-motor-function-classification-system/
0 notes
Photo

🔰Session for Ped Ortho Fellows & PGs
✳️ The role of GMFCS for orthopaedic management decisions in cerebral palsy
🗓 24th March ,Friday ⌚4:30 - 5.30 pm IST
👨⚕️Speaker : Prof. Matthias Axt, Australia
🔸 Experts: Dr Jayanth Sampath & Dr Abhay Gahukamble
💻Click to watch : http://bit.ly/OrthoTV-POALS-19
🤝OrthoTV Team: Dr Ashok Shyam, Dr Neeraj Bijlani
📺Streaming live on OrthoTV www.orthotvonline.com
0 notes
Video
youtube
The Precious Children of Moyale Kenya - GMFC / WFF
0 notes
Video
Electric bed 2 small size.mp4 from Sales Gilani Engineering on Vimeo.
Fully adjustable electric single hospital and home care bed with 5 settings
This Fully Adjustable Electric Bed has 5 different settings making it suitable for use in aged care centres, hospitals and at home. The adjustable electric bed is suitable for individuals with limited mobility as it is powered with a remote control making it easier to lift and transfer users.
Features of Gilani Engineering's 5 functions of the hospital bed: Height adjustable from floor to the base of the bed: 48cm-86cm Remote Controlled Hospital Bed PP head and footboards and side rails 5" Central locking castors 200cm long, 92cm wide and 48cm high from floor to base Safe Weight 225kg Internal width: 90cm Internal length: 200cm Medical High low five function adjustable electric bed features electric motor controls that raise the head, foot and integrated height of the bed frame with a push of a button via a remote control.
This type of bariatric medical adjustable electric bed is ideal for using at home, hospital. This top rated hospital bed is much convenient for the caregivers or nurse compared with the manual crank system.
Features of the automatic adjustable electric bed for hospitals: Back up & down Knee up & down Integrated heighten adjustable Tuck away hospital beds rails side design Adjustment together of back and knee position One key automatic regression of flat position (Push down the button of leg and back down.) Head and foot boards removable and provided with locking system for safety during transport Holes for IV holders, being positioned in the 4 extremities of the frame The head and the tail of the bed are made of ABS Injection moulding Equipped with advanced touch screen switch. Separate ABS guardrail, anti-pinch hand design, guardrail with embedded touch screen. A key flattening key allows the bed to return to the initial state at any angle. The chassis is equipped with ABS dust cover. The configuration of four braking control with 125 wheels, brake control. The backrest and legs, lifting and tilting function before and after electric five. The back 0-70 degrees; leg 0-35; Lift 0-400mm and 0-180mm degrees 0-12 tilt lift. Please see photos for further details. Delivery charges apply outside the local Western Sydney region. Free pickup. Delivered fully assembled, only putting the hand rails and wheels on. No tools required. The hospital bed is recommended for everyone including people with: Hemiparesis Unilateral paresis Quadriplegic Stroke Later stages in Multiple sclerosis (MS) or (MND) Cerebral Palsy GMFCS levels IV -V To proceed with After Pay on check out for orders over $2000.00, please contact us to purchase a valid coupon. Please Note that The product includes the Bed only and the Mattress can be purchased SEPARATELY. Electric Hospital Bed with split side rails, headboard and foot board for safety, five function remote control automatic bed This Electric Bed has 5 remote controlled automatic functions. In this image, it is shown with the head tilted fully down, however the legs are raised up
***HIRE TO BUY OPTION AVAILABLE*** Frequently asked questions: 1- Am I able to use my NDIS or Aged Care Package to purchase this hospital bed? Yes, of course, you can. We are an NDIS provider which enables us to work with support staff in finding the right package for you. 2-What types of extras or accessories do you have available on sale for the electric hospital bed? We are able to supply: various types of mattresses to come with this chair including pressure support overlay mattresses for people with limited mobility or people prone to developing pressure sores. 3-What makes the hospital bed stand out from other regular beds? This product is efficient to use and has safety bed rails for people with limited mobility. Similarly, it is easy to use and the remote allows you to use 5 different settings with the electric bed. 4-What settings can be adjusted on this electric hospital bed? This bed can be adjusted in 5 different ways. It can be raised or lowered The headrest can be raised or lowered The leg rest can be raised or lowered The knee area can fold providing support and going up and down The Back can be raised or lowered
0 notes
Text
case study mgt 441 labor relations
case study mgt 441 labor relations
Read the case study from Chapter 7. Locating the New RV Plant (my book = p. 219) • As a member of the planning committee for the new plant, write an email to the GMFC CEO and COO providing advice to the company on the issues that could help keep the new plant union-free. Consider the issues of size, location, staffing, compensation and any other issues. • Expect to take 1-2 pages, double…

View On WordPress
0 notes
Text
What did we learn about Dunfermline Athletic against Greenock Morton
Finally, a #DAFC victory against #GMFC. And it could not come at a better time as the Pars move back into second as Stevie Crawford may have taken more than three points out of the match. ✍️ @MichaelWood_SJ 📱RTs and likes are appreciated. ⬇️
By @MichaelWood_SJ Morton Maimed For one reason or another, the Inverclyde outfit has had the better of the Fifers. In the previous 10 years, the two clubs have met 29 times, with DAFC managing just eight victories – including Saturday’s effort. Considering the Ton have only finished as high as runners-up once since their relegation from the top flight in 1988 and their only major honour is…

View On WordPress
0 notes
Photo

A Study to Find Out the Effect of Arm Movement through Sensory Based Game on Improving Postural Control in Spastic Diplegic Cerebral Palsy
by Abhirupa Chakraborty | Mrs. Anurupa Senapati "A Study to Find Out the Effect of Arm Movement through Sensory Based Game on Improving Postural Control in Spastic Diplegic Cerebral Palsy"
Published in International Journal of Trend in Scientific Research and Development (ijtsrd), ISSN: 2456-6470, Volume-5 | Issue-1 , December 2020,
URL: https://www.ijtsrd.com/papers/ijtsrd38159.pdf
Paper URL : https://www.ijtsrd.com/medicine/other/38159/a-study-to-find-out-the-effect-of-arm-movement-through-sensory-based-game-on-improving-postural-control-in-spastic-diplegic-cerebral-palsy/abhirupa-chakraborty
ugcapprovedjournalswithlowpublicationfees
INTRODUCTION Poor control of trunk postural muscles and sensory disturbance is the key feature of children with cerebral palsy. These impairments affect the activities of daily living. It has been hypothesized that arm movement through sensory based game enhance proprioceptive and vestibular integration, resulting in improvement of spatial awareness, co contraction, postural stability and anticipatory motor or postural control.OBJECTIVE To enhance postural control following arm movement through sensory based game.DESIGN Pre test post test experimental designSETTING Occupational Therapy department, Swami Vivekanand National Institute of Rehabilitation Training and Research, Olatpur, Odisha, 754010PARTICIPANTS 30 children with spastic diplegic cerebral palsy randomly allocated into two groups each with 15 subjects in experimental group mean age=4.9 years and control group mean age=5.36 years . Baselines were collected for all subjects by using GMFCS, GMFM 88 and TCMS.INTERVENTION Subjects of both the group were provided therapy sessions for 45 minutes per day, 5 days in a week for 6 weeks. Both groups had received convensional occupational therapy for 45 minutes. The experimental group had received conventional occupational therapy for 15 minutes and sensory based game for 30 minutes. Sensory based game includes 5 games. They were intermittently structured according to sensory requirements. Post test measurement were assessed after 6 weeks.OUTCOME MEASURE TCMS,88GMFM,88 GMFCSRESULT From the statistical result of this study, it is seen that the subjects with spastic diplegic cerebral palsy improved in their GMFM and TCMS score on both the groups. However, the subjects in the experimental group have shown better effect than control group.CONCLUSION It can be concluded that conventional occupational therapy can include sensory based game which enhance active participation of children and ultimately increase motor control leads to postural control.
0 notes
Audio
IL SENTIERO RUVIDO
C F Bb C
Ter coragem para enfrentar o que não é brincadeira Atravessar os rios que desaguam na tristeza A vida não é fácil mas é importante voce sorrir Enxergar o que se pode e aquilo que não se vê
GmFC
Vá sorrir Fazer a sua história aqui Tropeços sempre haverão mas tente não ficar prostrado A vida as vezes é um trem descontrolado
C F Bb C
Voce pode até chorar mas o dia logo virá Tirando o breu da noite trazendo claridade Haverá beleza em seus olhos naquilo que acham feio Pois haverá em ti A compreensão pela dor
Paulo Marcos
3 notes
·
View notes
Text
12 Unexpected Ways Zelda Wall Decals Can Make Your Life Better | Zelda Wall Decals
Prime 2: Annihilate City!
101 Percent Items – In GMFC Compound, your declared to attestant a cutscene and again bang a chicken crate and accept the Missile Launcher. However, appropriate afore the “invisible wall” arch to actuate it, there is a cossack shaped formation. By jumping assimilate it, you will be propelled assimilate the ledge above, acceptance you to skip the activation of the cutscene and go beeline to the Missile Launcher. Afterwards accepting it and again activating the cutscene. The chicken crate will reappear with addition Missile Launcher. Accepting this and the actual 99 items in the bold will acquiesce you to accept 101 percent of the items at the end of the bold (your Missile calculation doesn’t go aloft 255).
Broken Sonic Locks in Main Research – Afterwards you action Aphotic Samus in Sanctuary Fortress and you access the Echo Visor, you accept to go to a allowance alleged Main Research. Aback you go there your cold is to conciliate 3 sonic locks in the room. However, if you abort 2 or beneath and leave the room, aback you appear aback and abort the actual locks the aperture that’s declared to accessible doesn’t open. The aperture will never accessible so your bold is ashore with no way to progress. This accessible annihilate wrecks your game.
Floaty Jump – This annihilate is activate in the Chykka bang-up fight. Aback breaking the aftermost fiber off the cocoon, accomplish abiding you are in the water. If you are in the baptize aback you breach the aftermost strand, afterwards the cutscene, you will be on land, but aback you jump you get an anti-gravity lift that lets you go abundantly far, and abundantly high. The bold still thinks you are in the baptize so your all-overs are like if you were in water. The disadvantage is, if you blow any water, the aftereffect wears off. Apparently, you charge be in aphotic baptize aback a cutscene occurs to actuate this, therefore, the Chykka action is the alone abode to actuate this.
Jump Guardian Trick – Afterwards entering the acumen pit, don’t access the ablaze apple in the average yet. Instead go about the allowance and jump up to a ablaze alarm to the appropriate of the door, and aim appear the blooming aperture beyond the room. Again activate battlefront in advanced of the Luminoth statue’s face and, if done correctly, your shots should be chock-full in midair by the jump guardian (he’s airy until the action begins). You can shoot him as abundant as you like and aback you alpha the action he will alpha with that abundant damage! (you can’t annihilate him afore the action begins but you can get him to the point area 1 attempt kills).
No accident aback falling into a pit – In the allowance alleged “Windchamber Gateway”, attending for a allotment of
12 Unexpected Ways Zelda Wall Decals Can Make Your Life Better | Zelda Wall Decals – zelda wall decals | Encouraged to help my own website, within this period I am going to demonstrate concerning keyword. And from now on, this is the initial impression:

calcomanía de Pared, Legend of Zelda Hylian Shield Gift Gaming Gamer Movie Video Game Cartel vinilo Kids Teen Boy sala Nursery recámara Wall Art Decor .. | zelda wall decals
What about impression above? can be that will wonderful???. if you think therefore, I’l t show you several image once again down below:
So, if you like to acquire all of these outstanding images regarding (12 Unexpected Ways Zelda Wall Decals Can Make Your Life Better | Zelda Wall Decals), simply click save button to save the pics to your computer. There’re available for download, if you love and wish to obtain it, simply click save badge on the page, and it will be directly saved to your laptop computer.} As a final point if you desire to receive unique and the latest photo related with (12 Unexpected Ways Zelda Wall Decals Can Make Your Life Better | Zelda Wall Decals), please follow us on google plus or book mark this website, we attempt our best to offer you regular up grade with all new and fresh images. We do hope you enjoy keeping right here. For most upgrades and recent news about (12 Unexpected Ways Zelda Wall Decals Can Make Your Life Better | Zelda Wall Decals) photos, please kindly follow us on tweets, path, Instagram and google plus, or you mark this page on bookmark area, We attempt to offer you up-date periodically with all new and fresh pics, like your browsing, and find the perfect for you.
Thanks for visiting our site, contentabove (12 Unexpected Ways Zelda Wall Decals Can Make Your Life Better | Zelda Wall Decals) published . Today we’re excited to declare we have discovered an awfullyinteresting nicheto be pointed out, namely (12 Unexpected Ways Zelda Wall Decals Can Make Your Life Better | Zelda Wall Decals) Lots of people searching for details about(12 Unexpected Ways Zelda Wall Decals Can Make Your Life Better | Zelda Wall Decals) and definitely one of them is you, is not it?

Zelda Glass Window Wall Decal Link Decal Sticker Shield Sword Windmaker Wall Decals Sticker Kids Bedroom Designs Zelda Mural Stickers, s12 – zelda wall decals | zelda wall decals

Legend of Zelda Wall Decal Gate of Time Vinyl Sticker Home Wall Art Decor (12zda) | eBay – zelda wall decals | zelda wall decals
Personalized Legend of Zelda Triforce Wall Decal (Removable and Replaceable) – zelda wall decals | zelda wall decals

Zelda Wind Waker: Boomerang Wall Decals by Nintendo – zelda wall decals | zelda wall decals

US $12.12 12% OFF|Legend of Zelda Wall Decal Sword Pattern Movie Wall Stickers Abstract Cartoon Home Decor For Kids Rooms Art Mural Design SYY712|wall .. | zelda wall decals

Hyrule Crest – Legend of Zelda – Wall Decal – zelda wall decals | zelda wall decals

Link™: The Legend of Zelda™ – Giant Officially Licensed Nintendo Removable Wall Decal – zelda wall decals | zelda wall decals

RoomMates Zelda: Ocarina Of Time 12D Peel And Stick Wall Decals – zelda wall decals | zelda wall decals

Zelda Stained Glass Wall Decals – zelda wall decals | zelda wall decals

The Legend of Zelda Wall Decal Video Game Vinyl Sticker Kids Playroom Decor Interior (12n) – zelda wall decals | zelda wall decals

Zelda Wall Decal Legend Of Zelda Poster Sign Emblem Vinyl Sticker Z Logo Master Sword Movie Decals Home Decor Living Room G12 – zelda wall decals | zelda wall decals
The post 12 Unexpected Ways Zelda Wall Decals Can Make Your Life Better | Zelda Wall Decals appeared first on Wallpaper Nifty.
from Wallpaper Nifty https://www.flowernifty.com/12-unexpected-ways-zelda-wall-decals-can-make-your-life-better-zelda-wall-decals/
0 notes
Photo

Tonight I am preparing for the two worst days of my career. We will say goodbye and honor a friend, a partner, a brother and a mentor. R.I.P. GMFC (at Hamtramck Police Dept) https://www.instagram.com/p/B8h7ty4HpBRsAj0J-T5o3LuI3yO8sG7zS_8D5A0/?igshid=843g1lkfgtjs
0 notes