#equine influenza transmission
Text
Molnupiravir Capsules 200 mg Understanding Its Uses and Benefits
Introduction
Molnupiravir, a ground-breaking antiviral drug, has recently attracted a lot of interest due to its potential to treat viral infections. Molnupiravir, which comes in 200 mg capsule form, is a potential strategy for treating a variety of viral infections. We will examine the advantages and applications of Molnupiravir capsules in this blog article, as well as how this drug may revolutionize the area of antiviral therapies.

Overview of Movfor Capsule
The investigational antiviral medication molnupiravir, sometimes referred to by its chemical name MK-4482/EIDD-2801, targets RNA viruses. It was primarily created to treat influenza, but it has attracted a lot of interest because of its potential application against other RNA viruses, such as coronaviruses. The medication is an oral prodrug that quickly breaks down into its active form, which prevents viral RNA from replicating.
Uses of Molnupiravir
About treating a variety of viral infections, molnupiravir has potential. Although clinical trials for several diseases are still ongoing, some possible applications are as follows:
Influenza: Molnupiravir was first created to treat influenza, and preliminary research indicates that it is effective in shortening the duration of symptoms and viral load in individuals with influenza A and B virus infections.
COVID-19: During the COVID-19 pandemic, molnupiravir received a lot of media attention. In individuals with mild to severe COVID-19 symptoms, preliminary trials show that it may be useful in lowering viral replication and shortening the length of sickness.
Molnupiravir has demonstrated action against some different RNA viruses, including respiratory syncytial virus (RSV), Venezuelan equine encephalitis virus (VEEV), and chikungunya virus, in addition to coronaviruses and influenza.
Molnupiravir is available in capsule form, making it simple and convenient to use by mouth.
Broad-Spectrum action: Molnupiravir exhibits action against some RNA viruses, suggesting the possibility of using it to treat diverse viral illnesses.
Early Treatment: Molnupiravir appears to be a promising early treatment option that might perhaps avert serious sickness and lower the likelihood of hospitalization.
Molnupiravir may aid in limiting viral transmission throughout populations by lowering viral load and minimizing the length of sickness.
Molnupiravir causes mistakes to be introduced into the viral RNA replication process to perform its antiviral effects. It is integrated into the developing viral RNA chain, causing alterations that obstruct effective replication and therefore lower viral load. For fast-changing RNA viruses that are prone to acquiring treatment resistance, this mechanism is very helpful.
Advantages and Possible Benefits
Several advantages and prospective advantages are provided by molnupiravir capsules:
Conclusion
200 mg molnupiravir capsules have the potential to completely transform antiviral therapy. With encouraging results against COVID-19 and influenza, this drug may become a crucial weapon in the battle against viral diseases. We eagerly anticipate more insights into the entire breadth of Molnupiravir's therapeutic effects when new data from current clinical trials become available.
For More Articles : - https://wakelet.com/wake/aTO5w1NghAa-v_3phbxKT
0 notes
Text
how is equine influenza spread?
Equine influenza is an exceptionally infectious influenza that spreads rapidly among horses. The good news is that it is rarely fatal in healthy horses. Zebras, jackasses and incapacitated steeds are not as fortunate and may capitulate to the infection. There are two sorts of the infection: Orthomyxovirus An/Equi-1 and Orthomyxovirus An/Equi-2. The last has caused pandemics in equine populaces and has turned out to being endemic in a few nations.

What If My Horse Has influenza?
FULL ARTICLE : https://theequines.blogspot.com/2019/01/how-is-equine-influenza-spread.html
#how is equine influenza spread#equine influenza#equine influenza causes#equine influenza transmission#equine influenza treatment#equine rhinopneumonitis influenza vaccine#equine influenza vaccine#what is equine influenza
0 notes
Text
Recent Mosquito Borne Diseases Rattled US
Any nuisance issue is irritating, yet mosquitoes are troubling in light of the fact that they can undermine your wellbeing.
Ongoing news reports about eastern equine encephalitis and West Nile infection may have you especially concerned. These startling sicknesses have one basic transporter: mosquitoes. You can't get them from someone else, yet one chomp from a tainted mosquito can be deadly.
Equipping yourself with the correct data and irritation security can help ensure you and your family.
Disease Transporters
Mosquitoes seemingly cause more human enduring than some other organic entity, executing more than 1,000,000 individuals consistently around the world. These bloodsucking irritations are maliciously compelling sickness transporters that can communicate diseases like intestinal sickness, dengue fever, Zika, and West Nile Infection by benefiting from the blood of a tainted bird, creature, or human, and afterward conveying the microorganism in their spit to their next dinner. Mosquitoes can likewise convey illnesses and parasites that mischief pets and domesticated animals, for example, heartworm in canines. That is on top of the less perilous, yet more normal mosquito-caused issue – red, irritated knocks that can make you insane.
Flare-ups Turned into a Viral
Eastern equine encephalitis (EEE) is the most recent mosquito-borne infection story in the news. Wellbeing authorities have detailed an uptick in instances of this uncommon, however conceivably lethal infection in focal Florida lately, and a solitary case in Massachusetts toward the beginning of August. Manifestations regularly seem four to 10 days after a mosquito chomp and start with an unexpected beginning of cerebral pain, high fever, chills, and heaving. Sometimes, side effects can advance to confusion, seizures, unconsciousness, and in around 33% of cases, passing. There is no particular treatment, and keeping in mind that immunization is accessible for ponies, there is none for people.
West Nile infection (WNV) is the main source of mosquito-borne sickness in the mainland US. In 2019, up until now, 128 instances of West Nile infection in 36 states have been accounted for to the Centers for Disease Control and Prevention (CDC). Luckily, a great many people tainted with WNV don't feel wiped out. Around 1 of every 5 individuals will create influenza-like manifestations; just 1 out of 150 build up a genuine sickness, which can be lethal. West Nile has been recognized in a wide range of kinds of mosquitoes.
Zika set off caution in 2015 when a flare-up hit focal and South America and the Caribbean. The vast majority tainted by Zika experience just gentle manifestations; many don't realize they're contaminated. In any case, the infection can prompt serious birth absconds, so it's especially troubling for ladies who are pregnant or intending to get pregnant. No neighborhood mosquito-borne Zika infection transmission has been accounted for in the mainland US over the most recent two years. Nonetheless, in the event that you are going outside of the mainland U.S., you ought to know about objections where Zika may represent a danger and play it safe. The CDC's online Voyagers' Wellbeing page offers explicit data.
Of all the mosquito-borne sicknesses, Malaria is the greatest executioner, for the most part among kids in sub-Saharan Africa. Mosquitoes communicate a parasite starting with one human then onto the next in regions where the sickness is predominant. Fortunately, jungle fever is treatable and not basic in the U.S. – around 1,700 cases are analyzed every year, except most include explorers from nations where jungle fever is far and wide.
If your properties and surroundings are exceedingly infested with Mosquitoes in NY, call "First Rate Solutions" a proficient Orange County Pest Control agency to root out mosquito issues.
1 note
·
View note
Text
Our Ten Most Popular Stories of 2020
https://sciencespies.com/nature/our-ten-most-popular-stories-of-2020/
Our Ten Most Popular Stories of 2020
SMITHSONIANMAG.COM |
Dec. 30, 2020, 7 a.m.
The year 2020 will go down in history as one of the most extraordinary in modern recollection. A devastating pandemic dominated conversations and our coverage, which detailed why the race for a coronavirus vaccine runs on horseshoe crab blood, explained how to avoid misinformation about Covid-19 and drew lessons from the past by examining diaries penned during the 1918 influenza pandemic. This summer, when a series of protests sparked an ongoing reckoning with systemic racism in the United States, we showed how myths about the past shape our present views on race and highlighted little-known stories about the lives and accomplishments of people of color. Toward the end of the year, amid one of the most bitterly divisive elections in recent history, we delved into the lengthy debate over mail-in voting and the origins of presidential concession speeches.
Despite the challenges posed by 2020, Americans still found reasons to celebrate: Ahead of the 100th anniversary of women’s suffrage, we profiled such pioneering figures as Geraldine Ferraro, the first woman nominated as vice president by a major party, and Fannie Lou Hamer, who fought to secure black voting rights. In the cultural sphere, the discovery of dozens of intact Egyptian coffins thrilled and amazed, as did the reemergence of a long-lost Jacob Lawrence painting. From murder hornets to Venice’s new inflatable floodgates, Catherine the Great and the Smithsonian’s new open-access platform, these were Smithsonian magazine’s top ten stories of 2020.
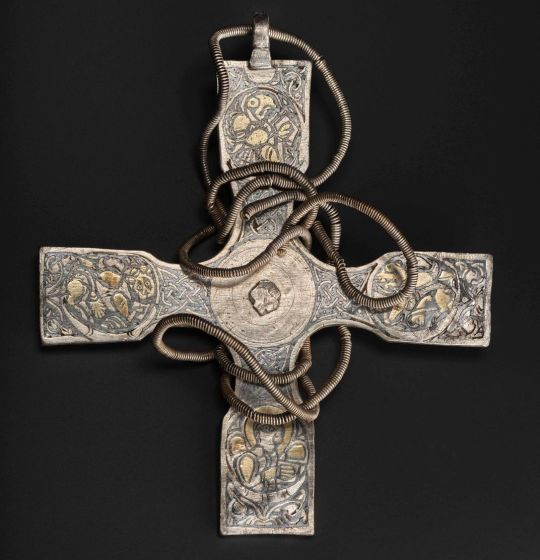
Our most popular story of 2020 underscored the value of skillful art restoration, presenting a welcome counter to the many botched conservation attempts reported in recent years. As the National Museum of Scotland announced this December, experts used a carved porcupine quill—a tool “sharp enough to remove … dirt yet soft enough not to damage the metalwork,” according to a statement—to clean an Anglo-Saxon cross for the first time in more than a millennium. The painstaking process revealed the silver artifact’s gold leaf adornments, as well as its intricate depictions of the four Gospel writers: Saint Matthew as a human, Saint Mark as a lion, Saint Luke as a calf and Saint John as an eagle. Per writer Nora McGreevy, the cross is one of around 100 objects included in the Galloway Hoard, a trove of Viking-era artifacts found by amateur treasure hunters in 2014.
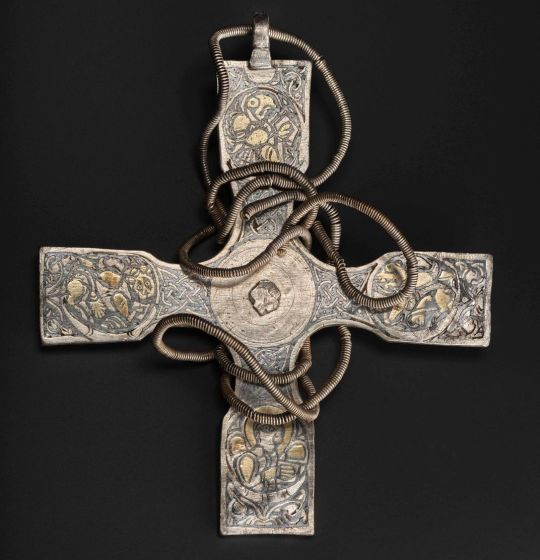
Curators used an improvised tool made of porcupine quill to gently clean the cross, which features engravings of the four Gospel writers.
(National Museums Scotland)
While most of England was on lockdown during the Covid-19 pandemic, archaeologist Matt Champion unwittingly unearthed more than 2,000 artifacts beneath the attic floorboards of Tudor-era Oxburgh Hall. Highlights of the trove included a 600-year-old parchment fragment still adorned with gold leaf and blue lettering, scraps of Tudor and Georgian silks, and pages torn from a 1568 copy of Catholic martyr John Fisher’s The Kynge’s Psalmes. Detailing the find in an August article, McGreevy noted that British nobleman Sir Edmund Bedingfeld commissioned the manor’s construction in 1482; his devoutly Catholic descendants may have used the religious objects found in the attic during secret masses held at a time when such services were outlawed.
In March, when the world was just beginning to understand the novel coronavirus, researchers learned that the SARS-CoV-2 virus—the pathogen that causes Covid-19—survives for days on glass and stainless steel but dies in a matter of hours if it lands on copper. (In later months, scientists would find that airborne transmission of the virus carries the greatest risk of infection, rather than touching contaminated surfaces.) The metal’s antimicrobial powers of copper are nothing new: As Michael G. Schmidt, a microbiologist and immunologist at the Medical University of South Carolina, told writer Jim Morrison this spring, “Copper is truly a gift from Mother Nature in that the human race has been using it for over eight millennia.” Crucially, copper doesn’t simply dispatch unwanted pathogens at an incredibly fast rate. Its bacteria-combating abilities also endure for long stretches of time. When Bill Keevil and his University of Southampton microbiology research team tested old railings at New York City’s Grand Central Terminal several years ago, for instance, they found that the copper worked “just like it did the day it was put in over 100 years ago.”

The Asian giant hornet, the world’s largest hornet, was sighted in North America for the first time.
(Washington State Dept. of Agriculture)
Another unwelcome surprise of 2020 was the rise of the Asian giant hornet, more infamously known as the “murder hornet” due to its ability to massacre entire hives of bees within hours. The first confirmed sightings of the insects in North America occurred in late 2019, but as Floyd Shockley, entomology collections manager at the Smithsonian’s National Museum of Natural History, pointed out in May, observers need not panic, as the hornets don’t realistically pose a threat to human health. Honey bees are more susceptible to the predators, but as Shockley said, “[I]s it going to be global devastation? No.” Still, it’s worth noting that officials in Washington state have since found and eradicated a nest thought to contain about 200 queens. Left unchecked, each of these hornets could have flown off and started a colony of its own. Efforts to contain the invasive species are ongoing.
In October, an engineering feat saved Venice from flooding not once, but twice. The barrier system of 78 giant, inflatable yellow floodgates—known as Mose—can currently be deployed to protect the Italian city from tides measuring up to three-and-a-half feet high. Upon its completion next year, Mose will be able to protect against tides of up to four feet. The floodgates’ installation follows the declaration of a state of emergency in Venice. Last year, the city experienced its worst floods in 50 years, sustaining more than $1 billion in damages and leaving parts of the metropolis under six feet of water. Built on muddy lagoons, Venice battles both a sinking foundation and rising sea levels. Despite the floodgates’ current success, some environmentalists argue that the barriers aren’t a sustainable solution, as they seal off the lagoon entirely, depleting the water’s oxygen and preventing pollution from flowing out.

While Hegra is being promoted to tourists for the first time, the story that still seems to get lost is that of the ancient empire responsible for its existence.
(Royal Commission for AlUla)
Desert-dwelling nomads turned master merchants, the Nabataeans controlled a broad swath of land between the Euphrates River and the Red Sea for some 500 years. But in the millennia following the civilization’s fall in the first century A.D., its culture was almost “lost entirely,” wrote Lauren Keith in November. Today, little written documentation of the Nabataeans survives; instead, archaeologists must draw on clues hidden within the empire’s ruins: namely, two monumental cities carved out of rock. One of these twin settlements—the “Rose City” of Petra in southern Jordan—attracts nearly one million visitors each year. But its sister city of Hegra remains relatively obscure—a fact that Saudi Arabia hopes to change as it shifts focus from oil to tourism. As several scholars told Keith, the Middle Eastern nation’s renewed marketing push represents a chance to learn more about the enigmatic culture. “[Visiting] should evoke in any good tourist with any kind of intellectual curiosity,” said David Graf, a Nabataean specialist, archeologist and professor at the University of Miami. “[W]ho produced these tombs? Who are the people who created Hegra? Where did they come from? How long were they here? To have the context of Hegra is very important.”
The May killing of George Floyd spurred nationwide protests against systemic injustice, acting as a call to action for the reformation of the U.S.’ treatment of black people. As Smithsonian Secretary Lonnie G. Bunch wrote in a short essay published in June, Floyd’s death in police custody forced the country to “confront the reality that, despite gains made in the past 50 years, we are still a nation riven by inequality and racial division.” To reflect this pivotal moment, Smithsonian magazine compiled a collection of resources “designed to foster an equal society, encourage commitment to unbiased choices and promote antiracism in all aspects of life,” according to assistant digital editor Meilan Solly. The resources are organized into six categories: historical context, systemic inequality, anti-black violence, protest, intersectionality, and allyship and education.
Human relationships can be difficult, but at least they don’t involve copulating until your inner organs fail. Yes, you read that correctly—death is the unfortunate fate for the male antechinus, a pint-sized marsupial that literally fornicates until it drops dead. Take similar comfort in the fact that humans don’t need to drink urine to start a relationship, as is the case with giraffes, nor inseminate each other via open wounds, as bed bugs do.
youtube
Today, stories of Catherine the Great’s salacious, equine love affairs dominate her legacy. But the reality of the Russian czarina’s life was far more nuanced. Ahead of the release of Hulu’s “The Great,” we explored Catherine’s 30-year reign, from her usurpation of power to her championing of Enlightenment ideals, early support of vaccination and myriad accomplishments in the cultural sphere. As Meilan Solly wrote in May, “Catherine was a woman of contradictions whose brazen exploits have long overshadowed the accomplishments that won her ‘the Great’ moniker in the first place.
For the first time in the 174-year history of the Smithsonian Institution, the organization released 2.8 million images from across all 19 museums, 9 research centers, libraries, archives and the National Zoo into the public domain. This initial release represents just two percent of the Smithsonian’s total collection, which boasts 155 million items and counting. It was part of an ongoing effort to digitize—and democratize—the Institution’s collections.
• An excerpt from Jennet Conant’s new book, The Great Secret: The Classified World War II Disaster That Launched the War on Cancer, in which she details how an investigation into a devastating Allied bombing of an Italian coastal town eventually led to an innovation in cancer treatment.
• A time-capsule story from the end of March about how and when we thought the pandemic might end. We were too optimistic about how long Americans would need to “flatten the curve,” and unmentioned in the story was how soon a vaccine would be developed.
• Another entry in our “True History of” series that looked at Tom Hanks’ World War II film from earlier this year, Greyhound
• An exploration of new research that rewrites the demise of Doggerland, a prehistoric land bridge between Britain and Europe
#Nature
2 notes
·
View notes
Text
Animal Vaccines Market will touch a new level in upcoming year 2027

Market Highlights
The surging incidences of livestock diseases are likely to favor the market growth. Vaccines help to make animals disease-immune for a specific disease. In terms of biology, vaccination against a certain pathogen mimics the development of naturally acquired immunity by the inoculation of non-pathogenic components of that certain pathogen. Veterinary vaccines are generally used to treat and prevent animal diseases. The market is likely to witness an upsurge owing to the rising spending on companion animals worldwide.
The global animal vaccines market Size is expected to have a market value of USD 13,209.14 million by 2027.
Market Potential and Pitfalls
The surging adoption of pet across the globe and the rising animal related diseases are the top factors encouraging the market growth during the appraisal period. The market players across the world are thus actively working in order to introduce more advanced animal vaccines in the market which is likely to influence its growth. For instance, Boehringer Ingelheim launched two swine vaccines in 2015 in the market against Porcine Reproductive and Respiratory Syndrome. Factors like rising prevalence of livestock diseases, growing adoption of companion animals, technological advancements in animal vaccines, and surging initiatives by the government are contributing to the growth of the market.
Animal vaccines enables controlling the transmission diseases, thereby providing protection to both the animal and human health, which is important considering the public dependency on animals. Animals serve as an important food source, milk, meat, protein, and other commercial products like wool and leather. Some of the most commonly used veterinary vaccines comprises foot & mouth diseases vaccines, rabies vaccines, and equine influenza virus vaccines, which help to prevent the transmission of infectious agents. With the continuous development of vaccines, the market is likely to flourishing. Moreover, the surging investment for R&D of vaccines, which impedes the growth of antibiotic-resistant organism, enhances the animal vaccines market growth.
Segment Analysis
The global animal marketing definition has been segmented on the basis of technology, type, composition, and indications.
By mode of type, the global animal vaccines market has been segmented into poultry vaccines, static porcine vaccines, companion animal vaccines, livestock vaccines, aquaculture vaccines, and others. Among these, the companion animal vaccines are likely to gain to gain prominence in the coming years owing to the increased awareness regarding companion animal vaccination, rising number of pets, surging incidences of zoonotic diseases in human beings, and growing pet ownership.
By mode of technology, the global animal vaccines market has been segmented into inactivated vaccines, live attenuated vaccines, recombinant vaccines, toxoid vaccines, and others. Among these, the live attenuated vaccines are estimated to expand at a significant rate owing to the ease of administration along with the long-term immunity offered by these vaccines.
By mode of indications, the global animal vaccines market has been segmented into parvovirus, foot & mouth disease, reproductive & respiratory syndrome, distemper, and others.
By mode of composition, the global animal vaccines market has been segmented into mono vaccine and combination vaccine.
Regional Analysis
Geographically, the animal vaccines market span across regions namely, Europe, America, Asia-Pacific and the Middle East & Africa.
Considering the global scenario, the American region is anticipated to dominate the global market due to the presence of prominent market players and increased pet adoption in developed nations like Canada and the U.S. As per the American Society for the Prevention of Cruelty to Animals, around 6.5 million companion animals enter the animal shelter every year. North America is a prominent economy, generating the maximum revenue. The rising consumption of milk and meat, the increased awareness associated with the benefits of using animal vaccines, and high adoption of companion animals are influencing the market in this region.
The European region is likely to occupy the second spot in the global market owing to the surging investments on research and development. For instance, Boehringer Ingelheim declared to reinforce its leading position in the veterinary market in 2018, with almost 70 million euro investment in the biological production and R&D activities.
The Asia Pacific region is estimated to expand at the fastest rate in the global market. The growth has been ascribed to the surging awareness regarding animal health which drives the regional markets. For instance, at the 5th Global Animal Health Conference in 2016, HealthforAnimals association called for greater cooperation among the national governments in order to improve the market access for veterinary medicines.
Competitive Dashboard:
Some of the key players operating in the animal vaccines market are Boehringer Ingelheim International GmbH (Germany), Zoetis Inc. (US), Ceva Santé Animale (France), Merck & Co., Inc. (US), Elanco Animal Health Incorporated (US), Virbac (France), Phibro Animal Health Corporation (US), Hipra (Spain), Biogénesis Bagó S.A.(Argentina), Neogen Corporation (US).
About Market Research Future:
At Market Research Future (MRFR), we enable our customers to unravel the complexity of various industries through our Cooked Research Report (CRR), Half-Cooked Research Reports (HCRR), & Consulting Services. MRFR team have supreme objective to provide the optimum quality market research and intelligence services to our clients.
Contact us:
Market Research Future (part of Wantstats Research and Media Private Limited),
99 Hudson Street, 5Th Floor,
New York, New York 10013
United States of America
+1 628 258 0071
Email: [email protected]
0 notes
Link
The“Animal Vaccines Market ”reportfocuses on the market status, future forecast, growth opportunities, market trends and leading players.
0 notes
Link
0 notes
Link
0 notes
Text
Animal Vaccines Market To Reach A New Threshold of Growth By 2025
Animal Vaccines Market is expected to reach USD 12861.68 Million by 2024 with a CAGR of 5.9% over the forecast period.
Veterinary/Animal Vaccines Market : Growing awareness of animal health, Technological innovations and increasing incidence of zoonotic diseases transmitted through contaminated foodare some key drivers for Global Veterinary/Animal Vaccines Market.
Scope of Veterinary/Animal Vaccines Market Reports – Veterinary/Animal vaccines are used for improvement of immunity of animals by sanitizing animal health which avoids transmission of diseases fromboth domestic as well as wildlife animals to humans.Veterinary/Animal vaccines are the most productive product segment of focus for Veterinary/Animal drug manufacturers.The vaccines can be administered intramuscularly i.e., into the muscleor subcutaneously i.e., under the skin to animal. Also the Veterinary/Animal vaccines improve livestock production in a very cost effective manner. The mainpurpose of Veterinary/Animal vaccines is to improve the health and welfare of pet animals, increase production of livestock in a cost-effective manner. The final fruitfulconclusion of vaccine research and development is the production of a product that will be available in the market or that will be used in the field to attain desired results.
The Veterinary/Animal vaccines have been produced to kill the viral, bacterial, protozoal and multicellular pathogens. The continuouscollaboration between animals and human researchers and health experts will be of foremost importance for adapting new technologies, providing animal models of disease and challenging new and emerging infectious diseases.Generally, Veterinary/Animal vaccines contain those for rabies, E. coli, distemper, hepatitis rotavirus, parvovirus, brucellosis and pinkeye. Many diseases such as foot-and-mouth disease and influenza adversely affect livestock across the globe. An Economic damage due to death of livestock issubstantial as it affects the supply of dairy products, meat and other poultry products.
Veterinary/Animal biologics are governed by the U.S. Department of Agriculture (USDA) Center for Veterinary/Animal Biologics. To fight against growingoccurrence of possiblylethal Veterinary/Animal diseases there is a significant rise in demand for combination vaccines that allow for higher accuracy and better stability of the finished product. Regulations are also concentrating on improving stability, consistency and quality of various animal vaccines. Maintaining the quality of production of Veterinary/Animal vaccines will avoid risk of adverse effects.
Global Veterinary/Animal Vaccines Market has been segmented on the basis of Type, Disease, Technology and Geography. On the basis of Type Global Veterinary/Animal Vaccines Market is classified into Porcine Vaccines, Poultry Vaccines, Livestock Vaccines, Companion Animal Vaccines, Aquaculture Vaccine, Equine Vaccines, Pig Vaccines,Cattle Vaccines and others.On the basis of Disease Global Veterinary/Animal Vaccines Market is classified into Porcinedisease, Poultry disease, Livestock disease, Companion Animal disease, Aquaculture disease and others.On the basis of Technology Global Veterinary/Animal Vaccines Market is classified into inactivated vaccines, live attenuated vaccines, subunit vaccines, toxoid vaccines, recombinant vaccines, DNA vaccines,conjugate vaccinesand others.
The regions covered in Global Veterinary/Animal Vaccines Market report are North America, Europe, Asia-Pacific and Rest of the World. On the basis of country level, Global Melanoma Drug Market sub divided in to U.S., Mexico, Canada, U.K., France, Germany, Italy, China, Japan, India, South East Asia, GCC, Africa, etc.
Key Players for Global Veterinary/Animal Vaccines Market Reports – Global Veterinary/Animal Vaccines Market reports cover prominent players like Biogenesis Bago, Boehringer Ingelheim, CevaAnimal Health, Inc., China Animal Husbandry, Hester, Hipra, IDT Biologika, Jinyu Bio-Technology, Merck Animal Health, Phibro Animal Health, Tianjin Ringpu, Vetoquinol, Virbac, Zoetis Inc.(Pfizer), Bayer Healthcare, Merial (Animal Health Division of Sanofi),Virbac, Bimeda Inc.,Eli Lily and Company, Indian Immunologicals Ltd.,Bioniche Animal Health, Brilliant Bio Pharma Ltd., Nisseiken Co., Ltd., C.A. Laboratorios Asociados (CALA), Dollvet,Avimex Animal Health, Zhaoqing Dahua Agriculture Bio-Pharm Co., Ltd.,Genera Inc., VETERINA Animal Health Ltd., INDOVAX Pvt. Ltd. and others.
Global Veterinary/Animal Vaccines Market Dynamics – Growing livestock population and increased acceptance of companion animals, increasingoccurrence of zoonotic diseases, initiatives by various government agencies, animal associations and leading players and the introduction of new types of vaccines are main key drivers that drives Global Veterinary/Animal Vaccines Market. Moreover, Growing Costs for the Storage of Vaccines and prevalence of chronic disease of animals arerestraints that hinder the growth of Global Veterinary/Animal Vaccines Market. Technological Revolution, growing awareness of Animal Health in Developing Countries,growing consumption of vegetarian food in major economies due to greater risk of obesity and other chronic disorders. Similarly, rising demand for milk, eggs, meat & animal protein and would denote the considerable opportunity in forecast periodfor Global Veterinary/Animal Vaccines Market.
Market Segmentation
By Type
Porcine Vaccines, Poultry Vaccines, Livestock Vaccines, Companion Animal Vaccines, Aquaculture Vaccine, Equine Vaccines, Pig Vaccines, Cattle Vaccines, Other
By Disease
Porcine disease, Poultry disease, Livestock disease, Companion Animal disease, Aquaculture disease, Other
By Technology
Inactivated Vaccines, Live Attenuated Vaccines, Subunit Vaccines, Toxoid Vaccines, Recombinant Vaccines, DNA Vaccines, Conjugate Vaccines, Others
By Region:
North America (US., Canada), Europe (UK., France, Germany, Italy), Asia Pacific (China, Japan, India, Southeast Asia), Latin America (Brazil, Mexico), Middle East and Africa (GCC, Africa, Rest of Middle East and Africa)
About us: Brandessence Market Research and Consulting Pvt. ltd.
Brandessence market research publishes market research reports & business insights produced by highly qualified and experienced industry analysts. Our research reports are available in a wide range of industry verticals including aviation, food & beverage, healthcare, ICT, Construction, Chemicals and lot more. Brand Essence Market Research report will be best fit for senior executives, business development managers, marketing managers, consultants, CEOs, CIOs, COOs, and Directors, governments, agencies, organizations and Ph.D. Students. We have a delivery center in Pune, India and our sales office is in London.
Contact us at: +44-2038074155 or mail us at [email protected]
0 notes
Text
Dog Flu: What Pet Parents Need To Know

Every year, many humans rush to get their flu shot in hopes of staying clear of the crippling virus. If you’ve ever had it, you can probably still remember the horrible body aches, fever, coughing, and overall feeling of yuck! Well, did you know our canine kids can be attacked by a similar virus? Read on to find out the causes and symptoms of dog flu. Plus, scroll down to the bottom for a quick overview of the recent 2017 outbreak.
A Quick Overview Of Dog Flu & The Symptoms
The canine influenza virus—more commonly referred to as the dog flu—is a highly contagious virus that causes a respiratory infection in dogs. Symptoms include coughing, sneezing, nasal discharge, lethargy, and loss of appetite. Dogs with severe cases can also develop a high fever and clinical signs of pneumonia.
While most dogs recover in about 2-3 weeks, the dog flu can be deadly—young, senior, and immunosuppressed dogs are at the highest risk. Fatality rates are less than 10%, according to the Texas A&M Veterinary Medical Diagnostic Laboratory.
The Background
In the United States, the canine influenza virus has been caused by two strains—H3N8 and H3N2.
H3N8 – This was the first strain reported in the United States in 2004. Reports show this strain is closely related to the virus that causes equine influenza.
H3N2 – Word of this strain spread in 2015 when an outbreak of dog flu started in Chicago. Experts say this strain was almost genetically identical to a strain previously reported in Korea, China, and Thailand.
How It Spreads
The dog flu is very contagious. In fact, veterinarians say if a dog comes into contact with the dog flu they will likely catch it. This virus is spread by direct contact with a sick dog, a human carrier, or a contaminated environment.
Environmental factors can include kennel surfaces, food bowls, water bowls, toys, beds, and crates. If an infected dog rides in a car or comes in contact with your clothing, they too can become infected. Experts say the virus is easily killed, though, by most disinfectants. So if you suspect your dog is sick wash everything—from your dog’s belongings to your own!
Can Humans Catch Dog Flu?
According to the Center For Disease Control and Prevention:
“To date, there is no evidence of transmission of canine influenza viruses from dogs to people and there has not been a single reported case of human infection with a canine influenza virus. However, influenza viruses are constantly changing and it is possible for a virus to change so that it could infect humans and spread easily between humans.”
While canine to human transmission poses little to no threat at this time, the CDC and its partners continue to monitor it.
Treatment
Although there is no cure for the dog flu, your vet will give supportive care. Just like when a human gets the flu, your pooch will need lots of rest and fluids. If he gets a secondary bacterial infection, the vet will likely give him an antibiotic. If you suspect your pooch has dog flu, don’t self-diagnose him. It’s very important that you see your vet for a medical exam to confirm the diagnosis and rule out other serious illnesses such as kennel cough, pneumonia, heart disease, etc., which can present with similar symptoms.
What Dog Parents Need To Know About The Latest 2017 Outbreak
This latest outbreak is caused by the H3N2 strain and is making its way across the country with reports in North Carolina, South Carolina, Florida, Georgia, Tennessee, Kentucky, Texas, and Illinois. *At the time this article was published.
There is a vaccine that can protect your pooch against the dog flu. Talk to your vet to see if their office carries it and if your dog would be a good candidate.
If you notice your dog coughing (or showing any of the symptoms mentioned above), take him to the vet immediately to get tested for H3N2.
0 notes
Text
Vets, farmers, and zookeepers can help prevent the next pandemic
There have been multiple confirmed cases of COVID-19 in tigers at New York City's Bronx Zoo. Scientists there are now researching the origins of the big cats' infection. (A G/Unsplash/)
Lynne Peeples writes about science, health, and the environment from her home office in Seattle. Her work has also appeared in Scientific American, Reuters, Popular Science, Environmental Health News, and Audubon, among other publications. This story originally featured on Undark.
Nadia began coughing on March 27. The 4-year-old Malayan tiger’s keepers at the Bronx Zoo in New York City also noticed she wasn’t finishing her daily allotment of raw meat. Concerned, they called in Paul Calle, the zoo’s head veterinarian.
The team immobilized and anesthetized Nadia, so she could be put through a series of X-rays, ultrasounds, and routine blood work to look for known causes of respiratory disease in cats. “Since New York City is the epicenter for COVID in the US,” says Calle, “we wanted to make sure we checked her for that, too.”
On April 5, the zoo reported that Nadia had been infected by SARS-CoV-2, the virus that causes COVID-19. Over the course of the next week, three other tigers and three lions at the zoo also began showing similar symptoms. The sick cats were later tested, along with another 8-year-old male Amur tiger named Alden, who hadn’t been showing any symptoms. Every test came back positive, according to a statement released by the zoo on April 22. All eight cats are now recovering well, and “only an occasional cough is heard,” Calle says.
Officials think that an asymptomatic zoo worker carrying the virus probably infected the animals. “People and animals and the environment are all closely linked and influence what happens to each other,” says Calle.
This is far from the first time, and certainly won’t be the last, that an infectious disease has bounced between humans and other animals. Evidence suggests that COVID-19 likely originated in a bat, possibly jumped to a pangolin—which looks like a scaly anteater—and then infected a human, maybe at a live animal market in Wuhan, China. Globally, an estimated 75 percent of newly appearing infectious diseases are “zoonotic” like this, meaning they can pass from non-human animals to people. Infectious-disease experts warn that nature harbors more than a million undiscovered viruses.
The animals we keep as pets can be part of the transmission process, too. Exotic pet rodents were implicated as the likely source of an outbreak of monkeypox in the Midwest in 2003. Pigs, obviously, spawned the 2009 swine flu pandemic. And, last month, the U.S. Centers for Disease Control and Prevention and the Department of Agriculture confirmed that two pet cats in New York had tested positive for SARS-CoV-2. A pug in North Carolina named Winston was also added to the list in late April.
Recognition of the link between humans and other animals for COVID-19 is driving the push to ban China’s live animal markets, which pose a high risk for contagion. And animal health expertise could help prevent outbreaks in other ways, some scientists say. For example, greater animal surveillance could detect new diseases earlier and stop them from being passed to humans. And techniques for controlling outbreaks in livestock, such as randomized surveillance strategies, could also improve efforts to limit the spread of disease in human populations.
Yet despite being recognized as useful, the field of animal health has long been siloed away from human medicine. Veterinarians as well as wildlife biologists, livestock farmers, and zookeepers remain a largely untapped resource for combatting diseases that threaten people. “There is still a very traditional divide among disciplines,” says Jon Epstein, a wildlife veterinarian and disease ecologist for the EcoHealth Alliance in New York. “We haven’t removed these barriers yet.”
That’s not to say that experts haven’t been trying. But progress in getting authorities to see the connectedness of human and animal health has been slow—and in some instances in recent decades, has even gone backwards.
“It’s time that we stopped using humans as sentinels of animal diseases,” says Joe Annelli, the executive vice president of the National Association of Federal Veterinarians and formerly with the USDA. Instead, he said, we should be aiming to identify diseases in other animals as early as possible, when there’s still a chance of preventing them from spreading to humans.
Nearly 20 years ago, the Bronx Zoo was in the spotlight as another contagion crept among the city’s people and non-human animals.
It was the summer of 1999, and a strange disease that caused weakness and confusion had begun popping up among dozens of New Yorkers. Meanwhile, dead crows had started landing on the zoo’s grounds. Then came casualties among captive species: Chilean flamingos, laughing gulls, a snowy owl, and a bald eagle named Clementine.
Clementine was the zoo’s mascot. “She looked perfectly fine and then, boom, she dropped dead,” says Tracey McNamara, then the chief veterinary pathologist at the zoo. Her necropsy of Clementine—standard procedure for any death at an accredited zoo in the US—showed the worst brain inflammation in a bird that McNamara had ever seen. Worried that her surgical mask wasn’t enough protection against whatever had killed the eagle, McNamara went home that night and wrote her will.
She also went on with her detective work, taking advantage of what she called “built-in sentinels” of disease naturally found at a zoo. The CDC, at the time, suspected a brain disease called Saint Louis encephalitis. But McNamara knew that this disease doesn’t typically harm birds. Inflammation in bird brains, she noted, instead suggested one of three usual suspects in the U.S. The first was eastern equine encephalitis. Emus are known to be particularly sensitive to this virus, yet the zoo’s emu flock showed no signs of sickness. That left the other two possibilities: virulent Newcastle disease and highly pathogenic avian influenza. Both of these affect chickens, and the petting zoo was full of healthy birds.
“That’s when I knew I was dealing with something unknown to veterinary medicine,” says McNamara, now a professor of pathology at Western University of Health Sciences in Pomona, California.
While the CDC initially dismissed McNamara’s suggestion that the same disease might be impacting both people and birds, the agency eventually came around. Tests weeks later revealed that New York was home to the first cases of West Nile virus ever reported in the Western hemisphere. And, as the U.S. General Accounting Office would report in September 2000, the animal infections preceded the first human cases by at least one or two months. “The West Nile events illustrate the value of communication between public and animal health communities,” the GAO wrote.
As this mosquito-borne disease swept from New York across the US, none of the traditional means of surveillance—tests of mosquito pools or chicken flocks—proved to be predictive of human risks. So McNamara pushed for the launch of a nationwide surveillance network across zoos, suggesting it could bolster the CDC’s power to prevent outbreaks. The agency was convinced. The zoo network went live and, between 2001 and 2006, nearly 180 zoos and other wildlife institutions submitted samples.
“We hoped that this was the beginning of sustainable zoonotic disease surveillance in urban centers,” says McNamara. “Every major city has a zoo. Every zoo has a spectrum of the animal kingdom, some of which are guaranteed to be susceptible to whatever new virus pops up.”
But efforts to secure continued funding—let alone money to expand the program beyond West Nile virus—were all denied.
Donald Noah, a veterinary epidemiologist at Lincoln Memorial University in Harrogate, Tennessee, was working with the U.S. Department of Homeland Security when McNamara’s team reached out to his agency for financial support. He lamented not being able to convince senior leadership to oblige. “Hopefully, given the situation now, there is a change in awareness and more realization of the importance,” Noah says.
Pets, wildlife, livestock, and zoo animals can all serve as early warning signs of an emergent threat to humans. When wildlife biologists notice squirrels lying around dead, for example, it could be an indication of the plague. “Whether it is plague or hantavirus or rabies—or now COVID-19—viruses may be circulating for an unknown period of time in an animal reservoir species and then all of a sudden became apparent in humans,” says Noah.
Spotting signs of disease in bats or an intermediary animal, such as pangolins, may have warned officials of the threat of COVID-19 before it went pandemic, notes Victoria Brookes, a zoonotic disease expert at Charles Sturt University in Wagga Wagga, Australia.
“We’re always looking at timeliness,” says Brookes, who is helping to launch a “disease detective” training program for animal workers across Southeast Asia and Oceania that will support the development of local surveillance systems to detect diseases before they spawn an outbreak.
Annelli underscored the need for such surveillance: “We put all this money and work into identifying the first person to have a particular disease, but we’ve spent nothing on identifying that disease in the animal population and working to eliminate it before it continues to infect people,” he says.
But if a sick animal is not of economic value, then testing for and reporting any illness remains especially difficult. “There is still no federal agency that has jurisdiction over surveillance of zoo animals, or dogs and cats,” adds McNamara. “We have a gigantic species gap in our biosurveillance efforts in the US.”
Dozens of stray cats were infected by bird flu during a small outbreak in New York City in 2017. (Ryne Anderson/Unsplash/)
For instance, towards the end of 2016, at an animal shelter in East Harlem about 6 miles from the Bronx Zoo, an orange-and-white cat named Mimi developed a respiratory infection, became very sick, and had to be euthanized. Cats in multiple other crowded New York shelters started falling ill over the following weeks. An attending veterinarian got sick as well.
The culprit turned out to be a strain of bird flu, H7N2, never before seen in cats. By the time a private foundation stepped in to cover the costs of testing and quarantining the potentially affected animals, about 1,000 felines had already been adopted out to families throughout the greater metropolitan area.
Sandra Newbury, director of the Shelter Medicine Program at the University of Wisconsin-Madison, worked with the shelters to contain the virus. Thanks to the private donor, they were able to offer free testing and medical care for the adopted cats, eventually isolating hundreds that had been infected. “We were really aggressive in our efforts to not let it spread,” Newbury says. She believes identifying such a large number of infected animals and quarantining them allowed the authorities to eradicate the virus. According to Newbury, no positive tests have been reported since March 2017.
“We were really very lucky. This could’ve turned into a new virus of cats,” says Newbury, noting the contrast with what’s playing out today. “A virus spreads more easily when you don’t know that it’s there. That’s what we’re seeing now with COVID-19 in humans. There’s not enough testing.”
While it would be impossible to identify every possible disease in non-human animals, notes Annelli, far more could be done to test for diseases known to occasionally spill over to humans, such as Ebola. He also believes we should be regularly sampling animals at live markets for influenza and coronaviruses, and testing wildlife in natural areas where they might closely overlap with domestic animals and people—such as deforested lands—to see how diseases evolve over time. The commingling of species provides an optimal environment for viruses to mutate to the point that they could infect people.
“When multiple species are mixed together that are not usually next to each other, then you can get all kinds of things popping up,” says Annelli. The 2003 monkeypox outbreak is another case in point: Gambian rats caught in Africa were shipped to the U.S. and ended up being housed next to prairie dogs, a species they had never been in close contact with in the wild. Once infected, prairie dogs can fairly easily transmit the virus to people. And evidence suggests they did.
Experts underscore the importance of finding not only the species that spread viruses in the first place, but also which animals may maintain them in the future. Even if control measures manage to curb COVID-19 in human populations, for example, might the virus simply hide out in domestic cats, local bats, or another non-human species, ready to re-emerge later? “That’s an open question that needs to be examined,” says Epstein.
A Chinese study published in March identified several species that SARS-CoV-2 might be able to infect, including cats, cows, pigeons, and pangolins. Another study underway in Germany is exposing different animals to the virus in hopes of deciphering whether it could infect as well as replicate within certain species—and so potentially sustain itself there. Early findings reported in April suggest that fruit bats and ferrets are susceptible, while pigs and chickens are not.
But just because an animal can be infected doesn’t necessarily mean it can spread the disease to others. Thankfully, the flu that affected the shelter cats turned out to be fairly mild and minimally transmissible to humans. “If this virus had been as dangerous and as virulent as the pandemic flu of 1918, then the battle would have already been lost,” says McNamara.
“We dodged a bullet, she adds. “But there’s no guarantee we’ll be as lucky the next time.”
In 2007, the bluetongue virus—a disease spread by midge bites—began to sweep through herds of sheep and cattle across Europe. Johanne Ellis-Iversen was serving as the veterinary adviser for the U.K.’s Department for Environment, Food, and Rural Affairs towards the end of the outbreak and as it was officially declared over in 2011. The U.K. has seen a number of major outbreaks of disease in food animals in recent decades, including bovine spongiform encephalopathy (aka “mad cow disease”) and foot-and-mouth disease. As a result, says Ellis-Iversen, it has a very structured and effective response for fighting epidemics among livestock.
In agricultural animal health, “outbreaks of exotic disease in well-regulated countries rarely get big because we identify and control them right away,” says Ellis-Iversen, now a senior adviser and veterinary epidemiologist at the National Food Institute at the Technical University of Denmark. She is also the co-author of a paper published in late March that describes how veterinary surveillance methods could be adapted to randomly survey human populations for COVID-19.
When dealing with infection among livestock, before a decision is made to lift control measures or reopen exports, it’s standard procedure to test animals at random to estimate the disease spread. Ellis-Iversen’s team did just that to prove the country was free of bluetongue. “We want to know what is happening in a population, not just the herds identified as ill,” she says.
In the case of COVID-19, some countries and US states have begun lifting social distancing and containment measures. Their typical plan: Keep an eye out for the re-emergence of infections and then re-enact control measures as necessary. But Ellis-Iversen cautions that if you only pick up infections by testing individuals admitted to hospital or by measuring deaths, then you miss a lot of valuable information—conducting monitoring so far down the line means anything done in response will have a delayed impact. “If officials see that hospital cases are creeping towards a threshold, then it would be another week or two before they can actually reduce the number going into the hospital,” she says.
“We’re wondering why public health isn’t looking more to using the experience from animal health,” adds Ellis-Iversen. Representative surveys of the population—like those used for livestock—could inform policy making, including outbreak control and exit strategies, she said.
While randomized surveys are not a replacement for other public health tools, such as identifying people who are ill and tracing who they might have infected, Ellis-Iversen believes they could provide some “extremely useful” data for deciding on control measures. Recognizing that some countries have limited testing capacity, she also notes that samples need not be large to provide valuable information. “You don’t need to test 10,000 people,” says Ellis-Iversen. “We just need to consider how we select the people we test.”
Germany is using just such a technique for human populations right now, in the hope that the data will inform what restrictions can be loosened without a resurgence of infections. Ellis-Iversen suggests that while randomized surveys are “used occasionally in public health,” they tend to be conducted more for studies rather than as ongoing surveillance for decision making. “It will be interesting to see the results,” says Ellis-Iversen. “If they show something unexpected, I am sure it will be food for thought around the world.”
Days before Nadia, the Bronx Zoo tiger, was diagnosed with COVID-19, the Wildlife Conservation Society issued a statement urging the closure of live animal markets. The international organization, which happens to be based at the Bronx Zoo, is among several environmental groups, politicians, and celebrities now advocating for a ban. Live animal markets were also implicated in the 2003 SARS outbreak.
“These emerging infectious diseases from animals are usually resulting from wildlife consumption and distribution on a commercial scale,” says Calle, the Bronx Zoo veterinarian. “It’s not a lone person hunting to feed their family. It’s markets and global supply chains, and encroachment on natural areas, that are the risk factors.”
Calle was also a veterinarian at the zoo during the West Nile virus outbreak. He’s seen a lot of growth over the last 20 years in terms of looking beyond human medicine to support public health. “There was not the same level of integration and coordination then that there is now,” he says.
About a decade ago, awareness of the interconnectedness of humans, other animals, and the environment began to ramp up—even reaching Hollywood. At the end of the 2011 film “Contagion” (which has enjoyed renewed popularity recently thanks to the pandemic), a flashback details the origins of the fictitious virus MEV-1, modeled after the real-life Nipah virus: A bulldozer clears a patch of trees and a displaced disease-carrying bat drops a chunk of banana into a pig farm. Viewers then watch a pig gobble up the fruit before being slaughtered and handled by a chef, who does not wash his hands before greeting Gwyneth Paltrow.
Around the same time as the movie’s release, a movement called One Health also emerged. In 2010, the World Health Organization, Food and Agriculture Organization, and the World Organization for Animal Health created a One Health collaboration they termed Tripartite; the CDC established its One Health Office in 2009.
Casey Barton Behravesh, director of the CDC office, highlights the collaboration between city, state, and federal officials in diagnosing Nadia as evidence of progress. “There’s definitely more to be done,” she says. “Historically, limited resources have been available for needed One Health activities.”
Other health experts, too, argue that current efforts don’t go far enough. “You can create One Health offices, but achieving any real coordination or integration is tough,” says Epstein. “Each agency has its mandate, and it’s hard to pay to attention to everything else.”
Dirk Pfeiffer, a professor of One Health at the City University of Hong Kong, added that the concept should also go further to include the social sciences. “If you want to control diseases, it’s the human behavior that you have to change or influence,” he says.
Simply closing down live animal markets could backfire, for example. “As long as there is still a demand, they’ll find a way of trading this stuff and then you won’t even know how to find it,” adds Pfeiffer.
Behavioral and cultural practices were at the core of Predict, a project the U.S. Agency for International Development launched in 2009. Working with partners in dozens of countries, the project aimed to bolster the world’s ability to identify viruses with pandemic potential. That effort included investigating the human behaviors and practices, as well as ecological and biological factors, that drive the emergence, transmission and spread of diseases.
Funding for the project ended in September 2019, just before COVID-19 emerged.
It’s not just at urban food markets where diseases spill over from animals into humans, says Epstein. Hunting or agricultural areas are among other hotspots, especially as humans increasingly encroach on wildlife habitats. “We need to be able to continue this kind of surveillance work—recognize where a spillover is likely to happen, then work with communities and governments to reduce that risk,” he adds, referring to the efforts launched via Predict. “The U.S. and global community has to commit to investing in a much bigger way. A lack of investment is what has gotten us to where we are now with COVID-19.”
Some politicians seem to be getting the message. One Health-related legislation is currently pending in Congress. The Advancing Emergency Preparedness Through One Health Act seeks to improve public health preparedness by requiring federal agencies to develop a One Health approach. Sen. Dianne Feinstein (D-Calif.) is a co-sponsor of the Senate bill. She also spearheaded, alongside Martha McSally (R-Ariz.), a bipartisan resolution for a National One Health Awareness Month, which passed the Senate in December, and is now calling for the creation of a new interagency government entity, the Center for Combating Infectious Disease, “to oversee all aspects of preventing, detecting, monitoring, and responding to major outbreaks such as coronavirus,” she told Undark in an email.
“As the planet’s climate continues to warm and humans and wild animals migrate in ways that bring them into greater contact, the potential for new pandemics that spread from animals to humans will also increase,” added Feinstein. COVID-19, she noted, “has highlighted the interactions of animals and people and the consequences of not monitoring those interactions closely.”
0 notes
Text
Vets, farmers, and zookeepers can help prevent the next pandemic
There have been multiple confirmed cases of COVID-19 in tigers at New York City's Bronx Zoo. Scientists there are now researching the origins of the big cats' infection. (A G/Unsplash/)
Lynne Peeples writes about science, health, and the environment from her home office in Seattle. Her work has also appeared in Scientific American, Reuters, Popular Science, Environmental Health News, and Audubon, among other publications. This story originally featured on Undark.
Nadia began coughing on March 27. The 4-year-old Malayan tiger’s keepers at the Bronx Zoo in New York City also noticed she wasn’t finishing her daily allotment of raw meat. Concerned, they called in Paul Calle, the zoo’s head veterinarian.
The team immobilized and anesthetized Nadia, so she could be put through a series of X-rays, ultrasounds, and routine blood work to look for known causes of respiratory disease in cats. “Since New York City is the epicenter for COVID in the US,” says Calle, “we wanted to make sure we checked her for that, too.”
On April 5, the zoo reported that Nadia had been infected by SARS-CoV-2, the virus that causes COVID-19. Over the course of the next week, three other tigers and three lions at the zoo also began showing similar symptoms. The sick cats were later tested, along with another 8-year-old male Amur tiger named Alden, who hadn’t been showing any symptoms. Every test came back positive, according to a statement released by the zoo on April 22. All eight cats are now recovering well, and “only an occasional cough is heard,” Calle says.
Officials think that an asymptomatic zoo worker carrying the virus probably infected the animals. “People and animals and the environment are all closely linked and influence what happens to each other,” says Calle.
This is far from the first time, and certainly won’t be the last, that an infectious disease has bounced between humans and other animals. Evidence suggests that COVID-19 likely originated in a bat, possibly jumped to a pangolin—which looks like a scaly anteater—and then infected a human, maybe at a live animal market in Wuhan, China. Globally, an estimated 75 percent of newly appearing infectious diseases are “zoonotic” like this, meaning they can pass from non-human animals to people. Infectious-disease experts warn that nature harbors more than a million undiscovered viruses.
The animals we keep as pets can be part of the transmission process, too. Exotic pet rodents were implicated as the likely source of an outbreak of monkeypox in the Midwest in 2003. Pigs, obviously, spawned the 2009 swine flu pandemic. And, last month, the U.S. Centers for Disease Control and Prevention and the Department of Agriculture confirmed that two pet cats in New York had tested positive for SARS-CoV-2. A pug in North Carolina named Winston was also added to the list in late April.
Recognition of the link between humans and other animals for COVID-19 is driving the push to ban China’s live animal markets, which pose a high risk for contagion. And animal health expertise could help prevent outbreaks in other ways, some scientists say. For example, greater animal surveillance could detect new diseases earlier and stop them from being passed to humans. And techniques for controlling outbreaks in livestock, such as randomized surveillance strategies, could also improve efforts to limit the spread of disease in human populations.
Yet despite being recognized as useful, the field of animal health has long been siloed away from human medicine. Veterinarians as well as wildlife biologists, livestock farmers, and zookeepers remain a largely untapped resource for combatting diseases that threaten people. “There is still a very traditional divide among disciplines,” says Jon Epstein, a wildlife veterinarian and disease ecologist for the EcoHealth Alliance in New York. “We haven’t removed these barriers yet.”
That’s not to say that experts haven’t been trying. But progress in getting authorities to see the connectedness of human and animal health has been slow—and in some instances in recent decades, has even gone backwards.
“It’s time that we stopped using humans as sentinels of animal diseases,” says Joe Annelli, the executive vice president of the National Association of Federal Veterinarians and formerly with the USDA. Instead, he said, we should be aiming to identify diseases in other animals as early as possible, when there’s still a chance of preventing them from spreading to humans.
Nearly 20 years ago, the Bronx Zoo was in the spotlight as another contagion crept among the city’s people and non-human animals.
It was the summer of 1999, and a strange disease that caused weakness and confusion had begun popping up among dozens of New Yorkers. Meanwhile, dead crows had started landing on the zoo’s grounds. Then came casualties among captive species: Chilean flamingos, laughing gulls, a snowy owl, and a bald eagle named Clementine.
Clementine was the zoo’s mascot. “She looked perfectly fine and then, boom, she dropped dead,” says Tracey McNamara, then the chief veterinary pathologist at the zoo. Her necropsy of Clementine—standard procedure for any death at an accredited zoo in the US—showed the worst brain inflammation in a bird that McNamara had ever seen. Worried that her surgical mask wasn’t enough protection against whatever had killed the eagle, McNamara went home that night and wrote her will.
She also went on with her detective work, taking advantage of what she called “built-in sentinels” of disease naturally found at a zoo. The CDC, at the time, suspected a brain disease called Saint Louis encephalitis. But McNamara knew that this disease doesn’t typically harm birds. Inflammation in bird brains, she noted, instead suggested one of three usual suspects in the U.S. The first was eastern equine encephalitis. Emus are known to be particularly sensitive to this virus, yet the zoo’s emu flock showed no signs of sickness. That left the other two possibilities: virulent Newcastle disease and highly pathogenic avian influenza. Both of these affect chickens, and the petting zoo was full of healthy birds.
“That’s when I knew I was dealing with something unknown to veterinary medicine,” says McNamara, now a professor of pathology at Western University of Health Sciences in Pomona, California.
While the CDC initially dismissed McNamara’s suggestion that the same disease might be impacting both people and birds, the agency eventually came around. Tests weeks later revealed that New York was home to the first cases of West Nile virus ever reported in the Western hemisphere. And, as the U.S. General Accounting Office would report in September 2000, the animal infections preceded the first human cases by at least one or two months. “The West Nile events illustrate the value of communication between public and animal health communities,” the GAO wrote.
As this mosquito-borne disease swept from New York across the US, none of the traditional means of surveillance—tests of mosquito pools or chicken flocks—proved to be predictive of human risks. So McNamara pushed for the launch of a nationwide surveillance network across zoos, suggesting it could bolster the CDC’s power to prevent outbreaks. The agency was convinced. The zoo network went live and, between 2001 and 2006, nearly 180 zoos and other wildlife institutions submitted samples.
“We hoped that this was the beginning of sustainable zoonotic disease surveillance in urban centers,” says McNamara. “Every major city has a zoo. Every zoo has a spectrum of the animal kingdom, some of which are guaranteed to be susceptible to whatever new virus pops up.”
But efforts to secure continued funding—let alone money to expand the program beyond West Nile virus—were all denied.
Donald Noah, a veterinary epidemiologist at Lincoln Memorial University in Harrogate, Tennessee, was working with the U.S. Department of Homeland Security when McNamara’s team reached out to his agency for financial support. He lamented not being able to convince senior leadership to oblige. “Hopefully, given the situation now, there is a change in awareness and more realization of the importance,” Noah says.
Pets, wildlife, livestock, and zoo animals can all serve as early warning signs of an emergent threat to humans. When wildlife biologists notice squirrels lying around dead, for example, it could be an indication of the plague. “Whether it is plague or hantavirus or rabies—or now COVID-19—viruses may be circulating for an unknown period of time in an animal reservoir species and then all of a sudden became apparent in humans,” says Noah.
Spotting signs of disease in bats or an intermediary animal, such as pangolins, may have warned officials of the threat of COVID-19 before it went pandemic, notes Victoria Brookes, a zoonotic disease expert at Charles Sturt University in Wagga Wagga, Australia.
“We’re always looking at timeliness,” says Brookes, who is helping to launch a “disease detective” training program for animal workers across Southeast Asia and Oceania that will support the development of local surveillance systems to detect diseases before they spawn an outbreak.
Annelli underscored the need for such surveillance: “We put all this money and work into identifying the first person to have a particular disease, but we’ve spent nothing on identifying that disease in the animal population and working to eliminate it before it continues to infect people,” he says.
But if a sick animal is not of economic value, then testing for and reporting any illness remains especially difficult. “There is still no federal agency that has jurisdiction over surveillance of zoo animals, or dogs and cats,” adds McNamara. “We have a gigantic species gap in our biosurveillance efforts in the US.”
Dozens of stray cats were infected by bird flu during a small outbreak in New York City in 2017. (Ryne Anderson/Unsplash/)
For instance, towards the end of 2016, at an animal shelter in East Harlem about 6 miles from the Bronx Zoo, an orange-and-white cat named Mimi developed a respiratory infection, became very sick, and had to be euthanized. Cats in multiple other crowded New York shelters started falling ill over the following weeks. An attending veterinarian got sick as well.
The culprit turned out to be a strain of bird flu, H7N2, never before seen in cats. By the time a private foundation stepped in to cover the costs of testing and quarantining the potentially affected animals, about 1,000 felines had already been adopted out to families throughout the greater metropolitan area.
Sandra Newbury, director of the Shelter Medicine Program at the University of Wisconsin-Madison, worked with the shelters to contain the virus. Thanks to the private donor, they were able to offer free testing and medical care for the adopted cats, eventually isolating hundreds that had been infected. “We were really aggressive in our efforts to not let it spread,” Newbury says. She believes identifying such a large number of infected animals and quarantining them allowed the authorities to eradicate the virus. According to Newbury, no positive tests have been reported since March 2017.
“We were really very lucky. This could’ve turned into a new virus of cats,” says Newbury, noting the contrast with what’s playing out today. “A virus spreads more easily when you don’t know that it’s there. That’s what we’re seeing now with COVID-19 in humans. There’s not enough testing.”
While it would be impossible to identify every possible disease in non-human animals, notes Annelli, far more could be done to test for diseases known to occasionally spill over to humans, such as Ebola. He also believes we should be regularly sampling animals at live markets for influenza and coronaviruses, and testing wildlife in natural areas where they might closely overlap with domestic animals and people—such as deforested lands—to see how diseases evolve over time. The commingling of species provides an optimal environment for viruses to mutate to the point that they could infect people.
“When multiple species are mixed together that are not usually next to each other, then you can get all kinds of things popping up,” says Annelli. The 2003 monkeypox outbreak is another case in point: Gambian rats caught in Africa were shipped to the U.S. and ended up being housed next to prairie dogs, a species they had never been in close contact with in the wild. Once infected, prairie dogs can fairly easily transmit the virus to people. And evidence suggests they did.
Experts underscore the importance of finding not only the species that spread viruses in the first place, but also which animals may maintain them in the future. Even if control measures manage to curb COVID-19 in human populations, for example, might the virus simply hide out in domestic cats, local bats, or another non-human species, ready to re-emerge later? “That’s an open question that needs to be examined,” says Epstein.
A Chinese study published in March identified several species that SARS-CoV-2 might be able to infect, including cats, cows, pigeons, and pangolins. Another study underway in Germany is exposing different animals to the virus in hopes of deciphering whether it could infect as well as replicate within certain species—and so potentially sustain itself there. Early findings reported in April suggest that fruit bats and ferrets are susceptible, while pigs and chickens are not.
But just because an animal can be infected doesn’t necessarily mean it can spread the disease to others. Thankfully, the flu that affected the shelter cats turned out to be fairly mild and minimally transmissible to humans. “If this virus had been as dangerous and as virulent as the pandemic flu of 1918, then the battle would have already been lost,” says McNamara.
“We dodged a bullet, she adds. “But there’s no guarantee we’ll be as lucky the next time.”
In 2007, the bluetongue virus—a disease spread by midge bites—began to sweep through herds of sheep and cattle across Europe. Johanne Ellis-Iversen was serving as the veterinary adviser for the U.K.’s Department for Environment, Food, and Rural Affairs towards the end of the outbreak and as it was officially declared over in 2011. The U.K. has seen a number of major outbreaks of disease in food animals in recent decades, including bovine spongiform encephalopathy (aka “mad cow disease”) and foot-and-mouth disease. As a result, says Ellis-Iversen, it has a very structured and effective response for fighting epidemics among livestock.
In agricultural animal health, “outbreaks of exotic disease in well-regulated countries rarely get big because we identify and control them right away,” says Ellis-Iversen, now a senior adviser and veterinary epidemiologist at the National Food Institute at the Technical University of Denmark. She is also the co-author of a paper published in late March that describes how veterinary surveillance methods could be adapted to randomly survey human populations for COVID-19.
When dealing with infection among livestock, before a decision is made to lift control measures or reopen exports, it’s standard procedure to test animals at random to estimate the disease spread. Ellis-Iversen’s team did just that to prove the country was free of bluetongue. “We want to know what is happening in a population, not just the herds identified as ill,” she says.
In the case of COVID-19, some countries and US states have begun lifting social distancing and containment measures. Their typical plan: Keep an eye out for the re-emergence of infections and then re-enact control measures as necessary. But Ellis-Iversen cautions that if you only pick up infections by testing individuals admitted to hospital or by measuring deaths, then you miss a lot of valuable information—conducting monitoring so far down the line means anything done in response will have a delayed impact. “If officials see that hospital cases are creeping towards a threshold, then it would be another week or two before they can actually reduce the number going into the hospital,” she says.
“We’re wondering why public health isn’t looking more to using the experience from animal health,” adds Ellis-Iversen. Representative surveys of the population—like those used for livestock—could inform policy making, including outbreak control and exit strategies, she said.
While randomized surveys are not a replacement for other public health tools, such as identifying people who are ill and tracing who they might have infected, Ellis-Iversen believes they could provide some “extremely useful” data for deciding on control measures. Recognizing that some countries have limited testing capacity, she also notes that samples need not be large to provide valuable information. “You don’t need to test 10,000 people,” says Ellis-Iversen. “We just need to consider how we select the people we test.”
Germany is using just such a technique for human populations right now, in the hope that the data will inform what restrictions can be loosened without a resurgence of infections. Ellis-Iversen suggests that while randomized surveys are “used occasionally in public health,” they tend to be conducted more for studies rather than as ongoing surveillance for decision making. “It will be interesting to see the results,” says Ellis-Iversen. “If they show something unexpected, I am sure it will be food for thought around the world.”
Days before Nadia, the Bronx Zoo tiger, was diagnosed with COVID-19, the Wildlife Conservation Society issued a statement urging the closure of live animal markets. The international organization, which happens to be based at the Bronx Zoo, is among several environmental groups, politicians, and celebrities now advocating for a ban. Live animal markets were also implicated in the 2003 SARS outbreak.
“These emerging infectious diseases from animals are usually resulting from wildlife consumption and distribution on a commercial scale,” says Calle, the Bronx Zoo veterinarian. “It’s not a lone person hunting to feed their family. It’s markets and global supply chains, and encroachment on natural areas, that are the risk factors.”
Calle was also a veterinarian at the zoo during the West Nile virus outbreak. He’s seen a lot of growth over the last 20 years in terms of looking beyond human medicine to support public health. “There was not the same level of integration and coordination then that there is now,” he says.
About a decade ago, awareness of the interconnectedness of humans, other animals, and the environment began to ramp up—even reaching Hollywood. At the end of the 2011 film “Contagion” (which has enjoyed renewed popularity recently thanks to the pandemic), a flashback details the origins of the fictitious virus MEV-1, modeled after the real-life Nipah virus: A bulldozer clears a patch of trees and a displaced disease-carrying bat drops a chunk of banana into a pig farm. Viewers then watch a pig gobble up the fruit before being slaughtered and handled by a chef, who does not wash his hands before greeting Gwyneth Paltrow.
Around the same time as the movie’s release, a movement called One Health also emerged. In 2010, the World Health Organization, Food and Agriculture Organization, and the World Organization for Animal Health created a One Health collaboration they termed Tripartite; the CDC established its One Health Office in 2009.
Casey Barton Behravesh, director of the CDC office, highlights the collaboration between city, state, and federal officials in diagnosing Nadia as evidence of progress. “There’s definitely more to be done,” she says. “Historically, limited resources have been available for needed One Health activities.”
Other health experts, too, argue that current efforts don’t go far enough. “You can create One Health offices, but achieving any real coordination or integration is tough,” says Epstein. “Each agency has its mandate, and it’s hard to pay to attention to everything else.”
Dirk Pfeiffer, a professor of One Health at the City University of Hong Kong, added that the concept should also go further to include the social sciences. “If you want to control diseases, it’s the human behavior that you have to change or influence,” he says.
Simply closing down live animal markets could backfire, for example. “As long as there is still a demand, they’ll find a way of trading this stuff and then you won’t even know how to find it,” adds Pfeiffer.
Behavioral and cultural practices were at the core of Predict, a project the U.S. Agency for International Development launched in 2009. Working with partners in dozens of countries, the project aimed to bolster the world’s ability to identify viruses with pandemic potential. That effort included investigating the human behaviors and practices, as well as ecological and biological factors, that drive the emergence, transmission and spread of diseases.
Funding for the project ended in September 2019, just before COVID-19 emerged.
It’s not just at urban food markets where diseases spill over from animals into humans, says Epstein. Hunting or agricultural areas are among other hotspots, especially as humans increasingly encroach on wildlife habitats. “We need to be able to continue this kind of surveillance work—recognize where a spillover is likely to happen, then work with communities and governments to reduce that risk,” he adds, referring to the efforts launched via Predict. “The U.S. and global community has to commit to investing in a much bigger way. A lack of investment is what has gotten us to where we are now with COVID-19.”
Some politicians seem to be getting the message. One Health-related legislation is currently pending in Congress. The Advancing Emergency Preparedness Through One Health Act seeks to improve public health preparedness by requiring federal agencies to develop a One Health approach. Sen. Dianne Feinstein (D-Calif.) is a co-sponsor of the Senate bill. She also spearheaded, alongside Martha McSally (R-Ariz.), a bipartisan resolution for a National One Health Awareness Month, which passed the Senate in December, and is now calling for the creation of a new interagency government entity, the Center for Combating Infectious Disease, “to oversee all aspects of preventing, detecting, monitoring, and responding to major outbreaks such as coronavirus,” she told Undark in an email.
“As the planet’s climate continues to warm and humans and wild animals migrate in ways that bring them into greater contact, the potential for new pandemics that spread from animals to humans will also increase,” added Feinstein. COVID-19, she noted, “has highlighted the interactions of animals and people and the consequences of not monitoring those interactions closely.”
0 notes
Link
The public health danger posed by potentially pandemic-causing viruses escaping from laboratories has become the subject of considerable discussion, spurred by “gain of function” experiments. The ostensible goal of these experiments—in which researchers manipulate already-dangerous pathogens to create or increase communicability among humans—is to develop tools to monitor the natural emergence of pandemic strains. Opponents, however, warn in a variety of recent research papers that the risk of laboratory escape of these high-consequence pathogens far outweighs any potential advance.
The danger of a manmade pandemic sparked by a laboratory escape is not hypothetical: One occurred in 1977, and it occurred because of concern that a natural pandemic was imminent. Many other laboratory escapes of high-consequence pathogens have occurred, resulting in transmission beyond laboratory personnel. Ironically, these laboratories were working with pathogens to prevent the very outbreaks they ultimately caused. For that reason, the tragic consequences have been called “self-fulfilling prophecies.”
Modern genetic analysis allows pathogens to be precisely identified, and because all circulating pathogens show genetic changes over time, the year that a particular example of a pathogen emerged can generally be determined, given a sufficient database of samples. If a pathogen appears in nature after not circulating for years or decades, it may be assumed to have escaped from a laboratory where it had been stored inert for many years, accumulating no genetic changes—that is, its natural evolution had been frozen.
The swine flu scare of 1976 and the H1N1 human influenza pandemic of 1977. Human H1N1 influenza virus appeared with the 1918 global pandemic and persisted, slowly accumulating small genetic changes, until 1957, when it appeared to go extinct after the H2N2 pandemic virus appeared. In 1976, H1N1 swine influenza virus struck Fort Dix, N.J., causing 13 hospitalizations and one death. The specter of a reprise of the deadly 1918 pandemic triggered an unprecedented effort to immunize all Americans. No swine H1N1 pandemic materialized, however, and complications of immunization truncated the program after 48 million immunizations, which eventually caused 25 deaths.
Human H1N1 virus reappeared in 1977, in the Soviet Union and China. Virologists, using serologic and early genetic tests, soon began to suggest the cause of the reappearance was a laboratory escape of a 1949-50 virus, and as genomic techniques advanced, it became clear that this was true. By 2010, researchers published it as fact: “The most famous case of a released laboratory strain is the re-emergent H1N1 influenza-A virus which was first observed in China in May of 1977 and in Russia shortly thereafter.” The virus may have escaped from a lab attempting to prepare an attenuated H1N1 vaccine in response to the U.S. swine flu pandemic alert.
The 1977 pandemic spread rapidly worldwide but was limited to those under 20 years of age: Older persons were immune from exposures before 1957. Its attack rate was high (20 to 70 percent) in schools and military camps, but mercifully it caused mild disease, and fatalities were few. It continued to circulate until 2009, when the pH1N1 virus replaced it. There has been virtually no public awareness of the 1977 H1N1 pandemic and its laboratory origins, despite the clear analogy to current concern about a potential H5N1 or H7N9 avian influenza pandemic and “gain of function” experiments. The consequences of escape of a highly lethal avian virus with enhanced transmissibility would almost certainly be much graver than the 1977 escape of a “seasonal,” possibly attenuated strain to a population with substantial existing immunity.
Smallpox releases in Great Britain. Eradication of natural smallpox transmission made the prospect of reintroduction of the virus intolerable. This risk was clearly demonstrated in the United Kingdom. From 1963-78 the U.K. saw only four cases of smallpox (with no deaths) occurred that were imported by travelers from areas where smallpox was endemic. During this same period at least 80 cases and three deaths resulted from three separate escapes from two different accredited smallpox laboratories.
The first recognized laboratory escape, in March 1972, occurred with the infection of a laboratory assistant at the London School of Hygiene and Tropical Medicine. She had observed the harvesting of live smallpox virus from eggs used as a growing medium; the process was performed on an uncontained lab table, as was then routine. She was hospitalized, but before she was placed in isolation, she infected two visitors to a patient in an adjacent bed, both of whom died. They in turn infected a nurse, who survived, as did the laboratory assistant.
In August of 1978, a medical photographer at Birmingham Medical School developed smallpox and died. She infected her mother, who survived. Her workplace was immediately above the smallpox laboratory at Birmingham Medical School. Faulty ventilation and shortcomings in technique were ultimately implicated.
Investigators then re-examined a 1966 smallpox outbreak, which was strikingly similar. The initial 1966 infection was also a medical photographer who worked at the same Birmingham Medical School facility. The earlier outbreak was caused by a low-virulence strain of smallpox (variola minor), and it caused at least 72 subsequent cases. There were no deaths. Laboratory logs revealed variola minor had been manipulated in the smallpox laboratory at a time appropriate to cause the infection in the photographer working a floor above.
Venezuelan equine encephalitis in 1995. Venezuelan equine encephalitis is a viral disease transmitted by mosquitoes. It intermittently erupts in regional or continental-scale outbreaks that involve equines (horses, donkeys, and mules) in the Western Hemisphere. There are often concurrent zoonotic epidemics among humans. VEE in humans causes a severe febrile illness; it can occasionally be fatal or may leave permanent neurological disability (epilepsy, paralysis, or mental retardation) in 4 to 14 percent of clinical cases, particularly those involving children.
There were significant outbreaks of VEE every few years from the 1930s to the 1970s. Modern analysis revealed most outbreaks were genetic matches to the original 1938 VEE isolation used in inactivated veterinary vaccines. It was clear that many batches of the veterinary VEE vaccines had not been completely inactivated, so residual infective virus remained.
From 1938 to 1972, the VEE vaccine caused most of the very outbreaks that it was called upon to prevent, a clear self-fulfilling prophecy.
In 1995 a major VEE animal and human outbreak struck Venezuela and Colombia. There were at least 10,000 human VEE cases with 11 deaths in Venezuela and an estimated 75,000 human cases in Colombia, with 3,000 neurological complications and 300 deaths. VEE virus was isolated from 10 stillborn or miscarried human fetuses.
Genomic analysis identified the 1995 virus as identical to a 1963 isolate, with no indication it had been circulating for 28 years. It was another case of frozen evolution, but unlike the vaccine-related VEE outbreaks, the 1963 virus had never been used in a vaccine. Suspicion fell on an inadvertent release from a virology lab, either by an unrecognized infection of a lab worker or visitor, or escape of an infected laboratory animal or mosquito. The major scientific group working on VEE published a paper in 2001 stating the 1995 outbreak most likely was a laboratory escape, with considerable circumstantial evidence: The outbreak strain was isolated from an incompletely inactivated antigen preparation used on the open bench in the VEE laboratory located at the outbreak epicenter. But clear proof was lacking, and the group subsequently said it was reconsidering this conclusion.
SARS outbreaks after the epidemic. The 2003 Severe Acute Respiratory Syndrome outbreak spread to 29 countries, causing more than 8,000 infections and at least 774 deaths. Because 21 percent of cases involved hospital workers, it had the potential to shut down health care services wherever it struck. It is particularly dangerous to handle in the laboratory because there is no vaccine, and it can be transmitted via aerosols.
Moreover, about 5 percent of SARS patients are “super-spreaders” who infect eight or more secondary cases. For instance, one patient spread SARS directly to 33 others (reflecting an infection rate of 45 percent) during a hospitalization, ultimately leading to the infection of 77 people, including three secondary super-spreaders. A super-spreader could turn even a single laboratory infection into a potential pandemic.
SARS has not re-emerged naturally, but there have been six escapes from virology labs: one each in Singapore and Taiwan, and four separate escapes at the same laboratory in Beijing.
The first was in Singapore in August 2003, in a virology graduate student at the National University of Singapore. He had not worked directly with SARS, but it was present in the laboratory where he worked. He recovered and produced no secondary cases. The World Health Organization formed an expert committee to revise SARS biosafety guidelines.
The second escape was in Taiwan in December 2003, when a SARS research scientist fell ill on a return flight after attending a medical meeting in Singapore. His 74 contacts in Singapore were quarantined, but again, fortunately, none developed SARS. Investigation revealed the scientist had handled leaking biohazard waste without gloves, a mask, or a gown. Ironically, the WHO expert committee called for augmented biosafety in SARS laboratories the day after this case was reported.
In April 2004, China reported a case of SARS in a nurse who had cared for a researcher at the Chinese National Institute of Virology. While ill, the researcher had traveled twice by train from Beijing to Anhui province, where she was nursed by her mother, a physician, who fell ill and died. The nurse in turn infected five third-generation cases, causing no deaths.
Subsequent investigation uncovered three unrelated laboratory infections in different researchers at the NIV. At least of two primary patients had never worked with live SARS virus. Many shortcomings in biosecurity were found at the NIV, and the specific cause of the outbreak was traced to an inadequately inactivated preparation of SARS virus that was used in general (that is, not biosecure) laboratory areas, including one where the primary cases worked. It had not been tested to confirm its safety after inactivation, as it should have been.
Foot-and-mouth disease in the U.K. in 2007. Foot-and-mouth disease infects cloven-hoofed animals such as pigs, sheep, and cattle. It has been eradicated in North America and most of Europe. It is highly transmissible, capable of spreading through direct contact on the boots of farm workers and by natural aerosol that can spread up to 250 kilometers. Outbreaks in FMD-free areas cause economic disaster because meat exports cease and animals are massively culled. A 2001 U.K. outbreak resulted in 10 million animals killed and $16 billion in economic losses.
In 2007, FMD appeared again in Britain, 4 kilometers from a biosafety level 4 laboratory—a designation indicating the highest level of lab security—located at Pirbright. The strain had caused a 1967 outbreak in the United Kingdom but was not then circulating in animals anywhere. It was, however, used in vaccine manufacture at the Pirbright facility. Investigations concluded that construction vehicles had carriedmud contaminated with FMD from a defective wastewater line at Pirbright to the first farm. That outbreak identified 278 infected animals and required 1,578 animals to be culled. It disrupted U.K. agricultural production and exports and cost an estimated 200 million pounds.
Federal law bans FMD virus from the continental United States, and it is held only at the U.S. Department of Agriculture Plum Island facility off Long Island, N.Y. Currently, however, its replacement, the National Bio and Agro-Defense Facility, is under construction in Manhattan, Kan., under the aegis of the Department of Homeland Security. Moving FMD research to the agricultural heartland of the United States was opposed by many groups, including the Government Accountability Office, but Homeland Security decided on the Kansas location. In upgrading facilities to counter the threat of agro-bioterrorism, the department is increasing the risk to U.S. agriculture of unintentional release.
* * *
These narratives of escaped pathogens have common themes. There are unrecognized technical flaws in standard biocontainment, as demonstrated in the U.K. smallpox and FMD cases. Inadequately inactivated preparations of dangerous pathogens are handled in laboratory areas with reduced biosecurity levels, as demonstrated in the SARS and VEE escapes. The first infection, or index case, happens in a person not working directly with the pathogen that infects him or her, as in the smallpox and SARS escapes. Poor training of personnel and slack oversight of laboratory procedures negate policy efforts by national and international bodies to achieve biosecurity, as shown in the SARS and smallpox escapes.
It is hardly reassuring that, despite stepwise technical improvements in containment facilities and increased policy demands for rigorous biosecurity procedures in the handling of dangerous pathogens, potentially high-consequence breaches of biocontainment occur nearly daily: In 2010, 244 unintended releases of bioweapon candidate “select agents” were reported.
Looking at the problem pragmatically, the question is not if such escapes will result in a major civilian outbreak, but rather what the pathogen will be and how such an escape may be contained, if indeed it can be contained at all.
Experiments that augment virulence and transmissibility of dangerous pathogens have been funded and performed, notably with the H5N1 avian influenza virus. The advisability of performing such experiments at all—particularly in laboratories placed at universities in heavily populated urban areas, where potentially exposed laboratory personnel are in daily contact with a multitude of susceptible and unaware citizens—is clearly in question.
If such manipulations should be allowed, it would seem prudent to conduct them in isolated laboratories where personnel are sequestered from the general public and must undergo a period of exit quarantine before re-entering civilian life. The historical record tells us it is not a matter of if but when ignoring such measures will cost health and even lives. Perhaps many lives.
A version of this essay originally appeared in the Bulletin of the Atomic Scientists. Itsummarizes a more detailed review of the historical record with appropriate scientific references; it is available on the website of the Center for Arms Control and Non-Proliferation.
Martin Furmanski is a medical doctor and medical historian who researches the development, use, and allegations of use of chemical and biological weapons.
0 notes
Text
Veterinary/Animal Vaccines Market Key Players | Applications and Types | Forecast To 2025
Global Veterinary/Animal Vaccines Market is expected to reach USD 12.6 billion by 2025. Vaccine administration is a process that increases the resistant or immune power to an infectious disease. The aim of veterinary/animal vaccines is to recover the welfare and health of companion animals, prevent the transmission of diseases from animals to human from wildlife as well as domestic animals, and cost-efficiently rise the production of livestock. The vaccines may be administered via oral or parenteral routes. The Veterinary Vaccines Market is estimated to grow at a significant CAGR over the forecast period as the scope and its applications are rising enormously across the globe.
Growing livestock population, rise in breakouts of livestock diseases, increasing zoonotic diseases, increasing initiative by government agencies, and growing number of key players are documented as major factors of Veterinary/Animal Vaccines industry that are estimated to enhance the growth in the years to come. However, high cost of vaccine and its storage are the factor that may restrain overall market growth in the coming years. Animal Vaccines Market is segmented based on type, disease type, technology, and region.
Request Sample Copy of this Market Research @ https://www.millioninsights.com/industry-reports/veterinary-animal-vaccines-market/request-sample
Aquaculture Vaccines, Porcine Vaccines, Companion Animal Vaccines, Poultry Vaccines, Livestock Vaccines, and other types could be explored in Veterinary/Animal Vaccines in the forecast period. Livestock vaccines include Small Ruminant Vaccines and Bovine Vaccines. On the other hand, companion animal vaccines include Feline Vaccines and Canine Vaccines.
The porcine vaccines sector accounted for the largest market share of Veterinary/Animal Vaccines in terms of value. In addition, Companion Animal Vaccines sector is estimated to grow at fastest pace in the coming years. This may be because of growing awareness regarding companion animal vaccination, increasing number of pet and pet ownership, and growing occurrence of zoonotic diseases in humans.
Aquaculture Diseases, Porcine Diseases, Companion Animal Diseases, Poultry Diseases, Livestock Diseases, and others are the diseases that could be explored in Veterinary/Animal Vaccines in the forecast period. The porcine sector accounted for the substantial market share and is estimated to lead the overall market in the coming years.
The enhanced technology includes Recombinant Vaccines, Live Attenuated Vaccines, Toxoid Vaccines, Inactivated Vaccines, and others that could be explored in the forecast period. The live attenuated vaccines sector accounted for the substantial market share of Veterinary/Animal Vaccines and is estimated to continue its dominance in the coming years. This may be because it offers long-term immunity and can be administered easily.
Globally, Europe is accounted for the substantial market share of Veterinary/Animal Vaccines in terms of revenue and is estimated to lead the overall market in the coming years. The reason behind the overall market growth could be rising use of enhanced technology and presence of key manufacturers in the region. Instead, North America and the Asia Pacific are also estimated to have a positive influence on the future growth.
North America is the second largest region with significant market share. However, Asia Pacific is estimated to grow at fastest pace with the highest CAGR in the foremost period. The aspects that may be ascribed to the growth comprise growing investment in vaccine manufacturing services in developing countries, growing pet adoption, and development of key manufacturers in the region.
The key players of Veterinary/Animal Vaccines Market are Virbac, Zoetis, Phibro Animal Health, Merck Animal Health, Ceva, Elanco, and BoehringerIngelheim. These players are concentrating on inorganic growth to sustain themselves amongst fierce competition. As companies all over the world have to believe that alliance with a market would permit them proportional market existence and authority to declare the leadership position.
Browse Full Research Report @ https://www.millioninsights.com/industry-reports/veterinary-animal-vaccines-market
Market Segment:
Product Outlook (Revenue, USD Million, 2014 - 2025)
• Attenuated Live Vaccines
• Inactivated Vaccines
• Subunit Vaccines
• DNA Vaccines
• Recombinant Vaccines
Animal Type Outlook (Revenue, USD Million, 2014 - 2025)
• Companion Animal Vaccines.
• Canine
• Distemper
• Kennel cough (Parainfluenza)
• Parvovirus
• Canine herpes
• Lyme Disease
• Feline
• Feline calicivirus
• Peritonitis (FIP)
• Feline FIV
• Cattle Vaccines
• BRSV
• Enzootic Bronchopneu
• IBR
• BVD/MD
• Poultry Vaccines
• Bronchitis
• Avian Influenza
• Marek's Disease
• Newcastle Disease
• Pig Vaccines
• Porcine reproductive disease
• Swine Influenza
• Swine Pneumonia
• Equine Vaccines
• Encephalomyelitis
• Rhinopneumonitis
• Influenza (Horse Flu)
Regional Outlook (Revenue, USD Million, 2014 - 2025)
• North America
• U.S.
• Canada
• Europe
• U.K.
• Germany
• Asia Pacific
• India
• China
• Latin America
• Brazil
• Mexico
• Middle East & Africa
• South Africa
For More Details Please Visit www.millioninsights.com
0 notes
Text
Animal Vaccines Market - Global Industry Analysis and Trends up to 2025
22th November 2018: The animal vaccines helps in the improvement of animal health in a cost effective manner by increasing the livestock production and preventing disease transmissions among animals. Animal vaccines market has gained a two-digit growth over the past few years. The global market for vet vaccines is driven by several factors like animal’s vulnerability to fatal diseases, and rapid change of diseases pattern among the animals. Veterinary vaccines have helped to reduce the heavy usage of drug treatments to curtail fatal diseases thereby preventing long term suffering and death. The global animal vaccines market has changed progressively during the past years with the increase usage of continuing cell lines as substrates and for antigen production adopting fermenting technology. Depending on the vaccine characteristics these vaccines are consumed either by parenteral or by oral routes. The global animal vaccines market has four segments like diseases, products, regions and technologies. The disease segment animal vaccines market is further divided into aquaculture diseases, poultry diseases, companion animal diseases, equine diseases and porcine diseases.

Browse Full Research Report @ https://www.millioninsights.com/industry-reports/animal-vaccines-market
Porcine diseases include Porcine parvovirus, Porcine reproductive respiratory syndrome (PRRS), Porcine circovirus II, Swine influenza, Swine pneumonia, Auzeszky's disease. Poultry diseases include Infectious bronchitis, Gumboro disease, Avian influenza, Coccidiosis, Marek’s disease, Newcastle disease, Mycoplasma. Equine diseases include Equine encephalomyelitis, Strangles tetanus equine, Influenza equine, Rhinopneumonitis. Aquaculture diseases include Vibriosis, Pasteurellosis, Furunculosis. Major animal vaccine production technologies are live attenuated vaccines, inactivated vaccines, subunit vaccines, toxic vaccines, conjugate vaccines, recombinant vaccines, and DNA vaccines. Under livestock diseases category the bovine vaccine is applicable for Foot-and-mouth disease, Bovine viral diarrhea, Bovine clostridia disease, brucellosis, Infectious bovine rhinotracheitis etc. Under companion diseases category canine vaccines is applicable for Canine rabies, Canine distemper, Canine parvovirus, and Infectious canine hepatitis. Feline Vaccines is applicable for Feline rabies, Feline panleukopenia, Feline viral rhinotracheitis, and Feline leukemia. Small ruminant animal vaccine is applicable for small ruminant clostridia disease, Scabby mouth infection, Pneumonia & Septicemia, Pox and Ovine Johne's disease. The DNA vaccines have the highest growth in veterinary vaccine technologies market in 2014.
The product segment animal vaccines market is further divided into livestock vaccine, porcine vaccines, poultry vaccines, equine vaccines, aquaculture vaccines, companion animal vaccines and other animal vaccines like vaccines for rabbits, deer, camels, elephants and bats. The companion animal vaccine in the product segment is the fastest-growing segment due to increase in growing pet population and increase of zoonotic diseases in humans. The growth of animal vaccines market is also fuelled by increasing investments by various government agencies, animal associations, and leading players; continuous innovations and introduction of new veterinary vaccines. The other key growth drivers are various technological innovations like DNA vaccines, animal health awareness in developing nations. On the parallel side increase in maintenance and storage costs of vaccines, increase in consumption of vegetarian food in major economies because of heightened risk in obesity and other chronic disorders, persistent economic downturn are the key factors restraining the growth of this market.
Breakthrough technology includes manufacturing and usage of DNA vaccines and other products ensuring increase in production and instant responses to immunity as compared to the conventional vaccines. Other driving factors like huge demand for various animal proteins which includes milk, meats, eggs and fishes and increase in the expenditure on healthcare sector which caters companion animals segment. To increase the awareness against heavy usage of antimicrobials the vaccine producers are significantly investing into NPD (New products development). Specific vaccines such as live bacterial vaccines and inactivated bacterial vaccines are being produced by local veterinary clinics or specialized vet meds manufacturing companies to meet product specific or on farm specific demands where there is none availability of commercial vaccines. Key leaders in the veterinary vaccines market are Bayer Healthcare from Germany, Bioniche Animal Health from Canada, Boehringer Ingelheim from Germany, Ceva from France, Elcano Animal Health from USA, Heska Co. from USA, Merck Animal Health from USA, Merial of Sanofi from USA, Virbac from France, and Zoetis of Pfizer from USA.
Get a Sample Copy of This Report @ https://www.millioninsights.com/industry-reports/animal-vaccines-market/request-sample
0 notes
Text
Happenings at OVC

Tuesday August 21, 2018
1:00 p.m.
Room 1642, Biomedical Sciences, Ontario Veterinary College
Interested members of the Ontario Veterinary College are invited to attend the MSc Thesis Defense
Ashutosh Patel, of the Department of Biomedical Sciences
Thesis Title: Muscarinic Receptor Isoforms Differentially Regulate the Excitability of Medial Prefrontal Cortex Layer 6 Pyramidal Neurons in CD-1 mice
Thursday August 23, 2018
9:00 a.m.
Rm 2106 Clinical Studies, Ontario Veterinary College
Interested members of the Ontario Veterinary College are invited to attend the Final Oral Examination for the Degree of Doctor of Veterinary Science of
Kimberly Hooi of the Department of Clinical Studies
Thesis Title: “Optimization of Imaging and Bronchoalveolar Lavage Techniques to Improve Diagnostic Yield of Feline Lower Respiratory Tract Samples.”
Examination Committee: Dr. Fiona James (Chair), Dr. Alice Defarges, Dr. Dorothee Bienzle, Dr. Tony Abrams-Ogg, Dr. Carol Reinero, Atlantic Veterinary College
Advisory Committee: Dr. Alice Defarges (Advisor), Dr. Dorothee Bienzle, Dr. Stephanie Nykamp, Dr. Scott J. Weese
Thursday August 23, 2018
9:00 a.m.
Room 1715 Lifetime Learning Centre, Ontario Veterinary College
Examination to follow, in Room 2511, Stewart Building
Interested members of the University Community are invited to attend the Final Oral Examination for the Degree of Master of Science in Population Medicine, of
Victoria Seip of the Department of Population Medicine
Thesis Title: “Investigation of novel approaches to improving nursery pig health”
Examination Committee: Dr. Andy Papadopoulos (Exam Chair), Dr. Bob Friendships, Dr. Vahab Farzan, Dr. Lee-Ann Huber
Advisory Committee: Dr. Robert Friendship (Advisor), Dr. Vahab Farzan
Monday, August 27, 2018
9:00 a.m.
Room 1715, Life Time Learning Centre, Ontario Veterinary College
Examination to follow in Room 2511, Stewart Building, OVC
Interested members of the Ontario Veterinary College are invited to attend the Final Oral Examination for the Degree of Doctor of Philosophy of
Rachael Milwid of the Department of Population Medicine
Thesis Title: “Use of empirical equine contact networks to quantify the effect of non-homogenous mixing patterns on disease dynamics”
Examination Committee: Dr. Olaf Berke (Chair), Dr. Amy Greer, Dr. Terri O’Sullivan, Dr. Theresa Bernardo, Dr. Jonathan Read
Advisory Committee: Dr. Amy Greer (Advisor), Dr. Terri O’Sullivan, Dr. Zvonimir Poljak, Dr. Marek Laskowski
Monday, August 27, 2018
1:30 p.m. - 2:30 p.m.
Room 1715, Life Time Learning Centre, Ontario Veterinary College
Examination to follow, in Room 2511, Stewart Building
Interested members of the University Community are invited to attend the Final Oral Examination for the Degree of Master of Science in Population Medicine, of
Erin Mcgill of the Department of Population Medicine
Thesis Title: “Heartworm Infection Among Domestic Dogs in Canada with a Focus on Ontario: Temporal Trend, Spatial Distribution and Risk Factors”
Examination Committee: Dr. Tracey Chenier (Exam Chair), Dr. Jennifer McWhirter, Dr. Olaf Berke, Dr. Zvonimir Poljak
Advisory Committee: Dr. Olaf Berke (Advisor), Dr. Andrew Peregrine, Dr. Scott Weese
Tuesday, August 28, 2018
9:00 a.m.
Room 1713 Lifetime Learning Centre, Ontario Veterinary College
Dr. Jonathan Read from Lancaster University will be giving a special lecture in Population Medicine entitled "Influenza transmission in schools and the importance of social networks”
8:30 am - coffee
9:00 am - seminar
10:00 am discussion
In addition, if faculty or graduate students would like to schedule time in the afternoon of August 27 to meet with Jon they can contact Amy Greer ([email protected]) to see what might be possible to setup.
Thursday, August 30, 2018
9:00 a.m.
Room 1715, Life Time Learning Centre, Ontario Veterinary College
Examination to follow, in Room 2527, Stewart Building
Interested members of the University Community are invited to attend the Final Oral Examination for the Degree of Master of Science in Population Medicine, of
Sabrina Van Schyndel of the Department of Population Medicine
Thesis Title: “The Effect of Imrestor on the Incidence of Clinical Disease, Production, and Reproduction in Early Lactation Dairy Cows”
Examination Committee: Dr. Bob Friendship (Exam Chair), Dr. David Kelton, Dr. Todd Duffield, Dr. Charlotte Winder
Advisory Committee: Dr. Stephen Leblanc (Advisor), Dr. Todd Duffield, Dr. David Kelton
0 notes