#dtpa renal scan
Explore tagged Tumblr posts
Text
Pelvi Ureteric Junction Obstruction Treatment Delhi: Expert Care
Advanced PUJ Obstruction Surgery in Delhi by Dr. Prashant Jain
Best Pelvi Ureteric Junction Obstruction Treatment in Delhi
Get advanced pelvi ureteric junction obstruction treatment Delhi with Dr. Prashant Jain. Expert care for PUJ obstruction. Book your consultation now!

Pelvi-Ureteric Junction (PUJ) obstruction is a condition where urine flow from the kidney to the ureter is blocked or restricted, leading to swelling in the kidney (hydronephrosis) and potential kidney damage. Early diagnosis and proper treatment are critical to prevent severe complications. With advanced healthcare infrastructure and renowned pediatric urologists like Dr. Prashant Jain, Pelvi Ureteric Junction Obstruction Treatment Delhi has become a top choice for patients seeking expert care.
Understanding Pelvi-Ureteric Junction Obstruction
What is Pelviureteric Junction Obstruction ?

It is a blockage or narrowing between the kidney pelvis and the ureter. PUJO impairs drainage of urine and this causes the urine to remain collected in the kidney causing swelling (Hydronephrosis). If it increases progressively then it causes back pressure on kidneys and subsequently affects the renal functions and may lead to a non functioning kidney.
How common is PUJ obstruction?
About 1 in 1500 childran have PUJ obstruction from birth (congenital). PUJ obstruction is one of the conditions that can cause hydronephrosis, which is the most common condition found in prenatal ultraound.
What are the symptoms of PUJ obstruction?
Sometimes there aren’t any outward symptoms of PUJ obstruction and it is only found when an ultrasound shows that the kidneys are swollen. This is called hydronephrosis. Some children may experience back or side (flank) pain, or a urinary tract infection (UTI). Some children experience pain that comes and goes.
How diagnosis of PUJ obstruction is confirmed ?
The diagnosis of PUJ obstruction is confirmed by a study called a DTPA scan. A DTPA scan shows how well the kidneys are working and also about the severity of blockage.
How is PUJ obstruction treated ?
The treatment for a PUJ obstruction depends on severity of the blockage. Blockages that are mild, appear to be stable or are improving over the time, will be monitored with ultrasound.
Blockage that are more severe or worsening can cause permanent kidney damage. These obstruction require a surgery to remove the portion of the blocked ureter. The surgery is called as pyeloplasty.
What is Pyeloplasty?
Pyeloplasty is the pocedure of choice for PUJ obstruction. The surgery involves removing the PUJ obstruction and joining the kidney pelvis onto the ureter (pyeloplasty). It has good results. This can be acheived through a traditional surgery (‘open pyeloplasty’) or by keyhole surgery (‘laparoscopic pyeloplasty’).
What can I expect after surgery?
The child needs to stay in the hospital for 1 to 2 days and then is called after 5 days for removal of the dressing. A tube called stent is placed in the ureter at the time of surgery to keep the ureter open and draining while it heals. Stents are temporary and need to be removed after 4-6 weeks after the surgery. Removing the stent is a day care surgery and is removed with a scope passed through the urethra into the bladder.
PUJ obstruction occurs at the junction where the kidney connects to the ureter, affecting the proper drainage of urine.
1. Causes of PUJ Obstruction
Congenital Defect: A birth defect causing abnormal narrowing at the PUJ.
Scarring or Injury: Previous surgeries or infections may lead to scar tissue formation.
Blood Vessels: Abnormal blood vessels near the PUJ can compress and obstruct urine flow.
2. Symptoms of PUJ Obstruction
Pain in the abdomen or flank, often aggravated by fluid intake.
Blood in urine (hematuria).
Recurrent urinary tract infections (UTIs).
Reduced urine output or difficulty urinating.
Nausea and vomiting associated with kidney swelling.
Diagnosis of PUJ Obstruction
Accurate diagnosis is vital to tailor the appropriate treatment plan.
1. Ultrasound
A non-invasive imaging test to detect kidney swelling (hydronephrosis).
2. Renal Scan
Evaluates kidney function and the degree of obstruction.
3. CT Urogram
Provides a detailed image of the urinary tract to identify abnormalities.
4. Voiding Cystourethrogram (VCUG)
A specialized X-ray to rule out reflux or other associated conditions.
Treatment Options for PUJ Obstruction
The choice of treatment for Pelvi Ureteric Junction Obstruction Treatment Delhi depends on the severity of the condition and the patient’s overall health.
1. Non-Surgical Management
Observation: In mild cases, regular monitoring may suffice, especially in infants where the condition may resolve naturally.
Medications: To manage symptoms like pain or prevent infections.
2. Surgical Interventions
Pyeloplasty:
A gold-standard surgical procedure that removes the obstructed segment and reconnects the healthy parts of the ureter and kidney.
Performed through open, laparoscopic, or robotic-assisted techniques.
Endopyelotomy:
A minimally invasive procedure to remove the blockage using endoscopic methods.
Stent Placement:
A temporary stent may be inserted to ensure proper urine flow post-surgery.
Benefits of Early PUJ Obstruction Treatment
Prevents Kidney Damage: Reduces the risk of permanent kidney impairment.
Improves Quality of Life: Relieves symptoms like pain and infections.
Minimally Invasive Options: Advanced techniques ensure quicker recovery and less discomfort.
Cost-Effective in Delhi: Affordable treatment options without compromising on quality.
Why Choose Delhi for PUJ Obstruction Treatment?
Delhi is a hub for advanced medical care, offering several advantages for those seeking Pelvi Ureteric Junction Obstruction Treatment Delhi.
1. Expert Pediatric Urologists
Dr. Prashant Jain is a leading specialist in treating PUJ obstruction with expertise in minimally invasive techniques.
2. State-of-the-Art Facilities
Delhi hospitals are equipped with the latest imaging and surgical tools to ensure accurate diagnosis and effective treatment.
3. Affordable Healthcare
Compared to global standards, Delhi offers high-quality yet cost-effective treatment options.
4. Comprehensive Patient Support
From diagnosis to post-operative care, patients receive holistic treatment and counseling.
5. Medical Tourism Destination
International patients often choose Delhi for its exceptional healthcare infrastructure and streamlined medical tourism processes.
Preparing for PUJ Obstruction Surgery
Proper preparation is essential for a successful outcome.
1. Pre-Surgery Consultation
A detailed discussion with Dr. Prashant Jain to understand the procedure and address concerns.
2. Diagnostic Tests
Blood tests and imaging studies to evaluate kidney function.
3. Preparing the Patient
Instructions on fasting and medications to be taken before surgery.
Post-Surgery Care and Recovery
Recovery after PUJ obstruction surgery depends on the type of procedure performed.
1. Hospital Stay
Typically, patients stay in the hospital for 1-3 days for observation.
2. Pain Management
Prescribed medications to ensure comfort during recovery.
3. Follow-Up Visits
Regular follow-ups to monitor healing and kidney function.
4. Lifestyle Adjustments
Ensure proper hydration and a healthy diet to support recovery.
Why Dr. Prashant Jain is the Right Choice
Dr. Prashant Jain is renowned for his expertise in Pelvi Ureteric Junction Obstruction Treatment Delhi. His patient-centered approach, combined with advanced surgical techniques, ensures the best outcomes for children and adults alike.
Conclusion
Pelvi-Ureteric Junction Obstruction is a serious condition that can lead to significant health issues if left untreated. Delhi offers world-class treatment for PUJ obstruction, with specialists like Dr. Prashant Jain providing expert care. For those seeking effective and affordable Pelvi Ureteric Junction Obstruction Treatment Delhi, consulting Dr. Jain is the first step towards better health and quality of life. Contact Dr. Jain today to explore your treatment options.
0 notes
Text
Living Donor Kidney Transplant in India
Kidney diseases are on the rise. Lifestyles, dietary habits, and excessive alcohol and tobacco consumption are the major factors responsible for kidney diseases. In India, there are many Kidney transplant specialist surgeons at many better-equipped hospitals to provide successful live donor Kidney transplants. As the awareness and availability of organ donation post-death(deceased Donor) are still in a very nascent stage, Kidney from deceased donors are not readily available and patients suffering from an end-stage renal disease requiring a kidney transplant depend on donation from living family members for live donor kidney transplants. At CMCS Health We are associated with the best and most experienced Kidney transplant surgeons and the best kidney transplant hospitals in India.
Who can be a living donor for a Kidney transplant needing patient in India?
A healthy blood-related family member usually a son or daughter/parents, grandparents and grandchildren, and brothers and sisters are considered blood relations. The donor needs to be a major in the age group of 18-55 years preferably and healthy enough to donate one of his kidneys, without any risk to his quality of life post-donation. Prelim tests for the fitness and compatibility of donors are done for screening and choosing the correct donor for a successful kidney transplant. Any other relative is considered an unrelated donor and certain documents are needed to prove to the Government of India-appointed organ transplant committee that the donor is related to the patient requiring kidney transplant. And donor is willing to donate one of his kidneys to the patient out of love and family bonding and not under any pressure or monetary obligations.
What happens to a Living Donor after a successful Kidney Donation?
A healthy and fit donor lives a perfectly normal life post the donation of one of his kidneys. The doctors do advise him on certain do's and do not post-donation. Anything that is not good for the health of a person with both kidneys functioning normally is also considered bad for the live donor. Regular and periodic checkups are suggested for a live donor. As high blood pressure and diabetes are considered two major causes of kidney function going bad, the donor is advised to follow a healthy lifestyle to remain disease-free.
Does live donors have a health risk or compromised life post-kidney donation?
A healthy donor lives a perfectly normal life, post-donation. Donation of a kidney does not hurt overall life or quality of life for the donor. Selecting the right donor is important as it cuts down the cost of dialysis and the need for frequent admission of patients till the time we get approval from the government of India-appointed transplant committee for kidney transplants. Once the approval is given by the Committee, the patient is given a date and time for surgery. The following tests for donors are required to lessen the chances of flying in the wrong donor and save time and money for guests till we fly in the right donor.
1. Urine ( SPOT), Protein creatinine ratio, LFT (Liver function test), Urea, Creatinine, Sodium(Na), Potassium (K), Blood sugar( Fasting and Postprandial), HBA1C, Calcium (Ca), Phosphate (Po4), Uric Acid, PTH, Lipid profile, Vitamin D level, T3, T4, TSH and LDH.
2. Complete Hemogram, BT, CT, PT, PTTK, and urine routine.
3. Urine culture, CMV-IGG, EBV(CAPSId)_IGG, for MALE patient PSA (if above 50 years of age). for Female patient CA-125 and pap smear.
4. Blood group, HBSAG, Anti HCV antibody, HIV1 & 2, HCV RNA qualitative, Anti-HBS antibody.
5. ECG, Echo/stress echo, Cardiac clearance.
6. Chest X-ray, Ultrasound-whole abdomen, CT (Angio) for renal vessels, DTPA scan, etc.
CMCS Health is a leading medical tourism company in India. We offer medical tourism services such as finding the right doctor, the right hospital, and cost estimation for medical treatment in India for foreign patients. Some of the main countries are Bangladesh, South Africa, Egypt, Kenya, Saudi Arabia, Ethiopia, Nigeria, Uganda, Zambia, Sudan, Dubai, Namibia, Iraq, and so on. We provide free medical assistance aplastic anemia treatment cost, stomach cancer treatment, sickle cell treatment cost, the best hospital for heart valve replacement, heart valve surgery, arthroscopic surgery, bone marrow transplant cost, best liver transplant hospital, brain tumor surgery cost, cosmetic andplastic surgery, heart surgery, kidney transplant cost,spine tumor surgery,cancer treatment cost, lung transplant,liver transplant cost, top knee replacement surgeons, knee replacement surgery cost, top shoulder replacement surgeons, hip replacement surgery cost, best bone marrow hospital, etc. If you are searching for free medical and healthcare consulting to find the best hospitals and top doctors and surgeons in India for any treatment then contact us- Cmcshealth.com.
Source: https://cmcshealth1.blogspot.com/2024/11/living-donor-kidney-transplant-in-india.html
0 notes
Text
Hydronephrosis Treatment In Delhi

Many people have never heard of the term hydronephrosis. That’s because it is only prevalent in around 1% of the general population according to a research paper published by Science Direct. Hydronephrosis can affect both children and adults. In fact, it can even affect babies in the womb; this can be found via prenatal ultrasound. The same study by Science Direct observed that 1 in 100 to 200 fetuses suffered from hydronephrosis. Because of this, finding out that you suffer from hydronephrosis and require surgery might seem daunting. But don’t worry about it. You can find hydronephrosis treatment in Delhi without breaking a sweat!
What exactly is it?
Hydronephrosis is a condition wherein one or both of the kidneys swell up. This happens either because of some blockage in drainage system of urineor urine refluxing back in the kidneys which can eventually damage the kidney of child.
Therefore, it is essential that you consult doctor once hydronephrosis has been diagnosed. Once the diagnosis is made child needs to be evaluated in detail. Not all hydronephrosis requires surgical intervention but needs to be monitored closely to avoid any renal damage.
Signs of Hydronephrosis
Here are some of the most commonly known signs and symptoms of hydronephrosis.
Antenatal diagnosis on ultrasound scan.
Urinary tract infection
Pain and lump in the back and the sides.
Urinary symptoms like frequent urination, crying during urination etc.
These signs are particularly useful to suspect hydronephrosis in children. Infants, in particular, can have failure to thrive. If you have suspicion that your child may be suffering from hydronephrosis or has all the signs mentioned above, it might be a good idea to consult a doctor.
Causes of Hydronephrosis
As mentioned above, hydronephrosis is a condition that prevents urine draining from the kidneys, which causes the kidneys to swell up. Hydronephrosis usually develops because of two main causes:
Obstruction in Urinary System
Blockage in the upper ureter (Pelvi-ureteric Junction) or lower ureter (Uretero-vesical junction) or Bladder oulet (Posterior urethral valve) can cause hydronephrosis on one side or both sides.
One of the commonest cause is blockage at ureteropelvic junction. This is essentially the very point (or junction) where the ureter and kidney meet.
Posterior Urethral valves are seen in boys and usually causes bilateral hydronephrosis. This is treated by endoscopic resection surgery. If not treated timely it can cause significant morbidity.
Vesicoureteral Reflux
Another cause of hydronephrosis is the vesicoureteral reflux where the urine flows backward from the bladder to the kidneys via the ureter. This condition is unique because usually the urine should only flow from the kidneys to the bladder- not the other way around.
Hydronephrosis treatment in Delhi
If you’re looking for hydronephrosis treatment in Delhi, then you’ll be happy to know that there’s plenty of options available. Your doctor who, after examination, ask for a few tests. This may include the following:
Blood test
Urine test
Ultrasound Imaging
Voiding Cystourethrogram
Renal Scan (DTPA or DMSA scan)
Combined, these tests examine your kidneys, bladder, Urethra and checks if they’re working fine. The kind of treatment you’ll receive for hydronephrosis depends strictly on how severe the condition is.
Some of the causes are self-limiting and may need just close observation with regular testings. Hydronephrosis causing recurrent urinary infections or deterioration of renal functions might require surgical intervention.
However, we do not recommend that you go with this approach as it can even lead to your mild case developing into a severe case of hydronephrosis, which will need surgery. Hydronephrosis surgery cost depends solely on how critical the situation is.
However, you should not look at hydronephrosis surgery costs when looking to treat the disease. As we mentioned, it’s not life-threatening at the same time living with hydronephrosis can severely impact your quality of living. So don’t wait it out!
#cause of hydronephrosis#hydronephrosis surgury#hydronephrosis treatment in delhi#signs of hydronephrosis
1 note
·
View note
Text
Best Nuclear Medicine Treatment in Trivandrum, India | KIMSHEALTH Hospital
Nuclear medicine is a medical specialty involving the application of radioactive substances in the diagnosis and treatment of disease

Procedures & Treatments
Nuclear medicine, in a sense, is “radiology done inside out” or “endoradiology” because it records radiation emitting from within the body rather than radiation that is generated by external sources like X-rays. In addition, nuclear medicine scans differ from radiology as the emphasis is not on imaging anatomy but the function and for such reason, it is called a physiological imaging modality.
Single Photon Emission Computed Tomography or SPECT and Positron Emission Tomography or PET scans are the two most common imaging modalities in nuclear medicine
HEART:
Myocardial viability PET and SPECT
Adenosine Stress perfusion scan
Stress Dobutamine Myocardial MIBI perfusion SPECT
Stress and Rest myocardial perfusion SPECT
MUGA scan
BRAIN:
FDG brain PET CT
F-18 DOPA PET CT
Brain perfusion SPECT
Ictal and interIctal SPECT
Trodat SPECT
Tumour Viability Study
SKELETAL SYSTEM:
Three Phase Bone scan
Whole body Bone scan
F18 Fluoride Bone PET CT.
FDG PET prosthesis/infection Imaging.
Graft viability imaging
GASTROINTESTINAL:
Salivary scan
GE Reflux scan
Gastric Emptying Time
RBC — GI Bleed scan
Meckel’s scan
Whole body DOTA PET CT
HEPATOBILIARY/LIVER — SPLEEN:
Liver Spleen scan
RBC Blood pool scan
Hepatobiliary (HIDA) scan
MAA Sunt
GENITOURINARY:
Diuretic DTPA Renal scan
GFR Estimation
EC Renal scan (ERPF)
DMSA Cortical Renal scan
Captopril Renal scan
VU Reflux study
Renal Transplant study
Lymphoscintigraphy for Chyluria
Whole body PSMA PET CT
ENDOCRINE:
Technetium Thyroid scan
MIBI Thyroid scan
MIBI Parathyroid Scan
MIBG scan
Octreotide SPECT CT
ONCOLOGY:
Whole body FDG PET CT
Whole body Gallium 68 DOTA scan
Whole body Gallium 68 PSMA scan
F-18 Choline PET CT
Whole body iodine scan
Post therapy scan
F-18 DOPA PET CT
Senthinal lymphoscintrigrapy
Scintimammography
HSA scan for protein leak
INFECTION IMAGING:
Whole body FDG PET infection Imaging
Gallium 67 scan
99mTc Ubiquicidin Imaging
RESPIRATORY:
Lung Perfusion Scan
Ventilation — Perfusion (V/Q) scan
Quantitative lung ventilation
Mucociliary clearance study
Ventilation
BLOOD:
Lymphoscintigraphy for Lymphoedema.
Sentinel Node Mapping
RADIONUCLIDE THERAPY:
Radio lodine treatment for Thyrotoxicosis ( < 10 mci)
Radio lodine treatment for Thyrotoxicosis ( > 10 mci)
Radioiodine therapy for Ca. Thyroid ( <100 mci )
Radioiodine therapy for Ca. Thyroid ( >100 mci )
rTSH Radioiodine therapy for Ca thyroid
177 Lutetium DOTA therapy for Neuroendocrine tumors.
177 Lutetium PSMA therapy for Ca. Prostate
Samarium Skeletal Pain Palliative Therapy
90 Yttrium Radiation Synovectomy.
131 Iodine Lipidiol TARE therapy for HCC.
90 Yttrium Lipidiol TARE therapy
Strontium 89 skeletal pain palliative therapy
PET SCAN (OUTSIDE ) REVIEW
CT CONTRAST (PET CT)
omnipaque
visipaque
oral contrast (PET CT)
RBC BLOOD POOL
F CHOLINE
0 notes
Photo

Grecian Super Speciality Hospital is proud to add the most advanced PET/CT Scan in its fleet of services. Bringing high-quality care to more patients. We offer PET CT Scan, MRI Scan, CT Scan at the best price. All Facilities Under one Roof ➤ Fully Automated Labs ➤ High-Quality Images ➤ Latest Technology and Equipment ➤ Scans Report Same Day ➤ Book an online appointment and get your Test Scan Today! 6283705192.
#PET CT Scan#pet scan cancer#pet scan price#pet scan for breast cancer#whole body pet ct scan#dtpa renal scan#whole body bone scan#bone scan#thyroid scan#grecian hospital
0 notes
Text
How Does Contrast Affect The Kidney?

In current medicine, the use of imaging tests has been widely extended as a fundamental support for both the diagnosis and therapeutics of different pathologies. DTPA renal scan provide a great deal of information; they are mostly non-invasive or minimally invasive and have good cost-effectiveness.
More Info: https://www.3hcare.in/how-does-contrast-affect-the-kidney
#dtpa renal scan#dtpa renal scan cost#dtpa renal scan for kidney function test#kft test cost#kidney function test
0 notes
Link
Know what you can expect during your Renal DTPA Scan.
0 notes
Text
Renal Function: What Tests to Perform?
The functioning of the kidneys is one of the most complicated subjects to study as they are involved in many notions of chemistry and physiology. For this reason, the two posts that follow on the topic will fly over the technical ideas behind what will be said. Referred to this
Kidney Test: Kidney is one of the most critical parts of our body, and it plays a vital role in keeping our good health. The kidney is also called organ. Kidney filter out the filth and waste in the blood and exits through the urine. Cleansing the blood is the primary function of the kidney.
Kidney works to maintain the level of water and all types of mineral elements in the body. The organ is helpful in maintaining the levels of hormones that keep normal RBCs, Vitamin D and blood pressure in the body. Because of many reasons, kidneys stop working correctly. Doctor kidney function tests to check kidney function. Through this test, all types of kidney function are checked.
What is the Kidney Function Test?
Kidney Function Test is used to find out if all the functions of the kidneys are working correctly in the range of their criteria. Through the DTPA renal scan, Doctor successfully tries to find out the levels of other minerals like creatinine, blood urea and uric acid in the body. The following tests come in the Kidney Function Test -

• Complete Blood Count Test
• Urine test
• Blood urea nitrogen (BUN)
• Level of electrolytes in the blood
• Creatinine examination in the blood
• Glomerular Filtration Rate
When is kidney function test done?
Kidney function test should be done when you are having signs of kidney related diseases. If you have any physical problems given below or have symptoms, then do the Kidney Function Test.
• Bleeding with urine
• Frequent urination
• Pain while piss
Issues at the beginning while piss
• Swelling of the legs and hands
• High blood pressure problem
What to do during Kidney Function Test
While doing kidney function tests, doctors first take blood samples from the patient's body. To make a blood sample, the elastic band or a tight bandage is tied to the patient's side. Now from where to get blood, that part of the hand is cleaned well through antiseptic. After this, the needle is placed in the vein present in that place. Blood sampling is now taken through the needle.
This blood is kept in a vial. Now, this blood bottle is sent to the laboratory ahead for the test. The patient may experience slight pain and prick if needle. As soon as the needle is detached from the vein, the doctor puts the bandage on the part to prevent blood or keep a piece of cotton.
0 notes
Text
Pelvi Ureteric Junction Obstruction
What is Pelviureteric Junction Obstruction ?
It is a blockage or narrowing between the kidney pelvis and the ureter. PUJO impairs drainage of urine and this causes the urine to remain collected in the kidney causing swelling (Hydronephrosis). If it increases progressively then it causes back pressure on kidneys and subsequently affects the renal functions and may lead to a non functioning kidney.
How common is PUJ obstruction?
About 1 in 1500 childran have PUJ obstruction from birth (congenital). PUJ obstruction is one of the conditions that can cause hydronephrosis, which is the most common condition found in prenatal ultraound.
What are the symptoms of PUJ obstruction?
Sometimes there aren’t any outward symptoms of PUJ obstruction and it is only found when an ultrasound shows that the kidneys are swollen. This is called hydronephrosis. Some children may experience back or side (flank) pain, or a urinary tract infection (UTI). Some children experience pain that comes and goes.
How diagnosis of PUJ obstruction is confirmed ?
The diagnosis of PUJ obstruction is confirmed by a study called a DTPA scan. A DTPA scan shows how well the kidneys are working and also about the severity of blockage.
How is PUJ obstruction treated ?
The treatment for a PUJ obstruction depends on severity of the blockage. Blockages that are mild, appear to be stable or are improving over the time, will be monitored with ultrasound.
Blockage that are more severe or worsening can cause permanent kidney damage. These obstruction require a surgery to remove the portion of the blocked ureter. The surgery is called as pyeloplasty.
What is Pyeloplasty?
Pyeloplasty is the pocedure of choice for PUJ obstruction. The surgery involves removing the PUJ obstruction and joining the kidney pelvis onto the ureter (pyeloplasty). It has good results. This can be acheived through a traditional surgery (‘open pyeloplasty’) or by keyhole surgery (‘laparoscopic pyeloplasty’).
What can I expect after surgery?
The child needs to stay in the hospital for 1 to 2 days and then is called after 5 days for removal of the dressing. A tube called stent is placed in the ureter at the time of surgery to keep the ureter open and draining while it heals. Stents are temporary and need to be removed after 4-6 weeks after the surgery. Removing the stent is a day care surgery and is removed with a scope passed through the urethra into the bladder.
Tags- best pediatric urologist in delhi best pediatric urologist in india best pediatric surgeon in india
#best pediatric urologist in delhi#best pediatric urologist in india#best pediatric surgeon in india
0 notes
Text
Hydronephrosis Treatment In Delhi - Dr Prashant Jain
Hydronephrosis Surgery
Many people have never heard of the term hydronephrosis. That’s because it is only prevalent in around 1% of the general population according to a research paper published by Science Direct. Hydronephrosis can affect both children and adults. In fact, it can even affect babies in the womb; this can be found via prenatal ultrasound. The same study by Science Direct observed that 1 in 100 to 200 fetuses suffered from hydronephrosis. Because of this, finding out that you suffer from hydronephrosis and require surgery might seem daunting. But don’t worry about it. You can find hydronephrosis treatment in Delhi without breaking a sweat!
What exactly is it?
Hydronephrosis is a condition wherein one or both of the kidneys swell up. This happens either because of some blockage in drainage system of urineor urine refluxing back in the kidneys which can eventually damage the kidney of child.
Therefore, it is essential that you consult doctor once hydronephrosis has been diagnosed. Once the diagnosis is made child needs to be evaluated in detail. Not all hydronephrosis requires surgical intervention but needs to be monitored closely to avoid any renal damage.
Signs of Hydronephrosis
Here are some of the most commonly known signs and symptoms of hydronephrosis.
Antenatal diagnosis on ultrasound scan.
Urinary tract infection
Pain and lump in the back and the sides.
Urinary symptoms like frequent urination, crying during urination etc.
These signs are particularly useful to suspect hydronephrosis in children. Infants, in particular, can have failure to thrive. If you have suspicion that your child may be suffering from hydronephrosis or has all the signs mentioned above, it might be a good idea to consult a doctor.
Causes of Hydronephrosis
As mentioned above, hydronephrosis is a condition that prevents urine draining from the kidneys, which causes the kidneys to swell up. Hydronephrosis usually develops because of two main causes:
Obstruction in Urinary System
Blockage in the upper ureter (Pelvi-ureteric Junction) or lower ureter (Uretero-vesical junction) or Bladder oulet (Posterior urethral valve) can cause hydronephrosis on one side or both sides.
One of the commonest cause is blockage at ureteropelvic junction. This is essentially the very point (or junction) where the ureter and kidney meet.
Posterior Urethral valves are seen in boys and usually causes bilateral hydronephrosis. This is treated by endoscopic resection surgery. If not treated timely it can cause significant morbidity.
Vesicoureteral Reflux
Another cause of hydronephrosis is the vesicoureteral reflux where the urine flows backward from the bladder to the kidneys via the ureter. This condition is unique because usually the urine should only flow from the kidneys to the bladder- not the other way around.
Hydronephrosis treatment in Delhi
If you’re looking for hydronephrosis treatment in Delhi, then you’ll be happy to know that there’s plenty of options available. Your doctor who, after examination, ask for a few tests. This may include the following:
Blood test
Urine test
Ultrasound Imaging
Voiding Cystourethrogram
Renal Scan (DTPA or DMSA scan)
Combined, these tests examine your kidneys, bladder, Urethra and checks if they’re working fine. The kind of treatment you’ll receive for hydronephrosis depends strictly on how severe the condition is.
Some of the causes are self-limiting and may need just close observation with regular testings. Hydronephrosis causing recurrent urinary infections or deterioration of renal functions might require surgical intervention.
However, we do not recommend that you go with this approach as it can even lead to your mild case developing into a severe case of hydronephrosis, which will need surgery. Hydronephrosis surgery cost depends solely on how critical the situation is.
However, you should not look at hydronephrosis surgery costs when looking to treat the disease. As we mentioned, it’s not life-threatening at the same time living with hydronephrosis can severely impact your quality of living. So don’t wait it out!
For More Info.(http://www.pedsurgerydelhi.com/)
Tag = best pediatric urologist in india, best paediatric surgeon in Delhi, hydronephrosis in child treatment delhi, vesicoureteral reflux surgery child in delhi
#best pediatric urologist in india#best paediatric surgeon in Delhi#hydronephrosis in child treatment delhi#vesicoureteral reflux surgery child in delhi
0 notes
Video
youtube
Kidney failure treatment in Ayurveda by Karma Ayurveda
Karma ayurveda under the supervision of Dr Puneet Dhawan developed an #ayurvedic_medicine for #kidney_failure_treatment .It was a result of long and extensive research carried out by 5th generations of dr puneet dhawan as a result of which major improvements were noticed in GFR(Renal scan DTPA) of patients suffering from kidney failure diseases.
#kidney disease treatment#]stop kidney dialysis#kidney care by ayurvedic medicine#chronic kidney disease treatment
16 notes
·
View notes
Text
Work updates
I work an 8-5 job now, for the first time ever in my life.
No oncalls, no nasty early morning rounds, no patients bugging you to be discharged early. It is a decent 8-5 job, normal, human hours.
After finishing housemanship, A and I were pretty set on pursuing emergency. We spent half a year in that department and was getting pretty confident at it. The hours weren’t so bad, the environment was not toxic, so emergency it is. If that didnt work out, second on the list is paeds. But then if we couldn’t get our main choices, we don’t see a point in sacrificing our time and soul into something we’d be half heartedly invested in.
So that’s where the kinder options came in. I scrolled through the list of departments we can apply for and saw the word nuclear medicine. Heard of it once during med school, second was when i bumped into a nuclear med guy who was too happy and healthy I actually asked where he came from. Clinical people don’t look like that- happy, contented, fresh.
In life I’ve learnt that we can only plan so much, and afterwards we just have to let God. So when i actually got into nuclear med instead of ED, i was surprised to feel a lightness in my chest. Something in me really thought I wanted ED, but also inside, my heart was at peace when i got nuclear med.
So Alhamdulillah for that. But mind you this job comes with challenges on its own. To put it simply, nuclear medicine is the department that does all your fancy scans that involve a nuclear radiopharmaceutical. We got technetium-99, bind it with something that goes to something, and then our camera can capture where those things go, and we interpret the image. To name a few, bone scans, your heart stress test, renal dtpa and mag 3, radio- iodine ablation. As a houseman, the most familiar you can be with this is sending a request form for it.
“OMG banyaknya cancer dia!”
“That is physiological tracer uptake with gi and urinary clearance, faizah.”
*image from google. script from real life experience.
** SOBS IN RADIOISOTOPE T.T
That, is how familiar I am with this new thing, literally sending a form for it. So I am now an MO, who has no idea in this new department, and everything throughout the hellish 2 years of housemanship, makes very little sense here. Basically I’m starting from scratch all over again. This new beginning is humbling, though radioactive, it is the least toxic place I’ve been to. People here are kind, haven’t met a single bad one yet. It’s new, it will take some getting used to, but it is worth a shot.
The other day on our 2 hour car ride home, A and I talked about how this balance we newly gathered in our life, felt odd. It didn't felt as satisfying as coming back from an ED shift; you didn't bring a dead guy back to life, there was no mystery that you’ve uncovered, you didn't solve a tricky diagnosis, you are just- scanning.
But then we concluded that we humans are always ungrateful. Back when we were practically walking zombies 2 months back from a hefty shift, all we wanted is what we have today. And now that you got what you were asking for, you missed the old life you had.

- we went for a little sight seeing during our lunch break. Like omg, did i even say that right, lunch break. lol.
0 notes
Text
Acute Hydrothorax Diagnosed Through Scintigraphy in a Patient on Peritoneal Dialysis- Juniper Publishers

Abstract
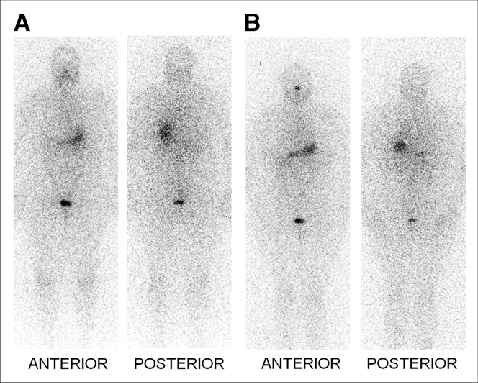
Acute hydrothorax after peritoneal dialysis (PD) is uncommon. Differential diagnoses of various clinical conditions that can result in pleural effusions are necessary. Erroneous diagnoses and subsequent management not only increase the time required for resolving a problem but also deteriorate a patient’s clinical condition. We report the case of a 55-year-old woman who received regular PD due to chronic renal failure. She experienced diffused abdominal pain 2 hours after PD. Furthermore, dyspnea developed the following morning. A chest plain film revealed a massive right-sided pleural effusion. Peritoneo-pleural communication caused by a diaphragmatic defect was diagnosed rapidly using lung perfusion scintigraphy.
Case presentation
Our patient, a 55-year-old woman, had a history of hypertension and chronic glomerulo-nephritis-related uremia. She had undergone peritoneal dialysis (PD) catheter insertion in September 2014 and started receiving continuous ambulatory peritoneal dialysis (CAPD) twice daily 1 month after catheter insertion. She experienced intermittent abdominal pain 3 months after the insertion. No fever or dyspnea were noted with the pain. However, a decrease in ultrafiltration volume or rate after the PD session was noted by the patient herself. A review of her medical history did not reveal recent trauma to the chest or previous diaphragmatic surgery. However, shortness of breath was noted 1 day later; hence, she presented to the emergency department (ED). Tachycardia (104bpm) and elevated blood pressure (185/111mmHg) were noted in triage, and her respiratory rate was 22 breaths/min with 98% oxygen saturation. No chest pain or abnormal findings in the electrocardiogram were noted during her ED stay. Laboratory results did not reveal leukocytosis or acidosis. A chest X-ray revealed a massive right-sided pleural effusion (Figure 1). Pleurocentesis was suggested, but the patient refused. We analyzed the dialysate instead of a sample of the pleural effusion fluid; no evidence of infection was found. We arranged lung perfusion scintigraphy, 5 mCi of Technetium-99m macro aggregated albumin (Tc-99m MAA) was injected into the PD fluids, and a rapid accumulation of radioactivity in the right hemithorax was observed in the images recorded at 30 min and 1 h after PD (Figure 2). Thus, peritoneo-pleural communication (right side) caused by diaphragmatic defect was diagnosed. PD was discontinued immediately and video-assisted thoracic surgery with thoracoscopic diaphragmatic fundoplication and pleurodesis was provided 2 days later. The patient was discharged uneventfully without the recurrence of pleural effusions during a 3-month follow-up.
Discussion
Hydrothorax-related to PD was first reported in 1967 by Edward and Unger [1]. The reported incidence rates of hydrothorax-related PD vary from 1.6% to 10% [2,3]. The incidence rate in new PD patients is <2% [2]. Pleural effusions are usually observed on the right side, presumably because the left side has diaphragmatic protection provided by the heart. Clinical symptoms of pleural effusions include sudden dyspnea, decrease in ultrafiltration rate, and pleuritic chest pain. One study reported that approximately 25% of patients are asymptomatic [4]. In patients with recurrent unilateral pleural effusions or acute respiratory distress after dialysate infusion, trans-diaphragmatic leakage or peritoneal fistulae should be considered. When transudative pleural effusions are confirmed using Light’s criteria in patients receiving PD, pleural effusion glucose levels can aid diagnosis. Some authors use a cutoff point of 300mg/dL of pleural effusion glucose for diagnosis [5], whereas others consider a pleural-fluid-to-serum (PF-S) glucose gradient of >50mg/dL, with a sensitivity of 100%, as an indicator [6]. A relatively objective measurement revealed that a PF-S glucose ratio of >1 is consistent with pleuroperitoneal communication because all other causes of transudative pleural effusions have similar or lower glucose concentrations in the pleural fluid compared with the serum (ratios of ≤1) [7]. Any image survey alone is insufficiently sensitive for detection. In most cases, peritoneo-pleural fistulae are diagnosed through scintigraphy or radionuclide scanning (for example, Tc-99m DTPA), with sensitivities of only 40% to 50% [8,9]. However, patients receiving CAPD who present with acute shortness of breath or recurrent unilateral pleural effusions should be examined through peritoneal scintigraphy to eliminate the possibility of a pleuro-peritoneal leak. Several therapeutic approaches can be adopted, including temporary discontinuation of PD, tetracycline instillation into the pleural space, and surgical patch grafting of the diaphragmatic defect. The strategy required to manage the effusion depends on the clinical condition of the patient; however, in all cases, immediate interruption of the PD is required. Surgical intervention was provided to this patient because she showed rapid accumulation of radioactive material in the right hemithorax.
Conclusion
In patients who receive regular PD, sudden accumulation of pleural effusion can be diagnosed by minimal invasive scintigraphy instead of pleural effusion tapping. Rapid diagnosis can help us decide whether to discontinue PD to prevent deterioration.
For more Open access journals please visit our site: Juniper Publishers
For more articles please click on Journal of Complementary Medicine & Alternative Healthcare
0 notes
Photo

PET CT Scan in Mohali - Grecian Hospital
Grecian Super Speciality Hospital is proud to add the most advanced PET/CT Scan in its fleet of services. Bringing high-quality care to more patients, our recent addition Siemens Biograph HorizonTM offers the flexibility to address a wide variety of clinical indications while introducing new efficiencies.
#pet ct scan#pet scan cancer#pet scan price#pet scan for breast cancer#whole body pet ct scan#dtpa renal scan#whole body bone scan#bone scan#thyroid scan
0 notes
Link
Kidney diseases evolve silently. Hence the importance of regularly performing blood and urine tests to check that his kidneys are working well. What are the different renal function parameters that appear on the test results?
More Info: https://www.3hcare.in/kidney-diseases-and-their-tests
0 notes
Video
youtube
(via https://www.youtube.com/watch?v=Aij7z0fJpT8)
Karma ayurveda under the supervision of Dr Puneet Dhawan developed an ayurvedic medicine for kidney failure.It was a result of long and extensive research carried out by 5GENERATIONS of dr puneet dhawan as a result of which major improvements were noticed in GFR(Renal scan DTPA) of patients suffering from kidney diseases. Research and Development Company under the leadership of Dr. Puneet Dhawan is actively engaged in research based ayurvedic medicines for kidney,as a result of which kidney cells gets rejuvenated with time. providing you a new life with a revived kidneys.
0 notes