#diabetic foot therapy
Explore tagged Tumblr posts
Text
Website : https://www.laserpodiatryassociates.com/
Address : 1604 Ridgeside Dr # 202, Mt Airy, MD 21771
Phone : +1 301-829-5111
Laser Podiatry Associates understands that if your feet hurt then your entire body suffers. Dr. Jennifer E. Mullendore is Board Certified by the American College of Foot and Ankle Surgeons and has a Doctorate of Podiatric Medicine. Our treatment options include minimally invasive techniques and procedures, endoscopic techniques and procedures, innovative therapies, and state-of-the-art technology.
Business Mail : [email protected]
#Ankle Pain#Bunions#Calluses#Corns#Diabetic Foot Care#Endoscopic Techniques#Foot and Ankle Ailments#Foot Injury#Foot Pain#Health & Wellness#Heel Pain#Ingrown Toenails#Innovative Therapies#Laser Podiatry#Laser Podiatry Associates#Podiatry#Warts
2 notes
·
View notes
Text
How Sydney Foot Clinics Are Tackling Common Mobility Issues
Mobility issues, especially those related to the feet, are increasingly common as people age or experience conditions like diabetes, arthritis, or sports injuries. These problems can impact daily activities, making it difficult to move around comfortably. Foot specialist Sydney clinics are at the forefront of addressing these challenges, offering effective solutions to enhance mobility and overall foot health. From pain relief to improved posture, foot clinics in Sydney play a crucial role in helping individuals regain their independence and live a more active lifestyle. This article will explore how foot specialists in Sydney are tackling common mobility issues and providing valuable care for those in need.

1. Addressing Common Foot Conditions Affecting Mobility
Many people suffer from foot conditions that directly affect their ability to walk, stand, or engage in physical activities. These issues range from structural problems to chronic pain conditions. A foot specialist Sydney provides a variety of treatments to address these common foot-related mobility issues.
✔️ Plantar Fasciitis: This condition involves inflammation of the tissue at the bottom of the foot, leading to sharp heel pain. Foot specialists offer treatments like custom orthotics, stretches, and physical therapy to relieve pain and improve mobility.
✔️ Flat Feet: People with flat feet often experience discomfort, especially when standing or walking for long periods. Foot specialists design custom arch supports to provide proper alignment and prevent further strain on the feet, ankles, and knees.
✔️ Arthritis: Arthritis can cause pain, swelling, and stiffness in the joints, including those in the feet. Foot specialist Sydney clinics use techniques like joint mobilisation, pain management strategies, and specific footwear recommendations to alleviate symptoms and improve mobility.
✔️ Bunions and Hammertoes: These deformities can make walking uncomfortable and affect the overall alignment of the foot. Foot specialists offer conservative treatments like padding, orthotics, or surgery if necessary to restore foot function.
By identifying and treating these common foot conditions, foot specialists in Sydney help individuals improve their mobility and regain comfort in their daily activities.
2. Customised Footwear and Orthotics for Better Support
A significant part of improving foot mobility involves ensuring that the feet are supported correctly. Foot specialists Sydney offer custom footwear and orthotics designed to improve posture, alleviate pain, and enhance movement.
✔️ Custom Orthotics: These are custom-made shoe inserts that provide support and cushioning. For individuals with conditions like flat feet, plantar fasciitis, or diabetic foot issues, orthotics can redistribute pressure, correct alignment, and reduce strain.
✔️ Footwear Recommendations: Wearing the right shoes is essential for proper foot health. Foot specialists evaluate the structure of your feet and recommend appropriate shoes that provide the necessary support, cushioning, and flexibility.
✔️ Sports Injury Recovery: Athletes and active individuals can benefit from custom orthotics designed to improve performance and prevent injury. These orthotics provide stability and prevent excessive pressure on specific areas of the feet.
By providing tailored orthotics and footwear solutions, foot specialists in Sydney ensure that individuals have the proper support they need to maintain mobility and avoid further injury.
3. Non-Surgical Treatments for Improved Mobility
For many people with mobility issues, surgery is not always the first option. Foot specialist Sydney clinics offer a range of non-invasive treatments that can relieve pain, improve mobility, and restore function without the need for surgery.
✔️ Shockwave Therapy: This therapy uses high-energy sound waves to treat conditions like plantar fasciitis, Achilles tendonitis, and other soft tissue injuries. Shockwave therapy stimulates healing and reduces pain, making it easier to move around.
✔️ Physical Therapy and Exercises: Foot specialists often recommend specific exercises to strengthen the muscles of the foot and ankle, improve flexibility, and enhance overall mobility. These exercises help alleviate pain, prevent injury, and improve foot function.
✔️ Podiatric Massage: Therapeutic massage can relieve tension, reduce swelling, and improve blood flow to the feet and lower limbs. This treatment is particularly beneficial for those with circulation issues or chronic foot pain.
✔️ Cryotherapy: Cold therapy is used to reduce inflammation and numb pain in specific areas of the foot. Cryotherapy is effective for treating acute injuries and providing relief from chronic conditions like arthritis.
These non-surgical treatments, provided by foot specialists in Sydney, are effective for managing and improving mobility without the risks associated with invasive procedures.

4. Diabetic Foot Care: A Key Focus for Improved Mobility
Diabetes can significantly impact foot health, leading to nerve damage, poor circulation, and an increased risk of infections. Foot specialist Sydney clinics are equipped to handle diabetic foot care, ensuring that individuals with diabetes maintain proper foot health and prevent complications that could impair mobility.
✔️ Regular Foot Exams: Individuals with diabetes should have their feet examined regularly by a foot specialist to check for any signs of infection, ulcers, or nerve damage. Early detection is critical in preventing more serious issues.
✔️ Wound Care and Ulcer Management: If foot ulcers or wounds develop, foot specialists in Sydney provide wound care, dressings, and proper treatment to promote healing and prevent infection.
✔️ Preventive Foot Care: Foot specialists provide education on proper foot hygiene, the importance of wearing well-fitting shoes, and how to monitor foot health daily to avoid complications.
Proper diabetic foot care is essential for maintaining mobility and preventing long-term issues. Foot specialists in Sydney offer the expertise and care needed to ensure individuals with diabetes can enjoy a high quality of life.
Conclusion
Foot specialists in Sydney play a crucial role in managing and improving mobility for individuals facing foot-related issues. Through customised treatments, non-invasive therapies, and expert care, they help individuals regain comfort, prevent further complications, and enhance overall foot health. With the right support, anyone can improve their mobility and enjoy a more active and pain-free lifestyle.
FAQs
1. What types of mobility issues can foot specialists treat? Foot specialists can treat a wide range of mobility issues, including plantar fasciitis, arthritis, flat feet, bunions, hammertoes, and sports injuries. They also provide custom orthotics and footwear solutions to improve mobility. Learn More About Foot Specialist Sydney.
2. Are custom orthotics necessary for everyone with foot pain? Custom orthotics are often recommended for individuals with specific foot conditions like flat feet, plantar fasciitis, or arthritis. They provide support and help relieve pressure, but they are not necessary for everyone. Your foot specialist will assess your needs.
3. How often should I visit a foot specialist? The frequency of visits depends on the severity of your foot condition and whether you have ongoing issues. For individuals with diabetes or chronic foot pain, regular check-ups are recommended to monitor and manage foot health.
4. Can foot specialists provide relief from diabetic foot pain? Yes, foot specialists are trained to manage diabetic foot pain by providing tailored care, including wound care, exercises, and proper footwear recommendations. Early intervention can help prevent serious complications.
5. What is shockwave therapy and how does it help with foot pain? Shockwave therapy uses high-energy sound waves to stimulate healing in soft tissue injuries like plantar fasciitis and Achilles tendonitis. It helps reduce pain and improve mobility by promoting blood flow and tissue regeneration.
#Orthotics Sydney#Ingrown Toenail Treatment Sydney#Shockwave Therapy Sydney#Heel Pain Specialist Sydney#Sports Podiatry Sydney#Foot Specialist Sydney#Foot Doctor Sydney#Diabetic Foot Care Sydney
0 notes
Text
#Diabetes treatment in Madurai#Diabetes specialist Madurai#Endocrinology services Madurai#Insulin therapy Madurai#Blood sugar management Madurai#Diabetic foot care Madurai#Gestational diabetes care Madurai#Pediatric diabetes treatment Madurai#Type 1 diabetes treatment Madurai#Type 2 diabetes treatment Madurai.
0 notes
Text
Global Negative Pressure Wound Therapy (NPWT) Devices Market Is Estimated To Witness High Growth Owing To Rising Prevalence of Chronic Wounds and Increase in Surgical Procedures

The global Negative Pressure Wound Therapy (NPWT) Devices market is estimated to be valued at USD 2,288.1 million in 2022 and is expected to exhibit a CAGR of 6.5% over the forecast period 2022-2030, as highlighted in a new report published by Coherent Market Insights.
Market Overview:
Negative Pressure Wound Therapy (NPWT) Devices are used in the treatment of chronic wounds such as diabetic foot ulcers, pressure ulcers, and venous leg ulcers. These devices create a vacuum environment around the wound, promoting faster wound healing and preventing infection. NPWT devices are widely used in hospitals, clinics, and home healthcare settings. The increasing prevalence of chronic wounds and the rise in surgical procedures are driving the demand for NPWT devices globally.
Market Dynamics:
One of the key drivers of the NPWT devices market is the rising prevalence of chronic wounds. According to the World Health Organization (WHO), around 9% of adults over the age of 60 suffer from chronic wounds. Additionally, the increasing incidence of diabetes, obesity, and other chronic diseases further contribute to the growing demand for NPWT devices.
Another driver is the increase in surgical procedures worldwide. With advancements in healthcare facilities and accessibility to healthcare services, the number of surgeries performed has significantly increased. NPWT devices are extensively used in surgical wound management, leading to increased adoption of these devices.
Market Key Trends:
One key trend observed in the NPWT devices market is the integration of advanced technologies such as telehealth and wearable devices. These technologies enable remote monitoring and real-time data collection, enhancing patient care and reducing hospital visits. For instance, Medela AG's Vario 18 and Medela LifeSense systems offer telehealth capabilities for effective wound management.
SWOT Analysis:
- Strength: Growing demand for Negative Pressure Wound Therapy (NPWT) Devices Market in the treatment of chronic wounds, Increasing adoption of advanced technologies in wound care.
- Weakness: High cost of NPWT devices, Lack of reimbursement policies in certain regions.
- Opportunity: Untapped potential in emerging markets, Increasing investments in research and development for innovative NPWT devices.
- Threats: Stringent regulatory guidelines, Competition from alternative wound care therapies.
Key Takeaways:
The global NPWT devices market is expected to witness high growth, exhibiting a CAGR of 6.5% over the forecast period, due to increasing prevalence of chronic wounds and rise in surgical procedures. North America is currently the fastest growing and dominating region in this market, attributed to the well-established healthcare infrastructure, high healthcare expenditure, and favorable reimbursement policies. The key players operating in the global NPWT devices market include 3M, Cardinal Health, Smith+Nephew, Genadyne, DeRoyal Industries, Inc., Medela AG, Convatec Inc., Mölnlycke Health Care AB, PAUL HARTMANN AG, ATMOS MedizinTechnik GmbH & Co. KG, Talley Group Ltd, Cork Medical, LLC, and Devon Medical Products.
In conclusion, the global NPWT devices market is poised for substantial growth in the coming years due to the increasing prevalence of chronic wounds and the rise in surgical procedures. The integration of advanced technologies and the focus on telehealth and wearable devices are key trends shaping the market. However, challenges such as high costs and lack of reimbursement policies need to be addressed. With the expanding geriatric population and the growing burden of chronic diseases, the demand for NPWT devices is expected to soar, presenting lucrative opportunities for market players.
#Negative Pressure Wound Therapy (NPWT) Devices Market#Negative Pressure Wound Therapy (NPWT) Devices Market GRowth#Negative Pressure Wound Therapy (NPWT) Devices Market Insights#Negative Pressure Wound Therapy (NPWT) Devices Market Forecast#Negative Pressure Wound Therapy (NPWT) Devices Market Values#Coherent Market Insights#granulation tissue#chronic wounds#Diabetic foot ulcers
0 notes
Text
Poor Circulation: The Hidden Culprit Behind Chronic Pain, Fibromyalgia, Neuropathy, and More

Poor circulation is a common but often overlooked cause of chronic pain, fibromyalgia, neuropathy, and other conditions. A recent estimate suggests that 8 million Americans have peripheral artery disease (PAD). Poor circulation is a major causative agent and results from conditions such as diabetes, hypertension, and obesity. In this article, we will explore the link between poor circulation and chronic pain and discuss ways to improve circulation for better health outcomes.
The Importance of Proper Blood Circulation for Optimal Health
Proper blood circulation is crucial for overall health and well-being. The body’s ability to heal itself and maintain optimal functioning is compromised without proper blood circulation. We will explore the importance of proper blood circulation and its connection to chronic pain, fibromyalgia, neuropathy, the autonomic nervous system, and cellular oxygenation.
Causes and Symptoms of Poor Microcirculation
When the capillaries and other tiny blood channels aren’t doing their job, we have poor microcirculation. Autonomic dysfunction, neuropathy, and persistent pain are only some of the consequences of this condition.
Common factors that lead to insufficient blood flow to the tissues are:
Cigarette smoking.
Insufficient physical activity, especially in the legs and feet, has been linked to impaired circulation [4].
Poor circulation can be a symptom of diabetes.
Hypertension.
Poor blood flow, especially to the legs and feet, is a common symptom of peripheral artery disease.
Varicose veins are a medical condition characterized by the appearance of enlarged, tortuous veins in the legs and feet.
Inadequate microcirculation may manifest as:
Inadequate circulation can lead to a chill in the extremities, such as the hands and feet.
Sensations of numbness or tingling in the hands and feet can result from decreased blood flow.
Embolization: Fluid accumulation in the legs and feet is a common symptom of poor circulation.
Pain in the legs, foot, and back can be caused by poor circulation and be classified as chronic.
Low energy and exhaustion are also symptoms of poor circulation, which in turn can diminish the body’s oxygen supply.
The Immune System: White Blood Cell Sub-types and Its Functions
Leukocytes, or white blood cells, act as the body’s defense mechanism known as the immune system. Listed below are the types of white blood cells and their role in immunity:
Most white blood cells are neutrophils, the most common kind. They assist the body in fighting off germs and other intruders by swallowing them whole and killing them.
Lymphocytes aid in the immune system’s detection and elimination of foreign invaders. Lymphocytes can be broken down into two categories. While T cells assist in coordinating the immune response and directly target diseased cells, B cells create antibodies that detect and attach to specific infections.
Monocytes scavenge the body for broken down or dead cells and other waste. In addition to aiding in infection prevention, they aid in defense by enveloping and killing off potential pathogens.
Eosinophils aid in the fight against parasites and other pathogens. In addition, they have a role in allergic reactions.
Basophils have a role in allergic reactions. They cause an increase in inflammation and other allergic symptoms by secreting histamine.
When it comes to the body’s defenses against various infections and foreign invaders, white blood cells play a crucial role.
Chronic Pain and Poor Circulation
Millions of people throughout the world deal with chronic pain on a daily basis. It’s defined as pain that lasts longer than three months and can have a major effect on a person’s standard of living. In addition, research has shown that poor circulation often contributes to chronic pain.
Studies have found that people with chronic pain have reduced blood flow and oxygenation to affected areas, leading to inflammation and tissue damage. For example, one study by researchers at the University of Michigan found that people with chronic pain had reduced blood flow to their brain’s thalamus, which is responsible for processing pain signals. This reduced blood flow can increase pain sensitivity and make it more difficult for the body to manage pain effectively [3].
Fibromyalgia and Poor Circulation
Over 5 million people in the United States have fibromyalgia, a disorder that causes widespread, persistent discomfort. Pain, exhaustion, and tenderness in muscles and joints are classic symptoms. In addition, research has shown that people with fibromyalgia often have reduced blood flow to affected areas, which can contribute to the development of the condition.
In a recent study, researchers suggested that people with fibromyalgia had reduced blood flow to their hands compared to healthy individuals. Moreover, this reduced blood flow may contribute to the cold and numb sensations that people with fibromyalgia often experience in their extremities.
Neuropathy and Poor Circulation
Neuropathy is a condition that affects the nerves and can cause tingling, numbness, and pain in the hands and feet. Research has shown that poor circulation can contribute to the development of neuropathy. Diabetic neuropathy reduces foot blood flow, according to a Journal of Diabetes and its Complications study. The researchers suggested that this reduced blood flow may contribute to the nerve damage characteristic of neuropathy [2].
The Role of the Autonomic Nervous System
The autonomic nervous system controls blood flow and circulation. The sympathetic nervous system, which controls the “fight or flight” response, can cause vasoconstriction, reducing blood flow. The “rest and digest” response of the parasympathetic nervous system improves blood flow and relaxation.
Stress and anxiety can cause the sympathetic nervous system to become overactive, leading to poor circulation and chronic pain. Relaxation and parasympathetic nervous system activation, achieved through practices like meditation, yoga, and prayer, can boost circulation and alleviate the symptoms of poor circulation.
Apart from that, the results of a recent study suggested that people with autonomic dysfunction had reduced blood flow to their legs compared to healthy individuals. The reduced blood flow may also contribute to the development of peripheral artery disease. This condition affects the blood vessels that supply blood to the legs and feet [1].
Understanding the Perfusion Index
Peripheral perfusion, or blood flow to the body’s tissues, can be measured non-invasively with the help of a metric called the perfusion index. It is expressed as a percentage and is determined by comparing the pulsatile blood flow with the non-pulsatile blood flow.
In a recent study published in the Annals of the Romanian Society for Cell Biology, researchers aimed to investigate the effectiveness of transdermal carbon dioxide (CO2) in increasing perfusion index in patients with placenta accreta undergoing temporary abdominal aortic cross-clamping. Serious maternal morbidity and mortality can result from placenta accreta, a pregnancy complication. The study, which included 20 participants, shows that transdermal CO2 is effective in enhancing perfusion in those affected by placenta accreta [20].
The findings further emphasize the significance of perfusion in preserving tissue health. Chronic pain, fibromyalgia, and neuropathy are just a few of the disorders that can develop from inadequate blood flow. Increasing perfusion is a proven method for treating these ailments and improving health as a whole.
Transdermal CO2 – A Promising Technology for Improving Perfusion
A customized device is used in transdermal CO2 therapy to supply CO2 to the skin’s surface in a non-invasive manner. The increased perfusion and accelerated healing are the results of the CO2 being absorbed through the skin and into the bloodstream. Many medical issues, such as chronic pain, wound healing, and skin rejuvenation, have benefited from the application of this technique.
Patients with placenta accreta receiving temporary abdominal aortic cross-clamping may benefit from transdermal CO2 therapy, according to the study’s findings. Patients reported no negative reactions to the treatment. The results of this study may have major ramifications for the management of placenta accreta and other disorders where enhanced perfusion is necessary [20].
Transdermal CO2 therapy is a non-invasive, low-risk substitute for invasive, conventional procedures. Patients have the option of self-administering the therapy at home or under medical supervision. Chronic pain, fibromyalgia, neuropathy, and other disorders may all benefit from transdermal CO2 therapy because of its capacity to increase blood flow and speed recovery.
Cellular Oxygenation and Blood Circulation
Proper cellular oxygenation is crucial for optimal health and well-being. When cells do not receive enough oxygen, they can become damaged and die, leading to various health problems. Research has shown that poor blood circulation can lead to reduced cellular oxygenation and contribute to various health conditions.
According to a study in PLOS ONE, researchers claimed that people with peripheral artery disease had reduced oxygen levels in their leg muscles compared to healthy individuals. The researchers suggested that this reduced oxygenation may contribute to the muscle pain and weakness that people with peripheral artery disease often experience [18].
Increasing blood flow to the brain through exercise was found to improve cognitive function in older persons, according to a study published in the American Journal of Physiology-Heart and Circulatory Physiology. The study suggests that proper blood flow and oxygenation to the brain are essential for maintaining cognitive function as we age [15].
Improving Blood Flow
Improving blood flow is key to reducing symptoms associated with poor circulation. In addition, exercise can help increase blood flow to muscles and improve overall cardiovascular health. For example, a Journal of the American Medical Association study mentioned that exercise improved walking distance and reduced leg pain in patients with PAD [10, 14].
One additional effective method of increasing circulation is through massage therapy. Patients with fibromyalgia who received massage therapy reported less pain and increased blood flow, according to research published in the International Journal of Therapeutic Massage and Bodywork [5]. Compression socks and stockings, for example, have been shown to increase circulation to the lower extremities. Compression therapy was found to be useful in reducing PAD symptoms in research published in the Journal of Vascular Surgery [6].
Natural supplements are another option for increasing circulation with the aforementioned techniques. L-arginine is an amino acid that has been shown to increase blood vessel dilatation, making it a potentially useful dietary supplement. L-arginine supplementation was reported to significantly increase blood flow and decrease PAD symptoms in a study published in the Journal of Cardiovascular Pharmacology [7]. Nitric oxide, a gas produced naturally by the body, is another supplement to control blood pressure. Supplemental nitric oxide significantly increased blood flow and decreased blood pressure in hypertensive patients, according to a study published in the Journal of Hypertension [9].
Improving Microcirculation
Microcirculation refers to blood circulation in the smallest blood vessels, including capillaries and arterioles. Improving microcirculation is important for promoting healing and reducing symptoms associated with poor circulation. One way to improve microcirculation is through the use of low-level laser therapy (LLLT), which involves using a low-power laser to stimulate blood flow. The Journal of the Neurological Sciences includes a study that suggests LLLT effectively improves microcirculation and reduces pain in patients with neuropathy [8, 19].
Another review summarizes the results of various clinical research that show how beneficial LLLT is for treating TMD. The clinical data suggest that LLLT can alleviate TMD-related discomfort, enhance jaw function, and reduce inflammation. Patients treated with LLLT showed statistically and clinically significant improvements in pain reduction and joint mobility compared to placebo individuals in one clinical study. LLLT has been shown to reduce pain and enhance function for up to six months after treatment, according to another study. Insights into the possibility of LLLT as a safe and effective therapy option for TMD are provided by the clinical evidence examined in this publication [12, 13].
Improving Cellular Oxygenation
Improving cellular oxygenation is also important for promoting healing and reducing symptoms associated with poor circulation. One way to improve cellular oxygenation is to practice deep breathing exercises, which can help increase blood oxygen levels. For example, a Journal of Rehabilitation Research and Development study mentioned that deep breathing exercises effectively improved oxygen saturation levels in patients with neuropathy [16].
Another way to improve cellular oxygenation is through hyperbaric oxygen therapy (HBOT), which involves breathing pure oxygen in a pressurized chamber. Not just that, researchers also suggested that HBOT effectively reduced pain and improved the quality of life in patients with fibromyalgia in a Journal of Pain Research study [17].
Conclusion
Poor circulation is a common but often overlooked cause of chronic pain, fibromyalgia, neuropathy, and other conditions. Improving blood flow, microcirculation, and cellular oxygenation can help to promote healing and reduce symptoms associated with poor circulation. Exercise, massage therapy, compression therapy, and natural supplements such as L-arginine and nitric oxide can all help to improve blood flow.
Low-level laser therapy and deep breathing exercises can improve microcirculation and cellular oxygenation. In contrast, mind-body therapies can help to activate the parasympathetic nervous system and reduce stress and anxiety. Individuals with chronic pain and other conditions can experience improved quality of life and better health outcomes by taking steps to improve circulation.
Author: Dr. Ubaid khan Published author with expertise in conducting meta-analysis, 20+ publications in PubMed indexed journals, research paper collaboration with neurosurgeons at Mayo Clinic, extensive medical knowledge, clinical experience, and providing exceptional patient care.
1 note
·
View note
Text
A Guide to Choosing between Diabetic Socks and Compression Socks Based on Your Needs
If you have diabetes or poor circulation, it’s possible that you may encounter foot pain, swelling, and even open sores. These conditions can make it a challenge to discover socks that provide both comfort and support. Although you may have come across diabetic socks and compression socks as potential remedies, it’s crucial to comprehend the distinctions between the two before deciding to…

View On WordPress
#are diabetic socks the same as compression socks#Blood circulation#circulation#compression socks#Compression therapy#Diabetes care#Diabetes management#Diabetic foot complications#diabetic socks#edema#foot health#leg swelling#medical socks#neuropathy#Orthopedic socks
0 notes
Text
Good News - July 8-14
Like these weekly compilations? Tip me at $Kaybarr1735! And if you tip me and give me a way to contact you, at the end of the month I'll send you a link to all of the articles I found but didn't use each week!
1. Zoo welcomes birth of four endangered horse foals

“[The Marwell Zoo in GB] said it was "delighted" to welcome the arrivals to the endangered Przewalski’s horse herd. All four are female and said to be "doing well" after two were born in May and two in June. […] “These horses, that were previously listed extinct in the wild, are an example of how zoo breeding programmes can help restore threatened species around the world.” […] All the Przewalski’s horses alive today are descended from just 12 individuals. Current estimates suggest there are 178 mature individuals living in the wild.”
2. Restoring woodlands and planting trees for sustainability success

“In 2023, [the Marwell Zoo] planted 9,000 new trees […] both within the zoo and on our surrounding land. […] Marwell tries to encourage natural feeding behaviour and nutrition by including leafy material [in animals’ feed] as much as possible. […] Planting more trees and enhancing management of our existing woodlands, prepares the way to further self-sufficiency in browse production in the future. Plus, it creates new habitats for wildlife in our woodland areas.”
3. Inclusive Playgrounds Allow Children Of All Abilities To Play

“With ramps allowing children in wheelchairs to ascend the central play structure, as well as numerous other swings and apparatus usable for children of all abilities, the 16,000-square-foot P.K.’s Place is St. Paul’s first fully inclusive playground. […] To be universally accessible, a play area must have at least 70% of its play features fully accessible, far more than required by the Americans with Disabilities Act (ADA). […] Play areas should allow parents and grandparents with disabilities to participate as well.”
4. Combination treatment can increase human insulin-producing cells in vivo
“[Diabetes-model mice] were treated with the combination therapy [of a plant product called harmine and “a widely used class of type 2 diabetes therapy”] and their diabetes was rapidly reversed. Strikingly, human beta cell numbers increased by 700 percent over three months with this drug combination. "This is the first time scientists have developed a drug treatment that is proven to increase adult human beta cell numbers in vivo. This research brings hope for the use of future regenerative therapies to potentially treat the hundreds of millions of people with diabetes," said Dr. Garcia-Ocaña, the paper's corresponding author.”
5. Decades of Dedication: Australia’s Largest Ongoing Urban Restoration Project

“[Friends of Lake Claremont] has transformed the area into a thriving ecosystem, re-establishing native habitats and fostering biodiversity. This year, 800 native seedlings (100 trees, 350 shrubs and 350 ground covers) have been planted on the northwestern buffer of Lake Claremont. Volunteers replaced a large Port Jackson fig (Ficus rubiginosa) affected by [beetle] infestation with native plants to enhance the local wildlife habitat, thereby benefiting insects, frogs, birds and brown bandicoots. […] Overall, the project contributes to the area’s function as a regional ecological corridor, linking inland bushlands, the Swan River and the Indian Ocean.”
6. Important habitat for fish in Heart of the Fraser now conserved

“British Columbia’s iconic salmon now have more protected spawning habitat in the lower Fraser River, thanks to the Nature Conservancy of Canada’s (NCC’s) conservation acquisition of Carey Island. […] Carey Island and its gravel channels offer calm and crucial spawning and rearing habitat for the river’s fish and aquatic species. […] The Pelólxw Tribe […is also] actively working to restore the resilience of aquatic habitat within this stretch of the Lower Fraser. NCC is exploring opportunities to collaborate with the Pelólxw Tribe in support of their vision for stewardship of the area, which prioritizes both ecological and cultural values.”
7. Prime editing efficiently corrects cystic fibrosis mutation in human lung cells
“[R]esearchers have developed a gene-editing approach that efficiently corrects the most common mutation that causes cystic fibrosis, found in 85 percent of patients. With further development, it could pave the way for treatments that are administered only once and have fewer side effects. The new method precisely and durably corrects the mutation in human lung cells, restoring cell function to levels similar to that of Trikafta [the standard treatment since 2019].”
8. Montana’s High Court Considers a Constitutional Right to a Stable Climate
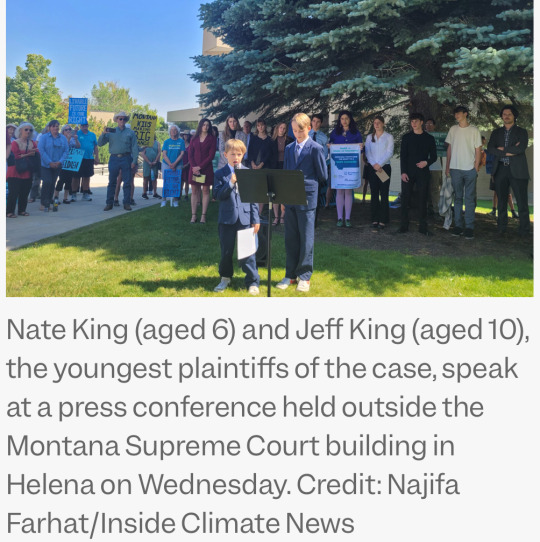
“At issue was the appeal of a decision last year, when a Montana judge blocked a state law that prohibited agencies from considering climate impacts when deciding whether to approve fossil fuel projects such as new power plants, pipelines or mining. The ruling, by District Judge Kathy Seeley, was prompted by a lawsuit filed by 16 youths who argued that the law violated Montana’s constitutional right to a “clean and healthful environment.” It was the first ruling in the United States to effectively establish constitutional rights to a stable climate[….]”
9. The US is about to get its first solar-covered canal

“The first canal-based solar project in the U.S. is nearing completion on tribal lands south of Phoenix, Arizona. […] The long, narrow solar array design would snake along the line of the canal and tap into the local electrical distribution grid every 1,000 feet, or every one megawatt. […] “Canal solar allows for greater power production per land size, cleaner water, less power transmission losses, and significant reduction in evaporation[….]” Covering the entire 8,000 miles of canals and waterways managed by the Bureau of Reclamation with solar panels could generate over 25 gigawatts of renewable energy and reduce water evaporation by tens of billions of gallons[….]”
10. Camera traps offer glimpse of first beaver born in Northumberland for 400 years

“"It’s such a relief that they have bred successfully and to see a new fluffy kit swimming with the family[….]” In just one year [since releasing the beavers], there has been a noticeable increase in resident trout, says the National Trust, along with more regular visits from kingfishers and grey herons. There are more insects at the site, too, thanks to the organic matter that builds up behind the dams, which in turn provides food for Daubenton’s bats. […] Beavers also play an important role in creating habitats that are more resilient to the effects of climate change[….]”
July 1-7 news here | (all credit for images and written material can be found at the source linked; I don’t claim credit for anything but curating.)
#hopepunk#good news#horse#zoo#nature#extinct species#sustainability#forest#children#disability#playground#disabled#wheelchair#diabetes#medicine#science#urban#biodiversity#ecosystem#fish#first nations#cystic fibrosis#gene editing#climate change#climate#youth#human rights#solar panels#solar energy#beaver
330 notes
·
View notes
Text
if I suffer, it must be doubled and given to the next fictional character.
Viktor with bad circulation to his feet, especially the bad right one.
No amount of compression socks made specifically for diabetics or varying, stacked disabilities worked. A warm water bottle is only warm so long, and troubling at the foot of the bed for two people who move too much. Medication does little to help with his condition, but at the end of a cold night, he’s helpless.
He’s got a heated blanket and wool socks on, but he can feel the numb cold at the tips of his toes. There’s an ache deep in his knee cap that he can’t rub out with his fingers, and he knows he’s going to have a restless night.
His nerves are going to keep him up with gentle nudges and helpless energy with no release.
But Jayce, at the first signs of discomfort, he’s there coddling his partner. He’s tucking himself under his warm blanket, rubbing his fingers into the tense muscles that couldn’t be worked out during physical therapy. He knows he’s needs to be gentle, so he takes his time while they watch a movie.
The touches are soft at first, presses to feel where there’s tightness and injury. When Viktor grimaces but says nothing, careful to not worry his partner more, Jayce is attentively watching from the corner of his eye. He takes note.
Reaching his feet, he begins around the swollen ankle and down his toes. The wool socks do nothing to help keep warmth, so he just clamps his warm palms around his toes and leaves them there until they become lukewarm. He thinks carefully.
The following night, another cold one, Viktor already has taken his bath and laid up in bed with Jayce says he has something that could help. Though pressing his toes into Jayce’s legs when they’re cold are an option, when they’re freezing, Jayce can only take it so much.
His gift to Viktor is a pack of large air activated warmers. At first it’s comical. He couldn’t be serious. But Jayce is dead serious. He took the chemical warmers from the wrappers, rubbing both sides, and the beads within began warming. It was gradual at first, and then a comfortable heat. He helped position them comfortably in Viktor’s socks, and they waited.
Viktor’s swelling didn’t progress as horribly as they usually did, but it was still evident. He could feel his toes further through the night, and compared to unbearably cold to a warmth on the tip of too much and too little, he found an in-between.
And Jayce’s victimized legs were cold-toe free.
(For a little while, Viktor likes to do it every once in a while just to see him in shock)
#jayvik#arcane jayvik#jayce talis#arcane viktor#jayce x viktor#arcane jayce#arcane netflix#arcane spoilers#izgnanik a
42 notes
·
View notes
Text
3 Warning Signs You Need Diabetic Foot Care from a Specialist in Sydney
Diabetes is a chronic condition that affects millions of people worldwide, and it often leads to complications that affect various parts of the body, including the feet. The nerves and blood vessels in the feet can become damaged, leading to conditions that may go unnoticed until they become serious. In Sydney, seeking diabetic foot care from a specialist is essential to prevent further complications. This article will cover three warning signs that indicate it's time to see a specialist for diabetic foot care in Sydney.

1. Numbness or Tingling Sensations in the Feet
When blood sugar levels remain high for extended periods, it can damage the nerves, leading to a condition called diabetic neuropathy. This condition often starts in the feet and legs, causing numbness or a tingling sensation, which may feel like a "pins and needles" feeling. The early stages of diabetic neuropathy can be mild and go unnoticed, but it's crucial not to ignore these sensations.
If numbness or tingling persists, it can lead to more severe complications. For example, the inability to feel pain means you may not notice cuts, blisters, or injuries on the feet, which could lead to infections. A diabetic foot care specialist in Sydney can conduct tests to assess nerve function and offer treatment options to help manage symptoms before they progress further.
2. Open Wounds or Sores That Won’t Heal
People with diabetes are at an increased risk of developing foot ulcers or sores. High blood sugar levels can impair the body's ability to fight infections and heal wounds properly. If you notice a wound or sore on your feet that doesn't seem to heal, it’s essential to seek the attention of a specialist. A diabetic foot care specialist in Sydney can assess the wound, provide treatment to prevent infection, and ensure proper healing.
In some cases, these wounds may become infected and cause serious complications, such as gangrene, which may require more intensive treatment or even amputation. Prompt care from a foot specialist can help prevent these outcomes and ensure that wounds heal effectively.
3. Changes in the Shape or Colour of the Feet
Changes in the appearance of your feet are another warning sign that may indicate a problem with your diabetes. If your feet become red, swollen, or have an unusual colour or texture, it could be a sign of poor circulation or infection. Swelling in the feet, especially if it's accompanied by pain or warmth, could indicate an underlying problem that requires immediate medical attention.
Changes in the shape of the feet, such as a loss of the arch, may also occur due to nerve damage or poor circulation. If left untreated, these changes can affect mobility and cause additional foot problems, making it essential to seek care from a diabetic foot specialist in Sydney as soon as possible.
Why Timely Diabetic Foot Care Matters in Sydney
Diabetic foot problems often go unnoticed until they become severe. Early intervention is key to preventing major complications, and seeking diabetic foot care from a specialist in Sydney is a vital step in maintaining healthy feet. By regularly monitoring your feet for these warning signs and seeing a specialist when necessary, you can reduce the risk of infections, ulcers, and other complications that can significantly impact your quality of life.
How a Diabetic Foot Care Specialist Can Help

A diabetic foot care specialist in Sydney is trained to assess the unique needs of individuals with diabetes. They can provide tailored care to help prevent complications and treat any issues before they become serious. Some of the services they offer include:
Foot assessments and check-ups: Regular check-ups can help detect early signs of diabetic neuropathy, poor circulation, or other foot problems.
Wound care and ulcer treatment: If you have an open wound or ulcer, a specialist can provide proper treatment to prevent infection and promote healing.
Diabetic footwear recommendations: Special shoes or insoles can help prevent pressure sores and further foot damage, improving comfort and mobility.
Education and advice: A foot care specialist can educate individuals with diabetes on how to properly care for their feet and avoid injury.
Conclusion
Taking care of your feet is an essential part of managing diabetes. The warning signs mentioned in this article—numbness or tingling sensations, non-healing wounds, and changes in the appearance of your feet—should not be ignored. If any of these symptoms arise, seeking diabetic foot care in Sydney is essential to avoid complications and preserve your mobility.
FAQs
What is diabetic neuropathy? Diabetic neuropathy is a condition caused by nerve damage due to high blood sugar levels. It often affects the feet and legs, causing numbness, tingling, and a loss of sensation.
Can a diabetic foot ulcer lead to amputation? Yes, if a diabetic foot ulcer becomes infected and is not treated promptly, it can lead to serious complications, including amputation. Early treatment from a specialist is essential.
How often should I see a diabetic foot care specialist? It’s recommended to have regular foot check-ups, at least once every six months, to detect any early signs of foot complications related to diabetes.
What are the signs of poor circulation in the feet? Poor circulation may cause symptoms such as cold feet, pale or bluish skin, swelling, and numbness. If you notice any of these signs, it's important to see a specialist.
What type of shoes should I wear if I have diabetes? Diabetic-friendly shoes are designed to reduce pressure and prevent injuries. A specialist can recommend appropriate footwear based on your specific needs.
#Orthotics Sydney#Ingrown Toenail Treatment Sydney#Shockwave Therapy Sydney#Heel Pain Specialist Sydney#Sports Podiatry Sydney#Foot Specialist Sydney#Foot Doctor Sydney#Diabetic Foot Care Sydney
0 notes
Text
Also preserved on our archive
Some interesting science analyzed
BY BROOKS LEITNER
Imagine lying back in an enclosed chamber where you bask for 90 minutes in a sea of pure oxygen at pressures two to three times that felt at sea level. This is the world of hyperbaric oxygen therapy (HBOT), a technology that’s been around for decades and is now being explored as a possible treatment for Long COVID.
"The silence on the inside is deafening at first,” says John M.,* who has undergone dozens of HBOT treatments for his persistent Long COVID symptoms. Fortunately, there is a television outside the chamber in view, and it is easy to communicate with the provider if needed. While the potential protocol is still being refined, patients may undergo up to 40 HBOT sessions to address some of the most problematic, lingering symptoms of this complex condition.
HBOT is a therapeutic process that has been widely used to treat such conditions as decompression sickness in scuba divers, carbon monoxide poisoning, and diabetic foot ulcers. In HBOT, the body is exposed to 100% oxygen, a significant increase from the 21% oxygen concentration we typically breathe. The therapy takes place in an enclosed chamber where the air pressure is elevated above normal levels. The combination of high-pressure and high-oxygen conditions enhances the amount of oxygen that can reach the body's tissues. The hope is that this therapy can provide the same relief and healing to people with Long COVID that it does for those with other conditions.
According to John M., HBOT was the first treatment that helped with his sleep and reduced his heart palpitations. “At one point after hospitalization, my Long COVID symptoms were so bad that I could barely walk or talk. HBOT was a great tool that really assisted with my recovery,” he said. John added that he hopes the medical community will achieve a better understanding of how HBOT can help relieve suffering for patients with Long COVID and that more research will increase access to this innovative therapy.
Does HBOT improve Long COVID symptoms? One key observation from the work of Inderjit Singh, MBChB, an assistant professor at Yale School of Medicine (YSM) specializing in pulmonary, critical care, and sleep medicine, is that Long COVID patients often experience debilitating fatigue. Based on Dr. Singh’s previous Long COVID research, the exhaustion is thought to be linked to the muscles’ inability to efficiently extract and utilize oxygen.
To picture how HBOT might work, you can think of your muscles as engines sputtering, struggling to get the fuel they need. If oxygen is the gas that fuels the muscles, it’s as if you are trying to complete your daily routine while the gas tank is running on “empty.” By aiming to directly address this oxygen utilization impairment, HBOT may be a potential solution.
A systematic review by researchers at the China Medical University Hospital noted that HBOT could tackle another major factor in the Long COVID puzzle: oxidative stress. This relates to the body's struggle to maintain balance when harmful molecules, known as free radicals, run amok, causing chronic inflammation.
Research co-authored by Sandra K. Wainwright, MD, medical director of the Center for Hyperbaric Medicine and Wound Healing at Greenwich Hospital in Connecticut, suggests that HBOT, with its high-oxygen environment, might dampen this chronic inflammation by improving mitochondrial activity and decreasing production of harmful molecules. Other potential benefits of HBOT in the treatment of Long COVID may include restoration of oxygen to oxygen-starved tissues, reduced production of inflammatory cytokines, and increased mobilization of hematopoietic stem cells—primary cells that transform into red blood cells, white blood cells, and platelets.
HBOT for Long COVID: Current and ongoing research Several small-scale reports have indicated that HBOT is safe for patients with Long COVID.
To address this question, a trial that followed the gold standard of modern medical research—a randomized, placebo-controlled, double-blind design—assigned 73 Long COVID patients to either receive 40 sessions of HBOT or a placebo of only 21% oxygen. The study observed positive changes in attention, sleep quality, pain symptoms, and energy levels among participants receiving HBOT. In a longitudinal follow-up study published in Scientific Reports, the authors at the Tel Aviv University found that clinical improvements persisted even one year after the last HBOT session was concluded. In a second study, the same authors focused on heart function, measured by an echocardiogram, and found a significant reduction in heart strain, known as global longitudinal strain, in patients who received HBOT.
In another study, 10 patients with Long COVID underwent 10 HBOT treatments over 12 consecutive days. Testing showed statistically significant improvement in fatigue and cognitive function. Meanwhile, an ongoing trial at the Karolinska Institute in Sweden has reported interim safety results wherein almost half of the Long COVID patients in the trial reported cough or chest discomfort during treatment. However, it was unclear whether HBOT exacerbated this symptom or if this adverse effect was due to the effort of participation by patients suffering from more severe Long COVID symptoms.
Is HBOT currently available as a treatment for Long COVID? For HBOT to become a mainstream treatment option for Long COVID, several critical priorities must be addressed. First, there is currently no established method for tailoring HBOT dosages to individual patients, so researchers must learn more about the specific features or symptoms that indicate potential benefits from HBOT. At the same time, we need to identify factors that may be associated with any adverse outcomes of HBOT. And finally, it’s important to determine how long these potentially beneficial effects last in a larger cohort. Will just a few HBOT trials be enough to restore patients to their baseline health, or will HBOT become a recurring component of their annual treatment regimen?
For now, HBOT remains an experimental therapy—and as such is not covered by insurance. This is a huge issue for patients because the therapy is expensive. According to Dr. Wainwright, a six-week course of therapy can run around $60,000. That’s a lot to pay for a therapy that’s still being studied. In the current completed studies, different treatment frequencies and intensities have been used, but it’s unclear how the treatment conditions affect the patient’s outcome.
“I have had some patients notice improvements after only 10 or 15 treatments, whereas some others need up to 45 treatments before they notice a difference,” notes Dr. Wainwright. “I think that HBOT is offering some promising results in many patients, but it is probably a strong adjunctive treatment to the other spectrum of things Long COVID patients should be doing, like participating in an exercise, rehab, and nutritional program.”
Dr. Singh notes that “a major challenge for research is the heterogeneity of Long COVID. It is hard to determine which symptoms to treat and enroll patients into trials based on them.”
Perhaps treatments that target multiple issues caused by Long COVID, like HBOT, may help overcome this challenge.
*Not his real name.
Brooks Leitner is an MD/PhD candidate at Yale School of Medicine.
The last word from Lisa Sanders, MD: Hyperbaric oxygen therapy (HBOT) is just one of the many existing treatments that are being looked at to treat Long COVID. We see this with many new diseases—trying to use a treatment that is effective in one set of diseases to treat another. And there is reason for optimism: We know that HBOT can deliver high levels of oxygen to tissues in need of oxygen. That’s why it’s used to treat soft tissue wounds. If reduced oxygen uptake is the cause of the devastating fatigue caused by Long COVID, as is suggested by many studies, then perhaps a better delivery system will help at least some patients.
Studies referenced:
bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-023-08002-8
www.ncbi.nlm.nih.gov/pmc/articles/PMC8806311/
www.nature.com/articles/s41598-024-53091-3
www.nature.com/articles/s41598-022-15565-0
www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2024.1354088/full
www.ncbi.nlm.nih.gov/pmc/articles/PMC11051078/#:~:text=Proposed%20Mechanism%20of%20HBOT%20o
#long covid#hbottherapy#HBOT#hyperbaric oxygen therapy#mask up#covid#pandemic#wear a mask#public health#covid 19#still coviding#wear a respirator#coronavirus#sars cov 2
59 notes
·
View notes
Text
Monthly Holidays: April
Monthly Beer Holidays
Alcohol Awareness Month
Craft Beer Month (Idaho)
NC Beer Month
Organic Beer Month
Monthly Food Holidays
Brussels Sprouts and Cabbage Month
Cranberries and Gooseberries Month
Fresh Florida Tomato Month
National Afternoon Tea Month
National BLT Month
National Brunch Month
National Food Month
National Fresh Celery Month
National Garlic Month
National Grilled Cheese Sandwich Month
National Pecan Month
National Soft Pretzel Month
National Soy Foods Month
Sonoma County Wine Month
Sprouted Grains Month
Tomatillo and Asian Pear Month
Monthly Health Holidays
Autism Awareness Month
Cesarean Awareness Month
Counseling Awareness Month
Defeat Diabetes Month
Distracted Driving Awareness Month
Emotional Overeating Awareness Month
Esophageal Cancer Awareness Month
Global Child Nutrition Month
Irritable Bowel Syndrome Awareness Month
Limb Loss and Limb Difference Awareness Month
National Anxiety Month
National Cancer Control Month
National Child Abuse Prevention Month
National Donate Life Month
National Facial Protection Month
National Foot Health Awareness Month
National Heartworm Awareness Month
National Minority Health Month
National Multiple Birth Awareness Month
National Parkinson Awareness Month
National Sjogren's Syndrome Awareness Month
National Sports Eye Safety Month
National Tar Syndrome Month
National Youth Sports Safety Month
Occupational Therapy Month
Oral Cancer Awareness Month
Parkinson’s Awareness Month
Pharmacists War on Diabetes Month
Physical Wellness Month
Rosacea Awareness Month
Sarcoidosis Awareness Month
Sexual Assault Awareness Month
STD Awareness Month
Stress Awareness Month
Testicular Cancer Awareness Month
Women's Eye Health and Safety Month
Worldwide Bereaved Spouses Awareness Month
Monthly Heritage Holidays
Arab American Heritage Month
Celebrate Diversity Month
Community Spirit Days
Couple Appreciation Month
Earth Month
English Language Month
Informed Woman Month
Jazz Appreciation Month
Keep America Beautiful Month
National Decorating Month
National Humor Month
National Month of Hope Month
National Poetry Month
National Volunteer Month
Poetic Earth Month
Scottish-American Heritage Month
Thai Heritage Month
Monthly Nature Holidays
Adopt a Ferret Month
Canine Fitness Month
Children and Nature Awareness Month
Dog Appreciation Month
National Adopt a Greyhound Month
National Frog Month
National Garden Month
National Landscape Architecture Month
National Pest Management Month
National Pet Month
Pet First Aid Awareness Month
Prevent Lyme Disease in Dogs Month
Prevention of Cruelty to Animals Month
World Habitat Awareness Month
Other Monthly Holidays
Car Care Month
Community Service Month
D.E.A.R — Drop Everything and Read Month
Genocide and Human Rights Awareness Month
Global Astronomy Month
Grange Month
Holy Humor Month
International Amateur Radio Month
International Guitar Month
International Twit Award Month
Listening Awareness Month
Mathematics Education Month
Month of the Military Child
Move More Month
National Cannabis Awareness Month
National Card & Letter Writing Month
National Fair Housing Month
National Kite Month
National Knuckles Down Month
National Pickleball Month
National Rebuilding Month
National Recycling Month
National Safe Digging Month
National Welding Month
National Woodworking Month
Parliamentary Law Month
School Library Month
Straw Hat Month
Summer Tire Changeover Month
Monthly Business Holidays
Financial Literacy Month
International Customer Loyalty Month
Mathematics and Statistics Awareness Month
National Internship Awareness Month
National Social Security Month
Records and Information Management Month
Workplace Conflict Awareness Month
2 notes
·
View notes
Text
A 5-year-old boy from Royal Oak died Friday morning during an explosion of a hyperbaric chamber at a Troy medical center, police said.
The medical facility, The Oxford Center, is located at 165 Kirts Boulevard. The explosion happened shortly before 8 a.m. and police said the boy was found dead inside the chamber. His mother, who was injured, was there with him at the facility, officials said.
The Oxford Center's website says that it provides therapy for children with numerous conditions, like autism, cancers, ADHD, autoimmune diseases, and a slew of others.
Troy Fire Lt. Keith Young said investigators do not yet know what exactly caused the explosion, but concentrated oxygen and the pressure used in hyperbaric chambers are fuel for fire.
In a statement from The Oxford Center, spokesman Andrew Kistner wrote in an email that the cause of the explosion is unknown and that Friday was an "exceptionally difficult day for all of us."
"As law enforcement officials have shared, at our location in Troy, Michigan this morning, a fire started inside of a hyperbaric oxygen chamber. The child being treated in that chamber did not survive and the child’s mother was injured," the statement reads.
"The safety and wellbeing of the children we serve is our highest priority. Nothing like this has happened in our more than 15 years of providing this type of therapy. We do not know why or how this happened and will participate in all of the investigations that now need to take place."
Troy Police Lt. Ben Hancock said the mother was standing right next to the chamber when it exploded and suffered injures to her arms.
He described the explosion as a "very sad incident"
For decades, hyperbaric oxygen therapy has been used to relieve the effects of decompression sickness for scuba divers, to help firefighters, miners and others who have carbon monoxide poisoning, to improve the success of skin grafts and to speed up healing of infections, such as diabetic foot ulcers and gangrene, and in treatment of crush injuries, according to Johns Hopkins Medicine.
Here’s how it works: People enter into either a monoplace chamber, which is built for one person, or a mulitplace chamber, which can fit two or more people.
In a monoplace chamber, a person lies down in a long, plastic tube that resembles an MRI machine. In a multiplace chamber, people breathe through masks or hoods.
Pure oxygen is pumped into a pressurized chamber, mask or hood and people inside breathe in the concentrated oxygen, which enters the bloodstream and tissues to boost healing and recovery from injury and helps the body fight infections.
Johns Hopkins Medicine reports that each session can last from 45 minutes to five hours, depending on the reason for the treatment.
The Oxford Center is among other alternative medical centers or medical spas who, in recent years, have offered hyperbaric oxygen therapy for conditions that are not approved by the U.S. Food and Drug Administration, such as autism spectrum disorder, cerebral palsy, sports injuries, COVID-19, depression, alopecia, HIV/AIDS, strokes, migraine headaches, and as an anti-aging treatment, the Cleveland Clinic reports.
The Oxford Center, which has locations in Brighton and Troy, has generated controversy. In August, the facility's former director Kimberly Coden pleaded guilty to nine charges after officials with Michigan Attorney General Dana Nessel’s office said she used false credentials to treat children with autism.
She falsely presented herself as a board-certified behavioral analyst without being licensed and without the proper education and used an actual analyst’s certification to get jobs within the health sector, officials said. And she’d also used professional business cards, verbal statements, written documents and presented university degrees she allegedly didn’t earn.
Coden also tried to intimidate a witness through text messages to keep them from testifying against her, officials said.
When Coden pleaded guilty, her lawyer said her client was "really, truly remorseful."
Hazards of hyperbaric chambers
A study was published in the medical journal Lancet reviewing hyperbaric chamber fires over 77 years, from 1923 to 1996, and found that 77 people died in 35 fires. Before 1980, most of the fires were caused by electrical ignition. But since then, they were sparked by something that was carried into the hyperbaric chamber.
Officials in Friday's explosion at the Oxford Center said they don't know whether someone brought something into the chamber before it exploded, but acknowledged the chambers create an environment that is "extremely combustible."
The National Fire Protection Association has written about the district hazards associated with hyperbaric facilities, including the increased pressure and presence of elevated oxygen levels.
In a Aug. 2021 blog post from the National Fire Protection Association, Brian O’Connor wrote:
"While oxygen itself is not flammable, it is an oxidizer that supports combustion and can increase the flammability of other materials," Brian O’Connor of the association wrote in Aug. 2021, including flame-resistant fabrics and materials.
“This means that care must be taken to prevent any means of ignition from entering the oxygen-enriched environment, since the conditions exist for a fire to grow rapidly."
O’Connor wrote that another fire safety problem with hyperbaric chamber facilities is that it’s difficult to evacuate the chamber when fires do occur.
“Since these chambers are pressurized, they must undergo a decompression process before occupants can safely exit. The process is required to take no more than six minutes for (multiplace) chambers and two minutes for (monoplace chambers) when returning from three times standard atmospheric pressure,” he wrote.
"These facts, he said, make it vital to ensure that any facility that uses a hyperbaric chamber adhere to strict fire safety regulations, such as allowing only certain fabrics to be worn and restricting other flammable materials to be brought inside the chamber, installing specialty sprinkler systems, and in some cases, independently supplied handlines."
Troy's Fire Lt. Keith Young said the state oversees hyperbaric medical chambers.
2 notes
·
View notes
Text

Why a Simple Foot Massage Before Bed Can Change Your Life
Barbara O'Neill
If you’ve ever experienced a foot massage, you know how deeply relaxing it can be, not just for your feet but for your entire body.
Experts highlight that our feet reap the most benefits from a good massage. Traditional Chinese medicine emphasizes that the feet contain multiple reflexology points that connect to various organs and systems in the body. Stimulating these points can greatly improve overall well-being.
There are several types of foot massage, such as Thai foot massage, Swedish massage, and reflexology, all offering unique health benefits. For centuries, foot massage has been used as a natural method to boost health and well-being. Today, it is recognized as a complementary therapy that millions of people use to relieve pain, reduce stress and anxiety, recover from injuries, and enhance their overall health.
Foot massage is effective in multiple ways. Physically, massaging the muscles increases blood flow, relieves joint pain, and aids lymphatic drainage, providing a therapeutic effect on its own.
Research has shown that foot massages can deliver additional health benefits, including reducing pain, lowering heart rates and blood pressure, and helping with mental health concerns like anxiety and depression. These benefits result from both the physical and psychological impacts of massage.
Scientific studies back up the healing benefits of massage:
Self-administered acupressure helps reduce stress and manage symptoms like allergies, nausea, and pain.
A 10-minute Chinese massage promotes relaxation.
A 15-minute massage improves physical, psychological, and emotional well-being in geriatric care patients.
Thai foot massage improved balance and mobility in diabetic patients with peripheral neuropathy.
Pre-operative anxiety levels decreased after just four 20-minute sessions.
Foot massages boosted mood, relaxation, and alertness in patients with dementia.
Twice-weekly 30-minute massages alleviated symptoms of gastroesophageal reflux disease and reduced stress in infants.
Start a nightly 5-10 minute foot massage, and you’ll soon experience the many health benefits of this ancient practice.
How to Give Yourself a Foot Massage:
Begin by soaking your feet in warm water, with a few drops of essential oil for added relaxation.
Sit comfortably, placing one foot on your lap while the other extends in front of you. Apply some lotion or oil to the foot.
Holding the bottom of the foot, use firm pressure to rub the top, while your thumbs work their way down the sole. Gently tap the sole with your fist to encourage blood flow.
Hold the foot beneath the arch with one hand while using the thumb and index finger of the other hand to stretch and pull each toe. Gently slide your fingers between the toes and rub the base of each one.
Rotate the foot at the ankle while massaging around the top of the foot with your fingers. Turn the foot in both directions a few times.
Overlap your thumbs and press into the arch, starting from the heel and moving up toward the ball of the foot. Use circular motions to massage the arch thoroughly.
Finally, wrap your hands around the foot, pressing your thumbs into the soles and sweeping them outward. Finish by stretching the foot.
After this simple yet effective routine, you’ll feel relief from aches, your mind will be at peace, and you’ll enjoy a deep, restful sleep!
4 notes
·
View notes
Text
Diabetes and Nerve Damage: The Numbness and Tingling ⚡


Understanding Diabetic Neuropathy
Ever experienced a pins-and-needles sensation or numbness in your hands or feet? If you have diabetes, you might be familiar with this uncomfortable feeling. This condition, known as diabetic neuropathy, occurs when high blood sugar levels damage nerves over time.
How Does Diabetes Affect Your Nerves?
When your blood sugar is consistently high, it can damage the small blood vessels that supply your nerves with the oxygen and nutrients they need to function properly. This damage can lead to a variety of symptoms, including:
Numbness and tingling: This is often the first sign of diabetic neuropathy. You may feel like you're wearing gloves or socks that are too tight.Pain: Nerve damage can cause sharp, shooting pains or a burning sensation.Weakness: Muscles may become weak, making it difficult to perform daily tasks.Loss of balance and coordination: Damage to the nerves in your feet can increase your risk of falls.Digestive problems: Neuropathy can affect the nerves in your digestive system, leading to constipation, diarrhea, or difficulty swallowing.
Types of Diabetic Neuropathy
There are different types of diabetic neuropathy, each affecting different parts of the body: Peripheral neuropathy: This is the most common type and affects the nerves in your hands and feet.Autonomic neuropathy: This affects the nerves that control your heart, blood pressure, and digestive system.Proximal neuropathy: This affects the nerves in your thighs, hips, and buttocks.Managing Diabetic NeuropathyWhile there is no cure for diabetic neuropathy, there are several ways to manage the symptoms and slow down the progression of the disease:
Strict blood sugar control: Keeping your blood sugar levels within a healthy range is the most important thing you can do to protect your nerves.Pain management: Over-the-counter pain relievers, prescription medications, and physical therapy can help relieve pain.Foot care: Regular foot exams and proper foot care can help prevent ulcers and infections.Lifestyle changes: Quit smoking, maintain a healthy weight, and exercise regularly.Living with Diabetic NeuropathyLiving with diabetic neuropathy can be challenging, but with the right management, you can still enjoy a good quality of life. It's important to work closely with your healthcare team to develop a personalized treatment plan.
Remember, you're not alone. There are many people living with diabetic neuropathy who have found ways to manage their condition and live fulfilling lives.
#diabetes#diabeticneuropathy#nervepain#neuropathy#bloodsugar#health#wellness#healthcare#footcare#painmanagement
3 notes
·
View notes
Text
The Ultimate Guide to Diabetic Socks and Compression Socks
Diabetic and compression socks are two popular types of socks that have benefits for people with diabetes or poor circulation. While both types of socks aim to improve foot health, they are not the same thing. In this ultimate guide to diabetic socks and compression socks, we will explore the differences between these two sock types and how they can benefit individuals with diabetes or…

View On WordPress
#are diabetic socks the same as compression socks#Blood circulation#circulation#compression socks#Compression therapy#Diabetes care#Diabetes management#Diabetic foot complications#diabetic socks#edema#foot health#leg swelling#medical socks#neuropathy#Orthopedic socks
1 note
·
View note
Text
Finding the Right Foot Doctor in Agoura Hills and West Hills, CA
Introduction:
Foot health is often overlooked, yet it plays a crucial role in our overall well-being and mobility. When foot problems arise, seeking professional care from a qualified foot doctor becomes essential. In Agoura Hills and West Hills, CA, residents have access to expert podiatrists who specialize in diagnosing and treating a wide range of foot and ankle conditions. In this article, we'll explore the importance of foot care, the role of a foot doctor, and how to find the right foot doctor in these California communities.

Understanding the Importance of Foot Care:
Foundation of Mobility: Our feet bear the weight of our entire body and facilitate movement. Healthy feet are essential for maintaining balance, stability, and mobility, allowing us to perform daily activities with ease.
Early Detection of Problems: Regular foot care appointments with a foot doctor enable early detection of foot problems such as bunions, corns, calluses, heel pain, and fungal infections. Timely intervention can prevent conditions from worsening and improve treatment outcomes.
Management of Chronic Conditions: Individuals with chronic conditions like diabetes or arthritis require specialized foot care to manage associated complications such as neuropathy, ulcers, and joint deformities. A foot doctor plays a crucial role in preventing complications and preserving foot health.
Customized Treatment Plans: Foot doctors create personalized treatment plans tailored to each patient's unique needs and goals. Whether addressing acute injuries, chronic conditions, or preventive care, they utilize advanced techniques and therapies to promote healing and improve quality of life.
The Role of a Foot Doctor in Agoura Hills and West Hills, CA:
Comprehensive Evaluation: A foot doctor begins by conducting a comprehensive evaluation of the patient's foot health, including a physical examination, medical history review, and diagnostic tests such as X-rays or ultrasounds. This thorough assessment allows for accurate diagnosis and treatment planning.
Diagnosis and Treatment: Once a diagnosis is established, the foot doctor develops a customized treatment plan that may include conservative measures such as orthotics, physical therapy, medication, or minimally invasive procedures. In cases requiring surgery, they perform precise and effective procedures to address foot and ankle issues.
Specialized Expertise: Foot doctors specialize in various areas of podiatric care, including sports injuries, pediatric foot conditions, diabetic foot care, orthopaedic foot and ankle surgery, and more. Their specialized expertise ensures comprehensive and effective management of a wide range of foot and ankle problems.
Patient Education and Prevention: In addition to treatment, foot doctors prioritize patient education on foot care practices, preventive measures, and lifestyle modifications to promote long-term foot health and prevent future problems. They empower patients to take an active role in their foot care journey.
Finding the Right Foot Doctor in Agoura Hills and West Hills, CA:
Referrals and Recommendations: Seek referrals and recommendations from primary care physicians, friends, family members, or trusted healthcare professionals to find a reputable foot doctor in Agoura Hills or West Hills. Personal experiences and testimonials can help guide your decision.
Credentials and Experience: Verify the credentials, certifications, and experience of potential foot doctors. Look for board-certified podiatrists with extensive experience in diagnosing and treating a diverse range of foot and ankle conditions.
Specialized Services: Consider the specific services and treatments offered by foot doctors, such as sports medicine, orthopaedic surgery, diabetic foot care, pediatric podiatry, and more. Choose a foot doctor whose expertise aligns with your individual needs and concerns.
Patient-Centred Care: Opt for a foot doctor who prioritizes patient-centred care, effective communication, and collaborative decision-making. A compassionate and attentive approach fosters a positive patient-doctor relationship and enhances the overall treatment experience.
Conclusion:
Foot health is integral to our overall well-being and quality of life. By prioritizing regular foot care and seeking professional assistance from a skilled foot doctor in West Hills, CA or Agoura Hills, individuals can address foot problems, prevent complications, and maintain optimal foot health for years to come. With a commitment to personalized care, specialized expertise, and patient education, foot doctors play a vital role in supporting patients on their journey to healthy, pain-free feet.
2 notes
·
View notes