#dermatophyte
Explore tagged Tumblr posts
Text

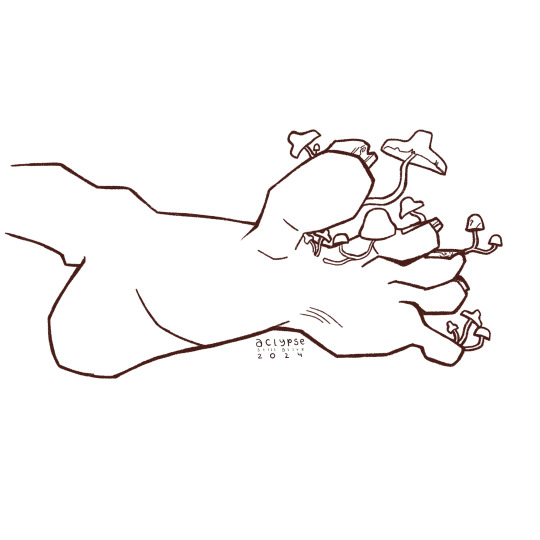

#art#artists on tumblr#drawing#artwork#digital art#krita#kritaart#digtal illustration#illustration#mycosis#skin disorder#skin condition#medicine#medical condition#health#dermatology#mushroom#mushrooms#fungi#fungus#fungi art#mushroom art#fungal infection#skin infection#digital painting#digital drawing#symptoms#poem#short poem#dermatophytes
5 notes
·
View notes
Link
1 note
·
View note
Text
Oh my god, you feel like shit and then it's just that times of the month. Again. Hell on earth
0 notes
Text
0 notes
Link
#AnimalShelters#dermatophytes#directcontact#dogparks#dogs#fungalinfection#grooming#indirecttransmission#prevention#ringworm#shareditems#symptoms#transmission#treatment#WhereDoDogsGetRingworm
1 note
·
View note
Text
Period Problems. Because not all women have periods and not all periods have women people with periods are women! And all women are humans and all humans are people.
I thought lol pppp all finished my thought so nvm.
My last appointment of the day was cancelled. I asked the front desk person why. The building was noisy and Ms. Front Desk said: “_-_-^-\_” [Quicj sidebar: that attempt to use text characters to draw what the intonation sounded like looks like Stork crawling on the ground pushing a hockey stick.]
_-_-^-\_
Now I see it as Stork flat on the ground as the hockey stick speeds awwy’nnn!! It’s like a flip book. Or a gif with two frames but it’s one image.
I don’t know whether I’m genuinely more creative right now or that my standards are lower and everything I do seems creative to me. I believe that like most things it is a combination but leans towards low standards.

Can’t tell if it’s head noise or the neighbors listening to what sounds like a holiday caroling oompah band going: “LalalalaLALAAALalalala.” It’s gone now.
I still see my friend, Snrlk the snipple snorfed snildebeest on my ceiling. He lives in the snowy white kingdom of the clouds. Earlier he took on a deep, fluid red shade. It faded to black until he returned to his home in the beyond the skinny sky skinks. I want to make up more words but I don’t want to accidentally type a hurtful word by accident and I’m too lazy to do that kind of multilingual spellcheck.
interrupted writing task
-I say 20 sentences aloud and have people write them down
-Something happens that interrupts them so they can’t finish the sentence. Like a bell rings. They have to stop immediately. How immediately can they stop? And most importantly: are they stopping mid-letter? Mid-word? Between words?
I don’t think it tells us anything other than information I’m interested in knowing.
Dear Future BFF:
This stuff coming up involves mildly gross feet. Protect your brain and stomach. In a big purple bear if you have to. So if that bothers you, flee

I had part of this out of order and was performing mental calculations for now to correctly move it but it was shockingly easy.
Trimming nails. What if an emory board was taken from a salmon or \¥’eone or someone and are expecting a ritzy palace and the. They arrive and it’s this mansion with lots of fountains and towers and stairways and swimming pools. Then it is conveyed by the butler (?) to the Criticallg Acclaimed Person owner and THEN… horrible feet. Inhabited by Matt, Toph, and Ike, cousins of Digger the Dermatophyte. But the story started with them and they are kind and peaceful, but it doesn’t change the fact that their toe farming is making gross feet. Now the Emory board must roll up its proverbial sleeves to save the feet and the Dermatophyte brothers.
More body horror:
I finally cut my toenail experiment. I grew a tonsil toenail for awhile without cutting jt. No real reason; just wanted to see what would happen. What happened - it got kind of long and was good for scratching my other leg. The skin on the tip of my big toe is enjoying the sensory experience with being able to touch surfaces again. Usually the nail blocked it like one of those porch awnings. Now every texture on it feels diving. I mean divine!
Rug. Pretend wood floor. Grass. Blanket. Tub.
But NOT the wall. Just thinking about that makes me about to throw up.
Dear Future Limestoner, please remember oh gorsh I plumb forgot wait, now I remember:
Criminals. Now I understand a way that criminals get caught because of context clues. Because you always wondered about it. That’s why it’s locker detective.
0 notes
Text
Potato Dextrose Broth

APHA (American Public Health Association) and FDA (U.S. Food and Drug Administration) endorse the utilization of Potato Dextrose Broth for conducting plate counts of yeasts and molds in the analysis of food and dairy items. This medium is additionally employed to encourage sporulation, sustain initial cultures of specific dermatophytes, and distinguish common types of dermatophytes by assessing their pigment production. Read More.
#Dehydrated Culture Media#APHA#FDA#plate counts#dermatophytes#potato dextrose broth#potato dextrose agar manufacturer
0 notes
Text
Understanding Onychomycosis: A Guide to Nail Fungus Treatment and Prevention
Introduction: Hey there! I’m Dr. Nunez, here to shed some light on a common fungal infection called onychomycosis, also known as toenail fungus. It’s a pesky condition that affects the nails of the toes or fingers, and today I’m going to help you understand its causes, symptoms, treatment options, and prevention strategies. So, let’s dive in! Photo by Quiet Shades Of Brown on Pexels.com Causes…

View On WordPress
0 notes
Note
Hi! Our 11-year old cat has a very long claw on one of her front paws since recently-ish. While she is not the most active cat (never has been) she moves and eats normally for her and the claw doesn't bother her usually (except sometimes getting stuck in fabric) I'm a bit concerned about it. I read here on that blog that overgrown nails can be the a sign of illness - anything I need to watch out for and/or discuss with a vet?
I'll get a nail trimmer for her tomorrow so I can at least remove the tip of the nail. Any advice on making it easy on my girl (except taking it slow and lots of treats)?
Sueanoi here,
Cat claws are usually self shedding by a cat scratching on scratch post, or some cats would just bite off the top layer (sometimes with gusto...), but if a cat is reluctant to display this behavior it could be a sign of joint pain, or other problems, too (example, nail bed dermatophyte, but it's obvious at one look.). but I usually see this on joint problem cats. That would be a topic starter for your conversation with your vet.
cutting a cat claw you must be careful and avoid cutting into the quick (pink flesh inside). Because that is extremely painful and the cat will never want to comply to nail cutting ever again. Better to do shallow trim often than risk pain and bleeding.
I hope this is helpful.
30 notes
·
View notes
Note
Yo feet liker, you know what type of foot fungus that wizard has? Is it a Dermatophytes?? Tinea pedis?? Onychomycosis?? What?
He has all of those and more. there's like, a whole digital ecosystem down here.
#wizard more like rizzard#the knights are nexos#nexo knights#merloks digital toes#nexoknights#nexo#milkisvibin#nexo knights merlok
11 notes
·
View notes
Text
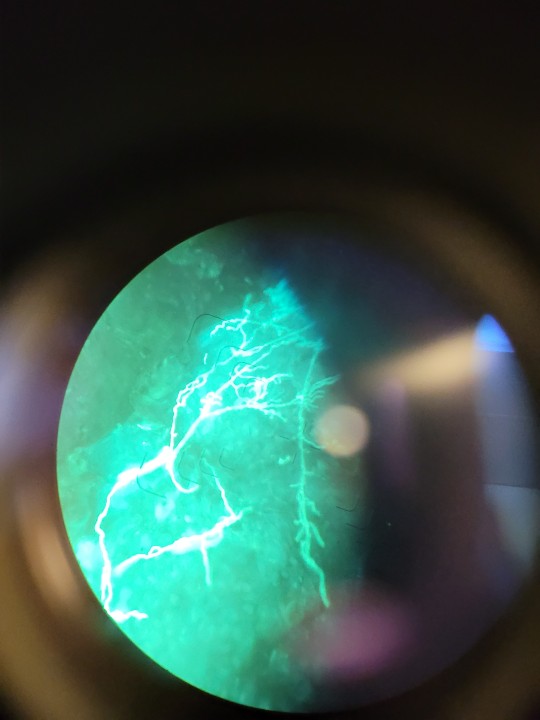

just wanted to share this very sweet calcoflour prep I did of a skin scraping that was absolutely heaving with a dermatophyte (mould) at work :) check those mycelia ouuuuut
2 notes
·
View notes
Link
1 note
·
View note
Text
Battling Skin Infections: A Dog Owner's Survival Guide"

As a dog owner, your furry friend's health and happiness are of utmost importance. One common health issue that can plague our canine companions is Skin infections in dogs. These infections can be uncomfortable and distressing for both you and your dog. However, armed with knowledge and proper care, you can effectively battle and prevent skin infections in your four-legged friend. In this guide, we will explore the causes, symptoms, treatment options, and prevention strategies to help you become a skin infection superhero for your beloved pet.
Understanding Skin Infections in Dogs
Skin infections in dogs can manifest in various forms, and they are typically caused by bacteria, fungi, or parasites. Understanding the underlying causes is crucial for effective management. Here are some common culprits:
Bacterial Infections: Staphylococcus and Streptococcus bacteria are often responsible for bacterial skin infections. These infections can occur when the skin barrier is compromised, allowing bacteria to infiltrate.
Fungal Infections: Fungi like yeast and dermatophytes can lead to fungal skin infections. These often occur in warm and moist areas of a dog's body, such as the ears, paws, and folds of skin.
Parasitic Infections: External parasites like fleas, ticks, and mites can cause skin irritations and infections. These parasites not only bite but can also transmit diseases that affect your dog's skin.
Click here to know more : -
Recognizing the Symptoms
Identifying the signs of a skin infection in your dog is crucial for prompt treatment. Common symptoms of skin infections in dogs include:
Itching: Dogs with skin infections often exhibit excessive itching and scratching. This can lead to hair loss and irritated skin.
Redness and Inflammation: The affected area may appear red, swollen, and warm to the touch.
Pustules or Pimples: Bacterial infections may cause pustules or pimple-like lesions on the skin.
Hair Loss: Dogs may experience localized or generalized hair loss in the affected area.
Odor: Skin infections can produce a foul odor, especially in cases of yeast overgrowth.
Open Sores or Wounds: Scratching and licking can lead to open sores and wounds, which may become infected.
Changes in Behavior: Your dog may exhibit signs of discomfort, restlessness, or changes in behavior due to the discomfort caused by the infection.
Seeking Veterinary Care
If you suspect your dog has a skin infection, it's crucial to consult with a veterinarian. They can diagnose the specific type of infection and recommend appropriate treatment. Treatment may involve:
Medication: Depending on the diagnosis, your vet may prescribe antibiotics for bacterial infections, antifungal medications for fungal infections, or parasitic control products for parasitic infections.
Topical Treatments: In some cases, topical treatments like shampoos, sprays, or ointments may be recommended to alleviate symptoms and promote healing.
Preventive Measures: Your veterinarian may provide guidance on preventing future skin infections. This might include recommendations for regular grooming, cleaning ears, or using parasite preventatives.
Dietary Changes: Dietary modifications, such as switching to a hypoallergenic or specialized diet, may be suggested for dogs with recurring skin issues.
Preventing Skin Infections in Dogs
Prevention is often the best strategy when it comes to skin infections in dogs. Here are some proactive steps you can take as a responsible dog owner:
Regular Grooming: Regular grooming is essential to maintaining your dog's skin health. Brushing your dog's coat helps remove loose hair, prevents matting, and promotes good circulation, which can reduce the risk of skin infections.
Clean Ears: If your dog is prone to ear infections, cleaning their ears regularly can help prevent issues. Use a vet-recommended ear cleaning solution and follow your veterinarian's advice.
Parasite Control: Keep your dog on a consistent flea and tick prevention regimen. Check your dog for parasites after walks or outdoor activities, and promptly remove any ticks you find.
Balanced Diet: Feeding your dog a balanced and high-quality diet can help support their overall health, including skin health. Consult with your veterinarian for dietary recommendations if your dog has a history of skin problems.
Hygiene: Bathing your dog with a mild, pet-friendly shampoo can help remove dirt and allergens from their skin. Be sure not to over-bathe, as excessive bathing can strip the skin of its natural oils.
Environmental Management: Keep your dog's living environment clean and dry. Wash their bedding regularly, vacuum your home to remove allergens, and ensure your dog has a comfortable and clean living space.
Regular Veterinary Check-Ups: Routine check-ups with your veterinarian are essential for detecting and addressing potential health issues before they become major problems.
In Conclusion
Skin infections in dogs can be a source of discomfort and concern for both you and your furry friend. By understanding the causes, recognizing the symptoms, and taking preventive measures, you can become a skin infection superhero for your canine companion. Remember, if you suspect a skin infection or any other health issue in your dog, consult your veterinarian promptly for expert guidance and treatment. With proper care, you can ensure that your dog's skin stays healthy, allowing them to lead a happy and itch-free life.
Read more : - When to Worry: Signs Your Dog Needs Cough Medicine
3 notes
·
View notes
Text
0 notes
Text

Very long time ago… This is a photo from the beginning of my work as a future/would-be mycologist. By the color of the test tubes, you can easily see that we are dealing with a medium with urea. In bacteriology, the urea hydrolysis test is used routinely for almost all bacteria. In turn, in the case of dermatophytes, although it is a differentiating feature, it usually gives unexpected results. By accident I managed (them) to get quite a nice color gradient from yellow (which doesn't happen often) to very pink (fuchsia/bishop color). And the culprit was Trichophyton verrucosum, which according to the literature should be urea positive. This yellow color (i.e. the opposite of the intended effect) is due to the fact that this strain of T. verrucosum very quickly used up a small amount of dextrose in the medium, which acidified the medium so much that the phenol red from a slightly orange color turned yellow. In general, we all use the term Christensen's medium, but every lab's composition is a little different. Note that there is such a thing as Stuart's medium for detecting urease, and it is not much different from Christiansen's medium. Virtually every laboratory uses a combination of these media so as not to add dextrose but at the same time the medium is "rich" enough for other microbes to grow on it. Hence, there are often considerable discrepancies - especially in mycology. Believe it or not, the same strain that gives a typical positive result in lab A will give +/- or the opposite in lab B.
#veterinary#veterinarymedicine#veterinaryjobs#laboratory#microbiology#microbiologist#jobapplication#mycology#examination#numbers#lookingforjob#microscope#infection#biochemistry#urea#ureabroth#trichophyton
8 notes
·
View notes
Text
Refining Terms Related to Pathogenicity
When discussing microbial infections clinically, it's important to refine the usage of common terms seen in microbiology. When we think of infections, we synonymize virulence, infectivity and pathogenicity, but their definitions are distinct. These terms represent different characteristics of pathogenicity, and their interplay can vary based on microbial species and the context of their host.
The efficiently and ease with which a microbe enters, survives, and multiplies in a host is defined by infectivity. This definition sounds synonymous to virulence. However, virulence relates to the severity damage its caused to their host. There can be a highly infective microbe that has low to no virulence. Rhinovirus is a highly infective virus, but only causes symptoms akin to the common cold. The inverse is seen through botulinum toxin produced by Clostridium botulinum. The toxin produced by C. botulinum causes muscle paralysis and death, but is low in terms of infectivity. Infectivity associated with this microbe commonly requires ingestion through canned goods or improperly stored or fermented food.
Pathogenicity refers to a microorganism's ability to cause disease in a host. Infectivity is an important prerequisite of pathogenicity, since a microbe must be infective to cause disease. Pathogenicity and its relation to virulence contributes to the measurement of severity of disease which can vary. Again, Rhinovirus is a highly infective virus that is pathogenic, but has low virulence. The Ebola virus is infective and causes highly virulent pathogenicity that can be fatal.
How infectivity, virulence, and pathogenicity are measured:
Infectivity is measured through the minimum number of microbes required to begin an infection in a susceptible host. This measurement is known as the infectious dose (ID). The higher the infectivity, the lower the ID value is.
Virulence is measured through the lethal dose 50 (LD50). As described by its title, the LD50 measures the dose of a pathogen or pathogen-related virulence factor that kills 50% of infected individuals. High virulence is associated with low LD50 values.
Pathogenesis can be measured through signs and symptoms, animal model studies, and histopathology. Observing signs and symptoms of an infection is evaluated by the patient and clinician. Animal models in laboratory animals help measure the onset and progression of pathogenesis. Histopathology examines tissues for signs of infection, inflammation and damage caused by the microbe. This information is foundational to microbe-related diagnostics in dermatology.
As discussed before, there is a close relationship between pathogenicity, virulence and infectivity. Infective pathogenic diagnoses that are virulent require strict control to prevent transmission. Dermatophytic infections, such as tinea corporis (ringworm), is a highly infective and moderately virulent diagnoses that can indirectly or directly spread. Necrotizing fasciitis is an example of a infective and highly virulent condition. Along with pharmaceutical treatment, prevention of transmission begins at the clinician's ability to educate the patient, and call for aid beyond the scope of dermatology. This includes critical care physicians, infectious disease specialists, surgeons, and pathologists. It's important for clinicians to get in touch with a patient's capacity to prevent, detect changes, and maintain well-being post-treatment. This plays a major role in disease prognosis and course of treatment.
In dermatology, preventing further pathogenesis, virulence and infectivity is largely determined by patient education. Treatment completion, personal hygiene, preventative measures, and proper wound care are not always understood or independently possible for a patient. Mental and physical disabilities require additions to a given care plan from the provider.
2 notes
·
View notes