#dengue outbreak response
Explore tagged Tumblr posts
Text
Jamshedpur Cracks Down on Dengue Breeding Sites
JNAC team fines building Rs 10,000 after larvae discovery in Kadma basement Jamshedpur officials intensify inspections and impose fines to combat rising dengue cases, with recent action taken in Kadma area. JAMSHEDPUR – Jamshedpur Notified Area Committee (JNAC) fined a Kadma building Rs 10,000 after discovering dengue larvae during a surprise inspection. Deputy Commissioner Ananya Mittal has…
#anti-dengue measures#जनजीवन#dengue outbreak response#Deputy Commissioner Ananya Mittal#Jamshedpur dengue control#Jamshedpur Public Health#JNAC inspection#Kadma dengue larvae#Life#mosquito breeding prevention#Municipal Health Initiatives#urban pest control
0 notes
Text
Also preserved on our archive
There could be a lot more here about non-pharmaceutical interventions like masking, but some pretty good analysis of the climate of vaccine "skepticism" and disease minimizing we live in.
By David Quammen
Health officials would like to remind you that we are entering that time of the year still quaintly known as flu season. That means autumn to spring. Kids go to school, adults spend more time gathered indoors, people breathe and speak and sneeze and cough at one another, and the latest influenza virus spreads widely.
The reason flu season seems a quaint idea is that we now hear about and maybe worry about so many viruses all year. And well we should.
What if there’s a simultaneous surge of Covid and seasonal flu this autumn? What if infections of respiratory syncytial virus, known as R.S.V., peak at unusual levels, as they did in the 2022-23 season? What if the new strain of mpox, which is especially virulent, continues spreading in Africa and beyond? What if this year’s flu combines with the dreaded H5N1 bird flu and emerges as a nightmare flu? What if a novel virus destined to be called SARS-CoV-3 emerges from a horseshoe bat in a rural village somewhere, gains a few key mutations and comes barreling through the world’s airports?
Oy vey and déjà vu. It’s always virus season now. Maybe none of those worst-case scenarios will happen, but to assume so is to count on fool’s luck.
The notion of flu season is a relic of times when one virus could transfix our response efforts and dominate our collective consciousness. Influenza in 1918. H.I.V. in 1980s and ’90s. Ebola in 2014. We can no longer afford to react on a case-by-case basis. Today we need a broader vision. We need personal, governmental and technological responses that address the full spectrum of viruses that disrupt our lives.
Because they will continue to disrupt our lives. We live amid viruses. We eat them. We breathe them. We touch them on doorknobs and cafeteria trays. All the wild and domestic animals with which we interact, from mosquitoes to mice to the sparrows on the bird feeder and the monkeys in the temple gardens, carry their own freights of them in wondrous variety. Most of these viruses have no chance of infecting a human, but many do. The best way to protect yourself and your family is just what health agencies recommend: Get the vaccines if reputable ones exist.
The best way to help protect your community, your country and the rest of humanity is a more complex proposition. The answers range from public health measures such as better virus surveillance to ending our bone-headed science denialism and finally supporting pandemic preparedness. But it’s not my purpose to unpack those big topics in this small spurt of words.
My purpose is more modest: to refresh your awareness of something you can’t see, not without the help of an electron microscope. Even the human genome contains a sizable portion — roughly 8 percent of it — that was once the genomes of ancient retroviruses, acquired and internalized by our ancestors in the course of infections.
Viruses of concern to humans come and go on various schedules. American dairy cows began their flu season this year around March 25, when the first infections with bird flu were reported in herds in Kansas and Texas. Measles outbreaks tend to be seasonal but more complex. In the tropics they may peak in the dry season, while in temperate climates measles correlates more with school schedules. And now that warmer temperatures are welcoming tropical mosquitoes farther north and south — including ones that transmit viral diseases like yellow fever and dengue — people in Florida and Italy may find that their worst virus season is summer. Climate change is the new force applied to the viral calendar.
Each year another seasonal vaccine is offered because influenza viruses evolve and mix continuously; their genomes entangle like shape-shifting snakes. The most concerning threat is different each year. This year’s flu vaccine in the United States is what’s called trivalent, or three-powered, meaning it contains elements from three different influenza viruses, all of which are circulating and any of which may prove most pervasive and problematic. Manufacturing flu vaccines takes months, so calculated decisions, mixing science and foresight, must be made long before autumn. Increasing efforts to produce even more kinds of vaccines, including some that target multiple virus strains, signal scientific awareness of the point I’m trying to make: We know a virus might get us, tomorrow or next season, but we can’t say which.
Hence the need for a universal flu vaccine, such as one that’s now in clinical trials at the National Institutes of Health. Hence the need for a universal coronavirus vaccine, toward which scientists at the California Institute of Technology, among other places, are working. Hence the need to create combination vaccines that protect against Covid-19 and influenza in one shot, which are also under development in the United States, China and elsewhere. Hence the need to improve ventilation systems for public and private buildings, which can significantly reduce the spread of respiratory viruses.
These are urgent challenges, at which laboratories and public health authorities all over the world are laboring busily. Science takes time; applying its findings takes patience. Persuading the public to adopt behavioral changes — some of which involve a prick in the arm, some of which require placing community welfare on a level with individual independence — is a task that may seem almost Sisyphean, but it remains crucial and doable.
Flu season in America is no illusory concept, and I don’t mean to deride it, merely to expand it. Get the jab if you’re not disqualified by special health conditions. Don’t disqualify yourself by indifference or groundless suspicions. But bear in mind that virus season doesn’t end with the first swallows of spring. We’re in it for the duration.
#mask up#covid#pandemic#public health#wear a mask#covid 19#wear a respirator#still coviding#coronavirus#sars cov 2#H5N1#Flu#avian influenza#influenza#RSV#Mpox#HIV
72 notes
·
View notes
Text
Effective Mosquito Control in Singapore
Mosquito Control
Singapore’s warm and humid climate makes it a perfect breeding ground for mosquitoes. Unfortunately, this also means a higher risk of mosquito-borne diseases like dengue fever. Effective mosquito control is essential not only for individual households but also for entire communities to stay safe from these tiny but dangerous pests.
Why Is Mosquito Control Important?
Mosquitoes aren’t just annoying—they can be deadly. Singapore has seen outbreaks of dengue fever, and with climate change, the risk is only increasing. Mosquito pest control is about more than just avoiding itchy bites; it’s about preventing the spread of diseases that can impact public health.
How Do Mosquitoes Breed?
Understanding how mosquitoes reproduce is key to controlling their population. Female mosquitoes lay eggs in stagnant water, and it takes just seven days for these eggs to turn into adult mosquitoes. Some common mosquito breeding spots include:
Clogged drains
Plant pots and trays
Open containers or buckets left outside
Roof gutters that collect rainwater
Eliminating these breeding sites is the first step toward effective mosquito control.
Ways to Control Mosquitoes in Singapore
1. Eliminate Stagnant Water
This is the most effective and natural way to reduce mosquito populations. The National Environment Agency (NEA) encourages residents to do the “5-Step Mozzie Wipeout” weekly:
Turn over water storage containers
Cover bamboo pole holders
Clear roof gutters
Empty potted plant trays
Check for stagnant water in common areas
2. Biological Mosquito Pest Control
One of the innovative ways Singapore is tackling mosquitoes is by using Wolbachia mosquitoes. These are male mosquitoes infected with a special bacteria that prevents mosquito eggs from hatching when they mate with female mosquitoes. This method has been successful in reducing mosquito populations in trial areas. Another natural mosquito predator is mosquito fish (Gambusia affinis), which feed on mosquito larvae. These fish are introduced into ponds and reservoirs to help control mosquito populations.
3. Chemical Control Methods
Singapore uses fogging to kill adult mosquitoes in high-risk areas, especially where dengue cases are reported. While this method is effective, it is used only when necessary to avoid overuse of pesticides.
Residents can also use mosquito repellent sprays or patches containing DEET, Picaridin, or Citronella oil to protect themselves from bites.
4. Community Involvement and Government Regulations
Singapore takes mosquito control seriously, and the government has strict regulations to ensure public health is protected. The NEA conducts regular inspections, and homeowners can be fined if mosquito breeding is found on their property.
In addition to regulations, community engagement is crucial. Residents are encouraged to report mosquito breeding sites and participate in dengue prevention campaigns.
How You Can Protect Yourself from Mosquitoes
Apart from eliminating mosquito breeding sites, here are some ways to keep mosquitoes away from your home:
Use mosquito nets and screens on windows and doors
Apply mosquito repellent when going outdoors
Wear light-colored clothing to avoid attracting mosquitoes
Use mosquito traps or electric zappers to reduce mosquito populations indoors
Final Thoughts
Mosquito control in Singapore is a shared responsibility. By taking small but effective steps, such as removing stagnant water, using repellents, and staying informed about government measures, we can significantly reduce the mosquito population and protect our health.
Contact ORIGIN for an eco-friendly mosquito control solution!
Visit our website today!
#mosquito control#mosquito bites#mosquitoprevention#pestcontrolsg#pest management#pest control services#singapore pest management#singapore
2 notes
·
View notes
Text
Brucellosis
Case Report
a 45M goat herder in Malaysia develops 3 weeks of fevers, lethargy, night sweats and headache
history revealed he drank unpasteurised milk from said goats, which he also sold to consumers
blood cultures were negative and he tested negative for more common tropical diseases such as malaria, dengue, typhus and lepto
eventually he tested positive for brucella serology, unfortunately about 80 people also developed brucellosis from drinking milk from his farm, and a few lab staff also picked it up from handling their blood samples
consider this differential in PUO

Microbiology
causative organism: Brucella melitensis
gram negative coccobacillus, facultative intracellular
hardy bacteria that can survive prolonged periods in meat/dairy products unless pasteurised/cooked as well as dust & surfaces
picked up in the intestinal submucosa on ingestion and transported by macropahges to lymphoid tissue
it then has the possibility of spreading haematogenously in the liver, spleen, joints etc. causing systemic or localized infection
Transmission
zoonoses (animal associated)
in particular: feral pigs, so hunters are often at increased risk (due to handling the carcasses), but also cattle, sheep, goat and dogs
outbreaks often associated with consumption of unpasteurized milk from infected animals

Epidemiology
global and notifiable disease in most countries
endemic to Mediterraena, South America and the indian subcontinent
in Australia - largely QLD and NT, but now NSW
Increased risk groups (i.e. what to ask on history and what clues on history to consider for brucellosis)
regular contact with animals (herders, abbatoir workers, vets - there are case reports of lab workers who pick up brucellosis etc)
people who ingest unpasteurized dairy/milk, or the undercooked meat of infected animals
History
first described by another European white man, Dr. George Cleghorn, British Army Surgeon in minorca in 1751 on the island of Malta following the Crimean war

it was named for another British white man, Sir David Bruce who led a commission into a fever outbreak among the army in Malta before they found the organism causing the disease (Sir Themistocles Zammit identified that goats transmit it in milk)
Sir bruce also discovered that trypanosoma brucei (also named for him) was the microbe responsible for animal trypanosomiasis/sleeping sickness. incidentally, he was born in Melbourne Australia
trivia with the Crimean war - was ironically a war fought between Russia and the UK + it's Western Allies and the empire that preceded Turkey (Ottoman)
Today the Crimean war is more well known for producing Florence Nightingale, founder of modern nursing and yay, finally a woman in random medical history that hardly is related to brucellosis.
Clinical features
PUO - cyclical fevers, fatigue, headache, insomnia, myalgias/arthralgias, weight loss, anorexia (fairly non specific, but also systemic)
incubation times can be long, which can be deceptive, reportedly up to 50 yrs from first exposure
otherwise, most cases it ranges from 3 days to several week, on average, expect 2-4
sometimes: hepatosplenomegaly
critical on history to clarify travel/living situation or contacts and consumption of unpasteurised dairy or undercooked meat
localized disease also possible, depending on organs involved
up to 40% will report peripheral arthritis, sacroillitis and spondylititis (kinda sounds like ank spa), at worst can cause osteomyelitis and septic arthritis
endocraditis is a rare but serious complication, with a 5% mortality rate, outside of this it's rarely fatal
if the lungs are affected, cough and SOB can occur but hte CXR will be lcear
GBS has been reported to occur following infection
hepatic abscess and granulmoa in a few
also possible: epididymoorchitis and skin manifestations like erythema nodosum
ocular changes like uveitis, cataracts etc.
it really feels rheum flavoured.
Investigations
hints on basic bloods - neutropaenia and anaemia, thromobcytopaenia in the case of hepatosplenomegaly or ITP
raised ESR and CRP, ALP and LDH
elevated LFTs in hepatomegaly
but diagnosis: blood cultures --> can take weeks as slow growing (due to aerosol transmission, must be handled in a biohazard hood as with the case report)
key really: serology is the most commonly used tool
PCR can also be used, including 16S
tissue also an option depending on organ affected
Management:
atypical cover: azith and doxy
several weeks of treatment usually - i.e. if uncomplicated, doxy for 6 weeks (however relapses are common on monotherapy, up to 40%), often rifampicin 600 mg daily for 6/52 is also added or gentamicin
where doxy can't be used, bactrim is the alternative

Sources
CDC guideilnes
WHO guidelines
ETG - behind a paywall, if your institution covers it, uptodate is gold standard, that said, plenty of free resources that provide a great start
Wikipaedia
Statpearls
Case report (There's actually a lot of background pathophysio, investigations and treatment listed in case reports and many are free)
#brucella#brucellosis#crimean war#medblr#infectious diseases#infectious disease#bacteriology#microbiology
8 notes
·
View notes
Text
Brazil snaps into action in response to dengue fever outbreak
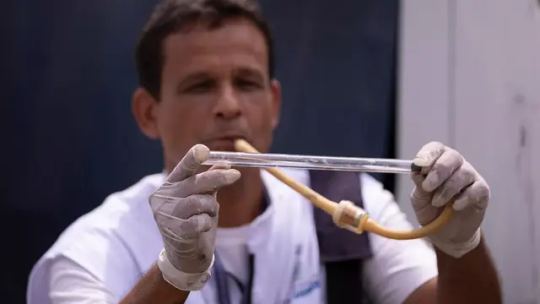
Health authorities in Rio de Janeiro have been working to capture and identify infected mosquitoes as an outbreak of dengue fever hit several of Brazil's cities.
The rise in dengue cases across Brazil has caused several states to declare public health emergencies. Among them are Acre, Minas Gerais and Goias, the Federal District and the city of Rio de Janeiro.
Cases of type 3 virus (DENV-3), which had not been circulating in the country since 2002, began to be reported, prompting Rio de Janeiro's health department to begin a project of vacuuming the mosquitoes to identify the type of virus they are infected with.
Said Mário Sérgio Ribeiro, Under-secretary of the Rio de Janeiro State Health Department said the variant is expected to affect a large portion of the population.
Continue reading.
6 notes
·
View notes
Text
WHO raises alarm on increase in dengue infections

The World Health Organisation, WHO, has raised alarm on the spike in dengue infections recorded in 2023 globally, which represents a potentially high public health threat. The UN health agency raised the alarm on Friday as it reported more than five million dengue infections and 5,000 deaths from the disease globally in 2023. Interfacing with newsmen at the UN headquarters in Geneva, Dr. Diana Rojas Alvarez, WHO Team Lead on Arboviruses, stated that the threat required maximal attention. According to him, the threat also required response from all levels of the UN health agency to support countries in curtailing current dengue outbreaks and prepare for the upcoming dengue season. Dengue is the most common viral infection transmitted to humans bitten by infected mosquitoes. It is mostly found in urban areas within tropical and sub-tropical climates. The increase in the number of reported cases of dengue in more countries is explained by the fact that infected mosquitoes now thrive in more countries because of global warming associated with rising emissions. “Climate change has an impact on dengue transmission because it increases rainfall, humidity and temperature. “These mosquitoes are very sensitive to temperature,” she said. Read the full article
3 notes
·
View notes
Text
Understanding BNS Chapter 15: How It Protects Public Health, Safety, and Morals in India

Imagine walking down a street where garbage is piled up, loudspeakers are blaring without reason, and vendors are selling food that smells off. Now imagine living in a neighborhood where people ignore quarantine rules during a disease outbreak or drive recklessly on narrow lanes. These aren't just everyday annoyances — they are acts that can affect the health, safety, and peace of an entire community.
That’s exactly what Chapter 15 of the Bharatiya Nyaya Sanhita, 2023 (BNS) deals with. It’s a set of laws that focuses on protecting public interest — our shared environment, the safety of our roads, the quality of our food and medicines, and even the moral and social standards of public spaces.
Let’s break this down in a simple, no-jargon way — the way you’d explain it to a friend or a curious student.
What is a Public Nuisance? (Section 270)
A public nuisance isn’t just something annoying — it’s an act that disturbs or harms a group of people in their shared spaces.
If someone dumps construction waste on a busy road, blocks traffic, or creates unbearable noise in a residential area, it affects everyone around. That’s a public nuisance.
The law takes these things seriously, because they directly impact how we live together.
Spreading Diseases Isn’t Just Irresponsible — It’s Criminal
India has had its share of public health emergencies — dengue, swine flu, COVID-19. During such times, personal actions have public consequences. That’s why the BNS covers several laws related to infectious diseases.
Section 271 punishes people who carelessly do something that could spread a dangerous infection. Example: A COVID-positive patient refusing to isolate and traveling by train.
Section 272 goes a step further. It applies when someone deliberately tries to spread an infection. Example: Coughing or spitting in public places knowing you’re carrying a virus.
Section 273 talks about disobeying quarantine rules. When health authorities issue a rule — say, to stay home after returning from abroad — it’s not optional. Disobeying can land you in trouble.
These sections remind us: personal freedom comes with social responsibility.
Food and Drug Safety: You Deserve to Know What You’re Consuming
Let’s say you walk into a street shop and buy a bottle of juice. Or you’re handed medicine from a local pharmacy. You expect them to be safe, right? This is where BNS steps in.
Section 274 makes it a crime to adulterate food or drink meant for sale. Mixing in harmful chemicals to increase quantity or shelf life isn’t just cheating — it can seriously harm people.
Section 275 targets those who knowingly sell noxious or unsafe food. Even if they didn’t adulterate it themselves — selling it is still a crime.
Sections 276 and 277 do the same, but for drugs. Tampering with medicines, or selling diluted or expired drugs, is not just unethical — it’s illegal.
Section 278 says: you cannot pass off one drug as another. Imagine being sold a sugar pill instead of antibiotics.
All of this adds up to a clear message: sellers must be accountable, and consumers must be protected.
Clean Water and Air Are Not a Luxury — They’re a Right
What happens when someone dumps sewage into a village pond? Or a factory releases toxic smoke near a school? That’s where Sections 279 and 280 come in.
Section 279 prohibits contaminating public springs or reservoirs. Clean drinking water isn’t optional.
Section 280 tackles pollution that harms the air. Burning plastic in an open area? That’s not only harmful, but punishable too.
These laws protect our shared environment — because one person’s carelessness can endanger an entire community.
On the Roads and Rivers: Safety Matters
Accidents on roads and waterways are often not due to fate — but human negligence.
Section 281 deals with rash driving. It’s not just about breaking traffic rules — it’s about putting lives at risk. Overspeeding on a narrow street or doing bike stunts in public are examples.
Section 282 talks about reckless handling of boats and ships.
Section 283 penalizes people who install false navigation signals like fake lights or buoys — a serious risk in marine zones.
Section 284 punishes those who ferry people in unsafe or overloaded boats. Festivals or floods often bring this into focus.
Section 285 tackles obstructions — like leaving construction debris in the middle of a public path or road.
These laws ensure our public spaces — roads, rivers, and footpaths — stay safe and navigable for everyone.
Handling Dangerous Stuff? You Better Be Careful
BNS Sections 286 to 291 talk about negligent handling of dangerous materials — from fire to chemicals to even animals.
Section 286: Careless use or storage of poisonous substances.
Section 287: Being irresponsible with fire or flammable items.
Section 288: Not handling explosives safely.
Section 289: Operating dangerous machinery without safety checks.
Section 290: Unsafe building repairs or demolitions.
Section 291: Letting dangerous animals roam free.
One small mistake — a loose wire, a gas leak, or an unattended dog — can lead to injury or death. These sections demand caution and accountability.
Continuing a Nuisance? The Law Won’t Go Easy
Section 292 is a general provision — if something is a public nuisance but not specifically listed elsewhere, it still counts.
Section 293 says: if a court tells you to stop creating a nuisance and you continue anyway, the punishment will be harsher.
This tells us the legal system doesn’t just punish the act — it also expects obedience when asked to correct it.
Morality in Public Spaces: What’s Okay and What’s Not
BNS also tries to regulate public morality — especially when it comes to what’s acceptable in public areas.
Section 294: Selling obscene books or images in public is an offence.
Section 295: Selling obscene content to children is viewed even more seriously.
Section 296: Performing vulgar acts or songs in public places is prohibited.
You may think of this as moral policing, but the idea is simple — everyone deserves to feel comfortable in public, regardless of age or gender.
Gambling Without License? That’s Illegal
Section 297 bans the running of unauthorized lottery offices. Online lotteries, WhatsApp betting groups, or unlicensed gambling setups all fall under this.
It’s about protecting people — especially the poor — from falling into debt traps through illegal gambling schemes.
Final Thoughts: Why This Chapter Matters
Chapter 15 of the Bharatiya Nyaya Sanhita isn’t about targeting individuals for minor mistakes. It’s about building a safer, cleaner, and more decent society for everyone.
Whether it’s ensuring your neighbour doesn’t burn garbage, that the milk you drink is safe, or that medicines you buy are genuine — these laws touch your life more often than you realise.
And they serve a reminder: our actions, even the ones we think are private, often ripple out into public spaces.Laws can’t create change alone — people do. But having a clear legal structure, like BNS Chapter 15, ensures there’s a system to protect the common good when personal responsibility fails.
#BNS Chapter 15#Bharatiya Nyaya Sanhita 2023#public health offences#Indian criminal law#public nuisance law#food adulteration law#rash driving law India#obscene acts law#quarantine rule India#environmental offences India
0 notes
Text
From Fever to Facts: The Role of PCR and NS1 Tests in Detecting Viral Infections
Infectious diseases like influenza and dengue continue to pose a significant public health challenge, especially in countries with seasonal outbreaks. Early and accurate diagnosis remains one of the most critical factors in effective patient management, containment, and treatment. Two diagnostic tools that have gained widespread clinical acceptance are the Influenza Virus PCR Test and the Dengue NS1 Antigen Test.
These tests not only help in detecting the presence of viruses in the early stages but also support clinical decisions that may reduce complications and improve recovery outcomes. In this blog, we will explore the significance of Influenza B Virus PCR Test, Dengue NS1 Rapid Test.
Why Influenza Testing Is Crucial Today
Influenza is often dismissed as a common seasonal illness, but certain strains can lead to serious respiratory complications, especially in vulnerable populations such as the elderly, children, and people with pre-existing health conditions. The Influenza Virus PCR Test, especially real-time RT-PCR, plays an important role in detecting Influenza A and B strains quickly and precisely.
PCR-based testing remains the gold standard for influenza diagnosis because it can detect the virus even when the viral load is low. This is particularly valuable during the early stage of infection when symptoms may still be mild or non-specific. The Influenza Panel Kit from 3B BlackBio is one such diagnostic tool that covers multiple influenza strains, including Influenza B virus, offering clinicians clarity and speed when it matters most.
Influenza B Virus PCR Test: A Focused Approach
Among the various influenza viruses, Influenza B virus has been responsible for many seasonal flu outbreaks. Unlike Influenza A, which can cause pandemics, Influenza B tends to circulate more predictably but can still cause significant illness.
The Influenza B virus PCR test provides accurate and sensitive detection of the Influenza B strain, allowing for precise and timely clinical decisions. Misdiagnosis or delay in identifying the specific strain can lead to inappropriate treatment, making precise testing essential. Kits like TRUPCR® reduce this uncertainty by providing reliable results, backed by robust internal controls and optimized primer designs.
Moreover, laboratory validation shows that these kits maintain high specificity and sensitivity even with minimal viral load, which is often the case in early infection or post-vaccination exposure. This makes it easier for public health authorities to track outbreaks and take swift action.
Dengue: A Persistent Threat in the Tropics
While influenza presents a seasonal burden, dengue continues to affect millions annually in tropical and subtropical regions. Caused by the dengue virus and transmitted via Aedes mosquitoes, this viral infection can lead to severe flu-like symptoms, hemorrhagic fever, and in extreme cases, death.
NS1 antigen serves as one of the earliest and most reliable markers for detecting dengue infection.Detectable within the first 1–9 days of illness, NS1 is a non-structural protein secreted by the dengue virus and serves as a direct indication of active infection.
The Dengue NS1 Antigen Test and Dengue NS1 Rapid Test are essential tools in the early diagnosis and management of dengue. The Dengue NS1 Test by 3B BlackBio offers both qualitative and rapid detection, significantly reducing the turnaround time for results.
Advantages of NS1 Rapid Testing in Dengue Diagnosis
Speed is critical in dengue diagnosis. Traditional methods like IgM/IgG antibody detection often detect the virus much later, which can delay treatment. On the other hand, the Dengue NS1 Rapid Test can offer results in just 15–20 minutes, often at the point of care. This is particularly helpful in outbreak scenarios or rural healthcare settings where lab access may be limited.
Rapid tests help in initiating early hydration, monitoring platelet counts, and avoiding the progression to severe dengue. Furthermore, early detection helps prevent unnecessary antibiotic use, which is ineffective against viruses and contributes to antimicrobial resistance.
The TRUPCR® Dengue NS1 Antigen Test meets global performance benchmarks, providing high accuracy with minimal false positives or negatives. This builds confidence among clinicians and allows timely referrals in serious cases.
Why Choose TRUPCR® Diagnostic Kits by 3B BlackBio
Both the Influenza Virus PCR Test and Dengue NS1 Antigen Test offered by 3B BlackBio Biotech India Ltd are designed with precision, ease of use, and reliability in mind. Whether you're running a busy diagnostic lab or a healthcare facility with limited infrastructure, these kits help streamline the testing workflow while delivering consistent results.
Each kit is backed by thorough validation, internal controls, and high-quality reagents. The company’s strong distribution network and technical support further ensure minimal downtime and smooth lab operations.
Accurate diagnosis of viral infections like influenza and dengue is no longer a luxury—it’s a necessity. In an era where timely action can save lives, having access to fast, accurate, and affordable diagnostic tests is critical.Whether you are a clinician, a lab technician, or a healthcare provider, integrating these trusted diagnostic solutions into your workflow can dramatically enhance your capacity to detect, treat, and manage viral infections effectively.
0 notes
Text
How Do Virology Testing Labs in Abu Dhabi Support Early Detection of Viral Outbreaks? | +971 554747210
In today’s interconnected world, early detection of viral outbreaks is essential for preventing widespread illness and safeguarding public health. Virology testing labs play a crucial role in this global health defense system by identifying viral pathogens rapidly and accurately. In Abu Dhabi, a leading healthcare and scientific hub in the Middle East, virology testing labs are at the forefront of detecting viral outbreaks early, enabling swift response and containment.
This blog explores how virology testing lab in Abu Dhabi support early detection of viral outbreaks, detailing their capabilities, technologies, collaborations, and impact on public health management.
The Importance of Early Detection in Viral Outbreaks
Early detection of viral outbreaks allows health authorities to:
Implement quarantine and isolation measures before widespread transmission occurs.
Conduct contact tracing to identify and monitor exposed individuals.
Accelerate vaccine development and distribution for at-risk populations.
Mobilize public health resources efficiently to affected regions.
Reduce mortality and morbidity rates through timely interventions.
In Abu Dhabi, where international travel and trade converge, the risk of viral diseases entering the community is significant. Hence, the city invests heavily in advanced virology testing labs that can detect outbreaks at the earliest stage.
Capabilities of Virology Testing Labs in Abu Dhabi
1. Comprehensive Viral Diagnostic Services
Virology labs in Abu Dhabi provide a wide range of diagnostic services that enable the identification of diverse viruses, including:
Respiratory viruses (e.g., influenza, RSV, SARS-CoV-2)
Bloodborne viruses (e.g., HIV, hepatitis B and C)
Emerging and re-emerging viruses (e.g., MERS-CoV, Zika, Dengue)
These labs use sophisticated molecular techniques such as polymerase chain reaction (PCR), next-generation sequencing (NGS), and antigen/antibody detection to accurately identify viral pathogens in clinical samples.
2. Rapid Turnaround Time
One of the key factors in early outbreak detection is the speed at which test results are delivered. Abu Dhabi’s virology testing labs are equipped with automated systems and streamlined workflows that enable rapid turnaround times, often within hours, allowing health officials to act quickly.
3. High Sensitivity and Specificity
Advanced molecular diagnostics and quality assurance practices ensure that Abu Dhabi labs maintain high sensitivity (detecting even low viral loads) and specificity (accurately identifying the virus without false positives). This precision reduces delays caused by repeat testing or misdiagnosis.
Advanced Technologies Driving Early Detection
1. Real-Time PCR (RT-PCR)
RT-PCR remains the gold standard for viral detection due to its ability to detect viral RNA/DNA with high accuracy and speed. Abu Dhabi labs utilize RT-PCR extensively for testing respiratory viruses and emerging pathogens.
2. Next-Generation Sequencing (NGS)
NGS technology allows labs to sequence the entire viral genome rapidly, facilitating:
Identification of new viral strains or mutations.
Monitoring of viral evolution during outbreaks.
Tracking transmission chains for epidemiological insights.
This technology was pivotal during the COVID-19 pandemic for identifying variants.
3. Point-of-Care Testing (POCT) and Mobile Labs
Some virology labs in Abu Dhabi support mobile testing units and point-of-care devices that enable testing outside conventional lab settings, such as airports and community clinics. These rapid tests help screen travelers and symptomatic individuals immediately.
Integration with Public Health Systems
Virology testing labs in Abu Dhabi work closely with government agencies like the Department of Health – Abu Dhabi (DOH) and the National Emergency Crisis and Disaster Management Authority (NCEMA) to ensure early warning systems are robust and responsive.
1. Data Sharing and Surveillance Networks
Labs feed real-time test results into centralized surveillance databases, enabling public health officials to monitor infection trends continuously. This integration supports:
Early outbreak detection.
Identification of hotspots and clusters.
Informing policy decisions such as travel restrictions and lockdowns.
2. Collaboration with Hospitals and Clinics
Virology labs maintain strong partnerships with healthcare providers for efficient sample collection and prompt testing. This network ensures that suspected cases are swiftly diagnosed and isolated.
Role in Outbreak Preparedness and Response
1. Routine Screening and Sentinel Surveillance
Regular screening of high-risk groups, such as healthcare workers and travelers, helps labs detect viral activity before it escalates into a larger outbreak.
Sentinel surveillance programs, where selected sites continuously monitor viral infections, provide early signals of unusual viral activity.
2. Research and Variant Tracking
Virology labs conduct ongoing research on viral pathogens, identifying mutations that could affect transmissibility or vaccine efficacy. Early identification of such variants enables timely updates to public health strategies.
Biosafety and Quality Assurance: Ensuring Reliable Early Detection
Maintaining biosafety and quality assurance standards is essential to prevent laboratory-acquired infections and ensure reliable results. Abu Dhabi’s virology labs adhere to ISO 15189 accreditation and follow WHO biosafety guidelines to maintain the highest standards in sample handling and testing procedures.
Case Study: COVID-19 Response in Abu Dhabi
During the COVID-19 pandemic, virology testing labs in Abu Dhabi demonstrated their critical role in early detection by:
Implementing large-scale RT-PCR testing facilities.
Deploying mobile testing units for remote access.
Sequencing viral genomes to identify and track variants.
Coordinating with health authorities for contact tracing and isolation measures.
These efforts helped Abu Dhabi maintain lower infection rates and informed a phased reopening of the economy.
The Future of Virology Testing Labs in Abu Dhabi
Looking ahead, Abu Dhabi is investing in:
Artificial Intelligence (AI) for faster analysis of viral test data.
Integrated digital platforms for seamless data sharing across healthcare systems.
Enhanced mobile labs to reach underserved areas rapidly.
Expanded research collaborations with global health organizations.
These innovations will further strengthen early detection capabilities and preparedness for future viral outbreaks.
Conclusion
Virology testing labs in Abu Dhabi are indispensable pillars in the early detection and management of viral outbreaks. Their cutting-edge technology, rapid diagnostic capabilities, integration with public health systems, and stringent quality controls enable timely identification of viral pathogens. This early detection facilitates swift containment measures, ultimately protecting public health and minimizing economic disruption.
For healthcare providers, policymakers, and the public, relying on Abu Dhabi’s accredited virology testing labs ensures accurate diagnostics and a resilient response system to emerging viral threats — a vital asset in today’s global health landscape.
0 notes
Text
The Role of Biotechnology Labs in Combating India’s Infectious Disease Burden
India, with its dense population and diverse climate, continues to face a significant burden of infectious diseases. From tuberculosis and malaria to emerging threats like COVID-19 and Nipah virus, timely and accurate diagnostics are crucial to control the spread and reduce mortality. In this battle, biotechnology labs in India are playing a pivotal role, driving innovation, accuracy, and speed in healthcare through advanced technologies.
Biotechnology Diagnostics in India: A Game-Changer
Over the past decade, biotechnology diagnostics in India have witnessed tremendous growth. These advanced diagnostic methods, powered by molecular biology, genomics, and data analytics, enable precise detection of pathogens at the genetic level. Unlike conventional diagnostic tools, which often rely on visible symptoms or delayed culture results, biotech-based diagnostics can detect infections even at the asymptomatic stage.
This advancement has proven especially critical in managing diseases like HIV, tuberculosis, hepatitis, dengue, and drug-resistant bacteria, where early intervention is the key to successful treatment.
Inside Biotechnology Labs in India
Modern biotechnology labs in India are equipped with sophisticated tools like real-time PCR machines, DNA sequencers, automated sample handling systems, and AI-powered analytics. These labs are not just limited to big cities anymore. With government support and private sector investment, diagnostic infrastructure is expanding into Tier 2 and Tier 3 cities.
Such decentralization ensures quicker access to quality diagnostics, helping health systems respond more rapidly during disease outbreaks.
These labs focus on various verticals including:
Infectious disease diagnostics
Cancer genomics
Prenatal and newborn screening
Genetic and hereditary disorders
The Bangalore Biotech Hub
A leading contributor to this ecosystem is the thriving biotechnology company in Bangalore segment. Bangalore, known as India’s Silicon Valley, is now also emerging as a biotech capital. The city hosts numerous biotech firms specializing in diagnostics, research, and product development.
These companies are at the forefront of developing cost-effective, high-throughput diagnostic kits tailored to India’s healthcare needs. Their R&D focuses heavily on local disease strains, antibiotic resistance patterns, and culturally adapted testing protocols.
The collaborative ecosystem of startups, research institutions, and healthcare providers in Bangalore has resulted in faster innovation cycles and scalable diagnostic solutions.
Advanced Genetic Testing Services in India
As personalized medicine gains momentum, advanced genetic testing services in India are becoming increasingly accessible. These services go beyond infectious disease detection — they allow for carrier screening, risk prediction, drug compatibility, and even lifestyle-related health assessments.
In the context of infectious diseases, genetic testing helps identify host factors like immune response genes or drug-metabolizing enzyme variants. This helps clinicians personalize treatment and avoid trial-and-error therapies, especially in antibiotic resistance cases.
Moreover, by understanding the genetic makeup of pathogens, researchers can develop better vaccines and targeted treatments.
Genetic Testing Labs in India: Meeting Global Standards
The expansion of genetic testing labs in India has made high-quality testing affordable and scalable. Many of these labs are NABL-accredited and comply with global standards such as CAP and CLIA, ensuring accurate and reliable results.
These labs are vital not only for individual diagnosis but also for public health surveillance. For instance, during the COVID-19 pandemic, many genetic testing labs contributed to large-scale genomic sequencing to track virus mutations and predict outbreak trends.
Such initiatives enhance the country’s preparedness for future pandemics.
Molecular Diagnostics Labs in India: Precision in Action
Molecular diagnostics labs in India are the backbone of precision medicine. By focusing on nucleic acid detection, these labs can identify specific pathogens with unparalleled sensitivity and specificity.
Techniques like RT-PCR, LAMP, and next-generation sequencing (NGS) are used extensively in these labs to diagnose infections like tuberculosis, HPV, hepatitis, and even fungal diseases.
The ability to detect multiple pathogens from a single sample — called multiplexing — is another breakthrough these labs are adopting, reducing testing time and improving diagnostic yield.
DNA Sequencing Services in India: Enabling Disease Surveillance
Another major development is the growth of DNA sequencing services in India. These services allow labs to decode the genetic structure of pathogens. Such insights are crucial for understanding mutations, tracking disease transmission, and developing vaccines.
During viral outbreaks, sequencing enables real-time monitoring of strain evolution and supports more accurate public health responses.
Conclusion
Biotechnology labs in India are no longer just support systems; they are active warriors in the country’s fight against infectious diseases. With the rise of biotechnology diagnostics in India, cutting-edge molecular diagnostics labs, and a robust network of genetic testing and DNA sequencing services, the country is better prepared to tackle both existing and emerging health threats.
As biotechnology companies in Bangalore and other hubs continue to innovate, the future of healthcare in India looks not only more responsive but also more personalized and data-driven. By investing in this ecosystem, India is making great strides toward a healthier and more resilient society.
0 notes
Text
How Are Vaccine Additives Transforming Immunization Strategies for a Healthier Future?
In the global pursuit of advanced immunization, vaccine additives—commonly known as vaccine adjuvants—are emerging as critical components that enhance vaccine efficacy and longevity. As we navigate complex public health challenges such as rising infectious diseases, zoonotic outbreaks, and the growing demand for personalized healthcare, vaccine immunogenicity modulators are at the forefront of next-generation vaccine design.
According to market projections, the global vaccine adjuvants market is expected to grow from USD 0.70 billion in 2024 to USD 0.96 billion by 2029, registering a CAGR of 6.5%. This growth trajectory is backed by escalating R&D investments, government immunization programs, and the need for robust immune responses through safer and more efficient formulations.
Download our executive market outlook report to explore strategic investment insights and technology forecasts for the vaccine additives market.
Why Are Vaccine Additives Gaining Prominence?
Vaccine additives play a pivotal role in boosting the immunogenicity of antigens. By enhancing the immune response, these substances reduce the amount of antigen required, minimize dosing frequency, and increase long-term protection. As the global vaccine landscape evolves, the importance of these vaccine immunogenicity modulators is becoming more pronounced, particularly in:
Pandemic preparedness (e.g., COVID-19, Influenza)
Emerging zoonotic diseases
Veterinary and combination vaccines
Personalized vaccine solutions
Moreover, the development of novel additives such as saponin-based adjuvants and Toll-like receptor (TLR) agonists are setting new standards for immune modulation, safety, and efficacy.
Who Are the Key Players Driving Innovation?
The vaccine adjuvants market is marked by intense competition and strategic innovation. Leading players are not only expanding their product portfolios but also strengthening their geographic reach to capitalize on global demand. Here’s how some of the top-tier companies are shaping the future of vaccine additives:
GSK Plc (UK)
A global leader in vaccine development, GSK offers a robust adjuvant portfolio backed by extensive R&D and manufacturing infrastructure. With a presence across North America, Europe, Asia, and emerging markets, GSK is well-positioned to address region-specific immunization needs. Its strategic focus on innovative vaccine immunogenicity modulators enables it to remain a preferred partner for public and private immunization programs.
SEPPIC (France)
Renowned for its innovative adjuvant technologies, SEPPIC delivers a wide array of squalene-based emulsions and polymer-based additives designed for both human and veterinary vaccines. Its product, MONTANIDE GR 01, launched in October 2022, showcases a tailored approach to veterinary oral vaccines. The company's commitment to next-gen immunogenicity modulators underscores its leadership in functional vaccine formulations.
Croda International Plc (UK)
With a presence spanning Europe, North America, Latin America, and Asia Pacific, Croda offers high-performance vaccine additives supported by state-of-the-art manufacturing and regulatory compliance. The company focuses on sustainable innovation and formulation science, delivering scalable adjuvant solutions for pandemic and routine immunizations alike.
Other significant players include:
Dynavax Technologies (US) – Known for its TLR9 agonist adjuvant CpG 1018 used in HEPLISAV-B.
Novavax (US) – Developer of Matrix-M™, a saponin-based adjuvant used in protein-subunit vaccines.
Merck KGaA (Germany) – Offers liposome and polymer-based adjuvants for therapeutic and prophylactic vaccines.
What Factors Are Fueling Market Growth?
Several macro and microeconomic trends are converging to drive demand for vaccine immunogenicity modulators, including:
Rising global disease burden: Persistent outbreaks of flu, dengue, RSV, and new pathogens are increasing the need for potent vaccine formulations.
Demand for combination and personalized vaccines: Targeted solutions require highly adaptive adjuvants.
Zoonotic disease surveillance: In both human and veterinary healthcare, the demand for safe and efficacious additives is on the rise.
Technological innovation: Advancements in nanotechnology, bioengineering, and delivery systems are enabling better absorption and immune response.
These forces, coupled with growing public-private partnerships and regulatory support, provide fertile ground for the vaccine additives market to thrive.
Where Are the Opportunities for Stakeholders?
For C-level executives, especially in pharmaceutical, biotech, and life sciences companies, the vaccine adjuvants market presents multiple strategic levers:
High-ROI R&D investments in immune-enhancing technologies
Collaborative ventures with public health agencies for global distribution
Regulatory acceleration in emerging markets
Supply chain innovations to ensure scalability and safety
Moreover, the rising interest in vaccine immunogenicity modulators opens avenues for IP licensing, custom adjuvant formulation services, and clinical trial partnerships, especially in precision medicine and rare disease vaccines.
How Can Organizations Stay Competitive?
To stay ahead in this fast-moving space, companies must:
Invest in next-gen adjuvants: Focus on TLR agonists, saponin derivatives, and biodegradable polymers.
Strengthen regulatory and manufacturing compliance: Ensure global cGMP and WHO prequalification standards.
Expand global footprint: Target regions with rising vaccine demand (e.g., Africa, Southeast Asia, Latin America).
Adopt digital platforms for R&D collaboration, supply chain tracking, and global distribution.
Final Thoughts: The Strategic Value of Vaccine Additives
The strategic role of vaccine additives as vaccine immunogenicity modulators cannot be overstated in the current public health landscape. As the world braces for future pandemics and pushes the envelope in personalized and veterinary vaccines, the need for efficient, adaptable, and safe adjuvants will only intensify.
Executives who recognize this shift—and align their operations, innovation strategies, and global partnerships accordingly—will not only achieve higher ROI but also play a vital role in building a more resilient and health-secure world.
Get 10% Free Customization on this Report
0 notes
Text
Creating a Safer Environment with Expert Disinfection and Pest Control Services in Delhi
In a city as dynamic and densely populated as Delhi, maintaining hygiene and controlling pests are vital for health, safety, and peace of mind. Urban living comes with its unique challenges—ranging from viral outbreaks to pest infestations—that can disrupt both residential and commercial spaces. Fortunately, a combination of professional disinfection and targeted pest control services can go a long way in safeguarding your surroundings.
Whether it’s a post-pandemic clean-up or a seasonal spike in mosquito populations, relying on certified experts ensures both effectiveness and safety. Here's why investing in Disinfection Services in Delhi and pest control solutions should be a priority for every responsible home and business owner.
The Critical Role of Disinfection Services in Delhi
Delhi’s fast-paced lifestyle and high population density make it particularly vulnerable to viral and bacterial outbreaks. From flu viruses to more severe infections, harmful pathogens can spread easily through shared surfaces, contaminated air, or human contact. This is where professional-grade Disinfection Services in Delhi play a vital role.
Using advanced fogging machines, hospital-grade disinfectants, and EPA-approved sanitizers, disinfection experts target viruses, bacteria, and fungi present on surfaces and in the air. These services are particularly crucial in:
Homes with vulnerable individuals like children or the elderly
Offices, schools, and gyms with high foot traffic
Restaurants and hotels striving to meet health and safety regulations
When you choose Professional Disinfection in Delhi, you're not just eliminating germs—you're investing in peace of mind. Unlike basic cleaning, professional disinfection targets pathogens at a microscopic level, ensuring thorough sanitation and long-term hygiene.

Fight the Bite with Mosquito Control Services in Delhi
The threat of mosquito-borne diseases like dengue, malaria, and chikungunya is a persistent concern in Delhi. Water stagnation, especially during monsoon season, creates ideal breeding grounds for mosquitoes across neighborhoods.
Mosquito Control Services in Delhi are essential to reduce the mosquito population and lower the risk of disease transmission. These services usually include:
Larvicide treatments in stagnant water sources
Adult mosquito fogging in outdoor areas
Indoor residual spraying for long-lasting protection
Integrated pest management also encourages educating residents about preventive measures like removing standing water, installing window screens, and using mosquito repellents. However, the real difference is made when you bring in trained experts with industrial-grade solutions.
Smart Solutions with mosquito pest control delhi
While DIY repellents and sprays may offer temporary relief, they seldom address the root cause of infestations. Professional mosquito pest control delhi solutions are designed for sustained impact. These services are tailored based on the specific environment—be it residential gardens, commercial lawns, or public parks.
Specialist teams use eco-friendly chemicals and modern application techniques to break the mosquito lifecycle at every stage. From larval control to adulticide sprays, mosquito pest control delhi ensures that mosquitoes are eliminated effectively and responsibly.
Keep Your Property Rodent-Free with Mouse Control in Delhi
Mice and rats may be small, but their impact can be massive. In addition to damaging property by gnawing on wires, insulation, and furniture, rodents are carriers of diseases like leptospirosis, hantavirus, and salmonella. Their rapid reproduction makes it difficult to control them without professional help.
That’s why Mouse Control in Delhi is a critical service for any space showing signs of rodent activity. These signs include:
Droppings around food packages or drawers
Scratching noises in walls or ceilings
Chewed wires or insulation
Professional Mouse Control in Delhi involves a combination of trapping, baiting, and sealing entry points. Experts also conduct a thorough assessment of the property to locate nests and high-activity zones, ensuring comprehensive removal and prevention.
The Power of Professionalism: Why Choose Expert Services?
With so many over-the-counter options available, you might wonder why hiring professional disinfection and pest control services is worth it. The answer lies in the quality, precision, and long-term results that only trained experts can provide.
Reputed providers like skuaspestcontrol follow industry-standard safety protocols and use scientifically tested methods. From handling hazardous chemicals with care to customizing treatment plans for individual spaces, professionals go beyond the surface to ensure health and safety at every level.
Moreover, scheduling regular services helps in maintaining hygiene and preventing infestations before they spiral out of control. Whether it’s quarterly disinfection or seasonal mosquito treatment, a proactive approach is the best defense.

Choosing the Right Partner for Your Needs
Not all pest control or disinfection services are created equal. When selecting a provider, consider the following:
Certifications and licensing
Use of eco-friendly and safe products
Transparent pricing and detailed inspection reports
Post-service guarantees and follow-up visits
Businesses and homeowners across Delhi have come to trust skuaspestcontrol for its reliability, skilled technicians, and commitment to customer satisfaction. Their tailored services, modern equipment, and results-driven approach make them a go-to solution for pest and hygiene management.
Conclusion
In today’s world, hygiene and pest control are not just about aesthetics—they’re essential for health and safety. With the rising risks of viral infections, vector-borne diseases, and rodent infestations, relying on professional services is no longer optional.
From comprehensive Disinfection Services in Delhi to effective Mosquito Control Services in Delhi and smart Mouse Control in Delhi, your health and comfort depend on timely action. Invest in your safety with reliable solutions that protect your space year-round.
1 note
·
View note
Text
What to Do When Fever Strikes: A Local Guide for Pune Residents

Fever is a common health issue that can affect anyone at any time. It is often the body’s natural response to infections, but ignoring it or treating it carelessly can lead to complications—especially during seasonal changes or sudden viral outbreaks. In a city like Pune, where the weather shifts quickly and infection rates can rise in certain months, knowing how to respond to fever is very important.
This guide will help Pune residents understand how to manage fever safely, when to seek help, and where to find trusted care nearby.
Understanding Fever: What Does It Mean?
Fever is not a disease but a symptom. It means your body is trying to fight off an infection. A normal body temperature is around 98.6°F (37°C). When it goes above 100.4°F (38°C), it's considered a fever.
Common Symptoms Along with Fever:
Body aches
Chills or sweating
Headache
Weakness
Loss of appetite
Feeling hot or flushed
Why Fever Is Common in Pune
Pune’s climate, especially during monsoon and winter, often leads to a rise in viral infections and flu cases. People in the city may experience sudden fever due to:
Viral infections like flu, cold, or dengue
Contaminated water or food
Seasonal allergies
Sudden weather change
Mosquito-borne illnesses in rainy seasons
Children, older adults, and those with low immunity may fall sick more often during such times.
What You Can Do at Home
Not all cases of fever need immediate hospital visits. For mild to moderate fever, home care can be helpful.
Steps to Follow at Home:
Get enough rest and sleep
Drink plenty of fluids (water, soup, juice)
Use a cold wet cloth on the forehead to reduce body heat
Wear light and comfortable clothing
Avoid heavy food; eat simple meals like khichdi or fruit
If needed, paracetamol may help reduce the temperature, but it should only be taken if advised by a doctor.
When You Should See a Doctor
While some fevers go away in a day or two, there are signs that mean you need professional medical help. Don't wait too long if:
Fever is above 102°F and lasts more than 2 days
There is a rash, vomiting, or severe headache
The person feels confused or very weak
The fever returns again after recovery
It's a child under 5 or an elderly person with other health issues
In such cases, it’s important to visit a nearby clinic or hospital for proper diagnosis and care.
Trusted Fever Treatment in Pune
For reliable fever treatment in Pune, there are many good hospitals, clinics, and fever OPD centres available across the city. From general practitioners to specialized fever clinics, help is available in every area.
Whether you live in Kothrud, Wakad, Hadapsar, or Camp, most areas have well-trained doctors and labs for quick testing. Residents looking for trusted fever treatment in Pune can easily find reliable care with experienced professionals.
Preventive Tips to Stay Safe
Taking care of your health before you fall sick is always better. Here are some simple ways Pune residents can protect themselves from common fever-related illnesses:
Wash hands regularly with soap
Drink clean and filtered water
Use mosquito nets or repellents in the rainy season
Avoid outside food during viral outbreaks
Keep your home clean and well-ventilated
Wear proper clothes according to the weather
Consider taking seasonal vaccines, like the flu shot
For Children and Elders: Extra Care Needed
Young children and elderly family members often have a weaker immune system. So, a simple fever can become serious quickly. Always keep a thermometer at home and check their temperature if they look tired or weak.
In case of any doubt, it is better to take them to a nearby pediatric or general physician without delay. Pune has several child specialists and elder care facilities available for timely support.
Conclusion
Fever is common, but it should not be ignored—especially in a city like Pune, where seasonal changes can trigger health issues. With proper care at home, awareness of danger signs, and easy access to medical support, most fevers can be managed well.
If symptoms don’t improve or if the fever is severe, always consult a local doctor. Many healthcare centres in Pune offer timely care, lab tests, and treatment that can prevent further health problems.
Stay aware, stay safe—and don’t delay care when needed.
you or someone in your family feels unwell with a fever, don’t guess—consult a nearby doctor for trusted fever treatment in Pune. Early care makes recovery faster and easier.
For More Information About Chest and TB Specialist in Pune - Click here
0 notes
Text
Serology Test Kits and CRP Turbilatex
In today’s healthcare landscape, early diagnosis and targeted treatment are crucial to improving patient outcomes. Two powerful diagnostic tools — the Serology Test Kit and the CRP Turbilatex — help clinicians make informed decisions quickly and efficiently. This blog explores how these tools work, what they detect, and why they’re so important in both routine and emergency medical settings.
What is a Serology Test Kit?
A Serology Test Kit is designed to detect antibodies or antigens in a patient’s blood. These kits are commonly used to diagnose infectious diseases, autoimmune disorders, and other conditions where the immune system plays a central role.
Common Uses:
Infectious diseases like HIV, hepatitis, syphilis, dengue, and COVID-19
Autoimmune diseases such as lupus or rheumatoid arthritis
Allergy testing and vaccine response assessment
How It Works:
Serology kits typically use ELISA (enzyme-linked immunosorbent assay), lateral flow, or chemiluminescent immunoassay technologies to detect the presence of IgM or IgG antibodies, or specific antigens.
Why It Matters:
Serological testing provides insights into a patient’s immune status and helps track the course of infection. It’s essential for outbreak control, epidemiological surveillance, and disease screening.
What is CRP Turbilatex?
CRP Turbilatex is a reagent used in turbidimetric immunoassays to measure C-reactive protein (CRP) levels in blood. CRP is an important biomarker of inflammation and is elevated in conditions such as:
Bacterial infections
Autoimmune diseases
Cardiovascular risk
Post-surgical complications
How It Works:
CRP Turbilatex uses latex particles coated with anti-CRP antibodies. When mixed with a patient’s serum, any CRP present binds to the latex particles, causing visible turbidity. This turbidity is measured by automated analyzers to determine CRP concentration.
Clinical Significance:
High CRP levels often suggest acute bacterial infection or severe inflammation
Moderate levels may indicate chronic inflammatory conditions
Normal levels can help rule out bacterial causes in differential diagnosis
Advantages:
Rapid and reliable
Automated and quantitative
Suitable for high-throughput laboratories
Combining Serology and CRP Testing for Better Diagnosis
While a Serology Test Kit helps determine exposure to specific pathogens or immune conditions, CRP Turbilatex offers insight into the severity and nature of inflammation. Used together, they provide a comprehensive picture:
In infectious disease diagnosis, serology can confirm the pathogen, and CRP helps assess the severity and guide treatment.
In autoimmune conditions, serology identifies specific autoantibodies, while CRP indicates ongoing inflammation.
For post-operative care, CRP monitoring can signal infection or complications even before clinical symptoms appear.
Final Thoughts
The combination of a Serology Test Kit and CRP Turbilatex is a powerful diagnostic strategy. These tools are widely used in hospitals, diagnostic labs, and clinics to support fast, accurate, and actionable healthcare decisions. As medical diagnostics continue to evolve, the integration of serological and inflammatory markers remains central to personalized and preventive medicine.
0 notes
Text
Why You Need a Travel Vaccine Clinic Before You Fly

Travel give tomorrow the memory of a lifetime: exploring the busy cities, trekking through the jungle, or just relaxing on an isolated island. But while you’d be very busy preparing your itinerary, booking flights, and shopping for gear, sometimes a key step will be easily overlooked: protecting your health and vaccines.
If travel vaccine clinic near Essex has been searched in your recent searches, the answer would be Icon Travel Clinic, a reputable name for travel health, thus assuring your protection wherever your trip takes you.
What Is a Travel Vaccine Clinic?
A travel vaccine clinic is a specialized type of healthcare practice that provides immunizations and health advice for international travelers. Unlike general practitioners, travel health specialists keep abreast of disease trends around the world and the specific demands of the various destinations.
From Africa through Asia, South America, or anywhere in between, a travel clinic makes sure you’ll be aware of:
What vaccines are compulsory or recommended
How to keep yourself safe against vector-borne diseases like malaria or dengue
Which medications you might have to take
Precautions for food and water, insect bites, and altitude sickness
Why Searching for a Travel Vaccine Clinic Near Essex Is Important
Typing travel vaccine clinic near Essex into your search bar means that you are not only looking for convenience, but above all, expertise, accurate information, and timely response.
Why you should visit local travel vaccination clinics such as Icon travel Clinic:
1. Destination-Specific Advice
Every country has different health risks and entry requirements. Therefore, a travel-medicine-specializing clinic will provide you with the most appropriate and personalized recommendations according to your destination and itinerary.
2. Expert Knowledge
Travel clinics keep themselves abreast of global outbreaks and health advisories so that they can give you current advice not supplied by normal GPs.
3. Last-Minute Appointments
Wet your vaccines and consultations if you will travel shortly. A clinic such as Icon Travel Clinic will provide you with a same-day or next-day appointment so that you can go with peace of mind.
4. Complete Health Preparation
From Yellow Fever certificates, prescriptions for malaria prophylactics, anti-malaria, or a travel adapter for first-aid kits, a good travel clinic provides more than merely vaccines. It sets you up for any medical eventuality whilst abroad.
Most Common Travel Vaccinations You May Need
According to your destination, your length of stay, and what activities you plan on doing, you may require some of the following vaccines:
Hepatitis A and B,
Typhoid,
Yellow Fever,
Rabies,
Japanese Encephalitis,
Meningococcal Meningitis,
Tetanus/diphtheria/polio,
Cholera.
Icon Travel Clinic carries out all of these vaccinations and even more, to ensure you get protected no matter where you go.
Why Choose Icon Travel Clinic?
The question behind looking for the best trusted answer to travel vaccine clinic near Essex highlights why Icon Travel Clinic stands out:
✓ Experienced Travel Health Specialists
Our clinicians are trained in travel medicine and keep themselves updated with international vaccination guidelines.
✓ Comprehensive Services
We cover pre-travel consultation, immunization for every single condition, travel medicines, and assistance after travel.
✓ Fast, Flexible Appointments
Travel comes with changes and we understand that. Keeping that in mind, we act fast and offer utmost flexibility in scheduling.
✓ Competitive Pricing
Being able to travel safely shouldn’t be a question of price. Hence, we keep prices competitive.
✓ Convenient Location
Located centrally and easily accessible, our clinic is a one-stop center for travelers in need of expert care, and that too speedy.
Final Thoughts
Seasoned or fresher adventurer, your health is your utmost concern. Looking for a travel vaccine clinic near Essex will deliver Icon Travel Clinic as your trusted partner, offering expert opinion fast and giving you complete coverage flexibly to suit your travel plans.
Travel safe with Icon Travel Clinic near Essex. Whether you’re trekking jungles or exploring cities, get expert advice, essential vaccines, and last-minute appointments. Our experienced specialists provide destination-specific care and complete health prep to ensure you’re protected abroad. Trust Icon for fast, reliable, and affordable travel health solutions.
Your health should never be left to chance. Travel well-prepared with your essential travel vaccines.
#travel vaccine clinic near Chigwell#travel vaccine clinic#travel vaccine#travel vaccine clinic in Chigwell#travel vaccine clinic in Essex#travel vaccine clinic near Essex
0 notes