#cough. fever. loss of appetite. congestion.
Explore tagged Tumblr posts
Text
How to handle the Outbreak of the Un-Named Virus.
Want to know if you or a friend/loved one has caught the outbreaking virus? Be sure to read up on the process of the infection! If you or anyone close to you is showing any signs, quarantine yourself immediately.
Keep in mind that the virus can be transmitted through the following:
deep bites that have broken through the skin,breathing in the wrong air, sneezing and coughing(germs), physical contact, and/or consuming the flesh of an infected person's corpse.
ALL STAGES OF THE VIRUS ARE CONTAGIOUS.
It is important to quarantine and stay indoors as much as possible during this virus outbreak, if it is necessary to go outside, wear a mask and protective clothing, and bring something with you in case you are found in a situation that requires self defense.
To know whether you or someone else is infected, look out for the following stages....
Tw for: emetophobia, body horror, self harm, death, thoughts of unaliving, implied animal death, and potentially more
Stage 1:
The first stage will seem like the infected has a mild cold or flu. The newly infected will become ill with the following symptoms.
Sneezing
Coughing
Headaches
Fevers and chills
Mild Nausea
Congestion
Sore/itchy throat
Mild body pain
The infected will start showing these symptoms within 15 minutes-3 days, depending on how they caught the virus.
Stage 2:
The stage 1 symptoms become worse, causing the infected person(s) to become violently ill as well as making it very hard to find the energy to move. Stage 2 infected will most likely remain in bed for the majority of the stage. Symptoms include:
Vomiting/heavy nausea
little ability to move (some infected have described the feeling to be like "as if someone was painfully holding them down in place")
loss of appetite
insomnia or oversleeping
throbbing headaches (described as "worse than migraines")
random bruising on the body
Stage 2 can last up to 2-3 weeks before rapidly throwing the infected into the next stage...
Stage 3:
The infected in this stage will suddenly be filled with energy while they are still sick. Their bodies become covered in bruises and small specks of mold begin to form. They have an unpleasant odor. Other symptoms include:
Random fits of happy and sad hysteria
unpleasant mud-like odor that doesn't seem to go away (no matter how much you shower or bathe)
Rapid on and off bursts of energy
Visible and Auditory hallucinations
Bruises and mold spots forming on the body overtime, as if the body is rotting
heavy chest pain
Flesh is beginning to peel and/or "melt" off.
Heightened Paranoia and/or a feeling some described as "A mid life crisis"
Eyes begin to become more "empty" (faded pupils and irises)
It is recommended that in this stage, you say your final goodbyes. Regardless of whether or not you are the infected.
Stage 4:
Stage four is described to be "the most horrifying" out of the five. The infected is no longer energetic and hyper, those feelings are replaced with terror and anger as their pain and suffering get worse. In addition to physical pain and mental torment, the infected is also battling against themselves, trying to stay awake as they fall in and out of consciousness. Symptoms:
More vivid visual and auditory hallucinations that the infected will try to physically or verbally fight.
Harming oneself out of fear and/or frustration (or trying to cause themselves pain to stay conscious)
Seemingly going in and out of "reality", On and off consciousness.
body is slowly beginning to mutate or change (painfully)
bleeding from the eyes, nose and/or ears.
Hair loss or hair growth
Heavy feelings and thoughts about taking ones life to end the suffering or to "stop" the infection from taking them or infecting others around them.
It is important to remember that in this stage, the infected will begin to bite people when they aren't conscious of their selves. If one wishes to kill an infected, it is best to do it in this stage, or allow the infected to end their own life, due to the last stage making the infected harder to kill....
Stage 5 (Final Stage):
Infected has reached the final stage of the virus. They no longer have any consciousness, and have "lost themselves". They are mindless and vicious and see everyone as either an enemy or prey. They actively try to bite and kill anyone who appears to be too close. Their bodies are constantly mutating into inhuman shapes. The process is bloody, the pain is agonizing, and none of it will end until the virus finally kills them from the inside out.
When an infected finally dies, the body will stop moving and begin to decompose rapidly, leaving acid and body parts as the only indication of their existence. However, Only 70% of infected seem to die....
Tips for the virus, quarantining, dealing with infected, and more:
always wear a mask around other people, even if you're inside your home (There is an exception if you live on your own)
If someone in your home is infected and being quarantined, it is advised to say your final goodbyes to them and avoid them at all costs, since as of right now, no cure exists, and the virus is fatal.
if an infected person asks to stay with you or enter your home, do NOT let them in. Even if they are only at the beginning of stage 1. Your safety is more important.
Keep your doors and windows locked at all times, keep the blinds and curtains closed.
If you are in a heavy populated area, try to evacuate and find shelter somewhere more secluded. if you are unable too, consider setting up more traps and security measures.
it is better to starve to death than to eat the flesh of the infected.
For more information and tips, visit our website or text/call our number.
Do not try to kill an infected unless it is out of self-defense.
Animals can also get infected. Their process is much faster and is similar to sickness and rabies. The virus has a 85% chance of killing a fully infected animal.
The government will be required and made to send out food and supplies to everyone once a week. Stay safe. Stay inside.
May all of this end and let us return to our everyday lives.
#hello puppets#hello puppets midnightshow#infected au#morts infected au#infection au#hello puppets au#tw gore#tw body horror#tw emetophobia#tw suicide#tw self harm#tw self destruction
17 notes
·
View notes
Note
what happens when a food objects gets mould? is that something food object owners have to watch out for often?
— ☕️🪶anon
27/09/24 (D/M/Y)
yes, mold is a very common illness in food objects, though other object types can also sometimes be infected. it usually starts through superficial cuts or scrapes that are then infected before the object's immune system can properly contain it, though sometimes infections can just... happen, likely from breathing in spores. it can then spread from the object's surface into the deeper tissues of their body, starting with the initial infection site and progressing to the brain, slowly killing the infected object. this can take anywhere from a couple weeks to up to a year. afterwards, spores will be released from the carcass if left alone, and it's common for fruiting bodies to grow from them. this can even sometimes be observed in living objects and usually is a sign that death is near. infected carcasses must be removed by a trained professional to ensure no further infections can occur.
symptoms include fever, congestion, rattling in the lungs, coughing, sneezing, chronic pain, irritability, aggression, and loss of appetite. even if there's no visible signs of illness, in prolonged infections spores can be found in nearly all body tissue under microscopes. infections that start in the extremities, like the hands or feet of an object, will almost always require amputation to fully remove, and if found in the body of an object surgery to remove large infected portions of the body can be necessary as well.
mold infections are a leading cause of premature death in all food objects. antifungal treatment is very expensive, unfortunately, and most pet owners can't afford it. in the case your object is susceptible to mold i highly recommend being especially cautious of even small injuries.
#answers#spec bio#object husbandry#foods#mold in objects#object diseases#object injury tw#object death tw#object disease tw#i've personally lost fostered objects to untreatable mold infections before#PLEASE take care of your objects. don't let them get infected by this. it's a horrible way to die#☕️🪶 anon
5 notes
·
View notes
Text
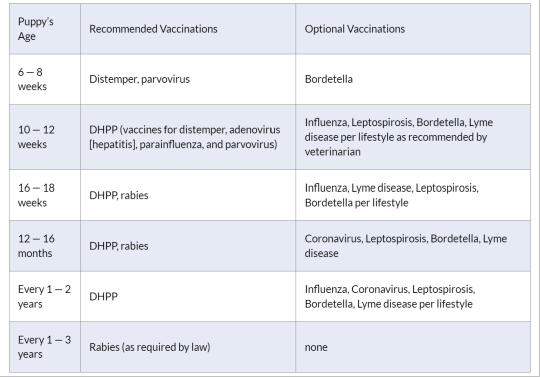
First-Year Puppy Vaccinations

When you bring that fuzzy ball of puppy energy into your home, you know right away that your new puppy depends on you for, well, everything. It’s up to you to give your new puppy all the care they need every day. It can be a little intimidating — your puppy needs the best puppy food, plenty of attention, puppy training, puppy-safe toys, puppy socialization, a comfortable place to sleep, and proper veterinary care. And that includes making sure to schedule puppy shots throughout your puppy’s first year.
Which Shots Do Puppies Need?
Going to the vet over several months for a series of puppy vaccinations—and then for boosters or titers throughout your dog’s life—may seem inconvenient, but the diseases that vaccinations will shield our puppies and dogs from are dangerous, potentially deadly, and, thankfully, mostly preventable.
We read about so many different dog vaccinations, for so many different illnesses, that it can sometimes be confusing to know which vaccinations puppies need and which puppy shots are important but optional. Here is an overview of the diseases that puppy vaccinations will help your pet avoid.
Bordetella Bronchiseptica
This highly infectious bacterium causes severe fits of coughing, whooping, vomiting, and, in rare cases, seizures and death. It is the primary cause of kennel cough. There are injectable and nasal spray vaccines available.
If you plan on boarding your puppy in the future, attending group training classes, or using dog daycare services, often proof of this vaccination will usually be required.
Canine Distemper
A severe and contagious disease caused by a virus that attacks the respiratory, gastrointestinal (GI), and nervous systems of dogs, raccoons, skunks, and other animals, distemper spreads through airborne exposure (through sneezing or coughing) from an infected animal. The virus can also be transmitted by shared food and water bowls and equipment. It causes discharges from the eyes and nose, fever, coughing, vomiting, diarrhea, seizures, twitching, paralysis, and, often, death. This disease used to be known as “hard pad” because it causes the footpad to thicken and harden.
There is no cure for distemper. Treatment consists of supportive care and efforts to prevent secondary infections, control symptoms of vomiting, seizures and more. If the animal survives the symptoms, it is hoped that the dog’s immune system will have a chance to fight it off. Infected dogs can shed the virus for months.
Canine Hepatitis
Infectious canine hepatitis is a highly contagious viral infection that affects the liver, kidneys, spleen, lungs, and the eyes of the affected dog. This disease of the liver is caused by a virus that is unrelated to the human form of hepatitis. Symptoms range from a slight fever and congestion of the mucous membranes to vomiting, jaundice, stomach enlargement, and pain around the liver. Many dogs can overcome the mild form of the disease, but the severe form can kill. There is no cure, but doctors can treat the symptoms.
Canine Parainfluenza
This is one of several viruses that can contribute to kennel cough.
Coronavirus
The canine coronavirus is not the same virus that causes COVID-19 in people. COVID-19 is not thought to be a health threat to dogs, and there is no evidence it makes dogs sick. Canine coronavirus usually affects dogs’ gastrointestinal systems, though it can also cause respiratory infections. Signs include most GI symptoms, including loss of appetite, vomiting, and diarrhea. Doctors can keep a dog hydrated, warm, and comfortable, and help alleviate nausea, but no drug kills coronaviruses.
Heartworm
When your puppy is around 12-to-16 weeks, talk to your vet about starting a heartworm preventive medication. Though there is no vaccine for heartworm in dogs, it is preventable with regularly administered heartworm medication that your veterinarian will prescribe.
The name is descriptive — these worms lodge in the right side of the heart and the pulmonary arteries (that send blood to the lungs), though they can travel through the rest of the body and sometimes invade the liver and kidneys. The worms can grow to 14 inches long and, if clumped together, block and injure organs.
A new heartworm infection often causes no symptoms, though dogs in later stages of the disease may cough, become lethargic, lose their appetite or have difficulty breathing. Infected dogs may tire after mild exercise. Unlike most of the conditions listed here, which are passed by urine, feces, and other body fluids, heartworms are transmitted by mosquitoes. Therefore, diagnosis is made via a blood test and not a fecal exam.
Kennel Cough
Also known as infectious tracheobronchitis, kennel cough results from inflammation of the upper airways. It can be caused by bacterial, viral, or other infections, such as Bordetella and canine parainfluenza, and often involves multiple infections simultaneously. Usually, the disease is mild, causing bouts of harsh, dry coughing; sometimes it’s severe enough to spur retching and gagging, along with a loss of appetite. In rare cases, it can be deadly. It is easily spread between dogs kept close together, which is why it passes quickly through kennels. Antibiotics are usually not necessary, except in severe, chronic cases. Your vet may prescribe a dog-safe cough suppressant to help your dog (and you) get some rest, and some dog-safe throat soothers can help make a dog more comfortable.
Leptospirosis
Unlike most diseases on this list, Leptospirosis is caused by bacteria, and some dogs may show no symptoms at all. Leptospirosis can be found worldwide in soil and water. It is a zoonotic disease, meaning that it can be spread from animals to people. When symptoms do appear, they can include fever, vomiting, abdominal pain, diarrhea, loss of appetite, severe weakness and lethargy, stiffness, jaundice, muscle pain, infertility, kidney failure (with or without liver failure). Antibiotics are effective, and the sooner they are given, the better.
Lyme Disease
Unlike the famous “bull’s-eye” rash that people exposed to Lyme disease often spot, no such telltale symptom occurs in dogs. Lyme disease (or borreliosis) is an infectious, tick-borne disease caused by a type of bacteria called a spirochete. Transmitted via ticks, an infected dog often starts limping, his lymph nodes swell, his temperature rises, and he stops eating. The disease can affect his heart, kidney, and joints, among other things, or lead to neurological disorders if left untreated. If diagnosed quickly, a course of antibiotics is extremely helpful, though relapses can occur months or even years later.
Talk to your vet about when your puppy will be old enough for tick preventatives. Once your puppy is old enough, keep your dog on tick preventative medication, topicals, or wearables to help stop ticks from biting in the first place.
Parvovirus
Parvo is a highly contagious virus that affects all dogs, but unvaccinated dogs and puppies less than four months of age are at the most risk to contract it. The virus attacks the gastrointestinal system and creates a loss of appetite, vomiting, fever, and often severe, bloody diarrhea. Extreme dehydration can come on rapidly and kill a dog within 48-to-72 hours, so prompt veterinary attention is crucial. There is no cure, so keeping the dog hydrated and controlling the secondary symptoms can keep him going until his immune system beats the illness.
Rabies
Rabies is a viral disease of mammals that invades the central nervous system, causing headache, anxiety, hallucinations, excessive drooling, fear of water, paralysis, and death. It is most often transmitted through the bite of a rabid animal. Treatment within hours of infection is essential, otherwise, death is highly likely. Most states require regular rabies vaccinations. Check with your vet about rabies vaccination laws and requirements in your area.
Talk with your veterinarian about more information and guidance on necessary and optional vaccinations.
Puppy Vaccination Schedule
The first thing to know is that there is not just one puppy vaccination schedule for all dogs. Factors such as which part of the country you live in, and your dog’s individual risk factors will come into play. Some dogs do not need every vaccine. This decision is between you and your veterinarian. Always discuss puppy vaccinations at your regularly scheduled appointments.
That said, here is a generally accepted guideline of the puppy vaccination schedule for the first year.
How Much Do Puppy Vaccinations Cost?
How much puppy vaccinations will cost depends on several factors. Where you live is a big one: Veterinarians in crowded and expensive urban areas will generally charge more than a rural vet in a small town. You may be able to find low-cost clinics providing rabies vaccinations sponsored by your local municipal government. But no matter what the range in costs, some vaccines, such as the “core vaccines” and rabies, are necessary.
The average cost can average around $75—100. These will include the core vaccines, which are administered in a series of three: at 6-, 12-, and 16 weeks old.
The core vaccines include the DHLPP (distemper, hepatitis, leptospirosis, parvo, and parainfluenza). Your pup will also need a rabies vaccination, which is usually around $15—20. (Some clinics include the cost of the rabies vaccination.)
Often animal shelters charge less for vaccines — approximately $20 — or are even free. If you acquired your dog from a shelter, he would most likely have been vaccinated, up until the age when you got him.
The initial puppy vaccination costs during the first year are higher than during adulthood.
Vaccinations for Adult Dogs: Boosters and Titers
There is a difference of opinion about having your adult dog vaccinated every year. Some vets believe too many vaccinations in adult dogs pose health risks. But others disagree, saying that yearly vaccinations will prevent dangerous diseases such as distemper. Talk with your vet to determine what kind of vaccination protocol works for you and your dog.
Many dog owners opt for titer tests before they administer annual vaccinations. Titer tests measure a dog’s immunity levels, and this can determine which, if any, vaccinations are necessary. One key exception to this is rabies: a titer test is not an option when it comes to the rabies vaccine. This vaccination is required by law across the United States. Your vet can tell you the schedule for your particular state, with boosters often lasting three years.
And it’s all worth it. For your effort and care your puppy will lavish you with lifelong love in return. This critical first year of her life is a fun and exciting time for both of you. As she grows physically, the wonderful bond between you will grow, too.
#puppy vacinations#puppy vaccines#puppy shots#puppy shots schedule#dog vaccinations#dog health#puppy health
5 notes
·
View notes
Text
Ayurveda , Doctor , Treatment , Nadi Pariksha , Medicine , Pure Herbs , Sri Sri Tattva , The Art of Living ,Sudarshan Kriya , Yoga , Meditation

Sri Sri Tattva Nadi Pariksha
youtube
“Ayurveda” is being recognized as a holistic system of medicine, Which holds that the body is the foundation of all Wisdom and Source of all Supreme Objectives of life.Ayurveda” have effective treatment for, Asthma, Mental Tension , Spinal Disorders , High blood pressure ,
Mental Stress, Spondylosis , High Cholesterol , Fatigue , Obesity , Headaches , Respiratory Problems , Heart Diseases , Migraine , Gastric Complaints , Chest Pain , Arthritis , Weight Loss , Osteoarthritis , Body Purification , Gynecological Disorders , Rheumatism , Anti-ageing , Chronic Constipation , Speech Disorders , Piles , Back Pain , Nervous Disorders , Hair Loss , Gout , Premature Graying , Skin Diseases , Psoriasis , Insomnia , Memory Loss , Pain , Gastric Problems , Immunity Problems , Anemia , Acne , Anorexia , Anxiety , Acidity , Bronchitis, Diabetes , Dyspepsia , Dysentery , Dandruff , Depression , Diarrhea , Dengue , Chikungunya , Indigestion , Urinary bladder disorder , Fungal infection , Nasal Congestion , Gum and Tooth diseases , Vitiation of blood , Burning Sensation , Oedema , Emaciation , Impotency , Inflammation , Ulcer , Thirst , Chloasma of face , Tastelessness , Pleurodria , Intercostal neuralgia , Pthisis , Vitiation of semen , Sciatica , Filariasis , Tumour , Intermittent fever , Lassitude , Hoarseness of voice , Mole , Conjunctivitis , Glaucoma , Myopia , Repeated Abortion , Duodenal ulcer , Malabsorption syndrome ,
youtube
Eczema , Flatulence , Fever , General Debility , Irregular Menstrual Cycle , Jaundice , Hepatitis , joint Pain , Kidney stone , Leucorrhea , Leukoderma ,
Liver Disorder , Menopause , Premenstrual Tension , Pyorrhea , Peptic Ulcer ,
Palpitation , Rheumatism , Ringworm , Stress Management , Sinusitis , Sore Throat , Skin Allergy , Sciatica , Sleeplessness ,Toothache , weight ,
Urinary Diseases , Vertigo , infection , Restlessness , Hypertension ,
Malarial Fever , Cough , Cold , Pimples , Black Heads , Appetite problem , Vomit , Eye problems , Abdominal fever , Abdominal lump ,
Swelling , Fibroid , Cyst , Bleeding , Infertility in men and women ,
Pneumonia , Curing Dryness , wounds, cuts, & burns .
Consult a certified Doctor for more details on Ayurvedic Treatment.
youtube
Sri Sri Tattva Ayurvedic Proprietary Medicine , Single Herbs and Classical Medicine at Glance to Promote Health and Wellness
NAOQ19
AMLAPITTARI VATI ,
AMRUTADI VATI ,
ANCHOLEAN TABLETS,
ATISARAHARA VATI ,
DEVA VATI ,
IMMUGEN TABLETS,
JANTUGHNA VATI ,
JVARA KEERTI VATI ,
KASAHARA VATI ,
LIV-ON TABLETS,
MAMATVA GRANULES ,
MEHANTAKA VATI ,
NARAYANA KALPA TABLET ,
NAVAHRIDAYA KALPA TABLETS,
OORJA FORTE TABLETS,
OORJA TABLET ,
OSPO-C TABLETS ,
PAVANAHARA VATI ,
PITTA BALANCE GRANULES ,
PRADARASHAMAKA VATI ,
PRANADA GUTIKA ,
PRATISHYAYAHARA VATI ,
PYLMUKTI OINTMENT ,
PYLMUKTI TABLET ,
QUICK HEAL CREAM ,
RAKTASHODHINI VATI ,
RAKTAVARDHINI TABLET ,
RAKTAVARDHINI SYRUP ,
SANDHIMITRA VATI ,
SHIRASHOOLARI VATI ,
SHWASA SHUDDHI VATI ,
TWAQURE OINTMENT ,
VEDANANTAKA BALM ,
VEDANANTAKA LINIMENT ,
VEDANANTAKA VATI ,
VIRECHANA VATI ,
VRIKKA SANJIVANI VATI ,
VITILWEL OINTMENT ,
VITILWEL TABLETS ,
AMLA TABLETS ,
AMRUTH TABLETS ,
ARJUNA TABLETS ,
ASHWAGANDHA TABLETS ,
ASHWAGANDHADI TABLETS ,
BRAHMI TABLETS ,
CHANDRAPRABHA VATI ,
CHITRAKADI GUTIKA TABLETS ,
DHATRI LAUH TABLETS ,
HARITAKI TABLETS ,
KAMADUDHA RASA TABLETS ,
KAPIKACCHU GRANULES ,
LAVANGADI VATI ,
NAVAYASA LAUHA TABLETS ,
NEEM TABLETS ,
NISHAMALAKI TABLETS ,
RASNADI VATI ,
SAPTHAMRUTH LAUHA TABLETS ,
SHATAVARI TABLETS ,
SHILAJIT LAUHA VATI ,
SUDARSHAN VATI ,
TRIPHALA TABLET ,
TULASI TABLET ,
VYAGHRYADI TABLET ,
YASHTIMADHU TABLET ,
GOKSHURADI GUGGULU ,
KANCHANARA GUGGULU ,
MAHAYOGRAJ GUGGULU ,
TRAYODASHANGA GUGGULU ,
AVIPATTIKARA CHURNA ,
HARIDRA KHANDA ,
HINGVASTAKA CHURNA ,
PAVANHARA CHURNA ,
SITOPALADI CHURNA ,
TALISADI CHURNA ,
TRIPHALA CHURNA ,
BRAHMA RASAYANA ,
CHITRAKAHARITAKI LEHYA ,
KUSHMANDA RASAYANA ,
NASYA NASAL INHALER ,
SRINETRA STERILE EYE DROPS,
SUDANTA TOOTH DROPS ,
KASAHARI COUGH SYRUP ,
MEDHYA RASAYANA SYRUP ,
PACHANI RASAYANA SYRUP ,
PRADARASHAMAKA SYRUP ,
RAKTASHODHINI ARISHTA ,
SARIVA SYRUP ,
USHIRA SYRUP ,
MAHATRIPHALADYA GHRITA ,
PHALASARPI ,
GOMUTRA ARKA ,
GULMAHARA ARKA ,
ORGANIC AJAMODA ARKA ,
ORGANIC TULASI ARKA,
SANDHIMITRA ARKA,
SHAKTI DROPS,
VRIKKA SANJIVANI ARKA ,
ANU TAILA,
KSHIRABALA TAILA,
NARAYANA TAILA,
PINDA TAILA,
SHISHU TAILA ,
OJASVITA RAGI,
PRADARSHAMAKA VATI,
ALOE VERA JUICE ,
AMLA JUICE,
ALOE VERA TRIPHALA JUICE,
KARELA JAMUN JUICE
KABASURA KUDINEER TABLETS,
KABASURA KUDINEER CHOORNAM ,
TURMERIC PLUS TABLETS ,
GILOY JUICE ,
GILOY TULASI JUICE
AYUSH KWATH TABLETS ,
SUDANTA TABS ,
AYUKANTI LEHYAM ,
OJASVITA GOLDEN LATTICE .
KALAMEGH TABLETS ,
AYUSH - 64 ,
SHANKHPUSHPI TABLETS ,
SUKESHA KALPA TABLETS ,
SUKESHA HAIR VITALISER CREAM ,
Giloy juice
Giloy Tulasi Juice
CHYAWANPRASH ,
ALMOND OIL VEG CAPSULE ,
EVENING PRIMROSE OIL VEG CAPSULE ,
FENUGREEK OIL VEG CAPSULE ,
FLAXSEED OIL VEG CAPSULE ,
GARLIC OIL VEG CAPSULE ,
NIGELLA OIL VEG CAPSULE ,
WHEAT GERM OIL VEG CAPSULE ,
APPLE CIDER VINEGAR JUICE ,
WHEATGRASS JUICE ,
MOORINGA JUICE ,
RAW NONI JUICE ,
Brahmi Vati Suvarnayukta
Bruhat Vata Chintamani Rasa
Mahalaxmivilas Rasa
Shwaskas Chintamani Rasa
Sootashekhar Rasa ( Gold)
Suvarna Vasant Malati
Vasant Kusumakar Rasa
Yogendra Rasa
#Rejuvenate yourself with Ayurveda and Yoga Campaign#Ayurveda#Doctor#Treatment#Nadi Pariksha#Medicine#Pure Herbs#Sudarshan Kriya#Youtube
3 notes
·
View notes
Text
the covid update no one asked for:
11 days since symptoms started
initial symptom was a tickly throat and minor cough
progressed to more of a cough and increased mucus (snot) production. days 2-4 had on-off fevers. the increased snot manifested in runny nose, congestion, and post-nasal drip that fed into the cough. at a certain point, i lost my sense of smell (maybe around day 4-5) along with my sense of taste, both both of those losses were only partial.
since the fever died off, i've still been dealing with brain fog where it's hard to keep track of thoughts in my head. i attempted to return to work on Tuesday (i guess day 9), but by halfway through the day, the brain fog and fatigue was too bad and i had to leave early. day 10 had really bad brain fog that felt like an out-of-body experience all day until maybe 3-4PM. luckily, since then, my brain has felt mostly normal
the snot is still very much real, and as long as that keeps going, i'm going to keep having a cough. i'm hoping it's steadily decreasing, but i guess we'll find out. at least today my appetite has returned, along with my smell and taste
5 notes
·
View notes
Text
"Effective Tuberculosis Treatment with Homeopathy Doctors in Hitech City"
https://g.co/kgs/pFmbS4

Overview of Tuberculosis (TB) and Homeopathy Treatment
Tuberculosis (TB) is a contagious bacterial infection caused by Mycobacterium tuberculosis. It primarily affects the lungs but can also spread to other parts of the body, such as the kidneys, spine, and brain. TB spreads through airborne droplets when an infected person coughs or sneezes.
Causes and Symptoms of Tuberculosis (TB)
Causes of Tuberculosis
Tuberculosis is caused by the bacterium Mycobacterium tuberculosis, which primarily affects the lungs but can also spread to other organs. TB is an airborne disease and spreads through tiny droplets released into the air when an infected person:
Coughs
Sneezes
Speaks
Laughs
Risk Factors for TB
Certain factors increase the risk of contracting TB:
Weak Immune System – HIV/AIDS, diabetes, malnutrition, or cancer can weaken immunity.
Close Contact with an Infected Person – Living or working with someone who has active TB increases exposure.
Overcrowded or Poor Living Conditions – TB spreads faster in congested spaces with poor ventilation.
Smoking and Substance Abuse – These weaken lung function, making it easier for TB bacteria to thrive.
Travel to High-Risk Areas – Countries with a high prevalence of TB pose a greater risk.
Symptoms of Tuberculosis
TB symptoms depend on whether the infection is latent (inactive) or active (symptomatic and contagious).
Common Symptoms of Active TB:
Persistent Cough – Lasting more than three weeks
Coughing Up Blood or Mucus
Chest Pain – Discomfort during breathing or coughing
Fever and Night Sweats – Common in TB infections
Unexplained Weight Loss – Loss of appetite and malnutrition
Fatigue and Weakness – Constant tiredness
Shortness of Breath – In advanced stages
Why Choose Spiritual Homeopathy for Tuberculosis (TB) Treatment?
Spiritual Homeopathy offers a holistic and natural approach to treating Tuberculosis (TB) by strengthening immunity, reducing symptoms, and addressing the root cause. Here’s why it stands out:
1. Natural & Safe Treatment
Homeopathic remedies are made from natural substances and are free from harmful chemicals, making them safe for long-term use without side effects.
2. Boosts Immunity for Faster Recovery
TB weakens the immune system, but homeopathy helps to enhance the body’s natural defense mechanism, speeding up recovery and preventing relapses.
3. Addresses the Root Cause
Unlike conventional medicine, which focuses only on symptoms, homeopathy treats the root cause of TB, whether it’s a weak immune system, nutritional deficiencies, or emotional stress.
4. Personalized Treatment for Every Patient
Every individual’s symptoms and body constitution are different. Spiritual Homeopathy offers customized treatments tailored to each patient's condition for better effectiveness.
5. Complements Conventional TB Treatment
Homeopathy works well alongside allopathic TB medications to reduce side effects, improve lung health, and enhance overall well-being.
Book an Appointment Today! Call/WhatsApp: 9030176176 📍 Visit Spiritual Homeopathy in Hitech City and start your journey towards natural healing and better health!
0 notes
Text
Common Newborn Cold Symptoms and Care Tips
Recognizing newborn cold symptoms early is critical for good care. Babies with a cold may have a runny or stuffy nose, sneezing, a low fever, and irritability. Other symptoms include coughing, loss of appetite, and difficulty sleeping due to nasal congestion.
A newborn's immune system is still growing, so even a minor cold might cause discomfort. Parents should keep a careful eye on their baby's symptoms and keep him or her hydrated. Using a humidifier, saline nasal drops, and gentle suction can all help ease congestion.
If baby cold symptoms last more than a few days or worsen, such as trouble breathing, a high fever, or unwillingness to nurse, seek medical assistance immediately. Keeping the baby away from sick people and practicing good cleanliness can help avoid colds.
Dressing the infant correctly for the weather and providing frequent feedings can help him recuperate. While colds are common in infants, appropriate care and attention can help alleviate symptoms and keep them comfortable. Always visit a pediatrician for advice on symptom management and treatment.
0 notes
Text
My Castle Anthrax
"The inhalation form presents with fever, chest pain, and shortness of breath. The intestinal form presents with diarrhea (which may contain blood), abdominal pains, nausea, and vomiting." - Wikipedia
But first this: "Rheumatoid arthritis is an autoimmune disease." - Also Wikipedia
"Inhalation anthrax usually develops within a week after exposure, but may take up to 2 months. During the first few days of illness, most people have fever, chills, and fatigue. These symptoms may be accompanied by cough, shortness of breath, chest pain, and nausea or vomiting, making inhalation anthrax difficult to distinguish from influenza and community-acquired pneumonia. This is often described as the prodromal period.
Over the next day or so, shortness of breath, cough, and chest pain become more common, and complaints not involving the chest such as nausea, vomiting, altered mental status, sweats, and headache develop in one-third or more of people. Upper respiratory tract symptoms occur in only a quarter of people, and muscle pains are rare. Altered mental status or shortness of breath generally brings people to healthcare and marks the fulminant phase of illness." - More Wikipedia
"About 40% of people who have rheumatoid arthritis also experience signs and symptoms that don't involve the joints. Areas that may be affected include: Skin, Eyes, Lungs, Heart, Kidneys, Salivary glands, Nerve tissue, Bone marrow, Blood vessels
Rheumatoid arthritis signs and symptoms may vary in severity and may even come and go. Periods of increased disease activity, called flares, alternate with periods of relative remission — when the swelling and pain fade or disappear. Over time, rheumatoid arthritis can cause joints to deform and shift out of place." - Not Wikipedia
I'm going to stop here since I'm narcissistic and care more about my own health than others §; for real though, there are many other neuromuscular disorders in Military members, especially Queer-coded (perceived to be queer by the doctor) individuals; which is part of the discrimination against Gays with Arthritis (as if Arthritis were contracted through fluids)
Unfortunately; that's not only a joke.
And that's because I suspect that I may be the patient-zero of Covid. (Narcissistic remember?§)
"Typical COVID-19 symptoms often show up 2 to 14 days after contact with the virus. Symptoms can include: Dry cough, Shortness of breath, Loss of taste or smell, Extreme tiredness, called fatigue, Digestive symptoms such as upset stomach, vomiting or loose stools--called diarrhea, Pain: such as headaches and body or muscle aches, Fever or chills, Cold-like symptoms such as congestion, runny nose or sore throat." - Also not Wikipedia
Ahaha I lied about being done quoting stuff.
"People (with the flu) may experience: Pain areas in the muscles, Cough: can be dry or with phlegm, Whole body: chills, dehydration, fatigue, fever, flushing, loss of appetite, body ache, or sweating, Nasal: congestion, runny nose, or sneezing
Also common: chest pressure, head congestion, headache, nausea, shortness of breath, sore throat, or swollen lymph nodes" - Mayo Clinic on the Flu
Am I starting to paint a vivid picture yet?
There are so many Flu and Flu variants these days; even some like Covid that don't respond as effectively to the Yearly Flu vaccine.
And they all have the same symptoms; and all those symptoms look like what we have termed "Millennial Burnout".
For me specifically; it's possible that I contracted Anthrax (The Flu variant with a Turban and a vest) it's possible that military operations overseas brought these members back (even after taking every measure possible to inoculate our people).
And that has become one of the Fluvid strains here.
Sorry about that; Was just doing muh job.
Now; is this theorycraft entirely accurate? I dunno... I see a bunch of millennial soldiers, airmen, and sea-fairing individuals with all these symptoms of "Millennial Burnout"
Which shares symptoms with neuromuscular disorders, flu, polio, meningitis, Arthritis, and I can't help but think they're all connected.
Now; if it's because Too much stress makes a human being's immune system less effective (and it does) that explains why it's possible to have back to back immunological responses to flu despite getting every single vaccine.
If it's because we've contacted something that looks like pneumonia and walks like Flu; it means there may be a relationship between Anthrax and Covid.
Whatever it is; my disability rating should definitely be higher...
At the very least; I shouldn't be judged so harshly when I feel like I have a mild form of paralytic polio and found *something* that helps reverse or alleviate that when the doctors have failed to find appropriate solutions.
Oh, right, Autoimmune disorders that aren't AIDs tend to be because of an overactive immune system. So they tend to prescribe Things like Humira; which makes you vulnerable to every other thing.
And if that means you're perpetually fending off some infection; it's possible something like Humira is only making the problem worse because they're treating the symptom as if it were the cause.

0 notes
Text
What Is Marjoram? Benefits, Side Effects, and Uses
What is marjoram used for?
Intestinal disorders
Anorexia, Dyspepsia, Diarrhea
Flatulence
Stomach cramps
Improving appetite and digestion
As an antispasmodic (reduces acid secretions of the stomach)
Topical
Ulcers
Clean wounds
Acne
As an antiseptic
Respiratory
Common cold
Runny nose
Cough
Asthma
Nervous disorders
Insomnia
Headache
Liver disorders
Disorders affecting bile flow in the liver
Gallstones
Hormonal issues
Menopause
Menstrual regulation
Premenstrual syndrome
Dysmenorrhea (menstrual cramps)
Ovarian cysts
Polycystic ovary syndrome
Genitourinary diseases
Urinary tract infections
Bladder inflammation
Skin issues
Delays aging
Improves appearance
Lightens dark circles
Chlorosis (decreased iron in the red blood cells)
Fever
Gingivitis
Stomatitis
Muscle or nerve pain
Rheumatic pains
Sprains
Weight loss
Diabetes
12 health benefits of marjoram
1. Antioxidant and anti-inflammatory properties
Marjoram contains antioxidants such as carvacrol, which help prevent cell damage from harmful radicals and reduce inflammation. These properties help reduce the risk of certain diseases, including diabetes, autoimmune disorders, and cancer.
2. Reduces stress
Marjoram oil is widely used in aromatherapy to produce a calming effect, reduce stress, and help ease symptoms of insomnia and depression.
3. Relieves pain
Marjoram may help relieve muscle pain associated with headaches and fevers.
4. Promotes heart health
Marjoram is an excellent source of antioxidants that protect blood vessels and can prevent hypertension and other heart problems.
5. Relieves digestive issues
Marjoram helps improve digestion, controls flatulence, and treats diarrhea and constipation.
It can also help stimulate appetite.
6. Eases common cold symptoms
Marjoram is often used to treat nasal congestion, runny nose, and ear and throat pain.
7. Controls blood sugar levels
Because it helps reduce the absorption of carbohydrates, marjoram may be effective in lowering or maintaining blood sugar levels.
8. Helps regulate hormones
Marjoram has been shown to help regulate menstrual cycles, relieve menopausal symptoms, restore hormonal imbalance, and treat polycystic ovarian syndrome.
9. Good for the kidneys
Marjoram works as a natural diuretic, flushing the system of excess water and toxins including excess sodium and uric acid.
10. Helps prevent infections
Marjoram acts as a natural antiseptic that helps prevent infections, treat acne, and lighten dark skin areas.
11. Slows skin aging
The antioxidants in marjoram oil can help prevent signs of premature aging, such as fine lines and wrinkles. When used regularly, it can make the skin look younger and healthier.
12. Improves hair health
Adding a few drops of marjoram essential oil to shampoo or conditioner can help strengthen hair and encourage healthy growth.
What are potential risks associated with marjoram?
Allergic reactions: Marjoram is not recommended for individuals who have a known allergy or sensitivity to it.
Pregnancy: During pregnancy, marjoram should be avoided because it has mucus-producing properties that can induce bleeding or pregnancy loss.
Breastfeeding: There is no scientific evidence to support the safety of using marjoram in women who are breastfeeding.
Skin irritation: Marjoram can cause contact dermatitis in people with highly sensitive skin.
Drug interactions: Caution is advised for people on medications for the following:
Ulcers
Bradycardia
Bleeding disorders
Scheduled for surgery
ALSO WITHIN THIS ARTICLE:
The 4 Best Spices and Herbs to Fight Inflammation
Reviewed By: Jabeen Begum, MD
Reviewed on 6/13/2022
Inflammation and the Body
Inflammation is an immune system response that supports healing. Although it causes symptoms like swelling and redness, it's a helpful process. But when inflammation becomes chronic, it can cause symptoms that include:
Pain in muscles and joints
Fatigue
Troubled sleep
Depression and anxiety
Digestive problems
Frequent infections
Inflammation is found in many chronic conditions, including heart disease, diabetes, arthritis, and Parkinson's disease. It's a factor in some forms of dementia and many cancers.
In Summary
Ginger, cinnamon, turmeric, and garlic have been used in human studies and have demonstrated anti-inflammatory qualities.
Ginger, cinnamon, turmeric, and garlic have been used in human studies and have demonstrated anti-inflammatory qualities. Other spices and herbs may fight inflammation but may not have been tested on humans. They may have been tested with animals or in the lab instead. These promising medicinal plants include:
Black pepper
Cardamom
Clove
Cumin
Fenugreek
Fennel
Onion
Rosemary
If you are interested in taking spices and herbs as supplements, check with your doctor. Cooking with herbs and spices is unlikely to harm you. Supplements can contain amounts large enough to impact your health. Herbs and spices come from nature, but that doesn't mean that large doses are natural for the human body. Also, supplements are considered food and are not regulated as prescription drugs are.
0 notes
Text
XEC Covid Variant: Symptoms, Spread, and How to Stay Protected This Winter
A new coronavirus variant, XEC, is rapidly spreading and could soon become the dominant strain this winter, according to scientists. First identified in Germany in June, XEC has since been reported in the UK, the US, Denmark, and other countries. Experts are now monitoring its growth closely, anticipating its potential impact during the colder months.
What Is the XEC Covid Variant?
XEC is a recombinant variant that combines characteristics of two previous Omicron subvariants: KS.1.1 and KP.3.3. These parent strains have contributed to recent Covid waves across the globe. KS.1.1, known as one of the "FLiRT variants," and KP.3.3, a part of the "FLuQE" family, exhibit unique mutations in the spike protein, giving XEC an edge in transmission.
Dr. Peter Chin-Hong, an infectious disease specialist at UCSF, notes that XEC possesses "tighter binding cells," potentially making it more transmissible and possibly more immune-evasive than earlier variants. While XEC may not cause a significant spike in hospitalizations or deaths, its enhanced ability to spread has scientists on alert.
How Does XEC Differ from Previous Variants?
XEC has unusual mutations, such as the T22N mutation and additional changes in the spike protein. These differences could provide it with a slight transmission advantage over other Covid variants circulating this fall. However, because XEC belongs to the Omicron lineage, its symptoms and overall severity are expected to be similar to those of previous Omicron strains.
Current Statistics on XEC and Covid-19 Spread
While specific case numbers for the XEC variant are limited, global health authorities continue to monitor its spread along with other Covid-19 variants. The World Health Organization (WHO) reports that globally, during the four-week period from June 24 to July 21, 2024, new Covid-19 cases increased by 30% and deaths by 26% compared to the previous 28-day period, with over 186,000 new cases reported across 96 countries(World Health Organization (WHO). This surge indicates that new variants like XEC may be contributing to the recent increase in cases.
The Centers for Disease Control and Prevention (CDC) in the United States provides regular updates on Covid-19 trends, including hospitalizations, emergency department visits, and test positivity rates. However, specific data on the XEC variant's prevalence in the U.S. is not yet available(CDC COVID-19 Data Tracker). Monitoring the overall Covid-19 trends is crucial as new variants emerge, especially as the XEC variant is believed to have a transmission advantage.
The European Centre for Disease Prevention and Control (ECDC) actively tracks and classifies SARS-CoV-2 variants of concern and interest. Detailed data on the spread of various variants, including XEC, across the EU/EEA, is regularly published, although specific numbers on XEC’s prevalence are still being analyzed.
Symptoms of XEC Covid
The symptoms of the XEC variant are similar to those of previous Omicron variants. These include:
High temperature or fever
Cough and sore throat
Fatigue and body aches
Loss of smell and appetite
Congestion and runny nose
Nausea, vomiting, or diarrhea in some cases
Most people recover within a few weeks, but those who are at higher risk, such as older adults or immunocompromised individuals, may experience more severe illness.
How Is XEC Spreading?
XEC has shown strong growth in Europe, especially in Denmark and Germany. Eric Topol, director of the Scripps Research Translational Institute, has suggested that XEC could become the next dominant variant over the winter. However, this process may take several weeks or even a couple of months.
Monitoring the spread of XEC is more challenging now due to less routine Covid testing compared to previous years. Health agencies, such as the CDC, are using alternative methods like wastewater surveillance to keep track of the virus's spread. Despite these limitations, early indications show that XEC is on the rise in various countries.
How Effective Are Current Vaccines Against XEC?
Since XEC is an offshoot of the Omicron lineage, existing vaccines are expected to provide protection against severe illness caused by this variant. Dr. Chin-Hong has expressed confidence in the updated vaccines, especially for those at higher risk, including older adults and individuals with weakened immune systems.
The vaccines, updated to target recent Covid variants, may not be specifically designed for XEC but should still offer a buffer of protection. Health experts recommend getting the updated booster shots to reduce the chance of infection and lower the risk of developing long Covid.
Who Should Get the Booster Shot?
Health authorities recommend that the following groups receive the updated booster:
Adults aged 65 years and over
Residents of care homes
Individuals over six months old in clinical risk groups
Front-line healthcare and social-care workers
The main vaccination drive for both flu and Covid-19 is set to start in October. However, those at higher risk or planning to travel in the fall should consider getting their booster shot earlier.
Expert opinion
Getting vaccinated is super important, especially for older adults. As we age, our immune systems just don’t work as well, which makes seniors more vulnerable to serious illnesses like COVID-19. During the pandemic, older adults were hit the hardest. In fact, according to the CDC, over 80% of COVID-19 deaths in the U.S. were among those 65 and older. This really shows why getting vaccinated is a must – it significantly reduces the risk of severe illness and death in older adults. Plus, it helps take some of the strain off our healthcare system and keeps our communities healthier overall.
Best regards, Anna Klyauzova LinkedIn Profile Prolife Home Care
Protect Yourself This Winter
As the XEC variant continues to spread, it's important to follow public health guidelines to stay protected. In addition to getting vaccinated, wearing masks in crowded places, practicing good hand hygiene, and maintaining social distancing can help reduce the risk of infection.
FAQs About the XEC Covid Variant
Q: What are the symptoms of the XEC variant? A: The symptoms are similar to previous Omicron variants and include fever, cough, sore throat, fatigue, body aches, congestion, and gastrointestinal issues.
Q: How is XEC different from other Covid variants? A: XEC is a recombinant variant from two Omicron subvariants, KS.1.1 and KP.3.3, with unique mutations that could make it more transmissible.
Q: Are current vaccines effective against the XEC variant? A: Yes, existing vaccines are expected to provide protection against severe illness caused by XEC, though they may not completely prevent infection.
Q: Who should get the updated Covid booster? A: Adults over 65, care home residents, people in clinical risk groups, and front-line healthcare workers are recommended to get the booster.
Conclusion
The XEC variant serves as a reminder that the Covid-19 virus continues to evolve. While vaccines may not be a complete shield against infection, they remain the best defense against severe illness and hospitalization. Global trends indicate a rise in Covid-19 cases, highlighting the importance of staying informed and following health recommendations. By getting vaccinated and adhering to public health guidelines, you can protect yourself and those around you as the winter season approaches.
#brooklyn#prolifehomecare#bronx#homecare#healthcare#manhattan#senior#cdpap#health care#cancer#covid 19#covid is not over#covid vaccine#long covid#xec
0 notes
Text
Spring 2024: It was a time of activity, it was a time of illness… but ultimately, a time of achievements.
So now, we find ourselves in early 2024. Vev’s 11th bday was more or less a non-event (at his own request) — except for us getting goofy and decorating our house with some salvaged decorations that he shamelessly stole after a work event. They were too perfect for Vev—- Pan Am theme!

(It occurs to me that I didn’t post anything about Dey’s 9th birthday, which was in December 2023. Oops, sorry Dey. Here, let me find a picture. We did celebrate it…somehow 😂)

Ok look - we DID do something. The reason I don’t remember is bc he pretty much tore into those Lego sets and was engrossed in building the entire day. Anyway.
Back to Feb 2024 and onward. The kids had a random half-day of school, and so happened that Dr. Spouse was asked by a local news affiliate to film a news segment on brain health - so I decided to take the kids down to the hospital and get a hands-on lesson on both healthcare and journalism. It was a fun and exciting little field trip!

Somewhere around this time, the kids had their respective Field Days at school. I was room parent for Vev’s room last year along with another friend, so I was heavily involved in organizing his class’ Field Day stuff - but I was on site and cheering for both kids, as was daddice for as much as he could manage.

March rolled in, and alas - minor disaster struck. Vev came down with what we thought was a cold… then he got a fever…and then, he was just very, very sick with flu-like symptoms including HIGH 104+ fevers, severe coughing and respiratory congestion, loss of appetite, and overall misery… for TWO WEEKS STRAIGHT. He missed 10 consecutive days of school and was just miserable for weeks - and we were too. Poor kiddo. I was juggling taking care of Dey, keeping him healthy and getting him off to/from school, along with nursing Vev, escorting him to (nightmarish and fury-inducing) pediatrician appointments (long story), sleeping in his room at night to help him get comfortable, overseeing round the clock meds and nebulizer treatments, and being a go-between for him, his teacher, and the school principal to keep him up to date on work. It was a LOT.

Thankfully, spring break immediately followed his two-week confinement, which gave him more time to recuperate - and even gave us a short getaway to Clearwater Beach for a few days once he was really feeling better.

Soon, it was April, then May. We were busy with lots of activities, including numerous Speech and Debate tournaments, and some medals won! I enjoyed volunteering as a judge for these tournaments. We also took a drive down to Ft. Lauderdale to see one of Vev’s drawings from Art class at school that was featured in a local art show for public school kids.

We had some other ups and downs in this time. Both cars were due for vet checkups….. always a time of hijinks and nerves (more for me than the cats). Pixel in particular had some adventures this year - due to her outstanding behavior 🤪 the vet prescribed her some gabapentin to “help her relax” during her physical exam. She was high as a kite.

An era came to an end. On May 5th, Dr. Spouse’s trusty 2014 Tesla Model S died a sudden and very peaceful (almost suspiciously peaceful) death, parked at the front of the kids’ Kumon center. Though the reality was hard to accept, we soon came to terms that we’d have to trade it in and lease a new car. So we all went to bid a final adieu to Red Flyer, aka “Lightning McQueen,” and welcome home Red Flyer 2.

Then, it was JUNE! And the end of the school year.was upon us. We were VERY proud of Dey for an awesome year at school, and of Vev for completing 5th grade, which in our community is a mini-graduation, as the kids head off to a whole new middle school in the fall!

So! This takes us to June 2024, and the end of the school year. Up next will be a synopsis of Summer 2024, which entailed some exciting travel, a bevy of summer camp adventures, and more. One final thought here - maybe it’s my paranoid mom brain, but I feel like this was a Vev-focused post, and I am concerned it looks like I don’t pay as much attention to Dey. But that couldn’t be further from the truth! Dey is everything, everywhere, all over at once - and even if one wanted to ignore him (which I don’t!) it would be impossible, bc he is a total cartoon, and keeps us laughing nonstop 😜 So I’ll make sure to bump up the Dey content in the next post!
0 notes
Text
Cough and Cold in Kids: Symptoms and Home Remedies

Coughs and colds are inevitable parts of childhood. While these common illnesses are typically not serious, they can cause significant discomfort. Knowing how to identify symptoms and treat them with effective home remedies can help your child recover more comfortably and quickly. This article will guide you through the symptoms and provide practical home remedies for managing coughs and colds in kids.
Understanding Cough and Cold Symptoms
Recognizing the symptoms of a cough or cold can help you take appropriate action early. Here’s a breakdown of common symptoms to look out for:
1. Runny or Stuffy Nose
A runny or stuffy nose is often the first sign of a cold.
Signs: Your child may frequently wipe their nose or sound congested. Mucus can be clear, yellow, or green and can vary in thickness.
Observation: Look for nasal discharge and frequent nose blowing.
2. Cough
Coughs can be dry (non-productive) or productive (with mucus).
Signs: Your child may have coughing fits, particularly at night, or a persistent cough during the day.
Observation: Listen for the type of cough and note if it disrupts sleep or daily activities.
3. Sore Throat
A sore throat can accompany a cough or cold, making swallowing painful.
Signs: Your child might complain of throat pain, especially when swallowing, or refuse to eat and drink.
Observation: Check for redness or swelling in the throat.
4. Sneezing
Sneezing is a common way the body expels irritants.
Signs: Frequent sneezing fits, often accompanied by a runny nose.
Observation: Note the frequency of sneezing and if it triggers other symptoms like runny eyes.
5. Fever
Fever often accompanies colds and can be low-grade or higher in some cases.
Signs: Your child might feel warm to the touch, have flushed cheeks, or experience chills.
Observation: Use a thermometer to check for elevated temperature.
6. Fatigue and Fussiness
Illness can make your child feel more tired and irritable than usual.
Signs: Increased napping, less interest in play, and crankiness.
Observation: Note changes in energy levels and mood.
7. Headache and Body Aches
Your child might experience general discomfort or pain, often associated with fever or congestion.
Signs: Complaints of head or body pain, reluctance to move, or holding the head.
Observation: Look for signs of discomfort or pain, particularly in the head and neck area.
8. Loss of Appetite
A reduced interest in eating can occur due to a sore throat or general malaise.
Signs: Skipping meals, eating less, or rejecting favorite foods.
Observation: Monitor eating habits and encourage small, frequent meals.
When to Seek Medical Attention
While most coughs and colds can be managed at home, certain symptoms warrant a visit to the doctor:
1. High Fever
Signs: A fever above 102°F (39°C) lasting more than two days, or any fever in a child under three months.
Action: Consult your pediatrician if the fever is high or persistent.
2. Difficulty Breathing
Signs: Rapid breathing, wheezing, or labored breathing.
Action: Seek immediate medical attention if your child struggles to breathe.
3. Persistent Cough
Signs: A cough that lasts more than two weeks or progressively worsens.
Action: See a doctor to rule out conditions like asthma or pneumonia.
4. Ear Pain
Signs: Complaints of ear pain, pulling at the ears, or discharge.
Action: Visit your pediatrician to check for ear infections.
5. Severe Sore Throat
Signs: Intense throat pain, difficulty swallowing, or refusal to eat or drink.
Action: Consult a doctor to rule out strep throat or other infections.
6. Signs of Dehydration
Signs: Dry mouth, no tears when crying, and reduced urine output.
Action: Increase fluid intake and seek medical advice if symptoms persist.
7. Unusual Symptoms
Signs: Persistent vomiting, rash, or extreme irritability.
Action: Consult a healthcare provider to identify any underlying issues.
Effective Home Remedies for Cough and Cold
Home remedies can help soothe your child's symptoms and promote recovery. Here are some tried-and-true methods:
1. Hydration
Keeping your child well-hydrated is essential.
Importance: Fluids thin mucus, soothe the throat, and prevent dehydration.
Tips: Offer water, clear soups, or electrolyte solutions. Avoid sugary or caffeinated drinks.
2. Honey (for Kids Over 1 Year)
Honey is a natural remedy for soothing the throat and reducing coughing.
Importance: Honey can help to calm a cough and ease throat irritation.
Tips: Give a teaspoon of honey before bedtime. Avoid giving honey to children under 1 year due to the risk of botulism.
3. Warm Fluids
Warm liquids can provide comfort and help with congestion.
Importance: Warm fluids ease throat discomfort and keep mucus moving.
Tips: Offer warm water, herbal teas, or clear soups. Ensure drinks are not too hot.
4. Saline Nasal Drops
Saline drops can help clear nasal congestion in younger children who can't blow their noses effectively.
Importance: Saline helps to loosen mucus and clear stuffiness.
Tips: Use a dropper to place a few drops in each nostril and then gently suction with a bulb syringe for infants.
5. Cool-Mist Humidifier
A cool-mist humidifier adds moisture to the air, making it easier for your child to breathe.
Importance: Humid air helps keep nasal passages moist and reduces coughing.
Tips: Place the humidifier in your child's room, especially at night. Clean the humidifier regularly to prevent mold and bacteria buildup.
6. Steam Inhalation
Inhaling steam can help loosen mucus and clear nasal passages.
Importance: Steam helps to reduce congestion and ease breathing.
Tips: Have your child sit in a steamy bathroom or over a bowl of hot water (with supervision). Ensure the water is not too hot to avoid burns.
7. Elevated Head During Sleep
Raising your child’s head while they sleep can help reduce nighttime coughing and congestion.
Importance: Elevation helps to drain mucus and prevent it from pooling in the throat.
Tips: Elevate the head of the mattress or use extra pillows to prop up your child’s head and upper body.
8. Warm Salt Water Gargle
Gargling with warm salt water can relieve a sore throat and reduce inflammation.
Importance: Salt water can help to reduce throat swelling and discomfort.
Tips: Mix half a teaspoon of salt in a glass of warm water. Teach older children to gargle and spit out the mixture.
9. Chest Rubs
Applying chest rubs can provide comfort and help with breathing.
Importance: Chest rubs provide soothing relief for coughing and congestion.
Tips: Use a mild, child-safe chest rub before bedtime. Avoid applying near the mouth or nose.
10. Avoid Irritants
Keeping your child away from irritants can help prevent symptoms from worsening.
Importance: Reducing exposure to irritants like smoke or strong scents helps to minimize symptom severity.
Tips: Maintain a smoke-free environment and avoid strong perfumes or cleaning products.
Preventive Measures
Taking steps to prevent coughs and colds can reduce their frequency and severity:
1. Frequent Handwashing
Encourage your child to wash their hands regularly to prevent the spread of germs.
Importance: Handwashing reduces the spread of viruses and bacteria.
Tips: Teach your child to wash their hands with soap and water for at least 20 seconds, especially before meals and after coughing or sneezing.
2. Proper Sneezing/Coughing Etiquette
Teach your child to cover their mouth and nose when sneezing or coughing to prevent the spread of viruses.
Importance: Covering coughs and sneezes prevents the spread of germs.
Tips: Show your child how to use a tissue or their elbow to cover their mouth and nose. Dispose of tissues immediately and wash hands afterwards.
3. Avoiding Sick Individuals
Keeping your child away from sick people can help prevent them from catching a cold or cough.
Importance: Limiting exposure to sick individuals reduces the risk of infection.
Tips: Avoid close contact with people who are visibly ill and steer clear of crowded places during cold and flu season.
4. Healthy Diet and Hydration
A balanced diet and adequate hydration support a strong immune system.
Importance: Good nutrition and hydration help the body fight off infections.
Tips: Provide a diet rich in fruits, vegetables, and fluids. Avoid.
1 note
·
View note
Text
Case Records of the Urgent Care 15: The Crimson Tongue
A 5 year old Hispanic girl presented to the urgent care yesterday for a chief complaint of fever. It was described as coming and going, felt from the forehead (tactile), associated with malaise and loss of appetite, lasting about 3 days. However, there was no cough, runny nose, congestion. The child had thrown up once on the day of presentation. There was also note of her toes turning red and…

View On WordPress
0 notes
Text
Rhinitis and Allergies Ayurvedic Treatment

OVERVIEW
Allergic rhinitis is a medical condition which is characterized by the overactive immune response of the body to certain tiny particles in air called allergens. When a person inhales these allergens through nose or mouth, the immune system of the body produces a chemical called histamine in increased amounts. This chemical is responsible for an allergic response of the body. The common symptoms include nasal congestion, frequent sneezing, irritation of nose or throat, etc. It is commonly known as common cold.
The allergens are present both outdoor and indoor such as dust mites, pet dander, molds, pollens, etc. These allergens initiate overactive immune response of the body towards the allergen. With good eating habits and healthy lifestyle, it can be easily managed and prevented. There are some self-care measures which are helpful in its treatment.
WHAT ARE THE CAUSES OF ALLERGIC RHINITIS?
The immune system of body produces white blood cells which help in providing protection to the body from foreign micro-organisms. But in allergic rhinitis, the immune system over-reacts to the presence of an allergen in body. The allergens are inhaled through nose or mouth. The immune system starts an inflammatory response in body. There occurs swelling of the mucous membranes of nose, mouth and throat. It is accompanied by itching in the affected area for the ejection of the allergen.
Some of the common allergens are:
Following are the signs and symptoms of allergic rhinitis:
Nasal congestion
Dust mites
Pollens
Animal dander
Cockroaches
Mold spores
WHAT ARE THE SIGNS AND SYMPTOMS OF ALLERGIC RHINITIS?
Sneezing
Allergy
Runny nose
Itching in nose and throat
Headache
Dark circles under the eyes
Increased mucus production
Malaise
General body weakness
Sore throat
Wheezing
Coughing
Difficulty in breathing
HOW THE DIAGNOSIS OF ALLERGIC RHINITIS IS MADE?
The doctor will ask about the signs and symptoms of the disease to the patient. He will ask patient about any allergies. He can suggest blood tests and an X-ray to the patient. He will ask about the past medical history also.
MANAGEMENT OF ALLERGIC RHINITIS WITH THE MEDICATIONS OF CHANDIGARH AYURVED CENTRE
Here are some of the medications of Chandigarh Ayurved centre which are used for the treatment of allergic rhinitis:1. Detox Premium Powder
These herbal sachets are prepared from ingredients such as Shankh bhasma, Sutshekhar ras, Parvalpishti, Shukta, Giloy, Kamdudha ras, Shvetparpati that gives calming effect on the stomach.
Shankh bhasma: This ayurvedic bhasma is prepared from conch shell. The bhasma shows antispasmodic, anti-inflammatory, antioxidant, antacid, digestive stimulant properties. The problems like indigestion, heartburn, acid reflux, GERD, abdominal pain, loss of appetite, etc are easily treated with it.
Sutshekhar ras: It is an ayurvedic preparation that maintains pitta dosha in the body. This ras provides effective results in abdominal pain, heartburn, nausea, fever, headache, epigastric tenderness, etc.
Parval pishti: This pishti is prepared from coral calcium processed in rose water. It provides effective results in acidity, burning sensation, headache, etc.
Shukta pishti: This pishti balances the pitta dosha in the body and removes all toxins from the body.
Giloy satv: Giloy satv possesses antioxidant, anti-inflammatory, carminative, immunomodulator, etc properties. It eliminates the ama from body hence provide good results in acidity problem.
Kamdudha ras: This ras reduces heat, burning sensation, epigastrium tenderness, irritability, heartburn, and acidity.
Shwet parpati: It is also effective in acidity.
Recommended Dosage: Take one sachet twice daily.
2. Nerve up tablet Nerve up tablets help in balancing the vata doshas. It reduces kapha dosha, and acts as nervine stimulant. It shows effective results in improving the central nervous system. It contains natural ingredients like shudha kuchala, shudha shilajeet, praval pishti, shankh bhasma etc. This tablet helps in the symptoms related to Allergy. Recommended Dosage– Take 1 tablet twice daily.
3. Curcumin Capsule Curcumin Capsule helps in pacifying all three doshas. Curcumin Capsule is beneficial for variety of skin conditions like Acne, Eczema, Psoriasis, and Dermatitis. This Capsule contains standardized extract of the herb Curcumin (Curcuma longa). Curcumin is the active ingredient in Turmeric having powerful Anti-inflammatory, Antibacterial, Antifungal, Anti-microbial and Antioxidant properties. Recommended Dosage: Take 2 capsules twice daily.
4. Amrit Tulsi Ras This herbal preparation is in drops form prepared from five types of Tulsi. Shama Tulsi (Ocimum sanctum), Rama Tulsi (Ocimum gratissimum), Kapoor Tulsi (Ocimum canum), Shwet Tulsi (Ocimum basilicum), Nimba Tulsi (Ocimum citriodorum) that provides good result in all allergic reactions. Recommended Dosage: Take two to three drops twice daily.
5. Immuno Booster Tablet It is a pure herbal combination that helps to build up immunity. It consists of effective levels of antioxidants. vitamin C and E circulate in the body to protect it against the damage caused by free radicals. It has natural immunity-boosting properties to prevent and ease cough, cold, headache, and infections. it provides quick relief from early signs of running nose, itching throat, body ache, and weakness. Recommended Dosage– Take 1 tablet twice daily.
0 notes
Text
Cold
Symptoms – sore throat, sneezing, runny/blocked nose, cough, mild fever, pressure in ears, headache, myalgia (pain in muscles)
Duration – 1-2 weeks, symptoms peak 2-3 days, incubation period 10-12 hrs
Referral criteria – suspected flu, earache not responding to analgesia, sinus pain not responding to decongestants, no improvement after 10-14 days self-medication
Complications - immunocompromised, who smoke, and with comorbidities such as diabetes mellitus, congestive heart failure, asthma, chronic obstructive pulmonary disease, cystic fibrosis, and sickle-cell disease
Sinusitis – prolonged nasal congestion and facial pain
LRTI - acute bronchitis, acute exacerbation of asthma or chronic obstructive pulmonary disease (COPD), and community-acquired pneumonia
Acute otitis media – common in younger patients
Differential diagnosis
Meningitis – high fever, drowsiness, blank expression, vomiting, loss of appetite, high pitched screaming, non-blanching rash, photophobia, severe headache, malaise
Upper airway obstruction – noisy breathing, drooling, inability to swallow.
Nasal foreign body – persistent discharge from 1 nose with no other symptoms
Management – paracetamol or ibuprofen for headache, muscle pain or fever – only continue use if distressed, change to other agent if not alleviated, don’t give both together
Paracetamol contraindicated in – liver/kidney problems, epileptic
Ibuprofen contraindicated in – pregnancy, perforated stomach, increased bleeding, severe HF, kidney or liver problems, high BP, asthma, hay fever
Intranasal decongestants – improve breathing and promote sleep and has fewer S/E than oral decongestants. Ephedrine HCL 0.5% nasal drops for 12 and older p 1-2 drops 4x daily for 1 week – contraindicated – diabetes, hypertension, hyper thyroidism, CVD, high BP, MAOI in last 2 weeks
Oral decongestants – relieve nasal congestion (phenylephrine) – max 1 week
Antitussive (cough) – dextromethorphan
Expectorants (guaifenesin)
Chlorphenamine or Beecham’s (contains phenylephrine and paracetamol) (Sedating antihistamine – dries up secretions)
Counselling points
Go to GP if
fever for more than 3 days
symptoms worsening after 5 days
symptoms not better after 10 days
follow up meeting
risk and complicated patients within the week
young children – 1 week
Headaches
Types of headaches
Primary – not associated with other conditions – migraines, tension types, cluster
Secondary – associated with other conditions – trauma/injury, vascular disorders, hyper-tension, withdrawal such as opioids, analgesics, or alcohol. Bacterial or viral infection.
Features of serious headache – referral
New severe or unexpected headache – sudden onset reaching max intensity 5 mins and new onset in over 50s
Progressive or persistent headaches that changed dramatically
Associated features – fever, impaired consciousness, seizure, stiffness, photophobia, neurological deficit, cognitive dysfunction, atypical aura (greater than 1 hour) or aura 1st time in patients using combined oral contraceptives.
Dizziness, visual disturbance, vomiting. Head trauma up to 3 months prior, triggered by coughing, sneeze, or physical exertion. Worsened by standing or lying down.
Compromised immunity
Diagnosis
Migraine without aura – at least 5 attacks lasting 4-72 hrs with unilateral location (half the face), pulsating, moderate to severe pain and aggravated by or causing avoidance of routine physical activity. Attack comes with nausea and/or vomiting, photophobia and phonophobia
Migraine with aura – 2 attacks with visual aura (zigzag lines or blind spots), pins and needles, speech/language symptoms, motor weakness, vertigo.
One aura spreading gradually for 5 mins and 2 or more occurring after
Each aura lasts for 5-60mins which is unilateral
Management – stop combined oral anticontraception – contraindicated
Ibuprofen 400mg, paracetamol 1g, advise med to be taken at start of attack – follow up 2 weeks
Tension type – recurrent episodes lasting 30 mins – 7 days with NO nausea or vomiting. May have phot/phono phobia
Bilateral (across head landscape), pressing or tight (not pulsating), mild to moderate pain, not aggravated by physical activity
Management – simple analgesia – paracetamol or NSAID
Identify comorbidities such as stress, mood disorders, chronic pain, sleep disorders to manage
Cluster headache – 5 attacks of severe/very severe unilateral orbital (around ONE eye), forehead or temporal pain lasting 15 mins to 3 hrs with nasal congestion, runny nose, eyelid oedema, sweating, facial slushing, fullness in ear or restlessness
Attacks occur between one every other day and 8 per day for more than half the time the disorder is active
Management – REFER
Advise to avoid triggers and risk of medication overuse, identify and manage comorbidities – insomnia, depression, and anxiety
Medication – occurs 15 days per month and have a pre-existing headache disorder. Regular overuse of drugs for 3 months
Management – withdrawal from medication and advice around this
Sinusitis
Sinusitis usually follows a cold and lasts less than 12 weeks
If over 12 weeks becomes chronic – risk groups are allergic rhinitis, asthma, immunosuppression
Symptoms
Adults
Nasal blockage (obstruction/congestion), nasal discharge, facial pain/pressure, frontal headache, loss, or reduction of smell, altered speech indicating nose blocked. Tenderness, swelling. Redness over cheekbone, cough, headache worse when bending or lying down. Toothache.
Children
Nose block, discoloured nasal discharge, facial pain, pressure and or cough at day or night-time
Bacterial sinusitis
More than 10 days, discoloured, pussy discharge (from 1 nose), severe local pain (1 side), fever over 38 degrees, deterioration after milder sickness
Refer to hospital immediately
If they have symptoms of acute sinusitis and;
Severe systemic infection
Intraorbital or periorbital complications, including periorbital oedema or cellulitis, displaced eyeball, double vision, or new reduced vision
Intracranial complications, including swelling over frontal bone, symptoms or signs of meningitis, severe frontal headache, or focal neurological signs
Refer to GP
Severe symptoms, painkillers don’t work, symptoms worsen, symptoms don’t improve after 1-week, recurrent infection, sudden worsening, antibiotic failure, unusual or resistant bacteria, recurrent episodes, immunocompromised, allergic cause
Treatment
Acute with symptoms less than 10 days
DON’T OFFER ANTIBIOTIC, assure that it usually self resolves without bacterial complications. Symptoms managed
Paracetamol or ibuprofen for pain, headache, and fever
Use nasal saline spray or decongestants spray
Clean nose with saltwater solution (boil 1 pint of water and add 1 teaspoon of salt and bicarbonate soda. Wash hands, stand over sink, cup the palm of 1 hand and pour small amount of solution into it. Sniff water into 1 nostril at a time, breath through mouth and allow water to pour into sink, don’t let it go into your throat. Do 3x daily)
Acute for 10 days or more with no improvement
High dose nasal corticosteroid for 2 weeks for over 12s (mometasone 200mcg 2x daily)
Counsel that It may improve symptoms but won’t make the infection any shorter, could have systemic effects, may be difficult to use correctly.
Symptoms should get better 3-5 days of treatment – REFER if not
1st line antibiotic for adult
If not life threatening - phenoxymethylpenicillin 500 mg four times a day for 5 days.
Is systemically unwell, symptoms of more serious illness or high risk of complications - co-amoxiclav 500/125 mg three times a day for 5 days.
Allergic or intolerant to penicillin - clarithromycin 500 mg twice a day for 5 days.
Pregnant or intolerant to penicillin - erythromycin 250 mg to 500 mg four times a day or
Children 1st line
Phenoxymethylpenicillin
1 to 11 months, 62.5 mg four times a day for 5 days.
1 to 5 years, 125 mg four times a day for 5 days.
6 to 11 years, 250 mg four times a day for 5 days.
12 to 17 years, 500 mg four times a day for 5 days.
If very unwell - co-amoxiclav
1 to 11 months, 0.25 mL/kg of 125/31 suspension three times a day for 5 days.
1 to 5 years, 5 mL of 125/31 suspension three times a day or 0.25 mL/ kg of 125/31 suspension three times a day for 5 days
6 to 11 years, 5 mL of 250/62 suspension three times a day or 0.15 mL/kg of 250/62 suspension three times a day for 5 days.
12 to 17 years, 250/125 mg three times a day or 500/125 mg three times a day for 5 days.
If allergic or intolerant to penicillin – clarithromycin
Under 8 kg, 7.5 mg/kg twice a day for 5 days.
8 to 11 kg, 62.5 mg twice a day for 5 days.
12 to 19 kg, 125 mg twice a day for 5 days.
20 to 29 kg, 187.5 mg twice a day for 5 days.
30 to 40 kg, 250 mg twice a day for 5 days.
12 to 17 years, 250 mg twice a day or 500 mg twice a day for 5 days.
2nd line – if symptoms are still worsening after 1st line treatment for 2-3 days
Adults – co-amoxiclav 500/125mg TD x 5 days
Children – specialist advice
ANTIHISTAMINES can be prescribed for allergic triggered sinusitis
Diabetes type 1
Body stops making insulin and the blood sugar (glucose) level goes extremely high - persistent hyperglycaemia (random plasma glucose of 11mmol/l or more). We must control glucose level with insulin injections, healthy diet and reduce the risk of other health complications. Typically occurs in children and young adults.
Symptoms of T1D- Frequently thirsty, pass a lot of urine, tiredness, weight loss and feeling generally unwell. Develops quite quickly, over days or weeks, as the pancreas stops making insulin.
Pathophysiology of T1D- Autoimmune disease (environmental & genetic factors). Antibodies attach to the beta cells in the pancreas destroying the cells that make insulin (pancreatic islet cells).
Diagnosing T1D- Simple dipstick test to detect glucose in a sample of urine BUT only way to confirm the diagnosis is to have a blood test to look at the level of glucose in your blood (level of 11.1 mmol/L or more in the blood sample indicates that you have diabetes) PLUS a fasting blood glucose level is taken (level of 7.0 mmol/L or more indicates that you have diabetes).
Management- Should be offered multiple daily injection basal-bolus insulin regimens as the first-line choice. Twice-daily insulin detemir should be offered as the long-acting basal insulin therapy. Once-daily insulin glargine may be prescribed if insulin detemir is not tolerated, or if a twice-daily regimen is not acceptable to the patient. Insulin detemir may also be offered as an alternative once-daily regimen. There are multiple types of insulin…
Rapid Acting- Insulin Aspart (Novorapid®), Lispro (Humalog®) and Glulisine (Apidra®)
Short Acting- Soluble insulin (Actrapid®)
Intermediate Acting- Isophane (Insulatard® or Humulin I®) & NPH - neutral protamine Hagedorn
Long Acting- Insulin glargine (Lantus®), detemir (Levemir®)
Combination insulins (biphasic)- e.g., Novomix 30®, Humalog Mix 25®, Humalog Mix 50®, Humulin M3® and Insuman Comb 50®
Diet & Lifestyle- Diet low in fat, salt, and sugar and high in fibre and with plenty of fruit and vegetables. If you are overweight try to lose weight, increase your physical activity even if it’s only going for a walk (community groups)
Other Health Complications- Get regular checks with your GP, podiatrist, and optometrist. Also get the flu jab every year.
Complications – microvascular, macrovascular (MI, stroke), metabolic (diabetic ketoacidosis) and hypoglycaemia (blood glucose less than 3.5mmol/l)
Psychological complications – anxiety, depression, and eating disorders and those at increased risk of developing autoimmune diseases
Suspect DKA in diabetics – greater than 11mmol/L
Increased thirst and urine frequency, inability to tolerate fluids, persistent vomiting, diarrhoea, visual disturbance, lethargy, fruity smell on breath, deep sighing when breathing and dehydrated
Management
HbA1c levels target of 48mmol/mol or lower - Measure 3-6 months but more often if not controlled
Self-monitoring – need glucose monitor, lancet, finger pricking device and testing strips
Taught at diagnosis and review technique 1 yearly.
Before breakfast, 2 hours after meals, during illness, before driving, if they feel hypo – at least 4 times a day including before and after meals and before bed.
More frequency required (up to 10x daily) if
Target HbA1c not achieved, frequency of hypo increases, during illness, before, during and after sports, planning, during and while breastfeeding.
Target glucose readings
Fasting plasma glucose level of 5–7 mmol/L on waking.
Plasma glucose level of 4–7 mmol/L before meals at other times of the day.
For adults who choose to test after meals, plasma glucose level of 5–9 mmol/L at least 90 minutes after eating.
Agree bedtime target plasma glucose levels with the person. This should:
Consider the timing of the last meal and its related insulin dose.
Be consistent with the recommended fasting level on waking.
Provide information of effects of food and drinks – carbohydrate training (match carb quantities to insulin doses)
Educate to be careful of body weight and diets, feasting and fasting, fibre and protein intake, diabetic foods and sweeteners, alcohol intake, matching carbs with insulin and physical activity
Advice on alcohol – avoid drinking on empty stomach, eat carb snack before and after drinking (extra insulin not required). Measure glucose more regularly and maintain it with carb intake. Alcohol can exacerbate or prolong hypoglycaemic effect.
Exercise – lower glucose levels and reduces CVD risk and can help weight
Sick day rules – never stop or skip insulin – dose may need altering seek advice. Check blood more frequently – 1-2 hours including in the night. Check blood or urine ketone levels – 3-4 hours including night and if 2+ or 3mmol/l or higher then contact GP immediately.
Maintain normal meal pattern where possible if not then replace meals with carb rich drinks, milk, fruit juices and sugary drinks. Aim to drink at least 3L of fluid to prevent dehydration.
Offer multiple daily injection basal-bolus insulin regimens as the first-line choice to all adults with type 1 diabetes.
Offer twice-daily insulin detemir as the long-acting basal insulin therapy
Offer a rapid-acting insulin analogue injected before meals for mealtime insulin replacement
If a multiple daily injection basal–bolus insulin regimen is not possible and a twice-daily mixed insulin regimen is preferred
Insulin pump therapy is recommended as a treatment option for adults with type 1 diabetes mellitus if condition isn’t controlled by treatment
Diabetes type 2
The body still makes insulin however, you do not make enough insulin for your body's needs OR the cells in your body do not use insulin properly (insulin resistance means you need more insulin than normal make to keep glucose levels down. Occurs mainly in people aged > 40 but inc diagnosed in younger people, commonly associated with obesity, physical inactivity, raised blood pressure, dyslipidaemia, and a tendency to develop thrombosis (CV risk).
Symptoms of T2D- Gradual (weeks-months) and can be quite vague at first. Frequent thirst, passing large amounts of urine, tiredness, which may be worse after meals. Some people also develop blurred vision and frequent infections, such as recurring thrush.
Management- Metformin HCl 1st choice for treatment of all patients (à weight loss, red risk of hypoglycaemic events and long-term CV benefits). Has an anti-hyperglycaemic effect, lowering both basal and postprandial blood-glucose conc. It does not stimulate insulin secretion and therefore, when given alone, does not cause hypoglycaemia. If metformin contra-indicated/not tolerated trial MR formulation or initial treatment should be a sulfonylurea e.g. gliclazide OR a dipeptidyl peptidase-4 inhibitor e.g. linagliptin OR Pioglitazone.
Insulin- can be added if intensification of treatment needed. If needed, bedtime basal insulin should be initiated, and the dose titrated against morning (fasting) glucose.
Diet & Lifestyle- Avoid foods heavy in saturated/trans fats, beef and processed meats, sugary drinks, high-fat dairy products and salty/fried foods & have fibrous fruits and vegetables, high omega-3 fatty acid food and poly/monosaturated fats. Lose weight and inc physical activity (min 5 x 30 min brisk walk / week) and smoking cessation. Also see optician regularly in case of damage to retina, GP and podiatrist.
EXTRA INFO FOR BOTH
Holiday- Pack about x3 the amount of insulin needed, test strips, lancets, needles or glucose tablets you would use, in case you need it (take cool bag to avoid insulin getting too hot). Carry your medicine in your hand luggage just in case checked-in bags go missing or get damaged (insulin can freeze and render it unusable). If injecting (i.e. will have needles/sharps) get a letter from your GP that says you need it to treat diabetes. If you use a pump or CGM, check with your airline before you travel about taking it on board as may require paperwork for medical equipment. If you use a pump, pack insulin pens in case it stops working. Take plenty of snacks in case there are any delays. Do not put your pump through the hand luggage scanner – let airport security know so they can check it another way.
<18 & Diabetic- Paediatric diabetes care team until 18 will help w injecting insulin, testing blood glucose levels, and diet. They can give advice on school or nursery and talk to your child's teachers and carers. Initially, every 1 - 2 weeks but will eventually be every 3 months.
Check Ups Needed- Annually get feet checked by podiatrist to check for loss of feeling in your feet, and for ulcers and infections. Get your eyes checked to check for any damage to blood vessels in the eyes, and checks for high blood pressure, heart, and kidney disease by your GP, also ensure to book in annually for a flu jab. Every 3 months have a blood sugar test (HbA1C test) checks your average blood sugar levels and how close they are to normal when newly diagnosed, then every 6 months once you're stable (~48-53 mmol/mol recommended).
Education- free education courses to help you learn more about and manage your diabetes, your GP will need to refer you. Diabetes UK run local charities for extra support, their website plus the NHS website offers a lot of diabetes information and advice. Maybe invest in a medical ID to carry w you.
Extra Lifestyle Advice- Eat a meal w carbs (e.g. pasta) before you drink alcohol and make sure people around you can recognise a hypo, choose diet soft drink mixers where possible, check your blood glucose regularly/before bed/the next day, drink plenty of water the next day. Avoid hypos by eating the right amount of carbs before, during and after exercise, adjust your insulin and check your blood glucose regularly, drink plenty of water. Recommended to have HbA1c <48mmol/mol when pregnant as high blood glucose levels can harm your baby, especially in the first 8 weeks of pregnancy, also a risk of having a large baby, which can cause complications during labour. Speak to your diabetes team If you're planning to get pregnant or if you get pregnant unexpectedly.
Item for disposal
Method of disposal
Needles
Sharps bin
Lancets
Sharps bin
Used blood test strips
Sharps bin
Leftover/expired insulin
Sharps bin/return to pharmacy
DVLA- tell the DVLA you’re diabetic or you could get fined due to hypoglycaemia/low sugar levels crisis. Check your blood glucose no longer than 2 hours before driving, check your blood glucose every 2 hours if you're on a long journey, travel with sugary snacks and snacks with long-lasting carbs, like a cereal bar or banana. If you feel your levels are low: stop the car when it's safe, remove the keys from the ignition, get out of the driver's seat, check your blood glucose, and treat your hypo, don't drive for 45 minutes from when you feel normal again.
Sharps Removal- Patients issued a sharps bin from the diabetes clinic/hospital on first diagnosis. Some pharmacies offer this sharps disposal service, or the diabetes clinic do too. Can arrange w GP/LHB for sharps collection (Cardiff Council does NOT offer kerbside sharps disposal)
Other Technologies- Insulin Pump (attached to skin via tiny tube which is replaced every 2-3 days & pump moved to diff part of body) will deliver a set background amount of insulin into blood day and night, can add your extra mealtime insulin using the pump. Continuous glucose monitoring (CGMs) means you can check your sugar levels at any time (see patterns in your levels, sends an alert if glucose too high/low) but as interstitial fluid sugar readings are a few mins behind your blood sugar levels you'll still need to do finger-prick checks every now and then. It’s a sensor you attach to your abdomen which needs replacing every 7 days, but some models can be worn for months. Free Style Libre is a flash glucose monitoring system measures your glucose levels continuously throughout the day via interstitial fluid (few mins behind). Attach sensor to your arm and a reader will scan to see your sugar levels (can also use a smartphone app to scan the sensor), sensors usually last for 14 days.
Testing blood glucose
Glucose monitor, specific in-date test strips, primed lancing device and cotton wool pad.
PRIMING LANCET
Twist cap off lancing device
Place fresh lancet into device so grooves line up and twist off the cover, so the needle is visible – change lancet every time so you don't get skin infections
Replace device cap - it should click and then adjust the depth metre – how far the needle will puncture – this is personal preference
Pull sliding barrel at bottom of device back to prime the lancet
CALIBRATING MONITOR
Turn on monitor – put new in-date test strip inside it and test it with in-date control solution – to make sure readings are correct
Do this every time you open a new pack of test strips, if you damage your monitor and if you think the readings are wrong.
TESTING process
Wash hands with warm water and soap and dry. Then rub hands for 10 seconds – warms hands to improve blood flow to fingers
Turn on monitor and place strip inside and wait for it say it’s ready for blood
Place device firmly on side of the finger (less nerves so less painful) and press release button then remove device from site. - change fingers regularly to stop hardening of skin.
Wipe first drop of blood away with cotton pad, use second one to test make sure by touching the blood onto the test strip
If successful wipe blood with cotton pad and apply plaster
Note readings
Remove cap of device exposing lancet. Place lancet cover on table and press lancet hard into this blue plastic cover – this will cover the needle and make it easy to remove
Place lancet and cotton pad in bin
Injecting insulin
Inject in stomach, thighs, or buttocks. Inject an inch away from previous site. Prevents lumps – this reduces absorption of insulin.
check that its correct insulin and is in date. Always check manufacturer’s instructions.
Wash hands with soap and warm water
Attach needle to pen – peel back cover, screw cap onto pen, remove white outer cover and the green cover to expose needle – change needle every time
Dial to 2 units and push plunger so you can see insulin coming out – to make sure no air stuck in there – can take multiple goes in new pens
Set correct dose
Press directly into skin and inject slowly – count to 10
Remove needle straight without bending it
Use the white outer cap to remove the needle and dispose in yellow sharps bin
Asthma
Symptoms – episodic, worse at night/early morning, triggered by exercise, infection and exposure to cold air or allergens. Triggered by emotion and laughter in children. In adults by NSAIDS and BB use.
Common with atopic eczema, dermatitis and allergic rhinitis and family history
ACUTE EXACERBATION OF ASTHMA IN ADULTS
First-line treatment for acute asthma is a high-dose inhaled short-acting beta2 agonist (such as salbutamol) given as soon as possible. For patients with mild to moderate acute asthma, a pressurised metered-dose inhaler and spacer can be used. For patients with acute severe or life-threatening symptoms, administration via an oxygen-driven nebuliser is recommended, if available. If the response to an initial dose of nebulised short-acting beta2 agonist is poor, consider continuous nebulisation with an appropriate nebuliser. Intravenous beta2 agonists are reserved for those patients in whom inhaled therapy cannot be used reliably.
In all cases of acute asthma, patients should be prescribed an adequate dose of oral prednisolone. Continue usual inhaled corticosteroid use during oral corticosteroid treatment. Parenteral hydrocortisone or intramuscular methylprednisolone are alternatives in patients who are unable to take oral prednisolone.
IN CHILDREN OVER 2
First-line treatment for acute asthma is an inhaled short-acting beta2 agonist (such as salbutamol) given as soon as possible. For children with mild to moderate acute asthma, a pressurised metered-dose inhaler and spacer device is the preferred option. The dose given should be individualised according to severity and adjusted based on response. For children with acute severe or life-threatening symptoms, administration via an oxygen-driven nebuliser is recommended, if available. Parents/carers of children with acute asthma at home, should seek urgent medical attention if initial symptoms are not controlled with up to 10 puffs of salbutamol via a spacer; if symptoms are severe, additional bronchodilator doses should be given as needed whilst awaiting medical attention. Urgent medical attention should also be sought if a child's symptoms return within 3-4 hours; if symptoms return within this time, a further or larger dose (maximum of 10 puffs of salbutamol via a spacer) should be given whilst awaiting medical attention.
COPD
Symptoms - persistent respiratory symptoms and airflow obstruction, which is usually progressive and not fully reversible, exertional breathlessness, chronic/recurrent cough, or regular sputum production, wheeze
Treatment – education on condition and risk factors, smoking cessation, pneumococcal and flu vaccination yearly, treatment of associated comorbidities
1st line – SABA or SAMA to relieve breathlessness and improve exercise tolerance – reviewing medication, adherence, and inhaler technique regularly
THEN IF they have NO asthmatic features or no features of steroid responsiveness – offer LABA AND LAMA
If they continue to have day-to-day symptoms, consider 3-month trial of LABA+LAMA+ICS
If NO improvement go back to LAMA+LABA only but if it works continue and review annually
If they have asthmatic or steroid responsiveness features offer LABA+ICS if they have day to day symptoms of 1 severe or 2 moderate exacerbations a year, then offer LABA+LAMA+ICS
WITH ICS DISCUSS RISK OF USING ICS including pneumonia
Acute exacerbation of COPD – triggered by infections, smoking and environmental pollutants
Severe breathlessness, increased cough, increased sputum production and change in colour, increased wheeze, and chest tightness, cold or sore throat, reduced exercise tolerance, ankle swelling, increased fatigue, and acute confusion
FOR SEVERE exacerbation – ADMISSION
FOR non-severe – increase dose or freq of SABA and maybe change to nebuliser for ease of admission
If no contraindications with significant increase in breathlessness – offer 30mg oral prednisolone OD x 5 days or if caused by infection then amoxicillin 500mg TD x 5 days, doxycycline 200mg day 1, 100mg OD x 5 days, or clarithromycin 500mg BD X 5 days
Epilepsy
Cause – abnormal excessive or synchronous brain activity
Symptoms
Short-lived (less than 1 minute), abrupt, generalised muscle stiffening with rapid recovery — suggestive of tonic seizure.
Generalised stiffening and subsequent rhythmic jerking of the limbs, urinary incontinence, tongue biting —suggestive of a generalised tonic-clonic seizure.
Behavioural arrest — indicative of absence seizure.
Sudden onset of loss of muscle tone — suggestive of atonic seizure.
Brief, 'shock-like' involuntary single or multiple jerks —suggestive of myoclonic seizure.
Management
During seizure – protect from injury by placing in recovery position. If tonic-clonic seizure is prolonged (more than 5 mins) or recurrent – emergency buccal midazolam or emergency admission
Annually reviewed – assess seizure control, how it’s affecting QOL, adverse effects and compliance with drug
Women of childbearing age – 13 to 60
Epileptic women not treated with drugs or on non-enzyme inducing antiepileptic (except lamotrigine) – contraceptive options are same as general population
Woman on exyzme-inducing drugs – drug can reduce effectiveness of combined hormonal contraception, progestogen-only pills, transdermal patches, the vaginal ring, and progestogen-only implants. OFFER medroxyprogesterone acetate injections or an intrauterine method (copper intrauterine device or the levonorgestrel-releasing intrauterine system)
Woman on lamotrigine – oestrogen containing contraceptive reduces efficacy of lamotrigine
USE progesterone only instead but educate them to report signs of lamotrigine toxicity
Category 1 (ensure the person is maintained on a specific manufacturer's product) — phenytoin, carbamazepine, phenobarbital, primidone.
S/E – common and usually mild, advise to report and can usually be fixed with dose adjustment or change of drug
Sedation and dizziness, suicidal thoughts and behaviour, acute psychotic reactions, weight gain and loss, skin rashes.
Safe in pregnancies – lamotrigine (Lamictal) and levetiracetam (Keppra) are safest options
Anxiety
Uncontrollable widespread worry and range of cognitive and behavioural symptoms
Slow onset and symptoms don’t usually improve but are better controlled with intervention
Diagnosis – worry associated with restlessness, insomnia and muscle tension, fatigue, poor concentration, irritable. ALWAYS ask about alcohol and drug use including OTC
Treatment
Establish diagnosis and severity of anxiety and any other comorbidities (usually insomnia and depression and whichever is the most pressing is treated first) – explaining the disorder and treatment opportunities and starting them with active monitoring of symptoms either self or through regular meetings
Offer CBT – non-facilitated self-help for 6 weeks, individual guided self-help, educational groups
High intensity CBT, applied relaxation or drug therapy
Drug therapy – 1st line is SSRI (sertraline, paroxetine, or escitalopram) 2nd line SNRI (duloxetine or venlafaxine). If both contraindicated or intolerable then Pregabalin.
Review effectiveness and ADR every 2-4 weeks during first 3 months then every 3 months.
Counsel on common effects during treatment initiation (suicidal thoughts and worsening of anxiety) but importance of reporting this instead of withdrawing from drug
SSRI – don’t take NSAIDS or if prescribed take with PPI
For pregnant women step 3
DO NOT give benzo or antipsychotics in primary care
Benzodiazepines (SCH 3 and 4)
Most commonly used anxiolytics and hypnotics
Short rem relief (2-4 weeks only) of anxiety that is severe, disabling, or causing the patient unacceptable distress
use to treat short-term ‘mild’ anxiety is inappropriate
Sch 4 CDs, apart from temazepam
Sch 3 (CD no register) and midazolam
Pharmacological effects of benzodiazepines
Sedation, sleep induction
sleep, but can still cause arousal
decreased anxiety, amnesia at higher doses
muscle relaxation (both midbrain and spinal effects)
anticonvulsant activity
Reduced aggression
Depression
Persistent low mood and/or loss of pleasure in most activities and range of emotional, cognitive, physical, and behavioural symptoms
Diagnosis
Low mood
Loss of interest/pleasure from normally pleasurable activities (anhedonia)
Reduced energy (fatigue)
Low self-esteem; feelings of guilt
Inability to think/concentrate
Altered psychomotor activity
Sleep disturbance; early morning wakening
Altered appetite
Suicidal thoughts
Diagnosis requires 2 core symptoms plus 2 or more others present for most of the day on most days for the last 2 weeks
Differential diagnosis
Ensure symptoms are not caused by physical illness, alcohol, medication, or illicit drug use
The symptoms aren’t caused by normal grief (death of family) – maybe consider very long grief
Never been a manic (severe levels of high mood) or hypomanic (to a reduced level) episode
Treatment
Dependant on accurate assessment and diagnosis of depression
Psychological
CBT, behavioural activation, interpersonal psychotherapy, problem solving therapy
Social
Identify stressors and work on strategies/signposting to other supporting organisations
Biological – moderate to severe
Antidepressant therapy or antidepressant and antipsychotic combination therapy in psychotic depression
Drug classes
Tricyclic antidepressants (TCAs) e.g., amitriptyline
Selective serotonin reuptake inhibitors (SSRIs) e.g., fluoxetine
Serotonin and NA uptake inhibitors (SNRIs) e.g., venlafaxine
Monoamine oxidase inhibitors (MAOIs)
Irreversible e.g., phenelzine (MAO-A and B)
Reversible e.g., Moclobemide
Atypical antidepressants e.g., Mirtazapine
Noradrenaline reuptake inhibitors (NRIs) e.g., Atomoxetine
TCA - S/E – Short lasting (days) sedation, confusion, and Incoordination in both normal and depressed patients, antimuscarinic effects, dry mouth, blurred vision, decreased mucus production. Dangerous CV effects in OD
Severe depressive at risk of suicide shouldn’t be given TCA
Interactions – potentiation of the effects of alcohol – alcohol is a depressant and will only compound the depressive effects
SSRI’s - S/E – nausea, anorexia, insomnia, and loss of sexual function
Less anticholinergic side-effects and less dangerous in OD than TCAs. Prolonged QTc – cardiovascular complications risk with citalopram interactions – NSAIDs, Anticoagulants, triptans
SNRI’s - S/E – significant withdrawal effects – have short half-lives so need to be taken regularly to avoid these effects. Complex nature of TCAs makes them difficult to prescribe to complex patients unlike SNRIs
Interactions – NSAIDs and anticoagulants
MAOIs - S/E – antimuscarinic effects, restlessness as a result of CNS excitation
Interactions – serious food and drug reactions e.g., cheese (tyramine from food such as cheese is broken down by MAO. The lack of breakdown from MAOIs can lead to tyramine actively displacing neurotransmitters such as 5HT, DA, NA – causing hypertensive crisis
VERY IMPORTANT COUNSELLING POINTS
No other drugs or illicit drugs with this
Side effects
Drug and food interactions are unacceptable.
“Cheese reaction”: this occurs when amines that are generated during fermentation, like tyramine, are ingested and absorbed from the gut. (The main danger is ripe cheese, yeast products - Marmite).
Large rise in systemic tyramine indirectly results in a large release
of catecholamines
Hypertensive crisis characterised by throbbing
headache, tachycardia & cardiac arrhythmias.
Same can occur with drugs (Pseudoephedrine)
Atypical antidepressants - S/E- sedation, weight gain, increased appetite – good in patients with anorexia or depression causing loss of appetite or weight
Blood disorders – counselling
Withdrawal issues
Can be used with other antidepressants that cause sleep issues
Interactions – alcohol
FDA black box warning – suicide
Treatment
Mild symptoms – psychological therapy
Persistent mild symptoms or moderate to severe symptoms – combination of psychological and drug therapy
1st line treatment usually SSRIs
2nd line switch to alternate SSRI
3rd line switch to different class (normally an SNRI)
Practical issues
Initiating an antidepressant can cause feelings of anxiety consider co-prescribing short course of benzodiazepines to counteract the anxiety
During the first few weeks of antidepressant treatment can have worsening suicidal thoughts with improved motivation so ensure counselling and regular reviews
Consider prescribing limited supply of meds to reduce chance of OD
Side effects often transient and improve with time
Caution when switching antidepressants – table of different half-lives and how to taper them
Treatment approach
If no response to 3 antidepressants, then check concordance, review diagnosis, and consider if social problems are maintaining depression
Consider augmentation – addition of drug to the current therapy
Mirtazapine – sleep
Quetiapine – mood
Aripiprazole
Lithium – mood stabiliser
Lamotrigine – mood stabiliser
Electroconvulsive therapy
Response
2-4 weeks usually for response to be seen (longer in elderly)
Improvement greatest during weeks 1-2
If no response during 2–4-week period, consider first increase in dosage then if again limited efficacy, then switch to alternative
Extended duration if treatment trial will lead to additional benefit in some
Differences between drugs
Mirtazapine, escitalopram, venlafaxine, and sertraline
more efficacious than
duloxetine, fluoxetine, fluvoxamine, paroxetine and reboxetine
Reboxetine less effective overall
Escitalopram and sertraline
better tolerated than
duloxetine, venlafaxine, fluvoxamine, paroxetine and reboxetine
Preventing relapse
Relapse rate 3-6 months post remission is 50% with no drug treatment
A/D treatment reduces absolute risk of relapse by about 50%
After 1st episode continue for 6-9 months
After 2nd episode continue for 12 months
After 3rd episode continue for 2 years
Insomnia – difficulty in getting to sleep or staying asleep long enough to feel refreshed the next morning
Causes
Recreational drugs
caffeine, nicotine, alcohol, cannabis)
Medicinal drugs
anticonvulsants, antipsychotics, b-blockers, SSRIs, MAOIs, steroids, decongestants, Alpha agonists and antagonists, narcotic analgesics
Drug withdrawal
from CNS depressants (eg alcohol, anxiolytics/hypnotics)
Physiological
Diet, late night exercise, shift work (night and evening work)
Environmental
Noise, bright lights, extremes of temperature
Medical conditions
Psychological - anxiety, depression, grief, stress
Non-psychological eg chronic pain, gastric reflux, asthma, sleep apnoea
Types of insomnia
Primary insomnia - insomnia not attributable to a medical psychiatric or environmental cause
Secondary insomnia- insomnia secondary to another condition
Transient (2-3 days) – caused by changes in routine (for eg. change in time zone, alteration of shift work)
Short term (<3 weeks) – may result from temporary environmental stress
Chronic insomnia (>3 weeks) –usually secondary to other conditions
Treatment
FIRST LINE IS ALWAYS NON-DRUG treatments e.g., lifestyle changes and CBT
Drug therapy – Hypnotics
Benzodiazepines
Benzodiazepine-like drugs (Z-class)
melatonin
BEFORE hypnotic is prescribed the cause of insomnia must be established and where possible, underlying factors should be treated
NICE recommends
if hypnotic medicine is the appropriate way to treat one for only short periods of time and strictly according to the licence for the drug. (Usually, 1-2 weeks and max 4 weeks) and should be prescribed on a weekly basis
Benzodiazepines
Most benzodiazepines
decrease time taken to get to sleep
in individuals who habitually sleep <6hr, the drug increases duration of sleep
Few short-acting BDZs recommended for insomnia (short-term treatment – max 2-4 weeks)
Should only be used when SEVERE, DISABLING or causing EXTREME DISTRESS
Benzodiazepine – like drugs
Z -Hypnotics – Zaleplon, zopiclone, zolpidem (Short acting – t1/2 < 8 hr)
Short term use only (2-4 weeks)
Lack of anxiolytic effects –drowsiness or dizziness - just induce sleep
Melatonin treatment
Prolonged release melatonin available for primary insomnia in over 55yr olds (can be used up to 3 weeks)
Antihistamine gen 1 – can cause drowsiness
Anxiolytics
Kalms, Kalms day, Karma, Karmamood, Potters Newrelax, Relaxherb, Stressless
Hops, valerian, passionflower, passiflora, vervain, St John’s Wort
Sedatives
Kalms night, Kalms sleep, Dormesean, Niteherb, Nytol herbal, Potters Nodoff, sominex herbal
Hops, valerian, vervain, skullcap, wild lettuce, passiflora
Some herbal remedies do contain active ingredients so be careful of interactions
Lifestyle changes – promote sleep hygiene
establishing fixed times for going to bed and waking up
trying to relax before going to bed
maintaining a comfortable sleeping environment avoiding napping during the day
avoiding caffeine, nicotine, and alcohol late at night
avoiding exercise within four hours of bedtime
avoiding eating a heavy meal late at night
avoiding watching or checking the clock throughout the night
using the bedroom mainly for sleep if possible
avoid going on phone, looking at screens immediately before bed or whilst in bed
ADHD
Persistent developmentally with inappropriate levels of over reactivity, inattention and/or impulsivity
Diagnosis – based on observation there are no biomed tests
Symptoms – 9 symptoms across 2 domains
Hyperactivity/impulsivity
Inattention
Can be combined type or dominant in one
ADHD – Predominantly inattentive type
Fails to give close attention to details or makes careless mistakes.
Has difficulty sustaining attention.
Does not appear to listen.
ADHD – predominantly Hyperactive/impulsive type
Fidgets with hands or feet or squirms in chair.
Acts as if driven by a motor.
Blurts out answers before questions have been completed.
Difficulty waiting or taking turns.
Interrupts or intrudes upon others.
ADHD – Combined type
Patient meets both sets of inattention and hyperactive/impulsive criteria
ADHD – Differential diagnosis
Sensory impairment – leading to under or over-sensitivity to triggers
Epilepsy and related states – could present as inattention
Effects of head injury
Acute or chronic medical illness
Poor nutrition – linked to poor behavior – not directly linked to ADHD
Sleep disorders – linked to poor behavior – not directly linked to ADHD
Side effects of medication
School or classroom difficulties – bullying or other factors
Large links to exposure to smoking and drinking during pregnancy, childhood illness such as meningitis or other viral infection, low birthweight/prematurity. HIGH heritability
Treatment
Mild-moderate –1st line - parent-training/education programmes with parent and child, group based or individual sessions. Teachers receive ADHD training and offer intervention in schools.
2nd line – CBT or social skills training
3rd line – DRUG THERAPY ONLY FOR SEVERE and should be offered along with psychological, behavioural, and educational interventions
Drug therapy
Methylphenidate – generally first choice
Atomoxetine - if other tics, Tourette's syndrome, anxiety disorder, stimulant misuse or risk of stimulant diversion are present
D-amphetamine – ONLY if other drugs ineffective at raised doses – CD2 high risk in addiction and dependence and misuse so used as last resort
Decide which drug treatment to use based on:
their different adverse effects
potential problems with compliance (for example, if a mid-day dose is needed at school)
potential for drug diversion (taken by others) and misuse
preferences of the child or young person and their parent or carer
When a decision has been made to treat children or young people with ADHD with drugs, healthcare professionals should consider: –
methylphenidate for ADHD without significant comorbidity
methylphenidate for ADHD with comorbid conduct disorder
methylphenidate or atomoxetine when tics, Tourette’s syndrome, anxiety disorder, stimulant misuse or risk of stimulant diversion are present
atomoxetine if methylphenidate has been tried and has been ineffective at the max dose, or the child intolerant to low or moderate doses of methylphenidate.
Atomoxetine
Closely observe children or young people taking atomoxetine for agitation, irritability, suicidal thinking, and self-harming behavior, particularly during the initial months of treatment, or after a dose change.
Liver damage in rare cases (usually presenting as abdominal pain, unexplained nausea, malaise, darkening of the urine or jaundice).
Treatment of adults
In adults, methylphenidate normally first line treatment
Consider atomoxetine or dexamphetamine if symptoms do not respond to methylphenidate or the person is intolerant to it ~6 weeks.
Selection of appropriate medication
Immediate-release preparations if more flexible dosing is required or during initial titration to using methylphenidate, consider determine correct dosing levels
If there is a choice of more than one drug, use the drug of lowest overall cost
modified-release preparations for convenience…
their pharmacokinetic profile,
improving adherence,
reducing stigma (because the drug does not need to be taken at school)
reducing problems of storing and administering controlled drugs in schools
abuse liability
AUTISM
Symptoms
Socialization
Impaired use of non-verbal behaviors to regulate interactions
Delayed peer interactions, few or no friendships, and little interaction
Absence of seeking to share enjoyment and interests
Delayed initiation of interactions
Little or no social reciprocity and absence of social judgment
Communication
Delay in verbal language without non-verbal compensation (gestures)
Impairment in expressive language and conversation, and disturbance in pragmatic language use
Treatments
NEED early diagnosis and defined biomarkers
Currently intervention is through family and educational support
Only some specific programs have an evidence base
Aim is to ‘improve the functional status…through skill acquisition in core areas’
Eg developing relationships
Achieving social and environmental milestones through play
Positive reinforcement of social communication
Pharmacological treatments for co-morbidities
Developmental
Hyperactivity/impulsivity (see ADHD)
Psychiatric
SSRIs, other antidepressants for depression
atypical antipsychotics for OCD
SSRI or a2 agonists for anxiety
Behavioural
Atypical antipsychotics (irritability, aggression)
Sensory
Neurological
anticonvulsants and fits, a2 agonists for tics
Gastrointestinal
Sleep disruption
melatonin and clonidine
Dementia
Symptoms –
Higher cognitive function affected
Memory, thinking, comprehension, learning capacity, language (speaking and understanding it)
Daily living activities/emotional behaviour (non-cognitive symptoms)
Behavioural and psychological symptoms of dementia (BPSD) – include agitation, apathy, depression, anxiety, delusions, hallucinations, irritability, and wandering
Treatment -
Acetylcholinesterase (AChE) inhibitors (donepezil, galantamine, and rivastigmine) — as monotherapies for managing mild to moderate Alzheimer's disease.
Memantine (a N-methyl-D-aspartic acid receptor antagonist):
As monotherapy for managing Alzheimer's disease for people with moderate Alzheimer's disease who are intolerant of, or have a contraindication to, AChE inhibitors, or for people with severe Alzheimer's disease.
In addition to an AChE for people with established moderate or severe Alzheimer's disease who are already taking an AChE
For people with non-Alzheimer's dementia the use of AChE inhibitors or memantine is unlicensed, but they may be prescribed by a specialist for people with:
Mild to moderate dementia with Lewy bodies:
Donepezil or rivastigmine are recommended first line.
Galantamine is an option if donepezil and rivastigmine are not tolerated.
Severe dementia with Lewy bodies:
Donepezil or rivastigmine are recommended.
Vascular dementia:
AChE inhibitors or memantine are options if the person has suspected comorbid Alzheimer's disease, Parkinson's disease dementia, or dementia with Lewy bodies.
Risperidone and haloperidol are the only antipsychotics licensed for treating non-cognitive symptoms of dementia, although other antipsychotics are often prescribed off-label for this purpose.
Acetylcholinesterase inhibitors
NMDA receptor antagonist
Cholinesterase inhibitors for mild to moderate AD (eventually stop working)
NMDA receptor antagonist for severe AD and moderate AD in some cases
Treatment must be started only by a specialist clinician
Rheumatoid arthritis
Inflammatory disease causing persistent symmetric joint synovitis
Presents as pain and joint stiffness with heat and swelling progressing at rest and after periods of inactivity with malaise, fatigue, fever, and weight loss
Risk factors – smoking, eating large amounts of red meat, drinks excessive coffee
Symptoms
Joints
Pain
Swelling
Stiffness
Systemic
Fatigue, depression, irritability
Anaemia
Flu-like symptoms, such as feeling generally ill, hot, and sweating
Pain worse in morning
Treatment
Drugs, mild exercise (enhance flexibility of joint and muscle strength), lifestyle changes (rich antioxidant diet, no smoking)
Main types of RA meds
NSAIDs (short term symptomatic relief) – reduce inflammation. OTC (ibuprofen, naproxen). POM (celecoxib, etoricoxib)
S/E – GI irritation, ulcers (use at lowest dose and take with food, use PPI to lessen effects)
Caution – asthmatics and renal impairment and patients with increased CV risk
Disease-modifying anti-rheumatic drugs (DMARDs) – 1ST LINE for active RA (methotrexate, sulfasalazine)
S/E – Nausea, diarrhoea, oral ulceration, alopecia, cough, SOB, bone marrow suppression – CAN BE REDUCED by co-prescribing FOLIC acid 1mg daily
Biological therapies (type of DMARD) – used when DMARDS don’t control RA
Glucocorticoids – short term treatment when starting new DMARD for rapid symprom control - also used in flares
Analgesics (painkillers)
Drug Treatment Schedule
Start two DMARD regime once diagnosed, using titration regimens
Use anti-inflammatories (NSAIDs), paracetamol with or without corticosteroids until effective
Review after 6 months: increase dose or switch as clinical condition determines.
Patient counselling in RA
Place of drugs in therapy
Onset of action
Side effects
Immunosuppression
Regular painkillers
Regular monitoring including blood tests
Dexterity aids, prescription services
Osteoarthritis
Predominantly non-inflammatory and caused by cartilage loss from synovial joints and bone remodelling due to excessive and repeated overloading on weight bearing joints or stress of a joint over tome and specific injuries
Risk factors – genetic, age, gender, obesity, damage, occupational, and stress
Symptoms
Pain – tends to be worse when using the joint and at end of the day (Worsens on use, resolves at rest)
Stiffness – feel stiff after rest, usually wears off as you get moving
Grating or grinding sensation (crepitus) – joints creak or crunch as you move
Swelling – may be caused by osteophytes (bone outgrowth) or caused by synovial thickening and extra fluid
Muscles around joint look thin/wasted
Unable to use joint normally – doesn’t move as freely or far as normal
Joints give way – muscles have weakened, and joint is less stable
Management
Provide information on sources of advice and support
Advice on self-care strategies such as;
Weight loss, local muscle strengthening exercises and aerobic fitness training
Appropriate footwear, local heat, or cold packs
Odder psychosocial support – career and occupational health assessments if needed
Advice on simple analgesia
Arranging regular reviews to assess response to treatment
MANAGEMENT GOAL – pain reduction and symptomatic relief
First line:
Paracetamol regularly – 4g daily
Topical NSAIDs
Additional treatment:
Oral NSAIDs– not first line
-Start with ibuprofen
-Monitor for side effects
-Possible place for topical therapy
Topical capsaicin – adjunct and helpful in knee and hand – works by stimulating then decreasing the pain sensation
Corticosteroid injection: â pain and inflammation of flare-up
Role of pharmacist
Counselling:
dosage regimen
side effects
warnings
Monitoring for side effects
Weight loss advice
Physiotherapy advice
Compliance aids & living aids
Gout
Type of inflammatory arthritis – causes severe pain and damage to joints
Caused by abnormal high levels of uric acid in blood which deposits urate crystals in joints and tissue
3 phases
Asymptomatic hyperuricaemia – can remain in this stage for life
Acute attack of gouty arthritis – can vary from months to years before another attack
Final period of chronic tophaceous gout – nodules effecting joints
Treatment
Acute
Ice
Rest affected joint
NSAIDs – short term, 7-14 days, high dose, for pain relief and anti-inflammatory
Colchicine (Dose: 500mcg 2-4 x daily until symptomatic relief or SE (stomach cramps, diarrhoea, vomiting)), steroids (used when NSAID and colchine is contraindicated or not useful)
Choice of drug dependant on comorbidities and renal function (NSAID cause fluid retention whereas colchicine doesn’t)
Colchicine use limited as it can have sudden toxicity at higher conc
Combination treatment can be used as well if monotherapy isn’t controlling the attack
Long term treatment to reduce urate
Lifestyle modifications (reduce dietary intake)
Drug therapy: Allopurinol (1st line – offer to all, 100mg od, increased in 100mg increments every 2-3 weeks) S/E – rashes
Febuxostat (2nd line only use when allopurinol intolerant or contraindicated – 60mg OD dose)
Monitor urate level – aim for < 360 μmol/L or 6 mg/dl (critical level)
Muscoskeletal
Sprain
Commonly ankle, wrist, thumb, knees – pain, swelling, tenderness, bruising, disabled use and no weight
Strain
Common in legs and lower back – pain, swelling, bruising, red, and reduced function
BOTH
Self-limiting gets better in 4-6 weeks and full recovery in 12 weeks
Non-pharma advice
PRICE (Protect, Rest (48-72hrs), Ice immediately after, Compression bandages and Elevate to reduce swelling
Reduce HARM (Heat, alcohol, running and massaging for 72hrs.
Avoid NSAIDs for 72hrs
Exercises for sprains
Gently move joint in all directions to increase and maintain flexibility (lack of movement can delay recovery BUT severe sprains with complete lack of movement rest for 10 days first)
Treatment – topical and oral analgesics
Refer – severe pain, possible break or fracture, no alleviation with OTC meds
Lower back pain
Symptoms – pain, tension, soreness, stiffness without underlying cause
6 weeks usual recovery can be up to 12 weeks
Advice
Back exercises, improve posture, yoga, avoid lying or sitting for too long, remain active.
Sleep in different positions, pillows between legs, under knees, hot baths, hot water bottles, ice packs.
Treatment
OTC – topical analgesics or co-codamol if still painful
Refer
No improvement in 3 days, continues for more than 6 weeks, pain travels higher, pain after injury, younger than 20, older than 50, pain affects sleep, unsteady on feet, unexplained weight loss
EMERGENCY
Pins and needles in back, genital, bum, both legs, lose urine or bowel control
Conjunctivitis
Symptoms
Bacterial
Viral
Allergic
Eyes affected
1 or 2
Both
Both
Discharge
Pussy
Watery
watery
Sensation
Gritty
Gritty
Itchy
Co-presenting symptoms
None
Cough/cold
Rhinitis
If pussy, red or gritty it is contagious – allergic ISNT contagious
Advice
Don’t wear contacts, hold cold flannel on eyes for few mins to cool them, use FBC water to gently wipe lashes and clean off crust and clean with cotton wool pad. Use a different one for each eye
Control spread by – reg wash hands with hot soapy water, cover mouth and nose when sneezing, don’t share towels or pillows and don’t rub eyes
Refer
Baby less than 28 days old with red eyes, allergic reaction, or spots on eyelids. For all – symptoms not resolved after 2 weeks
111 - Severe pain, sensitive to light, sudden changes to vision
Treatment
Viral – self-limiting, use hygiene and non-pharma advice
Allergic – Opticrom eye drops (Adults and child – 1-2 drops in each eye up to 4x daily)
Bacterial – over 2, chloramphenicol drops/ointment (Optrex Bacterial Conjunctivitis 1%w/w Eye Ointment) - apply a small amount of ointment in the affected eye 3-4 times daily for 5 days
Blepharitis
Symptoms
NOT contagious, rims of eyelids are inflamed, burning, soreness or stinging in the eyes, crusty lashes that stick together, itchy eyelids
Advice
Clean eyelids at least 1x daily, clean eyes even if symptoms clear, don’t wear contacts, or eye makeup
Cleaning eyes – soak a clean flannel/cotton wool in warm water and place on eye for 10 mins, gently massage eyelids for 30 secs, clean lids using cotton wool. Baby shampoo at 10:1 ratio good.
Refer
No improvement after 2 weeks of cleaning eyes
Treatment OTC
Brolene eye drops – 1-2 drops in each eye up to 4 x daily. If not better in 2 days refer
Dry eyes
Symptoms
Dry feeling, sensation of something in eye, burning, grittiness, itching, light sensitivity, over-blinking, redness, excess tears (randomly tearing)
Causes – over 50, contacts, digital screens, AC, windy/cold/dry/ dusty environment, smoking, alcohol, meds (antidepressants/BP) medical conditions (blepharitis)
Refer
Treatment failure after 2 weeks, change in eyelid shape
111 – severe pain and red, contact wearer with red eyes (could be an infection)
999 A&E – sudden change in sight, bursts of light sensitivity, severe headache/nausea, dark red eyes, injured/pierced eye, something stuck in eye
Advice
Clean eyes daily, take breaks when using screens, use screens below eye level, use humidifier, wear glasses instead of contacts
Treatment
Light lubricant – Optrex Double Action Drops for Dry and Tired Eyes - Apply 1-2 drops in each eye.
Hyaluronic Acid - Artelac Rebalance Drops, long lasting relief - Place 1 drop into the conjunctival sac 3-5 times daily or more frequently if required.
Hypromellose drops – 1-2 drops 3 x daily
Excessive ear wax
Symptoms – hearing loss, earache, noise/ringing, vertigo, dizziness, and nausea
Causes – narrow/damaged canals, hairy canal, skin condition affecting scalp around ear, inflammation of ear canal
Refer – not cleared in 5 days, badly blocked, severe, complete loss of hearing, likely infection
Advice – don’t use fingers or cotton buds to remove wax
Treatment
Olive oil drops – 2-3 drops in affected ear and massage around outside of ear BD x 7 days
Use dropper when lying down with head to one side to allow oil into ear, over 2 weeks then lumps should fall out, but symptoms should be better within 5 days
Otitis externa
Symptoms - pain, discharge, itch, irritation, external ear/canal appears red, swollen, eczema, deafness, skin swells, tender to touch
Refer – ear pain in children, inflamed pinna, unsuccessful treatment (after 4 days), hearing aids, excessive discharge (wax or pus), high fever, vomiting, fatigue, confusion, dizzy, stiff neck, rash, slurred speech, fits, light sensitivity
Advice – avoid under/over dressing feverish child, lower heating, offer regular fluids, avoid dummies when lying flat, give paracetamol/ibuprofen if child is unwell/distressed (not together)
Treatment
Acute localised (furunculosis) – infected hair follicles in outer-ear causing swelling and irritation
Treatment – hot flannel, oral analgesics, antibiotics if severe
Acute diffuse (over 3 months – more widespread inflammation of skin, bacterial/fungal infection or contact dermatitis due to irritant/allergens
Treatment – earwax plus or EarCalm
Otitis media
Symptoms – earache, discharge, hot, irritable, sleeplessness, ear pulling/rubbing, crying, temporary deafness
Refer – recurrent infections, no improvement in 3 days
Treatment
Self-limiting should be better in 3 days, single analgesics for pain
Hyperthyroidism
Too much thyroid hormones produced naturally
Symptoms
Tremor, warm sweaty palms, weigh loss despite increasing appetite, heat intolerance, diffused alopecia, hair thinning, tachycardia, diarrhoea
Advice
Healthy diet with foods rich in antioxidants, green leafy vegetables (broccoli, cabbage etc)
Vitamin D, omega 3 fatty acids and calcium rich foods. Smoking cessation
Treatment
Carbimazole (adjunct B blocker propylthiouracil for adrenergic symptoms) – block and replace regime
Combo of fixed high dose carbimazole and levothyroxine
Radioactive iodine destroys thyroid cells, surgery to remove some thyroid
Hypothyroidism
Thyroid gland doesn’t produce enough hormones caused by immune system attacking thyroid gland and damaging ait or by damage to thyroid that occurs during treatments for a hyperthyroidism or thyroid cancer
Symptoms
Fatigue, muscle pain, weakness, weight gain, sensitive to cold, dry skin, brittle hair, nails, depression, reduced libido
Advice
Eat antioxidant rich food, seeds and nuts, tyrosine (meat, dairy, legumes)
Avoid – soy, iodine rick food, leafy green vegs, caffeine, alcohol – quit smoking, alcohol.
Inform GP if pregnant (needs treatment and monitoring during)
Treatment
Levothyroxine 1st line – dose depends on blood test and progression – take tablet at same time every day (MORNING) If taking too much causes sweating, chest pain, headaches, diarrhoea, vomiting. Supressing thyroid supressing hormone with high doses causes atrial fibrillation, stroke, osteoporosis
Cold sores
Symptoms
Simplex - Pain, burning, itching, tingling before lesions and lasts 6-48 hrs
Crops of vesicles burst and crust over and heal, commonly on lower lip and ends of mouth
Gingivostomatitis – fever, malaise, sore throat, painful nodules in cervix or under jaw, excessive salivation. Painful vesicles on a red swollen base that rupture to form ulcers inside mouth, covered with yellow/grey membranes
Refer – immunocompromised, unable to swallow, risk of dehydration, severe infection, complication, pregnant, recurrent
Treatment
Paracetamol/ ibuprofen for symptoms
Topical acyclovir/penciclovir OTC – use from onset of symptoms before lesions until lesions heal
OTC topical anaesthetic or analgesics, mouthwashes, or lip barriers – topical analgesics aren’t licensed in children
DON’T prescribe oral antiviral for healthy people
Consider prescribing oral antiviral for healthy people with episode of primary oral herpes simplex, recurrent labialis if lesions are severe, frequent, or persistent and recurrent
And for those who are immunocompromised
Should take at onset and until lesions have healed – minimum of 5 days
Choice of aciclovir or valaciclovir based on preference, dose, regimen, and adherence
Advice
Reassure its usually self-limiting and heals without scarring
Adequate fluid intake
Offer leaflets or websites for more info
Avoid kissing, oral until lesions fully healed, don’t share pillows, makeup, or lip balms. Don’t touch lesions other than when applying treatment – dab instead of rubbing. Wash hands after touching.
Athletes foot
Interdigital — most common; affects the lateral toe web spaces first; usually caused by Trichophyton rubrum.
Moccasin or dry — diffuse chronic scaling and hyperkeratosis affecting the sole and lateral foot; usually caused by Trichophyton rubrum.
Vesicobullous — least common; multiple small vesicles and blisters mainly on the arches and soles of the feet; usually caused by Trichophyton interdigital.
Risk – hot, humid, occlusive footwear excessive sweating, contaminated surfaces, immunocompromised
Advice
Wear well fitting, open footwear that keep feet cool and dry, replace old shoes that may be contaminated. Maintain good foot hygiene – wear different pair of shoes every 2-3 days. Wear cotton, absorbent socks, don’t scratch skin, after washing feet dry then well and between toes, don’t share towels and wash towel freq.
Treatment
Topical antifungal cream in mild, non-extensive disease
Terbinafine 1% cream (12 and over – apply thinly to affected area 1 or 2 daily for 7 days) or clotrimazole 1% cream (2-3 times daily and continue for 4 weeks minimum) okay for kids – OTC for some ages
Additional mild topical corticosteroid if there’s inflammation
Hydrocortisone 1% cream (OD for max 7 days)
Adult severe or extensive – oral antifungal with confirmed fungal infection
1st choice – terbinafine (250 mg once daily for 2–6 weeks, depending on the severity of infection)
2nd – itraconazole, Griseofulvin if not tolerated or contraindicated
Refer
Treatment failure, severe pain, got, painful and red (indicative of serious infection), infection spreads, diabetic patient, immunocompromised
Warts and verrucae
Warts – small, rough growths caused by infection of skin with HPV, form anywhere on skin most commonly on hand and feet
Verruca – (plantar wart) wart on sold of feet
Spread by direct contact, occur and clear spontaneously at any time or may take years
Common warts are firm and raised with a rough surface that resembles a cauliflower (common on knuckles, knees, and fingers).
Periungual warts are common warts around the nails that can be painful and disturb nail growth — nail biting is a risk factor.
Plane warts are usually round, flat-topped, and skin coloured or greyish yellow (common on the backs of hands).
Filiform warts have a finger-like appearance and may have a stalk (more common on the face and neck).
Palmar and plantar warts grow on the palms and the soles of the feet (verrucae). They often have central dark dots (thrombosed capillaries) and may be painful.
Mosaic warts occur when palmar or plantar warts coalesce into larger plaques on the hands and feet.
Not harmful and don’t come with symptoms and resolve with treatment
Advice
Reducing transmission and limit spread, keep feet dry, wear slippers or waterproof plaster in shower and communal areas. don’t share towels, socks, shoes. Don’t scratch lesions, bite nails or suck fingers with warts
Refer
Painful, facial, uncertain diagnosis, immunocompromised, extensively infected
Treatment
Only treated if painful, cosmetically unsightly, or patient request and persistent as the treatment is long and can have side effects.
Topical salicylic acid – up to 12 weeks
Duofilm® (salicylic acid 16.7% plus lactic acid 16.7%) — licensed for plantar and mosaic warts.
Bazuka® extra strength gel (salicylic acid 26%) — licensed for warts and verrucae.
Occlusal® (salicylic acid 26%) — licensed for common and plantar warts.
Salactol® (salicylic acid 16.7% plus lactic acid 16.7%) — licensed for warts, plantar warts, and verrucae.
Apply OD at night, file and soften area by soaking in warm water for 5-10 mins, peel of remaining film before administering next dose, don’t apply on healthy skin
Cryotherapy – every 2 weeks for max 6 treatments
Liquid nitrogen – only for older children and adults
Corns and calluses
Hard or thick areas of skin that can be painful
Corns – lumps of hard skin on knuckles and joints of toes
Callouses – larger patches of rough, thick skin
Both can be tender and painful
Refer
Diabetic, heart disease, circulation issues. Bleeding or puss, treatment failure after 3 weeks, severe pain
Advice
Wear thick, cushioned socks, wear wide, comfortable shoes with low heel and soft sole, use insoles or heel pads, soak corns and calluses in warm water to soften them, use pumice stone regularly or foot file to remove hard skin. Moisturise.
Don’t try to cut them, walk, or stand for long period, wear high heels or tight pointy shoes, go barefoot
Treatment
Heel pads and insoles, OTC products, pain relief
Carnation brand caps for both – adhesive dressing
Fungal nail infection
Caused by dermatophyte and non-dermatophyte moulds and yeasts
Symptoms
Discoloured, abnormal, small flaky white patches and pits on top of nail and becomes rough and eroded. Nail lifted, wite or yellow opaque streaks on one side of nail, scaling, thickening
Refer
Diabetic, severe, treatment failure, spread to other nails
Advice
Keep nails trimmed short and filed, don’t share clippers and files. Well-fitting shoes, cotton socks, maintain good foot hygiene, weak shoes in communal places, avoid nail trauma
Treatment
Not needed if patient not troubled by appearance and infection is asymptomatic
Advise antifungal treatment if – walking uncomfortable, distress, cosmetic, co-morbid complication, or complication
If dermatophyte or candida infection conformed – topical antifungal treatment 0f 50% of nail involved, 2 nails infected, contraindication to oral antifungal
Topical – amorolfine 5% mail lacquer – OTC apply 1 or 2 weekly to affected nail after gentle nail filing – 6 months minimum for fingernails, 12 months for toenails
If dermatophyte nail infection is confirmed:
Prescribe oral terbinafine first-line.
250 mg once a day for between 6 weeks and 3 months for fingernails, and for 3–6 months for toenails
Oral itraconazole if an alternative drug is indicated.
Prescribe as pulsed therapy 200 mg twice a day for 1 week, with subsequent courses repeated after a further 21 days.
If Candida or non-dermatophyte nail infection is confirmed:
Prescribe oral itraconazole first-line.
Prescribe as pulsed therapy 200 mg twice a day for 1 week, with subsequent courses repeated after a further 21 days.
Prescribe oral terbinafine if an alternative drug is indicated.
Prescribe 250 mg once a day for between 6 weeks and 3 months for fingernails, and for 3–6 months for toenails.
0 notes
Text
Recognizing the Symptoms of Lung Cancer in Women
Lung cancer is well-known as a smoker’s disease which is directly related to men. Lung cancer cases have set alarming issues these days. As per research, it has been confirmed that women are more likely to get lung cancer as compared to men. Yes, It's true! Lung cancer in women is very common between the age of 30-60 years as compared to men. Well, women do not need to worry about it because the survival rates of lung cancer are improving too. However, it is important to detect lung cancer symptoms at an early stage for better recovery and a higher survival rate.

Juggling between personal and professional life, many women tend to ignore health issues. In this context,GS Cancer Hospital, Ghaziabad aims to spread awareness about recognizing the symptoms of lung cancer in women at an early stage. GS Hospital is the best lung cancer hospital in Ghaziabad known for its expertise in cancer therapy and prevention at its best. The hospital is equipped with quality cancer healthcare treatment and services under the guidanceof thebest oncologists in Meerut.
In this blog, we shall unleash how to recognize symptoms of lung cancer in women at an early stage under the expertise of GS Hospital, thebest lung cancer hospital in UP. Let’s begin!
Incidence and statistics of lung cancer cases in men and women
Lung cancer is known as the second most common type of cancer in males and females. Over the years, it has been noted that the incidence of lung cancer rate has reduced in men while there has been a sudden spike in the incidence of lung cancer cases in women which is quite alarming.
Globally, women must be educated about the same to take preventive measures for lung cancer. GS Cancer Hospital Ghaziabad has started its mission to global awareness about lung cancer in women this year 2024 to put an end to the alarming rates of increasing incidence of lung cancer cases in women. This is a shout-out call to all ladies out there to join hands in the mission with GS Hospital, India to spread awareness about lung cancer in women.
The first step towards this awareness is to recognize the symptoms of lung cancer at an early stage. Let us check out the symptoms of lung cancer in women in the next part of the article.
Signs and Symptoms of lung cancer in women
The signs and symptoms of lung cancer in women may differ at times. It may be alarming in some advanced cases. However, in the early stages, the symptoms may be not visible with minor discomfort. As lung cancer progresses, the symptoms may worsen affecting daily activities. Some of the common signs and symptoms of lung cancer in women are as follows-
Fatigue and tiredness in the initial stages
Changes in weight with sudden onset of weight loss
Loss of appetite with no desire to eat
Episodes of fever
A persistent cough that does not go away
Shortness of breath at rest or exertional dyspnea
Wheezing
Hoarseness of voice with changes in voice
Recurrent chest pain and chest congestion
Frequent occurrence of lung infection
These are the 10 most common symptoms of lung cancer in women. The symptoms of lung cancer in women may tend to differ at times due to the specific stages at which lung cancer is diagnosed. The severity of the lung cancer symptoms will depend on the stage of lung cancer. Hence, it is important to get diagnosed at an early stage of cancer through regular medical check-ups and screening. It has been noted that cancer does not cause any symptoms at an early stage.
The difference in lung cancer cases in men and women
The causes and symptoms of lung cancer in men and women would always differ. Lung cancer may affect different parts of the lung leading to different symptoms in men and women. The major types of lung cancer in women are as follows-
Non-small cell lung cancer (NSCLC)- This is the most common type of cancer affecting 80-90% of cases of lung cancer in both men and women.
Lung adenocarcinoma is the most common form of lung cancer seen commonly in women who have non-smoking status. These lung cancers have higher chances of metastasis with complications affecting different organs such as bones or stomach.
Squamous cell carcinoma is another common form of lung cancer that is seen in women who are prone to smoking due to blockage of airways.
Large cell carcinoma can grow anywhere in the lungs and tends to spread quickly.
Small cell lung cancer (SCLC)- This is the type of lung cancer affecting 10-20% of cases of lung cancer which is mostly commonly seen in smoking individuals.
Carcinoid tumors constitute about 1-2% of cases of lung cancers which tend to occur in younger women.
Risk factors of lung cancer
The risk factors of lung cancer are as follows-
Genetic - Family history of lung cancer
Aging leads to low immunity
Recurrent lung infections
Exposure to occupational and environmental carcinogens
Addictions like smoking and alcohol
Hormonal causes in women due to estrogen-specific hormone which may trigger cancer growth
Females are more prone to genetic mutations for cancer
As per research, it has been noted that women who have never smoked are diagnosed at the advanced stages of cancer with metastasis which can give rise to many complications. Moreover, women with comorbidities such as asthma or COPD (Chronic Obstructive Pulmonary Disease) have higher chances of lung cancer.
Prognosis of lung cancer in women
The prognosis of lung cancer would depend upon the diagnosis of lung cancer. It involves the following factors-
Stage of lung cancer
Metastasis of lung cancer
Severity of symptoms of lung cancer
With regular screenings and timely treatment, if you are in remission or have no evidence of disease (NED) for more than 5 years, you will be termed as a cured case for lung cancer by your doctor. However, it is always important to maintain preventive measures and regular check-ups for better respiratory health.
Prevention of lung cancer in women
The preventive measures for lung cancer are focused on reducing the risk of lung cancer. These include-
Avoid smoking and plan to quit. It may take around 5 years for the pulmonary function to recover from lung damage thus reducing the risk of lung cancer.
Stay away from second-hand smoke or passive smoking
Eat a healthy diet with good hydration to reduce the risk of lung cancer
Talk to your doctor for regular lung cancer screening tests.
Focus on self-cancer by keeping track of your follow-up and treatment
A Word from GS Hospital
The word “cancer” can bring an overwhelming situation for many patients. It can affect the overall quality of life with mental and physical symptoms which can take a toll on health. Cancer treatment is a long process and requires medical attention with monitoring.
GS Hospital is focused on providing the best healthcare treatment and preventive care for all patients. With new research and advancements in lung cancer, the hospital offers one of the best solutions for lung cancer treatment with a professional team of oncologists. Being the best cancer hospital in Meerut, the hospital has been witnessing a sudden spike in lung cancer cases in women which has been alarming.
At this stage of increasing lung cancer cases in women, it is advisable to go for routine check-ups and screening tests regularly. In such cases, awareness about recognizing the symptoms of lung cancer in women is very crucial.
0 notes