#claims process software
Explore tagged Tumblr posts
Text
The Claim Catalyst: Accelerate Your Workflow with Our Claims Processing Software
Reboot your claims management experience with our exceptional Claims Processing Software. Discover the power of inbuilt analytics that enhances your decision-making process, enjoy smart configuration for easy workflow customization, and a secure cloud-first platform designed for scalability and accessibility. Choose DataGenix for innovative solutions in Riverside, CA.
#claimmanagement#claimssoftware#claimmanagementsoftware#claims processing system insurance software#claims process software
0 notes
Text
The Importance of HIPAA Compliance in Oncology Billing
In the realm of healthcare services, oncology billing presents unique challenges due to the complexity of treatments, evolving medical coding requirements, and the sensitive nature of patient data. With an increasing reliance on technology in medical billing services, ensuring compliance with the Health Insurance Portability and Accountability Act (HIPAA) is critical. HIPAA compliance not only safeguards patient data but also ensures smooth claims processing, revenue cycle management, and operational efficiency. This article delves into the significance of HIPAA compliance in oncology billing services, highlighting its role in ensuring secure and efficient medical practices.
Protecting Patient Data in Oncology Billing
Oncology billing services handle highly sensitive patient information, including medical histories, treatment plans, and insurance details. Given the nature of oncology care, maintaining the confidentiality of this data is a top priority. HIPAA mandates stringent measures to secure protected health information (PHI) against unauthorized access, breaches, or misuse.
Adhering to HIPAA regulations ensures that oncology practices and medical billing services implement robust security measures, such as encryption and access controls. This not only protects patient privacy but also fosters trust between healthcare providers and their patients. With healthcare services increasingly leveraging electronic health records (EHRs) and digital claims management services, ensuring compliance reduces the risk of costly data breaches and legal repercussions.
Ensuring Accurate Claims Management
Claims management services play a crucial role in oncology billing by streamlining the submission and processing of insurance claims. HIPAA compliance is integral to this process, as it ensures that all patient data shared with insurers and clearinghouses adheres to federal standards for data security and accuracy.
Compliance minimizes errors in medical coding services, reducing claim denials and delays that can disrupt revenue cycle management. Accurate and secure claims submissions help oncology practices receive timely reimbursements, maintaining financial stability while focusing on patient care. By adhering to HIPAA, medical billing services ensure seamless communication between all stakeholders involved in the claims process.
Reducing Legal and Financial Risks
Non-compliance with HIPAA can lead to significant legal and financial repercussions for oncology practices and billing service providers. Penalties for violations range from thousands to millions of dollars, depending on the severity and intent of the breach. For oncology billing services that manage large volumes of sensitive data, these penalties can severely impact business operations.
HIPAA compliance reduces these risks by enforcing stringent guidelines for data handling, storage, and transmission. For instance, medical billing services must ensure secure communication channels when transferring patient data between healthcare providers, payers, and claims management services. Proactively addressing compliance requirements not only prevents potential penalties but also enhances the overall efficiency of oncology practices.
Enhancing Revenue Cycle Management
Revenue cycle management is a critical aspect of oncology billing services, encompassing patient registration, claims submission, payment collection, and reporting. HIPAA compliance ensures that each step of this process operates within a secure and efficient framework.
By adhering to HIPAA regulations, oncology practices can optimize their revenue cycle, reduce claim denials, and improve cash flow. Additionally, HIPAA mandates regular audits and compliance checks, helping medical billing services identify and rectify inefficiencies in the billing process. A compliant revenue cycle management system enables oncology practices to focus on delivering high-quality patient care while ensuring financial sustainability.
Conclusion: Compliance as a Cornerstone of Success
HIPAA compliance is not just a regulatory requirement; it is a cornerstone of effective oncology billing services. By protecting patient data, ensuring accurate claims management, and mitigating legal risks, compliance supports the financial and operational health of oncology practices. As the healthcare industry evolves, medical billing services must prioritize HIPAA compliance to meet the growing demands of secure and efficient claims management services.
For oncology providers, investing in HIPAA-compliant systems and practices is essential to delivering top-tier healthcare services while safeguarding patient trust. In an era where data security and revenue cycle management are paramount, compliance is the foundation of sustainable success.
#oncology billing services#medical billing services#claims management services#revenue cycle management#claims management software#healthcareclaims#claims processing
0 notes
Text
Explore Three Big Benefits of CMS Medicare Pricer Software
Healthcare professionals face the critical task of ensuring patients receive appropriate care daily. One such activity is claims processing, which can be time-consuming and error-prone if done manually. The CMS Medicare Pricer software allows for a good way out in processing claims, thus making precise and efficient claims handling possible.

Here are three key advantages of CMS Medicare Pricer Software in processing claims.
Enhanced Accuracy and Speed CMS Medicare Pricer software significantly reduces the probability of human error in calculating claims. Its automated algorithms ensure that claims are priced according to Medicare rates and save a lot of time with much accuracy. This, in turn, expedites the reimbursement process and improves healthcare facilities' cash flow.
Cost-efficient solution for Healthcare Providers Manual claims processing is time-consuming and labor-intensive that increases the operational cost. The CMS medicare pricer tool, on the other hand, is a SaaS-based application that assists in reducing the labor cost since it eliminates the repetitive tasks and the need for manual data entry. This would, therefore, enable healthcare providers to use their resources efficiently.
Adherence to Medicare Codes & Guidelines Medicare pricing rules can be very technical, and maintaining compliance is the only way to avoid penalties. CMS Medicare Pricer software is regularly upgraded to accommodate all the latest guidelines and updates, keeping healthcare providers in compliance easily. This helps ensure that claims are processed within regulatory standards, avoiding possible compliance issues.
Conclusion Therefore, SaaS-based CMS medicare pricer software is a powerful tool for any healthcare facility. By computerizing claims processing, it improves accuracy, cost efficiency, and compliance. If you are investing in one for your healthcare facility, make sure to choose the one with features like high security, 24/7 availability, and an easy installation method.
0 notes
Text
Uncover the significant benefits of claims management software, from improving efficiency to reducing manual errors. Learn how this software enhances the claims process, ensures compliance, and delivers faster resolutions for insurance and healthcare sectors.
#claims management software#claims processing#software benefits#insurance software#healthcare claims#claims automation#business compliance.
0 notes
Text
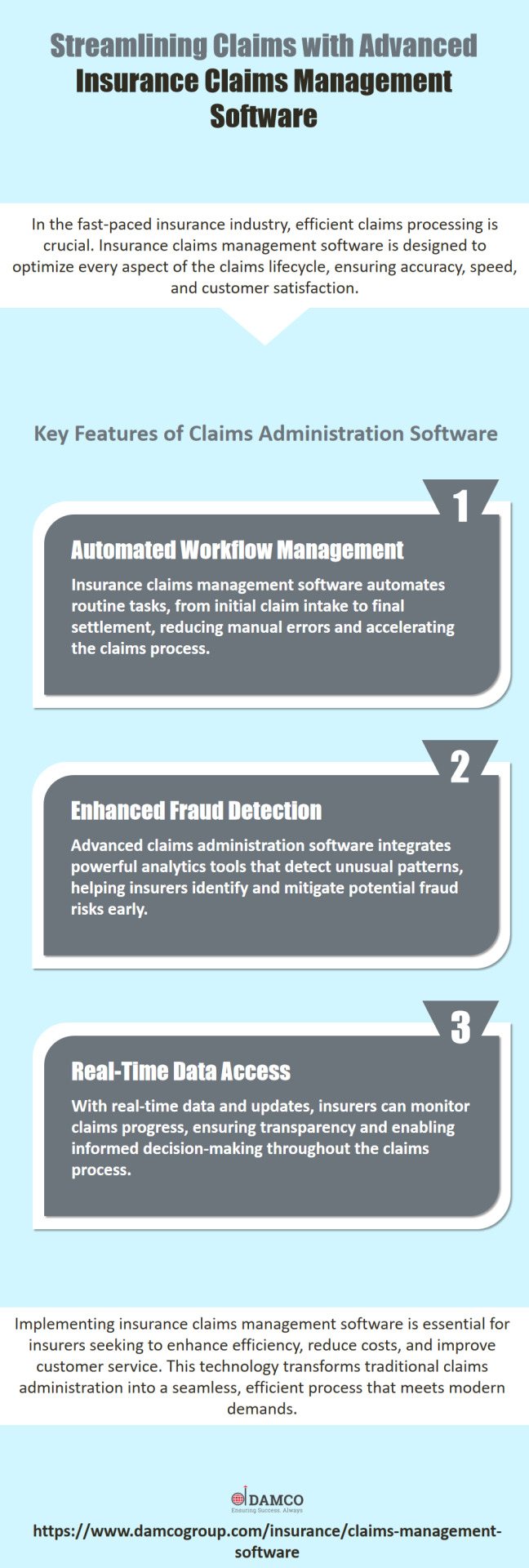
Transform your claims processing with our innovative claims administration software. Contact us today to see how we can enhance your insurance operations. Visit: https://www.damcogroup.com/insurance/claims-management-software
#insurance technology#insurance software#insurance solutions#claims management software#claims processing software#claims administration software
0 notes
Text
Revenue Cycle Management Market Will Grow At Highest Pace Owing To Increased Focus On Digitalizing Healthcare Billing Processes

Revenue cycle management (RCM) plays a critical role in healthcare organizations by handling all administrative and financial transactions related to patients, including registration, claims processing, payments, revenue generation, and reporting. RCM solutions assist in streamlining workflows to enhance organizational efficiency. It allows healthcare providers to accurately bill patients, insurance companies, and government agencies for clinical services rendered. Key advantages of RCM include improved billing accuracy, reduced claims denial, enhanced collection of valid receivables, and optimized revenue for healthcare organizations. Growing need to curtail escalating healthcare costs and digitize billing processes in the industry are fueling adoption of RCM solutions. The Global Revenue Cycle Management Market Size is estimated to be valued at US$ 156.68 Bn in 2024 and is expected to exhibit a CAGR of 11% over the forecast period 2024 to 2031.
Key Takeaways Key players operating in the Revenue Cycle Management are Athenahealth, Experian Health, Cerner, GE Healthcare, Coronis, Epic Systems, Conifer Health Solutions, eClinicalWorks, Change Healthcare, Optum, Waystar, McKesson Corporation, R1, Experian Health, Veradigm LLC, CareCloud Corporation, Access Healthcare, and AdvantEdge Healthcare Solutions. The growing demand for RCM solutions is attributed to increasing patient volume, rising healthcare insurance rates, complicated insurance regulations, and an aging US population requiring greater medical care. RCM tools assist providers in maximizing reimbursement through improved charge capture, billing accuracy, and collections. Technological advancements in cloud computing, artificial intelligence, and machine learning are boosting the growth of the RCM market. Vendors are increasingly leveraging emerging technologies to streamline workflows and develop intelligent solutions for claims processing, denial management, and payment posting. AI-enabled solutions are helping automate repetitive tasks and provide real-time insights into organizational performance. Market Trends There is growing adoption of cloud-based RCM solutions owing to benefits such as scalability, mobility, lower upfront costs, and easy access to real-time patient information. Cloud platforms are enabling improved collaboration between disparate healthcare organizations. Many vendors are offering SaaS-based models to drive market penetration. Mobile RCM technologies are also gaining popularity to support on-the-go access for physicians and financial counselors. Mobile apps allow capture of charges during patient consultations and improve connectivity with external partners. This is helping streamline workflows across care delivery settings.
Get More Insights On This Topic: Revenue Cycle Management Market
#Revenue Cycle Management Market#Healthcare Finance#Medical Billing#Claims Processing#Revenue Optimization#Financial Analytics#Healthcare Administration#Billing Software
0 notes
Text
Elevating Excellence: Why the Transportation and Logistics Industry Should Prioritize Enhanced Customer Service
In the fast-paced and competitive realm of transportation and logistics, the emphasis on enhanced customer service is becoming increasingly vital. This blog post delves into the reasons why the transportation and logistics industry should prioritize customer service, exploring how it can lead to increased customer satisfaction, improved operational efficiency, and a strengthened market position.

Transportation Customer Service:
Transportation customer service underscores the unique challenges and opportunities within the transportation sector. Acknowledging the specific needs of customers in the logistics chain is crucial for building lasting relationships and ensuring a positive overall experience.
Customer Support Management:
The customer support management highlights the strategic approach required to deliver exceptional customer service. Effective management of customer support processes, from order inquiries to issue resolution, is instrumental in meeting and exceeding customer expectations.
Multilingual Customer Support:
In an increasingly globalized world, the term Multilingual customer support becomes pivotal. Offering customer support in multiple languages is not just a convenience; it is a necessity in a diverse and interconnected marketplace. Multilingual customer support enhances accessibility, fosters international collaboration, and demonstrates a commitment to meeting the unique needs of a global customer base.
Reasons to Prioritize Enhanced Customer Service:
Customer Satisfaction: A focus on enhanced customer service directly correlates with increased customer satisfaction. By providing prompt and accurate information, addressing concerns proactively, and ensuring a seamless experience, businesses build trust and loyalty among their clientele.
Operational Efficiency: Streamlining customer support management contributes to operational efficiency. Resolving issues promptly, minimizing order discrepancies, and optimizing communication channels lead to smoother logistics operations and reduced disruptions.
Competitive Edge: In an industry where competition is fierce, superior customer service becomes a key differentiator. Companies that prioritize customer satisfaction gain a competitive edge, attracting and retaining clients in a market where service quality often defines success.
Brand Reputation: Customer service plays a crucial role in shaping a brand's reputation. Positive interactions with customers contribute to a positive brand image, while subpar customer service can lead to reputational damage. A strong brand reputation, built on excellent customer service, enhances market credibility and trust.
Conclusion: In conclusion, prioritizing enhanced customer service in the transportation and logistics industry is not just a matter of meeting expectations; it is a strategic imperative. From transportation customer service tailored to the unique needs of the industry to effective customer support management and multilingual support for a global clientele, the benefits are manifold. By placing customer satisfaction at the forefront, businesses in the transportation and logistics sector can navigate challenges, foster growth, and secure a prominent position in an ever-evolving and competitive marketplace. In a world where customer-centricity is paramount, elevating customer service becomes a pathway to sustained success and industry leadership.
#Transportation customer service#customer support management#Multilingual customer support#Trucking Dispatch Companies#Bpo services#Support center#Support ticket system#Live chat support#Online support#Customer support software#Healthcare bpo#Healthcare business process outsourcing#load board outsourcing#end to end supply chain#Data entry outsourcing#Business process outsourcing companies#Customer support outsourcing#claim managament#Bpo solutions#Customer support solutions#Customer support chat#supply chain outsourcing#Back office outsourcing#Customer support team#back office outsourcing services#carrier onboarding#logistics control tower#Offshore bpo#transporation customer service#Customer support ticket
0 notes
Note
What I don't get is that other your support of AI image generation, you're SO smart and well read and concerned with ethics. I genuinely looked up to you! So, what, ethics for everyone except for artists, or what? Is animation (my industry, so maybe I care more than the average person) too juvenile and simplistic a medium for you to care about its extinction at the hands of CEOs endorsing AI? This might sound juvenile too, but I'm kinda devastated, because I genuinely thought you were cool. You're either with artists or against us imho, on an issue as large as this, when already the layoffs in the industry are insurmountable for many, despite ongoing attempts to unionize. That user called someone a fascist for pointing this out, too. I guess both of you feel that way about those of us involved in class action lawsuits against AI image generation software.
i can't speak for anyone else or the things they've said or think of anyone. that said:
1. you should not look up to people on the computer. i'm just a girl running a silly little blog.
2. i am an artist across multiple mediums. the 'no true scotsman' bit where 'artists' are people who agree with you and you can discount anyone disagrees with you as 'not an artist' and therefore fundamentally unsympathetic to artists will make it very difficult to actually engage in substantive discussion.
3. i've stated my positions on this many times but i'll do it one more: i support unionization and industrial action. i support working class artists extracting safeguards from their employers against their immiseration by the introduction of AI technology into the work flow (i just made a post about this funnily enough). i think it is Bad for studio execs or publishers or whoever to replace artists with LLMs. However,
4. this is not a unique feature of AI or a unique evil built into the technology. this is just the nature of any technological advance under capitalism, that it will be used to increase productivity, which will push people out of work and use the increased competition for jobs to leverage that precarity into lower wages and worse conditions. the solution to this is not to oppose all advances in technology forever--the solution is to change the economic system under which technologies are leveraged for profit instead of general wellbeing.
5. this all said anyone involved in a class action lawsuit over AI is an enemy of art and everything i value in the world, because these lawsuits are all founded in ridiculous copyright claims that, if legitimated in court, would be cataclysmic for all transformative art--a victory for any of these spurious boondoggles would set a precedent that the bar for '''infringement''' is met by a process that is orders of magnitude less derivative than collage, sampling, found art, cut-ups, and even simple homage and reference. whatever windmills they think they are going to defeat, these people are crusading for the biggest expansion of copyright regime since mickey mouse and anyone who cares at all about art and creativity flourishing should hope they fail.
2K notes
·
View notes
Text
Medical Insurance Billing Software
Medical insurance billing software, also called electronic claims software, is now one of the most important elements of a successful medical practice. Medical insurance billing is no longer as time-consuming as it once was.
Now you have the opportunity to electronically file insurance policy claims quickly and resolve issues easily. You can spend more time processing the claim and less time in follow-up. This will keep costs down, as insurance processing will now run more efficiently and administrative work will be reduced. You may receive payments more quickly and spend less time on accounts receivable follow-up calls. Learn more about- Insurance Software Solutions, Claims Processing Software, Insurance Administration Software and much more related to the same.

Many medical offices utilize the power of the Internet to conduct everyday transactions more efficiently, more accurately, and less expensively than ever before. Some of the functions that can be performed via the Internet include checking eligibility and claims status, receiving referrals and authorizations, and acquiring pre-certifications.
A popular option that many experts recommend is web-based software. All you need is an average computer along with a broadband Internet connection. Web-based companies offer many services, such as software support, security, database management and training. Some of the specific services offered for medical insurance billing are the fact that claim files are automatically generated at scheduled times and submitted to the carriers and clearinghouses without user intervention, and automatically downloaded responses that are interpreted and converted into word processing format and claims marked as submitted when the response file is received through the carrier instead of once the biller saves the claim.
The web-based option eliminates the burden of maintaining network servers, backup tapes, upgrades or modems. Discover if the software package will fill all the medical insurance needs of your practice by finding providers who are experienced in health care management solutions and issues specific to healthcare insurance claims.
When searching for the appropriate medical insurance billing software, consider if the software makes the incomprehensible simple. Medical insurance software systems should include a comprehensive selection of features to ensure that you can manage your practice files, claims and billing with maximum ease and efficiency. Some important features to look for are access to the latest forms and guidelines, a step-by-step procedure that will prompt you through the claims process with relative ease, and features that may automatically print the proper forms, documents and bills when complete.
Why waste time on phone calls to insurance companies when medical insurance billing software can provide quick access to claims management. Let your health care insurance billing software interface directly with the carrier and your practice. Medical insurance billing software is just one of the many options now available that make operating a medical practice easier than ever before.
0 notes
Text

DataGenix provides an all-in-one solution for claims management, offering automated tools to streamline your operations and minimize manual errors. Perfect for healthcare and insurance sectors! Visit: https://datagenix.com/
#datagenix#Health Claims Software#Claims Management Software#Claims Processing Software#TPA Software#Medical Claims Software
0 notes
Text
Best Practices for Healthcare Providers to Maximize Telehealth Billing Efficiency
Telehealth has revolutionized healthcare, enabling providers to reach patients in remote locations and offering convenient access to medical services. However, along with its benefits, telehealth presents unique challenges in billing and reimbursement. As the demand for telehealth services grows, it becomes increasingly important for healthcare providers to optimize their telehealth billing processes. In this article, we explore the best practices for healthcare providers to streamline telehealth billing efficiency, ensuring accuracy and timeliness in claims, while maximizing revenue.
Understand Telehealth Billing Regulations and Policies
One of the key factors that affect telehealth billing efficiency is understanding the regulations and policies governing telehealth services. These rules vary significantly across states and insurers. For instance, Medicare, Medicaid, and private insurance companies have different guidelines when it comes to telehealth reimbursement, coding, and coverage.
To navigate these complexities, healthcare providers should regularly review updates from the Centers for Medicare & Medicaid Services (CMS) and stay informed about any policy changes related to telehealth billing. Understanding which telehealth services are eligible for reimbursement and ensuring that claims are compliant with regulatory requirements will help avoid claim rejections and delays. Regular training and keeping abreast of telehealth billing regulations are essential for improving your revenue cycle management.
Optimize Medical Billing and Coding for Telehealth Services
Efficient medical billing and coding is critical to the success of telehealth billing services. Coding errors are one of the most common reasons for claim denials, and in telehealth, the complexity increases as providers must use specific codes for virtual services. Healthcare providers need to ensure they are using accurate Current Procedural Terminology (CPT) codes and Healthcare Common Procedure Coding System (HCPCS) codes for telehealth visits.
Training your medical billing staff to correctly use telehealth-specific codes will significantly reduce errors. Implementing auditing procedures to catch discrepancies before claims are submitted will also improve efficiency. By aligning billing and coding practices with insurance claim processing requirements, healthcare providers can ensure faster reimbursement and a smoother telehealth billing process.
Implement Advanced Healthcare Information Management Systems
Technology plays a crucial role in improving the efficiency of telehealth billing services. Adopting an advanced healthcare information management system can automate many tasks in the billing process, including patient eligibility verification, claims submission, and follow-up on unpaid claims. These systems not only help reduce administrative burden but also minimize errors and expedite insurance claim processing.
Look for healthcare information management platforms that integrate with telehealth platforms and allow real-time data sharing between patient care and billing systems. Automating these processes ensures that patient records, telehealth visit documentation, and billing codes are accurately synced, reducing the chances of missed charges or coding errors. Efficient use of technology in telehealth billing services will lead to quicker claim approval and a more streamlined revenue cycle management process.
Enhance Revenue Cycle Management with Timely Claims Submission
A key element in maximizing telehealth billing efficiency is optimizing revenue cycle management (RCM). Timely submission of claims plays a major role in ensuring cash flow remains steady. Delays in claim submissions can lead to revenue losses or disruptions. Healthcare providers should prioritize submitting clean claims as quickly as possible to minimize the risk of rejections and denials.
Having a dedicated team to track and manage the status of insurance claims is crucial. By regularly monitoring the claims submission process, your team can follow up on unpaid or delayed claims, resubmit corrected claims, and address denials immediately. A robust RCM strategy should include real-time reporting tools that provide insights into the status of claims, allowing for faster decision-making and resolution.
Partner with a Specialized Telehealth Billing Service Provider
Managing telehealth billing in-house can be time-consuming and prone to errors, especially with the growing demand for virtual healthcare services. Outsourcing your telehealth billing services to a specialized provider can significantly enhance billing efficiency. Professional medical billing services have the expertise to handle telehealth-specific coding, insurance claim processing, and compliance with state and federal regulations.
By partnering with a telehealth billing company, healthcare providers can focus on delivering quality patient care while leaving the complex billing process to experts. Outsourcing also reduces overhead costs related to hiring and training in-house billing staff, allowing for a more cost-effective revenue cycle management approach. With a specialized provider managing your telehealth billing, you can maximize reimbursement rates and minimize claim denials.
Conclusion: Streamline Your Telehealth Billing Process for Maximum Efficiency
In today’s evolving healthcare landscape, telehealth is here to stay. To ensure its long-term viability, healthcare providers must adopt best practices in telehealth billing, such as staying updated on regulations, optimizing medical billing and coding, and leveraging advanced healthcare information management systems. With a focus on timely claim submissions and a robust revenue cycle management strategy, providers can enhance their telehealth billing efficiency and ensure continuous cash flow.
For those looking to take their telehealth billing to the next level, partnering with a professional telehealth billing service provider is a smart investment. At [Your Company Name], we offer specialized telehealth billing services in the USA, providing you with end-to-end support for all your medical billing needs. From accurate coding to insurance claim processing, our team ensures that your telehealth billing is seamless, compliant, and optimized for maximum revenue. Let us handle the complexities while you focus on delivering exceptional patient care.Contact us today to learn how our telehealth billing solutions can boost your revenue and streamline your operations.
#medical coding#healthcareclaims#claims management software#claims processing#medical billing services#revenue cycle management#medical billing and coding#Healthcare Insurance
0 notes
Text
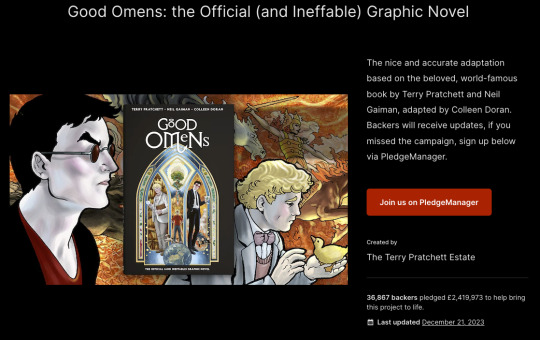
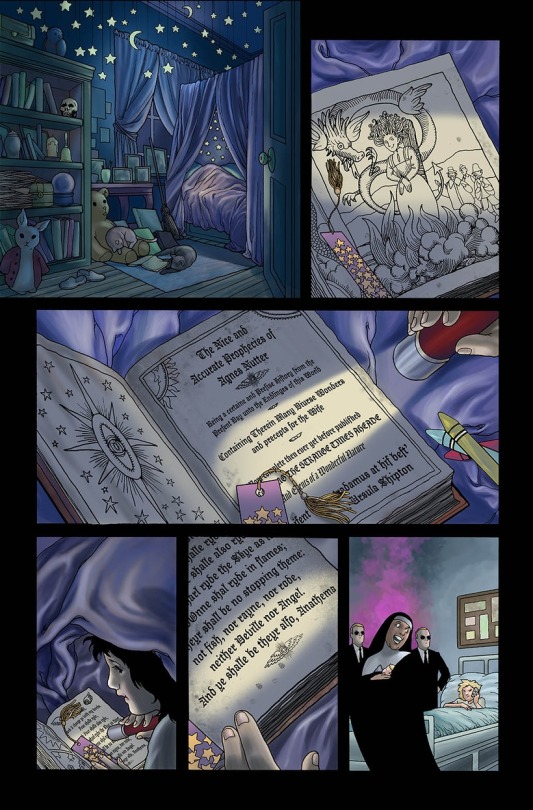
Great Big Good Omens Graphic Novel Update
AKA A Visit From Bildad the Shuhite.
The past year or so has been one long visit from this guy, whereupon he smiteth my goats and burneth my crops, woe unto the woeful cartoonist.
Gaze upon the horror of Bildad the Shuhite.

You kind of have to be a Good Omens fan to get this joke, but trust me, it's hilarious.
Anyway, as a long time Good Omens novel fan, you may imagine how thrilled I was to get picked to adapt the graphic novel.
Go me!

This is quite a task, I have to say, especially since I was originally going to just draw (and color) it, but I ended up writing the adaptation as well. Tricky to fit a 400 page novel into a 160-ish page graphic novel, especially when so much of the humor is dependent on the language, and not necessarily on the visuals.
Not complainin', just sayin'.
Anyway, I started out the gate like a herd of turtles, because right away I got COVID which knocked me on my butt.
And COVID brain fog? That's a thing. I already struggle with brain fog due to autoimmune disease, and COVID made it worse.
Not complainin' just sayin'.
This set a few of the assignments on my plate back, which pushed starting Good Omens back.
But hey, big fat lead time! No worries!
Then my computer crawled toward the grave.
My trusty MAC Pro Tower was nearly 15 years old when its sturdy heart ground to a near-halt with daily crashes. I finally got around to doing some diagnostics; some of its little brain actions were at 5% functionality. I had no reliable backups.
There are so many issues with getting a new computer when you haven't had a new computer or peripherals in nearly fifteen years and all of your software, including your Photoshop program is fifteen years old.
At the time, I was still on rural internet...which means dial-up speed.

Whatever you have for internet in the city, roll that clock back to about 2001.
That's what I had. I not only had to replace almost all of my hardware but I had to load and update all programs at dial-up speed.
Welcome to my gigabyte hell.
The entire process of replacing the equipment and programs took weeks and then I had to relearn all the software.
All of this was super expensive in terms of money and time cost.
But I was not daunted! Nosirree!
I still had a huge lead time! I can do anything! I have an iron will!
And boy, howdy, I was going to need it.
At about the same time, a big fatcat quadrillionaire client who had hired me years ago to develop a big, major transmedia project for which I was paid almost entirely in stock, went bankrupt leaving everyone holding the bag, and taking a huge chunk of my future retirement fund with it.
I wrote a very snarky almost hilarious Patreon post about it, but am not entirely in a position to speak freely because I don't want to get sued. Even though I had to go to court over it, (and I had to do that over Zoom at dial-up speed,) I'm pretty sure I'll never get anything out of this drama, and neither will anyone else involved, except millionaire dude and his buddies who all walked away with huge multi-million dollar bonuses weeks before they declared bankruptcy, all the while claiming they would not declare bankruptcy.
Even the accountant got $250,000 a month to shut down the business, while creators got nothing.
That in itself was enough drama for the year, but we were only at February by that point, and with all those months left, 2023 had a lot more to throw at me.
Fresh from my return from my Society of Illustrators show, and a lovely time at MOCCA, it was time to face practical medical issues, health updates, screening, and the like. I did my adult duty and then went back to work hoping for no news, but still had a weird feeling there would be news.

I know everyone says that, but I mean it. I had a bad feeling.
Then there was news.
I was called back for tests and more tests. This took weeks. The ubiquitous biopsy looked, even to me staring at the screen in real time, like bad news.
It also hurt like a mofo after the anesthesia wore off. I wasn't expecting that.
Then I got the official bad news.
Cancer which runs in my family finally got me. Frankly, I was surprised I didn't get it sooner.
Stage 0, and treatment would likely be fast and complication-free. Face the peril, get it over with, and get back to work.
I requested surgery months in the future so I could finish Good Omens first, but my doc convinced me the risk of waiting was too great. Get it done now.
"You're really healthy," my doc said. Despite an auto-immune issue which plagues me, I am way healthier than the average schmoe of late middle age. She informed me I would not even need any chemo or radiation if I took care of this now.

So I canceled my appearance at San Diego Comic Con. I did not inform the Good Omens team of my issues right away, thinking this would not interfere with my work schedule, but I did contact my agent to inform her of the issue. I also contacted a lawyer to rewrite my will and make sure the team had access to my digital files in case there were complications.
Then I got back to work, and hoped for the best.
Eff this guy.
Before I could even plant my carcass on the surgery table, I got a massive case of ocular shingles.
I didn't even know there was such a thing.
There I was, minding my own business. I go to bed one night with a scratchy eye, and by 4 PM the next day, I was in the emergency room being told if I didn't get immediate specialist treatment, I was in big trouble.
I got transferred to another hospital and got all the scary details, with the extra horrid news that I could not possibly have cancer surgery until I was free of shingles, and if I did not follow a rather brutal treatment procedure - which meant super-painful eye drops every half hour, twenty-four hours a day and daily hospital treatment - I could lose the eye entirely, or be blinded, or best case scenario, get permanent eye damage.
What was even funnier (yeah, hilarity) is the drops are so toxic if you don't use the medication just right, you can go blind anyway.
Hi Ho.
Ulcer is on the right. That big green blob.
I had just finished telling my cancer surgeon I did not even really care about getting cancer, was happy it was just stage zero, had no issues with scarring, wanted no reconstruction, all I cared about was my work.
Just cut it out and get me back to work.
And now I wondered if I was going to lose my ability to work anyway.
Shingles often accompanies cancer because of the stress on the immune system, and yeah, it's not pretty. This is me looking like all heck after I started to get better.

The first couple of weeks were pretty demoralizing as I expected a straight trajectory to wellness. But it was up and down all the way.
Some days I could not see out of either eye at all. The swelling was so bad that I had to reach around to my good eye to prop the lid open. Light sensitivity made seeing out of either eye almost impossible. Outdoors, even with sunglasses, I had to be led around by the hand.
I had an amazing doctor. I meticulously followed his instructions, and I think he was surprised I did. The treatment is really difficult, and if you don't do it just right no matter how painful it gets, you will be sorry.
To my amazement, after about a month, my doctor informed me I had no vision loss in the eye at all. "This never happens," he said.
I'd spent a couple of weeks there trying to learn to draw in the near-dark with one eye, and in the end, I got all my sight back.
I could no longer wear contact lenses (I don't really wear them anyway, unless I'm going to the movies,) would need hard core sun protection for awhile, and the neuralgia and sun sensitivity were likely to linger. But I could get back to work.
I have never been more grateful in my life.
Neuralgia sucks, by the way, I'm still dealing with it months later.
Anyway, I decided to finally go ahead and tell the Good Omens team what was going on, especially since this was all happening around the time the Kickstarter was gearing up.
Now that I was sure I'd passed the eye peril, and my surgery for Stage 0 was going to be no big deal, I figured all was a go. I was still pretty uncomfortable and weak, and my ideal deadline was blown, but with the book not coming out for more than a year, all would be OK. I quit a bunch of jobs I had lined up to start after Good Omens, since the project was going to run far longer than I'd planned.
Everybody on the team was super-nice, and I was pretty optimistic at this time. But work was going pretty slow during, as you may imagine.
But again...lots of lead time still left, go me.
Then I finally got my surgery.
Which was not as happy an experience as I had been hoping for.
My family said the doc came out of the operating room looking like she'd been pulled backwards through a pipe, She informed them the tumor which looked tiny on the scan was "...huge and her insides are a mess."
Which was super not fun news.
Eff this guy.

The tumor was hiding behind some dense tissue and cysts. After more tests, it was determined I'd need another surgery and was going to have to get further treatments after all.
The biopsy had been really painful, but the discomfort was gone after about a week, so no biggee. The second surgery was, weirdly, not as painful as the biopsy, but the fatigue was big time.
By then, the Good Omens Kickstarter had about run its course, and the record-breaker was both gratifying and a source of immense social pressure.
I'd already turned most of my social media over to an assistant, and I'm glad I did.
But the next surgery was what really kicked me on my keister.

All in all, they took out an area the size of a baseball. It was hard to move and wiped me out for weeks and weeks. I could not take care of myself. I'd begun losing hair by this time anyway, and finally just lopped it off since it was too heavy for me to care for myself. The cut hides the bald spots pretty well.
After about a month, I got the go-ahead to travel to my show at the San Diego Comic Con Museum (which is running until the first week of April, BTW). I was very happy I had enough energy to do it. But as soon as I got back, I had to return to treatment.
Since I live way out in the country, going into the city to various hospitals and pharmacies was a real challenge. I made more than 100 trips last year, and a drive to the compounding pharmacy which produced the specialist eye medicine I could not get anywhere else was six hours alone.
Naturally, I wasn't getting anything done during this time.
But at least my main hospital is super swank.


The oncology treatment went smoothly, until it didn't. The feels don't hit you until the end. By then I was flattened.
So flattened that I was too weak to control myself, fell over, and smashed my face into some equipment.

Nearly tore off my damn nostril.
Eff this guy.

Anyway, it was a bad year.
Here's what went right.
I have a good health insurance policy. The final tally on my health care costs ended up being about $150,000. I paid about 18% of that, including insurance. I had a high deductible and some experimental medicine insurance didn't cover. I had savings, enough to cover the months I wasn't working, and my Patreon is also very supportive. So you didn't see me running a Gofundme or anything.
Thanks to everyone who ever bought one of my books.
No, none of that money was Good Omens Kickstarter money. I won't get most of my pay on that for months, which is just as well because it kept my taxes lower last year when I needed a break.
So, yay.
My nose is nearly healed. I opted out of plastic surgery, and it just sealed up by itself. I'll never be ready for my closeup, but who the hell cares.
I got to ring the bell.

I had a very, VERY hard time getting back to work, especially with regard to focus and concentration. My work hours dropped by over 2/3. I was so fractured and weak, time kept slipping away while I sat in the studio like a zombie. Most of the last six months were a wash.
I assumed focus issues were due (in part) to stress, so sought counseling. This seemed like a good idea at first, but when the counselor asked me to detail my issues with anxiety, I spent two weeks doing just that and getting way more anxious, which was not helpful.
After that I went EFF THIS NOISE, I want practical tools, not touchy feelies (no judgment on people who need touchy-feelies, I need a pragmatic solution and I need it now,) so tried using the body doubling focus group technique for concentration and deep work.
Within two weeks, I returned to normal work hours.
I got rural broadband, jumping me from dial up speed to 1 GB per second.
It's a miracle.

Massive doses of Vitamin D3 and K2. Yay.
The new computer works great.
The Kickstarter did so well, we got to expand the graphic novel to 200 pages. Double yay.
I'm running late, but everyone on the Good Omens team is super supportive. I don't know if I am going to make the book late or not, but if I do, well, it surely wasn't on purpose, and it won't be super late anyway. I still have months of lead time left.
I used to be something of a social media addict, but now I hardly ever even look at it, haven't been directly on some sites in over a year, and no longer miss it. It used to seem important and now doesn't.
More time for real life.
While I think the last year aged me about twenty years, I actually like me better with short hair. I'm keeping it.

OK. Rough year.
Not complainin', just sayin'.
Back to work on The Book.
And only a day left to vote for Good Omens, Neil Gaiman, and Sandman in the Comicscene Awards. Thanks.
2K notes
·
View notes
Text
Discover the leading claims management software for healthcare in 2024. This article highlights the best tools for streamlining claims processing, reducing errors, and improving overall operational efficiency in healthcare.
#healthcare claims management software#top claims software 2024#healthcare IT solutions#medical claims processing tools.
0 notes
Text
From Reactive to Proactive: How a Claims Management System Can Help You Settle Claims Faster
Policyholders value efficient claims settlements over everything else. To ensure a smooth and speedy claim settlement process, insurers must deploy a modern claims management system. Read the full blog here:
#insurance technology#insurance software#insurance solutions#claims management system#claims processing software
0 notes
Text
I went down the internet rabbit hole trying to figure out wtf vegan cheese is made of and I found articles like this one speaking praises of new food tech startups creating vegan alternatives to cheese that Actually work like cheese in cooking so I was like huh that's neat and I looked up more stuff about 'precision fermentation' and. This is not good.
Basically these new biotech companies are pressuring governments to let them build a ton of new factories and pushing for governments to pay for them or to provide tax breaks and subsidies, and the factories are gonna cost hundreds of millions of dollars and require energy sources. Like, these things will have to be expensive and HUGE
I feel like I've just uncovered the tip of the "lab grown meat" iceberg. There are a bajillion of these companies (the one mentioned in the first article a $750 MILLION tech startup) that are trying to create "animal-free" animal products using biotech and want to build large factories to do it on a large scale
I'm trying to use google to find out about the energy requirements of such facilities and everything is really vague and hand-wavey about it like this article that's like "weeeeeell electricity can be produced using renewables" but it does take a lot of electricity, sugars, and human labor. Most of the claims about its sustainability appear to assume that we switch over to renewable electricity sources and/or use processes that don't fully exist yet.
I finally tracked down the source of some of the more radical claims about precision fermentation, and it comes from a think tank RethinkX that released a report claiming that the livestock industry will collapse by 2030, and be replaced by a system they're calling...
Food-as-Software, in which individual molecules engineered by scientists are uploaded to databases – molecular cookbooks that food engineers anywhere in the world can use to design products in the same way that software developers design apps.
I'm finding it hard to be excited about this for some odd reason
Where's the evidence for lower environmental impacts. That's literally what we're here for.
There will be an increase in the amount of electricity used in the new food system as the production facilities that underpin it rely on electricity to operate.
well that doesn't sound good.
This will, however, be offset by reductions in energy use elsewhere along the value chain. For example, since modern meat and dairy products will be produced in a sterile environment where the risk of contamination by pathogens is low, the need for refrigeration in storage and retail will decrease significantly.
Oh, so it will be better for the Earth because...we won't need to refrigerate. ????????
Oh Lord Jesus give me some numerical values.
Modern foods will be about 10 times more efficient than a cow at converting feed into end products because a cow needs energy via feed to maintain and build its body over time. Less feed consumed means less land required to grow it, which means less water is used and less waste is produced. The savings are dramatic – more than 10-25 times less feedstock, 10 times less water, five times less energy and 100 times less land.
There is nothing else in this report that I can find that provides evidence for a lower carbon footprint. Supposedly, an egg white protein produced through a similar process has been found to reduce environmental impacts, but mostly everything seems very speculative.
And crucially none of these estimations are taking into account the enormous cost and resource investment of constructing large factories that use this technology in the first place (existing use is mostly for pharmaceutical purposes)
It seems like there are more tech startups attempting to use this technology to create food than individual scientific papers investigating whether it's a good idea. Seriously, Google Scholar and JSTOR have almost nothing. The tech of the sort that RethinkX is describing barely exists.
Apparently Liberation Labs is planning to build the first large-scale precision fermentation facility in Richmond, Indiana come 2024 because of the presence of "a workforce experienced in manufacturing"
And I just looked up Richmond, Indiana and apparently, as of RIGHT NOW, the town is in the aftermath of a huge fire at a plastics recycling plant and is full of toxic debris containing asbestos and the air is full of toxic VOCs and hydrogen cyanide. ???????????? So that's how having a robust industrial sector is working out for them so far.
5K notes
·
View notes