#caydance
Explore tagged Tumblr posts
Text

Hawks bnha season 7 cosplay
Picture by kyo_cosplay_photography 🛐🩷🫶🏽
Assistant/Supportby @varukaart 🩷
Hawks is caydance
Original artwork by god of Bokunoheroacademia Horikoshi
#dokomi #dokomi24 #hawks #cosplay #hawkscosplay #hawksbnha #hawksmha #mha #bnha #myheroacademia #bokunoheroacademia #düsseldorf #messedüsseldorf #dokomidüsseldorf #dokomi2024 #mhaseason7 #hawksbnha
#cosplay#cosplayer#caydance#mha#hawks#bnha#bokunoheroacademia#hawks cosplay#mha cosplay#myheroacademiacosplay#dokomi#dokomi 2024#kohei horikoshi#hawks bnha#hawks bnha cosplay#hawks boku no hero academia#season 7#bnha season 7
282 notes
·
View notes
Text
Wait do we remember d*caydance wl competition. What was that fic called. I need to fully regress
0 notes
Text

ID: discord messages between fall (frog meister), clem (tapewormussy) and caydence (cayDANCE).
fall says: question, which is superior in tic tac toe, X or O? clem says: O caydence says: X fall says: X because there's no X in loser. however there IS an X in sex. i rest my case
later, fall quotes a message from caydence that says "fall you're too horny." fall responds with: strong words coming from someone with arctic monkeys lyrics in their profile.
End ID.
5 notes
·
View notes
Text
the beat + the caydance....hard.
https://youtu.be/Bxpa1DWNmPI
1 note
·
View note
Photo

Female Luffy - Caydance(Caydance) Monkey D. Luffy Cosplay Photo https://www.wig-supplier.com/
4 notes
·
View notes
Text
My Gayle
Gayle. I have to start this blog out by giving you all of my love. God said that if we love our wives like Christ loved the church then everything else in our lives will fall in to place. You are my best friend, my helper and my Queen. To everyone else you are Crystal....but to me you will always be my sweet Gayle.
I knew from the first time I saw you that you were very special. That I would pursue you. That you were an incredible woman! I remember how excited I was to go to Orlando during pre-season and steal a picture with you. I even brought my Dad to this game. I was pretty nervous to talk to you, because this was the first time any of your friends got to see me as well.

Shana Mitchell is the one that made everything happen between us....going to Rainbow River on our first date, bbq’s at their house, and the best House Of Blues weekend with you where I KNEW you were the woman for me!

Remember going to Momma’s and having so much fun. We had a BLAST that day, even cutting up with Kelsie in the Kitchen and heading to the beach!

What stole my heart for good was how sweet you were to the kiddos. Taking our first trip to Blairsville together and having picnics at Vogal Park.

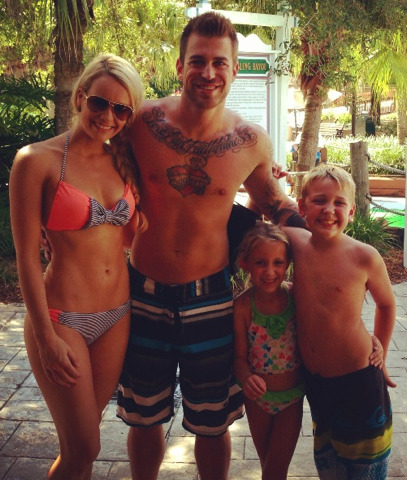
No one can deny how much this little girl looks up to you and especially how much she loves you!

I knew I knew I knew I had to make you my wife. So.....with your Daddy’s permission, I asked you for forever. You sad yes!!!!!!!!

The way we love each other can not possibly be expressed in words!



And there is the day we became one.....forever started this day
September 6th, 2015

We were now a family of four, but we both knew that we wanted more. There is nothing more amazing then experiencing making brand new life. You were born to be a Mom! So we tried for several months, praying that God would provide. Then we got the amazing news.....God always comes through!


We couldnt wait to find out what we were having. Boy or girl? Pink or blue? You got your little girl!!!!! (even though now we know she is a daddy’s girl)
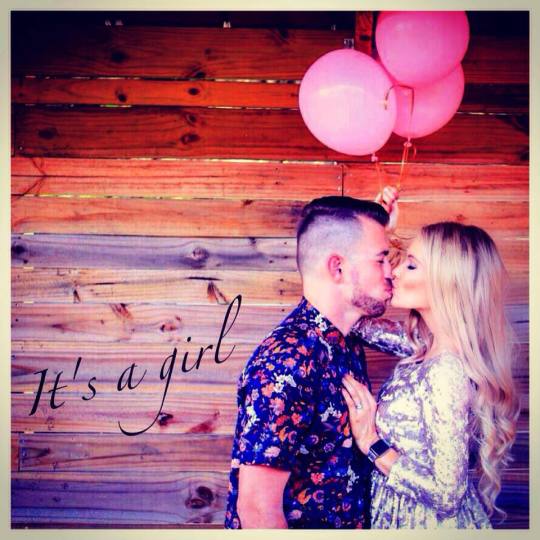
I swear that you are the most beautiful woman I have ever seen in my life. You glowed while pregnant and shined as bright as the sun!

Mommy is a dancer and daddy is a singer.....that’s how we picked the name “Caydance”
ca·denceˈkādns/
noun
noun:
cadence
; plural noun:
cadences
1.a modulation or inflection of the voice."the measured cadences that he employed in the Senate"synonyms:intonation, modulation, lilt, accent, inflection; More
2.MUSICa sequence of notes or chords comprising the close of a musical phrase."the final cadences of the Prelude"
a modulation in reading aloud as implied by the structure and ordering of words and phrases in written text."the dry cadences of the essay"
a fall in pitch of the voice at the end of a phrase or sentence.
rhythm."the thumping cadence of the engines"

Then suddenly on January 20th, 2017. Our family of four became an incredible family of five. So full of love and joy! What an amazing day!

Welcoming our sweet Caydance Grace Brown in to this world!

My precious Gayle....
You are such an incredible woman. You truly do inspire me everyday. You make me a better man, always pushing me to succeed. I will always give you all and intensely love and cherish you. Our family is complete and this life is only just starting for us! Always remember that you are my world, always remember that I will always give you ALL of my love!
Love...your husband,
Cliff (otherwise known as daddy)
1/21/2017
2 notes
·
View notes
Text
A Switch To Medicaid Managed Care Worries Some Illinois Foster Families
Rebecca and Bruce Austin in central Illinois have six kids — ranging in age from 4 to 22.
Five kids still live at home, and all of them came to the Austins through the foster care system. All told, they see 14 doctors.
Many states promise to provide health care to help foster and adoptive families keep kids healthy, but recently in Illinois, thousands of children temporarily lost coverage when the state switched their health plans. Some of Rebecca and Bruce’s children got caught in the coverage gap, which has the Austins wondering whether the state will fulfill its end of the bargain.
Three of the Austins’ children see psychiatrists. One has regular visits with specialists for epilepsy and other health conditions. Another has therapy four times a week for movement and speech delays.
“A typical day is pretty crazy,” Rebecca Austin said in an interview before the coronavirus shelter-in-place orders were issued. “I say I’m a stay-at-home mom, but with all the doctors’ appointments and therapies and appointments and stuff, I’m on the go all the time.”
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
Sign Up
Please confirm your email address below:
Sign Up
Their lives are full and busy already, and Austin is concerned Illinois’ health plan change will make juggling health care even more of a challenge.
The Austins live in Windsor, a rural town about 25 miles from the nearest hospital in Charleston, Illinois.
Since February, the state has been moving all current and former foster children covered by Medicaid into health plans provided by private insurers that contract with the state.
It’s a change to what’s known as Medicaid managed care. The shift has many families like the Austins concerned, because the initial phase of the rollout was rocky and because it’s not clear whether familiar, nearby health care providers will be designated as in-network.
More States Move To Managed Care
Most states already use managed-care companies to run their Medicaid health plans, which means state agencies pay insurance companies to provide health care to people in the Medicaid program.
More From The Midwest Bureau
View More
Proponents of the managed-care model say it can lower costs while increasing access to care.
States that switch to managed care often find their budgets become more predictable, because they no longer pay providers for each service. Instead, they pay insurers a set amount per enrollee for all health care needs.
But Michael Sparer, a health policy professor at Columbia University in New York City, said evidence is both limited and mixed as to whether managed care lowers costs and increases access to care. Success depends on whether states hold insurers to their promises to maintain an adequate provider network, he said.
“Network adequacy refers to a health plan’s ability to deliver the benefits promised by providing reasonable access to enough in-network primary care and specialty physicians, and all health care services included under the terms of the contract,” according to the National Association of Insurance Commissioners.
Sparer said success with Medicaid managed care also hinges on whether states “have the ability and have the oversight that’s required to make sure that the program works effectively.”
In recent years, Illinois switched most of the state’s Medicaid enrollees into managed care. Former foster children moved onto those plans on Feb. 1, and current foster children are set to eventually join them. The switch was initially planned for April 1, but the state has postponed the move for at least 30 days, citing the COVID-19 pandemic.
Some child advocates question whether the move is in the children’s best interests.
Many foster children have serious physical and mental health needs, and the switch could disrupt long-standing relationships with therapists and other providers, critics of managed care argue.
For thousands of families like the Austins, this means figuring out whether their children’s providers will still be in-network or whether they’ll have to use new doctors, who might be farther from home.
Austin said her family found a managed-care plan that allowed them to keep most of their children’s providers. But when the February switch was finalized, the Austin children were among the 2,500 former foster kids whose health coverage was interrupted.
Camdyn and Caydance Austin play in Camdyn’s bedroom at home in Windsor, Illinois.(Christine Herman/Illinois Public Media)
The “end date” for her kids’ coverage had been incorrectly listed in the computer system as Jan. 31 — one day prior to the coverage start date, Feb. 1, Rebecca said. This effectively left them without insurance. State officials blamed a glitch in the system for the error.
John Hoffman, a spokesman for the Illinois Department of Healthcare and Family Services, said in a statement that the agency worked with managed-care organizations “immediately to correct the error, resolving it within days.”
For the Austins, the error meant they had to cancel appointments and had problems getting prescriptions filled.
“My daughter who has epilepsy, her medicine was … a little over $1,000,” Austin said. “I didn’t have $1,045 to pay her for the medicine and, so, we were in a panic as to what to do because she had to have the medicine.”
Phone calls to pharmacies and insurers were onerous, she said, but she ultimately resolved the issue. Still, the Austins’ youngest, 4-year-old Camdyn, missed two weeks of therapy sessions, while they waited for the new insurer to approve them. Austin worries these delays will slow his progress.
Making Medicaid Managed Care Work
Heidi Dalenberg is an attorney with the ACLU of Illinois, which serves as a watchdog for the state’s child welfare agency. She said managed care can be beneficial, helping ensure all kids get regular well-checks and prevent doctors from overtreating or overmedicating children.
But those benefits will be realized only if the state has prepared for the transition and holds insurance companies to their contract requirements, she said. That includes ensuring managed-care organizations, or MCOs, have appropriate provider networks so children have access to doctors close to home.
“When it doesn’t work is when you have an MCO that is more worried about cutting costs and denying approvals for care than they are in making sure that kids get what they need,” Dalenberg said.
A retired federal judge is monitoring Illinois’ efforts to ensure foster children don’t lose access to care in the switch to Medicaid managed care, Dalenberg said.
Hoffman, the state DHS spokesman, said the switch to managed care, provided by the insurer YouthCare Illinois, will help improve health care for current and former foster children by coordinating and providing services.
“Right now, when a family needs a provider for their child, they’re left to navigate a complex system alone,” Hoffman said in a statement. “With YouthCare, families have a personal care coordinator who helps manage their overall care, researches providers and schedules appointments.”
He said the problems caused by February’s glitch have been resolved and will not resurface when 17,000 current foster children eventually get switched into managed-care plans as well.
The Austins’ foster daughter will be among them. And Austin worries her daughter will be forced to switch to a therapist an hour’s drive away, since the one she sees nearby is not in the managed-care network.
“She has established a relationship with that counselor. She’s been going there for almost two years and now we have to start all over again,” Austin said. “And that’s trauma. That’s a huge trauma.”
Illinois said even providers that are not in-network when the switch goes into effect can be paid for services during a six-month “continuity of care” period, and insurers will try to expand their networks during that time.
The Austins are trying to be optimistic, but the state’s track record doesn’t give them much assurance.
This story is part of a partnership that includes Side Effects Public Media, Illinois Public Media, NPR and Kaiser Health News.
A Switch To Medicaid Managed Care Worries Some Illinois Foster Families published first on https://smartdrinkingweb.weebly.com/
0 notes
Text
A Switch To Medicaid Managed Care Worries Some Illinois Foster Families
Rebecca and Bruce Austin in central Illinois have six kids — ranging in age from 4 to 22.
Five kids still live at home, and all of them came to the Austins through the foster care system. All told, they see 14 doctors.
Many states promise to provide health care to help foster and adoptive families keep kids healthy, but recently in Illinois, thousands of children temporarily lost coverage when the state switched their health plans. Some of Rebecca and Bruce’s children got caught in the coverage gap, which has the Austins wondering whether the state will fulfill its end of the bargain.
Three of the Austins’ children see psychiatrists. One has regular visits with specialists for epilepsy and other health conditions. Another has therapy four times a week for movement and speech delays.
“A typical day is pretty crazy,” Rebecca Austin said in an interview before the coronavirus shelter-in-place orders were issued. “I say I’m a stay-at-home mom, but with all the doctors’ appointments and therapies and appointments and stuff, I’m on the go all the time.”
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
Sign Up
Please confirm your email address below:
Sign Up
Their lives are full and busy already, and Austin is concerned Illinois’ health plan change will make juggling health care even more of a challenge.
The Austins live in Windsor, a rural town about 25 miles from the nearest hospital in Charleston, Illinois.
Since February, the state has been moving all current and former foster children covered by Medicaid into health plans provided by private insurers that contract with the state.
It’s a change to what’s known as Medicaid managed care. The shift has many families like the Austins concerned, because the initial phase of the rollout was rocky and because it’s not clear whether familiar, nearby health care providers will be designated as in-network.
More States Move To Managed Care
Most states already use managed-care companies to run their Medicaid health plans, which means state agencies pay insurance companies to provide health care to people in the Medicaid program.
More From The Midwest Bureau
View More
Proponents of the managed-care model say it can lower costs while increasing access to care.
States that switch to managed care often find their budgets become more predictable, because they no longer pay providers for each service. Instead, they pay insurers a set amount per enrollee for all health care needs.
But Michael Sparer, a health policy professor at Columbia University in New York City, said evidence is both limited and mixed as to whether managed care lowers costs and increases access to care. Success depends on whether states hold insurers to their promises to maintain an adequate provider network, he said.
“Network adequacy refers to a health plan’s ability to deliver the benefits promised by providing reasonable access to enough in-network primary care and specialty physicians, and all health care services included under the terms of the contract,” according to the National Association of Insurance Commissioners.
Sparer said success with Medicaid managed care also hinges on whether states “have the ability and have the oversight that’s required to make sure that the program works effectively.”
In recent years, Illinois switched most of the state’s Medicaid enrollees into managed care. Former foster children moved onto those plans on Feb. 1, and current foster children are set to eventually join them. The switch was initially planned for April 1, but the state has postponed the move for at least 30 days, citing the COVID-19 pandemic.
Some child advocates question whether the move is in the children’s best interests.
Many foster children have serious physical and mental health needs, and the switch could disrupt long-standing relationships with therapists and other providers, critics of managed care argue.
For thousands of families like the Austins, this means figuring out whether their children’s providers will still be in-network or whether they’ll have to use new doctors, who might be farther from home.
Austin said her family found a managed-care plan that allowed them to keep most of their children’s providers. But when the February switch was finalized, the Austin children were among the 2,500 former foster kids whose health coverage was interrupted.
Camdyn and Caydance Austin play in Camdyn’s bedroom at home in Windsor, Illinois.(Christine Herman/Illinois Public Media)
The “end date” for her kids’ coverage had been incorrectly listed in the computer system as Jan. 31 — one day prior to the coverage start date, Feb. 1, Rebecca said. This effectively left them without insurance. State officials blamed a glitch in the system for the error.
John Hoffman, a spokesman for the Illinois Department of Healthcare and Family Services, said in a statement that the agency worked with managed-care organizations “immediately to correct the error, resolving it within days.”
For the Austins, the error meant they had to cancel appointments and had problems getting prescriptions filled.
“My daughter who has epilepsy, her medicine was … a little over $1,000,” Austin said. “I didn’t have $1,045 to pay her for the medicine and, so, we were in a panic as to what to do because she had to have the medicine.”
Phone calls to pharmacies and insurers were onerous, she said, but she ultimately resolved the issue. Still, the Austins’ youngest, 4-year-old Camdyn, missed two weeks of therapy sessions, while they waited for the new insurer to approve them. Austin worries these delays will slow his progress.
Making Medicaid Managed Care Work
Heidi Dalenberg is an attorney with the ACLU of Illinois, which serves as a watchdog for the state’s child welfare agency. She said managed care can be beneficial, helping ensure all kids get regular well-checks and prevent doctors from overtreating or overmedicating children.
But those benefits will be realized only if the state has prepared for the transition and holds insurance companies to their contract requirements, she said. That includes ensuring managed-care organizations, or MCOs, have appropriate provider networks so children have access to doctors close to home.
“When it doesn’t work is when you have an MCO that is more worried about cutting costs and denying approvals for care than they are in making sure that kids get what they need,” Dalenberg said.
A retired federal judge is monitoring Illinois’ efforts to ensure foster children don’t lose access to care in the switch to Medicaid managed care, Dalenberg said.
Hoffman, the state DHS spokesman, said the switch to managed care, provided by the insurer YouthCare Illinois, will help improve health care for current and former foster children by coordinating and providing services.
“Right now, when a family needs a provider for their child, they’re left to navigate a complex system alone,” Hoffman said in a statement. “With YouthCare, families have a personal care coordinator who helps manage their overall care, researches providers and schedules appointments.”
He said the problems caused by February’s glitch have been resolved and will not resurface when 17,000 current foster children eventually get switched into managed-care plans as well.
The Austins’ foster daughter will be among them. And Austin worries her daughter will be forced to switch to a therapist an hour’s drive away, since the one she sees nearby is not in the managed-care network.
“She has established a relationship with that counselor. She’s been going there for almost two years and now we have to start all over again,” Austin said. “And that’s trauma. That’s a huge trauma.”
Illinois said even providers that are not in-network when the switch goes into effect can be paid for services during a six-month “continuity of care” period, and insurers will try to expand their networks during that time.
The Austins are trying to be optimistic, but the state’s track record doesn’t give them much assurance.
This story is part of a partnership that includes Side Effects Public Media, Illinois Public Media, NPR and Kaiser Health News.
A Switch To Medicaid Managed Care Worries Some Illinois Foster Families published first on https://nootropicspowdersupplier.tumblr.com/
0 notes
Text

The Sky ~
Hawks Bnha mha Cosplay my Hero Academia
Picture by Shattered light photography
Hawks is Caydance
#cosplay#caydance#mha#hawks#bnha#bokunoheroacademia#hawks cosplay#mha cosplay#myheroacademiacosplay#cosplayer#bnha keigo#keigo tamaki#hawks bnha cosplay
90 notes
·
View notes
Text
A Switch To Medicaid Managed Care Worries Some Illinois Foster Families
Rebecca and Bruce Austin in central Illinois have six kids — ranging in age from 4 to 22.
Five kids still live at home, and all of them came to the Austins through the foster care system. All told, they see 14 doctors.
Many states promise to provide health care to help foster and adoptive families keep kids healthy, but recently in Illinois, thousands of children temporarily lost coverage when the state switched their health plans. Some of Rebecca and Bruce’s children got caught in the coverage gap, which has the Austins wondering whether the state will fulfill its end of the bargain.
Three of the Austins’ children see psychiatrists. One has regular visits with specialists for epilepsy and other health conditions. Another has therapy four times a week for movement and speech delays.
“A typical day is pretty crazy,” Rebecca Austin said in an interview before the coronavirus shelter-in-place orders were issued. “I say I’m a stay-at-home mom, but with all the doctors’ appointments and therapies and appointments and stuff, I’m on the go all the time.”
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
Sign Up
Please confirm your email address below:
Sign Up
Their lives are full and busy already, and Austin is concerned Illinois’ health plan change will make juggling health care even more of a challenge.
The Austins live in Windsor, a rural town about 25 miles from the nearest hospital in Charleston, Illinois.
Since February, the state has been moving all current and former foster children covered by Medicaid into health plans provided by private insurers that contract with the state.
It’s a change to what’s known as Medicaid managed care. The shift has many families like the Austins concerned, because the initial phase of the rollout was rocky and because it’s not clear whether familiar, nearby health care providers will be designated as in-network.
More States Move To Managed Care
Most states already use managed-care companies to run their Medicaid health plans, which means state agencies pay insurance companies to provide health care to people in the Medicaid program.
More From The Midwest Bureau
View More
Proponents of the managed-care model say it can lower costs while increasing access to care.
States that switch to managed care often find their budgets become more predictable, because they no longer pay providers for each service. Instead, they pay insurers a set amount per enrollee for all health care needs.
But Michael Sparer, a health policy professor at Columbia University in New York City, said evidence is both limited and mixed as to whether managed care lowers costs and increases access to care. Success depends on whether states hold insurers to their promises to maintain an adequate provider network, he said.
“Network adequacy refers to a health plan’s ability to deliver the benefits promised by providing reasonable access to enough in-network primary care and specialty physicians, and all health care services included under the terms of the contract,” according to the National Association of Insurance Commissioners.
Sparer said success with Medicaid managed care also hinges on whether states “have the ability and have the oversight that’s required to make sure that the program works effectively.”
In recent years, Illinois switched most of the state’s Medicaid enrollees into managed care. Former foster children moved onto those plans on Feb. 1, and current foster children are set to eventually join them. The switch was initially planned for April 1, but the state has postponed the move for at least 30 days, citing the COVID-19 pandemic.
Some child advocates question whether the move is in the children’s best interests.
Many foster children have serious physical and mental health needs, and the switch could disrupt long-standing relationships with therapists and other providers, critics of managed care argue.
For thousands of families like the Austins, this means figuring out whether their children’s providers will still be in-network or whether they’ll have to use new doctors, who might be farther from home.
Austin said her family found a managed-care plan that allowed them to keep most of their children’s providers. But when the February switch was finalized, the Austin children were among the 2,500 former foster kids whose health coverage was interrupted.
Camdyn and Caydance Austin play in Camdyn’s bedroom at home in Windsor, Illinois.(Christine Herman/Illinois Public Media)
The “end date” for her kids’ coverage had been incorrectly listed in the computer system as Jan. 31 — one day prior to the coverage start date, Feb. 1, Rebecca said. This effectively left them without insurance. State officials blamed a glitch in the system for the error.
John Hoffman, a spokesman for the Illinois Department of Healthcare and Family Services, said in a statement that the agency worked with managed-care organizations “immediately to correct the error, resolving it within days.”
For the Austins, the error meant they had to cancel appointments and had problems getting prescriptions filled.
“My daughter who has epilepsy, her medicine was … a little over $1,000,” Austin said. “I didn’t have $1,045 to pay her for the medicine and, so, we were in a panic as to what to do because she had to have the medicine.”
Phone calls to pharmacies and insurers were onerous, she said, but she ultimately resolved the issue. Still, the Austins’ youngest, 4-year-old Camdyn, missed two weeks of therapy sessions, while they waited for the new insurer to approve them. Austin worries these delays will slow his progress.
Making Medicaid Managed Care Work
Heidi Dalenberg is an attorney with the ACLU of Illinois, which serves as a watchdog for the state’s child welfare agency. She said managed care can be beneficial, helping ensure all kids get regular well-checks and prevent doctors from overtreating or overmedicating children.
But those benefits will be realized only if the state has prepared for the transition and holds insurance companies to their contract requirements, she said. That includes ensuring managed-care organizations, or MCOs, have appropriate provider networks so children have access to doctors close to home.
“When it doesn’t work is when you have an MCO that is more worried about cutting costs and denying approvals for care than they are in making sure that kids get what they need,” Dalenberg said.
A retired federal judge is monitoring Illinois’ efforts to ensure foster children don’t lose access to care in the switch to Medicaid managed care, Dalenberg said.
Hoffman, the state DHS spokesman, said the switch to managed care, provided by the insurer YouthCare Illinois, will help improve health care for current and former foster children by coordinating and providing services.
“Right now, when a family needs a provider for their child, they’re left to navigate a complex system alone,” Hoffman said in a statement. “With YouthCare, families have a personal care coordinator who helps manage their overall care, researches providers and schedules appointments.”
He said the problems caused by February’s glitch have been resolved and will not resurface when 17,000 current foster children eventually get switched into managed-care plans as well.
The Austins’ foster daughter will be among them. And Austin worries her daughter will be forced to switch to a therapist an hour’s drive away, since the one she sees nearby is not in the managed-care network.
“She has established a relationship with that counselor. She’s been going there for almost two years and now we have to start all over again,” Austin said. “And that’s trauma. That’s a huge trauma.”
Illinois said even providers that are not in-network when the switch goes into effect can be paid for services during a six-month “continuity of care” period, and insurers will try to expand their networks during that time.
The Austins are trying to be optimistic, but the state’s track record doesn’t give them much assurance.
This story is part of a partnership that includes Side Effects Public Media, Illinois Public Media, NPR and Kaiser Health News.
from Updates By Dina https://khn.org/news/a-switch-to-medicaid-managed-care-worries-some-illinois-foster-families/
0 notes
Text
ID: discord messages between caydence (cayDANCE) and simon (radioactive cum). caydence asks "first of all, why are we talking about cum?" and simon replies "specifically radioactive cum. it's the stuff they put in glow sticks." End ID.
5 notes
·
View notes
Text

Hawks fumikage mha cosplay
Insta/
Tsukuyomi Fumikage Tokojami : xneiroxcosplayx
Picture: shattered_light_photography
Hawks: caydance_
#cosplay#cosplayer#caydance#mha#hawks#bnha#bokunoheroacademia#hawks cosplay#mha cosplay#myheroacademiacosplay
93 notes
·
View notes
Text

Hawks bnha mha
#cosplay#cosplayer#caydance#mha#hawks#bnha#bokunoheroacademia#hawks cosplay#mha cosplay#myheroacademiacosplay
85 notes
·
View notes
Text

Hawks bnha Cosplay mha
Hawks is caydance_
#cosplay#cosplayer#caydance#mha#hawks#bnha#bokunoheroacademia#hawks cosplay#mha cosplay#myheroacademiacosplay#mha takami keigo#keigo takami
91 notes
·
View notes
Text

Hawks Heroe
Mha
Picture shattered_light_photography
#cosplay#cosplayer#caydance#mha#hawks#bnha#bokunoheroacademia#hawks cosplay#myheroacademiacosplay#mha cosplay#keigo tamaki
69 notes
·
View notes