#bydureon
Explore tagged Tumblr posts
Text

Why Choose Mayfair Weight Loss Clinic?
We are a dedicated weight loss clinic with the most current information and access to the newest medical procedures. Run and supported by healthcare professionals with extensive experience managing weight reduction. We have prescribers, pharmacies, and a customer support team, allowing us to give you with best support on your weight reduction journey.
Visit Byetta Insulin Pen which will help you reach your weight loss goals. Enjoy the process as you go.
#byetta diabetes medication#byetta insulin pen#byetta pen injector#bydureon injection for diabetes#type 2 diabetes injection
0 notes
Text

Finding the Top Treatments for Type 2 Diabetes
-- FOLLOW US ON FACEBOOK FOR MORE ARTICLE'S LIKE THIS -- When considering non-insulin medications for managing type 2 diabetes, patients have a diverse array of options. This article explores these medications and the key factors to help determine which treatment may be the most suitable for you.
Non-Insulin Medications for Type 2 Diabetes
A variety of medication classes are prescribed for effectively treating type 2 diabetes:
Metformin
Metformin is typically the first-line medication recommended for type 2 diabetes unless contraindications exist. It is effective, safe, and cost-efficient, with additional benefits such as reducing the risk of cardiovascular events. Metformin helps in lowering hemoglobin A1C levels and can assist with weight management by decreasing the amount of glucose produced by the liver.
Sulfonylureas
Sulfonylureas include medications like glipizide, glyburide, and glimepiride. While generally inexpensive, these drugs can lead to hypoglycemia (low blood sugar) and may contribute to weight gain.
Insulin Sensitizers
Pioglitazone is in this category and is recognized for its efficacy without the risk of hypoglycemia. However, it does carry potential risks, including increased chance of cardiovascular disease and weight gain.
GLP-1 Receptor Agonists
This class includes medications such as exenatide (Byetta, Bydureon), liraglutide (Victoza, Saxenda), and dulaglutide (Trulicity). Some are administered via daily injection while others are given weekly. Semaglutides, like Ozempic, are also available as weekly injections, with an oral option (Rybelsus) taken daily. These medications can be beneficial for heart health and weight loss but may come with side effects like nausea and diarrhea.
Dipeptidyl Peptidase-4 Inhibitors (DPP-4 Inhibitors)
This category features drugs such as sitagliptin (Januvia), saxagliptin (Onglyza), and linagliptin (Tradjenta). These well-tolerated oral medications, taken once daily, provide a mild reduction in blood sugar levels, primarily decreasing post-meal glucose spikes.
Alpha-Glucosidase Inhibitors
Acarbose belongs to this group, although its use is infrequent due to common gastrointestinal side effects. It functions by inhibiting carbohydrate absorption in the intestines.
Sodium-Glucose Cotransporter-2 Inhibitors (SGLT-2 Inhibitors)
As the most recent addition to diabetes medications, SGLT-2 inhibitors work by expelling excess glucose through urine. There is increasing clinical evidence that these medications not only improve blood glucose control but also offer cardiovascular benefits and aid kidney function. Examples include empagliflozin (Jardiance), dapagliflozin (Farxiga), canagliflozin (Invokana), and ertugliflozin (Steglatro).
Factors Considered in Choosing a Treatment Plan
Recognizing that type 2 diabetes is a multifaceted chronic condition, effective management often requires a combination of risk-reduction strategies along with your specific blood sugar management goals. When devising a treatment plan, your healthcare provider will evaluate several critical factors:
History of Heart Disease: Any prior instances of heart attacks, strokes, or congestive heart failure.
Chronic Kidney Disease: Existing kidney issues can influence medication choice.
Risk of Hypoglycemia: The likelihood of low blood sugar when using various treatment options.
Potential Side Effects: Each medication has specific side effects that will be considered.
Weight Management: Your current weight and how medications may impact it.
Cost and Insurance Coverage: The financial aspect of medication is significant in the decision-making process.
Personal Preferences: Your willingness and ability to adhere to the proposed treatment plan.
Additionally, your A1C test results, which give insight into your average blood sugar levels over the prior three months, will also inform treatment decisions. Generally, the target A1C goal is under 7%, as per the guidelines set by the American Diabetes Association, but this may be tailored to your individual circumstances.
While Metformin is commonly the initial recommendation for type 2 diabetes management, numerous other effective medications exist, ensuring a tailored approach based on individual needs. It is crucial to maintain regular consultations with your healthcare provider to determine the ideal medication for you, alongside essential lifestyle changes, which play a vital role in managing type 2 diabetes effectively.
#bloodsugarcontrol#bloodsugar#bloodsugarlevel#CardiovascularHealth#chronickidneydisease#chronickidneydiseaseawareness#diabetesmanagement#diabetes#diabetesawareness#diabetescare#diabetic#DPP4#DPP4Inhibitors#GLP1#agonists#healthcare#insulinsensitizers#metformin#noninsulinmedications#SGLT2Inhibitors#SGLT2#SULFONYLUREAS#type2diabetes#weightmanagement
0 notes
Text
Understanding PCOS and GLP-1 Medications: A Path to Better Health
What is PCOS?
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder that affects individuals with ovaries, typically during their reproductive years. It is characterized by a range of symptoms that include:
• Irregular or absent menstrual cycles
• Elevated levels of androgens (male hormones), which may lead to symptoms like acne, excess hair growth (hirsutism), and male-pattern hair loss
• Polycystic ovaries, identified through ultrasound, where the ovaries appear enlarged and contain multiple small follicles
PCOS can also be associated with metabolic issues, including insulin resistance, weight gain, and an increased risk of type 2 diabetes and cardiovascular disease. For many, managing weight and improving insulin sensitivity are critical aspects of controlling PCOS symptoms.
What is a GLP-1 Medication?
Glucagon-Like Peptide-1 (GLP-1) receptor agonists are a class of medications originally developed to treat type 2 diabetes. These medications mimic the effects of the natural GLP-1 hormone, which is released in the gut in response to eating. GLP-1 helps regulate blood sugar levels, appetite, and digestion.
Some common GLP-1 medications include:
• Semaglutide (sold under brand names like Ozempic, Wegovy, and Rybelsus)
• Liraglutide (Victoza, Saxenda)
• Dulaglutide (Trulicity)
• Exenatide (Byetta, Bydureon)
These medications work by:
1. Slowing gastric emptying, which increases feelings of fullness and helps with appetite control
2. Enhancing insulin secretion in response to meals
3. Reducing the liver’s glucose production
While they are approved for type 2 diabetes, certain GLP-1 medications, such as Saxenda and Wegovy, are also approved for weight management in people with obesity or weight-related conditions.
Final Thoughts
PCOS is a complex condition that affects many aspects of physical and emotional health. GLP-1 medications offer a promising option for women struggling with weight and metabolic issues associated with PCOS. If you think a GLP-1 medication might help you, consult your healthcare provider to determine if it’s the right choice for your individual needs.
By combining the right treatments with a supportive healthcare team, managing PCOS is possible—and it can lead to a healthier, more fulfilling life.
0 notes
Text
Glucagon-like peptide-1 (GLP-1) is a hormone that regulates blood sugar levels. But sometimes, especially if you have diabetes, your body needs some extra help from the GLP-1 hormone. This is where natural alternatives to GLP-1 come in. They act like a sidekick, supporting your body's natural rhythms and helping to keep blood sugar levels normal. While much of the science continues to develop, let’s explore natural GLP-1 agonists and how they can complement your health journey. Does natural GLP-1 exist? The answer is not simply "yes" or "no." Some foods may make you feel fuller longer and slow digestion (like GLP-1 drugs), but they don't necessarily result in the same rapid weight loss. GLP-1 is a hormone produced naturally in the body. Intestinal cells secrete it to regulate blood sugar levels. GLP-1 tells the body to produce insulin, which tells cells to absorb sugar and produce energy. Also Slows digestionIt reduces hunger, promotes metabolic health and aids in weight loss. It directs the blood sugar orchestra and keeps it in harmony. The body is natural Adequate GLP-1 This is to keep your blood sugar in check, but if you have diabetes or insulin resistance, that may not be enough. Diabetes A condition in which blood sugar levels rise because the body can't produce or properly use insulin, which cells need to absorb sugar for energy. Insulin resistance It occurs when cells don't respond well to insulin. Without insulin, cells can't absorb sugar, leading to hyperglycemia. Therefore GLP-1 receptor agonists When taken into the body, they mimic the natural GLP-1 hormone and act as enhancers, increasing GLP-1 levels in the body and controlling blood sugar levels. They stimulate insulin release and promote insulin sensitivity. This allows your cells to absorb glucose, lowering your blood sugar levels, making you feel fuller for longer and suppressing your appetite. Several GLP-1 agonists The following medicines are available: Exenatide (Vietta, Bydureon) Liraglutide (Victoza, Saxenda) Dulaglutide (Trulicity) Weight loss drugs Semaglutide (Wegovi However, if GLP-1 medications don't suit you, you can consider incorporating certain foods into your diet that act as natural GLP-1 agonists and help control blood sugar levels. According to Stephanie Nelson, a registered dietitian at MyFitnessPal, "While dietary changes won't have the same effect as GLP-1 drugs, they will make you feel fuller for longer and slow down your digestion. And we're still learning a lot, so we'll know more as time goes on." Whatever the outcome of future research on natural GLP-1 agonists, simple changes to your diet and lifestyle could make a big difference in your overall health in the long run. So let’s take a look at some natural ingredients that can boost your GLP-1 levels. Top 5 Foods and Supplements to Increase GLP-1 Naturally Here are some natural GLP-1 agonists that can give your body that extra support to improve blood sugar control. 1. Eggs and a protein-rich breakfast Recent Research Consuming foods rich in protein and calcium for breakfast has been shown to promote the release of GLP-1 and aid in weight loss. Research into the potential link between protein-rich foods and GLP-1 release is ongoing, but the evidence is still limited. Still, adding protein to your breakfast has plenty of health benefits, so whether you naturally promote GLP-1 release or not, start your day with eggs and other protein-rich foods. Breakfast staples like eggs, milk, peanut butter toast, protein smoothies, quinoa porridge, and Greek yogurt with fruit provide essential nutrients and support healthy living, while also helping to regulate blood sugar levels and keep you fuller for longer. 2. Nuts as a nutritious snack Nuts are a delicious, nutritious snack that promotes a healthy diet. Nuts are said to boost GLP-1, but what do we actually know? The evidence is
conflicting: the study Nuts have been shown to increase GLP-1 levels, but another study Consuming nuts has been shown to decrease GLP-1 levels. Larger studies in different populations are needed to determine for sure whether nuts increase GLP-1. The good news? Nuts are a great source of protein, healthy fats, and dietary fiber. Eating nuts improves the quality of your diet, and a healthy diet leads to weight loss and a healthy weight. So, regardless of their effect on GLP-1, adding nuts to your diet is likely a nutritional boost. 3. High-Fiber Grains Stimulate GLP-1 Production Take it every day High Fiber Grains Stimulates natural GLP-1 production: Grains rich in soluble fiber, such as oats, barley, and rye, may promote the release of GLP-1, which may help manage blood sugar levels, improve insulin sensitivity, and promote digestive health. Replacing refined grains with high-fiber whole grains can also help. Weight loss Travel and improve your overall health. Many people believe they are meeting the recommended amount of dietary fiber, but in fact they are not getting enough. Most adults Women should aim to consume 25 grams of fiber per day, and men 38 grams. To get a better idea of how much fiber you're actually consuming, track your food intake with MyFitnessPal. Tracking your food can help you reach your nutritional goals. 4. Magnesium supplements to stabilize blood sugar levels magnesium is an essential mineral that has many health benefits. But most importantly, it helps maintain healthy blood sugar levels. In a study of diabetic rats, Magnesium supplements It promotes the release of GLP-1, regulates glucose metabolism, and improves insulin sensitivity, but there is a lack of human studies on the subject. Still, magnesium is an important nutrient that has health benefits beyond its potential effect on GLP-1 release. You can increase your dietary magnesium intake by enjoying foods such as spinach, leafy greens, nuts, peas, beans, whole grains and seeds, or by taking a magnesium supplement. 5. Eat lean protein to increase GLP-1 and maintain muscle mass Lean proteins such as chicken, fish, and tofu may help boost GLP-1 levels. Protein-rich foods It is rich in amino acids that promote the release of GLP-1, which may help preserve muscle mass and aid in weight management. Adding lean protein to your diet may help boost natural GLP-1 levels, stabilize blood sugar levels, and keep muscles healthy. Conclusion Including eggs, nuts, high fiber grains, magnesium supplements and lean protein in your diet can help support your overall health. These nutrient-rich foods contribute to a balanced diet and can help support the release of GLP-1, helping you maintain a healthy weight. Although we are still studying how these nutrient-rich foods affect GLP-1, we know that they can improve the quality of your diet, leading to weight loss and maintaining a healthy weight, so there’s no harm in including them in your diet. Food tracking tools My Fitness Pal Adopting a holistic approach to health is key to supporting your health journey. By making conscious food choices and incorporating natural GLP-1 alternatives, you can create a sustainable lifestyle that prioritizes your health. Whether your goal is to lose a little weight or simply improve your health, remember that small changes add up to big results, so start your journey to a healthier you, one step at a time.
0 notes
Text
What Are My Options for Type 2 Diabetes Medications?
There are different types, or classes, of medications that work in different ways to lower blood glucose (also known as blood sugar) levels. Some options are taken by mouth and others are injected. Some of the commonly used classes of non-insulin medications include:
Metformin
Dipeptidyl peptidase 4 (DPP-4) inhibitors
Glucagon-like peptide 1 (GLP-1) and dual GLP-1/gastric inhibitory peptide (GIP) receptor agonists
Sodium-glucose cotransporter 2 (SGLT2) inhibitors
Sulfonylureas
Thiazolidinediones (TZDs)
Metformin
Metformin (Glucophage) is classified as a biguanide medication and is the only available medication in this class. Metformin lowers blood glucose levels primarily by decreasing the amount of glucose produced by the liver. Metformin also helps lower blood glucose levels by making muscle tissue more sensitive to insulin so blood glucose can be used for energy.
It is usually taken two times a day. A side effect of metformin may be diarrhea, but this is improved when the drug is taken with food.
DPP-4 Inhibitors
DPP-4 inhibitors help improve A1C (a measure of average blood glucose levels over two to three months) without causing hypoglycemia (low blood glucose). They work by preventing the breakdown of naturally occurring hormones in the body, GLP-1 and GIP. These hormones reduce blood glucose levels in the body, but they are broken down very quickly so it does not work well when injected as a drug itself.
By interfering in the process that breaks down GLP-1 and GIP, DPP-4 inhibitors allow these hormones to remain active in the body longer, lowering blood glucose levels only when they are elevated. DPP-4 inhibitors do not cause weight gain and are usually very well tolerated.
There are four DPP-4 inhibitors currently on the market in the U.S.:
Alogliptin (Nesina)
Linagliptin (Tradjenta)
Saxagliptin (Onglyza)
Sitagliptin (Januvia)
GLP-1 and Dual GLP-1/GIP Receptor Agonists
As noted in the description for DPP-4 inhibitors, GLP-1 and GIP are natural hormones in the body that help maintain glucose levels. Use of GLP-1 and dual GLP-1/GIP receptor agonists is another strategy to help use these hormones to improve blood glucose management in people with type 2 diabetes.
These medications have similar effects to the GLP-1 and GIP produced in the body but are resistant to being broken down by the DPP-4 enzyme. These medications can result in large benefits on lowering blood glucose and body weight. Some agents in this class have also been shown to prevent heart disease. Most of these medications are injected, with the exception of one that is taken by mouth once daily, called semaglutide (Rybelsus).
Injectable GLP-1 receptor agonists currently on the market include:
Dulaglutide (Trulicity)
Exenatide (Byetta)
Exenatide extended-release (Bydureon)
Liraglutide (Victoza)
Lixisenatide (Adlyxin)
Injectable semaglutide (Ozempic)
One dual GLP-1/GIP receptor agonist is currently on the market called tirzepatide (Mounjaro). How often you need to inject these medications varies from twice daily to once weekly, depending on the medication. The most common side effect with these medications is nausea and vomiting, which is more common when starting or increasing the dose.
SGLT2 Inhibitors
Glucose in the bloodstream passes through the kidneys where it can either be excreted in the urine or reabsorbed back into the blood. Sodium-glucose cotransporter 2 (SGLT2) works in the kidney to reabsorb glucose. A new class of medication, SGLT2 inhibitors, block this action, causing excess glucose to be eliminated in the urine.
By increasing the amount of glucose excreted in the urine, people can see improved blood glucose, some weight loss, and small decreases in blood pressure. Bexagliflozin (Brenzavvy), canagliflozin (Invokana), dapagliflozin (Farxiga), and empagliflozin (Jardiance) are SGLT2 inhibitors that have been approved by the Food and Drug Administration (FDA) to treat type 2 diabetes. SGLT2 inhibitors are also known to help improve outcomes in people with heart disease, kidney disease, and heart failure.
For this reason, these medications are often used in people with type 2 diabetes who also have heart or kidney problems. Because they increase glucose levels in the urine, the most common side effects include genital yeast infections.
Sulfonylureas
Sulfonylureas have been in use since the 1950s and they stimulate beta cells in the pancreas to release more insulin. There are three main sulfonylurea drugs used today, glimepiride (Amaryl), glipizide (Glucotrol and Glucotrol XL), and glyburide (Micronase, Glynase, and Diabeta). These drugs are generally taken one to two times a day before meals.
All sulfonylurea drugs have similar effects on blood glucose levels, but they differ in side effects, how often they are taken, and interactions with other drugs. The most common side effects with sulfonylureas are low blood glucose and weight gain.
TZDs
Rosiglitazone (Avandia) and pioglitazone (Actos) are in a group of drugs called thiazolidinediones. These drugs help insulin work better in the muscle and fat and reduce glucose production in the liver.
A benefit of TZDs is that they lower blood glucose without having a high risk for causing low blood glucose. Both drugs in this class can increase the risk for heart failure in some individuals and can also cause fluid retention (edema) in the legs and feet.
0 notes
Text
When Is Paintless Dent Removal (Pdr) The Right Choice?

We truly realize that economy is and also well, we all are all trying in order to a sale! Just because the economy is bad doesn't implies that we should neglect our responsibilities which we already have. One of those responsibilities is our vehicles. It will pay that we maintain them and make the extra effort of auto body repairs that are needed. So, just because our economy is looking bad does not imply your vehicle should look bad just too! There are a regarding things could possibly do to get your vehicle looking great and still keep funds in your savings.
The main advantage of this method that it leaves embrace paint in place, taking out the job of finding exact match paint for a re-spray. Another advantage of applying this method has sucralose removes risks of bydureon of mistakes in repainting the damaged area, merely in eliminating as mentioned above but also the possibility more than spraying onto other regarding the car.
How is PDR accomplished? Damage is fixed by removing a panel that exhibits the wrong doing. The service person will then push it back into proper positioning with a specialized package. Panels are accessed through window openings or along the trim. The tech will tap and rub this particular are until it pops back into place.
A repair service may often keep car for a few of days, especially when are stored with appointments or that they are short on staff. If you don't possess another vehicle, you'll upward taking public transportation, renting a vehicle, or bumming a ride from a friend. This is when you actually use a service that focuses primarily on mobile car dent patch up. Bridgend, Cardiff, and Swansea, too as the encompassing area, could be a real pain inside your don't have your own transportation! To ensure that it makes sense to use a mobile service if an individual one with your area.
Collect information about how many paintless dent removal technicians are usually in your area and how are they operating within your potential sell off. What are the charges for their services the kind a relation does your competition have with your amount of potential market as well. Note all these things down for reference.
Income can increase hugely. I started in PDR making no more than $25,000 a full year. This month, I met some hail techs who will generate over $350,000 in income. Individual income will be above $100k this same year. Not bad for a non-college grad.
Since it's fairly in order to find tell that genuine and who is not, key of acquiring that desirable bargain end up being to buy just the car near a price you are happy featuring. If you do single pound per week you can bring yourself a pat about the back.
0 notes
Text
Diabetics face critical medicine shortages as their drugs are snapped up for weight loss treatment
Many of Britain’s 4.3 million registered diabetics face a critical medication shortage as their treatments are snapped up by dieters trying the latest trend – weight loss jabs. A leading testing expert says the UK’s diabetes epidemic means that key drugs should be saved for patients who critically depend on them. Wonder weight loss treatment drugs ‘Wonder’ weight loss drugs, such as Wegovy, have hit the headlines in recent weeks. They can help people shed 10%-15% of their bodyweight, largely by supressing their appetite. However, some of these weight loss jabs are based on semaglutide, first developed for treating type 2 diabetes. This means the boom in demand for ‘magic bullet’ weight loss jabs is contributing to a major shortage in key diabetes medication, says a leading expert. Leading blood testing expert, Dr Avinash Hari Narayanan (MBChB), Clinical Lead at London Medical Laboratory, says: ‘There is now a global shortage of semaglutide-based drugs for treating diabetes. Key among these is Wegovy’s sister drug, Ozempic, used by the NHS as a treatment for managing blood glucose levels in people with type 2 diabetes, which accounts for 90% of all diabetes cases in the UK. This will result in both acute and chronic medical complications if left unmanaged. ‘Both Wegovy and Ozempic are produced by the Danish pharmaceutical giant Novo Nordisk. The problem is that Ozempic has increasingly been prescribed off label (outside of its approved licence) for weight loss as an alternative to Wegovy. Now Novo Nordisk is warning of shortages of Ozempic stretching into 2025. ‘Ozempic and Wegovy became a social media phenomenon earlier this year as a weight loss cure, with demand for semaglutide spiralling after celebrity endorsements. That’s not what Ozempic was intended for and has resulted in demand far outstripping supply. Now Novo Nordisk’s official weight loss drug, Wegovy, is finally available in the UK on the NHS and as a private prescription. However, though this will relieve the demand on critical Ozempic stocks, supplies of all semaglutide-based treatments remain limited. Patients being treated for type 2 diabetes need to know that there are sufficient stocks of this treatment and, if not, patients need a plan to mitigate against supply disruptions. ‘Novo Nordisk now has a market cap of $419.79bn, making it the world's 17th most valuable company. Astonishingly, the market value of the Danish company has exceeded the size of Denmark’s domestic economy (£395.40bn). We are keen for Novo Nordisk to continue concentrating on the production of vital diabetes treatments, over other semaglutide-based products. The company has stated that it will prioritise treatments for existing patients, rather than focusing on introducing new people to Wegovy weight loss treatments. ‘We support Diabetes UK in urging clinicians to follow Department for Health and Social Care guidance, which states clinicians should not prescribe these drugs outside of their licensed use until the supply issues are rectified. ‘It’s not only in the UK that restricted supplies are causing problems; there’s a worldwide shortage. America’s FDA lists Wegovy and certain Ozempic dosages as being in short supply. So too does Australia’s Therapeutic Goods Administration (TGA), which says supplies of Ozempic will remain limited to diabetes treatments only until at least the end of December 2023, and that patients prescribed Ozempic for other conditions should contact their doctor to have their treatment reassessed. ‘The shortage doesn’t only impact on semaglutide-based drugs. All “GLP-1 analogues”, as this family of drugs are known, are in short supply. These include the brands Ozempic, Rybelsus, Trulicity, Victoza, Saxenda, Byetta and Bydureon. This appears to be pan-market disruption, complicated by exceeding demands. ‘All these drugs: - signal to your body to make more insulin (the hormone that controls the amount of sugar in your blood) - reduce the amount of glucose (gluconeogenesis) that your liver makes - slow down the digestion of food, so that it takes longer for your body to absorb the sugar from meals - reduce your appetite by increasing satiety ‘It’s the final effect that has created this unexpected surge in demand. However, there is some welcome news of another GLP-1 analogue drug just about to reach the UK. The National Institute for Health and Care Excellence (NICE) has approved the use of tirzepatide (brand name Mounjaro) for treating type 2 diabetes in England and Wales. Supplies of this new drug should come on stream within three months. ‘Again, it’s vital this new medication is prioritised as a further treatment for type 2 diabetes, rather than for other purposes. It, too, is likely to be in hot demand by people seeking to lose weight the easy way. In the US, clinical weight loss trials show Mounjaro is even more effective than Ozempic, with patients achieving 26.6% weight loss over 84 weeks. ‘By 2030, diabetes cases in the UK will have risen by 50% compared to 2007 levels, according to Diabetes UK. Unmanaged or undiagnosed diabetes is one of the leading causes of mortality. Diabetes is usually linked to factors such as weight, lifestyle, age and family history. One in ten people will have diabetes by the end of the next decade, and one in three will be at a much increased risk of developing it. The truly frightening thing is that it is quite common for people to have diabetes and not know about it. ‘Fortunately, there is a simple blood test that will categorically confirm whether or not you have type 2 diabetes – even in the earliest stages, long before any symptoms have developed. This home test checks your levels of HbA1c. This biomarker is used to confirm whether you have (or are at risk of developing) diabetes. For anyone who already knows they have diabetes, regular HbA1c checks are also essential to monitor progress. ‘London Medical Laboratory’s “Diabetes - Diagnosis and Monitoring test” can be taken at home through the post, or at one of the many drop-in clinics that offer these tests across London and nationwide in over 95 selected pharmacies and health stores. For full details, see: https://www.londonmedicallaboratory.com/product/diabetes-check Photo by Total Shape on Unsplash Read the full article
0 notes
Text
Diabetes. Infarmed autoriza medicamento estrangeiro para evitar rutura
A Autoridade Nacional do Medicamento (Infarmed) autorizou a utilização do fármaco Bydureon, indicado para pessoas com diabetes, com rotulagem em língua estrangeira para evitar rutura de stock em Portugal.

"Com o intuito de evitar a ocorrência de uma rutura de stock, o Infarmed autorizou, a título excecional, a utilização" do Bydureon (com a Denominação Comum Internacional de Exenatido), mantendo a comparticipação de 90% do Serviço Nacional de Saúde, adianta uma circular informativa hoje divulgada.
Este medicamento é indicado para adultos, adolescentes e crianças a partir dos 10 anos com diabetes tipo 2 para melhorar o controlo glicémico, em combinação com outros fármacos hipoglicemiantes.
Segundo o regulador nacional, para facilitar a acessibilidade dos utentes, o "número de registo e o preço desta apresentação será o mesmo do medicamento autorizado em Portugal, pelo que a prescrição e dispensa poderão ocorrer conforme habitual".
Este medicamento da farmacêutica AstraZeneca AB é administrado por injeção e tem um preço de venda de 96,73 euros.
As embalagens do Bydureon com rotulagem em italiano serão acompanhadas por um folheto informativo em português.
Cabe ao Infarmed monitorizar diariamente a informação sobre as faltas, as ruturas e as cessações de comercialização, no sentido de identificar e evitar situações críticas que possam afetar a disponibilidade dos medicamentos.
De acordo com o último relatório sobre a gestão da disponibilidade de medicamentos, em 2021 o Infarmed concedeu 77 autorizações de comercialização em língua estrangeira, uma redução face às 83 de 2020.
Além disso, em 2021 foram proibidos 3.152 pedidos de exportação de medicamentos que apresentavam problemas de disponibilidade em Portugal.
0 notes
Photo

Learn about the Bydureon pen at https://bydureonguide.com
4 notes
·
View notes
Photo
Check out https://bydureonguide.com/does-bydureon-cause-weight-loss/ about bydureon for weight loss in non diabetics.
1 note
·
View note
Photo
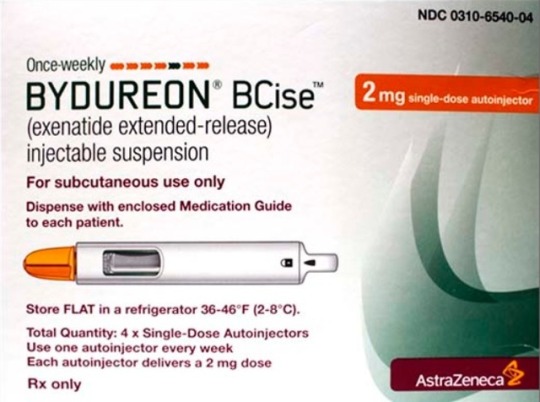
Bydureon pen ultimate guide: https://bydureonguide.com/
1 note
·
View note
Photo

My new #diabetes #medication is called #bydureon to lower my #bloodsugar #bloodsugarlevels - the #bydureounpen is #huge but I’m #thankfull the needle is fairly small. I have to #inject myself once a week and my #bsl is lowering, which is great! My #health is improving. I registered as over 31 mmol or 558 mg/dl - which is WAY too high! I could have died and was rushed straight to #hospital where I learned about Bydureon and agreed to the weekly #selfinjection schedule. When I got out of hospital I spent all my food budget on healthy, low carb, low sugar foods such as salad items, vegetables, diabetic ice cream and lollies. I’ve stopped drinking #pepsimax and switched to #water with #lemonjuice or #icedtea made from #lemonsorbet #tea from #t2 @t2tea or #earlgrey #earlgreytea without milk but no #sugar I love plain #greekyoghurt with #berries such as #blackberries #raspberries and some #kiwifruit in moderation. Also bought lots of protein such as #chicken #lamb #beef #prawns and @colessupermarkets #sausages with #apple and #cider - #yummy #delicious #nom #nomnom #watchthisspace #diabetesmedicine #type2diabetes #myhealthjourney #myhealth (at An Instant On The Lips) https://www.instagram.com/p/Buy_z0lHZOO/?utm_source=ig_tumblr_share&igshid=11v2j2z2tt4lf
#diabetes#medication#bydureon#bloodsugar#bloodsugarlevels#bydureounpen#huge#thankfull#inject#bsl#health#hospital#selfinjection#pepsimax#water#lemonjuice#icedtea#lemonsorbet#tea#t2#earlgrey#earlgreytea#sugar#greekyoghurt#berries#blackberries#raspberries#kiwifruit#chicken#lamb
0 notes
Photo

Can Bydureon make you lose weight even if you are non-diabetic? Find out here:
https://bydureonguide.com/does-bydureon-cause-weight-loss/
0 notes
Photo

New to the bydureon pen? Learn everything about Bydureon here at: https://bydureonguide.com
0 notes
Note
I saw your post about IIH from October. I have IIH too, diagnosed in 2020. I was considering a shunt, but decided to try exenatide as a last resort since the US govt gave it orphan drug status for IIH and clinical trials were promising. I take Bydureon injections once a week (4 months now) and it has done wonders for me - I can work full time and I'm planning on going back to school. it's expensive and I had to jump through a lot of hoops, but it's made my life liveable. my IIH is still there but I can function now.
Exenatide is usually sold as Byetta in NZ.
And I don't qualify for it under our health system unless I also have diabetes or prediabetes. I cannot afford it unfunded even if I find a Doc willing to try it as an off-label use med for IIH.
What's funny (read: infuriating) is that if I asked about it in relation to weight loss it's possible that I might be fully funded under that category.
I am trialing a CBD product currently and it seems to reduce my tinnitus, eye pain, head, neck, and upper back pain, light sensitivity, etc so it might be working to both reduce pain and pressure. And I've managed to finish 3 hardcopy books and a few ebooks in the last fortnight or so.
But I'm not anywhere near being able to study or work, yet.
Once this trial is finished it (beyetta) might be my step, treatment-wise.
2 notes
·
View notes
Text
Bydureon: ¿puede tomarse durante el embarazo?
Mujeres en edad fértil y bydureon pluma
Debido al largo periodo de eliminación de exenatida de liberación prolongada, las mujeres en edad fértil deben utilizar un método anticonceptivo durante el tratamiento con exenatida de liberación prolongada. Este medicamento debe suspenderse al menos 3 meses antes de un embarazo planificado.
Embarazo
Los datos sobre el uso de exenatida de liberación prolongada en mujeres embarazadas son inadecuados. Los estudios en animales han demostrado la toxicidad para la reproducción (véase la sección 5.3). Se desconoce el riesgo potencial para los seres humanos. La exenatida de liberación prolongada no debe utilizarse durante el embarazo y se recomienda el uso de insulina.
Lactancia materna
No se sabe si la exenatida se excreta en la leche materna. Exenatida de liberación prolongada no debe utilizarse durante la lactancia.
Fertilidad
No se han realizado estudios de fertilidad en humanos.
¡He tomado demasiado! ¿Qué hacer? También puede ocurrir que, por error o distracción, tome más medicamentos de los que le ha recetado su médico.
A veces ocurre que los niños pequeños se tragan juguetonamente los medicamentos dejados a su alcance. Siempre recomendamos que los medicamentos se guarden fuera del alcance de los niños, en un lugar cerrado y seguro.
¿Qué debo hacer si accidentalmente tomo demasiado Bydureon?
Sea cual sea la causa de la ingestión de una cantidad excesiva de medicamento, esto es lo que dice la ficha técnica de Bydureon en caso de sobredosis.
Bydureon: Sobredosis Los efectos de la sobredosis con exenatida (basados en estudios clínicos con exenatida de liberación inmediata) incluyen náuseas graves, vómitos intensos y un rápido descenso de la glucosa en sangre. En caso de sobredosis, debe iniciarse un tratamiento de apoyo adecuado en función de los signos y síntomas clínicos experimentados por el paciente.
Bydureon: Instrucciones especiales La pluma precargada es de un solo uso.
Los pacientes y el personal no sanitario deben ser instruidos por un profesional de la salud.
La pluma BCise debe sacarse de la nevera y dejarse reposar en posición horizontal durante al menos 15 minutos antes de la inyección. La suspensión debe mezclarse agitando enérgicamente durante al menos 15 segundos. La suspensión debe ser inspeccionada visualmente antes de su uso. La suspensión sólo debe utilizarse si está mezclada uniformemente, de color blanco a blanquecino y turbia, sin polvo blanco visible a lo largo del lateral, el fondo o la parte superior de la ventana de la pluma.
1 note
·
View note