#but the real issue. is if any of the humans/mers know if the mutation thing is still in the water
Explore tagged Tumblr posts
Note
Radioactive plants O\____________/O
Exactly.
Mutated sharks in the waters? Well guess what, the plants aren’t exempt from whatever went Wrong either, hehehehehehe >:)
OOOOOOOO wait wait wait. WAIT. Started writing this in the tags but no, i gotta move it up here too.
So like. Y’all remember how Jazz doesn’t remember what the ocean is like anymore, but remembers enough to know the waters in his tank are Wrong and Bad?
Hehehehe, IF whatever caused the mutation is still in the waters, if it is making the creatures and plants be unnatural, would Jazz even notice?
Jazz is finally free from the tank and back in the open ocean, the ocean came to HIM, he is free now, and he’s having a great time and he’s like “whoa!! I’ve missed these waters so much, they’re so different from the tank waters, it’s so much better! I’ve missed this, I feel so alive, it’s like my blood is singing!” And Prowl is like, “wait no, this is still Wrong, something is wrong, the waters are still wrong.”
Alas, the waters are still Wrong u_u
#apocalyptic ponyo#transformers stuff#merformers#answered asks#my writings#writing ideas#i’m still partial to fucked up and too close moon shenanigans#but yesssssssss the mutation didn’t stop at the sea creatures it includes the sea plants too#:))))) heheheheahahahahaha ooooo wait#is whatever caused the mutation STILL in the water?#who knows maybe not#but the real issue. is if any of the humans/mers know if the mutation thing is still in the water#hehehehehe add a new anxiety on top of. you know. trying to survive a post natural disaster event#(though ‘natural’ is questionable)
308 notes
·
View notes
Text
How Viruses Evolve
https://sciencespies.com/nature/how-viruses-evolve/
How Viruses Evolve

The unusual cases of pneumonia began to appear in midwinter, in China. The cause, researchers would later learn, was a coronavirus new to science. By March, the infection began to spread to other Asian countries and overseas. People were dying, and the World Health Organization issued a global health alert.
But this was 2003, not 2020, and the disease was SARS, not Covid-19. By June, the outbreak was almost gone, with just 8,098 confirmed infections and 774 deaths worldwide. No cases of SARS have been reported since 2004.
Contrast that with the closely related coronavirus that causes Covid-19 today: more than 13,600,000 confirmed cases as of July 16, and more than 585,000 deaths.
Why did SARS go away while today’s coronavirus just keeps on spreading? Why, for that matter, did both these coronaviruses spill over into people at all, from their original bat hosts?
And just as vital as those questions is another: What happens next?
As we face the current pandemic, it will be important to understand how SARS-CoV-2, the virus that causes Covid-19, is likely to evolve in the months and years ahead. It’s possible the virus could lose its lethal character and settle into an evolutionary détente with humanity. It might end up as just another cold virus, as may have happened to another coronavirus in the past. But it could also remain a serious threat or perhaps even evolve to become more lethal. The outcome depends on the complex and sometimes subtle interplay of ecological and evolutionary forces that shape how viruses and their hosts respond to one another.
“One thing you learn about evolution is never to generalize,” says Edward Holmes, an evolutionary virologist at the University of Sydney, Australia, and author of an article on the evolution of emerging viruses in the Annual Review of Ecology, Evolution, and Systematics. “It depends entirely on the biological nuance of the situation.”
Steps to viral success
Many of the scariest viruses that have caused past or current epidemics originated in other animals and then jumped to people: HIV from other primates, influenza from birds and pigs, and Ebola probably from bats. So, too, for coronaviruses: The ones behind SARS (severe acute respiratory syndrome), MERS (Middle East respiratory syndrome) and Covid-19 all probably originated in bats and arrived in people via another, stepping-stone species, likely palm civets, camels and possibly pangolins, respectively.
But making the jump from one species to another isn’t easy, because successful viruses have to be tightly adapted to their hosts. To get into a host cell, a molecule on the virus’s surface has to match a receptor on the outside of the cell, like a key fitting into a lock. Once inside the cell, the virus has to evade the cell’s immune defenses and then commandeer the appropriate parts of the host’s biochemistry to churn out new viruses. Any or all of these factors are likely to differ from one host species to another, so viruses will need to change genetically — that is, evolve — in order to set up shop in a new animal.
Pandemics — disease outbreaks of global reach — have visited humanity many times. Here are examples.

A recent mutation alters the SARS-CoV-2 spike protein to make it less fragile (the altered bits are shown as colored blobs). This added robustness appears to make the virus more infectious. Three sites are shown because the spike protein is composed of three identical subunits that bind together.
(DOE/Los Alamos National Laboratory)
Host switching actually involves two steps, though these can overlap. First, the virus has to be able to invade the new host’s cells: That’s a minimum requirement for making the host sick. But to become capable of causing epidemics, the virus also has to become infectious — that is, transmissible between individuals — in its new host. That’s what elevates a virus from an occasional nuisance to one capable of causing widespread harm.
SARS-CoV-2 shows these two stages clearly. Compared with the virus in bats, both the virus that infects people and a close relative in pangolins carry a mutation that changes the shape of the surface “ spike protein.” The alteration is right at the spot that binds to host cell receptors to let the virus in. This suggests that the mutation first arose either in pangolins or an as yet unidentified species and happened to allow the virus to jump over to people, too.
But SARS-CoV-2 carries other changes in the spike protein that appear to have arisen after it jumped to people, since they don’t occur in the bat or pangolin viruses. One is in a region called the polybasic cleavage site, which is known to make other coronaviruses and flu viruses more infectious. Another appears to make the spike protein less fragile, and in lab experiments with cell cultures, it makes the virus more infectious. The mutation has become more common as the Covid-19 pandemic goes on, which suggests — but does not prove — that it makes the virus more infectious in the real world, too. (Fortunately, though it may increase spread, it doesn’t seem to make people sicker.)
This evolutionary two-step — first spillover, then adaptation to the new host — is probably characteristic of most viruses as they shift hosts, says Daniel Streicker, a viral ecologist at the University of Glasgow. If so, emerging viruses probably pass through a “silent period” immediately after a host shift, in which the virus barely scrapes by, teetering on the brink of extinction until it acquires the mutations needed for an epidemic to bloom.
Streicker sees this in studies of rabies in bats — which is a good model for studying the evolution of emerging viruses, he says, since the rabies virus has jumped between different bat species many times. He and his colleagues looked at decades’ worth of genetic sequence data for rabies viruses that had undergone such host shifts. Since larger populations contain more genetic variants than smaller populations do, measuring genetic diversity in their samples enabled the scientists to estimate how widespread the virus was at any given time.
The team found that almost none of the 13 viral strains they studied took off immediately after switching to a new bat species. Instead, the viruses eked out a marginal existence for years to decades before they acquired the mutations — of as yet unknown function — that allowed them to burst out to epidemic levels. Not surprisingly, the viruses that emerged the fastest were those that needed the fewest genetic changes to blossom.
SARS-CoV-2 probably passed through a similar tenuous phase before it acquired the key adaptations that allowed it to flourish, perhaps the mutation to the polybasic cleavage site, perhaps others not yet identified. In any case, says Colin Parrish, a virologist at Cornell University who studies host shifts, “by the time the first person in Wuhan had been identified with coronavirus, it had probably been in people for a while.”
It was our bad luck that SARS-CoV-2 adapted successfully. Many viruses that spill over to humans never do. About 220 to 250 viruses are known to infect people, but only about half are transmissible — many only weakly — from one person to another, says Jemma Geoghegan, an evolutionary virologist at the University of Otago, New Zealand. The rest are dead-end infections. Half is a generous estimate, she adds, since many other spillover events probably fizzle out before they can even be counted.
Getting nicer — or nastier
SARS-CoV-2, of course, is well past the teetering stage. The big question now is: What happens next? One popular theory, endorsed by some experts, is that viruses often start off harming their hosts, but evolve toward a more benign coexistence. After all, many of the viruses we know of that trigger severe problems in a new host species cause mild or no disease in the host they originally came from. And from the virus’s perspective, this theory asserts, hosts that are less sick are more likely to be moving around, meeting others and spreading the infection onward.
“I believe that viruses tend to become less pathogenic,” says Burtram Fielding, a coronavirologist at the University of the Western Cape, South Africa. “The ultimate aim of a pathogen is to reproduce, to make more of itself. Any pathogen that kills the host too fast will not give itself enough time to reproduce.” If SARS-CoV-2 can spread faster and further by killing or severely harming fewer of the people it infects, we might expect that over time, it will become less harmful — or, as virologists term it, less virulent.
This kind of evolutionary gentling may be exactly what happened more than a century ago to one of the other human coronaviruses, known as OC43, Fielding suggests. Today, OC43 is one of four coronaviruses that account for up to a third of cases of the common cold (and perhaps occasionally more severe illness). But Fielding and a few others think it could also have been the virus behind a worldwide pandemic, usually ascribed to influenza, that began in 1890 and killed more than a million people worldwide, including Queen Victoria’s grandson and heir.

After rabbits were introduced to Australia, their population exploded. “They are very plentiful here,” says the handwritten inscription on the back of this postcard from around 1930. Scientists eventually introduced the myxoma virus to control the rabbit plague.
(Photographer Paul C. Nomchong / National Museum of Australia)
Scientists can’t prove that, because no virus samples survive from that pandemic, but some circumstantial evidence makes the case plausible, Fielding says. For one thing, people who were infected in the 1890 pandemic apparently experienced nervous-system symptoms we now see as more typical of coronaviruses than of influenza. And when Belgian researchers sequenced OC43’s genome in 2005 and compared it to other known coronaviruses, they concluded that it likely originated as a cattle virus and may have jumped to people right around 1890. They speculated that it may have caused the 1890 pandemic and then settled down to a less nasty coexistence as an ordinary cold virus.
Other evolutionary biologists disagree. The pandemic certainly faded as more people became immune, but there’s no solid evidence that OC43 itself evolved from highly virulent to mostly benign over the last century, they say. Even if it did, that does not mean SARS-CoV-2 will follow the same trajectory. “You can’t just say it’s going to become nicer, that somehow a well-adapted pathogen doesn’t harm its host. Modern evolutionary biology, and a lot of data, shows that doesn’t have to be true. It can get nicer, and it can get nastier,” says Andrew Read, an evolutionary microbiologist at Penn State University. (Holmes is blunter: “Trying to predict virulence evolution is a mug’s game,” he says.)
To understand why it’s so hard to predict changes in virulence, Read says it’s important to recognize the difference between virulence — that is, how sick a virus makes its host — and its transmissibility, or how easily it passes from one host individual to another. Evolution always favors increased transmissibility, because viruses that spread more easily are evolutionarily fitter — that is, they leave more descendants. But transmissibility and virulence aren’t linked in any dependable way, Read says. Some germs do just fine even if they make you very sick. The bacteria that cause cholera spread through diarrhea, so severe disease is good for them. Malaria and yellow fever, which are transmitted by mosquitos, can spread just fine even from a person at death’s door.

Funeral for a U.S. soldier who died of influenza in Russia in 1919. The 1918-1920 pandemic killed an estimated 50 million people worldwide.
(U.S. National Archives)
Respiratory viruses, like influenza and the human coronaviruses, need hosts that move around enough to breathe on one another, so extremely high virulence might be detrimental in some cases. But there’s no obvious evolutionary advantage for SARS-CoV-2 to reduce its virulence, because it pays little price for occasionally killing people: It spreads readily from infected people who are not yet feeling sick, and even from those who may never show symptoms of illness. “To be honest, the novel coronavirus is pretty fit already,” Geoghegan says.
Nor are there many documented instances of viruses whose virulence has abated over time. The rare, classic example is the myxoma virus, which was deliberately introduced to Australia in the 1950s from South America to control invasive European rabbits. Within a few decades, the virus evolved to reduce its virulence, albeit only down to 70 to 95 percent lethality from a whopping 99.8 percent. (It has since ticked up again.)
But myxoma stands nearly alone, Parrish says. For instance, he notes, there is no evidence that recent human pathogens such as Ebola, Zika or chikungunya viruses have shown any signs of becoming less pathogenic in the relatively short time since jumping to humans.
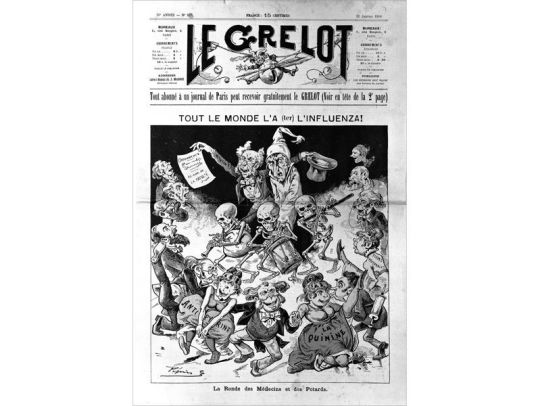
“Everyone has influenza,” reads a headline in a French publication from January 1890.
(Wellcome Collection via CC by 4.0)
The ones that went away
The faded nightmares of our past — pandemics that terrorized, then receded, such as SARS in 2003 and flu in 1918-20 and again in 1957, 1968 and 2009 — went away not because the viruses evolved to cause milder disease, but for other reasons. In the case of SARS, the virus made people sick enough that health workers were able to contain the disease before it got out of hand. “People who got SARS got very sick, very fast and were easily identified, easily tracked and readily quarantined — and their contacts were also readily identified and quarantined,” says Mark Cameron, an immunologist at Case Western Reserve University in Cleveland, who worked in a Toronto hospital during the height of the SARS outbreak there. That was never going to be as easy to do for Covid-19 because people who don’t show symptoms can spread the virus.
Flu pandemics, meanwhile, have tended to recede for another reason, one that offers more hope in our present moment: Enough of the population eventually becomes immune to slow the virus down. The H1N1 influenza virus that caused the 1918 pandemic continued as the main influenza virus until the 1950s, and its descendants still circulate in the human population. What made the virus such a threat in 1918-20 is that it was novel and people had little immunity. Once much of the population had been exposed to the virus and had developed immunity, the pandemic waned, although the virus persisted at a lower level of infections — as it does to this day. It appears less lethal now largely because older people, who are at greatest risk of dying from influenza, have usually encountered H1N1 influenza or something like it at some point in their lives and retain some degree of immunity, Read says.
With the new coronavirus, Parrish says, “we’re sort of in that 1918 period where the virus is spreading fast in a naive population.” But that will change as more people either catch Covid-19 or are vaccinated (if and when that becomes possible) and develop some level of immunity. “There’s no question that once the population is largely immune, the virus will die down,” Parrish says.
The question is how long that immunity will last: for a lifetime, like smallpox, or just a few years, like flu? In part, that will depend on whether the vaccine induces a permanent antibody response or just a temporary one. But it also depends on whether the virus can change to evade the antibodies generated by the vaccine. Although coronaviruses don’t accumulate mutations as fast as flu viruses, they do still change. And at least one, which causes bronchitis in chickens, has evolved new variants that aren’t covered by previous vaccines. But at this point, no one knows what to expect from SARS-CoV-2.
There is, at least, one encouraging aspect to all this. Even if we can’t predict how the virus will evolve or how it will respond to the coming vaccine, there is something all of us can do to reduce the risk of the virus evolving in dangerous ways. And it doesn’t involve any complicated new behaviors. “Viruses can only evolve if they’re replicating and transmitting,” Streicker says. “Anything that reduces the replication of a virus will in consequence reduce the amount of evolution that happens.” In other words, we can do our part to slow down the evolution of the Covid-19 virus by behaving exactly as we’ve been told to already to avoid catching it: Minimize contact with others, wash your hands and wear a mask.
This article originally appeared in Knowable Magazine, an independent journalistic endeavor from Annual Reviews. Sign up for the newsletter.
#Nature
3 notes
·
View notes
Text
AstraZeneca Vaccine: Blood Clot Danger? Think again...
So for those of you who’ve been living under a rock this last year, since November 2019, the threat from COVID-19 has been very real, putting the world into lockdown, wrecking the economy, turned politics into a war-ground and, much closer to home, has led to severe mental health implications for countless people since we’ve all been trapped indoors for over a year.
In Europe, the UK has been spearheading the biggest vaccination program its ever undertaken, with three different vaccines from three big Pharma companies: the Pfizer Vaccine, the Moderna Vaccine and the Oxford-AstraZeneca vaccine.
It’s that final one that is probably the most well-recognised one, given the notoriety it’s gained in the media these last few weeks. Now why is that?
Well, to understand why many are opposed to this COVID-19 vaccine, we need to understand why this vaccine has been surrounded by so much controversy.
At the start of the pandemic, the University of Oxford, in conjunction with AstraZeneca, worked day and night to develop a vaccine quickly because in the early days of the pandemic COVID-19 had not yet begun to mutate into genetically distinct strains. This window of opportunity was critical because SARs-CoV2 is a virus whose genetic material is encoded by RNA rather DNA (like humans) and because of this, the COVID-19 genome is more liable to mutate quickly, as RNA does not come equipped with the ‘proof-reading’ mechanisms that DNA comes with. So, when AstraZeneca had completed the clinical trials, in line with government requirements, the BBC reported that the UK government approved the vaccine on December 30th 2020, after carefully reviewing all the evidence from the trials.
Now at this point, the Pfizer Vaccine had already been approved and, in the South East of England, a new, much faster-spreading variant of COVID-19 had arisen in Kent, because (as we feared) the virus’s genome had mutated in a position in a way that caused the time between when a person was infected and when they became infectious to decrease significantly. This new variant then warranted another lockdown, because it was faster than the original virus and, eventually, it took its place as the new ‘apex predator’.
The AstraZeneca vaccine was rolled out from Monday 4th January 2021 and soon people began to speculate, leading to cruel (and untrue) rumours that the vaccine had been rushed and that the government had waived some of the assessment criteria out of desperation. In fairness, 2020 had been a crazy year, and given the desperate situation, the rumours weren’t totally insane...
But they were still untrue. The BBC released a statement from the University of Oxford which revealed that they had, in fact, been developing a new type of vaccine that was more effective than traditional vaccines since the Ebola crisis ended in 2016. Using this technique, they began studying coronaviruses such as SARs and MERs and had even successfully created one of these new vaccines to target MERs because they had realised that all coronaviruses have a vital weak spot: the spike protein that gives coronaviruses their name. The fact that they were able to develop a vaccine for SARs-Cov2 in 10 months (a process that does take 10 years usually) is because they already had a molecule to target (which usually is why vaccine development takes so long because scientists need to study the virus for longer to learn which physical features it has that would make a good vaccine target) and because of the amount of help they had: Oxford gained a tremendous amount of funding and support across the UK to help in their research centres and take part in their clinical trials.
So to reiterate: the AstraZeneca vaccine’s fast development was not due to cut corners. It was because everyone chipped in. Everyone pulled their weight together giving more time, money, effort and attention than has ever been given to any vaccine before. And instead of recognising the unprecedented amount of co-operation and effort that went into developing this vaccine, all the public could say about it was: “we don’t believe it”.
It didn’t help that the AstraZeneca Vaccine can occasionally cause side-effects in 1 in more than 10 people - which if you think about the number of people in the UK, that is a lot of people who were complaining about side-effects, so unsurprisingly the public learnt about this quickly and immediately rushed to criticise the vaccine further.
However, the side-effects are not severe, as the UK government’s Public assessment of the vaccine summary states, those who’ve had the vaccine’s first dose may feel “tenderness, pain, warmth, itching or bruising where the injection is given, generally feeling unwell, feeling tired (fatigue), chills or feeling feverish, headache, feeling sick (nausea), joint pain or muscle ache”. Or to put it simply, you feel a bit poorly for 1-3 days (maximum) and then you feel fine. You may feel like this because either you are allergic to some of the vaccine serum ingredients - which the nurses will ask before the injection and will take precautions as appropriate - or, the most likely explanation is that it’s just your immune system doing what it’s supposed to be doing.
One thing that is commonly overlooked when it comes to viral infections is that, unlike bacteria - which release toxins to cause cell damage which causes the symptoms of illness - the symptoms experienced when infected with a virus is purely down to your body’s immune response. If you have a temperature, it’s because the hotter your body is, the faster the essential chemical reactions and protein interactions that go into ridding the body of an infection can occur. Symptoms of illness that arise from the AstraZeneca vaccine are no different - your body is just practicing what it would do if it met the actual virus for the first time - once its done that, you will very unlikely suffer any symptoms in the future should you be exposed to the virus again because your body remembers how to deal with an infection and will do it so quickly, you will be virus-free before you can say “achoo”.
So, now that the first myth about the AstraZeneca vaccine has been busted (don’t believe us? Read the listed sources!), let’s talk about the current problem: the blood clot rumour.
So, not to inflame rumours, but yes it has been found that very rarely a blood clot in the brain (Specifically a Cerebral Venous Sinus Thrombosis or CVST) which can be fatal if it goes undetected - the UK’s Medical Regulation body (the MHRA) have reported that in a survey of 79 people (two-thirds women) who had the first dose and suffered a blood clot, 19 people died. However there was not enough evidence to say that the vaccine was the cause of a CVST. Just because something coincided with something, doesn’t mean that it was the cause. The likelihood that the vaccine was the direct cause for a blood clot in these people is further diminished by the fact that CVSTs only affect 5 in 1,000,000 (1 million) people! So those of you who roll your eyes when you hear that “birth control is more likely to give you a blood clot”, it’s true! And on top of that the vaccine has not even been proven to cause blood clots.
So in conclusion, does the vaccine have side-effects? Yes. Are you going to die from them? No. Does the vaccine cause blood clots? There’s not enough evidence to say yes or no, but the type of blood clot that the vaccine has coincided with is so rare, that it shouldn’t be an issue. The bottom line, is that the AstraZeneca vaccine shouldn’t be refused or suspended just because there might be a problem. The MHRA will review the safety and they’ll let us know if they find anything of concern. In the meantime, if people want this pandemic to finally end after nearly 18 months of death and misery then we need to start listening to health professionals and scientists who’ve worked long and tirelessly to return things to normal and trust that they know what they’re doing.
0 notes
Text
To Prevent Next Coronavirus, Stop the Wildlife Trade, Conservationists Say

The coronavirus spreading from China has sickened at least 73,000 people and killed at least 2,000, setting in motion a global health emergency. But humans aren’t the only species infected. Coronaviruses attack a variety of birds and mammals. The new virus seems to have leapt from wildlife to humans in a seafood and meat market in Wuhan, China, where live animals were slaughtered and sold as food. That’s a familiar story. The SARS epidemic, also caused by a coronavirus, began in China with the consumption of a catlike animal called the palm civet. The MERS epidemic began with a coronavirus transmitted to humans from camels in the Middle East. In the spread of yet another coronavirus, conservationists see a public health lesson: If you want to prevent epidemics that begin in animals, halt the global trade in wildlife. “This issue is not just a conservation issue anymore,” said Grace Ge Gabriel, Asia regional director of the International Fund for Animal Welfare. “It’s a public health issue, a biosafety issue and a national security issue.” China is a linchpin in the illegal trade. Last month, as the coronavirus spread, the central government in Beijing issued a nationwide but temporary ban on all trade in wild animals, including their transport and sale in markets, restaurants and via online platforms. The government order warned that officials would “severely investigate and punish” violators and provided a hotline for citizens to report infractions. Officials in Beijing now have drafted legislation to end “the pernicious habit of eating wildlife,” according to a statement released on Monday by the standing committee of the National Peoples Congress. Chinese citizens are “angry because they’ve learned that wildlife traded for food has once again caused a national health crisis, and because a small number of wildlife traders continue to hold the entire country hostage,” said Peter Li, an associate professor of East Asian politics at the University of Houston-Downtown who specializes in China’s domestic policies. Experts still do not know which species transmitted the new coronavirus, technically called SARS-CoV-2, to people. But pangolins, also known as scaly anteaters, are now the leading suspects. The world’s most trafficked mammal, pangolins are barred from international trade and are protected domestically in China. But pangolin meat and blood are considered delicacies on the black market, and sales of their scales for use in traditional Chinese medicine remain legal for certain hospitals and pharmacies. Updated Feb. 10, 2020 What is a Coronavirus? It is a novel virus named for the crown-like spikes that protrude from its surface. The coronavirus can infect both animals and people, and can cause a range of respiratory illnesses from the common cold to more dangerous conditions like Severe Acute Respiratory Syndrome, or SARS. How contagious is the virus? According to preliminary research, it seems moderately infectious, similar to SARS, and is possibly transmitted through the air. Scientists have estimated that each infected person could spread it to somewhere between 1.5 and 3.5 people without effective containment measures. How worried should I be? While the virus is a serious public health concern, the risk to most people outside China remains very low, and seasonal flu is a more immediate threat. Who is working to contain the virus? World Health Organization officials have praised China’s aggressive response to the virus by closing transportation, schools and markets. This week, a team of experts from the W.H.O. arrived in Beijing to offer assistance. What if I’m traveling? The United States and Australia are temporarily denying entry to noncitizens who recently traveled to China and several airlines have canceled flights. How do I keep myself and others safe? Washing your hands frequently is the most important thing you can do, along with staying at home when you’re sick. Whatever the source turns out to be, the new ban on wildlife trade comes too late to stanch the spread of this latest coronavirus. “Now that human-to-human transmission is happening, the ban has no real consequence for this outbreak at all,” said Christian Walzer, executive director of health at the Wildlife Conservation Society. The government’s ban also lasts only until “the epidemic situation is lifted nationwide,” according to the government’s order. Dr. Walzer and others believe that the ban needs to be permanent if it is to have any effect on reducing the risk of future zoonotic diseases. “Otherwise, we’ll be having this conversation at regular intervals,” he said. During the SARS epidemic in 2003, China enacted a narrower wildlife trade ban. Many conservationists and medical professionals, including members of the Chinese Academy of Sciences, hoped it would be permanent, but the trade roared back after the crisis ended. “Once a disease jumps into humans, all the responses are reactive and the focus is on human health,” said Dr. Alonso Aguirre, a wildlife ecologist at George Mason University. After the crisis passes, attention turns away from the trade that brought the disease to humans, he added. Scientists have been calling for permanent restrictions for at least three decades. “We never go back to the source of why these things happen in the first place,” Dr. Aguirre said.
Laboratories for creating new viruses
China and Southeast Asia are hot spots for emerging zoonotic diseases, pathogens that naturally occur in wildlife and find their way to domestic animals and humans through mutation or new contact. Biodiversity loss, combined with high rates of deforestation, raises the risk of these infections by bringing people and livestock into contact with wildlife, and by altering the environment to favor transmission of certain diseases, such as malaria, Zika and dengue. Demand for animals and their parts — to eat or for use in traditional medicine — carries potential pathogens far and wide. But the coronavirus outbreak has not snuffed out demand for wildlife, according to the Environmental Investigation Agency, a nonprofit group based in London that researches and campaigns against environmental crime. Even now, some online sellers in China and Laos are touting illegal traditional medicines containing rhino horn and other animal parts as cures for coronavirus, the group found. Some cite a document issued last month by China’s National Health Commission that lists traditional animal-based remedies as recommended treatments for coronavirus infection. No one knows the full scope of wildlife trade worldwide, but the numbers are staggering — on the order of millions of animals of hundreds of species trafficked each day, according to Vincent Nijman, a wildlife trade researcher at Oxford Brookes University in England. A study published last October in the journal Science estimated that wildlife trade includes 5,600 species, nearly one-fifth of the world’s known vertebrate animals. While some wildlife trade is illegal, much of the hidden industry comprises legal, oftentimes unregulated trade of unprotected species like rodents, bats, snakes and frogs. Wildlife trade in Asia is especially risky to human health, because these animals are often transported and sold live. “Even if one of these jumps is a rare occurrence, there are millions and millions of contacts that occur every day in these types of markets,” said Andres Gomez, an ecologist and veterinarian at ICF International, a global consulting services company based in Virginia. “You’re playing with fire.” Live meat markets are perfect laboratories for creating new viruses. Stressed animals shed more viruses and are more susceptible to infections, and cages are often stacked on top of each other, facilitating exposure. “You have a bird pooping on a turtle that poops on a civet,” Dr. Walzer said. “For getting new viruses to emerge, you couldn’t do it much better even if you tried.” Basic hygiene is usually lacking as well, Dr. Nijman added: “The same chopping block is being used for every piece of meat, the same knife for all species. No one is washing their hands.” Increasingly varied species and populations are mixed at markets. Better transportation — and the fact that many local species have disappeared — means that wildlife is imported from an ever-larger radius. Newer exotic species are frequently introduced for trade, as well. China has approved 54 wild species for commercial breeding and sale, including American red foxes, Australian zebra finches and African ostriches. This diversity was reflected at the market in Wuhan where the new coronavirus originated. A single meat shop there sold live peacocks, rats, foxes, crocodiles, wolf cubs, turtles, snakes, wild pigs and more. “The billboard from that store advertised feet, blood, intestines and other body parts from over 70 species,” said Ms. Gabriel, of the International Fund for Animal Welfare. “It’s staggering.” In Guangdong Province in 2003, these shops were temporarily shuttered as SARS emerged. Wildlife trade and consumption declined in the immediate aftermath, but the business resumed within about a year, despite calls for a permanent ban. “China should not have forgotten the pain after the wound was healed,” Dr. Li said. Some experts believe that a complete ban on wildlife trade is neither necessary nor practical. “Wildlife trade is not some horrific habit people have, something awful that shouldn’t be done,” said Peter Daszak, president of the EcoHealth Alliance, a nonprofit research group in New York City. “It’s a deep-seated part of human culture.” In Western countries, for example, people regularly consume meat caught in the wild, including venison, rabbit and game birds, Dr. Daszak said. Rather than ban all wildlife trade in China, he and other scientists have called for strictly monitored captive-breeding of certain wild species. Additional measures could include a permanent trade ban on certain high-risk species, like bats, and the introduction of “a series of common-sense hygiene and welfare rules,” Dr. Nijman said. Other scientists argue that without a full and permanent ban on wildlife trade, it is only a matter of time until the next virus emerges. “Unless something changes, this is just one in the series,” he said of the current coronavirus epidemic. “We have to decide as a society if we’re comfortable maintaining the risk that the next one is one that kills most people who get infected.” China’s authoritarian government has the power to permanently ban all wildlife trade, Dr. Li noted. But he is not optimistic that it will happen. The country’s wildlife policies are based on “the premise that wildlife is a natural resource to be utilized,” he said, and officials tend to view nature through an economic rather than ecological lens. Banning wildlife trade would require a fundamental shift. “The Chinese government has created an enormous problem for itself by encouraging wildlife use,” Dr. Li said. “Now it must choose whether to favor the economic interests of a small minority, or to favor the public health interests of 1.4 billion Chinese people and the world.” Read the full article
0 notes
Text
To Prevent the Next Coronavirus, Stop the Wildlife Trade
The coronavirus spreading from China has sickened at least 73,000 people and killed at least 2,000, setting in motion a global health emergency. But humans aren’t the only species infected.
Coronaviruses attack a variety of birds and mammals. The new virus seems to have leapt from wildlife to humans in a seafood and meat market in Wuhan, China, where live animals were slaughtered and sold as food.
That’s a familiar story. The SARS epidemic, also caused by a coronavirus, began in China with the consumption of a catlike animal called the palm civet. The MERS epidemic began with a coronavirus transmitted to humans from camels in the Middle East.
In the spread of yet another coronavirus, conservationists see a public health lesson: If you want to prevent epidemics that begin in animals, halt the global trade in wildlife.
“This issue is not just a conservation issue anymore,” said Grace Ge Gabriel, Asia regional director of the International Fund for Animal Welfare. “It’s a public health issue, a biosafety issue and a national security issue.”
China is a linchpin in the illegal trade. Last month, as the coronavirus spread, the central government in Beijing issued a nationwide but temporary ban on all trade in wild animals, including their transport and sale in markets, restaurants and via online platforms.
The government order warned that officials would “severely investigate and punish” violators and provided a hotline for citizens to report infractions. Officials in Beijing now have drafted legislation to end “the pernicious habit of eating wildlife,” according to a statement released on Monday by the standing committee of the National Peoples Congress.
Chinese citizens are “angry because they’ve learned that wildlife traded for food has once again caused a national health crisis, and because a small number of wildlife traders continue to hold the entire country hostage,” said Peter Li, an associate professor of East Asian politics at the University of Houston-Downtown who specializes in China’s domestic policies.
Experts still do not know which species transmitted the new coronavirus, technically called SARS-CoV-2, to people. But pangolins, also known as scaly anteaters, are now the leading suspects.
The world’s most trafficked mammal, pangolins are barred from international trade and are protected domestically in China. But pangolin meat and blood are considered delicacies on the black market, and sales of their scales for use in traditional Chinese medicine remain legal for certain hospitals and pharmacies.
Updated Feb. 10, 2020
What is a Coronavirus? It is a novel virus named for the crown-like spikes that protrude from its surface. The coronavirus can infect both animals and people, and can cause a range of respiratory illnesses from the common cold to more dangerous conditions like Severe Acute Respiratory Syndrome, or SARS.
How contagious is the virus? According to preliminary research, it seems moderately infectious, similar to SARS, and is possibly transmitted through the air. Scientists have estimated that each infected person could spread it to somewhere between 1.5 and 3.5 people without effective containment measures.
How worried should I be? While the virus is a serious public health concern, the risk to most people outside China remains very low, and seasonal flu is a more immediate threat.
Who is working to contain the virus? World Health Organization officials have praised China’s aggressive response to the virus by closing transportation, schools and markets. This week, a team of experts from the W.H.O. arrived in Beijing to offer assistance.
What if I’m traveling? The United States and Australia are temporarily denying entry to noncitizens who recently traveled to China and several airlines have canceled flights.
How do I keep myself and others safe? Washing your hands frequently is the most important thing you can do, along with staying at home when you’re sick.
Whatever the source turns out to be, the new ban on wildlife trade comes too late to stanch the spread of this latest coronavirus.
“Now that human-to-human transmission is happening, the ban has no real consequence for this outbreak at all,” said Christian Walzer, executive director of health at the Wildlife Conservation Society.
The government’s ban also lasts only until “the epidemic situation is lifted nationwide,” according to the government’s order. Dr. Walzer and others believe that the ban needs to be permanent if it is to have any effect on reducing the risk of future zoonotic diseases.
“Otherwise, we’ll be having this conversation at regular intervals,” he said.
During the SARS epidemic in 2003, China enacted a narrower wildlife trade ban. Many conservationists and medical professionals, including members of the Chinese Academy of Sciences, hoped it would be permanent, but the trade roared back after the crisis ended.
“Once a disease jumps into humans, all the responses are reactive and the focus is on human health,” said Dr. Alonso Aguirre, a wildlife ecologist at George Mason University.
After the crisis passes, attention turns away from the trade that brought the disease to humans, he added. Scientists have been calling for permanent restrictions for at least three decades.
“We never go back to the source of why these things happen in the first place,” Dr. Aguirre said.
Laboratories for creating new viruses
China and Southeast Asia are hot spots for emerging zoonotic diseases, pathogens that naturally occur in wildlife and find their way to domestic animals and humans through mutation or new contact.
Biodiversity loss, combined with high rates of deforestation, raises the risk of these infections by bringing people and livestock into contact with wildlife, and by altering the environment to favor transmission of certain diseases, such as malaria, Zika and dengue.
Demand for animals and their parts — to eat or for use in traditional medicine — carries potential pathogens far and wide.
But the coronavirus outbreak has not snuffed out demand for wildlife, according to the Environmental Investigation Agency, a nonprofit group based in London that researches and campaigns against environmental crime.
Even now, some online sellers in China and Laos are touting illegal traditional medicines containing rhino horn and other animal parts as cures for coronavirus, the group found. Some cite a document issued last month by China’s National Health Commission that lists traditional animal-based remedies as recommended treatments for coronavirus infection.
No one knows the full scope of wildlife trade worldwide, but the numbers are staggering — on the order of millions of animals of hundreds of species trafficked each day, according to Vincent Nijman, a wildlife trade researcher at Oxford Brookes University in England.
A study published last October in the journal Science estimated that wildlife trade includes 5,600 species, nearly one-fifth of the world’s known vertebrate animals.
While some wildlife trade is illegal, much of the hidden industry comprises legal, oftentimes unregulated trade of unprotected species like rodents, bats, snakes and frogs. Wildlife trade in Asia is especially risky to human health, because these animals are often transported and sold live.
“Even if one of these jumps is a rare occurrence, there are millions and millions of contacts that occur every day in these types of markets,” said Andres Gomez, an ecologist and veterinarian at ICF International, a global consulting services company based in Virginia. “You’re playing with fire.”
Live meat markets are perfect laboratories for creating new viruses. Stressed animals shed more viruses and are more susceptible to infections, and cages are often stacked on top of each other, facilitating exposure.
“You have a bird pooping on a turtle that poops on a civet,” Dr. Walzer said. “For getting new viruses to emerge, you couldn’t do it much better even if you tried.”
Basic hygiene is usually lacking as well, Dr. Nijman added: “The same chopping block is being used for every piece of meat, the same knife for all species. No one is washing their hands.”
Increasingly varied species and populations are mixed at markets. Better transportation — and the fact that many local species have disappeared — means that wildlife is imported from an ever-larger radius. Newer exotic species are frequently introduced for trade, as well.
China has approved 54 wild species for commercial breeding and sale, including American red foxes, Australian zebra finches and African ostriches.
This diversity was reflected at the market in Wuhan where the new coronavirus originated. A single meat shop there sold live peacocks, rats, foxes, crocodiles, wolf cubs, turtles, snakes, wild pigs and more.
“The billboard from that store advertised feet, blood, intestines and other body parts from over 70 species,” said Ms. Gabriel, of the International Fund for Animal Welfare. “It’s staggering.”
In Guangdong Province in 2003, these shops were temporarily shuttered as SARS emerged. Wildlife trade and consumption declined in the immediate aftermath, but the business resumed within about a year, despite calls for a permanent ban.
“China should not have forgotten the pain after the wound was healed,” Dr. Li said.
Some experts believe that a complete ban on wildlife trade is neither necessary nor practical.
“Wildlife trade is not some horrific habit people have, something awful that shouldn’t be done,” said Peter Daszak, president of the EcoHealth Alliance, a nonprofit research group in New York City. “It’s a deep-seated part of human culture.”
In Western countries, for example, people regularly consume meat caught in the wild, including venison, rabbit and game birds, Dr. Daszak said.
Rather than ban all wildlife trade in China, he and other scientists have called for strictly monitored captive-breeding of certain wild species.
Additional measures could include a permanent trade ban on certain high-risk species, like bats, and the introduction of “a series of common-sense hygiene and welfare rules,” Dr. Nijman said.
Other scientists argue that without a full and permanent ban on wildlife trade, it is only a matter of time until the next virus emerges.
“Unless something changes, this is just one in the series,” he said of the current coronavirus epidemic. “We have to decide as a society if we’re comfortable maintaining the risk that the next one is one that kills most people who get infected.”
China’s authoritarian government has the power to permanently ban all wildlife trade, Dr. Li noted. But he is not optimistic that it will happen.
The country’s wildlife policies are based on “the premise that wildlife is a natural resource to be utilized,” he said, and officials tend to view nature through an economic rather than ecological lens.
Banning wildlife trade would require a fundamental shift.
“The Chinese government has created an enormous problem for itself by encouraging wildlife use,” Dr. Li said. “Now it must choose whether to favor the economic interests of a small minority, or to favor the public health interests of 1.4 billion Chinese people and the world.”
from WordPress https://mastcomm.com/event/to-prevent-the-next-coronavirus-stop-the-wildlife-trade/
0 notes